10a697d4adfe212fda2adeab81fdad6d.ppt
- Количество слайдов: 56
 A Practical Approach to Cancer Pain Management
A Practical Approach to Cancer Pain Management
 The Problem: • One out of three people in the U. S. will develop cancer • One out to two people who develop cancer, will die of their disease • Three out of four patients who die of cancer, will have significant pain during their illness
The Problem: • One out of three people in the U. S. will develop cancer • One out to two people who develop cancer, will die of their disease • Three out of four patients who die of cancer, will have significant pain during their illness
 Impact of Uncontrolled Pain: • Physical: – symptom complex (fatigue, depression, NC) – decreased function (work, AIDLs, ADLs) • Emotional – total mood disorder – spiritual distress • Social – family interactions – alters support structures
Impact of Uncontrolled Pain: • Physical: – symptom complex (fatigue, depression, NC) – decreased function (work, AIDLs, ADLs) • Emotional – total mood disorder – spiritual distress • Social – family interactions – alters support structures
 Pain Assessment: • Intensity • Etiology • Type
Pain Assessment: • Intensity • Etiology • Type
 Measurement: • Scales: – Numeric rating scales – Visual analogue – Descriptive • Outcome Measure: – – – Pain intensity Distress Relief Interference Breakthrough dosing • Tools: – Brief Pain Index – Memorial Pain Assessment Card
Measurement: • Scales: – Numeric rating scales – Visual analogue – Descriptive • Outcome Measure: – – – Pain intensity Distress Relief Interference Breakthrough dosing • Tools: – Brief Pain Index – Memorial Pain Assessment Card
 Clinically Important Questions: • • Current pain level Average pain level Worst pain level Pain relief with medications
Clinically Important Questions: • • Current pain level Average pain level Worst pain level Pain relief with medications
 Etiology: • Treatable Causes: – pathologic fracture – bone met – chest wall recurrence • Emergent: – cord compression – brain met
Etiology: • Treatable Causes: – pathologic fracture – bone met – chest wall recurrence • Emergent: – cord compression – brain met
 Nociceptive Pain • Mechanism: Pain receptor activation • Subtypes: – Somatic • most common type in cancer patients • bone mets most common cause • characterized by aching, throbbing, gnawing – Visceral • deep, squeezing, crampy
Nociceptive Pain • Mechanism: Pain receptor activation • Subtypes: – Somatic • most common type in cancer patients • bone mets most common cause • characterized by aching, throbbing, gnawing – Visceral • deep, squeezing, crampy
 Neuropathic Pain: • Mechanism: Damage to receptor or nerve • Frequently unrecognized • Types of Syndromes: – Peripheral • Drug induced (Cisplatin, Taxol) – Central • Cord compression
Neuropathic Pain: • Mechanism: Damage to receptor or nerve • Frequently unrecognized • Types of Syndromes: – Peripheral • Drug induced (Cisplatin, Taxol) – Central • Cord compression
 Neuropathic Pain Syndromes: • • • Post-amputation Limb Pain Post-thoracotomy Pain Post-mastectomy Pain Brachial Plexopathy LS Plexopathy Celiac Infiltration
Neuropathic Pain Syndromes: • • • Post-amputation Limb Pain Post-thoracotomy Pain Post-mastectomy Pain Brachial Plexopathy LS Plexopathy Celiac Infiltration
