6f85d3a0b43ea5c43751c44c4f471ba3.ppt
- Количество слайдов: 20
Accountability through Ownership, Shared Responsibility and Financial Sustainability Presentation by Professor John Idoko Director-General National Agency for the Control of AIDS December 5, 2011
Setting the Scene: Celebrating Success. . • In 2000, very few people in low or middle income countries were receiving treatment. • At the start of 2011, over six million people were on Antiretroviral therapy (ART). • UNAIDS reports that by 2009, eight low and middle-countries had achieved universal access to ART • Innovation, generics & collaborative partnerships, have reduced cost 1 st line ARVs from several thousand US dollars to under $200 person per year • Over 30 countries have seen declines in overall HIV prevalence. • New technologies for HIV prevention
. . . Recognising the Challenges • Unprecedented, yet insufficient and fragile progress – New infections outpacing the response: 2. 6 m new infections vs 1. 8 m deaths and 9 m req treatment • Waning political commitment and fragile country ownership – Emerging leadership in many low/middle-income countries yet insufficient political will. Funding remains largely externally funded – unsustainable! • An unsustainable trajectory of program costs – Current costs of the response – transactions, drugs, commodities and delivery of services unsustainable • Declining available resources – Due to global economic crisis, available resources have not increased due to stagnation/decline in donor funding
Why do we face an AIDS response crisis ? 1. 2. 3. 4. 5. The need is immense and increasing yearly Demand from (patients & govs) is growing ART coverage and prevention are expanding. . costs are thus expanding rapidly. . while external financing has likely peaked The big questions • How much money will we require? • Who will pay? • Can efficiency improve so that money goes further ? • How do we best use the money we have, given the multiple claims to it?
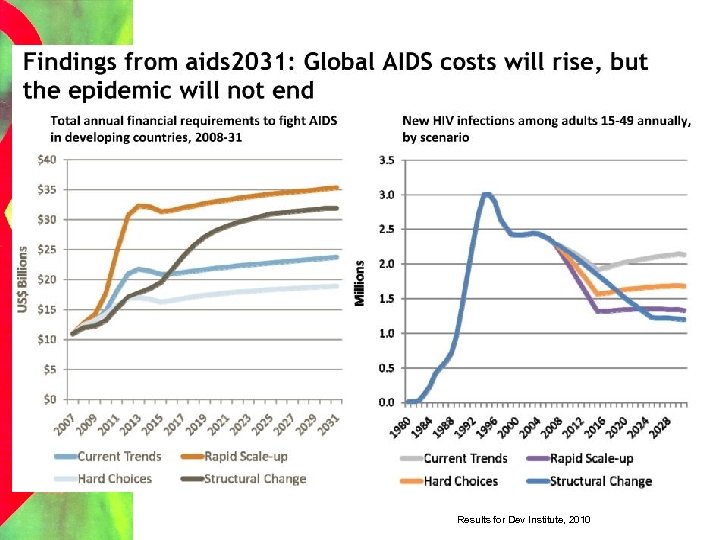
Results for Dev Institute, 2010
