a38a5f58cd8671979883091f1bb0d3f4.ppt
- Количество слайдов: 31
 Action Learning Pilot Programme Project Khaedu Prince Mshiyeni Memorial Hospital - preliminary findings 6 October 2005 1
Action Learning Pilot Programme Project Khaedu Prince Mshiyeni Memorial Hospital - preliminary findings 6 October 2005 1
 Agenda • Executive summary • Situation • Complications • Some suggestions 2
Agenda • Executive summary • Situation • Complications • Some suggestions 2
 Executive summary and key message Absolute shortage of key resources and poor physical layout of the hospital complicate opportunities for meaningful process improvement, but some opportunities do exist for improvement at macro level (reducing overall number of patients) and micro level (patient administration) PMMH is managing hundreds of thousands of patients per annum under very difficult conditions – patients are happy with your treatment; the remaining challenge is wait times and congestion 3
Executive summary and key message Absolute shortage of key resources and poor physical layout of the hospital complicate opportunities for meaningful process improvement, but some opportunities do exist for improvement at macro level (reducing overall number of patients) and micro level (patient administration) PMMH is managing hundreds of thousands of patients per annum under very difficult conditions – patients are happy with your treatment; the remaining challenge is wait times and congestion 3
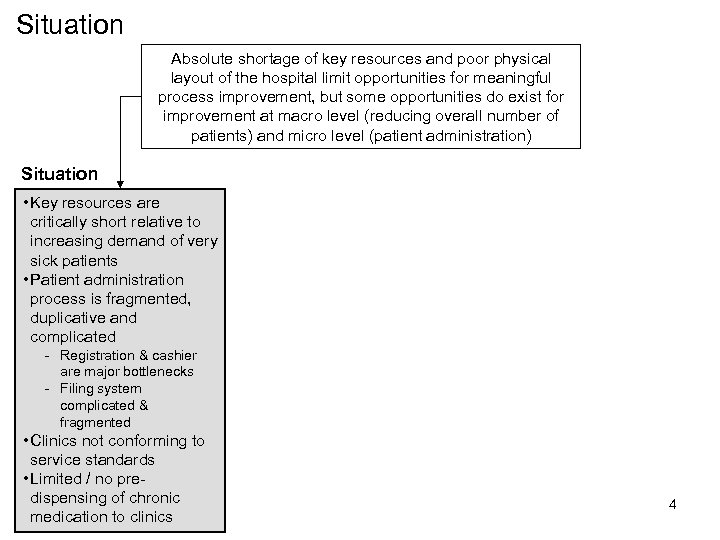 Situation Absolute shortage of key resources and poor physical layout of the hospital limit opportunities for meaningful process improvement, but some opportunities do exist for improvement at macro level (reducing overall number of patients) and micro level (patient administration) Situation • Key resources are critically short relative to increasing demand of very sick patients • Patient administration process is fragmented, duplicative and complicated - Registration & cashier are major bottlenecks - Filing system complicated & fragmented • Clinics not conforming to service standards • Limited / no predispensing of chronic medication to clinics 4
Situation Absolute shortage of key resources and poor physical layout of the hospital limit opportunities for meaningful process improvement, but some opportunities do exist for improvement at macro level (reducing overall number of patients) and micro level (patient administration) Situation • Key resources are critically short relative to increasing demand of very sick patients • Patient administration process is fragmented, duplicative and complicated - Registration & cashier are major bottlenecks - Filing system complicated & fragmented • Clinics not conforming to service standards • Limited / no predispensing of chronic medication to clinics 4
