Acute viral hepatitis.ppt
- Количество слайдов: 22
 Acute Viral Hepatitis
Acute Viral Hepatitis
 Acute viral hepatitis (AVH) – Group of acute inflammatory diseases of the liver parenchyma (mesenchymal), which are caused primary by hepatotropic viruses (HAV, HBV, HDV, HEV, HCV).
Acute viral hepatitis (AVH) – Group of acute inflammatory diseases of the liver parenchyma (mesenchymal), which are caused primary by hepatotropic viruses (HAV, HBV, HDV, HEV, HCV).
 Importance ü AVH are the leading course of acute liver diseases in children, contributing about 80% of all cases. ü Most cases (70%) of HAV are seen among children. ü 70 -80% of adult population have markers of HAV in anamnesis. ü 30% of first year old children with HBV develop acute liver insufficiency; among them, the case fatality rate is about 80%. ü 90% of infants with HBV and 30% of 1 -5 years old children with HBV develop chronic HB ü About 2 billions of people all around the world have markers of HBVinfection in anamnesis, 350 millions have chronic HBV and 1 million dies every year from liver cirrhosis and hepatocellular carcinoma due to HBV infection.
Importance ü AVH are the leading course of acute liver diseases in children, contributing about 80% of all cases. ü Most cases (70%) of HAV are seen among children. ü 70 -80% of adult population have markers of HAV in anamnesis. ü 30% of first year old children with HBV develop acute liver insufficiency; among them, the case fatality rate is about 80%. ü 90% of infants with HBV and 30% of 1 -5 years old children with HBV develop chronic HB ü About 2 billions of people all around the world have markers of HBVinfection in anamnesis, 350 millions have chronic HBV and 1 million dies every year from liver cirrhosis and hepatocellular carcinoma due to HBV infection.
