90ffdaca040954c6479c8a0208e0fe0f.ppt
- Количество слайдов: 29
 A Review and Meta. Analysis of Utility Values for Lung Cancer Julie Migrin ASPH Environmental Health Fellow at the U. S. EPA
A Review and Meta. Analysis of Utility Values for Lung Cancer Julie Migrin ASPH Environmental Health Fellow at the U. S. EPA
 Outline Background: QALYs and lung cancer n Illustrate the problem n Suggest potential explanations n Methods n Results and conclusions n Next steps n
Outline Background: QALYs and lung cancer n Illustrate the problem n Suggest potential explanations n Methods n Results and conclusions n Next steps n
 QALYs and utilities n Quality adjusted life year, QALY, is a measure of healthrelated quality of life ¨ n Incorporates measures of both quantity (years) and quality of life (utility) Utility value (preference score, preference weight) Ranges from 0 to 1 Indicator of global, health related quality of life ¨ No one way to elicit ¨ ¨ n Uses: Regulatory cost effectiveness analysis, medical decision making ·Assume a policy extends the baseline health profile (white) · The gain in QALYs is shown in gray
QALYs and utilities n Quality adjusted life year, QALY, is a measure of healthrelated quality of life ¨ n Incorporates measures of both quantity (years) and quality of life (utility) Utility value (preference score, preference weight) Ranges from 0 to 1 Indicator of global, health related quality of life ¨ No one way to elicit ¨ ¨ n Uses: Regulatory cost effectiveness analysis, medical decision making ·Assume a policy extends the baseline health profile (white) · The gain in QALYs is shown in gray
 Lung Cancer n n n 200, 000 new U. S. cases each year (CDC data) Cost: $9. 6 billion per year in U. S. (CDC data) Environmental/Occupational Causes ¨ Radon ¨ Pesticides ¨ Asbestos ¨ Polycyclic aromatic hydrocarbons ¨ Vinyl Chloride (monomer of PVC) ¨ Arsenic ¨ Chromium (PAHs) What’s Lurking in Your Countertop? July 24, 2008
Lung Cancer n n n 200, 000 new U. S. cases each year (CDC data) Cost: $9. 6 billion per year in U. S. (CDC data) Environmental/Occupational Causes ¨ Radon ¨ Pesticides ¨ Asbestos ¨ Polycyclic aromatic hydrocarbons ¨ Vinyl Chloride (monomer of PVC) ¨ Arsenic ¨ Chromium (PAHs) What’s Lurking in Your Countertop? July 24, 2008
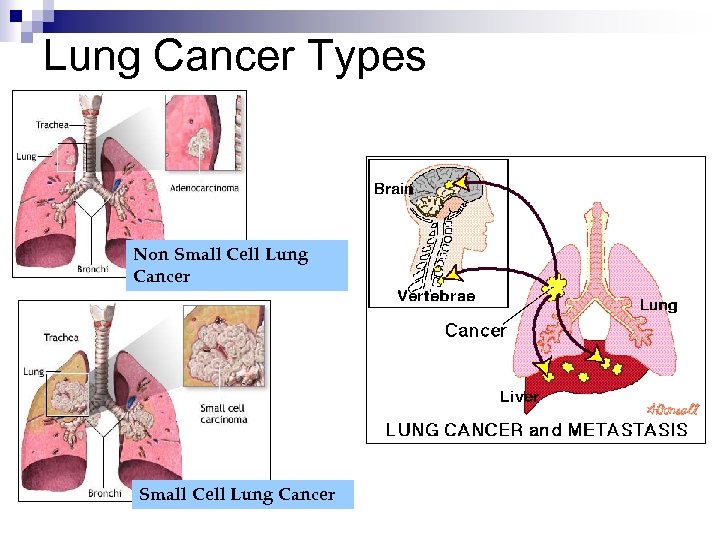 Lung Cancer Types Non Small Cell Lung Cancer
Lung Cancer Types Non Small Cell Lung Cancer
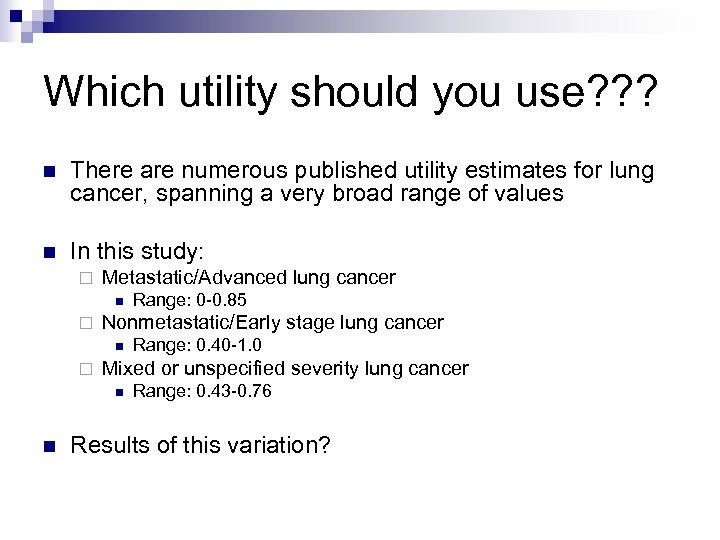 Which utility should you use? ? ? n There are numerous published utility estimates for lung cancer, spanning a very broad range of values n In this study: ¨ Metastatic/Advanced lung cancer n ¨ Nonmetastatic/Early stage lung cancer n ¨ Range: 0. 40 -1. 0 Mixed or unspecified severity lung cancer n n Range: 0 -0. 85 Range: 0. 43 -0. 76 Results of this variation?
Which utility should you use? ? ? n There are numerous published utility estimates for lung cancer, spanning a very broad range of values n In this study: ¨ Metastatic/Advanced lung cancer n ¨ Nonmetastatic/Early stage lung cancer n ¨ Range: 0. 40 -1. 0 Mixed or unspecified severity lung cancer n n Range: 0 -0. 85 Range: 0. 43 -0. 76 Results of this variation?
