ce87d8465ae3fc9490fd56a3b84dcd88.ppt
- Количество слайдов: 91
 Acute Stroke Redesign: Kaiser Telestroke Update TRILOK S. PUNIANI, MD May 6, 2017
Acute Stroke Redesign: Kaiser Telestroke Update TRILOK S. PUNIANI, MD May 6, 2017
 Statement of Disclosure v. I do not have affiliations that may constitute a conflict of interest with this program.
Statement of Disclosure v. I do not have affiliations that may constitute a conflict of interest with this program.
 Objectives: Briefly discuss types of strokes Risk factors for stroke Primary stroke center Telestroke: Acute Stroke Redesign
Objectives: Briefly discuss types of strokes Risk factors for stroke Primary stroke center Telestroke: Acute Stroke Redesign

 Test Your Knowledge Stroke is the leading cause of disability in the US A. True B. False
Test Your Knowledge Stroke is the leading cause of disability in the US A. True B. False
 Answer: A
Answer: A
 Strokes are not preventable. A. True B. False
Strokes are not preventable. A. True B. False
 Answer: B
Answer: B
 Strokes mainly effect elderly A. True B. False
Strokes mainly effect elderly A. True B. False
 Answer: B
Answer: B
 Stroke is the third leading cause of death in the US. A. True B. False
Stroke is the third leading cause of death in the US. A. True B. False
 Answer: B
Answer: B
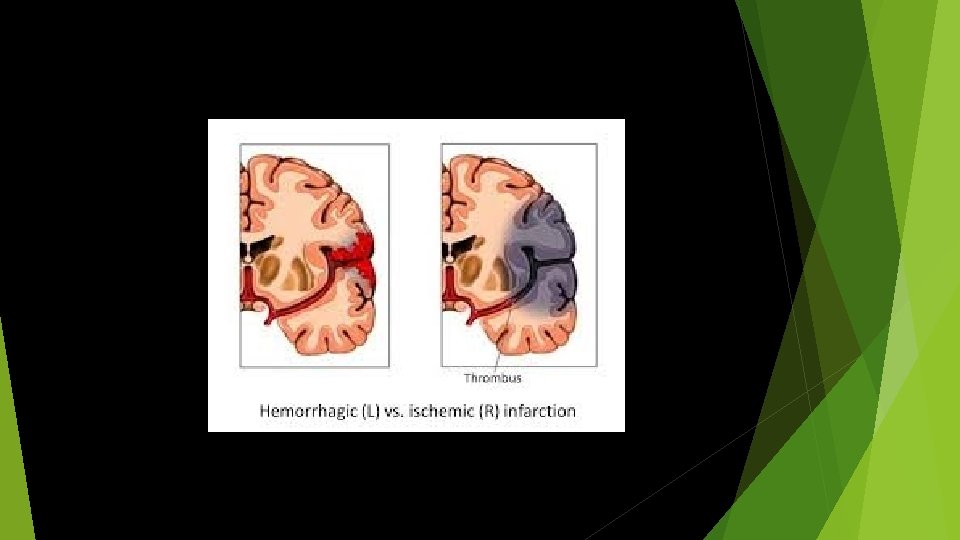
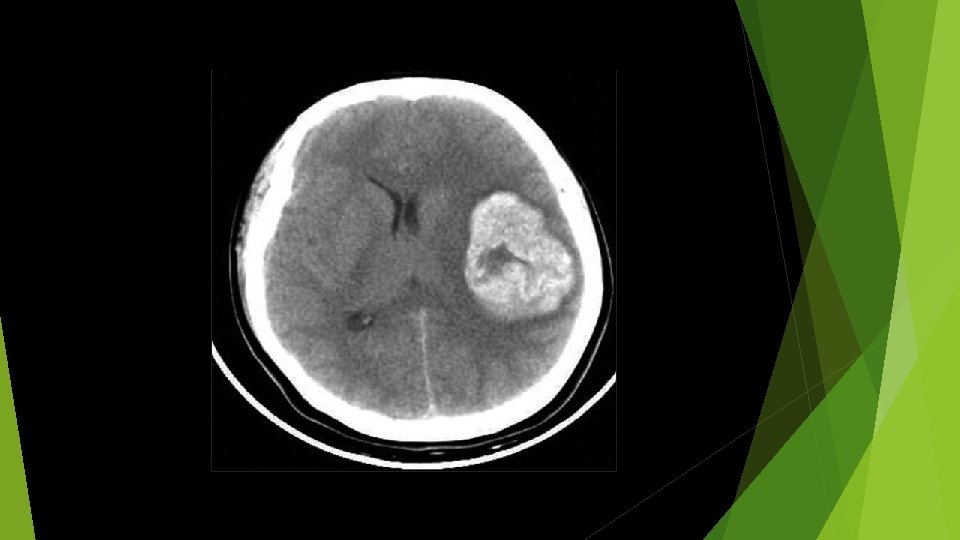
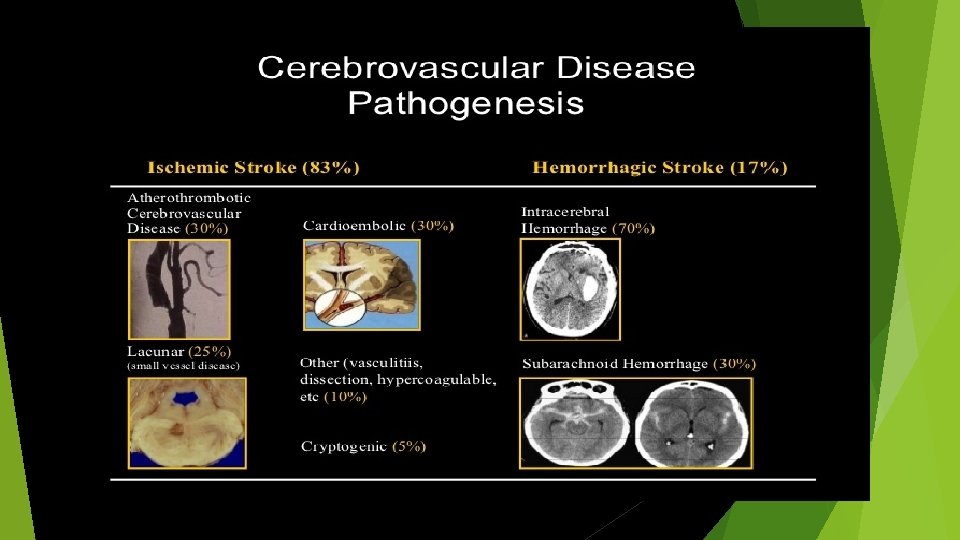
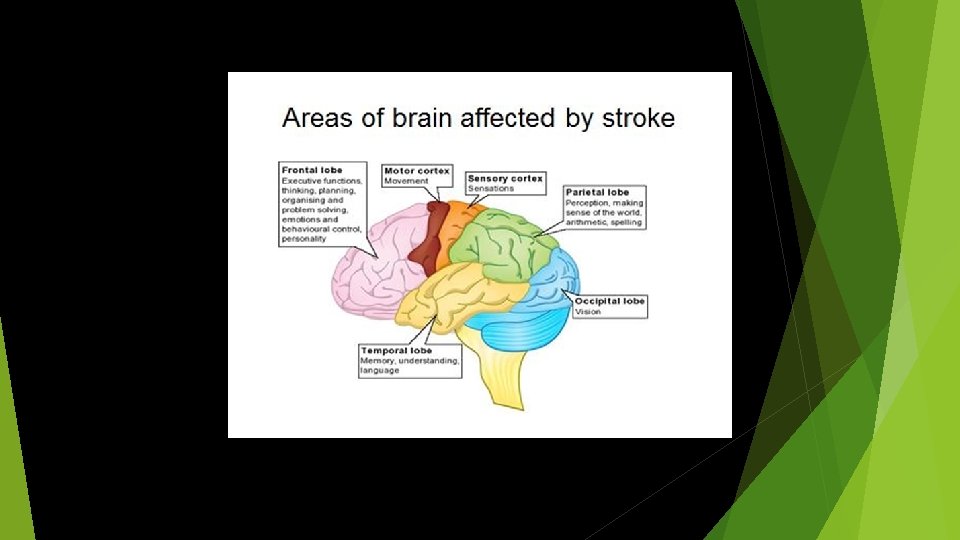
 What Is a Stroke ? Stroke is a sudden loss of neurologic function resulting from focal disturbance of cerebral blood flow due to ischemia or hemorrhage.
