b1a5324849ad8f79a7da98b55ea60e01.ppt
- Количество слайдов: 41
 Achieving the Triple Aim: The Simultaneous Pursuit of ØPopulation Health ØEnhanced Individual Care ØControlled Costs David Labby MD Ph. D Medical Director Care. Oregon Health Policy Board Presentation May, 2010
Achieving the Triple Aim: The Simultaneous Pursuit of ØPopulation Health ØEnhanced Individual Care ØControlled Costs David Labby MD Ph. D Medical Director Care. Oregon Health Policy Board Presentation May, 2010
 The Institute for Healthcare Improvement (IHI) • • • Independent not-for-profit organization helping to lead the improvement of health care throughout the world. Founded in 1991 and based in Cambridge, Massachusetts, IHI works to accelerate improvement by building the will for change, cultivating promising concepts for improving patient care, and helping health care systems put those ideas into action. First Decade: identification and spread of best practices – The Breakthrough Series Collaborative model. Work was organized around reducing defects and errors in microsystems such as the ED or the ICU. • Second Decade : focus on innovation, R&D, – Broad-scale Idealized Design projects, such as the Office Practice and the Medication System – Pursuing Perfection initiative in 2002 with the Robert Wood Johnson Foundation, working with ambitious organizations seeking total transformation of all major care processes. – 100, 000 Lives Campaign and 5 Million Lives Campaign, in which IHI spread best practice changes to thousands of hospitals through the United States, and created a national network for improvement focused on reducing needless deaths and preventing harm from care. • IHI is currently engaged in improvement initiatives in England, Scotland, Ghana, Malawi, and South Africa. www. ihi. org
The Institute for Healthcare Improvement (IHI) • • • Independent not-for-profit organization helping to lead the improvement of health care throughout the world. Founded in 1991 and based in Cambridge, Massachusetts, IHI works to accelerate improvement by building the will for change, cultivating promising concepts for improving patient care, and helping health care systems put those ideas into action. First Decade: identification and spread of best practices – The Breakthrough Series Collaborative model. Work was organized around reducing defects and errors in microsystems such as the ED or the ICU. • Second Decade : focus on innovation, R&D, – Broad-scale Idealized Design projects, such as the Office Practice and the Medication System – Pursuing Perfection initiative in 2002 with the Robert Wood Johnson Foundation, working with ambitious organizations seeking total transformation of all major care processes. – 100, 000 Lives Campaign and 5 Million Lives Campaign, in which IHI spread best practice changes to thousands of hospitals through the United States, and created a national network for improvement focused on reducing needless deaths and preventing harm from care. • IHI is currently engaged in improvement initiatives in England, Scotland, Ghana, Malawi, and South Africa. www. ihi. org
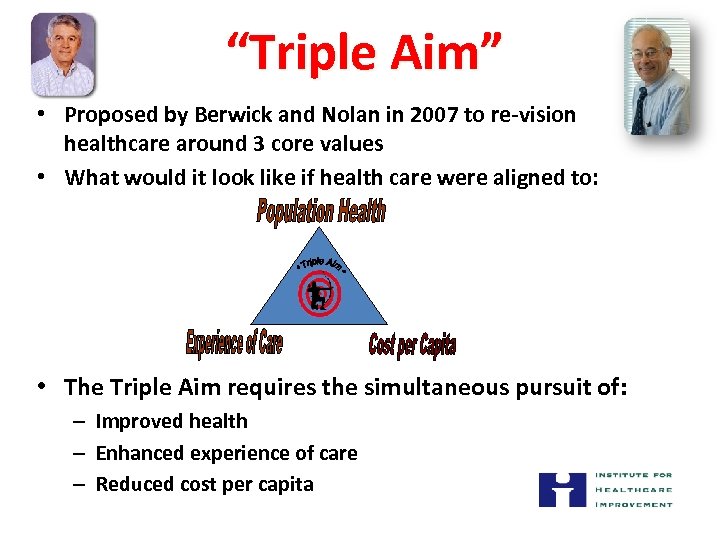 “Triple Aim” • Proposed by Berwick and Nolan in 2007 to re-vision healthcare around 3 core values • What would it look like if health care were aligned to: • The Triple Aim requires the simultaneous pursuit of: – Improved health – Enhanced experience of care – Reduced cost per capita
“Triple Aim” • Proposed by Berwick and Nolan in 2007 to re-vision healthcare around 3 core values • What would it look like if health care were aligned to: • The Triple Aim requires the simultaneous pursuit of: – Improved health – Enhanced experience of care – Reduced cost per capita
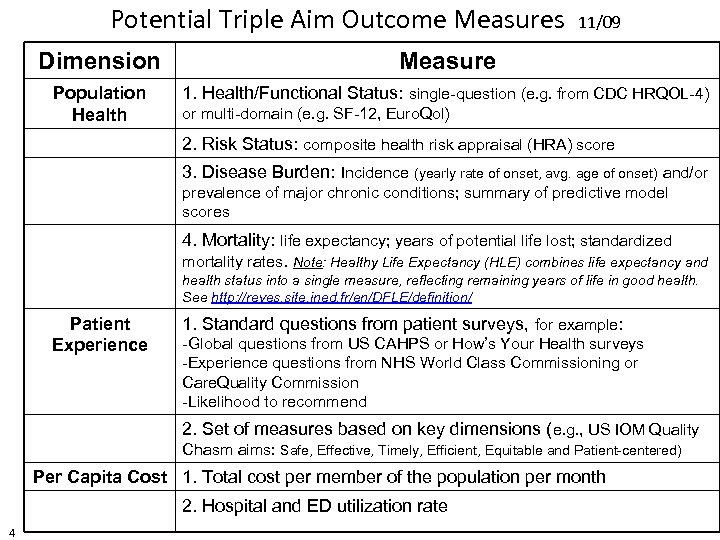 Potential Triple Aim Outcome Measures 11/09 Dimension Measure Population Health 1. Health/Functional Status: single-question (e. g. from CDC HRQOL-4) or multi-domain (e. g. SF-12, Euro. Qol) 2. Risk Status: composite health risk appraisal (HRA) score 3. Disease Burden: Incidence (yearly rate of onset, avg. age of onset) and/or prevalence of major chronic conditions; summary of predictive model scores 4. Mortality: life expectancy; years of potential life lost; standardized mortality rates. Note: Healthy Life Expectancy (HLE) combines life expectancy and health status into a single measure, reflecting remaining years of life in good health. See http: //reves. site. ined. fr/en/DFLE/definition/ Patient Experience 1. Standard questions from patient surveys, for example: -Global questions from US CAHPS or How’s Your Health surveys -Experience questions from NHS World Class Commissioning or Care. Quality Commission -Likelihood to recommend 2. Set of measures based on key dimensions (e. g. , US IOM Quality Chasm aims: Safe, Effective, Timely, Efficient, Equitable and Patient-centered) Per Capita Cost 1. Total cost per member of the population per month 2. Hospital and ED utilization rate 4
