503a6f3ce408a434d0dcb3661ebcbb7c.ppt
- Количество слайдов: 24
 Action Level Radiology Tags (ALRTs): Facilitating the Tracking of Incidental CT Findings March 11 th, 2013
Action Level Radiology Tags (ALRTs): Facilitating the Tracking of Incidental CT Findings March 11 th, 2013
 The Problem—Case Example #1 66 -year-old smoker admitted to community hospital with diverticulitis requiring IV antibiotics—discharged on Day 5 to follow-up with PCP. Incidental CT finding of LLL nodule recorded on radiology report, but not addressed by care team or mentioned in discharge summary. Lawsuit filed two years later for delay in diagnosis of metastatic lung cancer. 2
The Problem—Case Example #1 66 -year-old smoker admitted to community hospital with diverticulitis requiring IV antibiotics—discharged on Day 5 to follow-up with PCP. Incidental CT finding of LLL nodule recorded on radiology report, but not addressed by care team or mentioned in discharge summary. Lawsuit filed two years later for delay in diagnosis of metastatic lung cancer. 2
 The Problem—Case Example #2 50 -year-old male presents to ED with suspected appendicitis, confirmed by CT, which also reveals possible renal mass. Surgical team performs laparoscopic appendectomy, discharging patient the next morning, without addressing renal incidental finding. No discharge summary to PCP since this was an observation stay. Patient presents 12 months later to PCP with pulmonary mets from metastatic renal cell carcinoma. 3
The Problem—Case Example #2 50 -year-old male presents to ED with suspected appendicitis, confirmed by CT, which also reveals possible renal mass. Surgical team performs laparoscopic appendectomy, discharging patient the next morning, without addressing renal incidental finding. No discharge summary to PCP since this was an observation stay. Patient presents 12 months later to PCP with pulmonary mets from metastatic renal cell carcinoma. 3
 Root Causes I. Difficult to Fix Category: • PCPs no longer participate directly in hospital care • Length of stay (LOS) continues to shorten, so hard copy radiology reports often not posted in chart by discharge date • Short LOS also sets focus on getting the patient discharged, and not on addressing other issues that could be worked up as an outpatient • Discharge summaries not consistently required for observation stays • PCPs don’t want every hospital radiology report to appear in their EMR inbox, or on their desk 4
