3c3d94fa95886e8a2cff6dae3ceda997.ppt
- Количество слайдов: 51
 A Nurse Managed Computerized Program For Continuous IV Insulin Infusion: JIIP(Jefferson Insulin Infusion Protocol) and Non JIIP. Joan Moshang RN BSN MEd. CDE
A Nurse Managed Computerized Program For Continuous IV Insulin Infusion: JIIP(Jefferson Insulin Infusion Protocol) and Non JIIP. Joan Moshang RN BSN MEd. CDE
 CIII Program Content n Indications for JIIP and NON-JIIP n Physician, Nurse and Pharmacy responsibilities. n Practice Pathway for Titrating JIIP.
CIII Program Content n Indications for JIIP and NON-JIIP n Physician, Nurse and Pharmacy responsibilities. n Practice Pathway for Titrating JIIP.
 Requirements: RN will review the Power. Point presentation. n RN will practice titration guidelines on practice pathway on computer. n RN will complete program quiz with a grade of 100%. n Unit CNS will review quiz results with staff member. n
Requirements: RN will review the Power. Point presentation. n RN will practice titration guidelines on practice pathway on computer. n RN will complete program quiz with a grade of 100%. n Unit CNS will review quiz results with staff member. n
 Introduction n n Uncontrolled hyperglycemia in hospitalized patients results in poor clinical outcomes. IV insulin is the drug of choice for optimal glycemic management in many patients. Safe administration of IV insulin is a complex task. The Jefferson Hospital Insulin Infusion Protocol(JIIP) applies to all adult patients requiring IV insulin but ONLY if the JIIP is ordered.
Introduction n n Uncontrolled hyperglycemia in hospitalized patients results in poor clinical outcomes. IV insulin is the drug of choice for optimal glycemic management in many patients. Safe administration of IV insulin is a complex task. The Jefferson Hospital Insulin Infusion Protocol(JIIP) applies to all adult patients requiring IV insulin but ONLY if the JIIP is ordered.
 General Guidelines n Physicians who do not order the JIIP but want continuous IV insulin infusion (NONJIIP) for their patients, are responsible for the hourly titration of the infusion and specific fluid orders. n The RN may titrate a non –JIIP infusion based on previous infusion guidelines online but only if the glucose and piggyback protocol is followed.
General Guidelines n Physicians who do not order the JIIP but want continuous IV insulin infusion (NONJIIP) for their patients, are responsible for the hourly titration of the infusion and specific fluid orders. n The RN may titrate a non –JIIP infusion based on previous infusion guidelines online but only if the glucose and piggyback protocol is followed.
 SO…. n JIIP is a Jefferson Hospital nurse managed protocol for delivering continuous IV insulin. n Non JIIP Continuous IV insulin infusion orders are titrated hourly by the ordering physician and must comply with the glucose and piggyback guidelines. n RN may not hang an insulin infusion that is not piggybacked into another IV.
SO…. n JIIP is a Jefferson Hospital nurse managed protocol for delivering continuous IV insulin. n Non JIIP Continuous IV insulin infusion orders are titrated hourly by the ordering physician and must comply with the glucose and piggyback guidelines. n RN may not hang an insulin infusion that is not piggybacked into another IV.
 JIIP Candidates § ICU patients with BG>180 mg/dl x 2 consecutive measurements. n NOTE: Check Blood glucose (BG) on admission to ICU and q 4 hours thereafter. If BG <140 mg/dl for first 24 hours, measure BG daily or as clinically indicated.
JIIP Candidates § ICU patients with BG>180 mg/dl x 2 consecutive measurements. n NOTE: Check Blood glucose (BG) on admission to ICU and q 4 hours thereafter. If BG <140 mg/dl for first 24 hours, measure BG daily or as clinically indicated.
 JIIP Candidates n. All other patients with BG >250 mg/dl x 2 consecutive readings after initial oral diabetes medications or insulin therapy have failed. n. All DKA (Diabetic Ketoacidosis) or /HHS (Hyperosmolar Hyperglycemic State)-See separate guidelines for management of DKA and HHS.
JIIP Candidates n. All other patients with BG >250 mg/dl x 2 consecutive readings after initial oral diabetes medications or insulin therapy have failed. n. All DKA (Diabetic Ketoacidosis) or /HHS (Hyperosmolar Hyperglycemic State)-See separate guidelines for management of DKA and HHS.
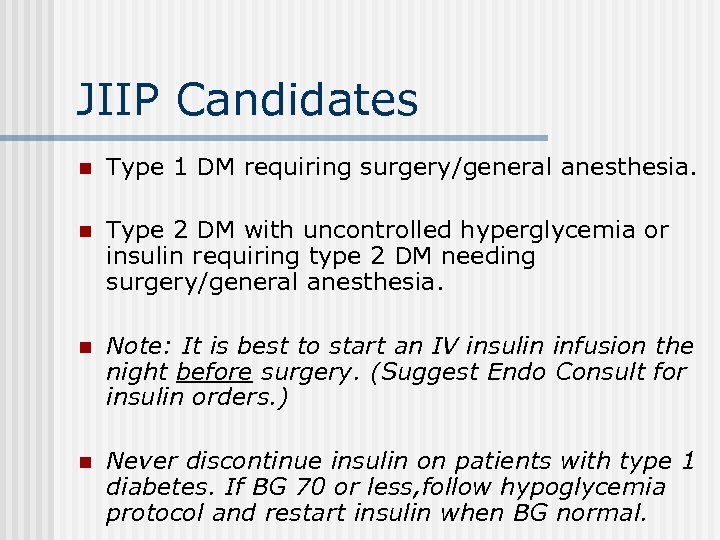 JIIP Candidates n Type 1 DM requiring surgery/general anesthesia. n Type 2 DM with uncontrolled hyperglycemia or insulin requiring type 2 DM needing surgery/general anesthesia. n Note: It is best to start an IV insulin infusion the night before surgery. (Suggest Endo Consult for insulin orders. ) n Never discontinue insulin on patients with type 1 diabetes. If BG 70 or less, follow hypoglycemia protocol and restart insulin when BG normal.
JIIP Candidates n Type 1 DM requiring surgery/general anesthesia. n Type 2 DM with uncontrolled hyperglycemia or insulin requiring type 2 DM needing surgery/general anesthesia. n Note: It is best to start an IV insulin infusion the night before surgery. (Suggest Endo Consult for insulin orders. ) n Never discontinue insulin on patients with type 1 diabetes. If BG 70 or less, follow hypoglycemia protocol and restart insulin when BG normal.