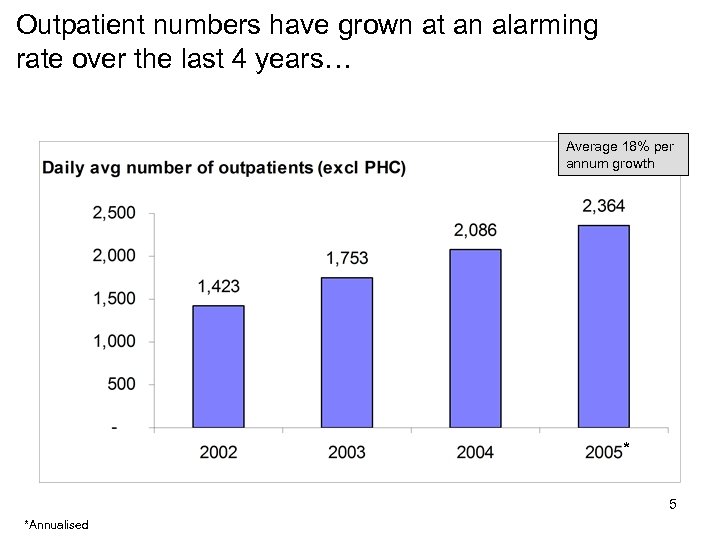 Outpatient numbers have grown at an alarming rate over the last 4 years… Average 18% per annum growth * 5 *Annualised
Outpatient numbers have grown at an alarming rate over the last 4 years… Average 18% per annum growth * 5 *Annualised
 …which has impacted service delivery 6
…which has impacted service delivery 6
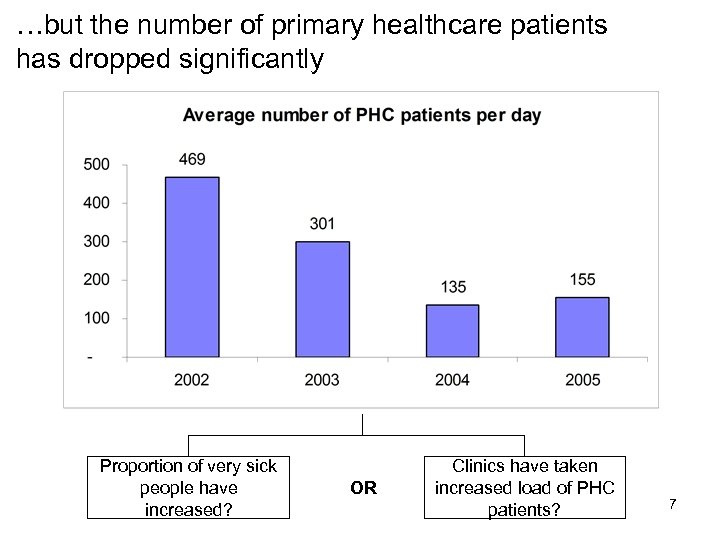 …but the number of primary healthcare patients has dropped significantly Proportion of very sick people have increased? OR Clinics have taken increased load of PHC patients? 7
…but the number of primary healthcare patients has dropped significantly Proportion of very sick people have increased? OR Clinics have taken increased load of PHC patients? 7
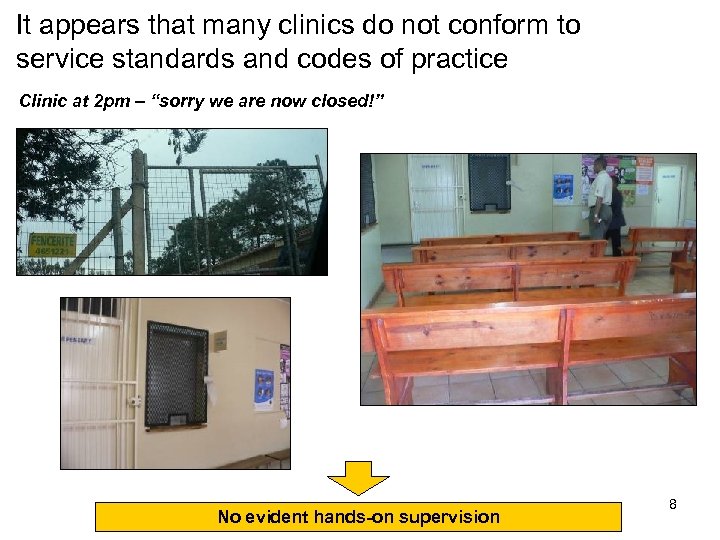 It appears that many clinics do not conform to service standards and codes of practice Clinic at 2 pm – “sorry we are now closed!” No evident hands-on supervision 8
It appears that many clinics do not conform to service standards and codes of practice Clinic at 2 pm – “sorry we are now closed!” No evident hands-on supervision 8
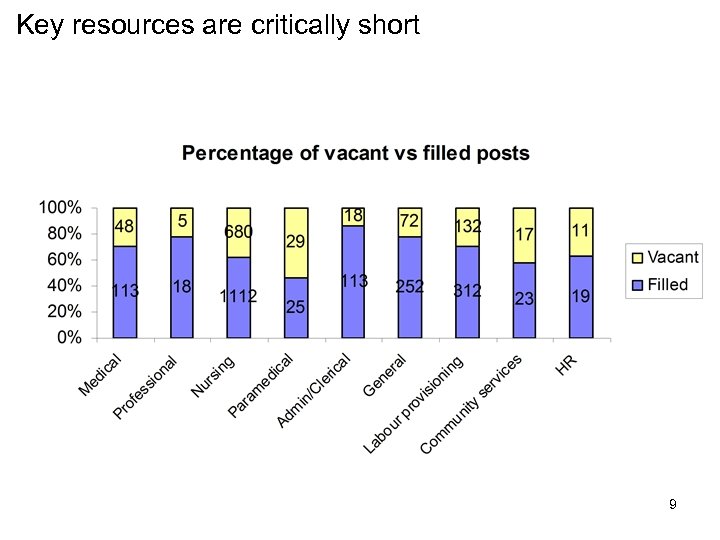 Key resources are critically short 9
Key resources are critically short 9
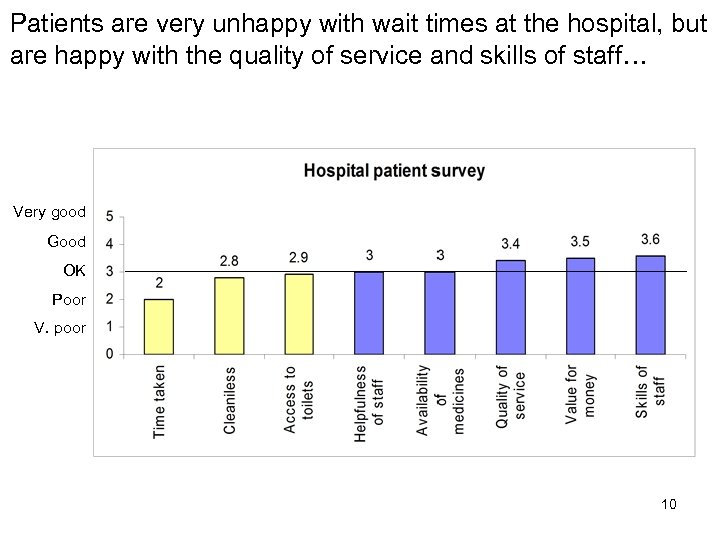 Patients are very unhappy with wait times at the hospital, but are happy with the quality of service and skills of staff… Very good Good OK Poor V. poor 10
Patients are very unhappy with wait times at the hospital, but are happy with the quality of service and skills of staff… Very good Good OK Poor V. poor 10
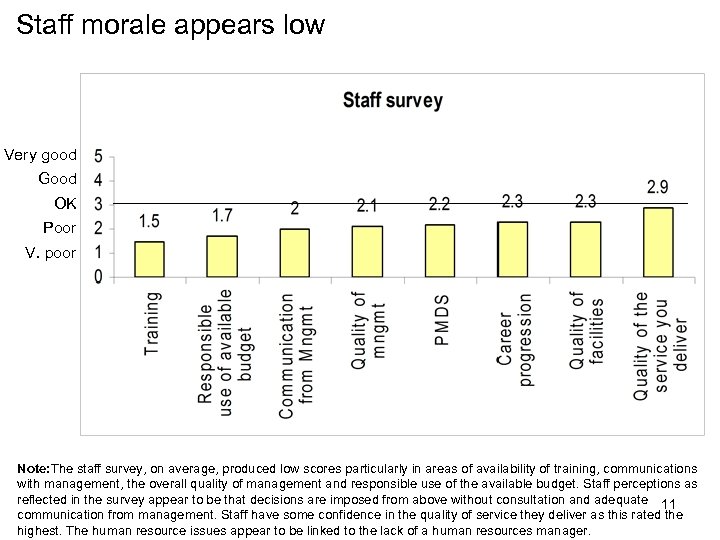 Staff morale appears low Very good Good OK Poor V. poor Note: The staff survey, on average, produced low scores particularly in areas of availability of training, communications with management, the overall quality of management and responsible use of the available budget. Staff perceptions as reflected in the survey appear to be that decisions are imposed from above without consultation and adequate 11 communication from management. Staff have some confidence in the quality of service they deliver as this rated the highest. The human resource issues appear to be linked to the lack of a human resources manager.
