f336eb460b1b944509a5ef6b83b6b5c0.ppt
- Количество слайдов: 20
ABSTRACT ID: IRIA - 1018
*Spinal cavernous angiomas are rare in the epidural location and therefore seldom considered in the differential diagnosis of spinal cord compression. *They result more frequently from the extradural extension of vertebral body cavernomas and have rarely a pure spinal epidural location. *The condition can be familial or sporadic.
*It usually presents in the 3 rd to 6 th decades of life with progressive paraparesis, sensory loss and pain. *Incase of any hemorrhage or thrombosis within the haemangioma, sudden onset of the symptoms may occur. *Microscopically, the lesions consists of large thin walled hyalinised endothelial-lined sinusoidal vascular spaces with absence of elastic and muscular tissue and intervening neural tissue. *It may be indistinguishable from chronic progressive radiculomyelopathy.
FOUR CLINICAL PATTERNS: 1. Discrete episodes of neurological deterioration with varying degrees of recovery between episodes. 2. Slow progression of neurological decline. 3. Acute onset of symptoms with rapid decline. 4. Acute onset of mild symptoms with subsequent gradual decline lasting weeks to months.
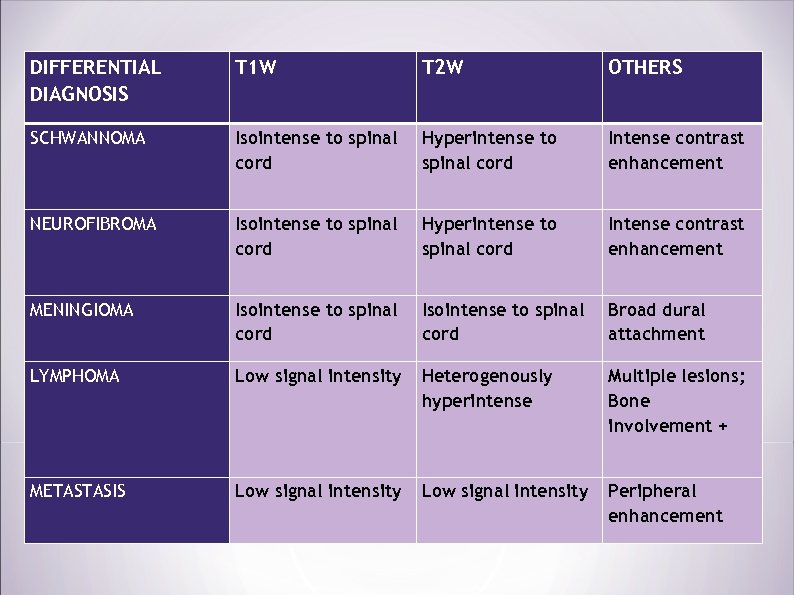
DIFFERENTIAL DIAGNOSIS T 1 W T 2 W OTHERS SCHWANNOMA Isointense to spinal cord Hyperintense to spinal cord Intense contrast enhancement NEUROFIBROMA Isointense to spinal cord Hyperintense to spinal cord Intense contrast enhancement MENINGIOMA Isointense to spinal cord Broad dural attachment LYMPHOMA Low signal intensity Heterogenously hyperintense Multiple lesions; Bone involvement + METASTASIS Low signal intensity Peripheral enhancement
OTHER DDs: 1. Epidural lipomatosis. 2. Extra-osseous Ewing’s sarcoma. 3. Epidural extramedullary haematopoiesis. 4. Epidural abscess. Surgical resection of the lesion is the treatment of choice with radiotherapy as an adjuvant.

*A 65 years old male patient had been referred to our department with complaints of, - Weakness and numbness of both lower limbs for the past 2 years. - Had decreased sensation in both lower limbs. - No h/o any trauma / urinary disturbances. - A known hypertensive for 10 years (not on medication).
CLINICAL EXAMINATION: *BP – 160/110 mm Hg *No pallor/icterus/cyanosis/clubbing/pedal edema/lymphadenopathy. *SYSTEMIC EXAMINATION: CVS/RS/ABD – normal.
CNS – *HMF & CN EXAMINATION: within normal limits. *MOTOR EXAMINATION: within normal limits. *SENSORY EXAMINATION: Graded hypoesthesia from T 10 downwards. Beever’s sign – positive.
B/L KNEE JERK – 3+ B/L ANKLE JERK – absent. RHOMBERG’S TEST – Positive. GAIT – mild ataxic gait. No cerebellar/meningeal signs. ? cervical myelopathy/IVDP L 4 -L 5.
