3bb9d7317fa6d5b3850d2fc587cb2e59.ppt
- Количество слайдов: 43
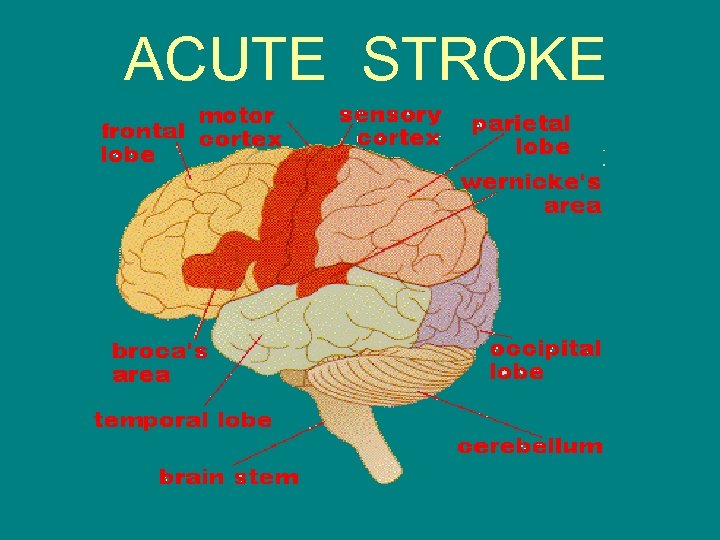 ACUTE STROKE
ACUTE STROKE
 DEFINITION • defined as a neurological deficit that has a sudden onset, lasting more than 24 hours and results from cerebrovascular disease • Occurs when there is a disruption of blood flow to a region of the brain caused by obstruction of a vessel, thrombus or embolus, or the rupture of a vessel
DEFINITION • defined as a neurological deficit that has a sudden onset, lasting more than 24 hours and results from cerebrovascular disease • Occurs when there is a disruption of blood flow to a region of the brain caused by obstruction of a vessel, thrombus or embolus, or the rupture of a vessel
 Stroke Statistics • • Affects 750, 000 people a year in US. 3 rd leading cause of death in the US 2 nd leading cause of death in the world. Leading cause of disability and long term institutionalization in the US. • Economic impact: approx. $30 billion/yr.
Stroke Statistics • • Affects 750, 000 people a year in US. 3 rd leading cause of death in the US 2 nd leading cause of death in the world. Leading cause of disability and long term institutionalization in the US. • Economic impact: approx. $30 billion/yr.
 Stroke Statistics … • Most common in the elderly, but do occur in children and young adults. • Kills twice as many women in the US than breast cancer. • 8% of Men and 11% of Women will have a stroke within 6 years of having a heart attack.
Stroke Statistics … • Most common in the elderly, but do occur in children and young adults. • Kills twice as many women in the US than breast cancer. • 8% of Men and 11% of Women will have a stroke within 6 years of having a heart attack.
 Are all ischemic strokes the same? • 3 Types of ischemic strokes: (88% of all strokes are ischemic) – 1. Thrombotic stroke – 2. Embolic stroke – 3. Systemic Hypoperfusion
Are all ischemic strokes the same? • 3 Types of ischemic strokes: (88% of all strokes are ischemic) – 1. Thrombotic stroke – 2. Embolic stroke – 3. Systemic Hypoperfusion
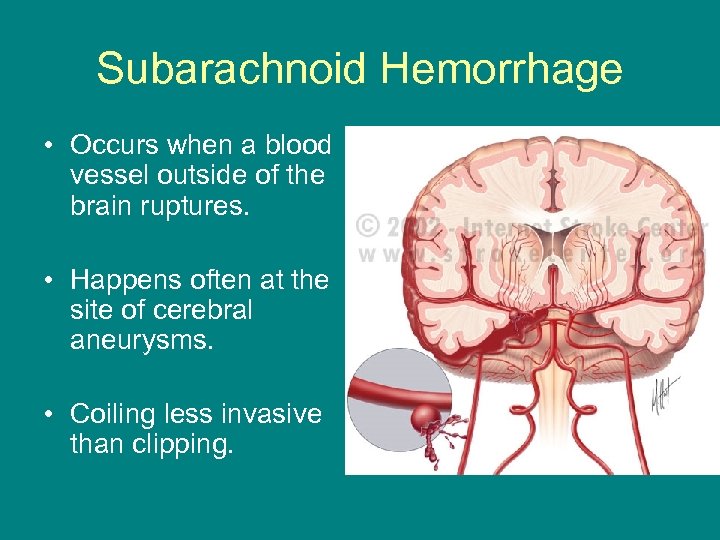 Subarachnoid Hemorrhage • Occurs when a blood vessel outside of the brain ruptures. • Happens often at the site of cerebral aneurysms. • Coiling less invasive than clipping.
Subarachnoid Hemorrhage • Occurs when a blood vessel outside of the brain ruptures. • Happens often at the site of cerebral aneurysms. • Coiling less invasive than clipping.