Potential Triple Aim Outcome Measures 11/09 Dimension Measure Population Health 1. Health/Functional Status: single-question (e. g. from CDC HRQOL-4) or multi-domain (e. g. SF-12, Euro. Qol) 2. Risk Status: composite health risk appraisal (HRA) score 3. Disease Burden: Incidence (yearly rate of onset, avg. age of onset) and/or prevalence of major chronic conditions; summary of predictive model scores 4. Mortality: life expectancy; years of potential life lost; standardized mortality rates. Note: Healthy Life Expectancy (HLE) combines life expectancy and health status into a single measure, reflecting remaining years of life in good health. See http: //reves. site. ined. fr/en/DFLE/definition/ Patient Experience 1. Standard questions from patient surveys, for example: -Global questions from US CAHPS or How’s Your Health surveys -Experience questions from NHS World Class Commissioning or Care. Quality Commission -Likelihood to recommend 2. Set of measures based on key dimensions (e. g. , US IOM Quality Chasm aims: Safe, Effective, Timely, Efficient, Equitable and Patient-centered) Per Capita Cost 1. Total cost per member of the population per month 2. Hospital and ED utilization rate 4
 Health Adjusted Life Expectancy (HALE) HALE = Product of average life expectancy and % rating their health status good or higher • Average Life Expectancy = Average number of years a baby born in a particular year is expected to live if current age-specific mortality trends continue to apply • Self-rated Health Status = Response to the question “How is your general health? ” on a 5 pt. scale from poor to excellent Kindig, D. Purchasing Population Health, 1997
Health Adjusted Life Expectancy (HALE) HALE = Product of average life expectancy and % rating their health status good or higher • Average Life Expectancy = Average number of years a baby born in a particular year is expected to live if current age-specific mortality trends continue to apply • Self-rated Health Status = Response to the question “How is your general health? ” on a 5 pt. scale from poor to excellent Kindig, D. Purchasing Population Health, 1997
 Triple Aim Initiative • Initial Prototyping (Sept ‘ 07 – April ‘ 08): – 15 Organizations recruited to a Learning Institute – Integrated Delivery Systems, Health Plans, Safety Net Organizations, Self Insured Employers, State Agencies • What can you do to accomplish these goals? – – Define a target population that you can impact What are you trying to accomplish for all three aims? What population oriented intervention are you going to implement? How will you measure impact? • Rapid growth to an international collaborative “learning system” of countries with technically advanced medical systems – National, International Collaborative Meetings – Biweekly conference calls – Focused workgroups
Triple Aim Initiative • Initial Prototyping (Sept ‘ 07 – April ‘ 08): – 15 Organizations recruited to a Learning Institute – Integrated Delivery Systems, Health Plans, Safety Net Organizations, Self Insured Employers, State Agencies • What can you do to accomplish these goals? – – Define a target population that you can impact What are you trying to accomplish for all three aims? What population oriented intervention are you going to implement? How will you measure impact? • Rapid growth to an international collaborative “learning system” of countries with technically advanced medical systems – National, International Collaborative Meetings – Biweekly conference calls – Focused workgroups
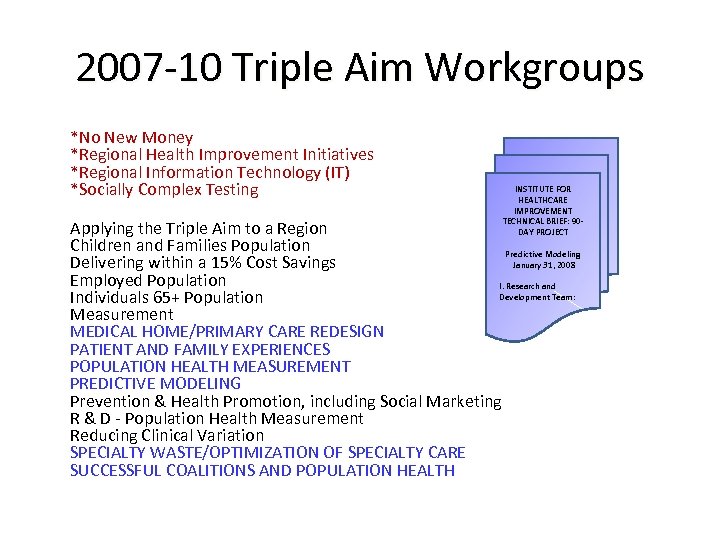 2007 -10 Triple Aim Workgroups *No New Money *Regional Health Improvement Initiatives *Regional Information Technology (IT) *Socially Complex Testing INSTITUTE FOR HEALTHCARE IMPROVEMENT TECHNICAL BRIEF: 90 DAY PROJECT Predictive Modeling January 31, 2008 Applying the Triple Aim to a Region Children and Families Population Delivering within a 15% Cost Savings Employed Population I. Research and Development Team: Individuals 65+ Population Measurement MEDICAL HOME/PRIMARY CARE REDESIGN PATIENT AND FAMILY EXPERIENCES POPULATION HEALTH MEASUREMENT PREDICTIVE MODELING Prevention & Health Promotion, including Social Marketing R & D - Population Health Measurement Reducing Clinical Variation SPECIALTY WASTE/OPTIMIZATION OF SPECIALTY CARE SUCCESSFUL COALITIONS AND POPULATION HEALTH
2007 -10 Triple Aim Workgroups *No New Money *Regional Health Improvement Initiatives *Regional Information Technology (IT) *Socially Complex Testing INSTITUTE FOR HEALTHCARE IMPROVEMENT TECHNICAL BRIEF: 90 DAY PROJECT Predictive Modeling January 31, 2008 Applying the Triple Aim to a Region Children and Families Population Delivering within a 15% Cost Savings Employed Population I. Research and Development Team: Individuals 65+ Population Measurement MEDICAL HOME/PRIMARY CARE REDESIGN PATIENT AND FAMILY EXPERIENCES POPULATION HEALTH MEASUREMENT PREDICTIVE MODELING Prevention & Health Promotion, including Social Marketing R & D - Population Health Measurement Reducing Clinical Variation SPECIALTY WASTE/OPTIMIZATION OF SPECIALTY CARE SUCCESSFUL COALITIONS AND POPULATION HEALTH
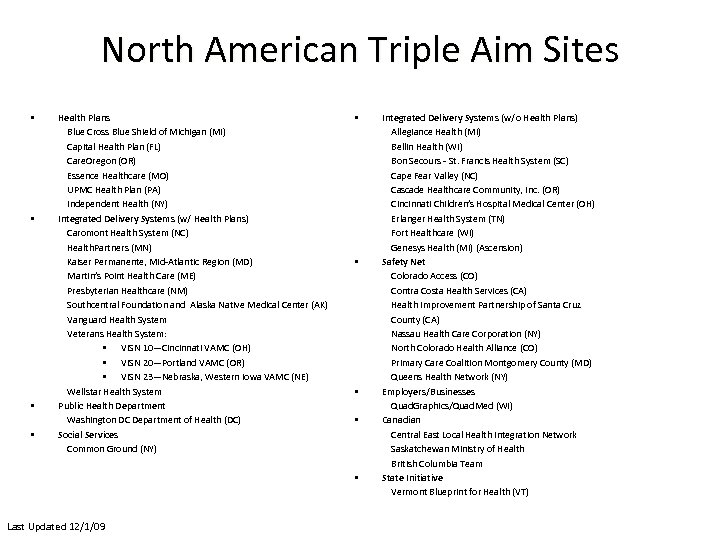 North American Triple Aim Sites • • Health Plans Blue Cross Blue Shield of Michigan (MI) Capital Health Plan (FL) Care. Oregon (OR) Essence Healthcare (MO) UPMC Health Plan (PA) Independent Health (NY) Integrated Delivery Systems (w/ Health Plans) Caromont Health System (NC) Health. Partners (MN) Kaiser Permanente, Mid-Atlantic Region (MD) Martin’s Point Health Care (ME) Presbyterian Healthcare (NM) Southcentral Foundation and Alaska Native Medical Center (AK) Vanguard Health System Veterans Health System: • VISN 10—Cincinnati VAMC (OH) • VISN 20—Portland VAMC (OR) • VISN 23—Nebraska, Western Iowa VAMC (NE) Wellstar Health System Public Health Department Washington DC Department of Health (DC) Social Services Common Ground (NY) • • • Last Updated 12/1/09 Integrated Delivery Systems (w/o Health Plans) Allegiance Health (MI) Bellin Health (WI) Bon Secours - St. Francis Health System (SC) Cape Fear Valley (NC) Cascade Healthcare Community, Inc. (OR) Cincinnati Children’s Hospital Medical Center (OH) Erlanger Health System (TN) Fort Healthcare (WI) Genesys Health (MI) (Ascension) Safety Net Colorado Access (CO) Contra Costa Health Services (CA) Health Improvement Partnership of Santa Cruz County (CA) Nassau Health Care Corporation (NY) North Colorado Health Alliance (CO) Primary Care Coalition Montgomery County (MD) Queens Health Network (NY) Employers/Businesses Quad. Graphics/Quad. Med (WI) Canadian Central East Local Health Integration Network Saskatchewan Ministry of Health British Columbia Team State Initiative Vermont Blueprint for Health (VT)
