824e45e51adb96e5f817fb02b56846bb.ppt
- Количество слайдов: 27
Abnormal Presentations, Prematurity, & VBAC Joe Dietrick, CRNA, M. A. Truman Medical Center Kansas City, MO
Objectives – Identify the three parameters associated with fetal presentation – Understand the anesthetic implications of the most common abnormal presentations – Define prematurity, PROM, and PPROM, and the anesthetic implications – Discuss current guidelines for vaginal birth after cesarean (VBAC) & the anesthetic implications
Presentation Parameters • Presentation: portion of fetus over the pelvis – Cephalic (vertex, brow, face) – Breech (frank, complete, incomplete) – Shoulder • Lie: alignment of fetal-maternal spines – Longitudinal – Transverse • Position: relationship of designated part to pelvis
Normal Presentation • Occiput anterior (OA) implies: – Cephalic vertex presentation – Longitudinal lie – Occiput of fetal head towards maternal pubic bone • Fetus normally rotates to this position from occiput transverse or occiput oblique
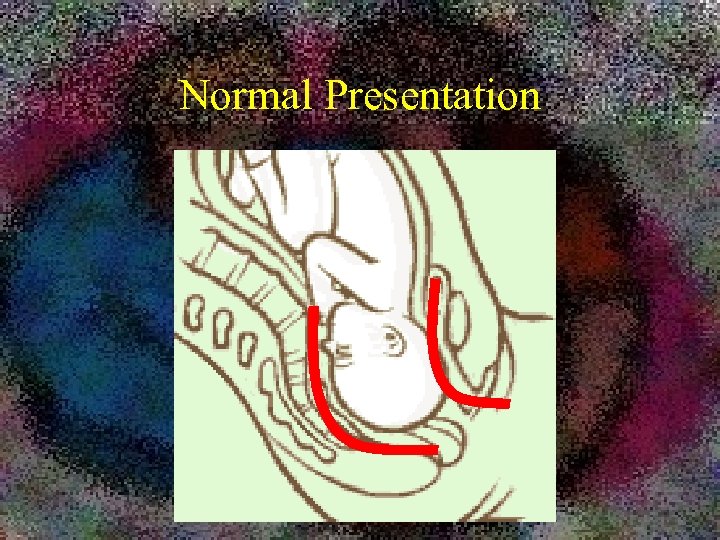
Normal Presentation
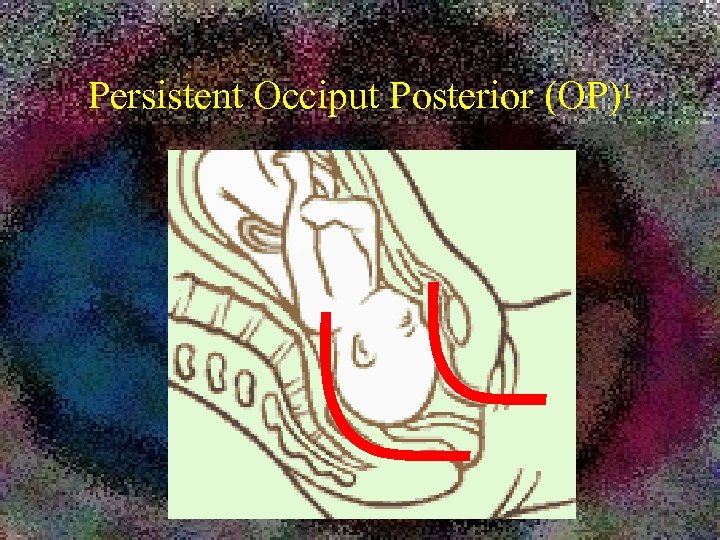
Persistent Occiput Posterior (OP)1
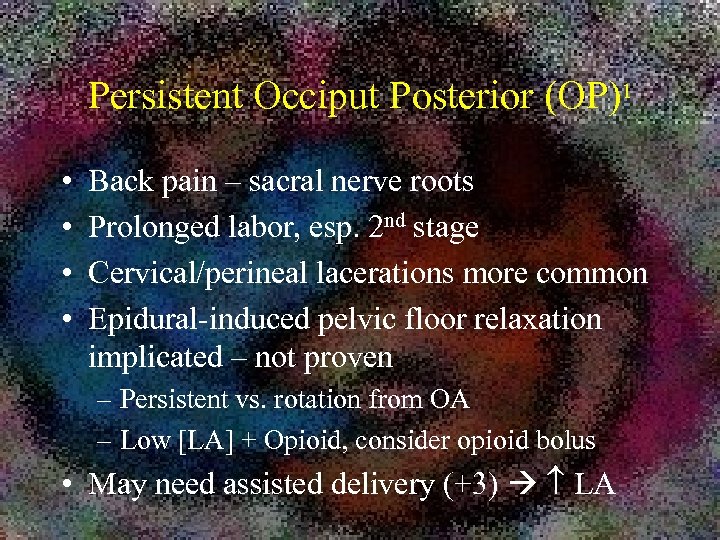
Persistent Occiput Posterior (OP)1 • • Back pain – sacral nerve roots Prolonged labor, esp. 2 nd stage Cervical/perineal lacerations more common Epidural-induced pelvic floor relaxation implicated – not proven – Persistent vs. rotation from OA – Low [LA] + Opioid, consider opioid bolus • May need assisted delivery (+3) LA
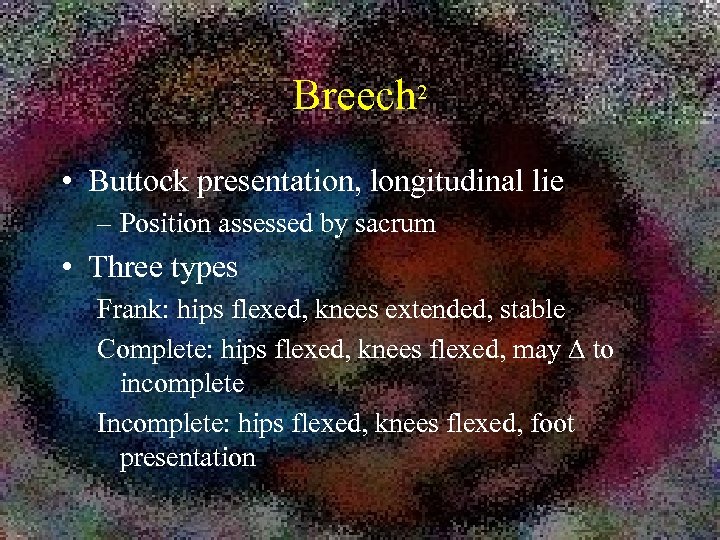
Breech 2 • Buttock presentation, longitudinal lie – Position assessed by sacrum • Three types Frank: hips flexed, knees extended, stable Complete: hips flexed, knees flexed, may to incomplete Incomplete: hips flexed, knees flexed, foot presentation
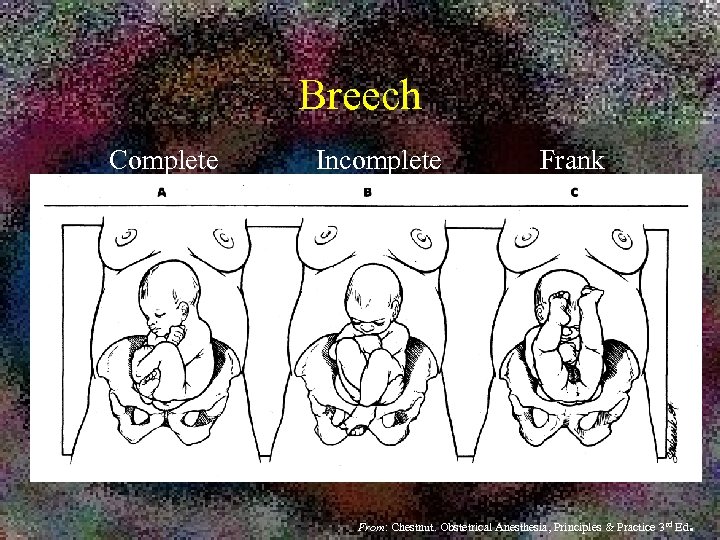
Breech Complete Incomplete Frank From: Chestnut. Obstetrical Anesthesia, Principles & Practice 3 rd Ed .

