5f03f5e6188816a3650501ddaeeed4d9.ppt
- Количество слайдов: 177

ACS MSN Diana Blum Metropolitan Community College 1
Statistics More than 71 million Americans have cardiovascular disease 2

review 3
4
5
What is cardiac output? What is Stroke Volume? What is normal HR? Why are these important? 6
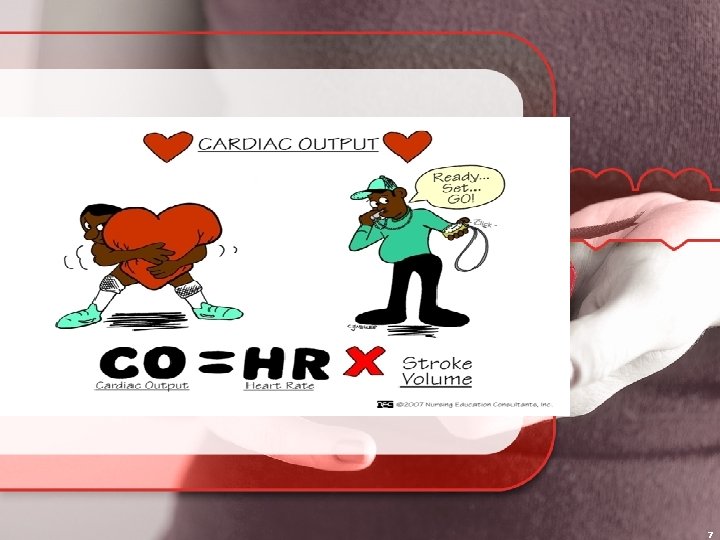
7
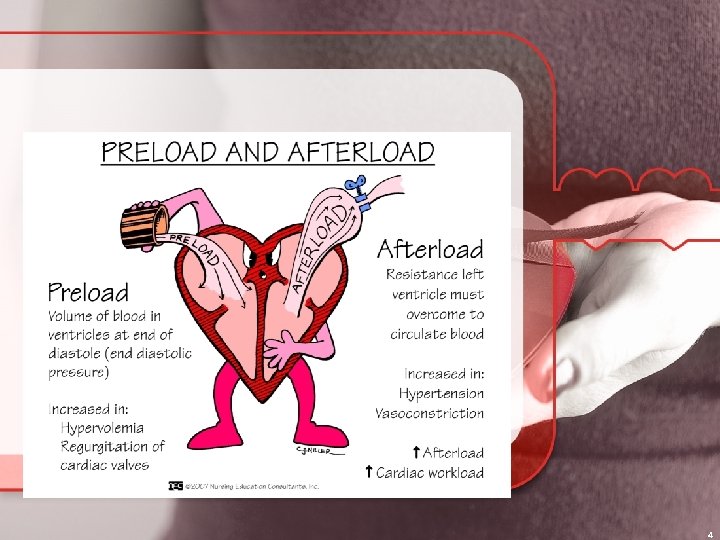
Factors affecting Stroke Volume Preload: the amount of blood remaining in the ventricles at the end of diastole or the pressure generated at the end of diastole Contractility: is the ability of the cardiac muscle fibers to shorten and produce a muscle contraction. (Inotropic, + or -) Afterload: amount of pressure the Ventricle must overcome to eject blood volume out 8
9
Autonomic Nervous System Built in control center of the body Regulates functions not under conscious control Blood vessels innervated by sympathetic system Fight or flight Nerve endings are adrenergic and nuerotransmitter is norepinephrine Increases HR and BP Parasympathetic is responsible for rest and digest Cholinergics are the nerve endings and acetylcholine is the neurotransmitter Decreases HR and BP Parasympathetic and sympathetic innervates heart 10
Exam General appearance Mentation Color Neck Veins Palpations Turgor Cap Refill Pulses Auscultation 11
Abnormal Heart tones S 3= sounds like kentucky (ventricular) S 4= sounds like tennesee (atrial) Gallop=when s 3 and 4 heard Rub= related to inflammation high pitched sweaky yet muffled like sandpaper Murmur=vibrati ons from turbulent flow aka bruit 12
CAD Arteries have 3 layers: tunica intima, tunica media, and tunica adventitia Disease process that occurs over time Starts in infancy Risk factors: age gender diet sedentary life smoking Atherosclerosis affects medium arteries that feed heart brain and kidneys as well as aorta 13
Arteriosclerosis: thickening and calcification of artery Atherosclerosis: component of arteriosclerosis that causes reduced myocardial blood flow Plaque (cholesterol, lipid, cellular debris) 3 stages of plaque growth: 1: yellow lesion (fatty streak)in intimal layer 2: plaque matures creating a lipid core with fibrous cap (white in appearance) and are mostly in bifurcated arteries 3: well established fibrous cap/lipid core possible rupture 14
s/s of CAD Angina which results from a lack of 0 xygen to the heart muscle 4 Es=exercise, eating, emotion, exposure to cold Weakness, diaphoresis, SOB N/V 15
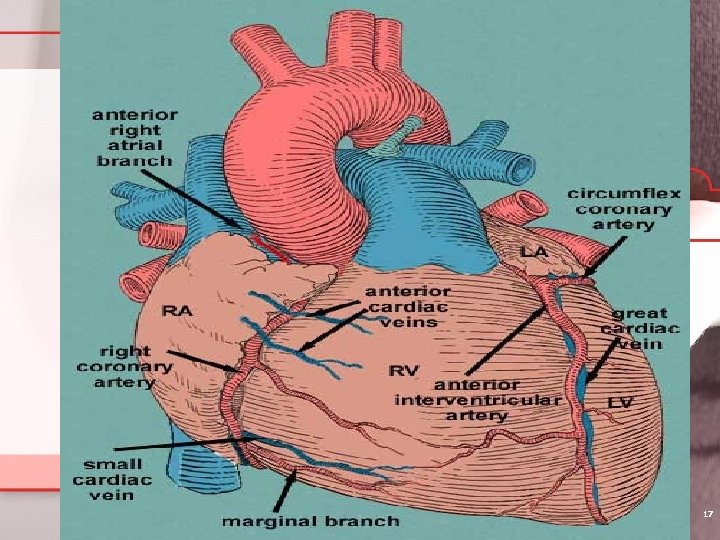
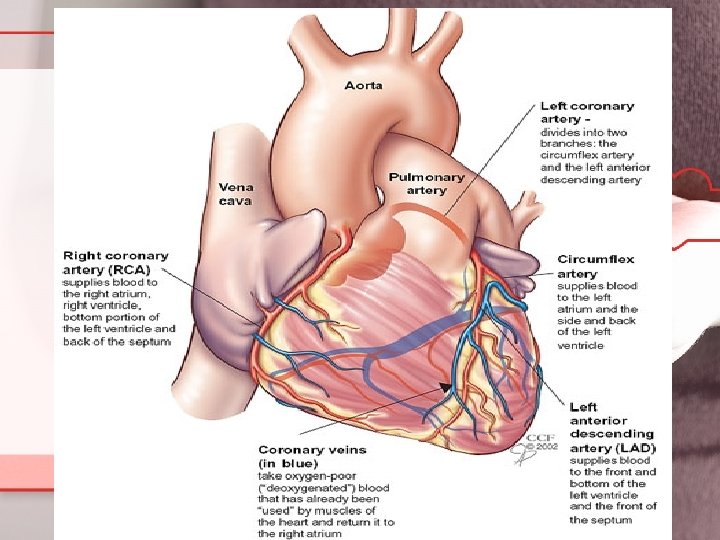
Coronary Arteries 2 branches off Aorta: Supplies posterior & inferior myocardium: 1. Right (Longest) coronary artery *occlusion results in inferior MI (30% of inferior MI’s include right ventricular infarction) *lower mortality than anterior MI *more mild AV node dysrhymias (first & second degree blocks) SYMPTOMS OF INFERIOR MI: - hypotension from a decrease in preload available to the LV due to ↓’d RV emptying 16
17
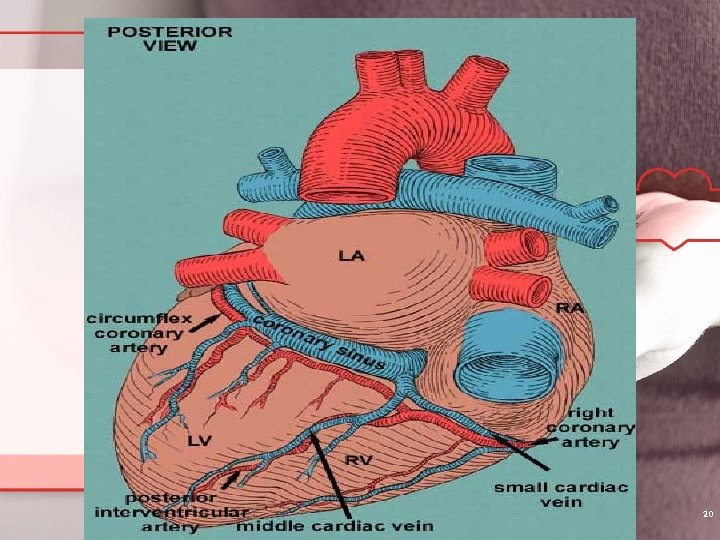
2 branches off the right coronary artery: a. Right marginal artery: b. Posterior descending artery: supplies blood to right atrium, right ventricle, bottom portion of both ventricles and back of septum 18
2. Left coronary artery begins out of Left side of ascending aorta and divides into the: left anterior descending artery(LAD) = supplies anterior and bottom of Left vent and front of the septum most involved with occlusions Blockage here results in anterior MI which has higher mortality rate AND more serious dysrhythmias !!!!! may include 2 nd & 3 rd degree blocks diminished ejection fraction & symptoms of heart failure !!!!! When > 40% of left vent. Is damaged mortality is extremely high circumflex= supplies the left atrium & back of left vent 19
20
Types of Chest Pain: the myocardial demand for oxygen exceeds the ability of the coronary vasculature to supply it. 1. Stable Angina: - no or minimal myocardial injury - collateral circulation develops - pain begins with exertion or stress - pain relieved with rest - pain lasts less than 20 minutes - relieved by NTG (may take SL up to 3 times every 5 minutes) If not relieved after these 3 doses, pt may be infarcting -ST segment depression with pain then returns to normal with pain subsides 22
Precautions with Nitrates and Viagra use: - reports of sudden death, dramatic drop in blood pressure, and further compromising restricted coronary arterial perfusion 23
What can cause angina? ? -reduced blood flow = reduced Hgb, or smoking -low oxygen content - excessive O 2 demand relative to perfusion =hypertension, exercise, metabolic rate -atherosclerosis -valvular dysfunction -hypotension -coronary vasospasm 24
Angina S/S - burning, squeezing “tight band” - heaviness, pressure in lower sternum - may radiate to neck, jaws, shoulders, arms, stomach OTHER symptoms specific to African. American & women: -fatigue, SOB, indigestion, shoulder/ back discomfort 25
Goal in treatment of Angina: dilate vessels, O 2 availability, ↓ O 2 demand Nitroglycerin Change lifestyle IF INCREASING in freq & intensity may need stress testing, cardiac cath beta blockers angioplasty or CABG to risk of MI 26
Angina or MI Angina without MI} often relieved with rest and NTG Angina with MI } may be relieved with rest, NTG, 02, MS, rescue angioplasty, etc. Think MONA Morphine Oxygen Nitroglycerin Aspirin http: //www. youtube. com/watch? v=4 Gl. Qm. Tl. P 2 j. E&feat ure=related http: //www. doctorsecrets. com/yourmedicine/heart-attack-cause-symptomstreatment. html 27
28