North American Triple Aim Sites • • Health Plans Blue Cross Blue Shield of Michigan (MI) Capital Health Plan (FL) Care. Oregon (OR) Essence Healthcare (MO) UPMC Health Plan (PA) Independent Health (NY) Integrated Delivery Systems (w/ Health Plans) Caromont Health System (NC) Health. Partners (MN) Kaiser Permanente, Mid-Atlantic Region (MD) Martin’s Point Health Care (ME) Presbyterian Healthcare (NM) Southcentral Foundation and Alaska Native Medical Center (AK) Vanguard Health System Veterans Health System: • VISN 10—Cincinnati VAMC (OH) • VISN 20—Portland VAMC (OR) • VISN 23—Nebraska, Western Iowa VAMC (NE) Wellstar Health System Public Health Department Washington DC Department of Health (DC) Social Services Common Ground (NY) • • • Last Updated 12/1/09 Integrated Delivery Systems (w/o Health Plans) Allegiance Health (MI) Bellin Health (WI) Bon Secours - St. Francis Health System (SC) Cape Fear Valley (NC) Cascade Healthcare Community, Inc. (OR) Cincinnati Children’s Hospital Medical Center (OH) Erlanger Health System (TN) Fort Healthcare (WI) Genesys Health (MI) (Ascension) Safety Net Colorado Access (CO) Contra Costa Health Services (CA) Health Improvement Partnership of Santa Cruz County (CA) Nassau Health Care Corporation (NY) North Colorado Health Alliance (CO) Primary Care Coalition Montgomery County (MD) Queens Health Network (NY) Employers/Businesses Quad. Graphics/Quad. Med (WI) Canadian Central East Local Health Integration Network Saskatchewan Ministry of Health British Columbia Team State Initiative Vermont Blueprint for Health (VT)
 International Triple Aim Sites • • • Jonkoping (Sweden) NHS Blackburn With Darwen PCT (NW England) NHS Bolton PCT (NW England) NHS Bournemouth and Poole (SW England) NHS East Lancashire Teaching PCT (NW England) NHS Eastern and Coastal Kent PCT (South East Coast England) NHS Forth Valley (Scotland) NHS Heywood, Middleton and Rochdale PCT (NW England) NHS North Lancashire Teaching PCT (NW England) NHS Medway (South East Coast England) NHS Oldham PCT (NW England) Last Updated 10/5/09 • • • • NHS Salford PCT (NW England) NHS Somerset PCT (SW England) NHS Swindon PCT (SW England) NHS Tayside (Scotland) NHS Torbay Care Trust (SW England) NHS Blackpool PCT (NW England) NHS Bury PCT (NW England) NHS Central Lancashire PCT (NW England) NHS Sefton PCT (NW England) NHS Warrington PCT (NW England) NHS Western Cheshire PCT (NW England) NHS Wirral PCT (NW England) State of South Australia, Ministry of Health (Australia) Western Health and Social Care Trust (Northern Ireland)
International Triple Aim Sites • • • Jonkoping (Sweden) NHS Blackburn With Darwen PCT (NW England) NHS Bolton PCT (NW England) NHS Bournemouth and Poole (SW England) NHS East Lancashire Teaching PCT (NW England) NHS Eastern and Coastal Kent PCT (South East Coast England) NHS Forth Valley (Scotland) NHS Heywood, Middleton and Rochdale PCT (NW England) NHS North Lancashire Teaching PCT (NW England) NHS Medway (South East Coast England) NHS Oldham PCT (NW England) Last Updated 10/5/09 • • • • NHS Salford PCT (NW England) NHS Somerset PCT (SW England) NHS Swindon PCT (SW England) NHS Tayside (Scotland) NHS Torbay Care Trust (SW England) NHS Blackpool PCT (NW England) NHS Bury PCT (NW England) NHS Central Lancashire PCT (NW England) NHS Sefton PCT (NW England) NHS Warrington PCT (NW England) NHS Western Cheshire PCT (NW England) NHS Wirral PCT (NW England) State of South Australia, Ministry of Health (Australia) Western Health and Social Care Trust (Northern Ireland)
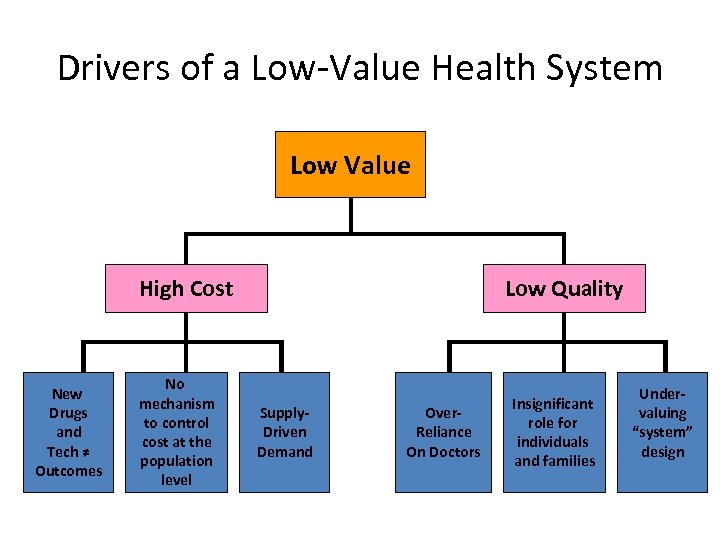 Drivers of a Low-Value Health System Low Value High Cost New Drugs and Tech ≠ Outcomes No mechanism to control cost at the population level Low Quality Supply. Driven Demand Over. Reliance On Doctors Insignificant role for individuals and families Undervaluing “system” design
Drivers of a Low-Value Health System Low Value High Cost New Drugs and Tech ≠ Outcomes No mechanism to control cost at the population level Low Quality Supply. Driven Demand Over. Reliance On Doctors Insignificant role for individuals and families Undervaluing “system” design
 Key Issues: • Social Determinants of Health • Fragmentation of Health Services • Misalignment of Incentives
Key Issues: • Social Determinants of Health • Fragmentation of Health Services • Misalignment of Incentives
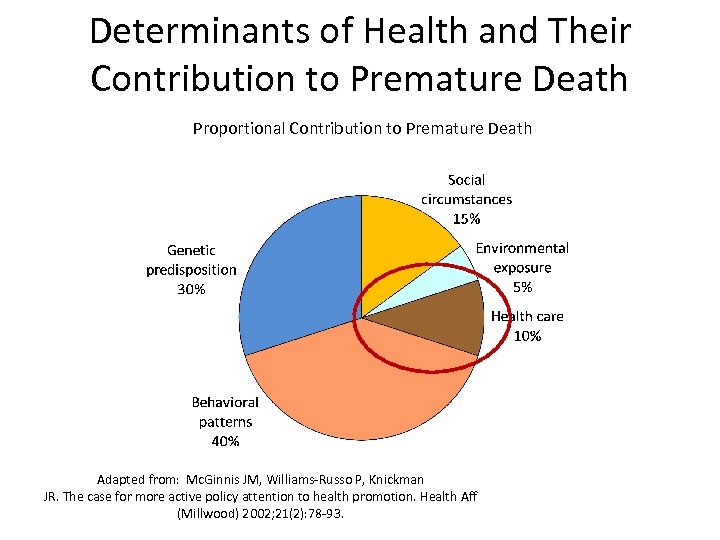 Determinants of Health and Their Contribution to Premature Death Proportional Contribution to Premature Death Adapted from: Mc. Ginnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood) 2002; 21(2): 78 -93.
Determinants of Health and Their Contribution to Premature Death Proportional Contribution to Premature Death Adapted from: Mc. Ginnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood) 2002; 21(2): 78 -93.
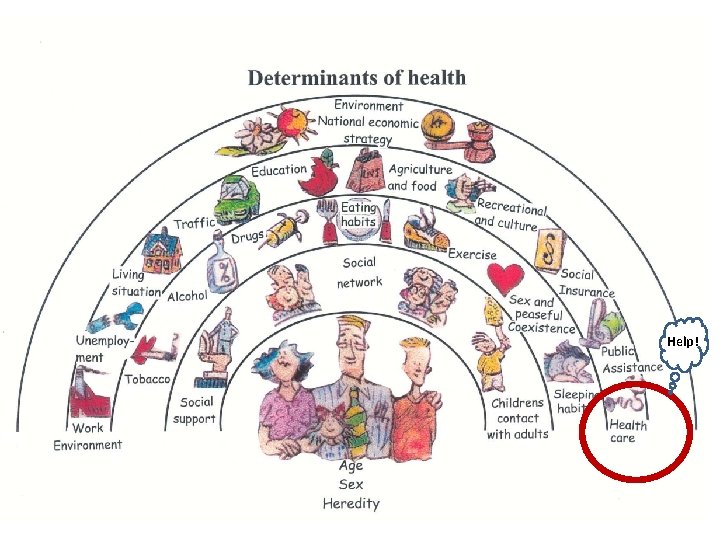 Help!
Help!
