557f20c67f85a1e83735d8d719d138ca.ppt
- Количество слайдов: 68
 ACR guidelines on Contrast Reactions and Management Z Liu, PGY-3 Boston University Medical Center, Department of Diagnostic Radiology Last reviewed May 9, 2015
ACR guidelines on Contrast Reactions and Management Z Liu, PGY-3 Boston University Medical Center, Department of Diagnostic Radiology Last reviewed May 9, 2015
 Disclaimer • The information provided herein is designed to aid in the BMC contrast reaction simulation course and may contain errors. • All treatments listed herein are for ADULTS. • DO NOT REFER TO THIS INFORMATION FOR ACTUAL PATIENT CARE Thank you, Your Radiology Simulation Team May 9, 2015
Disclaimer • The information provided herein is designed to aid in the BMC contrast reaction simulation course and may contain errors. • All treatments listed herein are for ADULTS. • DO NOT REFER TO THIS INFORMATION FOR ACTUAL PATIENT CARE Thank you, Your Radiology Simulation Team May 9, 2015
 INDEX Abbreviations 1. IV contrast media types 2. Risk factors for contrast reactions 3. Contrast related adverse reactions (CIN, NSF, etc) 4. IV contrast and pregnant patients 5. IV contrast and breast feeding 6. Premedication and BMC regime 7. Acute contrast reactions and management (per ACR guidelines 2013) 8. Reaction rebound prevention 9. MR specific protocol 10. Miscellaneous (translator phone, update allergy on Epic) References
INDEX Abbreviations 1. IV contrast media types 2. Risk factors for contrast reactions 3. Contrast related adverse reactions (CIN, NSF, etc) 4. IV contrast and pregnant patients 5. IV contrast and breast feeding 6. Premedication and BMC regime 7. Acute contrast reactions and management (per ACR guidelines 2013) 8. Reaction rebound prevention 9. MR specific protocol 10. Miscellaneous (translator phone, update allergy on Epic) References
 Abbreviations CIN Contrast-induced nephrotoxicity NSF Nephrogenic Systemic Fibrosis HOCM High-osmolality contrast media
Abbreviations CIN Contrast-induced nephrotoxicity NSF Nephrogenic Systemic Fibrosis HOCM High-osmolality contrast media
 Back to Index IV contrast media types
Back to Index IV contrast media types
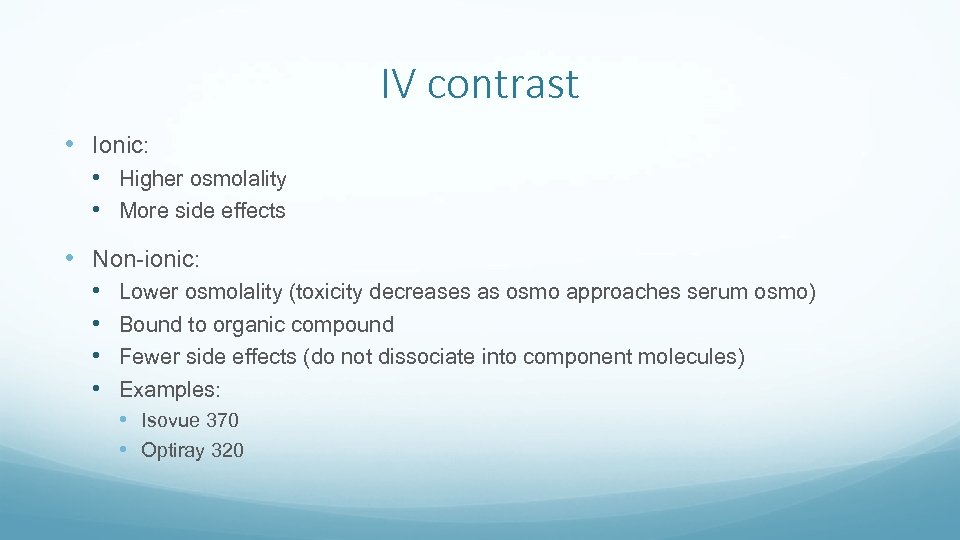 IV contrast • Ionic: • Higher osmolality • More side effects • Non-ionic: • • Lower osmolality (toxicity decreases as osmo approaches serum osmo) Bound to organic compound Fewer side effects (do not dissociate into component molecules) Examples: • Isovue 370 • Optiray 320
IV contrast • Ionic: • Higher osmolality • More side effects • Non-ionic: • • Lower osmolality (toxicity decreases as osmo approaches serum osmo) Bound to organic compound Fewer side effects (do not dissociate into component molecules) Examples: • Isovue 370 • Optiray 320
 MR IV contrast agents Gadolinium (Gd): Paramagnetic Most commonly used Chelated form- bind to an organic compound Extracellular fluid agents Ionic (Magnevist) Non ionic (Prohance) Blood pool agents Albumin-binding (Ablavar) Organ specific agent Eovist (liver)
MR IV contrast agents Gadolinium (Gd): Paramagnetic Most commonly used Chelated form- bind to an organic compound Extracellular fluid agents Ionic (Magnevist) Non ionic (Prohance) Blood pool agents Albumin-binding (Ablavar) Organ specific agent Eovist (liver)
 Back to Index Contrast reactions
Back to Index Contrast reactions
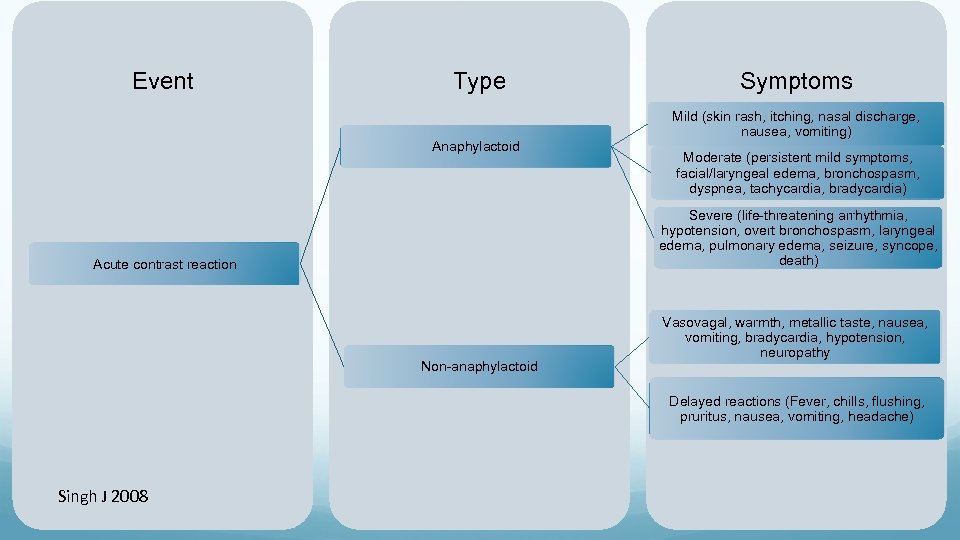 Event Type Anaphylactoid Symptoms Mild (skin rash, itching, nasal discharge, nausea, vomiting) Moderate (persistent mild symptoms, facial/laryngeal edema, bronchospasm, dyspnea, tachycardia, bradycardia) Severe (life-threatening arrhythmia, hypotension, overt bronchospasm, laryngeal edema, pulmonary edema, seizure, syncope, death) Acute contrast reaction Non-anaphylactoid Vasovagal, warmth, metallic taste, nausea, vomiting, bradycardia, hypotension, neuropathy Delayed reactions (Fever, chills, flushing, pruritus, nausea, vomiting, headache) Singh J 2008
Event Type Anaphylactoid Symptoms Mild (skin rash, itching, nasal discharge, nausea, vomiting) Moderate (persistent mild symptoms, facial/laryngeal edema, bronchospasm, dyspnea, tachycardia, bradycardia) Severe (life-threatening arrhythmia, hypotension, overt bronchospasm, laryngeal edema, pulmonary edema, seizure, syncope, death) Acute contrast reaction Non-anaphylactoid Vasovagal, warmth, metallic taste, nausea, vomiting, bradycardia, hypotension, neuropathy Delayed reactions (Fever, chills, flushing, pruritus, nausea, vomiting, headache) Singh J 2008
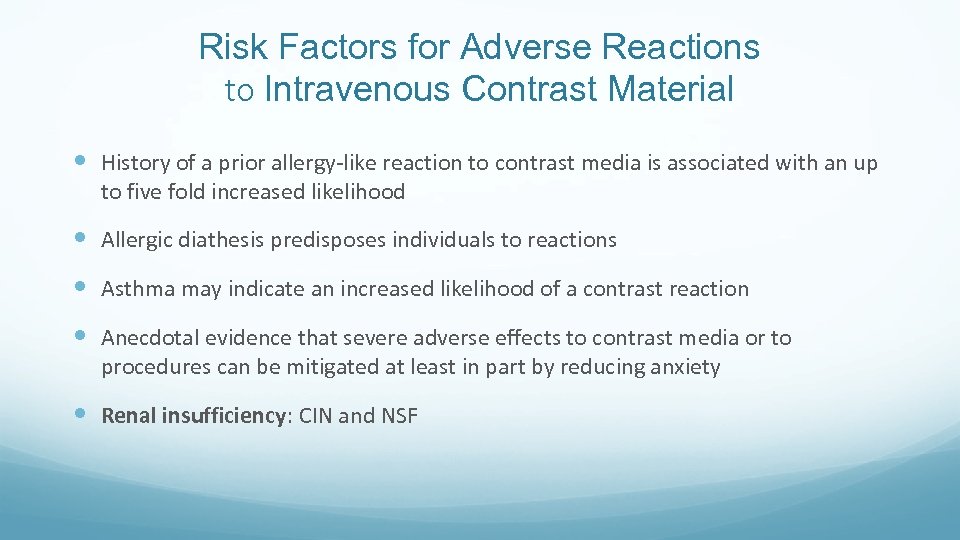 Risk Factors for Adverse Reactions to Intravenous Contrast Material History of a prior allergy-like reaction to contrast media is associated with an up to five fold increased likelihood Allergic diathesis predisposes individuals to reactions Asthma may indicate an increased likelihood of a contrast reaction Anecdotal evidence that severe adverse effects to contrast media or to procedures can be mitigated at least in part by reducing anxiety Renal insufficiency: CIN and NSF
Risk Factors for Adverse Reactions to Intravenous Contrast Material History of a prior allergy-like reaction to contrast media is associated with an up to five fold increased likelihood Allergic diathesis predisposes individuals to reactions Asthma may indicate an increased likelihood of a contrast reaction Anecdotal evidence that severe adverse effects to contrast media or to procedures can be mitigated at least in part by reducing anxiety Renal insufficiency: CIN and NSF
 Other risks Significant cardiac disease may be a risk factor for contrast reactions. These include symptomatic patients: patients with angina or congestive heart failure symptoms with minimal exertion patients with severe aortic stenosis, primary pulmonary hypertension, or severe but wellcompensated cardiomyopathy. Limit the volume and osmolality of the contrast media Paraproteinemias, particularly multiple myeloma, are known to predispose patients to irreversible renal failure after high-osmolality contrast media (HOCM) administration due to tubular protein precipitation and aggregation; however, there is no data predicting risk with the use of low-osmolality or isoosmolality agents. More on risk factors: ACR Manual on Contrast Media Version 9, 2013
Other risks Significant cardiac disease may be a risk factor for contrast reactions. These include symptomatic patients: patients with angina or congestive heart failure symptoms with minimal exertion patients with severe aortic stenosis, primary pulmonary hypertension, or severe but wellcompensated cardiomyopathy. Limit the volume and osmolality of the contrast media Paraproteinemias, particularly multiple myeloma, are known to predispose patients to irreversible renal failure after high-osmolality contrast media (HOCM) administration due to tubular protein precipitation and aggregation; however, there is no data predicting risk with the use of low-osmolality or isoosmolality agents. More on risk factors: ACR Manual on Contrast Media Version 9, 2013
