Acute purulent infections of soft tissues. A boil

Acute purulent infections of soft tissues
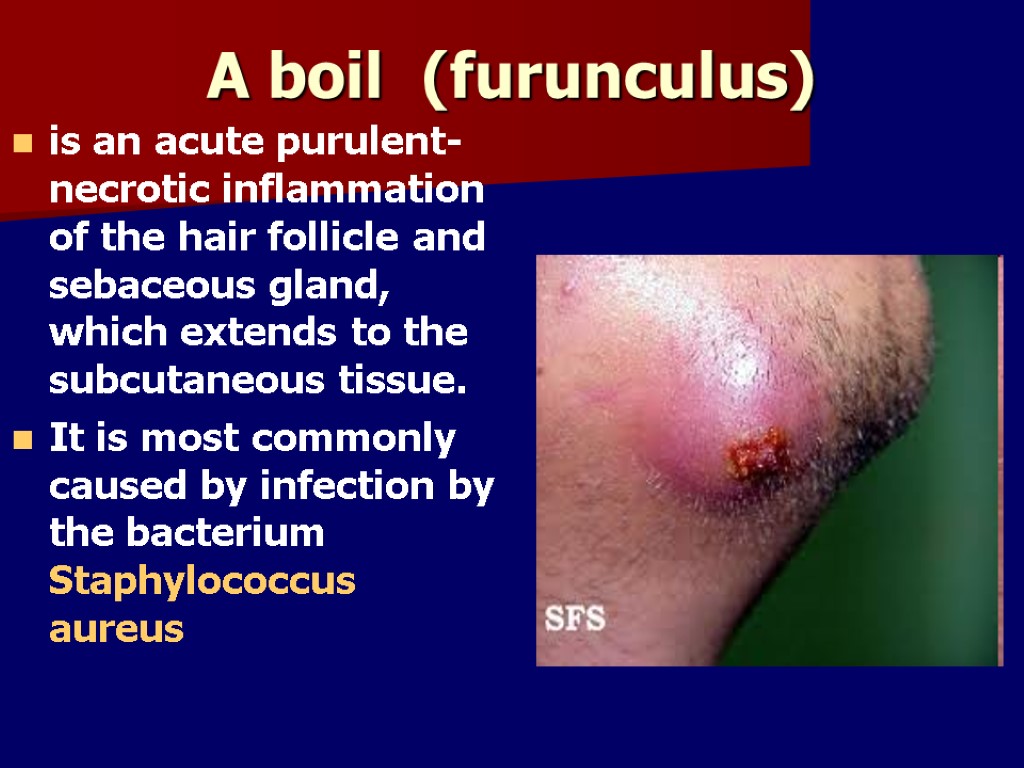
A boil (furunculus) is an acute purulent-necrotic inflammation of the hair follicle and sebaceous gland, which extends to the subcutaneous tissue. It is most commonly caused by infection by the bacterium Staphylococcus aureus

Boils are bumpy red, pus-filled lumps around a hair follicle that are tender, warm, and painful
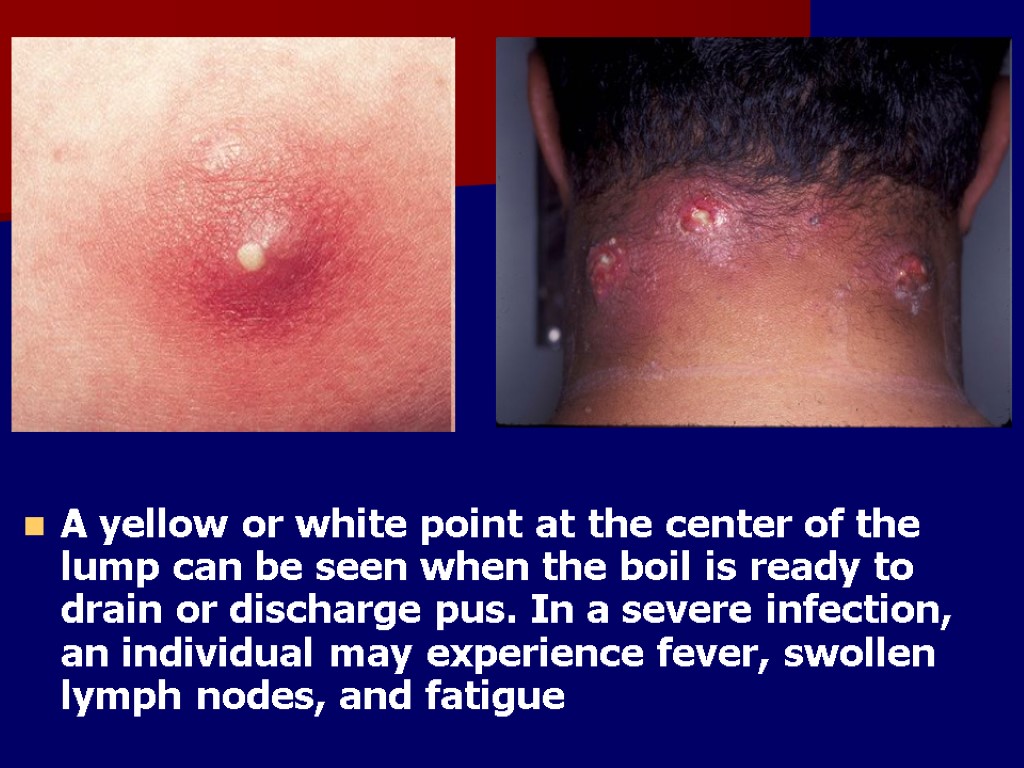
A yellow or white point at the center of the lump can be seen when the boil is ready to drain or discharge pus. In a severe infection, an individual may experience fever, swollen lymph nodes, and fatigue
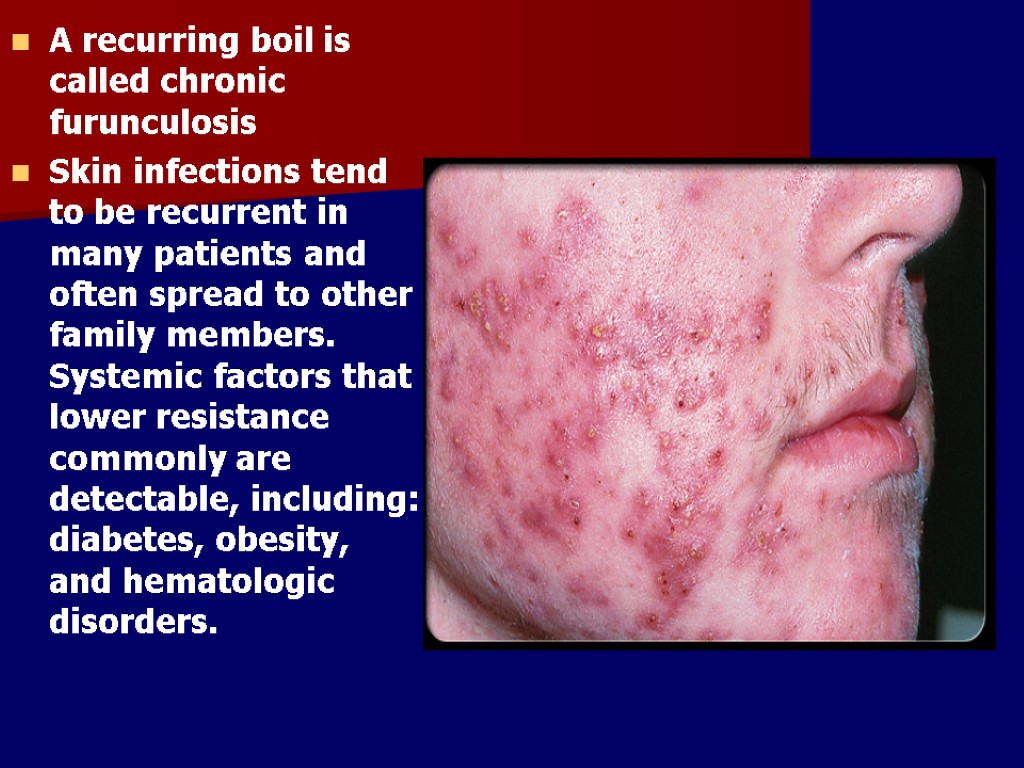
A recurring boil is called chronic furunculosis Skin infections tend to be recurrent in many patients and often spread to other family members. Systemic factors that lower resistance commonly are detectable, including: diabetes, obesity, and hematologic disorders.

Treatment Furuncles at risk of leading to serious complications should be incised and drained These include furuncles that are unusually large, last longer than two weeks, or are located in the middle of the face or near the spine
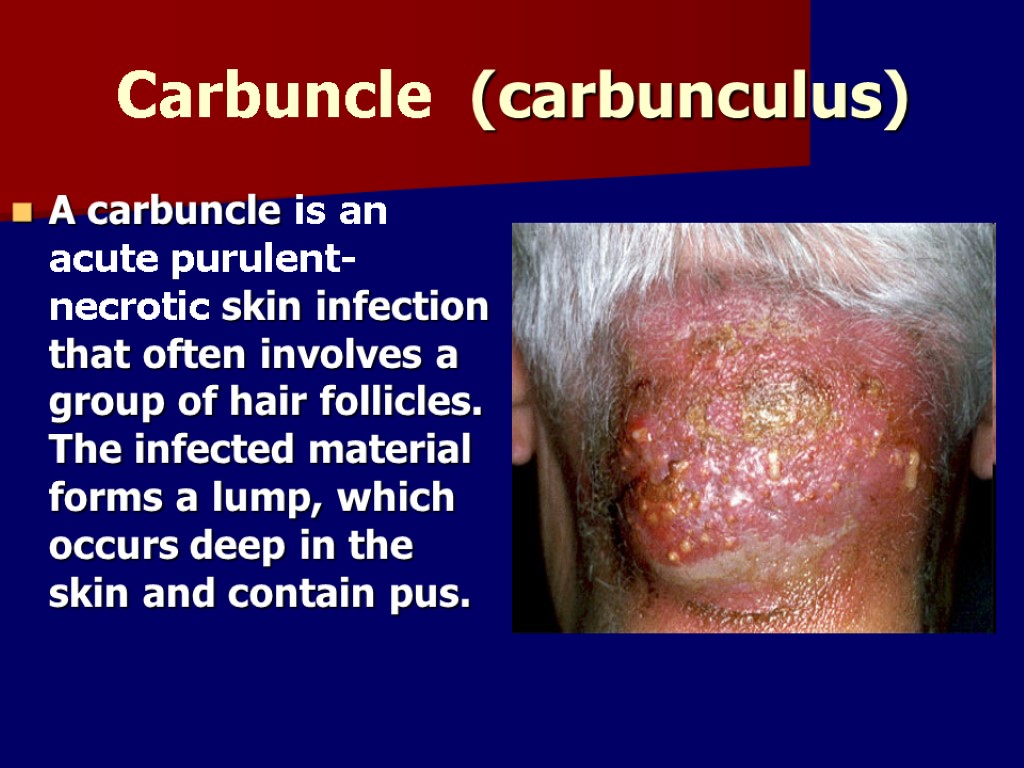
Carbuncle (саrbunculus) A carbuncle is an acute purulent-necrotic skin infection that often involves a group of hair follicles. The infected material forms a lump, which occurs deep in the skin and contain pus.
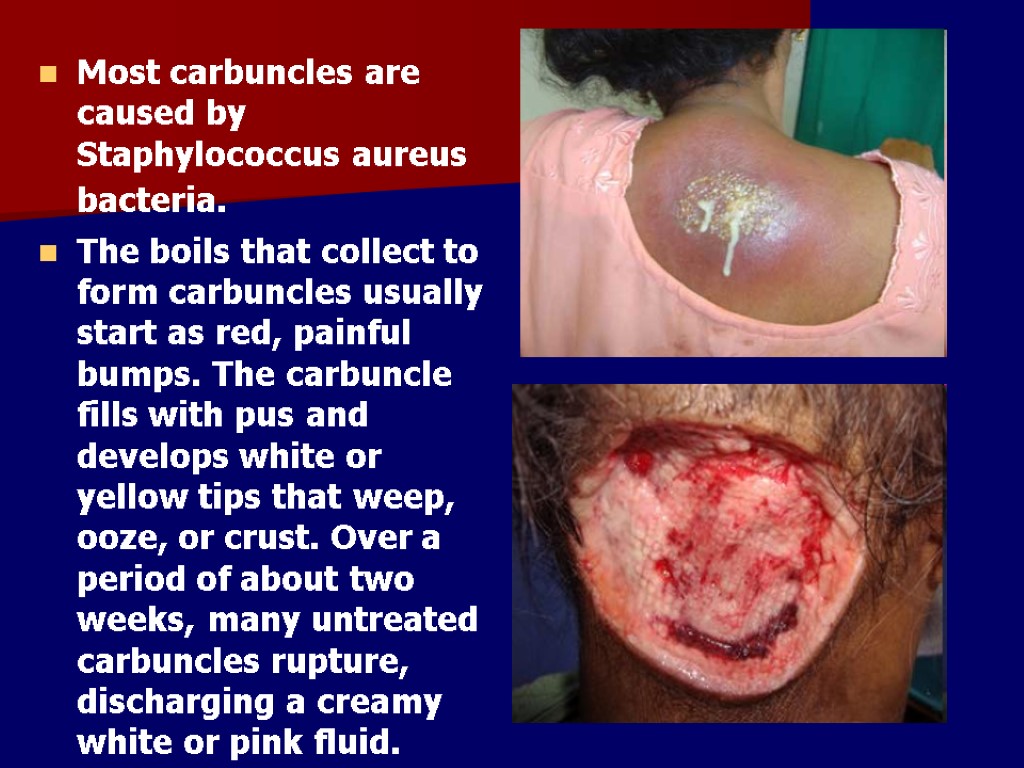
Most carbuncles are caused by Staphylococcus aureus bacteria. The boils that collect to form carbuncles usually start as red, painful bumps. The carbuncle fills with pus and develops white or yellow tips that weep, ooze, or crust. Over a period of about two weeks, many untreated carbuncles rupture, discharging a creamy white or pink fluid.
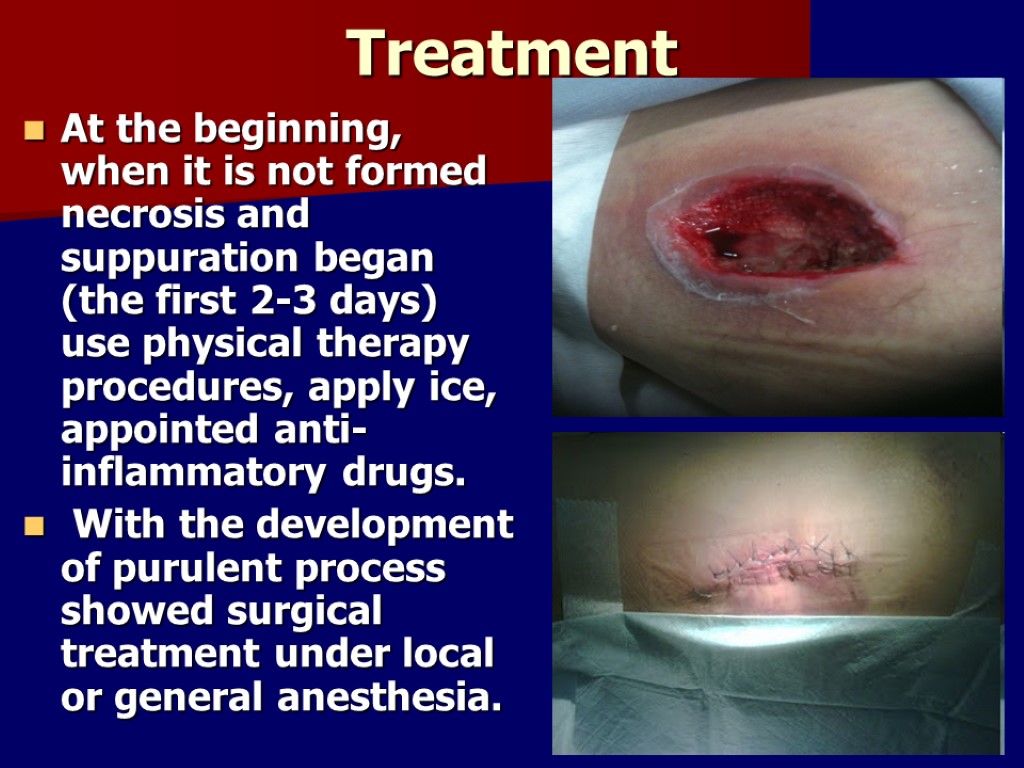
Treatment At the beginning, when it is not formed necrosis and suppuration began (the first 2-3 days) use physical therapy procedures, apply ice, appointed anti-inflammatory drugs. With the development of purulent process showed surgical treatment under local or general anesthesia.
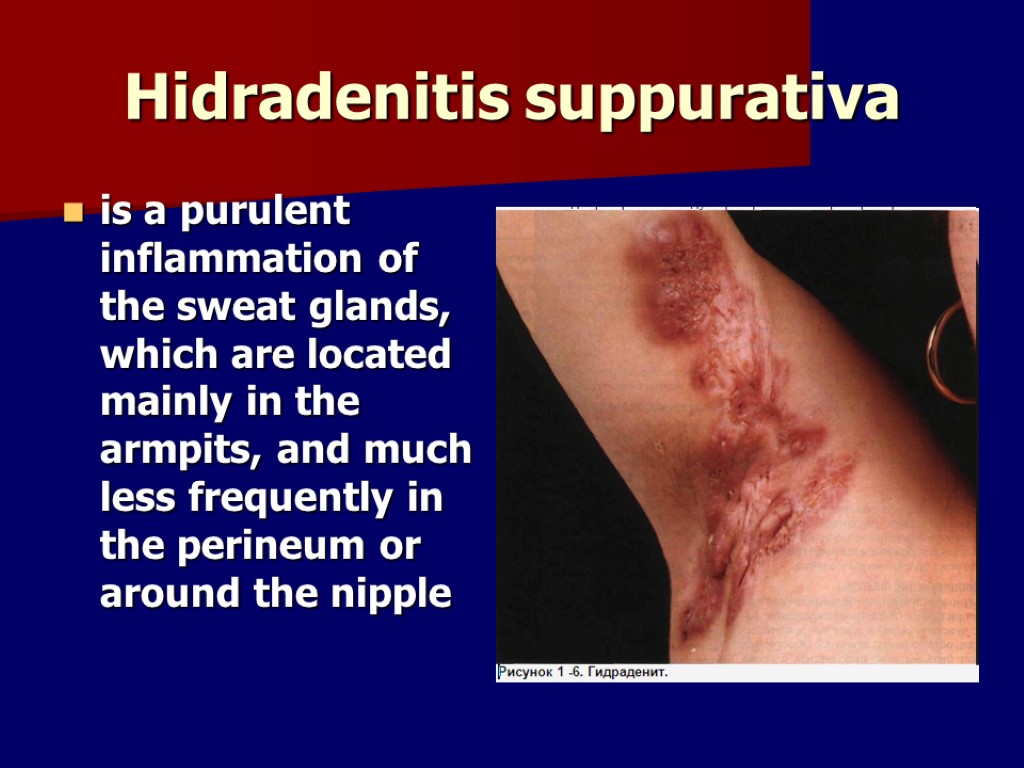
Hidradenitis suppurativa is a purulent inflammation of the sweat glands, which are located mainly in the armpits, and much less frequently in the perineum or around the nipple

