0a121c2c315e9cd24c4e7fb0c11a5517.ppt
- Количество слайдов: 65
 Acute Respiratory Failure
Acute Respiratory Failure
 Respiratory System • Consists of two parts: • Gas exchange organ (lung): responsible for OXYGENATION • Pump (respiratory muscles and respiratory control mechanism): responsible for VENTILATION NB: Alteration in function of gas exchange unit (oxygenation) OR of the pump mechanism (ventilation) can result in respiratory failure
Respiratory System • Consists of two parts: • Gas exchange organ (lung): responsible for OXYGENATION • Pump (respiratory muscles and respiratory control mechanism): responsible for VENTILATION NB: Alteration in function of gas exchange unit (oxygenation) OR of the pump mechanism (ventilation) can result in respiratory failure
 Normal Lung
Normal Lung
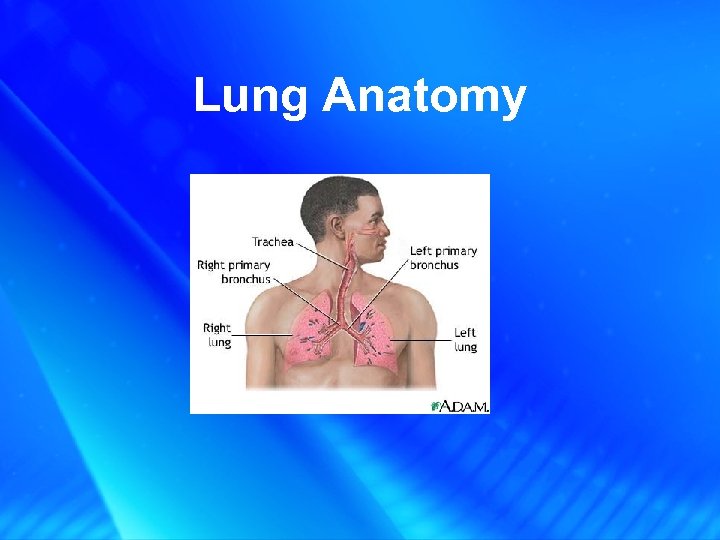 Lung Anatomy
Lung Anatomy
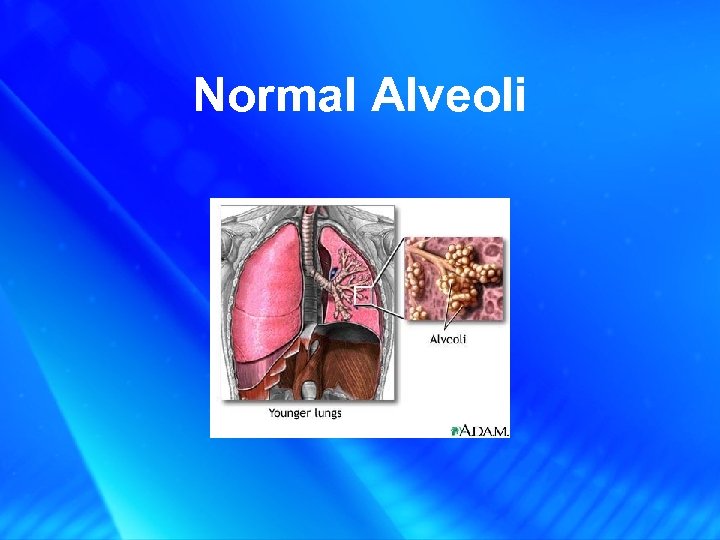 Normal Alveoli
Normal Alveoli
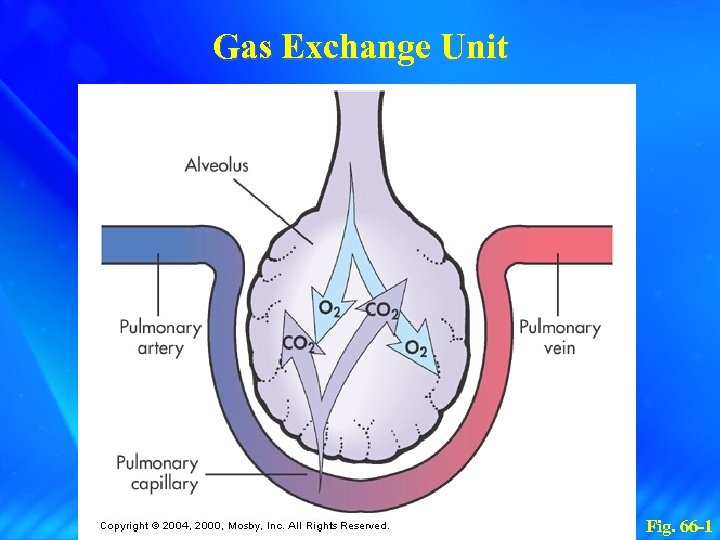 Gas Exchange Unit Fig. 66 -1
Gas Exchange Unit Fig. 66 -1
 Normal ABGs • p. H = 7. 35 -7. 45 • CO 2 = 35 -45 • HCO 3= 23 -27
Normal ABGs • p. H = 7. 35 -7. 45 • CO 2 = 35 -45 • HCO 3= 23 -27
 Respiratory and Metabolic Acidosis and Alkalosis • CO 2 is an acid and is controlled by the Respiratory (Lung) system • HCO 3 is an alkali and is controlled by the Metabolic (Renal) system • Respiratory response is immediate; Metabolic response can take up to 72 hours to respond (except in patients with COPD who are in a constant state of Compensation!)