What Is a Stroke ? Stroke is a sudden loss of neurologic function resulting from focal disturbance of cerebral blood flow due to ischemia or hemorrhage.
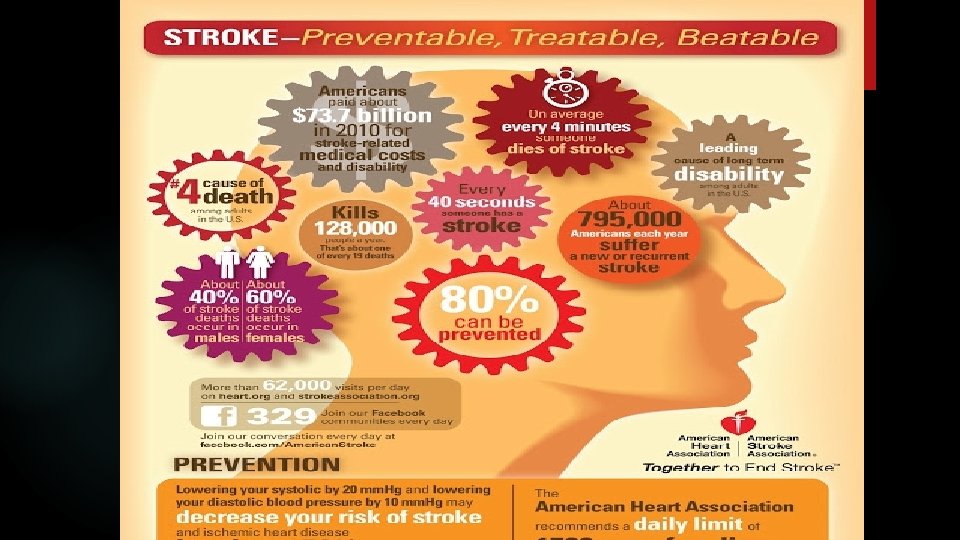
 Stroke was the third leading cause of death after heart disease and cancer. In 2008, it dropped to the fourth leading cause of death. Currently, stroke is the fifth leading cause of death. Stroke is a leading cause of disability in the United States. Improved care and stroke risk reduction measures by the primary care providers, public and health care professional education Acute interventions and multi-disciplinary care, GWTG, substantially improved the outcome for stroke patients.
Stroke was the third leading cause of death after heart disease and cancer. In 2008, it dropped to the fourth leading cause of death. Currently, stroke is the fifth leading cause of death. Stroke is a leading cause of disability in the United States. Improved care and stroke risk reduction measures by the primary care providers, public and health care professional education Acute interventions and multi-disciplinary care, GWTG, substantially improved the outcome for stroke patients.

 What are the risk factors for Stroke? There are two types of risk factors: - Non-modifiable (factors you cannot control) - Modifiable (factors you can control)
What are the risk factors for Stroke? There are two types of risk factors: - Non-modifiable (factors you cannot control) - Modifiable (factors you can control)
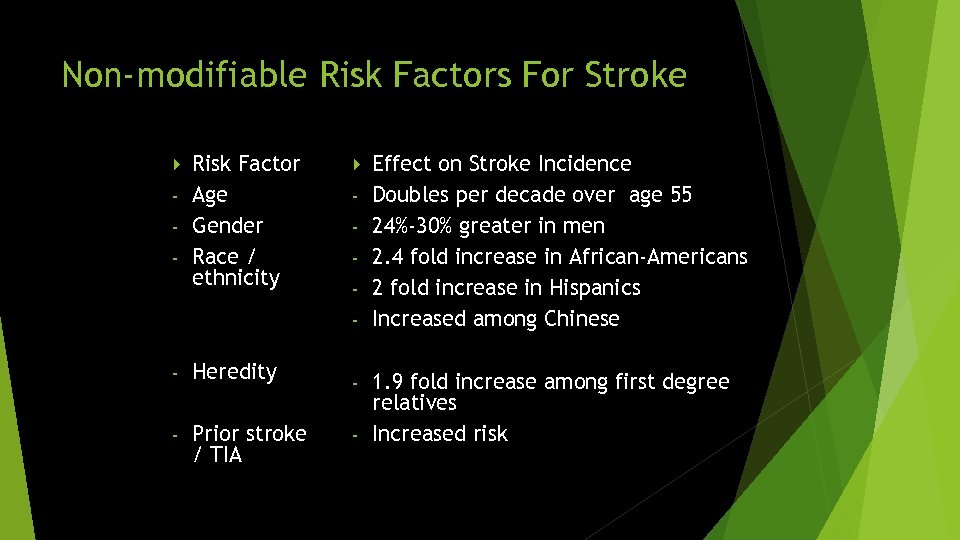 Non-modifiable Risk Factors For Stroke Risk Factor - Age - Gender - Race / ethnicity - - Heredity - Prior stroke / TIA Effect on Stroke Incidence Doubles per decade over age 55 24%-30% greater in men 2. 4 fold increase in African-Americans 2 fold increase in Hispanics Increased among Chinese 1. 9 fold increase among first degree relatives - Increased risk -
Non-modifiable Risk Factors For Stroke Risk Factor - Age - Gender - Race / ethnicity - - Heredity - Prior stroke / TIA Effect on Stroke Incidence Doubles per decade over age 55 24%-30% greater in men 2. 4 fold increase in African-Americans 2 fold increase in Hispanics Increased among Chinese 1. 9 fold increase among first degree relatives - Increased risk -
 Modifiable Risk Factors - About 90% of stroke risk may be explained by TEN major risk factors: Cardiac causes Hypertension Diabetes mellitus Diet Hyperlipidemia Cigarette smoking Abdominal obesity Physical inactivity / sedentary behavior Excess alcohol consumption Psychosocial stress and depression
Modifiable Risk Factors - About 90% of stroke risk may be explained by TEN major risk factors: Cardiac causes Hypertension Diabetes mellitus Diet Hyperlipidemia Cigarette smoking Abdominal obesity Physical inactivity / sedentary behavior Excess alcohol consumption Psychosocial stress and depression
 What is Stroke certification Recognition (i. e. Certification) by Joint Commission as a facility which provides stroke care for patients across the continuum who have suffered from TIA or stroke.