Pathogens of this disease are staphylococci. These bacteria enter the sweat glands or through their excretory ducts, or the lymph vessels, and then through the surrounding prostate tissue.
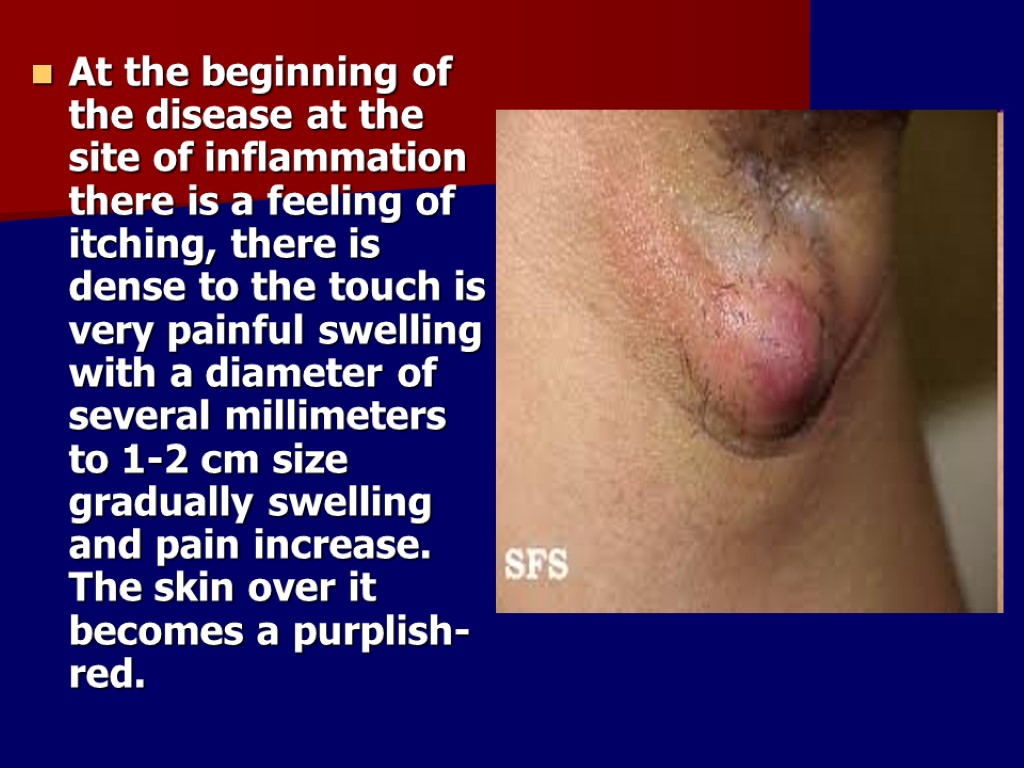
At the beginning of the disease at the site of inflammation there is a feeling of itching, there is dense to the touch is very painful swelling with a diameter of several millimeters to 1-2 cm size gradually swelling and pain increase. The skin over it becomes a purplish-red.

Treatment of gidradenitis

Abscess is a collection of pus that has accumulated in a cavity formed by the tissue in which the pus resides due to an infectious process (usually caused by bacteria or parasites) or other foreign materials (e.g., splinters, bullet wounds, or injecting needles).
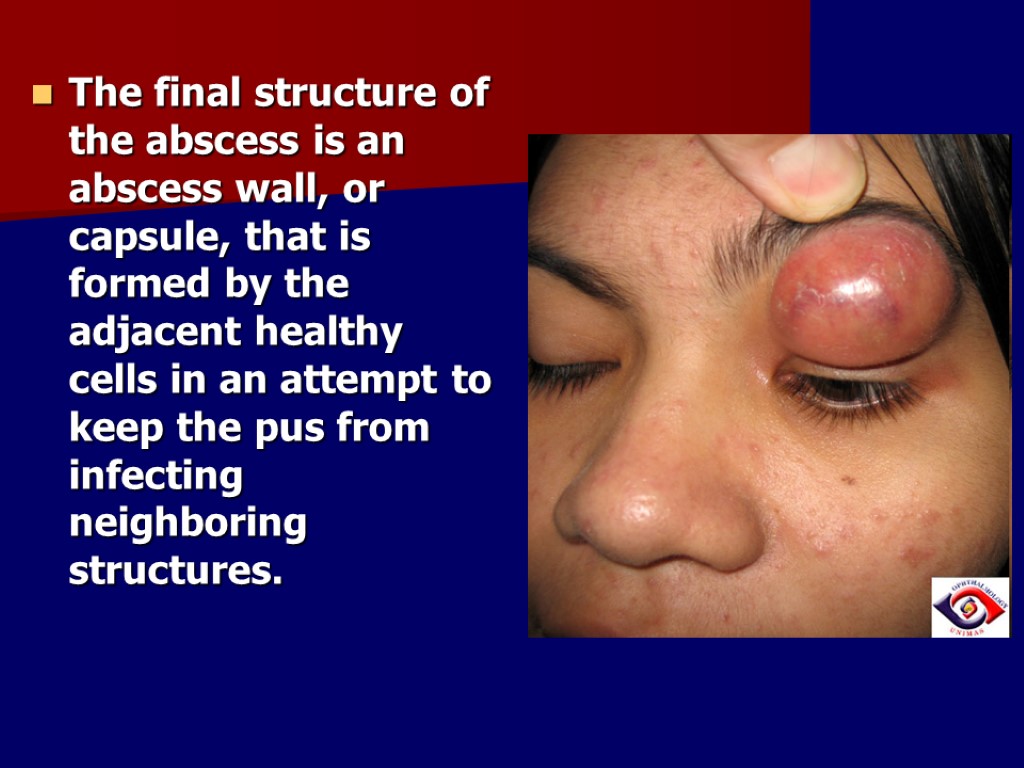
The final structure of the abscess is an abscess wall, or capsule, that is formed by the adjacent healthy cells in an attempt to keep the pus from infecting neighboring structures.

The cardinal symptoms and signs of any kind of inflammatory process are redness, heat, swelling, pain and loss of function.

Wound abscesses cannot be treated with antibiotics. They require surgical intervention, debridement, and curettage
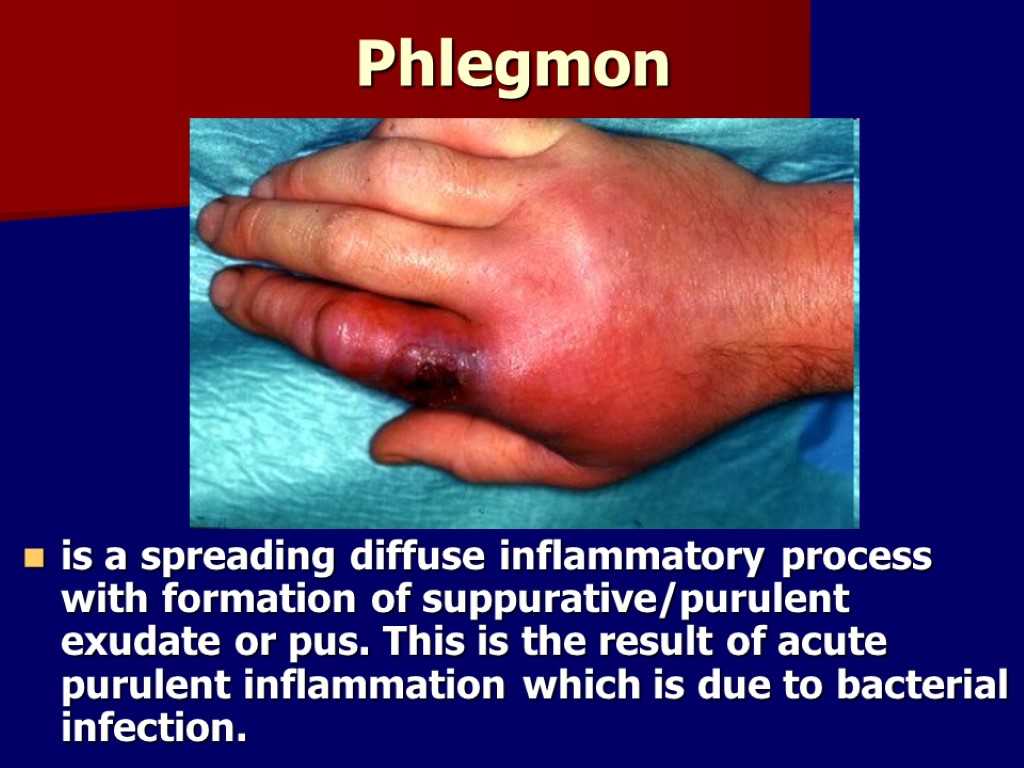
Phlegmon is a spreading diffuse inflammatory process with formation of suppurative/purulent exudate or pus. This is the result of acute purulent inflammation which is due to bacterial infection.
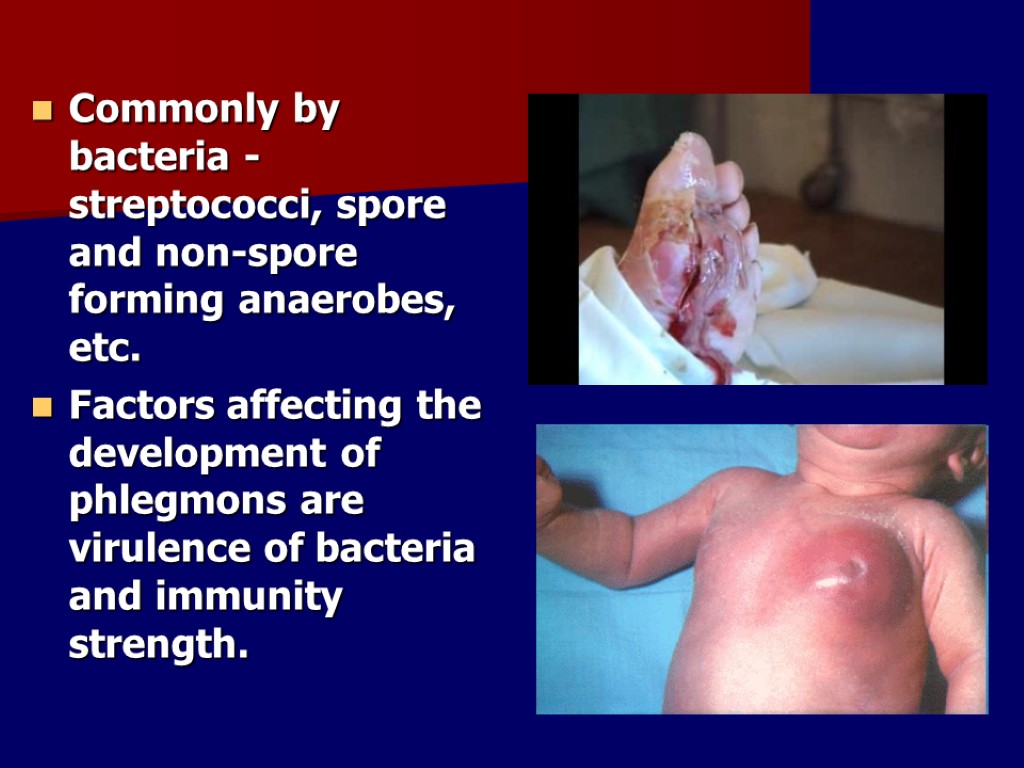
Commonly by bacteria - streptococci, spore and non-spore forming anaerobes, etc. Factors affecting the development of phlegmons are virulence of bacteria and immunity strength.
Clinical pictures Systemic features of infection such as increased body temperature (up to 38-40 °C), general fatigue, chills, sweatings, headache, loss of appetite). Inflammatory signs - dolor (localized pain), calor (increase local tissue temperature), rubor (skin redness/hyperemia), tumor (either clear or non-clear bordered tissue swelling), functio laesa (diminish affected function). NB: severity of patient condition with phlegmons is directly proportional to the degree of intoxication level i.e the severe the condition, the higher degree of intoxication level.
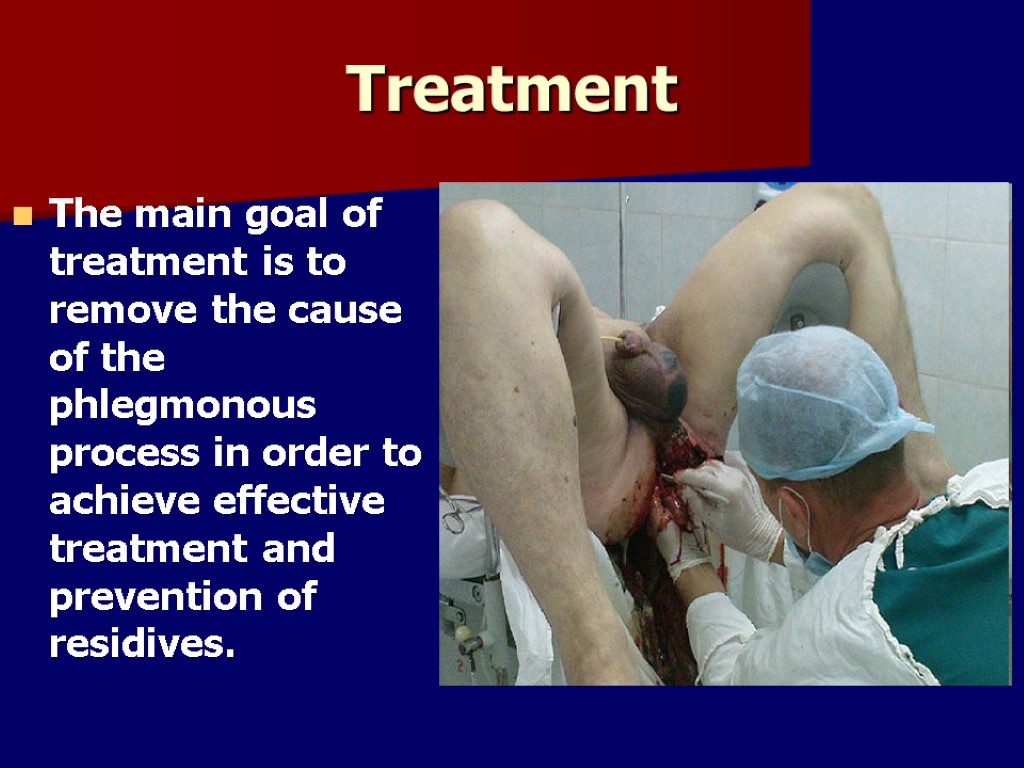
The main goal of treatment is to remove the cause of the phlegmonous process in order to achieve effective treatment and prevention of residives. Treatment

