acute pancreatitis.pptx
- Количество слайдов: 36
 Acute pancreatitis acute pancreatitis
Acute pancreatitis acute pancreatitis
 Definition Acute pancreatitis a sudden inflammation of the pancreas caused b y autodigestion and marked by symptoms of acu te abdomen andescape of pancreatic enzymes i nto the pancreatic tissues. introduction
Definition Acute pancreatitis a sudden inflammation of the pancreas caused b y autodigestion and marked by symptoms of acu te abdomen andescape of pancreatic enzymes i nto the pancreatic tissues. introduction
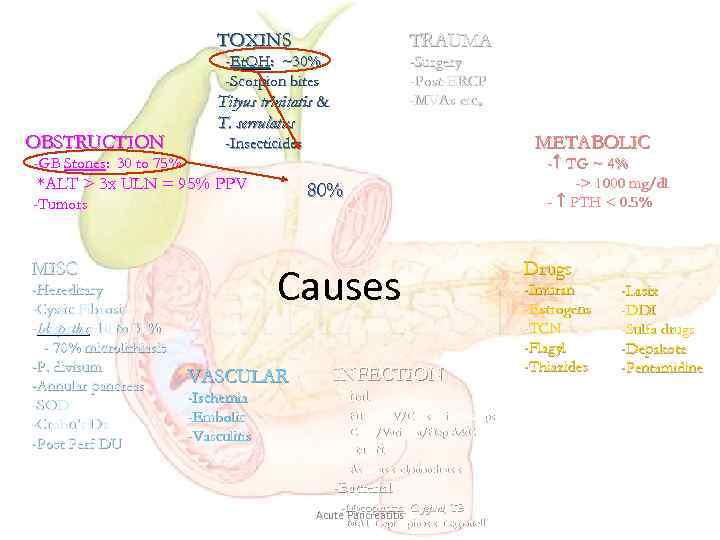 TOXINS TRAUMA -Et. OH: ~30% -Scorpion bites OBSTRUCTION -Surgery -Post-ERCP -MVAs etc. Tityus trinitatis & T. serrulatus METABOLIC -Insecticides - TG ~ 4% -> 1000 mg/dl - PTH < 0. 5% -GB Stones: 30 to 75% *ALT > 3 x ULN = 95% PPV 80% -Tumors MISC -Hereditary -Cystic Fibrosis -Idiopathic: 10 to 30% - 70% microlithiasis -P. divisum -Annular pancreas -SOD -Crohn’s Dz -Post Perf DU Causes VASCULAR -Ischemia -Embolic -Vasculitis INFECTION -Viral -HIV/EBV/Coxsackie/Mumps -CMV/Varicella/Hep A&C -Parasitic -Ascariasis, clonorchiasis -Bacterial -Mycoplasma, C. jejuni, TB Acute Pancreatitis -MAI, Leptospirosis, Legionella Drugs -Imuran -Estrogens -TCN -Flagyl -Thiazides -Lasix -DDI -Sulfa drugs -Depakote -Pentamidine
TOXINS TRAUMA -Et. OH: ~30% -Scorpion bites OBSTRUCTION -Surgery -Post-ERCP -MVAs etc. Tityus trinitatis & T. serrulatus METABOLIC -Insecticides - TG ~ 4% -> 1000 mg/dl - PTH < 0. 5% -GB Stones: 30 to 75% *ALT > 3 x ULN = 95% PPV 80% -Tumors MISC -Hereditary -Cystic Fibrosis -Idiopathic: 10 to 30% - 70% microlithiasis -P. divisum -Annular pancreas -SOD -Crohn’s Dz -Post Perf DU Causes VASCULAR -Ischemia -Embolic -Vasculitis INFECTION -Viral -HIV/EBV/Coxsackie/Mumps -CMV/Varicella/Hep A&C -Parasitic -Ascariasis, clonorchiasis -Bacterial -Mycoplasma, C. jejuni, TB Acute Pancreatitis -MAI, Leptospirosis, Legionella Drugs -Imuran -Estrogens -TCN -Flagyl -Thiazides -Lasix -DDI -Sulfa drugs -Depakote -Pentamidine
 Forms of the disease I. Edematous (interstitial) pancreatitis. II. The sterile pancreatic necrosis. - On the prevalence of lesions: a limited and widespread. - The nature of the defeat: fat, bloody, mixed. III. infected pancreatic necrosis