What is Stroke certification Recognition (i. e. Certification) by Joint Commission as a facility which provides stroke care for patients across the continuum who have suffered from TIA or stroke.
 Benefits of Primary Stroke Centers Improved efficiency of patient care Fewer peri-stroke complications Increased use of acute stroke therapies Reduced morbidity and mortality Improved long-term outcomes Reduced costs to healthcare system Increased patient satisfaction
Benefits of Primary Stroke Centers Improved efficiency of patient care Fewer peri-stroke complications Increased use of acute stroke therapies Reduced morbidity and mortality Improved long-term outcomes Reduced costs to healthcare system Increased patient satisfaction
 Major Elements of a Primary Stroke Center Patient Care Areas 1. Acute stroke teams 2. Written care protocols (GWTG) 3. Emergency medical services 4. Emergency department 5. Stroke Unit 6. Neurosurgical services 7. Radiology services 8. Laboratory services
Major Elements of a Primary Stroke Center Patient Care Areas 1. Acute stroke teams 2. Written care protocols (GWTG) 3. Emergency medical services 4. Emergency department 5. Stroke Unit 6. Neurosurgical services 7. Radiology services 8. Laboratory services
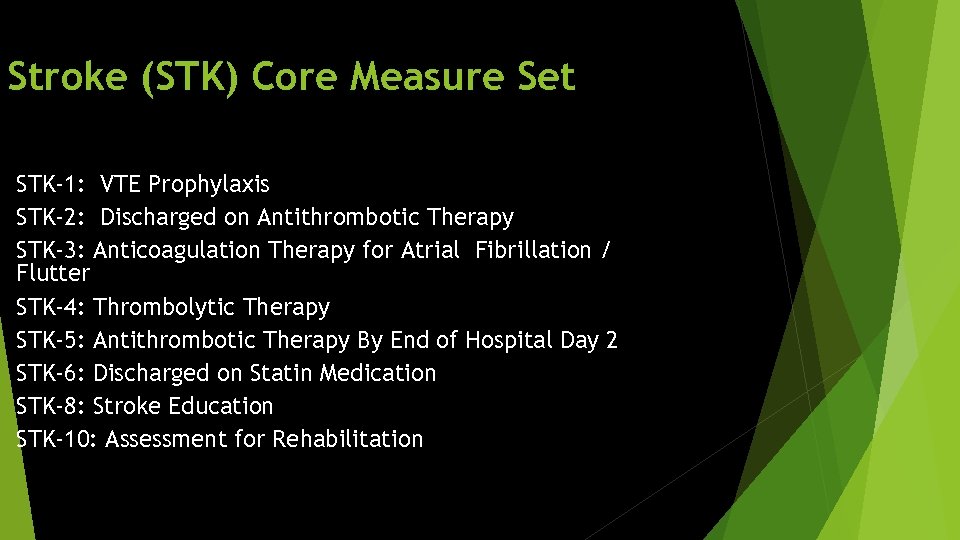 Stroke (STK) Core Measure Set STK-1: VTE Prophylaxis STK-2: Discharged on Antithrombotic Therapy STK-3: Anticoagulation Therapy for Atrial Fibrillation / Flutter STK-4: Thrombolytic Therapy STK-5: Antithrombotic Therapy By End of Hospital Day 2 STK-6: Discharged on Statin Medication STK-8: Stroke Education STK-10: Assessment for Rehabilitation
Stroke (STK) Core Measure Set STK-1: VTE Prophylaxis STK-2: Discharged on Antithrombotic Therapy STK-3: Anticoagulation Therapy for Atrial Fibrillation / Flutter STK-4: Thrombolytic Therapy STK-5: Antithrombotic Therapy By End of Hospital Day 2 STK-6: Discharged on Statin Medication STK-8: Stroke Education STK-10: Assessment for Rehabilitation
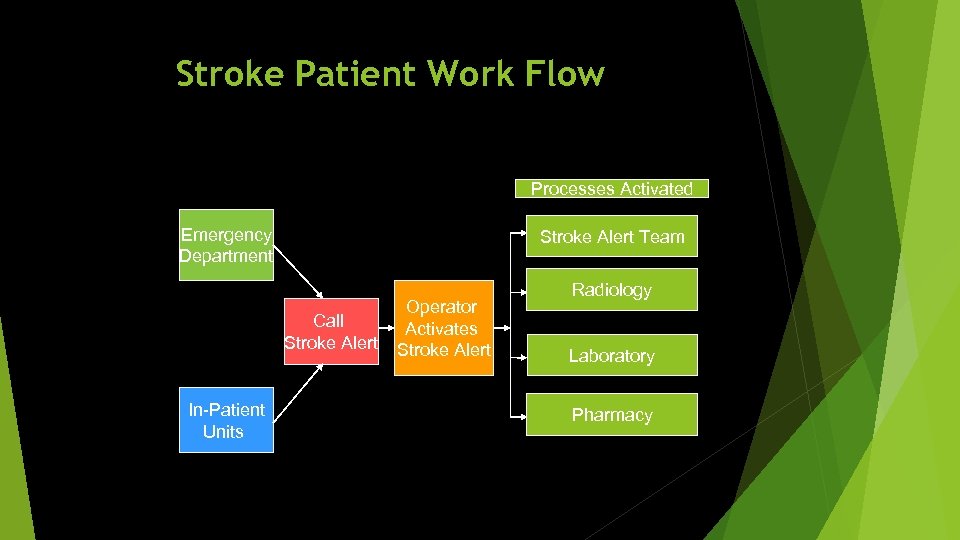 Stroke Patient Work Flow Processes Activated Emergency Department Stroke Alert Team Call Stroke Alert In-Patient Units Operator Activates Stroke Alert Radiology Laboratory Pharmacy