 Assessment of the Patient: • • Medical Problems Psychological Function Physical Function Cognitive Function Support Services Financial Services Educational Status
Assessment of the Patient: • • Medical Problems Psychological Function Physical Function Cognitive Function Support Services Financial Services Educational Status
 Ready to Prescribe: Rx
Ready to Prescribe: Rx
 Skill Sets Required for Adequate Pain Control: • Develop a framework for writing prescriptions • Write a fixed dose regimen • Calculate an appropriate breakthrough dose • Convert from one opioid to another • Dose titrate • Understand the issues of substance abuse
Skill Sets Required for Adequate Pain Control: • Develop a framework for writing prescriptions • Write a fixed dose regimen • Calculate an appropriate breakthrough dose • Convert from one opioid to another • Dose titrate • Understand the issues of substance abuse
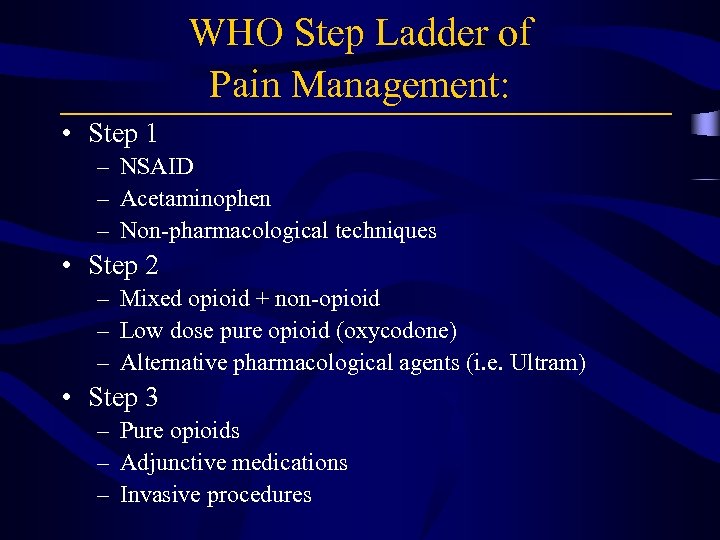 WHO Step Ladder of Pain Management: • Step 1 – NSAID – Acetaminophen – Non-pharmacological techniques • Step 2 – Mixed opioid + non-opioid – Low dose pure opioid (oxycodone) – Alternative pharmacological agents (i. e. Ultram) • Step 3 – Pure opioids – Adjunctive medications – Invasive procedures
WHO Step Ladder of Pain Management: • Step 1 – NSAID – Acetaminophen – Non-pharmacological techniques • Step 2 – Mixed opioid + non-opioid – Low dose pure opioid (oxycodone) – Alternative pharmacological agents (i. e. Ultram) • Step 3 – Pure opioids – Adjunctive medications – Invasive procedures
 Step 3: Basic Rules for Opioid Administration • Goal: Controlled Pain (4 or fewer rescues) • Dose Escalation: Quickly until controlled pain • Maximum Dose: Does not exist • Side Effects: – Accommodation in 7 -10 days – Treat aggressively – Bowel Regimen
Step 3: Basic Rules for Opioid Administration • Goal: Controlled Pain (4 or fewer rescues) • Dose Escalation: Quickly until controlled pain • Maximum Dose: Does not exist • Side Effects: – Accommodation in 7 -10 days – Treat aggressively – Bowel Regimen
 Basic Rules for Opioid Administration: • Use oral or transdermal formulations if possible • Start with immediate release formulations in patients with significant pain • Use medications around-the-clock for constant pain (fixed dosing) • Fixed dose interval should be based on T 1/2 of the agent • Rescue dose interval should be based on time to peak effect
Basic Rules for Opioid Administration: • Use oral or transdermal formulations if possible • Start with immediate release formulations in patients with significant pain • Use medications around-the-clock for constant pain (fixed dosing) • Fixed dose interval should be based on T 1/2 of the agent • Rescue dose interval should be based on time to peak effect
 Meperidine: • By product - normeperidine • T 1/2 of normeperidine is longer than meperidine • Normeperidine has a neuroexcitatory effect • Toxicity is seen when administered over a prolonged period or in patients with renal insufficiency
Meperidine: • By product - normeperidine • T 1/2 of normeperidine is longer than meperidine • Normeperidine has a neuroexcitatory effect • Toxicity is seen when administered over a prolonged period or in patients with renal insufficiency
 Fixed Dose Administration: • Goal: to maintain opioid levels within therapeutic window • Fixed dosing allows a steady state to be achieved • Once steady state is achieved, dose modifications can be made in a calculated way