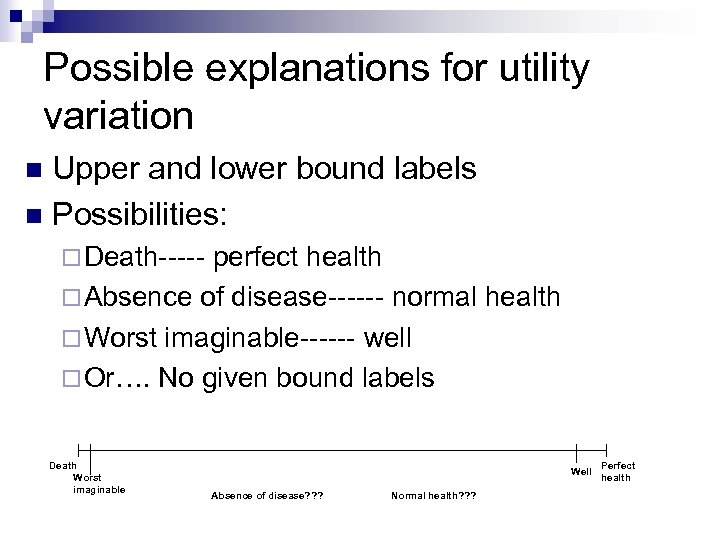 Possible explanations for utility variation Upper and lower bound labels n Possibilities: n ¨ Death----- perfect health ¨ Absence of disease------ normal health ¨ Worst imaginable------ well ¨ Or…. No given bound labels Death Worst imaginable Well Absence of disease? ? ? Normal health? ? ? Perfect health
Possible explanations for utility variation Upper and lower bound labels n Possibilities: n ¨ Death----- perfect health ¨ Absence of disease------ normal health ¨ Worst imaginable------ well ¨ Or…. No given bound labels Death Worst imaginable Well Absence of disease? ? ? Normal health? ? ? Perfect health
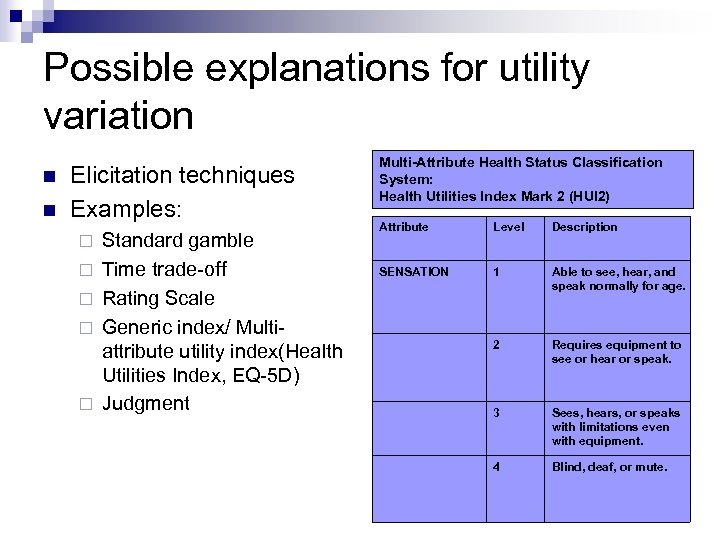 Possible explanations for utility variation n n Elicitation techniques Examples: ¨ ¨ ¨ Standard gamble Time trade-off Rating Scale Generic index/ Multiattribute utility index(Health Utilities Index, EQ-5 D) Judgment Multi-Attribute Health Status Classification System: Health Utilities Index Mark 2 (HUI 2) Attribute Level Description SENSATION 1 Able to see, hear, and speak normally for age. 2 Requires equipment to see or hear or speak. 3 Sees, hears, or speaks with limitations even with equipment. 4 Blind, deaf, or mute.
Possible explanations for utility variation n n Elicitation techniques Examples: ¨ ¨ ¨ Standard gamble Time trade-off Rating Scale Generic index/ Multiattribute utility index(Health Utilities Index, EQ-5 D) Judgment Multi-Attribute Health Status Classification System: Health Utilities Index Mark 2 (HUI 2) Attribute Level Description SENSATION 1 Able to see, hear, and speak normally for age. 2 Requires equipment to see or hear or speak. 3 Sees, hears, or speaks with limitations even with equipment. 4 Blind, deaf, or mute.
 Possible explanations for utility variation Respondent n Examples: n ¨ Patients ¨ Physicians or researchers ¨ Family members ¨ Members of the public
Possible explanations for utility variation Respondent n Examples: n ¨ Patients ¨ Physicians or researchers ¨ Family members ¨ Members of the public
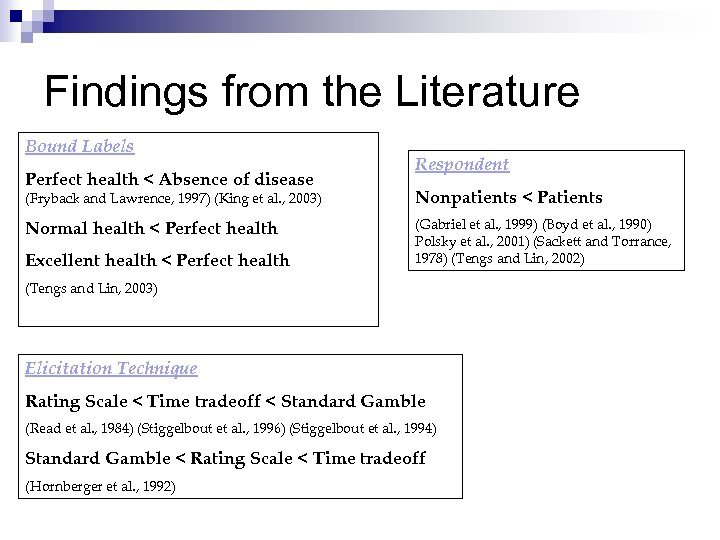 Findings from the Literature Bound Labels Perfect health < Absence of disease Respondent (Fryback and Lawrence, 1997) (King et al. , 2003) Nonpatients < Patients Normal health < Perfect health (Gabriel et al. , 1999) (Boyd et al. , 1990) Polsky et al. , 2001) (Sackett and Torrance, 1978) (Tengs and Lin, 2002) Excellent health < Perfect health (Tengs and Lin, 2003) Elicitation Technique Rating Scale < Time tradeoff < Standard Gamble (Read et al. , 1984) (Stiggelbout et al. , 1996) (Stiggelbout et al. , 1994) Standard Gamble < Rating Scale < Time tradeoff (Hornberger et al. , 1992)
Findings from the Literature Bound Labels Perfect health < Absence of disease Respondent (Fryback and Lawrence, 1997) (King et al. , 2003) Nonpatients < Patients Normal health < Perfect health (Gabriel et al. , 1999) (Boyd et al. , 1990) Polsky et al. , 2001) (Sackett and Torrance, 1978) (Tengs and Lin, 2002) Excellent health < Perfect health (Tengs and Lin, 2003) Elicitation Technique Rating Scale < Time tradeoff < Standard Gamble (Read et al. , 1984) (Stiggelbout et al. , 1996) (Stiggelbout et al. , 1994) Standard Gamble < Rating Scale < Time tradeoff (Hornberger et al. , 1992)
 Study Objectives n Objective 1: Provide pooled estimates which reflect the available lung cancer utility literature n Objective 2: Determine which methodological factors significantly influence the value of utility for lung cancer