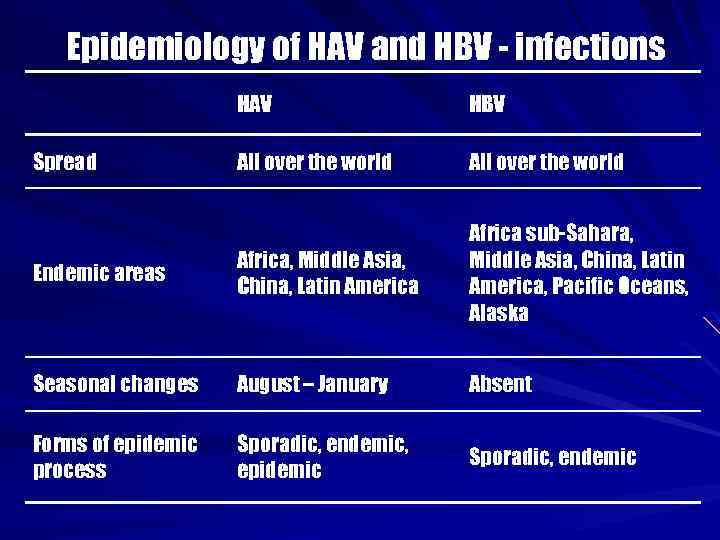 Epidemiology of HAV and HBV - infections HAV HBV All over the world Endemic areas Africa, Middle Asia, China, Latin America Africa sub-Sahara, Middle Asia, China, Latin America, Pacific Oceans, Alaska Seasonal changes August – January Absent Forms of epidemic process Sporadic, endemic, epidemic Sporadic, endemic Spread
Epidemiology of HAV and HBV - infections HAV HBV All over the world Endemic areas Africa, Middle Asia, China, Latin America Africa sub-Sahara, Middle Asia, China, Latin America, Pacific Oceans, Alaska Seasonal changes August – January Absent Forms of epidemic process Sporadic, endemic, epidemic Sporadic, endemic Spread
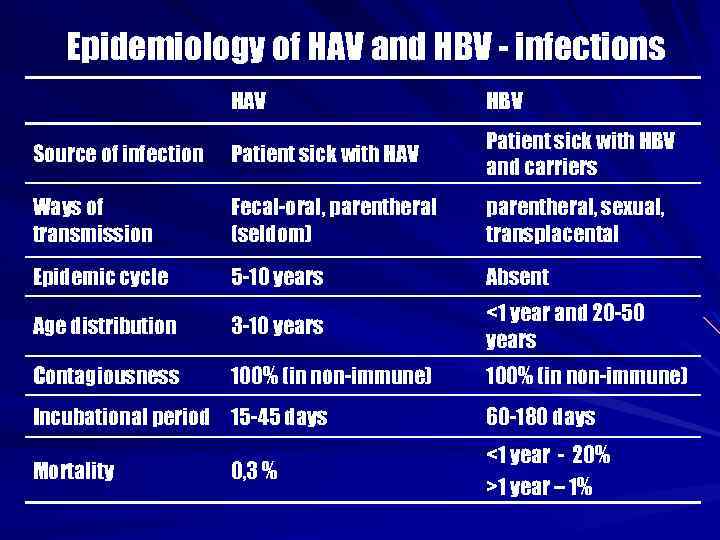 Epidemiology of HAV and HBV - infections HAV HBV Source of infection Patient sick with HAV Patient sick with HBV and carriers Ways of transmission Fecal-oral, parentheral (seldom) parentheral, sexual, transplacental Epidemic cycle 5 -10 years Absent Age distribution 3 -10 years <1 year and 20 -50 years Contagiousness 100% (in non-immune) Incubational period 15 -45 days 60 -180 days Mortality <1 year - 20% >1 year – 1% 0, 3 %
Epidemiology of HAV and HBV - infections HAV HBV Source of infection Patient sick with HAV Patient sick with HBV and carriers Ways of transmission Fecal-oral, parentheral (seldom) parentheral, sexual, transplacental Epidemic cycle 5 -10 years Absent Age distribution 3 -10 years <1 year and 20 -50 years Contagiousness 100% (in non-immune) Incubational period 15 -45 days 60 -180 days Mortality <1 year - 20% >1 year – 1% 0, 3 %
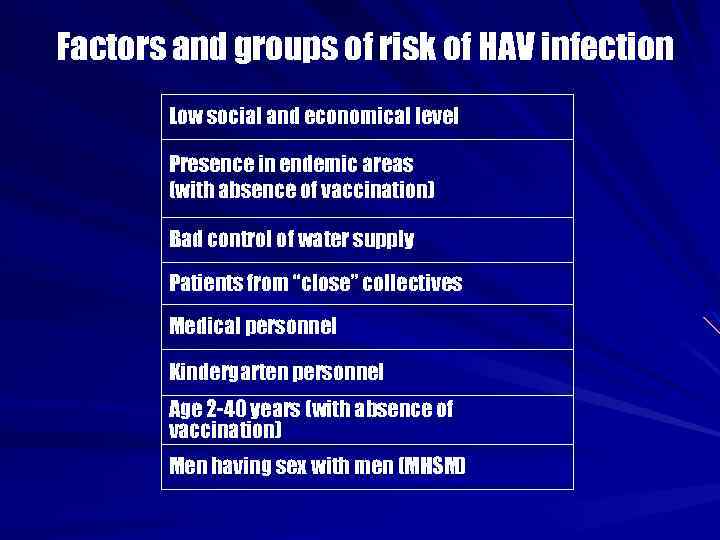 Factors and groups of risk of HAV infection Low social and economical level Presence in endemic areas (with absence of vaccination) Bad control of water supply Patients from “close” collectives Medical personnel Kindergarten personnel Age 2 -40 years (with absence of vaccination) Men having sex with men (MHSM)