2. Unstable Angina: - pain resolves with NTG - similar to stable angina BUT angina occurs more freq with less exertion - often begins at rest with increasing severity - normal cardiac enzymes - ST depression with prolonged CP 30
Unstable Angina (continued) Platelet activation = treat with GP IIb/IIIa inhibitors examples: Abciximab (Reo. Pro): 0. 25 mg/kg IV bolus followed by 0. 125 ug/kg/min for 12 hours (others: Integrilin, Aggrastat) 31
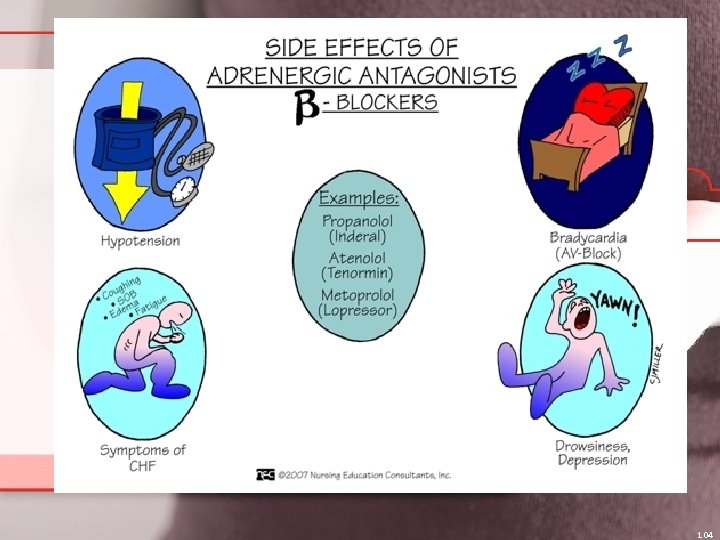
What precaution should we take with beta blockers ? ? ? Heart has Beta 1: so Beta Blockers lower BP slowing heart rate Lung has Beta 2: so Beta blockers constrict bronchioles, making it harder to breathe Propranolol blocks both types of beta receptors so SHOULD NOT BE USED IN ASTHMATICS Metopolol CAN be used since it is specific for Beta 1 and DOES NOT CONSTRICT BRONIOLES SO SAFE WITH ASTHMATICS. 32
3. variant (Prinzmetal) angina: - rare & associated with angina at rest - tend to be younger women (smokers) & pain occurs in early am & with menstrual - ST elevation (reversible) but cardiac enzymes norm - CAUSE: coronary artery spasm occurs at stenosed area Treat: responds to NTG long-term: calcium channel blockers 33
Other causes of CP: A. reflux or peptic ulcer disease B. chest wall pain (pain reproduced on palpation and localized) - occurs from bruised/ fx ribs C. esophageal problems - achalasia, esophageal spasm D. pericarditis (will be sed rate, low-grade fever, viral cause (coxsackievirus) E. pneumonia F. Aortic dissection (CV EMERGENCY) watch for severe pain radiating to back 34
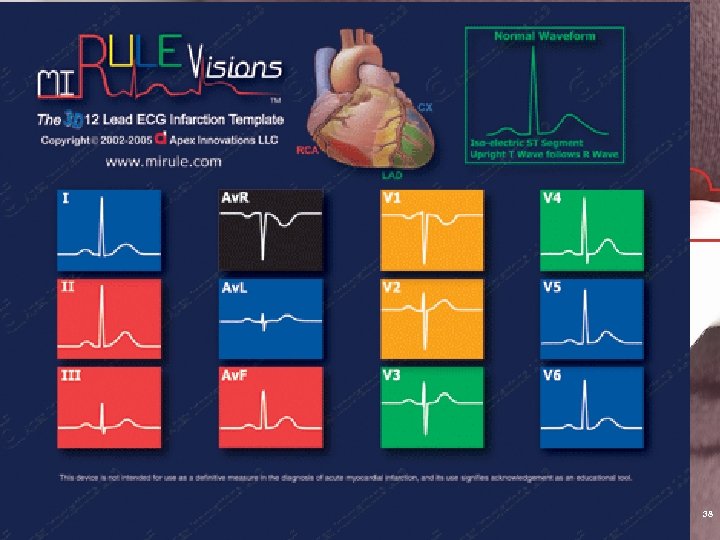
MI patterns (as more areas of heart becomes damaged, the more dangerous the MI becomes) Common patterns: Ant/lat inf/post ant/septal 25% of MI are “silent” : presents without chest pain (esp in diabetics with neuropathy) Patient presents with heart failure, shock, confusion, delirium (esp in elderly) 35
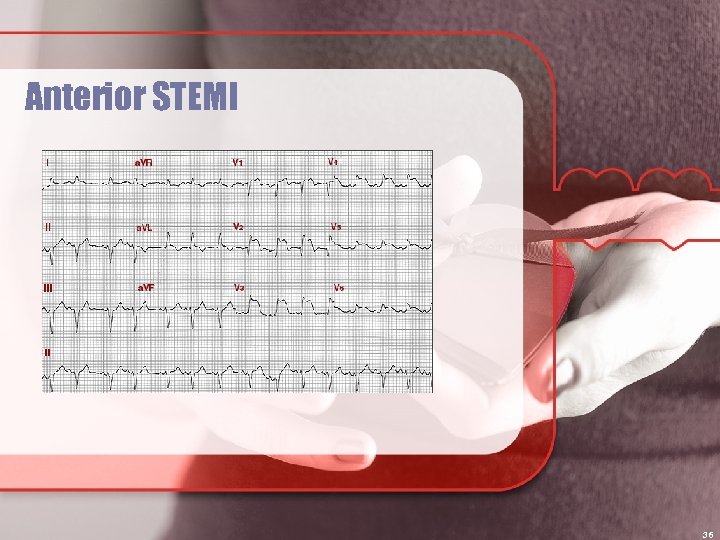
Anterior STEMI 36
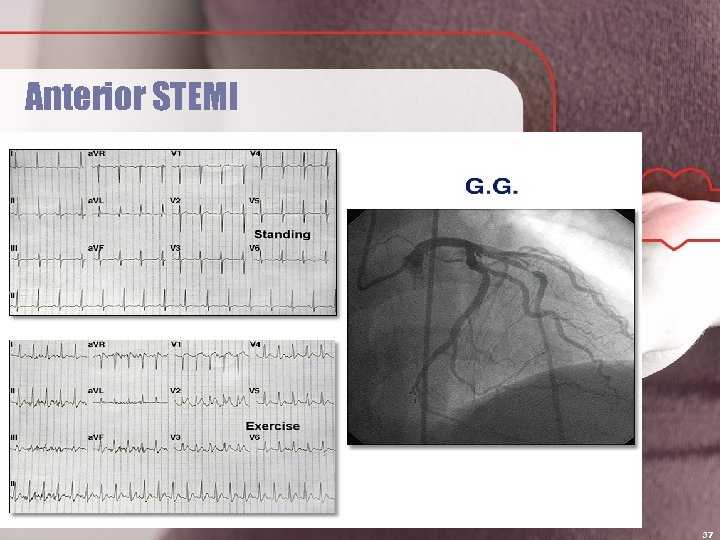
Anterior STEMI 37
38
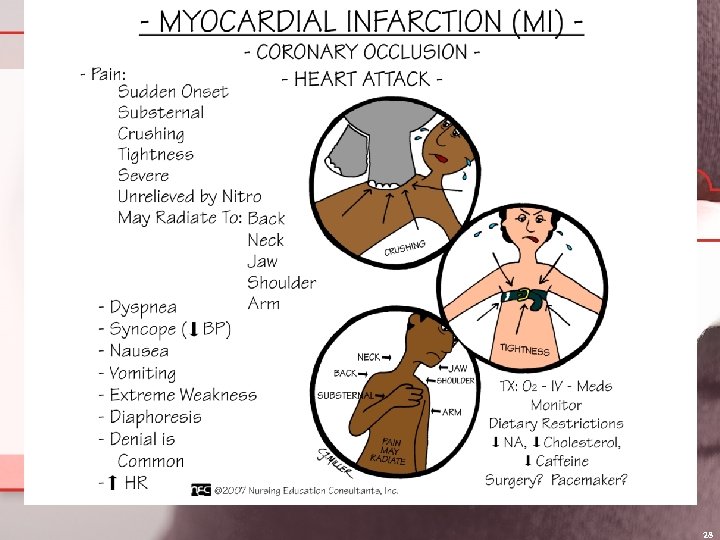
Myocardial Infarction Pain doesn’t resolve with NTG s/s: crushing, poorly localized substernal pain, radiates to shoulder, arm, jaw, diaphoretic, sense of impending doom, N/V, tachycardia or bradycardia, dyspnea, ST elevation, Q waves (occurs after 12 hours Duration: > 30 minutes with no relief Not relieved by rest & can even occur @ rest 39
MI subdivided into STEMI or NSTEMI - actual necrosis of myocardial tissue - most cases, atherosclerotic heart disease present = other cases is from artery spasm - IDENTIFICATION OF MI IS MOST IMPORTANT AS WITHIN 6 hours there is irreversible damage!!!! 40
Non STEMI No st segment elevation present If enzymes are increased it means severe injury Higher probability of death 41
STEMI ST segment elevation on EKG Severe anoxia Cellular damage present (ex. Complete blockage) If blood flow not re-established in 20 min. cell death occurs 42
Diagnostic Tests EKG: rate, rhythm, ischemia (T-inverted), injury (ST segment elevation), arrhythmias, strain, infarction (q wave) Echocardiogram: (TEE) sound wave test detects size of chambers, valve integrity, flow, wall motion, Cardiac Output 43
Diagnostic Tests Continued Biomarkers: Troponin I will show elevation 3 -12 hrs of MI period and normalizes after 1 -2 weeks <0. . 06 is negative 0. 10 -0. 60 is intermediate and may indicate injury >0. 60 is positive evidence of MI Myoglobin normal is 17 -106 ng/m. L CPK-MB will show increase 4 hrs after MI and normalizes 72 hr after infarct BNP can be elevated 48 hrs after MI which indicates heart failure 44
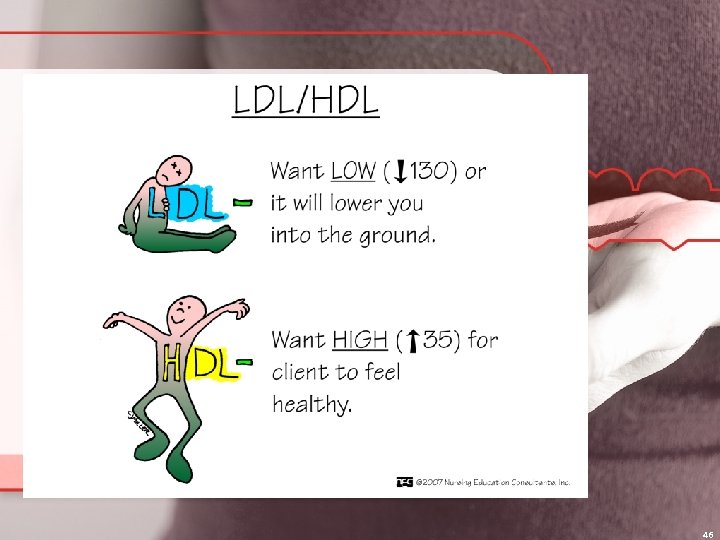
Diagnostic Tests Continued CBC: anemia CMP: screening K+, etc PT, INR PTT Lipid profile: looks at total cholesterol (good and bad) 45
46
Diagnostic Tests Continued ABG: assess acid/base levels Pulse Oximetry: generally >92% Holter monitoring: 24+ hr of EKG + events Stress test: treadmill or pharmacological Cardiac Catheterization: invasive, NPO 6 -8 h, consent. Visualizes chambers, valves, arteries, pressures, CO Heart-CT scan: assesses CAD Nuclear scans: assess heart muscle viability EPS: NPO, consent, IV, assess electrical activity 47
Complications of MI Depends on which vessel involved & region of the heart muscle Ischemia of condux system, causes arrythmias If lg enough area, CHF develops Occlusion of Left descending artery: left heart failure Occlusion of Right descending artery: Rt heart failure Infarct of vent wall can result in rupture, heart hemorrhage into pericardial sac leads to “tamponade” can be quickly fatal 48
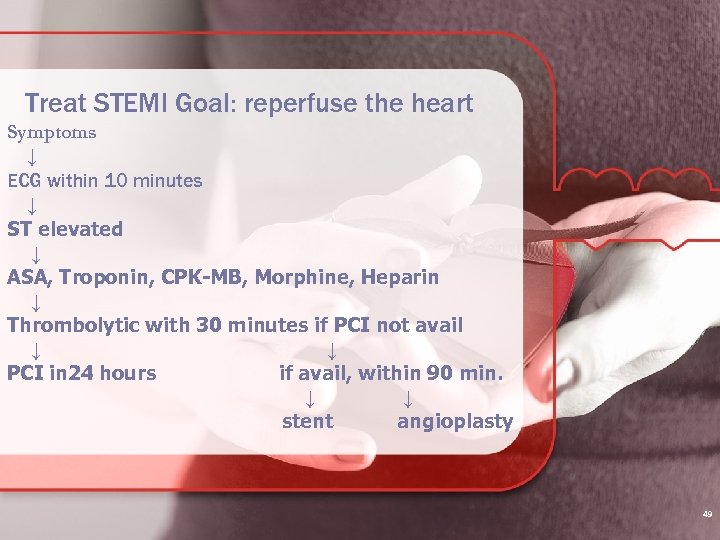
Treat STEMI Goal: reperfuse the heart Symptoms ↓ ECG within 10 minutes ↓ ST elevated ↓ ASA, Troponin, CPK-MB, Morphine, Heparin ↓ Thrombolytic with 30 minutes if PCI not avail ↓ ↓ PCI in 24 hours if avail, within 90 min. ↓ ↓ stent angioplasty 49
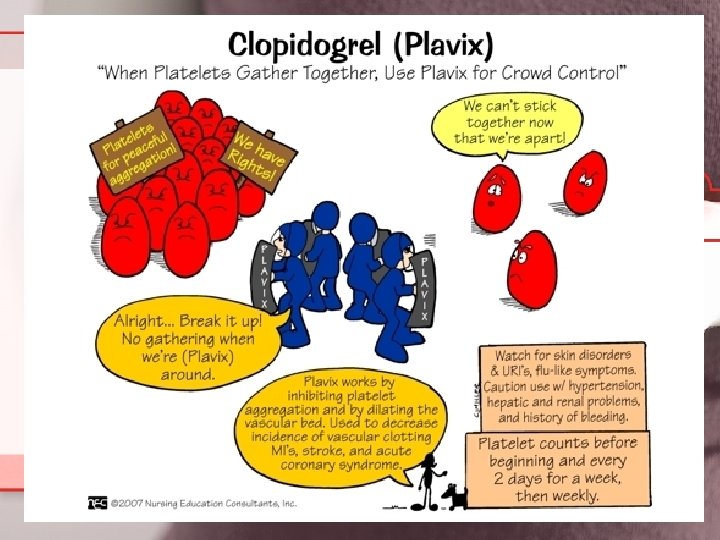
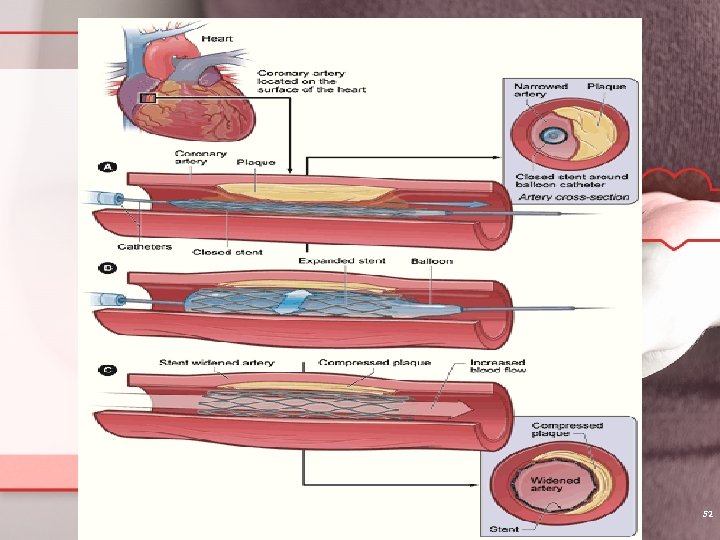
Angioplasty with Stent Procedure done at the time of cardiac cath. Balloon angioplasty is accomplished to widen or open specific coronary vesselstent is inserted to maintain patency of the vessel. pre-procedure Plavix given with follow up Plavix http: //preop. medselfed. com/asp/center. asp ? center. Id=heart&partner. Id=preop&id=&cac hedate=&email. Id=&aff. Id=&camp. Id=&hide. N av= 50
Stents Holds open the coronary artery where narrowed Drug eluding stent (DES) decreases /prevents endothelial overgrowth Antiplatelet therapy needed (Plavix) 51
52
NSTEMI and Unstable Angina Assessment & Treatment No ST elevation ↓ Draw Troponin I ↓ If elevated ↓ Cardiac cath vs Management Medical ↓ Echo, Stress test 53