if the patient's condition is severe, however, immediate operation is usually necessary with application of drainage system. All of these are done under general anaesthesia. During operation, the cavity or place of phlegmonous process are washed with antiseptic solutions.
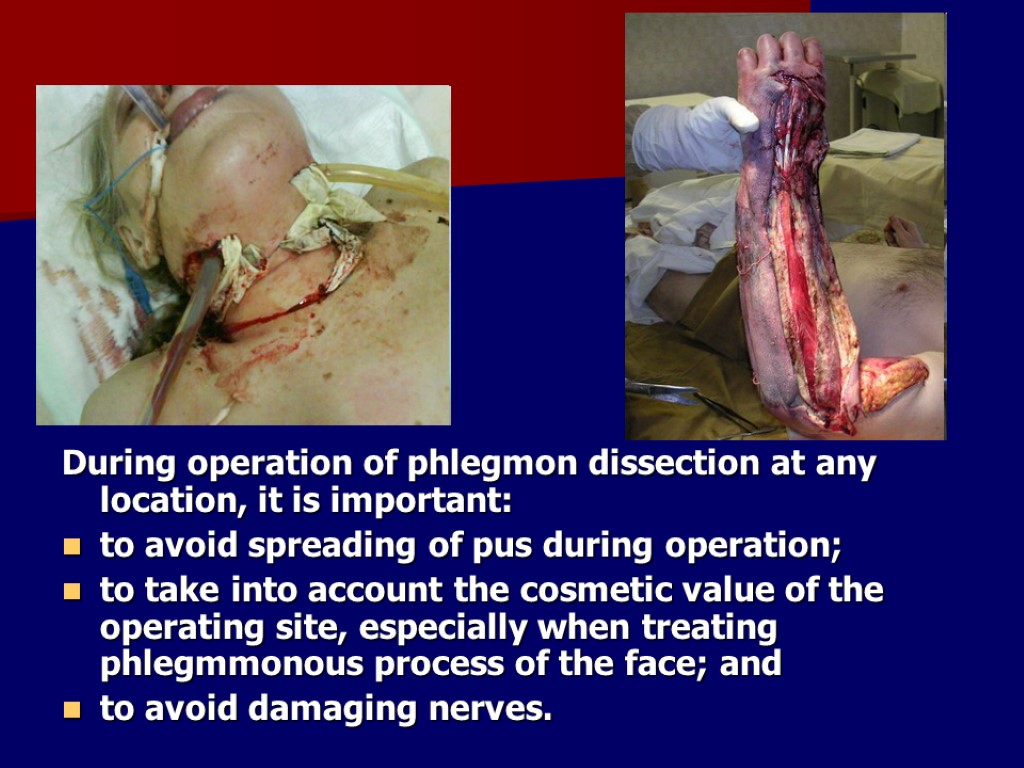
During operation of phlegmon dissection at any location, it is important: to avoid spreading of pus during operation; to take into account the cosmetic value of the operating site, especially when treating phlegmmonous process of the face; and to avoid damaging nerves.
In post-operative period, patients are treated with intravenous antibiotics, haemosorbtion, vitaminotherapy. Additionally, the use of i/v or i/m antistaphylococci γ-globulin or anatoxin can be taken as immunotherapy.
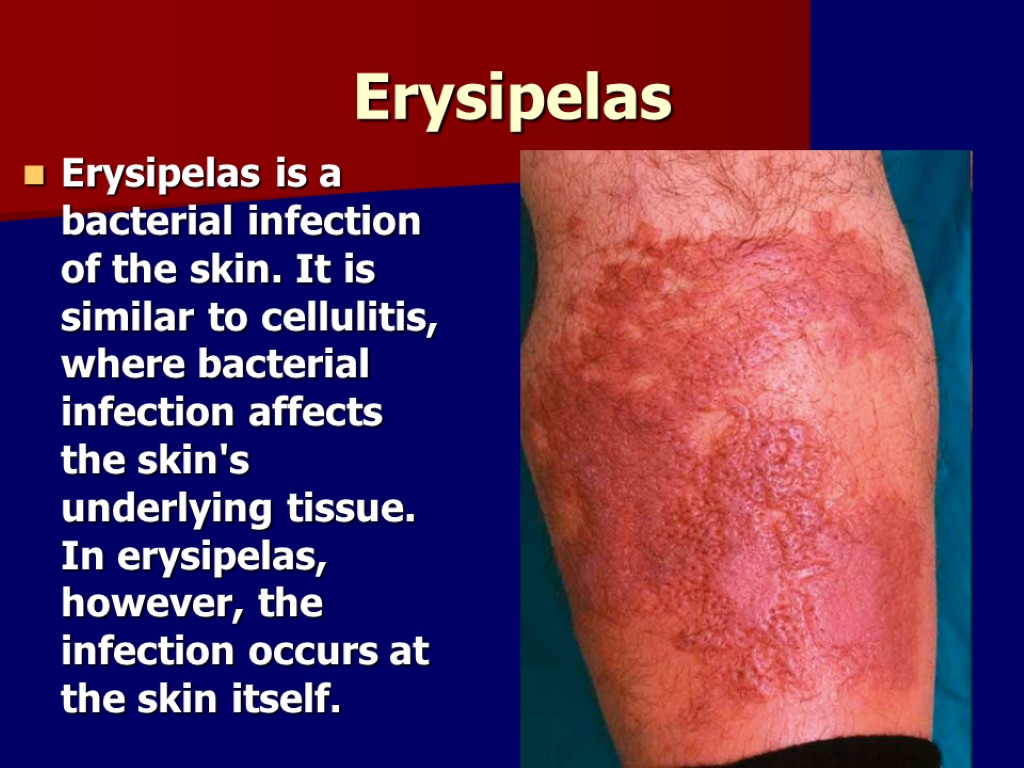
Erysipelas Erysipelas is a bacterial infection of the skin. It is similar to cellulitis, where bacterial infection affects the skin's underlying tissue. In erysipelas, however, the infection occurs at the skin itself.
The symptoms of erysipelas include: Sharply defined, bright red area of the skin Hot and painful area Slightly elevated as compared to the rest of the skin Sometimes a red streak extending to the lymph node can be noticed Fever and chills Vomiting
Most cases of erysipelas are due to Streptococcus pyogenes The infection may occur on any part of the skin including the face, arms, fingers, legs and toes, but it tends to favor the extremities. Fat tissue is most susceptible to infection, and facial areas typically around the eyes, ears, and cheeks.
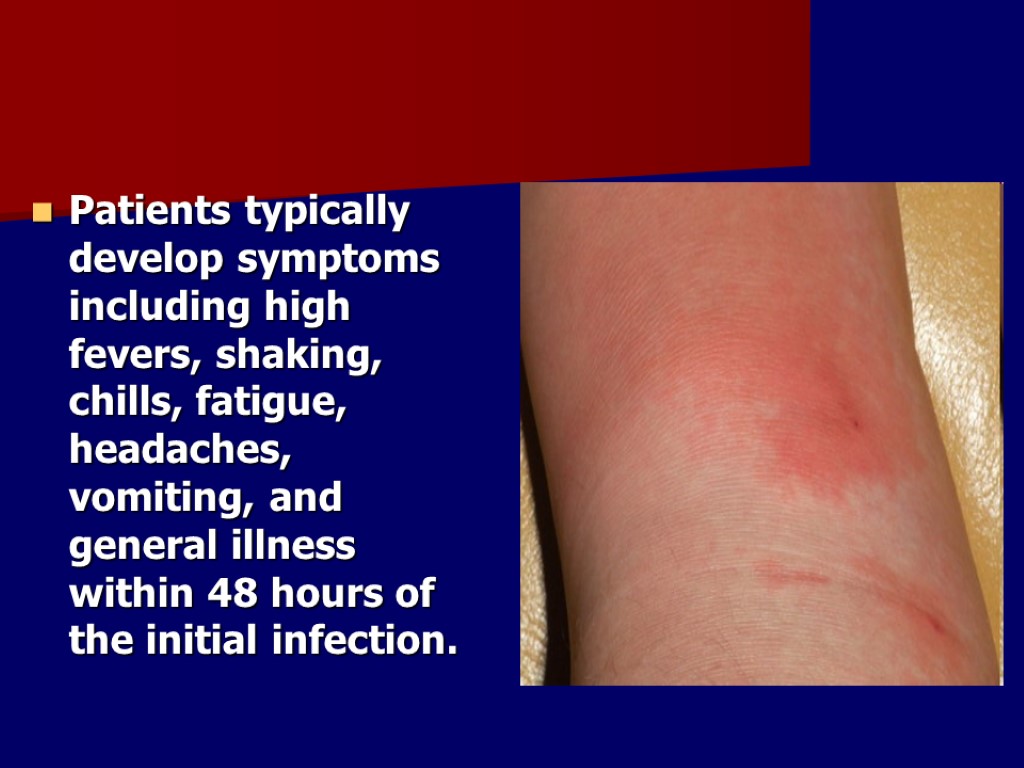
Patients typically develop symptoms including high fevers, shaking, chills, fatigue, headaches, vomiting, and general illness within 48 hours of the initial infection.
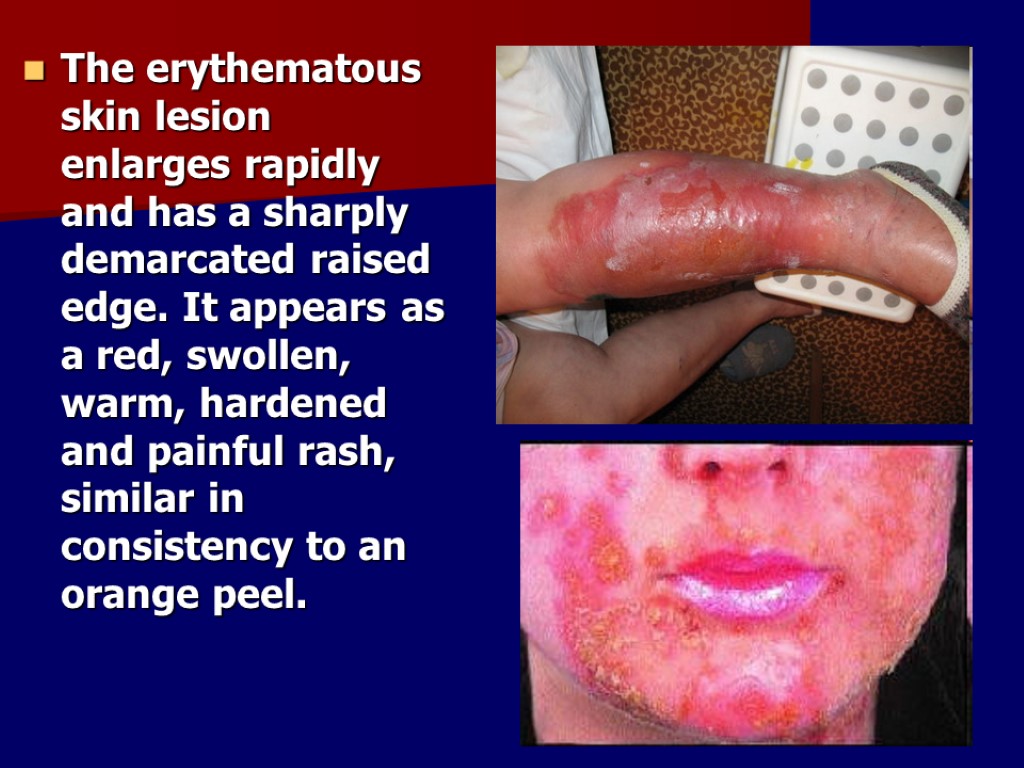
The erythematous skin lesion enlarges rapidly and has a sharply demarcated raised edge. It appears as a red, swollen, warm, hardened and painful rash, similar in consistency to an orange peel.
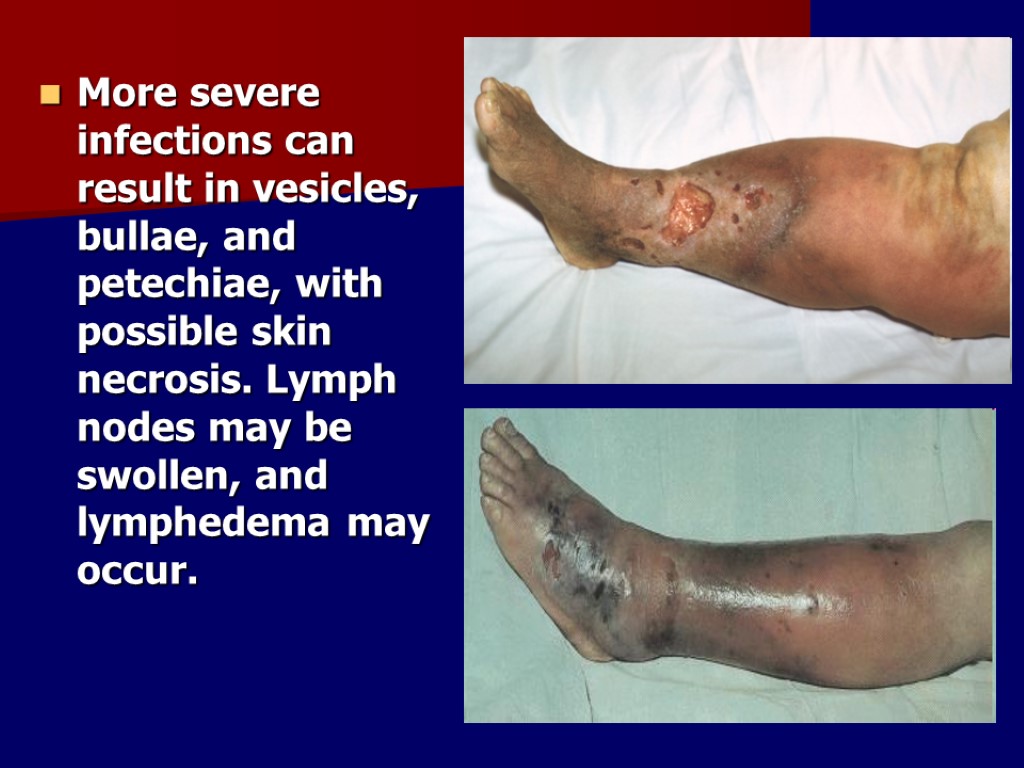
More severe infections can result in vesicles, bullae, and petechiae, with possible skin necrosis. Lymph nodes may be swollen, and lymphedema may occur.
Treatment Depending on the severity, treatment involves either oral or intravenous antibiotics, using penicillins, clindamycin or erythromycin. While illness symptoms resolve in a day or two, the skin may take weeks to return to normal. Because of the risk of reinfection, prophylactic antibiotics are sometimes used after resolution of the initial condition. However, this approach does not always stop reinfection.
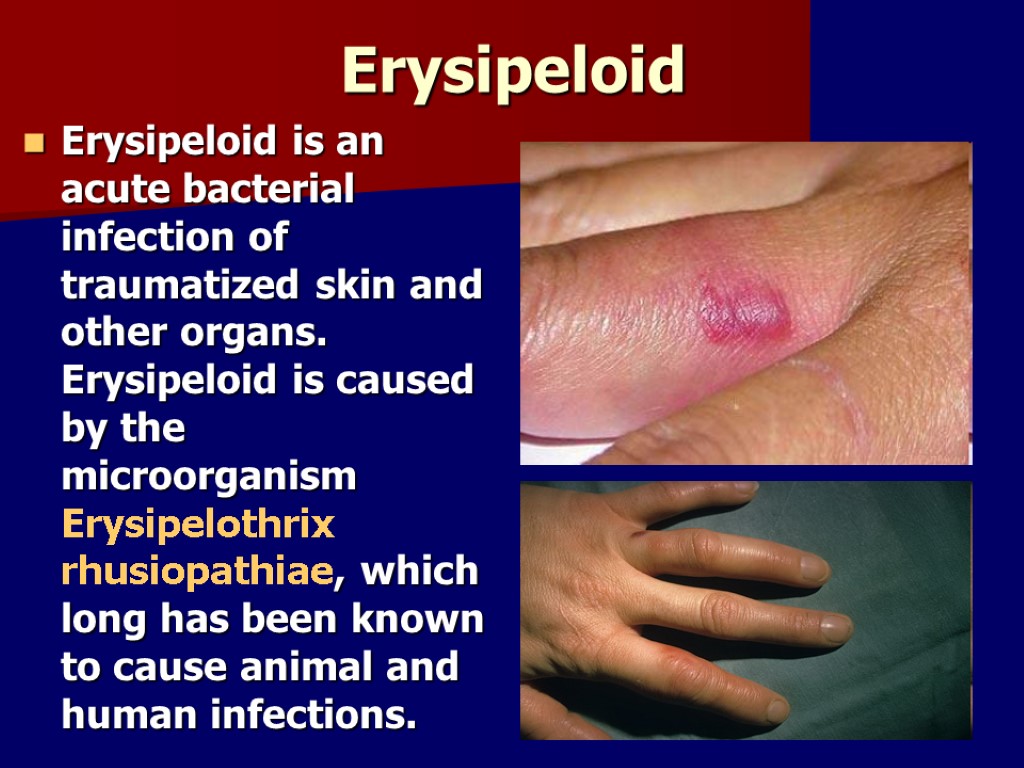
Erysipeloid Erysipeloid is an acute bacterial infection of traumatized skin and other organs. Erysipeloid is caused by the microorganism Erysipelothrix rhusiopathiae, which long has been known to cause animal and human infections.
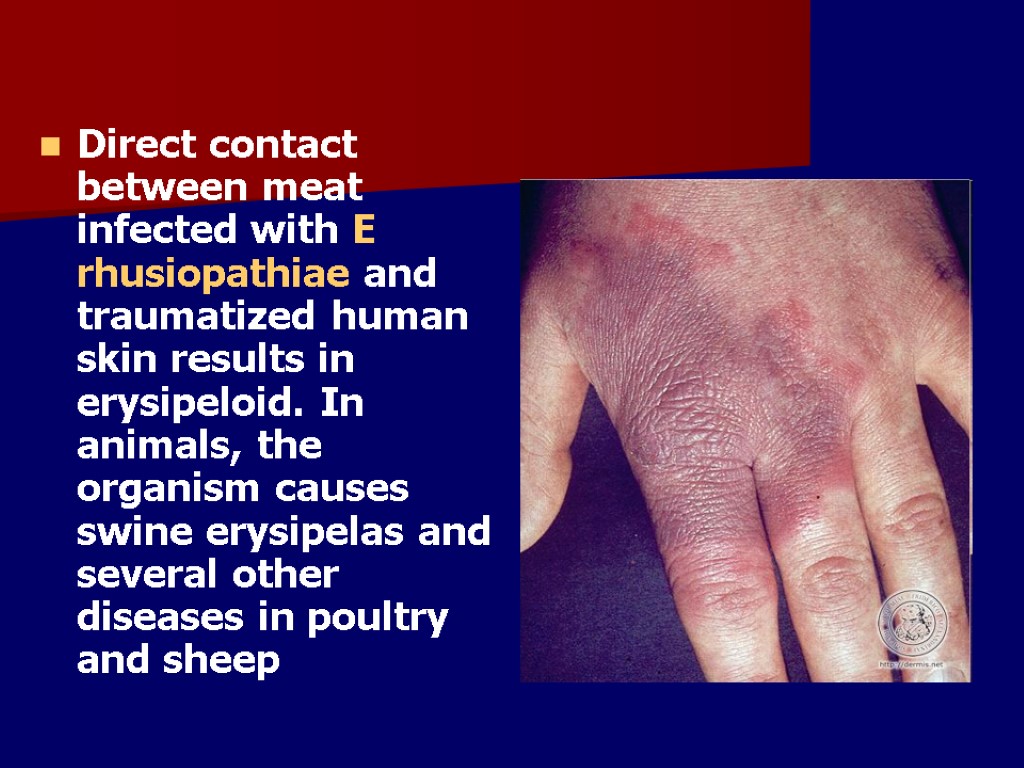
Direct contact between meat infected with E rhusiopathiae and traumatized human skin results in erysipeloid. In animals, the organism causes swine erysipelas and several other diseases in poultry and sheep
Humans acquire erysipeloid after direct contact with infected animals. Erysipeloid is more common among farmers, butchers, cooks, homemakers, and anglers. The infection is more likely to occur during the summer or early fall.