Root Causes I. Difficult to Fix Category: • PCPs no longer participate directly in hospital care • Length of stay (LOS) continues to shorten, so hard copy radiology reports often not posted in chart by discharge date • Short LOS also sets focus on getting the patient discharged, and not on addressing other issues that could be worked up as an outpatient • Discharge summaries not consistently required for observation stays • PCPs don’t want every hospital radiology report to appear in their EMR inbox, or on their desk 4
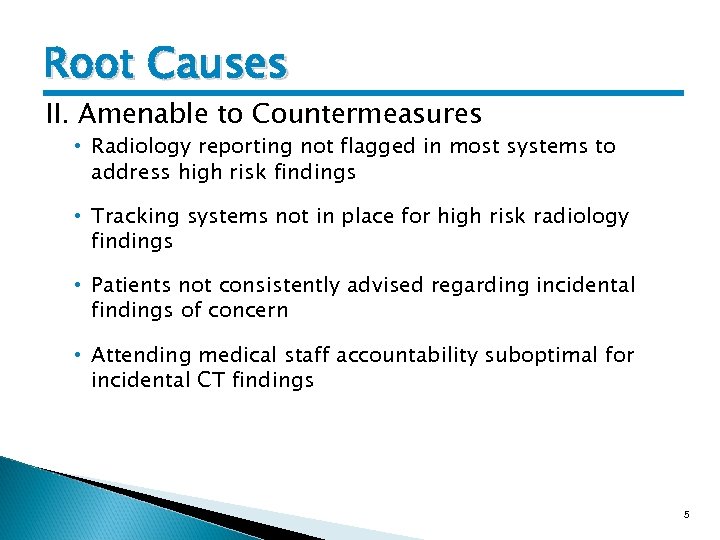 Root Causes II. Amenable to Countermeasures • Radiology reporting not flagged in most systems to address high risk findings • Tracking systems not in place for high risk radiology findings • Patients not consistently advised regarding incidental findings of concern • Attending medical staff accountability suboptimal for incidental CT findings 5
Root Causes II. Amenable to Countermeasures • Radiology reporting not flagged in most systems to address high risk findings • Tracking systems not in place for high risk radiology findings • Patients not consistently advised regarding incidental findings of concern • Attending medical staff accountability suboptimal for incidental CT findings 5
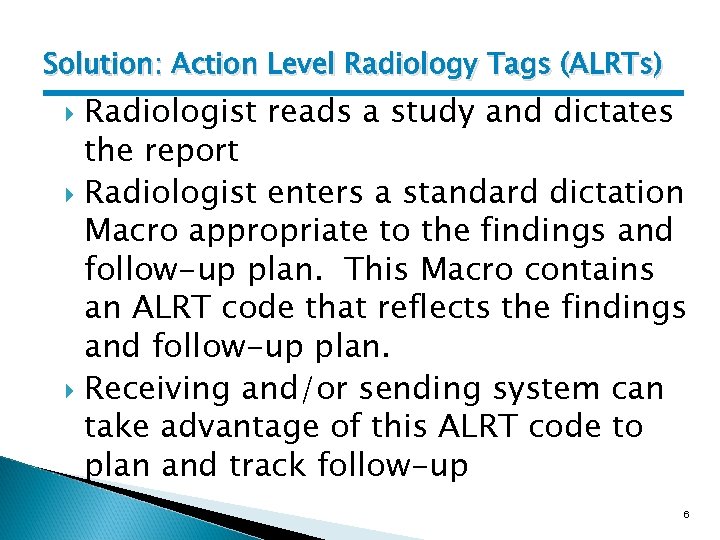 Solution: Action Level Radiology Tags (ALRTs) Radiologist reads a study and dictates the report Radiologist enters a standard dictation Macro appropriate to the findings and follow-up plan. This Macro contains an ALRT code that reflects the findings and follow-up plan. Receiving and/or sending system can take advantage of this ALRT code to plan and track follow-up 6
Solution: Action Level Radiology Tags (ALRTs) Radiologist reads a study and dictates the report Radiologist enters a standard dictation Macro appropriate to the findings and follow-up plan. This Macro contains an ALRT code that reflects the findings and follow-up plan. Receiving and/or sending system can take advantage of this ALRT code to plan and track follow-up 6