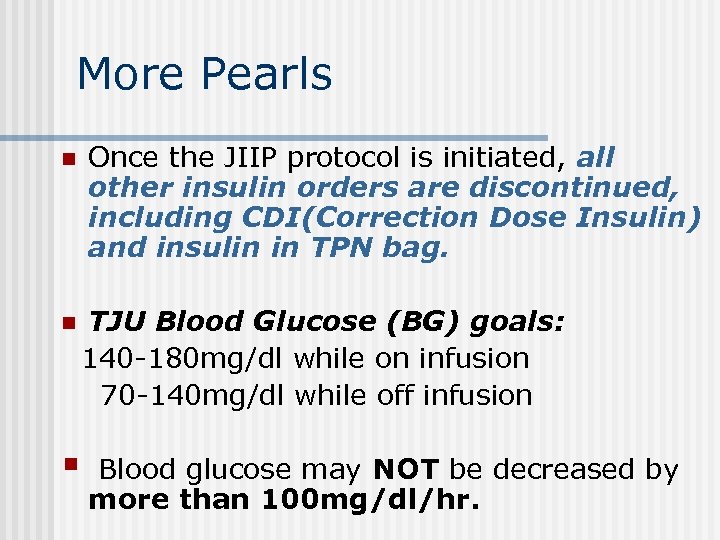 More Pearls n n § Once the JIIP protocol is initiated, all other insulin orders are discontinued, including CDI(Correction Dose Insulin) and insulin in TPN bag. TJU Blood Glucose (BG) goals: 140 -180 mg/dl while on infusion 70 -140 mg/dl while off infusion Blood glucose may NOT be decreased by more than 100 mg/dl/hr.
More Pearls n n § Once the JIIP protocol is initiated, all other insulin orders are discontinued, including CDI(Correction Dose Insulin) and insulin in TPN bag. TJU Blood Glucose (BG) goals: 140 -180 mg/dl while on infusion 70 -140 mg/dl while off infusion Blood glucose may NOT be decreased by more than 100 mg/dl/hr.
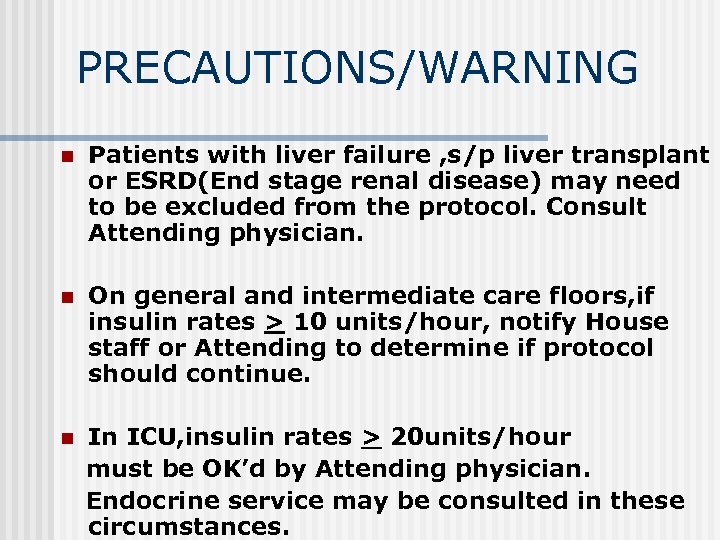 PRECAUTIONS/WARNING n Patients with liver failure , s/p liver transplant or ESRD(End stage renal disease) may need to be excluded from the protocol. Consult Attending physician. n On general and intermediate care floors, if insulin rates > 10 units/hour, notify House staff or Attending to determine if protocol should continue. n In ICU, insulin rates > 20 units/hour must be OK’d by Attending physician. Endocrine service may be consulted in these circumstances.
PRECAUTIONS/WARNING n Patients with liver failure , s/p liver transplant or ESRD(End stage renal disease) may need to be excluded from the protocol. Consult Attending physician. n On general and intermediate care floors, if insulin rates > 10 units/hour, notify House staff or Attending to determine if protocol should continue. n In ICU, insulin rates > 20 units/hour must be OK’d by Attending physician. Endocrine service may be consulted in these circumstances.
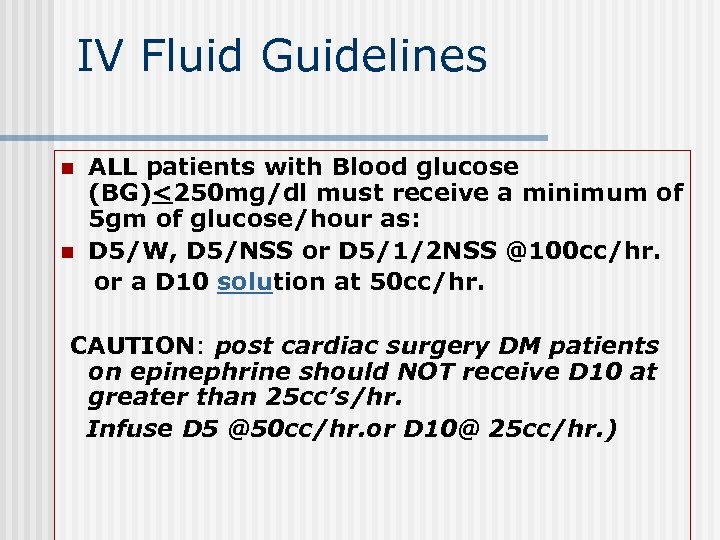 IV Fluid Guidelines n n ALL patients with Blood glucose (BG)<250 mg/dl must receive a minimum of 5 gm of glucose/hour as: D 5/W, D 5/NSS or D 5/1/2 NSS @100 cc/hr. or a D 10 solution at 50 cc/hr. CAUTION: post cardiac surgery DM patients on epinephrine should NOT receive D 10 at greater than 25 cc’s/hr. Infuse D 5 @50 cc/hr. or D 10@ 25 cc/hr. )
IV Fluid Guidelines n n ALL patients with Blood glucose (BG)<250 mg/dl must receive a minimum of 5 gm of glucose/hour as: D 5/W, D 5/NSS or D 5/1/2 NSS @100 cc/hr. or a D 10 solution at 50 cc/hr. CAUTION: post cardiac surgery DM patients on epinephrine should NOT receive D 10 at greater than 25 cc’s/hr. Infuse D 5 @50 cc/hr. or D 10@ 25 cc/hr. )
 RULE OF THUMB Patients with BG <250 mg/dl NOT receiving a source of dextrose/glucose cannot be on the JIIP. Attending physician must be notified for further instruction.
RULE OF THUMB Patients with BG <250 mg/dl NOT receiving a source of dextrose/glucose cannot be on the JIIP. Attending physician must be notified for further instruction.
 Rationale n The inclusion of D 5/W piggyback solution is a safety factor designed to avoid hypoglycemic events. n All Continuous Intravenous Insulin Infusions (CIII )MUST be piggybacked into another IV solution. n Normal saline or D 5/W at a “Keep open” rate is acceptable only if the patient is receiving tube feedings providing a minimum of 120 grams carbohydrates/day.
Rationale n The inclusion of D 5/W piggyback solution is a safety factor designed to avoid hypoglycemic events. n All Continuous Intravenous Insulin Infusions (CIII )MUST be piggybacked into another IV solution. n Normal saline or D 5/W at a “Keep open” rate is acceptable only if the patient is receiving tube feedings providing a minimum of 120 grams carbohydrates/day.
 Key Points n Continuous IV insulin infusions (CIII) are either JIIP or NON-JIIP. § Infusion rates >than 10 units/hr on general floors and >20 units/hr in ICU’s must be OK’d by physician. § Insulin infusions MUST be piggybacked into another appropriate solution.
Key Points n Continuous IV insulin infusions (CIII) are either JIIP or NON-JIIP. § Infusion rates >than 10 units/hr on general floors and >20 units/hr in ICU’s must be OK’d by physician. § Insulin infusions MUST be piggybacked into another appropriate solution.