Factors and groups of risk of HAV infection Low social and economical level Presence in endemic areas (with absence of vaccination) Bad control of water supply Patients from “close” collectives Medical personnel Kindergarten personnel Age 2 -40 years (with absence of vaccination) Men having sex with men (MHSM)
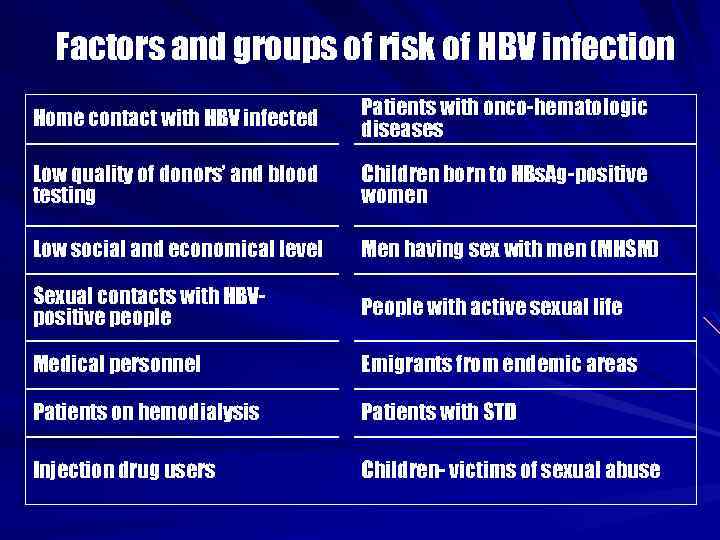 Factors and groups of risk of HBV infection Home contact with HBV infected Patients with onco-hematologic diseases Low quality of donors’ and blood testing Children born to HBs. Ag-positive women Low social and economical level Men having sex with men (MHSM) Sexual contacts with HBVpositive people People with active sexual life Medical personnel Emigrants from endemic areas Patients on hemodialysis Patients with STD Injection drug users Children- victims of sexual abuse
Factors and groups of risk of HBV infection Home contact with HBV infected Patients with onco-hematologic diseases Low quality of donors’ and blood testing Children born to HBs. Ag-positive women Low social and economical level Men having sex with men (MHSM) Sexual contacts with HBVpositive people People with active sexual life Medical personnel Emigrants from endemic areas Patients on hemodialysis Patients with STD Injection drug users Children- victims of sexual abuse
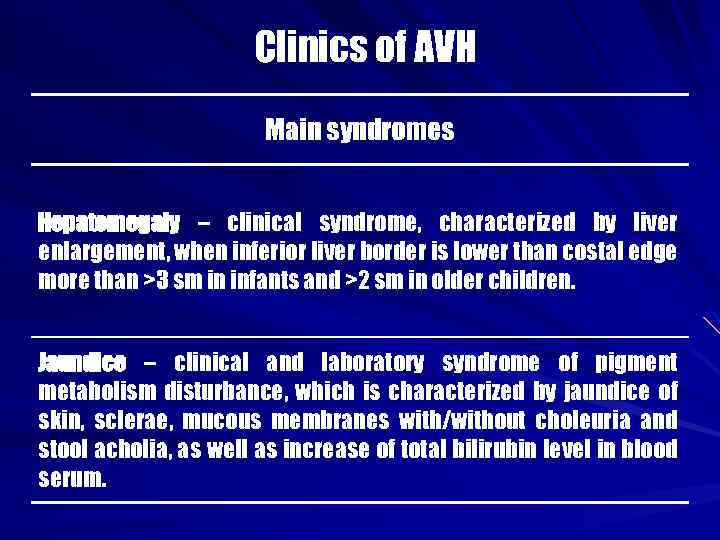 Clinics of AVH Main syndromes Hepatomegaly – clinical syndrome, characterized by liver enlargement, when inferior liver border is lower than costal edge more than >3 sm in infants and >2 sm in older children. Jaundice – clinical and laboratory syndrome of pigment metabolism disturbance, which is characterized by jaundice of skin, sclerae, mucous membranes with/without choleuria and stool acholia, as well as increase of total bilirubin level in blood serum.