 Thyroid disease and IV contrast Some patients with hyperthyroidism or other thyroid disease (especially when present in those who live in iodine-deficient areas) may develop iodine-provoked delayed hyperthyroidism. This effect may appear 4 to 6 weeks after the IV contrast administration in some of these patients. BMC Policy: [Pending policy update]
Thyroid disease and IV contrast Some patients with hyperthyroidism or other thyroid disease (especially when present in those who live in iodine-deficient areas) may develop iodine-provoked delayed hyperthyroidism. This effect may appear 4 to 6 weeks after the IV contrast administration in some of these patients. BMC Policy: [Pending policy update]
 Sickle cell trait or disease Risk to sickle cell patients from IV administered GBCM at currently approved dosages must be extremely low, and there is no reason to withhold these agents from patients with sickle cell disease. However, as in all patients, GBCM should be administered only when clinically indicated.
Sickle cell trait or disease Risk to sickle cell patients from IV administered GBCM at currently approved dosages must be extremely low, and there is no reason to withhold these agents from patients with sickle cell disease. However, as in all patients, GBCM should be administered only when clinically indicated.
 Metformin does not confer an increased risk of CIN. However, metformin can very rarely lead to lactic acidosis in patients with renal failure. Therefore, patients who develop CIN while taking metformin are susceptible to the development of lactic acidosis BMC policy: [Pending policy update]
Metformin does not confer an increased risk of CIN. However, metformin can very rarely lead to lactic acidosis in patients with renal failure. Therefore, patients who develop CIN while taking metformin are susceptible to the development of lactic acidosis BMC policy: [Pending policy update]
 Neonates and infants In children, it is prudent to follow the same guidelines that apply to adults. It should be noted, however, that e. GFR values in certain premature infants and neonates may be < 30 ml/min/1. 73 m 2 simply due to immature renal function (and not due to pathologic renal impairment). In these individuals, the ACR Committee on Drugs and Contrast Media believes that caution should still be used when administering GBCAs, although an e. GFR value < 30 ml/min/1. 73 m 2 should not be considered an absolute contraindication to GBCA administration.
Neonates and infants In children, it is prudent to follow the same guidelines that apply to adults. It should be noted, however, that e. GFR values in certain premature infants and neonates may be < 30 ml/min/1. 73 m 2 simply due to immature renal function (and not due to pathologic renal impairment). In these individuals, the ACR Committee on Drugs and Contrast Media believes that caution should still be used when administering GBCAs, although an e. GFR value < 30 ml/min/1. 73 m 2 should not be considered an absolute contraindication to GBCA administration.
 Back to Index Contrast related adverse reactions
Back to Index Contrast related adverse reactions
 Mechanisms of anaphylactoid contrast reactions ~90% of such adverse reactions are associated with direct release of histamine and other mediators from circulating basophils and eosinophils. Why use IV methylprednisone? Reduction in circulating basophils and eosinophils (which reach maximal statistical significance at the end of 4 hours). A reduction of histamine in sedimented leukocytes is also noted at 4 hours. Many of these effects reach their maximum at 8 hours.
Mechanisms of anaphylactoid contrast reactions ~90% of such adverse reactions are associated with direct release of histamine and other mediators from circulating basophils and eosinophils. Why use IV methylprednisone? Reduction in circulating basophils and eosinophils (which reach maximal statistical significance at the end of 4 hours). A reduction of histamine in sedimented leukocytes is also noted at 4 hours. Many of these effects reach their maximum at 8 hours.
 Nephrogenic systemic fibrosis Fibrosing disease involving skin and subcutaneous tissues, also lungs, esophagus, heart, skeletal muscles (contractures and joint immobility). Initial symptoms: skin thickening and or pruritis BMC policy: [Pending policy update]
Nephrogenic systemic fibrosis Fibrosing disease involving skin and subcutaneous tissues, also lungs, esophagus, heart, skeletal muscles (contractures and joint immobility). Initial symptoms: skin thickening and or pruritis BMC policy: [Pending policy update]
 Delayed reactions to contrast media Incidence: 0. 5 to 14%. Most commonly cutaneous (urticarial and/or a persistent rash) and may develop from 30 to 60 minutes to up to one week following contrast material exposure, with the majority occurring between three hours and two days. Treatment: supportive, antihistamines and or corticosteroids for cutaneous symptoms, antipyretics for fever, antiemetics for nausea, and fluid resuscitation for hypotension. REMEMBER: Nearly all life-threatening contrast reactions occur within the first 20 minutes after contrast medium injection.
Delayed reactions to contrast media Incidence: 0. 5 to 14%. Most commonly cutaneous (urticarial and/or a persistent rash) and may develop from 30 to 60 minutes to up to one week following contrast material exposure, with the majority occurring between three hours and two days. Treatment: supportive, antihistamines and or corticosteroids for cutaneous symptoms, antipyretics for fever, antiemetics for nausea, and fluid resuscitation for hypotension. REMEMBER: Nearly all life-threatening contrast reactions occur within the first 20 minutes after contrast medium injection.
 Contrast related reactions Air embolism Contrast induced nephrotoxicity Nephrogenic systemic fibrosis Delay reactions Acute contrast reactions (mild, moderate, severe/anaphylactic)
Contrast related reactions Air embolism Contrast induced nephrotoxicity Nephrogenic systemic fibrosis Delay reactions Acute contrast reactions (mild, moderate, severe/anaphylactic)
 Air embolism • Extremely rare complication • Power injection minimizes risk • Air bubbles or air fluid levels in the intrathoracic veins, main PA, or RV. • Symptoms: air hunger, dyspnea, cough, chest pain, pulmonary edema, tachycardia, hypotension, or expiratory wheezing. Neurologic deficits may result from stroke due to decreased cardiac output or paradoxical air embolism. • Treatment: 100% oxygen and placing the patient in the left lateral decubitus position (i. e. , left side down).
Air embolism • Extremely rare complication • Power injection minimizes risk • Air bubbles or air fluid levels in the intrathoracic veins, main PA, or RV. • Symptoms: air hunger, dyspnea, cough, chest pain, pulmonary edema, tachycardia, hypotension, or expiratory wheezing. Neurologic deficits may result from stroke due to decreased cardiac output or paradoxical air embolism. • Treatment: 100% oxygen and placing the patient in the left lateral decubitus position (i. e. , left side down).