 Physician Responsibilities q Physician enters order for JIIP and orders the bolus dose and the initial infusion rate as follows: Ø Non DKA/HHS ex: (Pre-surgery, uncontrolled hyperglycemia, NPO post surgery etc. ) Ø Divide initial BG by 100 and round to nearest 0. 1 unit. (Ex: Current BG 200 divided by 100=2 units bolus and 2 units/hr. )
Physician Responsibilities q Physician enters order for JIIP and orders the bolus dose and the initial infusion rate as follows: Ø Non DKA/HHS ex: (Pre-surgery, uncontrolled hyperglycemia, NPO post surgery etc. ) Ø Divide initial BG by 100 and round to nearest 0. 1 unit. (Ex: Current BG 200 divided by 100=2 units bolus and 2 units/hr. )
 Physician Responsibilities q DKA/HHS Ø Calculate dose as 0. 1 units/kg (Ex: Weight in Kg. = 50 Kg x 0. 1=5 Units bolus and 5 units/hr. ) Note difference between bolus and initial start rate of DKA/HHS AND NON DKA/HHS.
Physician Responsibilities q DKA/HHS Ø Calculate dose as 0. 1 units/kg (Ex: Weight in Kg. = 50 Kg x 0. 1=5 Units bolus and 5 units/hr. ) Note difference between bolus and initial start rate of DKA/HHS AND NON DKA/HHS.
 DKA/HHS(HHNK) n In addition to ordering the different bolus and initial infusion start rates for DKA/HHS, the physician must refer to DKA/HHS guidelines for BOH(Beta hydroxybuterate), anion gap, Potassium and fluid guidelines. n Once the bolus and initial infusion rates are administered, both DKA and NON-DKA are titrated by the RN according to the JIIP table.
DKA/HHS(HHNK) n In addition to ordering the different bolus and initial infusion start rates for DKA/HHS, the physician must refer to DKA/HHS guidelines for BOH(Beta hydroxybuterate), anion gap, Potassium and fluid guidelines. n Once the bolus and initial infusion rates are administered, both DKA and NON-DKA are titrated by the RN according to the JIIP table.
 DKA/HHS cont. n Patients in DKA on JIIP or Non JIIP with ketones present must remain on the infusion until their ketones are normalized, even if the BG is normal. Check the BOH(beta hydroxybuterate) and/or anion gap and the DKA guidelines. n (Must maintain insulin rate at minimum of 0. 02 units/kg/hr. Ex: 70 kg pt. x 0. 02=1. 4 units/hr. )in patients with DKA/HHS
DKA/HHS cont. n Patients in DKA on JIIP or Non JIIP with ketones present must remain on the infusion until their ketones are normalized, even if the BG is normal. Check the BOH(beta hydroxybuterate) and/or anion gap and the DKA guidelines. n (Must maintain insulin rate at minimum of 0. 02 units/kg/hr. Ex: 70 kg pt. x 0. 02=1. 4 units/hr. )in patients with DKA/HHS
 For DKA/HHS Drip Titration: a. If Insulin Rate calculation less than 0. 02 unit/kg/hr there is a pop up warning stating: b. The calculated rate is less than 0. 02 unit/kg/hr and a potentially suboptimal low insulin infusion rate. Please call physician to determine the appropriate amount of Dextrose IV. c. If BG less than 250, there is a pop up stating: Recommend IV fluids D 5 at 150 - 250 cc/hr
For DKA/HHS Drip Titration: a. If Insulin Rate calculation less than 0. 02 unit/kg/hr there is a pop up warning stating: b. The calculated rate is less than 0. 02 unit/kg/hr and a potentially suboptimal low insulin infusion rate. Please call physician to determine the appropriate amount of Dextrose IV. c. If BG less than 250, there is a pop up stating: Recommend IV fluids D 5 at 150 - 250 cc/hr
 DKA/HHS(HHNK) Patients in DKA with a normal or near normal BG …but still spilling ketones …will require a higher hourly rate of glucose to allow for continued insulin administration. Call physician for order change. Rationale n The Blood glucose is usually corrected before the ketones are cleared. Premature discontinuation of the insulin infusion will cause a rebound effect.
DKA/HHS(HHNK) Patients in DKA with a normal or near normal BG …but still spilling ketones …will require a higher hourly rate of glucose to allow for continued insulin administration. Call physician for order change. Rationale n The Blood glucose is usually corrected before the ketones are cleared. Premature discontinuation of the insulin infusion will cause a rebound effect.
 Caution! n n Note: although the physician is responsible for entering the correct order set, the RN must recognize the difference between DKA and non-DKA management guidelines for safe patient care. When communicating with the physician, always state if patient has type 1 or type 2 DM.
Caution! n n Note: although the physician is responsible for entering the correct order set, the RN must recognize the difference between DKA and non-DKA management guidelines for safe patient care. When communicating with the physician, always state if patient has type 1 or type 2 DM.
 FYI: Physician Order Sets n Include “pop ups” for DKA/HHS management including Potassium and fluid guidelines. n Multiple “pop up” reminders for monitoring, transition to subcutaneous insulin etc.
FYI: Physician Order Sets n Include “pop ups” for DKA/HHS management including Potassium and fluid guidelines. n Multiple “pop up” reminders for monitoring, transition to subcutaneous insulin etc.
 Pharmacy’s Responsibility n Pharmacy prepares and labels the infusion: 100 Units regular insulin in 100 cc’s NSS. n Pharmacy prepares and labels the bolus dose ordered by physician: -If not DKA/HHS, Initial BG divided by 100 and rounded to nearest 0. 1 unit. -If DKA/HHS, 0. 1 unit/kg.
Pharmacy’s Responsibility n Pharmacy prepares and labels the infusion: 100 Units regular insulin in 100 cc’s NSS. n Pharmacy prepares and labels the bolus dose ordered by physician: -If not DKA/HHS, Initial BG divided by 100 and rounded to nearest 0. 1 unit. -If DKA/HHS, 0. 1 unit/kg.
 Nursing’s Responsibilities 2 RN’s view the order and verify the label and rate changes. n RN flushes IV line with 20 cc of infusion to saturate insulin binding sites in tubing. n 2 RNs administer the IV bolus and initiate the infusion at rate ordered by physician. n 2 RNs titrates infusion as determined by calculations on insulin table. n
Nursing’s Responsibilities 2 RN’s view the order and verify the label and rate changes. n RN flushes IV line with 20 cc of infusion to saturate insulin binding sites in tubing. n 2 RNs administer the IV bolus and initiate the infusion at rate ordered by physician. n 2 RNs titrates infusion as determined by calculations on insulin table. n
 No protocol trumps clinical decision making. The RN must be vigilant in: --assessing patient for nutritional changes, -meds which can increase or decrease BG values, fever , etc. -Reason for infusion. DKA, Surgery, uncontrolled hyperglycemia? (the bolus and start rate depend on the reason why the infusion was initiated).
No protocol trumps clinical decision making. The RN must be vigilant in: --assessing patient for nutritional changes, -meds which can increase or decrease BG values, fever , etc. -Reason for infusion. DKA, Surgery, uncontrolled hyperglycemia? (the bolus and start rate depend on the reason why the infusion was initiated).