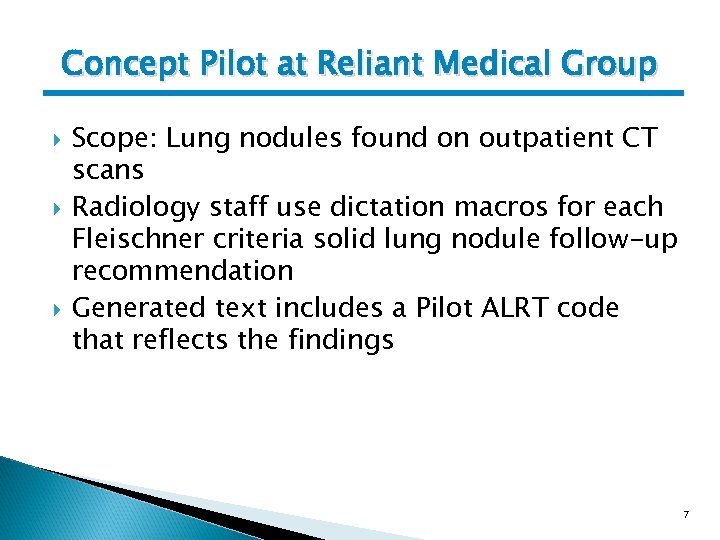 Concept Pilot at Reliant Medical Group Scope: Lung nodules found on outpatient CT scans Radiology staff use dictation macros for each Fleischner criteria solid lung nodule follow-up recommendation Generated text includes a Pilot ALRT code that reflects the findings 7
Concept Pilot at Reliant Medical Group Scope: Lung nodules found on outpatient CT scans Radiology staff use dictation macros for each Fleischner criteria solid lung nodule follow-up recommendation Generated text includes a Pilot ALRT code that reflects the findings 7
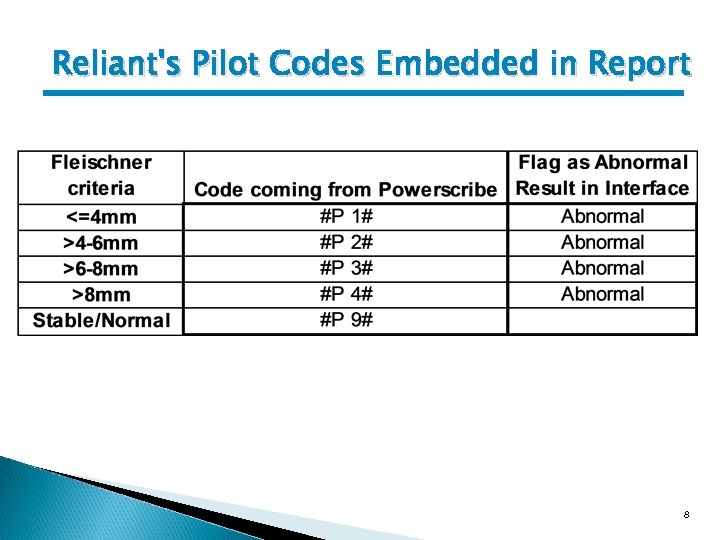 Reliant's Pilot Codes Embedded in Report 8
Reliant's Pilot Codes Embedded in Report 8
 Pilot code triggers flag in MD's EHR In. Basket © 2013 Epic Systems Corporation 9
Pilot code triggers flag in MD's EHR In. Basket © 2013 Epic Systems Corporation 9
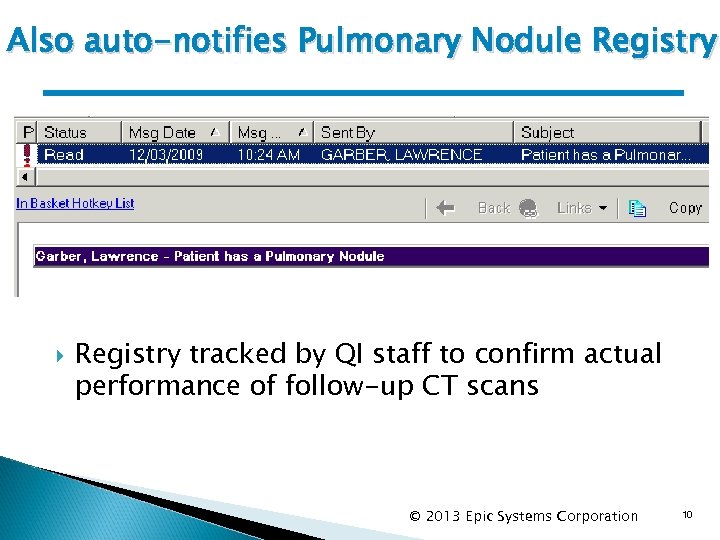 Also auto-notifies Pulmonary Nodule Registry tracked by QI staff to confirm actual performance of follow-up CT scans © 2013 Epic Systems Corporation 10
Also auto-notifies Pulmonary Nodule Registry tracked by QI staff to confirm actual performance of follow-up CT scans © 2013 Epic Systems Corporation 10
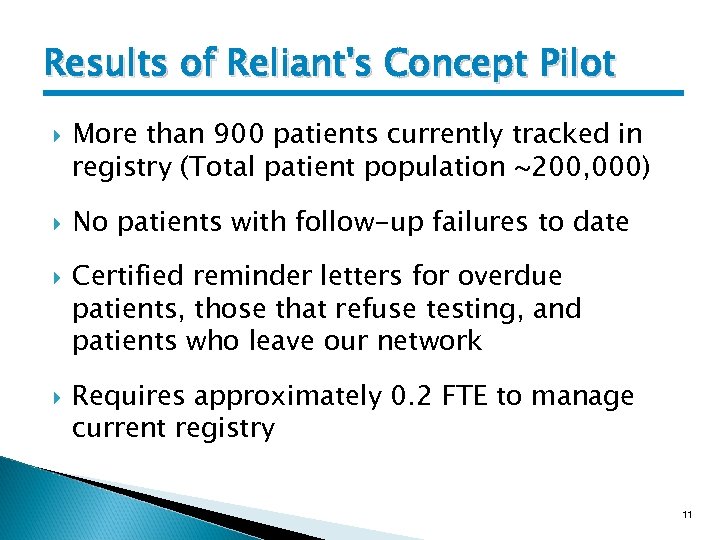 Results of Reliant's Concept Pilot More than 900 patients currently tracked in registry (Total patient population ~200, 000) No patients with follow-up failures to date Certified reminder letters for overdue patients, those that refuse testing, and patients who leave our network Requires approximately 0. 2 FTE to manage current registry 11
Results of Reliant's Concept Pilot More than 900 patients currently tracked in registry (Total patient population ~200, 000) No patients with follow-up failures to date Certified reminder letters for overdue patients, those that refuse testing, and patients who leave our network Requires approximately 0. 2 FTE to manage current registry 11
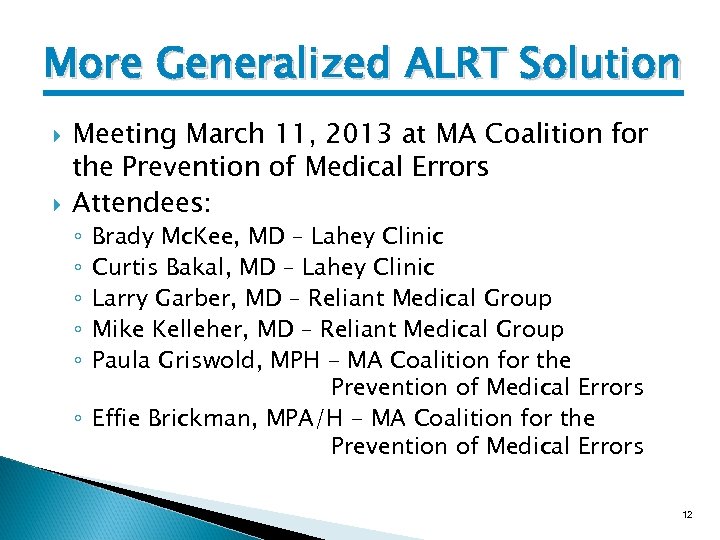 More Generalized ALRT Solution Meeting March 11, 2013 at MA Coalition for the Prevention of Medical Errors Attendees: Brady Mc. Kee, MD – Lahey Clinic Curtis Bakal, MD – Lahey Clinic Larry Garber, MD – Reliant Medical Group Mike Kelleher, MD – Reliant Medical Group Paula Griswold, MPH - MA Coalition for the Prevention of Medical Errors ◦ Effie Brickman, MPA/H - MA Coalition for the Prevention of Medical Errors ◦ ◦ ◦ 12