Erysipeloid may present in humans as one of 3 clinical forms. Localized cutaneous form (also known as erysipeloid of Rosenbach) Diffuse cutaneous form Generalized or systemic infection as evidenced by bacteremia: Endocarditis may or may not develop. In the first 2 forms of erysipeloid, patients present with local burning or pain at lesion sites. They may or not have fever, malaise, and other constitutional symptoms. In the generalized form, patients present with fever, chills, weight loss, and a variety of other symptoms (eg, joint pain, cough, headache), depending on the organ system involved.
Treatment The antibiotics of choice for the 3 forms of erysipeloid is penicillin or cephalosporin. E rhusiopathiae has been shown to be eradicated from surfaces by the use of simple home disinfectants; thus, an important step in the prevention of infection may be to spray hazardous work areas (eg, fishing boats, meat counters) with disinfectants.
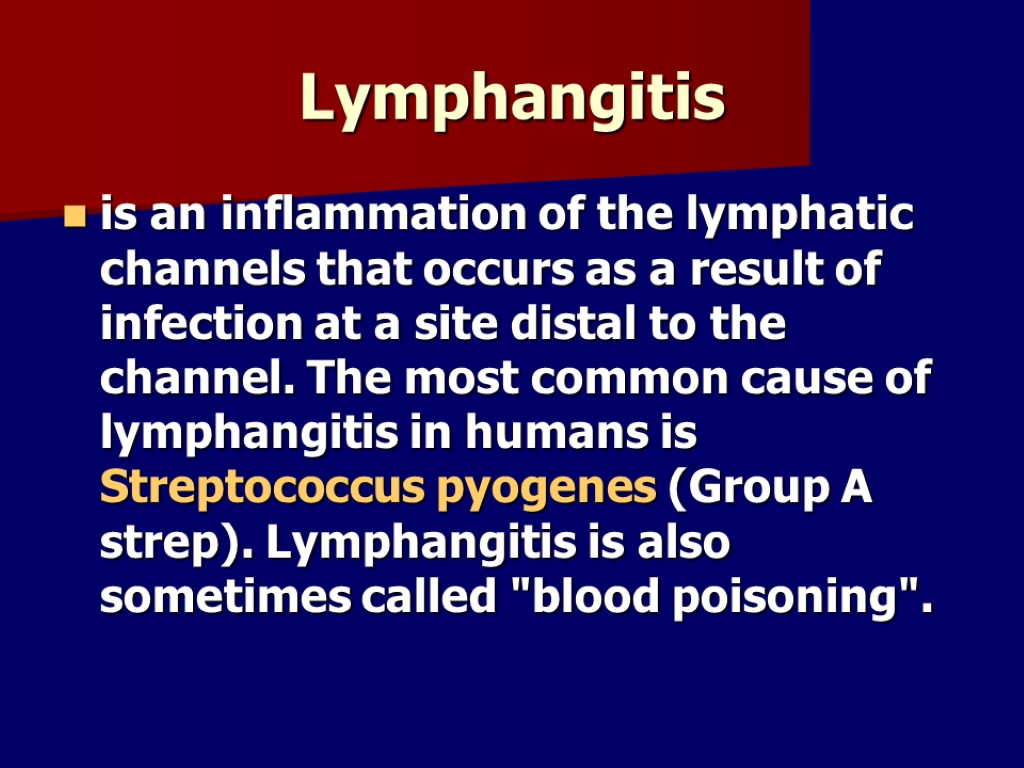
Lymphangitis is an inflammation of the lymphatic channels that occurs as a result of infection at a site distal to the channel. The most common cause of lymphangitis in humans is Streptococcus pyogenes (Group A strep). Lymphangitis is also sometimes called "blood poisoning".
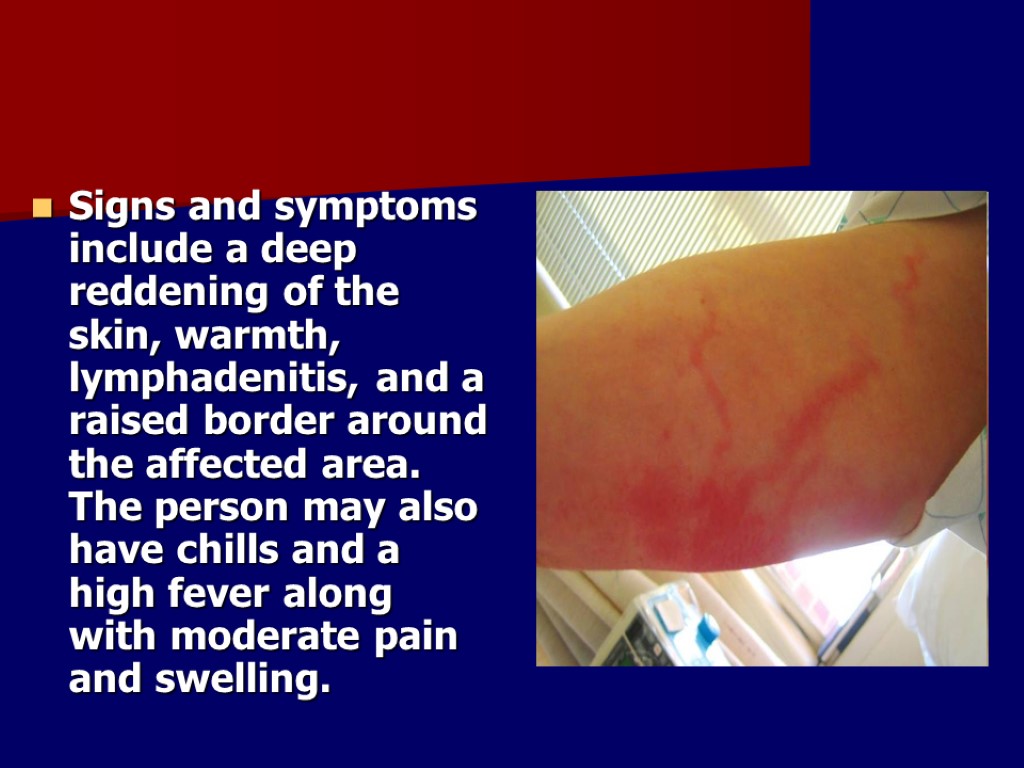
Signs and symptoms include a deep reddening of the skin, warmth, lymphadenitis, and a raised border around the affected area. The person may also have chills and a high fever along with moderate pain and swelling.
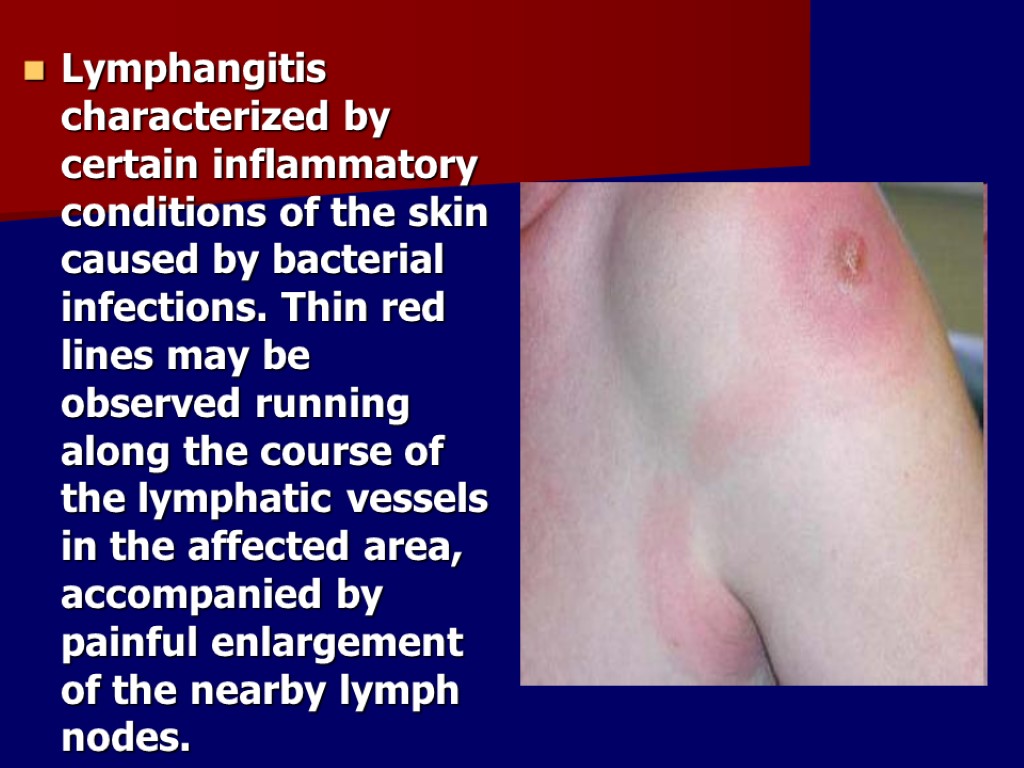
Lymphangitis characterized by certain inflammatory conditions of the skin caused by bacterial infections. Thin red lines may be observed running along the course of the lymphatic vessels in the affected area, accompanied by painful enlargement of the nearby lymph nodes.
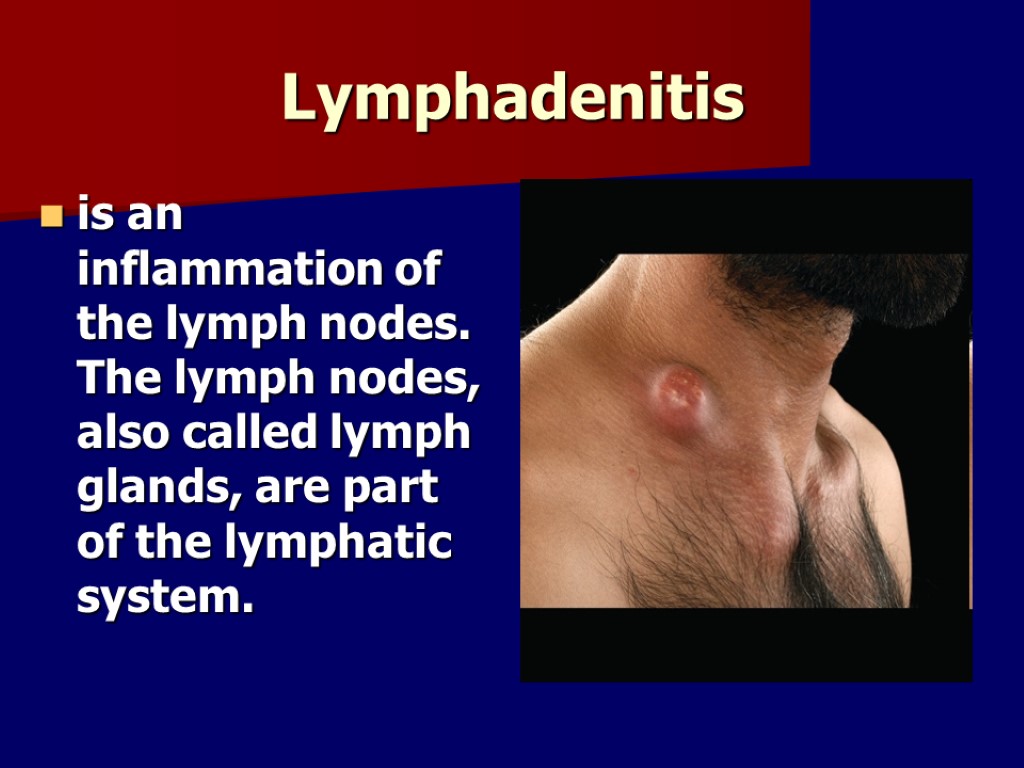
Lymphadenitis is an inflammation of the lymph nodes. The lymph nodes, also called lymph glands, are part of the lymphatic system.
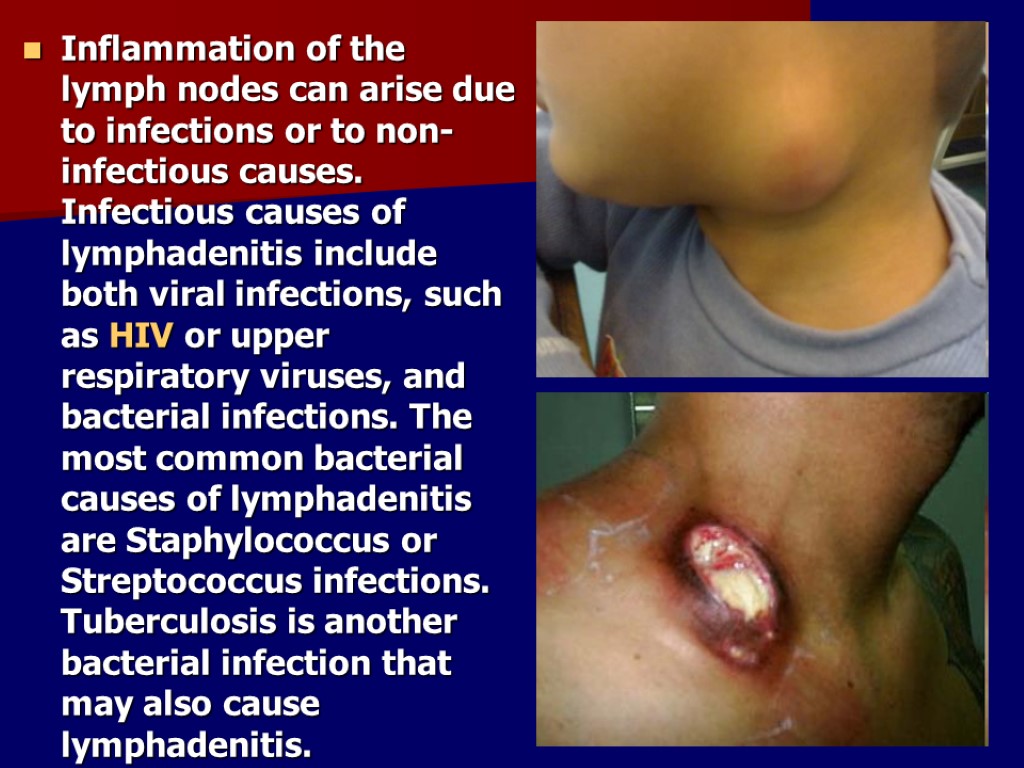
Inflammation of the lymph nodes can arise due to infections or to non-infectious causes. Infectious causes of lymphadenitis include both viral infections, such as HIV or upper respiratory viruses, and bacterial infections. The most common bacterial causes of lymphadenitis are Staphylococcus or Streptococcus infections. Tuberculosis is another bacterial infection that may also cause lymphadenitis.
Common symptoms of lymphadenitis Hard, swollen or tender lymph nodes Itchy skin Lump or mass that can be felt beneath the skin Rash Redness, warmth or swelling
life-threatening symptoms including: Difficulty breathing or rapid breathing High fever Rapid heart rate (tachycardia) Severe pain, redness, warmth or swelling
Treatments Analgesic drugs to control pain Antibiotic drugs to treat underlying infection Anti-inflammatory drugs to reduce swelling and inflammation Other drugs, depending upon the specific cause of lymphadenitis Surgery
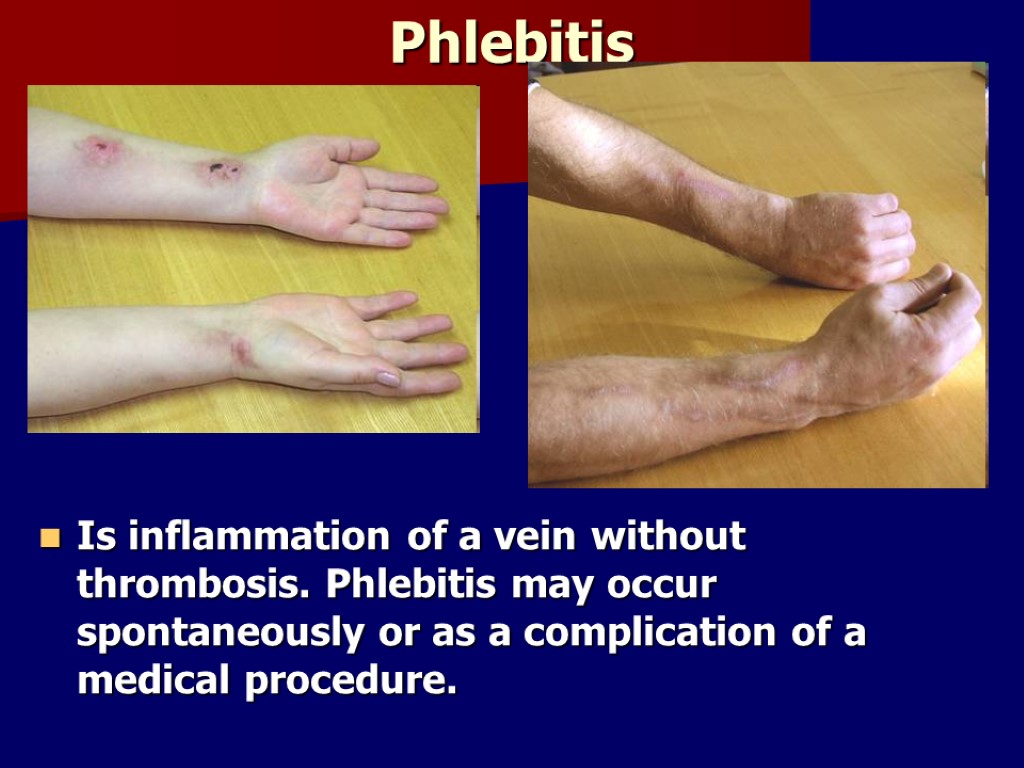
Phlebitis Is inflammation of a vein without thrombosis. Phlebitis may occur spontaneously or as a complication of a medical procedure.
Thrombophlebitis Thrombophlebitis is the term used when a blood clot in the vein causes the inflammation. Thrombophlebitis usually occurs in leg veins, but it may occur in an arm. The thrombus (clot) in the vein causes pain and irritation and may block blood flow in the veins. Phlebitis can occur in both the surface (superficial) or deep veins.
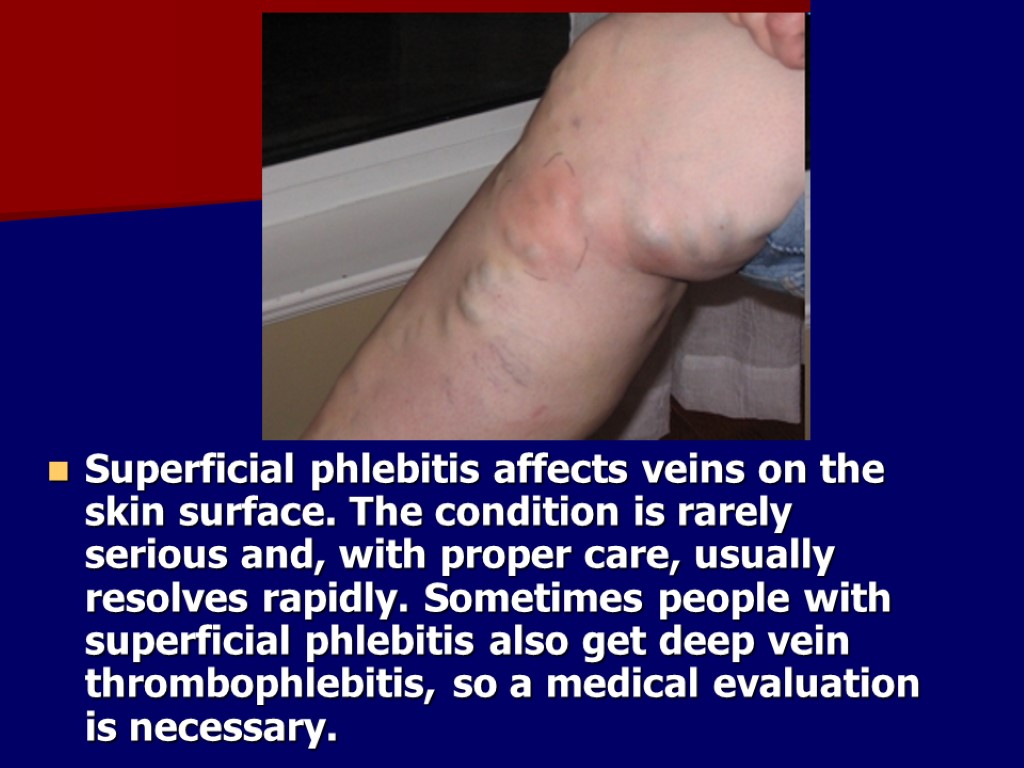
Superficial phlebitis affects veins on the skin surface. The condition is rarely serious and, with proper care, usually resolves rapidly. Sometimes people with superficial phlebitis also get deep vein thrombophlebitis, so a medical evaluation is necessary.

