7f207dd9f21560342b9ba17398033cd2.ppt
- Количество слайдов: 153
 A physiologic approach to scientific presentations Eugene H. Blackstone, MD
A physiologic approach to scientific presentations Eugene H. Blackstone, MD
 Objectives (1) Essential preparation • How long do I have? • Who is my audience? • What am I going to say? Text • A physiologic approach to oral scientific presentations
Objectives (1) Essential preparation • How long do I have? • Who is my audience? • What am I going to say? Text • A physiologic approach to oral scientific presentations
 Objectives (2) Visuals • The good, the bad, and the ugly • What Yahoo! taught us Delivery • Presidential secrets for effective speeches Q&A • What questions do you have for my answers?
Objectives (2) Visuals • The good, the bad, and the ugly • What Yahoo! taught us Delivery • Presidential secrets for effective speeches Q&A • What questions do you have for my answers?
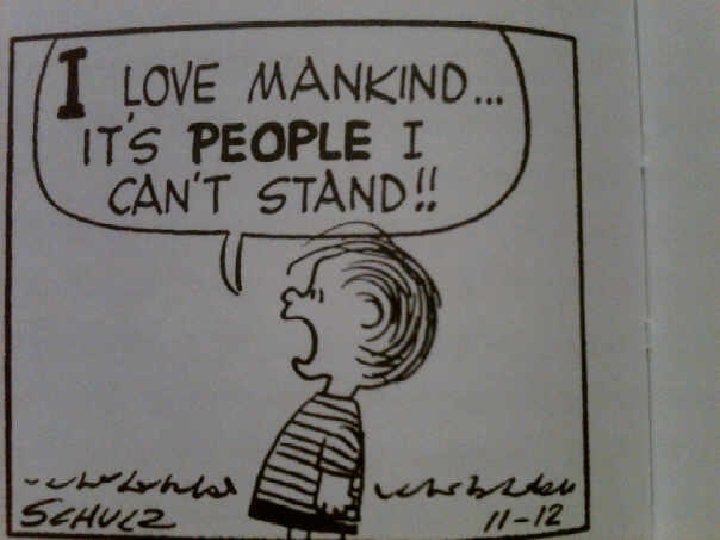
 Who cares? See one, do one, teach one • Most scientific presentations are poor models • Principles of a good presentation are rarely taught • Most principles not intuitively obvious—until pointed out
Who cares? See one, do one, teach one • Most scientific presentations are poor models • Principles of a good presentation are rarely taught • Most principles not intuitively obvious—until pointed out
 Talks I have listened to… What I hated What I liked …and why!
Talks I have listened to… What I hated What I liked …and why!
 Essential Preparation
Essential Preparation
 Before writing the text… How long do I have? Who is my audience? What is my message?
Before writing the text… How long do I have? Who is my audience? What is my message?
 How long do I have? Short • Original research presentation • 5 to 10 minute slide presentation • Selected on basis of abstract Long • Grand rounds, invited talk • 15 to 50 minutes (usually slides) • Assigned by organizers
How long do I have? Short • Original research presentation • 5 to 10 minute slide presentation • Selected on basis of abstract Long • Grand rounds, invited talk • 15 to 50 minutes (usually slides) • Assigned by organizers
 How long do I have? Short • Original research presentation • 5 to 10 minute slide presentation • Selected on basis of abstract Long Our et targ • Grand rounds, invited talk • 15 to 50 minutes (usually slides) • Assigned by organizers
How long do I have? Short • Original research presentation • 5 to 10 minute slide presentation • Selected on basis of abstract Long Our et targ • Grand rounds, invited talk • 15 to 50 minutes (usually slides) • Assigned by organizers
 Who is my audience? What can I assume they know? What are they not likely to know?
Who is my audience? What can I assume they know? What are they not likely to know?
 What is my message? For short talk • 2 -3 sentences, often the conclusions Purpose of talk • To marshal evidence supporting your message…no more, no less! Utility • They dictate key points & order for objectives and results Typically takes ~ 3 hours
What is my message? For short talk • 2 -3 sentences, often the conclusions Purpose of talk • To marshal evidence supporting your message…no more, no less! Utility • They dictate key points & order for objectives and results Typically takes ~ 3 hours
 Text
Text
 Organizational Structure How were various talks you have heard organized? • Describe different types • Evaluate effectiveness • What you liked, what you hated about organization How do you wish scientific talks were structured?
Organizational Structure How were various talks you have heard organized? • Describe different types • Evaluate effectiveness • What you liked, what you hated about organization How do you wish scientific talks were structured?
 Physiologic Approach Ears • First hearing—listener doesn’t know what to expect • Has to keep up—a serial process • Mind can’t wander or be distracted— but you are speaking at ½ speed of thinking (~114 wpm vs. ~ 300) • Relies on signposts you provide Make listening easy!
Physiologic Approach Ears • First hearing—listener doesn’t know what to expect • Has to keep up—a serial process • Mind can’t wander or be distracted— but you are speaking at ½ speed of thinking (~114 wpm vs. ~ 300) • Relies on signposts you provide Make listening easy!
 Easy Listening Structure clear • Purpose, results, conclusions in same order with same words Just in time listening • Introduce nothing before it is needed Leave no loose ends • Wrap up prevents missing both current point and next point
Easy Listening Structure clear • Purpose, results, conclusions in same order with same words Just in time listening • Introduce nothing before it is needed Leave no loose ends • Wrap up prevents missing both current point and next point
 Easy Listening One idea per sentence • Break into absorbable bites Semi-conversational • Balance formal vs. casual style • Active vs. passive Emphasize message • Complex methods and statistics loose audience if they are not central to the message
Easy Listening One idea per sentence • Break into absorbable bites Semi-conversational • Balance formal vs. casual style • Active vs. passive Emphasize message • Complex methods and statistics loose audience if they are not central to the message
 Easy Listening Connect with audience • Attitude, energy, motions Be plain • No bloat, unnecessary jargon, or speaking in abbreviations Keep audience in the present • Pairs: on the one hand, on the other • Tee up comparisons, anticipation • Occasional pauses; change pace
Easy Listening Connect with audience • Attitude, energy, motions Be plain • No bloat, unnecessary jargon, or speaking in abbreviations Keep audience in the present • Pairs: on the one hand, on the other • Tee up comparisons, anticipation • Occasional pauses; change pace
 Easy Listening A few specific observations • • • Things come in 3 s Talk vs. medical writing Bookends Nuggets The end
Easy Listening A few specific observations • • • Things come in 3 s Talk vs. medical writing Bookends Nuggets The end
 Easy Listening Things come in 3 s • Let’s get started. Together. Today. • I came. I saw. I conquered. • Of the people. For the people. By the people. • The good; the bad; the ugly
Easy Listening Things come in 3 s • Let’s get started. Together. Today. • I came. I saw. I conquered. • Of the people. For the people. By the people. • The good; the bad; the ugly
 From Trees to Wood and Back Eugene H. Blackstone, MD
From Trees to Wood and Back Eugene H. Blackstone, MD
 Trees Patient Data
Trees Patient Data
 Information Collection of • Workflow documentation • Recorded observations • Materials Usually • Recorded as narrative Usability • Low
Information Collection of • Workflow documentation • Recorded observations • Materials Usually • Recorded as narrative Usability • Low
 Data Definition • Organized values for variables Expression • Symbolically (numbers, controlled vocabulary) Presentation • Can be summarized by descriptive statistics
Data Definition • Organized values for variables Expression • Symbolically (numbers, controlled vocabulary) Presentation • Can be summarized by descriptive statistics
 Bases for Medical Practice Evidence-based medicine • Randomized trials • Crude guidelines for therapy Information-based medicine • Observational clinical data • Patient-specific therapy Personalized medicine • -omic studies + clinical data • Tailored (n=1) therapy
Bases for Medical Practice Evidence-based medicine • Randomized trials • Crude guidelines for therapy Information-based medicine • Observational clinical data • Patient-specific therapy Personalized medicine • -omic studies + clinical data • Tailored (n=1) therapy
 A talk is not a manuscript! IMRD structure • Introduction What question was studied? • Methods How was the question studied? • Results What was found? • Discussion What do the results mean?
A talk is not a manuscript! IMRD structure • Introduction What question was studied? • Methods How was the question studied? • Results What was found? • Discussion What do the results mean?
 IMRD Introduced • by Pasteur in 1870 s Neither • prose nor poetry A roadmap • with standardized signposts
IMRD Introduced • by Pasteur in 1870 s Neither • prose nor poetry A roadmap • with standardized signposts
 Why adopt IMRD? It is a standardized aid for… • Selective • Strategic …reading
Why adopt IMRD? It is a standardized aid for… • Selective • Strategic …reading
 Oops! Listening • Not reading • Not selective • Not strategic It’s serial!
Oops! Listening • Not reading • Not selective • Not strategic It’s serial!
 Early Listening—Bookends Story-telling • Once upon a time in a land far, far away… • …and they lived happily ever after!
Early Listening—Bookends Story-telling • Once upon a time in a land far, far away… • …and they lived happily ever after!
 Easy Listening Bookends • Capture attention immediately • What I am saying is important to you! • Return to this at end: what it means to you!
Easy Listening Bookends • Capture attention immediately • What I am saying is important to you! • Return to this at end: what it means to you!