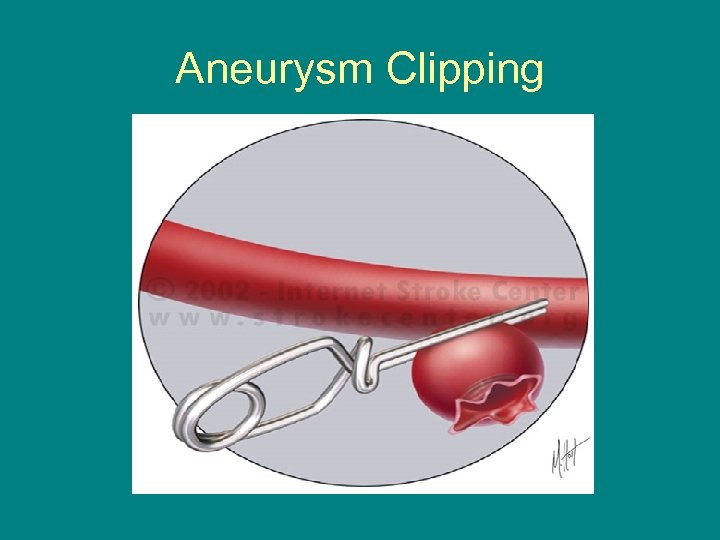 Aneurysm Clipping
Aneurysm Clipping
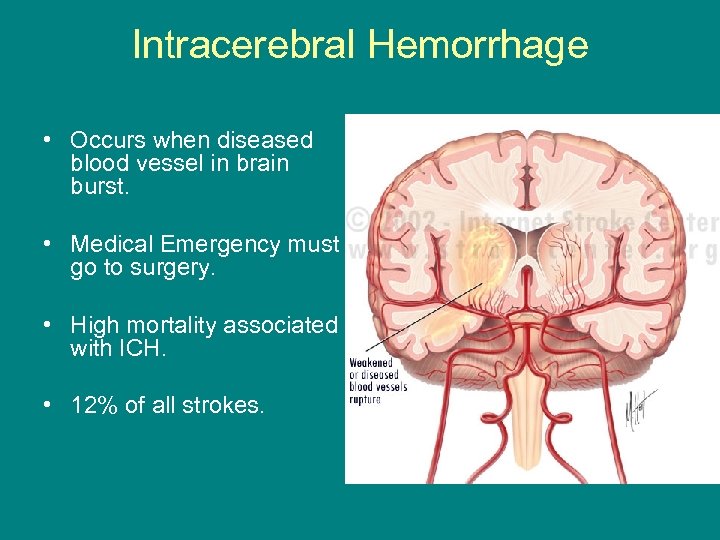 Intracerebral Hemorrhage • Occurs when diseased blood vessel in brain burst. • Medical Emergency must go to surgery. • High mortality associated with ICH. • 12% of all strokes.
Intracerebral Hemorrhage • Occurs when diseased blood vessel in brain burst. • Medical Emergency must go to surgery. • High mortality associated with ICH. • 12% of all strokes.
 Stroke Risk Factors Non-modifiable • AGE • Gender - Female • Race – Blacks > Asians or Hispanics> Whites • Family Hx. • Coagulation Disorders • Cardiac Disease
Stroke Risk Factors Non-modifiable • AGE • Gender - Female • Race – Blacks > Asians or Hispanics> Whites • Family Hx. • Coagulation Disorders • Cardiac Disease
 Stroke Risk Factors Modifiable • • Hypertension Diabetes mellitus Hypercholesterolemia Elevated LDL or Low HDL • Elevated homocystein • Smoking • Drug abuse • Alcohol Abuse • Oral Contraceptives • Pregnancy • Migraine Headaches • Obesity • Sleep apnea • Carotid stenosis A combination of these risk factors will increase risk of stroke!
Stroke Risk Factors Modifiable • • Hypertension Diabetes mellitus Hypercholesterolemia Elevated LDL or Low HDL • Elevated homocystein • Smoking • Drug abuse • Alcohol Abuse • Oral Contraceptives • Pregnancy • Migraine Headaches • Obesity • Sleep apnea • Carotid stenosis A combination of these risk factors will increase risk of stroke!
 “Brain Attack” Signs and Symptoms • SUDDEN onset of symptoms: • SUDDEN: - Dizziness or – Weakness, imbalance clumsiness, numbness or tingling on ONE side - Unusually severe of the body headache, “worst – Drooping on ONE side headache in my of the face life” - SAH – Slurred speech or difficulty understanding language
“Brain Attack” Signs and Symptoms • SUDDEN onset of symptoms: • SUDDEN: - Dizziness or – Weakness, imbalance clumsiness, numbness or tingling on ONE side - Unusually severe of the body headache, “worst – Drooping on ONE side headache in my of the face life” - SAH – Slurred speech or difficulty understanding language
 “Brain Attack” Signs and Symptoms – F. A. S. T. • F: FACE sudden drooping of ONE side of the face. • A: ARM sudden numbness, clumsiness, or weakness of ONE arm/leg. • S: SPEECH sudden difficulty speaking or understanding language: slurred speech. • T: TIME call 911 and get to the hospital immediately
“Brain Attack” Signs and Symptoms – F. A. S. T. • F: FACE sudden drooping of ONE side of the face. • A: ARM sudden numbness, clumsiness, or weakness of ONE arm/leg. • S: SPEECH sudden difficulty speaking or understanding language: slurred speech. • T: TIME call 911 and get to the hospital immediately
 NIH STROKE SCALE • http: //asa. trainingcampus. net/uas/modules /trees/windex. aspx • Free online training program for healthcare professionals. • Earn 2 contact hours for initial certification.