Fixed Dose Administration: • Goal: to maintain opioid levels within therapeutic window • Fixed dosing allows a steady state to be achieved • Once steady state is achieved, dose modifications can be made in a calculated way
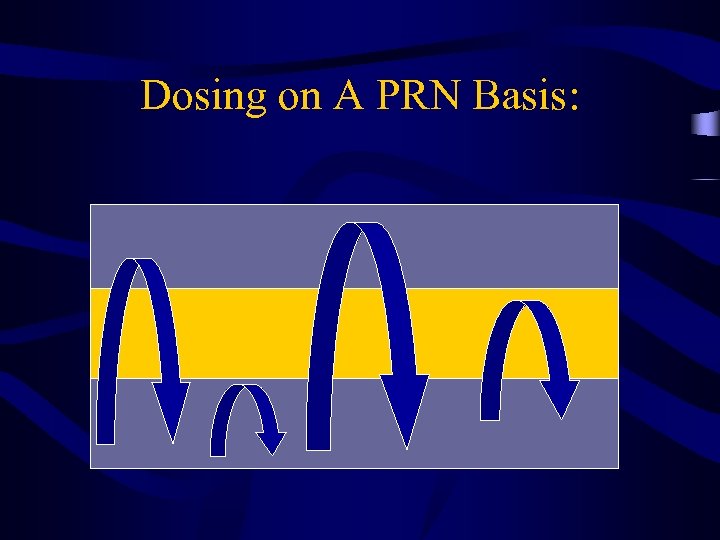
 Dosing on a Fixed Interval:
Dosing on a Fixed Interval:
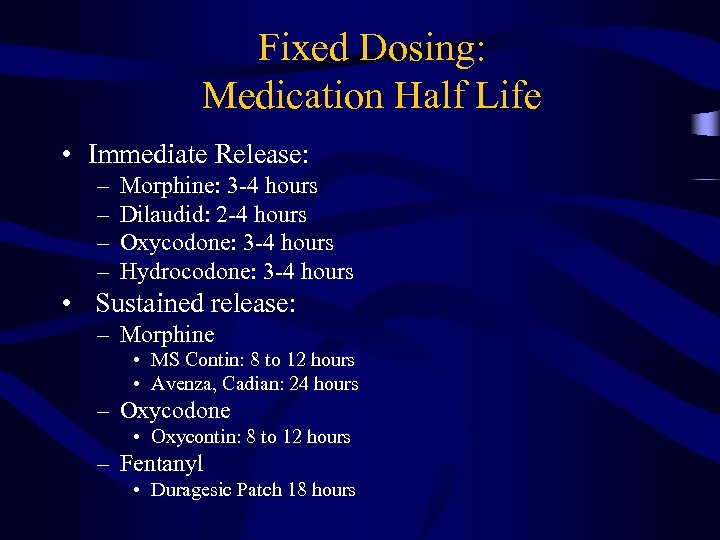
 PRN Dosing: • Patients take pain medication as needed, thus they are in pain when they take a dose. • Patients are in pain more frequently • They are more likely to have side effects
PRN Dosing: • Patients take pain medication as needed, thus they are in pain when they take a dose. • Patients are in pain more frequently • They are more likely to have side effects
 Dosing on A PRN Basis:
Dosing on A PRN Basis:
 Fixed Dosing: Medication Half Life • Immediate Release: – – Morphine: 3 -4 hours Dilaudid: 2 -4 hours Oxycodone: 3 -4 hours Hydrocodone: 3 -4 hours • Sustained release: – Morphine • MS Contin: 8 to 12 hours • Avenza, Cadian: 24 hours – Oxycodone • Oxycontin: 8 to 12 hours – Fentanyl • Duragesic Patch 18 hours
Fixed Dosing: Medication Half Life • Immediate Release: – – Morphine: 3 -4 hours Dilaudid: 2 -4 hours Oxycodone: 3 -4 hours Hydrocodone: 3 -4 hours • Sustained release: – Morphine • MS Contin: 8 to 12 hours • Avenza, Cadian: 24 hours – Oxycodone • Oxycontin: 8 to 12 hours – Fentanyl • Duragesic Patch 18 hours
 Write a Fixed Dose Prescription for the Following: • • • Morphine Sulfate IR 30 mg tabs MS Contin 30 mg tabs Dilaudid 4 mg IR tabs Duragesic 25 ug patch Oxycontin 20 mg tabs
Write a Fixed Dose Prescription for the Following: • • • Morphine Sulfate IR 30 mg tabs MS Contin 30 mg tabs Dilaudid 4 mg IR tabs Duragesic 25 ug patch Oxycontin 20 mg tabs
 Write a Fixed Dose Prescription for the Following: • Morphine Sulfate IR 30 mg po q 4 hours ATC • MS Contin 30 mg po q 12 hours • Dilaudid IR 4 mg po q 3 -4 hours ATC • Duragesic 25 ug patch to skin q 72 hours • Oxycontin 20 mg po q 12 hours
Write a Fixed Dose Prescription for the Following: • Morphine Sulfate IR 30 mg po q 4 hours ATC • MS Contin 30 mg po q 12 hours • Dilaudid IR 4 mg po q 3 -4 hours ATC • Duragesic 25 ug patch to skin q 72 hours • Oxycontin 20 mg po q 12 hours
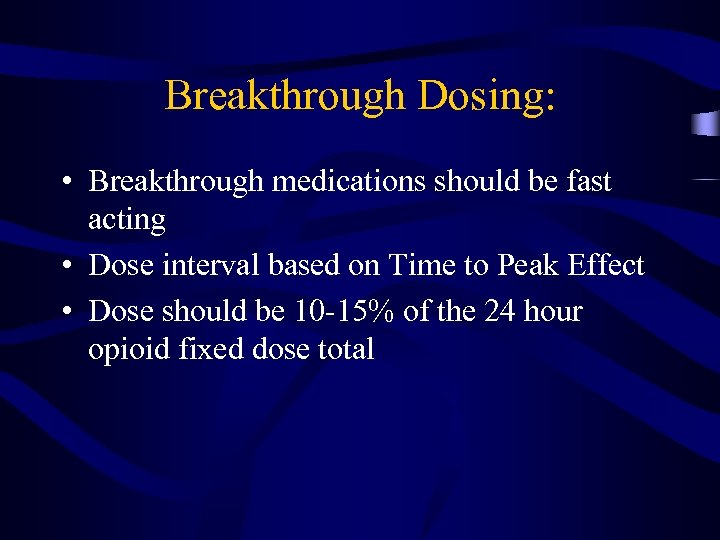 Breakthrough Dosing: • Breakthrough medications should be fast acting • Dose interval based on Time to Peak Effect • Dose should be 10 -15% of the 24 hour opioid fixed dose total
Breakthrough Dosing: • Breakthrough medications should be fast acting • Dose interval based on Time to Peak Effect • Dose should be 10 -15% of the 24 hour opioid fixed dose total
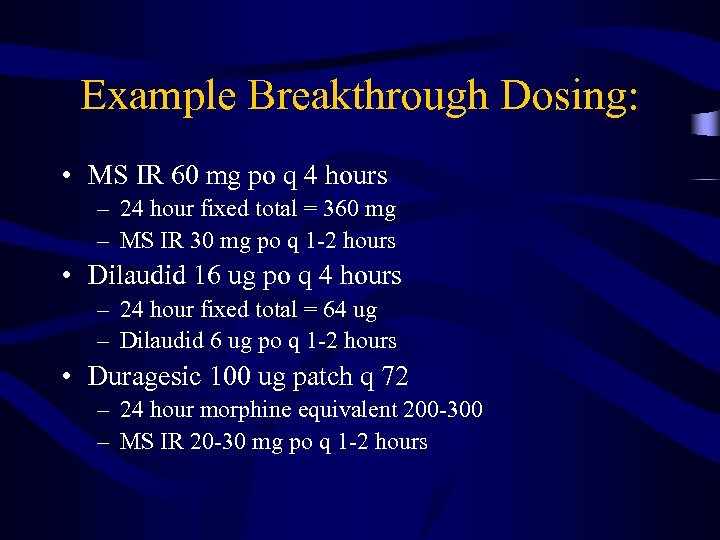 Example Breakthrough Dosing: • MS IR 60 mg po q 4 hours – 24 hour fixed total = 360 mg – MS IR 30 mg po q 1 -2 hours • Dilaudid 16 ug po q 4 hours – 24 hour fixed total = 64 ug – Dilaudid 6 ug po q 1 -2 hours • Duragesic 100 ug patch q 72 – 24 hour morphine equivalent 200 -300 – MS IR 20 -30 mg po q 1 -2 hours
Example Breakthrough Dosing: • MS IR 60 mg po q 4 hours – 24 hour fixed total = 360 mg – MS IR 30 mg po q 1 -2 hours • Dilaudid 16 ug po q 4 hours – 24 hour fixed total = 64 ug – Dilaudid 6 ug po q 1 -2 hours • Duragesic 100 ug patch q 72 – 24 hour morphine equivalent 200 -300 – MS IR 20 -30 mg po q 1 -2 hours