Stroke Patient Work Flow Processes Activated Emergency Department Stroke Alert Team Call Stroke Alert In-Patient Units Operator Activates Stroke Alert Radiology Laboratory Pharmacy
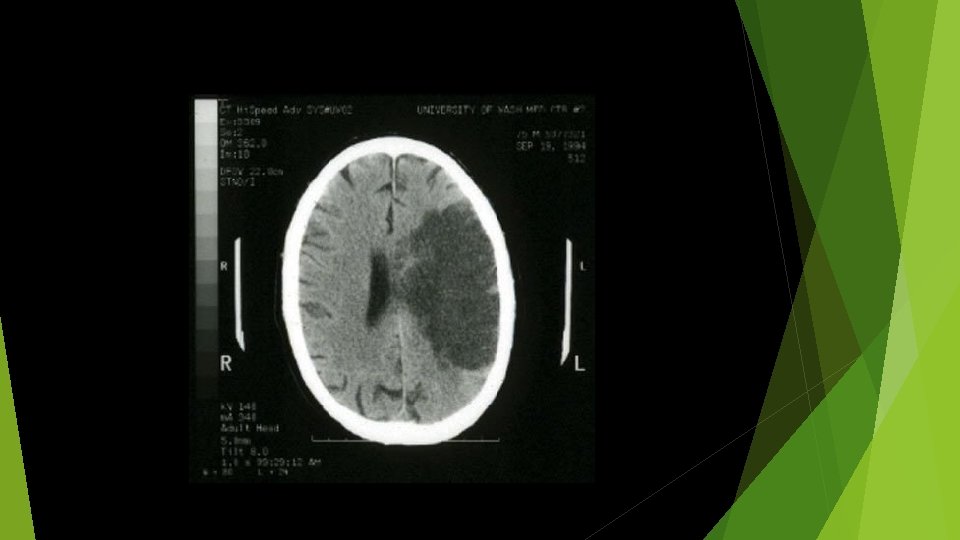
 Proven Strategies in Acute Ischemic Stroke Therapy Reperfusion Prevent Clot Propagation / Recanalization Supportive Care Early Implementation of Secondary Stroke Prevention
Proven Strategies in Acute Ischemic Stroke Therapy Reperfusion Prevent Clot Propagation / Recanalization Supportive Care Early Implementation of Secondary Stroke Prevention
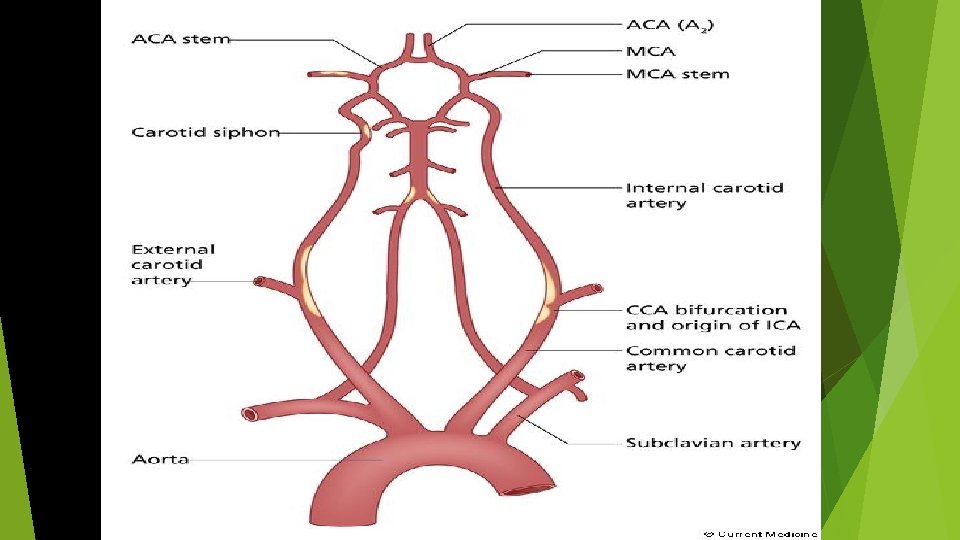
 REPERFUSION THERAPY Thrombolytic therapy is able to recanalize acute intracranial arterial occlusions. A strong correlation has been shown between arterial recanalization and neurological improvement in acute cerebral ischemia.
REPERFUSION THERAPY Thrombolytic therapy is able to recanalize acute intracranial arterial occlusions. A strong correlation has been shown between arterial recanalization and neurological improvement in acute cerebral ischemia.
 The vision of thrombolysis for reversal of acute ischemic stroke (AIS) was launched in 1958, but it was not until 1995 that 2 landmark studies, one in Europe and the other in the United States, established IV administration of tissue plasminogen activator (t. PA) as an effective treatment for AIS
The vision of thrombolysis for reversal of acute ischemic stroke (AIS) was launched in 1958, but it was not until 1995 that 2 landmark studies, one in Europe and the other in the United States, established IV administration of tissue plasminogen activator (t. PA) as an effective treatment for AIS
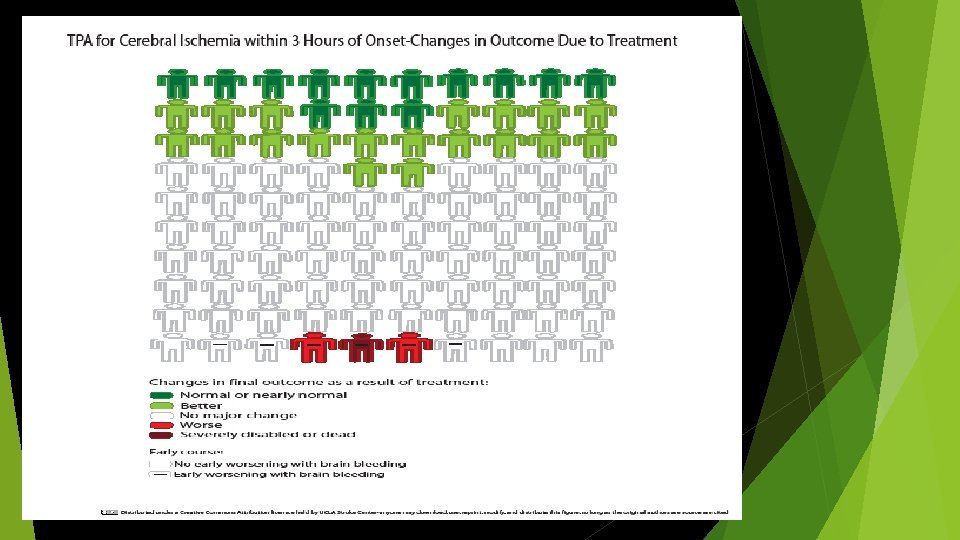
 Thrombolytic Therapy In June 1996, the FDA approved the use of IV recombinant tissue type plasminogen activator (rt. PA) for ischemic stroke within 3 hours of symptom onset. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group showed that treatment with IV t. PA within 3 hours of onset of ischemic stroke improved clinical outcome.
Thrombolytic Therapy In June 1996, the FDA approved the use of IV recombinant tissue type plasminogen activator (rt. PA) for ischemic stroke within 3 hours of symptom onset. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group showed that treatment with IV t. PA within 3 hours of onset of ischemic stroke improved clinical outcome.