More Generalized ALRT Solution Meeting March 11, 2013 at MA Coalition for the Prevention of Medical Errors Attendees: Brady Mc. Kee, MD – Lahey Clinic Curtis Bakal, MD – Lahey Clinic Larry Garber, MD – Reliant Medical Group Mike Kelleher, MD – Reliant Medical Group Paula Griswold, MPH - MA Coalition for the Prevention of Medical Errors ◦ Effie Brickman, MPA/H - MA Coalition for the Prevention of Medical Errors ◦ ◦ ◦ 12
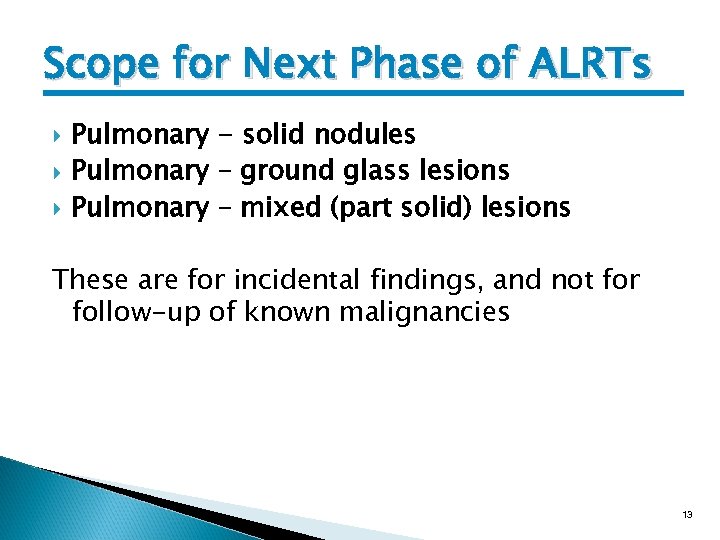 Scope for Next Phase of ALRTs Pulmonary - solid nodules Pulmonary – ground glass lesions Pulmonary – mixed (part solid) lesions These are for incidental findings, and not for follow-up of known malignancies 13
Scope for Next Phase of ALRTs Pulmonary - solid nodules Pulmonary – ground glass lesions Pulmonary – mixed (part solid) lesions These are for incidental findings, and not for follow-up of known malignancies 13
 Guidelines for Follow-up Reviewed Fleischner Society criteria for solid pulmonary nodules Reviewed Fleischner Society criteria for subsolid pulmonary nodules Reviewed National Comprehensive Cancer Network criteria for sub-solid pulmonary nodules Decided that each radiologist/organization can choose whichever guidelines they wish to follow. ALRTs will codify just the type of lesions and recommended follow-up 14
Guidelines for Follow-up Reviewed Fleischner Society criteria for solid pulmonary nodules Reviewed Fleischner Society criteria for subsolid pulmonary nodules Reviewed National Comprehensive Cancer Network criteria for sub-solid pulmonary nodules Decided that each radiologist/organization can choose whichever guidelines they wish to follow. ALRTs will codify just the type of lesions and recommended follow-up 14
 Size of Lesions Discussed the limits of accuracy in determining lesions size (e. g. Lahey just says, for example, 5 -6 mm or 6 -7 mm) Discussed inconsistency of use in guidelines (e. g. <5 mm vs. <=5 mm) Discussed that while conveying the size of the lesion could in theory enable automated tracking of lesion size, it would be impossible to know for certain that it’s the same lesion, and that realistically it would rarely add value to what the radiologists recommend for follow-up. Decided to not convey lesion size in ALRT code 15