Staff morale appears low Very good Good OK Poor V. poor Note: The staff survey, on average, produced low scores particularly in areas of availability of training, communications with management, the overall quality of management and responsible use of the available budget. Staff perceptions as reflected in the survey appear to be that decisions are imposed from above without consultation and adequate 11 communication from management. Staff have some confidence in the quality of service they deliver as this rated the highest. The human resource issues appear to be linked to the lack of a human resources manager.
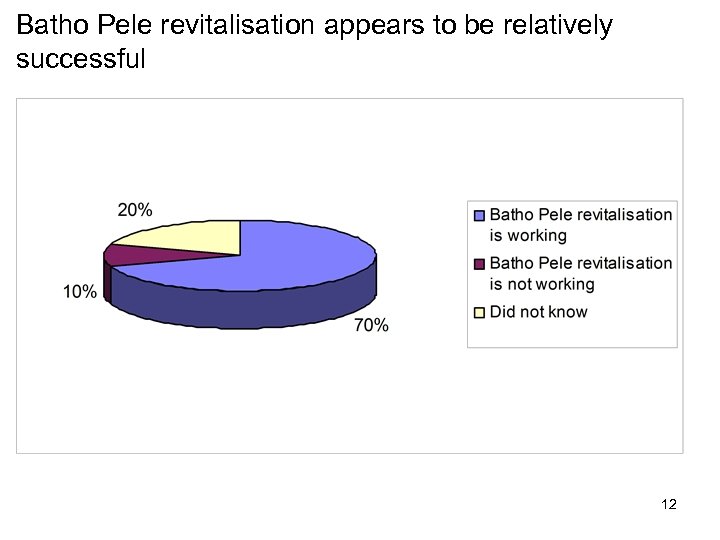 Batho Pele revitalisation appears to be relatively successful 12
Batho Pele revitalisation appears to be relatively successful 12
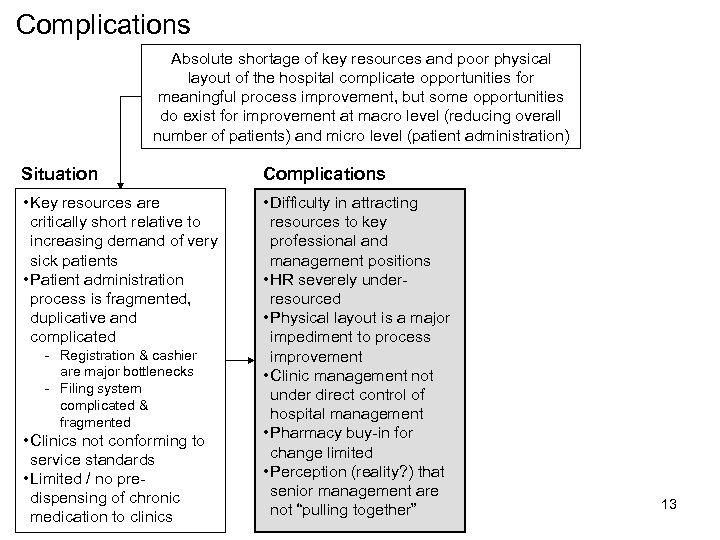 Complications Absolute shortage of key resources and poor physical layout of the hospital complicate opportunities for meaningful process improvement, but some opportunities do exist for improvement at macro level (reducing overall number of patients) and micro level (patient administration) Situation Complications • Key resources are critically short relative to increasing demand of very sick patients • Patient administration process is fragmented, duplicative and complicated • Difficulty in attracting resources to key professional and management positions • HR severely underresourced • Physical layout is a major impediment to process improvement • Clinic management not under direct control of hospital management • Pharmacy buy-in for change limited • Perception (reality? ) that senior management are not “pulling together” - Registration & cashier are major bottlenecks - Filing system complicated & fragmented • Clinics not conforming to service standards • Limited / no predispensing of chronic medication to clinics 13
Complications Absolute shortage of key resources and poor physical layout of the hospital complicate opportunities for meaningful process improvement, but some opportunities do exist for improvement at macro level (reducing overall number of patients) and micro level (patient administration) Situation Complications • Key resources are critically short relative to increasing demand of very sick patients • Patient administration process is fragmented, duplicative and complicated • Difficulty in attracting resources to key professional and management positions • HR severely underresourced • Physical layout is a major impediment to process improvement • Clinic management not under direct control of hospital management • Pharmacy buy-in for change limited • Perception (reality? ) that senior management are not “pulling together” - Registration & cashier are major bottlenecks - Filing system complicated & fragmented • Clinics not conforming to service standards • Limited / no predispensing of chronic medication to clinics 13