Respiratory and Metabolic Acidosis and Alkalosis • CO 2 is an acid and is controlled by the Respiratory (Lung) system • HCO 3 is an alkali and is controlled by the Metabolic (Renal) system • Respiratory response is immediate; Metabolic response can take up to 72 hours to respond (except in patients with COPD who are in a constant state of Compensation!)
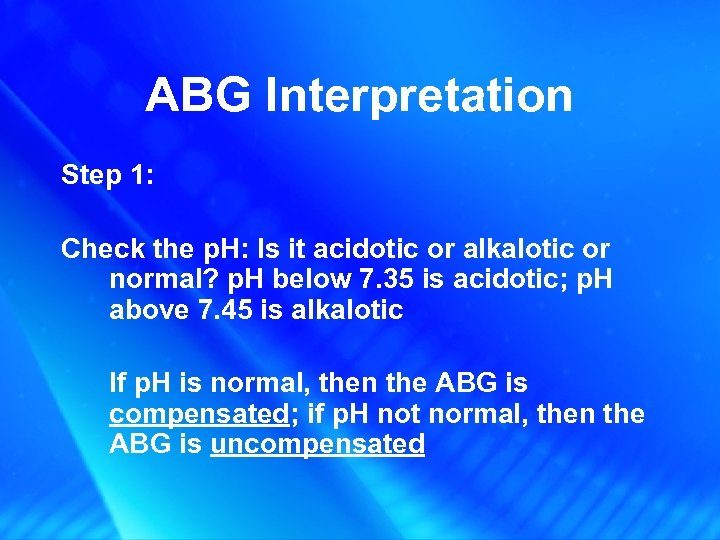 ABG Interpretation Step 1: Check the p. H: Is it acidotic or alkalotic or normal? p. H below 7. 35 is acidotic; p. H above 7. 45 is alkalotic If p. H is normal, then the ABG is compensated; if p. H not normal, then the ABG is uncompensated
ABG Interpretation Step 1: Check the p. H: Is it acidotic or alkalotic or normal? p. H below 7. 35 is acidotic; p. H above 7. 45 is alkalotic If p. H is normal, then the ABG is compensated; if p. H not normal, then the ABG is uncompensated
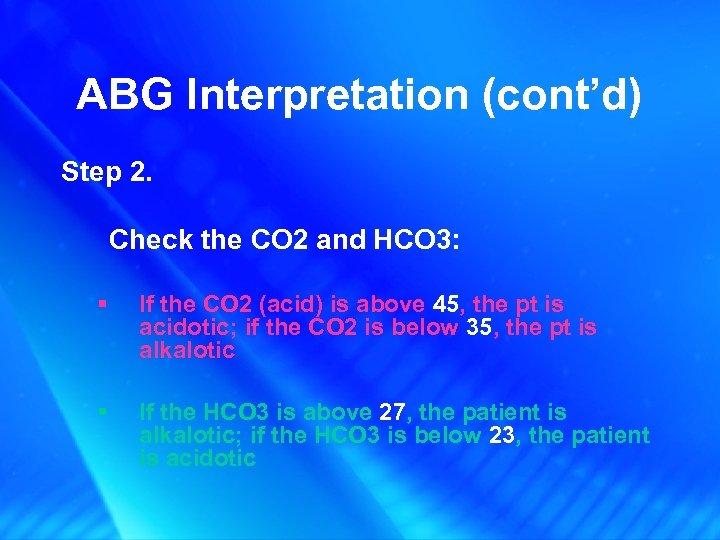 ABG Interpretation (cont’d) Step 2. Check the CO 2 and HCO 3: § If the CO 2 (acid) is above 45, the pt is acidotic; if the CO 2 is below 35, the pt is alkalotic § If the HCO 3 is above 27, the patient is alkalotic; if the HCO 3 is below 23, the patient is acidotic
ABG Interpretation (cont’d) Step 2. Check the CO 2 and HCO 3: § If the CO 2 (acid) is above 45, the pt is acidotic; if the CO 2 is below 35, the pt is alkalotic § If the HCO 3 is above 27, the patient is alkalotic; if the HCO 3 is below 23, the patient is acidotic
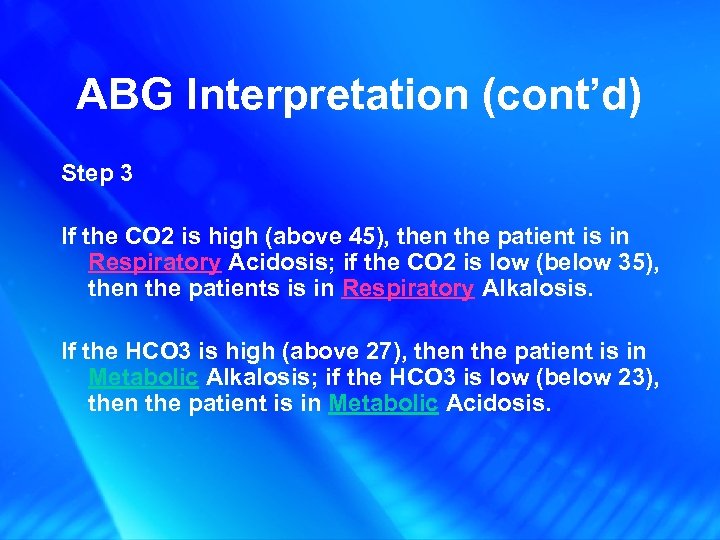 ABG Interpretation (cont’d) Step 3 If the CO 2 is high (above 45), then the patient is in Respiratory Acidosis; if the CO 2 is low (below 35), then the patients is in Respiratory Alkalosis. If the HCO 3 is high (above 27), then the patient is in Metabolic Alkalosis; if the HCO 3 is low (below 23), then the patient is in Metabolic Acidosis.
