85a4200a0211edddb3f22faed071163d.ppt
- Количество слайдов: 68
 Acute Decompensated Heart Failure for Generalists Eric M. Siegal, M. D. University of Wisconsin, Madison
Acute Decompensated Heart Failure for Generalists Eric M. Siegal, M. D. University of Wisconsin, Madison
 Overview n n Evolving definitions Epidemiology of ADHF Goals of acute management Evolving management paradigms: u Acute vasoactive therapy u Prevention of SCD u Biventricular pacing u Beta-blockers in the hospital u How “dry” is “dry”?
Overview n n Evolving definitions Epidemiology of ADHF Goals of acute management Evolving management paradigms: u Acute vasoactive therapy u Prevention of SCD u Biventricular pacing u Beta-blockers in the hospital u How “dry” is “dry”?
 Why “ADHF”? n n n Growing recognition that “CHF” does not adequately describe a broad spectrum of disease with multiple causes, presentations and clinical courses. Describe acuity, severity and underlying pathophysiology: u “ADHF with severe systolic dysfunction due to ischemic cardiomyopathy and mitral regurgitation” u “Compensated NYHA Class II HF with moderate diastolic dysfunction due to hypertension and diabetes” Where possible, treatment is tailored to the definition
Why “ADHF”? n n n Growing recognition that “CHF” does not adequately describe a broad spectrum of disease with multiple causes, presentations and clinical courses. Describe acuity, severity and underlying pathophysiology: u “ADHF with severe systolic dysfunction due to ischemic cardiomyopathy and mitral regurgitation” u “Compensated NYHA Class II HF with moderate diastolic dysfunction due to hypertension and diabetes” Where possible, treatment is tailored to the definition
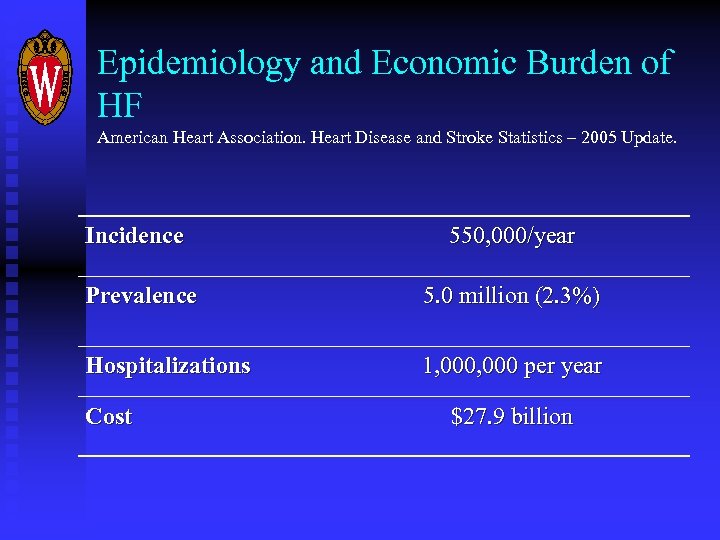 Epidemiology and Economic Burden of HF American Heart Association. Heart Disease and Stroke Statistics – 2005 Update. Incidence 550, 000/year Prevalence 5. 0 million (2. 3%) Hospitalizations 1, 000 per year Cost $27. 9 billion
Epidemiology and Economic Burden of HF American Heart Association. Heart Disease and Stroke Statistics – 2005 Update. Incidence 550, 000/year Prevalence 5. 0 million (2. 3%) Hospitalizations 1, 000 per year Cost $27. 9 billion
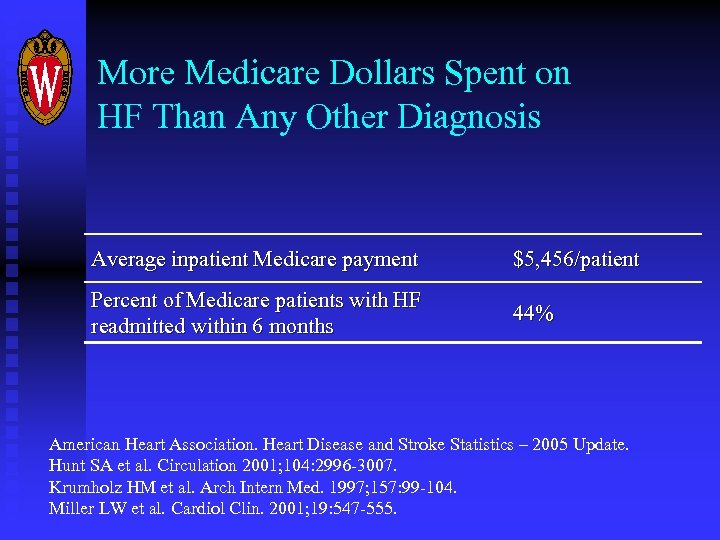 More Medicare Dollars Spent on HF Than Any Other Diagnosis Average inpatient Medicare payment $5, 456/patient Percent of Medicare patients with HF readmitted within 6 months 44% American Heart Association. Heart Disease and Stroke Statistics – 2005 Update. Hunt SA et al. Circulation 2001; 104: 2996 -3007. Krumholz HM et al. Arch Intern Med. 1997; 157: 99 -104. Miller LW et al. Cardiol Clin. 2001; 19: 547 -555.
More Medicare Dollars Spent on HF Than Any Other Diagnosis Average inpatient Medicare payment $5, 456/patient Percent of Medicare patients with HF readmitted within 6 months 44% American Heart Association. Heart Disease and Stroke Statistics – 2005 Update. Hunt SA et al. Circulation 2001; 104: 2996 -3007. Krumholz HM et al. Arch Intern Med. 1997; 157: 99 -104. Miller LW et al. Cardiol Clin. 2001; 19: 547 -555.
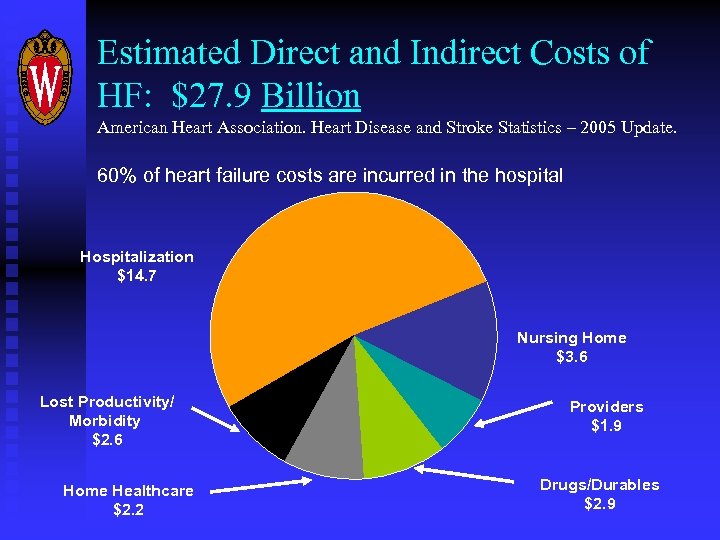 Estimated Direct and Indirect Costs of HF: $27. 9 Billion American Heart Association. Heart Disease and Stroke Statistics – 2005 Update. 60% of heart failure costs are incurred in the hospital Hospitalization $14. 7 Nursing Home $3. 6 Lost Productivity/ Morbidity $2. 6 Home Healthcare $2. 2 Providers $1. 9 Drugs/Durables $2. 9
Estimated Direct and Indirect Costs of HF: $27. 9 Billion American Heart Association. Heart Disease and Stroke Statistics – 2005 Update. 60% of heart failure costs are incurred in the hospital Hospitalization $14. 7 Nursing Home $3. 6 Lost Productivity/ Morbidity $2. 6 Home Healthcare $2. 2 Providers $1. 9 Drugs/Durables $2. 9
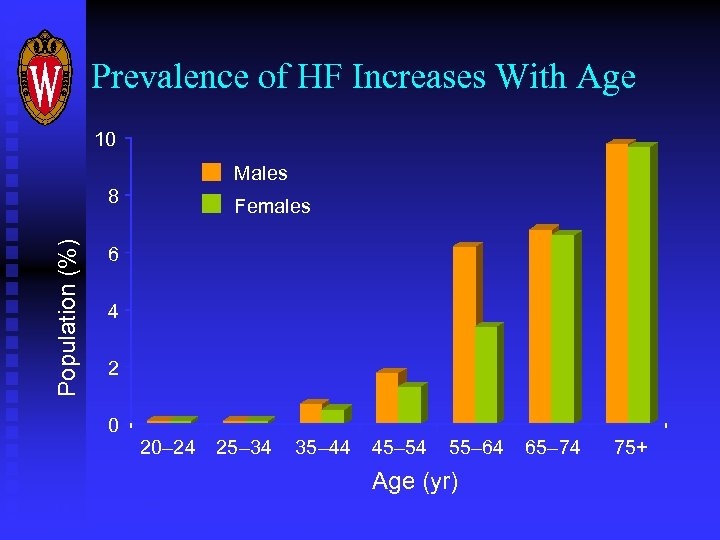 Prevalence of HF Increases With Age 10 Males Population (%) 8 Females 6 4 2 0 20– 24 25– 34 35– 44 45– 54 55– 64 Age (yr) US, 1988– 1994 AHA. Heart Disease and Stroke Statistics— 2004 Update 65– 74 75+
Prevalence of HF Increases With Age 10 Males Population (%) 8 Females 6 4 2 0 20– 24 25– 34 35– 44 45– 54 55– 64 Age (yr) US, 1988– 1994 AHA. Heart Disease and Stroke Statistics— 2004 Update 65– 74 75+
 Explosive Increase in HF AHA. Heart Disease and Stroke Statistics – 2005 Update n 1979 – 2002: Hospital discharges from HF rose from 377, 000 to 970, 000 per year n 1992 – 2002: Deaths increased 35. 3% n Number of patients with HF is expected to double in 30 years
Explosive Increase in HF AHA. Heart Disease and Stroke Statistics – 2005 Update n 1979 – 2002: Hospital discharges from HF rose from 377, 000 to 970, 000 per year n 1992 – 2002: Deaths increased 35. 3% n Number of patients with HF is expected to double in 30 years