Deep venous thrombosis refers to a blood clot embedded in one of the major deep veins of the lower legs, thighs, or pelvis.
Three factors may lead to formation of a clot inside a blood vessel: Damage to the inside of a blood vessel due to trauma or other conditions Changes in normal blood flow, including unusual turbulence, or partial or complete blockage of blood flow Hypercoagulability, a rare state in which the blood is more likely than usual to clot
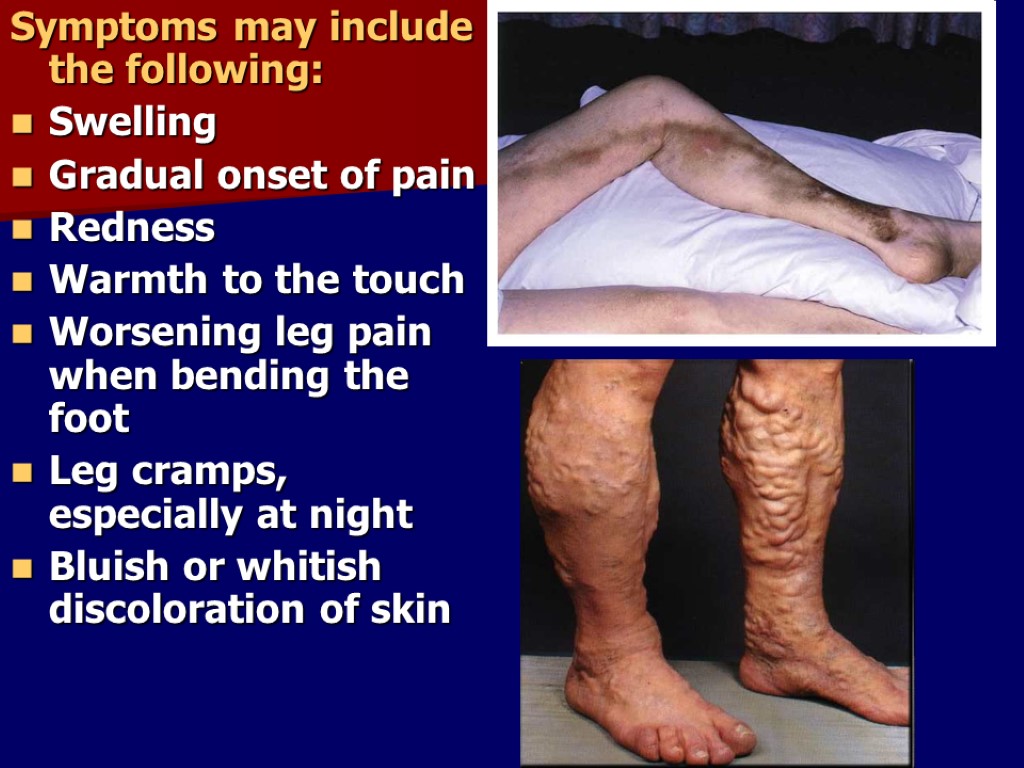
Symptoms may include the following: Swelling Gradual onset of pain Redness Warmth to the touch Worsening leg pain when bending the foot Leg cramps, especially at night Bluish or whitish discoloration of skin