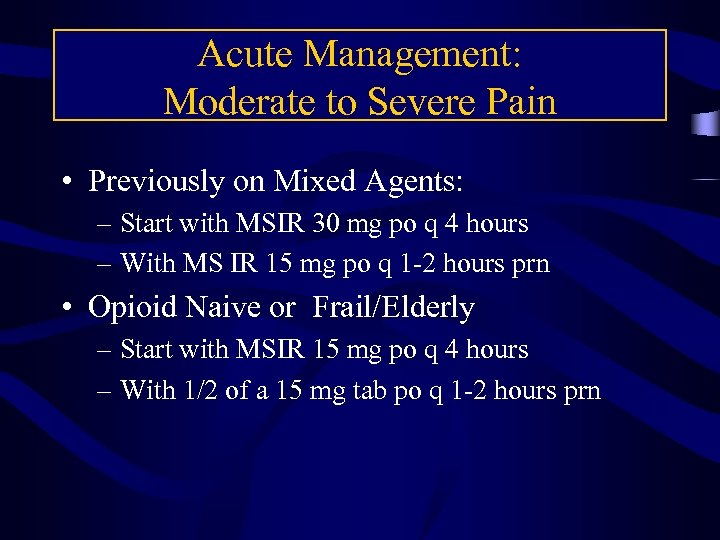 Acute Management: Moderate to Severe Pain • Previously on Mixed Agents: – Start with MSIR 30 mg po q 4 hours – With MS IR 15 mg po q 1 -2 hours prn • Opioid Naive or Frail/Elderly – Start with MSIR 15 mg po q 4 hours – With 1/2 of a 15 mg tab po q 1 -2 hours prn
Acute Management: Moderate to Severe Pain • Previously on Mixed Agents: – Start with MSIR 30 mg po q 4 hours – With MS IR 15 mg po q 1 -2 hours prn • Opioid Naive or Frail/Elderly – Start with MSIR 15 mg po q 4 hours – With 1/2 of a 15 mg tab po q 1 -2 hours prn
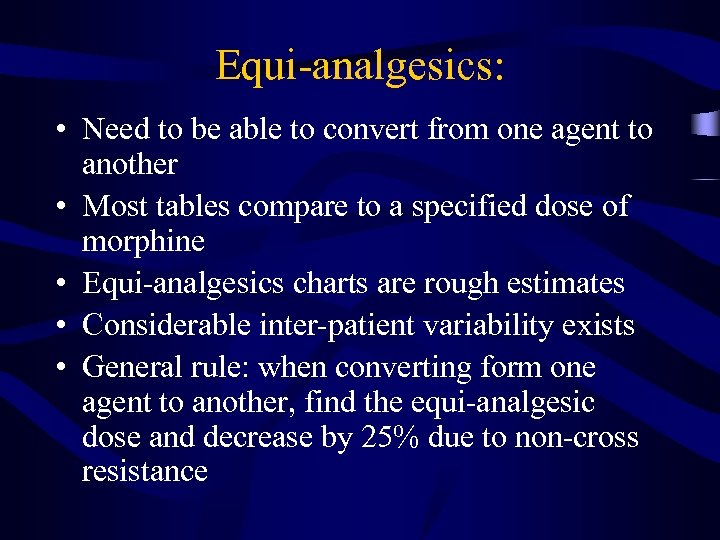 Equi-analgesics: • Need to be able to convert from one agent to another • Most tables compare to a specified dose of morphine • Equi-analgesics charts are rough estimates • Considerable inter-patient variability exists • General rule: when converting form one agent to another, find the equi-analgesic dose and decrease by 25% due to non-cross resistance
Equi-analgesics: • Need to be able to convert from one agent to another • Most tables compare to a specified dose of morphine • Equi-analgesics charts are rough estimates • Considerable inter-patient variability exists • General rule: when converting form one agent to another, find the equi-analgesic dose and decrease by 25% due to non-cross resistance
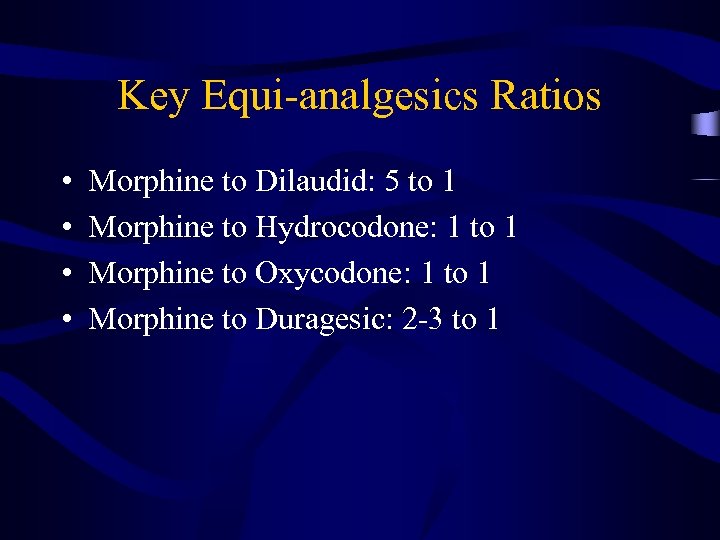 Key Equi-analgesics Ratios • • Morphine to Dilaudid: 5 to 1 Morphine to Hydrocodone: 1 to 1 Morphine to Oxycodone: 1 to 1 Morphine to Duragesic: 2 -3 to 1
Key Equi-analgesics Ratios • • Morphine to Dilaudid: 5 to 1 Morphine to Hydrocodone: 1 to 1 Morphine to Oxycodone: 1 to 1 Morphine to Duragesic: 2 -3 to 1
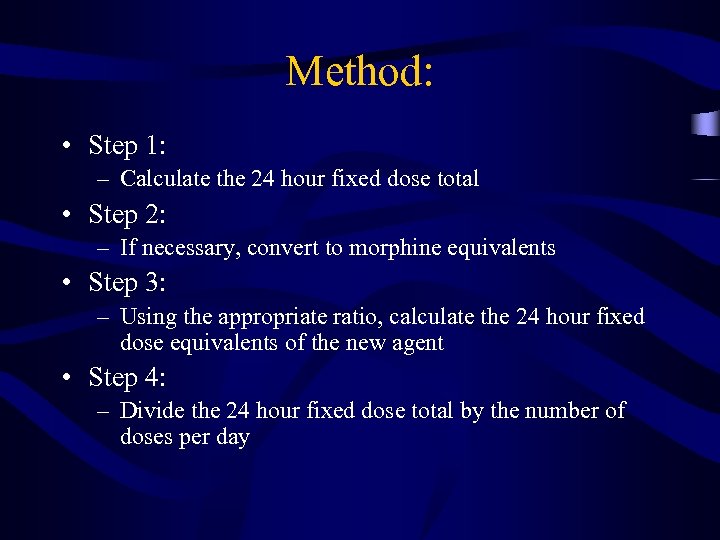 Method: • Step 1: – Calculate the 24 hour fixed dose total • Step 2: – If necessary, convert to morphine equivalents • Step 3: – Using the appropriate ratio, calculate the 24 hour fixed dose equivalents of the new agent • Step 4: – Divide the 24 hour fixed dose total by the number of doses per day
Method: • Step 1: – Calculate the 24 hour fixed dose total • Step 2: – If necessary, convert to morphine equivalents • Step 3: – Using the appropriate ratio, calculate the 24 hour fixed dose equivalents of the new agent • Step 4: – Divide the 24 hour fixed dose total by the number of doses per day
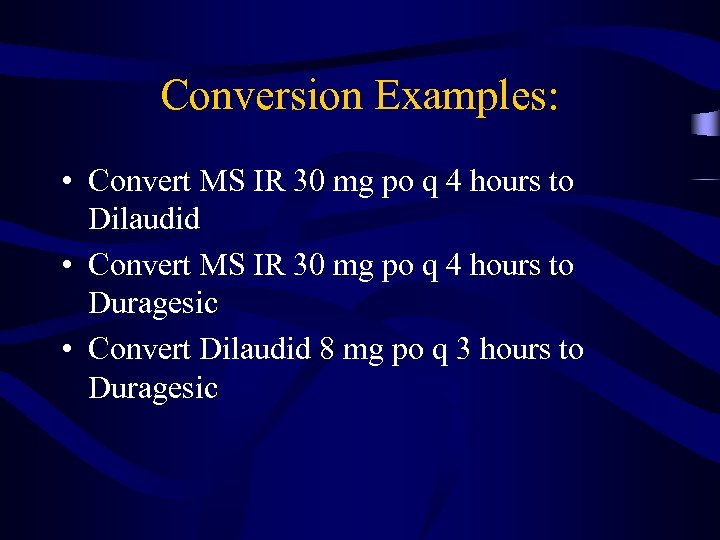 Conversion Examples: • Convert MS IR 30 mg po q 4 hours to Dilaudid • Convert MS IR 30 mg po q 4 hours to Duragesic • Convert Dilaudid 8 mg po q 3 hours to Duragesic
Conversion Examples: • Convert MS IR 30 mg po q 4 hours to Dilaudid • Convert MS IR 30 mg po q 4 hours to Duragesic • Convert Dilaudid 8 mg po q 3 hours to Duragesic
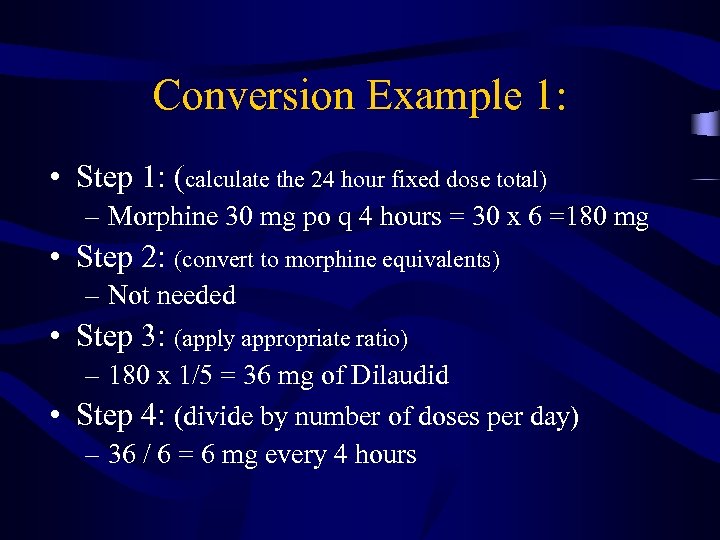 Conversion Example 1: • Step 1: (calculate the 24 hour fixed dose total) – Morphine 30 mg po q 4 hours = 30 x 6 =180 mg • Step 2: (convert to morphine equivalents) – Not needed • Step 3: (apply appropriate ratio) – 180 x 1/5 = 36 mg of Dilaudid • Step 4: (divide by number of doses per day) – 36 / 6 = 6 mg every 4 hours
Conversion Example 1: • Step 1: (calculate the 24 hour fixed dose total) – Morphine 30 mg po q 4 hours = 30 x 6 =180 mg • Step 2: (convert to morphine equivalents) – Not needed • Step 3: (apply appropriate ratio) – 180 x 1/5 = 36 mg of Dilaudid • Step 4: (divide by number of doses per day) – 36 / 6 = 6 mg every 4 hours