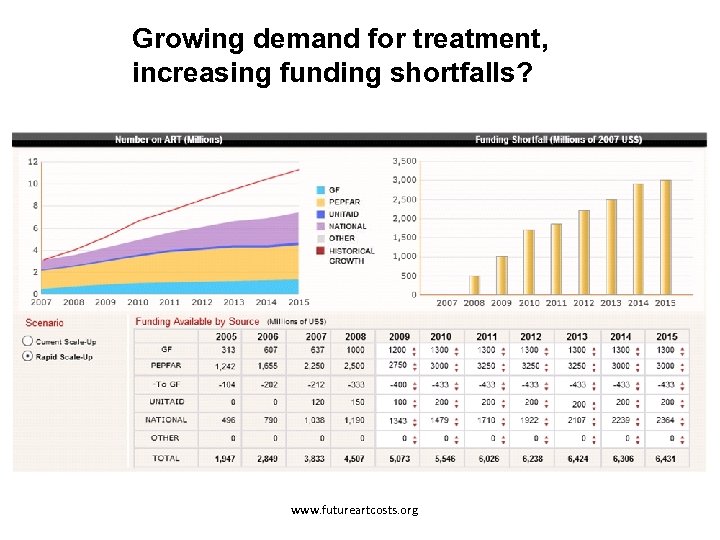
Growing demand for treatment, increasing funding shortfalls? www. futureartcosts. org
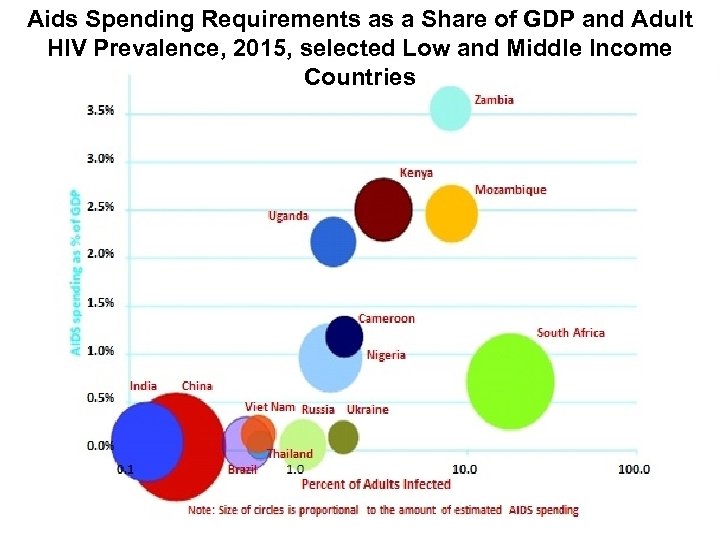
Aids Spending Requirements as a Share of GDP and Adult HIV Prevalence, 2015, selected Low and Middle Income Countries Results for Dev Institute, 2010
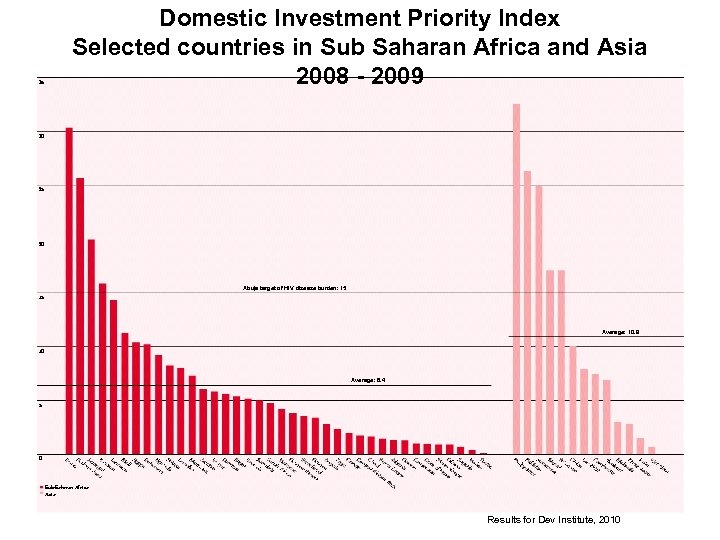
35 Domestic Investment Priority Index Selected countries in Sub Saharan Africa and Asia 2008 - 2009 30 25 20 Abuja target of HIV disease burden: 15 15 Average: 10. 9 10 Average: 6. 4 5 0 Sub-Saharan Africa Asia Results for Dev Institute, 2010
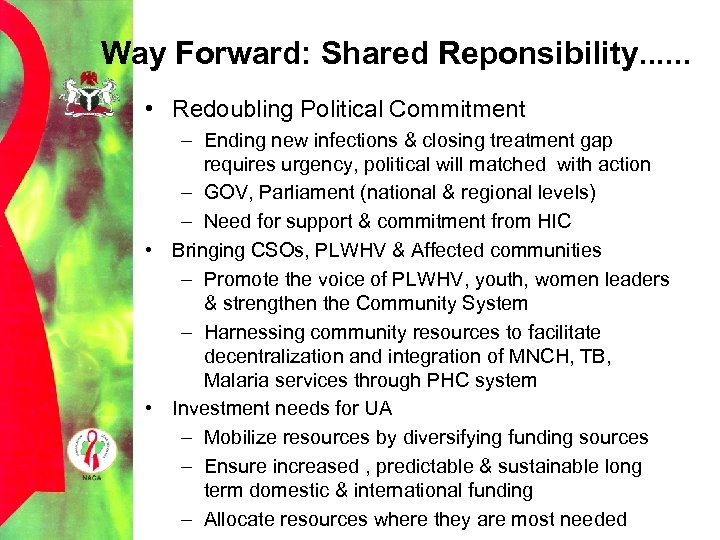
Way Forward: Shared Reponsibility. . . • Redoubling Political Commitment – Ending new infections & closing treatment gap requires urgency, political will matched with action – GOV, Parliament (national & regional levels) – Need for support & commitment from HIC • Bringing CSOs, PLWHV & Affected communities – Promote the voice of PLWHV, youth, women leaders & strengthen the Community System – Harnessing community resources to facilitate decentralization and integration of MNCH, TB, Malaria services through PHC system • Investment needs for UA – Mobilize resources by diversifying funding sources – Ensure increased , predictable & sustainable long term domestic & international funding – Allocate resources where they are most needed
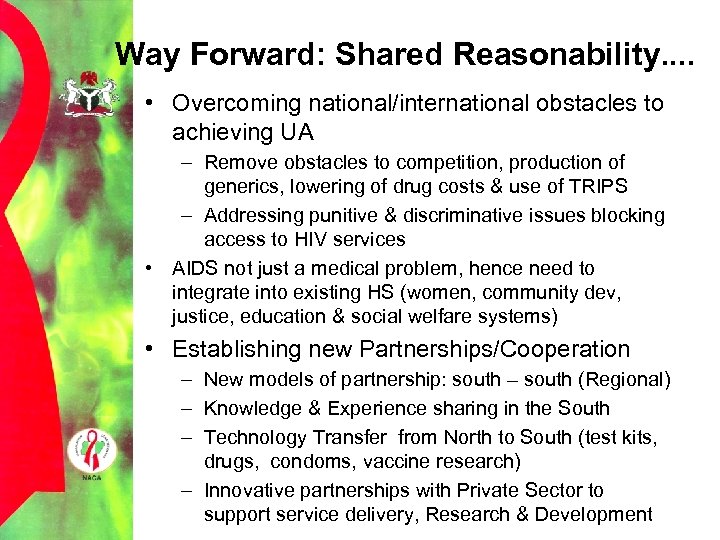
Way Forward: Shared Reasonability. . • Overcoming national/international obstacles to achieving UA – Remove obstacles to competition, production of generics, lowering of drug costs & use of TRIPS – Addressing punitive & discriminative issues blocking access to HIV services • AIDS not just a medical problem, hence need to integrate into existing HS (women, community dev, justice, education & social welfare systems) • Establishing new Partnerships/Cooperation – New models of partnership: south – south (Regional) – Knowledge & Experience sharing in the South – Technology Transfer from North to South (test kits, drugs, condoms, vaccine research) – Innovative partnerships with Private Sector to support service delivery, Research & Development