 Insulin Rate Adjustment table You must use the computer table to calculate rate changes. n A practice pathway will be available on each unit. n The table addresses rate change only. n For safe patient management, you must be aware of changes such as NPO status, steroid induction, clogged feeding tubes etc. n
Insulin Rate Adjustment table You must use the computer table to calculate rate changes. n A practice pathway will be available on each unit. n The table addresses rate change only. n For safe patient management, you must be aware of changes such as NPO status, steroid induction, clogged feeding tubes etc. n
 IN A NUTSHELL: Physician places order. n Pharmacy prepares fluids and bolus dose. n 2 RN’s check order which includes bolus and initial infusion rate. n RN administers bolus and starts infusion and enters current BG. n
IN A NUTSHELL: Physician places order. n Pharmacy prepares fluids and bolus dose. n 2 RN’s check order which includes bolus and initial infusion rate. n RN administers bolus and starts infusion and enters current BG. n
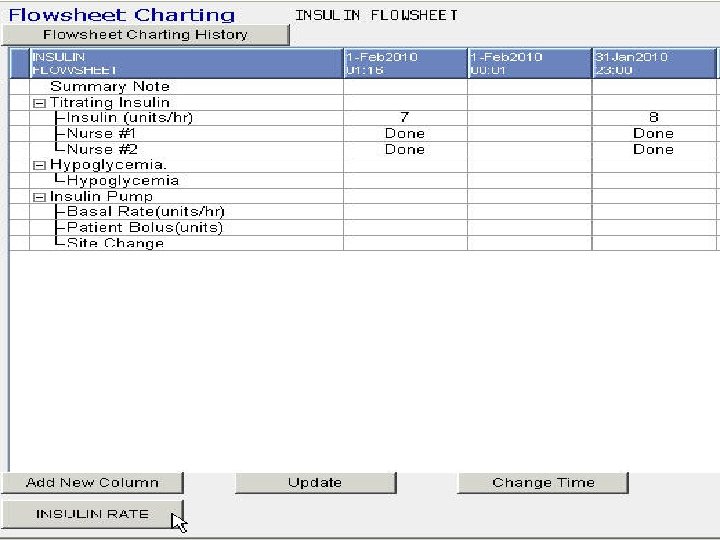
 RN n Rechecks BG in one hour, enters current BG on MAR and based on current and previous BG results:
RN n Rechecks BG in one hour, enters current BG on MAR and based on current and previous BG results:
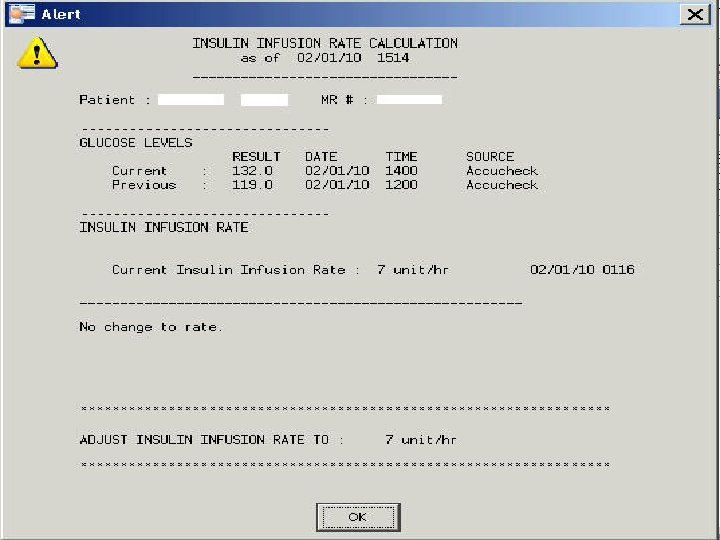
 nclicks on insulin rate tab (Bottom left of screen) and titrates according to the rate calculated by titration table.
nclicks on insulin rate tab (Bottom left of screen) and titrates according to the rate calculated by titration table.
 HOW’d THEY DO THIS? ? n Endocrine reviewed multiple adjustment guidelines. n Inserted multiple case scenarios and developed titration table. n Following are examples of how the titration units were determined. . n (For information only): You will not see this on the viewer)
HOW’d THEY DO THIS? ? n Endocrine reviewed multiple adjustment guidelines. n Inserted multiple case scenarios and developed titration table. n Following are examples of how the titration units were determined. . n (For information only): You will not see this on the viewer)