NIH STROKE SCALE • http: //asa. trainingcampus. net/uas/modules /trees/windex. aspx • Free online training program for healthcare professionals. • Earn 2 contact hours for initial certification.
 EMS response to 911 call: WILL QUESTION: • Time of onset of stroke symptoms. • Determine nature of neurological symptoms (F. A. S. T. ). • NIH Stroke Scale or Glasgow Coma Scale (language/motor response/eye movement). • Hx: recent illness, surgery or trauma. • Recent use of medication/illicit drugs/etoh. • Notify receiving hospital that patient appears to be an acute stroke and gives time window.
EMS response to 911 call: WILL QUESTION: • Time of onset of stroke symptoms. • Determine nature of neurological symptoms (F. A. S. T. ). • NIH Stroke Scale or Glasgow Coma Scale (language/motor response/eye movement). • Hx: recent illness, surgery or trauma. • Recent use of medication/illicit drugs/etoh. • Notify receiving hospital that patient appears to be an acute stroke and gives time window.
 “Stroke Alert” • EMS notifies receiving hospital of incoming acute stroke “running hot” – 2 peripheral 18 G IV of NS at 100 mls/hr – Oxygen at 2 L/min – HOB flat and monitor BP & HR *ECC staff prepare to meet the patient and notify radiology (CT) Staff of incoming possible stroke patient.
“Stroke Alert” • EMS notifies receiving hospital of incoming acute stroke “running hot” – 2 peripheral 18 G IV of NS at 100 mls/hr – Oxygen at 2 L/min – HOB flat and monitor BP & HR *ECC staff prepare to meet the patient and notify radiology (CT) Staff of incoming possible stroke patient.
 Stroke Alert • ECC staff receive patient from the EMS staff (RN and MD) goal: Accomplish w/in 10 mins. of arrival: – Bedside Neuro exam (NIH Stroke Scale) – Lab: CHEM 8, CBC, Coags, Type & Cross, Pregnancy test and drug screen if appropriate – Vital signs-(treat blood pressure if indicated: fever) – 12 lead EKG (common problems w/ ICH and SAH) – R/O seizure activity at the scene or in the ECC
Stroke Alert • ECC staff receive patient from the EMS staff (RN and MD) goal: Accomplish w/in 10 mins. of arrival: – Bedside Neuro exam (NIH Stroke Scale) – Lab: CHEM 8, CBC, Coags, Type & Cross, Pregnancy test and drug screen if appropriate – Vital signs-(treat blood pressure if indicated: fever) – 12 lead EKG (common problems w/ ICH and SAH) – R/O seizure activity at the scene or in the ECC
 Stroke Alert • • ECC physician confirms “acute stroke” Neurology stat consult “Stroke Alert” Neurointerventional radiology – standby Neuroscience Program coordinator (Rhonda Anderson, RN, MSN) – Notifies ICU and 9 WT re: potential admission – Notifies study coordinators of potential candidates Take patient to Radiology….
Stroke Alert • • ECC physician confirms “acute stroke” Neurology stat consult “Stroke Alert” Neurointerventional radiology – standby Neuroscience Program coordinator (Rhonda Anderson, RN, MSN) – Notifies ICU and 9 WT re: potential admission – Notifies study coordinators of potential candidates Take patient to Radiology….
 Stroke Alert • After the head CT…Radiologist will discuss findings with Neurologist Goal is to complete within 25 mins of presentation. • Determination made re: best course of treatment • Patient is screened for appropriateness for any current research studies.
Stroke Alert • After the head CT…Radiologist will discuss findings with Neurologist Goal is to complete within 25 mins of presentation. • Determination made re: best course of treatment • Patient is screened for appropriateness for any current research studies.
 Stroke Alert • If patient is candidate, then will proceed with thrombolytic therapy (t-PA). • Dosing: 0. 9 mg/kg; maximum dose less than or equal to 90 mg. – 10% of the total dose is administered as an IV bolus over 1 minute. – Remaining 90% is infused over 60 minutes – Follow up: admit to ICU or Stroke Unit, monitor Vital signs, Maintain SBP greater than 185 mm. Hg; No anticoagulant therapy for 24 hours.
Stroke Alert • If patient is candidate, then will proceed with thrombolytic therapy (t-PA). • Dosing: 0. 9 mg/kg; maximum dose less than or equal to 90 mg. – 10% of the total dose is administered as an IV bolus over 1 minute. – Remaining 90% is infused over 60 minutes – Follow up: admit to ICU or Stroke Unit, monitor Vital signs, Maintain SBP greater than 185 mm. Hg; No anticoagulant therapy for 24 hours.