Study Objectives n Objective 1: Provide pooled estimates which reflect the available lung cancer utility literature n Objective 2: Determine which methodological factors significantly influence the value of utility for lung cancer
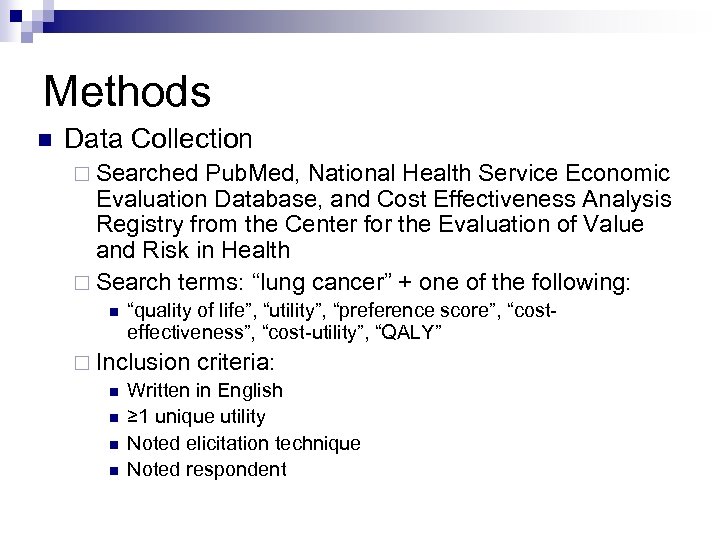 Methods n Data Collection ¨ Searched Pub. Med, National Health Service Economic Evaluation Database, and Cost Effectiveness Analysis Registry from the Center for the Evaluation of Value and Risk in Health ¨ Search terms: “lung cancer” + one of the following: n “quality of life”, “utility”, “preference score”, “costeffectiveness”, “cost-utility”, “QALY” ¨ Inclusion criteria: n Written in English n ≥ 1 unique utility n Noted elicitation technique n Noted respondent
Methods n Data Collection ¨ Searched Pub. Med, National Health Service Economic Evaluation Database, and Cost Effectiveness Analysis Registry from the Center for the Evaluation of Value and Risk in Health ¨ Search terms: “lung cancer” + one of the following: n “quality of life”, “utility”, “preference score”, “costeffectiveness”, “cost-utility”, “QALY” ¨ Inclusion criteria: n Written in English n ≥ 1 unique utility n Noted elicitation technique n Noted respondent
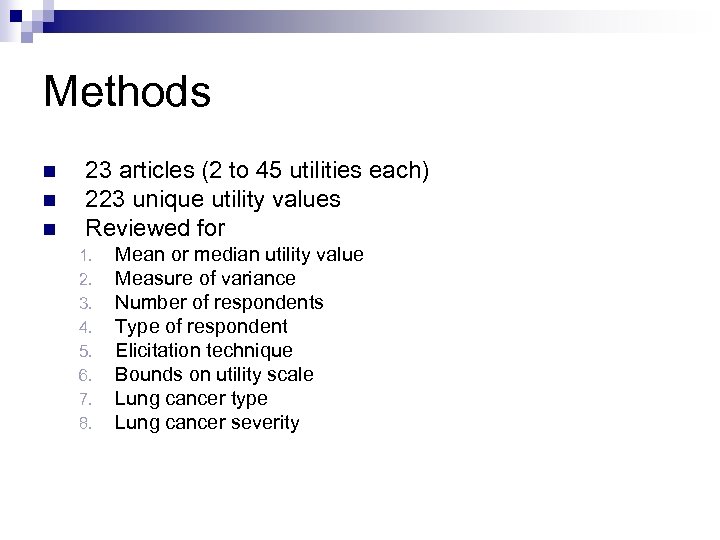 Methods n n n 23 articles (2 to 45 utilities each) 223 unique utility values Reviewed for 1. 2. 3. 4. 5. 6. 7. 8. Mean or median utility value Measure of variance Number of respondents Type of respondent Elicitation technique Bounds on utility scale Lung cancer type Lung cancer severity
Methods n n n 23 articles (2 to 45 utilities each) 223 unique utility values Reviewed for 1. 2. 3. 4. 5. 6. 7. 8. Mean or median utility value Measure of variance Number of respondents Type of respondent Elicitation technique Bounds on utility scale Lung cancer type Lung cancer severity
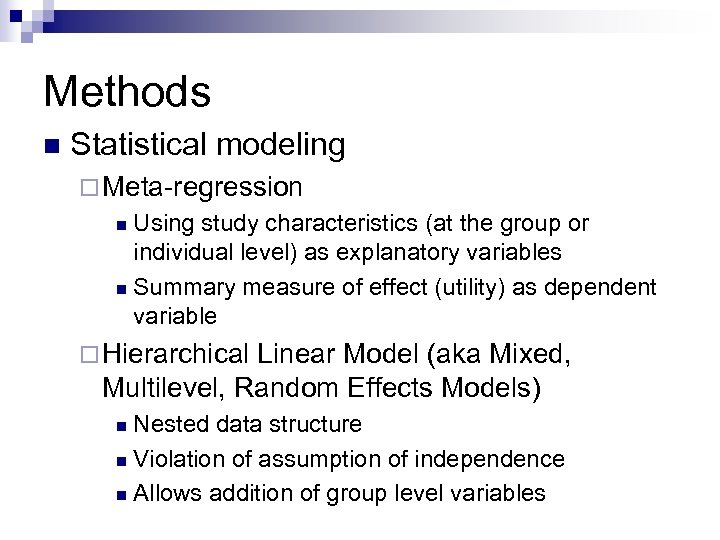 Methods n Statistical modeling ¨ Meta-regression Using study characteristics (at the group or individual level) as explanatory variables n Summary measure of effect (utility) as dependent variable n ¨ Hierarchical Linear Model (aka Mixed, Multilevel, Random Effects Models) Nested data structure n Violation of assumption of independence n Allows addition of group level variables n
Methods n Statistical modeling ¨ Meta-regression Using study characteristics (at the group or individual level) as explanatory variables n Summary measure of effect (utility) as dependent variable n ¨ Hierarchical Linear Model (aka Mixed, Multilevel, Random Effects Models) Nested data structure n Violation of assumption of independence n Allows addition of group level variables n
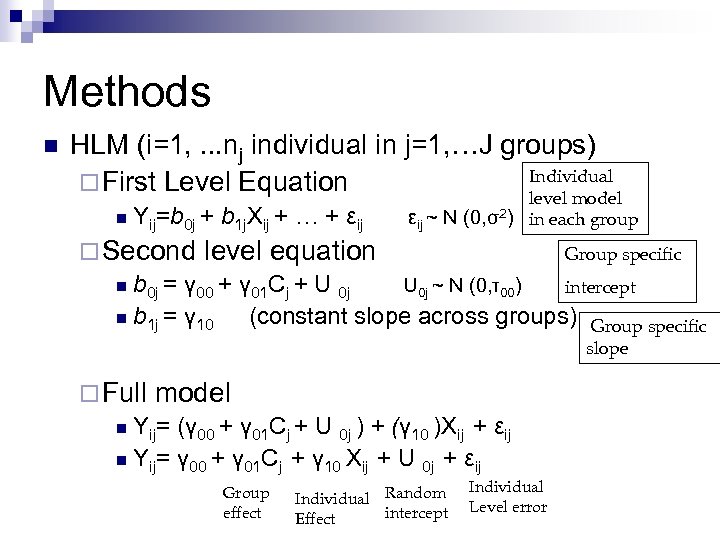 Methods n HLM (i=1, . . . nj individual in j=1, …J groups) Individual ¨ First Level Equation level model n Yij=b 0 j + b 1 j. Xij + … + εij ~ N (0, σ2) in each group ¨ Second level equation Group specific n b 0 j = γ 00 + γ 01 Cj + U 0 j ~ N (0, τ00) intercept n b 1 j = γ 10 (constant slope across groups) Group specific slope ¨ Full model n Yij= (γ 00 + γ 01 Cj + U 0 j ) + (γ 10 )Xij + εij n Yij= γ 00 + γ 01 Cj + γ 10 Xij + U 0 j + εij Group effect Individual Random intercept Effect Individual Level error