ABG Interpretation (cont’d) Step 3 If the CO 2 is high (above 45), then the patient is in Respiratory Acidosis; if the CO 2 is low (below 35), then the patients is in Respiratory Alkalosis. If the HCO 3 is high (above 27), then the patient is in Metabolic Alkalosis; if the HCO 3 is low (below 23), then the patient is in Metabolic Acidosis.
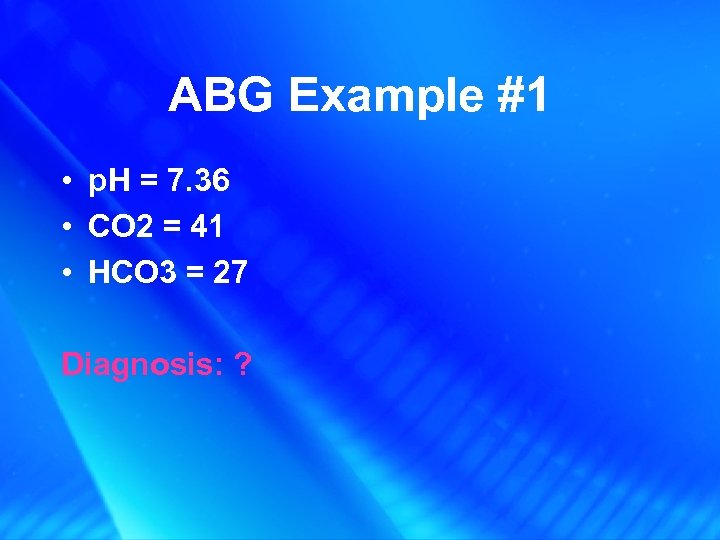 ABG Example #1 • p. H = 7. 36 • CO 2 = 41 • HCO 3 = 27 Diagnosis: ?
ABG Example #1 • p. H = 7. 36 • CO 2 = 41 • HCO 3 = 27 Diagnosis: ?
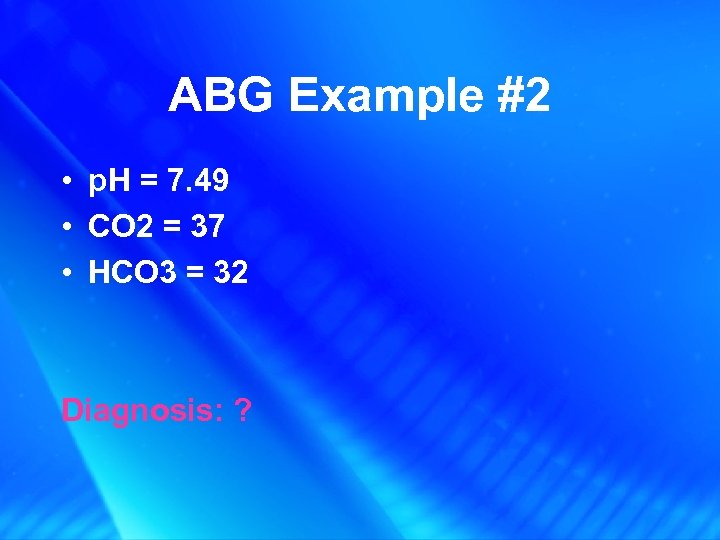 ABG Example #2 • p. H = 7. 49 • CO 2 = 37 • HCO 3 = 32 Diagnosis: ?
ABG Example #2 • p. H = 7. 49 • CO 2 = 37 • HCO 3 = 32 Diagnosis: ?