 The Basic Concept TIME IS BRAIN
The Basic Concept TIME IS BRAIN

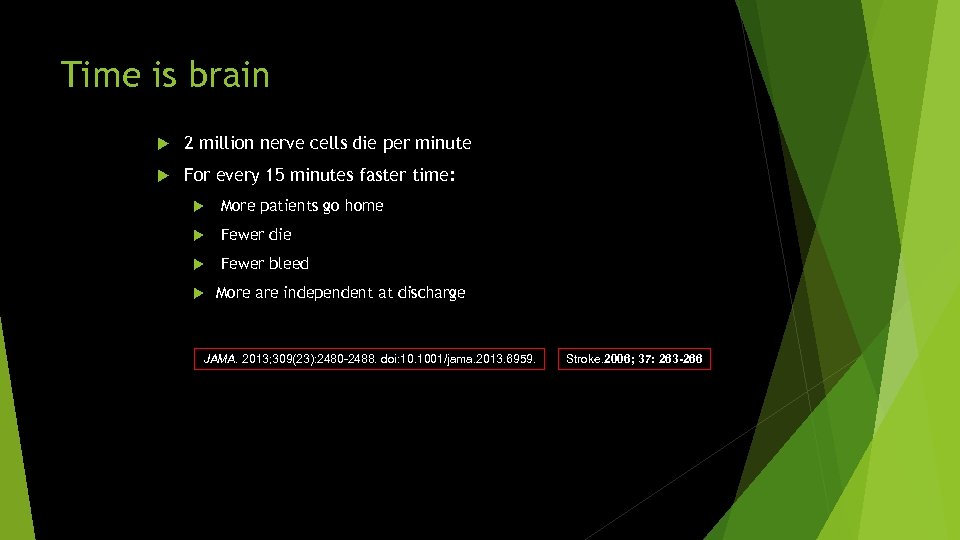 Time is brain 2 million nerve cells die per minute For every 15 minutes faster time: More patients go home Fewer die Fewer bleed More are independent at discharge JAMA. 2013; 309(23): 2480 -2488. doi: 10. 1001/jama. 2013. 6959. Stroke. 2006; 37: 263 -266
Time is brain 2 million nerve cells die per minute For every 15 minutes faster time: More patients go home Fewer die Fewer bleed More are independent at discharge JAMA. 2013; 309(23): 2480 -2488. doi: 10. 1001/jama. 2013. 6959. Stroke. 2006; 37: 263 -266
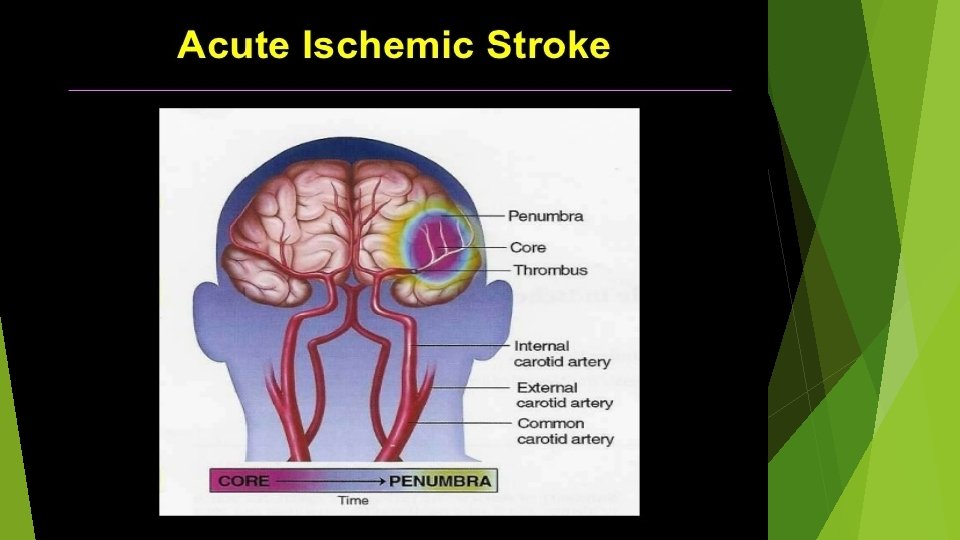
 Stroke Recovery The two most important concepts for recovery - Penumbra - Time is Brain Concept
Stroke Recovery The two most important concepts for recovery - Penumbra - Time is Brain Concept
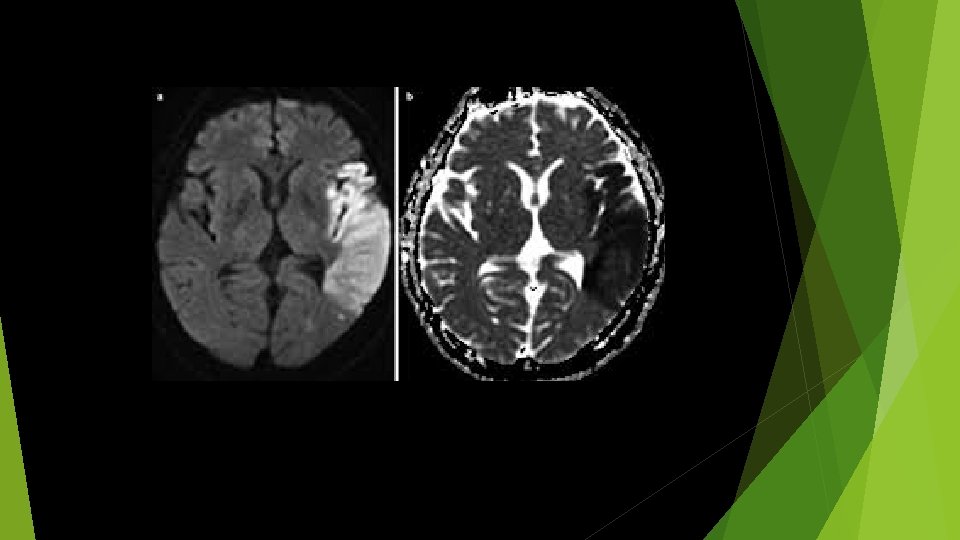
 Ischemic Penumbra: Latin pene “almost” + umbra “shadow” Zone of tissue around an infarct (ischemic core) which receives some collateral circulation Potentially restored salvageable if blood flow is
Ischemic Penumbra: Latin pene “almost” + umbra “shadow” Zone of tissue around an infarct (ischemic core) which receives some collateral circulation Potentially restored salvageable if blood flow is
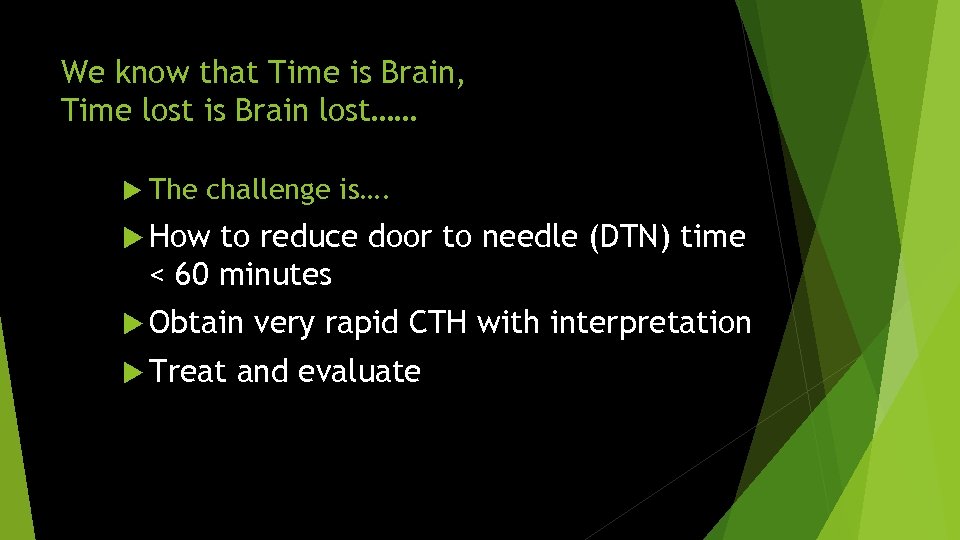 We know that Time is Brain, Time lost is Brain lost…… The challenge is…. How to reduce door to needle (DTN) time < 60 minutes Obtain Treat very rapid CTH with interpretation and evaluate
We know that Time is Brain, Time lost is Brain lost…… The challenge is…. How to reduce door to needle (DTN) time < 60 minutes Obtain Treat very rapid CTH with interpretation and evaluate


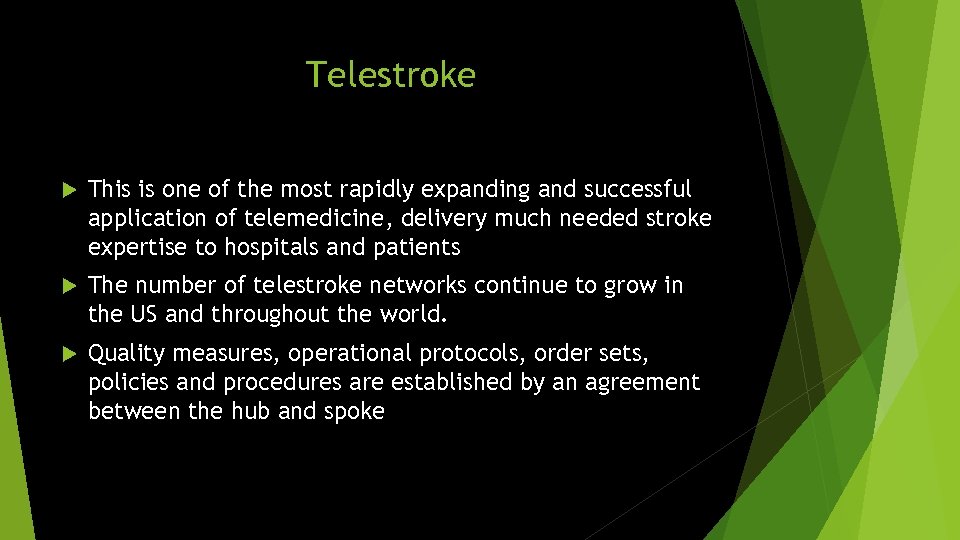 Telestroke This is one of the most rapidly expanding and successful application of telemedicine, delivery much needed stroke expertise to hospitals and patients The number of telestroke networks continue to grow in the US and throughout the world. Quality measures, operational protocols, order sets, policies and procedures are established by an agreement between the hub and spoke
Telestroke This is one of the most rapidly expanding and successful application of telemedicine, delivery much needed stroke expertise to hospitals and patients The number of telestroke networks continue to grow in the US and throughout the world. Quality measures, operational protocols, order sets, policies and procedures are established by an agreement between the hub and spoke