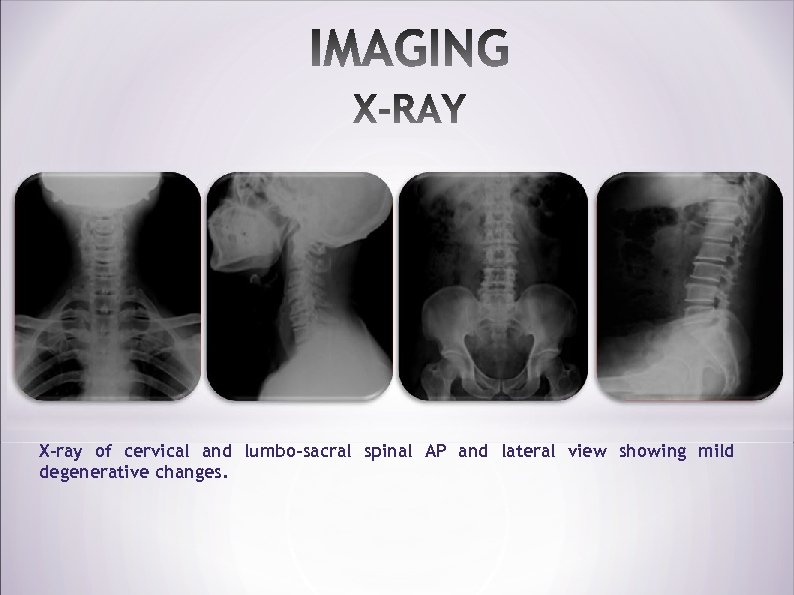
X-ray of cervical and lumbo-sacral spinal AP and lateral view showing mild degenerative changes.

MRI Whole Spine screening showing the extradural extramedullary lesion at the level of D 8 -D 10 vertebrae.
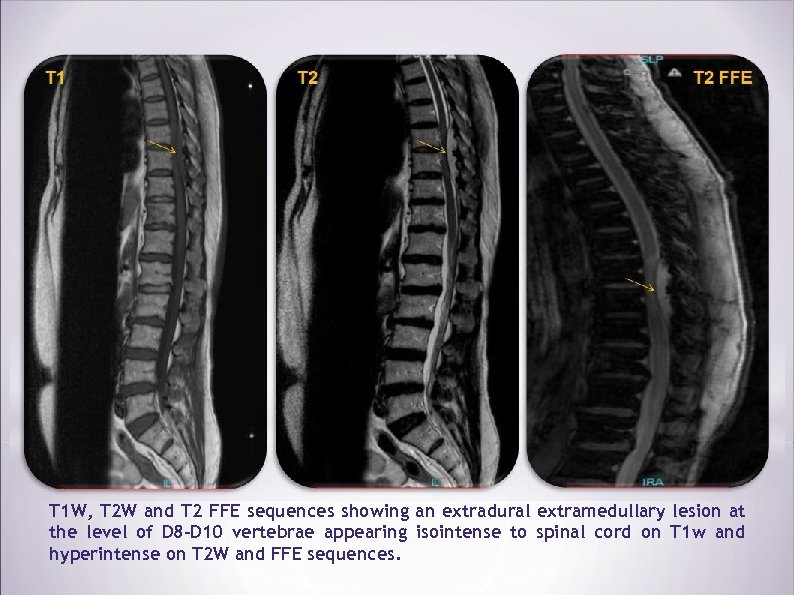
T 1 W, T 2 W and T 2 FFE sequences showing an extradural extramedullary lesion at the level of D 8 -D 10 vertebrae appearing isointense to spinal cord on T 1 w and hyperintense on T 2 W and FFE sequences.
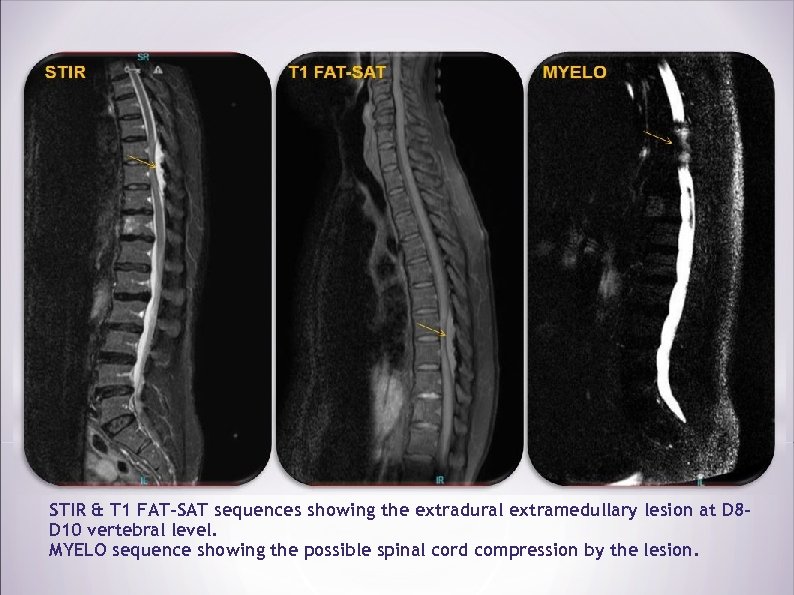
STIR & T 1 FAT-SAT sequences showing the extradural extramedullary lesion at D 8 D 10 vertebral level. MYELO sequence showing the possible spinal cord compression by the lesion.
