Acute_Renal_Failure II.pptx
- Количество слайдов: 49
ACUTE RENAL FAILURE STEPHEN HUMBERT DO
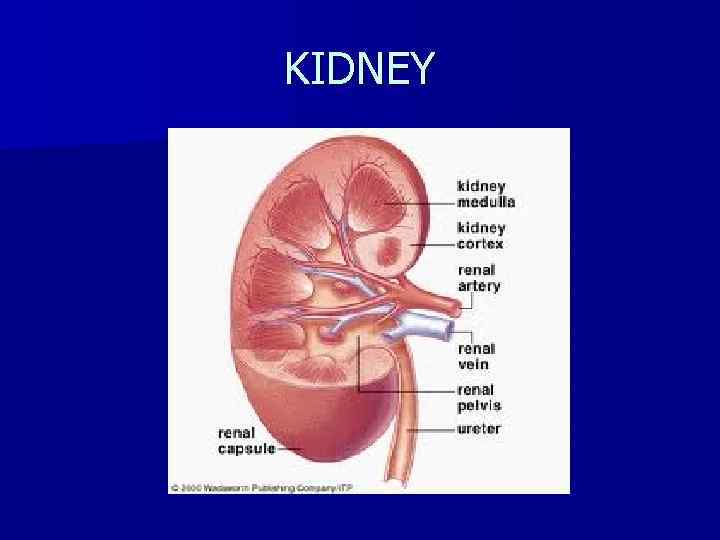
KIDNEY
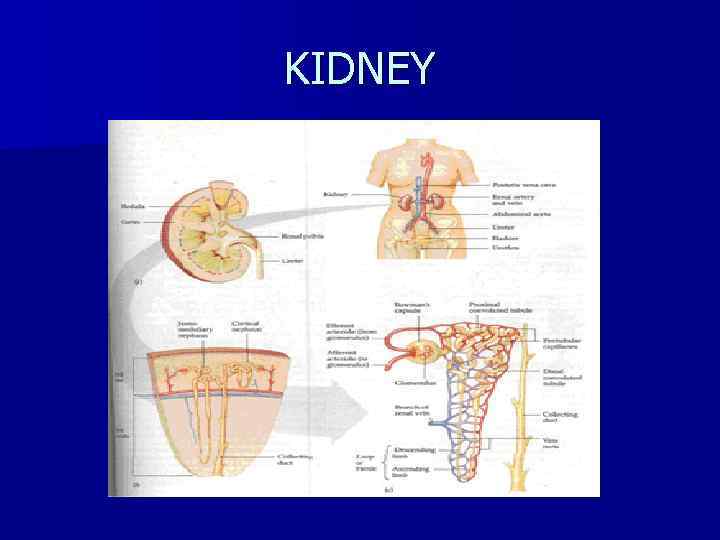
KIDNEY
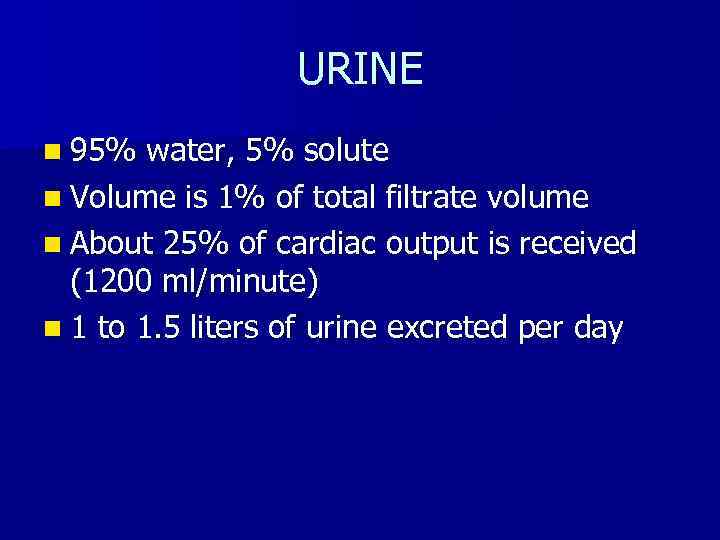
URINE n 95% water, 5% solute n Volume is 1% of total filtrate volume n About 25% of cardiac output is received (1200 ml/minute) n 1 to 1. 5 liters of urine excreted per day
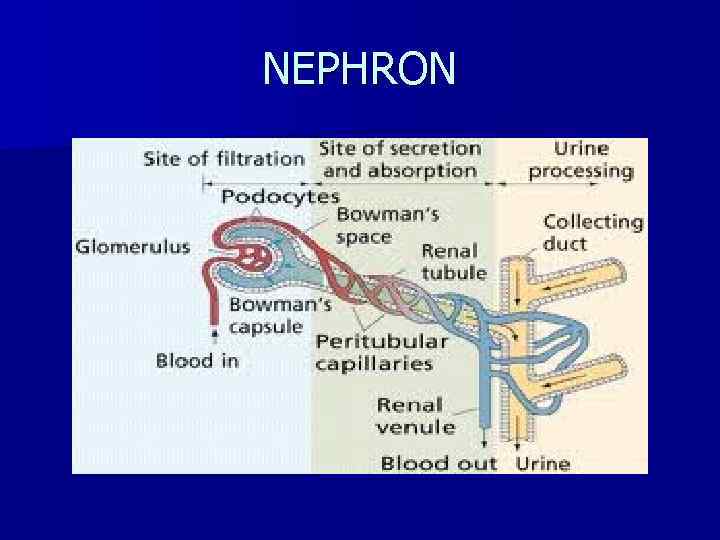
NEPHRON n Primary renal functional unit n About 1 million nephrons n glomerulus- filtering system n Tubule- the filtered liquid passes through this
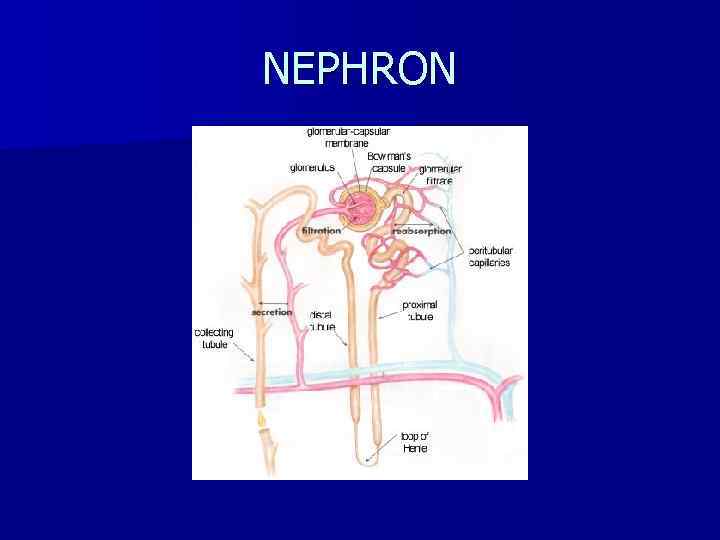
NEPHRON
GLOMERULUS n Capillary network surrounded by a membrane (Bowman’s capsule) n Afferent arteriole- blood from renal artery n Efferent arteriole- formed from capillaries rejoining at the distal glomerulus n Urine formation begins in the glomerular capillaries with dissolved substances passing into the proximal tubule from the force of blood pressure in afferent arteriole and in Bowman’s capsule