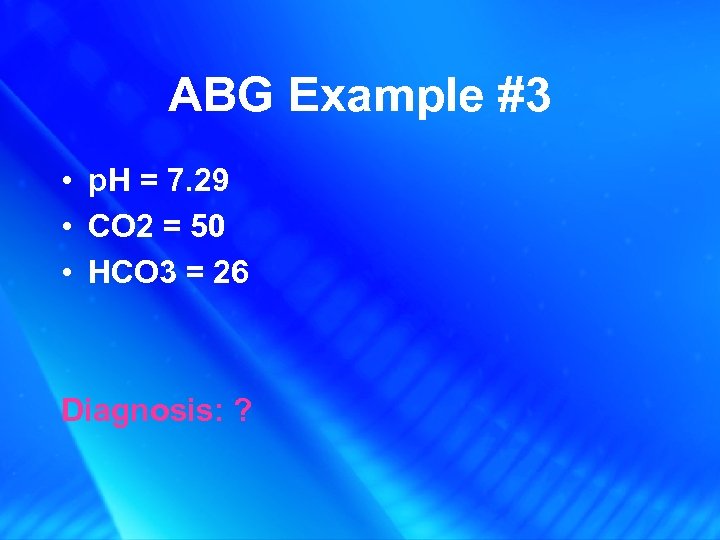 ABG Example #3 • p. H = 7. 29 • CO 2 = 50 • HCO 3 = 26 Diagnosis: ?
ABG Example #3 • p. H = 7. 29 • CO 2 = 50 • HCO 3 = 26 Diagnosis: ?
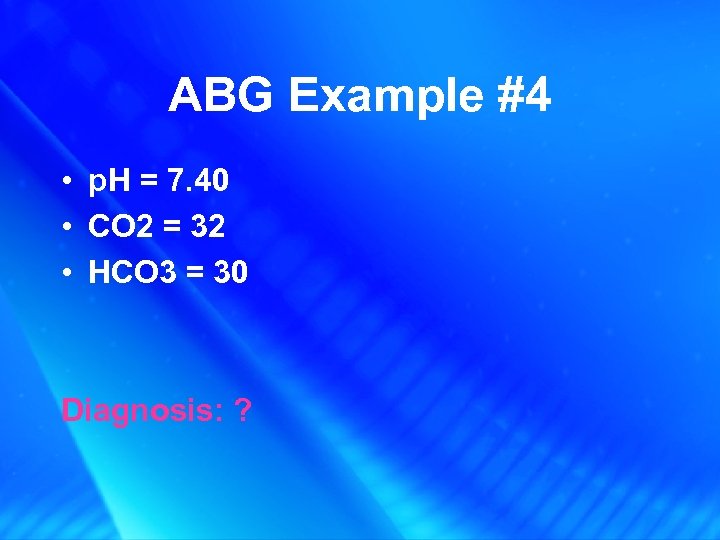 ABG Example #4 • p. H = 7. 40 • CO 2 = 32 • HCO 3 = 30 Diagnosis: ?
ABG Example #4 • p. H = 7. 40 • CO 2 = 32 • HCO 3 = 30 Diagnosis: ?
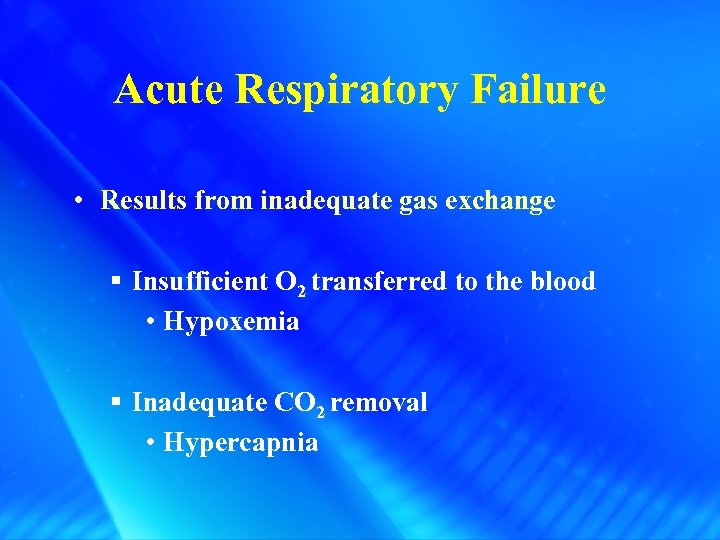 Acute Respiratory Failure • Results from inadequate gas exchange § Insufficient O 2 transferred to the blood • Hypoxemia § Inadequate CO 2 removal • Hypercapnia
Acute Respiratory Failure • Results from inadequate gas exchange § Insufficient O 2 transferred to the blood • Hypoxemia § Inadequate CO 2 removal • Hypercapnia
 Acute Respiratory Failure with Diffuse Bilateral Infiltrates
Acute Respiratory Failure with Diffuse Bilateral Infiltrates
 Acute Respiratory Failure • Not a disease but a condition • Result of one or more diseases involving the lungs or other body systems • NB: Acute Respiratory Failure: when oxygenation and/or ventilation is inadequate to meet the body’s needs
Acute Respiratory Failure • Not a disease but a condition • Result of one or more diseases involving the lungs or other body systems • NB: Acute Respiratory Failure: when oxygenation and/or ventilation is inadequate to meet the body’s needs
 Acute Respiratory Failure • Classification: – Hypoxemic respiratory failure (Failure of oxygenation) – Hypercapnic respiratory failure (Failure of ventilation)
Acute Respiratory Failure • Classification: – Hypoxemic respiratory failure (Failure of oxygenation) – Hypercapnic respiratory failure (Failure of ventilation)
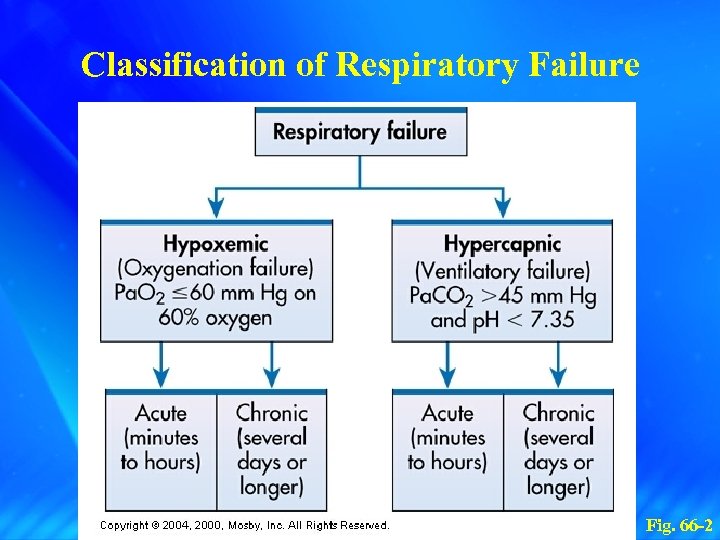 Classification of Respiratory Failure Fig. 66 -2
Classification of Respiratory Failure Fig. 66 -2
 Acute Respiratory Failure • Hypoxemic Respiratory Failure – Pa. O 2 of 60 mm Hg or less (Normal = 80 - 100 mm Hg) – Inspired O 2 concentration of 60% or greater
Acute Respiratory Failure • Hypoxemic Respiratory Failure – Pa. O 2 of 60 mm Hg or less (Normal = 80 - 100 mm Hg) – Inspired O 2 concentration of 60% or greater
 Acute Respiratory Failure • Hypercapnic Respiratory Failure – Pa. CO 2 above normal (>45 mm Hg) – Acidemia (p. H <7. 35)
Acute Respiratory Failure • Hypercapnic Respiratory Failure – Pa. CO 2 above normal (>45 mm Hg) – Acidemia (p. H <7. 35)
 Hypoxemic Respiratory Failure Etiology and Pathophysiology • Causes: – Ventilation-perfusion (V/Q) mismatch – Shunt – Diffusion limitation – Alveolar hypoventilation
Hypoxemic Respiratory Failure Etiology and Pathophysiology • Causes: – Ventilation-perfusion (V/Q) mismatch – Shunt – Diffusion limitation – Alveolar hypoventilation
 V-Q Mismatching I) V/Q mismatch • Normal ventilation of alveoli is comparable to amount of perfusion • Normal V/Q ratio is 0. 8 (more perfusion than ventilation) • Mismatch d/t: § Inadequate ventilation § Poor perfusion
V-Q Mismatching I) V/Q mismatch • Normal ventilation of alveoli is comparable to amount of perfusion • Normal V/Q ratio is 0. 8 (more perfusion than ventilation) • Mismatch d/t: § Inadequate ventilation § Poor perfusion
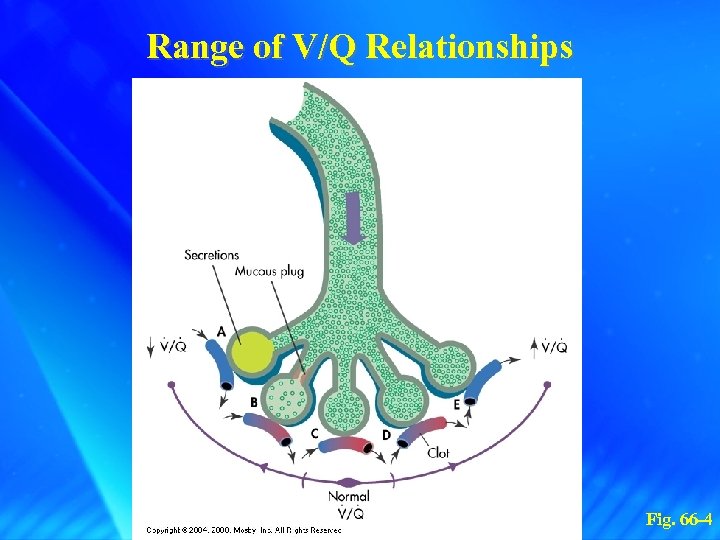 Range of V/Q Relationships Fig. 66 -4
Range of V/Q Relationships Fig. 66 -4