Forms of the disease I. Edematous (interstitial) pancreatitis. II. The sterile pancreatic necrosis. - On the prevalence of lesions: a limited and widespread. - The nature of the defeat: fat, bloody, mixed. III. infected pancreatic necrosis
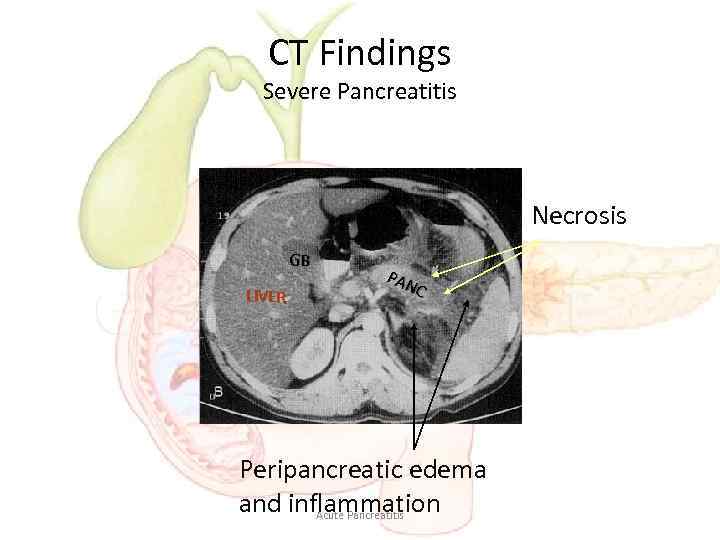 CT Findings Severe Pancreatitis Necrosis GB LIVER PAN C Peripancreatic edema and inflammation Acute Pancreatitis
CT Findings Severe Pancreatitis Necrosis GB LIVER PAN C Peripancreatic edema and inflammation Acute Pancreatitis
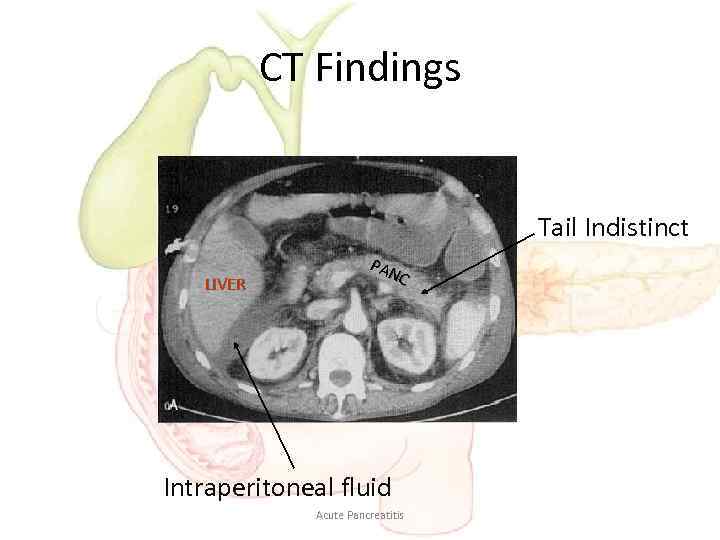 CT Findings Tail Indistinct LIVER PAN C Intraperitoneal fluid Acute Pancreatitis
CT Findings Tail Indistinct LIVER PAN C Intraperitoneal fluid Acute Pancreatitis
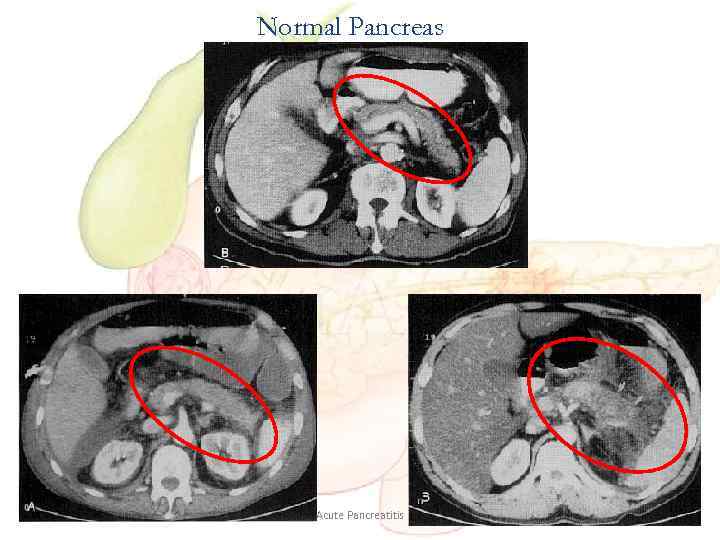 Normal Pancreas Acute Pancreatitis
Normal Pancreas Acute Pancreatitis
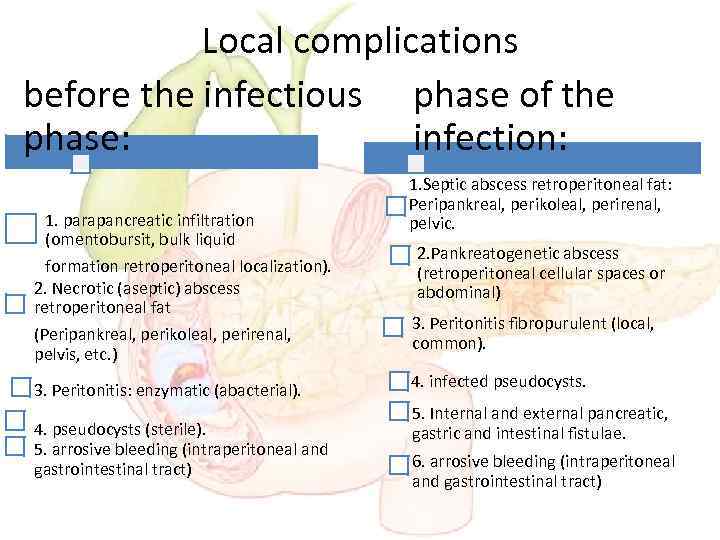 Local complications before the infectious phase of the phase: infection: 1. parapancreatic infiltration (omentobursit, bulk liquid formation retroperitoneal localization). 2. Necrotic (aseptic) abscess retroperitoneal fat (Peripankreal, perikoleal, perirenal, pelvis, etc. ) 3. Peritonitis: enzymatic (abacterial). 4. pseudocysts (sterile). 5. arrosive bleeding (intraperitoneal and gastrointestinal tract) 1. Septic abscess retroperitoneal fat: Peripankreal, perikoleal, perirenal, pelvic. 2. Pankreatogenetic abscess (retroperitoneal cellular spaces or abdominal) 3. Peritonitis fibropurulent (local, common). 4. infected pseudocysts. 5. Internal and external pancreatic, gastric and intestinal fistulae. 6. arrosive bleeding (intraperitoneal and gastrointestinal tract)
Local complications before the infectious phase of the phase: infection: 1. parapancreatic infiltration (omentobursit, bulk liquid formation retroperitoneal localization). 2. Necrotic (aseptic) abscess retroperitoneal fat (Peripankreal, perikoleal, perirenal, pelvis, etc. ) 3. Peritonitis: enzymatic (abacterial). 4. pseudocysts (sterile). 5. arrosive bleeding (intraperitoneal and gastrointestinal tract) 1. Septic abscess retroperitoneal fat: Peripankreal, perikoleal, perirenal, pelvic. 2. Pankreatogenetic abscess (retroperitoneal cellular spaces or abdominal) 3. Peritonitis fibropurulent (local, common). 4. infected pseudocysts. 5. Internal and external pancreatic, gastric and intestinal fistulae. 6. arrosive bleeding (intraperitoneal and gastrointestinal tract)