 Contrast induced nephrotoxicity • Pathophysiology: unclear but suggested etiologies include renal hemodynamic changes (vasoconstriction) and direct tubular toxicity • Absolute increase of Cr of 0. 5 mg/d. L. • Risk factors: pre-existing renal insufficiency, acute kidney injury • Other independent risk factors: diabetes mellitus, dehydration, cardiovascular disease, diuretic use, advanced age, multiple myeloma, hypertension, hyperuricemia, and multiple iodinated contrast medium doses in a short time interval (< 24 hours) • BMC policy: [Pending policy update]
Contrast induced nephrotoxicity • Pathophysiology: unclear but suggested etiologies include renal hemodynamic changes (vasoconstriction) and direct tubular toxicity • Absolute increase of Cr of 0. 5 mg/d. L. • Risk factors: pre-existing renal insufficiency, acute kidney injury • Other independent risk factors: diabetes mellitus, dehydration, cardiovascular disease, diuretic use, advanced age, multiple myeloma, hypertension, hyperuricemia, and multiple iodinated contrast medium doses in a short time interval (< 24 hours) • BMC policy: [Pending policy update]
 Back to Index IV contrast and pregnant patients
Back to Index IV contrast and pregnant patients
![IV contrast media and pregnant patients BMC policy: [Pending policy update] IV contrast media and pregnant patients BMC policy: [Pending policy update]](https://present5.com/presentation/557f20c67f85a1e83735d8d719d138ca/image-24.jpg) IV contrast media and pregnant patients BMC policy: [Pending policy update]
IV contrast media and pregnant patients BMC policy: [Pending policy update]
 Back to Index IV contrast and breast feeding
Back to Index IV contrast and breast feeding
 IV contrast media and breast feeding Plasma half life of IV contrast is ~ 2 hours Nearly 100% of contrast media is cleared renally within 24 hours given normal renal function <1 % is excreted into breast milk in first 24 hours so it is safe for the mother and infant to continue breast-feeding after receiving such an agent BMC policy: [Pending policy update]
IV contrast media and breast feeding Plasma half life of IV contrast is ~ 2 hours Nearly 100% of contrast media is cleared renally within 24 hours given normal renal function <1 % is excreted into breast milk in first 24 hours so it is safe for the mother and infant to continue breast-feeding after receiving such an agent BMC policy: [Pending policy update]
 Back to Index Premedication and BMC regime
Back to Index Premedication and BMC regime
 Premedication No randomized controlled clinical trials have demonstrated premedication protection against severe life-threatening adverse reactions. Target premedication to those whom, in the past, have had moderately severe or severe reactions requiring treatment. Oral administration of steroids is preferable to IV administration, and prednisone and methylprednisolone are equally effective. It is preferred that steroids be given beginning at least 6 hours prior to the injection of contrast media regardless of the route of steroid administration whenever possible. BMC policy: Pending policy update
Premedication No randomized controlled clinical trials have demonstrated premedication protection against severe life-threatening adverse reactions. Target premedication to those whom, in the past, have had moderately severe or severe reactions requiring treatment. Oral administration of steroids is preferable to IV administration, and prednisone and methylprednisolone are equally effective. It is preferred that steroids be given beginning at least 6 hours prior to the injection of contrast media regardless of the route of steroid administration whenever possible. BMC policy: Pending policy update
 BMC Premedication regime Patients who are able to take medication orally: Prednisone 50 mg tablet by mouth at 13 hours, 7 hours, and 1 hour before injection of contrast media. Or Methylprednisolone (Medrol®) 32 mg tablet by mouth at 12 hours and 2 hours before the injection of contrast media. Plus Diphenhydramine (Benadryl®) 50 mg intravenously, intramuscularly or by mouth 1 hour before the injection of contrast media.
BMC Premedication regime Patients who are able to take medication orally: Prednisone 50 mg tablet by mouth at 13 hours, 7 hours, and 1 hour before injection of contrast media. Or Methylprednisolone (Medrol®) 32 mg tablet by mouth at 12 hours and 2 hours before the injection of contrast media. Plus Diphenhydramine (Benadryl®) 50 mg intravenously, intramuscularly or by mouth 1 hour before the injection of contrast media.
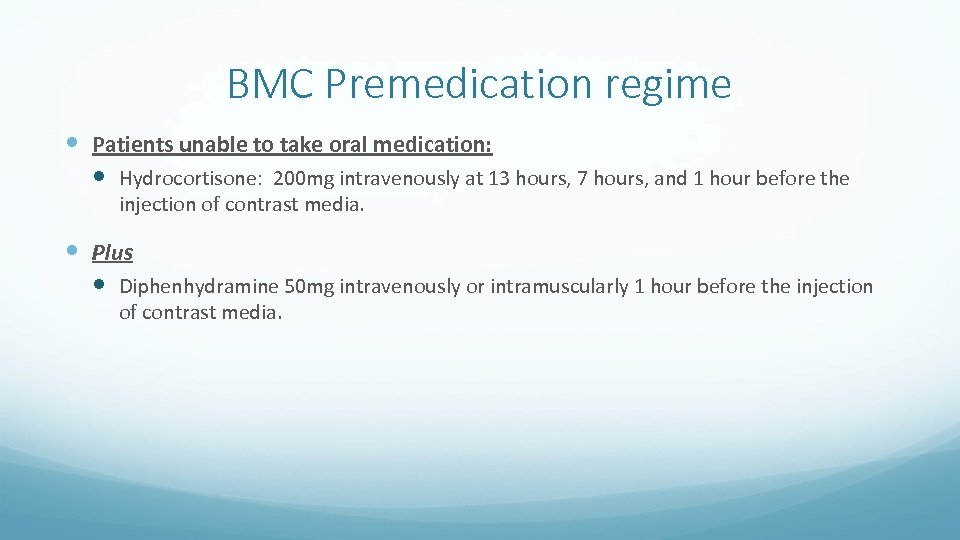 BMC Premedication regime Patients unable to take oral medication: Hydrocortisone: 200 mg intravenously at 13 hours, 7 hours, and 1 hour before the injection of contrast media. Plus Diphenhydramine 50 mg intravenously or intramuscularly 1 hour before the injection of contrast media.
BMC Premedication regime Patients unable to take oral medication: Hydrocortisone: 200 mg intravenously at 13 hours, 7 hours, and 1 hour before the injection of contrast media. Plus Diphenhydramine 50 mg intravenously or intramuscularly 1 hour before the injection of contrast media.
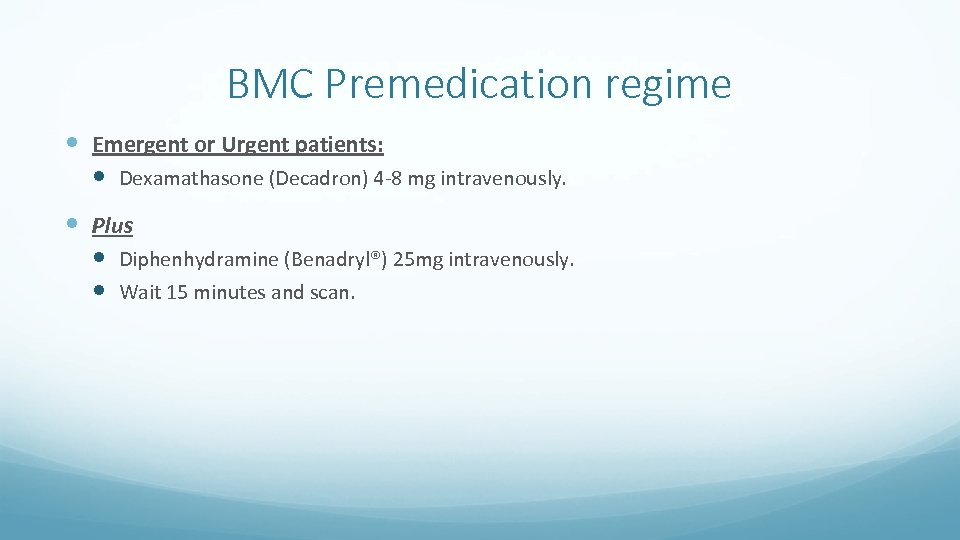 BMC Premedication regime Emergent or Urgent patients: Dexamathasone (Decadron) 4 -8 mg intravenously. Plus Diphenhydramine (Benadryl®) 25 mg intravenously. Wait 15 minutes and scan.
BMC Premedication regime Emergent or Urgent patients: Dexamathasone (Decadron) 4 -8 mg intravenously. Plus Diphenhydramine (Benadryl®) 25 mg intravenously. Wait 15 minutes and scan.
 Back to Index Contrast reactions & management
Back to Index Contrast reactions & management
 Assessing for potential contrast reaction How does the patient look? Can the patient speak? How does the patient’s voice sound? How is the patient’s breathing? What is the patient’s pulse strength and rate? What is the patient’s blood pressure?
Assessing for potential contrast reaction How does the patient look? Can the patient speak? How does the patient’s voice sound? How is the patient’s breathing? What is the patient’s pulse strength and rate? What is the patient’s blood pressure?