RENAL TUBULE n Reabsorption- remove solute from tubules and return them to blood stream n Secretion- some substances (eg. Hydrogen) eliminated at rate greater than GFR n Secretion and absorption: controlled by selective permeability of different areas of the tubule (H 2 O, Na, urea) and by response of distal tubule to hormones (aldosterone, antidiuretic & parathyroid hormones)
NEPHRON
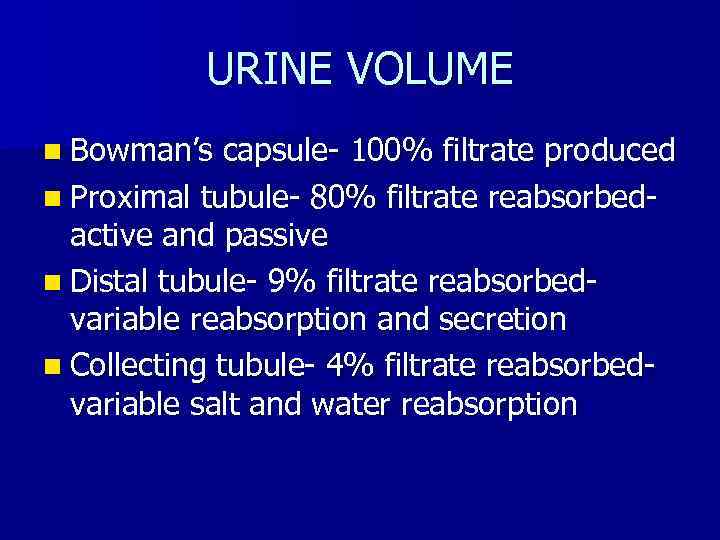
URINE VOLUME n Bowman’s capsule- 100% filtrate produced n Proximal tubule- 80% filtrate reabsorbedactive and passive n Distal tubule- 9% filtrate reabsorbedvariable reabsorption and secretion n Collecting tubule- 4% filtrate reabsorbedvariable salt and water reabsorption
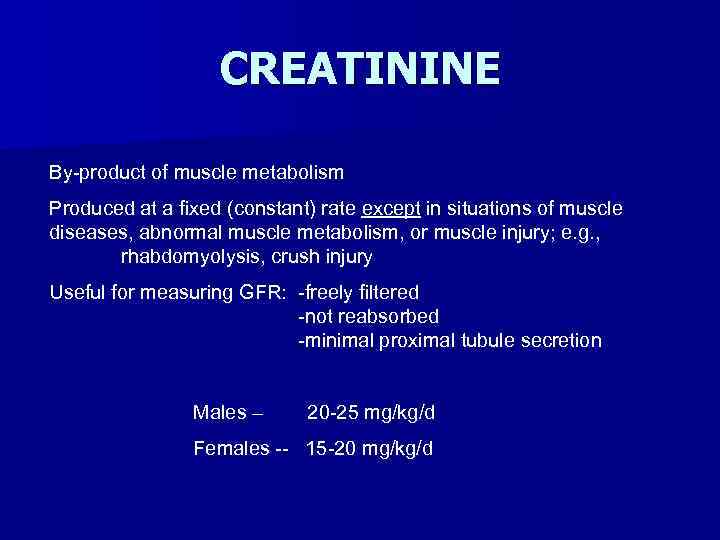
CREATININE By-product of muscle metabolism Produced at a fixed (constant) rate except in situations of muscle diseases, abnormal muscle metabolism, or muscle injury; e. g. , rhabdomyolysis, crush injury Useful for measuring GFR: -freely filtered -not reabsorbed -minimal proximal tubule secretion Males – 20 -25 mg/kg/d Females -- 15 -20 mg/kg/d
RENAL FAILURE n Loss of renal function n Uremia- retention of nitrogenous waste
ACUTE RENAL FAILURE n Rapid onset n Often reversible n Pre-renal, post-renal
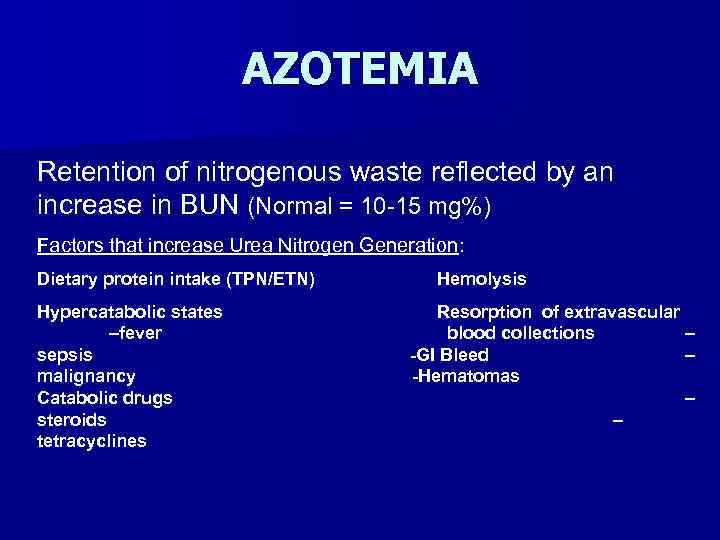