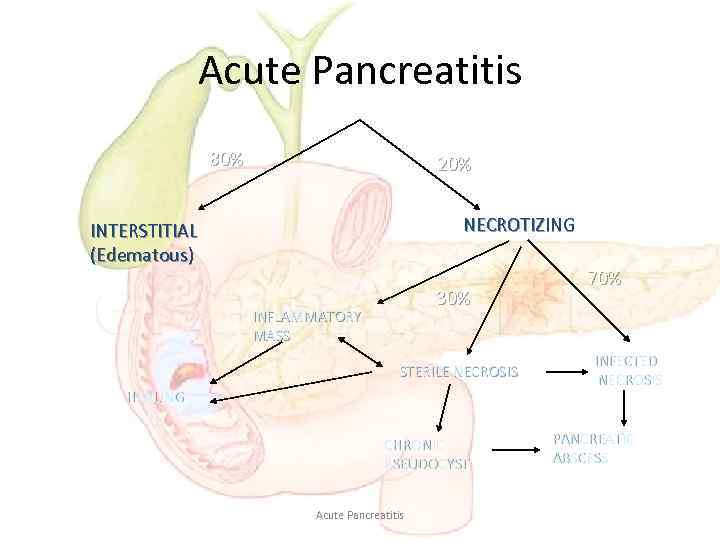 Acute Pancreatitis 80% 20% NECROTIZING INTERSTITIAL (Edematous) 30% INFLAMMATORY MASS STERILE NECROSIS HEALING CHRONIC PSEUDOCYST Acute Pancreatitis 70% INFECTED NECROSIS PANCREATIC ABSCESS
Acute Pancreatitis 80% 20% NECROTIZING INTERSTITIAL (Edematous) 30% INFLAMMATORY MASS STERILE NECROSIS HEALING CHRONIC PSEUDOCYST Acute Pancreatitis 70% INFECTED NECROSIS PANCREATIC ABSCESS
 Systemic complications 1. Pancreatogenic shock in sterile pancreatic necrosis and intra-abdominal complications. 2. Septic (infectious and toxic) shock when infected pancreatic necrosis and intraabdominal complications. 3. Multiple organ failure as in the sterile and infected necrotizing pancreatitis, and their complications.
Systemic complications 1. Pancreatogenic shock in sterile pancreatic necrosis and intra-abdominal complications. 2. Septic (infectious and toxic) shock when infected pancreatic necrosis and intraabdominal complications. 3. Multiple organ failure as in the sterile and infected necrotizing pancreatitis, and their complications.
 Clinical Presentation • Pain (95%) – Acute onset • Mid-abdominal or mid-epigastric • Radiates to the back (50%) – Peak intensity in 30 minutes • Lasts for several hours • Nausea and vomiting (80%) • Abdominal distension (75%) • Abdominal guarding and tenderness (50%) • Restlessness and agitation Acute Pancreatitis
Clinical Presentation • Pain (95%) – Acute onset • Mid-abdominal or mid-epigastric • Radiates to the back (50%) – Peak intensity in 30 minutes • Lasts for several hours • Nausea and vomiting (80%) • Abdominal distension (75%) • Abdominal guarding and tenderness (50%) • Restlessness and agitation Acute Pancreatitis
 Abdominal examination • Tenderness in epigastrium • Although severe pain, there may be little or no guarding of abdominal muscles at first. Later the upper abdomen becomes tender and rigid as peritoneal irritation increases. • Mild abdominal distention if paralytic ileus develops. • Severe advanced cases may develop bruising and discoloration in the left flank (Grey Turner’s sign due to tissue catabolism of Hb) and around the umbilicus (Cullen’s sign due to hemoperitoneum). These are the rare and late signs of extensive pancreatic destruction. abdominal examination
