c0008108ba4901b227cbf99a0648b693.ppt
- Количество слайдов: 64
 “A European network on cervical cancer surveillance and control in the new Member States - AURORA” 1 st Module: Scientific Background for Healthcare Professionals
“A European network on cervical cancer surveillance and control in the new Member States - AURORA” 1 st Module: Scientific Background for Healthcare Professionals
 Partners www. aurora-project. eu This publication arises from the project «AURORA» which has received funding from the European Union in the Framework of the Health Programme.
Partners www. aurora-project. eu This publication arises from the project «AURORA» which has received funding from the European Union in the Framework of the Health Programme.
 Index 1. Cervical cancer epidemiology 2. Introductory issues about STIs and HPV infection – transmission 3. Diagnosis of HPV infection. Screening tests (cervical cytology; liquid-based cervical cytology; visual inspection; colposcopy; HPV DNA testing) 4. How to organise a population based screening programme 5. Prevention of infection: vaccination 6. Diagnosis and treatment of cervical cancer disease
Index 1. Cervical cancer epidemiology 2. Introductory issues about STIs and HPV infection – transmission 3. Diagnosis of HPV infection. Screening tests (cervical cytology; liquid-based cervical cytology; visual inspection; colposcopy; HPV DNA testing) 4. How to organise a population based screening programme 5. Prevention of infection: vaccination 6. Diagnosis and treatment of cervical cancer disease
 Cervical cancer epidemiology
Cervical cancer epidemiology
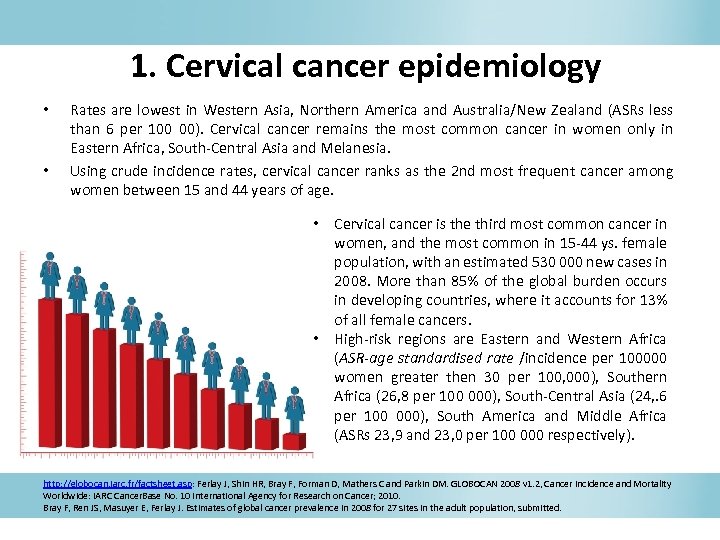 1. Cervical cancer epidemiology • • Rates are lowest in Western Asia, Northern America and Australia/New Zealand (ASRs less than 6 per 100 00). Cervical cancer remains the most common cancer in women only in Eastern Africa, South-Central Asia and Melanesia. Using crude incidence rates, cervical cancer ranks as the 2 nd most frequent cancer among women between 15 and 44 years of age. • Cervical cancer is the third most common cancer in women, and the most common in 15 -44 ys. female population, with an estimated 530 000 new cases in 2008. More than 85% of the global burden occurs in developing countries, where it accounts for 13% of all female cancers. • High-risk regions are Eastern and Western Africa (ASR-age standardised rate /incidence per 100000 women greater then 30 per 100, 000), Southern Africa (26, 8 per 100 000), South-Central Asia (24, . 6 per 100 000), South America and Middle Africa (ASRs 23, 9 and 23, 0 per 100 000 respectively). http: //globocan. iarc. fr/factsheet. asp: Ferlay J, Shin HR, Bray F, Forman D, Mathers C and Parkin DM. GLOBOCAN 2008 v 1. 2, Cancer Incidence and Mortality Worldwide: IARC Cancer. Base No. 10 International Agency for Research on Cancer; 2010. Bray F, Ren JS, Masuyer E, Ferlay J. Estimates of global cancer prevalence in 2008 for 27 sites in the adult population, submitted.
1. Cervical cancer epidemiology • • Rates are lowest in Western Asia, Northern America and Australia/New Zealand (ASRs less than 6 per 100 00). Cervical cancer remains the most common cancer in women only in Eastern Africa, South-Central Asia and Melanesia. Using crude incidence rates, cervical cancer ranks as the 2 nd most frequent cancer among women between 15 and 44 years of age. • Cervical cancer is the third most common cancer in women, and the most common in 15 -44 ys. female population, with an estimated 530 000 new cases in 2008. More than 85% of the global burden occurs in developing countries, where it accounts for 13% of all female cancers. • High-risk regions are Eastern and Western Africa (ASR-age standardised rate /incidence per 100000 women greater then 30 per 100, 000), Southern Africa (26, 8 per 100 000), South-Central Asia (24, . 6 per 100 000), South America and Middle Africa (ASRs 23, 9 and 23, 0 per 100 000 respectively). http: //globocan. iarc. fr/factsheet. asp: Ferlay J, Shin HR, Bray F, Forman D, Mathers C and Parkin DM. GLOBOCAN 2008 v 1. 2, Cancer Incidence and Mortality Worldwide: IARC Cancer. Base No. 10 International Agency for Research on Cancer; 2010. Bray F, Ren JS, Masuyer E, Ferlay J. Estimates of global cancer prevalence in 2008 for 27 sites in the adult population, submitted.
 Mortality Overall, the mortality incidence ratio is 52%, and cervical cancer is 52%, responsible for 275. 000 deaths in 2008, about 88% of which occur in 2008 developing countries: 53. 000 in Africa, 31. 700 in Latin America and the Caribbean, and 159. 800 in Asia. http: //globocan. iarc. fr/factsheet. asp: Ferlay J, Shin HR, Bray F, Forman D, Mathers C and Parkin DM. GLOBOCAN 2008 v 1. 2, Cancer Incidence and Mortality Worldwide: IARC Cancer. Base No. 10 International Agency for Research on Cancer; 2010. Bray F, Ren JS, Masuyer E, Ferlay J. Estimates of global cancer prevalence in 2008 for 27 sites in the adult population, submitted.
Mortality Overall, the mortality incidence ratio is 52%, and cervical cancer is 52%, responsible for 275. 000 deaths in 2008, about 88% of which occur in 2008 developing countries: 53. 000 in Africa, 31. 700 in Latin America and the Caribbean, and 159. 800 in Asia. http: //globocan. iarc. fr/factsheet. asp: Ferlay J, Shin HR, Bray F, Forman D, Mathers C and Parkin DM. GLOBOCAN 2008 v 1. 2, Cancer Incidence and Mortality Worldwide: IARC Cancer. Base No. 10 International Agency for Research on Cancer; 2010. Bray F, Ren JS, Masuyer E, Ferlay J. Estimates of global cancer prevalence in 2008 for 27 sites in the adult population, submitted.
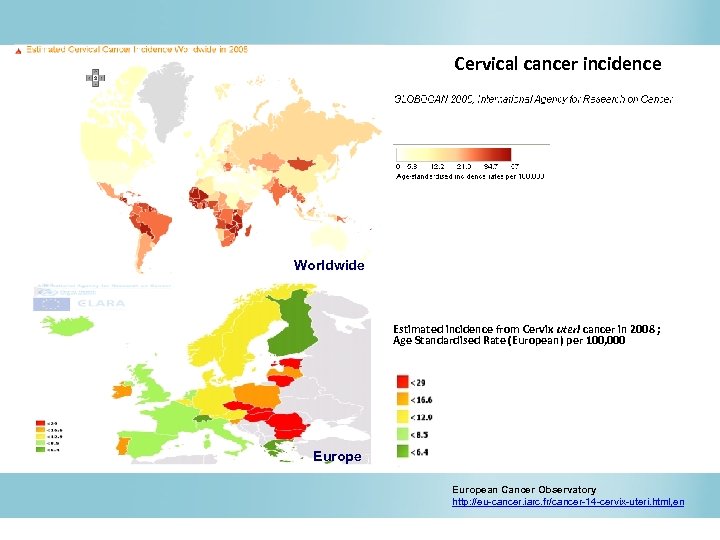 Cervical cancer incidence Worldwide Estimated incidence from Cervix uteri cancer in 2008 ; Age Standardised Rate (European) per 100, 000 European Cancer Observatory http: //eu-cancer. iarc. fr/cancer-14 -cervix-uteri. html, en
Cervical cancer incidence Worldwide Estimated incidence from Cervix uteri cancer in 2008 ; Age Standardised Rate (European) per 100, 000 European Cancer Observatory http: //eu-cancer. iarc. fr/cancer-14 -cervix-uteri. html, en
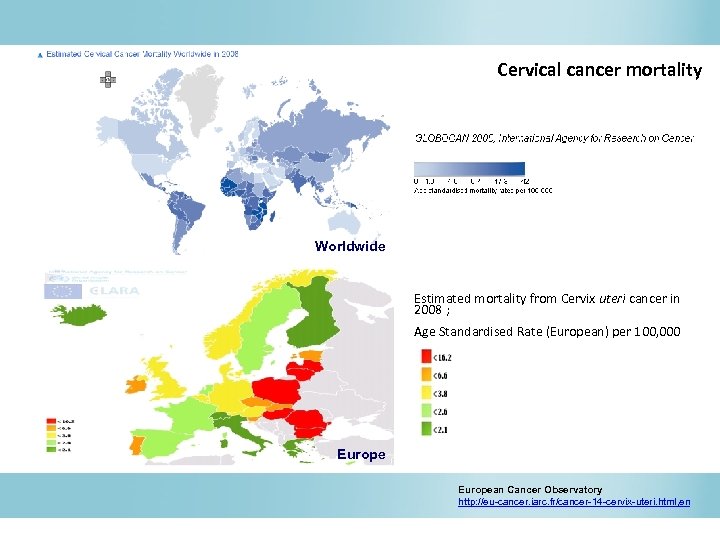 Cervical cancer mortality Worldwide Estimated mortality from Cervix uteri cancer in 2008 ; Age Standardised Rate (European) per 100, 000 European Cancer Observatory http: //eu-cancer. iarc. fr/cancer-14 -cervix-uteri. html, en
Cervical cancer mortality Worldwide Estimated mortality from Cervix uteri cancer in 2008 ; Age Standardised Rate (European) per 100, 000 European Cancer Observatory http: //eu-cancer. iarc. fr/cancer-14 -cervix-uteri. html, en
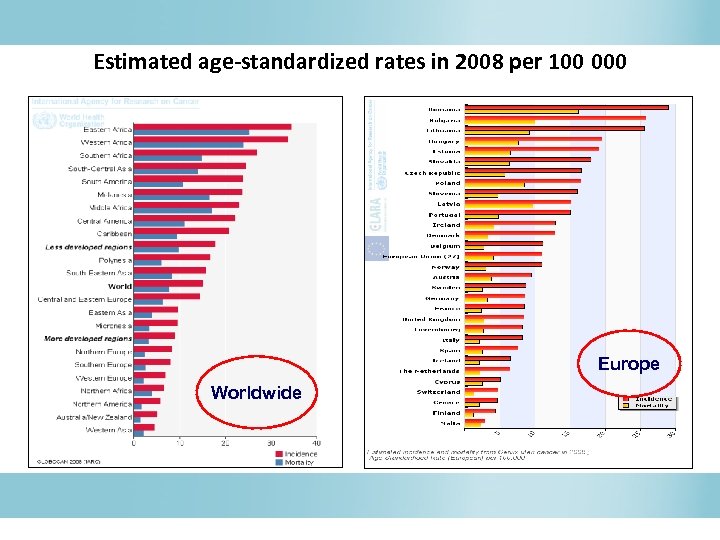 Estimated age-standardized rates in 2008 per 100 000 Europe Worldwide
Estimated age-standardized rates in 2008 per 100 000 Europe Worldwide
 Cervical cancer in EU Within the EU, wide variation is observed. The mortality was highest in Romania (world standardised rates of 13, 7/100. 000 women/year) and lowest in Finland (1, 1/ 100. 000/ year). The burden of cervical cancer is particularly high in the new member states. With the exception of Malta, all 11 other newly acceded members have higher incidence and mortality rates for cervix cancer than the 15 countries belonging to the European Union before the expansion in 2004 and 2007. Arbyn M et al. , 2007 a & b.