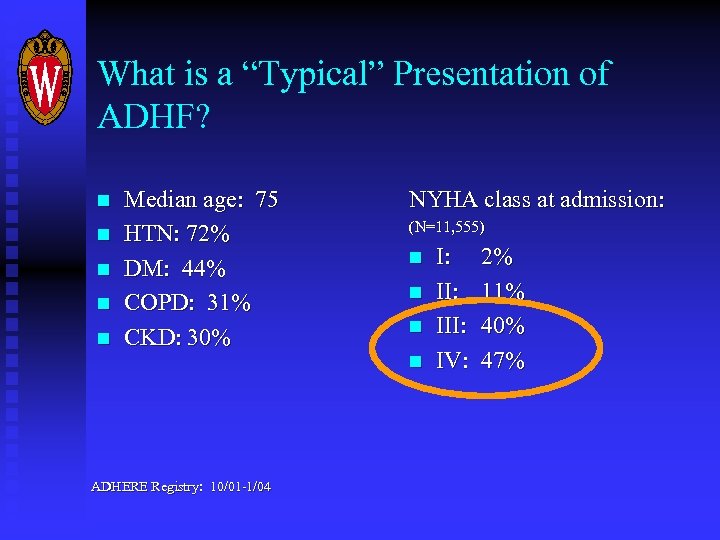 What is a “Typical” Presentation of ADHF? n n n Median age: 75 HTN: 72% DM: 44% COPD: 31% CKD: 30% NYHA class at admission: (N=11, 555) n n ADHERE Registry: 10/01 -1/04 I: III: IV: 2% 11% 40% 47%
What is a “Typical” Presentation of ADHF? n n n Median age: 75 HTN: 72% DM: 44% COPD: 31% CKD: 30% NYHA class at admission: (N=11, 555) n n ADHERE Registry: 10/01 -1/04 I: III: IV: 2% 11% 40% 47%
 What is a “Typical” Presentation of ADHF? Blood Pressure at admission (N=104, 573) n n n <90 mm. Hg: 2% 90 -140 mm. Hg: 48% >140 mm. Hg: 50% ADHERE Registry: 10/01 -1/04
What is a “Typical” Presentation of ADHF? Blood Pressure at admission (N=104, 573) n n n <90 mm. Hg: 2% 90 -140 mm. Hg: 48% >140 mm. Hg: 50% ADHERE Registry: 10/01 -1/04
 They’re Sicker Than We Think Mortality risk after 1 st hospitalization for ADHF: (Age, male gender, ischemia and decreased LVEF worsen prognosis) n. In-hospital: 3% n 30 -day: 7. 9% n. One year: 30% n. Five years: 60% Baker, DW et al. Am Heart J 2003; 146(2): 258 -64 Ho KK, et al. Circulation 1993; 88(1): 107 -15 Jong P, et al. Arch Int Med 2002; 162(15) 1689 -94 Narang R , et al. Eur Heart J 1996; 17(9) 1390 -1403
They’re Sicker Than We Think Mortality risk after 1 st hospitalization for ADHF: (Age, male gender, ischemia and decreased LVEF worsen prognosis) n. In-hospital: 3% n 30 -day: 7. 9% n. One year: 30% n. Five years: 60% Baker, DW et al. Am Heart J 2003; 146(2): 258 -64 Ho KK, et al. Circulation 1993; 88(1): 107 -15 Jong P, et al. Arch Int Med 2002; 162(15) 1689 -94 Narang R , et al. Eur Heart J 1996; 17(9) 1390 -1403
 Comparative Five Year Mortality n n n Adenocarcinoma of the colon (IIIB): 36% COPD (FEV 1 30 -39% predicted): 53% ESRD (dialysis-dependent): 60 -80%
Comparative Five Year Mortality n n n Adenocarcinoma of the colon (IIIB): 36% COPD (FEV 1 30 -39% predicted): 53% ESRD (dialysis-dependent): 60 -80%
 Summary n n Incidence of ADHF is skyrocketing. Huge strain on hospitals and health care financing Patients are extremely sick There are not enough cardiologists to manage ADHF Generalists will need to become expert in managing all but the sickest patients with ADHF
Summary n n Incidence of ADHF is skyrocketing. Huge strain on hospitals and health care financing Patients are extremely sick There are not enough cardiologists to manage ADHF Generalists will need to become expert in managing all but the sickest patients with ADHF
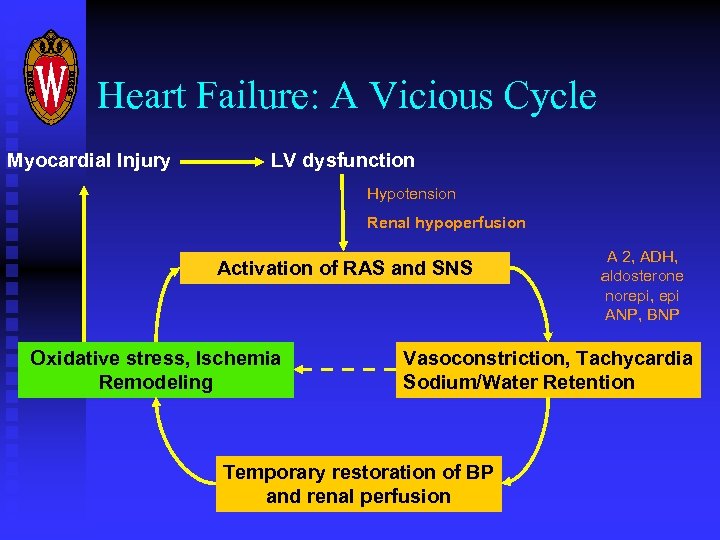 Heart Failure: A Vicious Cycle Myocardial Injury LV dysfunction Hypotension Renal hypoperfusion Activation of RAS and SNS Oxidative stress, Ischemia Remodeling A 2, ADH, aldosterone norepi, epi ANP, BNP Vasoconstriction, Tachycardia Sodium/Water Retention Temporary restoration of BP and renal perfusion
Heart Failure: A Vicious Cycle Myocardial Injury LV dysfunction Hypotension Renal hypoperfusion Activation of RAS and SNS Oxidative stress, Ischemia Remodeling A 2, ADH, aldosterone norepi, epi ANP, BNP Vasoconstriction, Tachycardia Sodium/Water Retention Temporary restoration of BP and renal perfusion
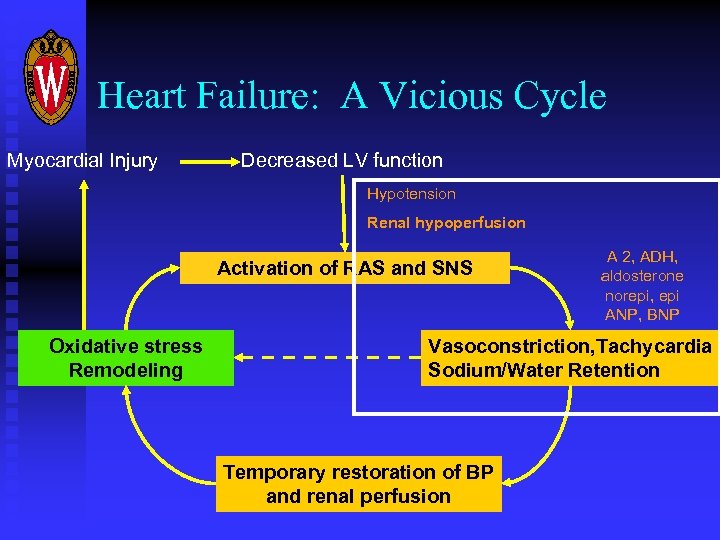 Heart Failure: A Vicious Cycle Myocardial Injury Decreased LV function Hypotension Renal hypoperfusion Activation of RAS and SNS Oxidative stress Remodeling A 2, ADH, aldosterone norepi, epi ANP, BNP Vasoconstriction, Tachycardia Sodium/Water Retention Temporary restoration of BP and renal perfusion
Heart Failure: A Vicious Cycle Myocardial Injury Decreased LV function Hypotension Renal hypoperfusion Activation of RAS and SNS Oxidative stress Remodeling A 2, ADH, aldosterone norepi, epi ANP, BNP Vasoconstriction, Tachycardia Sodium/Water Retention Temporary restoration of BP and renal perfusion
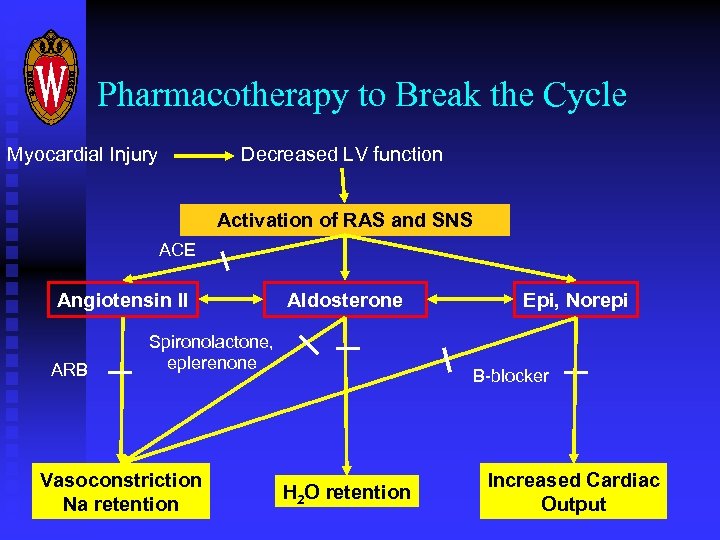 Pharmacotherapy to Break the Cycle Myocardial Injury Decreased LV function Activation of RAS and SNS ACE Angiotensin II ARB Aldosterone Spironolactone, eplerenone Vasoconstriction Na retention Epi, Norepi B-blocker H 2 O retention Increased Cardiac Output
Pharmacotherapy to Break the Cycle Myocardial Injury Decreased LV function Activation of RAS and SNS ACE Angiotensin II ARB Aldosterone Spironolactone, eplerenone Vasoconstriction Na retention Epi, Norepi B-blocker H 2 O retention Increased Cardiac Output
 Goals of Acute Management n n n n Rapidly improve symptoms while preserving organ function Restore function to pre-morbid levels Educate patient and family Initiate therapies/interventions shown to reduce long-term mortality Control costs Improve quality of life Reduce mortality
Goals of Acute Management n n n n Rapidly improve symptoms while preserving organ function Restore function to pre-morbid levels Educate patient and family Initiate therapies/interventions shown to reduce long-term mortality Control costs Improve quality of life Reduce mortality