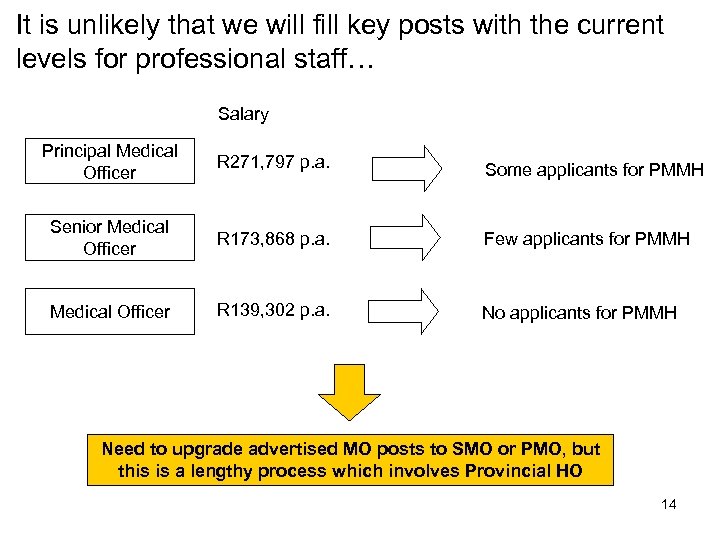 It is unlikely that we will fill key posts with the current levels for professional staff… Salary Principal Medical Officer R 271, 797 p. a. Some applicants for PMMH Senior Medical Officer R 173, 868 p. a. Few applicants for PMMH Medical Officer R 139, 302 p. a. No applicants for PMMH Need to upgrade advertised MO posts to SMO or PMO, but this is a lengthy process which involves Provincial HO 14
It is unlikely that we will fill key posts with the current levels for professional staff… Salary Principal Medical Officer R 271, 797 p. a. Some applicants for PMMH Senior Medical Officer R 173, 868 p. a. Few applicants for PMMH Medical Officer R 139, 302 p. a. No applicants for PMMH Need to upgrade advertised MO posts to SMO or PMO, but this is a lengthy process which involves Provincial HO 14
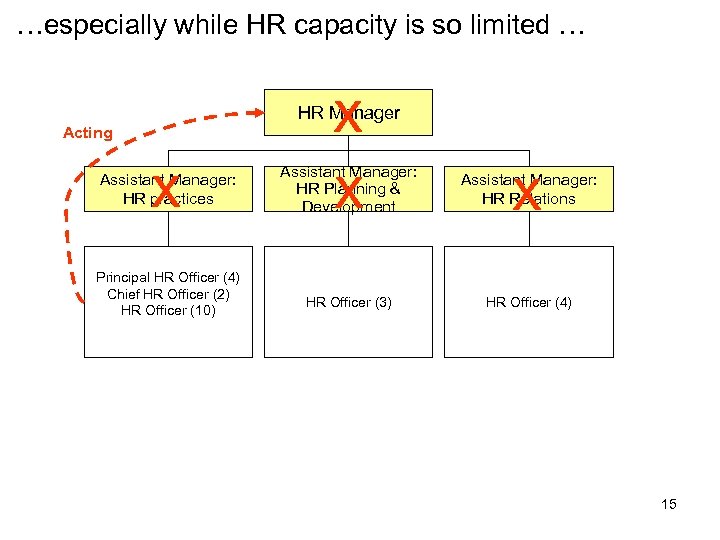 …especially while HR capacity is so limited … x x HR Manager Acting x Assistant Manager: HR practices Principal HR Officer (4) Chief HR Officer (2) HR Officer (10) x Assistant Manager: HR Planning & Development Assistant Manager: HR Relations HR Officer (3) HR Officer (4) 15
…especially while HR capacity is so limited … x x HR Manager Acting x Assistant Manager: HR practices Principal HR Officer (4) Chief HR Officer (2) HR Officer (10) x Assistant Manager: HR Planning & Development Assistant Manager: HR Relations HR Officer (3) HR Officer (4) 15
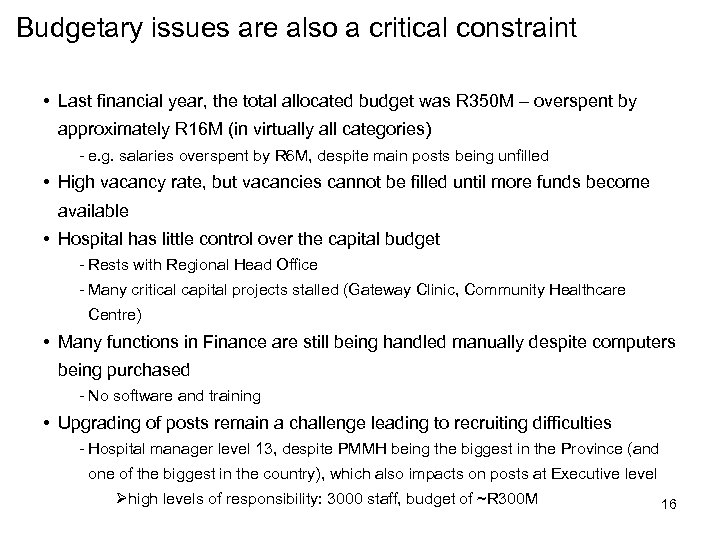 Budgetary issues are also a critical constraint • Last financial year, the total allocated budget was R 350 M – overspent by approximately R 16 M (in virtually all categories) - e. g. salaries overspent by R 6 M, despite main posts being unfilled • High vacancy rate, but vacancies cannot be filled until more funds become available • Hospital has little control over the capital budget - Rests with Regional Head Office - Many critical capital projects stalled (Gateway Clinic, Community Healthcare Centre) • Many functions in Finance are still being handled manually despite computers being purchased - No software and training • Upgrading of posts remain a challenge leading to recruiting difficulties - Hospital manager level 13, despite PMMH being the biggest in the Province (and one of the biggest in the country), which also impacts on posts at Executive level Øhigh levels of responsibility: 3000 staff, budget of ~R 300 M 16
Budgetary issues are also a critical constraint • Last financial year, the total allocated budget was R 350 M – overspent by approximately R 16 M (in virtually all categories) - e. g. salaries overspent by R 6 M, despite main posts being unfilled • High vacancy rate, but vacancies cannot be filled until more funds become available • Hospital has little control over the capital budget - Rests with Regional Head Office - Many critical capital projects stalled (Gateway Clinic, Community Healthcare Centre) • Many functions in Finance are still being handled manually despite computers being purchased - No software and training • Upgrading of posts remain a challenge leading to recruiting difficulties - Hospital manager level 13, despite PMMH being the biggest in the Province (and one of the biggest in the country), which also impacts on posts at Executive level Øhigh levels of responsibility: 3000 staff, budget of ~R 300 M 16
