488fff2f76969834fce93fa85eb0bbbc.ppt
- Количество слайдов: 36
 A Management Algorithm for Temporal Arteritis How Not to Miss this Blinding Disease Duncan P. Anderson, MD University of British Columbia Division of Neuro-Ophthalmology
A Management Algorithm for Temporal Arteritis How Not to Miss this Blinding Disease Duncan P. Anderson, MD University of British Columbia Division of Neuro-Ophthalmology
 55 year old female • 96 09 01: Frontal headache – acetaminophen • 96 09 15: Diplopia, left ptosis, 20 minutes of blurred vision after bending/lifting • 96 10 01: Increased headache (10/10), photophobia, diplopia, blurred vision, Left III palsy, dilated pupil, 20/100 OS Case Presentation, TA
55 year old female • 96 09 01: Frontal headache – acetaminophen • 96 09 15: Diplopia, left ptosis, 20 minutes of blurred vision after bending/lifting • 96 10 01: Increased headache (10/10), photophobia, diplopia, blurred vision, Left III palsy, dilated pupil, 20/100 OS Case Presentation, TA
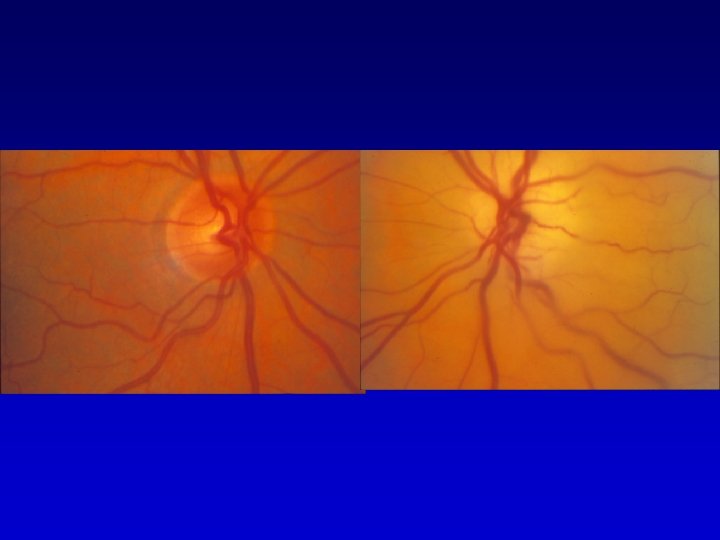
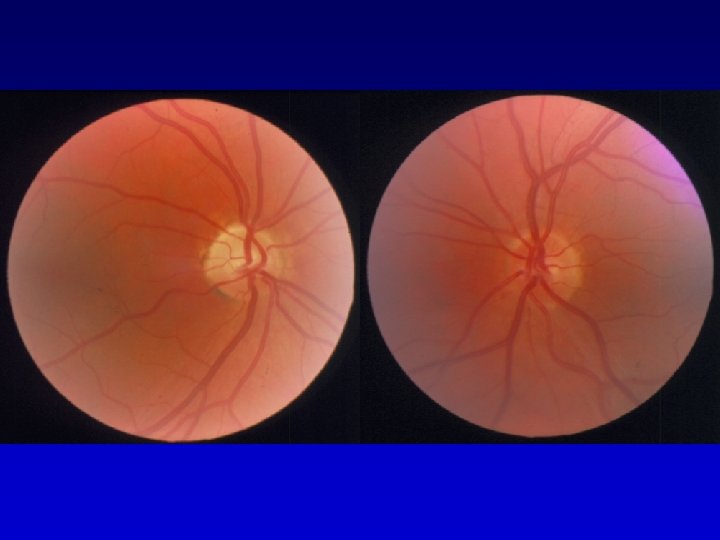
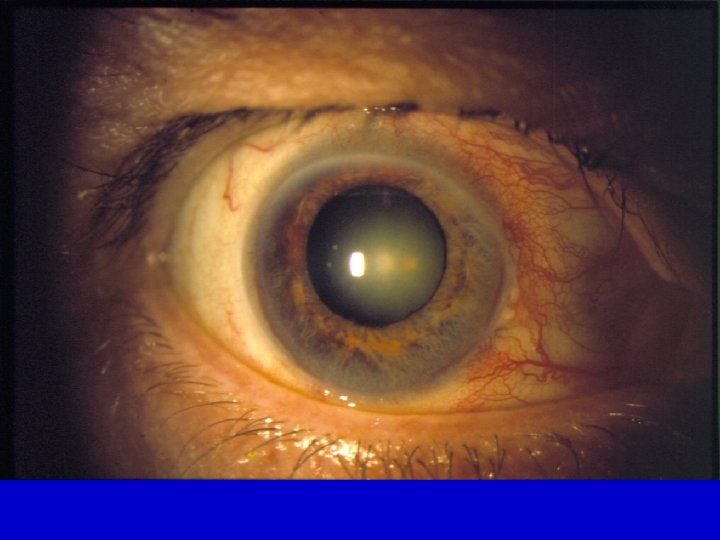
 • 96 10 02: Admitted to hospital. Normal head CT head, normal fundi, blind OS Angiogram requested. ESR 28 Left III palsy, 20/20 – NLP, Left afferent + efferent pupil defects Ophthalmodynanometry 50/20 – 0/0 Left Central Retinal Artery Occlusion Admits decreased appetite, weight, jaw pain treated with i. v. methylprednisolone, heparin Case Presentation, TA temporal artery biopsy requested