Clinics of AVH Main syndromes Hepatomegaly – clinical syndrome, characterized by liver enlargement, when inferior liver border is lower than costal edge more than >3 sm in infants and >2 sm in older children. Jaundice – clinical and laboratory syndrome of pigment metabolism disturbance, which is characterized by jaundice of skin, sclerae, mucous membranes with/without choleuria and stool acholia, as well as increase of total bilirubin level in blood serum.
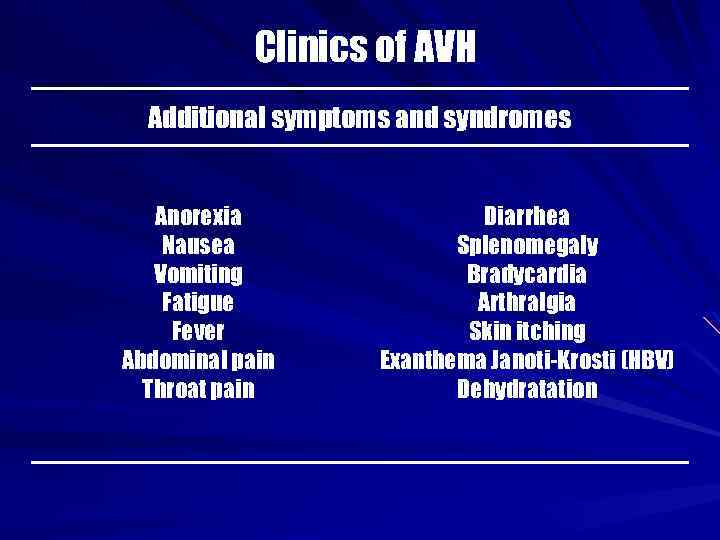 Clinics of AVH Additional symptoms and syndromes Anorexia Nausea Vomiting Fatigue Fever Abdominal pain Throat pain Diarrhea Splenomegaly Bradycardia Arthralgia Skin itching Exanthema Janoti-Krosti (HBV) Dehydratation
Clinics of AVH Additional symptoms and syndromes Anorexia Nausea Vomiting Fatigue Fever Abdominal pain Throat pain Diarrhea Splenomegaly Bradycardia Arthralgia Skin itching Exanthema Janoti-Krosti (HBV) Dehydratation
 Periods of AVH Pre-jaundice Jaundice Recovery
Periods of AVH Pre-jaundice Jaundice Recovery
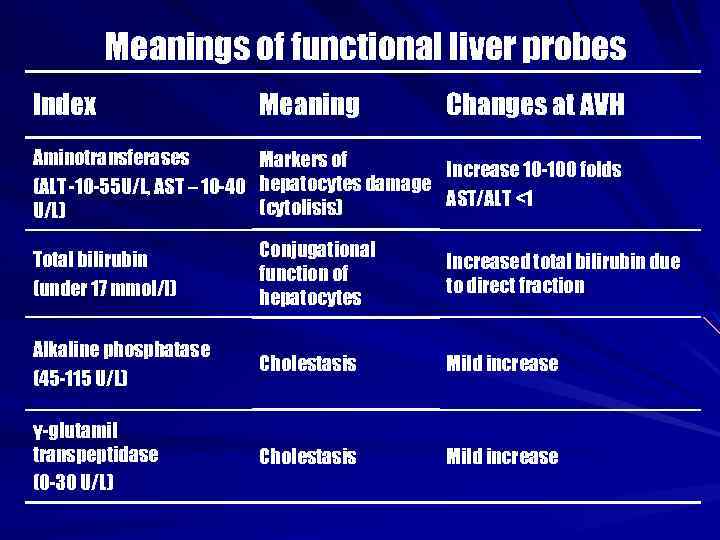 Meanings of functional liver probes Index Meaning Changes at AVH Aminotransferases (АLT -10 -55 U/L, АST – 10 -40 U/L) Markers of Increase 10 -100 folds hepatocytes damage АST/АLT <1 (cytolisis) Total bilirubin (under 17 mmol/l) Conjugational function of hepatocytes Increased total bilirubin due to direct fraction Alkaline phosphatase (45 -115 U/L) Cholestasis Mild increase γ-glutamil transpeptidase (0 -30 U/L) Cholestasis Mild increase
Meanings of functional liver probes Index Meaning Changes at AVH Aminotransferases (АLT -10 -55 U/L, АST – 10 -40 U/L) Markers of Increase 10 -100 folds hepatocytes damage АST/АLT <1 (cytolisis) Total bilirubin (under 17 mmol/l) Conjugational function of hepatocytes Increased total bilirubin due to direct fraction Alkaline phosphatase (45 -115 U/L) Cholestasis Mild increase γ-glutamil transpeptidase (0 -30 U/L) Cholestasis Mild increase
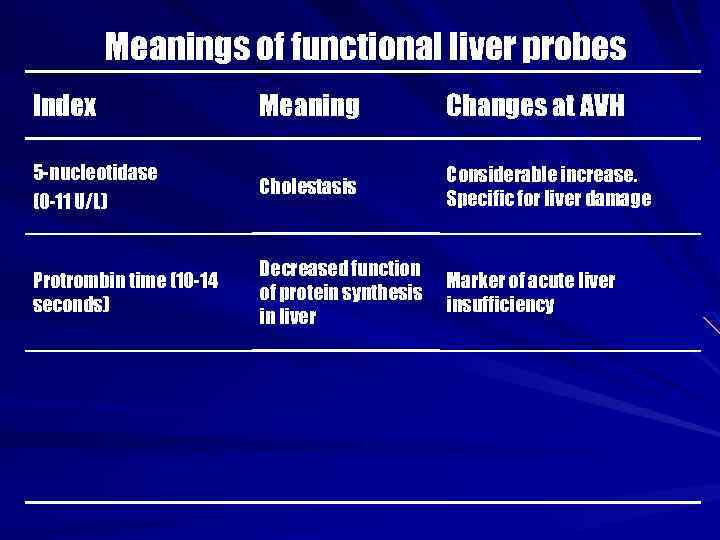 Meanings of functional liver probes Index Meaning Changes at AVH 5 -nucleotidase (0 -11 U/L) Cholestasis Considerable increase. Specific for liver damage Protrombin time (10 -14 seconds) Decreased function of protein synthesis in liver Marker of acute liver insufficiency