Addressing Sustainable Financing • Grouping countries into 2 categories based on HS funding levels, over all economy & HIV/AIDS prevalence: – Category 1: High prev, Low income eg Zambia, Mozambique • Greatest need for new & strengthened finance mechanisms • Require external resources (short, mid & long term) • Primary recipients of IFF & other external funds – Category 2: Low-High prev, Middle Income (Botswana, SA, Thailand) • Can achieve financial sustainability • Great opportunity for mobilization of domestic resources
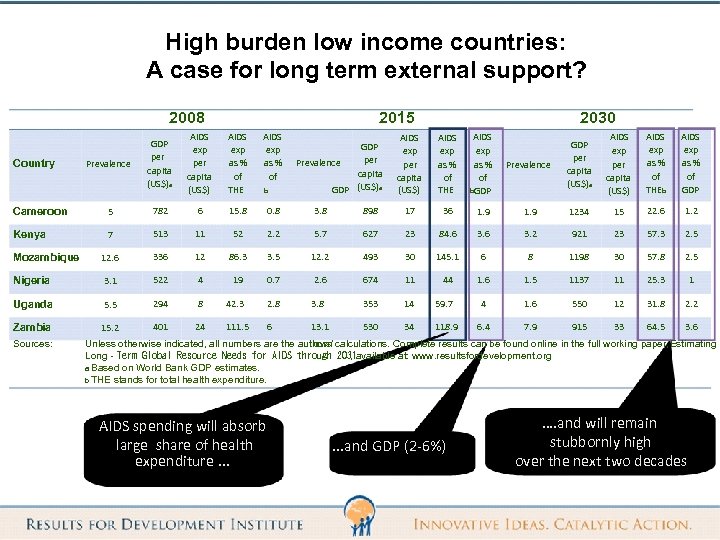
High burden low income countries: A case for long term external support? 2008 Country Prevalence 2015 GDP per capita (US$)a AIDS exp per capita (US$) AIDS exp as % of THE AIDS exp as % of b GDP per Prevalence capita (US$)a GDP 2030 AIDS exp per capita (US$) AIDS exp as % of THE AIDS exp as % of b GDP Prevalence GDP per capita (US$)a AIDS exp per capita (US$) AIDS exp as % of THEb AIDS exp as % of GDP Cameroon 5 782 6 15. 8 0. 8 3. 8 898 17 36 1. 9 1234 15 22. 6 1. 2 Kenya 7 513 11 52 2. 2 5. 7 627 23 84. 6 3. 2 921 23 57. 3 2. 5 12. 6 336 12 86. 3 3. 5 12. 2 493 30 145. 1 6 8 1198 30 57. 8 2. 5 Nigeria 3. 1 522 4 19 0. 7 2. 6 674 11 44 1. 6 1. 5 1137 11 25. 3 1 Uganda 5. 5 294 8 42. 3 2. 8 353 14 59. 7 4 1. 6 550 12 31. 8 2. 2 Zambia 15. 2 401 24 111. 5 6 13. 1 530 34 118. 9 6. 4 7. 9 915 33 64. 5 3. 6 Mozambique Sources: Unless otherwise indicated, all numbers are the authors’ own calculations. Complete results can be found online in the full working paper, Estimating Long‐Term Global Resource Needs for AIDS through 2031 , available at: www. resultsfordevelopment. org a Based on World Bank GDP estimates. b THE stands for total health expenditure. AIDS spending will absorb large share of health expenditure. . . and GDP (2‐ 6%) …. and will remain stubbornly high over the next two decades
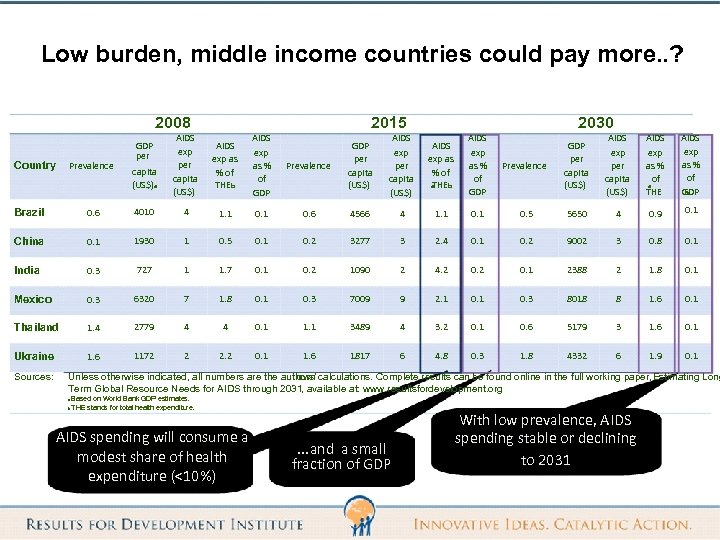