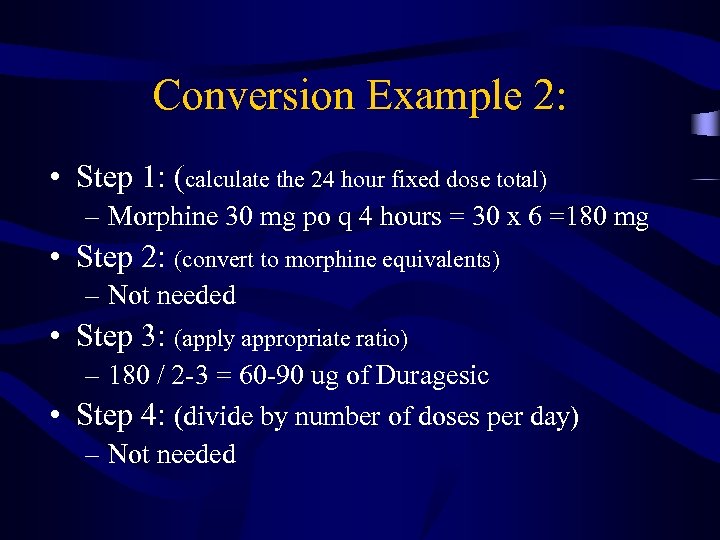 Conversion Example 2: • Step 1: (calculate the 24 hour fixed dose total) – Morphine 30 mg po q 4 hours = 30 x 6 =180 mg • Step 2: (convert to morphine equivalents) – Not needed • Step 3: (apply appropriate ratio) – 180 / 2 -3 = 60 -90 ug of Duragesic • Step 4: (divide by number of doses per day) – Not needed
Conversion Example 2: • Step 1: (calculate the 24 hour fixed dose total) – Morphine 30 mg po q 4 hours = 30 x 6 =180 mg • Step 2: (convert to morphine equivalents) – Not needed • Step 3: (apply appropriate ratio) – 180 / 2 -3 = 60 -90 ug of Duragesic • Step 4: (divide by number of doses per day) – Not needed
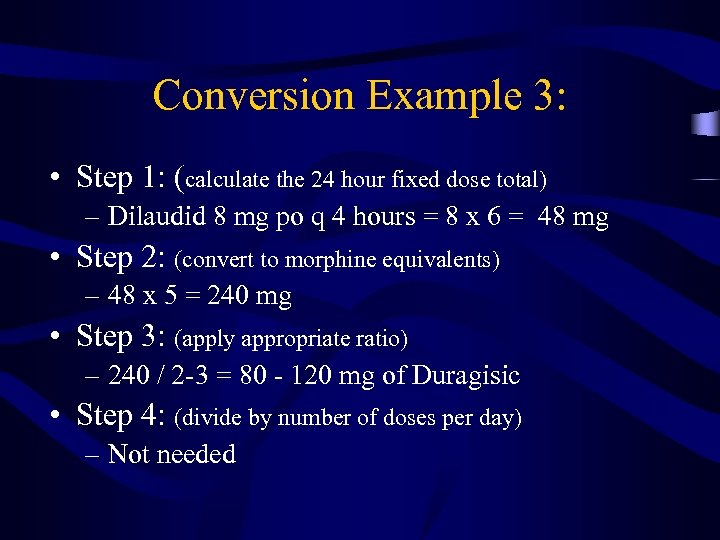 Conversion Example 3: • Step 1: (calculate the 24 hour fixed dose total) – Dilaudid 8 mg po q 4 hours = 8 x 6 = 48 mg • Step 2: (convert to morphine equivalents) – 48 x 5 = 240 mg • Step 3: (apply appropriate ratio) – 240 / 2 -3 = 80 - 120 mg of Duragisic • Step 4: (divide by number of doses per day) – Not needed
Conversion Example 3: • Step 1: (calculate the 24 hour fixed dose total) – Dilaudid 8 mg po q 4 hours = 8 x 6 = 48 mg • Step 2: (convert to morphine equivalents) – 48 x 5 = 240 mg • Step 3: (apply appropriate ratio) – 240 / 2 -3 = 80 - 120 mg of Duragisic • Step 4: (divide by number of doses per day) – Not needed
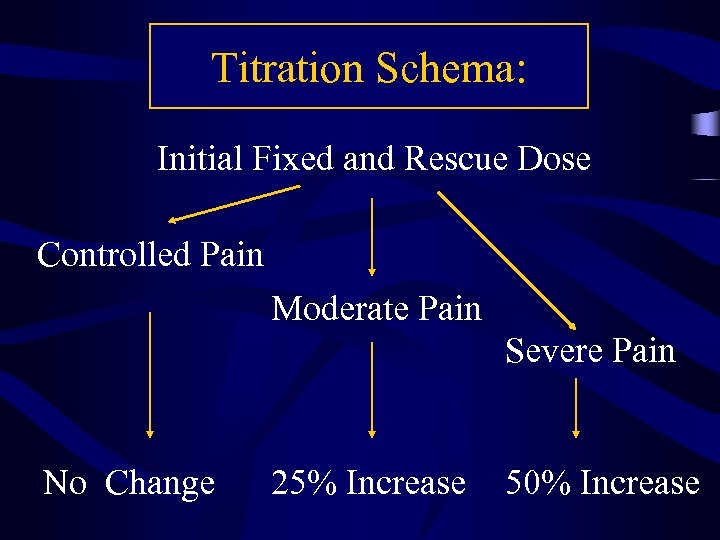 Titration Schema: Initial Fixed and Rescue Dose Controlled Pain Moderate Pain Severe Pain No Change 25% Increase 50% Increase
Titration Schema: Initial Fixed and Rescue Dose Controlled Pain Moderate Pain Severe Pain No Change 25% Increase 50% Increase
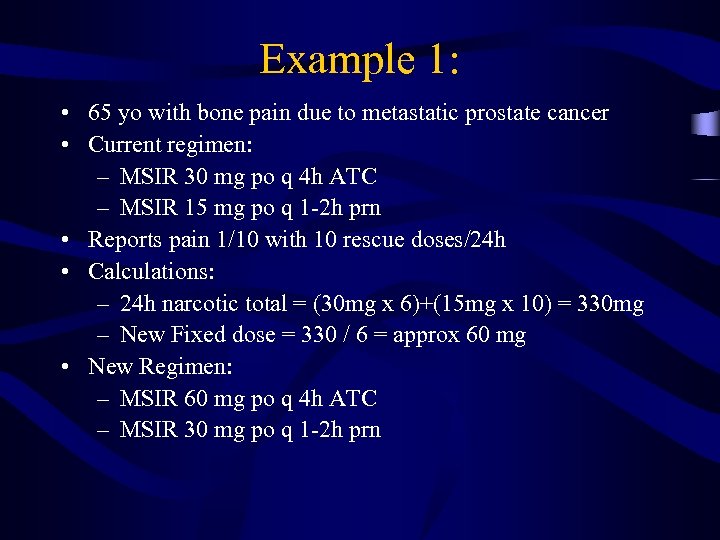 Example 1: • 65 yo with bone pain due to metastatic prostate cancer • Current regimen: – MSIR 30 mg po q 4 h ATC – MSIR 15 mg po q 1 -2 h prn • Reports pain 1/10 with 10 rescue doses/24 h • Calculations: – 24 h narcotic total = (30 mg x 6)+(15 mg x 10) = 330 mg – New Fixed dose = 330 / 6 = approx 60 mg • New Regimen: – MSIR 60 mg po q 4 h ATC – MSIR 30 mg po q 1 -2 h prn
Example 1: • 65 yo with bone pain due to metastatic prostate cancer • Current regimen: – MSIR 30 mg po q 4 h ATC – MSIR 15 mg po q 1 -2 h prn • Reports pain 1/10 with 10 rescue doses/24 h • Calculations: – 24 h narcotic total = (30 mg x 6)+(15 mg x 10) = 330 mg – New Fixed dose = 330 / 6 = approx 60 mg • New Regimen: – MSIR 60 mg po q 4 h ATC – MSIR 30 mg po q 1 -2 h prn
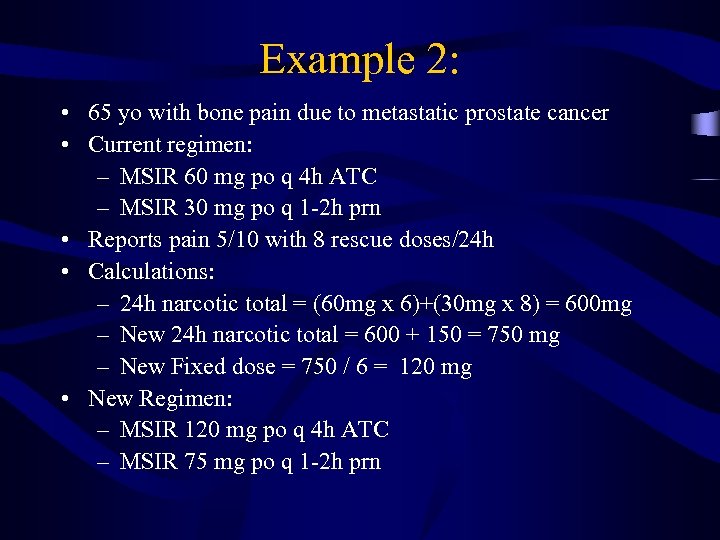 Example 2: • 65 yo with bone pain due to metastatic prostate cancer • Current regimen: – MSIR 60 mg po q 4 h ATC – MSIR 30 mg po q 1 -2 h prn • Reports pain 5/10 with 8 rescue doses/24 h • Calculations: – 24 h narcotic total = (60 mg x 6)+(30 mg x 8) = 600 mg – New 24 h narcotic total = 600 + 150 = 750 mg – New Fixed dose = 750 / 6 = 120 mg • New Regimen: – MSIR 120 mg po q 4 h ATC – MSIR 75 mg po q 1 -2 h prn
Example 2: • 65 yo with bone pain due to metastatic prostate cancer • Current regimen: – MSIR 60 mg po q 4 h ATC – MSIR 30 mg po q 1 -2 h prn • Reports pain 5/10 with 8 rescue doses/24 h • Calculations: – 24 h narcotic total = (60 mg x 6)+(30 mg x 8) = 600 mg – New 24 h narcotic total = 600 + 150 = 750 mg – New Fixed dose = 750 / 6 = 120 mg • New Regimen: – MSIR 120 mg po q 4 h ATC – MSIR 75 mg po q 1 -2 h prn