 Mitral anulus calcification: To debride or not to debride? Syed Tarique Hussain
Mitral anulus calcification: To debride or not to debride? Syed Tarique Hussain
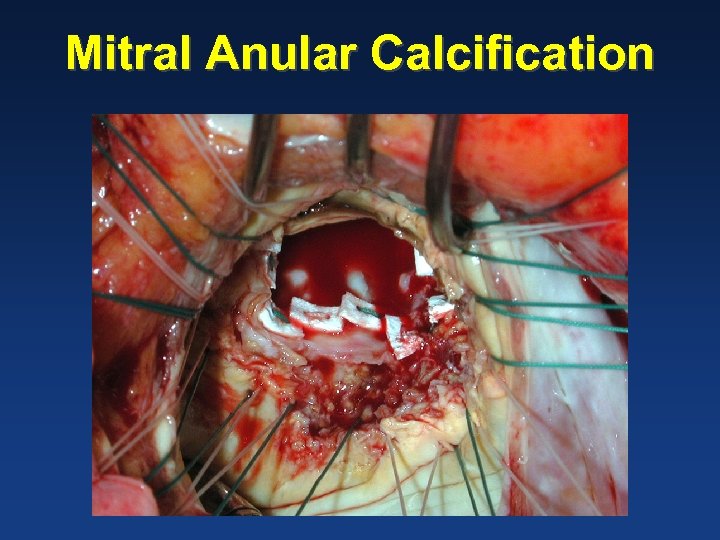 Mitral Anular Calcification
Mitral Anular Calcification
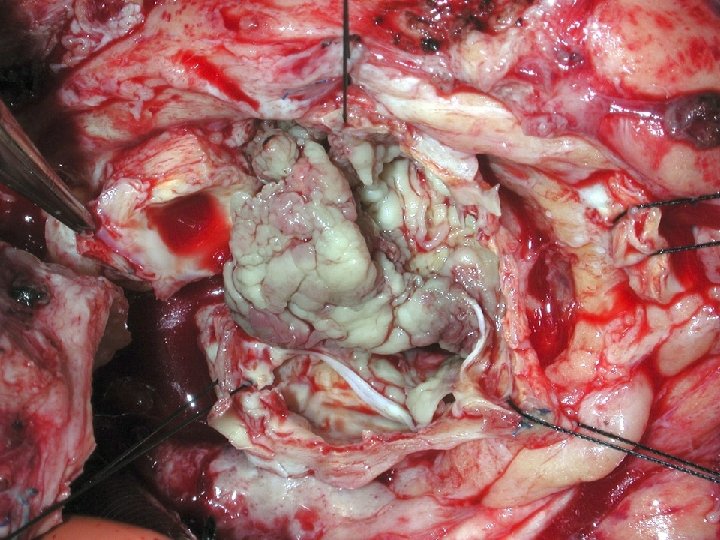
 Surgery for fungal infective endocarditis: A comparison with non-fungal cases Victor Chao
Surgery for fungal infective endocarditis: A comparison with non-fungal cases Victor Chao
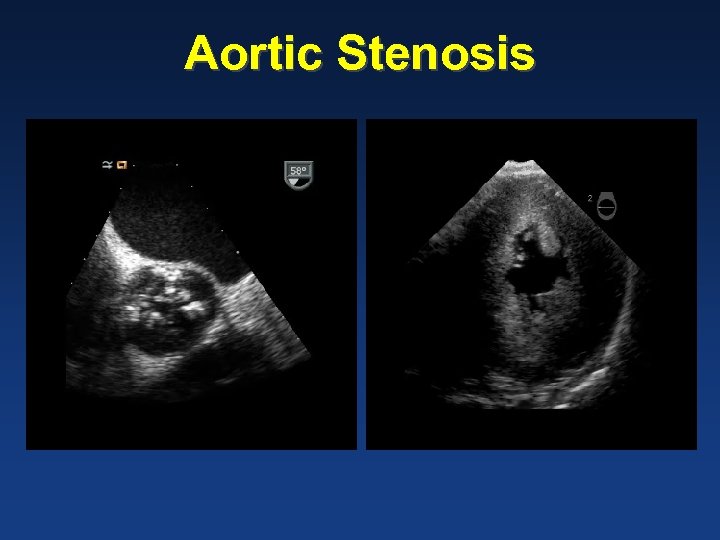 Aortic Stenosis Echo videos
Aortic Stenosis Echo videos
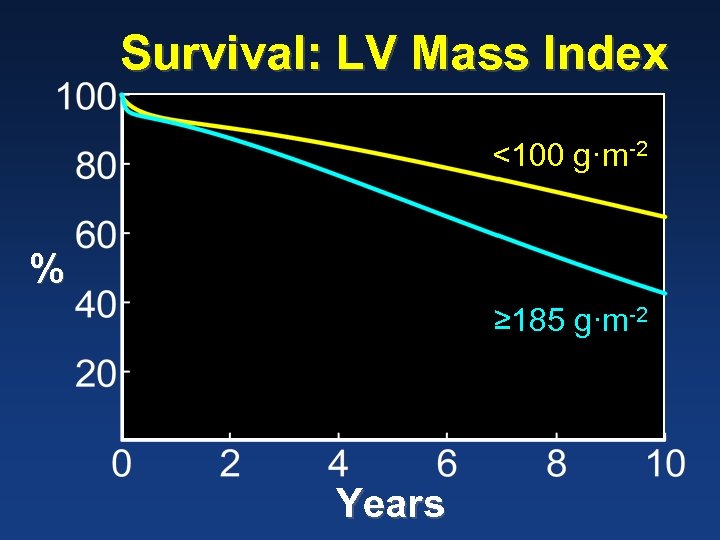 Survival: LV Mass Index <100 g·m-2 % ≥ 185 g·m-2 Years
Survival: LV Mass Index <100 g·m-2 % ≥ 185 g·m-2 Years
 Don't Wait for Symptoms! Watch the Ventricle Residual Hypertrophy After Aortic Valve Replacement Jocelyn Beach
Don't Wait for Symptoms! Watch the Ventricle Residual Hypertrophy After Aortic Valve Replacement Jocelyn Beach
 Easy Listening—Nuggets Objectives • The roadmap we’ll follow together Nuggets of discovery • They follow order of objectives • Include, if necessary, methods • Present results—what you have discovered • Discuss—wrap up the nugget
Easy Listening—Nuggets Objectives • The roadmap we’ll follow together Nuggets of discovery • They follow order of objectives • Include, if necessary, methods • Present results—what you have discovered • Discuss—wrap up the nugget
 Example Fungal & non-fungal endocarditis
Example Fungal & non-fungal endocarditis
 Objectives Compare • Early and late outcomes of surgery for fungal and non-fungal endocarditis Account for • Patient and disease characteristics
Objectives Compare • Early and late outcomes of surgery for fungal and non-fungal endocarditis Account for • Patient and disease characteristics
 Early Outcomes
Early Outcomes
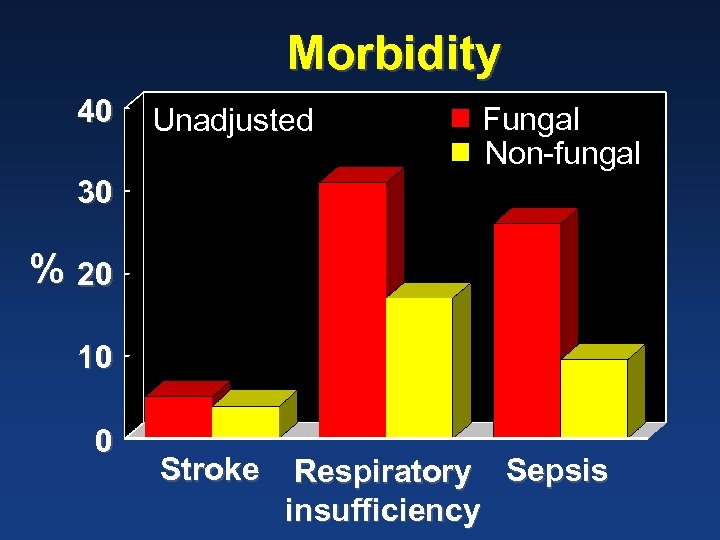 Morbidity 40 Unadjusted Fungal Non-fungal 30 % 20 10 0 Stroke Respiratory Sepsis insufficiency
Morbidity 40 Unadjusted Fungal Non-fungal 30 % 20 10 0 Stroke Respiratory Sepsis insufficiency
 Problem: Patient Characteristics Differ
Problem: Patient Characteristics Differ
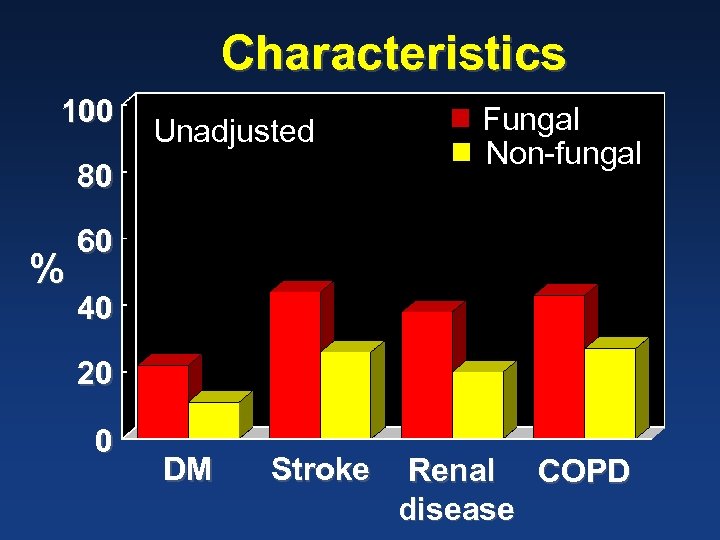 Characteristics 100 Unadjusted 80 % Fungal Non-fungal 60 40 20 0 DM Stroke Renal COPD disease
Characteristics 100 Unadjusted 80 % Fungal Non-fungal 60 40 20 0 DM Stroke Renal COPD disease
 39 Matched Pairs
39 Matched Pairs
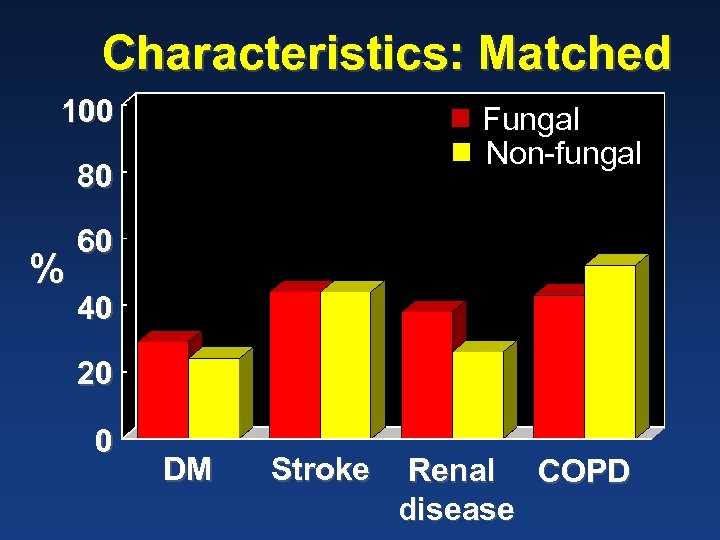 Characteristics: Matched 100 Fungal Non-fungal 80 % 60 40 20 0 DM Stroke Renal COPD disease
Characteristics: Matched 100 Fungal Non-fungal 80 % 60 40 20 0 DM Stroke Renal COPD disease
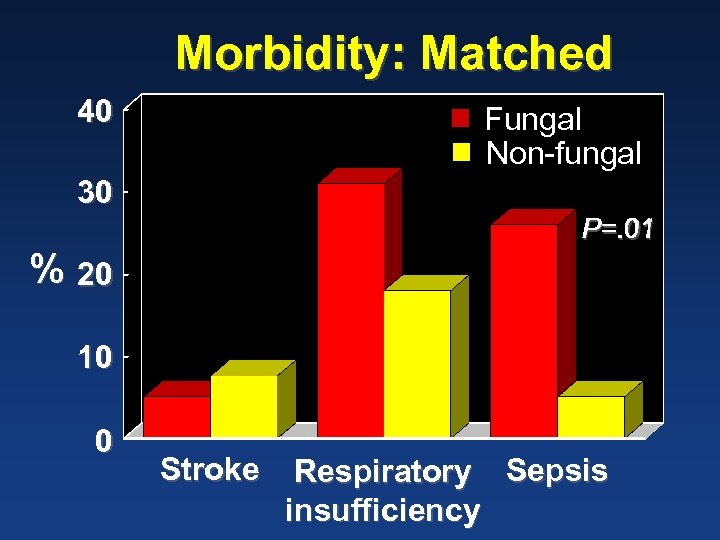 Morbidity: Matched 40 Fungal Non-fungal 30 P=. 01 % 20 10 0 Stroke Respiratory Sepsis insufficiency
Morbidity: Matched 40 Fungal Non-fungal 30 P=. 01 % 20 10 0 Stroke Respiratory Sepsis insufficiency
 Late Outcomes
Late Outcomes
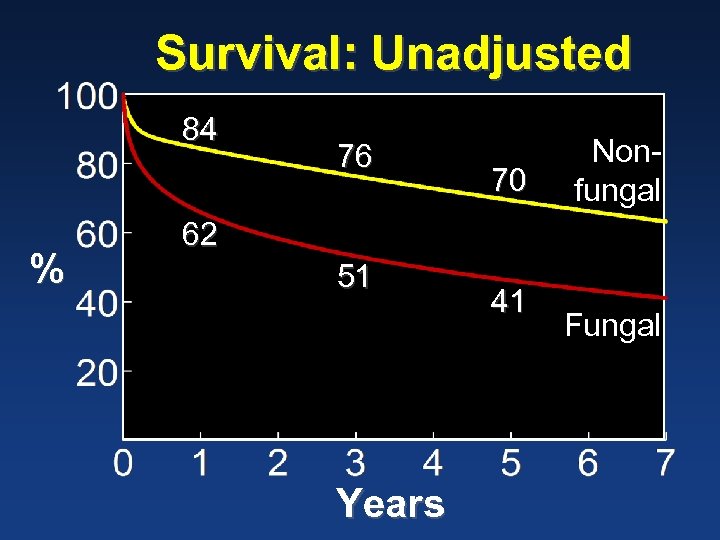 Survival: Unadjusted 84 % 76 70 Nonfungal 62 51 Years 41 Fungal
Survival: Unadjusted 84 % 76 70 Nonfungal 62 51 Years 41 Fungal
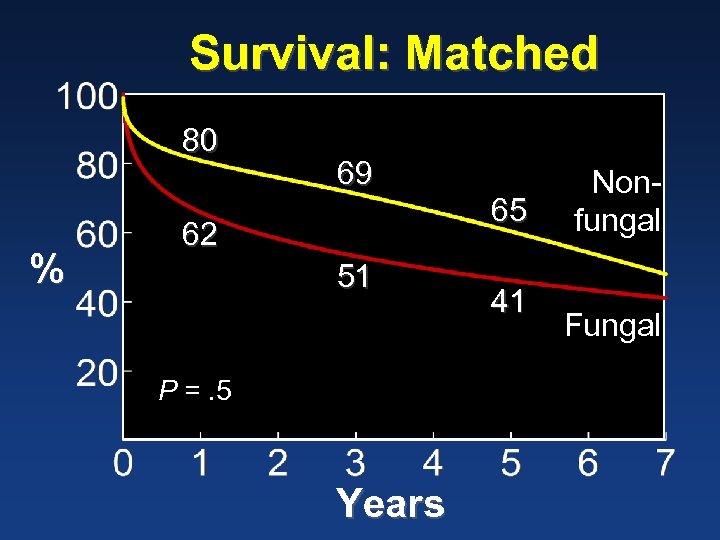 Survival: Matched 80 % 69 62 51 P =. 5 Years 65 41 Nonfungal Fungal
Survival: Matched 80 % 69 62 51 P =. 5 Years 65 41 Nonfungal Fungal
 Easy Listening—the Message What do you want to hear at the end of a talk?
Easy Listening—the Message What do you want to hear at the end of a talk?