 Hypoxemic Respiratory Failure Etiology and Pathophysiology Causes V/Q mismatch – COPD – Pneumonia – Asthma – Atelectasis – Pulmonary embolus
Hypoxemic Respiratory Failure Etiology and Pathophysiology Causes V/Q mismatch – COPD – Pneumonia – Asthma – Atelectasis – Pulmonary embolus
 Hypoxemic Respiratory Failure Etiology and Pathophysiology II) Shunt – An extreme V/Q mismatch – Blood passes through parts of respiratory system that receives no ventilation • d/t obstruction OR fluid accumulation • Not Correctable with 100% O 2
Hypoxemic Respiratory Failure Etiology and Pathophysiology II) Shunt – An extreme V/Q mismatch – Blood passes through parts of respiratory system that receives no ventilation • d/t obstruction OR fluid accumulation • Not Correctable with 100% O 2
 Diffusion Limitations III) Diffusion Limitations • Distance between alveoli and pulmonary capillary is one- two cells thick • With diffusion abnormalities: there is an increased distance between alveoli (may be d/t fluid) • Correctable with 100% O 2
Diffusion Limitations III) Diffusion Limitations • Distance between alveoli and pulmonary capillary is one- two cells thick • With diffusion abnormalities: there is an increased distance between alveoli (may be d/t fluid) • Correctable with 100% O 2
 Hypoxemic Respiratory Failure Etiology and Pathophysiology Causes Diffusion limitations – Severe emphysema – Recurrent pulmonary emboli – Pulmonary fibrosis – Hypoxemia present during exercise
Hypoxemic Respiratory Failure Etiology and Pathophysiology Causes Diffusion limitations – Severe emphysema – Recurrent pulmonary emboli – Pulmonary fibrosis – Hypoxemia present during exercise
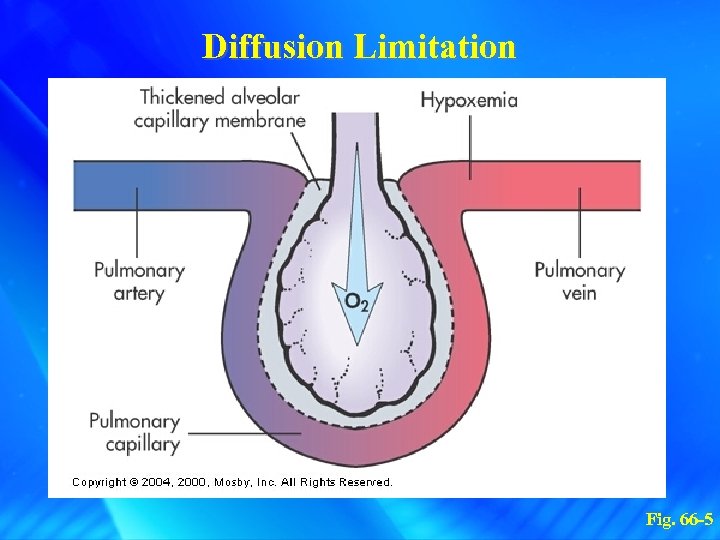 Diffusion Limitation Fig. 66 -5
Diffusion Limitation Fig. 66 -5
 Alveolar Hypoventilation IV) Alveolar Hypoventilation • Is a generalized decrease in ventilation of lungs and resultant buildup of CO 2
Alveolar Hypoventilation IV) Alveolar Hypoventilation • Is a generalized decrease in ventilation of lungs and resultant buildup of CO 2
 Hypoxemic Respiratory Failure Etiology and Pathophysiology Causes Alveolar hypoventilation – Restrictive lung disease – CNS disease – Chest wall dysfunction – Neuromuscular disease
Hypoxemic Respiratory Failure Etiology and Pathophysiology Causes Alveolar hypoventilation – Restrictive lung disease – CNS disease – Chest wall dysfunction – Neuromuscular disease
 Hypoxemic Respiratory Failure Etiology and Pathophysiology • Interrelationship of mechanisms – Hypoxemic respiratory failure is frequently caused by a combination of two or more of these four mechanisms • Effects of hypoxemia – – Build up of lactic acid → metabolic acidosis → cell death CNS depression Heart tries to compensate → ↑ HR and CO If no compensation: ↓ O 2, ↑ acid, heart fails, shock, multisystem organ failure
Hypoxemic Respiratory Failure Etiology and Pathophysiology • Interrelationship of mechanisms – Hypoxemic respiratory failure is frequently caused by a combination of two or more of these four mechanisms • Effects of hypoxemia – – Build up of lactic acid → metabolic acidosis → cell death CNS depression Heart tries to compensate → ↑ HR and CO If no compensation: ↓ O 2, ↑ acid, heart fails, shock, multisystem organ failure