• 96 10 02: Admitted to hospital. Normal head CT head, normal fundi, blind OS Angiogram requested. ESR 28 Left III palsy, 20/20 – NLP, Left afferent + efferent pupil defects Ophthalmodynanometry 50/20 – 0/0 Left Central Retinal Artery Occlusion Admits decreased appetite, weight, jaw pain treated with i. v. methylprednisolone, heparin Case Presentation, TA temporal artery biopsy requested
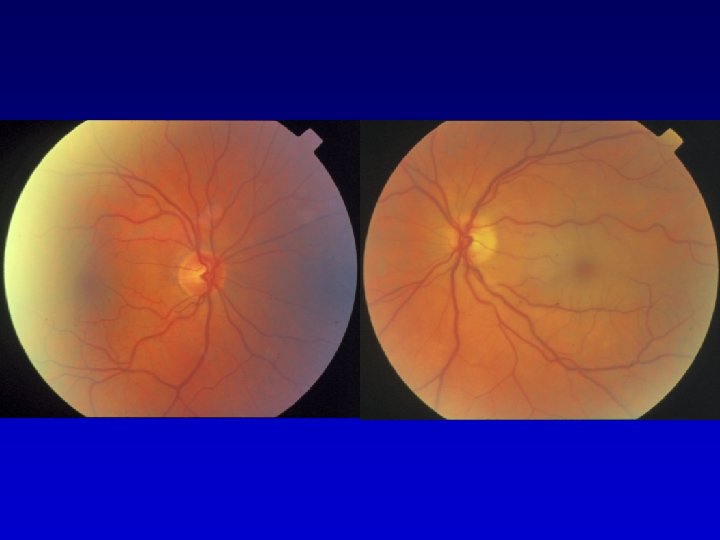
 • 96 10 03: temporal artery biopsy positive 20/20 OD, no light perception OS ophthalmodynamometry 40/20 OD, 1/10 OS intraocular pressure 10 mm. Hg OD, 2 mm. Hg OS left ophthalmic artery occlusion, bilateral carotid stenosis • 96 10 09: 20/20 OD, no light perception OS ophthalmodynamometry 40/20 OD, 10/5 OS intraocular pressure 15 mm. Hg OD, 6 mm. Hg OS Case Presentation, TA treated with prednisone and coumadin
• 96 10 03: temporal artery biopsy positive 20/20 OD, no light perception OS ophthalmodynamometry 40/20 OD, 1/10 OS intraocular pressure 10 mm. Hg OD, 2 mm. Hg OS left ophthalmic artery occlusion, bilateral carotid stenosis • 96 10 09: 20/20 OD, no light perception OS ophthalmodynamometry 40/20 OD, 10/5 OS intraocular pressure 15 mm. Hg OD, 6 mm. Hg OS Case Presentation, TA treated with prednisone and coumadin
 • 96 11 05: 20/20 OD, no light perception OS ophthalmodynanometry 70/30 OD, 35/10 OS intraocular pressure 16 OD, 12 OS mm. Hg left III palsy improving Prednisone 80 mg/day • 97 11 05: stopped steroids Blurriness ]right eye, headache, ESR 42 Prednisone re-started at 60 mg/day • 98 04 : tapered to Prednisone 10 mg/day Case Presentation, TA