 Staff perceive that senior management do not work together as a team • One of the major issues highlighted in the discussion with Labour was perceived conflicts in management that is impeding the effective running of the institution • The institution is perceived as having a “pariah” status as compared to other institutions as a result of its problems. • Labour also pointed to staff shortages and the increased workload it places on existing staff • Labour also identified a lack of availability of training and career progression for nurses at the institution • Problems in human resources have been attributed to the lack of a human resources manager. 17
Staff perceive that senior management do not work together as a team • One of the major issues highlighted in the discussion with Labour was perceived conflicts in management that is impeding the effective running of the institution • The institution is perceived as having a “pariah” status as compared to other institutions as a result of its problems. • Labour also pointed to staff shortages and the increased workload it places on existing staff • Labour also identified a lack of availability of training and career progression for nurses at the institution • Problems in human resources have been attributed to the lack of a human resources manager. 17
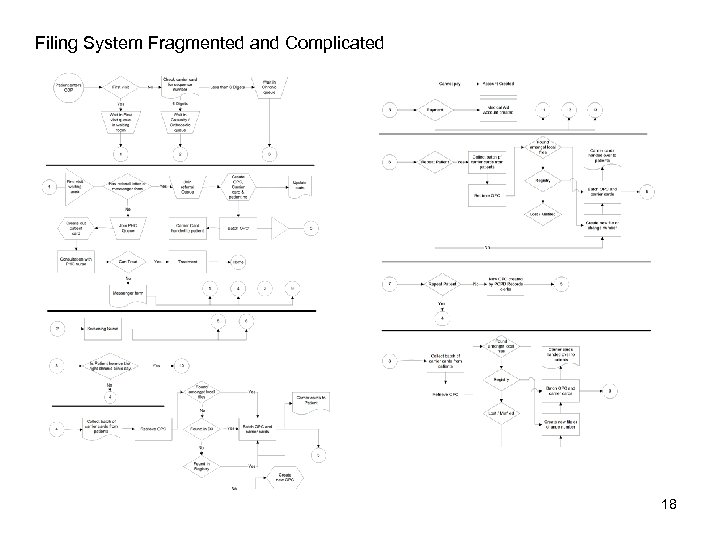 Filing System Fragmented and Complicated 18
Filing System Fragmented and Complicated 18
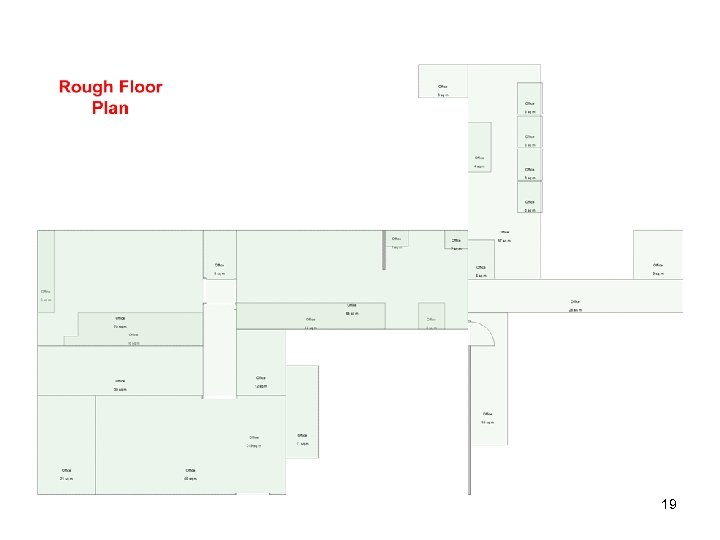 19
19
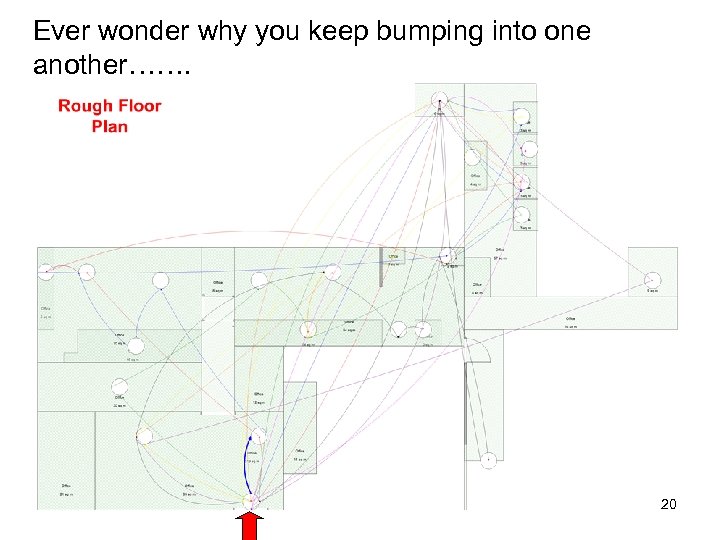 Ever wonder why you keep bumping into one another……. 20
Ever wonder why you keep bumping into one another……. 20
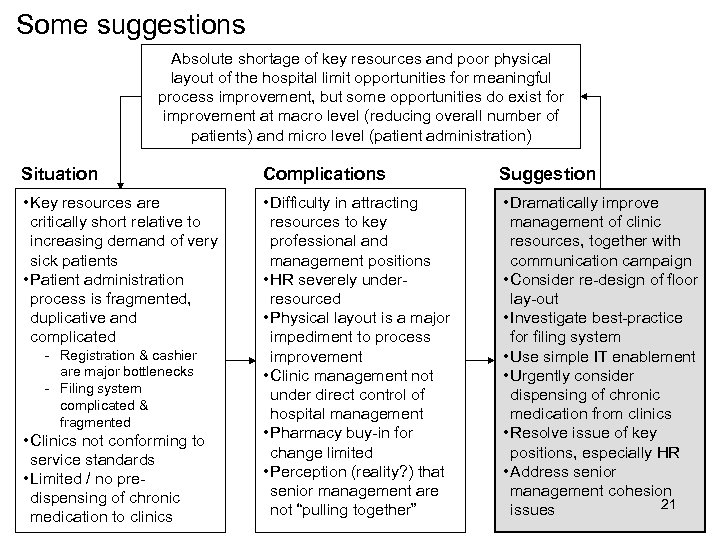 Some suggestions Absolute shortage of key resources and poor physical layout of the hospital limit opportunities for meaningful process improvement, but some opportunities do exist for improvement at macro level (reducing overall number of patients) and micro level (patient administration) Situation Complications Suggestion • Key resources are critically short relative to increasing demand of very sick patients • Patient administration process is fragmented, duplicative and complicated • Difficulty in attracting resources to key professional and management positions • HR severely underresourced • Physical layout is a major impediment to process improvement • Clinic management not under direct control of hospital management • Pharmacy buy-in for change limited • Perception (reality? ) that senior management are not “pulling together” • Dramatically improve management of clinic resources, together with communication campaign • Consider re-design of floor lay-out • Investigate best-practice for filing system • Use simple IT enablement • Urgently consider dispensing of chronic medication from clinics • Resolve issue of key positions, especially HR • Address senior management cohesion 21 issues - Registration & cashier are major bottlenecks - Filing system complicated & fragmented • Clinics not conforming to service standards • Limited / no predispensing of chronic medication to clinics