Meanings of functional liver probes Index Meaning Changes at AVH 5 -nucleotidase (0 -11 U/L) Cholestasis Considerable increase. Specific for liver damage Protrombin time (10 -14 seconds) Decreased function of protein synthesis in liver Marker of acute liver insufficiency
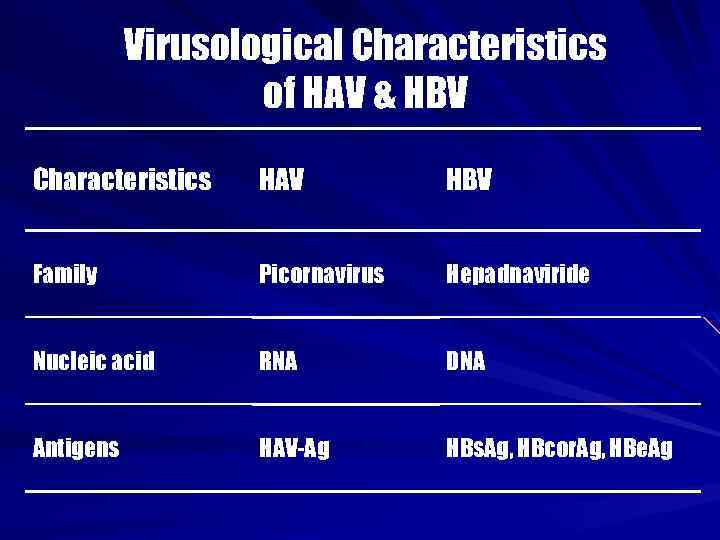 Virusological Characteristics of HAV & HBV Characteristics HAV HBV Family Picornavirus Hepadnaviride Nucleic acid RNA DNA Antigens HAV-Ag HBs. Ag, HBcor. Ag, HBe. Ag
Virusological Characteristics of HAV & HBV Characteristics HAV HBV Family Picornavirus Hepadnaviride Nucleic acid RNA DNA Antigens HAV-Ag HBs. Ag, HBcor. Ag, HBe. Ag
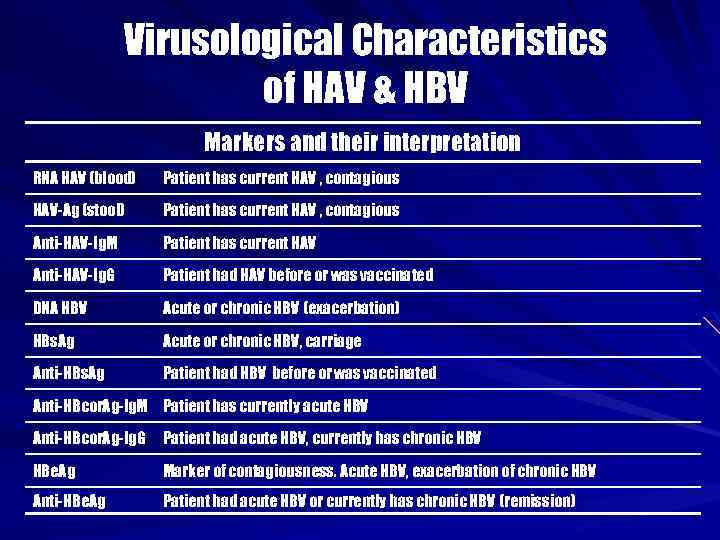 Virusological Characteristics of HAV & HBV Markers and their interpretation RNA HAV (blood) Patient has current HAV , contagious НАV-Ag (stool) Patient has current HAV , contagious Anti-HAV-Ig. M Patient has current HAV Anti-HAV-Ig. G Patient had HAV before or was vaccinated DNA HBV Acute or chronic HBV (exacerbation) HBs. Ag Acute or chronic HBV, carriage Anti-HBs. Ag Patient had HBV before or was vaccinated Anti-HBcor. Ag-Ig. M Patient has currently acute HBV Anti-HBcor. Ag-Ig. G Patient had acute HBV, currently has chronic HBV HBe. Ag Marker of contagiousness. Acute HBV, exacerbation of chronic HBV Anti-HBe. Ag Patient had acute HBV or currently has chronic HBV (remission)
Virusological Characteristics of HAV & HBV Markers and their interpretation RNA HAV (blood) Patient has current HAV , contagious НАV-Ag (stool) Patient has current HAV , contagious Anti-HAV-Ig. M Patient has current HAV Anti-HAV-Ig. G Patient had HAV before or was vaccinated DNA HBV Acute or chronic HBV (exacerbation) HBs. Ag Acute or chronic HBV, carriage Anti-HBs. Ag Patient had HBV before or was vaccinated Anti-HBcor. Ag-Ig. M Patient has currently acute HBV Anti-HBcor. Ag-Ig. G Patient had acute HBV, currently has chronic HBV HBe. Ag Marker of contagiousness. Acute HBV, exacerbation of chronic HBV Anti-HBe. Ag Patient had acute HBV or currently has chronic HBV (remission)