• 96 11 05: 20/20 OD, no light perception OS ophthalmodynanometry 70/30 OD, 35/10 OS intraocular pressure 16 OD, 12 OS mm. Hg left III palsy improving Prednisone 80 mg/day • 97 11 05: stopped steroids Blurriness ]right eye, headache, ESR 42 Prednisone re-started at 60 mg/day • 98 04 : tapered to Prednisone 10 mg/day Case Presentation, TA
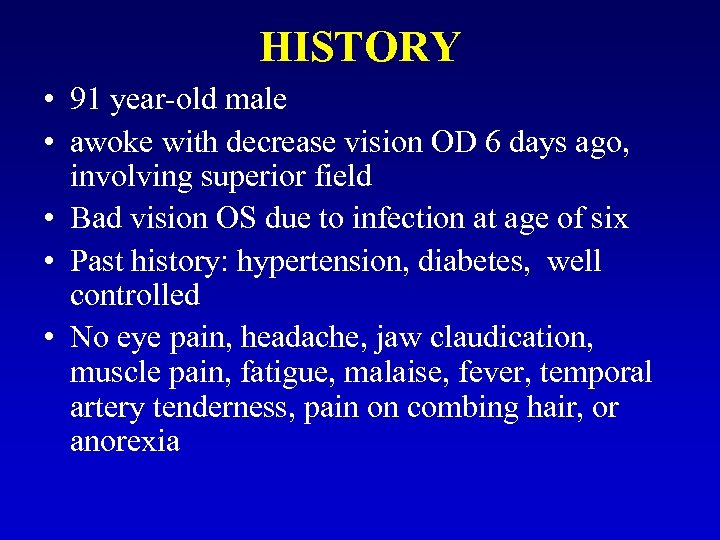 HISTORY • 91 year-old male • awoke with decrease vision OD 6 days ago, involving superior field • Bad vision OS due to infection at age of six • Past history: hypertension, diabetes, well controlled • No eye pain, headache, jaw claudication, muscle pain, fatigue, malaise, fever, temporal artery tenderness, pain on combing hair, or anorexia
HISTORY • 91 year-old male • awoke with decrease vision OD 6 days ago, involving superior field • Bad vision OS due to infection at age of six • Past history: hypertension, diabetes, well controlled • No eye pain, headache, jaw claudication, muscle pain, fatigue, malaise, fever, temporal artery tenderness, pain on combing hair, or anorexia
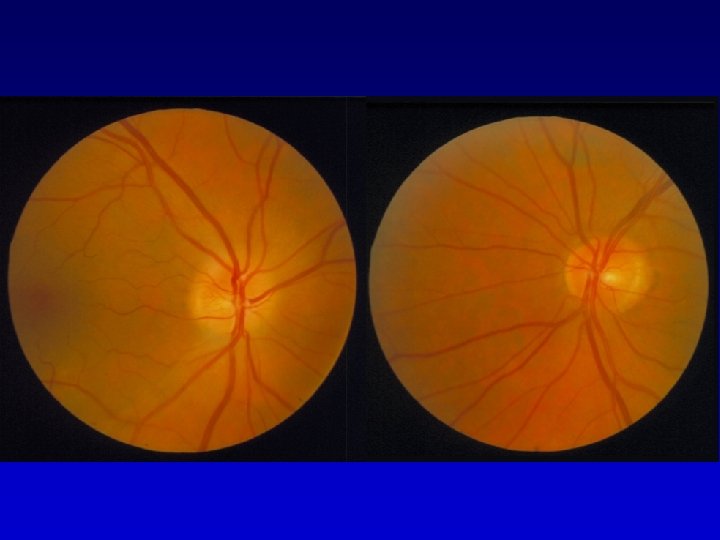
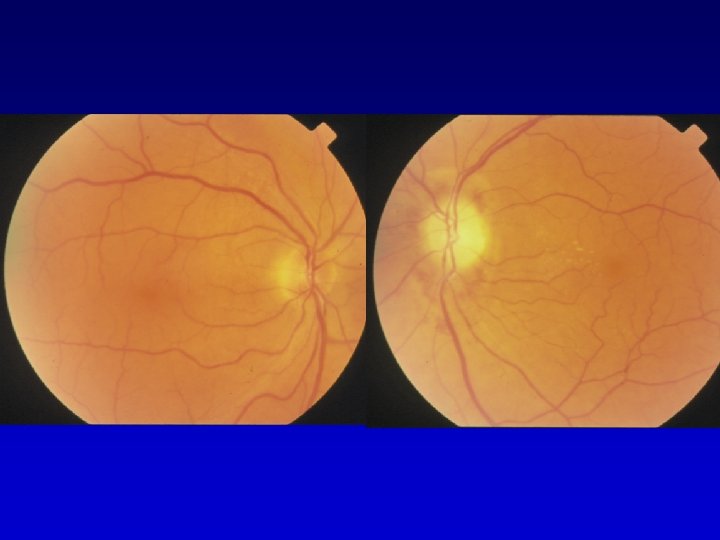
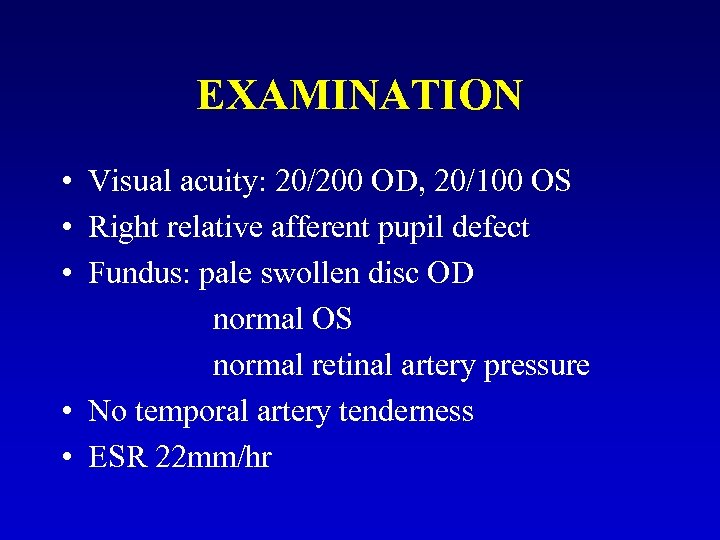 EXAMINATION • Visual acuity: 20/200 OD, 20/100 OS • Right relative afferent pupil defect • Fundus: pale swollen disc OD normal OS normal retinal artery pressure • No temporal artery tenderness • ESR 22 mm/hr
EXAMINATION • Visual acuity: 20/200 OD, 20/100 OS • Right relative afferent pupil defect • Fundus: pale swollen disc OD normal OS normal retinal artery pressure • No temporal artery tenderness • ESR 22 mm/hr