 Easy Listening—the Message Summary? • In short talk it shouldn’t be necessary Conclusions • Take home message • May include recommendations Clear ending • Bookend • Thank you!
Easy Listening—the Message Summary? • In short talk it shouldn’t be necessary Conclusions • Take home message • May include recommendations Clear ending • Bookend • Thank you!
 Visuals (“slides”) with thanks to Yahoo!
Visuals (“slides”) with thanks to Yahoo!
 Critique some slides…
Critique some slides…
 • Reflective of the scarcity of resource, complexities of donor organ allocation and increased number of patients awaiting cardiac transplantation, is the acuity of those undergoing the procedure. In 1988, 42. 2% of patients undergoing transplant were Status II, waiting at home. In 1994, only 38. 3% were called in from home.
• Reflective of the scarcity of resource, complexities of donor organ allocation and increased number of patients awaiting cardiac transplantation, is the acuity of those undergoing the procedure. In 1988, 42. 2% of patients undergoing transplant were Status II, waiting at home. In 1994, only 38. 3% were called in from home.
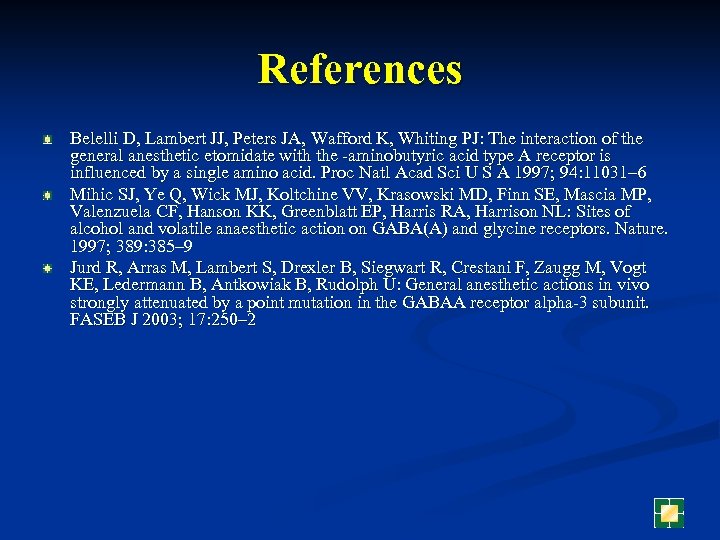 References Belelli D, Lambert JJ, Peters JA, Wafford K, Whiting PJ: The interaction of the general anesthetic etomidate with the -aminobutyric acid type A receptor is influenced by a single amino acid. Proc Natl Acad Sci U S A 1997; 94: 11031– 6 Mihic SJ, Ye Q, Wick MJ, Koltchine VV, Krasowski MD, Finn SE, Mascia MP, Valenzuela CF, Hanson KK, Greenblatt EP, Harris RA, Harrison NL: Sites of alcohol and volatile anaesthetic action on GABA(A) and glycine receptors. Nature. 1997; 389: 385– 9 Jurd R, Arras M, Lambert S, Drexler B, Siegwart R, Crestani F, Zaugg M, Vogt KE, Ledermann B, Antkowiak B, Rudolph U: General anesthetic actions in vivo strongly attenuated by a point mutation in the GABAA receptor alpha-3 subunit. FASEB J 2003; 17: 250– 2
References Belelli D, Lambert JJ, Peters JA, Wafford K, Whiting PJ: The interaction of the general anesthetic etomidate with the -aminobutyric acid type A receptor is influenced by a single amino acid. Proc Natl Acad Sci U S A 1997; 94: 11031– 6 Mihic SJ, Ye Q, Wick MJ, Koltchine VV, Krasowski MD, Finn SE, Mascia MP, Valenzuela CF, Hanson KK, Greenblatt EP, Harris RA, Harrison NL: Sites of alcohol and volatile anaesthetic action on GABA(A) and glycine receptors. Nature. 1997; 389: 385– 9 Jurd R, Arras M, Lambert S, Drexler B, Siegwart R, Crestani F, Zaugg M, Vogt KE, Ledermann B, Antkowiak B, Rudolph U: General anesthetic actions in vivo strongly attenuated by a point mutation in the GABAA receptor alpha-3 subunit. FASEB J 2003; 17: 250– 2
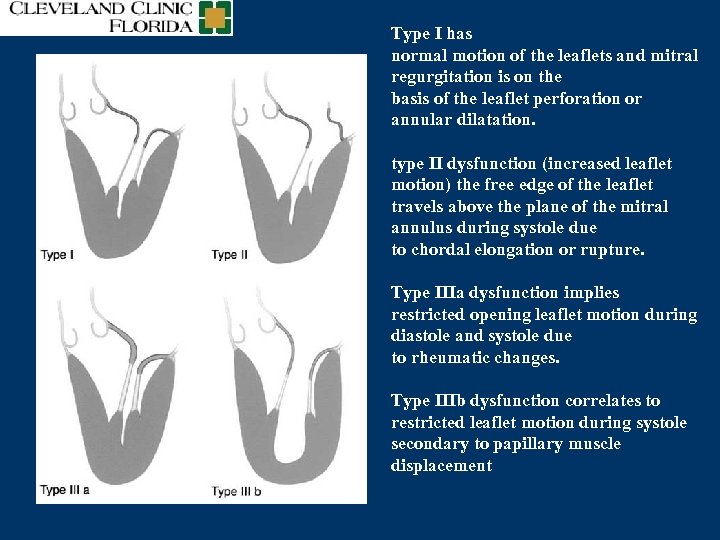 Type I has normal motion of the leaflets and mitral regurgitation is on the basis of the leaflet perforation or annular dilatation. type II dysfunction (increased leaflet motion) the free edge of the leaflet travels above the plane of the mitral annulus during systole due to chordal elongation or rupture. Type IIIa dysfunction implies restricted opening leaflet motion during diastole and systole due to rheumatic changes. Type IIIb dysfunction correlates to restricted leaflet motion during systole secondary to papillary muscle displacement
Type I has normal motion of the leaflets and mitral regurgitation is on the basis of the leaflet perforation or annular dilatation. type II dysfunction (increased leaflet motion) the free edge of the leaflet travels above the plane of the mitral annulus during systole due to chordal elongation or rupture. Type IIIa dysfunction implies restricted opening leaflet motion during diastole and systole due to rheumatic changes. Type IIIb dysfunction correlates to restricted leaflet motion during systole secondary to papillary muscle displacement
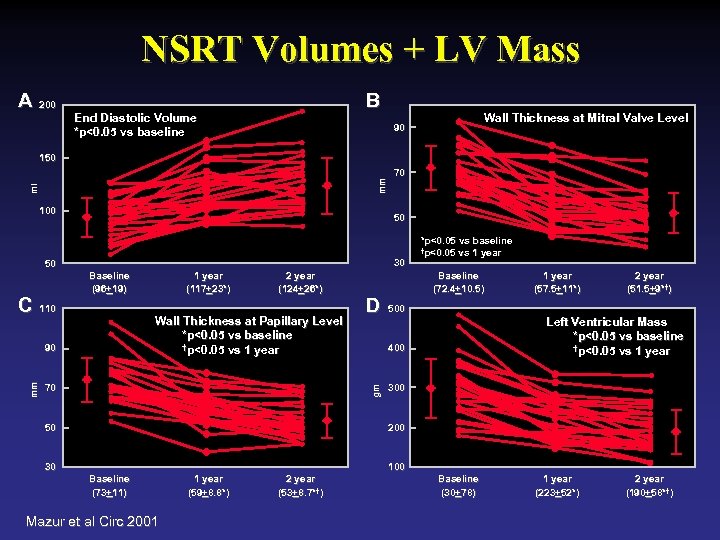 NSRT Volumes + LV Mass A 200 B End Diastolic Volume *p<0. 05 vs baseline Wall Thickness at Mitral Valve Level 90 ml mm 150 100 50 30 50 C 110 Baseline (96+19) (96+ 1 year (117+23*) (117+ 2 year (124+26*) (124+ Wall Thickness at Papillary Level *p<0. 05 vs baseline †p<0. 05 vs 1 year 90 70 D 50 *p<0. 05 vs baseline †p<0. 05 vs 1 year Baseline (72. 4+10. 5) (72. 4+ 1 year (57. 5+11*) (57. 5+ 2 year (51. 5+9*†) (51. 5+ 500 Left Ventricular Mass *p<0. 05 vs baseline †p<0. 05 vs 1 year 400 gm mm 70 300 200 30 100 Baseline (73+11) (73+ Mazur et al Circ 2001 1 year (59+8. 8*) (59+ 2 year (53+8. 7*†) (53+ Baseline (30+78) (30+ 1 year (223+52*) (223+ 2 year (190+58*†) (190+
NSRT Volumes + LV Mass A 200 B End Diastolic Volume *p<0. 05 vs baseline Wall Thickness at Mitral Valve Level 90 ml mm 150 100 50 30 50 C 110 Baseline (96+19) (96+ 1 year (117+23*) (117+ 2 year (124+26*) (124+ Wall Thickness at Papillary Level *p<0. 05 vs baseline †p<0. 05 vs 1 year 90 70 D 50 *p<0. 05 vs baseline †p<0. 05 vs 1 year Baseline (72. 4+10. 5) (72. 4+ 1 year (57. 5+11*) (57. 5+ 2 year (51. 5+9*†) (51. 5+ 500 Left Ventricular Mass *p<0. 05 vs baseline †p<0. 05 vs 1 year 400 gm mm 70 300 200 30 100 Baseline (73+11) (73+ Mazur et al Circ 2001 1 year (59+8. 8*) (59+ 2 year (53+8. 7*†) (53+ Baseline (30+78) (30+ 1 year (223+52*) (223+ 2 year (190+58*†) (190+
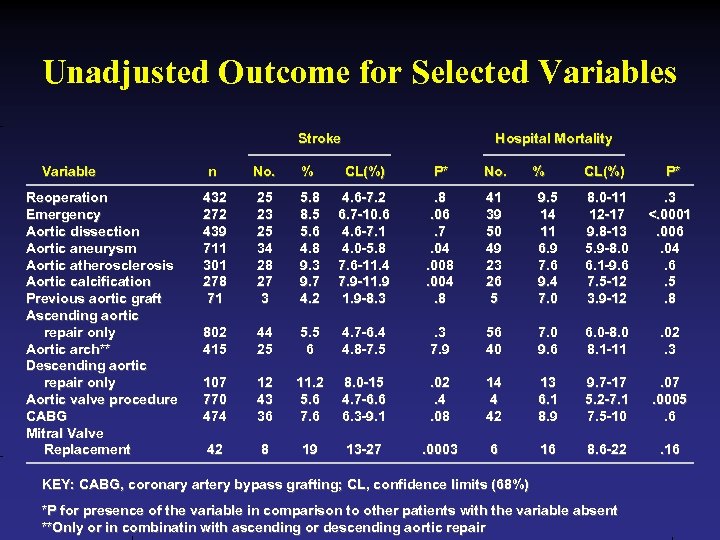 Unadjusted Outcome for Selected Variables Stroke Variable Reoperation Emergency Aortic dissection Aortic aneurysm Aortic atherosclerosis Aortic calcification Previous aortic graft Ascending aortic repair only Aortic arch** Descending aortic repair only Aortic valve procedure CABG Mitral Valve Replacement Hospital Mortality n No. % CL(%) P* No. 432 272 439 711 301 278 71 25 23 25 34 28 27 3 5. 8 8. 5 5. 6 4. 8 9. 3 9. 7 4. 2 4. 6 -7. 2 6. 7 -10. 6 4. 6 -7. 1 4. 0 -5. 8 7. 6 -11. 4 7. 9 -11. 9 -8. 3 . 8. 06. 7. 04. 008. 004. 8 41 39 50 49 23 26 5 802 415 44 25 5. 5 6 4. 7 -6. 4 4. 8 -7. 5 . 3 7. 9 107 770 474 12 43 36 11. 2 5. 6 7. 6 8. 0 -15 4. 7 -6. 6 6. 3 -9. 1 42 8 19 13 -27 % CL(%) P* 9. 5 14 11 6. 9 7. 6 9. 4 7. 0 8. 0 -11 12 -17 9. 8 -13 5. 9 -8. 0 6. 1 -9. 6 7. 5 -12 3. 9 -12 . 3 <. 0001. 006. 04. 6. 5. 8 56 40 7. 0 9. 6 6. 0 -8. 0 8. 1 -11 . 02. 3 . 02. 4. 08 14 4 42 13 6. 1 8. 9 9. 7 -17 5. 2 -7. 1 7. 5 -10 . 07. 0005. 6 . 0003 6 16 8. 6 -22 . 16 KEY: CABG, coronary artery bypass grafting; CL, confidence limits (68%) *P for presence of the variable in comparison to other patients with the variable absent **Only or in combinatin with ascending or descending aortic repair