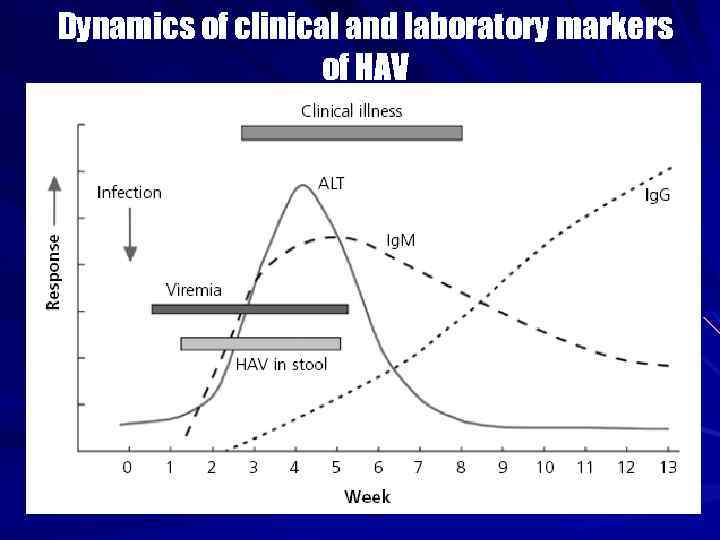 Dynamics of clinical and laboratory markers of HAV
Dynamics of clinical and laboratory markers of HAV
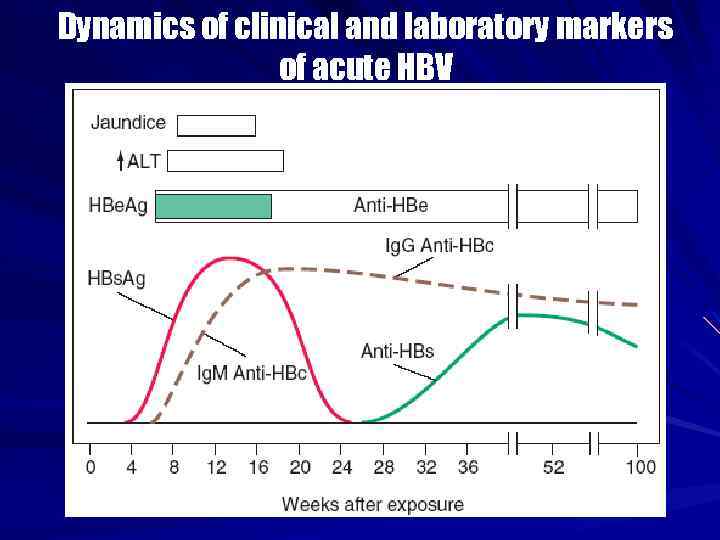 Dynamics of clinical and laboratory markers of acute HBV
Dynamics of clinical and laboratory markers of acute HBV
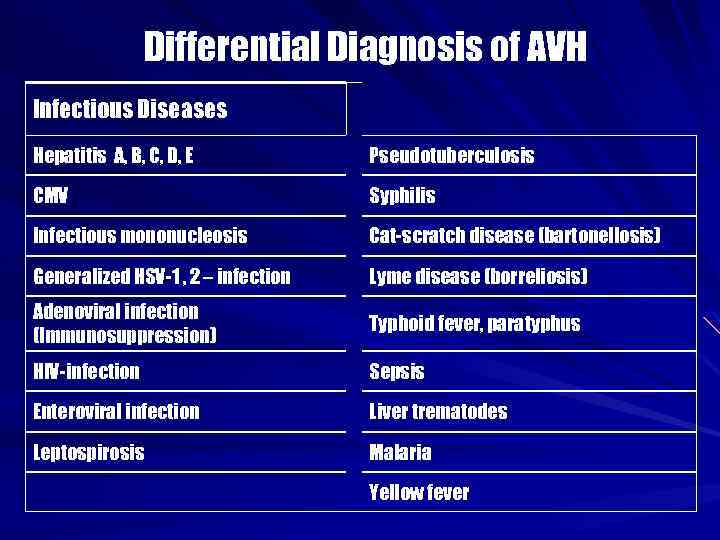 Differential Diagnosis of AVH Infectious Diseases Hepatitis A, B, C, D, E Pseudotuberculosis CMV Syphilis Infectious mononucleosis Cat-scratch disease (bartonellosis) Generalized HSV-1 , 2 – infection Lyme disease (borreliosis) Adenoviral infection (Immunosuppression) Typhoid fever, paratyphus HIV-infection Sepsis Enteroviral infection Liver trematodes Leptospirosis Malaria Yellow fever
Differential Diagnosis of AVH Infectious Diseases Hepatitis A, B, C, D, E Pseudotuberculosis CMV Syphilis Infectious mononucleosis Cat-scratch disease (bartonellosis) Generalized HSV-1 , 2 – infection Lyme disease (borreliosis) Adenoviral infection (Immunosuppression) Typhoid fever, paratyphus HIV-infection Sepsis Enteroviral infection Liver trematodes Leptospirosis Malaria Yellow fever
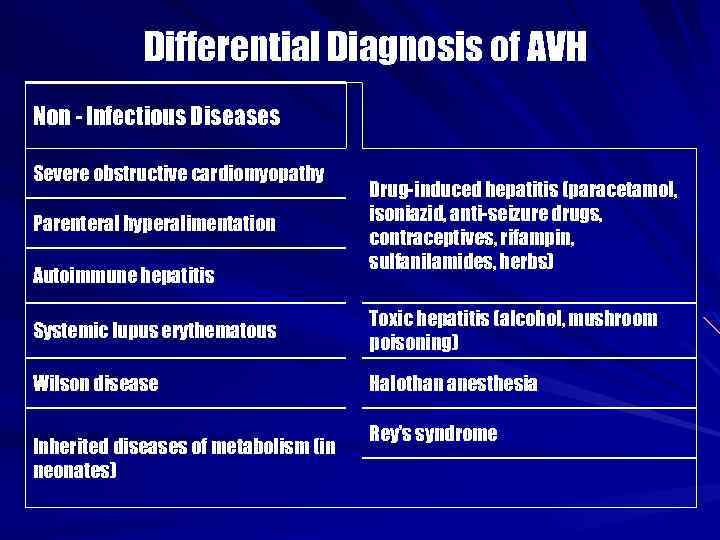 Differential Diagnosis of AVH Non - Infectious Diseases Severe obstructive cardiomyopathy Parenteral hyperalimentation Autoimmune hepatitis Drug-induced hepatitis (paracetamol, isoniazid, anti-seizure drugs, contraceptives, rifampin, sulfanilamides, herbs) Systemic lupus erythematous Toxic hepatitis (alcohol, mushroom poisoning) Wilson disease Halothan anesthesia Inherited diseases of metabolism (in neonates) Rey’s syndrome
