7c5af3e2f530f398ba4c51359fb3a757.ppt
- Количество слайдов: 42
 Acute Renal Replacement Therapy for the Infant Jordan M. Symons, MD University of Washington School of Medicine Children’s Hospital & Regional Medical Center Seattle, WA jordan. symons@seattlechildrens. org
Acute Renal Replacement Therapy for the Infant Jordan M. Symons, MD University of Washington School of Medicine Children’s Hospital & Regional Medical Center Seattle, WA jordan. symons@seattlechildrens. org
 Objectives • Indications and goals for acute renal replacement therapy • Modalities for renal replacement therapy – Peritoneal dialysis – Intermittent hemodialysis – Continuous renal replacement therapy (CRRT) • Special issues related to the infant
Objectives • Indications and goals for acute renal replacement therapy • Modalities for renal replacement therapy – Peritoneal dialysis – Intermittent hemodialysis – Continuous renal replacement therapy (CRRT) • Special issues related to the infant
 Indications for Renal Replacement • • Volume overload Metabolic imbalance Toxins (endogenous or exogenous) Inability to provide needed daily fluids due to insufficient urinary excretion
Indications for Renal Replacement • • Volume overload Metabolic imbalance Toxins (endogenous or exogenous) Inability to provide needed daily fluids due to insufficient urinary excretion
 Goals of Renal Replacement • Restore fluid, electrolyte and metabolic balance • Remove endogenous or exogenous toxins as rapidly as possible • Permit needed therapy and nutrition • Limit complications
Goals of Renal Replacement • Restore fluid, electrolyte and metabolic balance • Remove endogenous or exogenous toxins as rapidly as possible • Permit needed therapy and nutrition • Limit complications
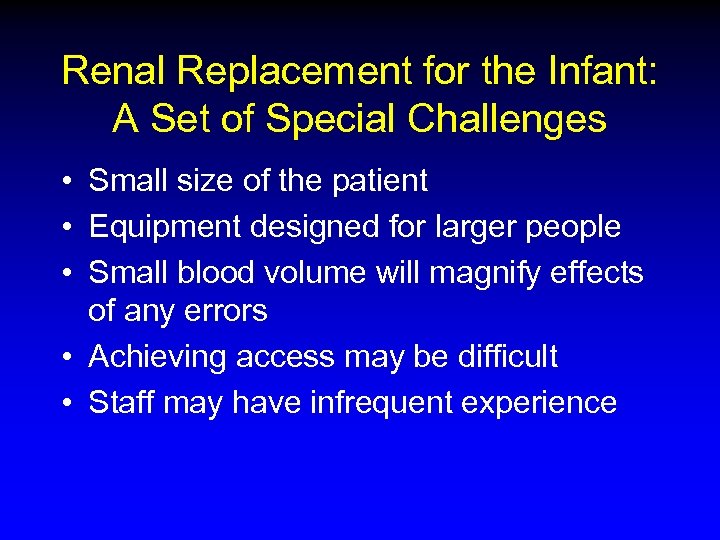 Renal Replacement for the Infant: A Set of Special Challenges • Small size of the patient • Equipment designed for larger people • Small blood volume will magnify effects of any errors • Achieving access may be difficult • Staff may have infrequent experience