Medical treatment in MI treatment output: For low cardiac - dobutamine +inotropic -milrinone +inotropic For hypotension: - dopamine ( or at low doses used to improve renal perfusion) May need Intraaortic balloon pump 54
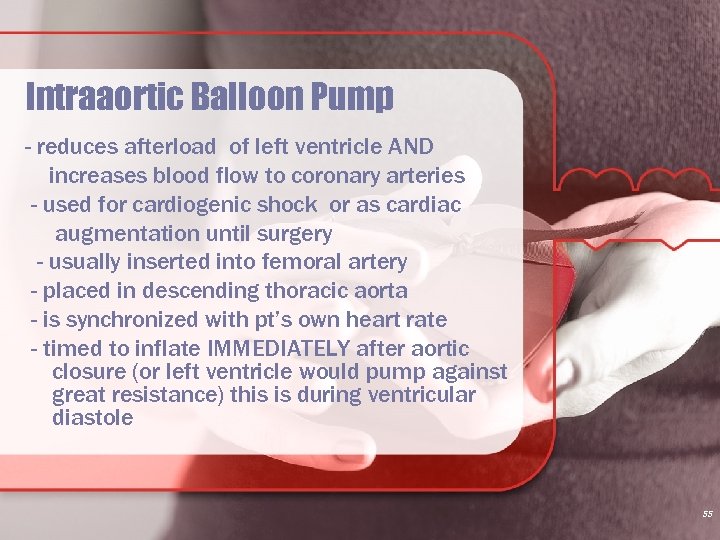
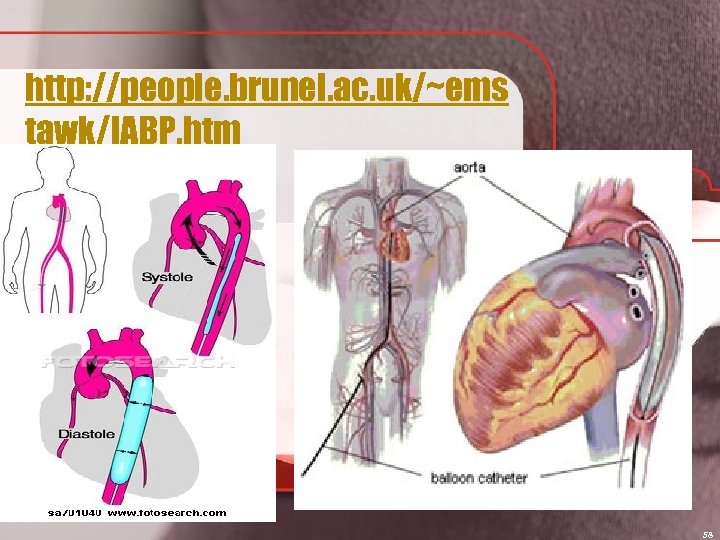
Intraaortic Balloon Pump - reduces afterload of left ventricle AND increases blood flow to coronary arteries - used for cardiogenic shock or as cardiac augmentation until surgery - usually inserted into femoral artery - placed in descending thoracic aorta - is synchronized with pt’s own heart rate - timed to inflate IMMEDIATELY after aortic closure (or left ventricle would pump against great resistance) this is during ventricular diastole 55
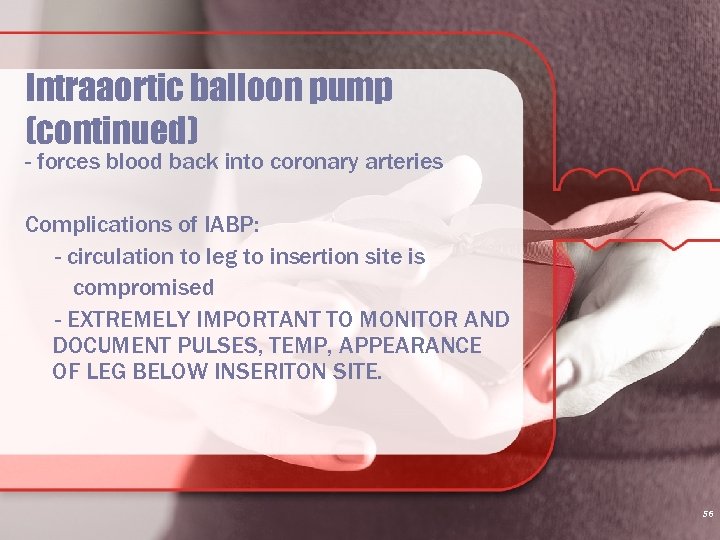
Intraaortic balloon pump (continued) - forces blood back into coronary arteries Complications of IABP: - circulation to leg to insertion site is compromised - EXTREMELY IMPORTANT TO MONITOR AND DOCUMENT PULSES, TEMP, APPEARANCE OF LEG BELOW INSERITON SITE. 56
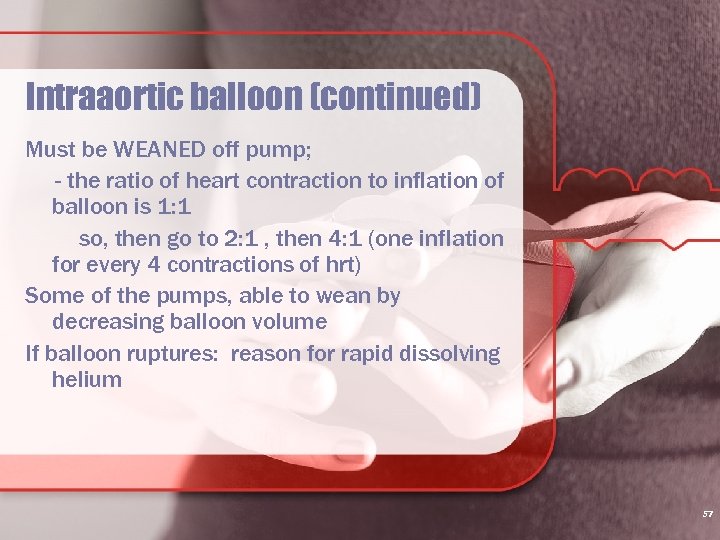
Intraaortic balloon (continued) Must be WEANED off pump; - the ratio of heart contraction to inflation of balloon is 1: 1 so, then go to 2: 1 , then 4: 1 (one inflation for every 4 contractions of hrt) Some of the pumps, able to wean by decreasing balloon volume If balloon ruptures: reason for rapid dissolving helium 57
http: //people. brunel. ac. uk/~ems tawk/IABP. htm 58
Contraindications for Balloon Pump: Aortic or ventricular aneurysms Ventricular septal defects Aortic regurgitation 59

Medical support (MI continued) Vasodilators to reduce preload/afterload - nitroglycern or nitroprusside ACE inhibitors: - reduce afterload Beta blockers: - reduce myocardial oxygen consumption - decrease heart rate and BP Statins: - restrict development of artherosclerosis & also have anti-inflammatory effects Platelet inhibitors: - ASA 60
Specifics on Fibrinolytic agents: must be within 12 hour of symptoms Streptokinase: depletes fibrinogen to predisposed to systemic bleeding & allergic reaction possible with second time use Alteplase (t. PA, Activase): used most often Reteplase (r. PA, Retavase) a synthetic, 2 nd generation that works more quickly & lower bleeding 61
Nursing Interventions if fibrinolytic used: Minimal arterial or venous sticks Use finger oximetry Avoid automated blood pressure cuffs (bruising Assess for signs of bleeding(hypotension, tachycardia, reduced level of consciousness) Reperfusion arrhythmias common - bradycardia and V-tach most common IF BLEEDING COMPLICATIONS: -stop fibrinolytic agent, FFP &/or cryoprecipitate to replenish fibrin & clotting factors, Aminocaproic acid (Amicar) 62
Absolute Contraindications to Thrombolytic Therapy: Hx of intracranial hemorrhage Known structural cerebrovascular lesion Known intracranial tumor Ischemic stroke <3 months Severe uncontrolled hypertension Acute pancreatis Aortic dissection Hx of hemorrhagic stroke pregnancy 63
Monitoring/interventions MI (continued) Continuous cardiac monitoring Oxygen IV line Hemodynamic monitoring (discuss in a bit) Bed rest Emotional support Need passive & active ROM to reduce risk of thromboembolism (immobility) 64
Recovery MI Begins as soon as MI stop Scar tissue dev. at necrotic area (takes 6 -8 wks May see stages of grief in pt with MI - - we need to identify depression as mortality at 1 to 5 years with associated depression !!!! MUCH TEACHING NEEDED; - MODIFY RISK FACTORS, LIFESTYLE CHANGES, WORK WITH BOTH FAMILY/PT 65
Lethal complications of MI that can occur 5 to 10 days post MI: Papillary muscle rupture Ventricular aneurysm Ventricular rupture 66
Treatments Low fat low cholesterol diet Prescribed exercise program 5 -7 days a week Knows correct use of NTG for angina Management of DM, HTN Stop smoking Medications to reduce work load or dilate 67
Exercise 5 -7 X week is goal to include stretches with warm-up, progressive walking program, light weights, stretches with cool down. Strengthens heart muscle, reduces BP, BS, weight, stress, tension, appetite, LDLs. Increases HDLs, energy and self esteem and improves immune system 68
Principles of Exercise Practice on regular basis Know how to do own pulse Strive for target heart rate Stop if chest pain occurs Complications: CHF & Dysrhythmias 69
Nursing Diagnosis Decreased cardiac output r/t Dysrhythmias Pain r/t lack of 02 to myocardium Anxiety r/t to feeling of doom, lack of understanding of medical diagnosis 70
You are asked to evaluate a 55 -year old Caucasian woman who presents to the Emergency Department with the chief complaint of chest pain for several hours. She awoke with the discomfort at 4: 00 AM today, and it has been a "ten out of ten" since then. The pain is substernal, radiates to her back, and is associated with moderate-to-severe shortness of breath and nausea. No previous such episodes are reported, but the patient states there is a strong family history of cardiac disease, and that she has smoked one-half pack of cigarettes daily for the past thirty-five years. Other than that, she denies past medical or surgical conditions, takes only hormone replacement therapy, and has no known drug allergies. Social history reveals that the patient is married, has three children, and works as an accountant. On physical exam, the patient appears to be in mild discomfort due to chest pain, but otherwise appears normal. Temperature is 97. 7 F, pulse is 110, blood pressure is 150/100, and respirations are 20. Head and neck, lung, heart, and abdominal exams are normal. An EKG is performed, which shows nonspecific T-wave changes in the lateral leads. Other tests, including troponin-I, cardiac enzymes, and chest x-ray have been performed, but results are still pending.