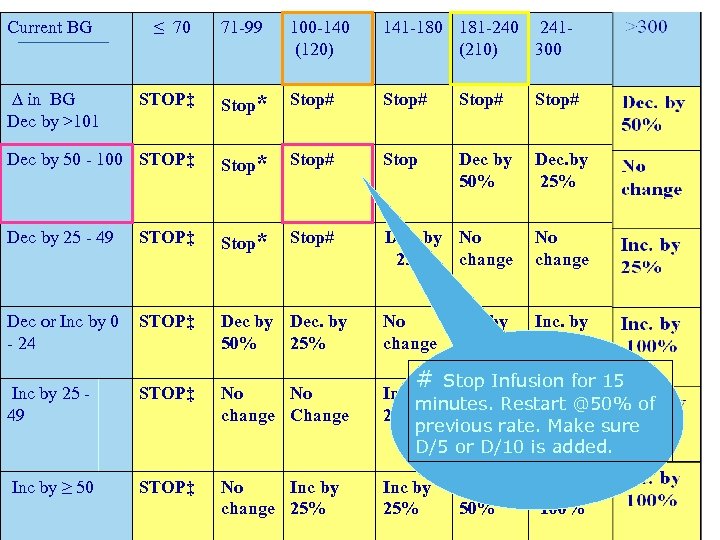 Current BG ≤ 70 71 -99 100 -140 (120) 141 -180 181 -240 241(210) 300 STOP‡ Stop* Stop# Dec by 50 - 100 STOP‡ Stop* Stop# Stop Dec by 50% Dec. by 25% Dec by 25 - 49 STOP‡ Stop* Stop# Dec. by No 25% change No change Dec or Inc by 0 - 24 STOP‡ Dec by Dec. by 50% 25% No change Inc. by 50% Inc by 25 49 STOP‡ No No change Change # Stop by Inc. for 15 Infusion Inc by minutes. Restart @50% of 25% 50% previous rate. Make sure D/5 or D/10 is added. Inc by ≥ 50 STOP‡ No Inc by change 25% Inc by 25% ∆ in BG Dec by >101 Inc by 25% Inc by 50% Inc. by 100%
Current BG ≤ 70 71 -99 100 -140 (120) 141 -180 181 -240 241(210) 300 STOP‡ Stop* Stop# Dec by 50 - 100 STOP‡ Stop* Stop# Stop Dec by 50% Dec. by 25% Dec by 25 - 49 STOP‡ Stop* Stop# Dec. by No 25% change No change Dec or Inc by 0 - 24 STOP‡ Dec by Dec. by 50% 25% No change Inc. by 50% Inc by 25 49 STOP‡ No No change Change # Stop by Inc. for 15 Infusion Inc by minutes. Restart @50% of 25% 50% previous rate. Make sure D/5 or D/10 is added. Inc by ≥ 50 STOP‡ No Inc by change 25% Inc by 25% ∆ in BG Dec by >101 Inc by 25% Inc by 50% Inc. by 100%
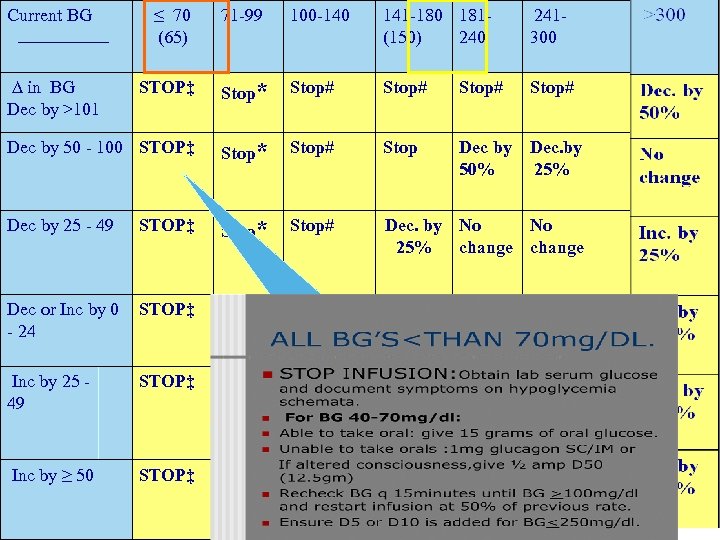 Current BG ≤ 70 (65) 71 -99 100 -140 141 -180 181(150) 240 241300 STOP‡ Stop* Stop# Dec by 50 - 100 STOP‡ Stop* Stop# Stop Dec by 50% Dec. by 25% Dec by 25 - 49 STOP‡ Stop* Stop# Dec. by No No 25% change Dec or Inc by 0 - 24 STOP‡ Dec by Dec. by 50% 25% No change Inc by 25% Inc. by 50% Inc by 25 49 STOP‡ No No change Change Inc by 25% Inc. by 50% Inc by ≥ 50 STOP‡ No Inc by change 25% Inc by 50% Inc. by 100% ∆ in BG Dec by >101
Current BG ≤ 70 (65) 71 -99 100 -140 141 -180 181(150) 240 241300 STOP‡ Stop* Stop# Dec by 50 - 100 STOP‡ Stop* Stop# Stop Dec by 50% Dec. by 25% Dec by 25 - 49 STOP‡ Stop* Stop# Dec. by No No 25% change Dec or Inc by 0 - 24 STOP‡ Dec by Dec. by 50% 25% No change Inc by 25% Inc. by 50% Inc by 25 49 STOP‡ No No change Change Inc by 25% Inc. by 50% Inc by ≥ 50 STOP‡ No Inc by change 25% Inc by 50% Inc. by 100% ∆ in BG Dec by >101
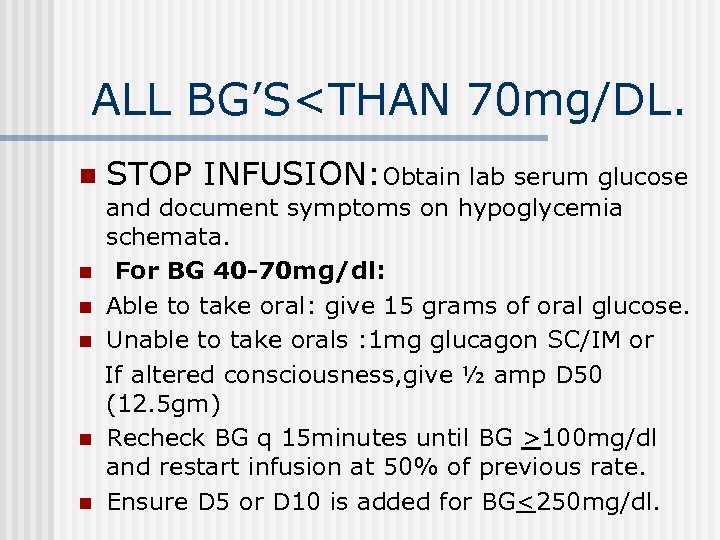 ALL BG’S
ALL BG’S
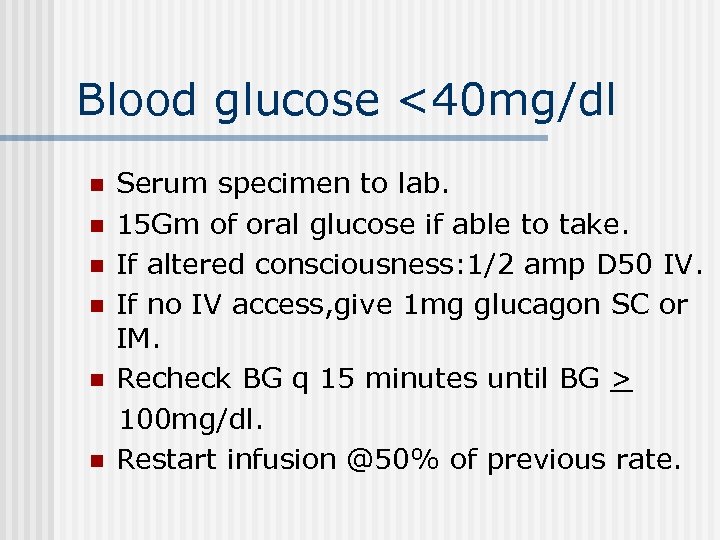 Blood glucose <40 mg/dl n n n Serum specimen to lab. 15 Gm of oral glucose if able to take. If altered consciousness: 1/2 amp D 50 IV. If no IV access, give 1 mg glucagon SC or IM. Recheck BG q 15 minutes until BG > 100 mg/dl. Restart infusion @50% of previous rate.
Blood glucose <40 mg/dl n n n Serum specimen to lab. 15 Gm of oral glucose if able to take. If altered consciousness: 1/2 amp D 50 IV. If no IV access, give 1 mg glucagon SC or IM. Recheck BG q 15 minutes until BG > 100 mg/dl. Restart infusion @50% of previous rate.