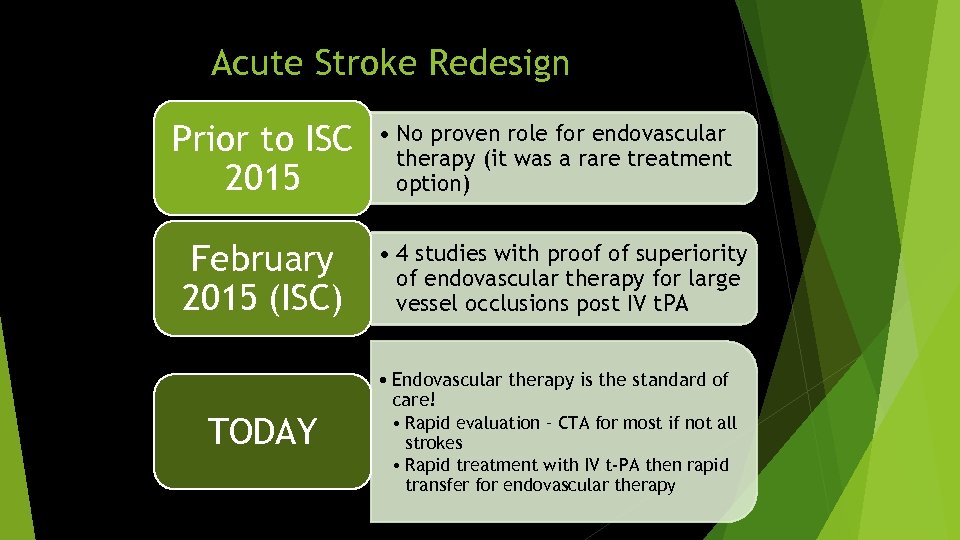 Acute Stroke Redesign Prior to ISC 2015 February 2015 (ISC) TODAY • No proven role for endovascular therapy (it was a rare treatment option) • 4 studies with proof of superiority of endovascular therapy for large vessel occlusions post IV t. PA • Endovascular therapy is the standard of care! • Rapid evaluation – CTA for most if not all strokes • Rapid treatment with IV t-PA then rapid transfer for endovascular therapy
Acute Stroke Redesign Prior to ISC 2015 February 2015 (ISC) TODAY • No proven role for endovascular therapy (it was a rare treatment option) • 4 studies with proof of superiority of endovascular therapy for large vessel occlusions post IV t. PA • Endovascular therapy is the standard of care! • Rapid evaluation – CTA for most if not all strokes • Rapid treatment with IV t-PA then rapid transfer for endovascular therapy

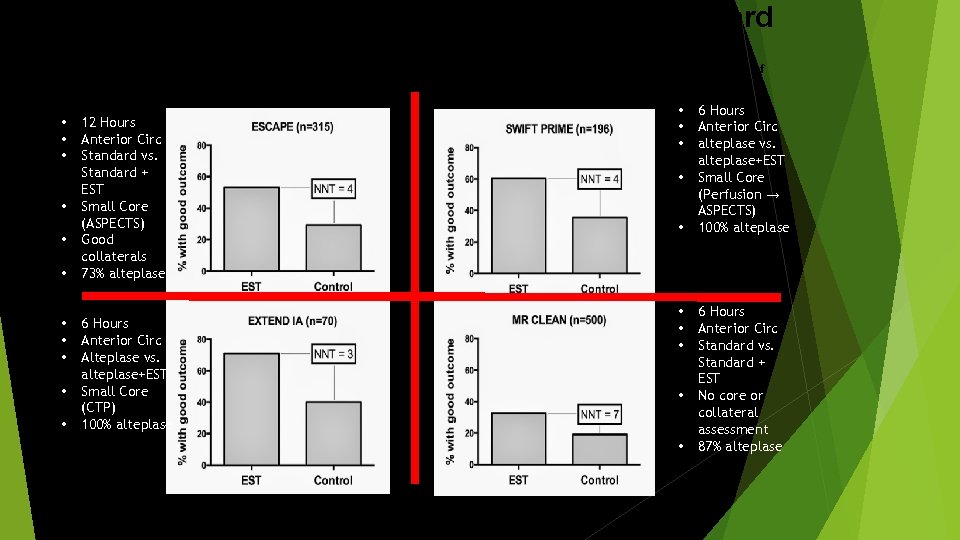 Comparison of RCTs for EST vs. Standard of Care Now there is a 5 th trial REVASCAT (206 patients. Similar outcomes. NNT= 6. 3) showing effectiveness of EST • • • 12 Hours Anterior Circ Standard vs. Standard + EST Small Core (ASPECTS) Good collaterals 73% alteplase 6 Hours Anterior Circ Alteplase vs. alteplase+EST Small Core (CTP) 100% alteplase • • • 6 Hours Anterior Circ alteplase vs. alteplase+EST Small Core (Perfusion → ASPECTS) 100% alteplase 6 Hours Anterior Circ Standard vs. Standard + EST No core or collateral assessment 87% alteplase
Comparison of RCTs for EST vs. Standard of Care Now there is a 5 th trial REVASCAT (206 patients. Similar outcomes. NNT= 6. 3) showing effectiveness of EST • • • 12 Hours Anterior Circ Standard vs. Standard + EST Small Core (ASPECTS) Good collaterals 73% alteplase 6 Hours Anterior Circ Alteplase vs. alteplase+EST Small Core (CTP) 100% alteplase • • • 6 Hours Anterior Circ alteplase vs. alteplase+EST Small Core (Perfusion → ASPECTS) 100% alteplase 6 Hours Anterior Circ Standard vs. Standard + EST No core or collateral assessment 87% alteplase
 What would it take to… Achieve 20 -30 minutes door to needle (DTN) times? Obtain very rapid CTH / CTA performance and interpretation Treat, evaluate, and transfer for endovascular therapy in less than 45 minutes?