Unadjusted Outcome for Selected Variables Stroke Variable Reoperation Emergency Aortic dissection Aortic aneurysm Aortic atherosclerosis Aortic calcification Previous aortic graft Ascending aortic repair only Aortic arch** Descending aortic repair only Aortic valve procedure CABG Mitral Valve Replacement Hospital Mortality n No. % CL(%) P* No. 432 272 439 711 301 278 71 25 23 25 34 28 27 3 5. 8 8. 5 5. 6 4. 8 9. 3 9. 7 4. 2 4. 6 -7. 2 6. 7 -10. 6 4. 6 -7. 1 4. 0 -5. 8 7. 6 -11. 4 7. 9 -11. 9 -8. 3 . 8. 06. 7. 04. 008. 004. 8 41 39 50 49 23 26 5 802 415 44 25 5. 5 6 4. 7 -6. 4 4. 8 -7. 5 . 3 7. 9 107 770 474 12 43 36 11. 2 5. 6 7. 6 8. 0 -15 4. 7 -6. 6 6. 3 -9. 1 42 8 19 13 -27 % CL(%) P* 9. 5 14 11 6. 9 7. 6 9. 4 7. 0 8. 0 -11 12 -17 9. 8 -13 5. 9 -8. 0 6. 1 -9. 6 7. 5 -12 3. 9 -12 . 3 <. 0001. 006. 04. 6. 5. 8 56 40 7. 0 9. 6 6. 0 -8. 0 8. 1 -11 . 02. 3 . 02. 4. 08 14 4 42 13 6. 1 8. 9 9. 7 -17 5. 2 -7. 1 7. 5 -10 . 07. 0005. 6 . 0003 6 16 8. 6 -22 . 16 KEY: CABG, coronary artery bypass grafting; CL, confidence limits (68%) *P for presence of the variable in comparison to other patients with the variable absent **Only or in combinatin with ascending or descending aortic repair
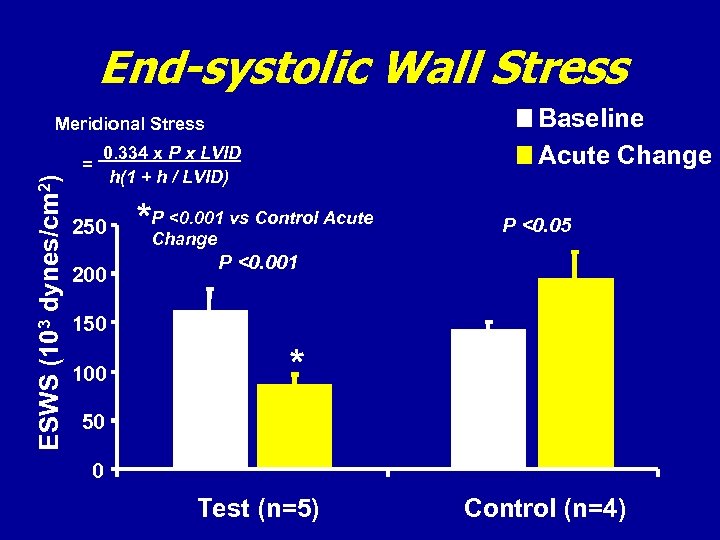 End-systolic Wall Stress Baseline Acute Change Meridional Stress ESWS (103 dynes/cm 2) = 0. 334 x P x LVID h(1 + h / LVID) 250 200 * P <0. 001 vs Control Acute Change P <0. 05 P <0. 001 150 100 * 50 0 Test (n=5) Control (n=4)
End-systolic Wall Stress Baseline Acute Change Meridional Stress ESWS (103 dynes/cm 2) = 0. 334 x P x LVID h(1 + h / LVID) 250 200 * P <0. 001 vs Control Acute Change P <0. 05 P <0. 001 150 100 * 50 0 Test (n=5) Control (n=4)
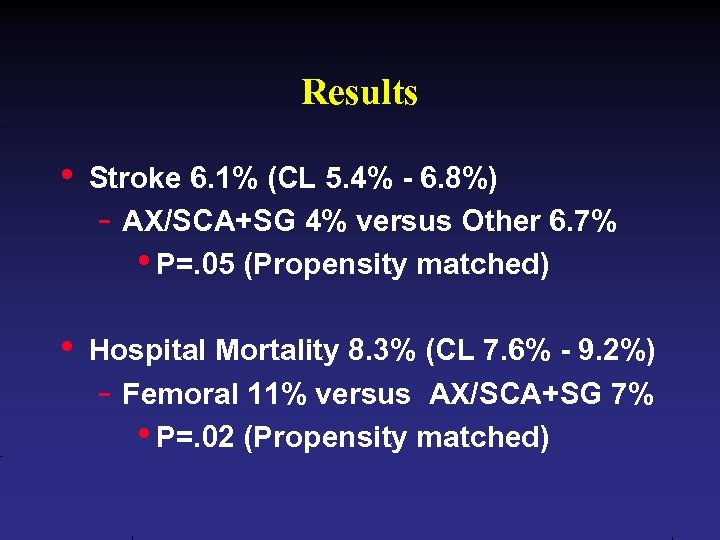 Results • Stroke 6. 1% (CL 5. 4% - 6. 8%) - AX/SCA+SG 4% versus Other 6. 7% • P=. 05 (Propensity matched) • Hospital Mortality 8. 3% (CL 7. 6% - 9. 2%) - Femoral 11% versus AX/SCA+SG 7% • P=. 02 (Propensity matched)
Results • Stroke 6. 1% (CL 5. 4% - 6. 8%) - AX/SCA+SG 4% versus Other 6. 7% • P=. 05 (Propensity matched) • Hospital Mortality 8. 3% (CL 7. 6% - 9. 2%) - Femoral 11% versus AX/SCA+SG 7% • P=. 02 (Propensity matched)
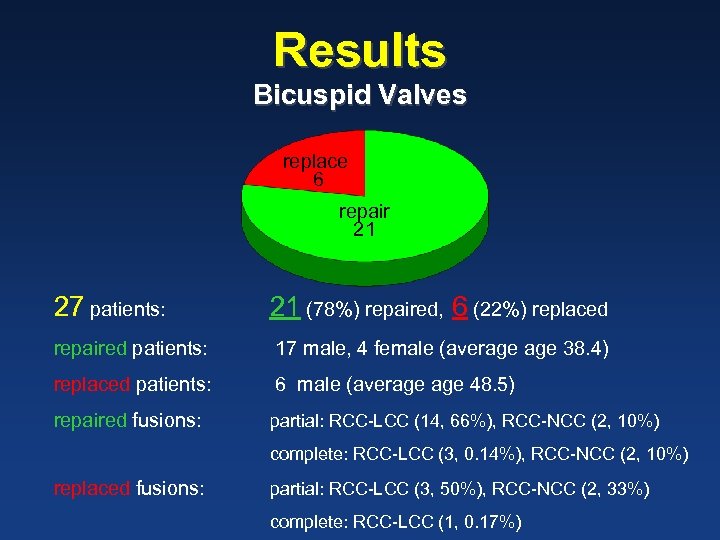 Results Bicuspid Valves replace 6 repair 21 27 patients: 21 (78%) repaired, 6 (22%) replaced repaired patients: 17 male, 4 female (average 38. 4) replaced patients: 6 male (average 48. 5) repaired fusions: partial: RCC-LCC (14, 66%), RCC-NCC (2, 10%) complete: RCC-LCC (3, 0. 14%), RCC-NCC (2, 10%) replaced fusions: partial: RCC-LCC (3, 50%), RCC-NCC (2, 33%) complete: RCC-LCC (1, 0. 17%)
Results Bicuspid Valves replace 6 repair 21 27 patients: 21 (78%) repaired, 6 (22%) replaced repaired patients: 17 male, 4 female (average 38. 4) replaced patients: 6 male (average 48. 5) repaired fusions: partial: RCC-LCC (14, 66%), RCC-NCC (2, 10%) complete: RCC-LCC (3, 0. 14%), RCC-NCC (2, 10%) replaced fusions: partial: RCC-LCC (3, 50%), RCC-NCC (2, 33%) complete: RCC-LCC (1, 0. 17%)
 Can we do better than this?
Can we do better than this?
 Purpose What is the purpose of slides? Are they always needed? Must they be visible all the time?
Purpose What is the purpose of slides? Are they always needed? Must they be visible all the time?
 Purpose Who’s the driver? • The talk? • The slides? • Opinion: Ideas drive the visuals and not the reverse Entertainment? Parallel / supplemental information? Talk to the slides?
Purpose Who’s the driver? • The talk? • The slides? • Opinion: Ideas drive the visuals and not the reverse Entertainment? Parallel / supplemental information? Talk to the slides?
 Color Background / foreground • Give audience a break! • Contrast, but not stark • Easiest on the eyes in dark room is darker background, lighter letters • Reverse for light room Example • Blue background • Yellow and white letters
Color Background / foreground • Give audience a break! • Contrast, but not stark • Easiest on the eyes in dark room is darker background, lighter letters • Reverse for light room Example • Blue background • Yellow and white letters
 Problem Colors Red • Can stand out • Can disappear--unpredictable Pastels • Can be perfect • Can be bland be indistinguishable from white
Problem Colors Red • Can stand out • Can disappear--unpredictable Pastels • Can be perfect • Can be bland be indistinguishable from white
 Background Keep it plain! • No distractions—nothing, absolutely nothing, extraneous on slide • Avoid textured and watermarked backgrounds • If shading used: darker on top, lighter on bottom • Avoid “cute” transitions
Background Keep it plain! • No distractions—nothing, absolutely nothing, extraneous on slide • Avoid textured and watermarked backgrounds • If shading used: darker on top, lighter on bottom • Avoid “cute” transitions
 • Reflective of the scarcity of resource, complexities of donor organ allocation and increased number of patients awaiting cardiac transplantation, is the acuity of those undergoing the procedure. In 1988, 42. 2% of patients undergoing transplant were Status II, waiting at home. In 1994, only 38. 3% were called in from home.
• Reflective of the scarcity of resource, complexities of donor organ allocation and increased number of patients awaiting cardiac transplantation, is the acuity of those undergoing the procedure. In 1988, 42. 2% of patients undergoing transplant were Status II, waiting at home. In 1994, only 38. 3% were called in from home.
 Word Slides Use as few as possible • Simple graphs & simple figures more effective • One thought “package” per slide • Avoid complete sentences & articles
Word Slides Use as few as possible • Simple graphs & simple figures more effective • One thought “package” per slide • Avoid complete sentences & articles
 Word Slides Layout • Avoid multiline titles • 3 or fewer major heads / slide • First level needs no bullet Implications • “One concept per slide” • Fewest possible words • Minimize depth of “indents”
Word Slides Layout • Avoid multiline titles • 3 or fewer major heads / slide • First level needs no bullet Implications • “One concept per slide” • Fewest possible words • Minimize depth of “indents”
 MVRr with LV Reconstruction © © © The combination of LV reconstruction, MV repair, and coronary revascularization provides significant reduction in LV volumes and improvement in LV ejection fraction Sustained for at least 1 year with a cardiac event free survival of 84% at the first year. MV repair, if successful, may prevent LV redilation, as patients with recurrent MR demonstrate increases in LV volumes and less functional improvement Importance of the mitral valve repair in patients with ischemic mitral regurgitation. Further studies are needed to address the causes and effects of recurrent MR in patients with LV reconstruction. Gillinov et. al. Circulation. 2003; 108[suppl II]: II-241 -II-246.
MVRr with LV Reconstruction © © © The combination of LV reconstruction, MV repair, and coronary revascularization provides significant reduction in LV volumes and improvement in LV ejection fraction Sustained for at least 1 year with a cardiac event free survival of 84% at the first year. MV repair, if successful, may prevent LV redilation, as patients with recurrent MR demonstrate increases in LV volumes and less functional improvement Importance of the mitral valve repair in patients with ischemic mitral regurgitation. Further studies are needed to address the causes and effects of recurrent MR in patients with LV reconstruction. Gillinov et. al. Circulation. 2003; 108[suppl II]: II-241 -II-246.