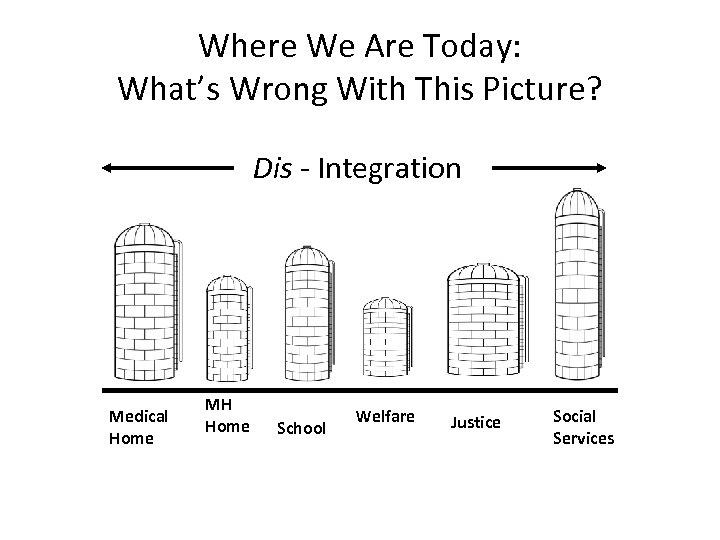 Where We Are Today: What’s Wrong With This Picture? Dis - Integration Medical Home MH Home School Welfare Justice Social Services
Where We Are Today: What’s Wrong With This Picture? Dis - Integration Medical Home MH Home School Welfare Justice Social Services
 Needed: The “Integrator” • It may or may not be a new structure or organization. • It pulls together the resources to support a defined population. • It builds alliances and coalitions. • It optimizes the Triple Aim for the sake of a defined population. • It works with and helps to improve microsystems to support individuals.
Needed: The “Integrator” • It may or may not be a new structure or organization. • It pulls together the resources to support a defined population. • It builds alliances and coalitions. • It optimizes the Triple Aim for the sake of a defined population. • It works with and helps to improve microsystems to support individuals.
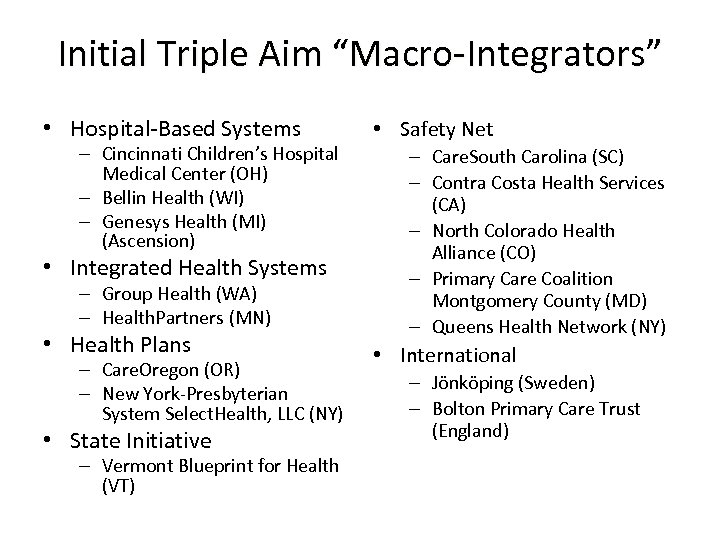 Initial Triple Aim “Macro-Integrators” • Hospital-Based Systems – Cincinnati Children’s Hospital Medical Center (OH) – Bellin Health (WI) – Genesys Health (MI) (Ascension) • Integrated Health Systems – Group Health (WA) – Health. Partners (MN) • Health Plans – Care. Oregon (OR) – New York-Presbyterian System Select. Health, LLC (NY) • State Initiative – Vermont Blueprint for Health (VT) • Safety Net – Care. South Carolina (SC) – Contra Costa Health Services (CA) – North Colorado Health Alliance (CO) – Primary Care Coalition Montgomery County (MD) – Queens Health Network (NY) • International – Jönköping (Sweden) – Bolton Primary Care Trust (England)
Initial Triple Aim “Macro-Integrators” • Hospital-Based Systems – Cincinnati Children’s Hospital Medical Center (OH) – Bellin Health (WI) – Genesys Health (MI) (Ascension) • Integrated Health Systems – Group Health (WA) – Health. Partners (MN) • Health Plans – Care. Oregon (OR) – New York-Presbyterian System Select. Health, LLC (NY) • State Initiative – Vermont Blueprint for Health (VT) • Safety Net – Care. South Carolina (SC) – Contra Costa Health Services (CA) – North Colorado Health Alliance (CO) – Primary Care Coalition Montgomery County (MD) – Queens Health Network (NY) • International – Jönköping (Sweden) – Bolton Primary Care Trust (England)
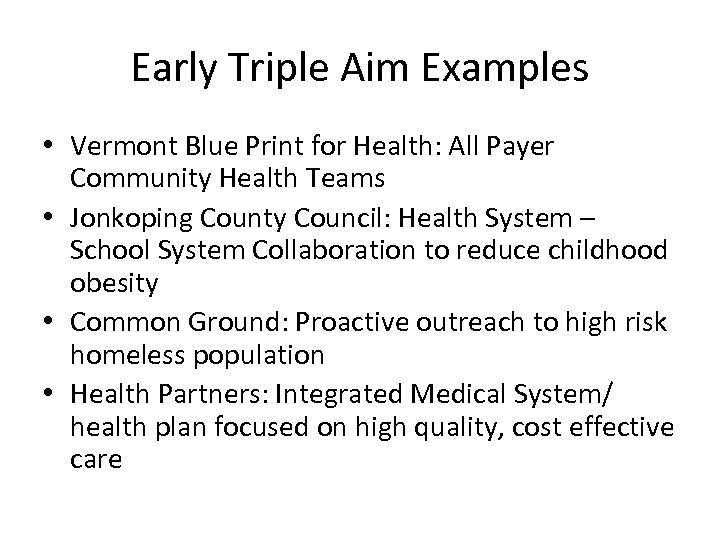 Early Triple Aim Examples • Vermont Blue Print for Health: All Payer Community Health Teams • Jonkoping County Council: Health System – School System Collaboration to reduce childhood obesity • Common Ground: Proactive outreach to high risk homeless population • Health Partners: Integrated Medical System/ health plan focused on high quality, cost effective care
Early Triple Aim Examples • Vermont Blue Print for Health: All Payer Community Health Teams • Jonkoping County Council: Health System – School System Collaboration to reduce childhood obesity • Common Ground: Proactive outreach to high risk homeless population • Health Partners: Integrated Medical System/ health plan focused on high quality, cost effective care
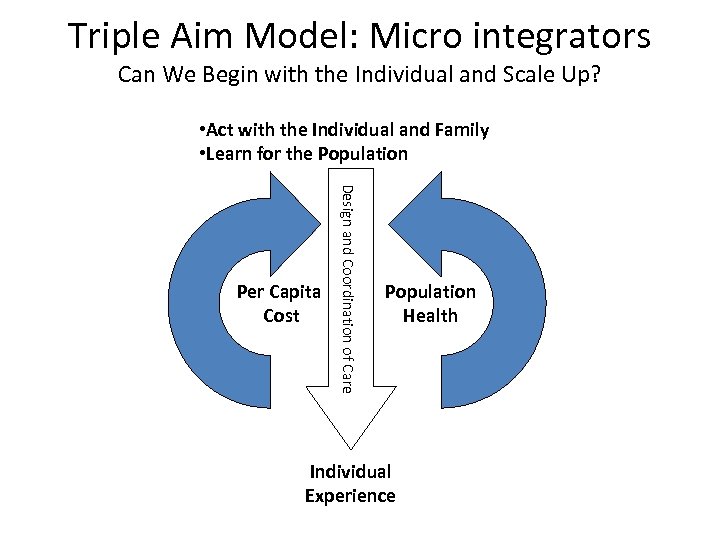 Triple Aim Model: Micro integrators Can We Begin with the Individual and Scale Up? • Act with the Individual and Family • Learn for the Population Design and Coordination of Care Per Capita Cost Population Health Individual Experience
Triple Aim Model: Micro integrators Can We Begin with the Individual and Scale Up? • Act with the Individual and Family • Learn for the Population Design and Coordination of Care Per Capita Cost Population Health Individual Experience
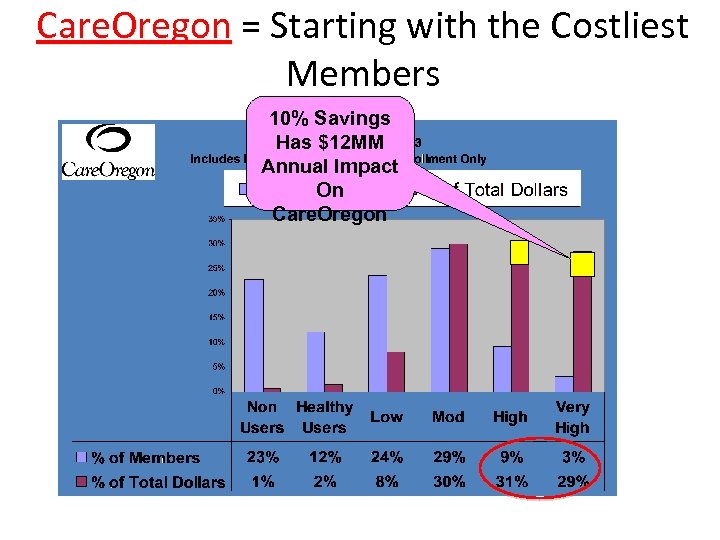 Care. Oregon = Starting with the Costliest Care. Oregon Members 10% Savings Has $12 MM Annual Impact On Care. Oregon
Care. Oregon = Starting with the Costliest Care. Oregon Members 10% Savings Has $12 MM Annual Impact On Care. Oregon