Cervical cancer in EU Within the EU, wide variation is observed. The mortality was highest in Romania (world standardised rates of 13, 7/100. 000 women/year) and lowest in Finland (1, 1/ 100. 000/ year). The burden of cervical cancer is particularly high in the new member states. With the exception of Malta, all 11 other newly acceded members have higher incidence and mortality rates for cervix cancer than the 15 countries belonging to the European Union before the expansion in 2004 and 2007. Arbyn M et al. , 2007 a & b.
 HPV infection and transmission
HPV infection and transmission
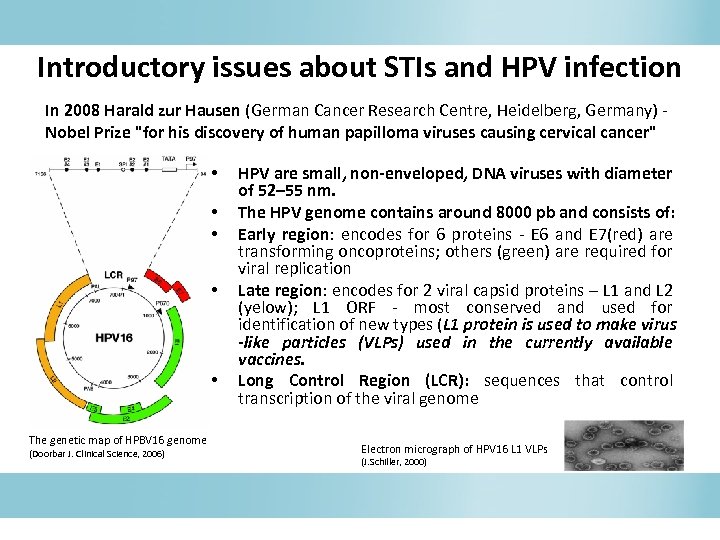 Introductory issues about STIs and HPV infection In 2008 Harald zur Hausen (German Cancer Research Centre, Heidelberg, Germany) Nobel Prize "for his discovery of human papilloma viruses causing cervical cancer" • • • The genetic map of HPBV 16 genome (Doorbar J. Clinical Science, 2006) HPV are small, non-enveloped, DNA viruses with diameter of 52– 55 nm. The HPV genome contains around 8000 pb and consists of: Early region: encodes for 6 proteins - E 6 and E 7(red) are transforming oncoproteins; others (green) are required for viral replication Late region: encodes for 2 viral capsid proteins – L 1 and L 2 (yelow); L 1 ORF - most conserved and used for identification of new types (L 1 protein is used to make virus -like particles (VLPs) used in the currently available vaccines. Long Control Region (LCR): sequences that control transcription of the viral genome Electron micrograph of HPV 16 L 1 VLPs (J. Schiller, 2000)
Introductory issues about STIs and HPV infection In 2008 Harald zur Hausen (German Cancer Research Centre, Heidelberg, Germany) Nobel Prize "for his discovery of human papilloma viruses causing cervical cancer" • • • The genetic map of HPBV 16 genome (Doorbar J. Clinical Science, 2006) HPV are small, non-enveloped, DNA viruses with diameter of 52– 55 nm. The HPV genome contains around 8000 pb and consists of: Early region: encodes for 6 proteins - E 6 and E 7(red) are transforming oncoproteins; others (green) are required for viral replication Late region: encodes for 2 viral capsid proteins – L 1 and L 2 (yelow); L 1 ORF - most conserved and used for identification of new types (L 1 protein is used to make virus -like particles (VLPs) used in the currently available vaccines. Long Control Region (LCR): sequences that control transcription of the viral genome Electron micrograph of HPV 16 L 1 VLPs (J. Schiller, 2000)
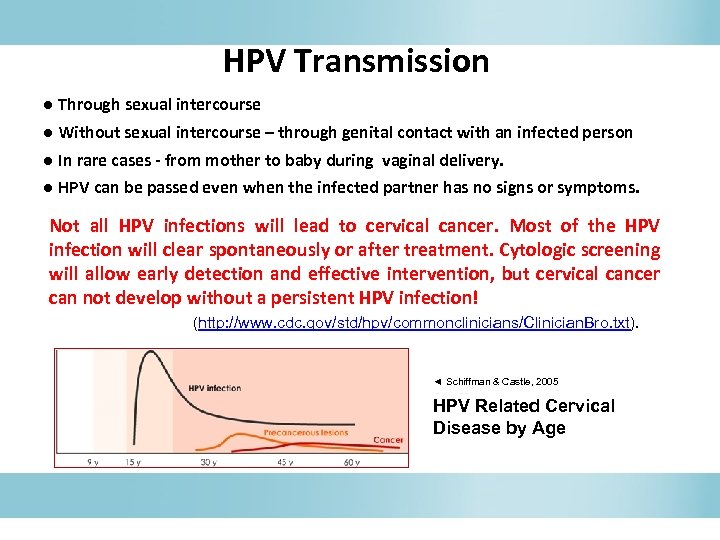 HPV Transmission ● Through sexual intercourse ● Without sexual intercourse – through genital contact with an infected person ● In rare cases - from mother to baby during vaginal delivery. ● HPV can be passed even when the infected partner has no signs or symptoms. Not all HPV infections will lead to cervical cancer. Most of the HPV infection will clear spontaneously or after treatment. Cytologic screening will allow early detection and effective intervention, but cervical cancer can not develop without a persistent HPV infection! (http: //www. cdc. gov/std/hpv/commonclinicians/Clinician. Bro. txt). ◄ Schiffman & Castle, 2005 HPV Related Cervical Disease by Age
HPV Transmission ● Through sexual intercourse ● Without sexual intercourse – through genital contact with an infected person ● In rare cases - from mother to baby during vaginal delivery. ● HPV can be passed even when the infected partner has no signs or symptoms. Not all HPV infections will lead to cervical cancer. Most of the HPV infection will clear spontaneously or after treatment. Cytologic screening will allow early detection and effective intervention, but cervical cancer can not develop without a persistent HPV infection! (http: //www. cdc. gov/std/hpv/commonclinicians/Clinician. Bro. txt). ◄ Schiffman & Castle, 2005 HPV Related Cervical Disease by Age
 Risk Factors HPV infection is the necessary cause of cervical cancer, but HPV infection is not sufficient to cause cervical cancer. Most of women infected with an oncogenic HPV type never develop cervical cancer, therefore additional factors contribute to cervical cancer development. Age of sexual debut, lifetime number of sexual partners, history of sexually transmitted infections, and other characteristics of sexual activity are linked to the likelihood of HPV infection, but are not cofactors for the progression from HPV infection to cervical cancer. Parity, use of oral contraceptives, tobacco smoking, immunosuppression (particularly related to HIV), infection with other sexually transmitted diseases, and poor nutrition, have been associated, to various extents, with the development of invasive cervical cancer. http: //screening. iarc. fr/doc/RH_fs_risk_factors. pdf
Risk Factors HPV infection is the necessary cause of cervical cancer, but HPV infection is not sufficient to cause cervical cancer. Most of women infected with an oncogenic HPV type never develop cervical cancer, therefore additional factors contribute to cervical cancer development. Age of sexual debut, lifetime number of sexual partners, history of sexually transmitted infections, and other characteristics of sexual activity are linked to the likelihood of HPV infection, but are not cofactors for the progression from HPV infection to cervical cancer. Parity, use of oral contraceptives, tobacco smoking, immunosuppression (particularly related to HIV), infection with other sexually transmitted diseases, and poor nutrition, have been associated, to various extents, with the development of invasive cervical cancer. http: //screening. iarc. fr/doc/RH_fs_risk_factors. pdf
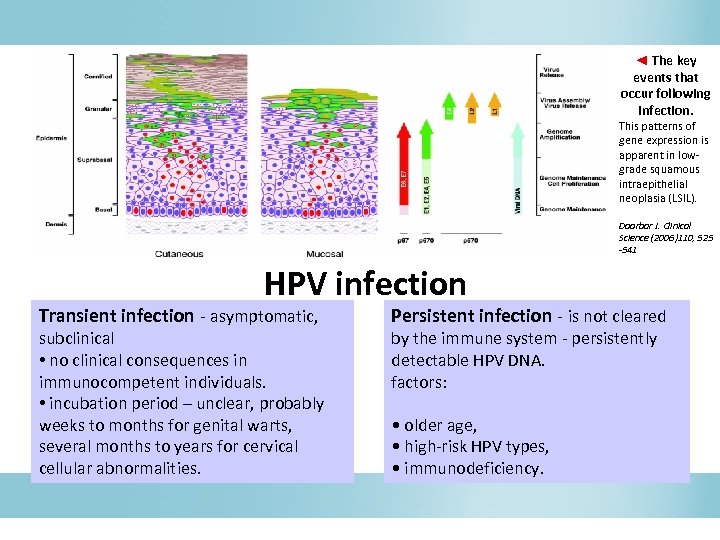 ◄ The key events that occur following infection. This patterns of gene expression is apparent in lowgrade squamous intraepithelial neoplasia (LSIL). Doorbar J. Clinical Science (2006)110, 525 -541 HPV infection Transient infection - asymptomatic, subclinical • no clinical consequences in immunocompetent individuals. • incubation period – unclear, probably weeks to months for genital warts, several months to years for cervical cellular abnormalities. Persistent infection - is not cleared by the immune system - persistently detectable HPV DNA. factors: • older age, • high-risk HPV types, • immunodeficiency.