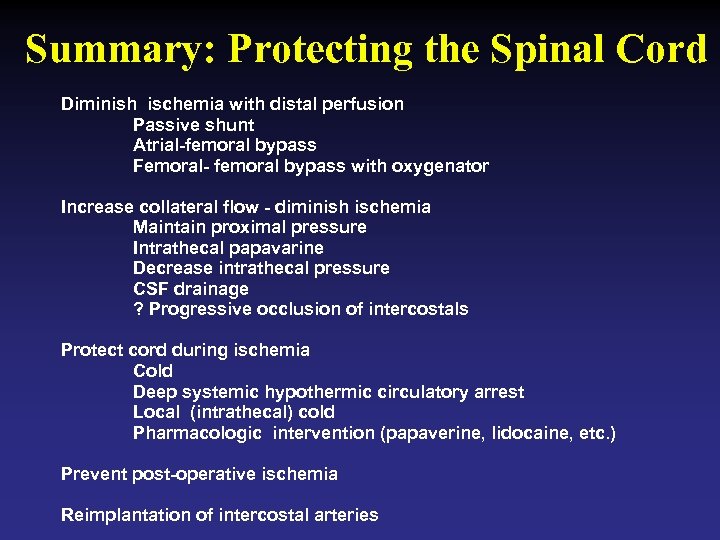 Summary: Protecting the Spinal Cord Diminish ischemia with distal perfusion Passive shunt Atrial-femoral bypass Femoral- femoral bypass with oxygenator Increase collateral flow - diminish ischemia Maintain proximal pressure Intrathecal papavarine Decrease intrathecal pressure CSF drainage ? Progressive occlusion of intercostals Protect cord during ischemia Cold Deep systemic hypothermic circulatory arrest Local (intrathecal) cold Pharmacologic intervention (papaverine, lidocaine, etc. ) Prevent post-operative ischemia Reimplantation of intercostal arteries
Summary: Protecting the Spinal Cord Diminish ischemia with distal perfusion Passive shunt Atrial-femoral bypass Femoral- femoral bypass with oxygenator Increase collateral flow - diminish ischemia Maintain proximal pressure Intrathecal papavarine Decrease intrathecal pressure CSF drainage ? Progressive occlusion of intercostals Protect cord during ischemia Cold Deep systemic hypothermic circulatory arrest Local (intrathecal) cold Pharmacologic intervention (papaverine, lidocaine, etc. ) Prevent post-operative ischemia Reimplantation of intercostal arteries
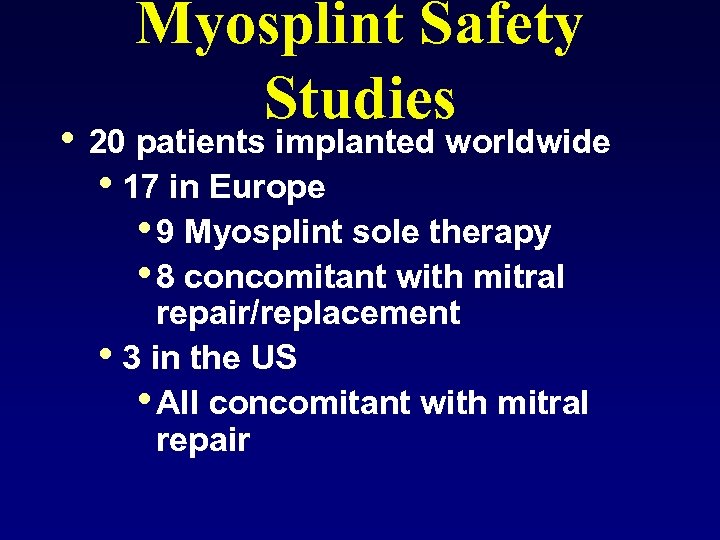 Myosplint Safety Studies • 20 patients implanted worldwide • 17 in Europe • 9 Myosplint sole therapy • 8 concomitant with mitral repair/replacement • 3 in the US • All concomitant with mitral repair
Myosplint Safety Studies • 20 patients implanted worldwide • 17 in Europe • 9 Myosplint sole therapy • 8 concomitant with mitral repair/replacement • 3 in the US • All concomitant with mitral repair
 Word Slides Format • Keep words in same location, even if the slide looks bare! • Avoid centering • Avoid unique spacing from slide to slide Rationale • Minimize work of audience!
Word Slides Format • Keep words in same location, even if the slide looks bare! • Avoid centering • Avoid unique spacing from slide to slide Rationale • Minimize work of audience!
 Example Fungal & non-fungal endocarditis
Example Fungal & non-fungal endocarditis
 Another Later Example Cues • Identify before talking • Keep colors consistent
Another Later Example Cues • Identify before talking • Keep colors consistent
 Example Fungal & non-fungal endocarditis
Example Fungal & non-fungal endocarditis
 Another Later Example Cues • Identify before talking • Keep colors consistent
Another Later Example Cues • Identify before talking • Keep colors consistent
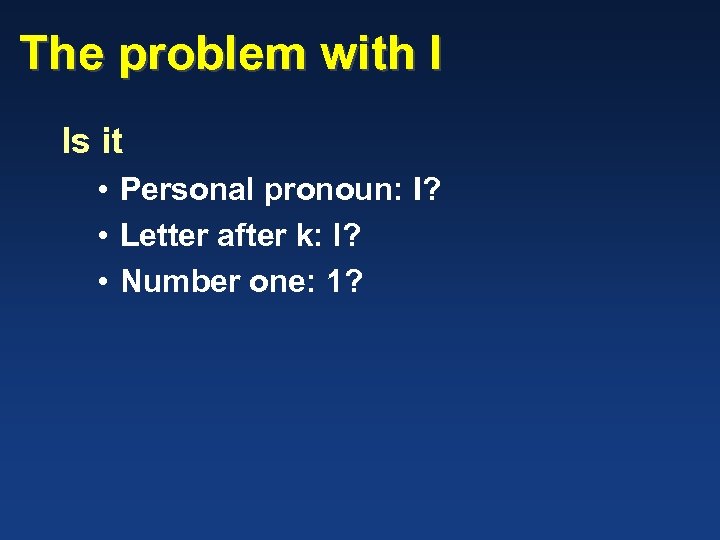
 Word Slides Font • Mixed upper- & lower case most readable • Sans serif • At the moment: Arial Font size • Minimum 32 point A new kid on the block! • Clearview
Word Slides Font • Mixed upper- & lower case most readable • Sans serif • At the moment: Arial Font size • Minimum 32 point A new kid on the block! • Clearview
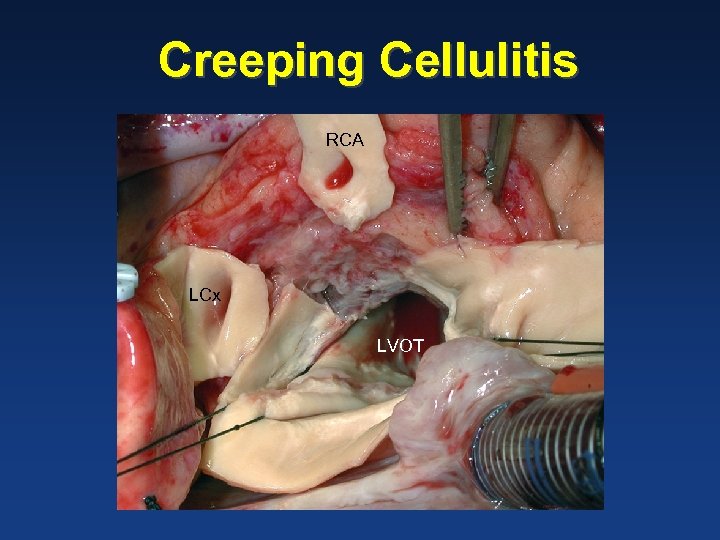 Creeping Cellulitis RCA LCx LVOT
Creeping Cellulitis RCA LCx LVOT
 Creeping Cellulitis RCA LCx LVOT
Creeping Cellulitis RCA LCx LVOT
 The problem with I Is it • Personal pronoun: I? • Letter after k: l? • Number one: 1?
The problem with I Is it • Personal pronoun: I? • Letter after k: l? • Number one: 1?
 Old & New: Clearview
Old & New: Clearview
 Clearview Highway Signs
Clearview Highway Signs
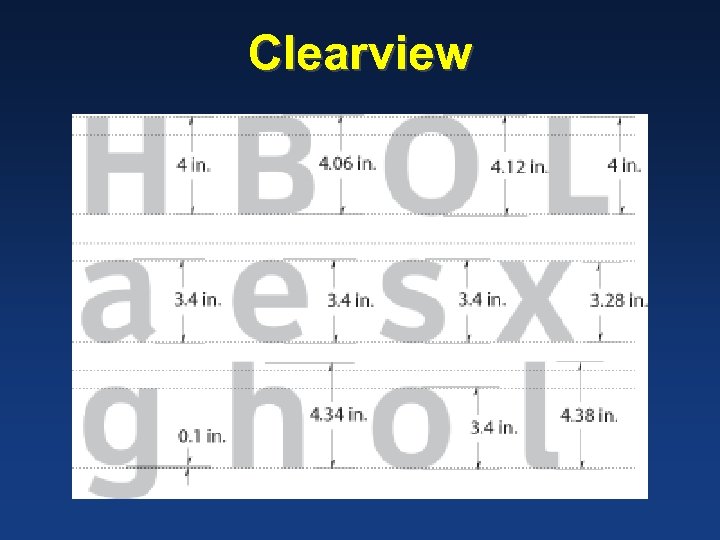 Clearview
Clearview
 Physiologic Approach Minimize • Fewest words • Simplest graphs Visual order • Top to bottom • Left to right • Clockwise
Physiologic Approach Minimize • Fewest words • Simplest graphs Visual order • Top to bottom • Left to right • Clockwise
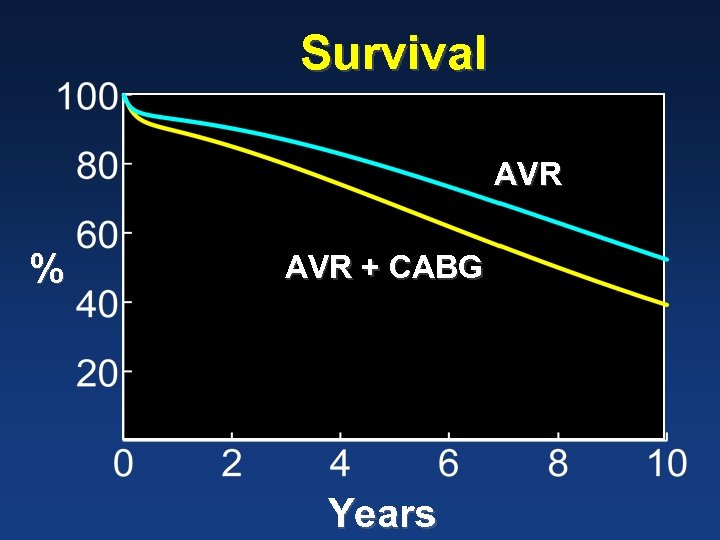 Survival AVR % AVR + CABG Years
Survival AVR % AVR + CABG Years
 Patients 1990 to 2008 n = 2, 277 Left-sided Valve Lesion With Functional TR