Breech 2 • More common: – premature > term – Uterine distension / relaxation – Uterine / pelvic abnormalities – Fetal abnormalities – Variety of obstetric conditions • Previous breech • Placenta previa
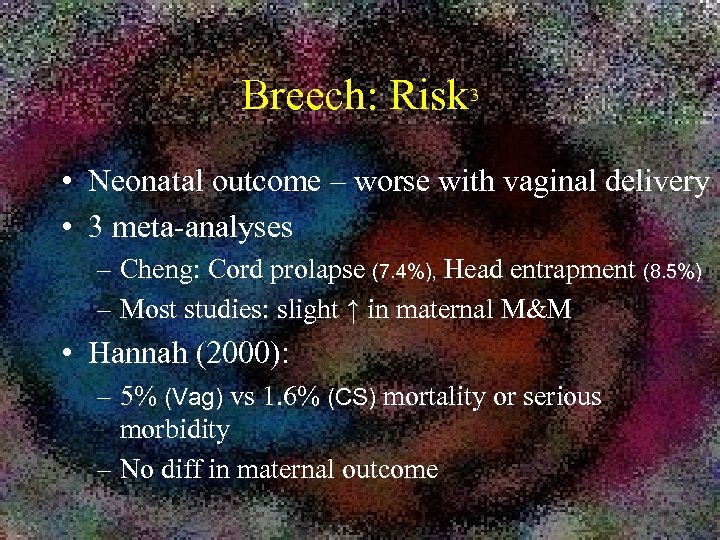
Breech: Risk 3 • Neonatal outcome – worse with vaginal delivery • 3 meta-analyses – Cheng: Cord prolapse (7. 4%), Head entrapment (8. 5%) – Most studies: slight ↑ in maternal M&M • Hannah (2000): – 5% (Vag) vs 1. 6% (CS) mortality or serious morbidity – No diff in maternal outcome
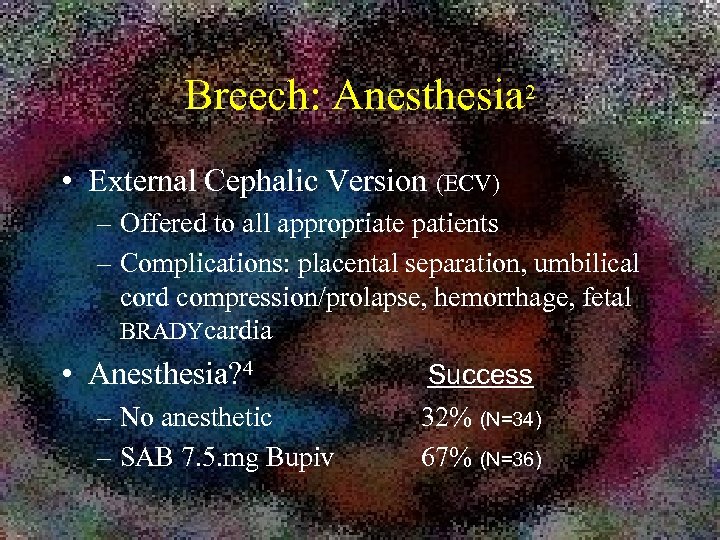
Breech: Anesthesia 2 • External Cephalic Version (ECV) – Offered to all appropriate patients – Complications: placental separation, umbilical cord compression/prolapse, hemorrhage, fetal BRADYcardia • Anesthesia? 4 – No anesthetic – SAB 7. 5. mg Bupiv Success 32% (N=34) 67% (N=36)
Breech: Anesthesia • ACOG Guidelines revised 20065 – Allow SVD with appropriate experience – Must have protocols for eligibility & management – “detailed patient informed consent” • CS most common 2 – Regional anesthesia • Uterine relaxation may be inadequate • NTG 50 g IV
Breech: Anesthesia 2 • Vaginal delivery (frank or complete only) – Normally spontaneous • Less freq assisted; no induction or augmentation – Increased M&M – Epidural desirable • Pain relief • Inhibition of early pushing • Option for CS or perineal dosing for delivery of head • Us: delivery in CS room; neonate resusc.