 Vasoactive Therapy for ADHF
Vasoactive Therapy for ADHF
 Parenteral Drugs for ADHF n n n Diuretics Morphine Vasodilators: nitroglycerin, nesiritide, enalaprilat Afterload reducers: nitroprusside, hydralazine Inotropes: dobutamine, milrinone, amrinone, digoxin
Parenteral Drugs for ADHF n n n Diuretics Morphine Vasodilators: nitroglycerin, nesiritide, enalaprilat Afterload reducers: nitroprusside, hydralazine Inotropes: dobutamine, milrinone, amrinone, digoxin
 What Does the Literature Tell Us? n n n Very little Almost no randomized, placebo-controlled trials of ANY agent for the management of ADHF. “Standard of care” is based almost entirely upon expert opinion and case studies
What Does the Literature Tell Us? n n n Very little Almost no randomized, placebo-controlled trials of ANY agent for the management of ADHF. “Standard of care” is based almost entirely upon expert opinion and case studies
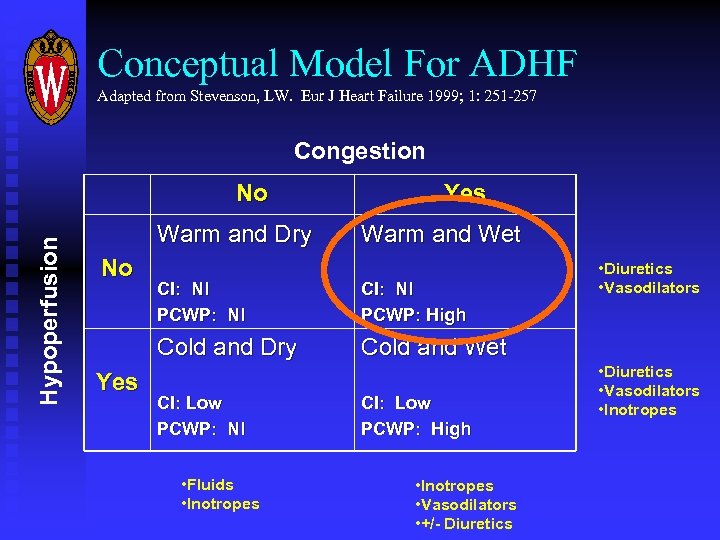 Conceptual Model For ADHF Adapted from Stevenson, LW. Eur J Heart Failure 1999; 1: 251 -257 Congestion Hypoperfusion No Warm and Dry No Yes Warm and Wet CI: Nl PCWP: High Cold and Dry Yes CI: Nl PCWP: Nl • Diuretics • Vasodilators Cold and Wet CI: Low PCWP: Nl • Fluids • Inotropes CI: Low PCWP: High • Inotropes • Vasodilators • +/- Diuretics • Diuretics • Vasodilators • Inotropes
Conceptual Model For ADHF Adapted from Stevenson, LW. Eur J Heart Failure 1999; 1: 251 -257 Congestion Hypoperfusion No Warm and Dry No Yes Warm and Wet CI: Nl PCWP: High Cold and Dry Yes CI: Nl PCWP: Nl • Diuretics • Vasodilators Cold and Wet CI: Low PCWP: Nl • Fluids • Inotropes CI: Low PCWP: High • Inotropes • Vasodilators • +/- Diuretics • Diuretics • Vasodilators • Inotropes
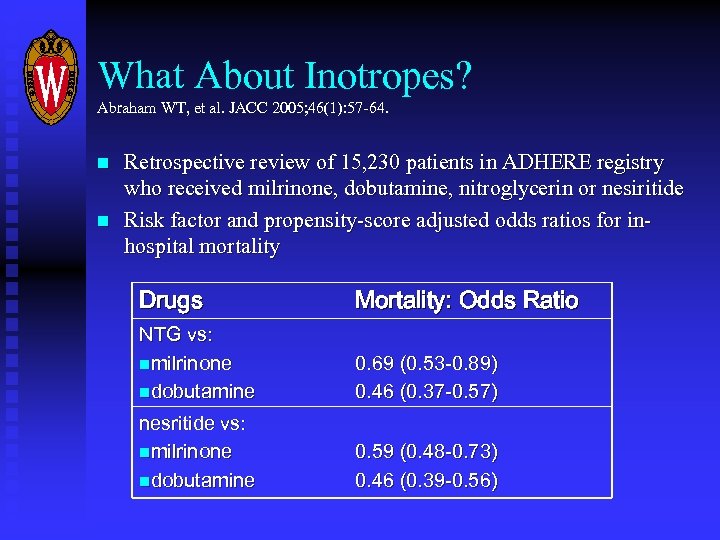 What About Inotropes? Abraham WT, et al. JACC 2005; 46(1): 57 -64. n n Retrospective review of 15, 230 patients in ADHERE registry who received milrinone, dobutamine, nitroglycerin or nesiritide Risk factor and propensity-score adjusted odds ratios for inhospital mortality Drugs Mortality: Odds Ratio NTG vs: nmilrinone ndobutamine 0. 69 (0. 53 -0. 89) 0. 46 (0. 37 -0. 57) nesritide vs: nmilrinone ndobutamine 0. 59 (0. 48 -0. 73) 0. 46 (0. 39 -0. 56)
What About Inotropes? Abraham WT, et al. JACC 2005; 46(1): 57 -64. n n Retrospective review of 15, 230 patients in ADHERE registry who received milrinone, dobutamine, nitroglycerin or nesiritide Risk factor and propensity-score adjusted odds ratios for inhospital mortality Drugs Mortality: Odds Ratio NTG vs: nmilrinone ndobutamine 0. 69 (0. 53 -0. 89) 0. 46 (0. 37 -0. 57) nesritide vs: nmilrinone ndobutamine 0. 59 (0. 48 -0. 73) 0. 46 (0. 39 -0. 56)
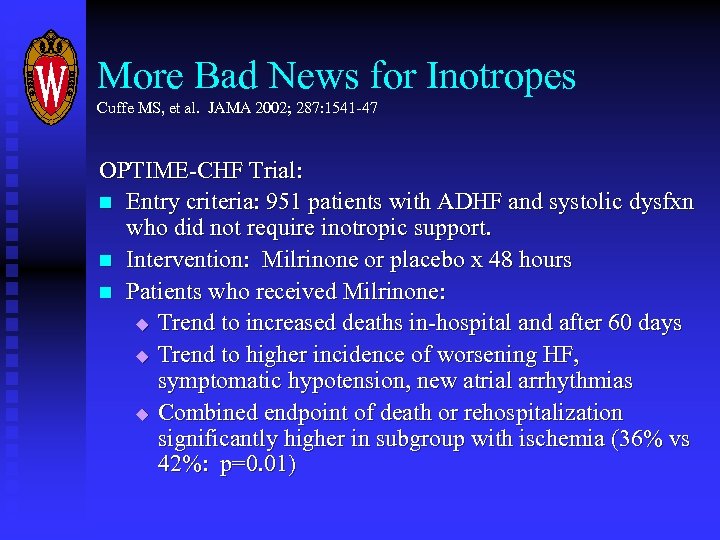 More Bad News for Inotropes Cuffe MS, et al. JAMA 2002; 287: 1541 -47 OPTIME-CHF Trial: n Entry criteria: 951 patients with ADHF and systolic dysfxn who did not require inotropic support. n Intervention: Milrinone or placebo x 48 hours n Patients who received Milrinone: u Trend to increased deaths in-hospital and after 60 days u Trend to higher incidence of worsening HF, symptomatic hypotension, new atrial arrhythmias u Combined endpoint of death or rehospitalization significantly higher in subgroup with ischemia (36% vs 42%: p=0. 01)
More Bad News for Inotropes Cuffe MS, et al. JAMA 2002; 287: 1541 -47 OPTIME-CHF Trial: n Entry criteria: 951 patients with ADHF and systolic dysfxn who did not require inotropic support. n Intervention: Milrinone or placebo x 48 hours n Patients who received Milrinone: u Trend to increased deaths in-hospital and after 60 days u Trend to higher incidence of worsening HF, symptomatic hypotension, new atrial arrhythmias u Combined endpoint of death or rehospitalization significantly higher in subgroup with ischemia (36% vs 42%: p=0. 01)
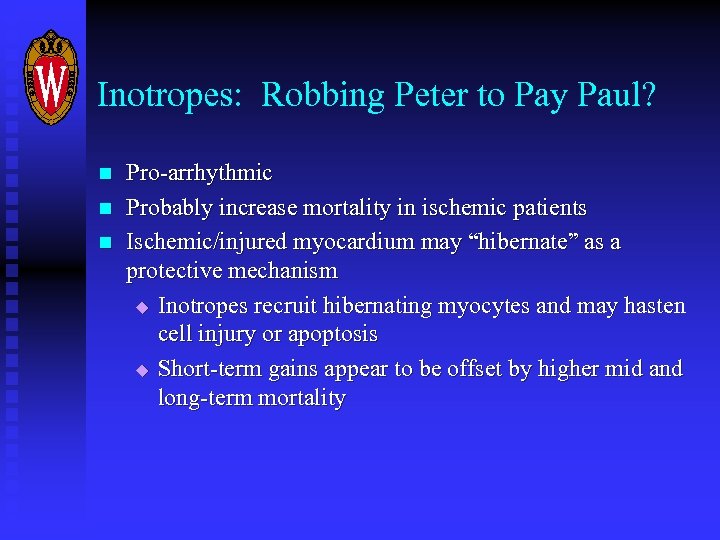 Inotropes: Robbing Peter to Pay Paul? n n n Pro-arrhythmic Probably increase mortality in ischemic patients Ischemic/injured myocardium may “hibernate” as a protective mechanism u Inotropes recruit hibernating myocytes and may hasten cell injury or apoptosis u Short-term gains appear to be offset by higher mid and long-term mortality
Inotropes: Robbing Peter to Pay Paul? n n n Pro-arrhythmic Probably increase mortality in ischemic patients Ischemic/injured myocardium may “hibernate” as a protective mechanism u Inotropes recruit hibernating myocytes and may hasten cell injury or apoptosis u Short-term gains appear to be offset by higher mid and long-term mortality