 Hypercapnic Respiratory Failure Etiology and Pathophysiology • Imbalance between ventilatory supply and demand • Occurs when CO 2 is increased
Hypercapnic Respiratory Failure Etiology and Pathophysiology • Imbalance between ventilatory supply and demand • Occurs when CO 2 is increased
 Causes Hypercapnic Respiratory Failure I) Alveolar Hypoventilation and VQ Mismatch: – Ventilation not adequate to eliminate CO 2 – Leads to respiratory acidosis – Eg. Narcotic OD; Guillian-Barre, ALS, COPD, asthma
Causes Hypercapnic Respiratory Failure I) Alveolar Hypoventilation and VQ Mismatch: – Ventilation not adequate to eliminate CO 2 – Leads to respiratory acidosis – Eg. Narcotic OD; Guillian-Barre, ALS, COPD, asthma
 Causes Hypercapnic Respiratory Failure II) VQ Mismatch: - Leads to increased work of breathing - Insufficient energy to overcome resistance; ventilation falls; ↑PCO 2; respiratory acidosis
Causes Hypercapnic Respiratory Failure II) VQ Mismatch: - Leads to increased work of breathing - Insufficient energy to overcome resistance; ventilation falls; ↑PCO 2; respiratory acidosis
 Hypercapnic Respiratory Failure Categories of Causative Conditions • I) Airways and alveoli – Asthma – Emphysema – Chronic bronchitis – Cystic fibrosis
Hypercapnic Respiratory Failure Categories of Causative Conditions • I) Airways and alveoli – Asthma – Emphysema – Chronic bronchitis – Cystic fibrosis
 Hypercapnic Respiratory Failure Categories of Causative Conditions • II) Central nervous system – Drug overdose – Brainstem infarction – Spinal cord injuries
Hypercapnic Respiratory Failure Categories of Causative Conditions • II) Central nervous system – Drug overdose – Brainstem infarction – Spinal cord injuries
 Hypercapnic Respiratory Failure Categories of Causative Conditions • III) Chest wall – Flail chest – Fractures – Mechanical restriction – Muscle spasm
Hypercapnic Respiratory Failure Categories of Causative Conditions • III) Chest wall – Flail chest – Fractures – Mechanical restriction – Muscle spasm
 Hypercapnic Respiratory Failure Categories of Causative Conditions • IV) Neuromuscular conditions – Muscular dystrophy – Multiple sclerosis
Hypercapnic Respiratory Failure Categories of Causative Conditions • IV) Neuromuscular conditions – Muscular dystrophy – Multiple sclerosis
 Respiratory Failure Tissue Oxygen Needs • Major threat is the inability of the lungs to meet the oxygen demands of the tissues
Respiratory Failure Tissue Oxygen Needs • Major threat is the inability of the lungs to meet the oxygen demands of the tissues
 Respiratory Failure Clinical Manifestations • Sudden or gradual onset • A sudden in Pa. O 2 or rapid in Pa. CO 2 is a serious condition
Respiratory Failure Clinical Manifestations • Sudden or gradual onset • A sudden in Pa. O 2 or rapid in Pa. CO 2 is a serious condition
 Respiratory Failure Clinical Manifestations • When compensatory mechanisms fail, respiratory failure occurs • Signs may be specific or nonspecific
Respiratory Failure Clinical Manifestations • When compensatory mechanisms fail, respiratory failure occurs • Signs may be specific or nonspecific
 Respiratory Failure Clinical Manifestations • Severe morning headache • Cyanosis – Late sign • Tachycardia and mild hypertension – Early signs