Breech: Anesthesia 2 • “Holy ___ Batman”: Fetal head entrapment – Cervical incisions – Uterine & cervical relaxation • Epidural • NTG? – CS, with fetal replacement…….
Other presentations 2 • Face – 70 -80% deliver vaginally • Brow – CS • Compound vertex (arm) – CS for cord prolapse or failure to progress • Shoulder (not shoulder dystocia) – Transverse lie – May attempt ECV – Normally CS
Preterm Labor & Delivery • Premature rupture of membranes – PROM: ROM before onset of labor – PPROM: PROM + prematurity • ACOG #80, 20076 – ≥ 34 wks: induce & deliver – 31 weeks: expectant management – “tweener”: evaluate fetal lung maturity – Abx prophylaxis
Shoulder Dystocia 2 • Vaginal delivery of vertex presentation – Anterior shoulder trapped under pubic bone after delivery of head – Umbilical cord trapped in pelvis • “Recognition that should dystocia exists often is followed by (calmness) giving way to panic. ” • Outcomes – Fetal death, brachial plexus injury – Maternal hemorrhage
Shoulder Dystocia 2 • Risk factors – Macrosomia – Maternal DM – Previous shoulder dystocia – Labor components • Delayed active phase • Prolonged second stage • Operative vaginal delivery
Shoulder Dystocia 2 • OB management – Suprapubic pressure – Hyperflexion of maternal hips (Mc. Robert’s) – Vaginal maneuvers • • Extend episiotomy Rotate posterior shoulder (corkscrew: Woods) Deliver posterior arm Deliberate clavicular fracture – Cephalad replacement (Zavanelli) CS
Shoulder Dystocia 2 • Anesthesia – You can’t do anything about the problem – Prepare for STAT CS. – Uterine relaxation? • May help relieve • Allows cephalad replacement • Drugs – Nitroglycerin 50 -100 mcg IV ? – Terbutaline 0. 25 mg SQ – General anesthesia/volatile agents
VBAC & TOLAC • VBAC: vaginal birth after cesarean – One “attempts VBAC” until one has delivered • TOLAC: trial of labor after cesarean – technically more correct, but rarely used • Risks – Uterine rupture (0. 5 – 0. 9% for low tranverse)8 – Factors: 7 • no prev SVD • mult CS • induced/augmented labor: 100/124 ruptures received oxytocic
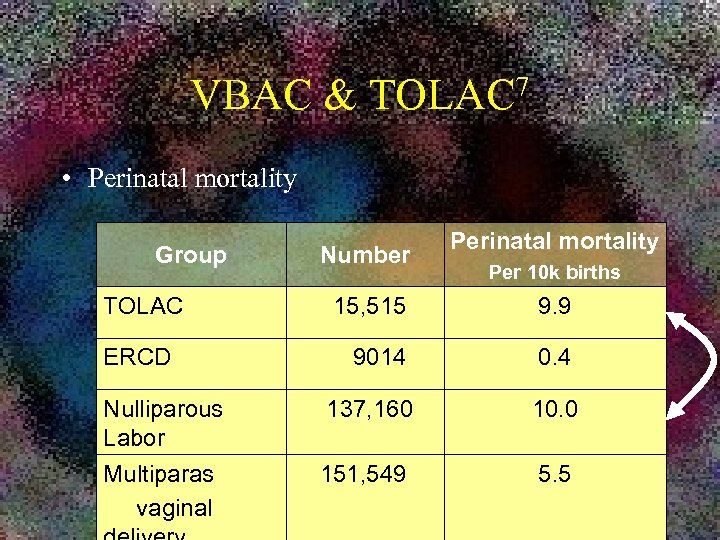
VBAC & 7 TOLAC • Perinatal mortality Group TOLAC Number Perinatal mortality Per 10 k births 15, 515 9. 9 9014 0. 4 Nulliparous Labor 137, 160 10. 0 Multiparas vaginal 151, 549 5. 5 ERCD