 Acute adverse reactions • May be allergic-like (not true allergy, often idiosyncratic and may differ immunologically from true allergies despite similar clinical presentations) or physiologic (a physiologic response to contrast material). • Mild • Moderate • Severe
Acute adverse reactions • May be allergic-like (not true allergy, often idiosyncratic and may differ immunologically from true allergies despite similar clinical presentations) or physiologic (a physiologic response to contrast material). • Mild • Moderate • Severe
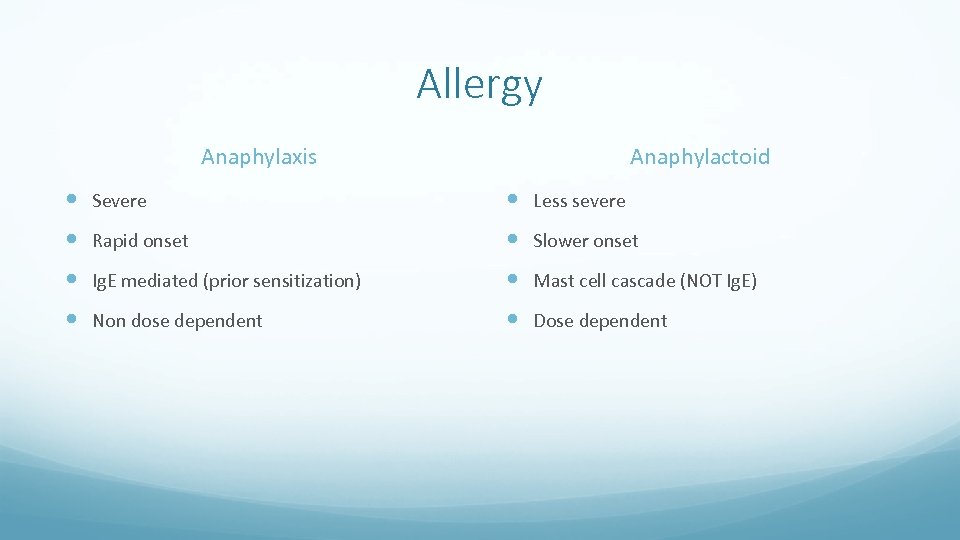 Allergy Anaphylaxis Anaphylactoid Severe Less severe Rapid onset Slower onset Ig. E mediated (prior sensitization) Mast cell cascade (NOT Ig. E) Non dose dependent Dose dependent
Allergy Anaphylaxis Anaphylactoid Severe Less severe Rapid onset Slower onset Ig. E mediated (prior sensitization) Mast cell cascade (NOT Ig. E) Non dose dependent Dose dependent
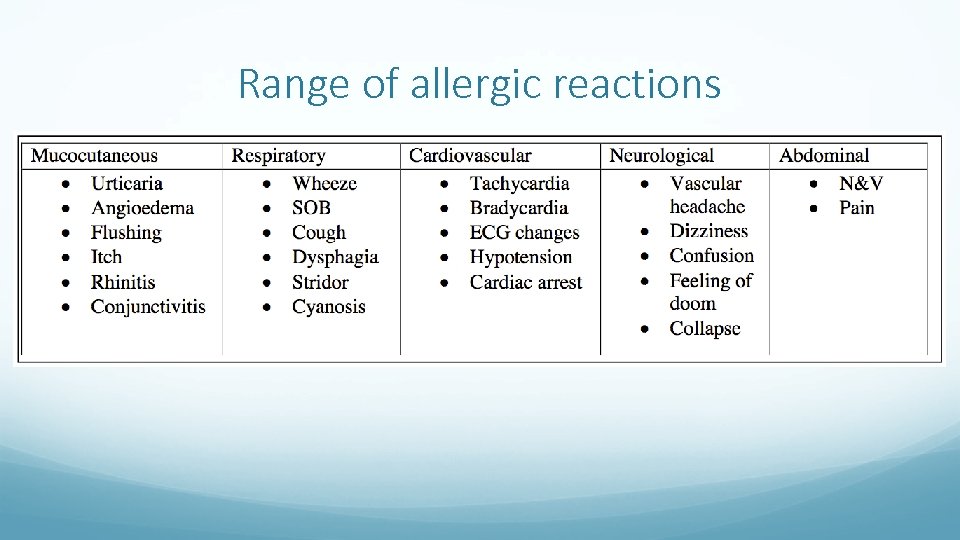 Range of allergic reactions
Range of allergic reactions
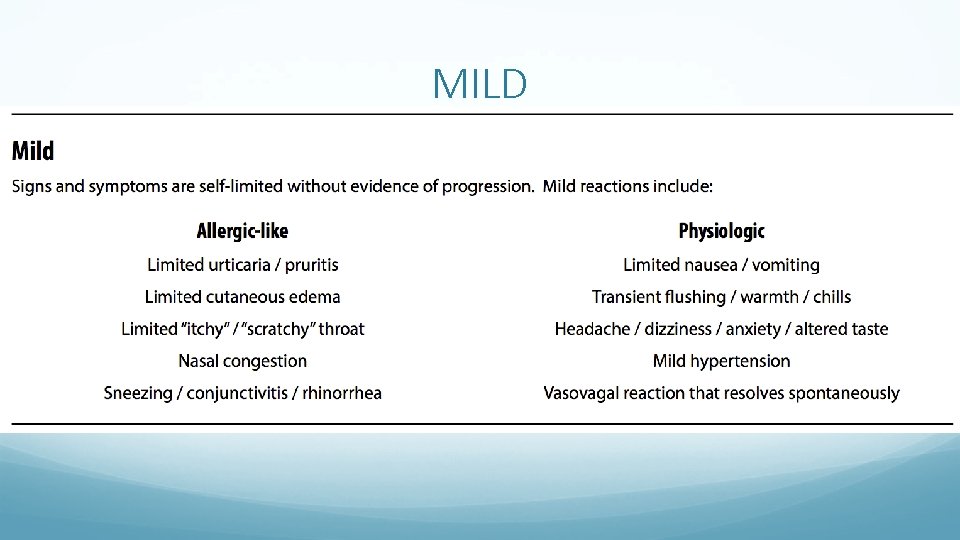 MILD
MILD
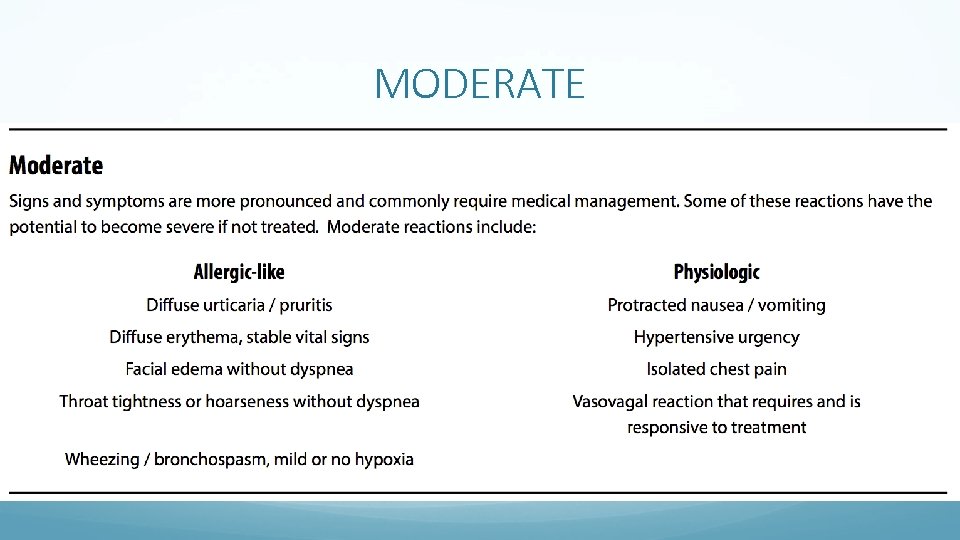 MODERATE
MODERATE
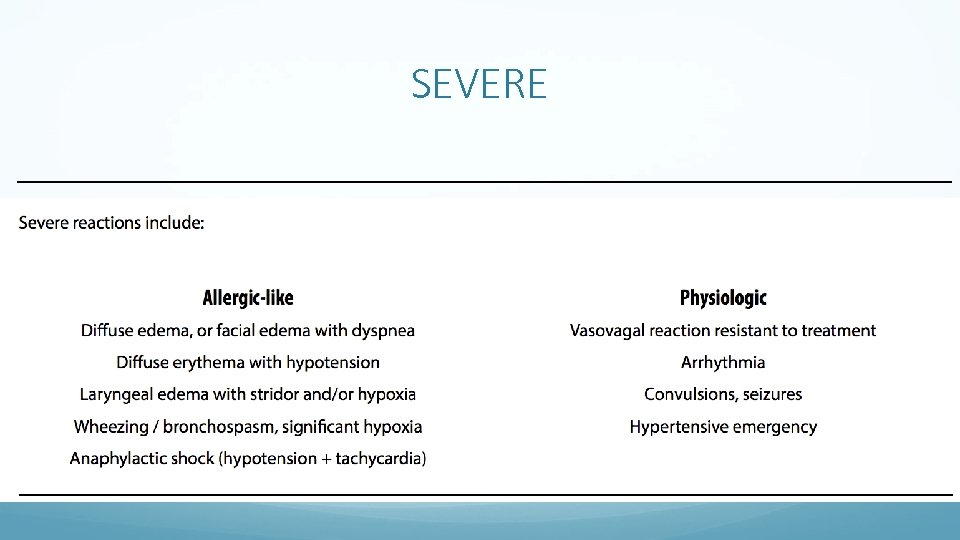 SEVERE
SEVERE
 Severe Cardiopulmonary arrest Pulmonary edema: rare
Severe Cardiopulmonary arrest Pulmonary edema: rare
 HIVES-GENERAL Observe patient until hives are resolving. Further observation may be necessary if treatment is administered. BMC policy: [Pending policy update]
HIVES-GENERAL Observe patient until hives are resolving. Further observation may be necessary if treatment is administered. BMC policy: [Pending policy update]
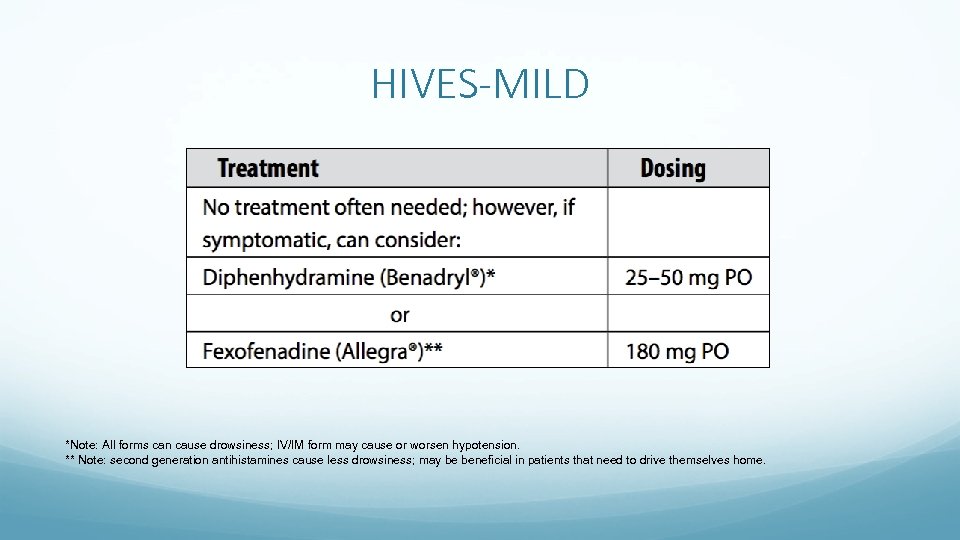 HIVES-MILD *Note: All forms can cause drowsiness; IV/IM form may cause or worsen hypotension. ** Note: second generation antihistamines cause less drowsiness; may be beneficial in patients that need to drive themselves home.