Methods n HLM (i=1, . . . nj individual in j=1, …J groups) Individual ¨ First Level Equation level model n Yij=b 0 j + b 1 j. Xij + … + εij ~ N (0, σ2) in each group ¨ Second level equation Group specific n b 0 j = γ 00 + γ 01 Cj + U 0 j ~ N (0, τ00) intercept n b 1 j = γ 10 (constant slope across groups) Group specific slope ¨ Full model n Yij= (γ 00 + γ 01 Cj + U 0 j ) + (γ 10 )Xij + εij n Yij= γ 00 + γ 01 Cj + γ 10 Xij + U 0 j + εij Group effect Individual Random intercept Effect Individual Level error
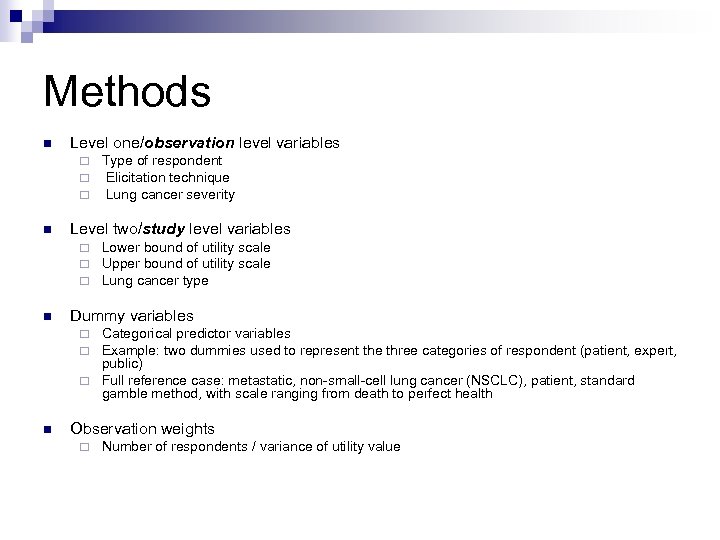 Methods n Level one/observation level variables ¨ ¨ ¨ n Level two/study level variables ¨ ¨ ¨ n Type of respondent Elicitation technique Lung cancer severity Lower bound of utility scale Upper bound of utility scale Lung cancer type Dummy variables Categorical predictor variables Example: two dummies used to represent the three categories of respondent (patient, expert, public) ¨ Full reference case: metastatic, non-small-cell lung cancer (NSCLC), patient, standard gamble method, with scale ranging from death to perfect health ¨ ¨ n Observation weights ¨ Number of respondents / variance of utility value
Methods n Level one/observation level variables ¨ ¨ ¨ n Level two/study level variables ¨ ¨ ¨ n Type of respondent Elicitation technique Lung cancer severity Lower bound of utility scale Upper bound of utility scale Lung cancer type Dummy variables Categorical predictor variables Example: two dummies used to represent the three categories of respondent (patient, expert, public) ¨ Full reference case: metastatic, non-small-cell lung cancer (NSCLC), patient, standard gamble method, with scale ranging from death to perfect health ¨ ¨ n Observation weights ¨ Number of respondents / variance of utility value
 Results. Study Characteristics Variable Number of utilities (n=223) Percentage of utilities Upper bound Perfect health 125 55. 6 Nonmetastatic 41 17. 9 59 26. 5 Lung cancer type 26. 5 Well / Full health 65 29. 1 Normal health 47 21. 1 52 23. 3 Patient Metastatic 61 Not stated Cancer stage Mixed/Not specified Number of utilities (n=223) 164 73. 6 Respondent NSCLC 147 65. 0 Expert 51 22. 9 SCLC 11 4. 9 Public 10 3. 6 Mixed/Not specified 67 30. 1 Standard Gamble 56 24. 2 Judgment 35 15. 7 Direct rating 54 24. 2 HALex 6 2. 7 AQOL 37 16. 6 EQ-5 D 25 11. 2 Time trade-off 12 5. 4 Lower bound Death 175 77. 6 Worst imaginable 2 0. 9 Not stated 48 21. 5 Elicitation technique
Results. Study Characteristics Variable Number of utilities (n=223) Percentage of utilities Upper bound Perfect health 125 55. 6 Nonmetastatic 41 17. 9 59 26. 5 Lung cancer type 26. 5 Well / Full health 65 29. 1 Normal health 47 21. 1 52 23. 3 Patient Metastatic 61 Not stated Cancer stage Mixed/Not specified Number of utilities (n=223) 164 73. 6 Respondent NSCLC 147 65. 0 Expert 51 22. 9 SCLC 11 4. 9 Public 10 3. 6 Mixed/Not specified 67 30. 1 Standard Gamble 56 24. 2 Judgment 35 15. 7 Direct rating 54 24. 2 HALex 6 2. 7 AQOL 37 16. 6 EQ-5 D 25 11. 2 Time trade-off 12 5. 4 Lower bound Death 175 77. 6 Worst imaginable 2 0. 9 Not stated 48 21. 5 Elicitation technique
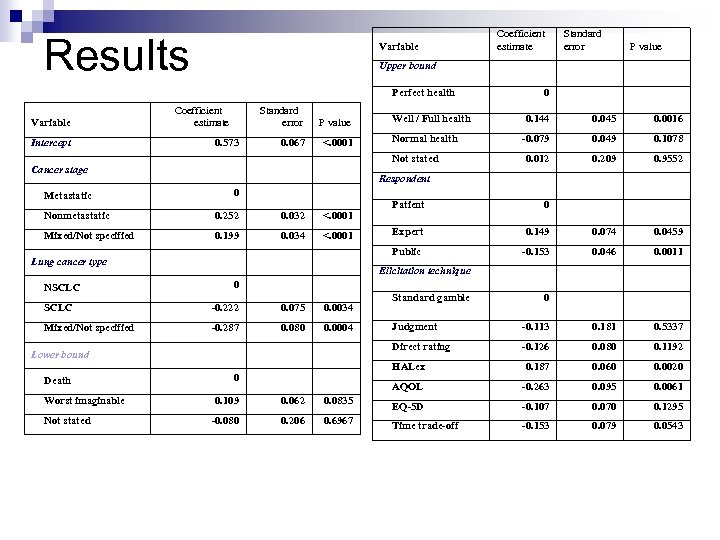 Results Variable Intercept Coefficient estimate Standard error 0. 573 P value 0. 067 <. 0001 Mixed/Not specified 0. 199 0. 034 <. 0001 Lung cancer type 0. 045 0. 0016 -0. 079 0. 049 0. 1078 0. 012 0. 209 0. 9552 Patient 0 Expert 0. 149 0. 074 0. 0459 -0. 153 0. 046 0. 0011 Elicitation technique 0 SCLC -0. 222 0. 075 0. 0034 Mixed/Not specified -0. 287 0. 080 0. 0004 Standard gamble 0 0. 062 0. 0835 -0. 080 0. 206 0. 6967 0. 181 0. 5337 -0. 126 0. 080 0. 1192 0. 187 0. 060 0. 0020 AQOL 0. 109 -0. 113 HALex 0 Judgment Direct rating Lower bound Not stated 0. 144 Public 0. 032 Worst imaginable Normal health 0 Respondent 0. 252 Death P value 0 Nonmetastatic NSCLC Well / Full health Not stated Cancer stage Metastatic Standard error Upper bound Perfect health Variable Coefficient estimate -0. 263 0. 095 0. 0061 EQ-5 D -0. 107 0. 070 0. 1295 Time trade-off -0. 153 0. 079 0. 0543