What would it take to… Achieve 20 -30 minutes door to needle (DTN) times? Obtain very rapid CTH / CTA performance and interpretation Treat, evaluate, and transfer for endovascular therapy in less than 45 minutes?
 The world has changed
The world has changed
 KP STROKE EXPRESS (EXpediting the PRocess of Evaluating and Stopping Stroke)
KP STROKE EXPRESS (EXpediting the PRocess of Evaluating and Stopping Stroke)
 The key to speed… Key components = early involvement of stroke neurologist Don’t room – straight to CT Order TPA before CT TPA in CT Problem: small volumes cannot justify in house stroke neurologist Solution: video consultation + redesigned process
The key to speed… Key components = early involvement of stroke neurologist Don’t room – straight to CT Order TPA before CT TPA in CT Problem: small volumes cannot justify in house stroke neurologist Solution: video consultation + redesigned process
 KP Stroke EXPRESS EXpediting the PRocess of Evaluating & Stopping Stroke
KP Stroke EXPRESS EXpediting the PRocess of Evaluating & Stopping Stroke
 Acute Stroke Redesign: Stroke Neurologists involved early in the workflow via video (7 AM – MIDNIGHT)
Acute Stroke Redesign: Stroke Neurologists involved early in the workflow via video (7 AM – MIDNIGHT)

 Neurology Telestroke Hub Centralized hub of specialized stroke neurologists working remotely 7 AM to Midnight to examine all potential stroke patients early in the workflow via CISCO video carts
Neurology Telestroke Hub Centralized hub of specialized stroke neurologists working remotely 7 AM to Midnight to examine all potential stroke patients early in the workflow via CISCO video carts
 • Call to Neurologist via central 800 number - neurologist activates tele-presence unit • Clinical assessment and exam by stroke neurologist by video • Clinical assessment by ED physician • IV access • Lab • Blood sugar testing • INR if on warfarin or unknown
• Call to Neurologist via central 800 number - neurologist activates tele-presence unit • Clinical assessment and exam by stroke neurologist by video • Clinical assessment by ED physician • IV access • Lab • Blood sugar testing • INR if on warfarin or unknown
 Step One: Rapid assessment on arrival with video
Step One: Rapid assessment on arrival with video


 Inclusion Criteria for IV alteplase Diagnosis of acute ischemic stroke LKWT (last known well time) is < 3 hours and in some cases < 4. 5 hours from start of IV alteplase Over 18 years of age 7.
Inclusion Criteria for IV alteplase Diagnosis of acute ischemic stroke LKWT (last known well time) is < 3 hours and in some cases < 4. 5 hours from start of IV alteplase Over 18 years of age 7.
 • Discussion of t-PA / CTA risks, benefits, alternatives • IV t-PA ordered as soon as possible (allows time for mixing) • Call on / off stroke alert based on clinical assessment • Checklist / time out before leaving for CT
• Discussion of t-PA / CTA risks, benefits, alternatives • IV t-PA ordered as soon as possible (allows time for mixing) • Call on / off stroke alert based on clinical assessment • Checklist / time out before leaving for CT
 ØDirect to CT scanner - Once t. PA is determined appropriate in the ambulance bay or triage area the patient will go directly to the CT scanner
ØDirect to CT scanner - Once t. PA is determined appropriate in the ambulance bay or triage area the patient will go directly to the CT scanner

 in CT scanner - IV t. PA will be delivered and pushed in the CT suite directly after the CT is completed Øt. PA
in CT scanner - IV t. PA will be delivered and pushed in the CT suite directly after the CT is completed Øt. PA
 ØCTA completed directly after CT or t. PA - CTA completed on nearly all stroke patients
ØCTA completed directly after CT or t. PA - CTA completed on nearly all stroke patients
 KP STROKE EXPRESS Telestroke neurologist plays an active role in establishing diagnosis of stroke, ensuring inclusion/exclusion criteria for alteplase /endovascular Rx, obtaining consent, ordering alteplase, initiating administration of alteplase, and discussing with the neurointerventional radiologist whether endovascular Rx is appropriate.
KP STROKE EXPRESS Telestroke neurologist plays an active role in establishing diagnosis of stroke, ensuring inclusion/exclusion criteria for alteplase /endovascular Rx, obtaining consent, ordering alteplase, initiating administration of alteplase, and discussing with the neurointerventional radiologist whether endovascular Rx is appropriate.