AZOTEMIA Retention of nitrogenous waste reflected by an increase in BUN (Normal = 10 -15 mg%) Factors that increase Urea Nitrogen Generation: Dietary protein intake (TPN/ETN) Hypercatabolic states –fever sepsis malignancy Catabolic drugs steroids tetracyclines Hemolysis Resorption of extravascular blood collections – -GI Bleed – -Hematomas – –
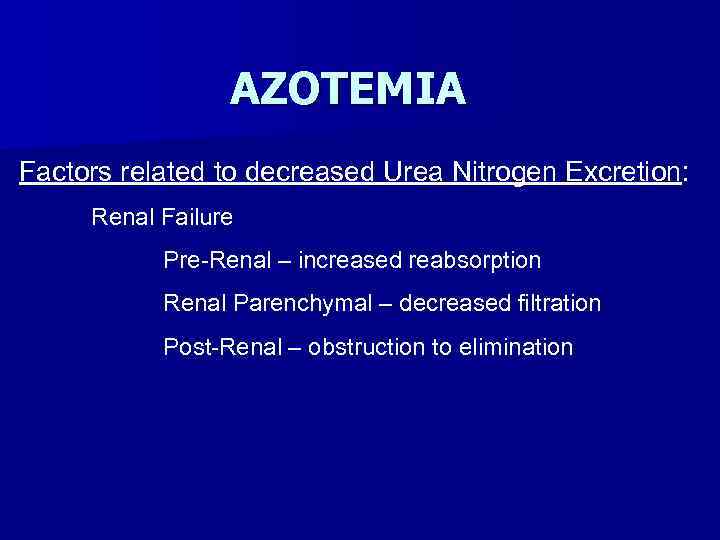
AZOTEMIA Factors related to decreased Urea Nitrogen Excretion: Renal Failure Pre-Renal – increased reabsorption Renal Parenchymal – decreased filtration Post-Renal – obstruction to elimination
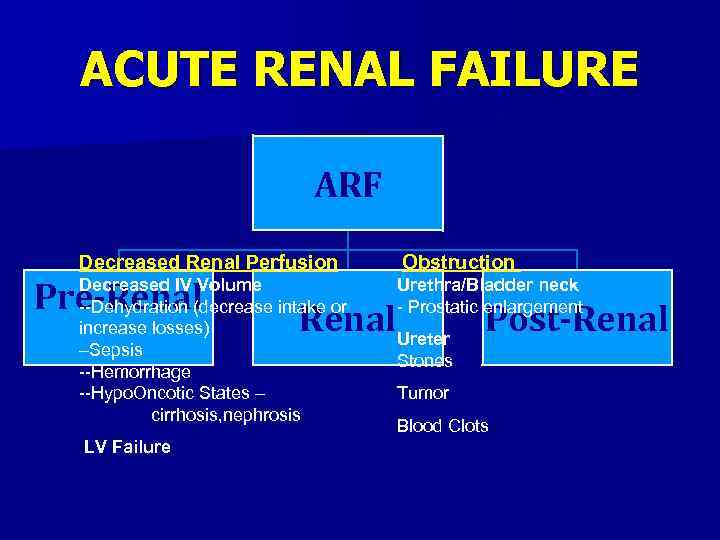
ACUTE RENAL FAILURE ARF Decreased Renal Perfusion Pre-Renal Decreased IV Volume --Dehydration (decrease intake or increase losses) –Sepsis --Hemorrhage --Hypo. Oncotic States – cirrhosis, nephrosis LV Failure Obstruction Urethra/Bladder neck - Prostatic enlargement Renal. Ureter Post-Renal Stones Tumor Blood Clots
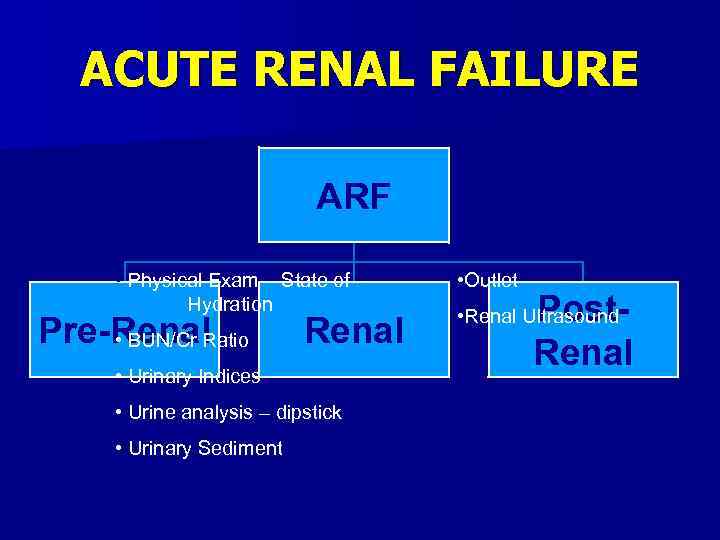
ACUTE RENAL FAILURE ARF • Physical Exam – State of Hydration Pre-Renal • BUN/Cr Ratio Renal • Urinary Indices • Urine analysis – dipstick • Urinary Sediment • Outlet Post. Renal • Renal Ultrasound