Results Variable Intercept Coefficient estimate Standard error 0. 573 P value 0. 067 <. 0001 Mixed/Not specified 0. 199 0. 034 <. 0001 Lung cancer type 0. 045 0. 0016 -0. 079 0. 049 0. 1078 0. 012 0. 209 0. 9552 Patient 0 Expert 0. 149 0. 074 0. 0459 -0. 153 0. 046 0. 0011 Elicitation technique 0 SCLC -0. 222 0. 075 0. 0034 Mixed/Not specified -0. 287 0. 080 0. 0004 Standard gamble 0 0. 062 0. 0835 -0. 080 0. 206 0. 6967 0. 181 0. 5337 -0. 126 0. 080 0. 1192 0. 187 0. 060 0. 0020 AQOL 0. 109 -0. 113 HALex 0 Judgment Direct rating Lower bound Not stated 0. 144 Public 0. 032 Worst imaginable Normal health 0 Respondent 0. 252 Death P value 0 Nonmetastatic NSCLC Well / Full health Not stated Cancer stage Metastatic Standard error Upper bound Perfect health Variable Coefficient estimate -0. 263 0. 095 0. 0061 EQ-5 D -0. 107 0. 070 0. 1295 Time trade-off -0. 153 0. 079 0. 0543
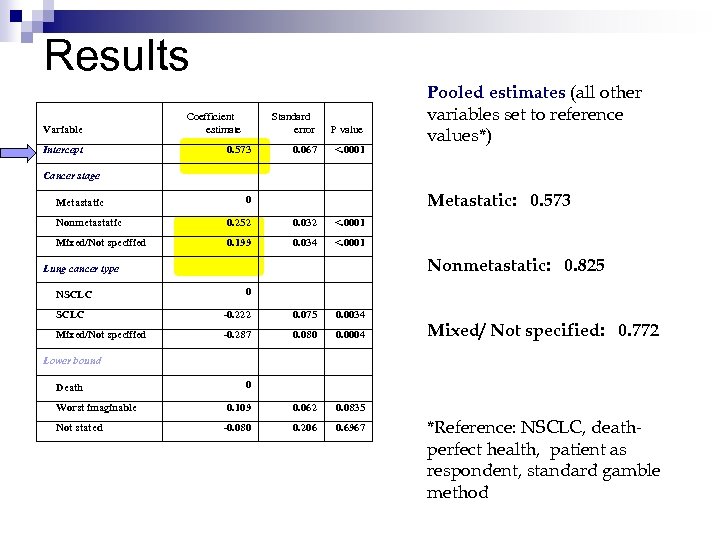 Results Variable Intercept Coefficient estimate Standard error 0. 573 P value 0. 067 <. 0001 Pooled estimates (all other variables set to reference values*) Cancer stage Metastatic: 0. 573 0 Nonmetastatic 0. 252 0. 032 <. 0001 Mixed/Not specified 0. 199 0. 034 <. 0001 Nonmetastatic: 0. 825 Lung cancer type NSCLC 0 SCLC -0. 222 0. 075 0. 0034 Mixed/Not specified -0. 287 0. 080 0. 0004 0. 109 0. 062 0. 0835 -0. 080 0. 206 0. 6967 Mixed/ Not specified: 0. 772 Lower bound Death Worst imaginable Not stated 0 *Reference: NSCLC, deathperfect health, patient as respondent, standard gamble method
Results Variable Intercept Coefficient estimate Standard error 0. 573 P value 0. 067 <. 0001 Pooled estimates (all other variables set to reference values*) Cancer stage Metastatic: 0. 573 0 Nonmetastatic 0. 252 0. 032 <. 0001 Mixed/Not specified 0. 199 0. 034 <. 0001 Nonmetastatic: 0. 825 Lung cancer type NSCLC 0 SCLC -0. 222 0. 075 0. 0034 Mixed/Not specified -0. 287 0. 080 0. 0004 0. 109 0. 062 0. 0835 -0. 080 0. 206 0. 6967 Mixed/ Not specified: 0. 772 Lower bound Death Worst imaginable Not stated 0 *Reference: NSCLC, deathperfect health, patient as respondent, standard gamble method
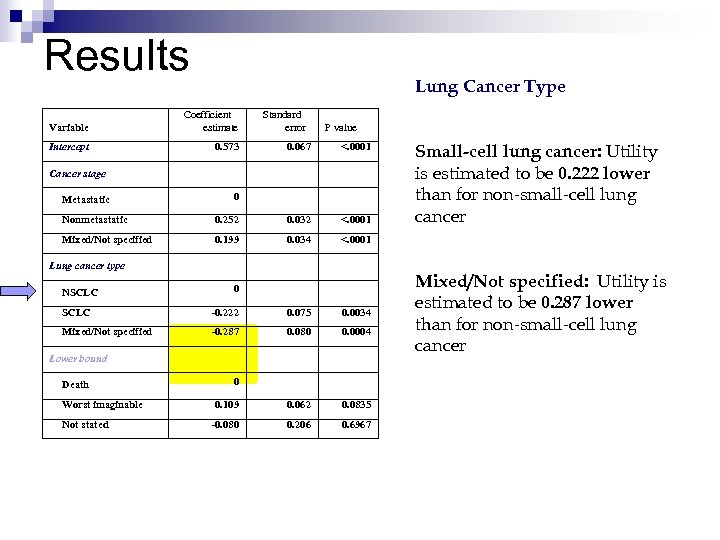 Results Lung Cancer Type Variable Coefficient estimate Intercept 0. 573 Standard error P value 0. 067 <. 0001 Cancer stage Metastatic 0 Nonmetastatic 0. 252 0. 032 <. 0001 Mixed/Not specified 0. 199 0. 034 Small-cell lung cancer: Utility is estimated to be 0. 222 lower than for non-small-cell lung cancer <. 0001 Lung cancer type NSCLC 0 SCLC -0. 222 0. 075 0. 0034 Mixed/Not specified -0. 287 0. 080 0. 0004 0. 109 0. 062 0. 0835 -0. 080 0. 206 0. 6967 Lower bound Death Worst imaginable Not stated 0 Mixed/Not specified: Utility is estimated to be 0. 287 lower than for non-small-cell lung cancer
Results Lung Cancer Type Variable Coefficient estimate Intercept 0. 573 Standard error P value 0. 067 <. 0001 Cancer stage Metastatic 0 Nonmetastatic 0. 252 0. 032 <. 0001 Mixed/Not specified 0. 199 0. 034 Small-cell lung cancer: Utility is estimated to be 0. 222 lower than for non-small-cell lung cancer <. 0001 Lung cancer type NSCLC 0 SCLC -0. 222 0. 075 0. 0034 Mixed/Not specified -0. 287 0. 080 0. 0004 0. 109 0. 062 0. 0835 -0. 080 0. 206 0. 6967 Lower bound Death Worst imaginable Not stated 0 Mixed/Not specified: Utility is estimated to be 0. 287 lower than for non-small-cell lung cancer