What are risk factors? What are you concerned with? What to do? 72
Cardiac Surgery Coronary artery bypass graft- done after confirmation with cardiac catheterization. Re-route blood vessels using mammary or saphenous v from aorta around block in coronary artery. Valve replacement or repair Septal repair and other congenital repairs CCU post op, chest tubes Pre-op teaching with post op expectations 73
CABG procedure overview: Pt cooled to reduce O 2 demand Placed on cardiopulmonary bypass – which diverts blood from heart but oxgenates & removes CO 2 New procedures include working on a beating heart or the MIDCAB 74
Physiological consequences of CABG: 1. damage to blood (platelets, RBCs WBCs & plasma proteins) 2. Incorporation of abnormal substances into blood (bubbles, fibrin, platelet aggregates) 3. a systemic inflammatory response 4. increase in systemic vascular resistance 5. increase catecholamines 75
Nursing interventions for CABG 1. fluid status (fluid leaks from vessels) 2. O 2 sats (indicates excess capillary leaking) 3. postop bleeding from anticoagulation for procedure 4. hemodynamic monitoring 5. pain relief 6. dysrhythmia control 7. warming pt may need vasopressors to maintain BP initially (undesirable to let pt shiver as oxygen demands) (use warmed blankets, warmed blood to infuse, warmed inspired gases) 76
Nursing interventions CABG (continued) 8. bleeding not to exceed 300 m. L/hour in first couple hours then 150 -200 ml/hour but average blood loss is 1 L. Notify physician if excessive. Autotransfusion of medialstinal blood is filtered & infused 9. aggressive suctioning then enc coughing 10. monitor electrolytes to prevent dysrhthmias 77
11. dysrhythmias treated pharmacologically 12. pacing wires placed on right atrium and ventricle before surgical closure. Postop BRADYCARDIA most common indication for need of pacer. 78
Complications of CABG Hemorrhage, cardiac tamponade, MI, ventricular dysfunction, dysrhythmias, death Cardiac tamponade: - watch for pts that have bleeding in chest tube (significant) then suddenly STOPS bleeding & becomes hypotensive - reopen & immed return to OR 79
Congestive Heart Failure 80
DEFINITION: EF < 35% or when the myocardium is no longer able to pump efficiently and fluid accumulates in the lungs and or selected areas of the body as a result 81
Causes of CHF CAD, advancing age HTN is a major factor > CHF x 3 DM, Smoking, Obesity Valvular incompetency, alcohol or other chemicals, idiopathic, (unknown) 82
CHF (continued): Right side failure: (blood backing up causing congestion in body) s/s due to blood pooling JVD, dependent edema, hepatic congestion, a-fib, fatigue, wt loss, cyanosis With a-fib be aware of risk for embolization Echocardiogram: reveals ↓ CO 83
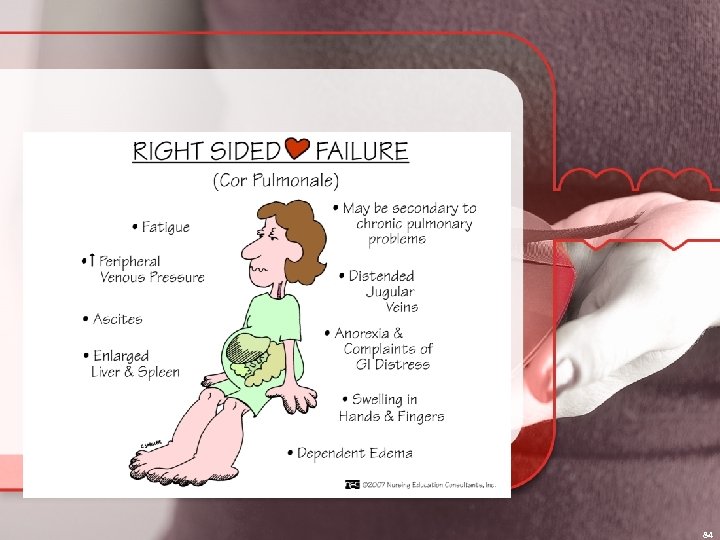
84
S/S of Left Sided CHF (blood backing up into pulmonary structures) Fatigue Angina Tachycardia Cool extremities Hacking cough Crackles Frothy sputum Gallop 85
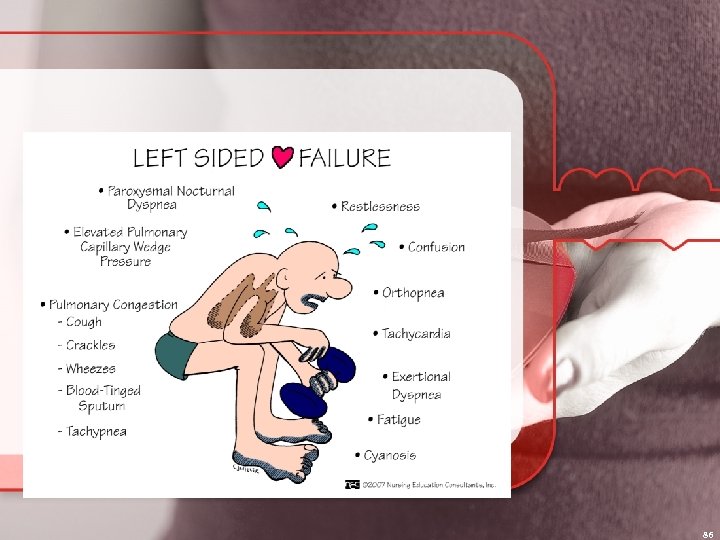
86
System Compensation Mediated thru Sympathetic Nervous System: as CO drops, baroreceptors alert brain>>>signals adrenal glands to release catecholamines{norepinephrine and epinephrine} This causes stimulation Beta 1=>>HR Stimulation Beta 2= bronchodilation Activate Alpha receptors peripherally=constriction=>>bp 87
Compensation Causing S/S of CHF because: Contractility decreases Stroke volume and CO continue to decrease Afterload (pressure on the other side of the aorta) increases Preload ( pressure caused by increase volume to heart creating an exaggerated stretch in the muscle) increases 88
Renal Compensation CO drops initiating renin-angiotensin mechanism Results in powerful vasoconstrictor angiotensin II, >> aldosterone (hormone) which causes kidneys to retain Na and H 20 which increases blood volume 89
Ventricular Hypertrophy The heart enlarges which results in strain The increase in volume causes the ventricles to dilate Eventually remodeling will occur 90
Diagnostic Tests H&P Chest x-ray: see size of heart and fluid in lungs EKG: strain, MI Echocardiogram: size of heart and CO CBC: anemia CMP: screening Thyroid function ABGs BNP=B type natriuretic peptide= hormone released in response to Ventricular stretch ( CHF peptide) Nuclear studies to determine heart function, EF, tissue viability Cardiac Cath to determine exact nature of heart function 91
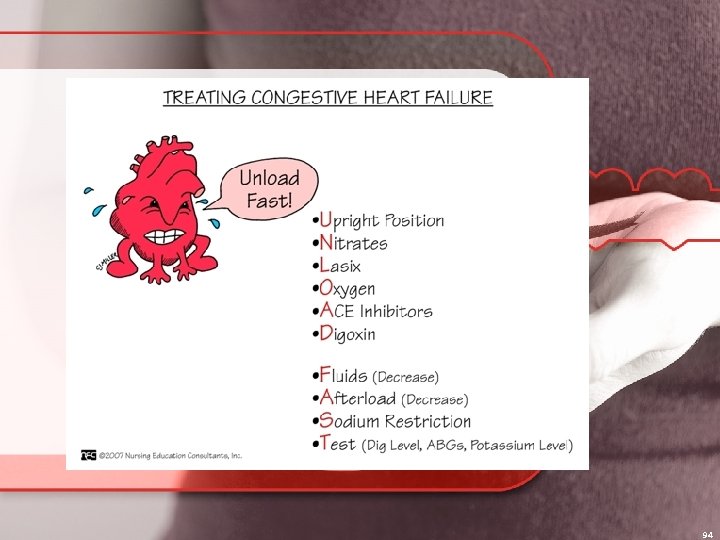
CHF Management Directed at: Improving LV function (Contractility) by decreasing intravascular volume and decreasing vascular resistance Decreasing venous return (Preload) Decreasing BP (Afterload) Improving gas exchange and 02 Increasing the CO and reducing anxiety 92
Treatment of CHF Treat underlying cause Rest and hi Fowlers to reduce work load and improve ventilation 02 at 2 -6 L/min with 02 sats >92% to increase available 02 and prevent hypoxemia Freq VS and cardiac monitoring 93
94
Treatment continued I & O q shift Daily am weights before breakfast and after voiding. 2 -3# weight gain in 1 -4 days call MD Sodium restricted diet Medications: to decrease intravascular volume thus reducing venous return, dilate and reduce BP and improve contractility surgery http: //chfsolutions. com/zip_how_aquaphere sis_works. html# 95
ULTRAFILTRATION allows for the production of plasma water from whole blood across a semipermeable membrane in response to a transmembrane pressure gradient The ensuing fluid or ultrafiltrate is isotonic to plasma Ronco et al. Cardiology. 2001; 96: 155 -168.