Renal Replacement for the Infant: A Set of Special Challenges • Small size of the patient • Equipment designed for larger people • Small blood volume will magnify effects of any errors • Achieving access may be difficult • Staff may have infrequent experience
 Modalities for Renal Replacement • Peritoneal dialysis • Intermittent hemodialysis • Continuous renal replacement therapy (CRRT)
Modalities for Renal Replacement • Peritoneal dialysis • Intermittent hemodialysis • Continuous renal replacement therapy (CRRT)
 Modalities for Renal Replacement • Peritoneal dialysis • Intermittent hemodialysis • Continuous renal replacement therapy (CRRT)
Modalities for Renal Replacement • Peritoneal dialysis • Intermittent hemodialysis • Continuous renal replacement therapy (CRRT)
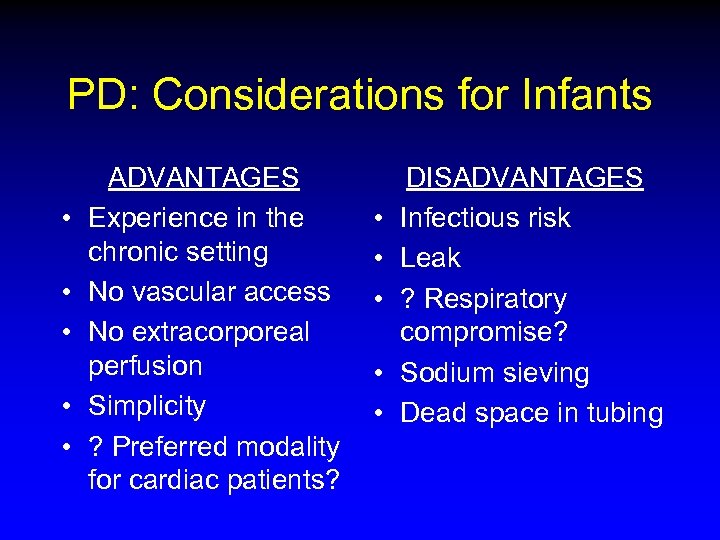 PD: Considerations for Infants • • • ADVANTAGES Experience in the chronic setting No vascular access No extracorporeal perfusion Simplicity ? Preferred modality for cardiac patients? • • • DISADVANTAGES Infectious risk Leak ? Respiratory compromise? Sodium sieving Dead space in tubing
PD: Considerations for Infants • • • ADVANTAGES Experience in the chronic setting No vascular access No extracorporeal perfusion Simplicity ? Preferred modality for cardiac patients? • • • DISADVANTAGES Infectious risk Leak ? Respiratory compromise? Sodium sieving Dead space in tubing
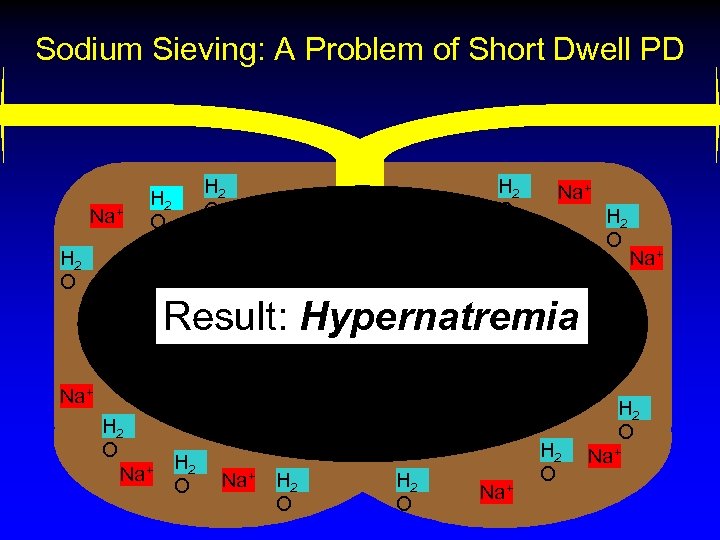 Sodium Sieving: A Problem of Short Dwell PD Na+ H 2 O Na+ H 2 O Na+ Result: Hypernatremia Na+ H 2 O H 2 O Na+
Sodium Sieving: A Problem of Short Dwell PD Na+ H 2 O Na+ H 2 O Na+ Result: Hypernatremia Na+ H 2 O H 2 O Na+
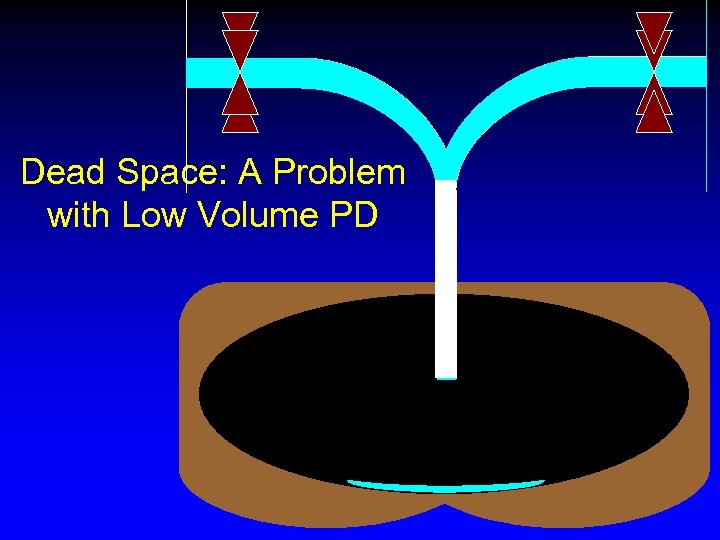 Dead Space: A Problem with Low Volume PD
Dead Space: A Problem with Low Volume PD
 Modalities for Renal Replacement • Peritoneal dialysis • Intermittent hemodialysis • Continuous renal replacement therapy (CRRT)
Modalities for Renal Replacement • Peritoneal dialysis • Intermittent hemodialysis • Continuous renal replacement therapy (CRRT)
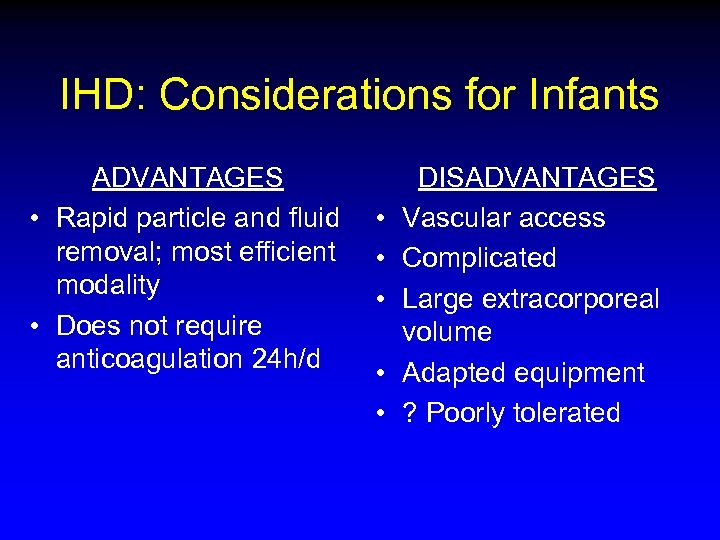 IHD: Considerations for Infants ADVANTAGES • Rapid particle and fluid removal; most efficient modality • Does not require anticoagulation 24 h/d • • • DISADVANTAGES Vascular access Complicated Large extracorporeal volume Adapted equipment ? Poorly tolerated