Abdominal examination • Tenderness in epigastrium • Although severe pain, there may be little or no guarding of abdominal muscles at first. Later the upper abdomen becomes tender and rigid as peritoneal irritation increases. • Mild abdominal distention if paralytic ileus develops. • Severe advanced cases may develop bruising and discoloration in the left flank (Grey Turner’s sign due to tissue catabolism of Hb) and around the umbilicus (Cullen’s sign due to hemoperitoneum). These are the rare and late signs of extensive pancreatic destruction. abdominal examination
 Cullen’s sign Grey Turner’s sign abdominal examination
Cullen’s sign Grey Turner’s sign abdominal examination
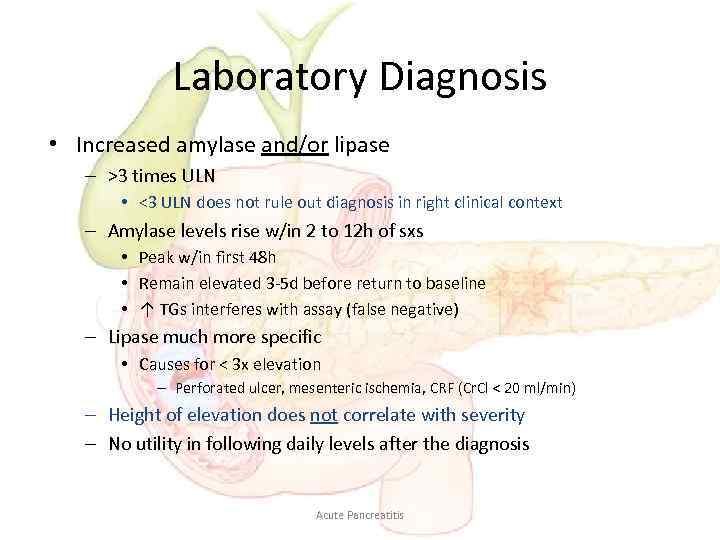 Laboratory Diagnosis • Increased amylase and/or lipase – >3 times ULN • <3 ULN does not rule out diagnosis in right clinical context – Amylase levels rise w/in 2 to 12 h of sxs • Peak w/in first 48 h • Remain elevated 3 -5 d before return to baseline • ↑ TGs interferes with assay (false negative) – Lipase much more specific • Causes for < 3 x elevation – Perforated ulcer, mesenteric ischemia, CRF (Cr. Cl < 20 ml/min) – Height of elevation does not correlate with severity – No utility in following daily levels after the diagnosis Acute Pancreatitis
Laboratory Diagnosis • Increased amylase and/or lipase – >3 times ULN • <3 ULN does not rule out diagnosis in right clinical context – Amylase levels rise w/in 2 to 12 h of sxs • Peak w/in first 48 h • Remain elevated 3 -5 d before return to baseline • ↑ TGs interferes with assay (false negative) – Lipase much more specific • Causes for < 3 x elevation – Perforated ulcer, mesenteric ischemia, CRF (Cr. Cl < 20 ml/min) – Height of elevation does not correlate with severity – No utility in following daily levels after the diagnosis Acute Pancreatitis
 Lab studies • Other causes for amylase – – – • Calcium SBO mesenteric ischemia tubo-ovarian disease renal insufficiency macroamylasemia brain injury/brain trauma – Ca as a cause – Ca as a complication • saponification of fats in retroperitoneum • TG • LTFs – ALT > 3 x ULN = 95% PPV for biliary etiology Acute Pancreatitis – Can be falsely low during an attack
Lab studies • Other causes for amylase – – – • Calcium SBO mesenteric ischemia tubo-ovarian disease renal insufficiency macroamylasemia brain injury/brain trauma – Ca as a cause – Ca as a complication • saponification of fats in retroperitoneum • TG • LTFs – ALT > 3 x ULN = 95% PPV for biliary etiology Acute Pancreatitis – Can be falsely low during an attack