Some suggestions Absolute shortage of key resources and poor physical layout of the hospital limit opportunities for meaningful process improvement, but some opportunities do exist for improvement at macro level (reducing overall number of patients) and micro level (patient administration) Situation Complications Suggestion • Key resources are critically short relative to increasing demand of very sick patients • Patient administration process is fragmented, duplicative and complicated • Difficulty in attracting resources to key professional and management positions • HR severely underresourced • Physical layout is a major impediment to process improvement • Clinic management not under direct control of hospital management • Pharmacy buy-in for change limited • Perception (reality? ) that senior management are not “pulling together” • Dramatically improve management of clinic resources, together with communication campaign • Consider re-design of floor lay-out • Investigate best-practice for filing system • Use simple IT enablement • Urgently consider dispensing of chronic medication from clinics • Resolve issue of key positions, especially HR • Address senior management cohesion 21 issues - Registration & cashier are major bottlenecks - Filing system complicated & fragmented • Clinics not conforming to service standards • Limited / no predispensing of chronic medication to clinics
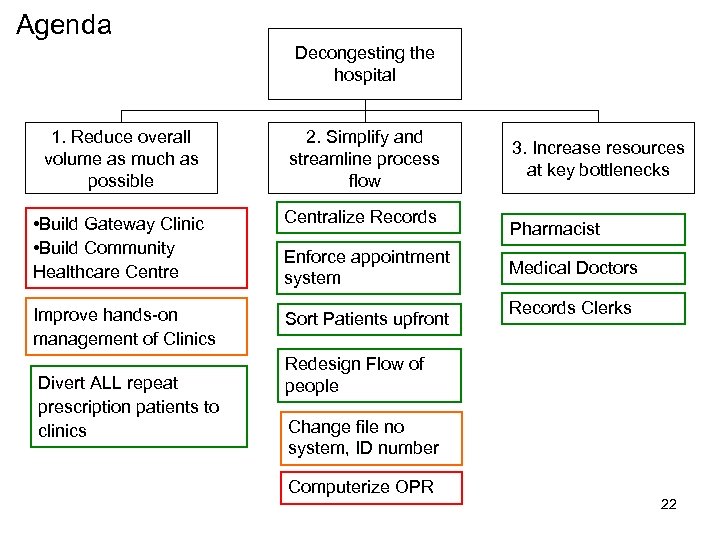 Agenda Decongesting the hospital 1. Reduce overall volume as much as possible 2. Simplify and streamline process flow • Build Gateway Clinic • Build Community Healthcare Centralize Records Improve hands-on management of Clinics Sort Patients upfront Divert ALL repeat prescription patients to clinics Enforce appointment system 3. Increase resources at key bottlenecks Pharmacist Medical Doctors Records Clerks Redesign Flow of people Change file no system, ID number Computerize OPR 22
Agenda Decongesting the hospital 1. Reduce overall volume as much as possible 2. Simplify and streamline process flow • Build Gateway Clinic • Build Community Healthcare Centralize Records Improve hands-on management of Clinics Sort Patients upfront Divert ALL repeat prescription patients to clinics Enforce appointment system 3. Increase resources at key bottlenecks Pharmacist Medical Doctors Records Clerks Redesign Flow of people Change file no system, ID number Computerize OPR 22
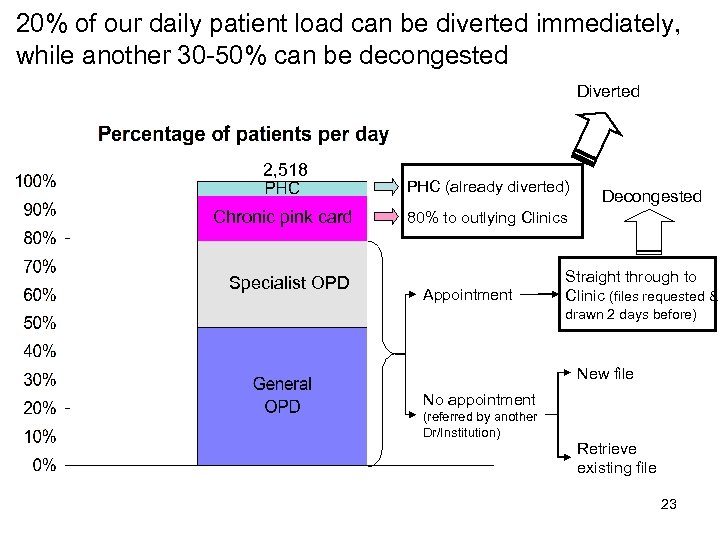 20% of our daily patient load can be diverted immediately, while another 30 -50% can be decongested Diverted 2, 518 Chronic pink card Specialist OPD PHC (already diverted) Decongested 80% to outlying Clinics Appointment Straight through to Clinic (files requested & drawn 2 days before) New file No appointment (referred by another Dr/Institution) Retrieve existing file 23