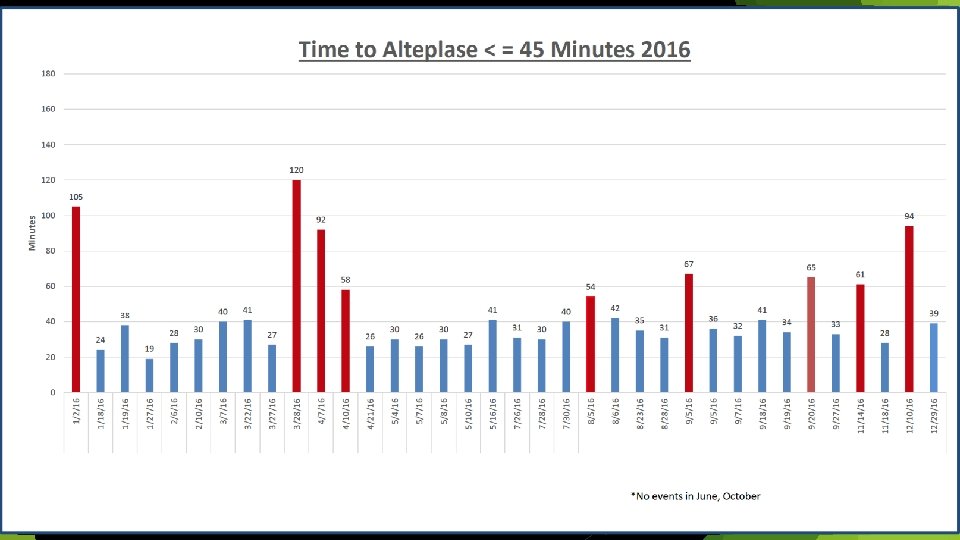
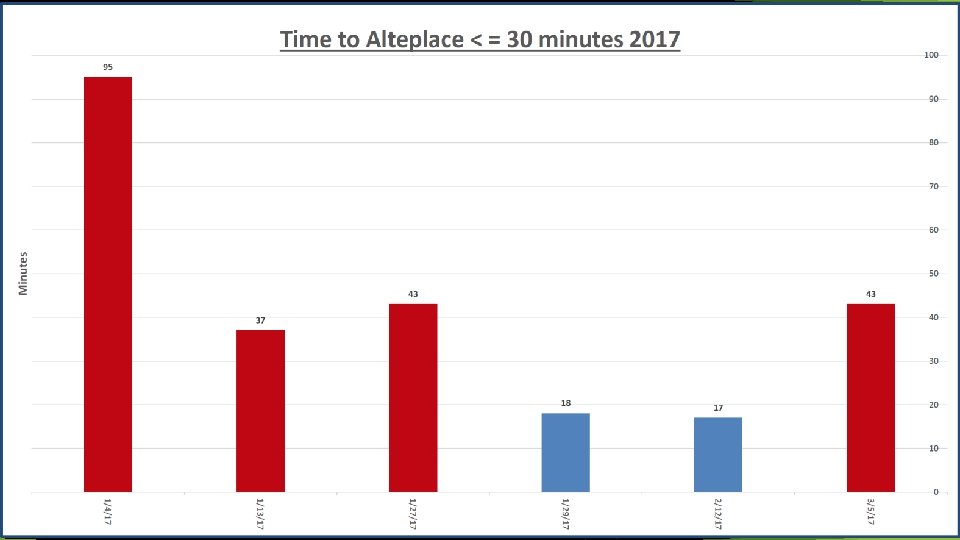
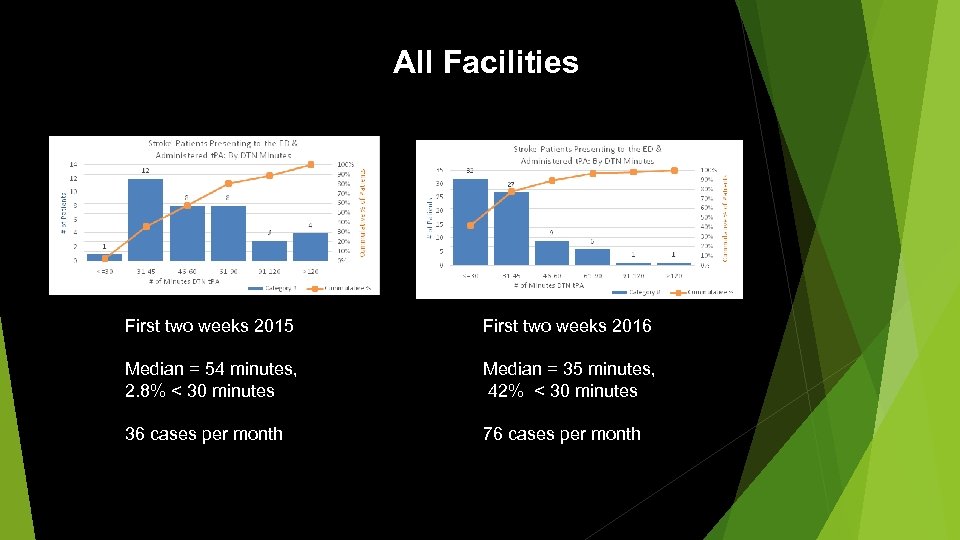 All Facilities First two weeks 2015 First two weeks 2016 Median = 54 minutes, 2. 8% < 30 minutes Median = 35 minutes, 42% < 30 minutes 36 cases per month 76 cases per month
All Facilities First two weeks 2015 First two weeks 2016 Median = 54 minutes, 2. 8% < 30 minutes Median = 35 minutes, 42% < 30 minutes 36 cases per month 76 cases per month
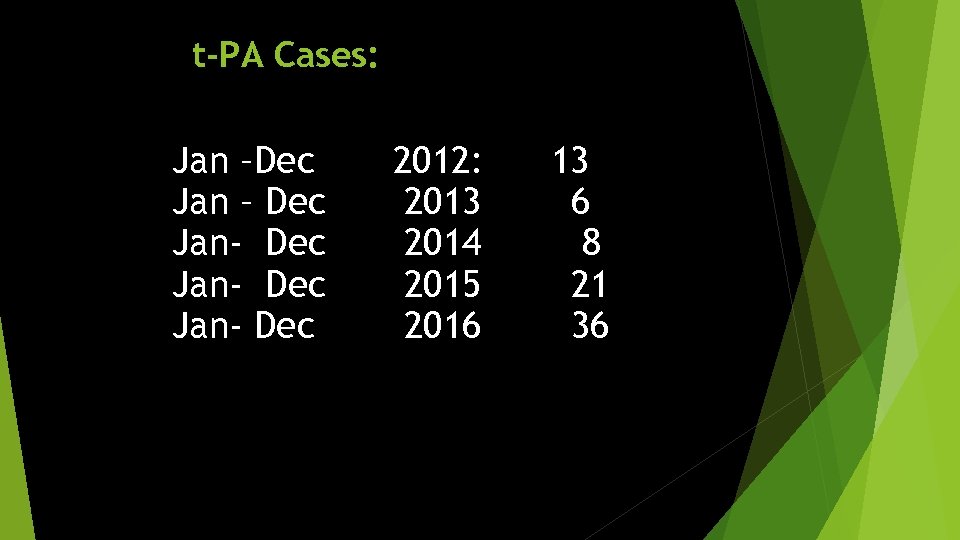 t-PA Cases: Jan –Dec Jan – Dec Jan- Dec 2012: 2013 2014 2015 2016 13 6 8 21 36
t-PA Cases: Jan –Dec Jan – Dec Jan- Dec 2012: 2013 2014 2015 2016 13 6 8 21 36
 STROKES ARE PREVENTABLE
STROKES ARE PREVENTABLE