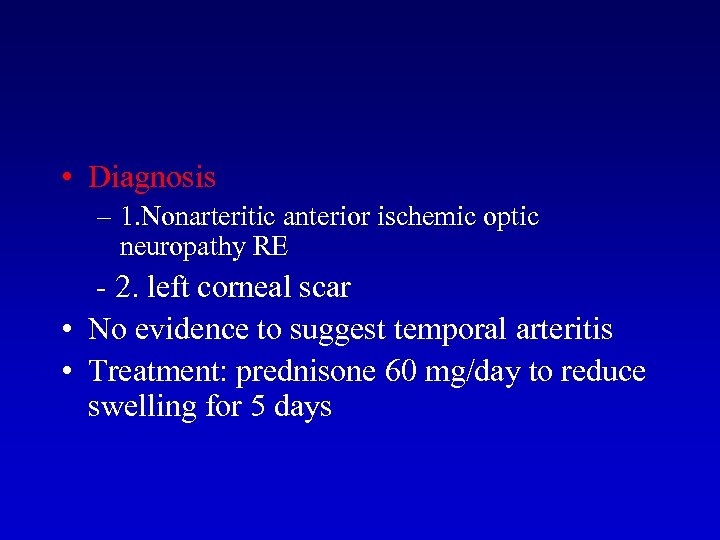 • Diagnosis – 1. Nonarteritic anterior ischemic optic neuropathy RE - 2. left corneal scar • No evidence to suggest temporal arteritis • Treatment: prednisone 60 mg/day to reduce swelling for 5 days
• Diagnosis – 1. Nonarteritic anterior ischemic optic neuropathy RE - 2. left corneal scar • No evidence to suggest temporal arteritis • Treatment: prednisone 60 mg/day to reduce swelling for 5 days
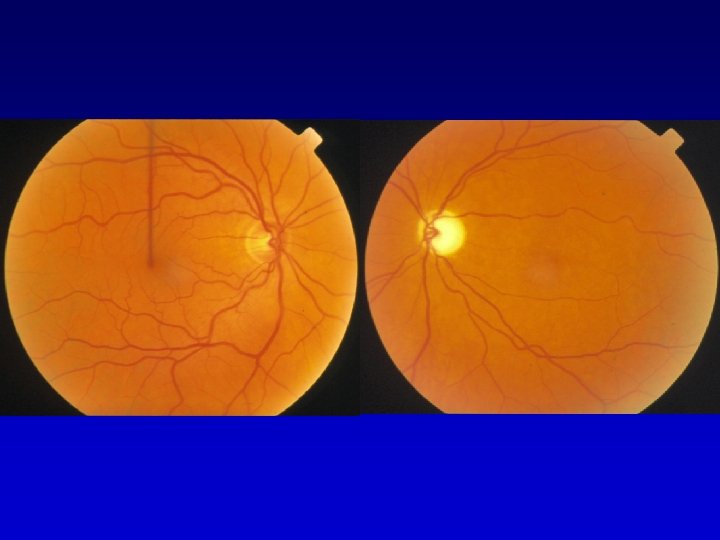
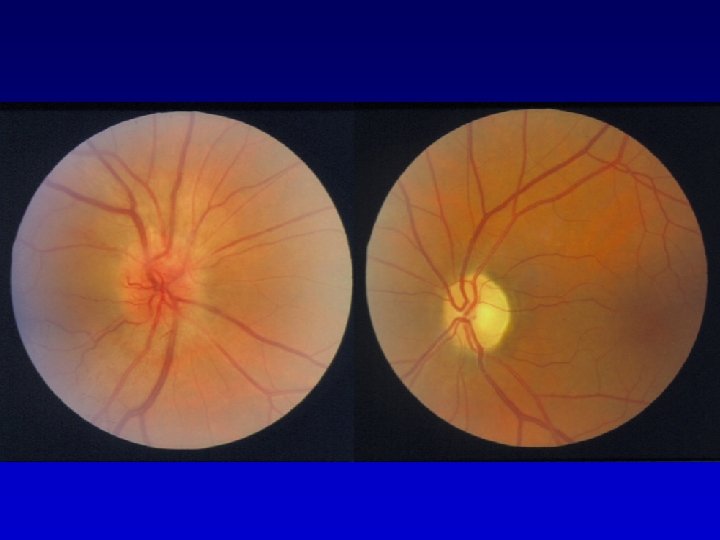
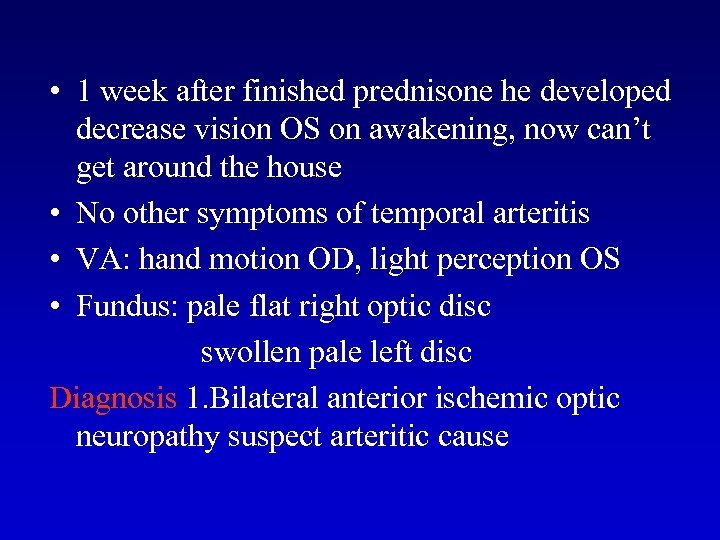 • 1 week after finished prednisone he developed decrease vision OS on awakening, now can’t get around the house • No other symptoms of temporal arteritis • VA: hand motion OD, light perception OS • Fundus: pale flat right optic disc swollen pale left disc Diagnosis 1. Bilateral anterior ischemic optic neuropathy suspect arteritic cause
• 1 week after finished prednisone he developed decrease vision OS on awakening, now can’t get around the house • No other symptoms of temporal arteritis • VA: hand motion OD, light perception OS • Fundus: pale flat right optic disc swollen pale left disc Diagnosis 1. Bilateral anterior ischemic optic neuropathy suspect arteritic cause
 Plan: immediate temporal artery biopsy Rx: predisone 1000 mg/day x 2 day then taper off • Temporal artery biopsy positive for arteritis • ESR 34/hr • Final visual acuity: count fingers OD, hand motion OS.