IHD: Considerations for Infants ADVANTAGES • Rapid particle and fluid removal; most efficient modality • Does not require anticoagulation 24 h/d • • • DISADVANTAGES Vascular access Complicated Large extracorporeal volume Adapted equipment ? Poorly tolerated
 Modalities for Renal Replacement • Peritoneal dialysis • Intermittent hemodialysis • Continuous renal replacement therapy (CRRT)
Modalities for Renal Replacement • Peritoneal dialysis • Intermittent hemodialysis • Continuous renal replacement therapy (CRRT)
 Pediatric CRRT: Vicenza, 1984
Pediatric CRRT: Vicenza, 1984
 CRRT for Infants: A Series of Challenges • • • Small patient with small blood volume Equipment designed for bigger people No specific protocols Complications may be magnified No clear guidelines Limited outcome data
CRRT for Infants: A Series of Challenges • • • Small patient with small blood volume Equipment designed for bigger people No specific protocols Complications may be magnified No clear guidelines Limited outcome data
 Potential Complications of Infant CRRT • • • Volume related problems Biochemical and nutritional problems Hemorrhage, infection Thermic loss Technical problems Logistical problems
Potential Complications of Infant CRRT • • • Volume related problems Biochemical and nutritional problems Hemorrhage, infection Thermic loss Technical problems Logistical problems
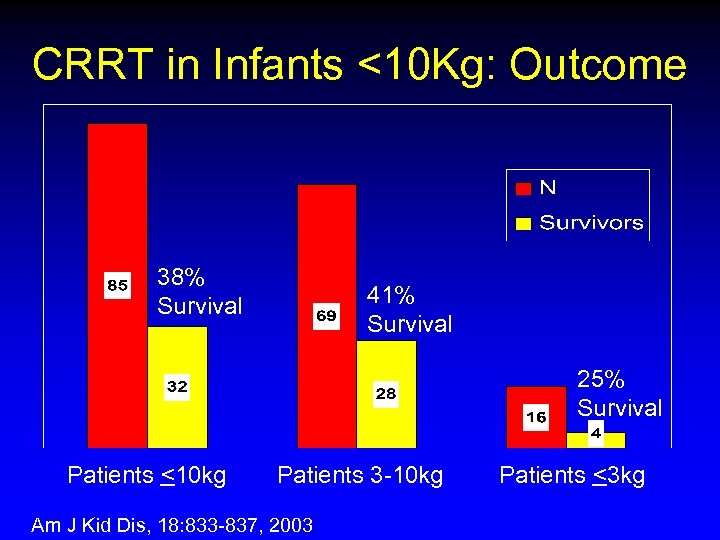 CRRT in Infants <10 Kg: Outcome 38% Survival 41% Survival 25% Survival Patients <10 kg Patients 3 -10 kg Am J Kid Dis, 18: 833 -837, 2003 Patients <3 kg
CRRT in Infants <10 Kg: Outcome 38% Survival 41% Survival 25% Survival Patients <10 kg Patients 3 -10 kg Am J Kid Dis, 18: 833 -837, 2003 Patients <3 kg
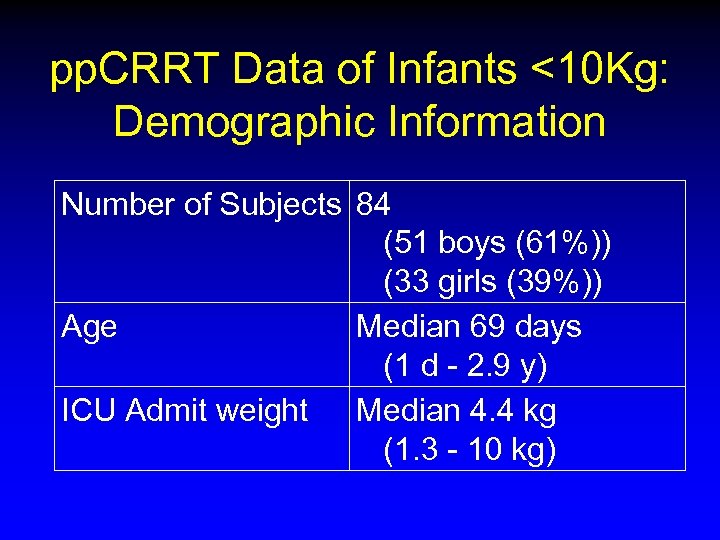 pp. CRRT Data of Infants <10 Kg: Demographic Information Number of Subjects 84 (51 boys (61%)) (33 girls (39%)) Age Median 69 days (1 d - 2. 9 y) ICU Admit weight Median 4. 4 kg (1. 3 - 10 kg)