Differential Diagnosis of AVH Non - Infectious Diseases Severe obstructive cardiomyopathy Parenteral hyperalimentation Autoimmune hepatitis Drug-induced hepatitis (paracetamol, isoniazid, anti-seizure drugs, contraceptives, rifampin, sulfanilamides, herbs) Systemic lupus erythematous Toxic hepatitis (alcohol, mushroom poisoning) Wilson disease Halothan anesthesia Inherited diseases of metabolism (in neonates) Rey’s syndrome
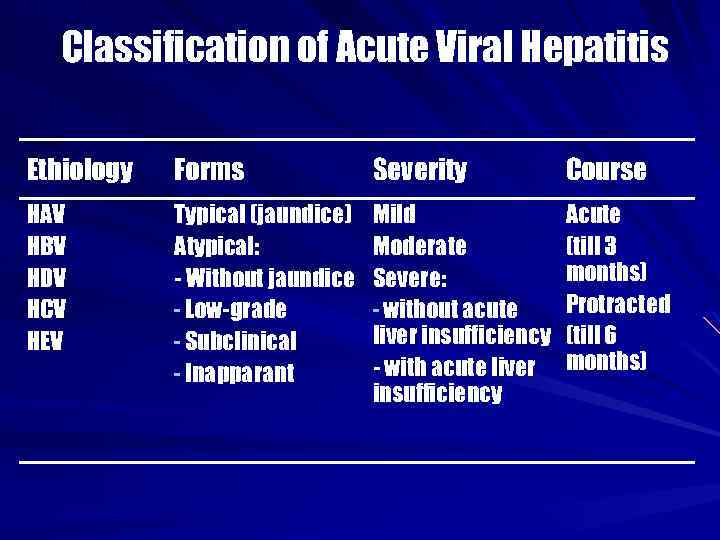 Classification of Acute Viral Hepatitis Ethiology Forms Severity Course HAV HBV HDV HCV HEV Typical (jaundice) Atypical: - Without jaundice - Low-grade - Subclinical - Inapparant Mild Moderate Severe: - without acute liver insufficiency - with acute liver insufficiency Acute (till 3 months) Protracted (till 6 months)
Classification of Acute Viral Hepatitis Ethiology Forms Severity Course HAV HBV HDV HCV HEV Typical (jaundice) Atypical: - Without jaundice - Low-grade - Subclinical - Inapparant Mild Moderate Severe: - without acute liver insufficiency - with acute liver insufficiency Acute (till 3 months) Protracted (till 6 months)
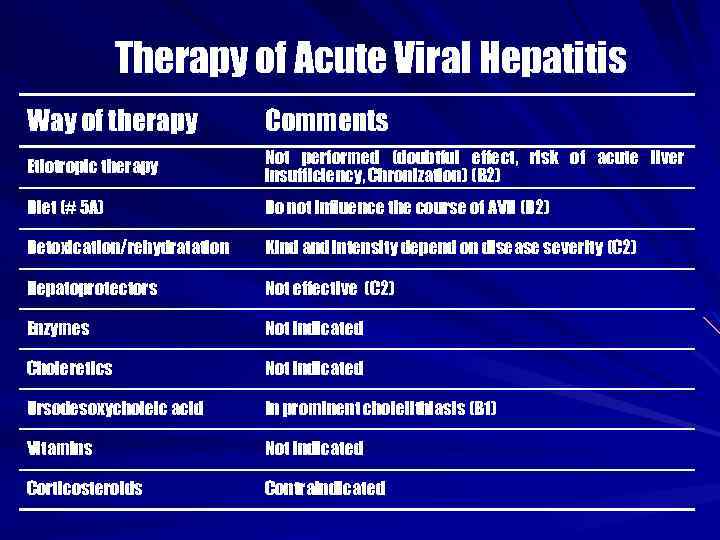 Therapy of Acute Viral Hepatitis Way of therapy Comments Etiotropic therapy Not performed (doubtful effect, risk of acute liver insufficiency, Chronization) (В 2) Diet (# 5 А) Do not influence the course of AVH (D 2) Detoxication/rehydratation Kind and intensity depend on disease severity (С 2) Hepatoprotectors Not effective (С 2) Enzymes Not indicated Choleretics Not indicated Ursodesoxycholeic acid In prominent cholelithiasis (В 1) Vitamins Not indicated Corticosteroids Contraindicated
Therapy of Acute Viral Hepatitis Way of therapy Comments Etiotropic therapy Not performed (doubtful effect, risk of acute liver insufficiency, Chronization) (В 2) Diet (# 5 А) Do not influence the course of AVH (D 2) Detoxication/rehydratation Kind and intensity depend on disease severity (С 2) Hepatoprotectors Not effective (С 2) Enzymes Not indicated Choleretics Not indicated Ursodesoxycholeic acid In prominent cholelithiasis (В 1) Vitamins Not indicated Corticosteroids Contraindicated