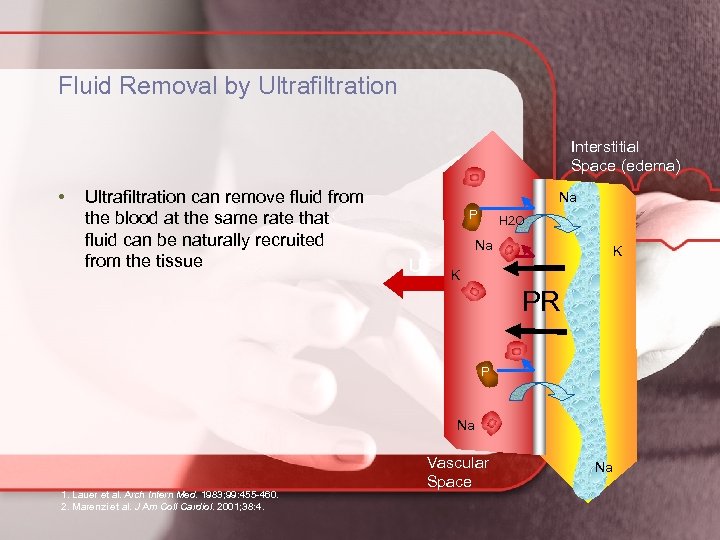
Fluid Removal by Ultrafiltration Interstitial Space (edema) • Ultrafiltration can remove fluid from the blood at the same rate that fluid can be naturally recruited from the tissue Na P H 2 O Na UF K K PR P Na Vascular Space 1. Lauer et al. Arch Intern Med. 1983; 99: 455 -460. 2. Marenzi et al. J Am Coll Cardiol. 2001; 38: 4. Vascular Space Na
Ultrafiltration Compared to Loop Diuretics • Ultrafiltrate is isotonic with plasma, whereas the diuresis of loop diuretics is virtually always hypotonic to plasma • Ultrafiltration removes more sodium than diuretic therapy • No electrolyte disturbances • Ultrafiltration decreases ECF volume more than a comparable volume of diuretic-induced fluid loss Schrier. J Am Coll Cardiol. 2006; 47: 1 -8.
Educating the CHF Client Education re: heart failure Explanation of heart failure Expected S/S and when to call MD Self monitoring of daily weights Know medications and need to take them 2000 mg sodium restricted diet Importance of low level daily exercise program (energy conservation) Prognosis / advanced directives 99
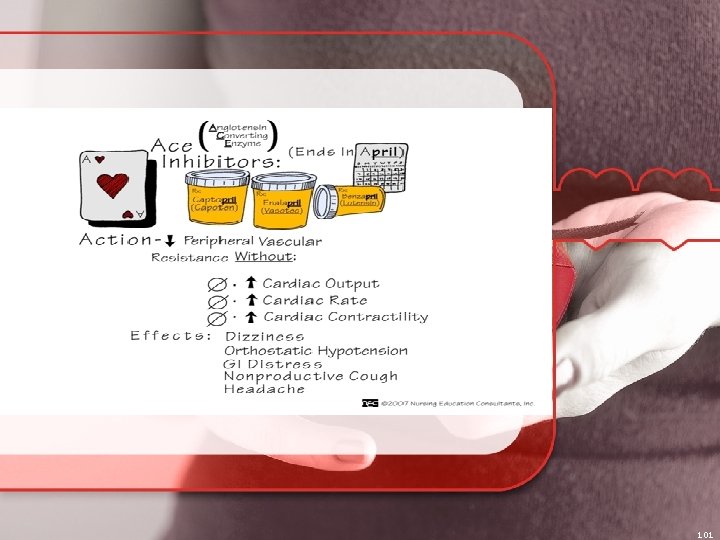
First line treatment for right side failure: ACE inhibitors ( proven to ↓ mortality in CHF Beta blockers (proved to ↓ mortality) - begin once pt diuresis occurs) Diuretics (loop and K+ sparing) Spironolactone (proven to ↓ mortality in class IV CHF) Digoxin may be used (doesn’t improve mortality in CHF BUT improves symptoms, ↓ hosptialization 100
101
102
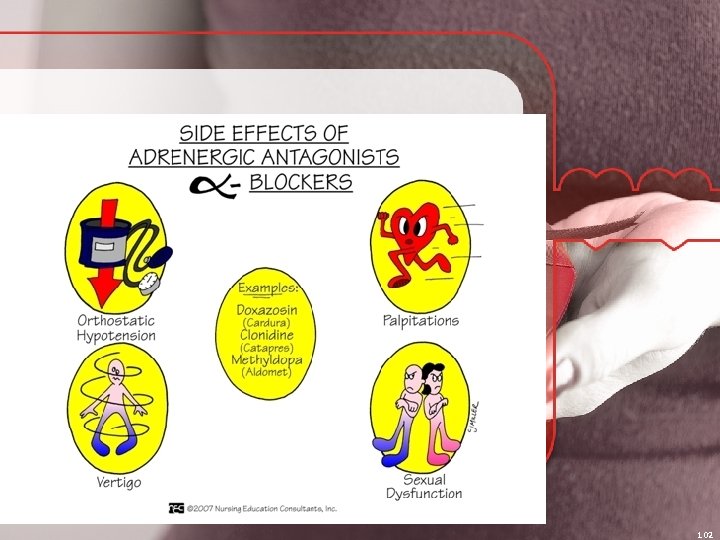
Treatment with BETA BLOCKERS with heart failure: ABSOLUTE improved systolic functioning & reverses cardiac remodeling Initially may have exacerbation of symptoms Decreases heart rate & inhibits release of renin Two drugs approved for heart failure: 1. Carvedilol (nonselective Badrenoreceptor antagonist that also blocks α adrenoreceptors 2. Metoprolol (selective B 1 selective antagonist) 103
104
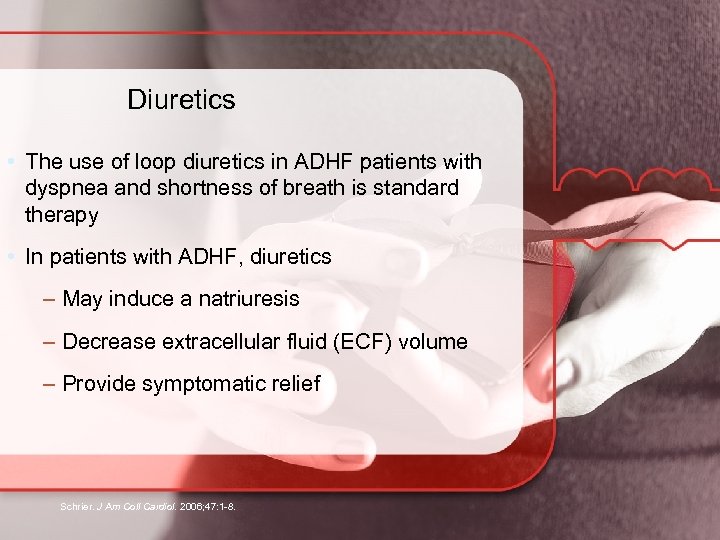
Diuretics • The use of loop diuretics in ADHF patients with dyspnea and shortness of breath is standard therapy • In patients with ADHF, diuretics – May induce a natriuresis – Decrease extracellular fluid (ECF) volume – Provide symptomatic relief Schrier. J Am Coll Cardiol. 2006; 47: 1 -8.
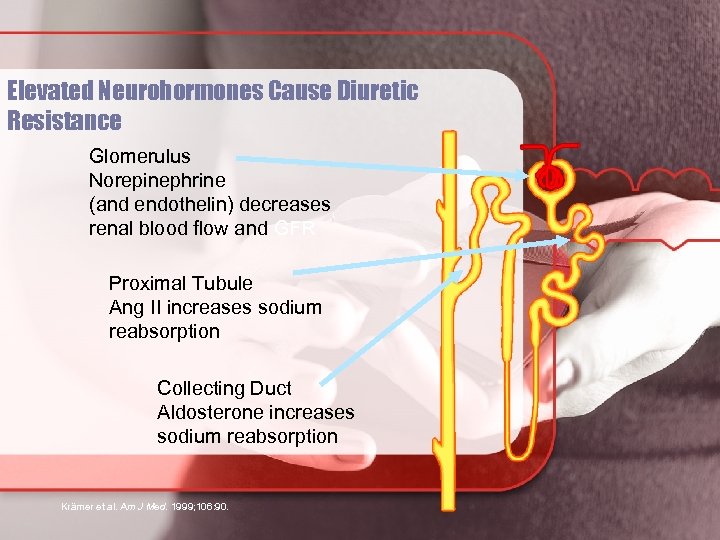
Elevated Neurohormones Cause Diuretic Resistance Glomerulus Norepinephrine (and endothelin) decreases renal blood flow and GFR Proximal Tubule Ang II increases sodium reabsorption Collecting Duct Aldosterone increases sodium reabsorption Krämer et al. Am J Med. 1999; 106: 90.