 Plain Abdominal Radiograph
Plain Abdominal Radiograph
 Plain Abdominal Radiograph • • Bowel ileus “Sentinel Loop” “Colon cut off sign” Loss of psoas shadow • Helps exclude other causes of abdominal pain: bowel obstruction and perforation
Plain Abdominal Radiograph • • Bowel ileus “Sentinel Loop” “Colon cut off sign” Loss of psoas shadow • Helps exclude other causes of abdominal pain: bowel obstruction and perforation
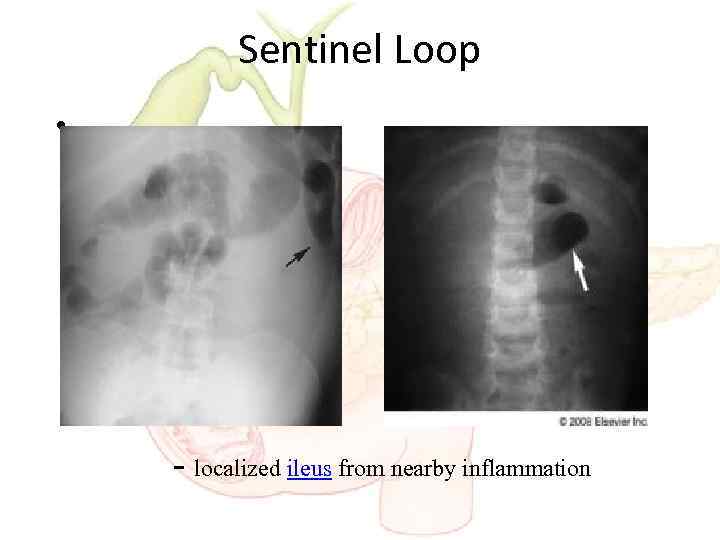 Sentinel Loop • - localized ileus from nearby inflammation
Sentinel Loop • - localized ileus from nearby inflammation
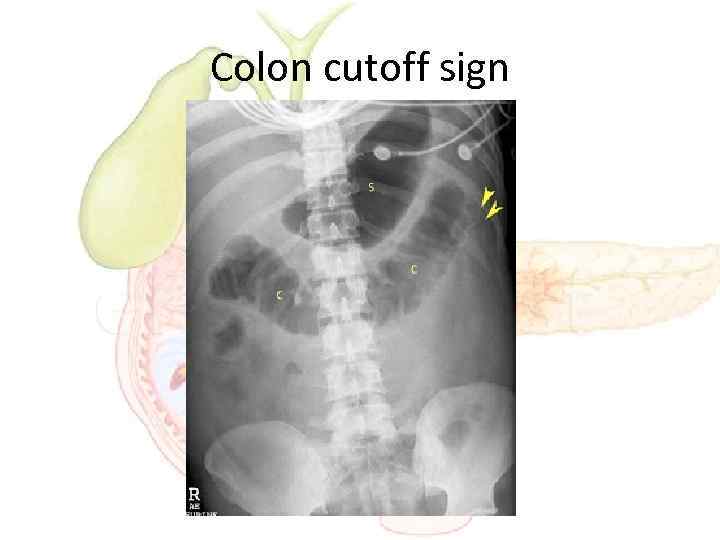 Colon cutoff sign
Colon cutoff sign
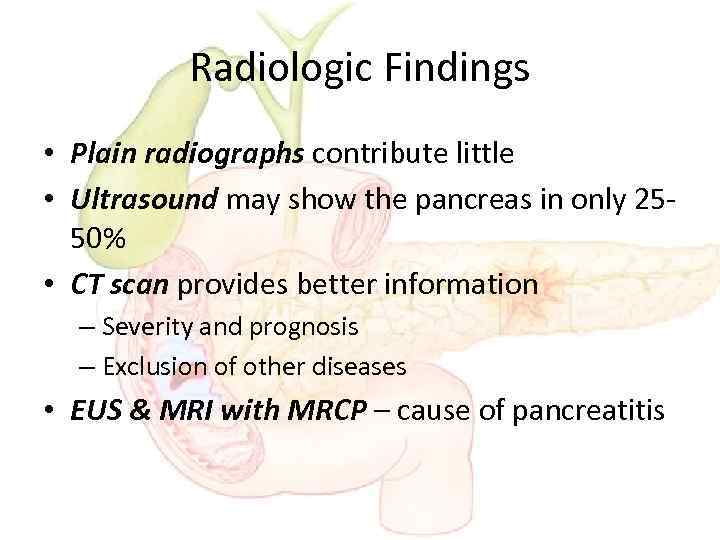 Radiologic Findings • Plain radiographs contribute little • Ultrasound may show the pancreas in only 2550% • CT scan provides better information – Severity and prognosis – Exclusion of other diseases • EUS & MRI with MRCP – cause of pancreatitis
Radiologic Findings • Plain radiographs contribute little • Ultrasound may show the pancreas in only 2550% • CT scan provides better information – Severity and prognosis – Exclusion of other diseases • EUS & MRI with MRCP – cause of pancreatitis
 Assessment of severity
Assessment of severity
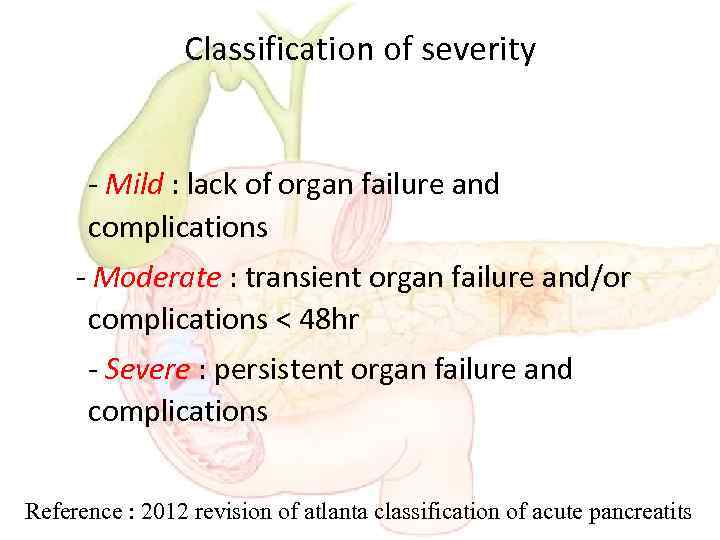 Classification of severity - Mild : lack of organ failure and complications - Moderate : transient organ failure and/or complications < 48 hr - Severe : persistent organ failure and complications Reference : 2012 revision of atlanta classification of acute pancreatits
Classification of severity - Mild : lack of organ failure and complications - Moderate : transient organ failure and/or complications < 48 hr - Severe : persistent organ failure and complications Reference : 2012 revision of atlanta classification of acute pancreatits
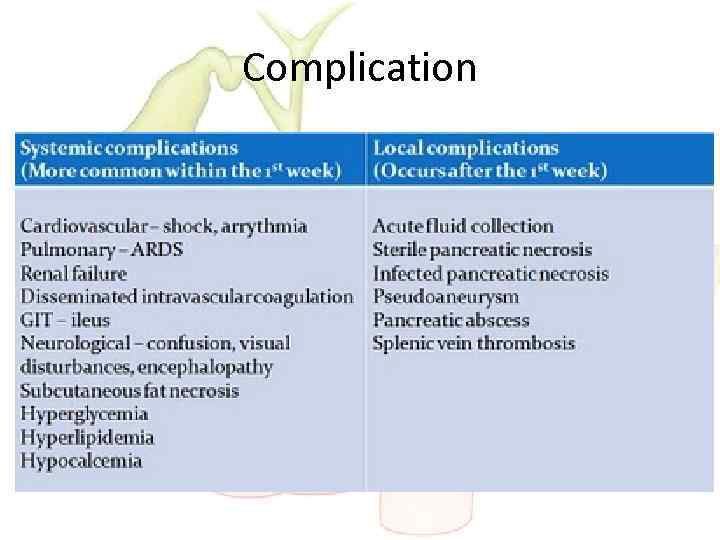 Complication
Complication
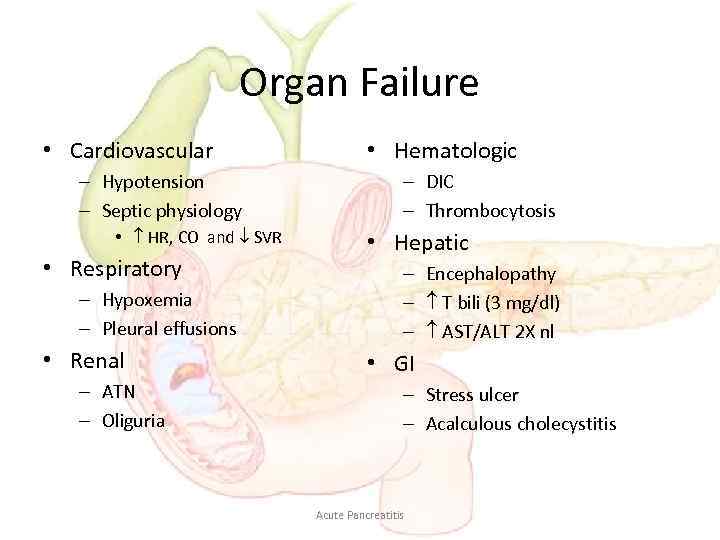 Organ Failure • Cardiovascular – Hypotension – Septic physiology • HR, CO and SVR • Respiratory – Hypoxemia – Pleural effusions • Renal – ATN – Oliguria • Hematologic – DIC – Thrombocytosis • Hepatic – Encephalopathy – T bili (3 mg/dl) – AST/ALT 2 X nl • GI – Stress ulcer – Acalculous cholecystitis Acute Pancreatitis