Low burden, middle income countries could pay more. . ? 2008 Country Prevalence GDP per capita (US$)a 2015 AIDS exp per capita (US$) AIDS exp as % of THEb AIDS exp as % of GDP 2030 Prevalence GDP per capita (US$) AIDS exp as % of a THEb AIDS exp as % of GDP Prevalence GDP per capita (US$) AIDS exp as % of a THE AIDS exp as % of GDP b Brazil 0. 6 4010 4 1. 1 0. 6 4566 4 1. 1 0. 5 5650 4 0. 9 0. 1 China 0. 1 1930 1 0. 5 0. 1 0. 2 3277 3 2. 4 0. 1 0. 2 9002 3 0. 8 0. 1 India 0. 3 727 1 1. 7 0. 1 0. 2 1090 2 4. 2 0. 1 2388 2 1. 8 0. 1 Mexico 0. 3 6320 7 1. 8 0. 1 0. 3 7009 9 2. 1 0. 3 8018 8 1. 6 0. 1 Thailand 1. 4 2779 4 4 0. 1 1. 1 3489 4 3. 2 0. 1 0. 6 5179 3 1. 6 0. 1 Ukraine 1. 6 1172 2 2. 2 0. 1 1. 6 1817 6 4. 8 0. 3 1. 8 4332 6 1. 9 0. 1 Sources: Unless otherwise indicated, all numbers are the authors’ own calculations. Complete results can be found online in the full working paper, Estimating Long Term Global Resource Needs for AIDS through 2031, available at: www. resultsfordevelopment. org a b Based on World Bank GDP estimates. THE stands for total health expenditure. AIDS spending will consume a modest share of health expenditure (<10%) . . . and a small fraction of GDP With low prevalence, AIDS spending stable or declining to 2031
Why Sustainable Financing is Critical • Ensuring adequate and fair financing in the future for HIV/AIDS and related diseases require: – New sources of funding be explored (global, private, domestic) – New mechanisms dev for health sector financing which are equitable and sustainable (external & domestic; public & private) – Existing & emerging innovative health systems financing schemes (eg social insurance, VSC, taxes, etc) protected from collapse – Plans for sustainability developed at country level which absorbs impact of HIV/AIDS into overall health system financing programs
Available Models of Innovative Financing • Voluntary Solidarity Contribution (Air/Mobile) • Targeted taxes (Air line, Mobile, VAT, etc) – UNITAID, Kenya, Nigeria, Ghana • National AIDS Trust Fund (Zimbabwe) • Massive Good • International Financial Facility (IFFIm) • Currency Transactional Levy • Global Lottery • Debt 2 Health • Insurance schemes (Rwanda, Nigeria) • Procurement (Market dynamics, pooled proc)