Size of Lesions Discussed the limits of accuracy in determining lesions size (e. g. Lahey just says, for example, 5 -6 mm or 6 -7 mm) Discussed inconsistency of use in guidelines (e. g. <5 mm vs. <=5 mm) Discussed that while conveying the size of the lesion could in theory enable automated tracking of lesion size, it would be impossible to know for certain that it’s the same lesion, and that realistically it would rarely add value to what the radiologists recommend for follow-up. Decided to not convey lesion size in ALRT code 15
 Follow-up Recommendations Consists of timeframe and modality Differs based on whether a patient is highrisk for malignancy or not Radiologists can’t be expected to consistently know whether the patient fits into the highrisk category Decided that each report macro text will include follow-up recommendations for highrisk patient, non-high-risk patients, as well as a statement of criteria for “high risk” 16
Follow-up Recommendations Consists of timeframe and modality Differs based on whether a patient is highrisk for malignancy or not Radiologists can’t be expected to consistently know whether the patient fits into the highrisk category Decided that each report macro text will include follow-up recommendations for highrisk patient, non-high-risk patients, as well as a statement of criteria for “high risk” 16
 Follow-up Timeframes It was discussed that, while some of the guidelines have ranges (e. g. 6 -12 months), these are not useful to the ordering physician or to an automated follow-up system Decided that radiologist must choose a single integer time interval for ALRT. When the guideline is a range, the radiologist can put the range in the text, but either use the minimum, maximum, or average of the range in the ALRT. Pilot will try just using the # of months (as opposed to allowing specifying # of weeks) 17