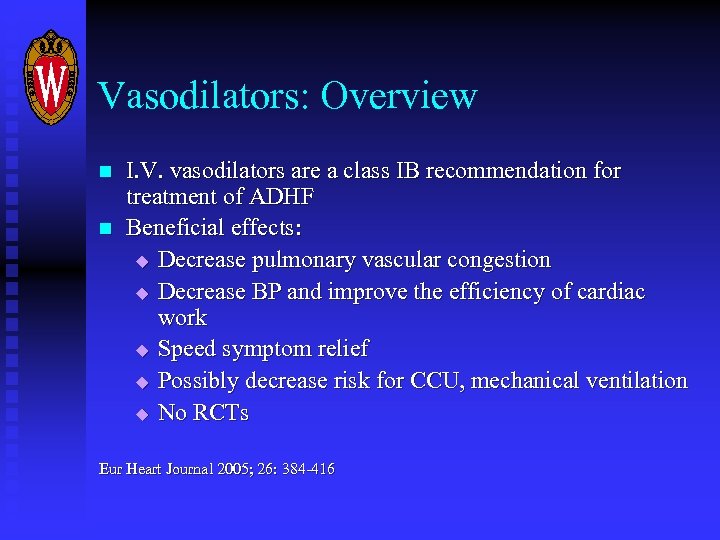 Vasodilators: Overview n n I. V. vasodilators are a class IB recommendation for treatment of ADHF Beneficial effects: u Decrease pulmonary vascular congestion u Decrease BP and improve the efficiency of cardiac work u Speed symptom relief u Possibly decrease risk for CCU, mechanical ventilation u No RCTs Eur Heart Journal 2005; 26: 384 -416
Vasodilators: Overview n n I. V. vasodilators are a class IB recommendation for treatment of ADHF Beneficial effects: u Decrease pulmonary vascular congestion u Decrease BP and improve the efficiency of cardiac work u Speed symptom relief u Possibly decrease risk for CCU, mechanical ventilation u No RCTs Eur Heart Journal 2005; 26: 384 -416
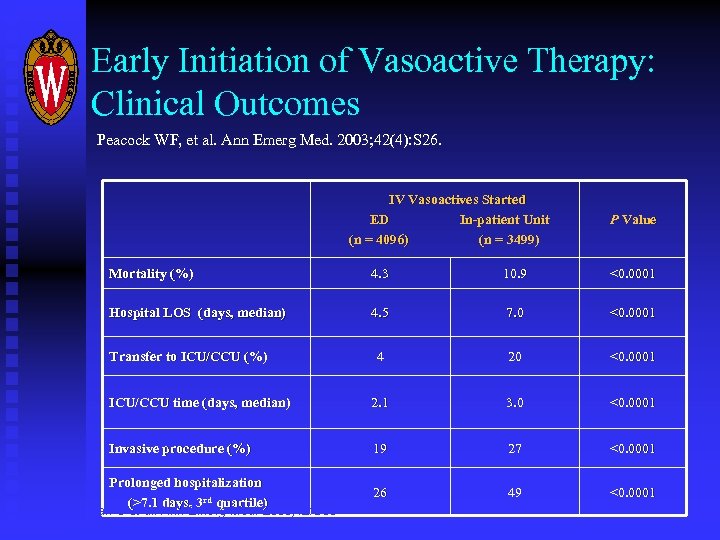 Early Initiation of Vasoactive Therapy: Clinical Outcomes Peacock WF, et al. Ann Emerg Med. 2003; 42(4): S 26. IV Vasoactives Started ED In-patient Unit (n = 4096) (n = 3499) P Value Mortality (%) 4. 3 10. 9 <0. 0001 Hospital LOS (days, median) 4. 5 7. 0 <0. 0001 4 20 <0. 0001 ICU/CCU time (days, median) 2. 1 3. 0 <0. 0001 Invasive procedure (%) 19 27 <0. 0001 Prolonged hospitalization (>7. 1 days, 3 rd quartile) 26 49 <0. 0001 Transfer to ICU/CCU (%) Emerman C et al. Ann Emerg Med. 2003; 42: S 36 Fonarow GC for ADHERE Scientific Advisory Committee. Rev Cardiovasc Med. 2003; 4(suppl 7): S 21
Early Initiation of Vasoactive Therapy: Clinical Outcomes Peacock WF, et al. Ann Emerg Med. 2003; 42(4): S 26. IV Vasoactives Started ED In-patient Unit (n = 4096) (n = 3499) P Value Mortality (%) 4. 3 10. 9 <0. 0001 Hospital LOS (days, median) 4. 5 7. 0 <0. 0001 4 20 <0. 0001 ICU/CCU time (days, median) 2. 1 3. 0 <0. 0001 Invasive procedure (%) 19 27 <0. 0001 Prolonged hospitalization (>7. 1 days, 3 rd quartile) 26 49 <0. 0001 Transfer to ICU/CCU (%) Emerman C et al. Ann Emerg Med. 2003; 42: S 36 Fonarow GC for ADHERE Scientific Advisory Committee. Rev Cardiovasc Med. 2003; 4(suppl 7): S 21
 Choices of I. V. Vasodilators n n n Nitroglycerin Nitroprusside ACE inhibitors (enalaprilat) Morphine? Nesiritide (Natrecor)
Choices of I. V. Vasodilators n n n Nitroglycerin Nitroprusside ACE inhibitors (enalaprilat) Morphine? Nesiritide (Natrecor)
 Nesiritide: Overview n n n Recombinant B-naturetic peptide BNP is released when myocardium is stretched Effects: u Natriuresis / diuresis u Arterial and venous vasodilatation u Suppression of RAS and catechols u Indirect increase of cardiac output
Nesiritide: Overview n n n Recombinant B-naturetic peptide BNP is released when myocardium is stretched Effects: u Natriuresis / diuresis u Arterial and venous vasodilatation u Suppression of RAS and catechols u Indirect increase of cardiac output
 Nesiritide: NSGET Trial Colucci W, et al. NEJM 2000; 343(4): 246 -53 n n n Open label efficacy trial of 432 patients with ADHF—vast majority with NYHA III or IV sx 6 hour infusion of nesiritide decreased PCWP and improved symptoms No acute difference when compared with standard vasoactive agents (inotropes, nitroglycerin, nitroprusside) Not powered to look at outcomes Conclusion: “Intravenous nesiritide is useful for the shortterm treatment of decompensated CHF”
Nesiritide: NSGET Trial Colucci W, et al. NEJM 2000; 343(4): 246 -53 n n n Open label efficacy trial of 432 patients with ADHF—vast majority with NYHA III or IV sx 6 hour infusion of nesiritide decreased PCWP and improved symptoms No acute difference when compared with standard vasoactive agents (inotropes, nitroglycerin, nitroprusside) Not powered to look at outcomes Conclusion: “Intravenous nesiritide is useful for the shortterm treatment of decompensated CHF”
 Nesiritide: VMAC Trial JAMA 2002; 287(12) 1531 -40 n n n Randomized, placebo-controlled, double-dummy trial. 489 patients, all with NYHA class IV CHF. Nesiritide vs nitroglycerin vs placebo x 3 hours, followed by nesiritide or NTG x 24 hours Outcomes: u Nesiritide decreased PCWP more effectively than NTG u Nesiritide offered faster symptom relief u No difference in outcomes btwn nesiritide and NTG
Nesiritide: VMAC Trial JAMA 2002; 287(12) 1531 -40 n n n Randomized, placebo-controlled, double-dummy trial. 489 patients, all with NYHA class IV CHF. Nesiritide vs nitroglycerin vs placebo x 3 hours, followed by nesiritide or NTG x 24 hours Outcomes: u Nesiritide decreased PCWP more effectively than NTG u Nesiritide offered faster symptom relief u No difference in outcomes btwn nesiritide and NTG
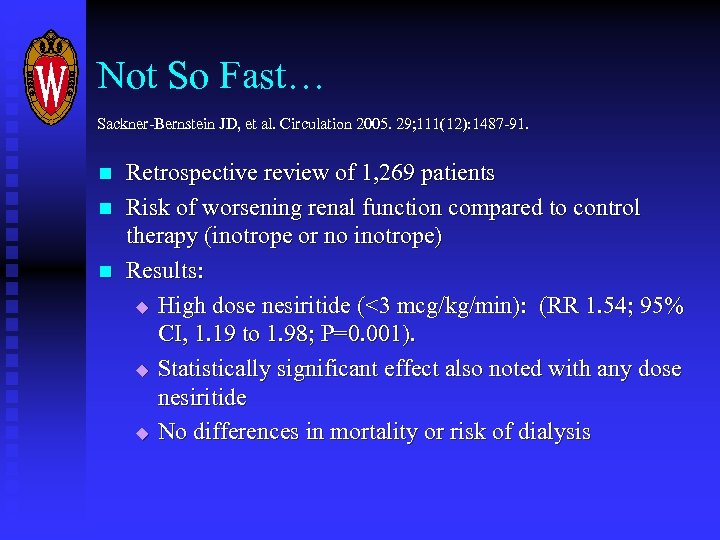 Not So Fast… Sackner-Bernstein JD, et al. Circulation 2005. 29; 111(12): 1487 -91. n n n Retrospective review of 1, 269 patients Risk of worsening renal function compared to control therapy (inotrope or no inotrope) Results: u High dose nesiritide (<3 mcg/kg/min): (RR 1. 54; 95% CI, 1. 19 to 1. 98; P=0. 001). u Statistically significant effect also noted with any dose nesiritide u No differences in mortality or risk of dialysis