Patients 1990 to 2008 n = 2, 277 Left-sided Valve Lesion With Functional TR
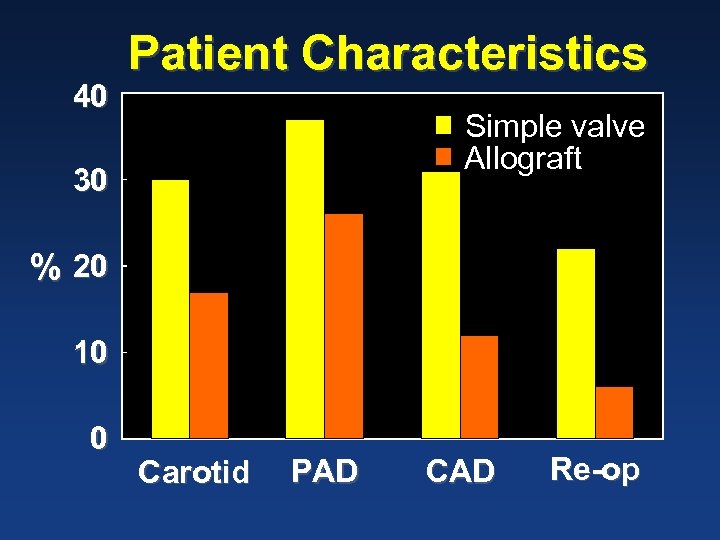 40 Patient Characteristics Simple valve Allograft 30 % 20 10 0 Carotid PAD CAD Re-op
40 Patient Characteristics Simple valve Allograft 30 % 20 10 0 Carotid PAD CAD Re-op
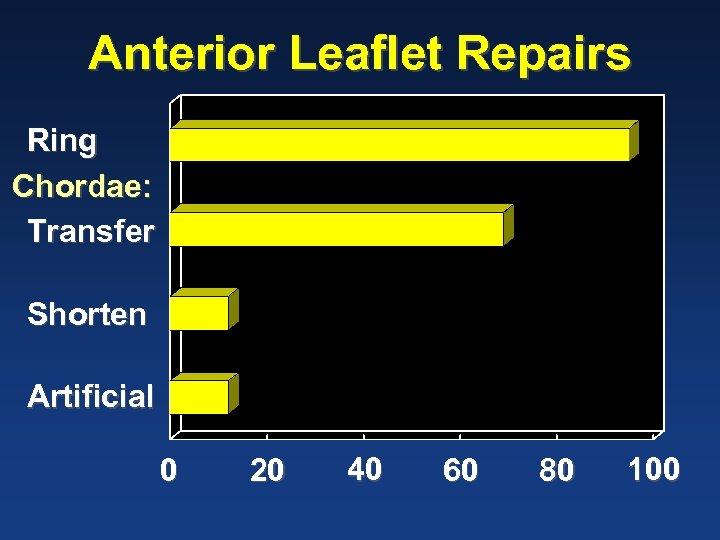 Anterior Leaflet Repairs Ring Chordae: Transfer Shorten Artificial 0 20 40 60 80 100
Anterior Leaflet Repairs Ring Chordae: Transfer Shorten Artificial 0 20 40 60 80 100
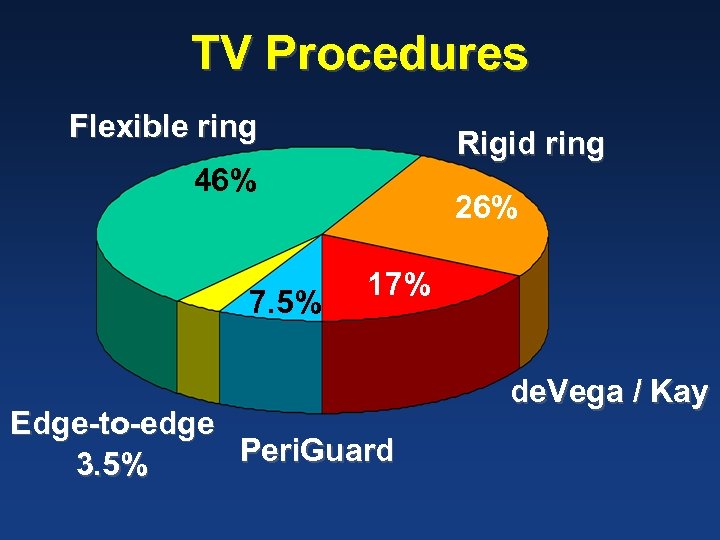 TV Procedures Flexible ring Rigid ring 46% 7. 5% 26% 17% Edge-to-edge Peri. Guard 3. 5% de. Vega / Kay
TV Procedures Flexible ring Rigid ring 46% 7. 5% 26% 17% Edge-to-edge Peri. Guard 3. 5% de. Vega / Kay
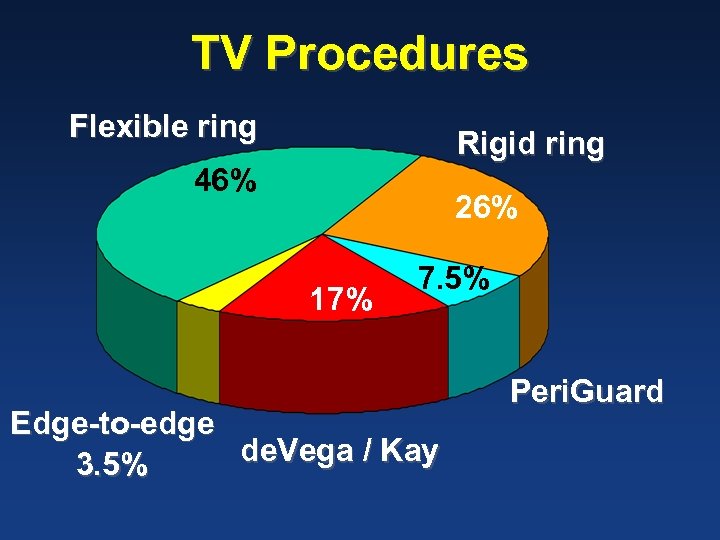 TV Procedures Flexible ring Rigid ring 46% 26% 17% 7. 5% Edge-to-edge de. Vega / Kay 3. 5% Peri. Guard
TV Procedures Flexible ring Rigid ring 46% 26% 17% 7. 5% Edge-to-edge de. Vega / Kay 3. 5% Peri. Guard
 Physiologic Approach Cues • Identify before talking • Keep colors consistent
Physiologic Approach Cues • Identify before talking • Keep colors consistent
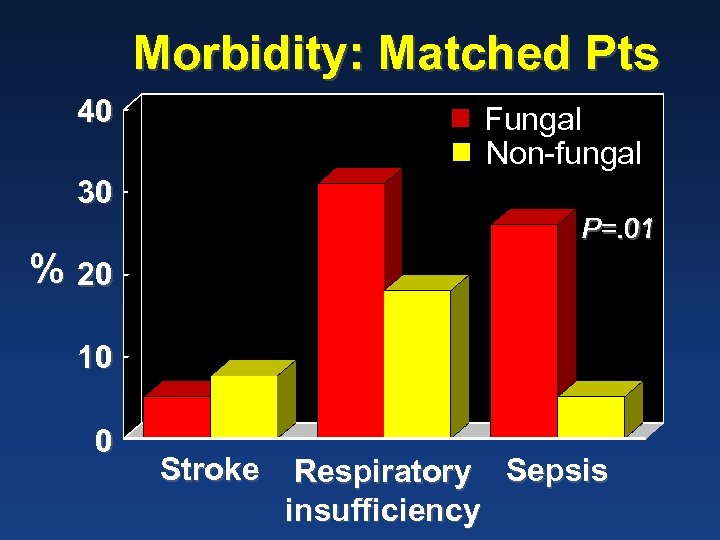 Morbidity: Matched Pts 40 Fungal Non-fungal 30 P=. 01 % 20 10 0 Stroke Respiratory Sepsis insufficiency
Morbidity: Matched Pts 40 Fungal Non-fungal 30 P=. 01 % 20 10 0 Stroke Respiratory Sepsis insufficiency
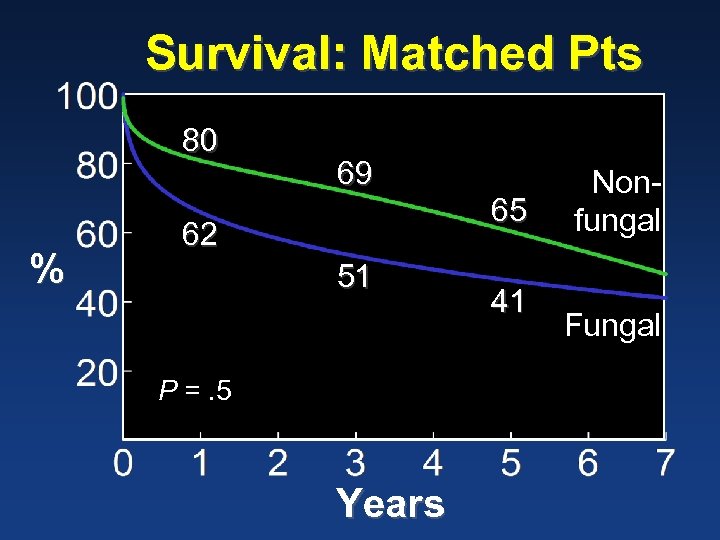 Survival: Matched Pts 80 % 69 62 51 P =. 5 Years 65 41 Nonfungal Fungal
Survival: Matched Pts 80 % 69 62 51 P =. 5 Years 65 41 Nonfungal Fungal
 Physiologic Approach Distractions • Minimize “entertainment” that can obscure message • No jumping slides • Non-obvious title centering
Physiologic Approach Distractions • Minimize “entertainment” that can obscure message • No jumping slides • Non-obvious title centering
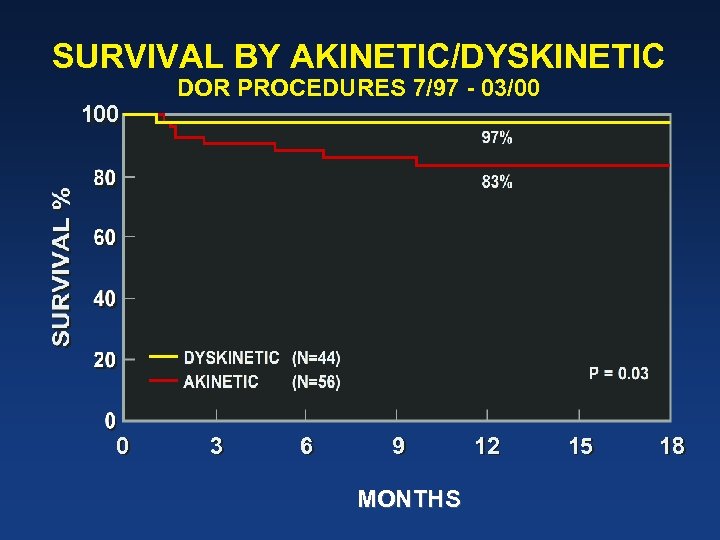 SURVIVAL BY AKINETIC/DYSKINETIC 100 0 DOR PROCEDURES 7/97 - 03/00 3 6 9 MONTHS 12 15 18
SURVIVAL BY AKINETIC/DYSKINETIC 100 0 DOR PROCEDURES 7/97 - 03/00 3 6 9 MONTHS 12 15 18
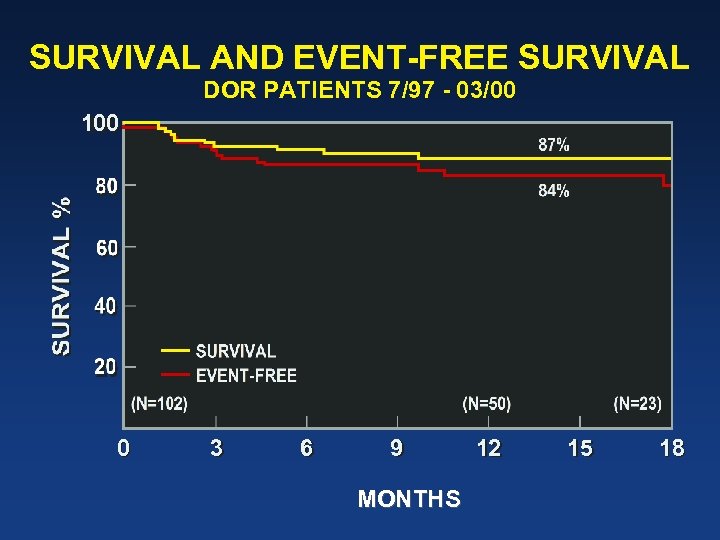 SURVIVAL AND EVENT-FREE SURVIVAL DOR PATIENTS 7/97 - 03/00 100 0 3 6 9 MONTHS 12 15 18
SURVIVAL AND EVENT-FREE SURVIVAL DOR PATIENTS 7/97 - 03/00 100 0 3 6 9 MONTHS 12 15 18
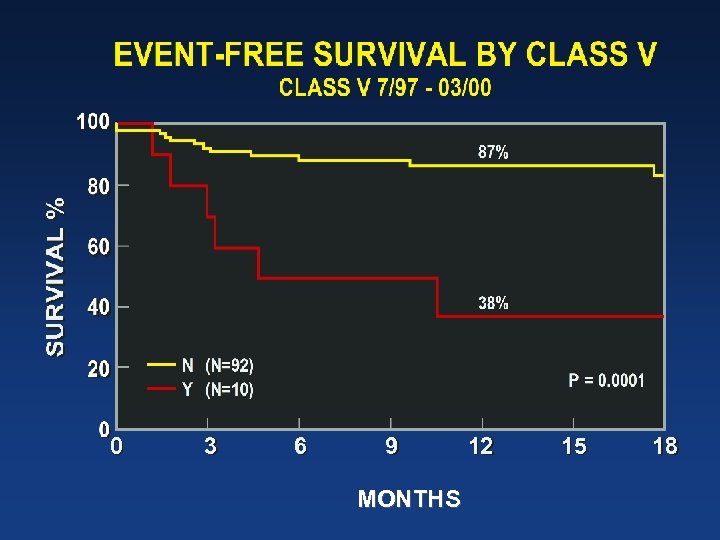 0 3 6 9 MONTHS 12 15 18
0 3 6 9 MONTHS 12 15 18
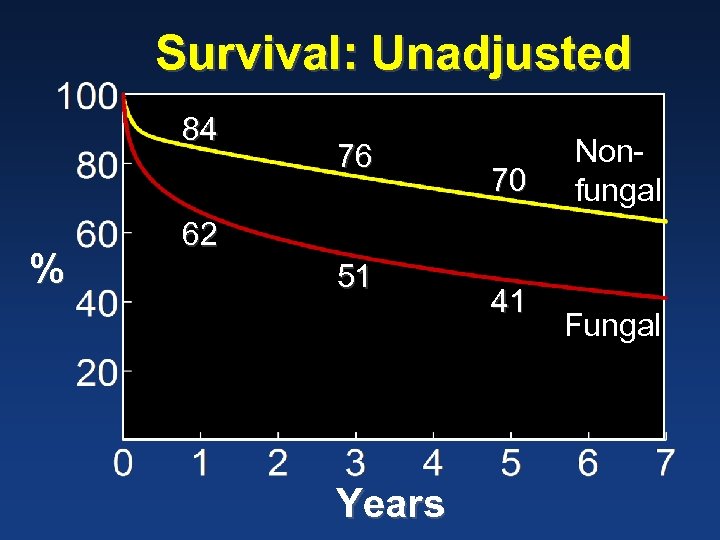 Survival: Unadjusted 84 % 76 70 Nonfungal 62 51 Years 41 Fungal
Survival: Unadjusted 84 % 76 70 Nonfungal 62 51 Years 41 Fungal
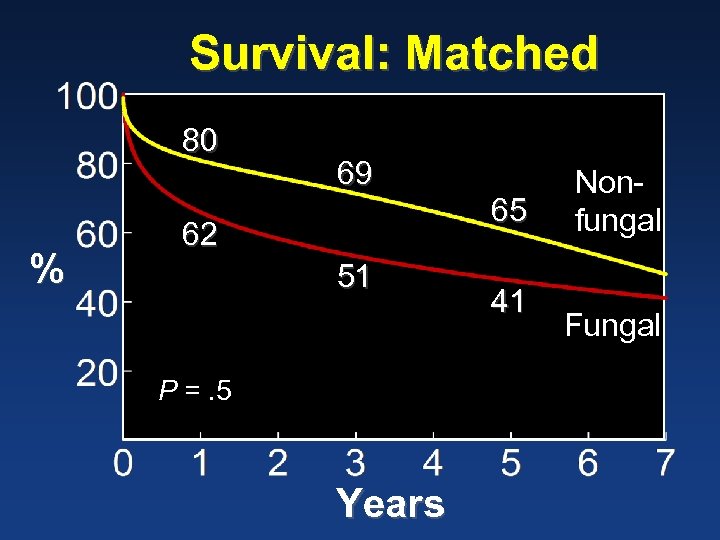 Survival: Matched 80 % 69 62 51 P =. 5 Years 65 41 Nonfungal Fungal
Survival: Matched 80 % 69 62 51 P =. 5 Years 65 41 Nonfungal Fungal
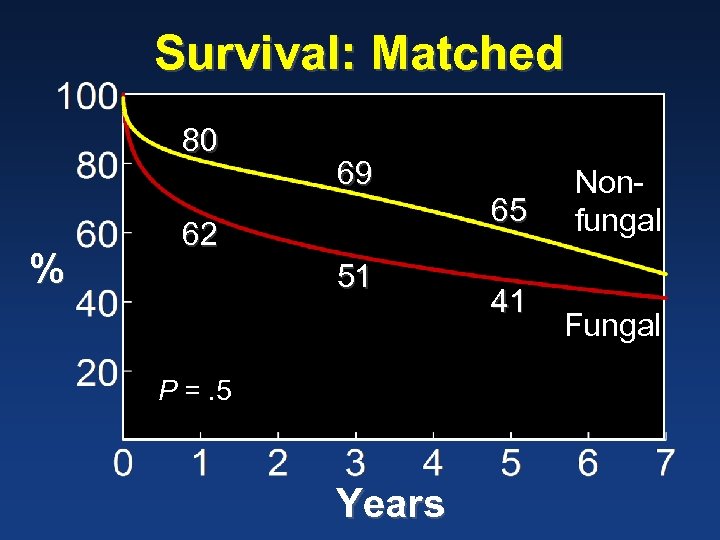 Survival: Matched 80 % 69 62 51 P =. 5 Years 65 41 Nonfungal Fungal
Survival: Matched 80 % 69 62 51 P =. 5 Years 65 41 Nonfungal Fungal
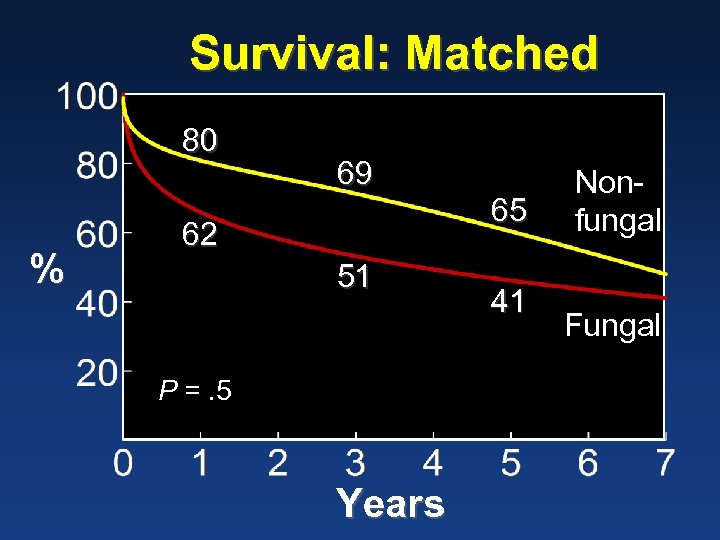 Survival: Matched 80 % 69 62 51 P =. 5 Years 65 41 Nonfungal Fungal
Survival: Matched 80 % 69 62 51 P =. 5 Years 65 41 Nonfungal Fungal
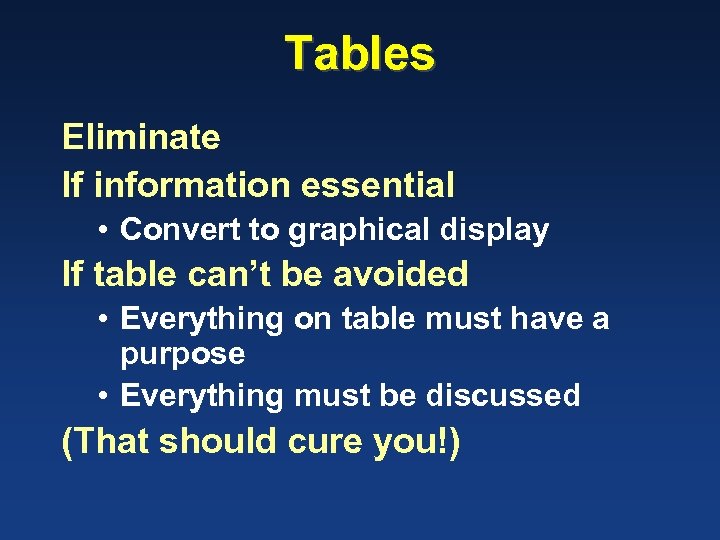 Tables Eliminate If information essential • Convert to graphical display If table can’t be avoided • Everything on table must have a purpose • Everything must be discussed (That should cure you!)
Tables Eliminate If information essential • Convert to graphical display If table can’t be avoided • Everything on table must have a purpose • Everything must be discussed (That should cure you!)