VBAC: ACOG Practice Bulletin #115, 20108 • Safety: VBAC > Elect Repeat CS > Failed TOLAC • Changes – OK for…. – 2 previous LTCS – Ext Cephalic Version – Twin (prev LTCS x 1) – Induction – Unknown uterine scar (unless classical highly likely) • Staff availability – Patient autonomy allows acceptance of increased levels of risk after being clearly informed.
OB Litigation 10 • Clark et al (2008) : OB physician ligation reduction by 1. In-house 24° CS team coverage 2. Adherence to protocols for high-risk medications 3. Improved procedure note in shoulder dystocia 4. More conservative approach to VBAC
VBAC selection 10 • Parameters – TOLAC for spontaneous labor only – Normal labor curve w/o augmentation – Absence of repetitive mod/severe decels • Outcome – uterine rupture – adverse neonatal problems
References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Gorman Maloney. S & Levinson, G (2001). Anesthesia for Abnormal Positions & Presentations, Shoulder Dystocia & Multiple Births. In Hughes, et al (Ed), Shnider & Levinson’s Anesthesia for Obstetrics, 4 th Ed. (pg 287). Philadelphia: Lippincot Williams & Wlikins, Koffel, B. (2004). Abnormal Presentation & Multiple Gestation. In D. Chestnut (Ed. ), Obstetrical Anesthesia: Principles & Practice (pp. 623 -639). Philadelphia: Elsevier Mosby. Pratt, S. (2003). Anesthesia for Breech Presentation & Multiple Gestation. Clinical Obstetrics & Gynecology, 46(3), 711 -729. Weiniger et al (2007). Spinal Analgesia for External Cephalic Version. OBSTETRICS & GYNECOLOGY, 110(6), 1343 -1350. ACOG Committee Opinion, No. 340 (2006). Term Singleton Breech Delivery. OBSTETRICS & GYNECOLOGY, 108(1), 235 -237. ACOG Practice Bulletin No. 80 (2007). Premature rupture of membranes. OBSTETRICS & GYNECOLOGY , 109(4), 1007 -1019. Welischar, J, & Quirk, J (2009). Trial of labor after cesarean delivery. Retrieved 04/03/09 from Up. To. Date. Website: http: //uptodateonline. com/online/content/topic. do? topic. Key=labordel/9085&selected. Title=1~150 ACOG Practice Bulletin No. 115 (2010). Vaginal Birth After Previous Cesarean Delivery. OBSTETRICS & GYNECOLOGY, 116(2), 450 -463. Yamamura Y, et al (2006). Trial of vaginal breech delivery: current role. Clin Obstet Gynecol, 50(2): 526 -36. Clark, S. et al (2008). Reducing Obstertic Litigation Through Alterations in Practice Patterns. OBSTETRICS & GYNECOLOGY, 112(6): 1279 -
824e45e51adb96e5f817fb02b56846bb.ppt