Medical Treatment The treatment of blood clots depends upon their location in the body. Most commonly, though, anticoagulation or blood thinning medication is prescribed to prevent further clot formation and to minimize the risk that part of the blood clot will break off and travel to the lung and cause pulmonary embolism.
Anticoagulation is the treatment of choice and is a two stage process. Low molecular weight heparin (enoxaparin [Lovenox], dalteparin [Fragmin]) injections are started to begin immediate blood thinning.
Compression stockings are useful in preventing a complication of a leg blood clot called postthrombotic syndrome or postphlebitis syndrome, in which the affected leg swells and becomes chronically painful. These stockings may be purchased over-the-counter or can be custom fitted. It is recommended that they be worn for at least a year after the diagnosis of deep venous thrombosis.
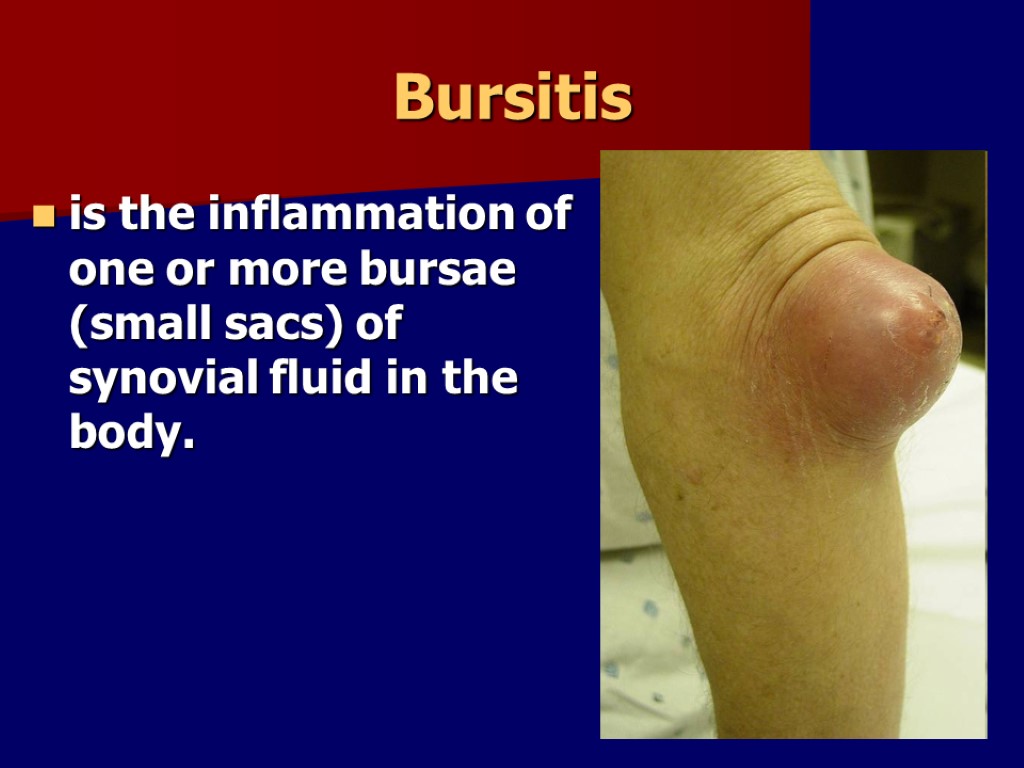
Bursitis is the inflammation of one or more bursae (small sacs) of synovial fluid in the body.
Bursitis is commonly caused by repetitive movement and excessive pressure. Elbows and knees are the most commonly affected. Inflammation of the bursae might also be caused by other inflammatory conditions such as rheumatoid arthritis.
Traumatic injury is another cause of bursitis. The inflammation irritates because the bursa no longer fits in the original small area between the bone and the functionary muscle or tendon. When the bone increases pressure upon the bursa, bursitis results.