 Bus Pass $23 versus ED $1400 • “Member was seen in the ED 21 times in Dec. 2007. ” • “History of heroin use, transportation barriers to receiving Methadone treatment and from seeing her PCP on a regular basis. ” • “We bought a bus pass. ” • “No ED visits for two months and she is much more engaged in CD treatment and her PCP relationship. ”
Bus Pass $23 versus ED $1400 • “Member was seen in the ED 21 times in Dec. 2007. ” • “History of heroin use, transportation barriers to receiving Methadone treatment and from seeing her PCP on a regular basis. ” • “We bought a bus pass. ” • “No ED visits for two months and she is much more engaged in CD treatment and her PCP relationship. ”
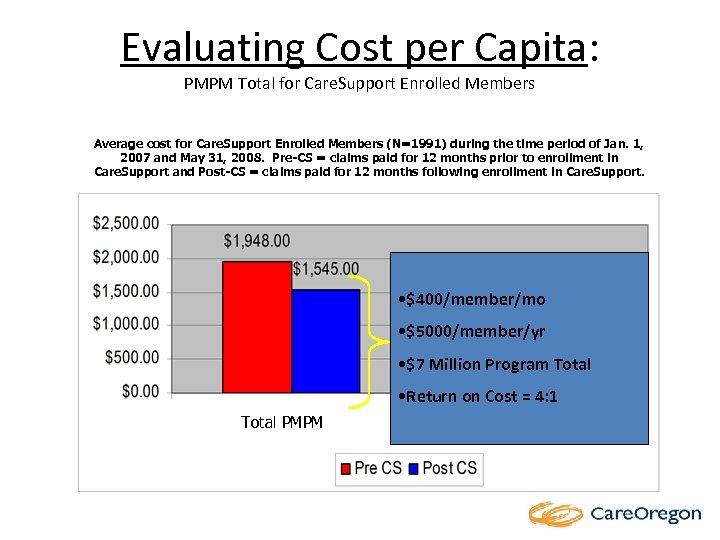 Evaluating Cost per Capita: PMPM Total for Care. Support Enrolled Members Average cost for Care. Support Enrolled Members (N=1991) during the time period of Jan. 1, 2007 and May 31, 2008. Pre-CS = claims paid for 12 months prior to enrollment in Care. Support and Post-CS = claims paid for 12 months following enrollment in Care. Support. • $400/member/mo • $5000/member/yr • $7 Million Program Total • Return on Cost = 4: 1 Total PMPM Hospital PMPM
Evaluating Cost per Capita: PMPM Total for Care. Support Enrolled Members Average cost for Care. Support Enrolled Members (N=1991) during the time period of Jan. 1, 2007 and May 31, 2008. Pre-CS = claims paid for 12 months prior to enrollment in Care. Support and Post-CS = claims paid for 12 months following enrollment in Care. Support. • $400/member/mo • $5000/member/yr • $7 Million Program Total • Return on Cost = 4: 1 Total PMPM Hospital PMPM
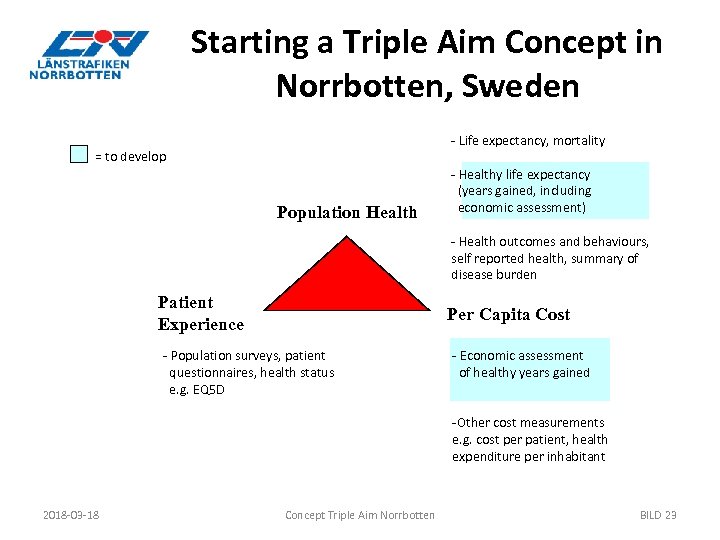 Starting a Triple Aim Concept in Norrbotten, Sweden - Life expectancy, mortality = to develop Population Health - Healthy life expectancy (years gained, including economic assessment) - Health outcomes and behaviours, self reported health, summary of disease burden Patient Experience Per Capita Cost - Population surveys, patient questionnaires, health status e. g. EQ 5 D - Economic assessment of healthy years gained -Other cost measurements e. g. cost per patient, health expenditure per inhabitant 2018 -03 -18 Concept Triple Aim Norrbotten BILD 23
Starting a Triple Aim Concept in Norrbotten, Sweden - Life expectancy, mortality = to develop Population Health - Healthy life expectancy (years gained, including economic assessment) - Health outcomes and behaviours, self reported health, summary of disease burden Patient Experience Per Capita Cost - Population surveys, patient questionnaires, health status e. g. EQ 5 D - Economic assessment of healthy years gained -Other cost measurements e. g. cost per patient, health expenditure per inhabitant 2018 -03 -18 Concept Triple Aim Norrbotten BILD 23
 Concept Goal and Target Groups Ø Goal: Lower disease burden caused by overweight and obesity Ø Target groups: - Children through childrens primary care, dentists and schools - Families through the children - Risk patients through primary care and screening at age 30, together with specialist care - General public through local alliances 2018 -03 -18 Concept Triple Aim Norrbotten BILD 24
Concept Goal and Target Groups Ø Goal: Lower disease burden caused by overweight and obesity Ø Target groups: - Children through childrens primary care, dentists and schools - Families through the children - Risk patients through primary care and screening at age 30, together with specialist care - General public through local alliances 2018 -03 -18 Concept Triple Aim Norrbotten BILD 24
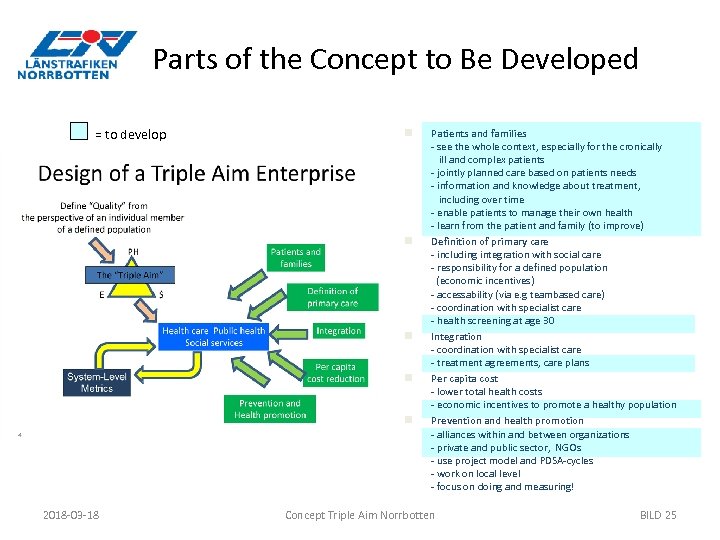 Parts of the Concept to Be Developed = to develop n n n 2018 -03 -18 Patients and families - see the whole context, especially for the cronically ill and complex patients - jointly planned care based on patients needs - information and knowledge about treatment, including over time - enable patients to manage their own health - learn from the patient and family (to improve) Definition of primary care - including integration with social care - responsibility for a defined population (economic incentives) - accessability (via e. g teambased care) - coordination with specialist care - health screening at age 30 Integration - coordination with specialist care - treatment agreements, care plans Per capita cost - lower total health costs - economic incentives to promote a healthy population Prevention and health promotion - alliances within and between organizations - private and public sector, NGOs - use project model and PDSA-cycles - work on local level - focus on doing and measuring! Concept Triple Aim Norrbotten BILD 25