pp. CRRT Data of Infants <10 Kg: Demographic Information Number of Subjects 84 (51 boys (61%)) (33 girls (39%)) Age Median 69 days (1 d - 2. 9 y) ICU Admit weight Median 4. 4 kg (1. 3 - 10 kg)
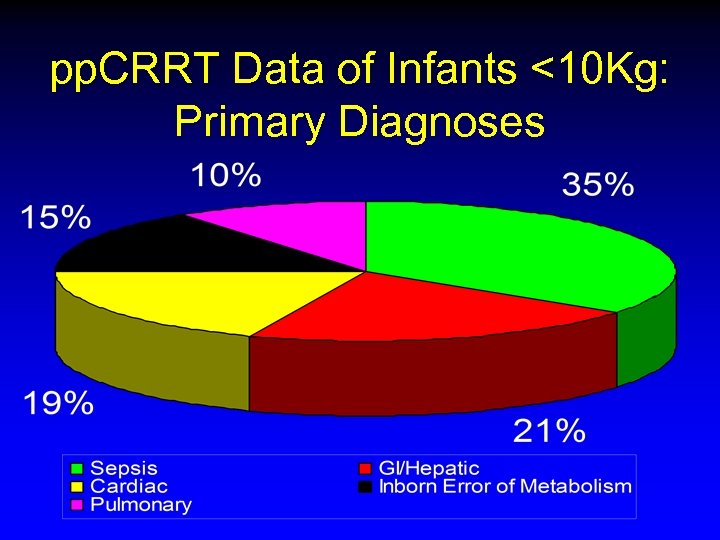 pp. CRRT Data of Infants <10 Kg: Primary Diagnoses
pp. CRRT Data of Infants <10 Kg: Primary Diagnoses
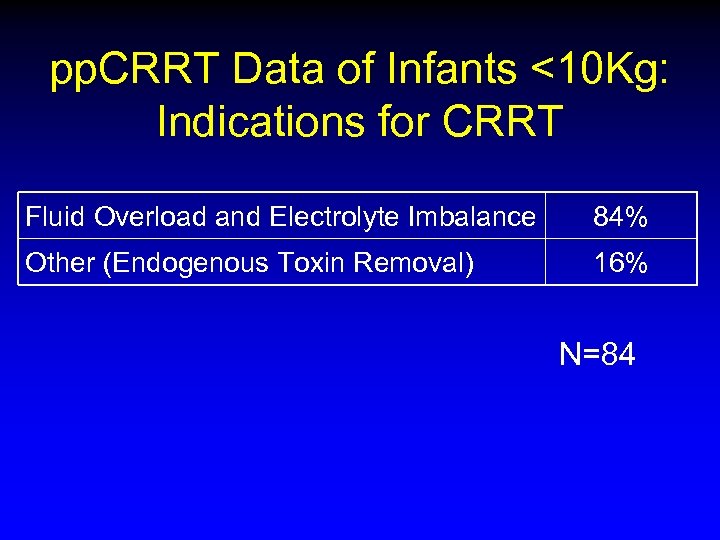 pp. CRRT Data of Infants <10 Kg: Indications for CRRT Fluid Overload and Electrolyte Imbalance 84% Other (Endogenous Toxin Removal) 16% N=84
pp. CRRT Data of Infants <10 Kg: Indications for CRRT Fluid Overload and Electrolyte Imbalance 84% Other (Endogenous Toxin Removal) 16% N=84
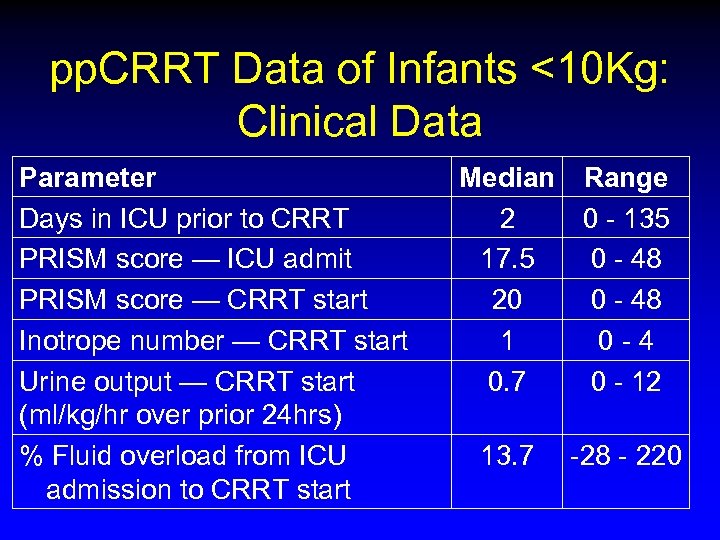 pp. CRRT Data of Infants <10 Kg: Clinical Data Parameter Days in ICU prior to CRRT PRISM score — ICU admit PRISM score — CRRT start Inotrope number — CRRT start Urine output — CRRT start (ml/kg/hr over prior 24 hrs) % Fluid overload from ICU admission to CRRT start Median Range 2 0 - 135 17. 5 0 - 48 20 0 - 48 1 0 -4 0. 7 0 - 12 13. 7 -28 - 220
pp. CRRT Data of Infants <10 Kg: Clinical Data Parameter Days in ICU prior to CRRT PRISM score — ICU admit PRISM score — CRRT start Inotrope number — CRRT start Urine output — CRRT start (ml/kg/hr over prior 24 hrs) % Fluid overload from ICU admission to CRRT start Median Range 2 0 - 135 17. 5 0 - 48 20 0 - 48 1 0 -4 0. 7 0 - 12 13. 7 -28 - 220
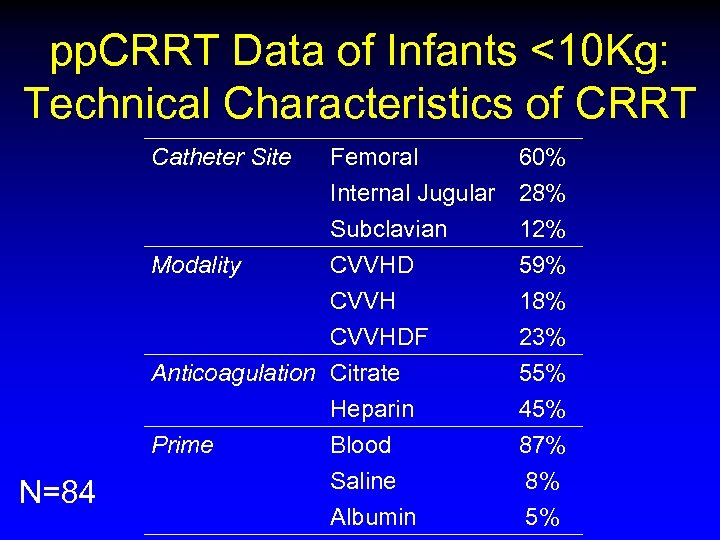 pp. CRRT Data of Infants <10 Kg: Technical Characteristics of CRRT Catheter Site Modality N=84 Femoral Internal Jugular Subclavian CVVHDF Anticoagulation Citrate Heparin Prime Blood Saline Albumin 60% 28% 12% 59% 18% 23% 55% 45% 87% 8% 5%
pp. CRRT Data of Infants <10 Kg: Technical Characteristics of CRRT Catheter Site Modality N=84 Femoral Internal Jugular Subclavian CVVHDF Anticoagulation Citrate Heparin Prime Blood Saline Albumin 60% 28% 12% 59% 18% 23% 55% 45% 87% 8% 5%
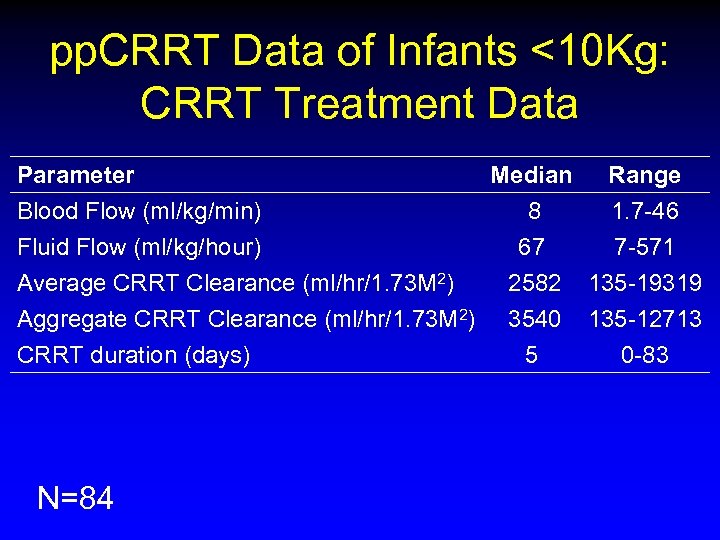 pp. CRRT Data of Infants <10 Kg: CRRT Treatment Data Parameter Blood Flow (ml/kg/min) Fluid Flow (ml/kg/hour) Average CRRT Clearance (ml/hr/1. 73 M 2) Aggregate CRRT Clearance (ml/hr/1. 73 M 2) CRRT duration (days) N=84 Median Range 8 1. 7 -46 67 7 -571 2582 135 -19319 3540 5 135 -12713 0 -83