Follow-up Timeframes It was discussed that, while some of the guidelines have ranges (e. g. 6 -12 months), these are not useful to the ordering physician or to an automated follow-up system Decided that radiologist must choose a single integer time interval for ALRT. When the guideline is a range, the radiologist can put the range in the text, but either use the minimum, maximum, or average of the range in the ALRT. Pilot will try just using the # of months (as opposed to allowing specifying # of weeks) 17
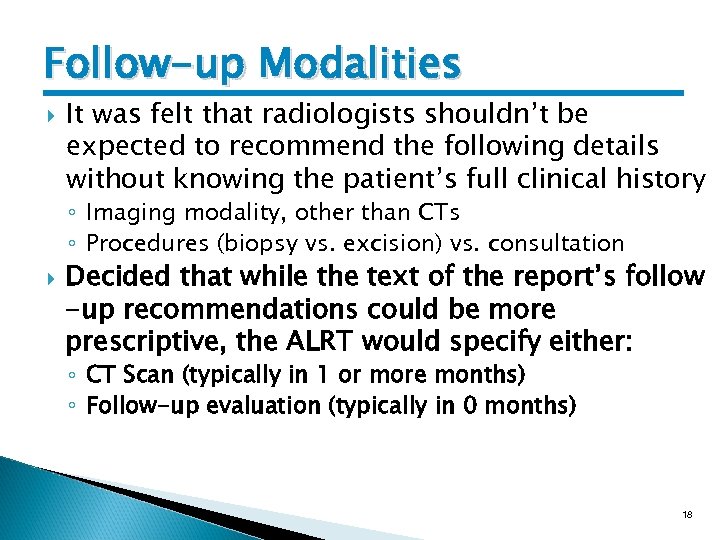 Follow-up Modalities It was felt that radiologists shouldn’t be expected to recommend the following details without knowing the patient’s full clinical history ◦ Imaging modality, other than CTs ◦ Procedures (biopsy vs. excision) vs. consultation Decided that while the text of the report’s follow -up recommendations could be more prescriptive, the ALRT would specify either: ◦ CT Scan (typically in 1 or more months) ◦ Follow-up evaluation (typically in 0 months) 18
Follow-up Modalities It was felt that radiologists shouldn’t be expected to recommend the following details without knowing the patient’s full clinical history ◦ Imaging modality, other than CTs ◦ Procedures (biopsy vs. excision) vs. consultation Decided that while the text of the report’s follow -up recommendations could be more prescriptive, the ALRT would specify either: ◦ CT Scan (typically in 1 or more months) ◦ Follow-up evaluation (typically in 0 months) 18
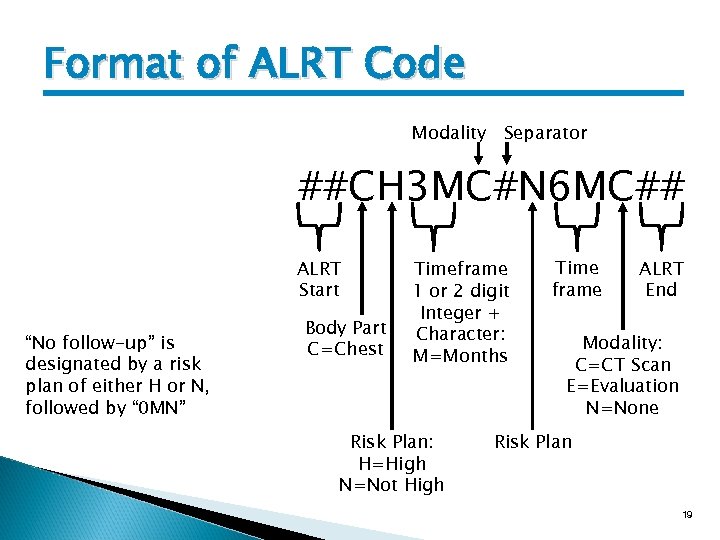 Format of ALRT Code Modality Separator ##CH 3 MC#N 6 MC## ALRT Start “No follow-up” is designated by a risk plan of either H or N, followed by “ 0 MN” Body Part C=Chest Timeframe 1 or 2 digit Integer + Character: M=Months Risk Plan: H=High N=Not High Time frame ALRT End Modality: C=CT Scan E=Evaluation N=None Risk Plan 19
Format of ALRT Code Modality Separator ##CH 3 MC#N 6 MC## ALRT Start “No follow-up” is designated by a risk plan of either H or N, followed by “ 0 MN” Body Part C=Chest Timeframe 1 or 2 digit Integer + Character: M=Months Risk Plan: H=High N=Not High Time frame ALRT End Modality: C=CT Scan E=Evaluation N=None Risk Plan 19