 GOAL – Provide thrombolytic within 60 mins of the patient reaching the ECC. – Within the 3 hours of beginning signs and symptoms (or within 6 hours for basilar or vertebral arteries) *Must be informed on time of start of symptoms in order to treat with thrombolytic.
GOAL – Provide thrombolytic within 60 mins of the patient reaching the ECC. – Within the 3 hours of beginning signs and symptoms (or within 6 hours for basilar or vertebral arteries) *Must be informed on time of start of symptoms in order to treat with thrombolytic.
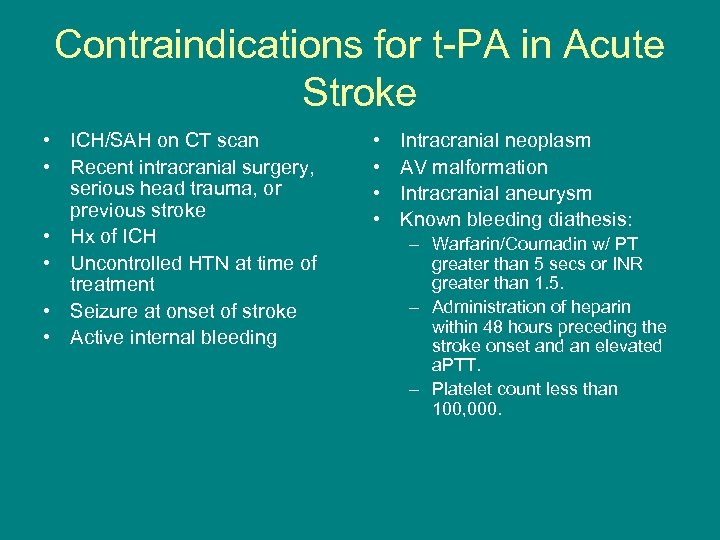 Contraindications for t-PA in Acute Stroke • ICH/SAH on CT scan • Recent intracranial surgery, serious head trauma, or previous stroke • Hx of ICH • Uncontrolled HTN at time of treatment • Seizure at onset of stroke • Active internal bleeding • • Intracranial neoplasm AV malformation Intracranial aneurysm Known bleeding diathesis: – Warfarin/Coumadin w/ PT greater than 5 secs or INR greater than 1. 5. – Administration of heparin within 48 hours preceding the stroke onset and an elevated a. PTT. – Platelet count less than 100, 000.
Contraindications for t-PA in Acute Stroke • ICH/SAH on CT scan • Recent intracranial surgery, serious head trauma, or previous stroke • Hx of ICH • Uncontrolled HTN at time of treatment • Seizure at onset of stroke • Active internal bleeding • • Intracranial neoplasm AV malformation Intracranial aneurysm Known bleeding diathesis: – Warfarin/Coumadin w/ PT greater than 5 secs or INR greater than 1. 5. – Administration of heparin within 48 hours preceding the stroke onset and an elevated a. PTT. – Platelet count less than 100, 000.
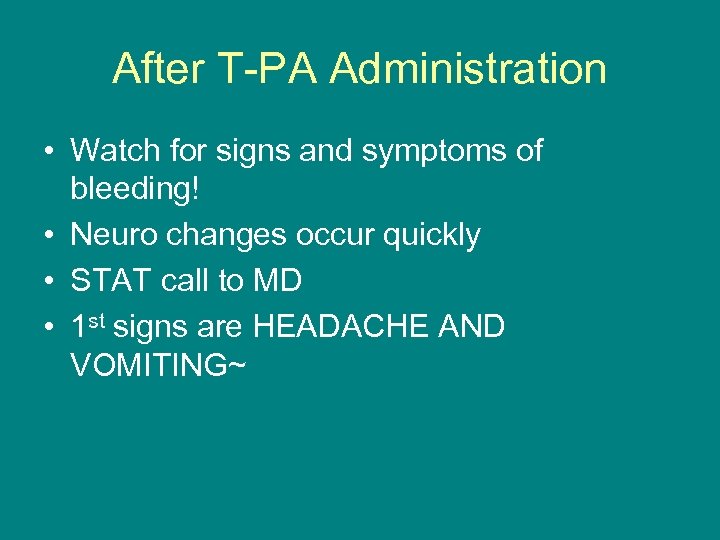 After T-PA Administration • Watch for signs and symptoms of bleeding! • Neuro changes occur quickly • STAT call to MD • 1 st signs are HEADACHE AND VOMITING~
After T-PA Administration • Watch for signs and symptoms of bleeding! • Neuro changes occur quickly • STAT call to MD • 1 st signs are HEADACHE AND VOMITING~