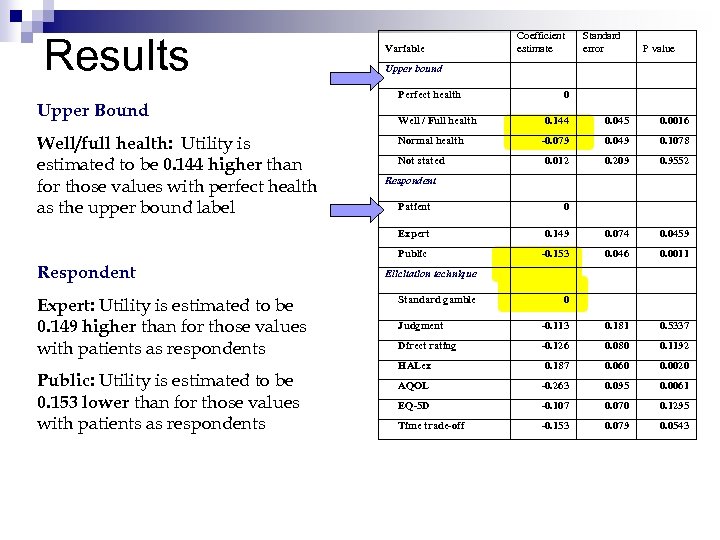 Results Upper Bound Well/full health: Utility is estimated to be 0. 144 higher than for those values with perfect health as the upper bound label Variable Coefficient estimate Standard error P value Upper bound Perfect health Well / Full health Normal health Not stated 0 0. 144 0. 045 0. 0016 -0. 079 0. 049 0. 1078 0. 012 0. 209 0. 9552 Respondent Public: Utility is estimated to be 0. 153 lower than for those values with patients as respondents 0. 149 0. 074 0. 0459 Public Expert: Utility is estimated to be 0. 149 higher than for those values with patients as respondents 0 Expert Respondent Patient -0. 153 0. 046 0. 0011 Elicitation technique Standard gamble 0 Judgment -0. 113 0. 181 0. 5337 Direct rating -0. 126 0. 080 0. 1192 HALex 0. 187 0. 060 0. 0020 AQOL -0. 263 0. 095 0. 0061 EQ-5 D -0. 107 0. 070 0. 1295 Time trade-off -0. 153 0. 079 0. 0543
Results Upper Bound Well/full health: Utility is estimated to be 0. 144 higher than for those values with perfect health as the upper bound label Variable Coefficient estimate Standard error P value Upper bound Perfect health Well / Full health Normal health Not stated 0 0. 144 0. 045 0. 0016 -0. 079 0. 049 0. 1078 0. 012 0. 209 0. 9552 Respondent Public: Utility is estimated to be 0. 153 lower than for those values with patients as respondents 0. 149 0. 074 0. 0459 Public Expert: Utility is estimated to be 0. 149 higher than for those values with patients as respondents 0 Expert Respondent Patient -0. 153 0. 046 0. 0011 Elicitation technique Standard gamble 0 Judgment -0. 113 0. 181 0. 5337 Direct rating -0. 126 0. 080 0. 1192 HALex 0. 187 0. 060 0. 0020 AQOL -0. 263 0. 095 0. 0061 EQ-5 D -0. 107 0. 070 0. 1295 Time trade-off -0. 153 0. 079 0. 0543
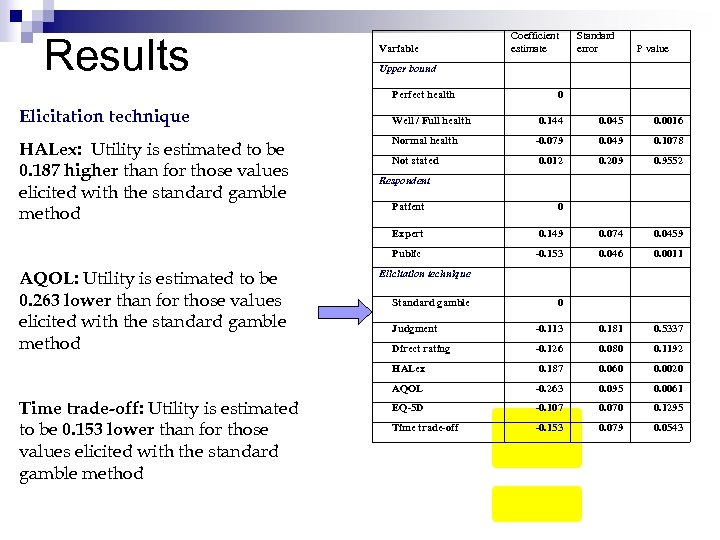 Results Variable HALex: Utility is estimated to be 0. 187 higher than for those values elicited with the standard gamble method Standard error P value Upper bound Perfect health Elicitation technique Coefficient estimate Well / Full health Normal health Not stated 0 0. 144 0. 045 0. 0016 -0. 079 0. 049 0. 1078 0. 012 0. 209 0. 9552 Respondent 0 Expert 0. 149 0. 074 0. 0459 Public AQOL: Utility is estimated to be 0. 263 lower than for those values elicited with the standard gamble method Patient -0. 153 0. 046 0. 0011 Elicitation technique Standard gamble 0 -0. 113 0. 181 0. 5337 Direct rating -0. 126 0. 080 0. 1192 HALex 0. 187 0. 060 0. 0020 AQOL Time trade-off: Utility is estimated to be 0. 153 lower than for those values elicited with the standard gamble method Judgment -0. 263 0. 095 0. 0061 EQ-5 D -0. 107 0. 070 0. 1295 Time trade-off -0. 153 0. 079 0. 0543
Results Variable HALex: Utility is estimated to be 0. 187 higher than for those values elicited with the standard gamble method Standard error P value Upper bound Perfect health Elicitation technique Coefficient estimate Well / Full health Normal health Not stated 0 0. 144 0. 045 0. 0016 -0. 079 0. 049 0. 1078 0. 012 0. 209 0. 9552 Respondent 0 Expert 0. 149 0. 074 0. 0459 Public AQOL: Utility is estimated to be 0. 263 lower than for those values elicited with the standard gamble method Patient -0. 153 0. 046 0. 0011 Elicitation technique Standard gamble 0 -0. 113 0. 181 0. 5337 Direct rating -0. 126 0. 080 0. 1192 HALex 0. 187 0. 060 0. 0020 AQOL Time trade-off: Utility is estimated to be 0. 153 lower than for those values elicited with the standard gamble method Judgment -0. 263 0. 095 0. 0061 EQ-5 D -0. 107 0. 070 0. 1295 Time trade-off -0. 153 0. 079 0. 0543