Plan: immediate temporal artery biopsy Rx: predisone 1000 mg/day x 2 day then taper off • Temporal artery biopsy positive for arteritis • ESR 34/hr • Final visual acuity: count fingers OD, hand motion OS.
 JW 85 YEAR OLD ♀ Sept 25 Flashes & Blur OD 26 Flashes & Blur OS ESR 71 – No arteritic symptoms i. v. methylprednisolone 1 gm/day for 6 days then oral prednisone 100 mg/day Oct 2 ESR 24 TAB Positive 12 HM Visual Hallucinations ESR 8
JW 85 YEAR OLD ♀ Sept 25 Flashes & Blur OD 26 Flashes & Blur OS ESR 71 – No arteritic symptoms i. v. methylprednisolone 1 gm/day for 6 days then oral prednisone 100 mg/day Oct 2 ESR 24 TAB Positive 12 HM Visual Hallucinations ESR 8
 EP 77 YEAR OLD ♀ Late Aug Sept 23 25 headache, Fatigue, jaw claudication, weight loss Blur OD ESR > 100 IV methylprednisolone 1 gm/day x 3 days 27 Blur OS IV methylprednisolone 1 gm/day x 3 days oral prednisone 100 mg/day Oct 2 18 temporal artery biopsy positive LP V tapered to prednisone 20 mg/day LP
EP 77 YEAR OLD ♀ Late Aug Sept 23 25 headache, Fatigue, jaw claudication, weight loss Blur OD ESR > 100 IV methylprednisolone 1 gm/day x 3 days 27 Blur OS IV methylprednisolone 1 gm/day x 3 days oral prednisone 100 mg/day Oct 2 18 temporal artery biopsy positive LP V tapered to prednisone 20 mg/day LP

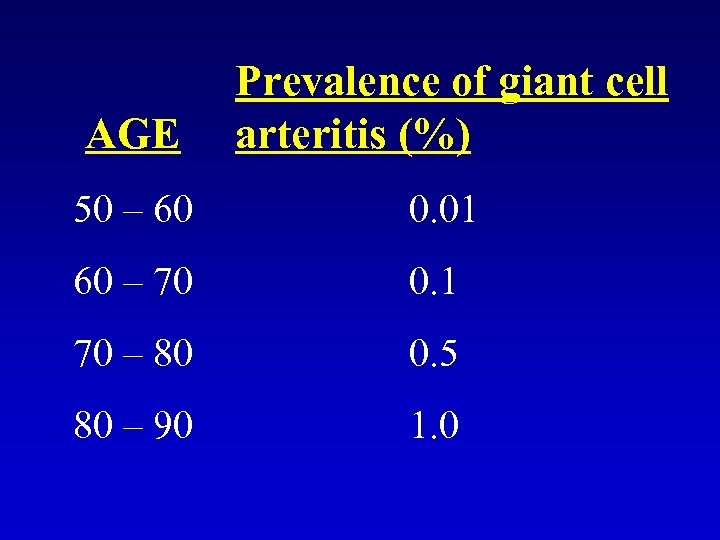 AGE Prevalence of giant cell arteritis (%) 50 – 60 0. 01 60 – 70 0. 1 70 – 80 0. 5 80 – 90 1. 0
AGE Prevalence of giant cell arteritis (%) 50 – 60 0. 01 60 – 70 0. 1 70 – 80 0. 5 80 – 90 1. 0
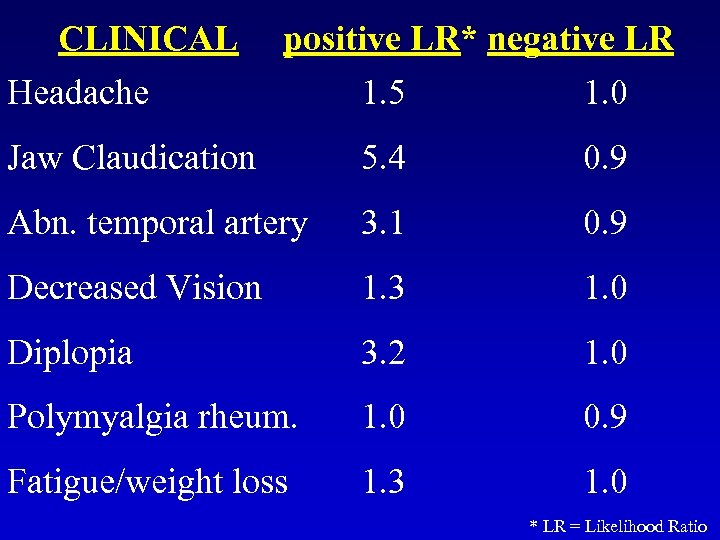 CLINICAL positive LR* negative LR Headache 1. 5 1. 0 Jaw Claudication 5. 4 0. 9 Abn. temporal artery 3. 1 0. 9 Decreased Vision 1. 3 1. 0 Diplopia 3. 2 1. 0 Polymyalgia rheum. 1. 0 0. 9 Fatigue/weight loss 1. 3 1. 0 * LR = Likelihood Ratio