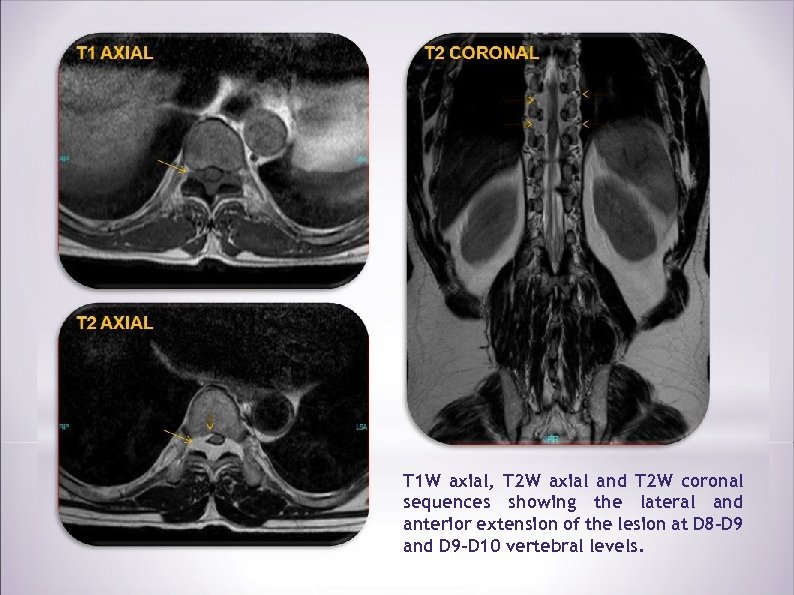
T 1 W axial, T 2 W axial and T 2 W coronal sequences showing the lateral and anterior extension of the lesion at D 8 -D 9 and D 9 -D 10 vertebral levels.
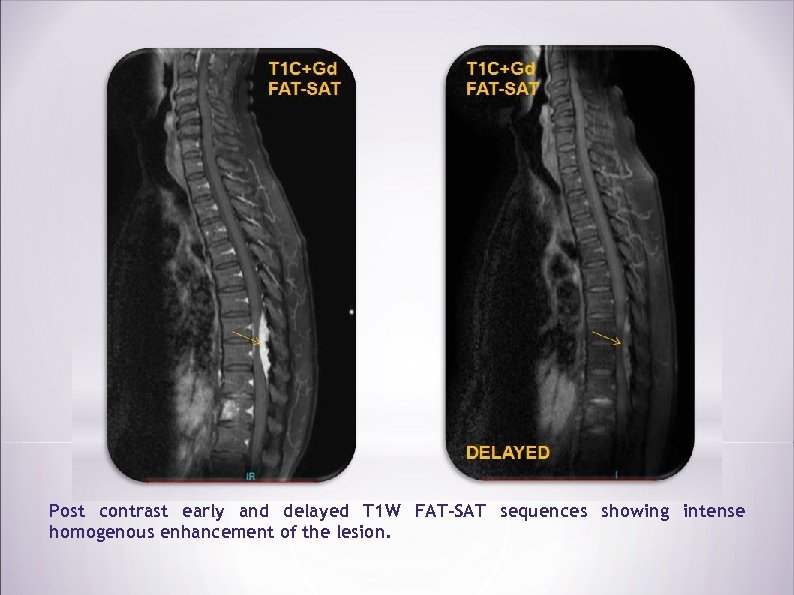
Post contrast early and delayed T 1 W FAT-SAT sequences showing intense homogenous enhancement of the lesion.