◄ The key events that occur following infection. This patterns of gene expression is apparent in lowgrade squamous intraepithelial neoplasia (LSIL). Doorbar J. Clinical Science (2006)110, 525 -541 HPV infection Transient infection - asymptomatic, subclinical • no clinical consequences in immunocompetent individuals. • incubation period – unclear, probably weeks to months for genital warts, several months to years for cervical cellular abnormalities. Persistent infection - is not cleared by the immune system - persistently detectable HPV DNA. factors: • older age, • high-risk HPV types, • immunodeficiency.
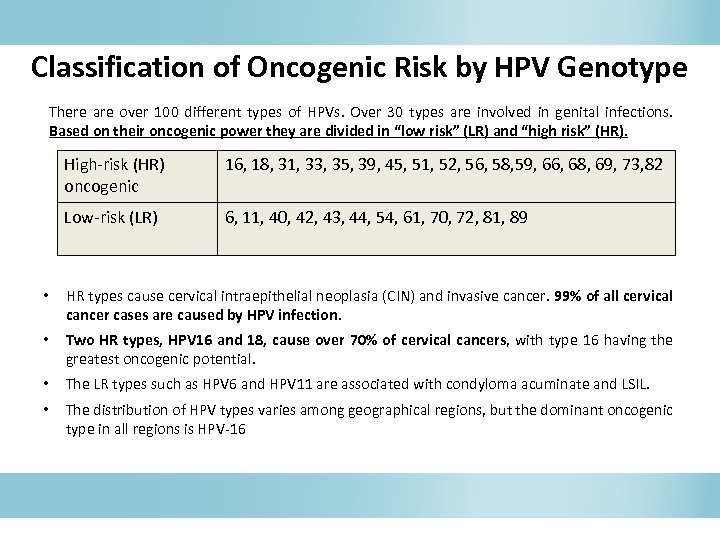 Classification of Oncogenic Risk by HPV Genotype There are over 100 different types of HPVs. Over 30 types are involved in genital infections. Based on their oncogenic power they are divided in “low risk” (LR) and “high risk” (HR). High-risk (HR) oncogenic 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68, 69, 73, 82 Low-risk (LR) 6, 11, 40, 42, 43, 44, 54, 61, 70, 72, 81, 89 • HR types cause cervical intraepithelial neoplasia (CIN) and invasive cancer. 99% of all cervical cancer cases are caused by HPV infection. • Two HR types, HPV 16 and 18, cause over 70% of cervical cancers, with type 16 having the greatest oncogenic potential. • The LR types such as HPV 6 and HPV 11 are associated with condyloma acuminate and LSIL. • The distribution of HPV types varies among geographical regions, but the dominant oncogenic type in all regions is HPV-16
Classification of Oncogenic Risk by HPV Genotype There are over 100 different types of HPVs. Over 30 types are involved in genital infections. Based on their oncogenic power they are divided in “low risk” (LR) and “high risk” (HR). High-risk (HR) oncogenic 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68, 69, 73, 82 Low-risk (LR) 6, 11, 40, 42, 43, 44, 54, 61, 70, 72, 81, 89 • HR types cause cervical intraepithelial neoplasia (CIN) and invasive cancer. 99% of all cervical cancer cases are caused by HPV infection. • Two HR types, HPV 16 and 18, cause over 70% of cervical cancers, with type 16 having the greatest oncogenic potential. • The LR types such as HPV 6 and HPV 11 are associated with condyloma acuminate and LSIL. • The distribution of HPV types varies among geographical regions, but the dominant oncogenic type in all regions is HPV-16
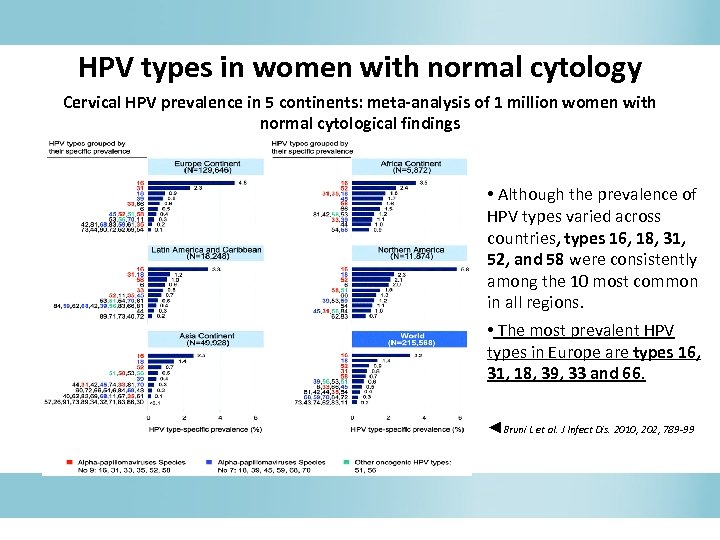 HPV types in women with normal cytology Cervical HPV prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings • Although the prevalence of HPV types varied across countries, types 16, 18, 31, 52, and 58 were consistently among the 10 most common in all regions. • The most prevalent HPV types in Europe are types 16, 31, 18, 39, 33 and 66. ◄Bruni L et al. J Infect Dis. 2010, 202, 789 -99
HPV types in women with normal cytology Cervical HPV prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings • Although the prevalence of HPV types varied across countries, types 16, 18, 31, 52, and 58 were consistently among the 10 most common in all regions. • The most prevalent HPV types in Europe are types 16, 31, 18, 39, 33 and 66. ◄Bruni L et al. J Infect Dis. 2010, 202, 789 -99
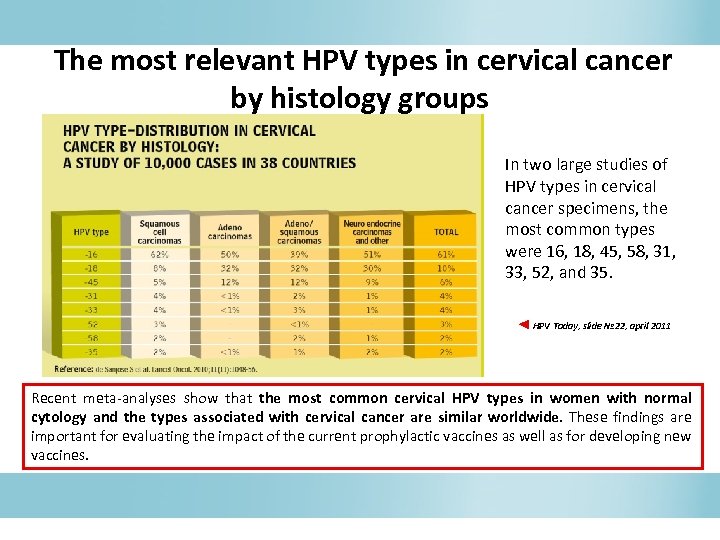 The most relevant HPV types in cervical cancer by histology groups In two large studies of HPV types in cervical cancer specimens, the most common types were 16, 18, 45, 58, 31, 33, 52, and 35. ◄ HPV Today, slide № 22, april 2011 Recent meta-analyses show that the most common cervical HPV types in women with normal cytology and the types associated with cervical cancer are similar worldwide. These findings are important for evaluating the impact of the current prophylactic vaccines as well as for developing new vaccines.
The most relevant HPV types in cervical cancer by histology groups In two large studies of HPV types in cervical cancer specimens, the most common types were 16, 18, 45, 58, 31, 33, 52, and 35. ◄ HPV Today, slide № 22, april 2011 Recent meta-analyses show that the most common cervical HPV types in women with normal cytology and the types associated with cervical cancer are similar worldwide. These findings are important for evaluating the impact of the current prophylactic vaccines as well as for developing new vaccines.
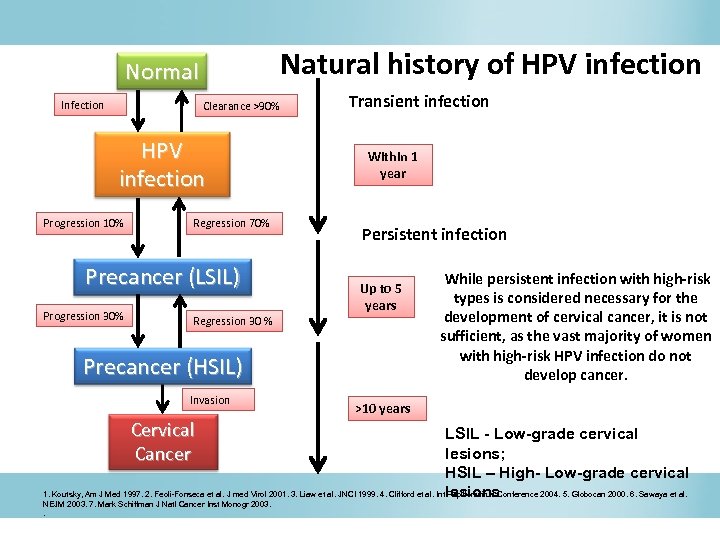 Natural history of HPV infection Normal Infection Clearance >90% HPV infection Progression 10% Regression 70% Precancer (LSIL) Progression 30% Transient infection Within 1 year Persistent infection Up to 5 years Regression 30 % Precancer (HSIL) Invasion Cervical Cancer While persistent infection with high-risk types is considered necessary for the development of cervical cancer, it is not sufficient, as the vast majority of women with high-risk HPV infection do not develop cancer. >10 years LSIL - Low-grade cervical lesions; HSIL – High- Low-grade cervical 1. Koutsky, Am J Med 1997. 2. Feoli-Fonseca et al. J med Virol 2001. 3. Liaw et al. JNCI 1999. 4. Clifford et al. Intlesions Papillomvirus Conference 2004. 5. Globocan 2000. 6. Sawaya et al. NEJM 2003. 7. Mark Schiffman J Natl Cancer Inst Monogr 2003. .