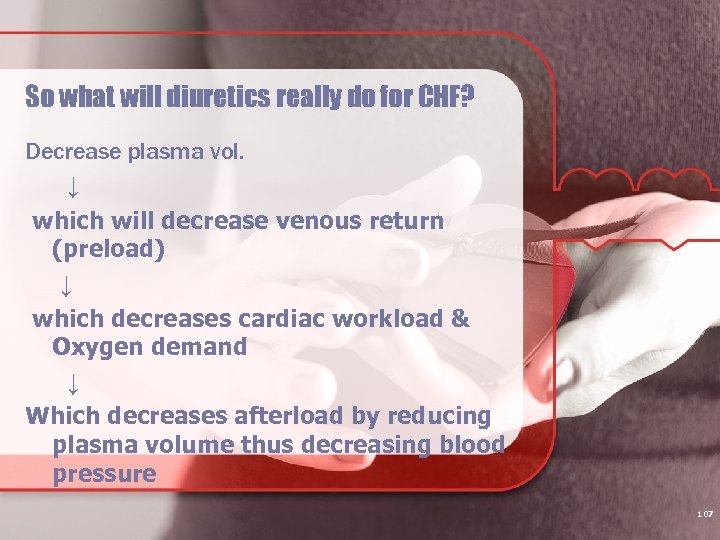
So what will diuretics really do for CHF? Decrease plasma vol. ↓ which will decrease venous return (preload) ↓ which decreases cardiac workload & Oxygen demand ↓ Which decreases afterload by reducing plasma volume thus decreasing blood pressure 107
When giving ACE inhibitors to your patient, what should you remember? ? ? Food decreases absorption Give on an empty stomach Postural hypotension (monitor) Watch for hyperkalemia, angioedema, PERSISTENT DRY COUGH NOT TO BE USED WITH PREGNANT WOMEN AS IT IS FETOTOXIC !!!! 108
When should Angiotensin-receptor blockers be used: Prototype: LOSARTAN Similar actions to ACE inhibitor These meds are a substitute for pts who cannot tolerate ACE inhibitors (those with severe cough or angioedema) - lowers BP - reduces morbidity & mortality assoc. with hypertension Only need once a day dosing Adverse effects similar to ACE inhibitors but without the cough Contraindicated with pregnancy 109
Treatment with direct vasodilators for heart failure: By dilating venous blood vessels, leads to decrease in cardiac preload By dilating arterial vessels, leads to reduction of systemic arteriolar resistance & decrease afterload NITRATES 110
Digoxin Since metabolized by the liver before excreted in feces, the pt with hepatic disease may require decreased dosing. HYPOKALEMIA PREDISPOSES THIS PATIENT TO DIGOXIN TOXICITY. What can be used to detoxify the body from dig? DIGOXIN IMMUNE FAB (THIS BINDS AND INACTIVATES THE DRUG) 111
Digoxin (continued) ADVERSE EFFECTS: Cardiac: progressively more severe dysrhythmias, eventually to complete heart block That is why is is so important to make sure K+ is normal !! GI: anorexia, n/v CNS: headache, fatigue, confusion, blurred vision, alterations of color perception, HALOS 112
Dig Toxicity: Hypokalemia leads to serious arrhythmias - will see this most in pts on thiazide or loop diuretics (prevented by using a potassiumsparing diuretic OR supplement with potassium chloride ) ALSO note that: Hypercalcemia AND hypomagnesemia ALSO predispose to dig toxicity !!!! 113
Inflammatory Heart Diseases 114
Rheumatic Heart Disease Complication of rheumatic fever Long term damage and scarring of valves Leading cause of death 100 years ago Occurs mostly in kids 5 -15 yrs old Develops from pharyngitis Group A beta hemolytic streptococcus Incubation period= 2 -4 days Valves swell and vegetation occurs on valves S/S: 1 -6 wks after strep (murmur, fever, malaise, HA, swollen tender joints, SOB, increased WBC, CP, tachycardia, HF signs 115
Rheumatic Heart Disease Diagnosis: CBC, Chest X-ray, C reactive protein, EKG, Heart Cath, blood cultures Interventions: PREVENTION is key, PCN like antibx, NSAIDS for joint pain, Cardiac meds, Bedrest Educate pt and family about prophylactic Antibx treatment 116
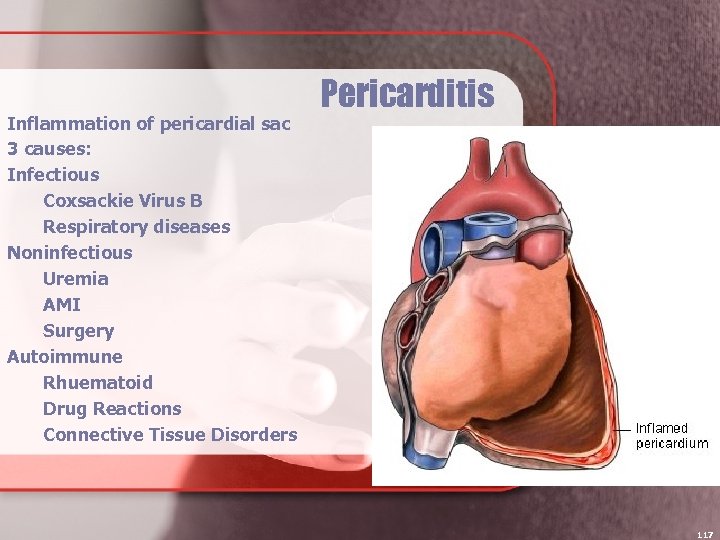
Inflammation of pericardial sac 3 causes: Infectious Coxsackie Virus B Respiratory diseases Noninfectious Uremia AMI Surgery Autoimmune Rhuematoid Drug Reactions Connective Tissue Disorders Pericarditis 117
S/S Chest pain is hallmark Friction rub Effusion Tamponade (see slides) Most severe on inspiration, sharp, stabbing, or dull and burning. Pain is relieved by sitting up or leaning forward Dyspnea, chills and fever 118
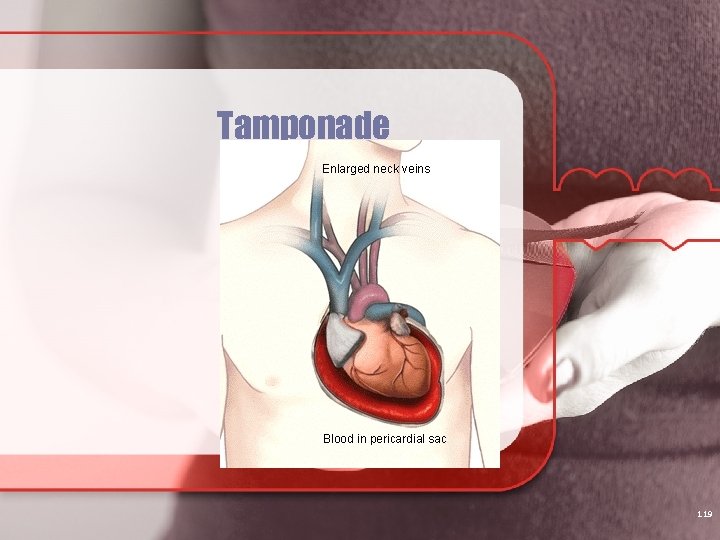
Tamponade 119
Tamponade Medical emergency Acummulation of pus or blood in pericardial sac Pressure increases causing back up of blood into the venous system Decreases cardiac output **key to finding** Beck’s Triad Decreased bp, muffled heart tones, JVD Weak pulses also occur May lose Consciousness 120
Nursing interventions for pericarditis: ECG monitoring for dysryhthmias Supplies ready for emergency pericardioicentesis Auscultate cardiac sounds Meds for pain Arterial blood gases or pulse ox Emotional support and explanations 121
Myocarditis Uncommon Frequently associated with pericarditis Usually viral in nature S/S: fatigue, malaise, achy joints, GI upset, flu like symptoms Dx: WBC, chest x-ray, heart cath, echo, cardio enzymes, etc Tx: immune therapy, antimicrobials, ACE, Antidysrhythmics, anticoagulants, antianxiety Scarring causes permanent damage 122
Endocarditis Inner layer: tends to affect the valves (Mitral). Organisms (Bacterial or fungal) present in blood stream and collect (colonize) on the valves Strep Rheumatic heart disease May be from IV drug use or invasive procedures 123
Endocarditis Infective endocarditis caused by gram+cocci A deformed or damaged valve is usual focus of infection Dental procedures can cause bacteremia Diagnosis: cultures, transesophageal echocardiography 124
S/S Fever- (99 -105) Chills and night sweats may accompany Malaise, fatigue and weight loss Appearance of petechiae in the mouth, conjunctiva and legs Chest and abdominal pain indicating embolization 125
Treatment and Diagnostics H&P and Lab tests CBC with diff with leukocytosis, > sed rate, blood cultures May have heart murmur Echocardiogram to visualize valves and vegetation Chest x-ray: CHF Long term antibiotics, rest, limited activity, prophylactic anticoagulants, valve replacement after inflammation treated 126
Endocarditis treatment: High doses antimicrobials for extended periods S. aureus & gram- bacilli most likely pathogens Vancomycin IV PLUS gentamicin or tobramycin IV For MRSA : Vancomycin Usually improvement in 3 to 10 days 127
Clients with known valvular disease need to be treated with prophylactic antibiotics prior to any invasive procedure including dental. Immunosuppression and any source of contamination places clients at risk 128