 Results
Results
 Limitations ¨ Lack of gray literature ¨ Model predicts values outside standard range of 0 -1 ¨ No demographic information included ¨ Using weights
Limitations ¨ Lack of gray literature ¨ Model predicts values outside standard range of 0 -1 ¨ No demographic information included ¨ Using weights
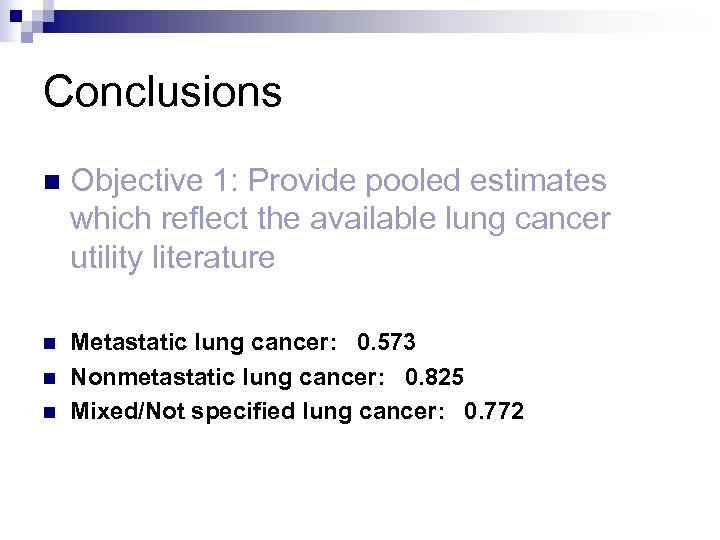 Conclusions n Objective 1: Provide pooled estimates which reflect the available lung cancer utility literature n Metastatic lung cancer: 0. 573 Nonmetastatic lung cancer: 0. 825 Mixed/Not specified lung cancer: 0. 772 n n
Conclusions n Objective 1: Provide pooled estimates which reflect the available lung cancer utility literature n Metastatic lung cancer: 0. 573 Nonmetastatic lung cancer: 0. 825 Mixed/Not specified lung cancer: 0. 772 n n
 Conclusions n Objective 2: Determine which methodological factors significantly influence the value of utility for lung cancer n Significant predictors: Lung cancer stage, lung cancer subtype, respondent Near significant: Elicitation method Not significant: Upper and lower bound labels n n
Conclusions n Objective 2: Determine which methodological factors significantly influence the value of utility for lung cancer n Significant predictors: Lung cancer stage, lung cancer subtype, respondent Near significant: Elicitation method Not significant: Upper and lower bound labels n n
 Next steps… n Larger meta-analysis looking at 12 common cancers n Do different kinds of cancers impact quality of life more of less severely? With a larger sample, which methodological factors significantly impact the value of utility? Which demographic factors significantly impact the value of utility? n n
Next steps… n Larger meta-analysis looking at 12 common cancers n Do different kinds of cancers impact quality of life more of less severely? With a larger sample, which methodological factors significantly impact the value of utility? Which demographic factors significantly impact the value of utility? n n
 Thank you!!! Chris Dockins n Will Wheeler n Colleen Reid n
Thank you!!! Chris Dockins n Will Wheeler n Colleen Reid n
 References n n n Fryback, D. G. and W. F. Lawrence, Jr. , Dollars may not buy as many QALYs as we think: a problem with defining quality-of-life adjustments. Medical Decision Making, 1997. 17(3): p. 276284. King, J. T. , et al. , "Perfect health" versus "disease free": the impact of anchor point choice on the measurement of preferences and the calculation of disease-specific disutilities. Medical Decision Making, 2003. 23(3): p. 212 -225. Tengs, T. O. and T. H. Lin, A meta-analysis of quality-of-life estimates for stroke. Pharmacoeconomics, 2003. 21(3): p. 191 -200. Read, J. L. , et al. , Preferences for health outcomes. Comparison of assessment methods. Medical Decision Making, 1984. 4(3): p. 315 -329. Stiggelbout, A. M. , et al. , The 'utility' of the visual analog scale in medical decision making and technology assessment. Is it an alternative to the time trade-off? International Journal of Technology Assessment in Health Care, 1996. 