Organ Failure • Cardiovascular – Hypotension – Septic physiology • HR, CO and SVR • Respiratory – Hypoxemia – Pleural effusions • Renal – ATN – Oliguria • Hematologic – DIC – Thrombocytosis • Hepatic – Encephalopathy – T bili (3 mg/dl) – AST/ALT 2 X nl • GI – Stress ulcer – Acalculous cholecystitis Acute Pancreatitis
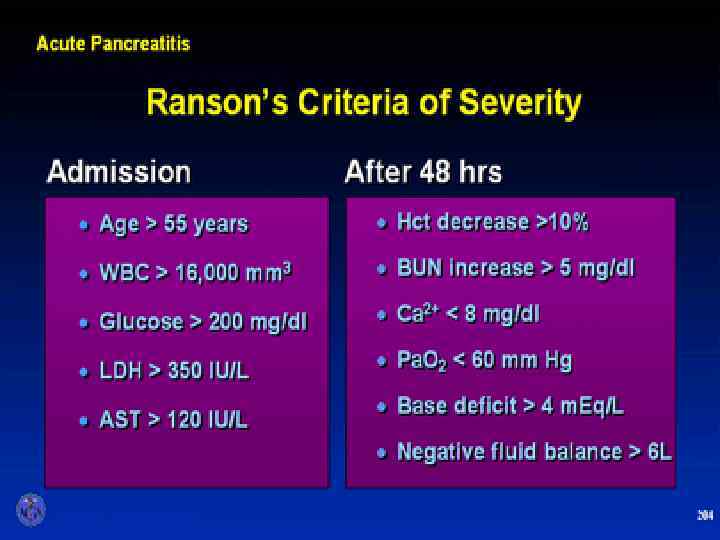
 Early prognostic sign • Ranson’s score • APACHE II
Early prognostic sign • Ranson’s score • APACHE II
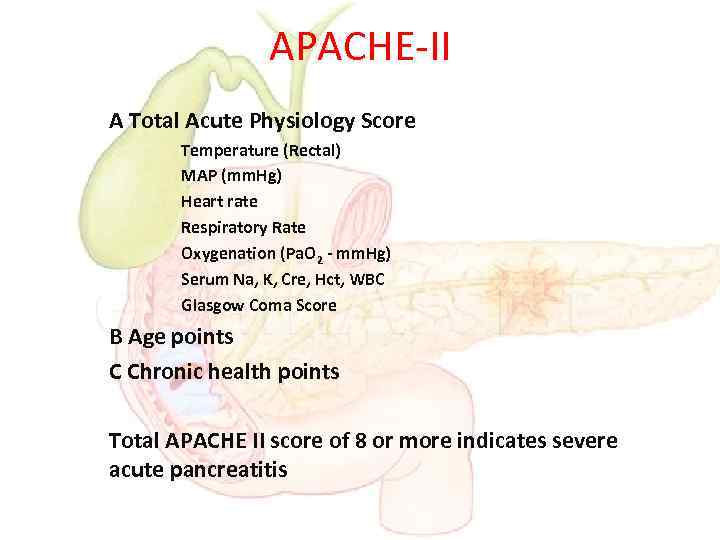 APACHE-II A Total Acute Physiology Score Temperature (Rectal) MAP (mm. Hg) Heart rate Respiratory Rate Oxygenation (Pa. O 2 - mm. Hg) Serum Na, K, Cre, Hct, WBC Glasgow Coma Score B Age points C Chronic health points Total APACHE II score of 8 or more indicates severe acute pancreatitis
APACHE-II A Total Acute Physiology Score Temperature (Rectal) MAP (mm. Hg) Heart rate Respiratory Rate Oxygenation (Pa. O 2 - mm. Hg) Serum Na, K, Cre, Hct, WBC Glasgow Coma Score B Age points C Chronic health points Total APACHE II score of 8 or more indicates severe acute pancreatitis
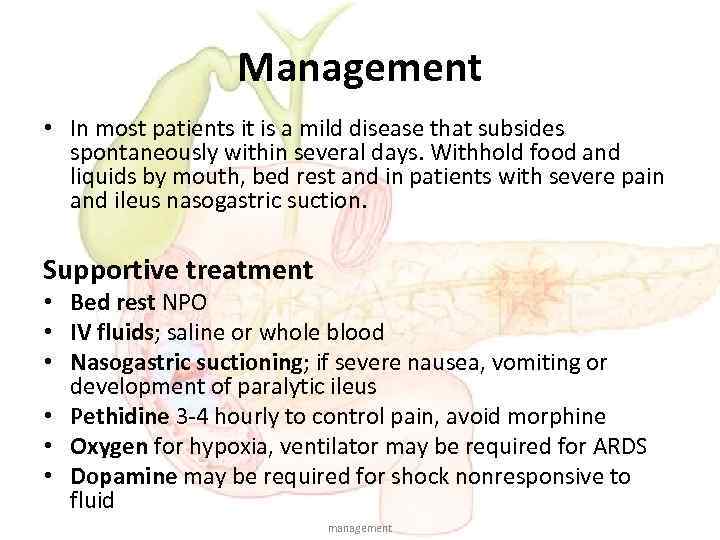 Management • In most patients it is a mild disease that subsides spontaneously within several days. Withhold food and liquids by mouth, bed rest and in patients with severe pain and ileus nasogastric suction. Supportive treatment • Bed rest NPO • IV fluids; saline or whole blood • Nasogastric suctioning; if severe nausea, vomiting or development of paralytic ileus • Pethidine 3 -4 hourly to control pain, avoid morphine • Oxygen for hypoxia, ventilator may be required for ARDS • Dopamine may be required for shock nonresponsive to fluid management
Management • In most patients it is a mild disease that subsides spontaneously within several days. Withhold food and liquids by mouth, bed rest and in patients with severe pain and ileus nasogastric suction. Supportive treatment • Bed rest NPO • IV fluids; saline or whole blood • Nasogastric suctioning; if severe nausea, vomiting or development of paralytic ileus • Pethidine 3 -4 hourly to control pain, avoid morphine • Oxygen for hypoxia, ventilator may be required for ARDS • Dopamine may be required for shock nonresponsive to fluid management
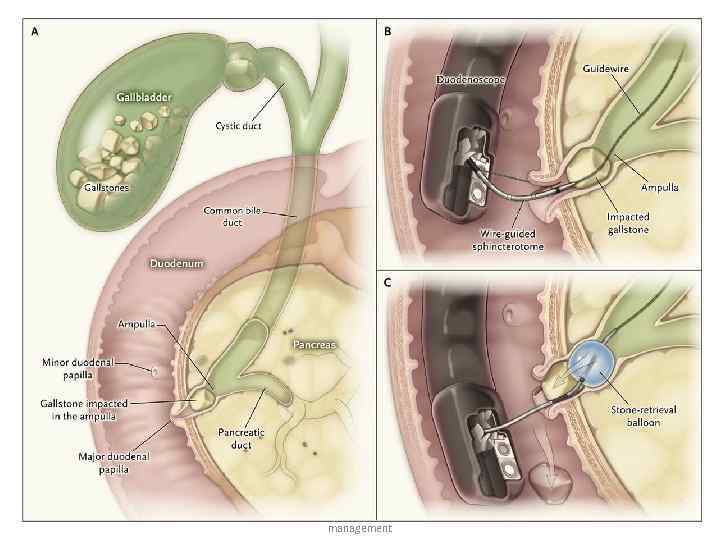