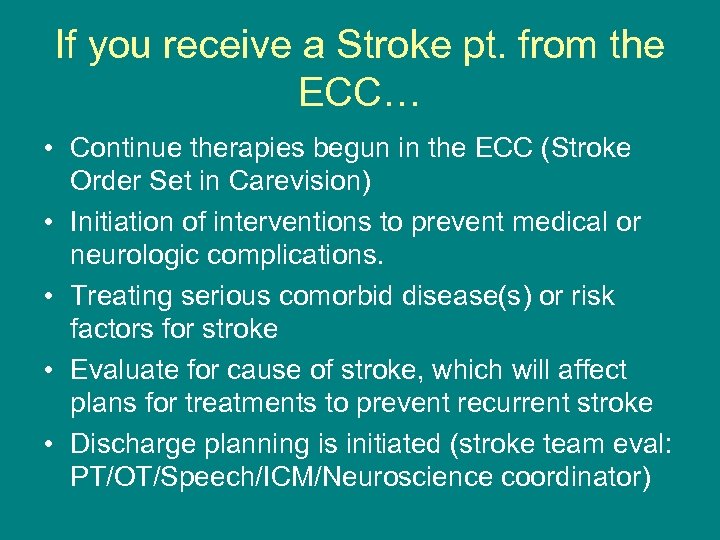 If you receive a Stroke pt. from the ECC… • Continue therapies begun in the ECC (Stroke Order Set in Carevision) • Initiation of interventions to prevent medical or neurologic complications. • Treating serious comorbid disease(s) or risk factors for stroke • Evaluate for cause of stroke, which will affect plans for treatments to prevent recurrent stroke • Discharge planning is initiated (stroke team eval: PT/OT/Speech/ICM/Neuroscience coordinator)
If you receive a Stroke pt. from the ECC… • Continue therapies begun in the ECC (Stroke Order Set in Carevision) • Initiation of interventions to prevent medical or neurologic complications. • Treating serious comorbid disease(s) or risk factors for stroke • Evaluate for cause of stroke, which will affect plans for treatments to prevent recurrent stroke • Discharge planning is initiated (stroke team eval: PT/OT/Speech/ICM/Neuroscience coordinator)
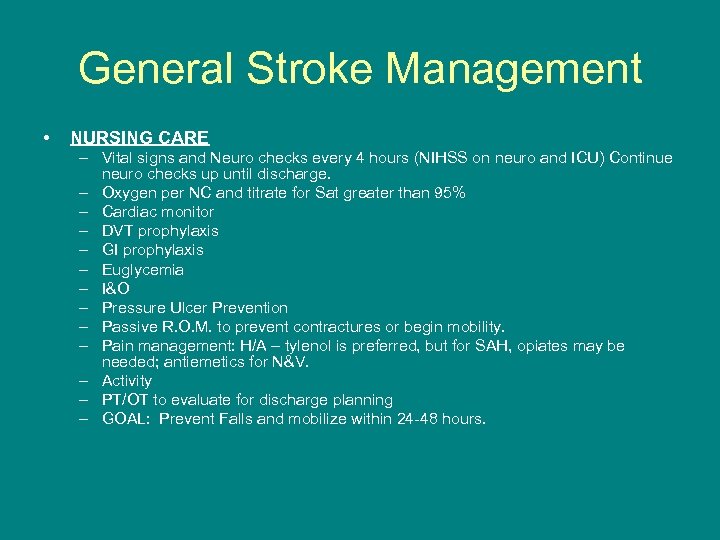 General Stroke Management • NURSING CARE – Vital signs and Neuro checks every 4 hours (NIHSS on neuro and ICU) Continue neuro checks up until discharge. – Oxygen per NC and titrate for Sat greater than 95% – Cardiac monitor – DVT prophylaxis – GI prophylaxis – Euglycemia – I&O – Pressure Ulcer Prevention – Passive R. O. M. to prevent contractures or begin mobility. – Pain management: H/A – tylenol is preferred, but for SAH, opiates may be needed; antiemetics for N&V. – Activity – PT/OT to evaluate for discharge planning – GOAL: Prevent Falls and mobilize within 24 -48 hours.
General Stroke Management • NURSING CARE – Vital signs and Neuro checks every 4 hours (NIHSS on neuro and ICU) Continue neuro checks up until discharge. – Oxygen per NC and titrate for Sat greater than 95% – Cardiac monitor – DVT prophylaxis – GI prophylaxis – Euglycemia – I&O – Pressure Ulcer Prevention – Passive R. O. M. to prevent contractures or begin mobility. – Pain management: H/A – tylenol is preferred, but for SAH, opiates may be needed; antiemetics for N&V. – Activity – PT/OT to evaluate for discharge planning – GOAL: Prevent Falls and mobilize within 24 -48 hours.