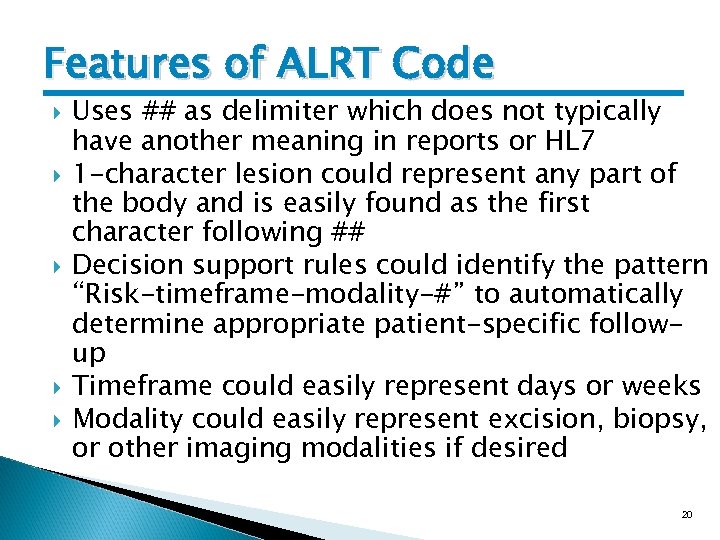 Features of ALRT Code Uses ## as delimiter which does not typically have another meaning in reports or HL 7 1 -character lesion could represent any part of the body and is easily found as the first character following ## Decision support rules could identify the pattern “Risk-timeframe-modality-#” to automatically determine appropriate patient-specific followup Timeframe could easily represent days or weeks Modality could easily represent excision, biopsy, or other imaging modalities if desired 20
Features of ALRT Code Uses ## as delimiter which does not typically have another meaning in reports or HL 7 1 -character lesion could represent any part of the body and is easily found as the first character following ## Decision support rules could identify the pattern “Risk-timeframe-modality-#” to automatically determine appropriate patient-specific followup Timeframe could easily represent days or weeks Modality could easily represent excision, biopsy, or other imaging modalities if desired 20
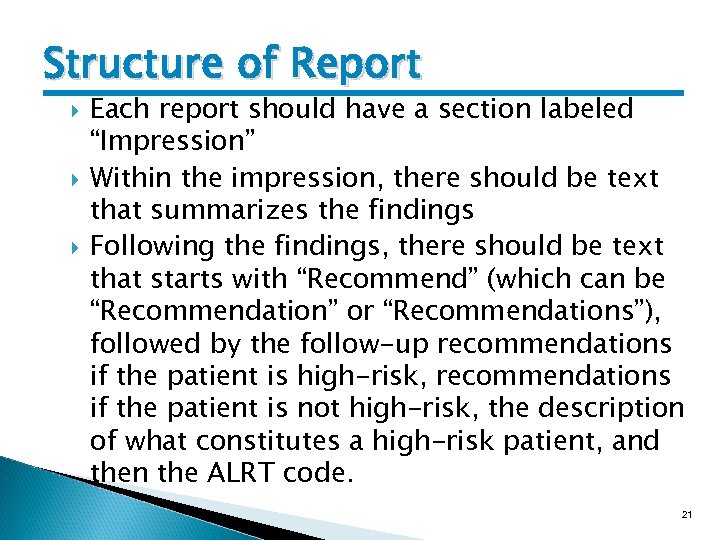 Structure of Report Each report should have a section labeled “Impression” Within the impression, there should be text that summarizes the findings Following the findings, there should be text that starts with “Recommend” (which can be “Recommendation” or “Recommendations”), followed by the follow-up recommendations if the patient is high-risk, recommendations if the patient is not high-risk, the description of what constitutes a high-risk patient, and then the ALRT code. 21
Structure of Report Each report should have a section labeled “Impression” Within the impression, there should be text that summarizes the findings Following the findings, there should be text that starts with “Recommend” (which can be “Recommendation” or “Recommendations”), followed by the follow-up recommendations if the patient is high-risk, recommendations if the patient is not high-risk, the description of what constitutes a high-risk patient, and then the ALRT code. 21
 Best Practices for Using ALRTs Report to ordering provider flagged to highlight abnormality Abnormal studies cc’d to PCP if not the ordering provider (particularly important in cases ordered by ED, surgeon, or hospitalist) Copies of abnormal studies automatically given to patient, for example, at time of hospital discharge and/or mailed to patient Abnormals cc’d to registries for tracking purposes Study rates of contacting patients for follow-up Study rates of obtaining follow-up per radiology recommendations 22