Natural history of HPV infection Normal Infection Clearance >90% HPV infection Progression 10% Regression 70% Precancer (LSIL) Progression 30% Transient infection Within 1 year Persistent infection Up to 5 years Regression 30 % Precancer (HSIL) Invasion Cervical Cancer While persistent infection with high-risk types is considered necessary for the development of cervical cancer, it is not sufficient, as the vast majority of women with high-risk HPV infection do not develop cancer. >10 years LSIL - Low-grade cervical lesions; HSIL – High- Low-grade cervical 1. Koutsky, Am J Med 1997. 2. Feoli-Fonseca et al. J med Virol 2001. 3. Liaw et al. JNCI 1999. 4. Clifford et al. Intlesions Papillomvirus Conference 2004. 5. Globocan 2000. 6. Sawaya et al. NEJM 2003. 7. Mark Schiffman J Natl Cancer Inst Monogr 2003. .
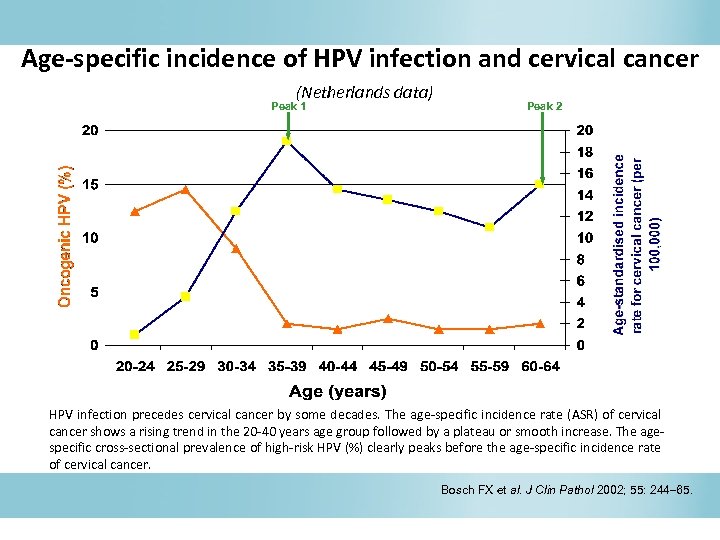 Age-specific incidence of HPV infection and cervical cancer (Netherlands data) Peak 1 Peak 2 HPV infection precedes cervical cancer by some decades. The age-specific incidence rate (ASR) of cervical cancer shows a rising trend in the 20 -40 years age group followed by a plateau or smooth increase. The agespecific cross-sectional prevalence of high-risk HPV (%) clearly peaks before the age-specific incidence rate of cervical cancer. Bosch FX et al. J Clin Pathol 2002; 55: 244 65.
Age-specific incidence of HPV infection and cervical cancer (Netherlands data) Peak 1 Peak 2 HPV infection precedes cervical cancer by some decades. The age-specific incidence rate (ASR) of cervical cancer shows a rising trend in the 20 -40 years age group followed by a plateau or smooth increase. The agespecific cross-sectional prevalence of high-risk HPV (%) clearly peaks before the age-specific incidence rate of cervical cancer. Bosch FX et al. J Clin Pathol 2002; 55: 244 65.
 Diagnosis
Diagnosis
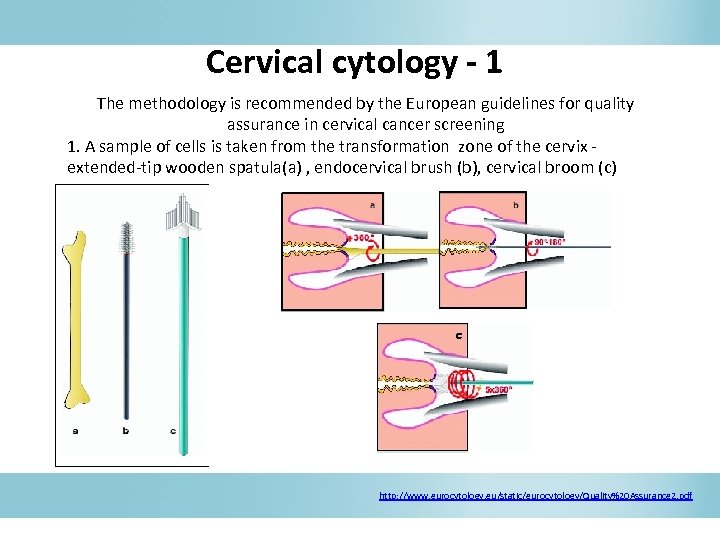 Cervical cytology - 1 The methodology is recommended by the European guidelines for quality assurance in cervical cancer screening 1. A sample of cells is taken from the transformation zone of the cervix - extended-tip wooden spatula(a) , endocervical brush (b), cervical broom (c) c http: //www. eurocytology. eu/static/eurocytology/Quality%20 Assurance 2. pdf
Cervical cytology - 1 The methodology is recommended by the European guidelines for quality assurance in cervical cancer screening 1. A sample of cells is taken from the transformation zone of the cervix - extended-tip wooden spatula(a) , endocervical brush (b), cervical broom (c) c http: //www. eurocytology. eu/static/eurocytology/Quality%20 Assurance 2. pdf
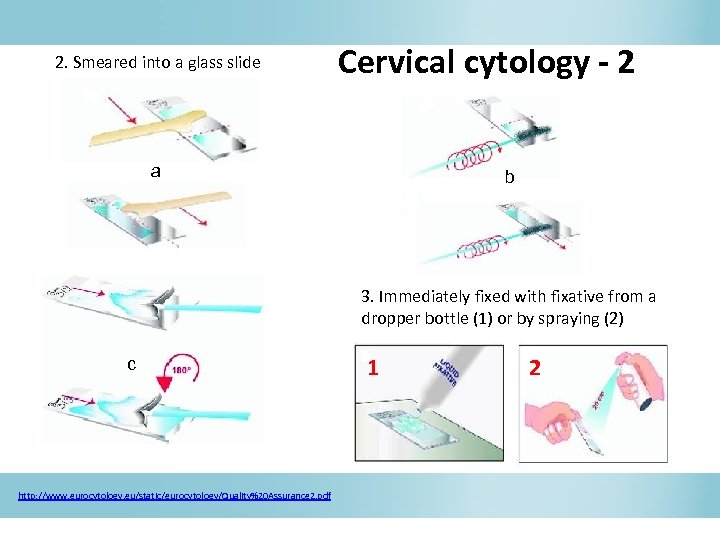 2. Smeared into a glass slide Cervical cytology - 2 a b 3. Immediately fixed with fixative from a dropper bottle (1) or by spraying (2) c http: //www. eurocytology. eu/static/eurocytology/Quality%20 Assurance 2. pdf 1 2
2. Smeared into a glass slide Cervical cytology - 2 a b 3. Immediately fixed with fixative from a dropper bottle (1) or by spraying (2) c http: //www. eurocytology. eu/static/eurocytology/Quality%20 Assurance 2. pdf 1 2
 Liquid-based cervical cytology • • a plastic spatula with either an endocervical brush or a cervical broom; the sample is rinsed into a vial containing preservative solution; centrifuged to produce a cell pellet OR drawn through a filter under negative pressure to collect cells; the resulting cell sample is fixed onto a glass slide and stained for examination under a microscope. Advantages • • • There are fewer unsatisfactory specimens. Each specimen requires a shorter interpretation time, leading to increased efficiency and cost-effectiveness. The material collected can also be tested for HPV DNA.
Liquid-based cervical cytology • • a plastic spatula with either an endocervical brush or a cervical broom; the sample is rinsed into a vial containing preservative solution; centrifuged to produce a cell pellet OR drawn through a filter under negative pressure to collect cells; the resulting cell sample is fixed onto a glass slide and stained for examination under a microscope. Advantages • • • There are fewer unsatisfactory specimens. Each specimen requires a shorter interpretation time, leading to increased efficiency and cost-effectiveness. The material collected can also be tested for HPV DNA.
 Results interpretation - 1 • Normal cytology - No abnormal cells are observed on the surface of their cervix upon cytology. • Cervical Intraepithelial Neoplasia (CIN) / Squamous Intraepithelial Lesions (SIL) precancerous lesions or the abnormal growth of squamous cells observed in the cervix. SIL - cervical cytological screening or Pap smear testing. CIN - histological diagnosis - biopsy or surgical excision. • Low-grade cervical lesions (CIN-1/ LSIL) - early changes in size, shape, and number of abnormal cells formed on the surface of the cervix • High-grade cervical lesions (CIN-2; CIN-3/ CIS/ HSIL) - a large number of precancerous cells on the surface of the cervix that are distinctly different from normal cells. They have the potential to become cancerous cells and invade deeper tissues of the cervix.
Results interpretation - 1 • Normal cytology - No abnormal cells are observed on the surface of their cervix upon cytology. • Cervical Intraepithelial Neoplasia (CIN) / Squamous Intraepithelial Lesions (SIL) precancerous lesions or the abnormal growth of squamous cells observed in the cervix. SIL - cervical cytological screening or Pap smear testing. CIN - histological diagnosis - biopsy or surgical excision. • Low-grade cervical lesions (CIN-1/ LSIL) - early changes in size, shape, and number of abnormal cells formed on the surface of the cervix • High-grade cervical lesions (CIN-2; CIN-3/ CIS/ HSIL) - a large number of precancerous cells on the surface of the cervix that are distinctly different from normal cells. They have the potential to become cancerous cells and invade deeper tissues of the cervix.