 General Acute Stroke Management • DIAGNOSTIC TESTING – 2 D Echo: ventricular or atrial clots/valve disease – Carotid Doppler studies – 12 lead EKG: atrial fibrillation – EEG if seizure activity noted – MRI or MRA
General Acute Stroke Management • DIAGNOSTIC TESTING – 2 D Echo: ventricular or atrial clots/valve disease – Carotid Doppler studies – 12 lead EKG: atrial fibrillation – EEG if seizure activity noted – MRI or MRA
 Medical Acute Stroke Management • Strategies to control any seizure activity or brain edema begun in the ECC will continue: Mannitol or Phenytoin/Depakote. • Antihypertensive management • Cholesterol lowering agents • Aspirin, if ischemic stroke • Beta Blockers to prevent cardiac complication
Medical Acute Stroke Management • Strategies to control any seizure activity or brain edema begun in the ECC will continue: Mannitol or Phenytoin/Depakote. • Antihypertensive management • Cholesterol lowering agents • Aspirin, if ischemic stroke • Beta Blockers to prevent cardiac complication
 General Management following admission to the Hospital • 10 -20 % of all stroke patients will experience a deterioration during the first 24 hours and outcomes in these patients are worse. • Neurological worsening can be due to: – – – – – Brain edema Acute hydrocephalus Seizures Progression of thrombosis Early recurrent embolization Vasospasm ->brain ischemia Continued bleeding Recurrent hemorrhage Medical Complications
General Management following admission to the Hospital • 10 -20 % of all stroke patients will experience a deterioration during the first 24 hours and outcomes in these patients are worse. • Neurological worsening can be due to: – – – – – Brain edema Acute hydrocephalus Seizures Progression of thrombosis Early recurrent embolization Vasospasm ->brain ischemia Continued bleeding Recurrent hemorrhage Medical Complications
 In-House Stroke Alerts RAPID RESPONSE TEAM • For sudden changes in Level of Consciousness or suspected stroke, call x 3911 and tell the operator to page the Rapid Response Team to room______! Staff should also STAT page the attending/primary treating physician. • RRT: ICU nurse and RT will respond, assess the patient as would EMS, and can activate the STROKE ALERT order set. ICU or Intervention RN should accompany patient to radiology.
In-House Stroke Alerts RAPID RESPONSE TEAM • For sudden changes in Level of Consciousness or suspected stroke, call x 3911 and tell the operator to page the Rapid Response Team to room______! Staff should also STAT page the attending/primary treating physician. • RRT: ICU nurse and RT will respond, assess the patient as would EMS, and can activate the STROKE ALERT order set. ICU or Intervention RN should accompany patient to radiology.
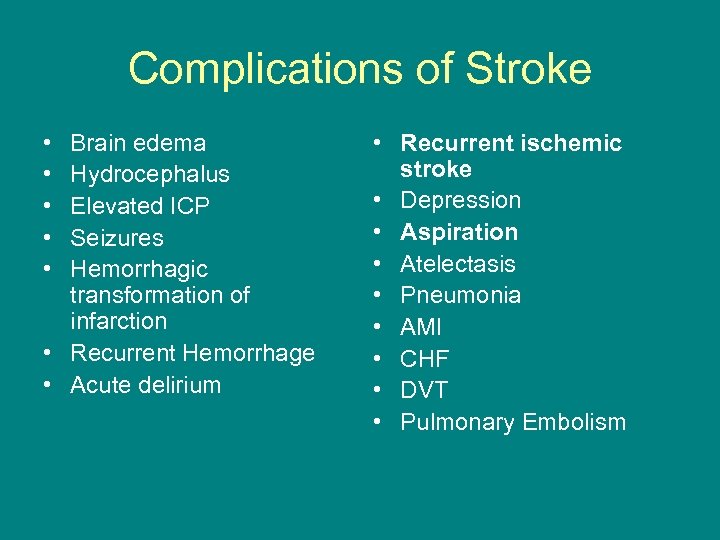 Complications of Stroke • • • Brain edema Hydrocephalus Elevated ICP Seizures Hemorrhagic transformation of infarction • Recurrent Hemorrhage • Acute delirium • Recurrent ischemic stroke • Depression • Aspiration • Atelectasis • Pneumonia • AMI • CHF • DVT • Pulmonary Embolism
Complications of Stroke • • • Brain edema Hydrocephalus Elevated ICP Seizures Hemorrhagic transformation of infarction • Recurrent Hemorrhage • Acute delirium • Recurrent ischemic stroke • Depression • Aspiration • Atelectasis • Pneumonia • AMI • CHF • DVT • Pulmonary Embolism
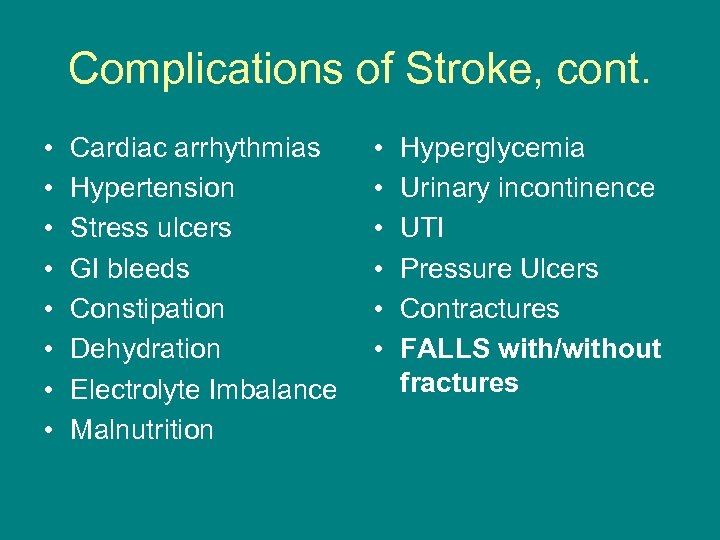 Complications of Stroke, cont. • • Cardiac arrhythmias Hypertension Stress ulcers GI bleeds Constipation Dehydration Electrolyte Imbalance Malnutrition • • • Hyperglycemia Urinary incontinence UTI Pressure Ulcers Contractures FALLS with/without fractures
Complications of Stroke, cont. • • Cardiac arrhythmias Hypertension Stress ulcers GI bleeds Constipation Dehydration Electrolyte Imbalance Malnutrition • • • Hyperglycemia Urinary incontinence UTI Pressure Ulcers Contractures FALLS with/without fractures
 Lifestyle changes to prevent a second stroke • STOP SMOKING! • Provide smoking cessation information and document your education!