CLINICAL positive LR* negative LR Headache 1. 5 1. 0 Jaw Claudication 5. 4 0. 9 Abn. temporal artery 3. 1 0. 9 Decreased Vision 1. 3 1. 0 Diplopia 3. 2 1. 0 Polymyalgia rheum. 1. 0 0. 9 Fatigue/weight loss 1. 3 1. 0 * LR = Likelihood Ratio
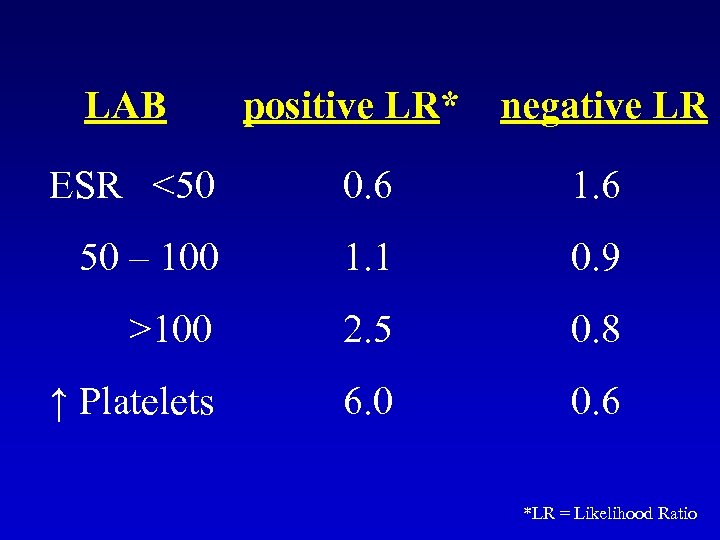 LAB positive LR* negative LR ESR <50 0. 6 1. 6 50 – 100 1. 1 0. 9 >100 2. 5 0. 8 ↑ Platelets 6. 0 0. 6 *LR = Likelihood Ratio
LAB positive LR* negative LR ESR <50 0. 6 1. 6 50 – 100 1. 1 0. 9 >100 2. 5 0. 8 ↑ Platelets 6. 0 0. 6 *LR = Likelihood Ratio
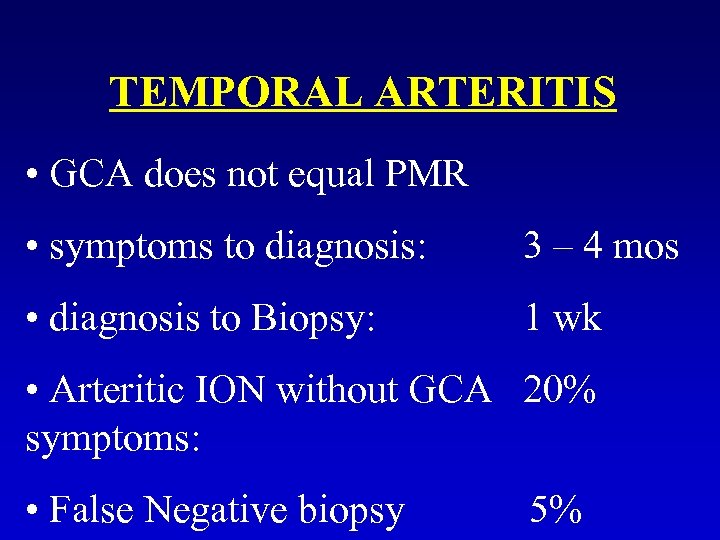 TEMPORAL ARTERITIS • GCA does not equal PMR • symptoms to diagnosis: 3 – 4 mos • diagnosis to Biopsy: 1 wk • Arteritic ION without GCA 20% symptoms: • False Negative biopsy 5%
TEMPORAL ARTERITIS • GCA does not equal PMR • symptoms to diagnosis: 3 – 4 mos • diagnosis to Biopsy: 1 wk • Arteritic ION without GCA 20% symptoms: • False Negative biopsy 5%
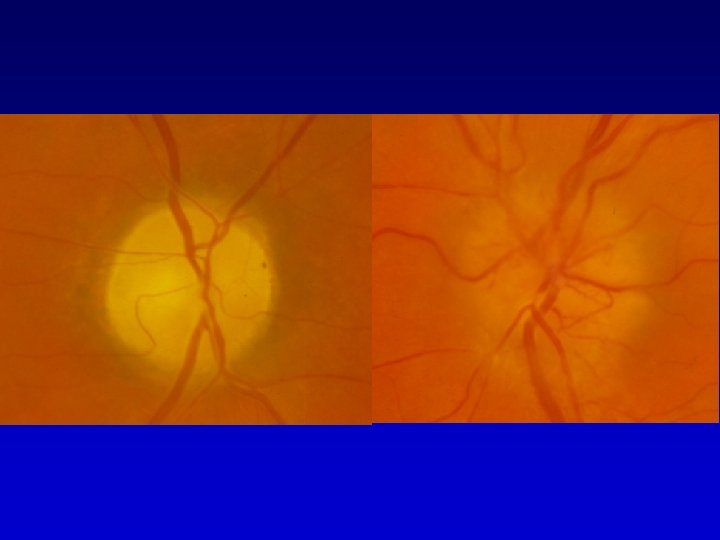
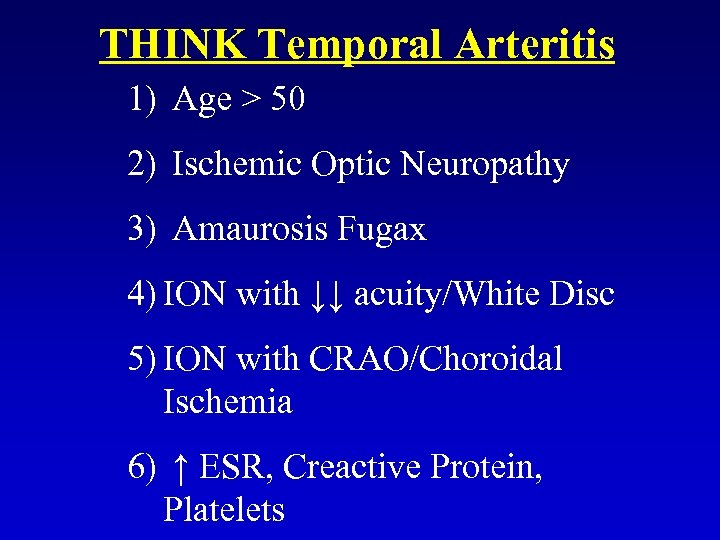 THINK Temporal Arteritis 1) Age > 50 2) Ischemic Optic Neuropathy 3) Amaurosis Fugax 4) ION with ↓↓ acuity/White Disc 5) ION with CRAO/Choroidal Ischemia 6) ↑ ESR, Creactive Protein, Platelets
THINK Temporal Arteritis 1) Age > 50 2) Ischemic Optic Neuropathy 3) Amaurosis Fugax 4) ION with ↓↓ acuity/White Disc 5) ION with CRAO/Choroidal Ischemia 6) ↑ ESR, Creactive Protein, Platelets
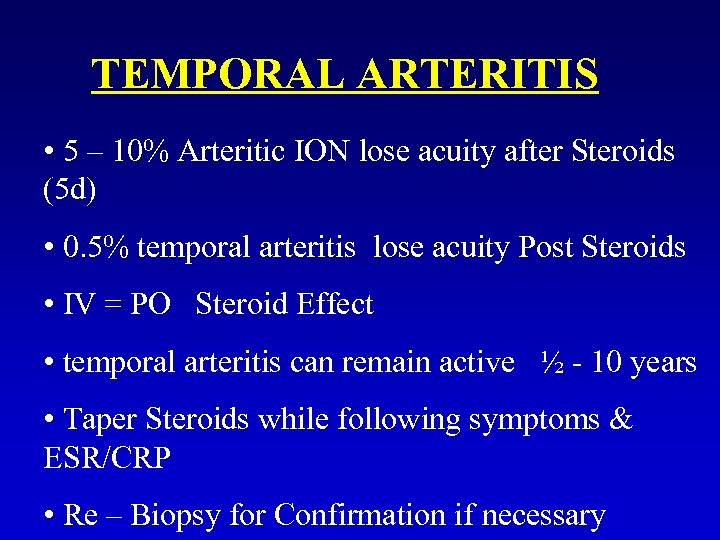 TEMPORAL ARTERITIS • 5 – 10% Arteritic ION lose acuity after Steroids (5 d) • 0. 5% temporal arteritis lose acuity Post Steroids • IV = PO Steroid Effect • temporal arteritis can remain active ½ - 10 years • Taper Steroids while following symptoms & ESR/CRP • Re – Biopsy for Confirmation if necessary