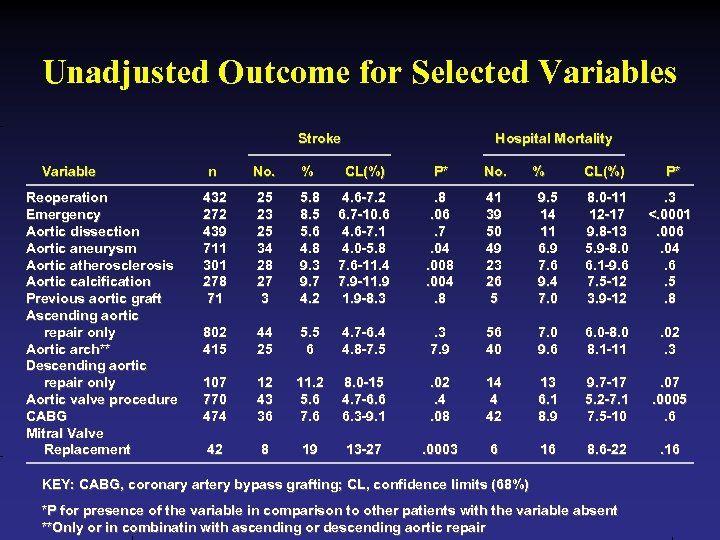 Unadjusted Outcome for Selected Variables Stroke Variable Reoperation Emergency Aortic dissection Aortic aneurysm Aortic atherosclerosis Aortic calcification Previous aortic graft Ascending aortic repair only Aortic arch** Descending aortic repair only Aortic valve procedure CABG Mitral Valve Replacement Hospital Mortality n No. % CL(%) P* No. 432 272 439 711 301 278 71 25 23 25 34 28 27 3 5. 8 8. 5 5. 6 4. 8 9. 3 9. 7 4. 2 4. 6 -7. 2 6. 7 -10. 6 4. 6 -7. 1 4. 0 -5. 8 7. 6 -11. 4 7. 9 -11. 9 -8. 3 . 8. 06. 7. 04. 008. 004. 8 41 39 50 49 23 26 5 802 415 44 25 5. 5 6 4. 7 -6. 4 4. 8 -7. 5 . 3 7. 9 107 770 474 12 43 36 11. 2 5. 6 7. 6 8. 0 -15 4. 7 -6. 6 6. 3 -9. 1 42 8 19 13 -27 % CL(%) P* 9. 5 14 11 6. 9 7. 6 9. 4 7. 0 8. 0 -11 12 -17 9. 8 -13 5. 9 -8. 0 6. 1 -9. 6 7. 5 -12 3. 9 -12 . 3 <. 0001. 006. 04. 6. 5. 8 56 40 7. 0 9. 6 6. 0 -8. 0 8. 1 -11 . 02. 3 . 02. 4. 08 14 4 42 13 6. 1 8. 9 9. 7 -17 5. 2 -7. 1 7. 5 -10 . 07. 0005. 6 . 0003 6 16 8. 6 -22 . 16 KEY: CABG, coronary artery bypass grafting; CL, confidence limits (68%) *P for presence of the variable in comparison to other patients with the variable absent **Only or in combinatin with ascending or descending aortic repair
Unadjusted Outcome for Selected Variables Stroke Variable Reoperation Emergency Aortic dissection Aortic aneurysm Aortic atherosclerosis Aortic calcification Previous aortic graft Ascending aortic repair only Aortic arch** Descending aortic repair only Aortic valve procedure CABG Mitral Valve Replacement Hospital Mortality n No. % CL(%) P* No. 432 272 439 711 301 278 71 25 23 25 34 28 27 3 5. 8 8. 5 5. 6 4. 8 9. 3 9. 7 4. 2 4. 6 -7. 2 6. 7 -10. 6 4. 6 -7. 1 4. 0 -5. 8 7. 6 -11. 4 7. 9 -11. 9 -8. 3 . 8. 06. 7. 04. 008. 004. 8 41 39 50 49 23 26 5 802 415 44 25 5. 5 6 4. 7 -6. 4 4. 8 -7. 5 . 3 7. 9 107 770 474 12 43 36 11. 2 5. 6 7. 6 8. 0 -15 4. 7 -6. 6 6. 3 -9. 1 42 8 19 13 -27 % CL(%) P* 9. 5 14 11 6. 9 7. 6 9. 4 7. 0 8. 0 -11 12 -17 9. 8 -13 5. 9 -8. 0 6. 1 -9. 6 7. 5 -12 3. 9 -12 . 3 <. 0001. 006. 04. 6. 5. 8 56 40 7. 0 9. 6 6. 0 -8. 0 8. 1 -11 . 02. 3 . 02. 4. 08 14 4 42 13 6. 1 8. 9 9. 7 -17 5. 2 -7. 1 7. 5 -10 . 07. 0005. 6 . 0003 6 16 8. 6 -22 . 16 KEY: CABG, coronary artery bypass grafting; CL, confidence limits (68%) *P for presence of the variable in comparison to other patients with the variable absent **Only or in combinatin with ascending or descending aortic repair
 Physiologic Approach Keep it natural • If a slide does not feel right, it probably is not right
Physiologic Approach Keep it natural • If a slide does not feel right, it probably is not right
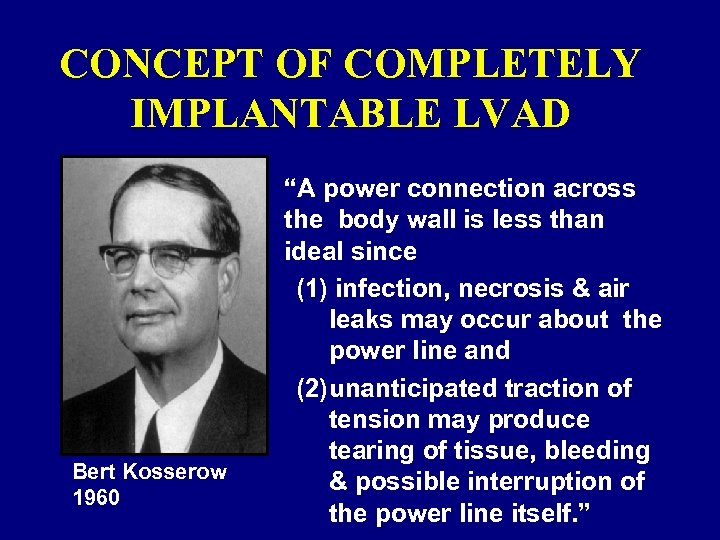 CONCEPT OF COMPLETELY IMPLANTABLE LVAD Bert Kosserow 1960 “A power connection across the body wall is less than ideal since (1) infection, necrosis & air leaks may occur about the power line and (2)unanticipated traction of tension may produce tearing of tissue, bleeding & possible interruption of the power line itself. ”
CONCEPT OF COMPLETELY IMPLANTABLE LVAD Bert Kosserow 1960 “A power connection across the body wall is less than ideal since (1) infection, necrosis & air leaks may occur about the power line and (2)unanticipated traction of tension may produce tearing of tissue, bleeding & possible interruption of the power line itself. ”
 CONCEPT OF COMPLETELY IMPLANTABLE LVAD “A power connection across the body wall is less than ideal since (1) infection, necrosis & air leaks may occur about the power line and (2)unanticipated traction of tension may produce tearing of tissue, bleeding & possible interruption of the power line itself. ” Bert Kosserow 1960
CONCEPT OF COMPLETELY IMPLANTABLE LVAD “A power connection across the body wall is less than ideal since (1) infection, necrosis & air leaks may occur about the power line and (2)unanticipated traction of tension may produce tearing of tissue, bleeding & possible interruption of the power line itself. ” Bert Kosserow 1960
 Delivery
Delivery
 Delivery Memorize? Read? Wing it?