Not So Fast… Sackner-Bernstein JD, et al. Circulation 2005. 29; 111(12): 1487 -91. n n n Retrospective review of 1, 269 patients Risk of worsening renal function compared to control therapy (inotrope or no inotrope) Results: u High dose nesiritide (<3 mcg/kg/min): (RR 1. 54; 95% CI, 1. 19 to 1. 98; P=0. 001). u Statistically significant effect also noted with any dose nesiritide u No differences in mortality or risk of dialysis
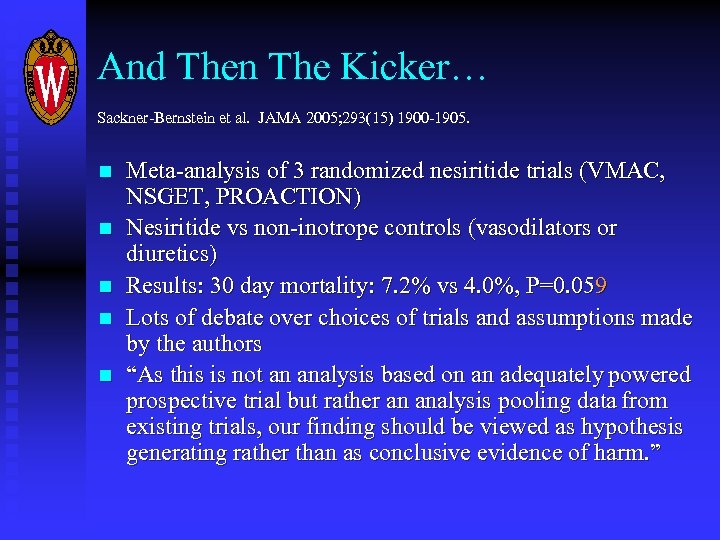 And Then The Kicker… Sackner-Bernstein et al. JAMA 2005; 293(15) 1900 -1905. n n n Meta-analysis of 3 randomized nesiritide trials (VMAC, NSGET, PROACTION) Nesiritide vs non-inotrope controls (vasodilators or diuretics) Results: 30 day mortality: 7. 2% vs 4. 0%, P=0. 059 Lots of debate over choices of trials and assumptions made by the authors “As this is not an analysis based on an adequately powered prospective trial but rather an analysis pooling data from existing trials, our finding should be viewed as hypothesis generating rather than as conclusive evidence of harm. ”
And Then The Kicker… Sackner-Bernstein et al. JAMA 2005; 293(15) 1900 -1905. n n n Meta-analysis of 3 randomized nesiritide trials (VMAC, NSGET, PROACTION) Nesiritide vs non-inotrope controls (vasodilators or diuretics) Results: 30 day mortality: 7. 2% vs 4. 0%, P=0. 059 Lots of debate over choices of trials and assumptions made by the authors “As this is not an analysis based on an adequately powered prospective trial but rather an analysis pooling data from existing trials, our finding should be viewed as hypothesis generating rather than as conclusive evidence of harm. ”

 What About the Other Vasodilators? Are there better choices than nesiritide?
What About the Other Vasodilators? Are there better choices than nesiritide?
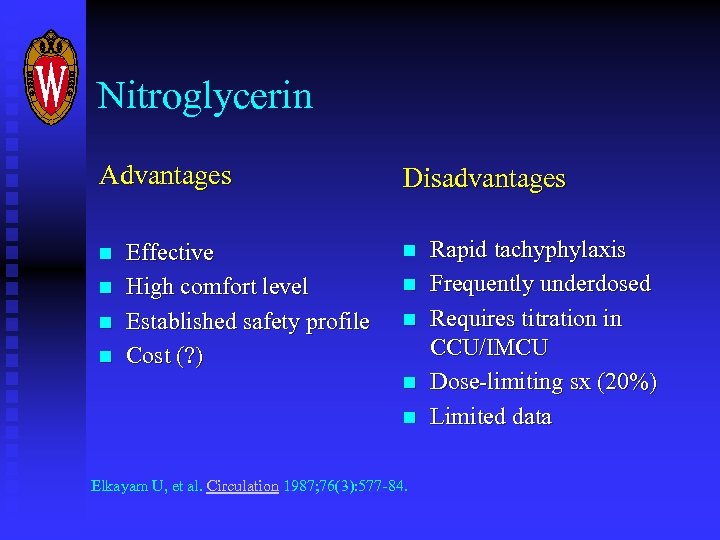 Nitroglycerin Advantages n n Effective High comfort level Established safety profile Cost (? ) Disadvantages n n n Elkayam U, et al. Circulation 1987; 76(3): 577 -84. Rapid tachyphylaxis Frequently underdosed Requires titration in CCU/IMCU Dose-limiting sx (20%) Limited data
Nitroglycerin Advantages n n Effective High comfort level Established safety profile Cost (? ) Disadvantages n n n Elkayam U, et al. Circulation 1987; 76(3): 577 -84. Rapid tachyphylaxis Frequently underdosed Requires titration in CCU/IMCU Dose-limiting sx (20%) Limited data
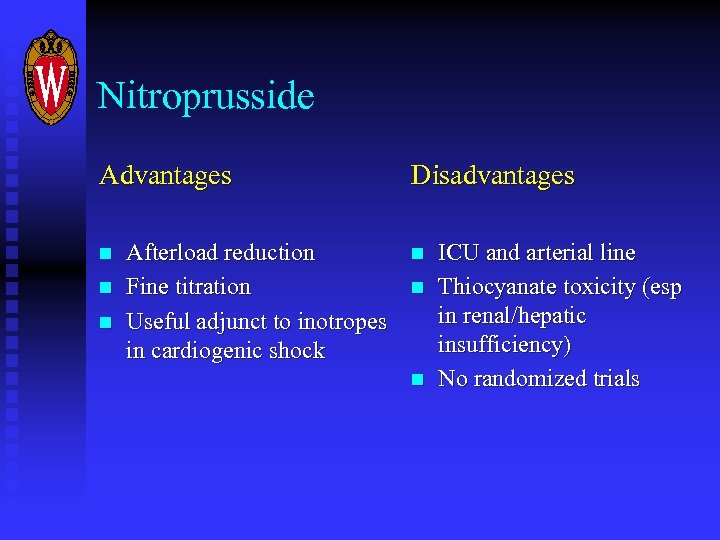 Nitroprusside Advantages n n n Afterload reduction Fine titration Useful adjunct to inotropes in cardiogenic shock Disadvantages n n n ICU and arterial line Thiocyanate toxicity (esp in renal/hepatic insufficiency) No randomized trials
Nitroprusside Advantages n n n Afterload reduction Fine titration Useful adjunct to inotropes in cardiogenic shock Disadvantages n n n ICU and arterial line Thiocyanate toxicity (esp in renal/hepatic insufficiency) No randomized trials
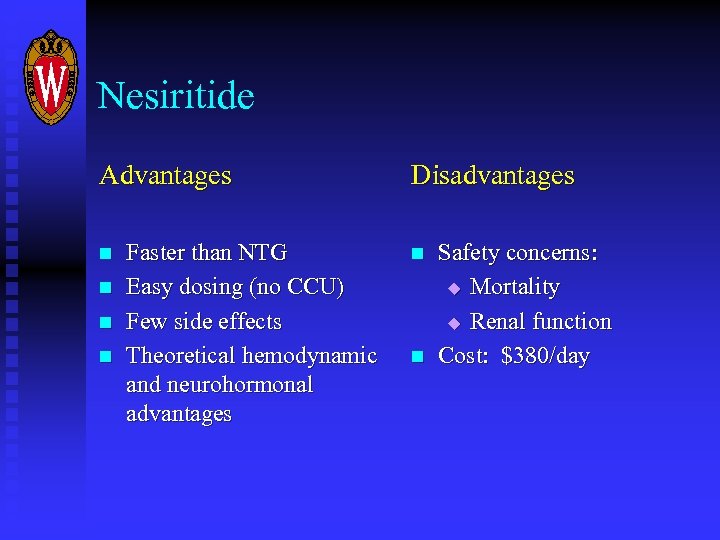 Nesiritide Advantages n n Faster than NTG Easy dosing (no CCU) Few side effects Theoretical hemodynamic and neurohormonal advantages Disadvantages n n Safety concerns: u Mortality u Renal function Cost: $380/day
Nesiritide Advantages n n Faster than NTG Easy dosing (no CCU) Few side effects Theoretical hemodynamic and neurohormonal advantages Disadvantages n n Safety concerns: u Mortality u Renal function Cost: $380/day
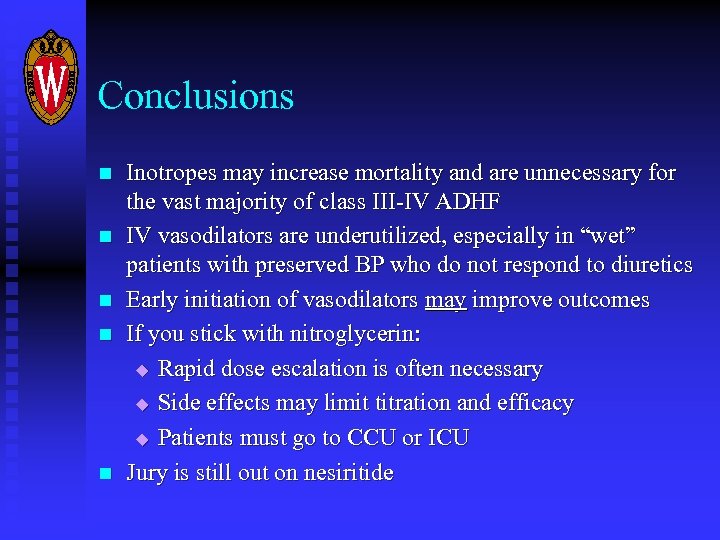 Conclusions n n n Inotropes may increase mortality and are unnecessary for the vast majority of class III-IV ADHF IV vasodilators are underutilized, especially in “wet” patients with preserved BP who do not respond to diuretics Early initiation of vasodilators may improve outcomes If you stick with nitroglycerin: u Rapid dose escalation is often necessary u Side effects may limit titration and efficacy u Patients must go to CCU or ICU Jury is still out on nesiritide
Conclusions n n n Inotropes may increase mortality and are unnecessary for the vast majority of class III-IV ADHF IV vasodilators are underutilized, especially in “wet” patients with preserved BP who do not respond to diuretics Early initiation of vasodilators may improve outcomes If you stick with nitroglycerin: u Rapid dose escalation is often necessary u Side effects may limit titration and efficacy u Patients must go to CCU or ICU Jury is still out on nesiritide
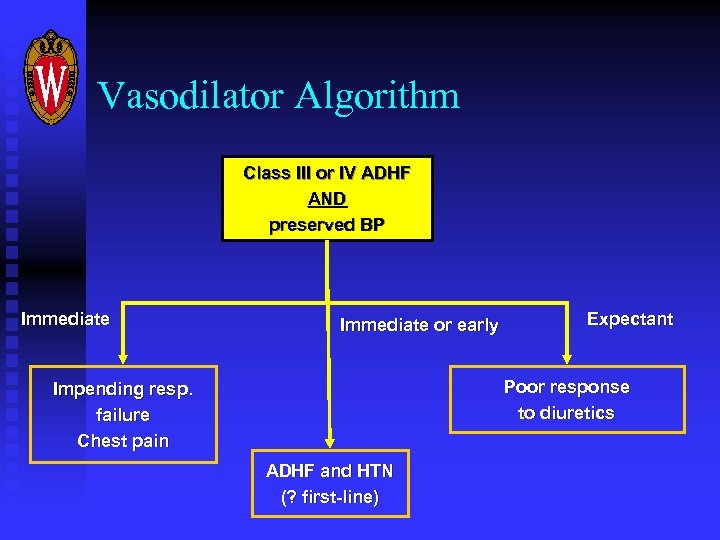 Vasodilator Algorithm Class III or IV ADHF AND preserved BP Immediate or early Expectant Poor response to diuretics Impending resp. failure Chest pain ADHF and HTN (? first-line)
Vasodilator Algorithm Class III or IV ADHF AND preserved BP Immediate or early Expectant Poor response to diuretics Impending resp. failure Chest pain ADHF and HTN (? first-line)