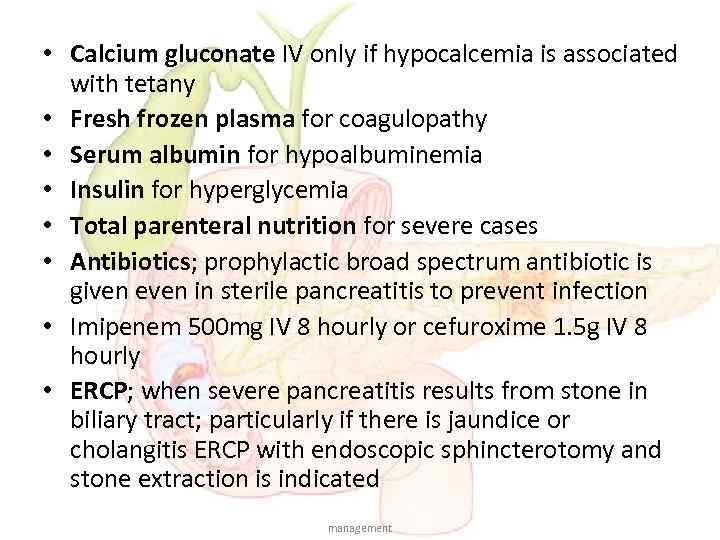 • Calcium gluconate IV only if hypocalcemia is associated with tetany • Fresh frozen plasma for coagulopathy • Serum albumin for hypoalbuminemia • Insulin for hyperglycemia • Total parenteral nutrition for severe cases • Antibiotics; prophylactic broad spectrum antibiotic is given even in sterile pancreatitis to prevent infection • Imipenem 500 mg IV 8 hourly or cefuroxime 1. 5 g IV 8 hourly • ERCP; when severe pancreatitis results from stone in biliary tract; particularly if there is jaundice or cholangitis ERCP with endoscopic sphincterotomy and stone extraction is indicated management
• Calcium gluconate IV only if hypocalcemia is associated with tetany • Fresh frozen plasma for coagulopathy • Serum albumin for hypoalbuminemia • Insulin for hyperglycemia • Total parenteral nutrition for severe cases • Antibiotics; prophylactic broad spectrum antibiotic is given even in sterile pancreatitis to prevent infection • Imipenem 500 mg IV 8 hourly or cefuroxime 1. 5 g IV 8 hourly • ERCP; when severe pancreatitis results from stone in biliary tract; particularly if there is jaundice or cholangitis ERCP with endoscopic sphincterotomy and stone extraction is indicated management
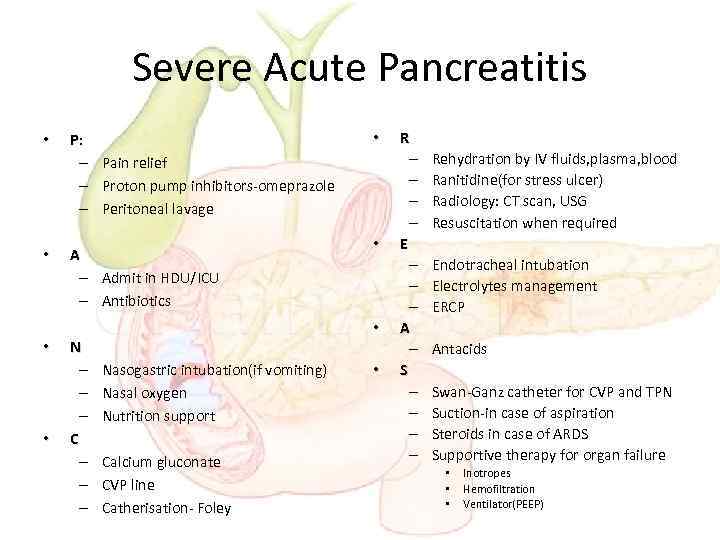 Severe Acute Pancreatitis • • P: – Pain relief – Proton pump inhibitors-omeprazole – Peritoneal lavage A – Admit in HDU/ICU – Antibiotics N – – – C – – – • • • Nasogastric intubation(if vomiting) Nasal oxygen Nutrition support Calcium gluconate CVP line Catherisation- Foley • R – – E – – – A – S – – Rehydration by IV fluids, plasma, blood Ranitidine(for stress ulcer) Radiology: CT scan, USG Resuscitation when required Endotracheal intubation Electrolytes management ERCP Antacids Swan-Ganz catheter for CVP and TPN Suction-in case of aspiration Steroids in case of ARDS Supportive therapy for organ failure • • • Inotropes Hemofiltration Ventilator(PEEP)
Severe Acute Pancreatitis • • P: – Pain relief – Proton pump inhibitors-omeprazole – Peritoneal lavage A – Admit in HDU/ICU – Antibiotics N – – – C – – – • • • Nasogastric intubation(if vomiting) Nasal oxygen Nutrition support Calcium gluconate CVP line Catherisation- Foley • R – – E – – – A – S – – Rehydration by IV fluids, plasma, blood Ranitidine(for stress ulcer) Radiology: CT scan, USG Resuscitation when required Endotracheal intubation Electrolytes management ERCP Antacids Swan-Ganz catheter for CVP and TPN Suction-in case of aspiration Steroids in case of ARDS Supportive therapy for organ failure • • • Inotropes Hemofiltration Ventilator(PEEP)