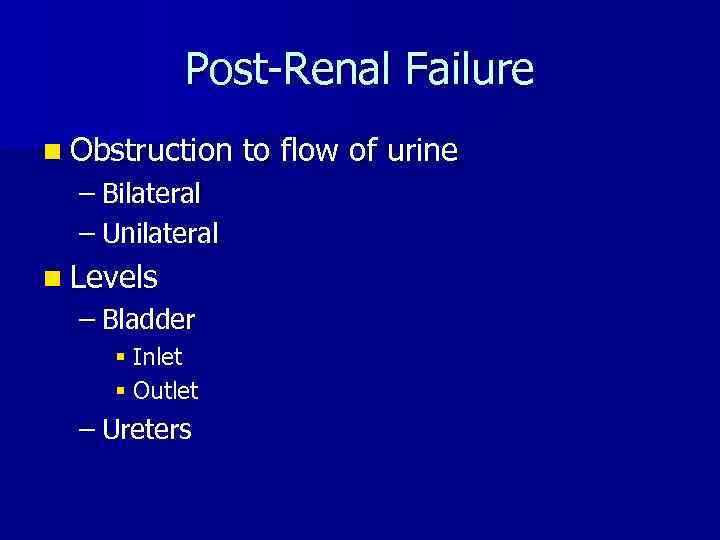
Post-Renal Failure n Obstruction – Bilateral – Unilateral n Levels – Bladder § Inlet § Outlet – Ureters to flow of urine
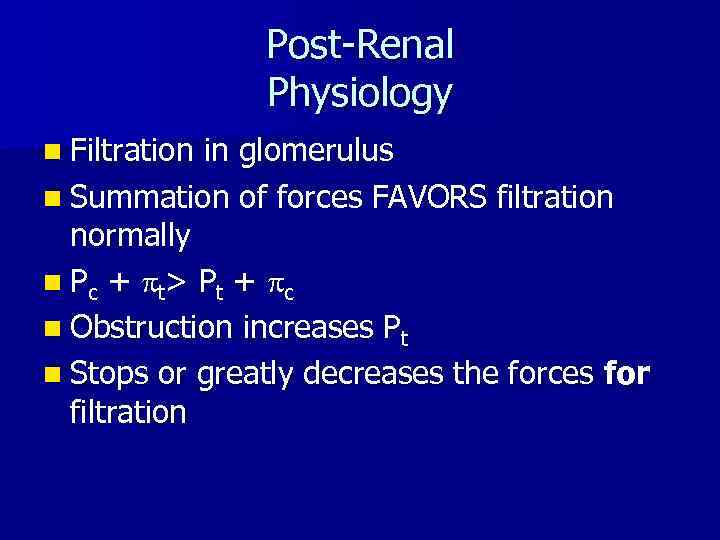
Post-Renal Physiology n Filtration in glomerulus n Summation of forces FAVORS filtration normally n Pc + p t> P t + p c n Obstruction increases Pt n Stops or greatly decreases the forces for filtration
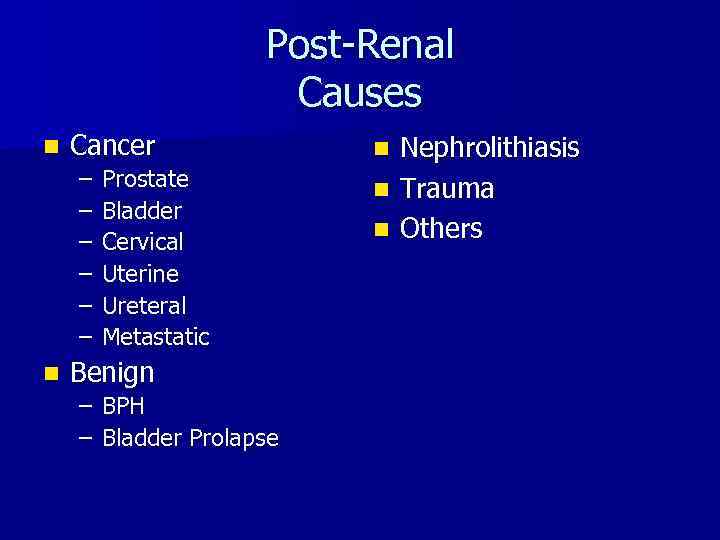
Post-Renal Causes n Cancer – – – n Prostate Bladder Cervical Uterine Ureteral Metastatic Benign – BPH – Bladder Prolapse Nephrolithiasis n Trauma n Others n
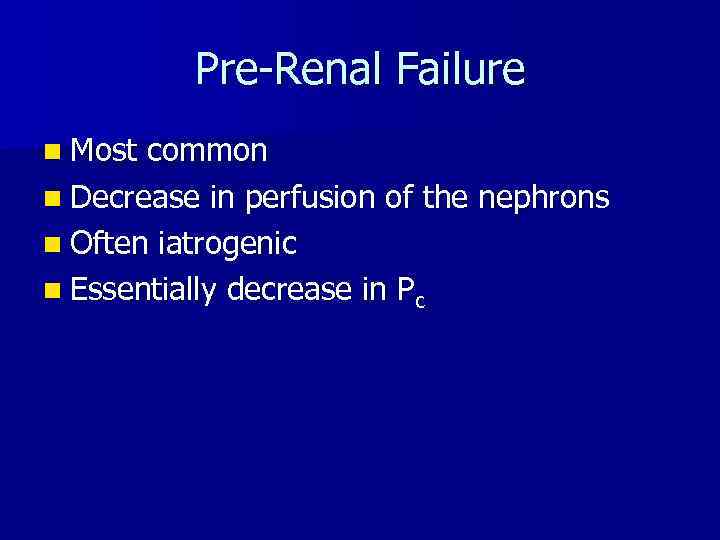
Pre-Renal Failure n Most common n Decrease in perfusion of the nephrons n Often iatrogenic n Essentially decrease in Pc
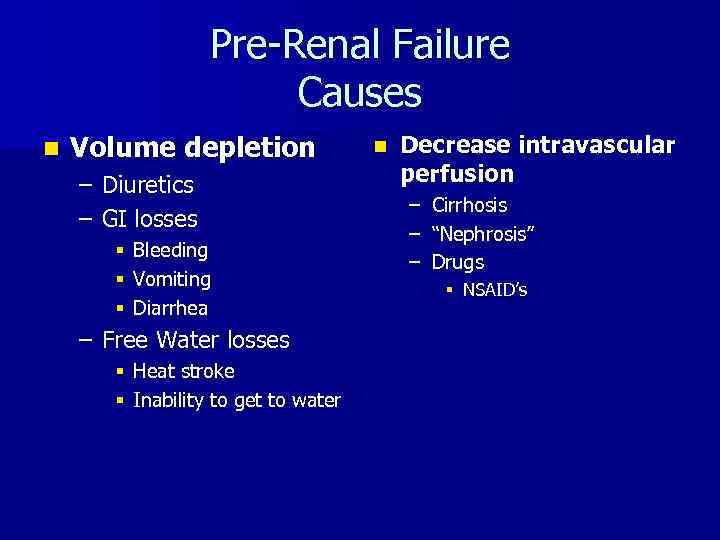
Pre-Renal Failure Causes n Volume depletion – Diuretics – GI losses § Bleeding § Vomiting § Diarrhea – Free Water losses § Heat stroke § Inability to get to water n Decrease intravascular perfusion – – – Cirrhosis “Nephrosis” Drugs § NSAID’s
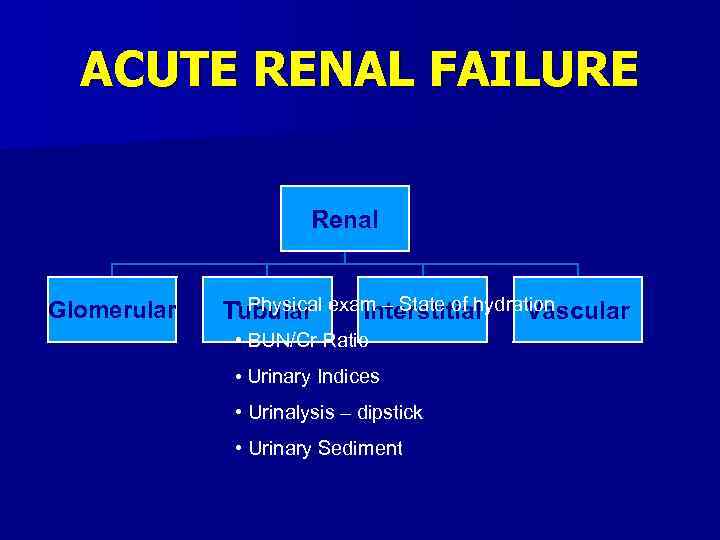
ACUTE RENAL FAILURE Renal Glomerular • Physical Tubular exam – State of hydration Interstitial Vascular • BUN/Cr Ratio • Urinary Indices • Urinalysis – dipstick • Urinary Sediment