Parts of the Concept to Be Developed = to develop n n n 2018 -03 -18 Patients and families - see the whole context, especially for the cronically ill and complex patients - jointly planned care based on patients needs - information and knowledge about treatment, including over time - enable patients to manage their own health - learn from the patient and family (to improve) Definition of primary care - including integration with social care - responsibility for a defined population (economic incentives) - accessability (via e. g teambased care) - coordination with specialist care - health screening at age 30 Integration - coordination with specialist care - treatment agreements, care plans Per capita cost - lower total health costs - economic incentives to promote a healthy population Prevention and health promotion - alliances within and between organizations - private and public sector, NGOs - use project model and PDSA-cycles - work on local level - focus on doing and measuring! Concept Triple Aim Norrbotten BILD 25
 Implementation Ø Use Triple Aim as lever! - Coordinate with and enhance work already in progress e. g. strategy for obesity patients, public health management, the County Political Strategy for Population Health Ø Build project structure with coordinator from the county council together with coordinator for the municipalities for the local alliances Ø Select two pilot municipalities/primary care centres to act as PDSAcycles before county-wide implementation. 2018 -03 -18 Concept Triple Aim Norrbotten BILD 26
Implementation Ø Use Triple Aim as lever! - Coordinate with and enhance work already in progress e. g. strategy for obesity patients, public health management, the County Political Strategy for Population Health Ø Build project structure with coordinator from the county council together with coordinator for the municipalities for the local alliances Ø Select two pilot municipalities/primary care centres to act as PDSAcycles before county-wide implementation. 2018 -03 -18 Concept Triple Aim Norrbotten BILD 26
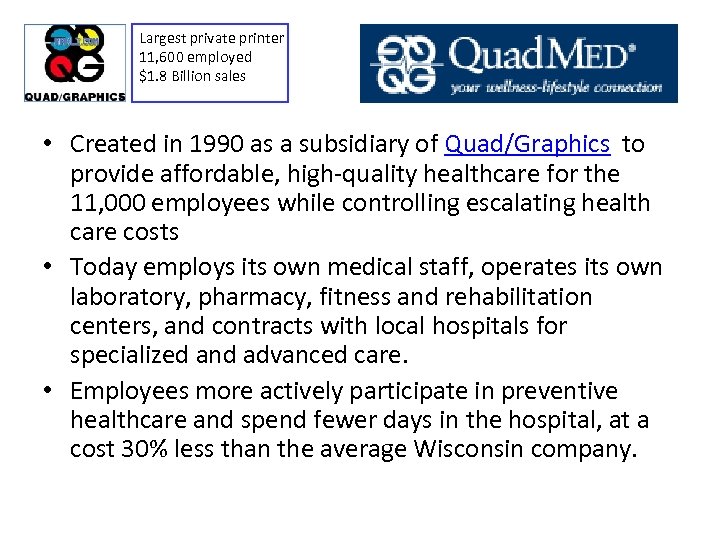 Largest private printer 11, 600 employed $1. 8 Billion sales • Created in 1990 as a subsidiary of Quad/Graphics to provide affordable, high-quality healthcare for the 11, 000 employees while controlling escalating health care costs • Today employs its own medical staff, operates its own laboratory, pharmacy, fitness and rehabilitation centers, and contracts with local hospitals for specialized and advanced care. • Employees more actively participate in preventive healthcare and spend fewer days in the hospital, at a cost 30% less than the average Wisconsin company.
Largest private printer 11, 600 employed $1. 8 Billion sales • Created in 1990 as a subsidiary of Quad/Graphics to provide affordable, high-quality healthcare for the 11, 000 employees while controlling escalating health care costs • Today employs its own medical staff, operates its own laboratory, pharmacy, fitness and rehabilitation centers, and contracts with local hospitals for specialized and advanced care. • Employees more actively participate in preventive healthcare and spend fewer days in the hospital, at a cost 30% less than the average Wisconsin company.
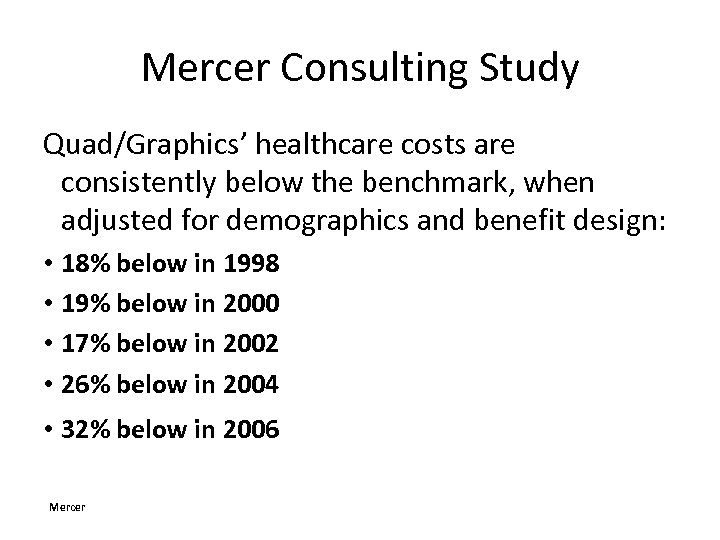 Mercer Consulting Study Quad/Graphics’ healthcare costs are consistently below the benchmark, when adjusted for demographics and benefit design: • 18% below in 1998 • 19% below in 2000 • 17% below in 2002 • 26% below in 2004 • 32% below in 2006 Mercer