 Prevention of Sudden Cardiac Death
Prevention of Sudden Cardiac Death
 Implantable Cardioverter. Defibrillators (ICDs)
Implantable Cardioverter. Defibrillators (ICDs)
 ICDs: Rationale n n Sudden cardiac death (SCD) is the second most common cause of death in patients with HF (after pump failure) Antiarrhythmics are ineffective if not outright dangerous
ICDs: Rationale n n Sudden cardiac death (SCD) is the second most common cause of death in patients with HF (after pump failure) Antiarrhythmics are ineffective if not outright dangerous
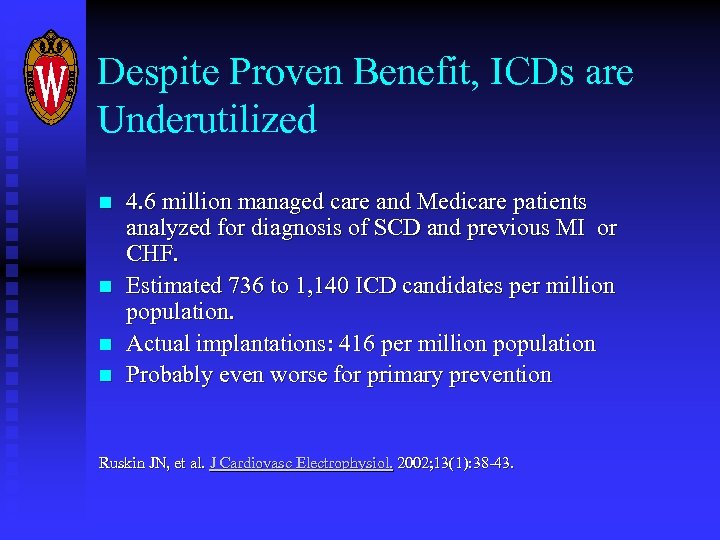 Despite Proven Benefit, ICDs are Underutilized n n 4. 6 million managed care and Medicare patients analyzed for diagnosis of SCD and previous MI or CHF. Estimated 736 to 1, 140 ICD candidates per million population. Actual implantations: 416 per million population Probably even worse for primary prevention Ruskin JN, et al. J Cardiovasc Electrophysiol. 2002; 13(1): 38 -43.
Despite Proven Benefit, ICDs are Underutilized n n 4. 6 million managed care and Medicare patients analyzed for diagnosis of SCD and previous MI or CHF. Estimated 736 to 1, 140 ICD candidates per million population. Actual implantations: 416 per million population Probably even worse for primary prevention Ruskin JN, et al. J Cardiovasc Electrophysiol. 2002; 13(1): 38 -43.
 Primary Prevention Trials n n n n MADIT-II CABG Patch MUSTT DINAMIT CAT AMIOVERT
Primary Prevention Trials n n n n MADIT-II CABG Patch MUSTT DINAMIT CAT AMIOVERT
 ICDs: MADIT-I n n 196 patients enrolled Entry criteria: Prior MI, NSVT, LVEF <35%, EPS: Inducible sustained VT not suppressed with procainamide Intervention: ICD vs amiodarone Average survival at 4 years: u ICD: 3. 7 years u Conventional therapy: 2. 8 years Moss AJ, et al. NEJM 1996; 335: 1933
ICDs: MADIT-I n n 196 patients enrolled Entry criteria: Prior MI, NSVT, LVEF <35%, EPS: Inducible sustained VT not suppressed with procainamide Intervention: ICD vs amiodarone Average survival at 4 years: u ICD: 3. 7 years u Conventional therapy: 2. 8 years Moss AJ, et al. NEJM 1996; 335: 1933
 MUSTT n n 704 patients enrolled Entry criteria: Prior MI, Inducible VT, LVEF <40% Intervention: No therapy vs EPS-guided antiarrhythmic tx (drug or AICD) Outcomes: u Death at 2 years: 12% vs 18% u Death at 5 years: 25% vs 32 % u Mortality reduction due to ICDs, not medication Buxton AE, et al. Circulation 2002; 106: 2466
MUSTT n n 704 patients enrolled Entry criteria: Prior MI, Inducible VT, LVEF <40% Intervention: No therapy vs EPS-guided antiarrhythmic tx (drug or AICD) Outcomes: u Death at 2 years: 12% vs 18% u Death at 5 years: 25% vs 32 % u Mortality reduction due to ICDs, not medication Buxton AE, et al. Circulation 2002; 106: 2466
 MADIT-II n n 1232 patients enrolled Entry criteria: u MI >30 days prior to enrollment, LVEF<30% u No EPS done. Presence of VT not an entry criterion Intervention: ICD vs conventional therapy Outcomes: u Prematurely terminated u Mortality 14. 2% (ICD) vs 19. 8% (no ICD) u Sudden death 3. 8% vs 10. 0% Moss AJ, et al. NEJM 2002; 346: 877
MADIT-II n n 1232 patients enrolled Entry criteria: u MI >30 days prior to enrollment, LVEF<30% u No EPS done. Presence of VT not an entry criterion Intervention: ICD vs conventional therapy Outcomes: u Prematurely terminated u Mortality 14. 2% (ICD) vs 19. 8% (no ICD) u Sudden death 3. 8% vs 10. 0% Moss AJ, et al. NEJM 2002; 346: 877
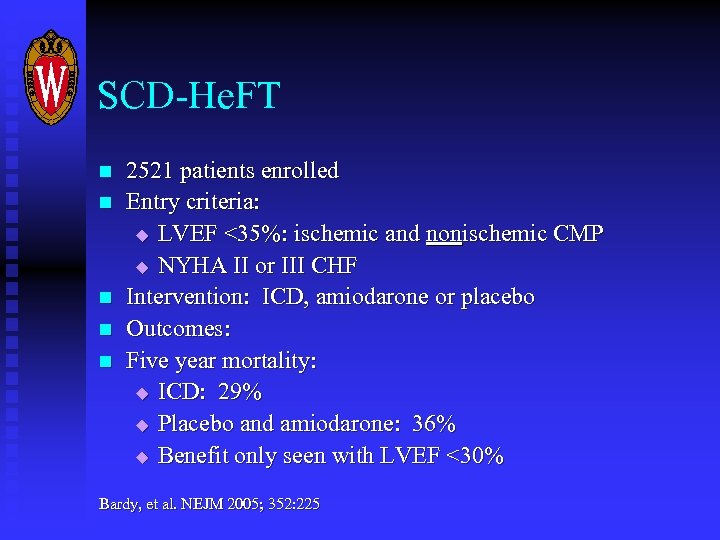 SCD-He. FT n n n 2521 patients enrolled Entry criteria: u LVEF <35%: ischemic and nonischemic CMP u NYHA II or III CHF Intervention: ICD, amiodarone or placebo Outcomes: Five year mortality: u ICD: 29% u Placebo and amiodarone: 36% u Benefit only seen with LVEF <30% Bardy, et al. NEJM 2005; 352: 225
SCD-He. FT n n n 2521 patients enrolled Entry criteria: u LVEF <35%: ischemic and nonischemic CMP u NYHA II or III CHF Intervention: ICD, amiodarone or placebo Outcomes: Five year mortality: u ICD: 29% u Placebo and amiodarone: 36% u Benefit only seen with LVEF <30% Bardy, et al. NEJM 2005; 352: 225
 More for Everyone! Increasingly broad indications for ICDs: u Ischemic CMP with inducible VT u Ischemic CMP with or without VT u Nonischemic CMP
More for Everyone! Increasingly broad indications for ICDs: u Ischemic CMP with inducible VT u Ischemic CMP with or without VT u Nonischemic CMP
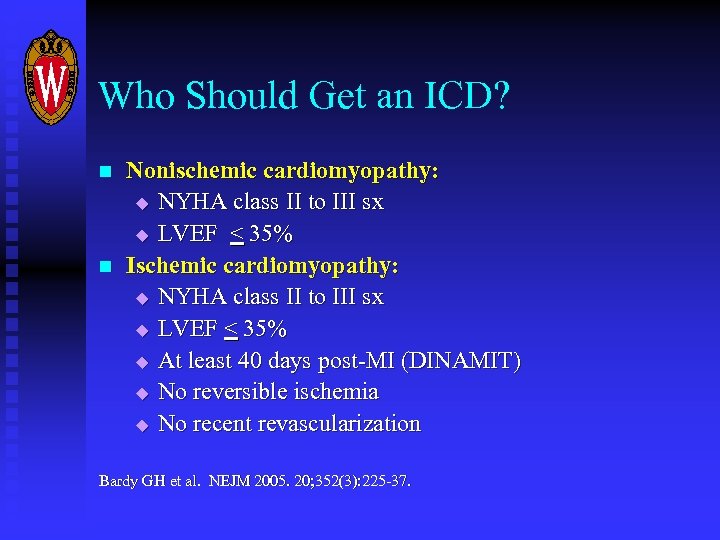 Who Should Get an ICD? n n Nonischemic cardiomyopathy: u NYHA class II to III sx u LVEF < 35% Ischemic cardiomyopathy: u NYHA class II to III sx u LVEF < 35% u At least 40 days post-MI (DINAMIT) u No reversible ischemia u No recent revascularization Bardy GH et al. NEJM 2005. 20; 352(3): 225 -37.