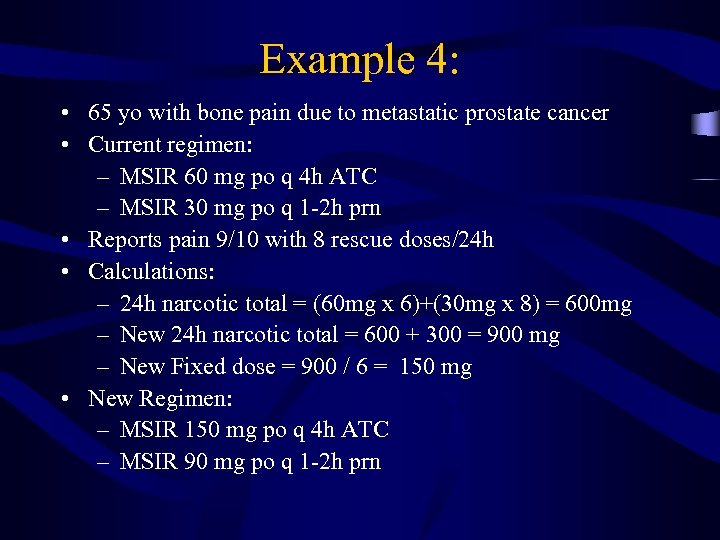 Example 4: • 65 yo with bone pain due to metastatic prostate cancer • Current regimen: – MSIR 60 mg po q 4 h ATC – MSIR 30 mg po q 1 -2 h prn • Reports pain 9/10 with 8 rescue doses/24 h • Calculations: – 24 h narcotic total = (60 mg x 6)+(30 mg x 8) = 600 mg – New 24 h narcotic total = 600 + 300 = 900 mg – New Fixed dose = 900 / 6 = 150 mg • New Regimen: – MSIR 150 mg po q 4 h ATC – MSIR 90 mg po q 1 -2 h prn
Example 4: • 65 yo with bone pain due to metastatic prostate cancer • Current regimen: – MSIR 60 mg po q 4 h ATC – MSIR 30 mg po q 1 -2 h prn • Reports pain 9/10 with 8 rescue doses/24 h • Calculations: – 24 h narcotic total = (60 mg x 6)+(30 mg x 8) = 600 mg – New 24 h narcotic total = 600 + 300 = 900 mg – New Fixed dose = 900 / 6 = 150 mg • New Regimen: – MSIR 150 mg po q 4 h ATC – MSIR 90 mg po q 1 -2 h prn
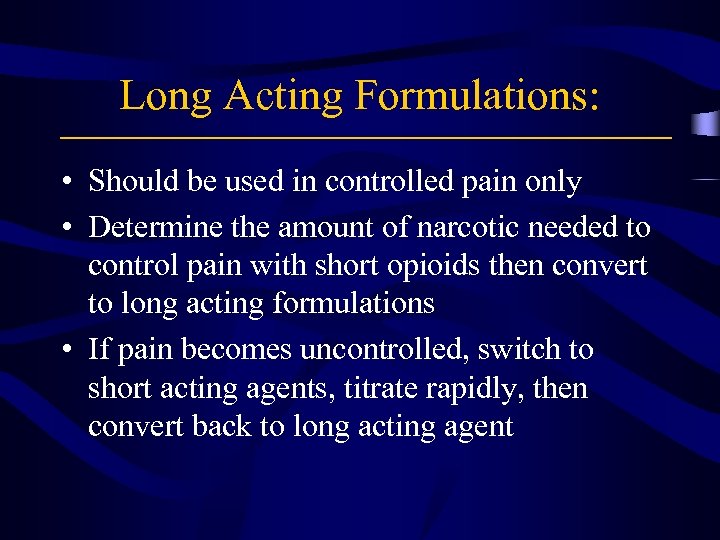 Long Acting Formulations: • Should be used in controlled pain only • Determine the amount of narcotic needed to control pain with short opioids then convert to long acting formulations • If pain becomes uncontrolled, switch to short acting agents, titrate rapidly, then convert back to long acting agent
Long Acting Formulations: • Should be used in controlled pain only • Determine the amount of narcotic needed to control pain with short opioids then convert to long acting formulations • If pain becomes uncontrolled, switch to short acting agents, titrate rapidly, then convert back to long acting agent
 Sustained Release Formulations: • Morphine • Oxycodone • Fentanyl • Dilaudid
Sustained Release Formulations: • Morphine • Oxycodone • Fentanyl • Dilaudid
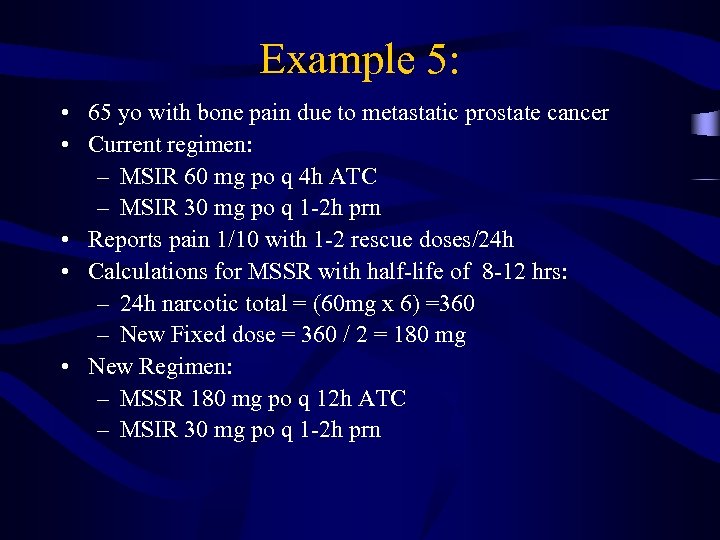 Example 5: • 65 yo with bone pain due to metastatic prostate cancer • Current regimen: – MSIR 60 mg po q 4 h ATC – MSIR 30 mg po q 1 -2 h prn • Reports pain 1/10 with 1 -2 rescue doses/24 h • Calculations for MSSR with half-life of 8 -12 hrs: – 24 h narcotic total = (60 mg x 6) =360 – New Fixed dose = 360 / 2 = 180 mg • New Regimen: – MSSR 180 mg po q 12 h ATC – MSIR 30 mg po q 1 -2 h prn
Example 5: • 65 yo with bone pain due to metastatic prostate cancer • Current regimen: – MSIR 60 mg po q 4 h ATC – MSIR 30 mg po q 1 -2 h prn • Reports pain 1/10 with 1 -2 rescue doses/24 h • Calculations for MSSR with half-life of 8 -12 hrs: – 24 h narcotic total = (60 mg x 6) =360 – New Fixed dose = 360 / 2 = 180 mg • New Regimen: – MSSR 180 mg po q 12 h ATC – MSIR 30 mg po q 1 -2 h prn
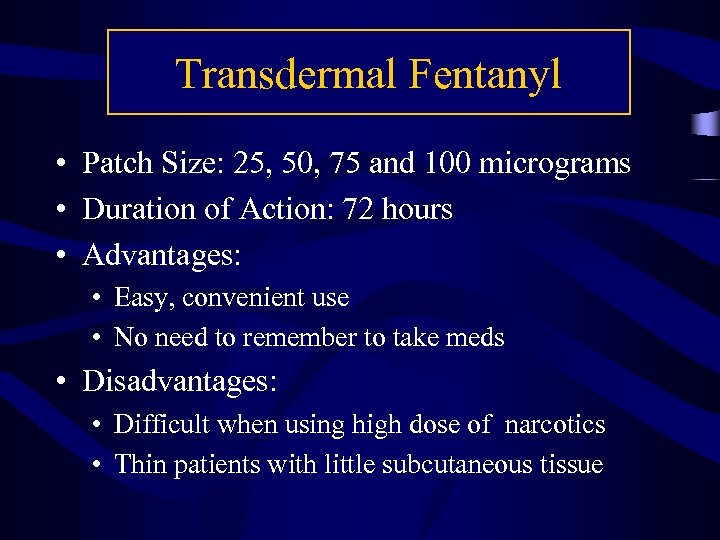 Transdermal Fentanyl • Patch Size: 25, 50, 75 and 100 micrograms • Duration of Action: 72 hours • Advantages: • Easy, convenient use • No need to remember to take meds • Disadvantages: • Difficult when using high dose of narcotics • Thin patients with little subcutaneous tissue
Transdermal Fentanyl • Patch Size: 25, 50, 75 and 100 micrograms • Duration of Action: 72 hours • Advantages: • Easy, convenient use • No need to remember to take meds • Disadvantages: • Difficult when using high dose of narcotics • Thin patients with little subcutaneous tissue
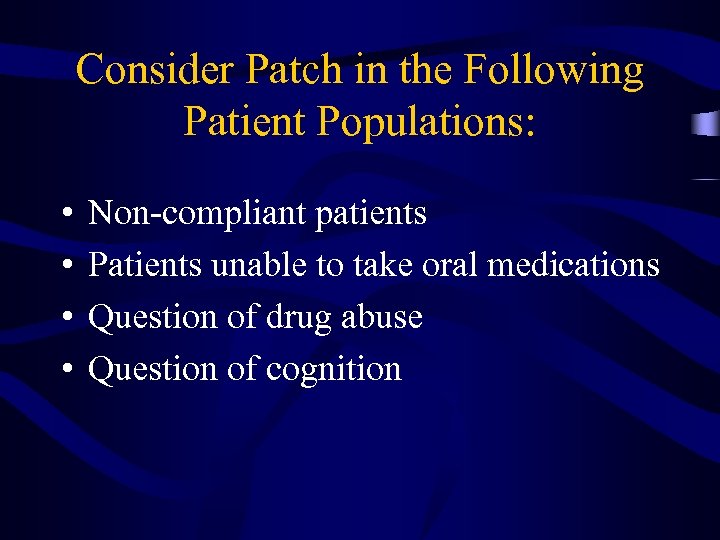 Consider Patch in the Following Patient Populations: • • Non-compliant patients Patients unable to take oral medications Question of drug abuse Question of cognition
Consider Patch in the Following Patient Populations: • • Non-compliant patients Patients unable to take oral medications Question of drug abuse Question of cognition