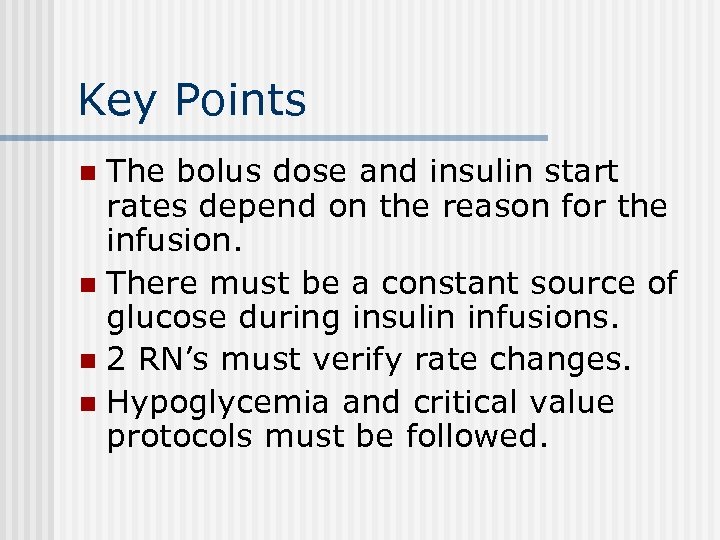 Key Points The bolus dose and insulin start rates depend on the reason for the infusion. n There must be a constant source of glucose during insulin infusions. n 2 RN’s must verify rate changes. n Hypoglycemia and critical value protocols must be followed. n
Key Points The bolus dose and insulin start rates depend on the reason for the infusion. n There must be a constant source of glucose during insulin infusions. n 2 RN’s must verify rate changes. n Hypoglycemia and critical value protocols must be followed. n
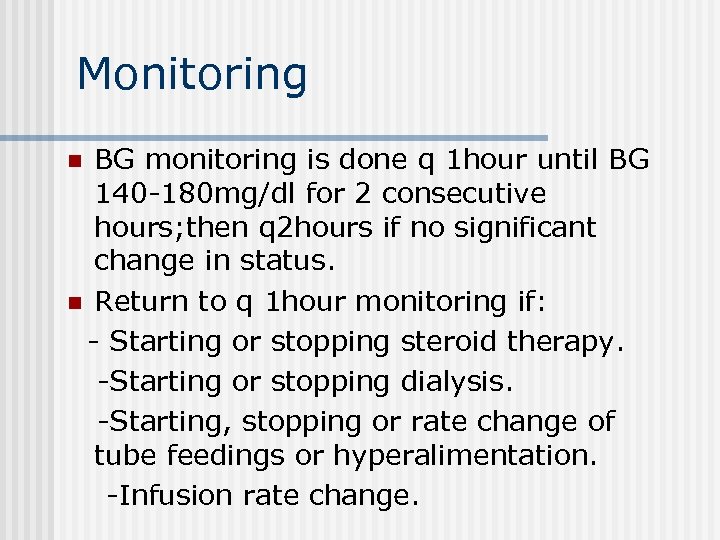 Monitoring BG monitoring is done q 1 hour until BG 140 -180 mg/dl for 2 consecutive hours; then q 2 hours if no significant change in status. n Return to q 1 hour monitoring if: - Starting or stopping steroid therapy. -Starting or stopping dialysis. -Starting, stopping or rate change of tube feedings or hyperalimentation. -Infusion rate change. n
Monitoring BG monitoring is done q 1 hour until BG 140 -180 mg/dl for 2 consecutive hours; then q 2 hours if no significant change in status. n Return to q 1 hour monitoring if: - Starting or stopping steroid therapy. -Starting or stopping dialysis. -Starting, stopping or rate change of tube feedings or hyperalimentation. -Infusion rate change. n
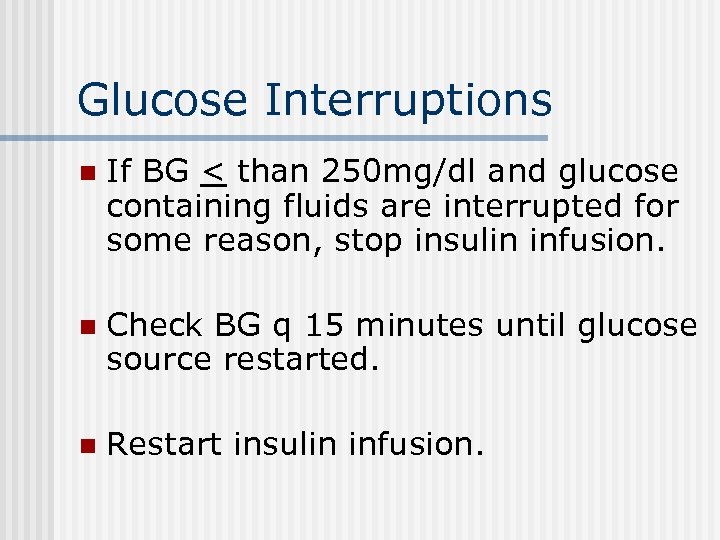 Glucose Interruptions n If BG < than 250 mg/dl and glucose containing fluids are interrupted for some reason, stop insulin infusion. n Check BG q 15 minutes until glucose source restarted. n Restart insulin infusion.
Glucose Interruptions n If BG < than 250 mg/dl and glucose containing fluids are interrupted for some reason, stop insulin infusion. n Check BG q 15 minutes until glucose source restarted. n Restart insulin infusion.
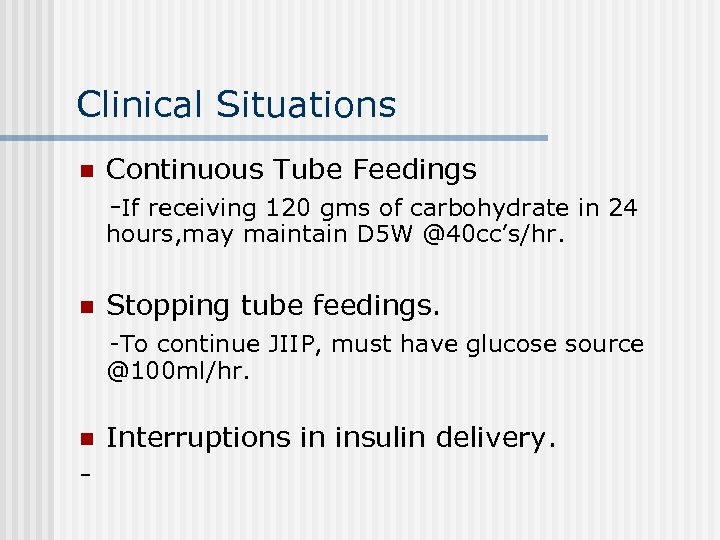 Clinical Situations n Continuous Tube Feedings -If receiving 120 gms of carbohydrate in 24 hours, may maintain D 5 W @40 cc’s/hr. n Stopping tube feedings. -To continue JIIP, must have glucose source @100 ml/hr. n - Interruptions in insulin delivery.
Clinical Situations n Continuous Tube Feedings -If receiving 120 gms of carbohydrate in 24 hours, may maintain D 5 W @40 cc’s/hr. n Stopping tube feedings. -To continue JIIP, must have glucose source @100 ml/hr. n - Interruptions in insulin delivery.
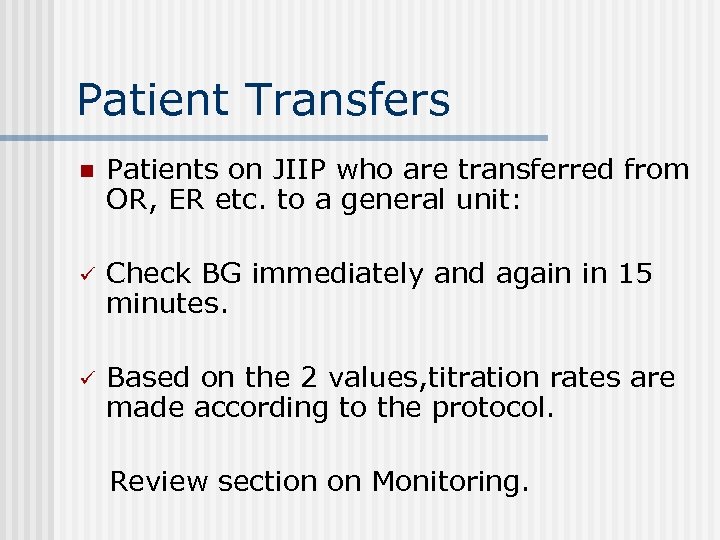 Patient Transfers n Patients on JIIP who are transferred from OR, ER etc. to a general unit: ü Check BG immediately and again in 15 minutes. ü Based on the 2 values, titration rates are made according to the protocol. Review section on Monitoring.