Who Should Get an ICD? n n Nonischemic cardiomyopathy: u NYHA class II to III sx u LVEF < 35% Ischemic cardiomyopathy: u NYHA class II to III sx u LVEF < 35% u At least 40 days post-MI (DINAMIT) u No reversible ischemia u No recent revascularization Bardy GH et al. NEJM 2005. 20; 352(3): 225 -37.
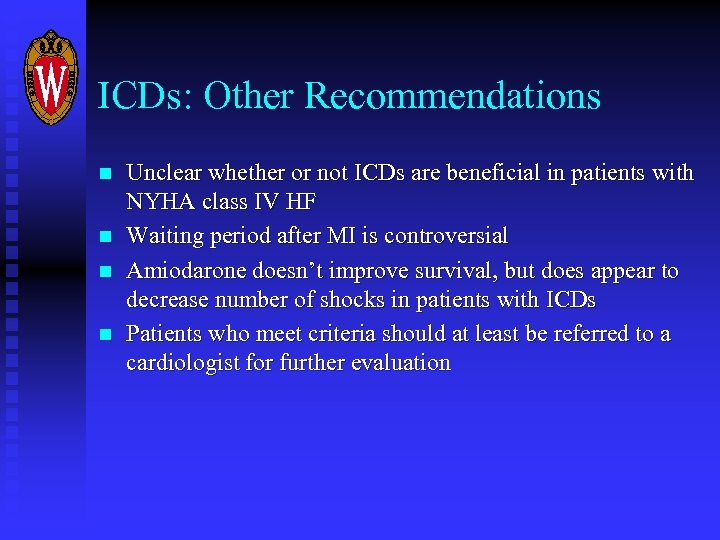 ICDs: Other Recommendations n n Unclear whether or not ICDs are beneficial in patients with NYHA class IV HF Waiting period after MI is controversial Amiodarone doesn’t improve survival, but does appear to decrease number of shocks in patients with ICDs Patients who meet criteria should at least be referred to a cardiologist for further evaluation
ICDs: Other Recommendations n n Unclear whether or not ICDs are beneficial in patients with NYHA class IV HF Waiting period after MI is controversial Amiodarone doesn’t improve survival, but does appear to decrease number of shocks in patients with ICDs Patients who meet criteria should at least be referred to a cardiologist for further evaluation
 Mechanical Resynchronization
Mechanical Resynchronization
 Cardiac Resynchronization Therapy (CRT) n What it is: Using biventricular pacing to re-synchronize LV and RV contraction in patients with HF and IVCD n Rationale: u u u IVCD and LBBB worsen HF by causing ventricular dyssynchrony Patients with HF and IVCD/BBB have increased sx and worse outcomes than patients with normal ventricular conduction. Dual-chamber pacing is associated with poor outcomes.
Cardiac Resynchronization Therapy (CRT) n What it is: Using biventricular pacing to re-synchronize LV and RV contraction in patients with HF and IVCD n Rationale: u u u IVCD and LBBB worsen HF by causing ventricular dyssynchrony Patients with HF and IVCD/BBB have increased sx and worse outcomes than patients with normal ventricular conduction. Dual-chamber pacing is associated with poor outcomes.
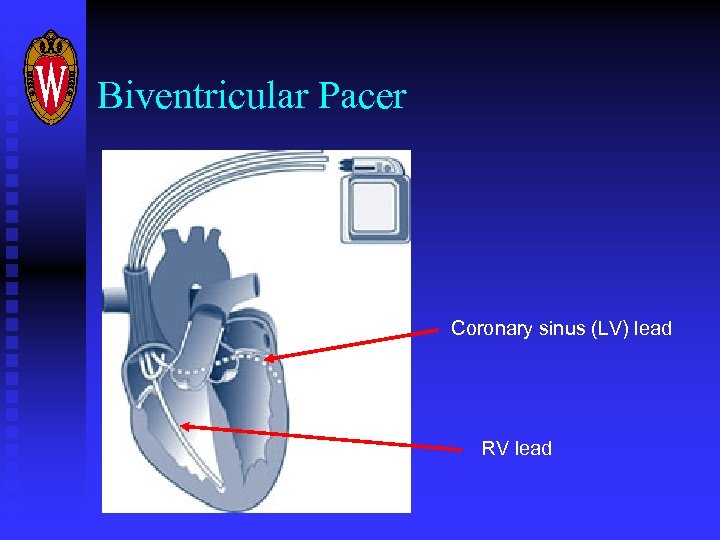 Biventricular Pacer Coronary sinus (LV) lead RV lead
Biventricular Pacer Coronary sinus (LV) lead RV lead
 CRT: Outcomes n n Meta-analysis of 3216 patients Increased likelihood of improving at least one NYHA class (58% vs 37%) Reduced hospitalization for CHF (RR 0. 65) for patients with NYHA III or IV CHF Reduced mortality (RR 0. 79) due to fewer deaths from progressive HF Mc. Calister FA, et al. Ann Int Med 2004; 141: 381 -390.
CRT: Outcomes n n Meta-analysis of 3216 patients Increased likelihood of improving at least one NYHA class (58% vs 37%) Reduced hospitalization for CHF (RR 0. 65) for patients with NYHA III or IV CHF Reduced mortality (RR 0. 79) due to fewer deaths from progressive HF Mc. Calister FA, et al. Ann Int Med 2004; 141: 381 -390.
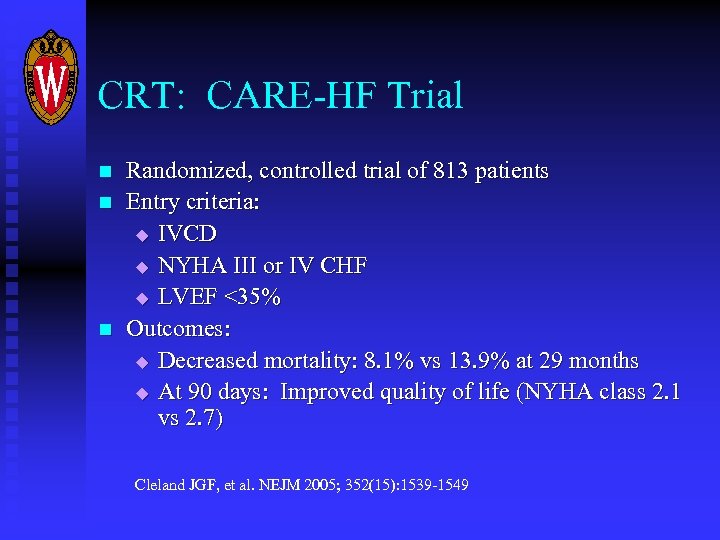 CRT: CARE-HF Trial n n n Randomized, controlled trial of 813 patients Entry criteria: u IVCD u NYHA III or IV CHF u LVEF <35% Outcomes: u Decreased mortality: 8. 1% vs 13. 9% at 29 months u At 90 days: Improved quality of life (NYHA class 2. 1 vs 2. 7) Cleland JGF, et al. NEJM 2005; 352(15): 1539 -1549
CRT: CARE-HF Trial n n n Randomized, controlled trial of 813 patients Entry criteria: u IVCD u NYHA III or IV CHF u LVEF <35% Outcomes: u Decreased mortality: 8. 1% vs 13. 9% at 29 months u At 90 days: Improved quality of life (NYHA class 2. 1 vs 2. 7) Cleland JGF, et al. NEJM 2005; 352(15): 1539 -1549
 CRT: Recommendations n n Indicated for patients with LBBB or IVCD and: u LVEF < 35% u Sinus rhythm u NYHA III-IV symptoms despite optimal medical mgmt These patients are also candidates for ICD placement and should be considered for a dual-function device. J Am Coll Cardiol. 2005 Sep 20; 46(6): 1116 -43.