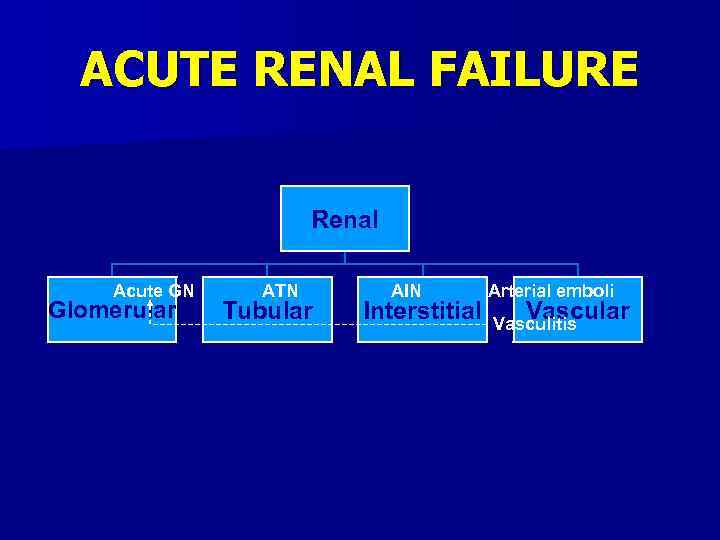
ACUTE RENAL FAILURE Renal Acute GN Glomerular ATN Tubular AIN Interstitial Arterial emboli Vascular Vasculitis
Intrinsic Renal Failure n Vessels n Glomerulus n Tubulo-interstitial
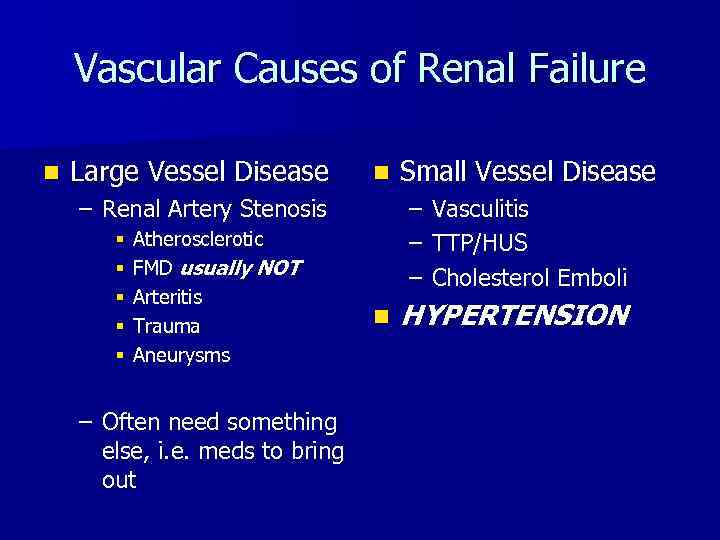
Vascular Causes of Renal Failure n Large Vessel Disease n – Renal Artery Stenosis § § § Atherosclerotic FMD usually NOT Arteritis Trauma Aneurysms – Often need something else, i. e. meds to bring out Small Vessel Disease – – – n Vasculitis TTP/HUS Cholesterol Emboli HYPERTENSION
Glomerular n Glomerulonephritis – Acute – Chronic – Primary – Secondary
Secondary GN n Most common – Diabetic – HIV associated nephropathy (HIVAN) – SLE – Systemic vasculitides – Others Can be acute or chronic
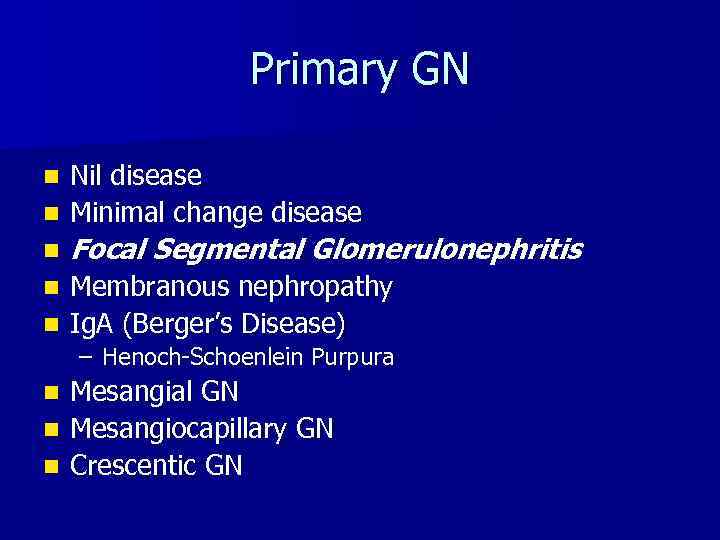
Primary GN Nil disease n Minimal change disease n n Focal Segmental Glomerulonephritis Membranous nephropathy n Ig. A (Berger’s Disease) n – Henoch-Schoenlein Purpura Mesangial GN n Mesangiocapillary GN n Crescentic GN n
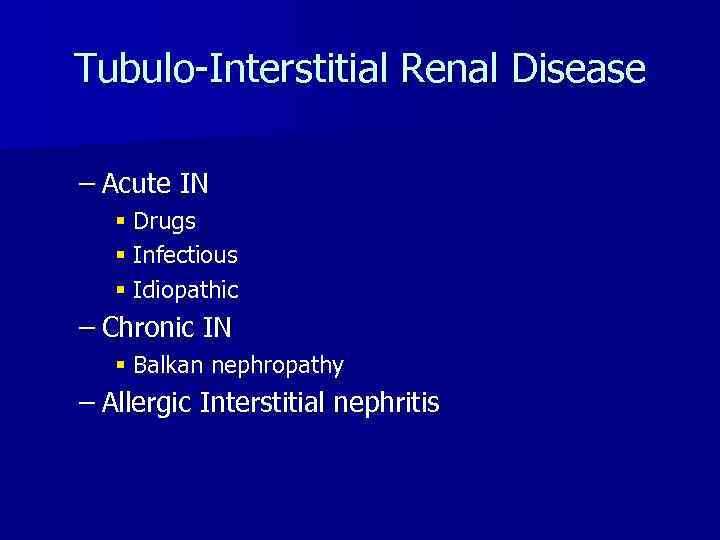