Best Practices for Using ALRTs Report to ordering provider flagged to highlight abnormality Abnormal studies cc’d to PCP if not the ordering provider (particularly important in cases ordered by ED, surgeon, or hospitalist) Copies of abnormal studies automatically given to patient, for example, at time of hospital discharge and/or mailed to patient Abnormals cc’d to registries for tracking purposes Study rates of contacting patients for follow-up Study rates of obtaining follow-up per radiology recommendations 22
 Next Steps Approval of this “minutes” presentation Pilot at: ◦ Lahey Hospital/Clinic ◦ Reliant Medical Group and St. Vincent Hospital If workable, the present to MA Radiological Society with recommendations to: ◦ Use ALRT codes in dictation macros for pulmonary lesions, including text that defines “high risk” ◦ Consider implementing one or more Best Practices 23
Next Steps Approval of this “minutes” presentation Pilot at: ◦ Lahey Hospital/Clinic ◦ Reliant Medical Group and St. Vincent Hospital If workable, the present to MA Radiological Society with recommendations to: ◦ Use ALRT codes in dictation macros for pulmonary lesions, including text that defines “high risk” ◦ Consider implementing one or more Best Practices 23
 Potential Future Actions Get statewide consensus on minimum lesion size that could warrant a follow-up Improved the conveyance of risk factors (and history) to the radiologist Create standardized letters to patients (similar to mammography letters) that explain findings, recommended follow-up, risks, benefits, and alternatives Share standard dictation macros for the various lesions 24
Potential Future Actions Get statewide consensus on minimum lesion size that could warrant a follow-up Improved the conveyance of risk factors (and history) to the radiologist Create standardized letters to patients (similar to mammography letters) that explain findings, recommended follow-up, risks, benefits, and alternatives Share standard dictation macros for the various lesions 24


