213e60a2c6d9b999ce8e8f882c3a1d79.ppt
- Количество слайдов: 26
 Acute ischemic stroke: Not a moment to lose By Julie Miller, RN, CCRN, BSN, & Janice Mink, RN, CCRN, CNRN Nursing 2009, May 2009 2. 1 ANCC contact hours Online: www. nursingcenter. com © 2009 by Lippincott Williams & Wilkins. All world rights reserved.
Acute ischemic stroke: Not a moment to lose By Julie Miller, RN, CCRN, BSN, & Janice Mink, RN, CCRN, CNRN Nursing 2009, May 2009 2. 1 ANCC contact hours Online: www. nursingcenter. com © 2009 by Lippincott Williams & Wilkins. All world rights reserved.
 Stroke l 87% are ischemic, resulting from impaired blood flow to a localized area of the brain l Impaired circulation due to thrombosis, atherogenic plaque, or embolism l 13% of strokes are from hemorrhage, rupture of a blood vessel (intracerebral or subarachnoid)
Stroke l 87% are ischemic, resulting from impaired blood flow to a localized area of the brain l Impaired circulation due to thrombosis, atherogenic plaque, or embolism l 13% of strokes are from hemorrhage, rupture of a blood vessel (intracerebral or subarachnoid)
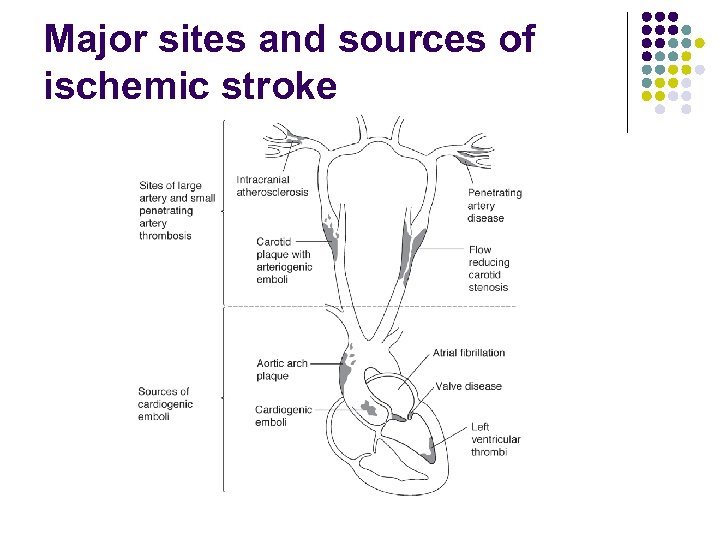 Major sites and sources of ischemic stroke
Major sites and sources of ischemic stroke
 Improving response improves outcomes l In 1996, original AHA guidelines for use of rt. PA, a fibrinolytic agent, were approved to treat acute ischemic stroke l Since then, transport, community awareness of acute stroke signs and symptoms, and treatment have improved immensely
Improving response improves outcomes l In 1996, original AHA guidelines for use of rt. PA, a fibrinolytic agent, were approved to treat acute ischemic stroke l Since then, transport, community awareness of acute stroke signs and symptoms, and treatment have improved immensely
 Improving response improves outcomes l Research shows that most stroke patients now arrive at hospitals within 3 hours of symptom onset; more than half of these patients are transported via emergency medical transport l Treating acute ischemic stroke with I. V. rt. PA within 3 hours of stroke onset dramatically reduces deaths and disabilities
Improving response improves outcomes l Research shows that most stroke patients now arrive at hospitals within 3 hours of symptom onset; more than half of these patients are transported via emergency medical transport l Treating acute ischemic stroke with I. V. rt. PA within 3 hours of stroke onset dramatically reduces deaths and disabilities
 Improving response improves outcomes l Recent advances in intra-arterial fibrinolysis and endovascular clot retrieval devices allow for effective intervention in some acute ischemic stroke patients who arrive up to 8 hours after onset of symptoms
Improving response improves outcomes l Recent advances in intra-arterial fibrinolysis and endovascular clot retrieval devices allow for effective intervention in some acute ischemic stroke patients who arrive up to 8 hours after onset of symptoms
 Evaluating the patient using the seven D’s 1. Detection: early recognition of signs and symptoms onset, includes public education 2. Dispatch: EMS activation and rapid intervention 3. Delivery: advanced prehospital notification and transport to nearest acute stroke care facility
Evaluating the patient using the seven D’s 1. Detection: early recognition of signs and symptoms onset, includes public education 2. Dispatch: EMS activation and rapid intervention 3. Delivery: advanced prehospital notification and transport to nearest acute stroke care facility
 Evaluating the patient using the seven D’s 4. Door: rapid triage in ED, giving stroke signs and symptoms high priority 5. Data: history, neurologic assessment, diagnostic testing to include CT or MRI done within 25 minutes and read within 45 minutes
Evaluating the patient using the seven D’s 4. Door: rapid triage in ED, giving stroke signs and symptoms high priority 5. Data: history, neurologic assessment, diagnostic testing to include CT or MRI done within 25 minutes and read within 45 minutes
 Evaluating the patient using the seven D’s 6. Decision: evaluation of inclusion and exclusion criteria for rt. PA 7. Drug: initiation of weight-based rt. PA within 3 hours of symptom onset - patient meets all inclusion criteria - has no exclusion criteria
Evaluating the patient using the seven D’s 6. Decision: evaluation of inclusion and exclusion criteria for rt. PA 7. Drug: initiation of weight-based rt. PA within 3 hours of symptom onset - patient meets all inclusion criteria - has no exclusion criteria