Patient Transfers n Patients on JIIP who are transferred from OR, ER etc. to a general unit: ü Check BG immediately and again in 15 minutes. ü Based on the 2 values, titration rates are made according to the protocol. Review section on Monitoring.
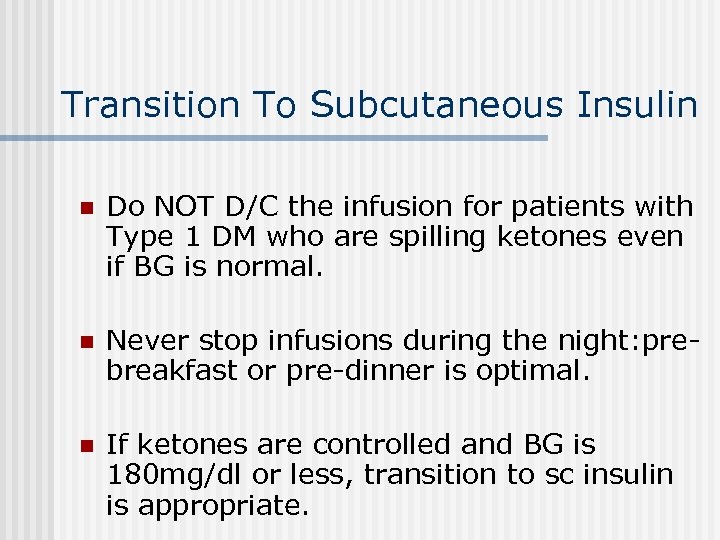 Transition To Subcutaneous Insulin n Do NOT D/C the infusion for patients with Type 1 DM who are spilling ketones even if BG is normal. n Never stop infusions during the night: prebreakfast or pre-dinner is optimal. n If ketones are controlled and BG is 180 mg/dl or less, transition to sc insulin is appropriate.
Transition To Subcutaneous Insulin n Do NOT D/C the infusion for patients with Type 1 DM who are spilling ketones even if BG is normal. n Never stop infusions during the night: prebreakfast or pre-dinner is optimal. n If ketones are controlled and BG is 180 mg/dl or less, transition to sc insulin is appropriate.
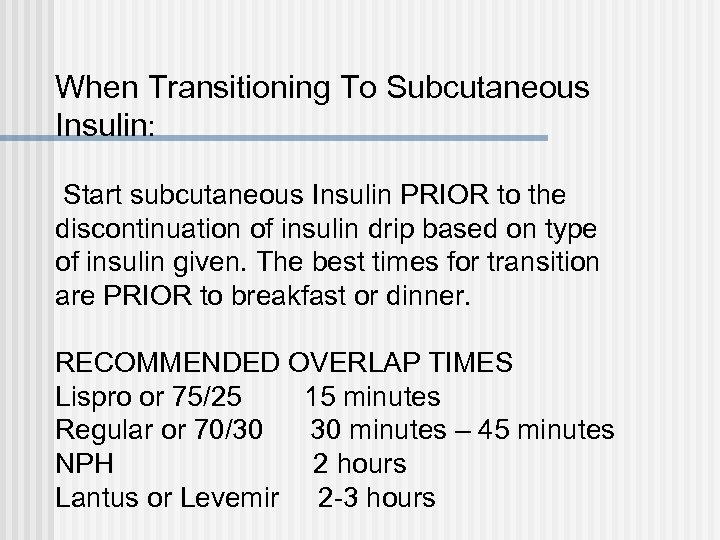 When Transitioning To Subcutaneous Insulin: Start subcutaneous Insulin PRIOR to the discontinuation of insulin drip based on type of insulin given. The best times for transition are PRIOR to breakfast or dinner. RECOMMENDED OVERLAP TIMES Lispro or 75/25 15 minutes Regular or 70/30 30 minutes – 45 minutes NPH 2 hours Lantus or Levemir 2 -3 hours
When Transitioning To Subcutaneous Insulin: Start subcutaneous Insulin PRIOR to the discontinuation of insulin drip based on type of insulin given. The best times for transition are PRIOR to breakfast or dinner. RECOMMENDED OVERLAP TIMES Lispro or 75/25 15 minutes Regular or 70/30 30 minutes – 45 minutes NPH 2 hours Lantus or Levemir 2 -3 hours
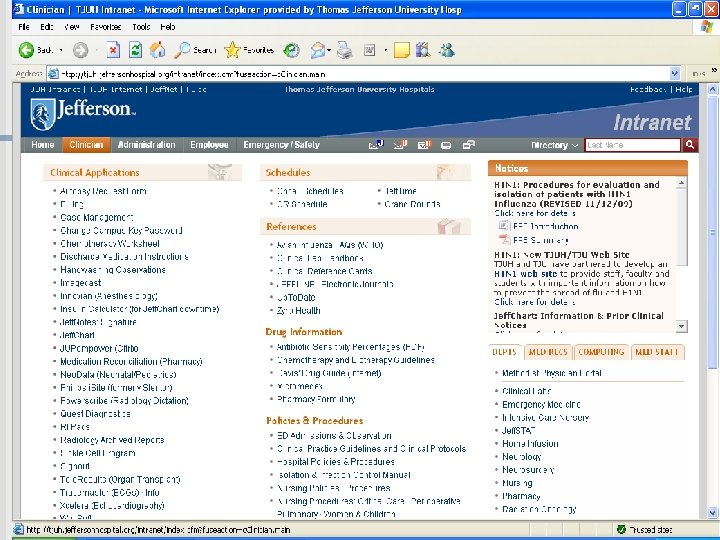
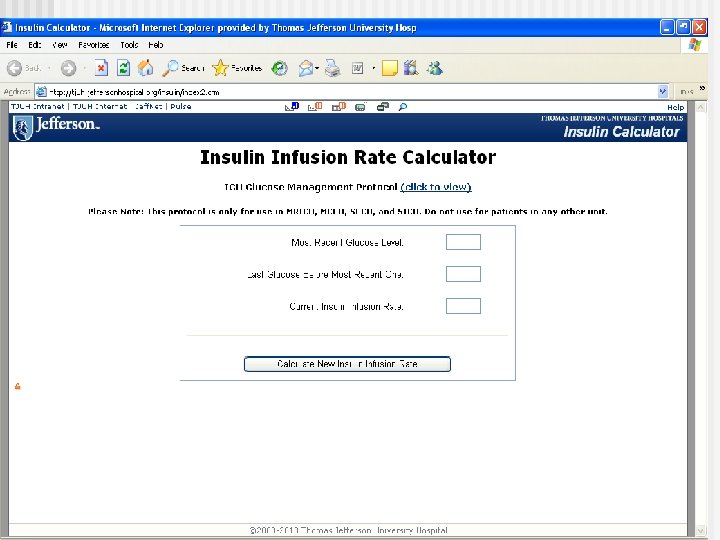
 Computer downtime n Click on clinician on Intranet. n Under clinical applications, scroll down to: n Insulin calculator for Jeff chart downtime. Note: Actual calculator will be updated to reflect use on all care units-not only Intensive care units.