pp. CRRT Data of Infants <10 Kg: CRRT Treatment Data Parameter Blood Flow (ml/kg/min) Fluid Flow (ml/kg/hour) Average CRRT Clearance (ml/hr/1. 73 M 2) Aggregate CRRT Clearance (ml/hr/1. 73 M 2) CRRT duration (days) N=84 Median Range 8 1. 7 -46 67 7 -571 2582 135 -19319 3540 5 135 -12713 0 -83
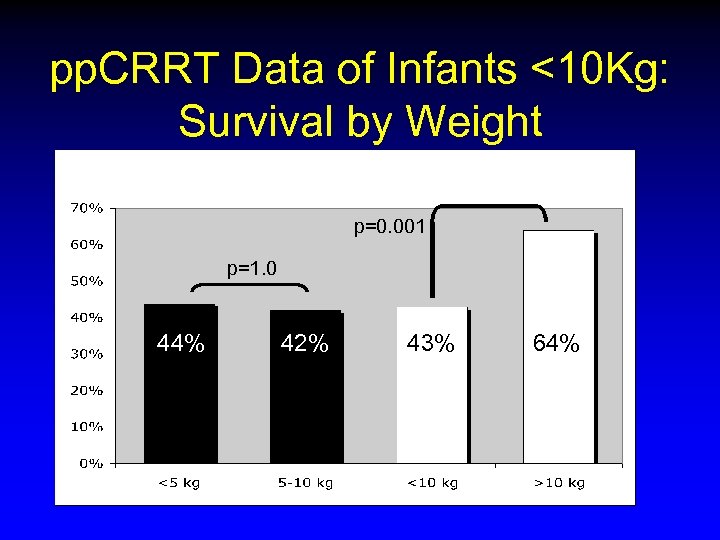 pp. CRRT Data of Infants <10 Kg: Survival by Weight p=0. 001 p=1. 0 44% 42% 43% 64%
pp. CRRT Data of Infants <10 Kg: Survival by Weight p=0. 001 p=1. 0 44% 42% 43% 64%
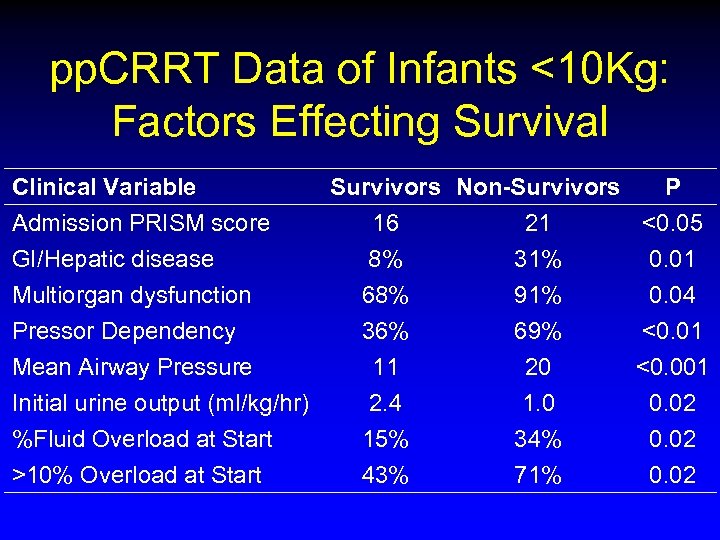 pp. CRRT Data of Infants <10 Kg: Factors Effecting Survival Clinical Variable Admission PRISM score GI/Hepatic disease Multiorgan dysfunction Pressor Dependency Mean Airway Pressure Initial urine output (ml/kg/hr) %Fluid Overload at Start >10% Overload at Start Survivors Non-Survivors P 16 21 <0. 05 8% 31% 0. 01 68% 91% 0. 04 36% 11 2. 4 15% 43% 69% 20 1. 0 34% 71% <0. 01 <0. 001 0. 02
pp. CRRT Data of Infants <10 Kg: Factors Effecting Survival Clinical Variable Admission PRISM score GI/Hepatic disease Multiorgan dysfunction Pressor Dependency Mean Airway Pressure Initial urine output (ml/kg/hr) %Fluid Overload at Start >10% Overload at Start Survivors Non-Survivors P 16 21 <0. 05 8% 31% 0. 01 68% 91% 0. 04 36% 11 2. 4 15% 43% 69% 20 1. 0 34% 71% <0. 01 <0. 001 0. 02
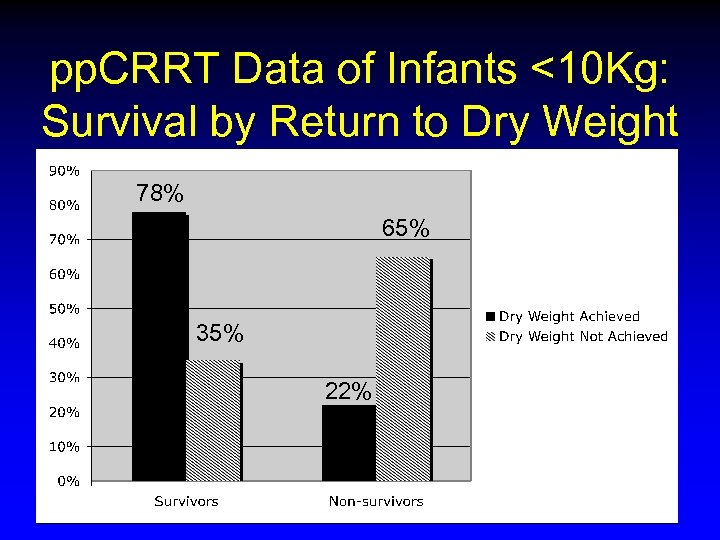 pp. CRRT Data of Infants <10 Kg: Survival by Return to Dry Weight 78% 65% 35% 22%
pp. CRRT Data of Infants <10 Kg: Survival by Return to Dry Weight 78% 65% 35% 22%
 Infant CRRT at Children’s Hospital & Regional Medical Center, Seattle
Infant CRRT at Children’s Hospital & Regional Medical Center, Seattle
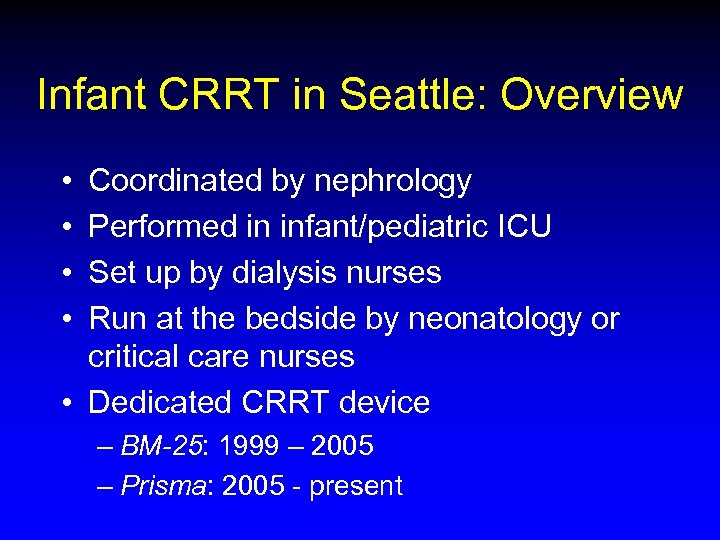 Infant CRRT in Seattle: Overview • • Coordinated by nephrology Performed in infant/pediatric ICU Set up by dialysis nurses Run at the bedside by neonatology or critical care nurses • Dedicated CRRT device – BM-25: 1999 – 2005 – Prisma: 2005 - present
Infant CRRT in Seattle: Overview • • Coordinated by nephrology Performed in infant/pediatric ICU Set up by dialysis nurses Run at the bedside by neonatology or critical care nurses • Dedicated CRRT device – BM-25: 1999 – 2005 – Prisma: 2005 - present