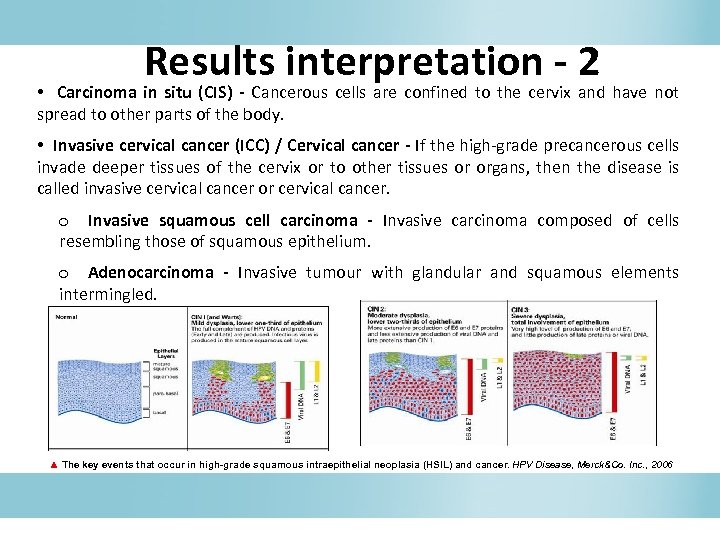 Results interpretation - 2 • Carcinoma in situ (CIS) - Cancerous cells are confined to the cervix and have not spread to other parts of the body. • Invasive cervical cancer (ICC) / Cervical cancer - If the high-grade precancerous cells invade deeper tissues of the cervix or to other tissues or organs, then the disease is called invasive cervical cancer or cervical cancer. o Invasive squamous cell carcinoma - Invasive carcinoma composed of cells resembling those of squamous epithelium. o Adenocarcinoma - Invasive tumour with glandular and squamous elements intermingled. ▲ The key events that occur in high-grade squamous intraepithelial neoplasia (HSIL) and cancer. HPV Disease, Merck&Co. Inc. , 2006
Results interpretation - 2 • Carcinoma in situ (CIS) - Cancerous cells are confined to the cervix and have not spread to other parts of the body. • Invasive cervical cancer (ICC) / Cervical cancer - If the high-grade precancerous cells invade deeper tissues of the cervix or to other tissues or organs, then the disease is called invasive cervical cancer or cervical cancer. o Invasive squamous cell carcinoma - Invasive carcinoma composed of cells resembling those of squamous epithelium. o Adenocarcinoma - Invasive tumour with glandular and squamous elements intermingled. ▲ The key events that occur in high-grade squamous intraepithelial neoplasia (HSIL) and cancer. HPV Disease, Merck&Co. Inc. , 2006
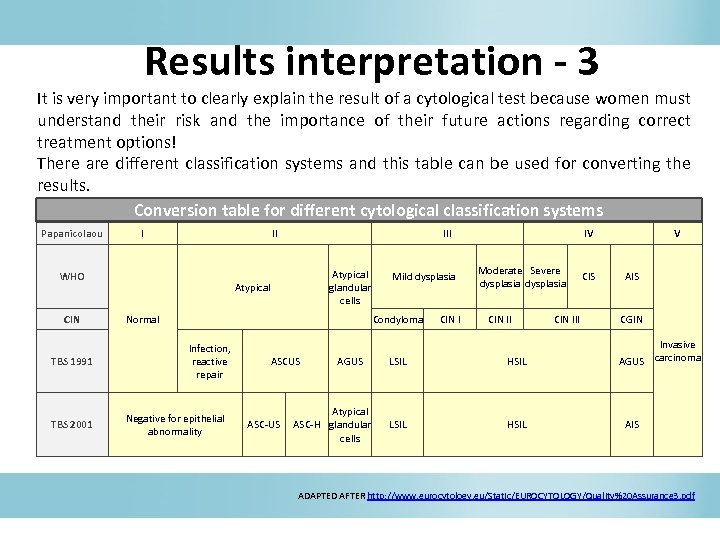 Results interpretation - 3 It is very important to clearly explain the result of a cytological test because women must understand their risk and the importance of their future actions regarding correct treatment options! There are different classification systems and this table can be used for converting the results. Conversion table for different cytological classification systems Papanicolaou I II WHO CIN TBS 1991 TBS 2001 III Atypical glandular cells Atypical Mild dysplasia Condyloma Normal Infection, reactive repair Negative for epithelial abnormality ASCUS ASC-US AGUS Atypical ASC-H glandular cells CIN I IV Moderate Severe dysplasia CIN II LSIL HSIL CIN III CIS V AIS CGIN Invasive AGUS carcinoma AIS ADAPTED AFTER http: //www. eurocytology. eu/Static/EUROCYTOLOGY/Quality%20 Assurance 3. pdf
Results interpretation - 3 It is very important to clearly explain the result of a cytological test because women must understand their risk and the importance of their future actions regarding correct treatment options! There are different classification systems and this table can be used for converting the results. Conversion table for different cytological classification systems Papanicolaou I II WHO CIN TBS 1991 TBS 2001 III Atypical glandular cells Atypical Mild dysplasia Condyloma Normal Infection, reactive repair Negative for epithelial abnormality ASCUS ASC-US AGUS Atypical ASC-H glandular cells CIN I IV Moderate Severe dysplasia CIN II LSIL HSIL CIN III CIS V AIS CGIN Invasive AGUS carcinoma AIS ADAPTED AFTER http: //www. eurocytology. eu/Static/EUROCYTOLOGY/Quality%20 Assurance 3. pdf
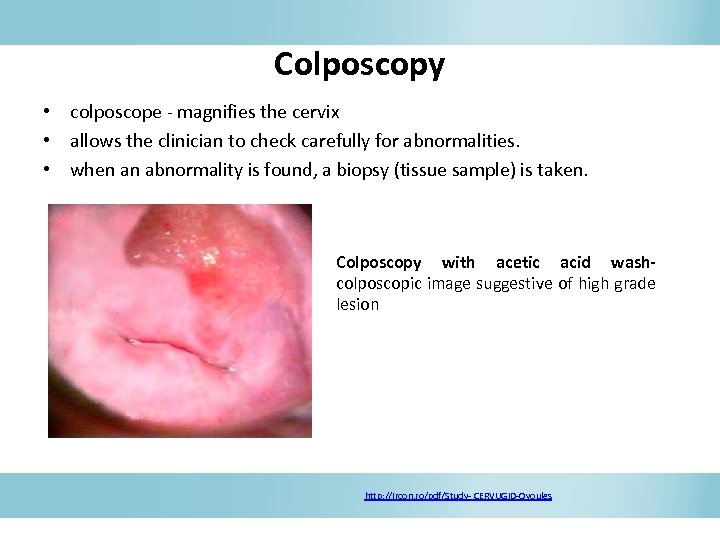 Colposcopy • colposcope - magnifies the cervix • allows the clinician to check carefully for abnormalities. • when an abnormality is found, a biopsy (tissue sample) is taken. Colposcopy with acetic acid wash- colposcopic image suggestive of high grade lesion http: //ircon. ro/pdf/Study- CERVUGID-Ovoules
Colposcopy • colposcope - magnifies the cervix • allows the clinician to check carefully for abnormalities. • when an abnormality is found, a biopsy (tissue sample) is taken. Colposcopy with acetic acid wash- colposcopic image suggestive of high grade lesion http: //ircon. ro/pdf/Study- CERVUGID-Ovoules
 HPV- DNA testing Currently the most widely used HPV testing methods are based on the detection of HPV DNA and include: • polymerase chain reaction (PCR)-based methods • nucleic acid hybridization assays with signal amplification.
HPV- DNA testing Currently the most widely used HPV testing methods are based on the detection of HPV DNA and include: • polymerase chain reaction (PCR)-based methods • nucleic acid hybridization assays with signal amplification.
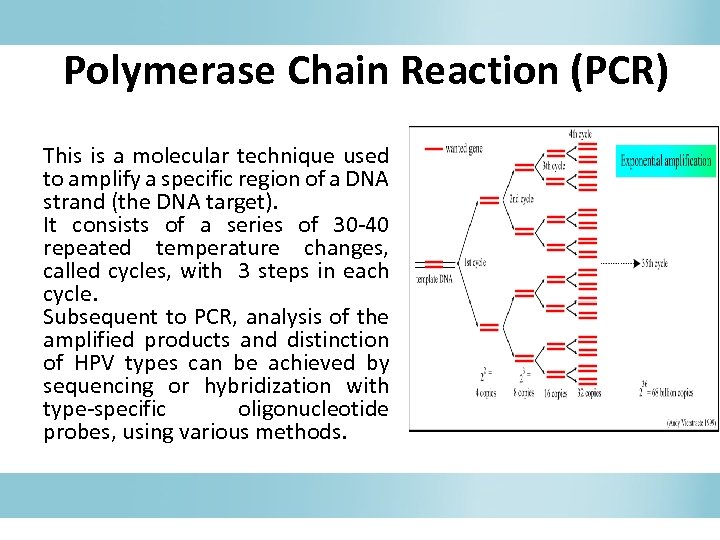 Polymerase Chain Reaction (PCR) This is a molecular technique used to amplify a specific region of a DNA strand (the DNA target). It consists of a series of 30 -40 repeated temperature changes, called cycles, with 3 steps in each cycle. Subsequent to PCR, analysis of the amplified products and distinction of HPV types can be achieved by sequencing or hybridization with type-specific oligonucleotide probes, using various methods.
Polymerase Chain Reaction (PCR) This is a molecular technique used to amplify a specific region of a DNA strand (the DNA target). It consists of a series of 30 -40 repeated temperature changes, called cycles, with 3 steps in each cycle. Subsequent to PCR, analysis of the amplified products and distinction of HPV types can be achieved by sequencing or hybridization with type-specific oligonucleotide probes, using various methods.
 3 steps of PCR 1. denaturation (the DNA strands separate to form single strands) 2. annealing, one primer binds to one DNA strand another binds to the complementary strand. The annealing sites of the primers are chosen so that they will prime DNA synthesis in the region of interest during extension 3. extension: The DNA polymerase synthesises a complementary strand. The enzyme reads the opposing strand sequence and extends the primers by adding nucleotides in the order in which they can pair.
3 steps of PCR 1. denaturation (the DNA strands separate to form single strands) 2. annealing, one primer binds to one DNA strand another binds to the complementary strand. The annealing sites of the primers are chosen so that they will prime DNA synthesis in the region of interest during extension 3. extension: The DNA polymerase synthesises a complementary strand. The enzyme reads the opposing strand sequence and extends the primers by adding nucleotides in the order in which they can pair.
 Nucleic acid hybridization assays with signal amplification A group of qualitative or semi-quantitative multiplex assays in which the DNA of the targeted HPV types is detected using mixtures of probes (probe cocktails) for several HPV types with similar clinical characteristics. None of the assays from this group allow the exact determination of HPV type(s) present in a clinical specimen, but show the results of the tested group of HPV types as positive or negative.
Nucleic acid hybridization assays with signal amplification A group of qualitative or semi-quantitative multiplex assays in which the DNA of the targeted HPV types is detected using mixtures of probes (probe cocktails) for several HPV types with similar clinical characteristics. None of the assays from this group allow the exact determination of HPV type(s) present in a clinical specimen, but show the results of the tested group of HPV types as positive or negative.