Tubulo-Interstitial Renal Disease – Acute IN § Drugs § Infectious § Idiopathic – Chronic IN § Balkan nephropathy – Allergic Interstitial nephritis
ACUTE RENAL FAILURE LABORATORY The laboratory findings are used to confirm your clinical suspicion.
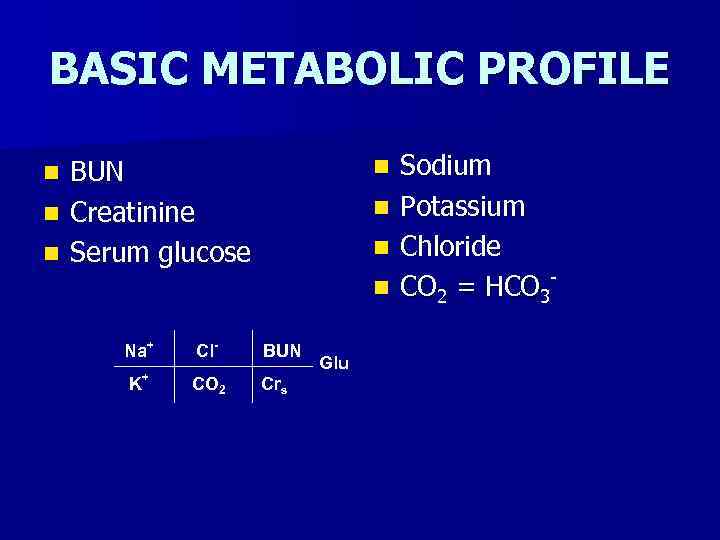
BASIC METABOLIC PROFILE BUN n Creatinine n Serum glucose n n n Na+ K + Cl- BUN CO 2 Crs Glu Sodium Potassium Chloride CO 2 = HCO 3
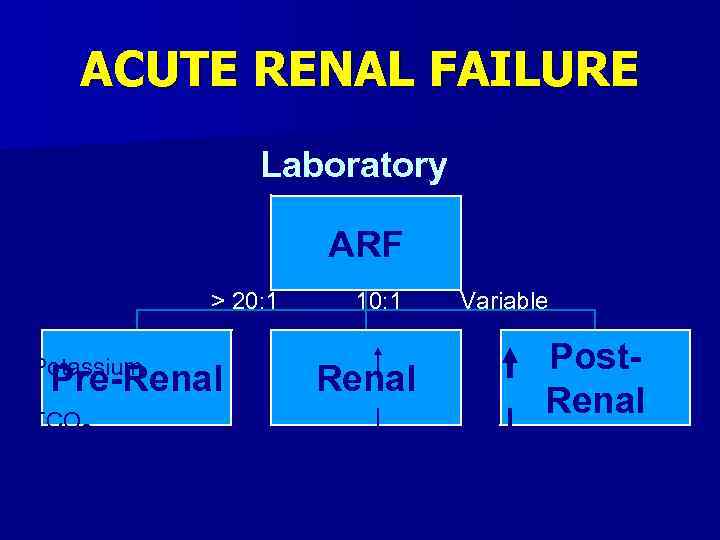
ACUTE RENAL FAILURE Laboratory ARF BUN/Cr Ratio Potassium > 20: 1 Pre-Renal TCO 2 10: 1 Renal Variable Post. Renal
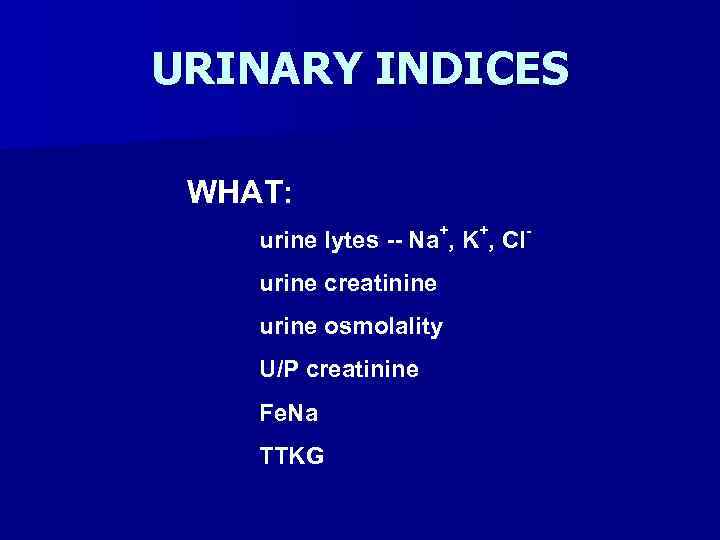
URINARY INDICES WHAT: urine lytes -- Na+, K+, Clurine creatinine urine osmolality U/P creatinine Fe. Na TTKG
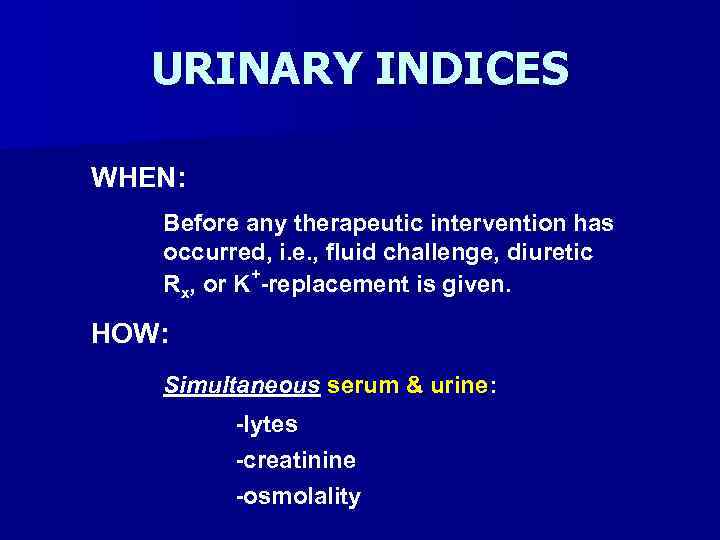
URINARY INDICES WHEN: Before any therapeutic intervention has occurred, i. e. , fluid challenge, diuretic Rx, or K+-replacement is given. HOW: Simultaneous serum & urine: -lytes -creatinine -osmolality
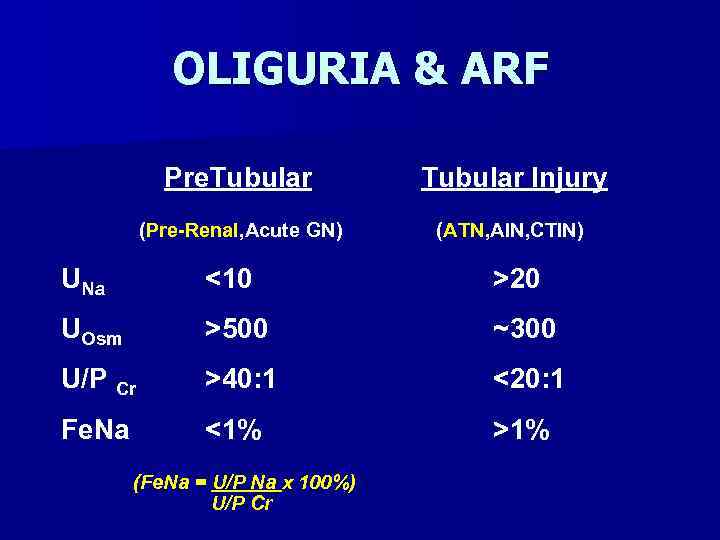
OLIGURIA & ARF Pre. Tubular Injury (Pre-Renal, Acute GN) (ATN, AIN, CTIN) UNa <10 >20 UOsm >500 ~300 U/P Cr >40: 1 <20: 1 Fe. Na <1% >1% (Fe. Na = U/P Na x 100%) U/P Cr