 AHA algorithm for suspected stroke In first 10 minutes after arrival: l Alert stroke team l Assess patient’s ABCs and vital signs l Establish or confirm venous access l Treat abnormal glucose levels l Obtain blood specimens for baseline l Ensure CT order communicated to radiology to be done upon patient’s arrival l Obtain 12 -lead ECG
AHA algorithm for suspected stroke In first 10 minutes after arrival: l Alert stroke team l Assess patient’s ABCs and vital signs l Establish or confirm venous access l Treat abnormal glucose levels l Obtain blood specimens for baseline l Ensure CT order communicated to radiology to be done upon patient’s arrival l Obtain 12 -lead ECG
 AHA algorithm for suspected stroke Within 25 minutes of arrival: l Establish or confirm stroke symptom onset l Perform neurologic exam using NIHSS l Ensure CT or MRI has been started
AHA algorithm for suspected stroke Within 25 minutes of arrival: l Establish or confirm stroke symptom onset l Perform neurologic exam using NIHSS l Ensure CT or MRI has been started
 Using a stroke assessment tool l National Institutes of Health Stroke Scale (NIHSS) offers tools for patients with language and motor difficulties l Administer NIHSS in this order: - level of consciousness - gaze - visual fields - facial movement
Using a stroke assessment tool l National Institutes of Health Stroke Scale (NIHSS) offers tools for patients with language and motor difficulties l Administer NIHSS in this order: - level of consciousness - gaze - visual fields - facial movement
 Using a stroke assessment tool - motor function of arms and legs - limb ataxia - sensory responses - language - articulation - extinction and inattention l Score greater than 22: patient has high risk of hemorrhage, requiring caution to use rt. PA
Using a stroke assessment tool - motor function of arms and legs - limb ataxia - sensory responses - language - articulation - extinction and inattention l Score greater than 22: patient has high risk of hemorrhage, requiring caution to use rt. PA
 Using a stroke assessment tool l Recommendation is to administer NIHSS every 12 hours for first 24 hours, then every 24 hours until discharge. Check facility’s stroke protocol for time frames l NIHSS must be administered the same way each time it’s performed, so all NIHSS evaluators should undergo same training to ensure accuracy, reliability, validity
Using a stroke assessment tool l Recommendation is to administer NIHSS every 12 hours for first 24 hours, then every 24 hours until discharge. Check facility’s stroke protocol for time frames l NIHSS must be administered the same way each time it’s performed, so all NIHSS evaluators should undergo same training to ensure accuracy, reliability, validity
 Inclusion criteria that must be met for rt. PA administration l 18 years of age or older l Clinical diagnosis of acute ischemic stroke with measurable neurologic deficit l Time of symptom onset less than 180 minutes (3 hours) before fibrinolytic therapy would begin
Inclusion criteria that must be met for rt. PA administration l 18 years of age or older l Clinical diagnosis of acute ischemic stroke with measurable neurologic deficit l Time of symptom onset less than 180 minutes (3 hours) before fibrinolytic therapy would begin
 Exclusion criteria for rt. PA l History or evidence of intracranial hemorrhage l Multilobar infarction on CT scan l Signs of subarachnoid hemorrhage
Exclusion criteria for rt. PA l History or evidence of intracranial hemorrhage l Multilobar infarction on CT scan l Signs of subarachnoid hemorrhage
 Exclusion criteria for rt. PA l Known arteriovenous malformation, neoplasm or aneurysm l Systolic BP >185 mm. Hg or diastolic >110 mm. Hg despite repeated measurements and treatment
Exclusion criteria for rt. PA l Known arteriovenous malformation, neoplasm or aneurysm l Systolic BP >185 mm. Hg or diastolic >110 mm. Hg despite repeated measurements and treatment
 Exclusion criteria for rt. PA l Acute bleeding tendencies: - platelet count <100, 00/mm 3 - prothrombin time (PT) >15 seconds - international normalized ratio (INR) >1. 7 - activated partial thromboplastin time (a. PTT) > upper normal limit l Active internal bleeding or acute trauma
Exclusion criteria for rt. PA l Acute bleeding tendencies: - platelet count <100, 00/mm 3 - prothrombin time (PT) >15 seconds - international normalized ratio (INR) >1. 7 - activated partial thromboplastin time (a. PTT) > upper normal limit l Active internal bleeding or acute trauma