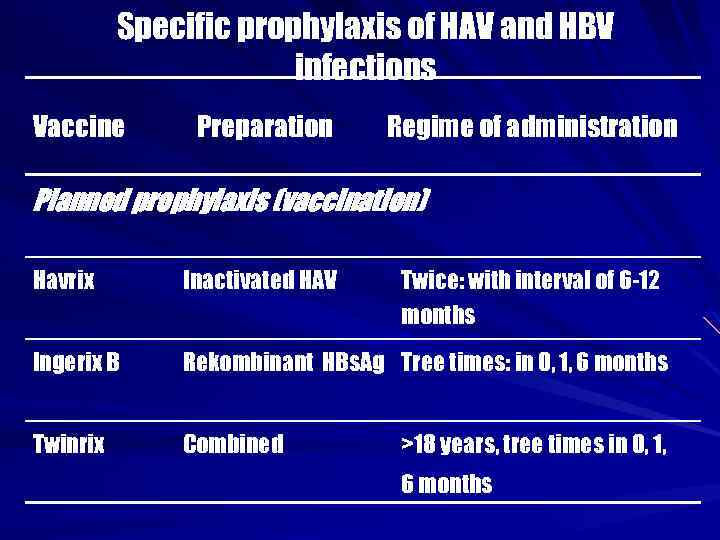 Specific prophylaxis of HAV and HBV infections Vaccine Preparation Regime of administration Planned prophylaxis (vaccination) Havrix Inactivated HAV Twice: with interval of 6 -12 months Ingerix B Rekombinant HBs. Ag Tree times: in 0, 1, 6 months Twinrix Combined >18 years, tree times in 0, 1, 6 months
Specific prophylaxis of HAV and HBV infections Vaccine Preparation Regime of administration Planned prophylaxis (vaccination) Havrix Inactivated HAV Twice: with interval of 6 -12 months Ingerix B Rekombinant HBs. Ag Tree times: in 0, 1, 6 months Twinrix Combined >18 years, tree times in 0, 1, 6 months
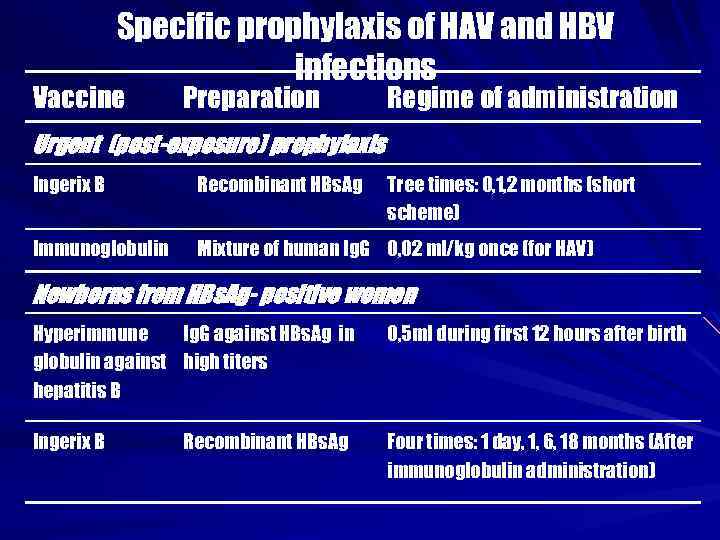 Specific prophylaxis of HAV and HBV infections Vaccine Preparation Regime of administration Urgent (post-exposure) prophylaxis Ingerix B Recombinant HBs. Ag Tree times: 0, 1, 2 months (short scheme) Immunoglobulin Mixture of human Ig. G 0, 02 ml/kg once (for HAV) Newborns from HBs. Ag- positive women Hyperimmune Ig. G against HBs. Ag in globulin against high titers hepatitis B 0, 5 ml during first 12 hours after birth Ingerix B Four times: 1 day, 1, 6, 18 months (After immunoglobulin administration) Recombinant HBs. Ag
Specific prophylaxis of HAV and HBV infections Vaccine Preparation Regime of administration Urgent (post-exposure) prophylaxis Ingerix B Recombinant HBs. Ag Tree times: 0, 1, 2 months (short scheme) Immunoglobulin Mixture of human Ig. G 0, 02 ml/kg once (for HAV) Newborns from HBs. Ag- positive women Hyperimmune Ig. G against HBs. Ag in globulin against high titers hepatitis B 0, 5 ml during first 12 hours after birth Ingerix B Four times: 1 day, 1, 6, 18 months (After immunoglobulin administration) Recombinant HBs. Ag