 management
management
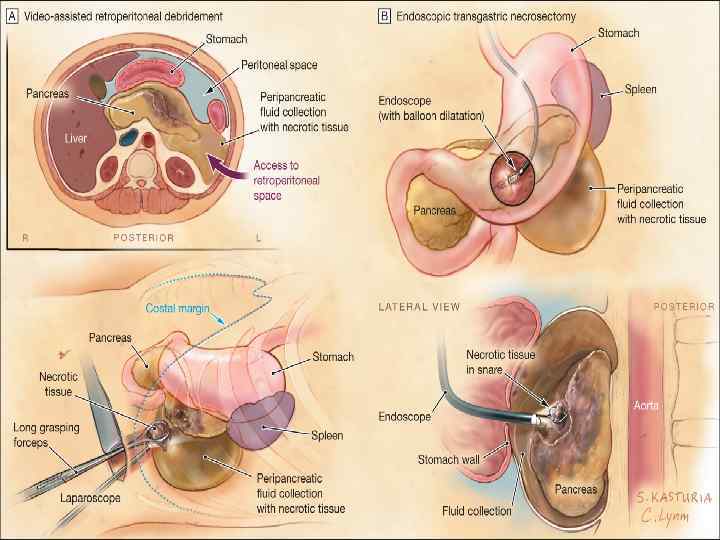
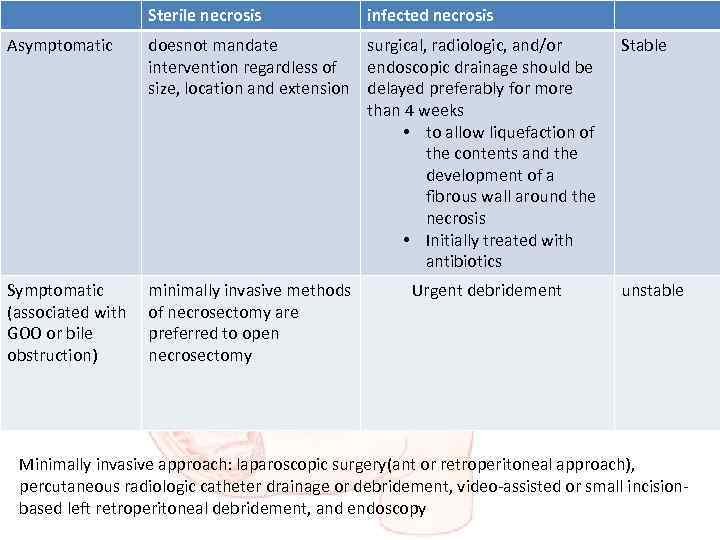 Sterile necrosis Asymptomatic infected necrosis doesnot mandate surgical, radiologic, and/or intervention regardless of endoscopic drainage should be size, location and extension delayed preferably for more than 4 weeks • to allow liquefaction of the contents and the development of a fibrous wall around the necrosis • Initially treated with antibiotics Stable minimally invasive methods of necrosectomy are preferred to open necrosectomy unstable Symptomatic (associated with GOO or bile obstruction) Urgent debridement Minimally invasive approach: laparoscopic surgery(ant or retroperitoneal approach), percutaneous radiologic catheter drainage or debridement, video-assisted or small incisionbased left retroperitoneal debridement, and endoscopy
Sterile necrosis Asymptomatic infected necrosis doesnot mandate surgical, radiologic, and/or intervention regardless of endoscopic drainage should be size, location and extension delayed preferably for more than 4 weeks • to allow liquefaction of the contents and the development of a fibrous wall around the necrosis • Initially treated with antibiotics Stable minimally invasive methods of necrosectomy are preferred to open necrosectomy unstable Symptomatic (associated with GOO or bile obstruction) Urgent debridement Minimally invasive approach: laparoscopic surgery(ant or retroperitoneal approach), percutaneous radiologic catheter drainage or debridement, video-assisted or small incisionbased left retroperitoneal debridement, and endoscopy
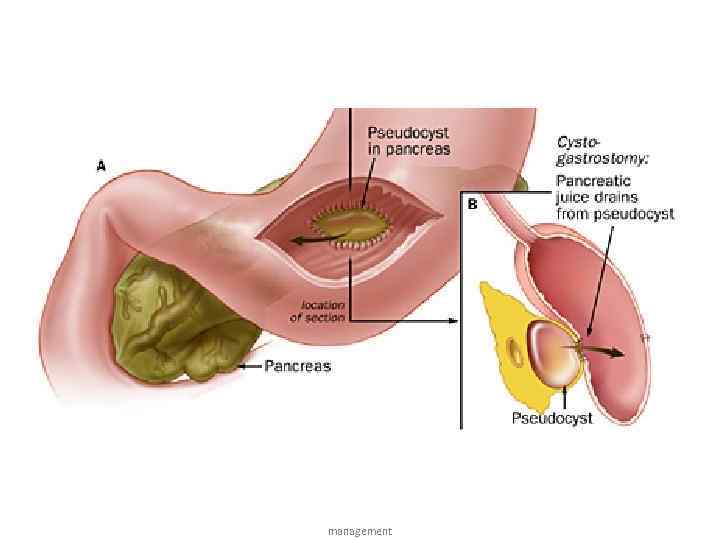 management
management
 References • Davidson’s principles and practice of medicine 22 nd edition • Short textbook of medical diagnosis and management 11 th international edition (Inam Danish) • Kaplan medical USMLE step 2 CK internal medicine lecture notes references
References • Davidson’s principles and practice of medicine 22 nd edition • Short textbook of medical diagnosis and management 11 th international edition (Inam Danish) • Kaplan medical USMLE step 2 CK internal medicine lecture notes references
 Thank you
Thank you