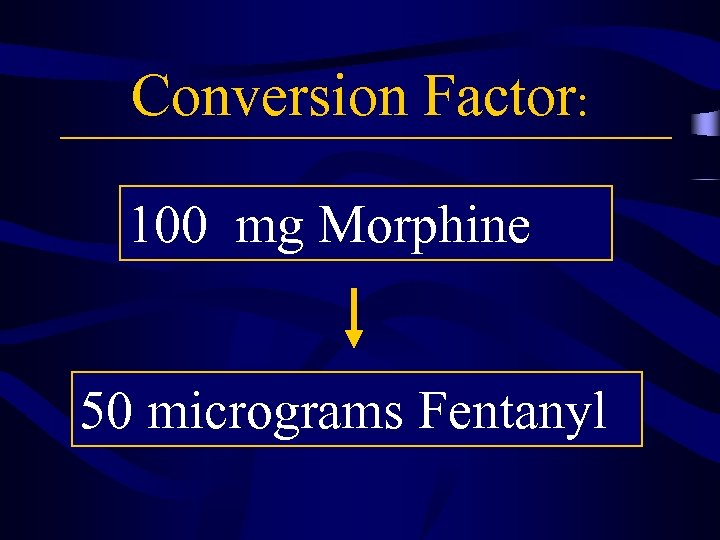 Conversion Factor: 100 mg Morphine 50 micrograms Fentanyl
Conversion Factor: 100 mg Morphine 50 micrograms Fentanyl
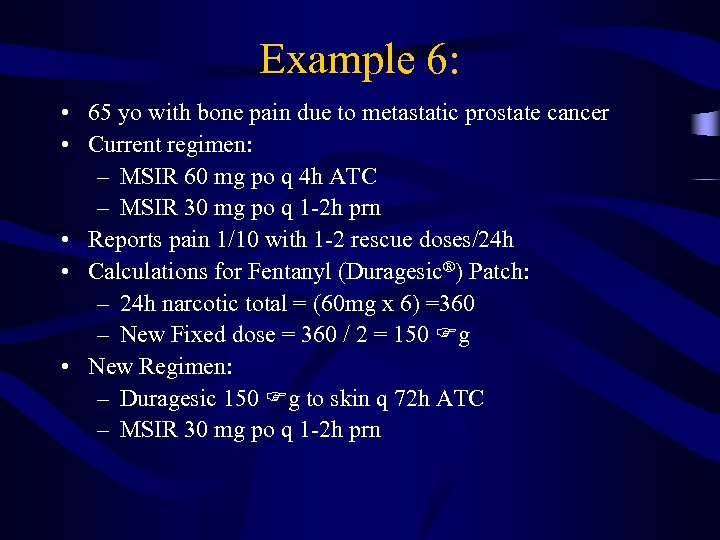 Example 6: • 65 yo with bone pain due to metastatic prostate cancer • Current regimen: – MSIR 60 mg po q 4 h ATC – MSIR 30 mg po q 1 -2 h prn • Reports pain 1/10 with 1 -2 rescue doses/24 h • Calculations for Fentanyl (Duragesic®) Patch: – 24 h narcotic total = (60 mg x 6) =360 – New Fixed dose = 360 / 2 = 150 g • New Regimen: – Duragesic 150 g to skin q 72 h ATC – MSIR 30 mg po q 1 -2 h prn
Example 6: • 65 yo with bone pain due to metastatic prostate cancer • Current regimen: – MSIR 60 mg po q 4 h ATC – MSIR 30 mg po q 1 -2 h prn • Reports pain 1/10 with 1 -2 rescue doses/24 h • Calculations for Fentanyl (Duragesic®) Patch: – 24 h narcotic total = (60 mg x 6) =360 – New Fixed dose = 360 / 2 = 150 g • New Regimen: – Duragesic 150 g to skin q 72 h ATC – MSIR 30 mg po q 1 -2 h prn
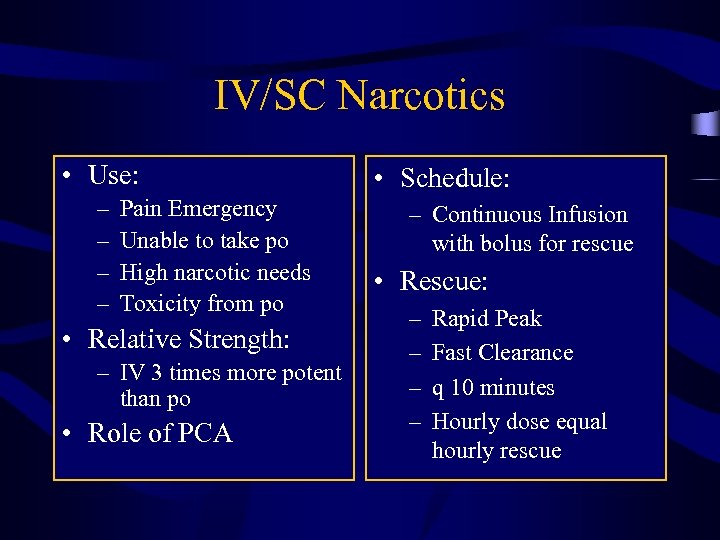 IV/SC Narcotics • Use: – – Pain Emergency Unable to take po High narcotic needs Toxicity from po • Relative Strength: – IV 3 times more potent than po • Role of PCA • Schedule: – Continuous Infusion with bolus for rescue • Rescue: – – Rapid Peak Fast Clearance q 10 minutes Hourly dose equal hourly rescue
IV/SC Narcotics • Use: – – Pain Emergency Unable to take po High narcotic needs Toxicity from po • Relative Strength: – IV 3 times more potent than po • Role of PCA • Schedule: – Continuous Infusion with bolus for rescue • Rescue: – – Rapid Peak Fast Clearance q 10 minutes Hourly dose equal hourly rescue
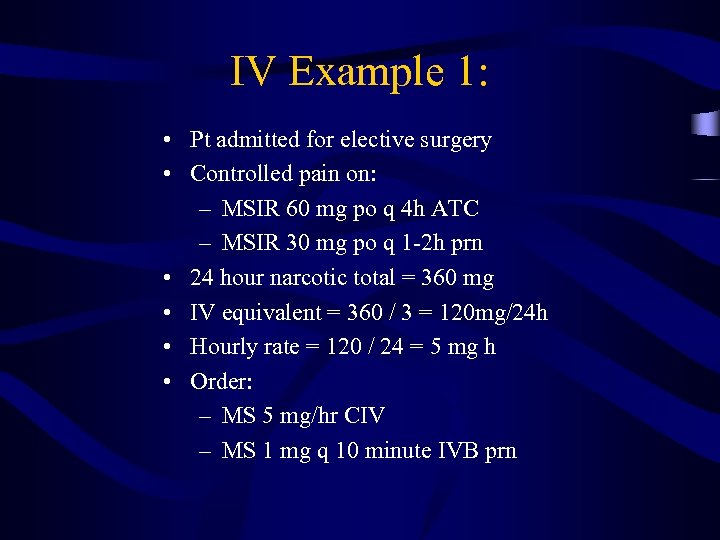 IV Example 1: • Pt admitted for elective surgery • Controlled pain on: – MSIR 60 mg po q 4 h ATC – MSIR 30 mg po q 1 -2 h prn • 24 hour narcotic total = 360 mg • IV equivalent = 360 / 3 = 120 mg/24 h • Hourly rate = 120 / 24 = 5 mg h • Order: – MS 5 mg/hr CIV – MS 1 mg q 10 minute IVB prn
IV Example 1: • Pt admitted for elective surgery • Controlled pain on: – MSIR 60 mg po q 4 h ATC – MSIR 30 mg po q 1 -2 h prn • 24 hour narcotic total = 360 mg • IV equivalent = 360 / 3 = 120 mg/24 h • Hourly rate = 120 / 24 = 5 mg h • Order: – MS 5 mg/hr CIV – MS 1 mg q 10 minute IVB prn
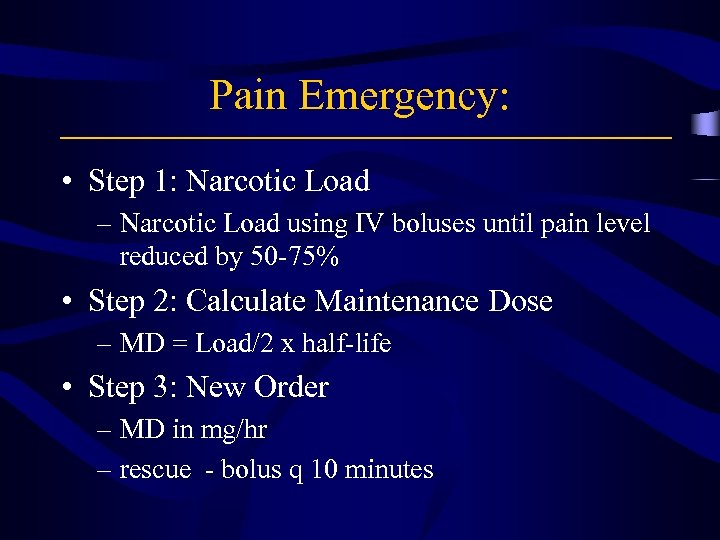 Pain Emergency: • Step 1: Narcotic Load – Narcotic Load using IV boluses until pain level reduced by 50 -75% • Step 2: Calculate Maintenance Dose – MD = Load/2 x half-life • Step 3: New Order – MD in mg/hr – rescue - bolus q 10 minutes
Pain Emergency: • Step 1: Narcotic Load – Narcotic Load using IV boluses until pain level reduced by 50 -75% • Step 2: Calculate Maintenance Dose – MD = Load/2 x half-life • Step 3: New Order – MD in mg/hr – rescue - bolus q 10 minutes
 Pain Emergency • High Dose Decadron • Anesthesiology Consult • Neurosurgery Consult
Pain Emergency • High Dose Decadron • Anesthesiology Consult • Neurosurgery Consult
 Barrier Reduction: • Patient education: – Endpoint to be assessed: • Beliefs • Communication skills • Knowledge pain control – Outcome of interventions: • Improve beliefs and adherence • Results variable for improved pain control • Physician and staff education: – Endpoints to be assessed: • • Knowledge Attitudes Practice patterns Pain control