HIVES-MILD *Note: All forms can cause drowsiness; IV/IM form may cause or worsen hypotension. ** Note: second generation antihistamines cause less drowsiness; may be beneficial in patients that need to drive themselves home.
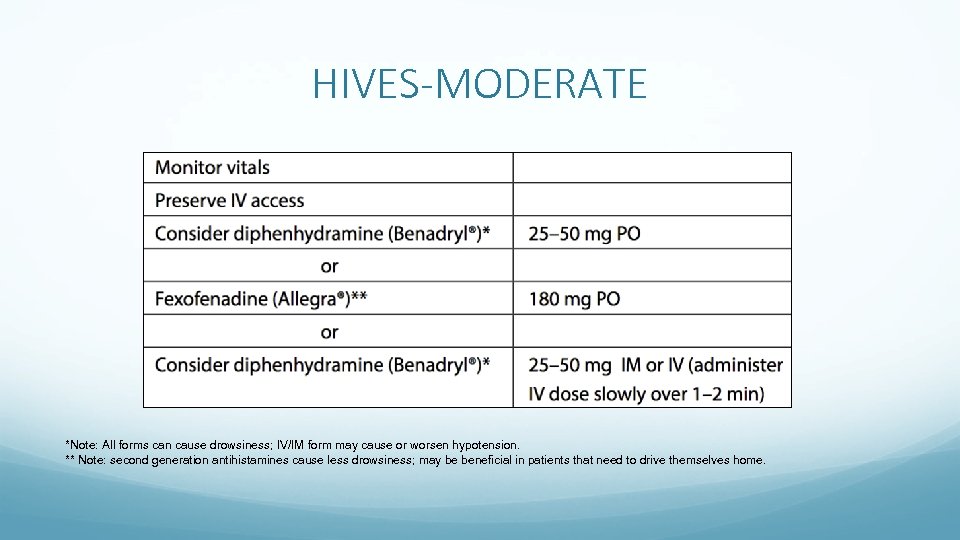 HIVES-MODERATE *Note: All forms can cause drowsiness; IV/IM form may cause or worsen hypotension. ** Note: second generation antihistamines cause less drowsiness; may be beneficial in patients that need to drive themselves home.
HIVES-MODERATE *Note: All forms can cause drowsiness; IV/IM form may cause or worsen hypotension. ** Note: second generation antihistamines cause less drowsiness; may be beneficial in patients that need to drive themselves home.
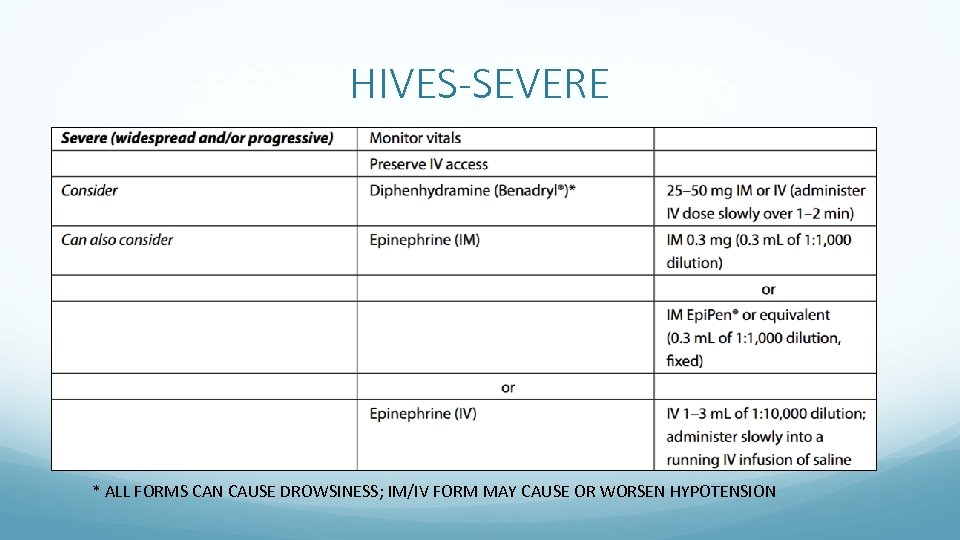 HIVES-SEVERE * ALL FORMS CAN CAUSE DROWSINESS; IM/IV FORM MAY CAUSE OR WORSEN HYPOTENSION
HIVES-SEVERE * ALL FORMS CAN CAUSE DROWSINESS; IM/IV FORM MAY CAUSE OR WORSEN HYPOTENSION
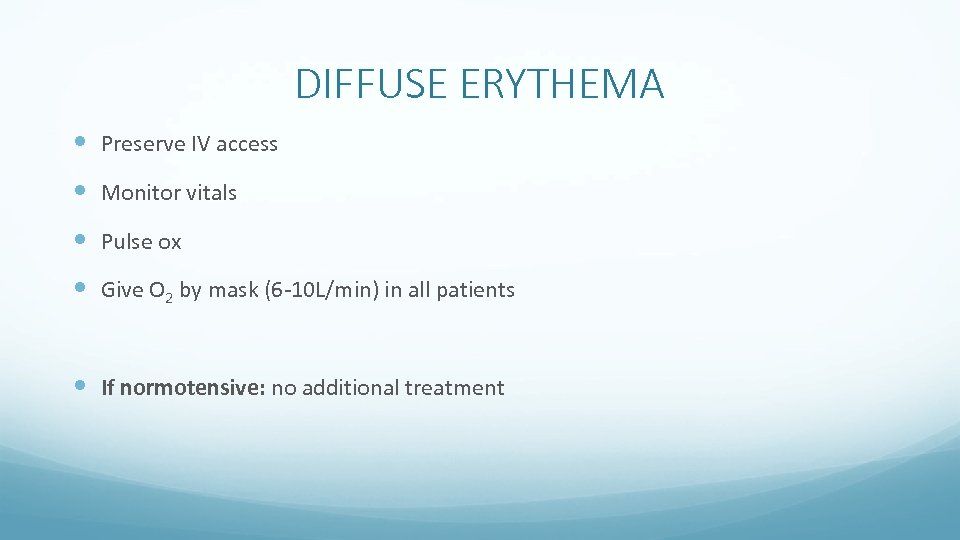 DIFFUSE ERYTHEMA Preserve IV access Monitor vitals Pulse ox Give O 2 by mask (6 -10 L/min) in all patients If normotensive: no additional treatment
DIFFUSE ERYTHEMA Preserve IV access Monitor vitals Pulse ox Give O 2 by mask (6 -10 L/min) in all patients If normotensive: no additional treatment
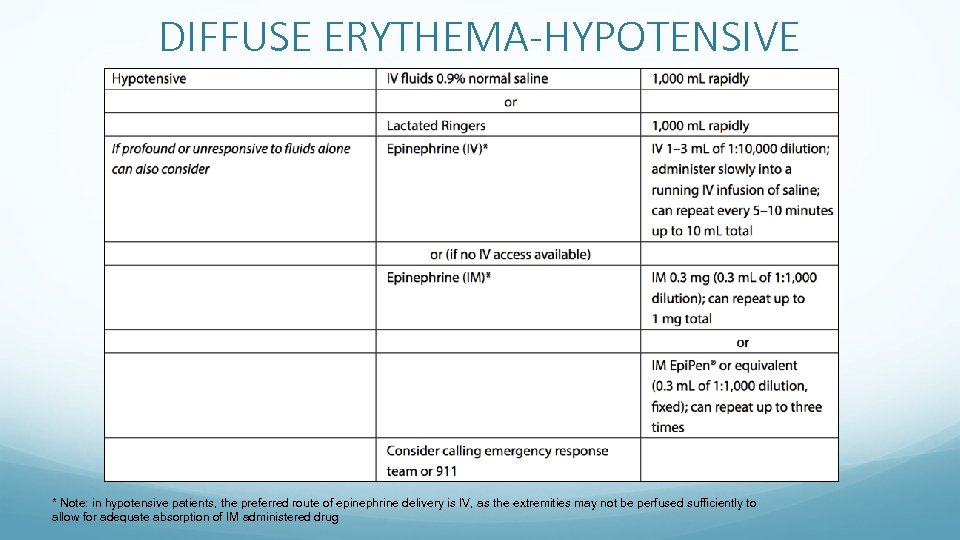 DIFFUSE ERYTHEMA-HYPOTENSIVE * Note: in hypotensive patients, the preferred route of epinephrine delivery is IV, as the extremities may not be perfused sufficiently to allow for adequate absorption of IM administered drug
DIFFUSE ERYTHEMA-HYPOTENSIVE * Note: in hypotensive patients, the preferred route of epinephrine delivery is IV, as the extremities may not be perfused sufficiently to allow for adequate absorption of IM administered drug
 Bronchospasm • Preserve IV access • Monitor vitals • Pulse ox • Give O 2 by mask (6 -10 L/min) in all patients
Bronchospasm • Preserve IV access • Monitor vitals • Pulse ox • Give O 2 by mask (6 -10 L/min) in all patients
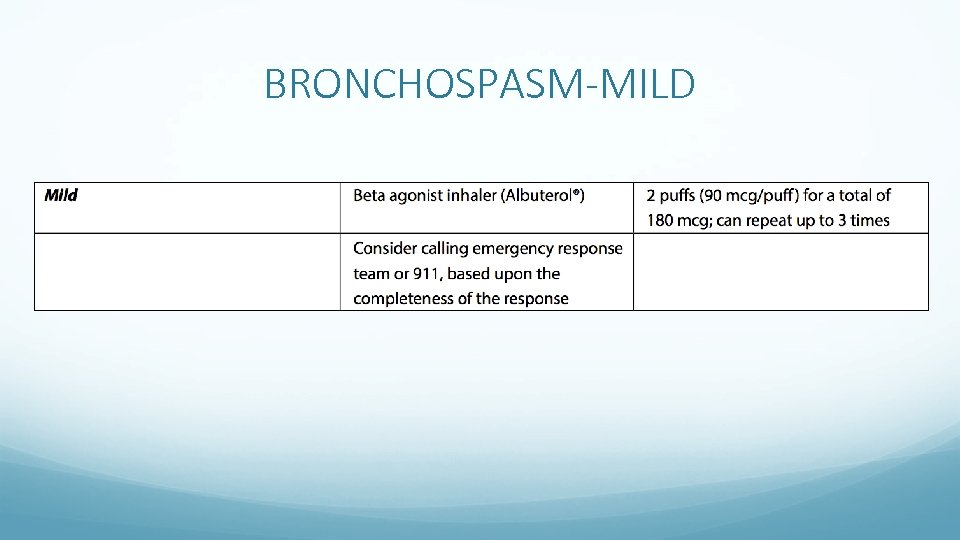 BRONCHOSPASM-MILD
BRONCHOSPASM-MILD
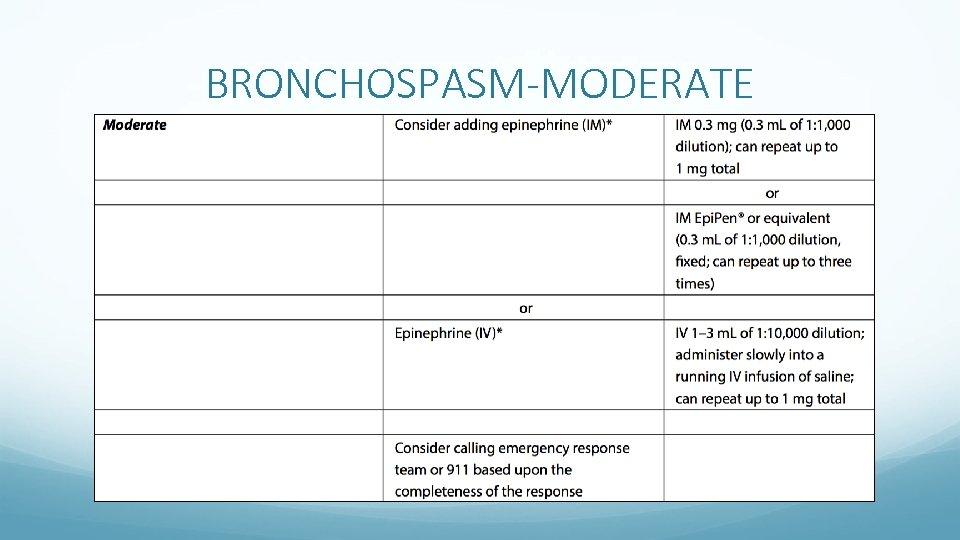 BRONCHOSPASM-MODERATE
BRONCHOSPASM-MODERATE
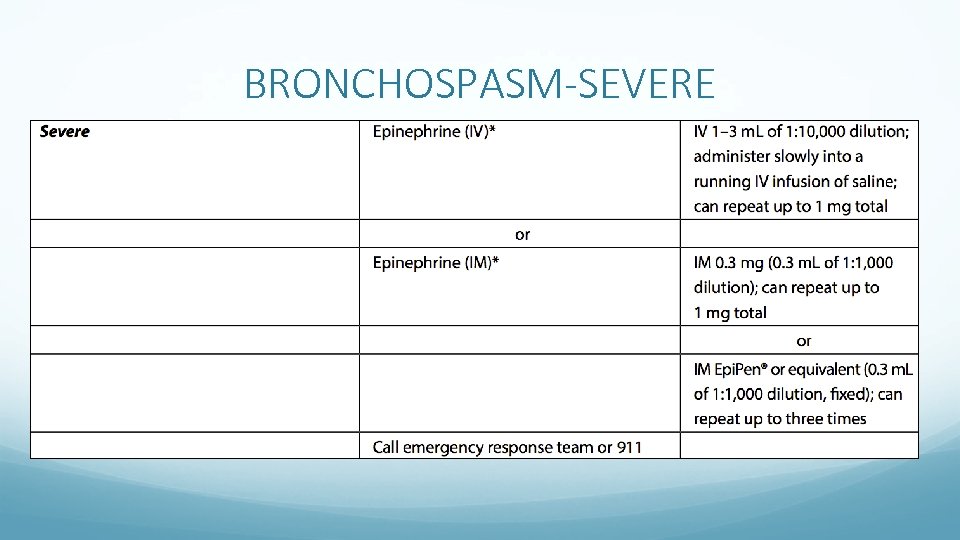 BRONCHOSPASM-SEVERE
BRONCHOSPASM-SEVERE
 Laryngeal Edema • Preserve IV access • Monitor vitals • Pulse ox • Give O 2 by mask (6 -10 L/min) in all patients
Laryngeal Edema • Preserve IV access • Monitor vitals • Pulse ox • Give O 2 by mask (6 -10 L/min) in all patients
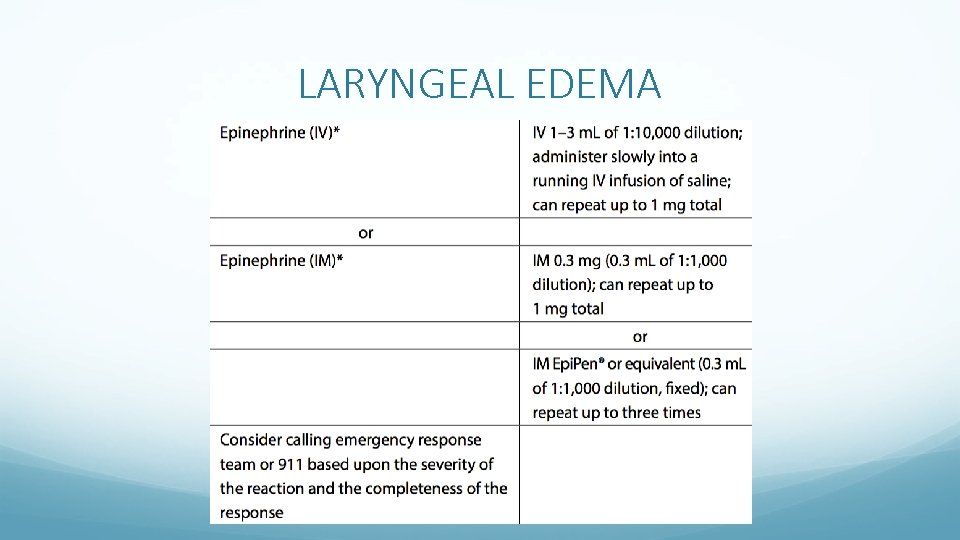 LARYNGEAL EDEMA
LARYNGEAL EDEMA
 Hypotension Systolic BP < 90 mm Hg Two forms: Hypotension with bradycardia Hypotension with tachycardia
Hypotension Systolic BP < 90 mm Hg Two forms: Hypotension with bradycardia Hypotension with tachycardia
 Hypotension Preserve IV access Monitor vitals Pulse ox Give O 2 by mask (6 -10 L/min) in all patients Elevate legs at least 60 degrees Consider IV fluids: 0. 9% Normal Saline or Latcted Ringers, 1, 000 m. L rapidly