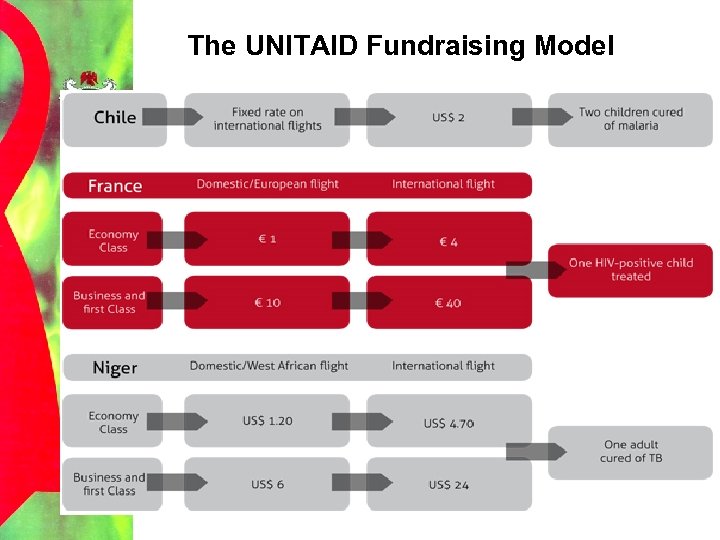
The UNITAID Fundraising Model
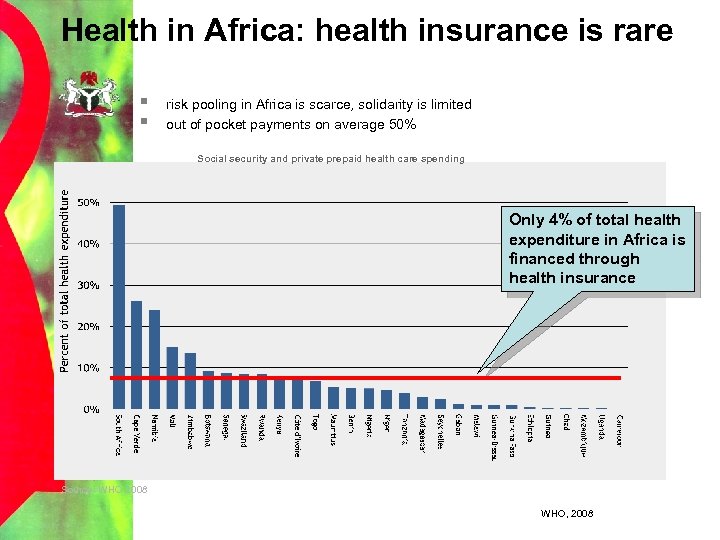
Health in Africa: health insurance is rare § § risk pooling in Africa is scarce, solidarity is limited out of pocket payments on average 50% Social security and private prepaid health care spending Only 4% of total health expenditure in Africa is financed through health insurance Source: WHO 2008 WHO, 2008
Getting more value for money. . . • Choosing interventions strategically • Focusing them where they will have maximum benefit • Improve implementation efficiency – Better management – Strategic integration with other services • Transparency and accountability • Addressing HR shortages: – – Improved networking with community level providers Expert clients Task shifting Integrating HIV/AIDS service provision into primary health care • Maximize long-term benefit – Efforts to finance AIDS program should consider what is needed now and what is needed in the long term
How can we solve the AIDS crisis? 1. Intensify prevention – today’s infection are tomorrow’s ART patients – – Do what we know works Invest in biomedical breakthroughs 2. Make Treatment cheaper – – Reduce further the cost of drugs and tests Design/implement/evaluate less expensive delivery models 3. Strengthen domestic funding – – – Reach towards self sufficiency in more middle income countries Expand national financial ownership Bridge treatment costs with financial protection schemes 4. Redirect/Re-prioritize donor funding – – – Focus on high burden countries Align Donor funding with national plans Ensure country oversight of domestic/donor funds and integration into the country systems 5. Make the money work smarter – – Reduce organizational and management inefficiencies Ensure effective HR management (Task Shifting)
THANK YOU!
6f85d3a0b43ea5c43751c44c4f471ba3.ppt