 HPV genotyping tests After PCR amplification, distinction of HPV types is achieved by reverse hybridization with type-specific probes using a variety of formats. With type-specific PCR, primers are chosen that will only amplify a single HPV genotype.
HPV genotyping tests After PCR amplification, distinction of HPV types is achieved by reverse hybridization with type-specific probes using a variety of formats. With type-specific PCR, primers are chosen that will only amplify a single HPV genotype.
 Sensitivity and specificity Test accuracy refers to: Sensitivity – proportion of truly ill people in the screened population who are identified as ill by the screening test Specificity – proportion of truly healthy people who are so identified by the screening test
Sensitivity and specificity Test accuracy refers to: Sensitivity – proportion of truly ill people in the screened population who are identified as ill by the screening test Specificity – proportion of truly healthy people who are so identified by the screening test
 Tests for CC screening As far as today there is sufficient evidence that screening for cancer precursors every 3 -5 years between the ages 35 and 64 years by conventional cytology in a high-quality programme reduces the incidence of invasive cancer by 80% or more among the women screened. HPV molecular tests are very sensitive, but they do not discriminate between transient and persistent infection and this means less specificity. HPV test was accepted for the triage of equivocal cytology (ASCUS) and follow up of treated lesions. New strategies can simplify the screening process or reduce the cost of screening. Recently, many wide, randomized clinical trials show that carcinogenic HPV DNA screening is more sensitive than cytological screening for detecting histological CIN 3. A negative HPV test provides long-term risk stratification; this high negative predictive value permits safe and cost-effective lengthening of the cervical screening interval when HPV testing is used. IARC Handbooks on Cancer Prevention 2005; www. ecca. info; Ronco G et al. Lancet Oncol. 2010; Mayrand MH et al. N Engl J Med. 2007; Bulk S et al. Int J Cancer. 2007; Naucler P et al. N Engl J Med. 2007; Sankaranarayanan R et al. N Engl J Med. 2009; Bulkmans NW et al. Lancet. 2007; Khan MJ et al. J Natl Cancer Inst. 2005; Dillner J et al. BMJ. 2008.
Tests for CC screening As far as today there is sufficient evidence that screening for cancer precursors every 3 -5 years between the ages 35 and 64 years by conventional cytology in a high-quality programme reduces the incidence of invasive cancer by 80% or more among the women screened. HPV molecular tests are very sensitive, but they do not discriminate between transient and persistent infection and this means less specificity. HPV test was accepted for the triage of equivocal cytology (ASCUS) and follow up of treated lesions. New strategies can simplify the screening process or reduce the cost of screening. Recently, many wide, randomized clinical trials show that carcinogenic HPV DNA screening is more sensitive than cytological screening for detecting histological CIN 3. A negative HPV test provides long-term risk stratification; this high negative predictive value permits safe and cost-effective lengthening of the cervical screening interval when HPV testing is used. IARC Handbooks on Cancer Prevention 2005; www. ecca. info; Ronco G et al. Lancet Oncol. 2010; Mayrand MH et al. N Engl J Med. 2007; Bulk S et al. Int J Cancer. 2007; Naucler P et al. N Engl J Med. 2007; Sankaranarayanan R et al. N Engl J Med. 2009; Bulkmans NW et al. Lancet. 2007; Khan MJ et al. J Natl Cancer Inst. 2005; Dillner J et al. BMJ. 2008.
 Screening algorithms: new perspective • The rationale for the change is to invert the current algorithm Pap Test>Colposcopy-HPV test, first running the most sensitive test (HPV test) and then the most specific test (Pap test). • HPV Vaccination will request further adjustments in screening algorithm in the next future.
Screening algorithms: new perspective • The rationale for the change is to invert the current algorithm Pap Test>Colposcopy-HPV test, first running the most sensitive test (HPV test) and then the most specific test (Pap test). • HPV Vaccination will request further adjustments in screening algorithm in the next future.
 Population based oncological screening
Population based oncological screening
 Definition of oncological screening “Screening” is an organized, controlled, systematic, public health intervention actively and periodically proposed, that involves the application of a relatively simple, innocuous, acceptable, ripetible, and relative cheap (for the organization, free for the involved population) test, to an asymptomatic and well defined population, to obtain detection of cancer at an earlier stage or of a precancerous lesion, with the goal to decrease the mortality and, if possible, the incidence of the tumor, with an effective and conservative treatment, possibly less aggressive than in clinically detected cases.
Definition of oncological screening “Screening” is an organized, controlled, systematic, public health intervention actively and periodically proposed, that involves the application of a relatively simple, innocuous, acceptable, ripetible, and relative cheap (for the organization, free for the involved population) test, to an asymptomatic and well defined population, to obtain detection of cancer at an earlier stage or of a precancerous lesion, with the goal to decrease the mortality and, if possible, the incidence of the tumor, with an effective and conservative treatment, possibly less aggressive than in clinically detected cases.
 Definition of population based screening A screening programme with individual identification and personal invitation of the elegible population. An optimal program is a screening program with quality assured at every step in the process: identification and personal invitation of the target population, performance of the test, compliance, call/recall system, second level diagnosis and treatment of the lesions detected, data registration, communication and training. von Karsa et al. , 2008, Antilla et al. , 2009
Definition of population based screening A screening programme with individual identification and personal invitation of the elegible population. An optimal program is a screening program with quality assured at every step in the process: identification and personal invitation of the target population, performance of the test, compliance, call/recall system, second level diagnosis and treatment of the lesions detected, data registration, communication and training. von Karsa et al. , 2008, Antilla et al. , 2009
 Cervical cancer screening Among all malignant tumours, cervical cancer is the one that can be most effectively controlled by screening. Detection of cytological abnormalities by microscopic examination of Pap smears, and subsequent treatment of women with high-grade cytological abnormalities avoids development of cancer. Miller, 1993
Cervical cancer screening Among all malignant tumours, cervical cancer is the one that can be most effectively controlled by screening. Detection of cytological abnormalities by microscopic examination of Pap smears, and subsequent treatment of women with high-grade cytological abnormalities avoids development of cancer. Miller, 1993
 Impact • If an optimal CCS policy is implemented in their countries, with adequate funds and supports, the figures of cervical cancer cases and deaths could substantially decrease. • As far as today many European countries have developed population-based screening programs for cervical cancers, although they differ greatly in terms of organizational characteristics, implementation stage, coverage and quality assurance. von Karsa et al. , 2008, Antilla et al. , 2009
Impact • If an optimal CCS policy is implemented in their countries, with adequate funds and supports, the figures of cervical cancer cases and deaths could substantially decrease. • As far as today many European countries have developed population-based screening programs for cervical cancers, although they differ greatly in terms of organizational characteristics, implementation stage, coverage and quality assurance. von Karsa et al. , 2008, Antilla et al. , 2009
 Finland • In Finland organised cervical screening was introduced in the early 1960 s; from the early 1970 s the screening invitational coverage has been almost complete. • During 1955– 1964 the incidence of invasive cervical cancer in Finland was at a level of 15 cases per 100, 000 woman-years age-adjusted to the world standard population; currently the age-adjusted rate is 4 cases per 100, 000 woman-years. • The age-standardized mortality rates decreased over 80% from the level of 7. 0 deaths per 100, 000 in early 1960 s to 1. 2 deaths per 100, 000 in the 1990’s (rates adjusted for age to the world standard population). Hristova & Hakama, 1997; Anttila & Laara, 2000
Finland • In Finland organised cervical screening was introduced in the early 1960 s; from the early 1970 s the screening invitational coverage has been almost complete. • During 1955– 1964 the incidence of invasive cervical cancer in Finland was at a level of 15 cases per 100, 000 woman-years age-adjusted to the world standard population; currently the age-adjusted rate is 4 cases per 100, 000 woman-years. • The age-standardized mortality rates decreased over 80% from the level of 7. 0 deaths per 100, 000 in early 1960 s to 1. 2 deaths per 100, 000 in the 1990’s (rates adjusted for age to the world standard population). Hristova & Hakama, 1997; Anttila & Laara, 2000
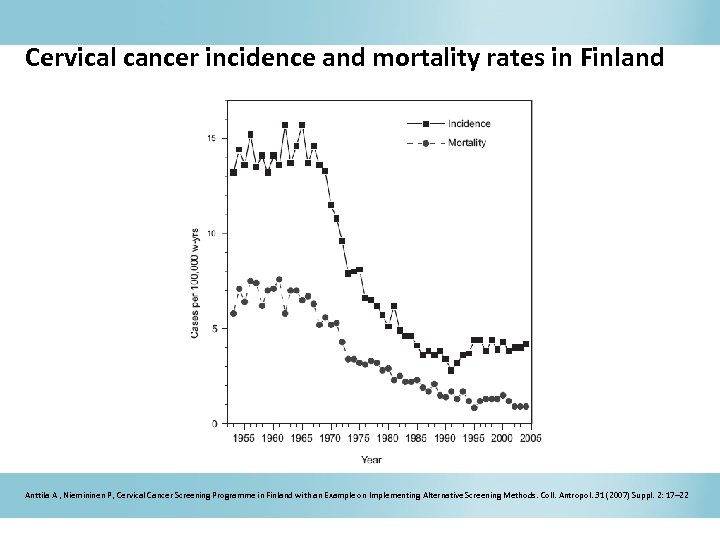 Cervical cancer incidence and mortality rates in Finland Anttila A , Niemininen P, Cervical Cancer Screening Programme in Finland with an Example on Implementing Alternative Screening Methods. Coll. Antropol. 31 (2007) Suppl. 2: 17– 22
Cervical cancer incidence and mortality rates in Finland Anttila A , Niemininen P, Cervical Cancer Screening Programme in Finland with an Example on Implementing Alternative Screening Methods. Coll. Antropol. 31 (2007) Suppl. 2: 17– 22
 UK Cytological screening was introduced in the 1960 s, but an organised programme including a call/recall system and quality assurance was not initiated until 1988. In the preceding years, mortality and incidence decreased by 1 -2% per year, whereas since 1988 the decrease has been about 7% per year, despite an increased underlying risk of disease inwomen born since 1940 Sasieni et al. , 1995; Quinn et al. , 1999; Sasieni & Adams, 1999; Peto et al. , 2004; Bray et al. , 2005; IARC, 2005
UK Cytological screening was introduced in the 1960 s, but an organised programme including a call/recall system and quality assurance was not initiated until 1988. In the preceding years, mortality and incidence decreased by 1 -2% per year, whereas since 1988 the decrease has been about 7% per year, despite an increased underlying risk of disease inwomen born since 1940 Sasieni et al. , 1995; Quinn et al. , 1999; Sasieni & Adams, 1999; Peto et al. , 2004; Bray et al. , 2005; IARC, 2005
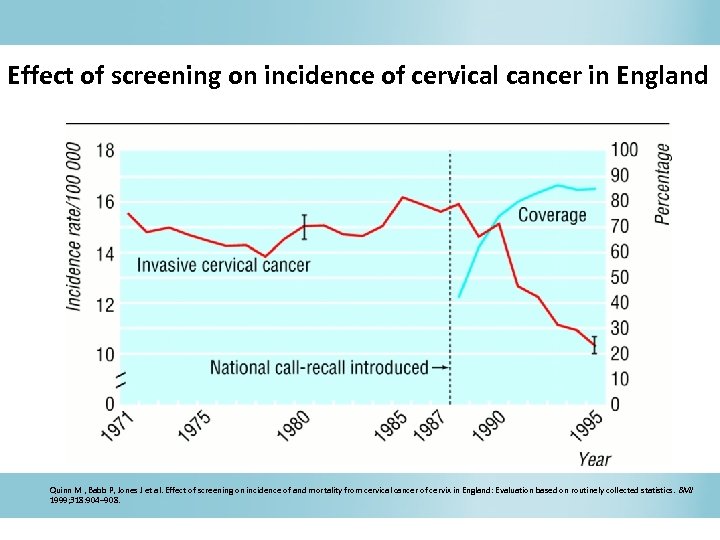 Effect of screening on incidence of cervical cancer in England Quinn M , Babb P, Jones J et al. Effect of screening on incidence of and mortality from cervical cancer of cervix in England: Evaluation based on routinely collected statistics. BMJ 1999; 318: 904– 908.