 Exclusion criteria for rt. PA l Serious head trauma, stroke, or surgery in past 3 months l Arterial puncture at noncompressible site in last week l Postmyocardial infarction pericarditis l Minor or rapidly improving stroke symptoms
Exclusion criteria for rt. PA l Serious head trauma, stroke, or surgery in past 3 months l Arterial puncture at noncompressible site in last week l Postmyocardial infarction pericarditis l Minor or rapidly improving stroke symptoms
 Exclusion criteria for rt. PA l Abnormal blood glucose (<50 or >400 mg/d. L) l Major surgery or serious trauma within 14 days l Recent acute MI (within 3 months) l Recent GI or urinary tract hemorrhage
Exclusion criteria for rt. PA l Abnormal blood glucose (<50 or >400 mg/d. L) l Major surgery or serious trauma within 14 days l Recent acute MI (within 3 months) l Recent GI or urinary tract hemorrhage
 Administering rt. PA l Weight-based l Monitor patient’s neurologic status and BP l Risk of hemorrhage is higher if BP >180/105 l Lower BP conservatively; 15 to 25% first day
Administering rt. PA l Weight-based l Monitor patient’s neurologic status and BP l Risk of hemorrhage is higher if BP >180/105 l Lower BP conservatively; 15 to 25% first day
 Administering rt. PA l Sodium nitroprusside is only drug recommended for treating BP not controlled by labetalol or nicardipine l Assess for signs of internal bleeding l Following rt. PA administration, admit patient to ICU or stroke unit for close monitoring
Administering rt. PA l Sodium nitroprusside is only drug recommended for treating BP not controlled by labetalol or nicardipine l Assess for signs of internal bleeding l Following rt. PA administration, admit patient to ICU or stroke unit for close monitoring
 How stroke centers compare l Brain Attack Coalition published recommendations in 2000 advocating for implementation of primary stroke centers and comprehensive stroke centers l Primary stroke centers have essential components to manage uncomplicated strokes: expert personnel, protocols, infrastructure, capacity to admit patients into a stroke unit
How stroke centers compare l Brain Attack Coalition published recommendations in 2000 advocating for implementation of primary stroke centers and comprehensive stroke centers l Primary stroke centers have essential components to manage uncomplicated strokes: expert personnel, protocols, infrastructure, capacity to admit patients into a stroke unit
 How stroke centers compare l Early evidence shows patients with acute ischemic stroke treated at a primary stroke center are more likely to receive fibrinolytic agents l Comprehensive stroke centers fulfill requirements for primary stroke centers, provide diagnostic services (MRI, interventional neuroradiology) for endovascular treatments
How stroke centers compare l Early evidence shows patients with acute ischemic stroke treated at a primary stroke center are more likely to receive fibrinolytic agents l Comprehensive stroke centers fulfill requirements for primary stroke centers, provide diagnostic services (MRI, interventional neuroradiology) for endovascular treatments
 How stroke centers compare l Guidelines recommend transporting a patient suspected of having a stroke to closest, most appropriate facility; EMS should bypass facilities that don’t have resources or institutional commitment to treat a patient with stroke if a facility with proper resources is reasonably close
How stroke centers compare l Guidelines recommend transporting a patient suspected of having a stroke to closest, most appropriate facility; EMS should bypass facilities that don’t have resources or institutional commitment to treat a patient with stroke if a facility with proper resources is reasonably close
 Other treatment options l Catheter-directed intra-arterial fibrinolysis for patients past 3 -hour window - inclusion criteria are same - exclusion criteria vary based on clinical trials and facility protocols - can be administered up to 6 hours after stroke - currently no fibrinolytic has FDA approval
Other treatment options l Catheter-directed intra-arterial fibrinolysis for patients past 3 -hour window - inclusion criteria are same - exclusion criteria vary based on clinical trials and facility protocols - can be administered up to 6 hours after stroke - currently no fibrinolytic has FDA approval