CRT: Recommendations n n Indicated for patients with LBBB or IVCD and: u LVEF < 35% u Sinus rhythm u NYHA III-IV symptoms despite optimal medical mgmt These patients are also candidates for ICD placement and should be considered for a dual-function device. J Am Coll Cardiol. 2005 Sep 20; 46(6): 1116 -43.
 Neurohormonal Modulation in the Hospital
Neurohormonal Modulation in the Hospital
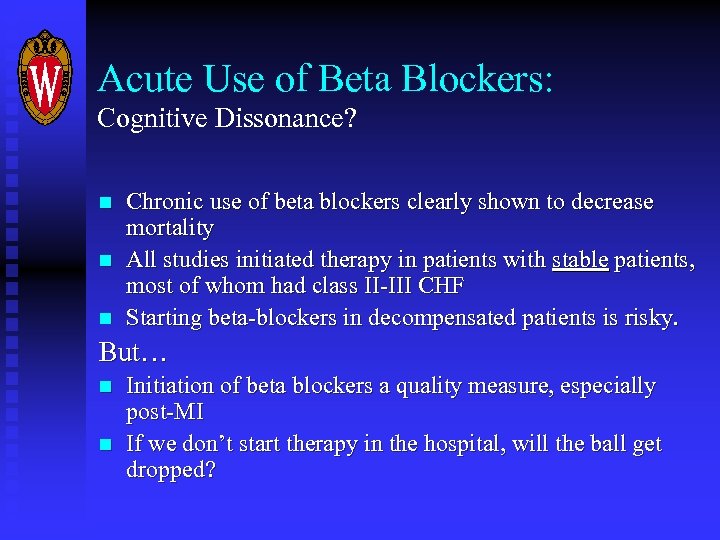 Acute Use of Beta Blockers: Cognitive Dissonance? n n n Chronic use of beta blockers clearly shown to decrease mortality All studies initiated therapy in patients with stable patients, most of whom had class II-III CHF Starting beta-blockers in decompensated patients is risky. But… n n Initiation of beta blockers a quality measure, especially post-MI If we don’t start therapy in the hospital, will the ball get dropped?
Acute Use of Beta Blockers: Cognitive Dissonance? n n n Chronic use of beta blockers clearly shown to decrease mortality All studies initiated therapy in patients with stable patients, most of whom had class II-III CHF Starting beta-blockers in decompensated patients is risky. But… n n Initiation of beta blockers a quality measure, especially post-MI If we don’t start therapy in the hospital, will the ball get dropped?
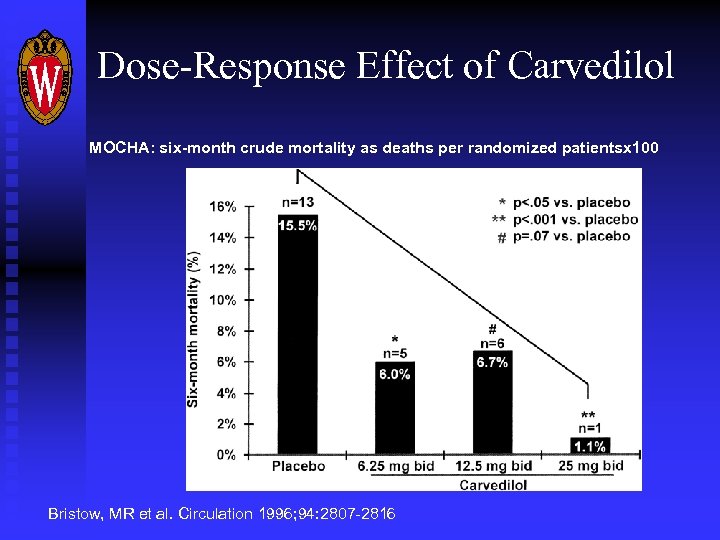 Dose-Response Effect of Carvedilol MOCHA: six-month crude mortality as deaths per randomized patientsx 100 Bristow, MR et al. Circulation 1996; 94: 2807 -2816
Dose-Response Effect of Carvedilol MOCHA: six-month crude mortality as deaths per randomized patientsx 100 Bristow, MR et al. Circulation 1996; 94: 2807 -2816
 Beta Blockers Are Not Equal Four beta-blockers shown to decrease mortality in systolic HF: u u Carvedilol Metoprolol Bisoprolol Bucindolol
Beta Blockers Are Not Equal Four beta-blockers shown to decrease mortality in systolic HF: u u Carvedilol Metoprolol Bisoprolol Bucindolol
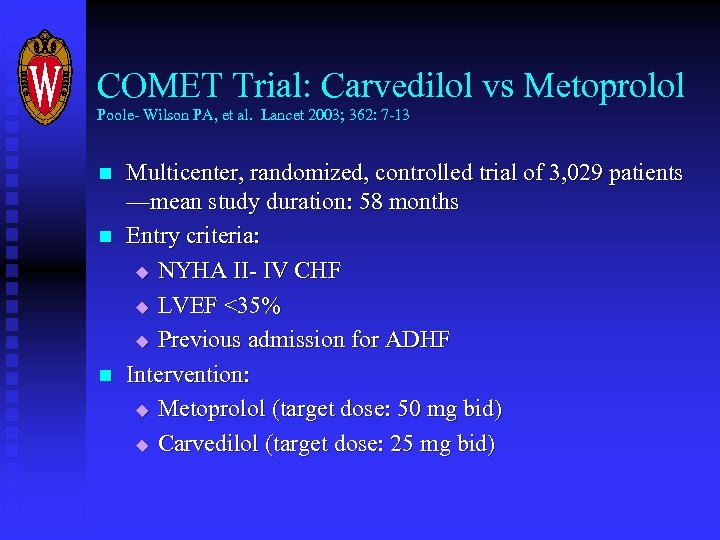 COMET Trial: Carvedilol vs Metoprolol Poole- Wilson PA, et al. Lancet 2003; 362: 7 -13 n n n Multicenter, randomized, controlled trial of 3, 029 patients —mean study duration: 58 months Entry criteria: u NYHA II- IV CHF u LVEF <35% u Previous admission for ADHF Intervention: u Metoprolol (target dose: 50 mg bid) u Carvedilol (target dose: 25 mg bid)
COMET Trial: Carvedilol vs Metoprolol Poole- Wilson PA, et al. Lancet 2003; 362: 7 -13 n n n Multicenter, randomized, controlled trial of 3, 029 patients —mean study duration: 58 months Entry criteria: u NYHA II- IV CHF u LVEF <35% u Previous admission for ADHF Intervention: u Metoprolol (target dose: 50 mg bid) u Carvedilol (target dose: 25 mg bid)
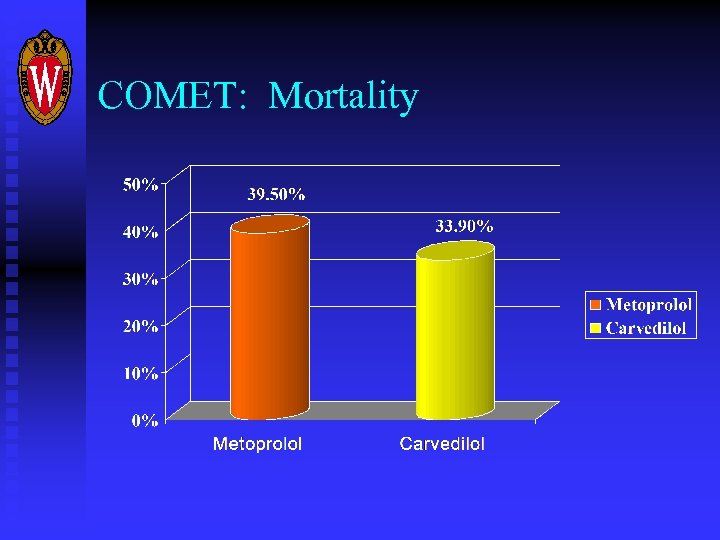 COMET: Mortality
COMET: Mortality
 Huge Cost Differential One month supply at doses per COMET Trial: AWP (drugstore. com) n n Metoprolol tartrate (50 mg bid) $12. 09 Carvedilol (25 mg bid) $95. 00
Huge Cost Differential One month supply at doses per COMET Trial: AWP (drugstore. com) n n Metoprolol tartrate (50 mg bid) $12. 09 Carvedilol (25 mg bid) $95. 00
 Beta Blockers: Bottom Line n n n Most of the benefit from carvedilol occurs at low dose It’s probably reasonable to start beta-blockers in-house, especially if patient is hypertensive In non-hypertensive and elderly patients: Start low and titrate slowly Metoprolol is good, but carvedilol is better Many patients cannot afford carvedilol
Beta Blockers: Bottom Line n n n Most of the benefit from carvedilol occurs at low dose It’s probably reasonable to start beta-blockers in-house, especially if patient is hypertensive In non-hypertensive and elderly patients: Start low and titrate slowly Metoprolol is good, but carvedilol is better Many patients cannot afford carvedilol
 Conclusions n n n n Acute and chronic HF may be the single most common inpatient dx managed by hospitalists/internists Economic burden is huge and growing Consider vasodilators in patients with ADHF, preserved BP. Inotropes should be reserved for patients with hypotension and evidence of end-organ hypoperfusion. Think ICD in any patient with symptomatic HF, EF <35% and no reversible etiology. Think CRT for patients with EF <35%, IVCD and sx not improved with medical therapy Choose the right beta-blocker and titrate slowly in-house
Conclusions n n n n Acute and chronic HF may be the single most common inpatient dx managed by hospitalists/internists Economic burden is huge and growing Consider vasodilators in patients with ADHF, preserved BP. Inotropes should be reserved for patients with hypotension and evidence of end-organ hypoperfusion. Think ICD in any patient with symptomatic HF, EF <35% and no reversible etiology. Think CRT for patients with EF <35%, IVCD and sx not improved with medical therapy Choose the right beta-blocker and titrate slowly in-house