Mercer Consulting Study Quad/Graphics’ healthcare costs are consistently below the benchmark, when adjusted for demographics and benefit design: • 18% below in 1998 • 19% below in 2000 • 17% below in 2002 • 26% below in 2004 • 32% below in 2006 Mercer
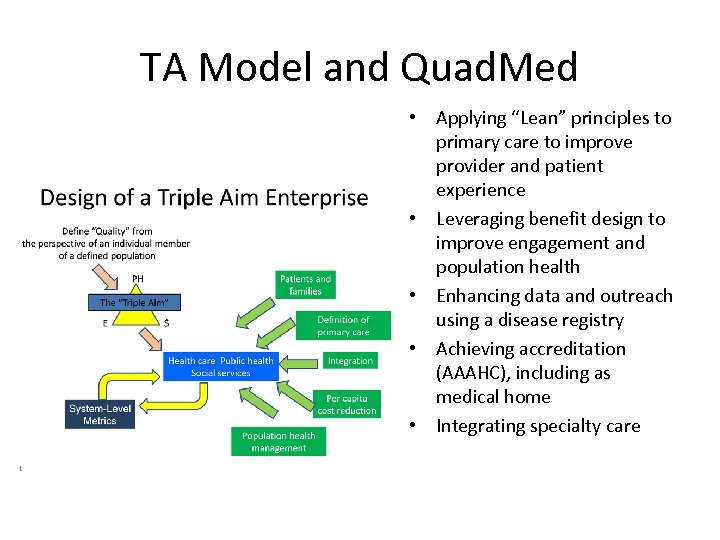 TA Model and Quad. Med • Applying “Lean” principles to primary care to improve provider and patient experience • Leveraging benefit design to improve engagement and population health • Enhancing data and outreach using a disease registry • Achieving accreditation (AAAHC), including as medical home • Integrating specialty care
TA Model and Quad. Med • Applying “Lean” principles to primary care to improve provider and patient experience • Leveraging benefit design to improve engagement and population health • Enhancing data and outreach using a disease registry • Achieving accreditation (AAAHC), including as medical home • Integrating specialty care
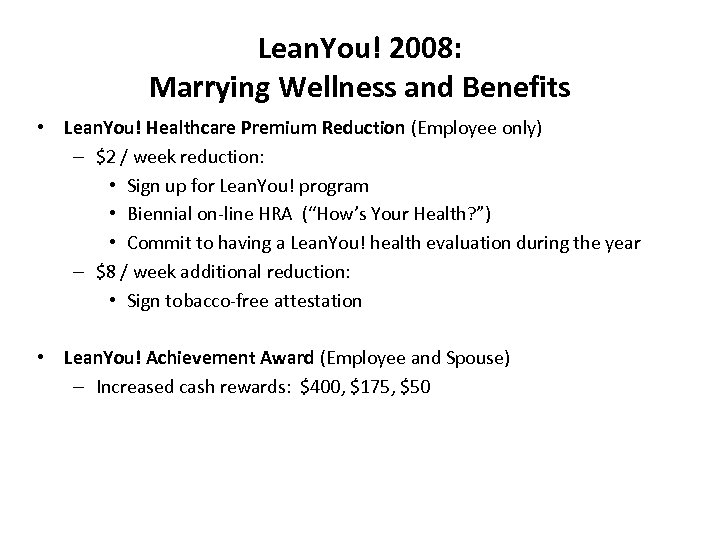 Lean. You! 2008: Marrying Wellness and Benefits • Lean. You! Healthcare Premium Reduction (Employee only) – $2 / week reduction: • Sign up for Lean. You! program • Biennial on-line HRA (“How’s Your Health? ”) • Commit to having a Lean. You! health evaluation during the year – $8 / week additional reduction: • Sign tobacco-free attestation • Lean. You! Achievement Award (Employee and Spouse) – Increased cash rewards: $400, $175, $50
Lean. You! 2008: Marrying Wellness and Benefits • Lean. You! Healthcare Premium Reduction (Employee only) – $2 / week reduction: • Sign up for Lean. You! program • Biennial on-line HRA (“How’s Your Health? ”) • Commit to having a Lean. You! health evaluation during the year – $8 / week additional reduction: • Sign tobacco-free attestation • Lean. You! Achievement Award (Employee and Spouse) – Increased cash rewards: $400, $175, $50
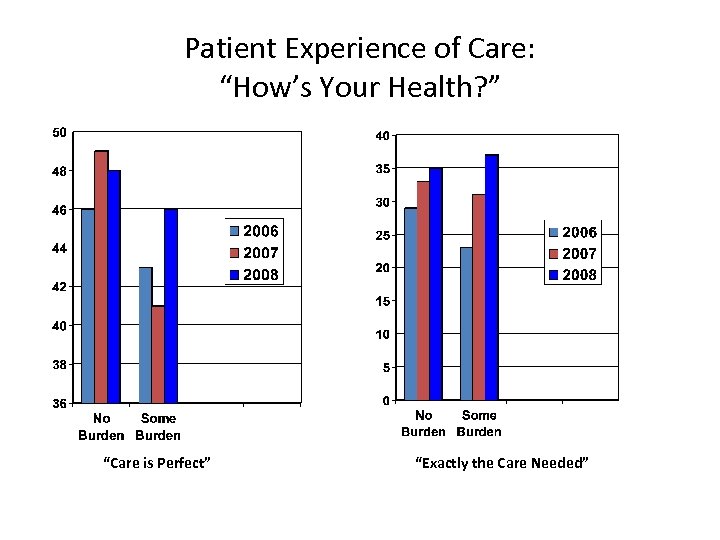 Patient Experience of Care: “How’s Your Health? ” “Care is Perfect” “Exactly the Care Needed”
Patient Experience of Care: “How’s Your Health? ” “Care is Perfect” “Exactly the Care Needed”
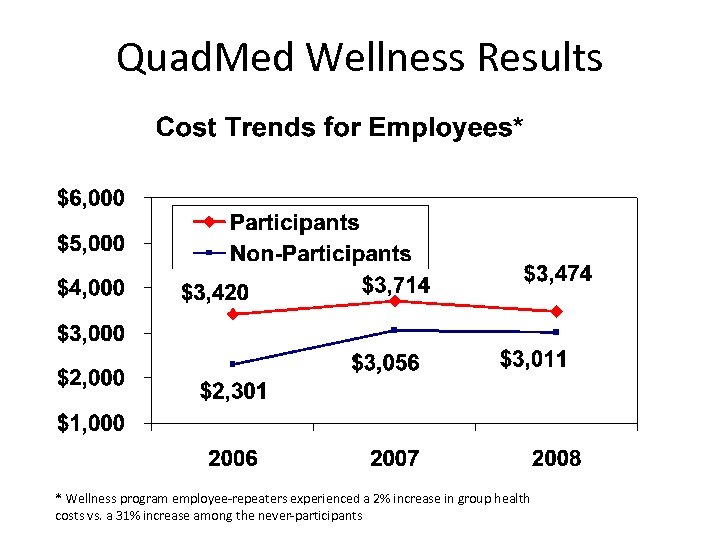 Quad. Med Wellness Results * Wellness program employee-repeaters experienced a 2% increase in group health costs vs. a 31% increase among the never-participants
Quad. Med Wellness Results * Wellness program employee-repeaters experienced a 2% increase in group health costs vs. a 31% increase among the never-participants
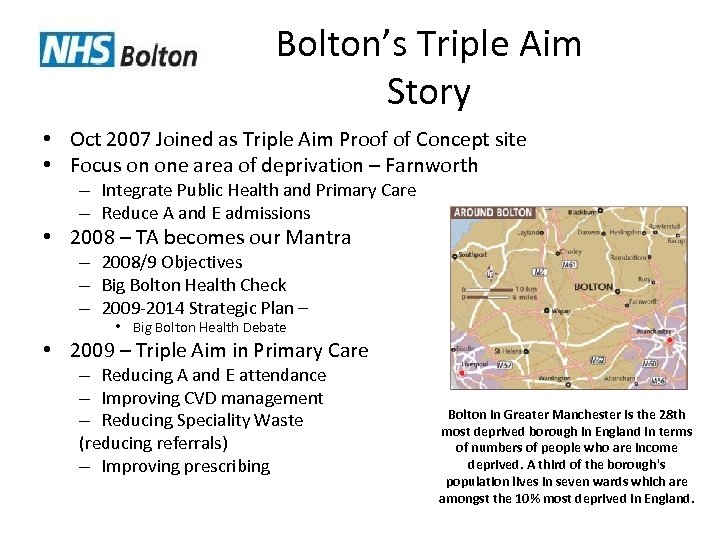 Bolton’s Triple Aim Story • Oct 2007 Joined as Triple Aim Proof of Concept site • Focus on one area of deprivation – Farnworth – Integrate Public Health and Primary Care – Reduce A and E admissions • 2008 – TA becomes our Mantra – 2008/9 Objectives – Big Bolton Health Check – 2009 -2014 Strategic Plan – • Big Bolton Health Debate • 2009 – Triple Aim in Primary Care – Reducing A and E attendance – Improving CVD management – Reducing Speciality Waste (reducing referrals) – Improving prescribing Bolton in Greater Manchester is the 28 th most deprived borough in England in terms of numbers of people who are income deprived. A third of the borough's population lives in seven wards which are amongst the 10% most deprived in England.
Bolton’s Triple Aim Story • Oct 2007 Joined as Triple Aim Proof of Concept site • Focus on one area of deprivation – Farnworth – Integrate Public Health and Primary Care – Reduce A and E admissions • 2008 – TA becomes our Mantra – 2008/9 Objectives – Big Bolton Health Check – 2009 -2014 Strategic Plan – • Big Bolton Health Debate • 2009 – Triple Aim in Primary Care – Reducing A and E attendance – Improving CVD management – Reducing Speciality Waste (reducing referrals) – Improving prescribing Bolton in Greater Manchester is the 28 th most deprived borough in England in terms of numbers of people who are income deprived. A third of the borough's population lives in seven wards which are amongst the 10% most deprived in England.