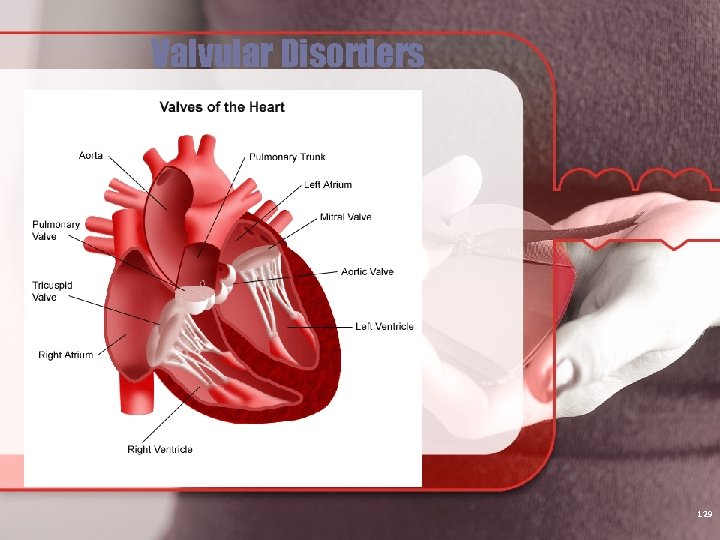
Valvular Disorders 129
Mitral Stenosis Mitral valve leaflets become thickened and fibrotic. Rheumatic heart disease is a common cause Affect women age 20 -40 S/S: dyspnea, afib, dry cough, palpitations, angina, crackles, fatigue, CHF may develop TX if failure develops: Digoxin, Lasix, beta blockers, and anti arrhythmics, lo Na diet, etc Will monitor with yearly echocardiogram Surgery if worsens Prophylactic antibiotics prior to invasive procedure or dental work 130
Insufficiency (Also referred to as regurgitation) The inability of the valves to close completely. Allows the blood to backflow. i. e. , After the L A has contracted some of the blood will flow back into the L A Mitral valve is the most commonly affected 131
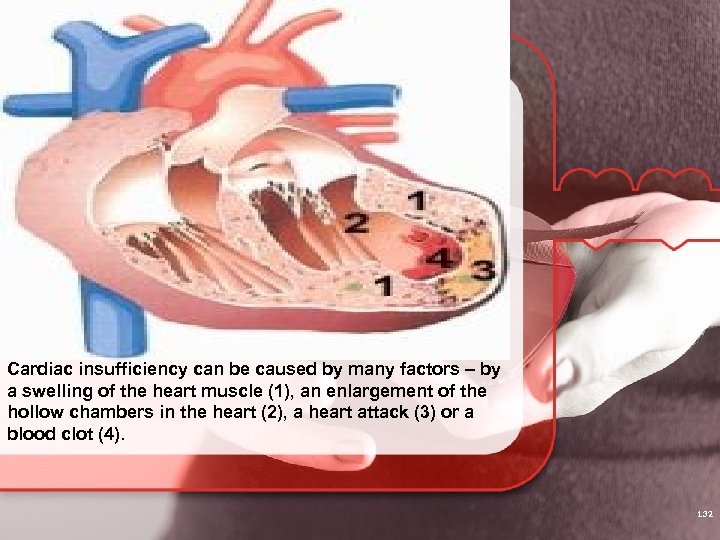
Cardiac insufficiency can be caused by many factors – by a swelling of the heart muscle (1), an enlargement of the hollow chambers in the heart (2), a heart attack (3) or a blood clot (4). 132
Mitral Insufficiency Often accompanies mitral stenosis as a result of rheumatic fever. Valve leaflet become rigid and shorten, prevents closure of valve. Hypertrophy of Left Atrium and Ventricle = L sided heart failure occurs Murmur heard. F/U with echocardiogram Edema and shock appear quickly Afib is common TX: vasodilators, same as for stenosis 133
Aortic Stenosis Occurs when valve cusps become fibrotic and calcify. Most commonly caused by aging and atherosclerosis. Occurs most predominantly in men Untreated will lead to Left sided CHF S/S: dyspnea is most common, syncope, angina 134
Aortic Insufficiency Caused primarily by rheumatic fever May also be caused by chronic HTN Predominantly in men Hypertrophy of the Left ventricle and eventually to left sided CHF Blood may eventually back up into the pulmonary system and lead to Right Ventricle failure S/S: palpatations, diastolic murmur is classic sign 135
S/S and Treatment Aortic murmur, tachycardia, palpitations, CHF with fatigue, SOB, Ascites Monitored with echocardiogram assessing L ventricular dilatation Chest X-ray-enlargement of heart May do cardiac cath May need valve repair or replacement 136
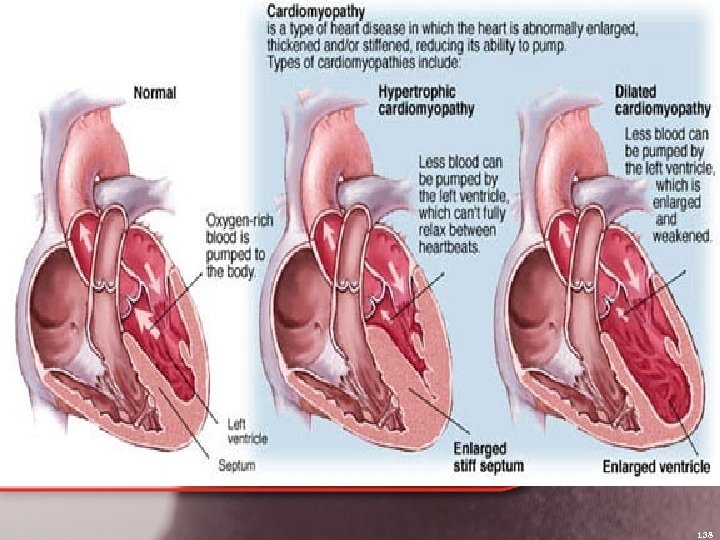
Cardiomyopathies: heart muscle disease Presents with increased ventricular pressures 3 common presentations of: 1. dilated (most common) 2. hypertrophic 3. constrictive Prognosis is POOR NO CURATIVE MEASURES AT THIS TIME 137
138
Dilated cardiomyopathy: Causes Idiopathic Inflammatory Autoimmune Toxic (drugs, alcohol) Hereditary Ischemic Metabolic (uremia, vit defic) Endocrine (thyroid 139
Dilated cardiomyopathy (continued) Dilated cardiomyopathy: dilation of cardiac chambers redux of ventricular contractile funx Diagnosed: echocardiogram TREATMENT: similar to CHF - inotropic agents -diuretics - vasodilators (ACE inhibitors) -beta blockers To prevent sudden cardiac death; implant cardioverter-defibrillator Need intra-aortic balloon to stabilize pt NEED HEART TRANSPLANT 140
Hypertrophic cardiomyopathy: Inability of heart to relax during diastole Goal: reduce afterload (beta-blockers, diuretics) Causes: idiopathic, systemic hypertension, genetic -atrial & vent arrhythmias seen in ½ of these pts are responsible for sudden death S/S: - dyspnea, angina, arrhythmias cardiac failure, very forceful apical impulse sudden death (most common in ages 10 to 35 and occurs during strenuous exertion) 141
Hypertrophic (continued) B-blockers Calcium channel blockers Diuretics Echocardiogram is key May need heart transplant 142
Restrictive cardiomyopathy - very noncompliant ventricular muscle -diminished LV cavity dimensions - ventricular volumes decreased CAUSES: - idiopathic - interstitial disease - radiation - drug toxicity 143
Restrictive treatment: Diuretics, afterload reducers Goal: to improve diastolic function Eventually hypotension occurs 144
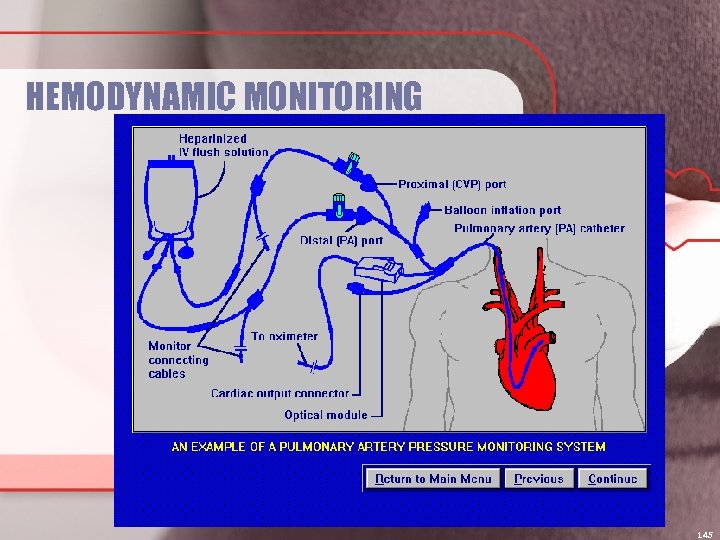
HEMODYNAMIC MONITORING 145
Monitoring of the blood flow and opressures within the body Purposes: Aid in diagnosis Assist in guiding therapies Evaluating response to therapies Can be invasive or non invasive Consent is needed especially if invasive unless in ICU when crashing 146
Components Monitor Flush system Transducer High pressure tubing Catheter 147
Setup Obtain IV NS 0. 9% and transducer system Attach the transducer to the IV flush solution and prime the tubing, removing air bubbles Replace all vented caps with non vented sterile dead end caps Inflate pressure bag to 300 mm. Hg Assist the patient into supine position with HOB <or = to 45 degrees Measure and mark phlebostatic axis with marker Level air fluid interface with that axis Zero the system Set alarm limits 148
System requires constant flow of sterile solution in order to maintain patency Saline bag placed in pressure bag 1 -3 ml per hour is common The transducer converts the pressure at the tip into electrical signal This signal is what is seen on monitor 149
Heparin vs No heparin Heparin influences the patency of the art lines Care should be taken so heparin induced thrombocytopenia is not initiated Occurs 4 -7 days after heparin exposure Client at risk for immune response Thrombosis risk increases 150
Leveling Means placing transducer at same level as tip of cath in the patient Use the phlebostatic axis (pg 562 osborn) *****important to use same reference each time is key**** Positioning above the transducer lowers the pressure reading Positioning below the transducer increases pressure reading Both can lead to incorrect treatment and fatality 151