ACUTE TUBULAR NECROSIS Ischemic ATN – prolonged hypotension & shock -precipitous -oliguria -muddy brown casts Nephrotoxic ATN – aminoglycosides -gradual onset -non-oliguric -RTE’s & RTE casts
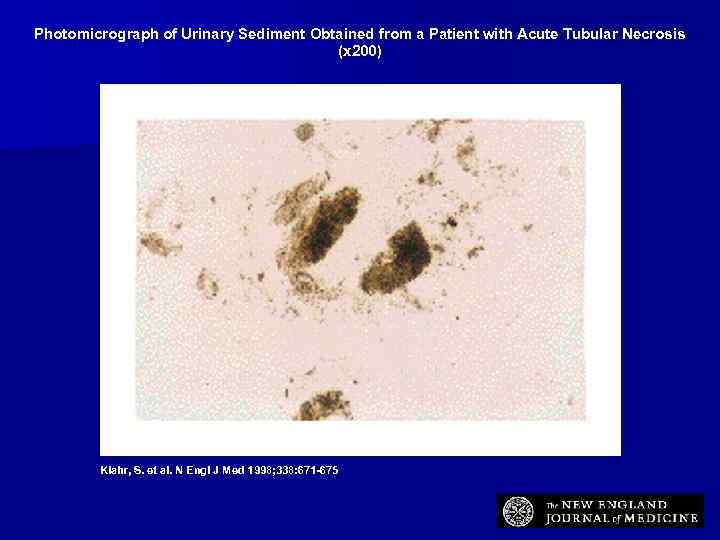
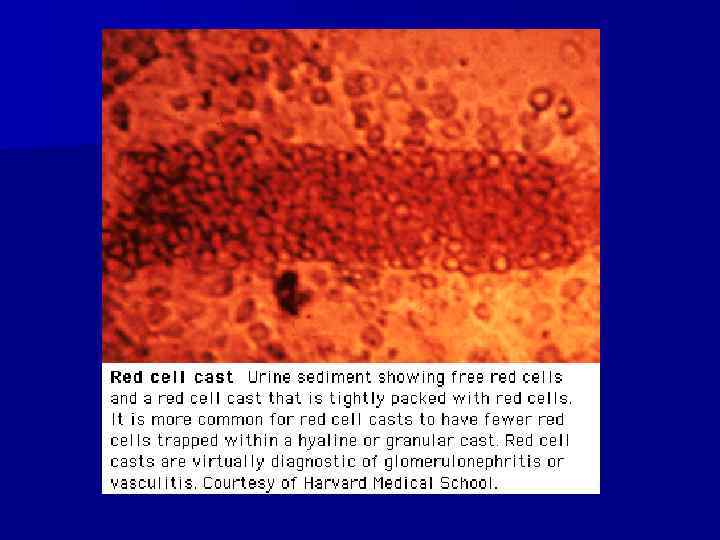
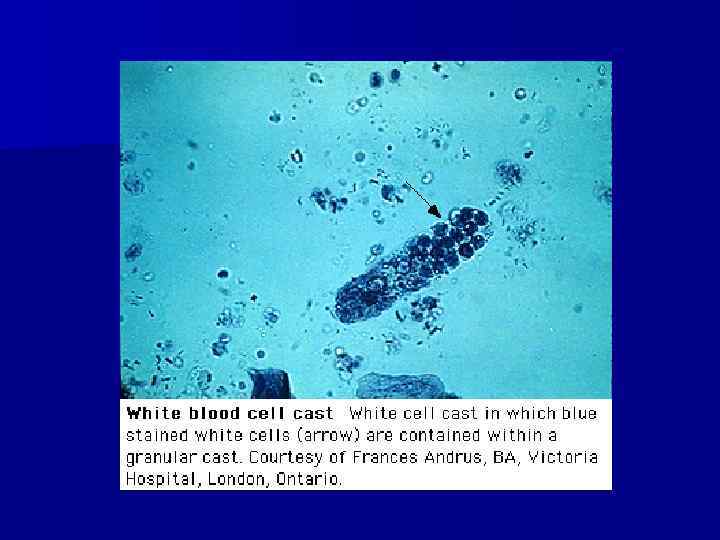
Photomicrograph of Urinary Sediment Obtained from a Patient with Acute Tubular Necrosis (x 200) Klahr, S. et al. N Engl J Med 1998; 338: 671 -675
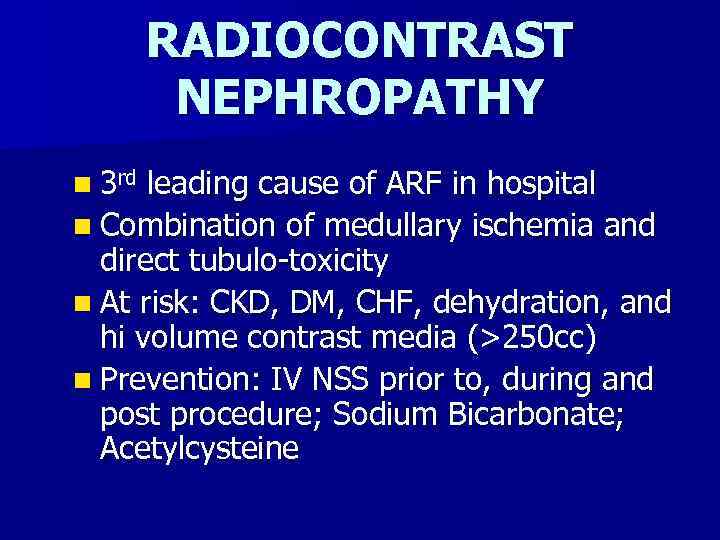
RADIOCONTRAST NEPHROPATHY n 3 rd leading cause of ARF in hospital n Combination of medullary ischemia and direct tubulo-toxicity n At risk: CKD, DM, CHF, dehydration, and hi volume contrast media (>250 cc) n Prevention: IV NSS prior to, during and post procedure; Sodium Bicarbonate; Acetylcysteine
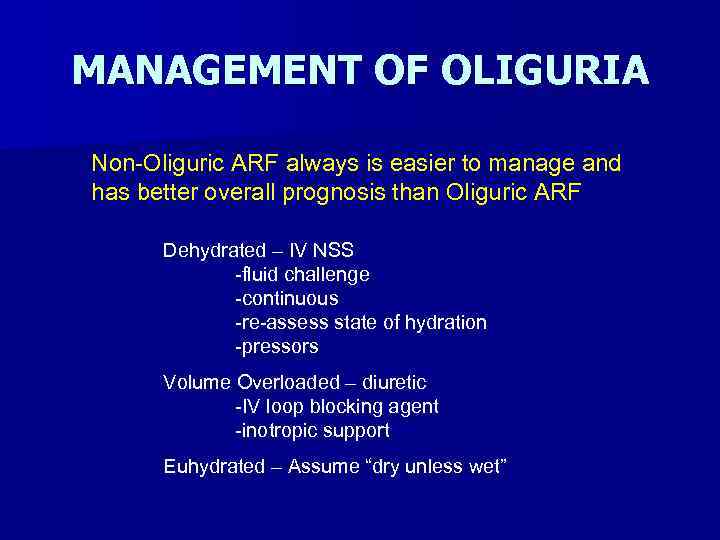
MANAGEMENT OF OLIGURIA Non-Oliguric ARF always is easier to manage and has better overall prognosis than Oliguric ARF Dehydrated – IV NSS -fluid challenge -continuous -re-assess state of hydration -pressors Volume Overloaded – diuretic -IV loop blocking agent -inotropic support Euhydrated – Assume “dry unless wet”