Treatment Bursae that are not infected can be treated with rest, ice, elevation, physiotherapy, anti-inflammatory drugs and pain medication. Since bursitis is caused by increased friction from the adjacent structures, a compression bandage is contraindicated because compression would create more friction on movement (passive and active). Advanced massage therapy techniques can also be employed to help with the inflammatory process of bursitis.
Bursae that are infected requires further investigation and antibiotic therapy. In cases when all conservative treatment fails, surgical therapy may be necessary. In a bursectomy the bursa is cut out either endoscopically or with open surgery. The bursa grows back in place after a couple of weeks but without any inflammatory component.
Septic arthritis Septic arthritis is a rather rare but important disease characterized by inflammation of a synovial membrane with purulent effusion into the joint capsule, usually due to bacterial infection. It typically affects monoarticular joints. This disease entity also is referred to in the literature as bacterial, suppurative, purulent, or infectious arthritis.

Treatment Treatment consists of a combined medical and surgical approach. If rapid improvement is not achieved with needle aspiration, open drainage and lavage (arthroscopically or via arthrotomy) is strongly recommended.
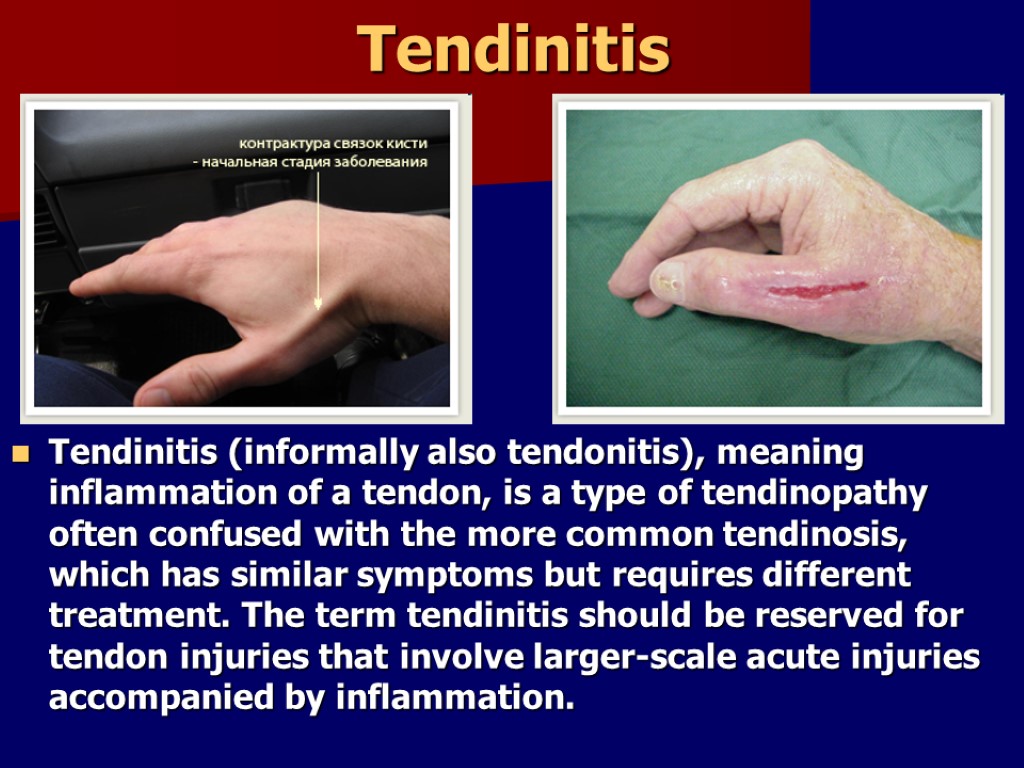
Tendinitis Tendinitis (informally also tendonitis), meaning inflammation of a tendon, is a type of tendinopathy often confused with the more common tendinosis, which has similar symptoms but requires different treatment. The term tendinitis should be reserved for tendon injuries that involve larger-scale acute injuries accompanied by inflammation.
Symptoms can vary from aches or pains and local stiffness, to a burning that surrounds the whole joint around the inflamed tendon. Swelling may happen along with heat and redness, but not in all cases, there may be visible knots surrounding joint. With this condition, the pain is usually worse during and after activity, and the tendon and joint area can become stiffer the following day as muscles tighten from the movement of the tendon.
Treatment Treatment of tendon injuries is largely conservative. Use of non-steroidal anti-inflammatory drugs, rest, and gradual return to exercise is a common therapy. Resting assists in the prevention of further damage to the tendon. Ice, compression and elevation are also frequently recommended. Physical therapy, orthotics or braces may also be useful. Initial recovery is typically within 2 to 3 days and full recovery is within 4 to 6 weeks.
Empyema is a collection of pus in the space between the lung and the inner surface of the chest wall (pleural space). Empyema is usually caused by an infection that spreads from the lung. It leads to a buildup of pus in the pleural space. There can be a pint or more of infected fluid. This fluid puts pressure on the lungs.
Symptoms Chest pain, which worsens when you breathe in deeply (pleurisy) Dry cough Excessive sweating, especially night sweats Fever and chills General discomfort, uneasiness, or ill feeling Shortness of breath Weight loss (unintentional)
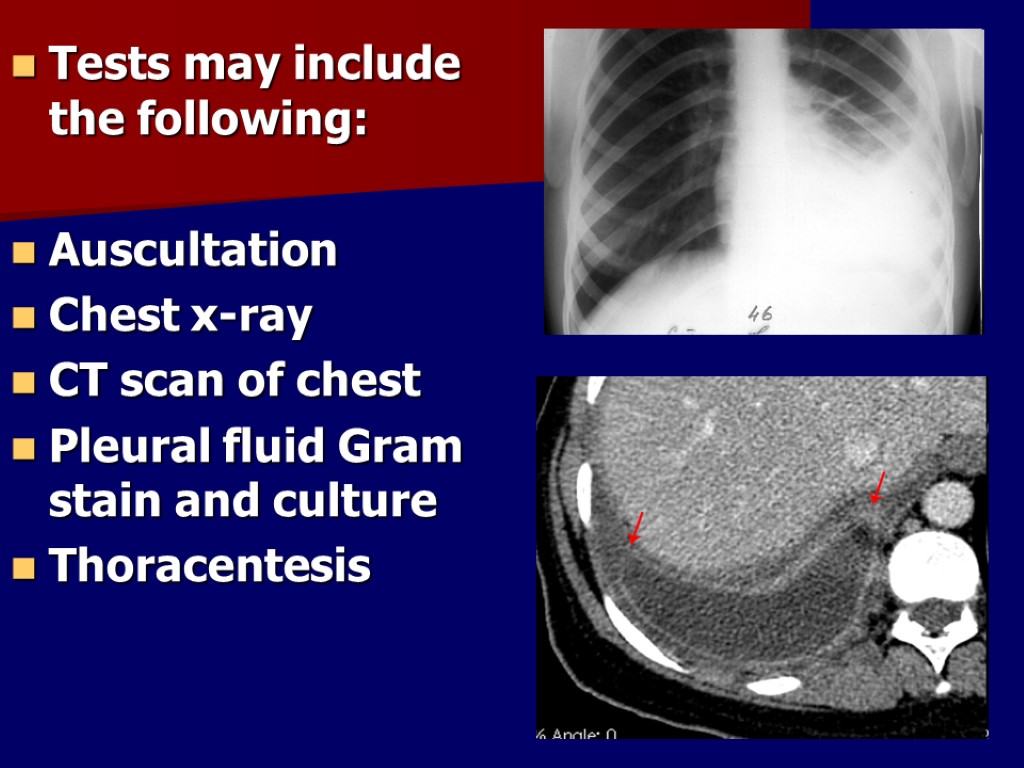
Tests may include the following: Auscultation Chest x-ray CT scan of chest Pleural fluid Gram stain and culture Thoracentesis
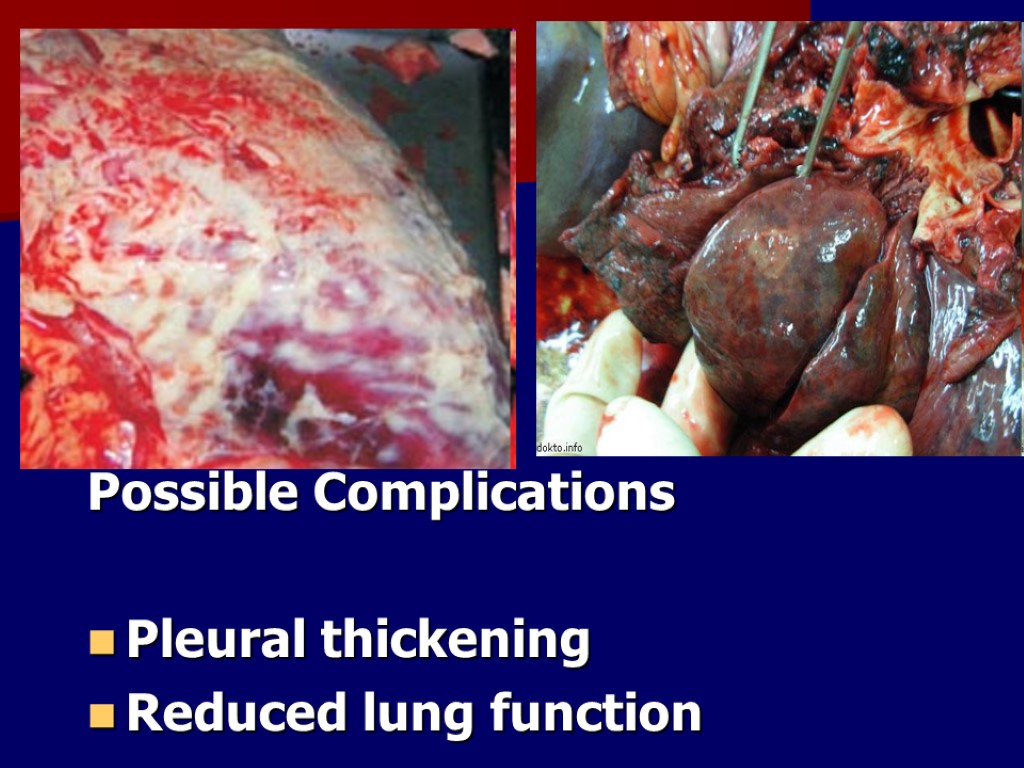
Possible Complications Pleural thickening Reduced lung function
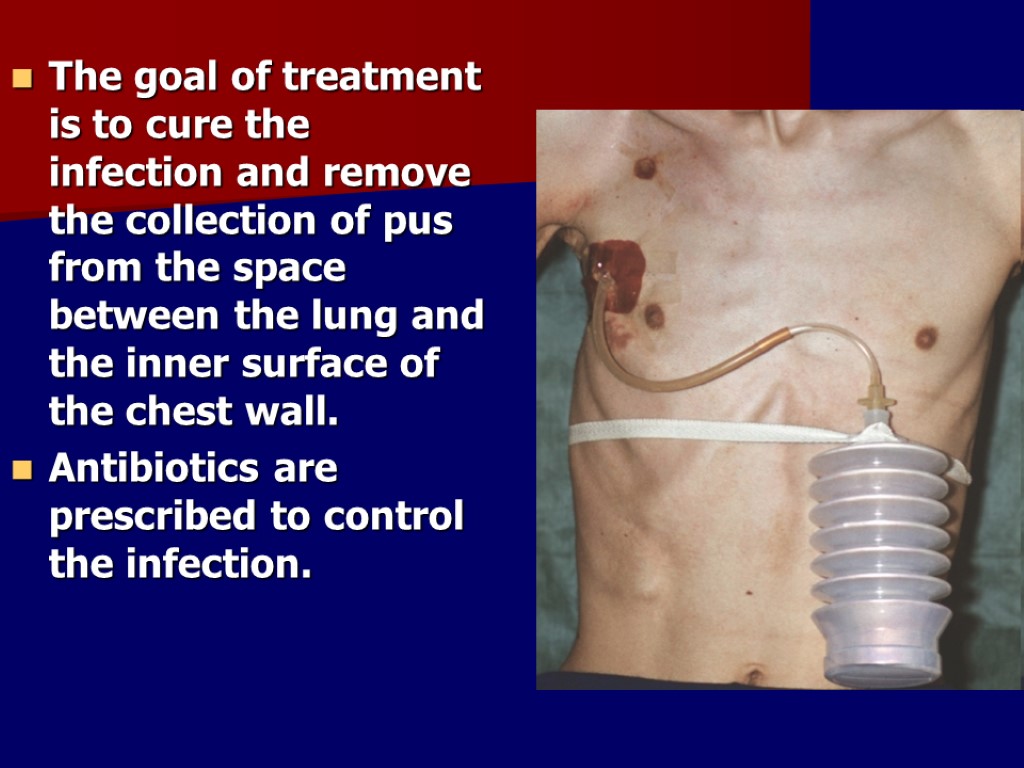
The goal of treatment is to cure the infection and remove the collection of pus from the space between the lung and the inner surface of the chest wall. Antibiotics are prescribed to control the infection.
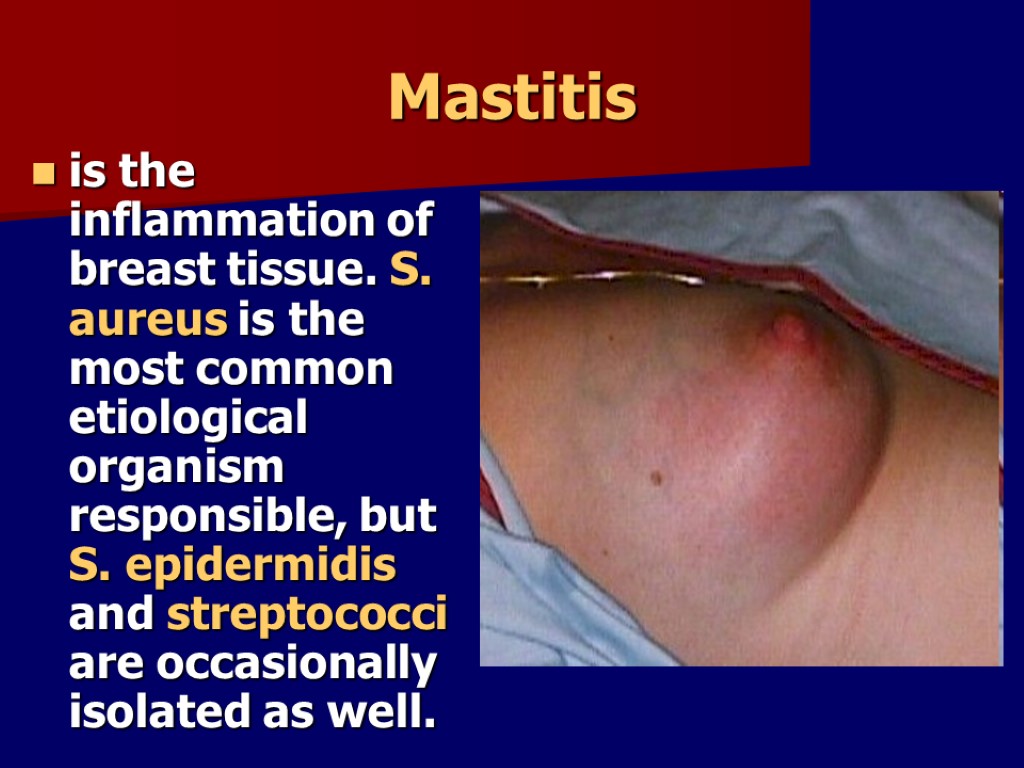
Mastitis is the inflammation of breast tissue. S. aureus is the most common etiological organism responsible, but S. epidermidis and streptococci are occasionally isolated as well.
Mastitis typically develops when the milk is not properly removed from the breast. Milk stasis can lead to the milk ducts in the breasts becoming blocked, as the breast milk not being properly and regularly expressed. Mastitis may occur when the baby is not appropriately attached to the breast while feeding, when the baby has infrequent feeds or has problems suckling the milk out of the breast.
Types: serosal infiltrative purulent abscessed phlegmonous gangrenous
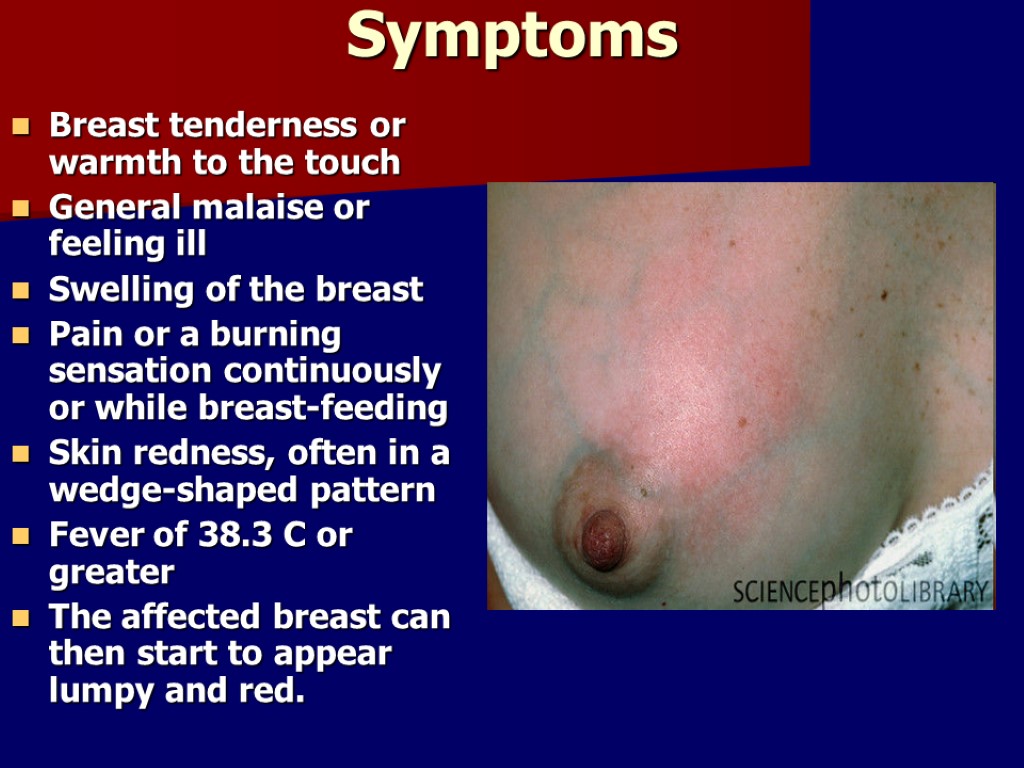
Symptoms Breast tenderness or warmth to the touch General malaise or feeling ill Swelling of the breast Pain or a burning sensation continuously or while breast-feeding Skin redness, often in a wedge-shaped pattern Fever of 38.3 C or greater The affected breast can then start to appear lumpy and red.
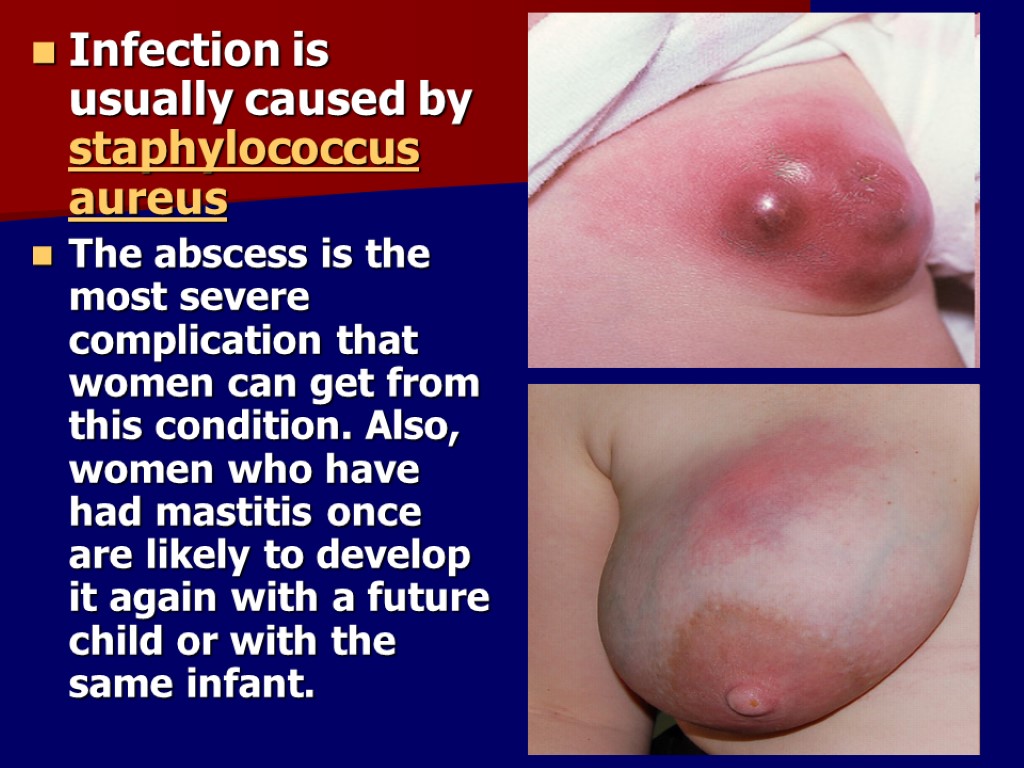
Infection is usually caused by staphylococcus aureus The abscess is the most severe complication that women can get from this condition. Also, women who have had mastitis once are likely to develop it again with a future child or with the same infant.
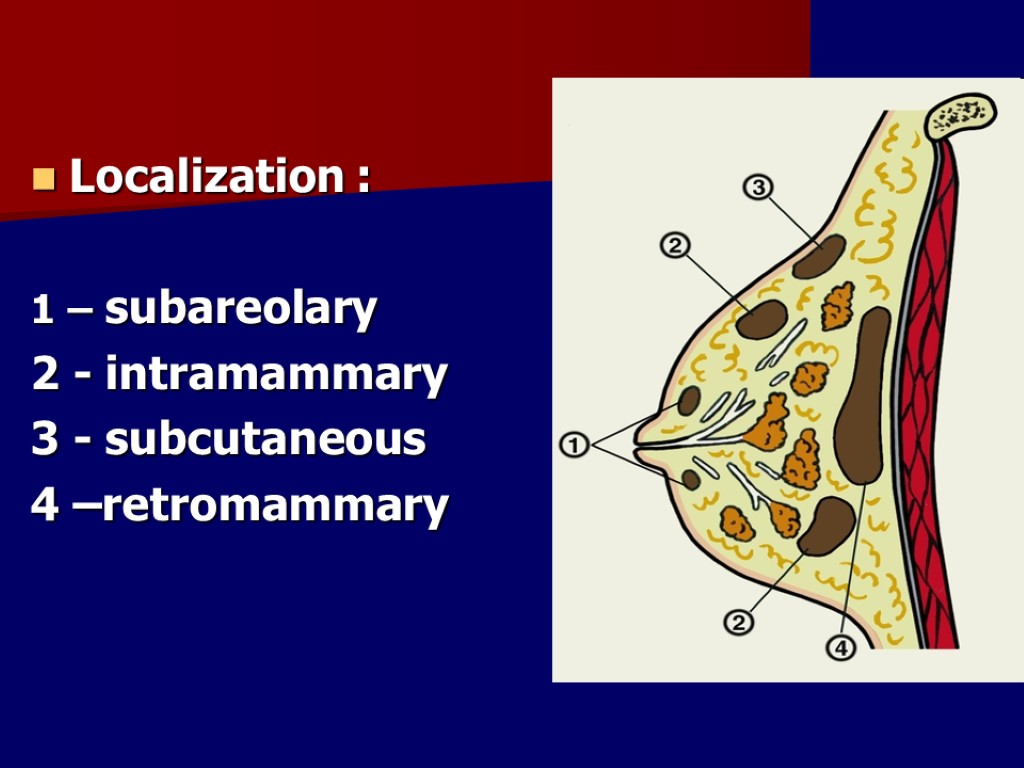
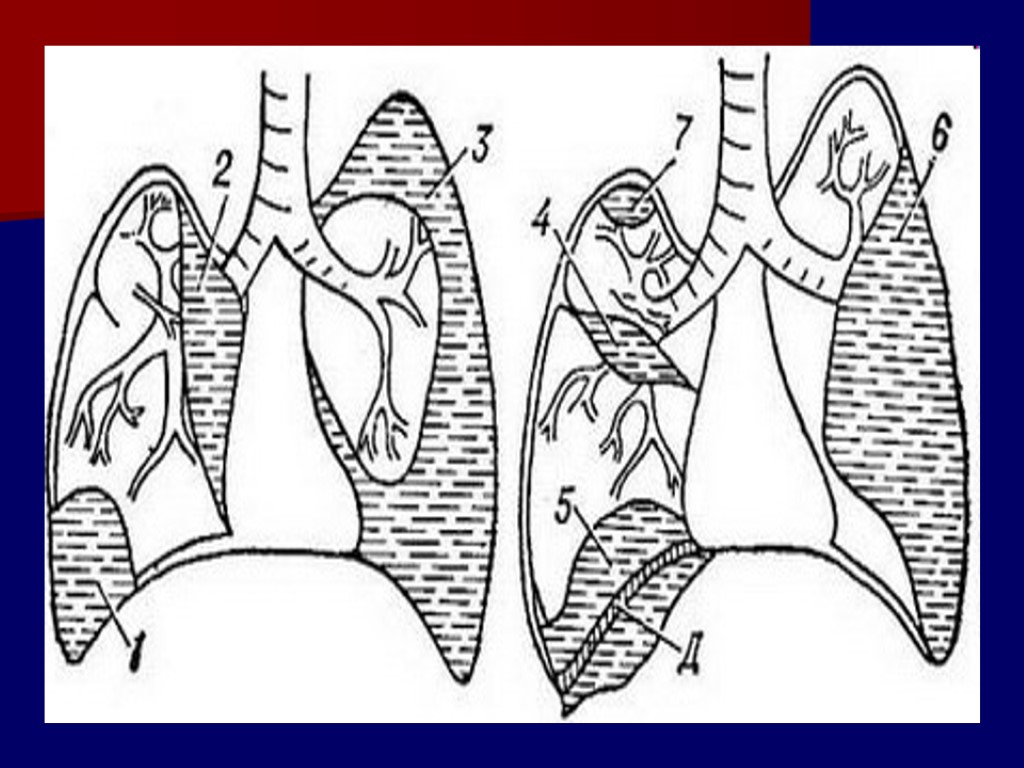
Localization : 1 – subareolary 2 - intramammary 3 - subcutaneous 4 –retromammary
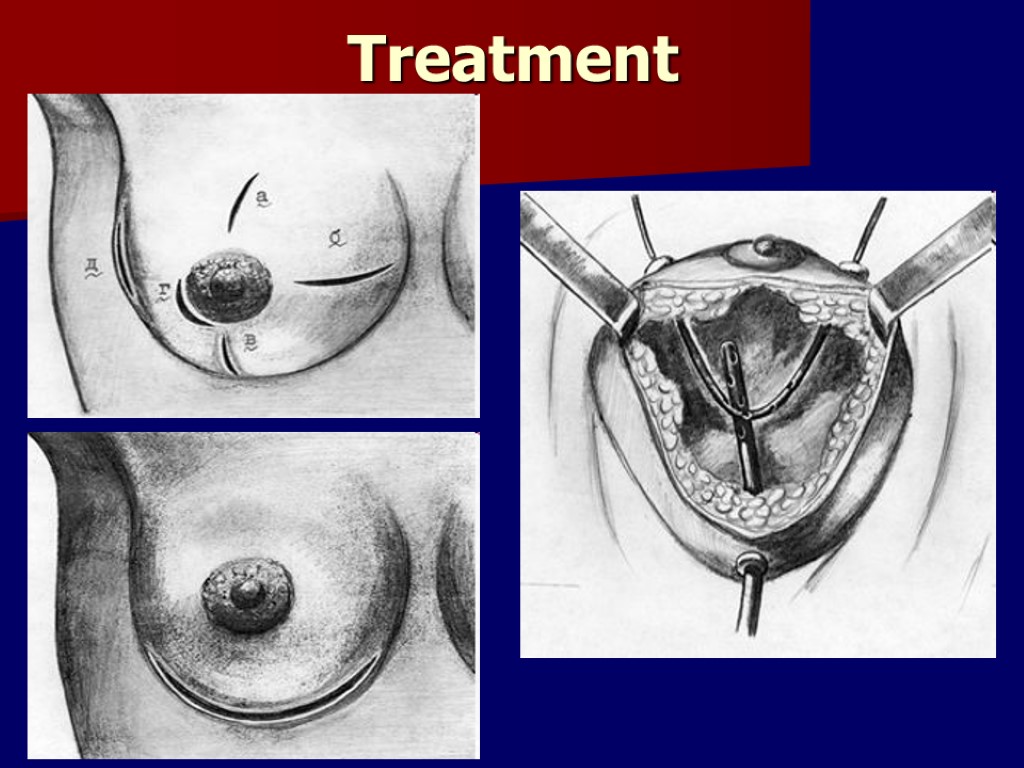
Treatment
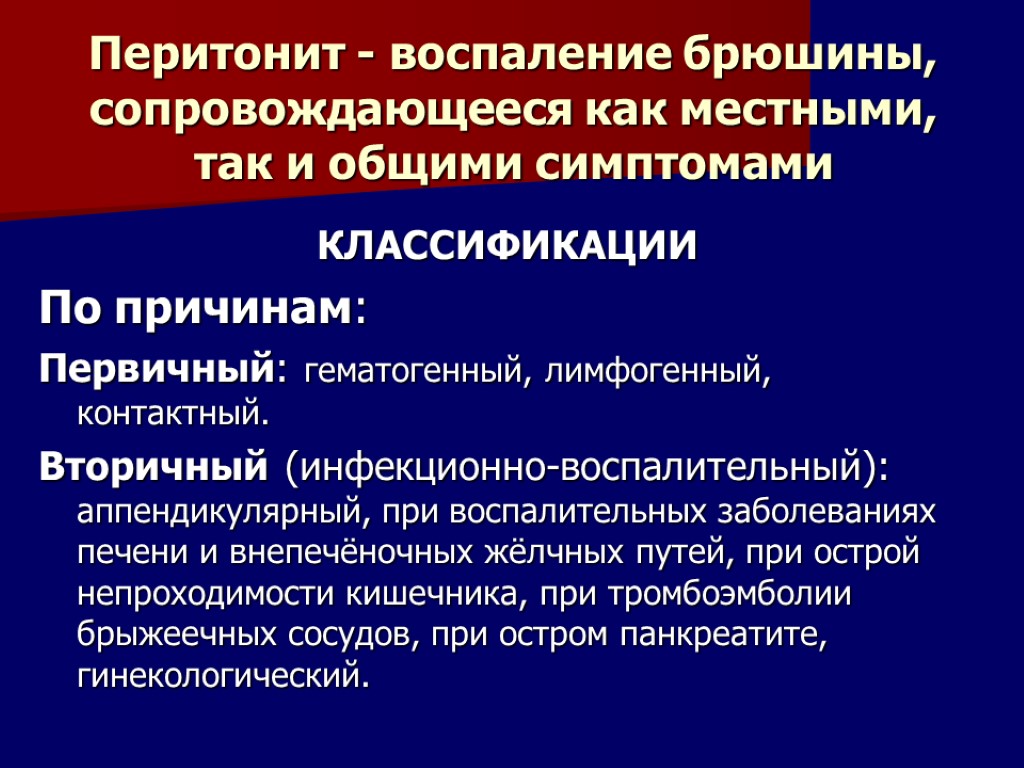
Перитонит - воспаление брюшины, сопровождающееся как местными, так и общими симптомами КЛАССИФИКАЦИИ По причинам: Первичный: гематогенный, лимфогенный, контактный. Вторичный (инфекционно-воспалительный): аппендикулярный, при воспалительных заболеваниях печени и внепечёночных жёлчных путей, при острой непроходимости кишечника, при тромбоэмболии брыжеечных сосудов, при остром панкреатите, гинекологический.
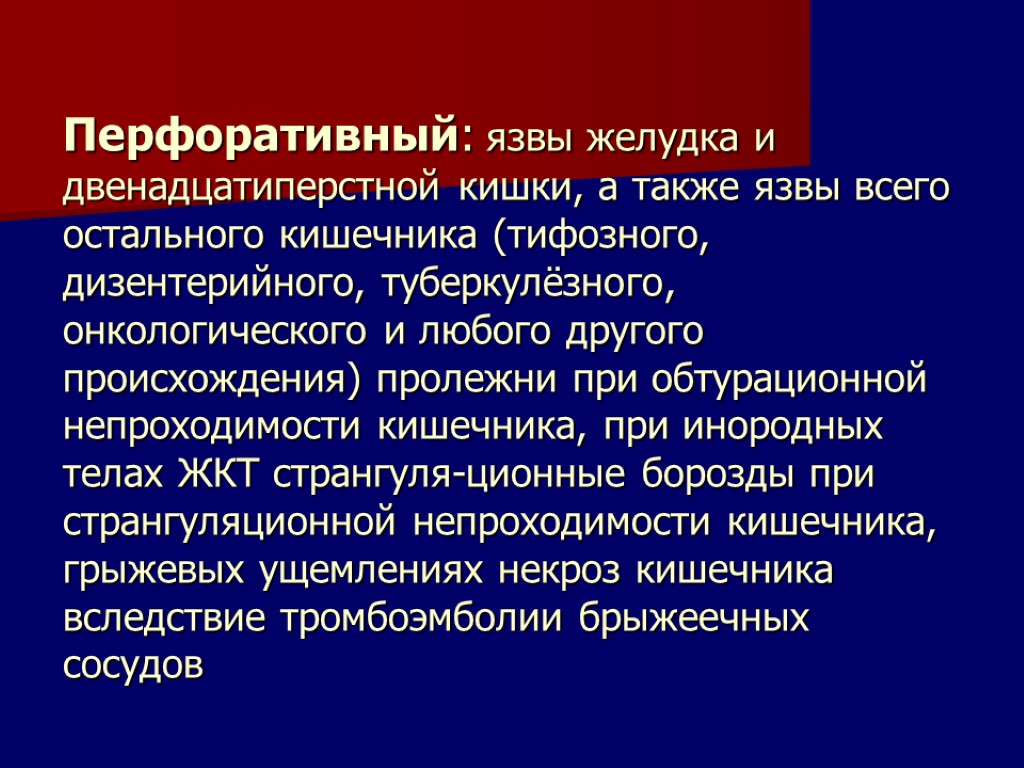
Перфоративный: язвы желудка и двенадцатиперстной кишки, а также язвы всего остального кишечника (тифозного, дизентерийного, туберкулёзного, онкологического и любого другого происхождения) пролежни при обтурационной непроходимости кишечника, при инородных телах ЖКТ странгуля-ционные борозды при странгуляционной непроходимости кишечника, грыжевых ущемлениях некроз кишечника вследствие тромбоэмболии брыжеечных сосудов
Травматический: при открытых и закрытых повреждениях органов брюшной полости Послеоперационный: несостоятельность швов после операций на органах брюшной полости, инфицирование брюшной полости во время операции, дефекты наложения лигатур на большие участки сальника и брыжейки с последующим некрозом тканей дистальнее лигатуры, механическое повреждение брюшины, её высыхание, кровоизлияние в свободную брюшную полость при недостаточно надёжном гемостазе.
По характеру экссудата: серозный, фибринозный, гнойный, геморрагический, каловый, гнилостный, сочетания вышеперечисленных форм (например, серозно-фибринозный, фибринозно-гнойный и т.п.).
По степени распространения Отграниченный перитонит (абсцесс или инфильтрат): аппендикулярный, поддиафрагмальный, подпечёночный, тазовый, межкишечный. Диффузный перитонит Местный - в непосредственной близости от источника инфекции, занимает одну анатомическую область живота. Склонен к генерализации Распространённый - занимает две анатомические области живота и более Общий - тотальное поражение брюшины
По фазам развития Реактивная (первые 24 ч) - в клинической картине превалирует местная симптоматика Токсическая (24-72 ч) -фаза нарастающей интоксикации. Соответствует понятию эндотоксиновый шок Терминальная (свыше 72 ч) - равнозначна понятию септический шок
Этиология Микробный (бактериальный) перитонит Неспецифический (вызванный микрофлорой ЖКТ) Специфический (вызванный микрофлорой, не имеющей отношения к ЖКТ) Асептический (абактериальный, токсико-химический) Особые формы перитонита (канцероматозный, паразитарный, ревматоидный, гранулематозный)
Патогенез Интоксикация Гипоксия Нарушения моторики ЖКТ, гемодинамики, метаболизма, иммунной защиты Полиорганная недостаточность
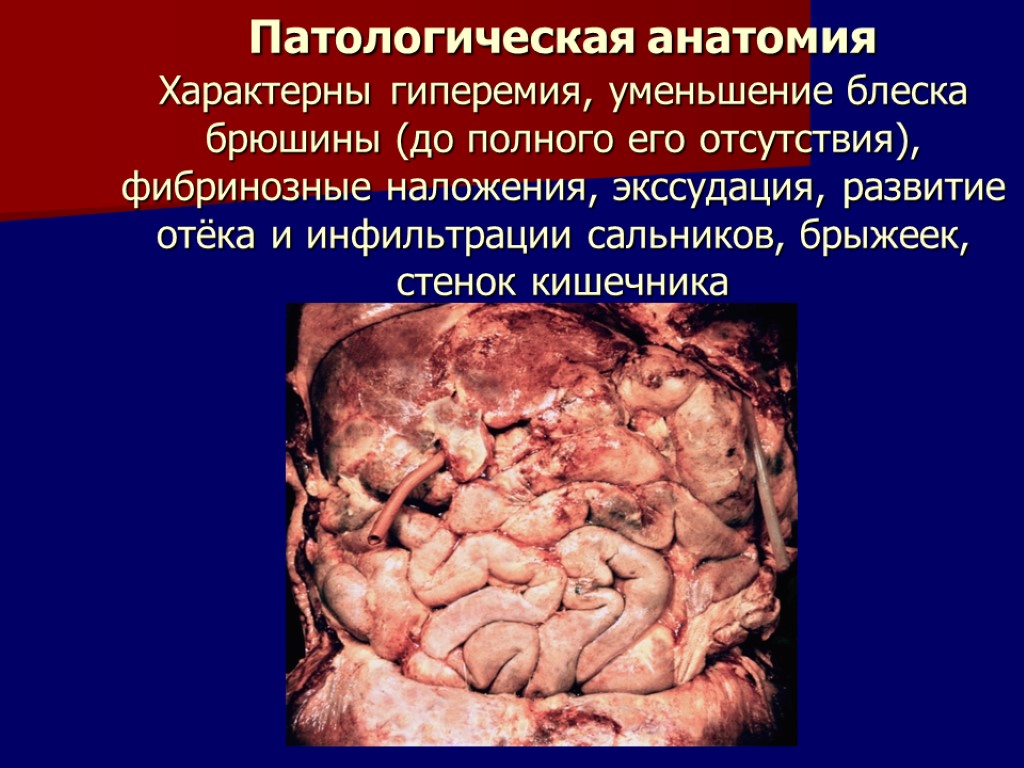
Патологическая анатомия Характерны гиперемия, уменьшение блеска брюшины (до полного его отсутствия), фибринозные наложения, экссудация, развитие отёка и инфильтрации сальников, брыжеек, стенок кишечника
Клиническая картина Боль Иррадиация боли в плечи или надключичные области (симптом Элеккера) Напряжение мышц передней брюшной стенки (Реактивная фаза - доскообразное напряжение. Токсическая фаза -расслабление мышц) Симптомы раздражения брюшины (Щёткина- Блюмберга, Менделя, Воскресенского) Тошнота и рвота
Диагностика Пальцевое исследование прямой кишки и влагалищное исследование - выраженная болезненность передней стенки прямой кишки или сводов влагалища (симптом Куленкампффа) Лабораторные исследования: лейкоцитоз, нейтрофилёз, сдвиг лейкоцитарной формулы влево, увеличение СОЭ. Увеличение остаточного азота крови. Сгущение крови по показателю Ht. Метаболический ацидоз. Дыхательный ацидоз.