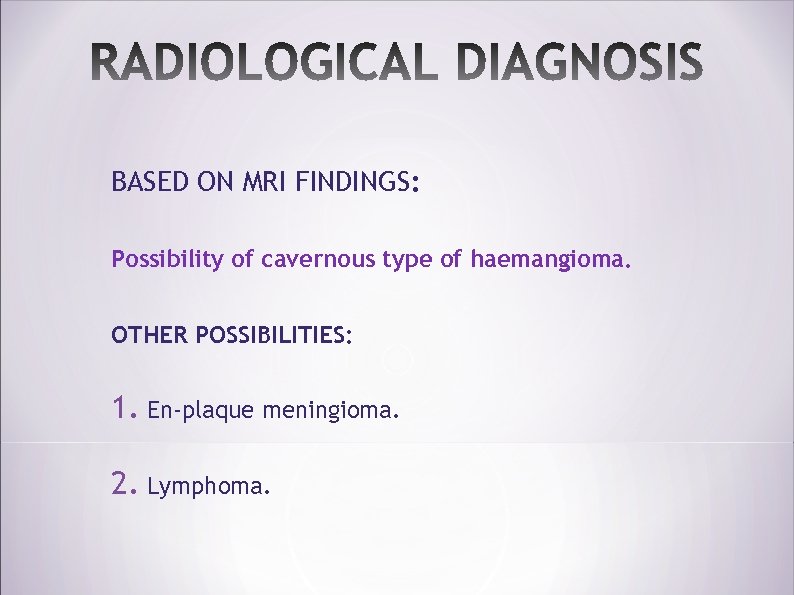
BASED ON MRI FINDINGS: Possibility of cavernous type of haemangioma. OTHER POSSIBILITIES: 1. En-plaque meningioma. 2. Lymphoma.
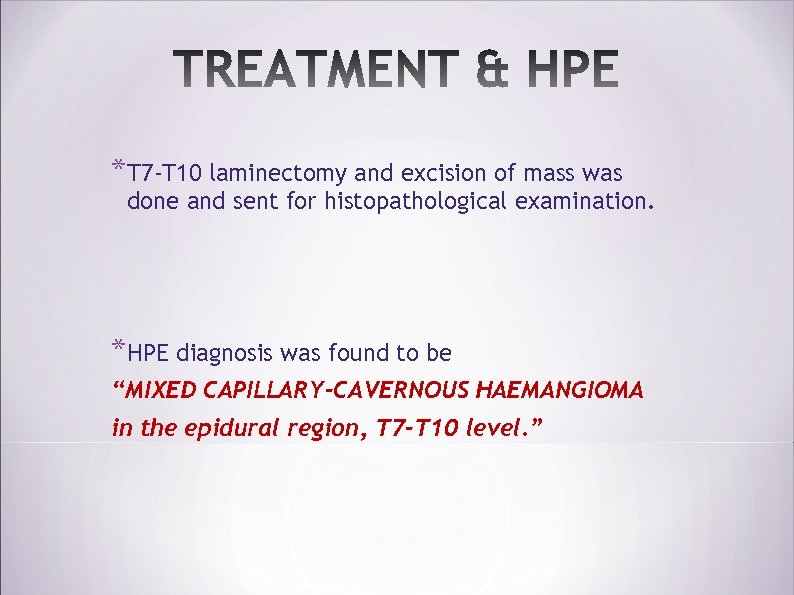
*T 7 -T 10 laminectomy and excision of mass was done and sent for histopathological examination. *HPE diagnosis was found to be “MIXED CAPILLARY-CAVERNOUS HAEMANGIOMA in the epidural region, T 7 -T 10 level. ”
*Spinal cavernous haemangioma is a rare condition to occur in the level of thoracic spine. *The case was reported for its difficulty in making a preoperative diagnosis clinically.
1. Goyal A, Singh AK, Gupta V, Tatke M. Spinal epidural cavernous haemangioma: a case report and review of literature. Spinal Cord 2002; 40: 200 -2. 2. Shin JH, Lee HK. Rhim SC. Park SH, Choi CG. Suh DC. Spinal cpi dural cavernous hemangioma: MR findings. J Comput Assist Tomogr 2001; 25: 257 -61. 3. Saringer W, Nobauer I, Haberler C, et al. Extraforaminal, thoracic, epiduralcavernoushaemangioma: casereportwithanalysisofmagneticresonanceimaging characteristics and review of the literature. Acta Neurochir (Wien) 2001; 143: 1293– 9 4. Morioka T, Nakagaki H, Matsushima T, et al. Dumbbell-shaped spinal epidural cavernous angioma. Surg Neurol 1986; 25: 142– 44. 5. Jalladeau E, Carpentier AF, Napolitano M, Delattre JY. Lipomatose épidurale corticoinduite. Rev Neurol 2000; 156: 517 -519. 6. Harrington JF, Khan A, Grunnet M. Spinal epidural cavernous angioma presenting as a lumbar radiculopathy with analysis of magnetic resonance imaging chraracteristics: Case report. Neurosurgery 1995; 36: 581 -584.
f336eb460b1b944509a5ef6b83b6b5c0.ppt