Lifestyle changes to prevent a second stroke • STOP SMOKING! • Provide smoking cessation information and document your education!
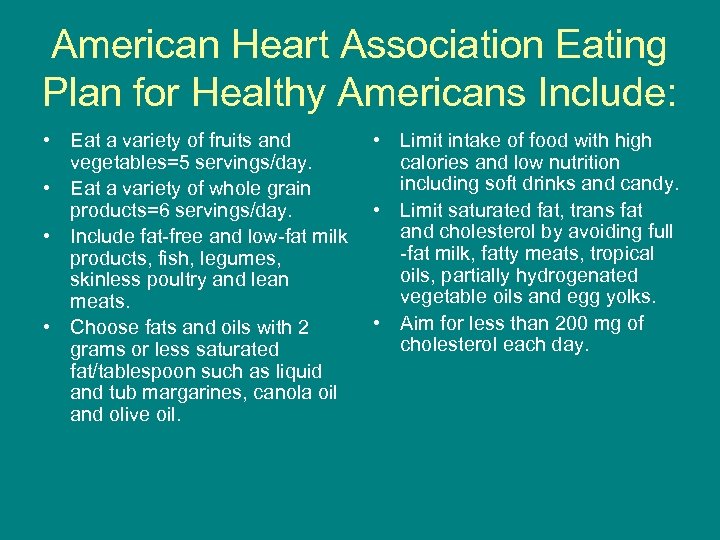 American Heart Association Eating Plan for Healthy Americans Include: • Eat a variety of fruits and vegetables=5 servings/day. • Eat a variety of whole grain products=6 servings/day. • Include fat-free and low-fat milk products, fish, legumes, skinless poultry and lean meats. • Choose fats and oils with 2 grams or less saturated fat/tablespoon such as liquid and tub margarines, canola oil and olive oil. • Limit intake of food with high calories and low nutrition including soft drinks and candy. • Limit saturated fat, trans fat and cholesterol by avoiding full -fat milk, fatty meats, tropical oils, partially hydrogenated vegetable oils and egg yolks. • Aim for less than 200 mg of cholesterol each day.
American Heart Association Eating Plan for Healthy Americans Include: • Eat a variety of fruits and vegetables=5 servings/day. • Eat a variety of whole grain products=6 servings/day. • Include fat-free and low-fat milk products, fish, legumes, skinless poultry and lean meats. • Choose fats and oils with 2 grams or less saturated fat/tablespoon such as liquid and tub margarines, canola oil and olive oil. • Limit intake of food with high calories and low nutrition including soft drinks and candy. • Limit saturated fat, trans fat and cholesterol by avoiding full -fat milk, fatty meats, tropical oils, partially hydrogenated vegetable oils and egg yolks. • Aim for less than 200 mg of cholesterol each day.
 Eating a Healthy Diet • Eating a healthy diet can help to change 3 modifiable risk factors for a second stroke: 1. Lower high cholesterol 2. Lower high blood pressure 3. Decrease extra body weight! *Stroke survivors should get less than 30% of their calories from fat, and less than 7% from saturated fat. For a 2, 000 cal diet that translated into less than 67 grams of fat/day.
Eating a Healthy Diet • Eating a healthy diet can help to change 3 modifiable risk factors for a second stroke: 1. Lower high cholesterol 2. Lower high blood pressure 3. Decrease extra body weight! *Stroke survivors should get less than 30% of their calories from fat, and less than 7% from saturated fat. For a 2, 000 cal diet that translated into less than 67 grams of fat/day.
 MANAGE CHOLESTEROL LDL and HDL GET MOVING!
MANAGE CHOLESTEROL LDL and HDL GET MOVING!
 LOWER BLOOD PRESSURE • HYPERTENSION is a major risk factor for a primary and secondary stroke. • Compliance with medical management of hypertension is crucial. • Blood Pressure readings should be below 120/80.
LOWER BLOOD PRESSURE • HYPERTENSION is a major risk factor for a primary and secondary stroke. • Compliance with medical management of hypertension is crucial. • Blood Pressure readings should be below 120/80.
 LIMIT AMOUNT OF ALCOHOL INTAKE • Women should have no more than one drink per day and men no more than two per day. • NO Illegal Drug use – IV drug abuse has high incident of stroke. (Cocaine, Meth, Heroine…)
LIMIT AMOUNT OF ALCOHOL INTAKE • Women should have no more than one drink per day and men no more than two per day. • NO Illegal Drug use – IV drug abuse has high incident of stroke. (Cocaine, Meth, Heroine…)
 MAINTAIN GOOD CONTROL OVER BLOOD GLUCOSE LEVELS Having good glycemic control will reduce the occurrence of microvascular complications that could lead to a stroke.