Delivery Memorize? Read? Wing it?
 Cameron Speech Box Used • By presidents from at least Nixon through Clinton
Cameron Speech Box Used • By presidents from at least Nixon through Clinton
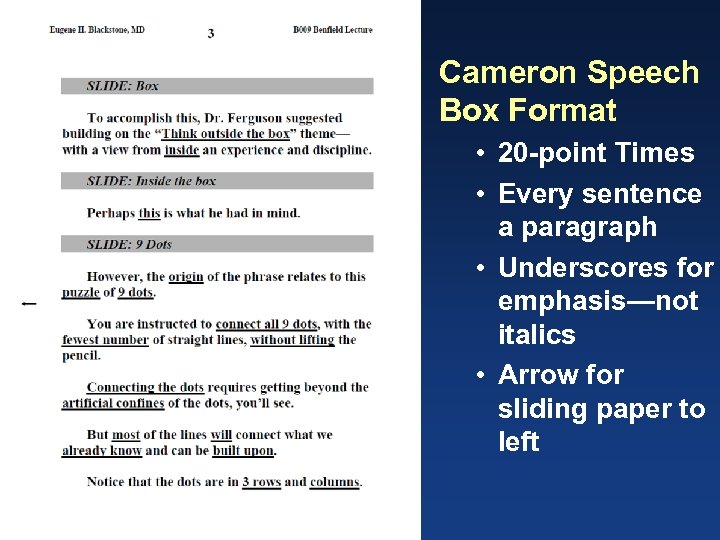 Cameron Speech Box Format • 20 -point Times • Every sentence a paragraph • Underscores for emphasis—not italics • Arrow for sliding paper to left
Cameron Speech Box Format • 20 -point Times • Every sentence a paragraph • Underscores for emphasis—not italics • Arrow for sliding paper to left
 Delivery Let’s practice!
Delivery Let’s practice!
 The Future of Healthcare Delivery A View from Inside and Outside the Box
The Future of Healthcare Delivery A View from Inside and Outside the Box
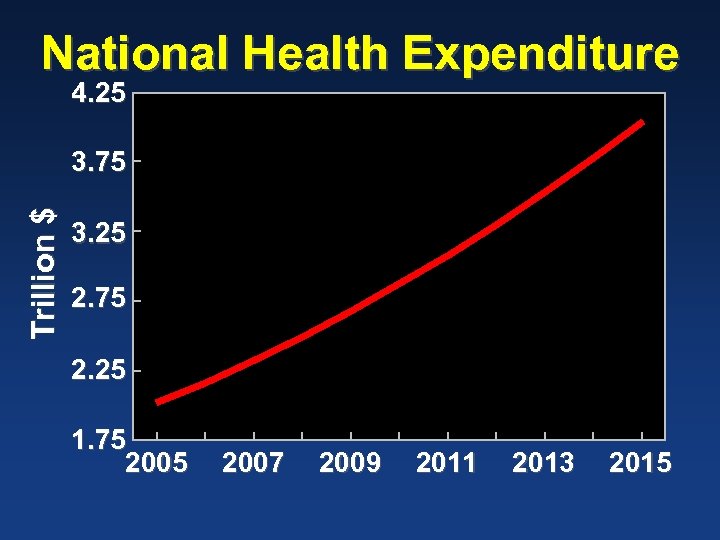 National Health Expenditure 4. 25 Trillion $ 3. 75 3. 25 2. 75 2. 25 1. 75 2007 2009 2011 2013 2015
National Health Expenditure 4. 25 Trillion $ 3. 75 3. 25 2. 75 2. 25 1. 75 2007 2009 2011 2013 2015

 Future of Healthcare Delivery 3 themes… • Importance of data • Importance of analytics • Importance of people …and their potential contribution to the future of healthcare delivery
Future of Healthcare Delivery 3 themes… • Importance of data • Importance of analytics • Importance of people …and their potential contribution to the future of healthcare delivery
 A Christmas Carol “You don't believe in me, ” observed the Ghost. “I don't, ” said Scrooge. “What evidence would you have of my reality beyond that of your senses? ” “I don't know, ” said Scrooge…”
A Christmas Carol “You don't believe in me, ” observed the Ghost. “I don't, ” said Scrooge. “What evidence would you have of my reality beyond that of your senses? ” “I don't know, ” said Scrooge…”
 Lies, D…d Lies, & Statistics
Lies, D…d Lies, & Statistics
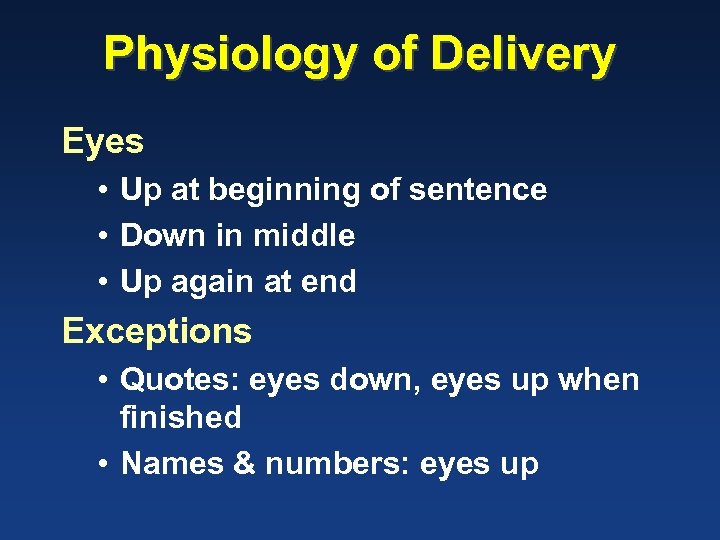 Physiology of Delivery Eyes • Up at beginning of sentence • Down in middle • Up again at end Exceptions • Quotes: eyes down, eyes up when finished • Names & numbers: eyes up
Physiology of Delivery Eyes • Up at beginning of sentence • Down in middle • Up again at end Exceptions • Quotes: eyes down, eyes up when finished • Names & numbers: eyes up
 Q&A With Thanks to Richard Butterfield
Q&A With Thanks to Richard Butterfield
 Q&A Characterize Q & A period you have liked Characterize those you have hated • • What is terrifying? What should you say? What shouldn’t you say? Is there a strategy here? ? ?
Q&A Characterize Q & A period you have liked Characterize those you have hated • • What is terrifying? What should you say? What shouldn’t you say? Is there a strategy here? ? ?
 Q&A Reality, attitude, and opportunity • It is a part of your presentation
Q&A Reality, attitude, and opportunity • It is a part of your presentation
 Dangers Saying too much • Over-elaboration • Wandering off target Flubbing a question • …for which you are unprepared Loosing control • To hostile or aggressive questioning Promissory notes
Dangers Saying too much • Over-elaboration • Wandering off target Flubbing a question • …for which you are unprepared Loosing control • To hostile or aggressive questioning Promissory notes
 Preparation Anticipation • Anticipate and prepare for questions You’re not alone • Get help from knowledgeable source Arm yourself • Against hostility
Preparation Anticipation • Anticipate and prepare for questions You’re not alone • Get help from knowledgeable source Arm yourself • Against hostility
 Mind Set You are not a schoolchild trying to please the teacher! • This is your opportunity to drive home your message — to say what you want to say • Because it comes last, it constitutes the audience’s lasting impression of you
Mind Set You are not a schoolchild trying to please the teacher! • This is your opportunity to drive home your message — to say what you want to say • Because it comes last, it constitutes the audience’s lasting impression of you
 Learn from politicians… What questions do you have for my answers? • You don’t have to answer the question asked • Answer the question they should have asked • Answer most questions with something you have already said — repeat key messages
Learn from politicians… What questions do you have for my answers? • You don’t have to answer the question asked • Answer the question they should have asked • Answer most questions with something you have already said — repeat key messages
 Learn from politicians… What questions do you have for my answers? • • There’s a bigger issue… What may not be apparent here… We have been more interested in… I’d like to return to what’s really important…
Learn from politicians… What questions do you have for my answers? • • There’s a bigger issue… What may not be apparent here… We have been more interested in… I’d like to return to what’s really important…
 You! Confidence • You are the expert • You know what you know • You know what you don’t know Danger • Not knowing what you don’t know!
You! Confidence • You are the expert • You know what you know • You know what you don’t know Danger • Not knowing what you don’t know!
 You! Body language • Open posture • Sparkle a bit! • Pretend audience is your friend not your enemy
You! Body language • Open posture • Sparkle a bit! • Pretend audience is your friend not your enemy
 You! Tone & attitude • Confident • Inspired, informative, interactive • Address questioner at first, then deliver message to audience
You! Tone & attitude • Confident • Inspired, informative, interactive • Address questioner at first, then deliver message to audience
 You! Non-defensive • Deflect the “negative” questioner • Admit limitations • But!!! …drive toward a positive focus on what you have discovered
You! Non-defensive • Deflect the “negative” questioner • Admit limitations • But!!! …drive toward a positive focus on what you have discovered
 You! Golden Rule: Think of others • Don’t waste time • Make the point • Stop — let others ask a question
You! Golden Rule: Think of others • Don’t waste time • Make the point • Stop — let others ask a question
 Caught off Guard! Buy yourself some time • Repeat question • Rephrase question to the way you want to answer it • Pause and think, answer deliberately and honestly • “I don’t have a good answer right now, but…” …transition to message, not a promissory note!
Caught off Guard! Buy yourself some time • Repeat question • Rephrase question to the way you want to answer it • Pause and think, answer deliberately and honestly • “I don’t have a good answer right now, but…” …transition to message, not a promissory note!
 Special Situations Non-questions Hostile questioner There are no questions
Special Situations Non-questions Hostile questioner There are no questions
 The Non-Question Temptation • “Thank you for sharing your experience. ” Instead • Tie it to your message
The Non-Question Temptation • “Thank you for sharing your experience. ” Instead • Tie it to your message
 Hostile Questioner Manage the hostility • Correct clear false statements • Choose non-inflammatory terms: “limitation” not “fatal flaw” • Stay on track with message • No sarcasm — be careful about jokes • Stick to the truth, and nothing but the truth
Hostile Questioner Manage the hostility • Correct clear false statements • Choose non-inflammatory terms: “limitation” not “fatal flaw” • Stay on track with message • No sarcasm — be careful about jokes • Stick to the truth, and nothing but the truth
 No Questions! For shame! • The moderator is unprepared! Opportunity to reinforce message • “You may be wondering…” • “One question I’ve been thinking about…” This approach • Encourages audience to ask questions
No Questions! For shame! • The moderator is unprepared! Opportunity to reinforce message • “You may be wondering…” • “One question I’ve been thinking about…” This approach • Encourages audience to ask questions