20% of our daily patient load can be diverted immediately, while another 30 -50% can be decongested Diverted 2, 518 Chronic pink card Specialist OPD PHC (already diverted) Decongested 80% to outlying Clinics Appointment Straight through to Clinic (files requested & drawn 2 days before) New file No appointment (referred by another Dr/Institution) Retrieve existing file 23
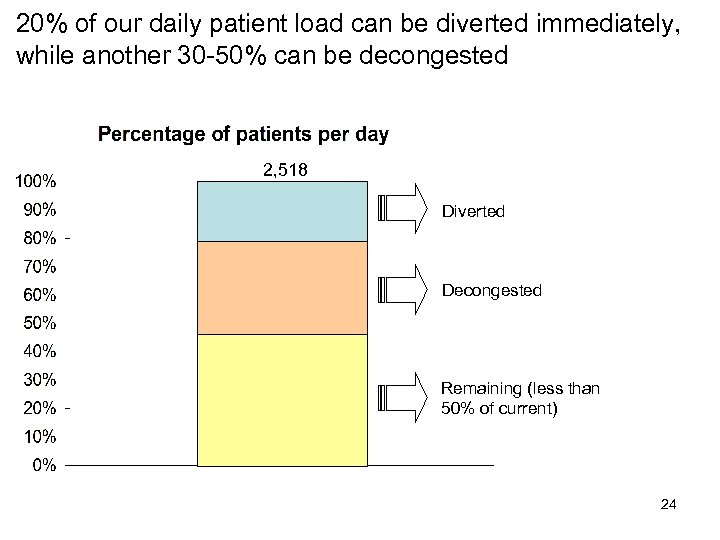 20% of our daily patient load can be diverted immediately, while another 30 -50% can be decongested 2, 518 Chronic pink card Specialist OPD Diverted Decongested Remaining (less than 50% of current) 24
20% of our daily patient load can be diverted immediately, while another 30 -50% can be decongested 2, 518 Chronic pink card Specialist OPD Diverted Decongested Remaining (less than 50% of current) 24
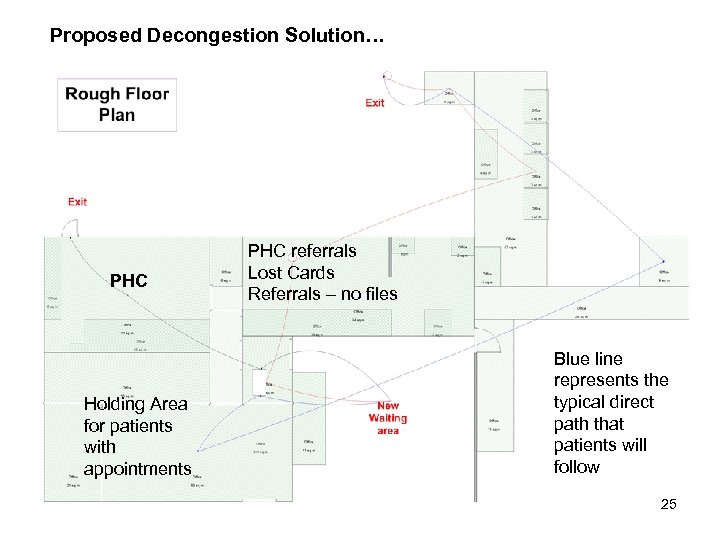 Proposed Decongestion Solution… PHC Holding Area for patients with appointments PHC referrals Lost Cards Referrals – no files Blue line represents the typical direct path that patients will follow 25
Proposed Decongestion Solution… PHC Holding Area for patients with appointments PHC referrals Lost Cards Referrals – no files Blue line represents the typical direct path that patients will follow 25
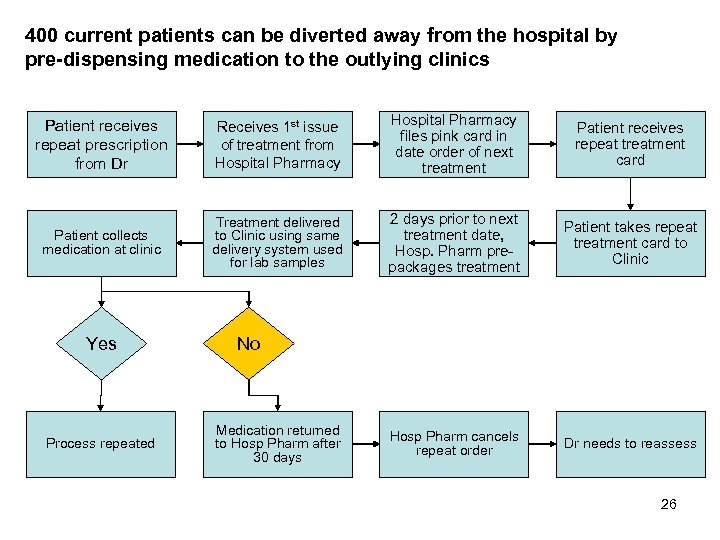 400 current patients can be diverted away from the hospital by pre-dispensing medication to the outlying clinics Patient receives repeat prescription from Dr Receives 1 st issue of treatment from Hospital Pharmacy files pink card in date order of next treatment Patient receives repeat treatment card Patient collects medication at clinic Treatment delivered to Clinic using same delivery system used for lab samples 2 days prior to next treatment date, Hosp. Pharm prepackages treatment Patient takes repeat treatment card to Clinic Hosp Pharm cancels repeat order Dr needs to reassess Yes Process repeated No Medication returned to Hosp Pharm after 30 days 26
400 current patients can be diverted away from the hospital by pre-dispensing medication to the outlying clinics Patient receives repeat prescription from Dr Receives 1 st issue of treatment from Hospital Pharmacy files pink card in date order of next treatment Patient receives repeat treatment card Patient collects medication at clinic Treatment delivered to Clinic using same delivery system used for lab samples 2 days prior to next treatment date, Hosp. Pharm prepackages treatment Patient takes repeat treatment card to Clinic Hosp Pharm cancels repeat order Dr needs to reassess Yes Process repeated No Medication returned to Hosp Pharm after 30 days 26
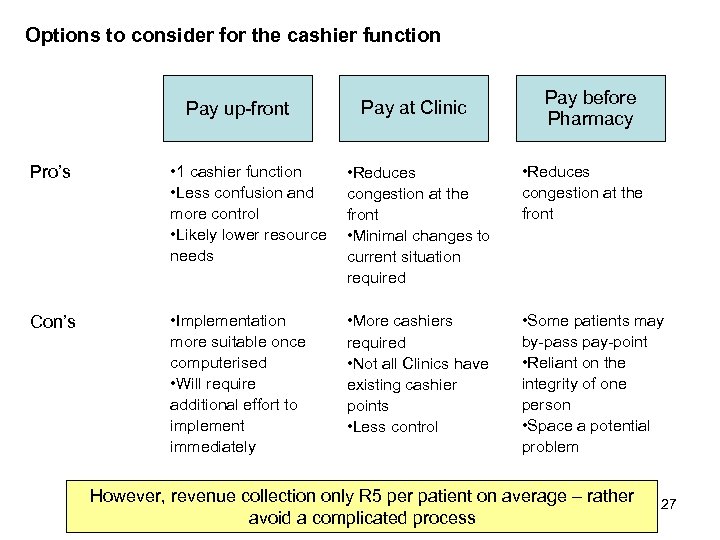 Options to consider for the cashier function Pay up-front Pay at Clinic Pay before Pharmacy Pro’s • 1 cashier function • Less confusion and more control • Likely lower resource needs • Reduces congestion at the front • Minimal changes to current situation required • Reduces congestion at the front Con’s • Implementation more suitable once computerised • Will require additional effort to implement immediately • More cashiers required • Not all Clinics have existing cashier points • Less control • Some patients may by-pass pay-point • Reliant on the integrity of one person • Space a potential problem However, revenue collection only R 5 per patient on average – rather avoid a complicated process 27