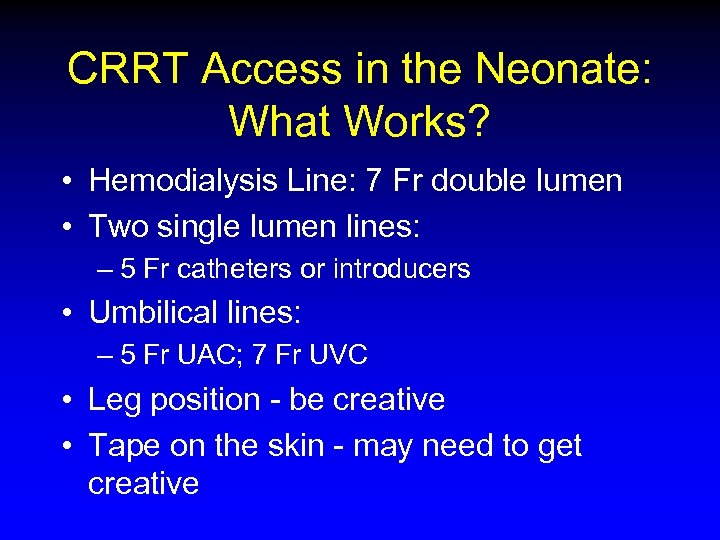 CRRT Access in the Neonate: What Works? • Hemodialysis Line: 7 Fr double lumen • Two single lumen lines: – 5 Fr catheters or introducers • Umbilical lines: – 5 Fr UAC; 7 Fr UVC • Leg position - be creative • Tape on the skin - may need to get creative
CRRT Access in the Neonate: What Works? • Hemodialysis Line: 7 Fr double lumen • Two single lumen lines: – 5 Fr catheters or introducers • Umbilical lines: – 5 Fr UAC; 7 Fr UVC • Leg position - be creative • Tape on the skin - may need to get creative
 PRISMA • Dedicated CRRT device • Highly automated • Designed for ease of use at the bedside
PRISMA • Dedicated CRRT device • Highly automated • Designed for ease of use at the bedside
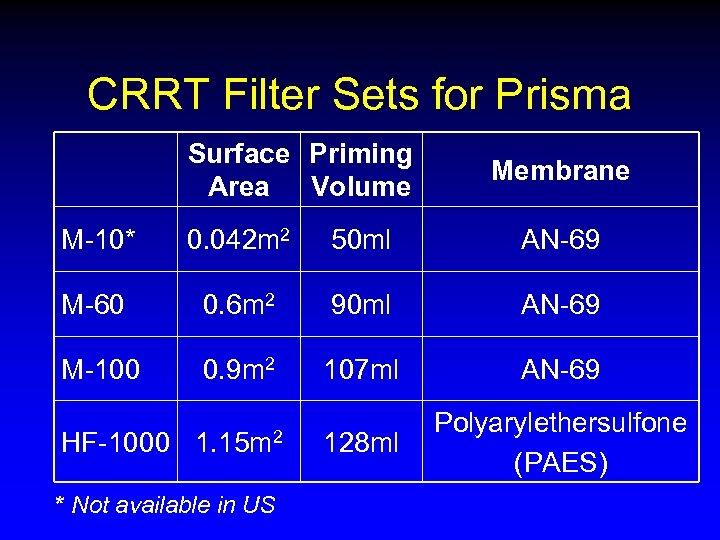 CRRT Filter Sets for Prisma Surface Priming Area Volume Membrane M-10* 0. 042 m 2 50 ml AN-69 M-60 0. 6 m 2 90 ml AN-69 M-100 0. 9 m 2 107 ml AN-69 HF-1000 1. 15 m 2 128 ml Polyarylethersulfone (PAES) * Not available in US
CRRT Filter Sets for Prisma Surface Priming Area Volume Membrane M-10* 0. 042 m 2 50 ml AN-69 M-60 0. 6 m 2 90 ml AN-69 M-100 0. 9 m 2 107 ml AN-69 HF-1000 1. 15 m 2 128 ml Polyarylethersulfone (PAES) * Not available in US
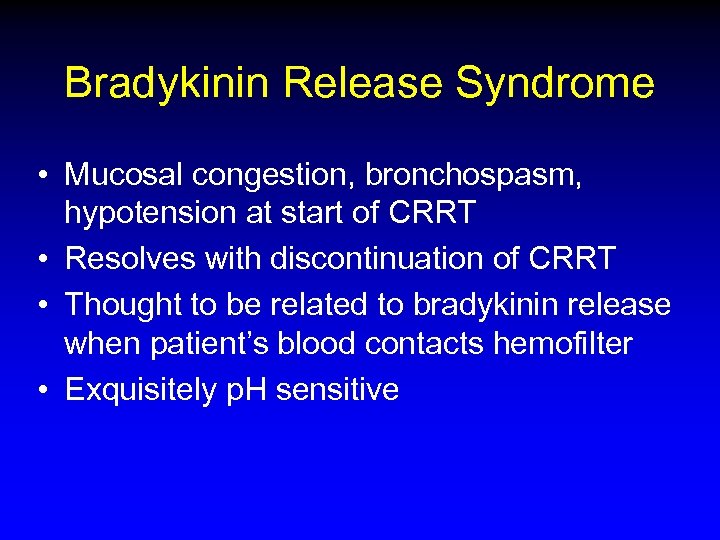 Bradykinin Release Syndrome • Mucosal congestion, bronchospasm, hypotension at start of CRRT • Resolves with discontinuation of CRRT • Thought to be related to bradykinin release when patient’s blood contacts hemofilter • Exquisitely p. H sensitive
Bradykinin Release Syndrome • Mucosal congestion, bronchospasm, hypotension at start of CRRT • Resolves with discontinuation of CRRT • Thought to be related to bradykinin release when patient’s blood contacts hemofilter • Exquisitely p. H sensitive
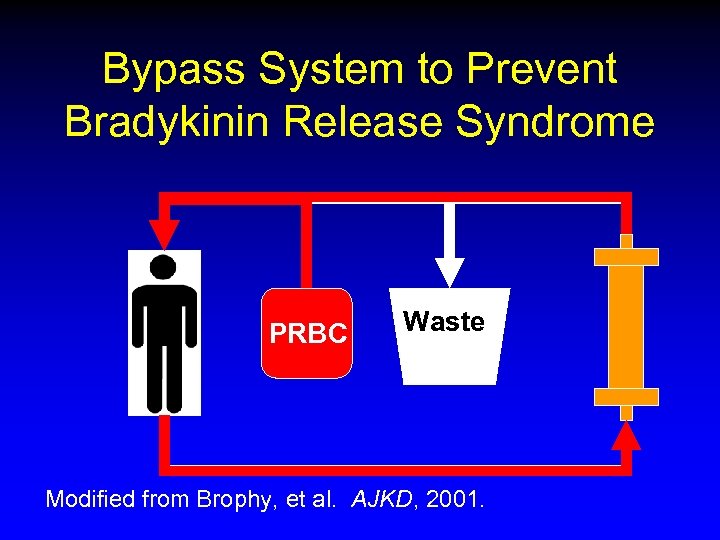 Bypass System to Prevent Bradykinin Release Syndrome PRBC Waste Modified from Brophy, et al. AJKD, 2001.
Bypass System to Prevent Bradykinin Release Syndrome PRBC Waste Modified from Brophy, et al. AJKD, 2001.