Effect of screening on incidence of cervical cancer in England Quinn M , Babb P, Jones J et al. Effect of screening on incidence of and mortality from cervical cancer of cervix in England: Evaluation based on routinely collected statistics. BMJ 1999; 318: 904– 908.
 Strategy The strategy of a screening programme must clearly establish: • Who is the target population o general population o certain age groups / gender categories o certain geographic regions o those with a certain risk level • What detection tests shall be used, in what order and at what intervals they shall be applied • Who shall apply the tests and where they shall be carried out • A screening programme must have a quality assurance structure
Strategy The strategy of a screening programme must clearly establish: • Who is the target population o general population o certain age groups / gender categories o certain geographic regions o those with a certain risk level • What detection tests shall be used, in what order and at what intervals they shall be applied • Who shall apply the tests and where they shall be carried out • A screening programme must have a quality assurance structure
 Hard to reach population Important problems are associated with conducting the screening on hard-toreach population. Definition of Hard to reach population (HTRP): those sections of the community that are difficult to involve in public participation. The term can be used to refer to minority group such as ethnic group, sometimes to hidden populations such as illegal immigrants, sometimes to unserved groups (no services available for these groups) or service “resistants” (people failing to access the services that are available). • no homogeneity in the term • certain groups may be hard to reach in some contexts or locations and not in others • the term can bring some prejudices about the people “hard to reach” • paradoxically top business women, can be “hard to reach” for cervical cancer screening, because of lack of time
Hard to reach population Important problems are associated with conducting the screening on hard-toreach population. Definition of Hard to reach population (HTRP): those sections of the community that are difficult to involve in public participation. The term can be used to refer to minority group such as ethnic group, sometimes to hidden populations such as illegal immigrants, sometimes to unserved groups (no services available for these groups) or service “resistants” (people failing to access the services that are available). • no homogeneity in the term • certain groups may be hard to reach in some contexts or locations and not in others • the term can bring some prejudices about the people “hard to reach” • paradoxically top business women, can be “hard to reach” for cervical cancer screening, because of lack of time
 Prevention of infection: vaccination
Prevention of infection: vaccination
 Prevention of infection: vaccination - 1 Prevention activities aimed at reducing the incidence or spreading of disease, or at least minimizing the consequences of disease or health disorders There are three levels of prevention: • Primary prevention – the aim is to prevent disease – as an example is vaccination or provizion of drinking water. . • Secondary prevention – a number of measures to allow early detection and rapid intervention – ex. screening cervical cancer • Tertiary prevention – reduces the number of complications and consequences of diseases and disorders of health - it increases the chance of extending life expectancy – ex. in oncology, follow-up of patients after therapy with the aim of early detection of relapse of disease.
Prevention of infection: vaccination - 1 Prevention activities aimed at reducing the incidence or spreading of disease, or at least minimizing the consequences of disease or health disorders There are three levels of prevention: • Primary prevention – the aim is to prevent disease – as an example is vaccination or provizion of drinking water. . • Secondary prevention – a number of measures to allow early detection and rapid intervention – ex. screening cervical cancer • Tertiary prevention – reduces the number of complications and consequences of diseases and disorders of health - it increases the chance of extending life expectancy – ex. in oncology, follow-up of patients after therapy with the aim of early detection of relapse of disease.
 Prevention of infection: vaccination - 2 The vaccination protects a person from future infection by the HPV high-risk types that can lead to cancer. It is not a vaccine against cancer itself. A person receives a series of three shots over a 6 -month period. Health professionals inject these virus-like particles (VLPs) into muscle tissue. These particles induce a strong immune response, vaccinated persons create specific antibodies that can detect, bind and neutralize the L 1 protein on the surface of HPV. Both available vaccines Gardasil/Silgard (quadrivalent – types 6, 11, 16 and 18) and Cervarix (bivalent – types 16 and 18) demonstrate also a certain degree of crossprotection towards HPV types genetically and antigenically related to those included in the vaccines, as follows: HPV 31, 33, 52, 58 similar with HPV 16; HPV 39, 45, 59 similar with HPV 18.
Prevention of infection: vaccination - 2 The vaccination protects a person from future infection by the HPV high-risk types that can lead to cancer. It is not a vaccine against cancer itself. A person receives a series of three shots over a 6 -month period. Health professionals inject these virus-like particles (VLPs) into muscle tissue. These particles induce a strong immune response, vaccinated persons create specific antibodies that can detect, bind and neutralize the L 1 protein on the surface of HPV. Both available vaccines Gardasil/Silgard (quadrivalent – types 6, 11, 16 and 18) and Cervarix (bivalent – types 16 and 18) demonstrate also a certain degree of crossprotection towards HPV types genetically and antigenically related to those included in the vaccines, as follows: HPV 31, 33, 52, 58 similar with HPV 16; HPV 39, 45, 59 similar with HPV 18.
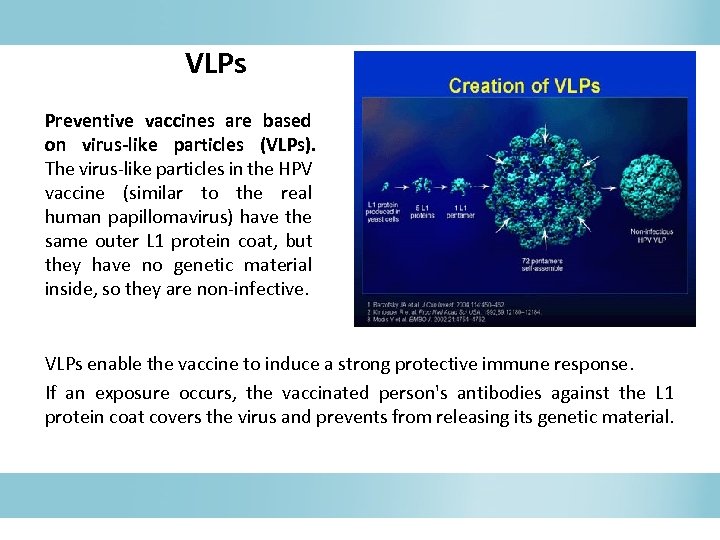 VLPs Preventive vaccines are based on virus-like particles (VLPs). The virus-like particles in the HPV vaccine (similar to the real human papillomavirus) have the same outer L 1 protein coat, but they have no genetic material inside, so they are non-infective. VLPs enable the vaccine to induce a strong protective immune response. If an exposure occurs, the vaccinated person's antibodies against the L 1 protein coat covers the virus and prevents from releasing its genetic material.
VLPs Preventive vaccines are based on virus-like particles (VLPs). The virus-like particles in the HPV vaccine (similar to the real human papillomavirus) have the same outer L 1 protein coat, but they have no genetic material inside, so they are non-infective. VLPs enable the vaccine to induce a strong protective immune response. If an exposure occurs, the vaccinated person's antibodies against the L 1 protein coat covers the virus and prevents from releasing its genetic material.