POTENTIAL OUTCOMES OF INTERVENTION Successful Reversal of oliguria Pulmonary artery catheterization (Swan. Ganz Catheter) Dialysis
ARF DUE TO ACUTE GN n Hematuria (RBC’s +/- RBC casts) n Proteinuria (albuminuria) n Hypertension n Edema n Azotemia
ARF DUE TO AIN n Pyuria (WBC’s +/- WBC Casts) n Tubular proteinuria n Hypertension n Edema n Azotemia
Acute vs. Chronic Renal Failure n Clinical determination – Only really an educated guess n Renal biopsy n CLUES – History – Physical exam – Kidney size – Anemia, PO 4, Ca++, U/A, acid-base very little help in determining chronicity of GN
Minimum Work-up n U/A, C&S n Urine eosinophils n Renal Ultrasound n Renal Flow scan n 24 hr urine collection for protein, creatinine and protein electrophoresis n CBC with diff
Full Work-up n “Minimum” plus: – ANA, C 3, C 4, ANCA, ASO titer, Hepatitis profile, SPEP, UPEP, HIV – ? Renal biopsy – ? Doppler US renal arteries – ? MRA – ? Renal arteriogram – Other tests, guided by H&P
Summary n Approach renal failure patients as you would ANY OTHER PATIENT n Try to make differential diagnosis based on H&P n Order tests compatible with proving or disproving the diff dx n Go from there
Acute_Renal_Failure II.pptx