Hypotension Preserve IV access Monitor vitals Pulse ox Give O 2 by mask (6 -10 L/min) in all patients Elevate legs at least 60 degrees Consider IV fluids: 0. 9% Normal Saline or Latcted Ringers, 1, 000 m. L rapidly
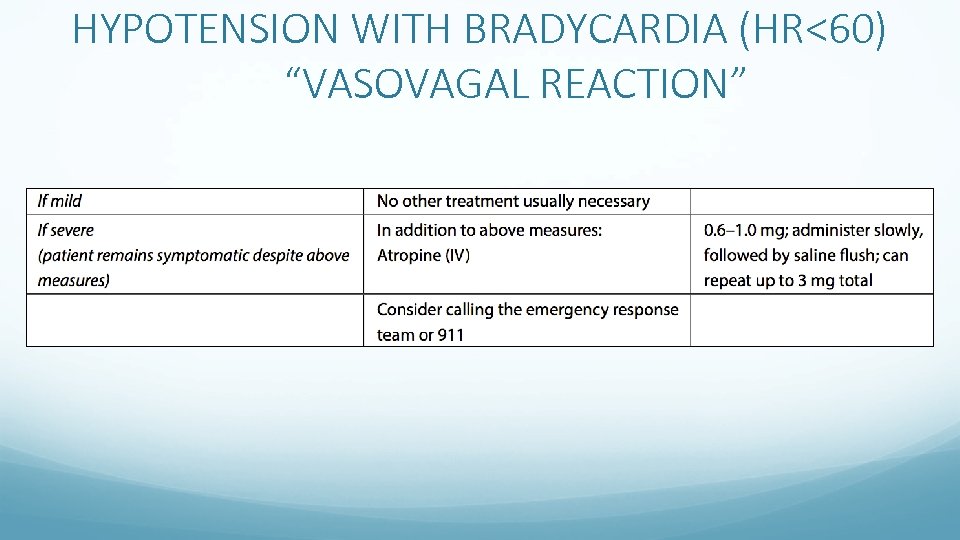 HYPOTENSION WITH BRADYCARDIA (HR<60) “VASOVAGAL REACTION”
HYPOTENSION WITH BRADYCARDIA (HR<60) “VASOVAGAL REACTION”
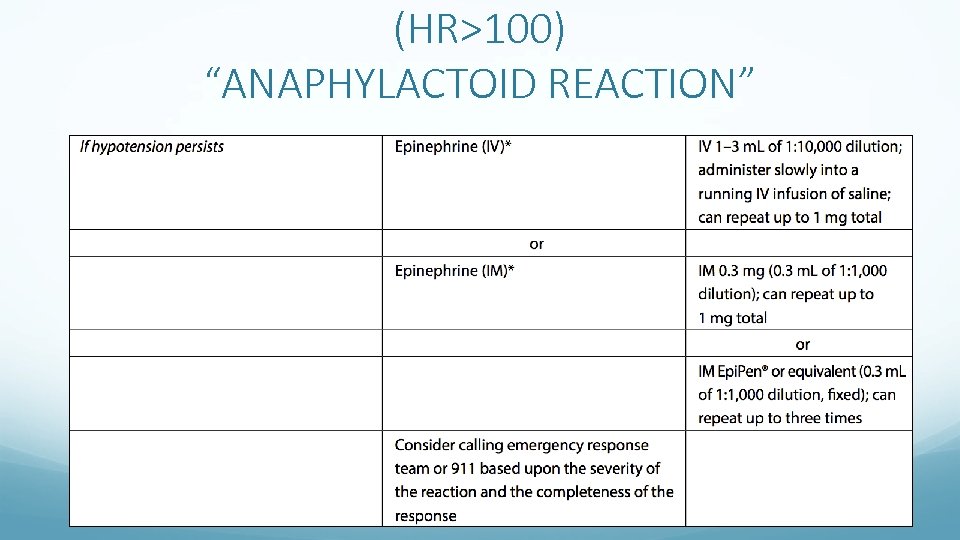 (HR>100) “ANAPHYLACTOID REACTION”
(HR>100) “ANAPHYLACTOID REACTION”
 UNRESPONSIVE AND PULSELESS • Apply BLS, ACLS • Activate emergency response team • If at Menino or ENC, call 4 -7777 • If at Shapiro, call public safety 4 -4444 (they will call 911)
UNRESPONSIVE AND PULSELESS • Apply BLS, ACLS • Activate emergency response team • If at Menino or ENC, call 4 -7777 • If at Shapiro, call public safety 4 -4444 (they will call 911)
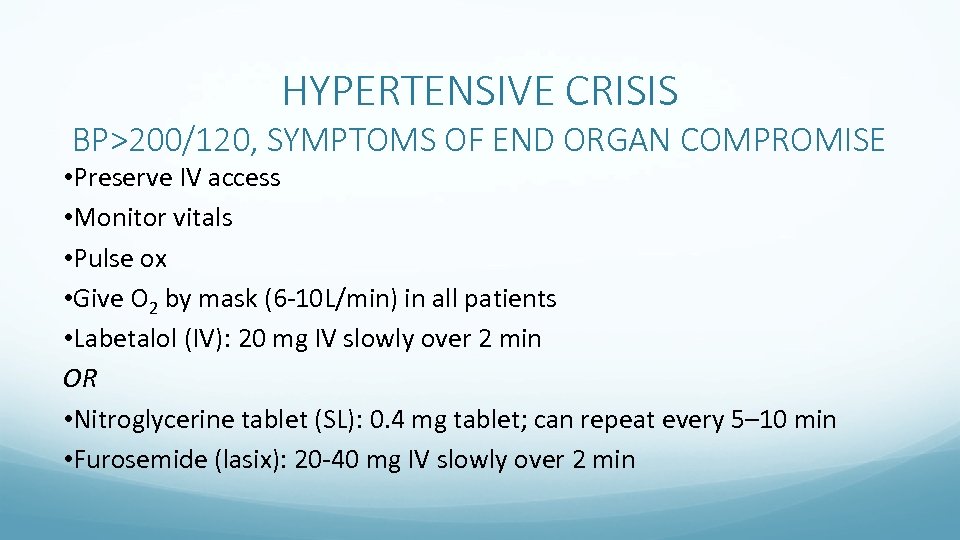 HYPERTENSIVE CRISIS BP>200/120, SYMPTOMS OF END ORGAN COMPROMISE • Preserve IV access • Monitor vitals • Pulse ox • Give O 2 by mask (6 -10 L/min) in all patients • Labetalol (IV): 20 mg IV slowly over 2 min OR • Nitroglycerine tablet (SL): 0. 4 mg tablet; can repeat every 5– 10 min • Furosemide (lasix): 20 -40 mg IV slowly over 2 min
HYPERTENSIVE CRISIS BP>200/120, SYMPTOMS OF END ORGAN COMPROMISE • Preserve IV access • Monitor vitals • Pulse ox • Give O 2 by mask (6 -10 L/min) in all patients • Labetalol (IV): 20 mg IV slowly over 2 min OR • Nitroglycerine tablet (SL): 0. 4 mg tablet; can repeat every 5– 10 min • Furosemide (lasix): 20 -40 mg IV slowly over 2 min
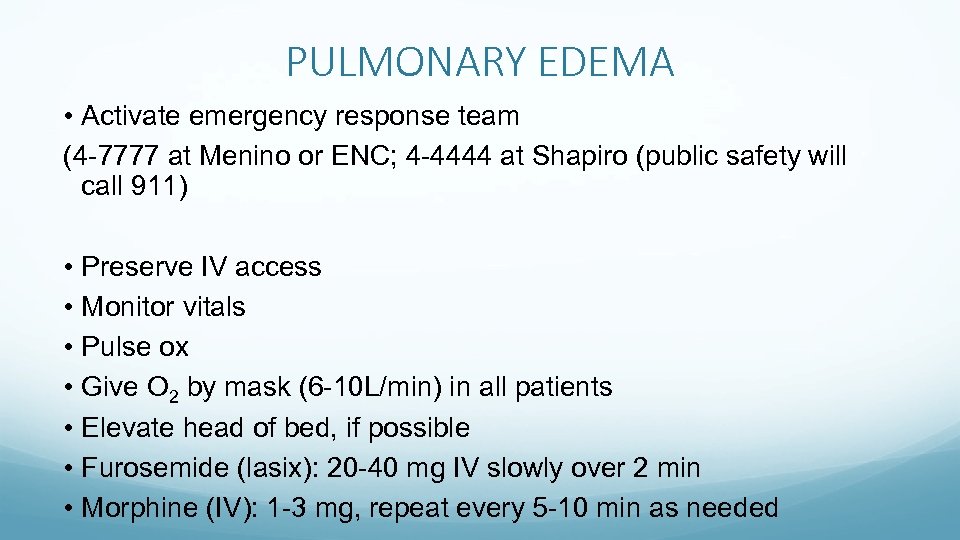 PULMONARY EDEMA • Activate emergency response team (4 -7777 at Menino or ENC; 4 -4444 at Shapiro (public safety will call 911) • Preserve IV access • Monitor vitals • Pulse ox • Give O 2 by mask (6 -10 L/min) in all patients • Elevate head of bed, if possible • Furosemide (lasix): 20 -40 mg IV slowly over 2 min • Morphine (IV): 1 -3 mg, repeat every 5 -10 min as needed
PULMONARY EDEMA • Activate emergency response team (4 -7777 at Menino or ENC; 4 -4444 at Shapiro (public safety will call 911) • Preserve IV access • Monitor vitals • Pulse ox • Give O 2 by mask (6 -10 L/min) in all patients • Elevate head of bed, if possible • Furosemide (lasix): 20 -40 mg IV slowly over 2 min • Morphine (IV): 1 -3 mg, repeat every 5 -10 min as needed
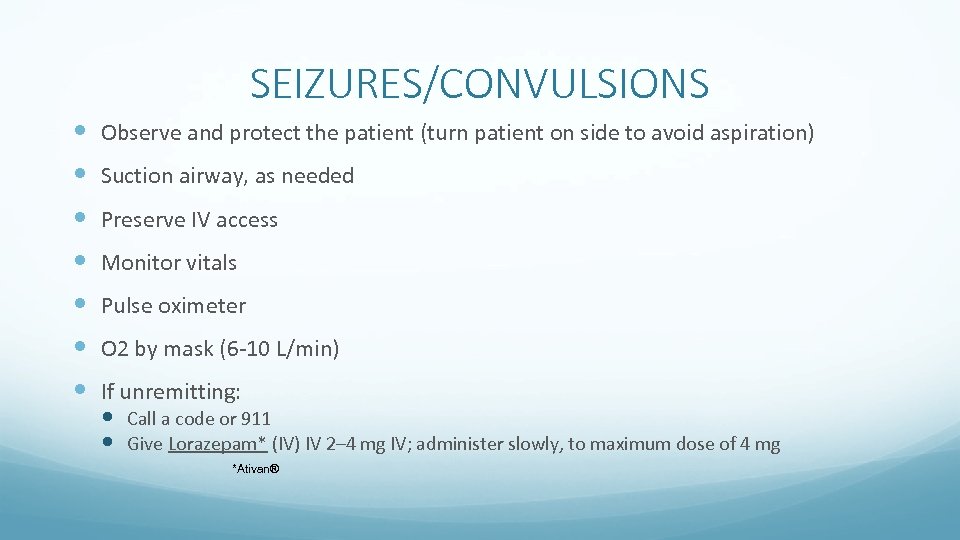 SEIZURES/CONVULSIONS Observe and protect the patient (turn patient on side to avoid aspiration) Suction airway, as needed Preserve IV access Monitor vitals Pulse oximeter O 2 by mask (6 -10 L/min) If unremitting: Call a code or 911 Give Lorazepam* (IV) IV 2– 4 mg IV; administer slowly, to maximum dose of 4 mg *Ativan®
SEIZURES/CONVULSIONS Observe and protect the patient (turn patient on side to avoid aspiration) Suction airway, as needed Preserve IV access Monitor vitals Pulse oximeter O 2 by mask (6 -10 L/min) If unremitting: Call a code or 911 Give Lorazepam* (IV) IV 2– 4 mg IV; administer slowly, to maximum dose of 4 mg *Ativan®