Options to consider for the cashier function Pay up-front Pay at Clinic Pay before Pharmacy Pro’s • 1 cashier function • Less confusion and more control • Likely lower resource needs • Reduces congestion at the front • Minimal changes to current situation required • Reduces congestion at the front Con’s • Implementation more suitable once computerised • Will require additional effort to implement immediately • More cashiers required • Not all Clinics have existing cashier points • Less control • Some patients may by-pass pay-point • Reliant on the integrity of one person • Space a potential problem However, revenue collection only R 5 per patient on average – rather avoid a complicated process 27
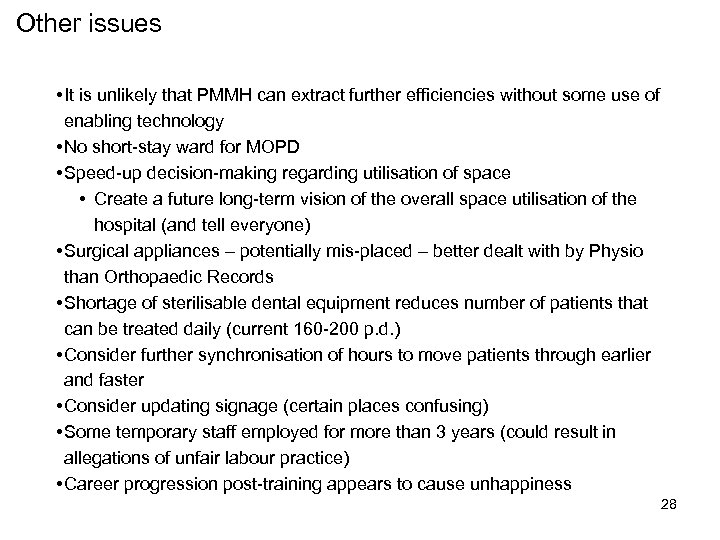 Other issues • It is unlikely that PMMH can extract further efficiencies without some use of enabling technology • No short-stay ward for MOPD • Speed-up decision-making regarding utilisation of space • Create a future long-term vision of the overall space utilisation of the hospital (and tell everyone) • Surgical appliances – potentially mis-placed – better dealt with by Physio than Orthopaedic Records • Shortage of sterilisable dental equipment reduces number of patients that can be treated daily (current 160 -200 p. d. ) • Consider further synchronisation of hours to move patients through earlier and faster • Consider updating signage (certain places confusing) • Some temporary staff employed for more than 3 years (could result in allegations of unfair labour practice) • Career progression post-training appears to cause unhappiness 28
Other issues • It is unlikely that PMMH can extract further efficiencies without some use of enabling technology • No short-stay ward for MOPD • Speed-up decision-making regarding utilisation of space • Create a future long-term vision of the overall space utilisation of the hospital (and tell everyone) • Surgical appliances – potentially mis-placed – better dealt with by Physio than Orthopaedic Records • Shortage of sterilisable dental equipment reduces number of patients that can be treated daily (current 160 -200 p. d. ) • Consider further synchronisation of hours to move patients through earlier and faster • Consider updating signage (certain places confusing) • Some temporary staff employed for more than 3 years (could result in allegations of unfair labour practice) • Career progression post-training appears to cause unhappiness 28
 Backup 29
Backup 29
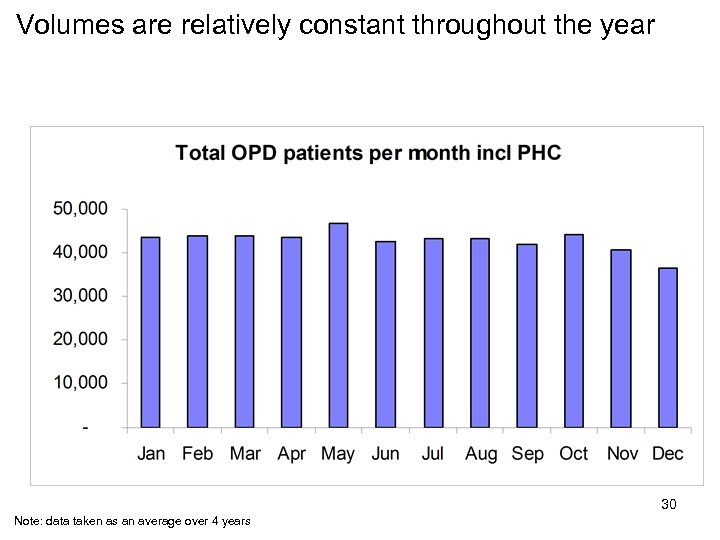 Volumes are relatively constant throughout the year 30 Note: data taken as an average over 4 years
Volumes are relatively constant throughout the year 30 Note: data taken as an average over 4 years
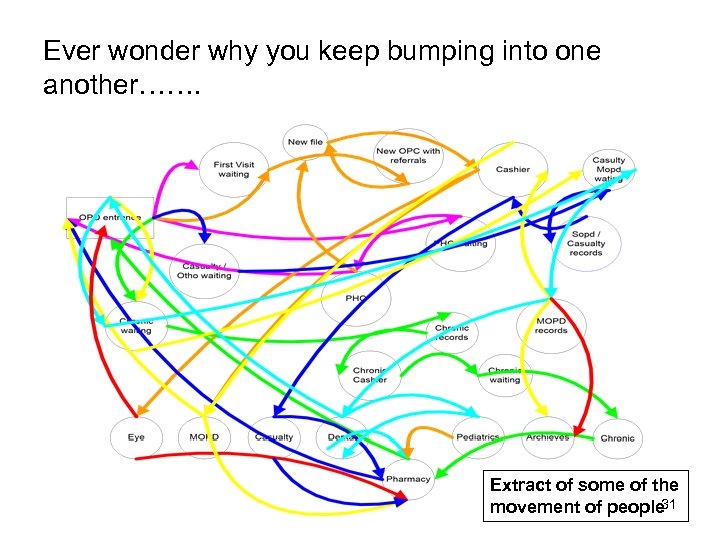 Ever wonder why you keep bumping into one another……. Extract of some of the 31 movement of people
Ever wonder why you keep bumping into one another……. Extract of some of the 31 movement of people