Рентгенологическое исследование

УЗИ: наличие свободной жидкости, абсцессы
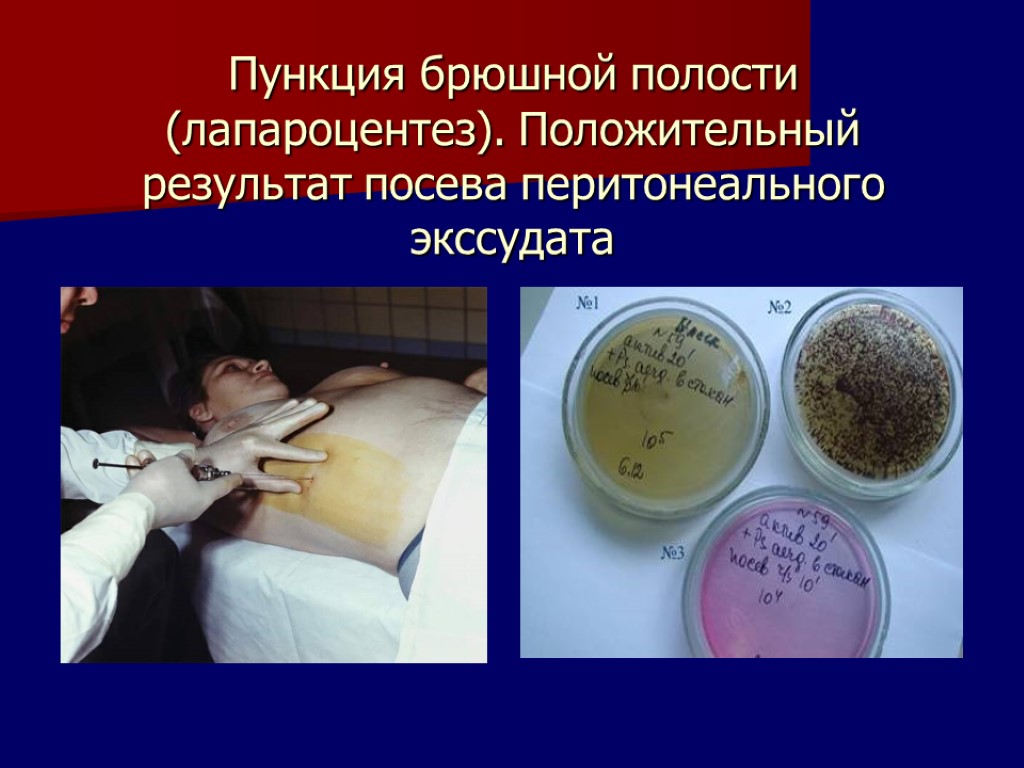
Пункция брюшной полости (лапароцентез). Положительный результат посева перитонеального экссудата

Диагностическая лапароскопия
Дифференциальная диагностика Заболевания лёгких и плевры (пневмония, плеврит, повреждения лёгких и рёбер, гемо- и пневмоторакс) Сердечно-сосудистые заболевания (стенокардия, инфаркт миокарда, аневризма брюшной аорты и её ветвей) Повреждения позвоночника и спинного мозга (туберкулёзный спондилит, опухоли и остеомиелит позвоночника) Эндокринные заболевания и метаболические расстройства (сахарный диабет, гиперкальциемия, гипокалиемия,уремия)
Дифференциальная диагностика Инфекционные болезни (пищевые токсикоинфекции, вирусный гепатит, грипп, тонзиллит, скарлатина, дифтерия, дизентерия, брюшной тиф) Заболевания мочеполовых органов (подвижная почка, мочекаменная болезнь, острый пиелит, гидронефроз, опухоли и амилоидоз почек) Заболевания и повреждения передней брюшной стенки (гематомы, абсцессы, опухоли)
ЛЕЧЕНИЕ ПРЕДОПЕРАЦИОННАЯ ПОДГОТОВКА Длительность предоперационной подготовки от 1-го до 3-х часов Инфузионная терапия в высоком темпе через 2-3 венозных сосуда одновременно в условиях ОРИТ Борьба с эндотоксическим и гиповолемическим шоком
АНЕСТЕЗИЯ - операцию выполняют под общим обезболиванием с интубацией трахеи и применением миорелаксантов.
ЦЕЛИ ОПЕРАЦИИ: Устранение (отграничение) источника перитонита Удаление из брюшной полости экссудата и тщательная санация Введение в брюшной полость антибиотиков Декомпрессия ЖКТ при наличии выраженного пареза или паралича кишечника Установка в забрюшинной пространство катетеров для осуществления тотальной пролонгированной забрюшинной нейровегетативной блокады Адекватное дренирование брюшной полости
Оперативный доступ: срединная лапаротомия с аппаратной коррекцией доступа по методике Сигала

Интраоперационная санация брюшной полости

Декомпрессия кишечника: назогастроинтестинальная интубация тонкой кишки по Эбботту-Миллеру

Дренирование брюшной полости: хлорвиниловые или резиновые трубки, многоканальные силиконовые дренажи, дренаж из полупроницаемой гидратцеллюлозной мембраны

Завершение операции: закрытый метод, полуоткрытый метод (плановые релапаротомии), открытый метод (перитонеостомия)
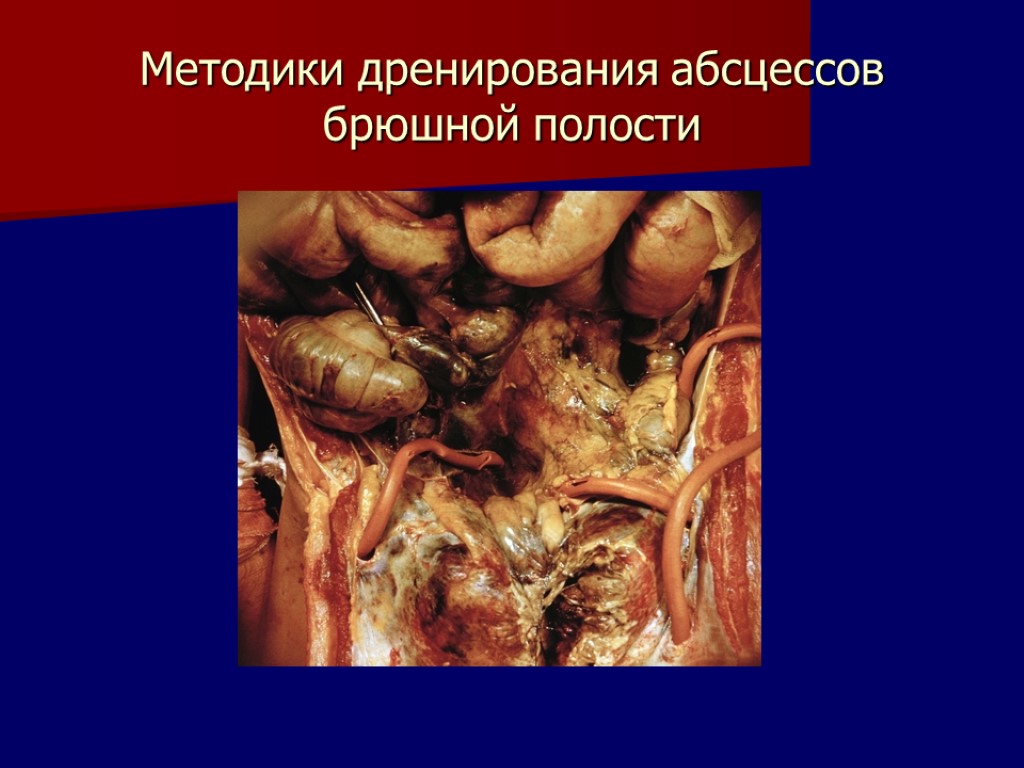
Методики дренирования абсцессов брюшной полости

Пункция и дренирование абсцесса под контролем УЗИ

Пункционное дренирование поддиафрагмального и подпеченочного абсцессов

Пункционное лечение подпеченочных абсцессов
Консервативная терапия в послеоперационном периоде Адекватное обезболивание Сбалансированная инфузионная терапия Профилактика и лечение синдрома полиорганной недостаточности Коррекция метаболических сдвигов
Выведение токсинов методами эфферентной хирургии: гемосорбция гемодиализ ультрафильтрация лечебный плазмаферез поэтажная сорбционная гемоперфузия брюшной полости энтеросорбция экстракорпоральная оксигенация

Антибактериальная терапия Иммунная терапия Восстановление функций ЖКТ
Течение и прогноз Летальность при распространённом гнойном перитоните - 25-30%, при развитии полиорганной недостаточности -85-90%
acute_purulent_infections.ppt
- Количество слайдов: 111