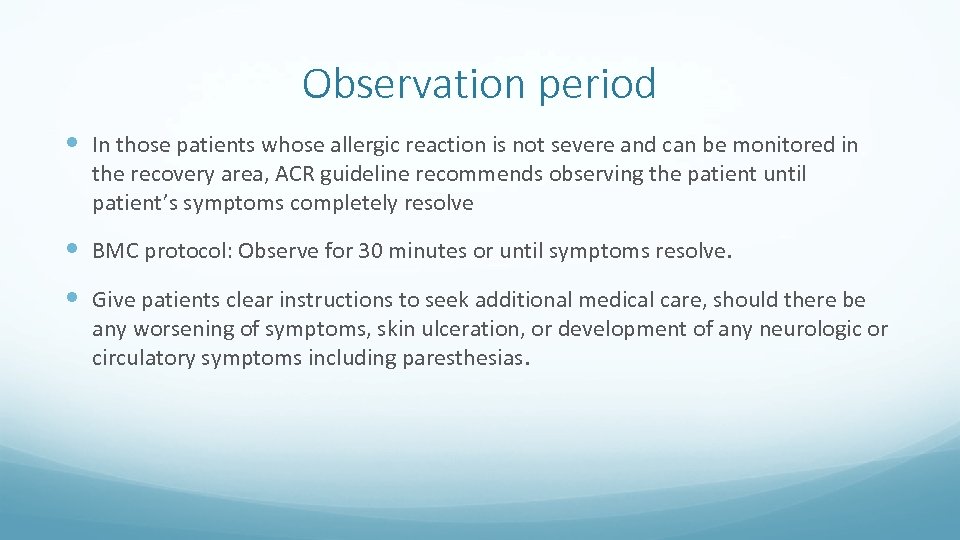 Observation period In those patients whose allergic reaction is not severe and can be monitored in the recovery area, ACR guideline recommends observing the patient until patient’s symptoms completely resolve BMC protocol: Observe for 30 minutes or until symptoms resolve. Give patients clear instructions to seek additional medical care, should there be any worsening of symptoms, skin ulceration, or development of any neurologic or circulatory symptoms including paresthesias.
Observation period In those patients whose allergic reaction is not severe and can be monitored in the recovery area, ACR guideline recommends observing the patient until patient’s symptoms completely resolve BMC protocol: Observe for 30 minutes or until symptoms resolve. Give patients clear instructions to seek additional medical care, should there be any worsening of symptoms, skin ulceration, or development of any neurologic or circulatory symptoms including paresthesias.
 Back to Index MR specific protocol
Back to Index MR specific protocol
 MR specific protocol Leave all metal objects at Zone II or III including cell phones, credit cards, etc. Must first transfer patient (in Zone IV) to Zone II (outside magnet area) on MRI compatible stretcher before any further assessment and treatment. Zone I: All areas freely accessible to the general public without supervision. Magnetic fringe fields in this area are less than 5 Gauss (0. 5 m. T). Zone II: Still a public area, but the interface between unregulated Zone I and the strictly controlled Zones III and IV. MR safety screening typically occurs here. Zone III: An area near the magnet room where the fringe, gradient, or RF magnetic fields are sufficiently strong to present a physical hazard to unscreened patients and personnel. Zone IV: Synonymous with the MR magnet room itself.
MR specific protocol Leave all metal objects at Zone II or III including cell phones, credit cards, etc. Must first transfer patient (in Zone IV) to Zone II (outside magnet area) on MRI compatible stretcher before any further assessment and treatment. Zone I: All areas freely accessible to the general public without supervision. Magnetic fringe fields in this area are less than 5 Gauss (0. 5 m. T). Zone II: Still a public area, but the interface between unregulated Zone I and the strictly controlled Zones III and IV. MR safety screening typically occurs here. Zone III: An area near the magnet room where the fringe, gradient, or RF magnetic fields are sufficiently strong to present a physical hazard to unscreened patients and personnel. Zone IV: Synonymous with the MR magnet room itself.
 Back to Index Miscellaneous (translator phone, update allergies on Epic)
Back to Index Miscellaneous (translator phone, update allergies on Epic)
 How to call a code At Menino and ENC: 4 -7777 At Shapiro: Call 4 -4444 (public safety will call 911) Know relevant information when calling a code (Name, adult vs child, location, type of contrast event, what happened, any pertinent medical history).