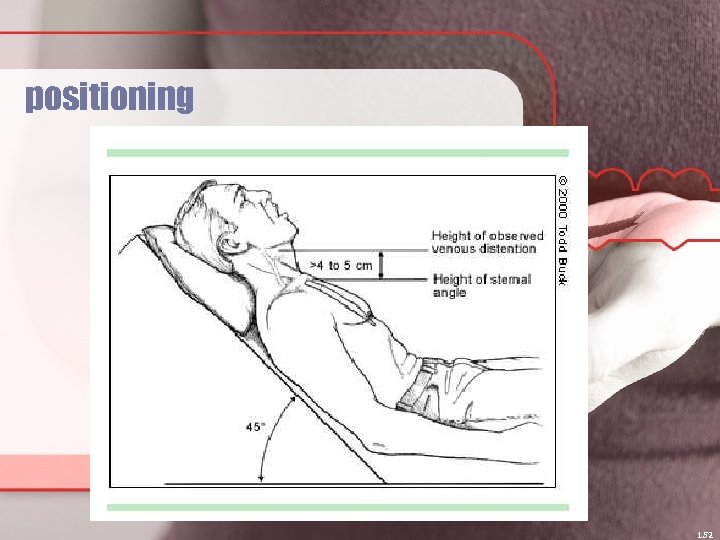
positioning 152
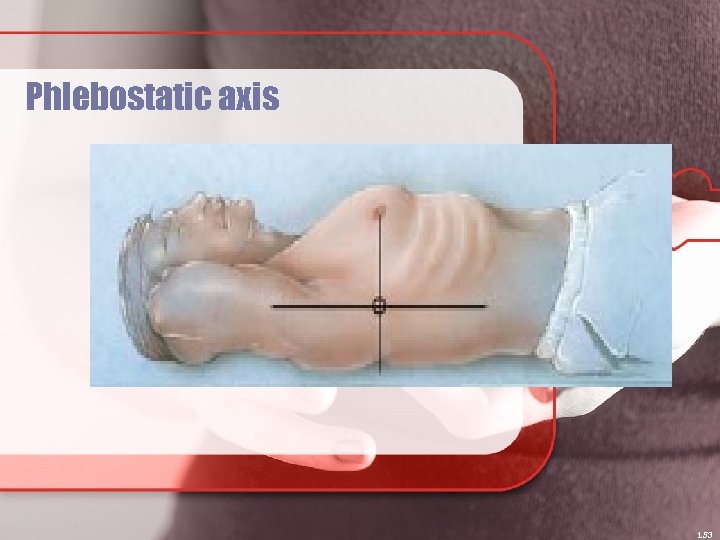
Phlebostatic axis 153
Zero referencing First make sure system is intact…no air bubbles, no leaks, and tight connections Do Qshift and with each turn Zeroing calibrates the system to atmospheric pressure. Procedure: Turn stopcock closest to pt to off position Remove cap Hit zeroing on monitor Wait for display to say zero Turn stopcock to neutral position 154
Square wave test Uses built in flush system (pigtail) Quickly pull and release Perform Q 8 -12 hours, after blood sampling, or if accuracy is questioned Page 563 osborn 155
Art Line Indwelling cath inserted by doctor into artery to monitor BP Allen test prior to is done to assess circulation Systolic pressure is max left ventricular systolic pressure The dicrotic notch represents closure of aortic valve and diastolic is pressure at rest Complications : hemorrhage, emboli, spasm, infection NSG management: explain reasons for, assess site 156
CVP Monitors central venous pressure and reflects preload Right atrium Uses: sepsis, Obtain consent Trendelenburg or Supine position for placement DO NOT USE FOR IV infusion or monitoring until xray placement confirmation Reflects BP in vena cava and rt atrium 2 -6 mm. Hg is adequate range Assess site at least Qshift. 157
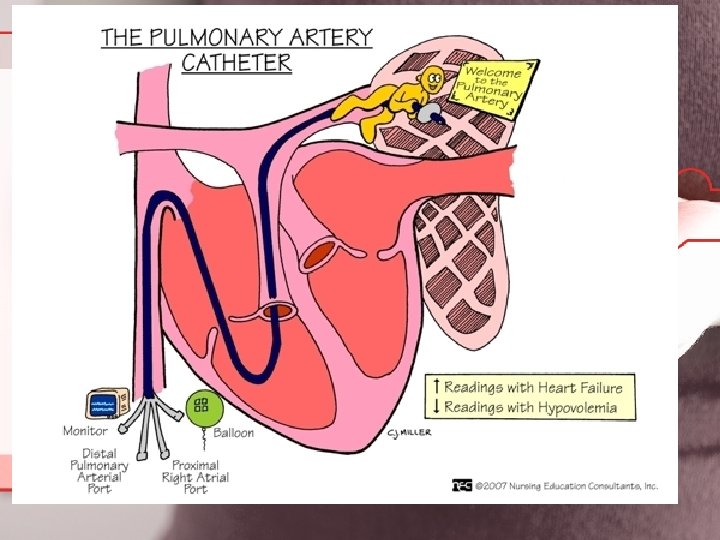
Pulmonary Artery Cath Multiple lumen Can measure temp in pulmonary artery Balloon is inflated up to 1. 5 ml air Over inflation can rupture artery and balloon Hemoptysis is presenting sign Place pt with affected side down to prevent leaking into unaffected side and call doctor immediately. Once inserted leave uninflated a pressure reading is needed. Assess patient (electrolytes, coag. , acid base) Set up per facility policy or like example earlier Complications: infection, air emboli, pneumothorax, artery rupture, pulmonary infarction, arrythmias 158
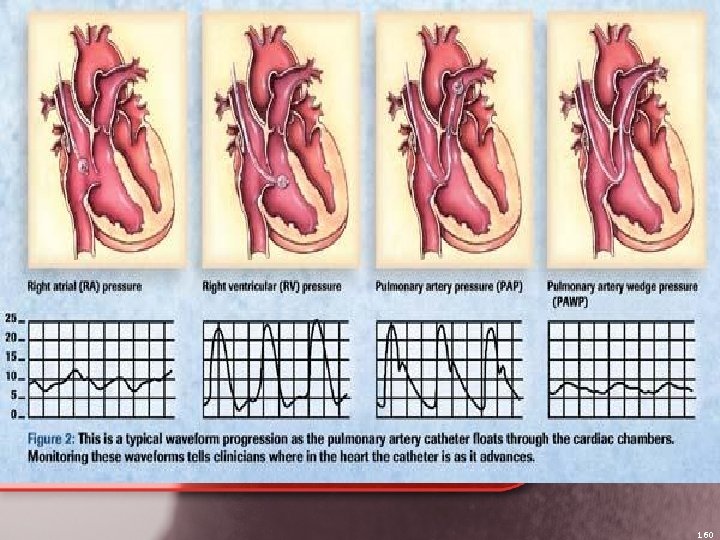
160
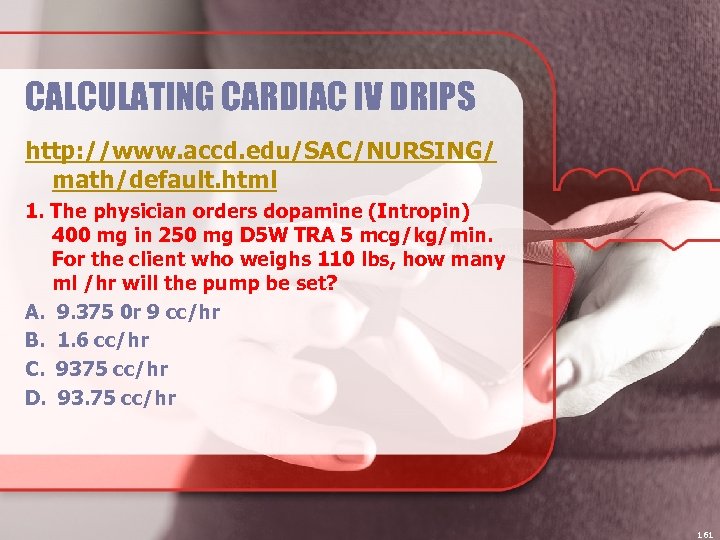
CALCULATING CARDIAC IV DRIPS http: //www. accd. edu/SAC/NURSING/ math/default. html 1. The physician orders dopamine (Intropin) 400 mg in 250 mg D 5 W TRA 5 mcg/kg/min. For the client who weighs 110 lbs, how many ml /hr will the pump be set? A. 9. 375 0 r 9 cc/hr B. 1. 6 cc/hr C. 9375 cc/hr D. 93. 75 cc/hr 161
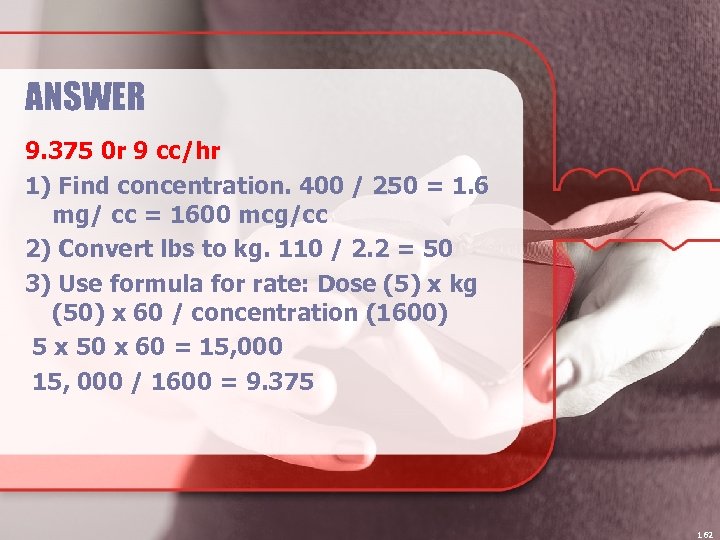
ANSWER 9. 375 0 r 9 cc/hr 1) Find concentration. 400 / 250 = 1. 6 mg/ cc = 1600 mcg/cc 2) Convert lbs to kg. 110 / 2. 2 = 50 3) Use formula for rate: Dose (5) x kg (50) x 60 / concentration (1600) 5 x 50 x 60 = 15, 000 / 1600 = 9. 375 162
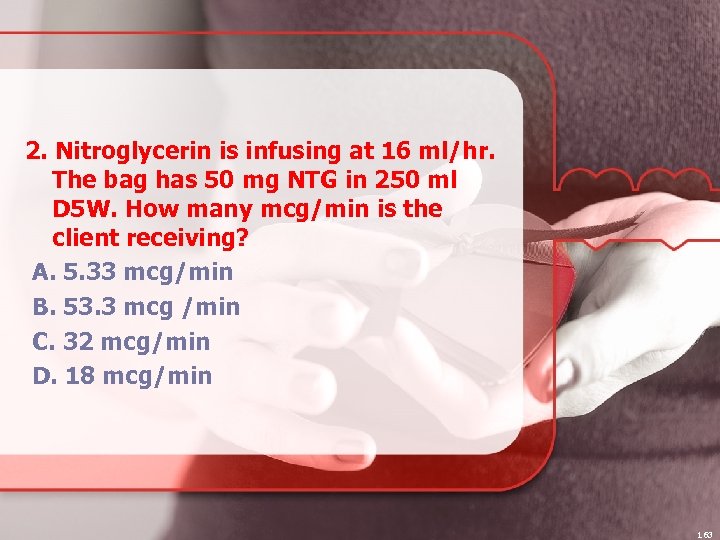
2. Nitroglycerin is infusing at 16 ml/hr. The bag has 50 mg NTG in 250 ml D 5 W. How many mcg/min is the client receiving? A. 5. 33 mcg/min B. 53. 3 mcg /min C. 32 mcg/min D. 18 mcg/min 163
ANSWER 53. 3 mcg /min 1) Find concentration. 50 / 250 = 0. 2 mg/cc = 200 mcg/cc 2) Use Dose formula: Rate (16) x Concentration (200) = 3200 / 60 = 53. 33 164
3. Sodium nitroprusside (Nipride) 50 mg / 250 ml of D 5 W is hanging. The physician orders include titrating the Nipride to keep Mr. Granger's systolic BP <140 mm Hg. The IV is infusing at 20 ml / hr. Mr. Granger weighs 56 kg. What is the dosage (mcg / kg / min the client is receiving? A. 3. 6 B. 1. 2 C. 2. 4 D. 0. 8 165
ANSWER 1. 2 166
4. Mr. Rouse is admitted to CCU for chest pain. A nitroglycerine drip is started at 12 ml/hr. The label indicates 100 mcg/ml. How many mcg/min of nitroglycerin is he receiving? A. 10 mcg/min B. 18 mcg/min C. 32 mcg/min D. 20 mcg/min 167
ANSWER 100 x 12 / 60 = 20 mcg/min 168
The Five Rights of Medication Administration Right patient Right medication Right dose Right route Right time 169
The Three Checks of Medication Administration 1. Read the label of the medication as it is removed from the shelf, unit dose cart, refrigerator, or dispensing system 2. Read the label of the medication when comparing it with the MAR 3. Read the medication label again before administering the medication to the patient 170
• LOOK at the label for verification of the medication name, dosage, route, and expiration date CHECK the medication itself, NOT just the pharmacy label Be overly cautious with regards to dose, proper dilution, and administration rate Watch decimal points Be aware of the unit Is the medication dispensed in mcg or mg? What is ordered in comparison? • • • 171

COMPLICATIONS OF IV 172

Extravasation Infiltration
Cardiac Transplant Criteria 1. end-stage, ischemic, valvular, or congenital heart disease with maximum med therapy, not amendable to surgery 2. Class III –IV heart failure with max med therapy 3. prognosis for 1 year survival <75% 4. age <65 years 5. psychologically stable, compliant 6. strong family support system 174
Cardiac transplant criteria (continued) 7. able to adhere to complex med regimen 8. absence of the following - systemic disease or infection - serious, irreversible impariment of hepatic, renal, pulmonary functions - recent CVA or neurologic defects - peptic ulcer disease - active substance abuse - pulmonary vascular resistance >6 wood units - psychological instability - malignancy 9. relative contraindications: - diabetes and advanced periph atherosclerosis 175
Cardiac transplant (continued) Success rate very good - 1 year survival at 76% and thereafter approx 4% mortality per year over 11 years major reason for improving outcome over years: immunosuppression Transplanted heart has NO innervation from the autonomic system, so pt feels no angina pain 176
The End
5f03f5e6188816a3650501ddaeeed4d9.ppt