Respiratory Failure Clinical Manifestations • Severe morning headache • Cyanosis – Late sign • Tachycardia and mild hypertension – Early signs
 Respiratory Failure Clinical Manifestations • Consequences of hypoxemia and hypoxia – Metabolic acidosis and cell death – Cardiac output – Impaired renal function
Respiratory Failure Clinical Manifestations • Consequences of hypoxemia and hypoxia – Metabolic acidosis and cell death – Cardiac output – Impaired renal function
 Respiratory Failure Clinical Manifestations • Specific clinical manifestations – Rapid, shallow breathing pattern – Sitting upright – Dyspnea
Respiratory Failure Clinical Manifestations • Specific clinical manifestations – Rapid, shallow breathing pattern – Sitting upright – Dyspnea
 Respiratory Failure Clinical Manifestations • Specific clinical manifestations – Pursed-lip breathing – Retractions – Change in Inspiratory: Expiratory ratio
Respiratory Failure Clinical Manifestations • Specific clinical manifestations – Pursed-lip breathing – Retractions – Change in Inspiratory: Expiratory ratio
 Respiratory Failure Diagnostic Studies • • • Physical assessment ABG analysis Chest x-ray CBC ECG
Respiratory Failure Diagnostic Studies • • • Physical assessment ABG analysis Chest x-ray CBC ECG
 Respiratory Failure Diagnostic Studies • • Serum electrolytes Urinalysis V/Q lung scan Pulmonary artery catheter (severe cases)
Respiratory Failure Diagnostic Studies • • Serum electrolytes Urinalysis V/Q lung scan Pulmonary artery catheter (severe cases)
 Acute Respiratory Failure Nursing and Collaborative Management • Nursing Assessment – Past health history – Medications – Surgery – Tachycardia
Acute Respiratory Failure Nursing and Collaborative Management • Nursing Assessment – Past health history – Medications – Surgery – Tachycardia
 Acute Respiratory Failure Nursing and Collaborative Management • Nursing Assessment – Fatigue – Sleep pattern changes – Headache – Restlessness
Acute Respiratory Failure Nursing and Collaborative Management • Nursing Assessment – Fatigue – Sleep pattern changes – Headache – Restlessness
 Acute Respiratory Failure Nursing and Collaborative Management • Nursing Diagnoses – Ineffective airway clearance – Ineffective breathing pattern – Risk for imbalanced fluid volume – Anxiety
Acute Respiratory Failure Nursing and Collaborative Management • Nursing Diagnoses – Ineffective airway clearance – Ineffective breathing pattern – Risk for imbalanced fluid volume – Anxiety
 Acute Respiratory Failure Nursing and Collaborative Management • Nursing Diagnoses – Impaired gas exchange – Imbalanced nutrition: less than body requirements
Acute Respiratory Failure Nursing and Collaborative Management • Nursing Diagnoses – Impaired gas exchange – Imbalanced nutrition: less than body requirements
 Acute Respiratory Failure Nursing and Collaborative Management • Planning – Overall goals: • ABGs and breath sounds within baseline • No dyspnea • Effective cough
Acute Respiratory Failure Nursing and Collaborative Management • Planning – Overall goals: • ABGs and breath sounds within baseline • No dyspnea • Effective cough
 Acute Respiratory Failure Nursing and Collaborative Management • Prevention – Thorough physical assessment – History