Computer downtime n Click on clinician on Intranet. n Under clinical applications, scroll down to: n Insulin calculator for Jeff chart downtime. Note: Actual calculator will be updated to reflect use on all care units-not only Intensive care units.
 Proceed to quiz if you are able to: State the rationale and indications for continuous insulin infusions. n State the bolus and insulin start rate for DKA/HHS vs. Non-DKA/HHS. § Utilize titration table correctly. § Manage hypoglycemic events per protocol. § State transition times from insulin infusion to subcutaneous insulin based on type of insulin ordered. n
Proceed to quiz if you are able to: State the rationale and indications for continuous insulin infusions. n State the bolus and insulin start rate for DKA/HHS vs. Non-DKA/HHS. § Utilize titration table correctly. § Manage hypoglycemic events per protocol. § State transition times from insulin infusion to subcutaneous insulin based on type of insulin ordered. n
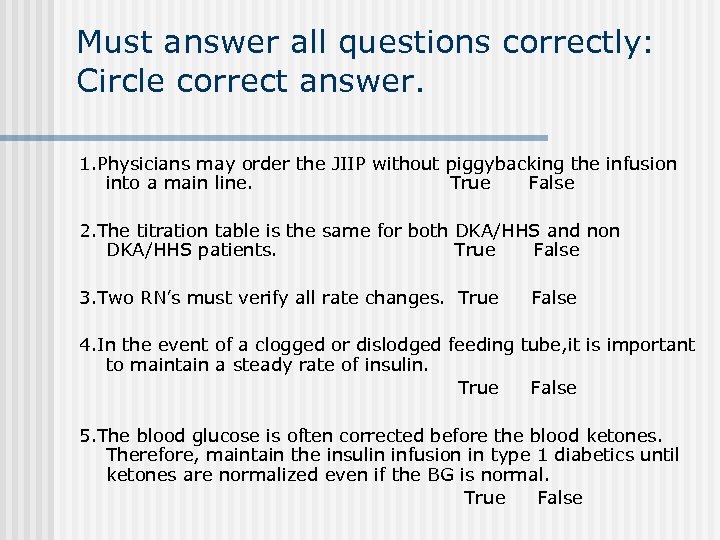 Must answer all questions correctly: Circle correct answer. 1. Physicians may order the JIIP without piggybacking the infusion into a main line. True False 2. The titration table is the same for both DKA/HHS and non DKA/HHS patients. True False 3. Two RN’s must verify all rate changes. True False 4. In the event of a clogged or dislodged feeding tube, it is important to maintain a steady rate of insulin. True False 5. The blood glucose is often corrected before the blood ketones. Therefore, maintain the insulin infusion in type 1 diabetics until ketones are normalized even if the BG is normal. True False
Must answer all questions correctly: Circle correct answer. 1. Physicians may order the JIIP without piggybacking the infusion into a main line. True False 2. The titration table is the same for both DKA/HHS and non DKA/HHS patients. True False 3. Two RN’s must verify all rate changes. True False 4. In the event of a clogged or dislodged feeding tube, it is important to maintain a steady rate of insulin. True False 5. The blood glucose is often corrected before the blood ketones. Therefore, maintain the insulin infusion in type 1 diabetics until ketones are normalized even if the BG is normal. True False
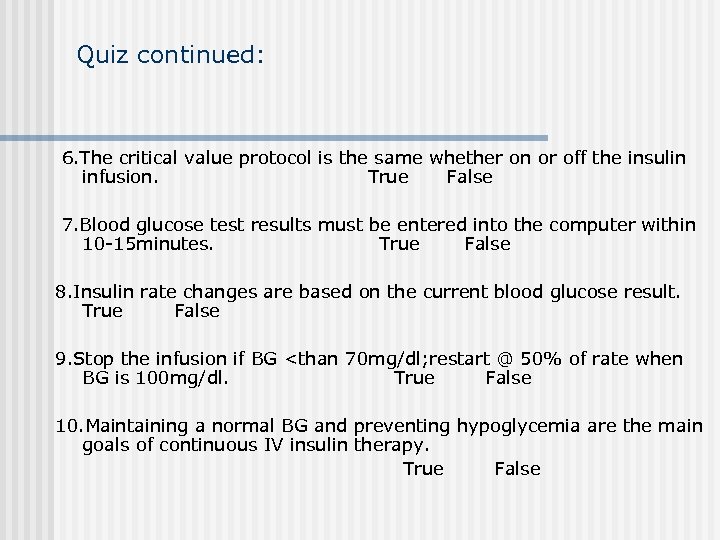 Quiz continued: 6. The critical value protocol is the same whether on or off the insulin infusion. True False 7. Blood glucose test results must be entered into the computer within 10 -15 minutes. True False 8. Insulin rate changes are based on the current blood glucose result. True False 9. Stop the infusion if BG
Quiz continued: 6. The critical value protocol is the same whether on or off the insulin infusion. True False 7. Blood glucose test results must be entered into the computer within 10 -15 minutes. True False 8. Insulin rate changes are based on the current blood glucose result. True False 9. Stop the infusion if BG
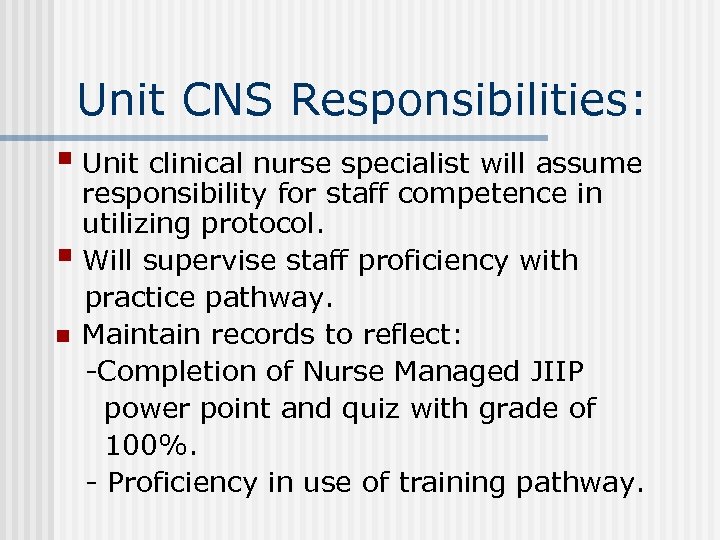 Unit CNS Responsibilities: § Unit clinical nurse specialist will assume responsibility for staff competence in utilizing protocol. § Will supervise staff proficiency with practice pathway. n Maintain records to reflect: -Completion of Nurse Managed JIIP power point and quiz with grade of 100%. - Proficiency in use of training pathway.
Unit CNS Responsibilities: § Unit clinical nurse specialist will assume responsibility for staff competence in utilizing protocol. § Will supervise staff proficiency with practice pathway. n Maintain records to reflect: -Completion of Nurse Managed JIIP power point and quiz with grade of 100%. - Proficiency in use of training pathway.