TEMPORAL ARTERITIS • 5 – 10% Arteritic ION lose acuity after Steroids (5 d) • 0. 5% temporal arteritis lose acuity Post Steroids • IV = PO Steroid Effect • temporal arteritis can remain active ½ - 10 years • Taper Steroids while following symptoms & ESR/CRP • Re – Biopsy for Confirmation if necessary

 TREATMENT p. o. Prednisone 80 mg/d 40 mg/d 1 - 2 weeks 2 - 3 months 1 - 2 years
TREATMENT p. o. Prednisone 80 mg/d 40 mg/d 1 - 2 weeks 2 - 3 months 1 - 2 years
 TREATMENT IV Methylprednisolone 1 gm/day for: • bilateral disease • second eye • progressive disease
TREATMENT IV Methylprednisolone 1 gm/day for: • bilateral disease • second eye • progressive disease
 SUMMARY - TEMPORAL ARTERITIS Diagnosis: • history • temporal artery biopsy within 1 - 2 weeks Treatment: • steroids (STAT) • medical emergency • taper slowly (mos) • manage steroid complications • switch to methotrexate
SUMMARY - TEMPORAL ARTERITIS Diagnosis: • history • temporal artery biopsy within 1 - 2 weeks Treatment: • steroids (STAT) • medical emergency • taper slowly (mos) • manage steroid complications • switch to methotrexate
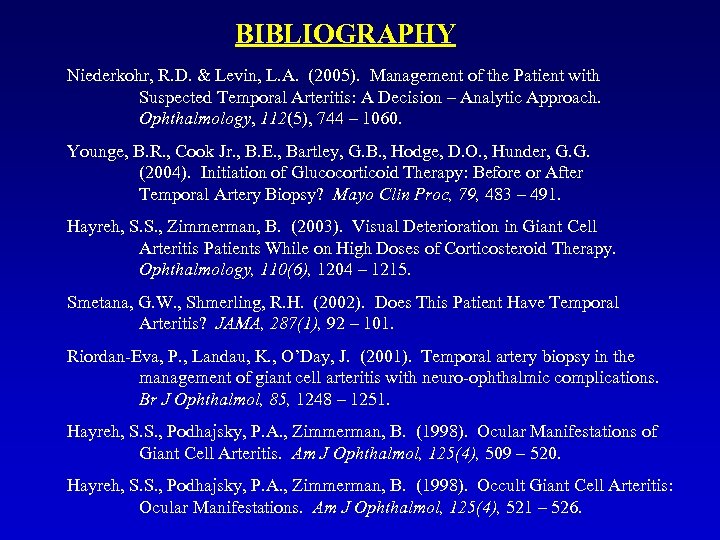 BIBLIOGRAPHY Niederkohr, R. D. & Levin, L. A. (2005). Management of the Patient with Suspected Temporal Arteritis: A Decision – Analytic Approach. Ophthalmology, 112(5), 744 – 1060. Younge, B. R. , Cook Jr. , B. E. , Bartley, G. B. , Hodge, D. O. , Hunder, G. G. (2004). Initiation of Glucocorticoid Therapy: Before or After Temporal Artery Biopsy? Mayo Clin Proc, 79, 483 – 491. Hayreh, S. S. , Zimmerman, B. (2003). Visual Deterioration in Giant Cell Arteritis Patients While on High Doses of Corticosteroid Therapy. Ophthalmology, 