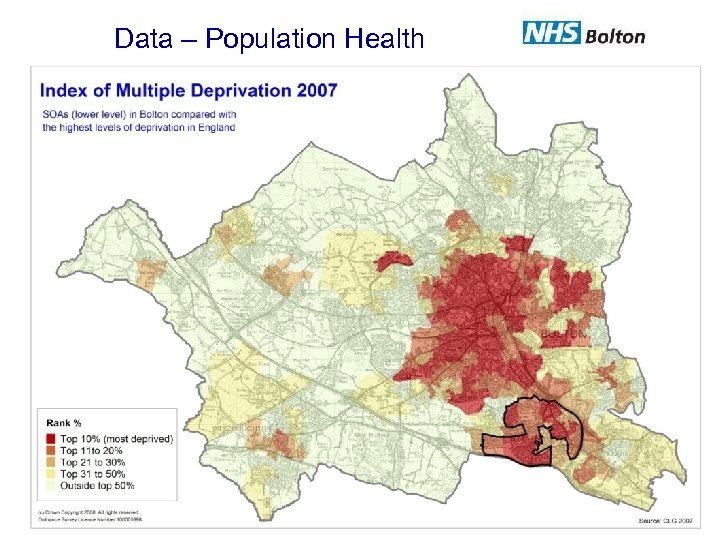 Data – Population Health
Data – Population Health
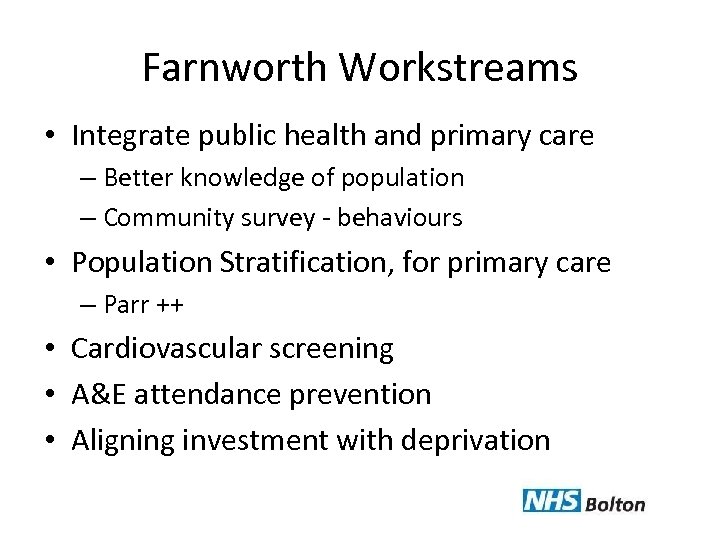 Farnworth Workstreams • Integrate public health and primary care – Better knowledge of population – Community survey - behaviours • Population Stratification, for primary care – Parr ++ • Cardiovascular screening • A&E attendance prevention • Aligning investment with deprivation
Farnworth Workstreams • Integrate public health and primary care – Better knowledge of population – Community survey - behaviours • Population Stratification, for primary care – Parr ++ • Cardiovascular screening • A&E attendance prevention • Aligning investment with deprivation
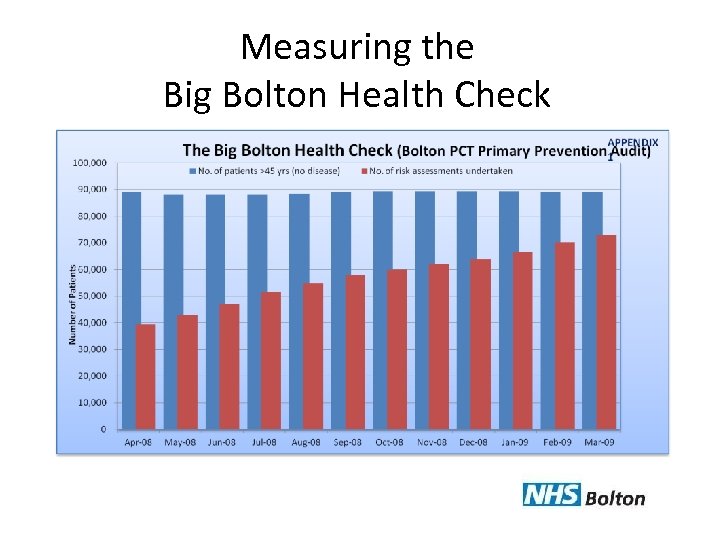 Measuring the Big Bolton Health Check
Measuring the Big Bolton Health Check
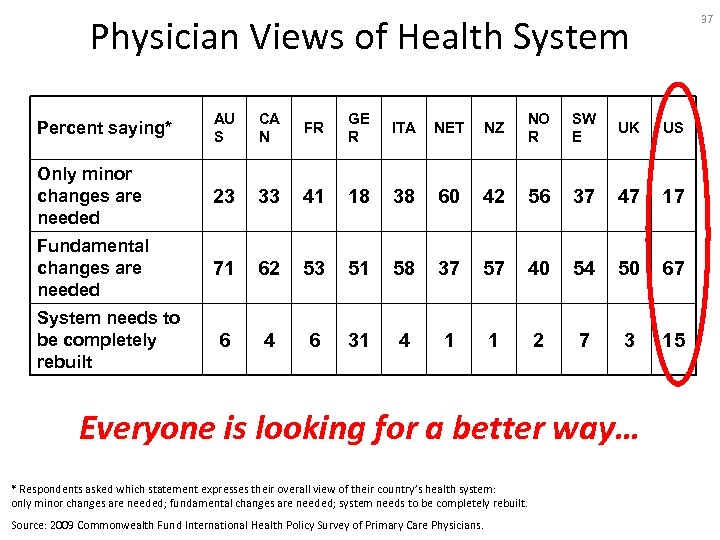 Physician Views of Health System 37 Percent saying* AU S CA N FR GE R ITA NET NZ NO R SW E UK US Only minor changes are needed 23 33 41 18 38 60 42 56 37 47 17 Fundamental changes are needed 71 62 53 51 58 37 57 40 54 50 67 6 4 6 31 4 1 1 2 7 3 15 System needs to be completely rebuilt Everyone is looking for a better way… * Respondents asked which statement expresses their overall view of their country’s health system: only minor changes are needed; fundamental changes are needed; system needs to be completely rebuilt. Source: 2009 Commonwealth Fund International Health Policy Survey of Primary Care Physicians.
Physician Views of Health System 37 Percent saying* AU S CA N FR GE R ITA NET NZ NO R SW E UK US Only minor changes are needed 23 33 41 18 38 60 42 56 37 47 17 Fundamental changes are needed 71 62 53 51 58 37 57 40 54 50 67 6 4 6 31 4 1 1 2 7 3 15 System needs to be completely rebuilt Everyone is looking for a better way… * Respondents asked which statement expresses their overall view of their country’s health system: only minor changes are needed; fundamental changes are needed; system needs to be completely rebuilt. Source: 2009 Commonwealth Fund International Health Policy Survey of Primary Care Physicians.
 Triple Aim as Social Movement • Triple Aim is now an international movement of 60+ organizations engaged in health system redesign – All from countries with a high levels of medical technology -- recognize that science / technology itself does not deliver health outcomes – All with different delivery systems… and outcomes… • Creating our “best possible health…” • How care is delivered is a major determinant of health, experience, cost, at every level from the bottom up… • What is delivered must include much more than medical therapies, addressing social determinants as well… • Who drives change critically determines how effectively any system truly meets the wants and needs of those it is meant to serve.
Triple Aim as Social Movement • Triple Aim is now an international movement of 60+ organizations engaged in health system redesign – All from countries with a high levels of medical technology -- recognize that science / technology itself does not deliver health outcomes – All with different delivery systems… and outcomes… • Creating our “best possible health…” • How care is delivered is a major determinant of health, experience, cost, at every level from the bottom up… • What is delivered must include much more than medical therapies, addressing social determinants as well… • Who drives change critically determines how effectively any system truly meets the wants and needs of those it is meant to serve.
 What Creates Value in Health Care? • New Triple Aim Paradigm: Health systems are Triple Aim accountable for population outcomes – “System design” recognized as a determinant of health – Value is created by “systems of care” with appropriate expertise – New emphasis on patient engagement, patient driven care – “Quality” redefined as best possible “medical service” delivery AND best possible health and cost outcomes
What Creates Value in Health Care? • New Triple Aim Paradigm: Health systems are Triple Aim accountable for population outcomes – “System design” recognized as a determinant of health – Value is created by “systems of care” with appropriate expertise – New emphasis on patient engagement, patient driven care – “Quality” redefined as best possible “medical service” delivery AND best possible health and cost outcomes
 Triple Aim Moving Forward • “Regional” Triple Aim Initiatives – Bending the cost curve – Integration Medical and Social Services – Realignment of incentives: ACOs? • Regional Triple Aim Collaboratives? – Multiple Triple Aim efforts within a region – Local “learning systems”
Triple Aim Moving Forward • “Regional” Triple Aim Initiatives – Bending the cost curve – Integration Medical and Social Services – Realignment of incentives: ACOs? • Regional Triple Aim Collaboratives? – Multiple Triple Aim efforts within a region – Local “learning systems”
 Stages of Facing Reality • “The data are wrong” • “The data are right, but it’s not a problem” • “The data are right; it is a problem; but it is not my problem. ” • “I accept the burden of improvement”
Stages of Facing Reality • “The data are wrong” • “The data are right, but it’s not a problem” • “The data are right; it is a problem; but it is not my problem. ” • “I accept the burden of improvement”