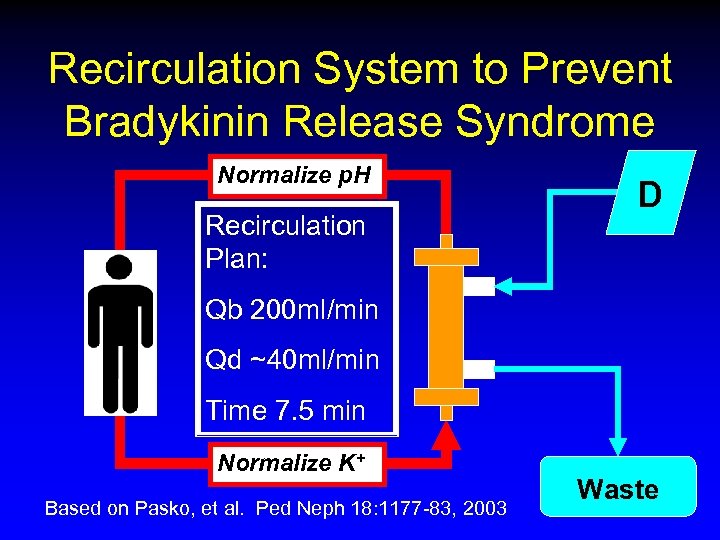 Recirculation System to Prevent Bradykinin Release Syndrome Normalize p. H Recirculation Plan: D Qb 200 ml/min Qd ~40 ml/min Time 7. 5 min Normalize K+ Based on Pasko, et al. Ped Neph 18: 1177 -83, 2003 Waste
Recirculation System to Prevent Bradykinin Release Syndrome Normalize p. H Recirculation Plan: D Qb 200 ml/min Qd ~40 ml/min Time 7. 5 min Normalize K+ Based on Pasko, et al. Ped Neph 18: 1177 -83, 2003 Waste
 Simple Systems to Limit Likelihood of Bradykinin Release Syndrome • Don’t prime on with blood • Don’t use the AN-69 membrane
Simple Systems to Limit Likelihood of Bradykinin Release Syndrome • Don’t prime on with blood • Don’t use the AN-69 membrane
 Thermal Regulation • • Hotline® blood warming tubing Place at venous return to patient Leave on at set temperature of 39 C Treat temp elevations if they occur
Thermal Regulation • • Hotline® blood warming tubing Place at venous return to patient Leave on at set temperature of 39 C Treat temp elevations if they occur
 Infant CRRT in Seattle: CRRT Staffing • • Dialysis RN sets-up & initiates therapy PICU/IICU RN manages patient Nephrology/Dialysis RN on call 24/7 Acuity assigned to pump as if a separate patient • Staffing determined by acuity
Infant CRRT in Seattle: CRRT Staffing • • Dialysis RN sets-up & initiates therapy PICU/IICU RN manages patient Nephrology/Dialysis RN on call 24/7 Acuity assigned to pump as if a separate patient • Staffing determined by acuity
 Infant CRRT in Seattle: How to Handle a Rare Procedure • Developed an Acute Initiation Checklist defining specific roles/actions for: – Infant ICU MD – Nephrology MD – Infant ICU RN – Dialysis RN – IV access MD
Infant CRRT in Seattle: How to Handle a Rare Procedure • Developed an Acute Initiation Checklist defining specific roles/actions for: – Infant ICU MD – Nephrology MD – Infant ICU RN – Dialysis RN – IV access MD
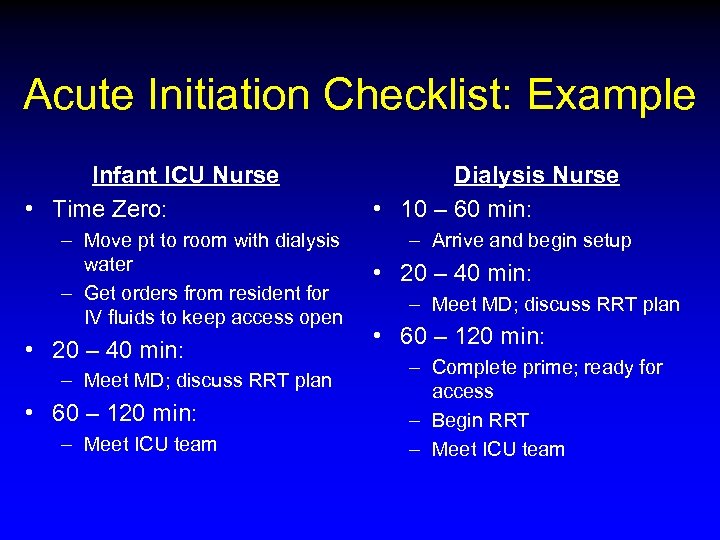 Acute Initiation Checklist: Example Infant ICU Nurse • Time Zero: – Move pt to room with dialysis water – Get orders from resident for IV fluids to keep access open • 20 – 40 min: – Meet MD; discuss RRT plan • 60 – 120 min: – Meet ICU team Dialysis Nurse • 10 – 60 min: – Arrive and begin setup • 20 – 40 min: – Meet MD; discuss RRT plan • 60 – 120 min: – Complete prime; ready for access – Begin RRT – Meet ICU team