110(6), 1204 – 1215. Smetana, G. W. , Shmerling, R. H. (2002). Does This Patient Have Temporal Arteritis? JAMA, 287(1), 92 – 101. Riordan-Eva, P. , Landau, K. , O’Day, J. (2001). Temporal artery biopsy in the management of giant cell arteritis with neuro-ophthalmic complications. Br J Ophthalmol, 85, 1248 – 1251. Hayreh, S. S. , Podhajsky, P. A. , Zimmerman, B. (1998). Ocular Manifestations of Giant Cell Arteritis. Am J Ophthalmol, 125(4), 509 – 520. Hayreh, S. S. , Podhajsky, P. A. , Zimmerman, B. (1998). Occult Giant Cell Arteritis: Ocular Manifestations. Am J Ophthalmol, 125(4), 521 – 526.
BIBLIOGRAPHY Niederkohr, R. D. & Levin, L. A. (2005). Management of the Patient with Suspected Temporal Arteritis: A Decision – Analytic Approach. Ophthalmology, 112(5), 744 – 1060. Younge, B. R. , Cook Jr. , B. E. , Bartley, G. B. , Hodge, D. O. , Hunder, G. G. (2004). Initiation of Glucocorticoid Therapy: Before or After Temporal Artery Biopsy? Mayo Clin Proc, 79, 483 – 491. Hayreh, S. S. , Zimmerman, B. (2003). Visual Deterioration in Giant Cell Arteritis Patients While on High Doses of Corticosteroid Therapy. Ophthalmology, 110(6), 1204 – 1215. Smetana, G. W. , Shmerling, R. H. (2002). Does This Patient Have Temporal Arteritis? JAMA, 287(1), 92 – 101. Riordan-Eva, P. , Landau, K. , O’Day, J. (2001). Temporal artery biopsy in the management of giant cell arteritis with neuro-ophthalmic complications. Br J Ophthalmol, 85, 1248 – 1251. Hayreh, S. S. , Podhajsky, P. A. , Zimmerman, B. (1998). Ocular Manifestations of Giant Cell Arteritis. Am J Ophthalmol, 125(4), 509 – 520. Hayreh, S. S. , Podhajsky, P. A. , Zimmerman, B. (1998). Occult Giant Cell Arteritis: Ocular Manifestations. Am J Ophthalmol, 125(4), 521 – 526.