12(2): p. 291 -298. Stiggelbout, A. M. , et al. , Utility assessment in cancer patients: adjustment of time tradeoff scores for the utility of life years and comparison with standard gamble scores. Medical Decision Making, 1994. 14(1): p. 82 -90. Hornberger, J. C. , D. A. Redelmeier, and J. Petersen, Variability among methods to assess patients' well-being and consequent effect on a cost-effectiveness analysis. Journal of Clinical Epidemiology, 1992. 45(5): p. 505 -512. Gabriel, S. E. , T. S. Kneeland, and L. J. Melton, Health-related quality of life in economic evaluations for osteoporosis: whose values should we use? Medical Decision Making, 1999. 19: p. 141 -8. Boyd, N. F. , et al. , Whose utilities for decision analysis? Medical Decision Making, 1990. 10(1): p. 58 -67. Polsky, D. , et al. , A comparison of scoring weights for the Euro. Qol derived from patients and the general public. Health Economics, 2001. 10(1): p. 27 -37. Sackett, D. L. and G. W. Torrance, The utility of different health states as perceived by the general public. Journal of Chronic Disease, 1978. 31: p. 697 -704. Tengs, T. O. and T. H. Lin, A meta-analysis of utility estimates for HIV/AIDS. Medical Decision Making, 2002. 22: p. 475 -481.
References n n n Fryback, D. G. and W. F. Lawrence, Jr. , Dollars may not buy as many QALYs as we think: a problem with defining quality-of-life adjustments. Medical Decision Making, 1997. 17(3): p. 276284. King, J. T. , et al. , "Perfect health" versus "disease free": the impact of anchor point choice on the measurement of preferences and the calculation of disease-specific disutilities. Medical Decision Making, 2003. 23(3): p. 212 -225. Tengs, T. O. and T. H. Lin, A meta-analysis of quality-of-life estimates for stroke. Pharmacoeconomics, 2003. 21(3): p. 191 -200. Read, J. L. , et al. , Preferences for health outcomes. Comparison of assessment methods. Medical Decision Making, 1984. 4(3): p. 315 -329. Stiggelbout, A. M. , et al. , The 'utility' of the visual analog scale in medical decision making and technology assessment. Is it an alternative to the time trade-off? International Journal of Technology Assessment in Health Care, 1996. 12(2): p. 291 -298. Stiggelbout, A. M. , et al. , Utility assessment in cancer patients: adjustment of time tradeoff scores for the utility of life years and comparison with standard gamble scores. Medical Decision Making, 1994. 14(1): p. 82 -90. Hornberger, J. C. , D. A. Redelmeier, and J. Petersen, Variability among methods to assess patients' well-being and consequent effect on a cost-effectiveness analysis. Journal of Clinical Epidemiology, 1992. 45(5): p. 505 -512. Gabriel, S. E. , T. S. Kneeland, and L. J. Melton, Health-related quality of life in economic evaluations for osteoporosis: whose values should we use? Medical Decision Making, 1999. 19: p. 141 -8. Boyd, N. F. , et al. , Whose utilities for decision analysis? Medical Decision Making, 1990. 10(1): p. 58 -67. Polsky, D. , et al. , A comparison of scoring weights for the Euro. Qol derived from patients and the general public. Health Economics, 2001. 10(1): p. 27 -37. Sackett, D. L. and G. W. Torrance, The utility of different health states as perceived by the general public. Journal of Chronic Disease, 1978. 31: p. 697 -704. Tengs, T. O. and T. H. Lin, A meta-analysis of utility estimates for HIV/AIDS. Medical Decision Making, 2002. 22: p. 475 -481.