Acute Initiation Checklist: Example Infant ICU Nurse • Time Zero: – Move pt to room with dialysis water – Get orders from resident for IV fluids to keep access open • 20 – 40 min: – Meet MD; discuss RRT plan • 60 – 120 min: – Meet ICU team Dialysis Nurse • 10 – 60 min: – Arrive and begin setup • 20 – 40 min: – Meet MD; discuss RRT plan • 60 – 120 min: – Complete prime; ready for access – Begin RRT – Meet ICU team
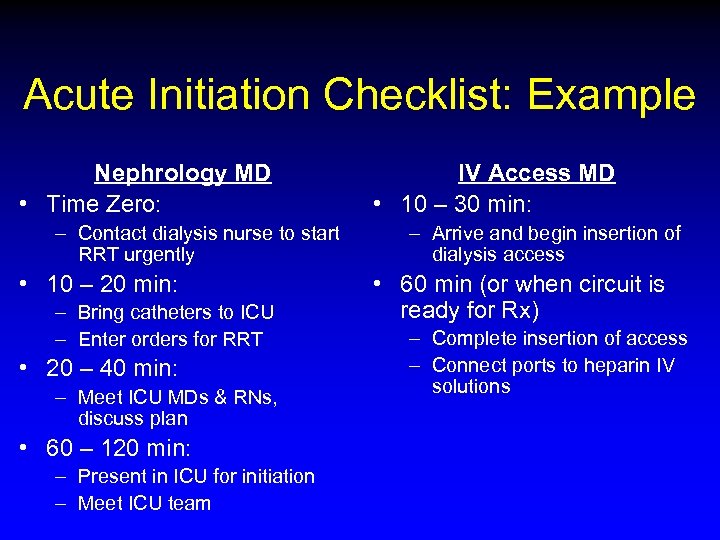 Acute Initiation Checklist: Example Nephrology MD • Time Zero: – Contact dialysis nurse to start RRT urgently • 10 – 20 min: – Bring catheters to ICU – Enter orders for RRT • 20 – 40 min: – Meet ICU MDs & RNs, discuss plan • 60 – 120 min: – Present in ICU for initiation – Meet ICU team IV Access MD • 10 – 30 min: – Arrive and begin insertion of dialysis access • 60 min (or when circuit is ready for Rx) – Complete insertion of access – Connect ports to heparin IV solutions
Acute Initiation Checklist: Example Nephrology MD • Time Zero: – Contact dialysis nurse to start RRT urgently • 10 – 20 min: – Bring catheters to ICU – Enter orders for RRT • 20 – 40 min: – Meet ICU MDs & RNs, discuss plan • 60 – 120 min: – Present in ICU for initiation – Meet ICU team IV Access MD • 10 – 30 min: – Arrive and begin insertion of dialysis access • 60 min (or when circuit is ready for Rx) – Complete insertion of access – Connect ports to heparin IV solutions
 Infant RRT: Summary • • All modalities of RRT possible for infants No modality is perfect Technical challenges can be met Careful planning with institution, program, and individuals improves care • Cooperation, communication, and collaboration will increase our success
Infant RRT: Summary • • All modalities of RRT possible for infants No modality is perfect Technical challenges can be met Careful planning with institution, program, and individuals improves care • Cooperation, communication, and collaboration will increase our success
 Thanks!
Thanks!