MAINTAIN GOOD CONTROL OVER BLOOD GLUCOSE LEVELS Having good glycemic control will reduce the occurrence of microvascular complications that could lead to a stroke.
 ANTIPLATELET ANGENTS • Stress the importance of compliance with antiplatelet agents. • Aspirin, Plavix, ticlopidine or Aggrenox will help prevent the formation of clots in small arteries as platelets stick together.
ANTIPLATELET ANGENTS • Stress the importance of compliance with antiplatelet agents. • Aspirin, Plavix, ticlopidine or Aggrenox will help prevent the formation of clots in small arteries as platelets stick together.
 EDUCATION IS KEY! • Educate patients and family members of stroke victims on modifiable risk factors and lifestyle changes that will prevent disability or death caused by a second ischemic stroke.
EDUCATION IS KEY! • Educate patients and family members of stroke victims on modifiable risk factors and lifestyle changes that will prevent disability or death caused by a second ischemic stroke.
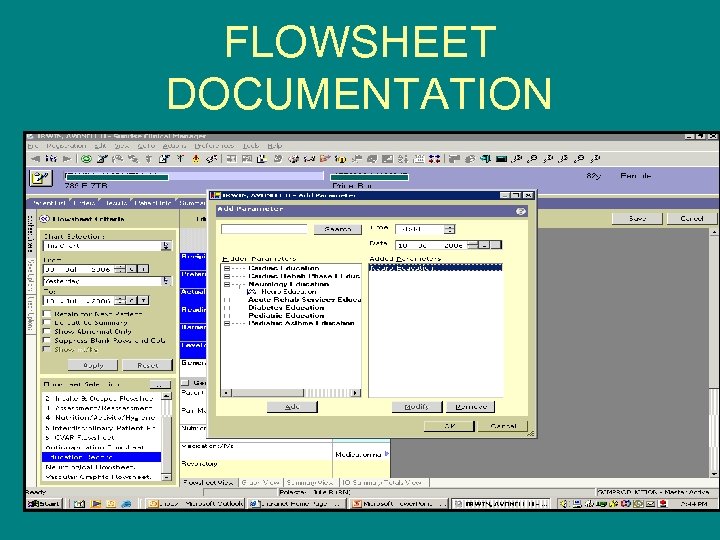 FLOWSHEET DOCUMENTATION
FLOWSHEET DOCUMENTATION
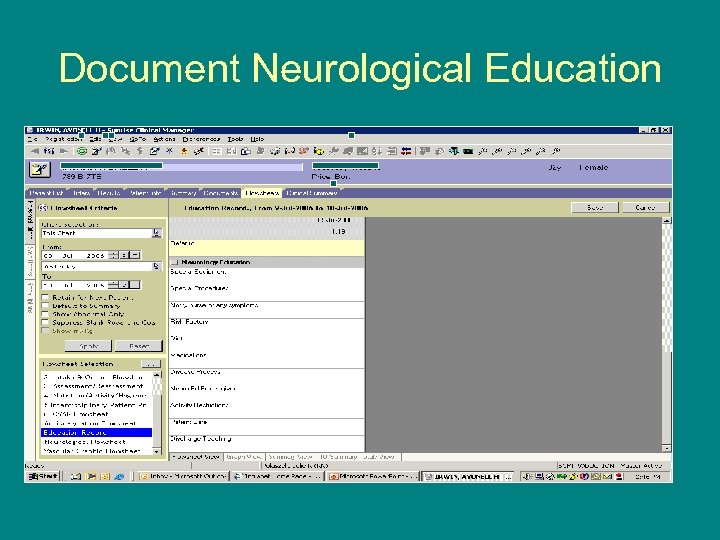 Document Neurological Education
Document Neurological Education
 Patient & Family Stroke Education Classes: Tuesdays at 11: 00 a. m. or Thursdays at 2: 00 p. m. in the 9 WT waiting room. • Patients & Families are encouraged to attend a 45 minute class to learn about: – Signs & Symptoms of Stroke – Risk Factor modification to prevent a second stroke – Medications – Stroke Recovery & Rehabilitation therapy – Discharge planning
Patient & Family Stroke Education Classes: Tuesdays at 11: 00 a. m. or Thursdays at 2: 00 p. m. in the 9 WT waiting room. • Patients & Families are encouraged to attend a 45 minute class to learn about: – Signs & Symptoms of Stroke – Risk Factor modification to prevent a second stroke – Medications – Stroke Recovery & Rehabilitation therapy – Discharge planning
 EDUCATION TOPICS FOR THE STROKE PATIENT • • Stop Smoking Healthy Diet Manage Cholesterol Increase physical activity Lower blood pressure Limit alcohol, no illicit drugs Maintain good blood sugar Take antiplatelet agents as prescribed
EDUCATION TOPICS FOR THE STROKE PATIENT • • Stop Smoking Healthy Diet Manage Cholesterol Increase physical activity Lower blood pressure Limit alcohol, no illicit drugs Maintain good blood sugar Take antiplatelet agents as prescribed