How to call a code At Menino and ENC: 4 -7777 At Shapiro: Call 4 -4444 (public safety will call 911) Know relevant information when calling a code (Name, adult vs child, location, type of contrast event, what happened, any pertinent medical history).
 How to use the translator phone If using the blue phone-press on the pre-programmed blue button or dial 7 -8787 to get a translator. Will ask for language, department you are calling from, and patient’s MRN. If using a white phone, dial 7 -6767. Follow the same steps as above. If using a red phone (in house translator), directly asks for an available in house translator (might have to wait).
How to use the translator phone If using the blue phone-press on the pre-programmed blue button or dial 7 -8787 to get a translator. Will ask for language, department you are calling from, and patient’s MRN. If using a white phone, dial 7 -6767. Follow the same steps as above. If using a red phone (in house translator), directly asks for an available in house translator (might have to wait).
 Updating allergic reaction on Epic Click on the allergies tab on the left hand side, click on add a new agent, a drop down menu will appear and you can add the new agent and the associated reactions. New contrast allergies can be updated by contacting CT manager Christine Seay.
Updating allergic reaction on Epic Click on the allergies tab on the left hand side, click on add a new agent, a drop down menu will appear and you can add the new agent and the associated reactions. New contrast allergies can be updated by contacting CT manager Christine Seay.
 References Back to Index ACR Manual on contrast media 2013 version 9 BMC Adverse reactions to contrast media and contrast extravasations BMC recommendation for serum creatinine for contrast administration BMC Guidelines for management of acute contrast reactions in adults BMC Contrast media allergy prophylactic medication regimens BMC contrast media and the pregnant patient Singh J, Daftary A. Iodinated contrast media and their adverse reactions. J Nucl Med Technol. 2008 Jun; 36(2): 69 -74; quiz 76 -7. doi: 10. 2967/jnmt. 107. 047621. Epub 2008 May 15. Review. Pub. Med PMID: 18483141. http: //mri-q. com/acr-safety-zones. html
References Back to Index ACR Manual on contrast media 2013 version 9 BMC Adverse reactions to contrast media and contrast extravasations BMC recommendation for serum creatinine for contrast administration BMC Guidelines for management of acute contrast reactions in adults BMC Contrast media allergy prophylactic medication regimens BMC contrast media and the pregnant patient Singh J, Daftary A. Iodinated contrast media and their adverse reactions. J Nucl Med Technol. 2008 Jun; 36(2): 69 -74; quiz 76 -7. doi: 10. 2967/jnmt. 107. 047621. Epub 2008 May 15. Review. Pub. Med PMID: 18483141. http: //mri-q. com/acr-safety-zones. html