Barrier Reduction: • Patient education: – Endpoint to be assessed: • Beliefs • Communication skills • Knowledge pain control – Outcome of interventions: • Improve beliefs and adherence • Results variable for improved pain control • Physician and staff education: – Endpoints to be assessed: • • Knowledge Attitudes Practice patterns Pain control
 Ongoing Education: Testing Two Intervention Strategies • Patient population: – Patients with cancer related pain requiring narcotics • Design: – Group 1: baseline education only – Group 2: “hot line” for questions or emergencies – Group 3: Provider initiated weekly follow-up • Results: – Improvement in beliefs with baseline education – No improvement in outcome with ongoing interventions
Ongoing Education: Testing Two Intervention Strategies • Patient population: – Patients with cancer related pain requiring narcotics • Design: – Group 1: baseline education only – Group 2: “hot line” for questions or emergencies – Group 3: Provider initiated weekly follow-up • Results: – Improvement in beliefs with baseline education – No improvement in outcome with ongoing interventions
 Narcotic Titration Order Schema: A Pilot Trial • Endpoint: – severe adverse events • Patient Selection: – pain with a level of 3 or greater – requiring narcotics • Methods: – nurse managed order schema with “physician contact” parameters – tools: • Patients: MMSE, pain dairy, BPI, CES-D, STAI • Family: F-COPES, FIRM, CSI
Narcotic Titration Order Schema: A Pilot Trial • Endpoint: – severe adverse events • Patient Selection: – pain with a level of 3 or greater – requiring narcotics • Methods: – nurse managed order schema with “physician contact” parameters – tools: • Patients: MMSE, pain dairy, BPI, CES-D, STAI • Family: F-COPES, FIRM, CSI
 Narcotic Titration Order Schema: A Pilot Trial • Results: – No severe adverse events – Feasible in the clinic setting • Future Directions: – Phase III Trial through VICCAN • Issues for further exploration: – Non-compliance – Effect if pain on family functioning
Narcotic Titration Order Schema: A Pilot Trial • Results: – No severe adverse events – Feasible in the clinic setting • Future Directions: – Phase III Trial through VICCAN • Issues for further exploration: – Non-compliance – Effect if pain on family functioning
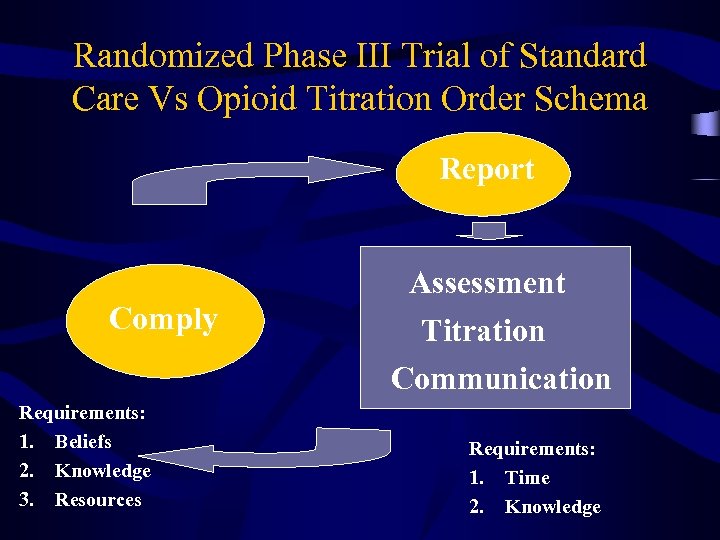 Randomized Phase III Trial of Standard Care Vs Opioid Titration Order Schema Report Comply Requirements: 1. Beliefs 2. Knowledge 3. Resources Assessment Titration Communication Requirements: 1. Time 2. Knowledge
Randomized Phase III Trial of Standard Care Vs Opioid Titration Order Schema Report Comply Requirements: 1. Beliefs 2. Knowledge 3. Resources Assessment Titration Communication Requirements: 1. Time 2. Knowledge
 Cancer Pain Management: Requirements for Success • • • Setting the Right Priorities Dedicated Team Willing to Take Time Systematic Approach Understanding of the Basic Principles of Symptom Control
Cancer Pain Management: Requirements for Success • • • Setting the Right Priorities Dedicated Team Willing to Take Time Systematic Approach Understanding of the Basic Principles of Symptom Control
 Instructors can impart only a fraction of the teaching. It is through your own devoted practice that the mysteries are brought to life. Morihei Ueshiba
Instructors can impart only a fraction of the teaching. It is through your own devoted practice that the mysteries are brought to life. Morihei Ueshiba