Acute Respiratory Failure Nursing and Collaborative Management • Prevention – Thorough physical assessment – History
 Acute Respiratory Failure Nursing and Collaborative Management • Respiratory Therapy – Oxygen therapy – Mobilization of secretions • Effective coughing and positioning
Acute Respiratory Failure Nursing and Collaborative Management • Respiratory Therapy – Oxygen therapy – Mobilization of secretions • Effective coughing and positioning
 Acute Respiratory Failure Nursing and Collaborative Management • Respiratory Therapy – Mobilization of secretions • Hydration and humidification • Chest physical therapy • Airway suctioning
Acute Respiratory Failure Nursing and Collaborative Management • Respiratory Therapy – Mobilization of secretions • Hydration and humidification • Chest physical therapy • Airway suctioning
 Acute Respiratory Failure Nursing and Collaborative Management • Respiratory Therapy – Positive pressure ventilation (PPV)
Acute Respiratory Failure Nursing and Collaborative Management • Respiratory Therapy – Positive pressure ventilation (PPV)
 Acute Respiratory Failure Nursing and Collaborative Management • Drug Therapy – Relief of bronchospasm • Bronchodilators
Acute Respiratory Failure Nursing and Collaborative Management • Drug Therapy – Relief of bronchospasm • Bronchodilators
 Acute Respiratory Failure Nursing and Collaborative Management • Drug Therapy – Reduction of airway inflammation • Corticosteroids
Acute Respiratory Failure Nursing and Collaborative Management • Drug Therapy – Reduction of airway inflammation • Corticosteroids
 Acute Respiratory Failure Nursing and Collaborative Management • Drug Therapy – Reduction of pulmonary congestion • IV diuretics
Acute Respiratory Failure Nursing and Collaborative Management • Drug Therapy – Reduction of pulmonary congestion • IV diuretics
 Acute Respiratory Failure Nursing and Collaborative Management • Drug Therapy – Treatment of pulmonary infections • IV antibiotics
Acute Respiratory Failure Nursing and Collaborative Management • Drug Therapy – Treatment of pulmonary infections • IV antibiotics
 Acute Respiratory Failure Nursing and Collaborative Management • Drug Therapy – Reduction of severe anxiety, pain, and agitation • Benzodiazepines • Narcotics
Acute Respiratory Failure Nursing and Collaborative Management • Drug Therapy – Reduction of severe anxiety, pain, and agitation • Benzodiazepines • Narcotics
 Acute Respiratory Failure Nursing and Collaborative Management • Medical Supportive Therapy – Treat the underlying cause – Maintain adequate cardiac output and hemoglobin concentration – Monitor BP, O 2 saturation, urine output
Acute Respiratory Failure Nursing and Collaborative Management • Medical Supportive Therapy – Treat the underlying cause – Maintain adequate cardiac output and hemoglobin concentration – Monitor BP, O 2 saturation, urine output
 Acute Respiratory Failure Nursing and Collaborative Management • Nutritional Therapy – Maintain protein and energy stores – Enteral or parenteral nutrition – Supplements
Acute Respiratory Failure Nursing and Collaborative Management • Nutritional Therapy – Maintain protein and energy stores – Enteral or parenteral nutrition – Supplements