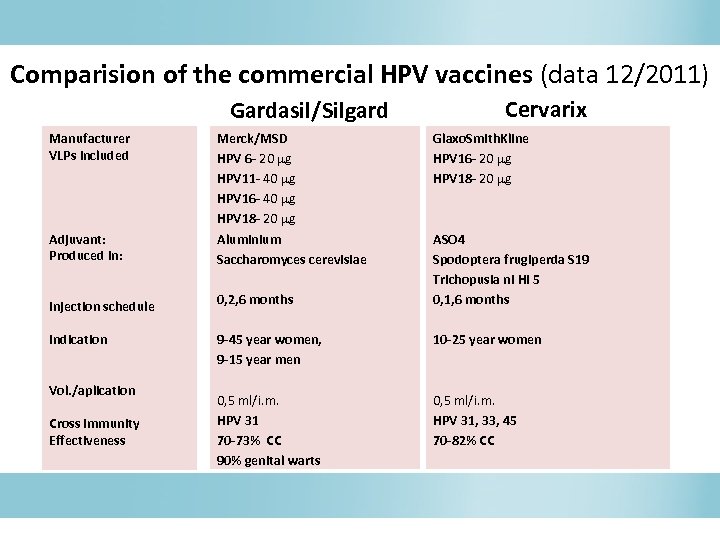 Comparision of the commercial HPV vaccines (data 12/2011) Gardasil/Silgard Manufacturer VLPs included Adjuvant: Produced in: Merck/MSD HPV 6 - 20 g HPV 11 - 40 g HPV 16 - 40 g HPV 18 - 20 g Aluminium Saccharomyces cerevisiae Cervarix Glaxo. Smith. Kline HPV 16 - 20 g HPV 18 - 20 g ASO 4 Spodoptera frugiperda S 19 Trichopusia ni Hi 5 0, 1, 6 months Injection schedule 0, 2, 6 months Indication 9 -45 year women, 9 -15 year men 10 -25 year women 0, 5 ml/i. m. HPV 31 70 -73% CC 90% genital warts 0, 5 ml/i. m. HPV 31, 33, 45 70 -82% CC Vol. /aplication Cross immunity Effectiveness
Comparision of the commercial HPV vaccines (data 12/2011) Gardasil/Silgard Manufacturer VLPs included Adjuvant: Produced in: Merck/MSD HPV 6 - 20 g HPV 11 - 40 g HPV 16 - 40 g HPV 18 - 20 g Aluminium Saccharomyces cerevisiae Cervarix Glaxo. Smith. Kline HPV 16 - 20 g HPV 18 - 20 g ASO 4 Spodoptera frugiperda S 19 Trichopusia ni Hi 5 0, 1, 6 months Injection schedule 0, 2, 6 months Indication 9 -45 year women, 9 -15 year men 10 -25 year women 0, 5 ml/i. m. HPV 31 70 -73% CC 90% genital warts 0, 5 ml/i. m. HPV 31, 33, 45 70 -82% CC Vol. /aplication Cross immunity Effectiveness
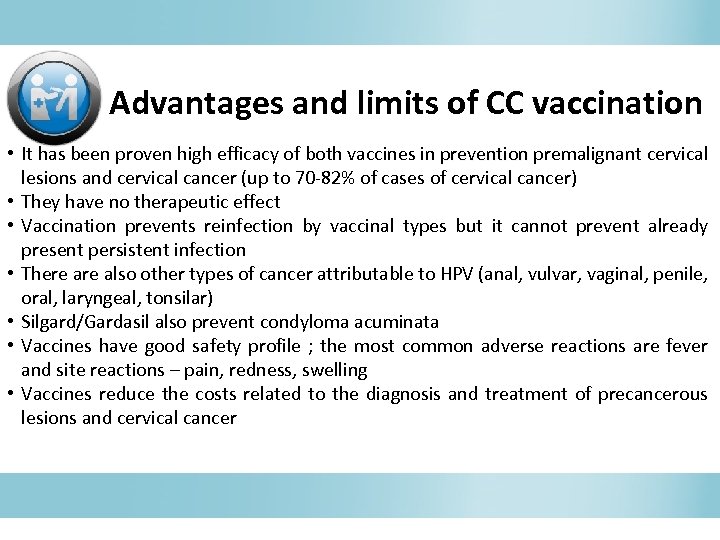 Advantages and limits of CC vaccination • It has been proven high efficacy of both vaccines in prevention premalignant cervical prevention lesions and cervical cancer (up to 70 -82% of cases of cervical cancer) • They have no therapeutic effect • Vaccination prevents reinfection by vaccinal types but it cannot prevent already present persistent infection • There also other types of cancer attributable to HPV (anal, vulvar, vaginal, penile, oral, laryngeal, tonsilar) • Silgard/Gardasil also prevent condyloma acuminata • Vaccines have good safety profile ; the most common adverse reactions are fever and site reactions – pain, redness, swelling • Vaccines reduce the costs related to the diagnosis and treatment of precancerous lesions and cervical cancer
Advantages and limits of CC vaccination • It has been proven high efficacy of both vaccines in prevention premalignant cervical prevention lesions and cervical cancer (up to 70 -82% of cases of cervical cancer) • They have no therapeutic effect • Vaccination prevents reinfection by vaccinal types but it cannot prevent already present persistent infection • There also other types of cancer attributable to HPV (anal, vulvar, vaginal, penile, oral, laryngeal, tonsilar) • Silgard/Gardasil also prevent condyloma acuminata • Vaccines have good safety profile ; the most common adverse reactions are fever and site reactions – pain, redness, swelling • Vaccines reduce the costs related to the diagnosis and treatment of precancerous lesions and cervical cancer
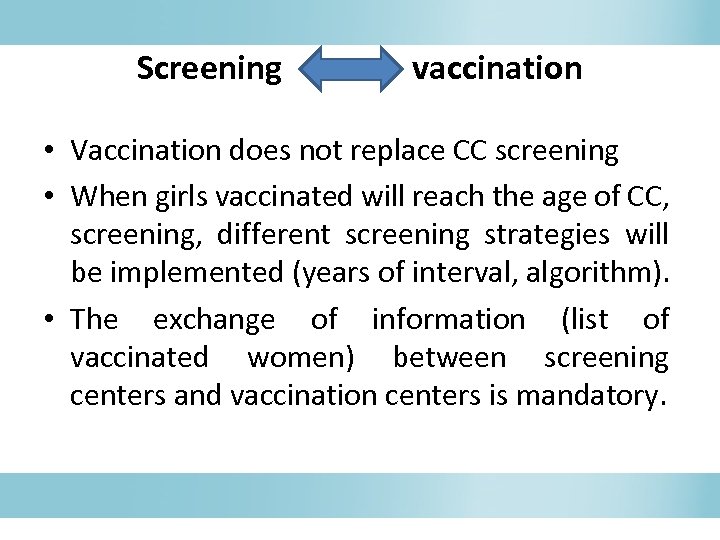 Screening vaccination • Vaccination does not replace CC screening • When girls vaccinated will reach the age of CC, screening, different screening strategies will be implemented (years of interval, algorithm). • The exchange of information (list of vaccinated women) between screening centers and vaccination centers is mandatory.
Screening vaccination • Vaccination does not replace CC screening • When girls vaccinated will reach the age of CC, screening, different screening strategies will be implemented (years of interval, algorithm). • The exchange of information (list of vaccinated women) between screening centers and vaccination centers is mandatory.
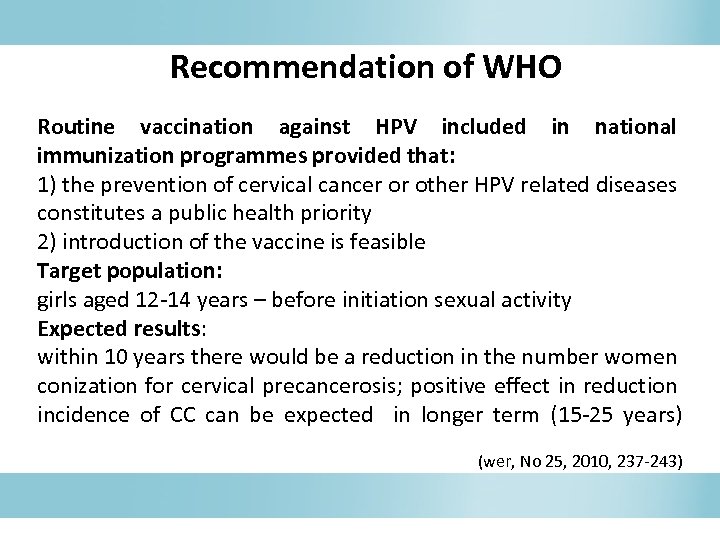 Recommendation of WHO Routine vaccination against HPV included in national immunization programmes provided that: 1) the prevention of cervical cancer or other HPV related diseases constitutes a public health priority 2) introduction of the vaccine is feasible Target population: girls aged 12 -14 years – before initiation sexual activity Expected results: within 10 years there would be a reduction in the number women conization for cervical precancerosis; positive effect in reduction incidence of CC can be expected in longer term (15 -25 years) (wer, No 25, 2010, 237 -243)
Recommendation of WHO Routine vaccination against HPV included in national immunization programmes provided that: 1) the prevention of cervical cancer or other HPV related diseases constitutes a public health priority 2) introduction of the vaccine is feasible Target population: girls aged 12 -14 years – before initiation sexual activity Expected results: within 10 years there would be a reduction in the number women conization for cervical precancerosis; positive effect in reduction incidence of CC can be expected in longer term (15 -25 years) (wer, No 25, 2010, 237 -243)
 Diagnosis and treatment of cervical pre-cancer lesions and cancer disease
Diagnosis and treatment of cervical pre-cancer lesions and cancer disease
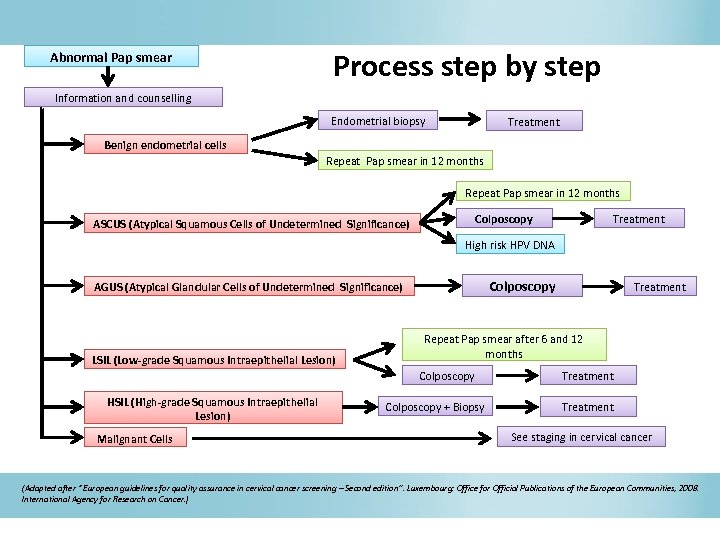 Abnormal Pap smear Process step by step Information and counselling Endometrial biopsy Treatment Benign endometrial cells Repeat Pap smear in 12 months Colposcopy ASCUS (Atypical Squamous Cells of Undetermined Significance) Treatment High risk HPV DNA Colposcopy AGUS (Atypical Glandular Cells of Undetermined Significance) LSIL (Low-grade Squamous Intraepithelial Lesion) Repeat Pap smear after 6 and 12 months Colposcopy HSIL (High-grade Squamous Intraepithelial Lesion) Malignant Cells Treatment Colposcopy + Biopsy Treatment See staging in cervical cancer (Adapted after “ European guidelines for quality assurance in cervical cancer screening – Second edition”. Luxembourg: Office for Official Publications of the European Communities, 2008. International Agency for Research on Cancer. )
Abnormal Pap smear Process step by step Information and counselling Endometrial biopsy Treatment Benign endometrial cells Repeat Pap smear in 12 months Colposcopy ASCUS (Atypical Squamous Cells of Undetermined Significance) Treatment High risk HPV DNA Colposcopy AGUS (Atypical Glandular Cells of Undetermined Significance) LSIL (Low-grade Squamous Intraepithelial Lesion) Repeat Pap smear after 6 and 12 months Colposcopy HSIL (High-grade Squamous Intraepithelial Lesion) Malignant Cells Treatment Colposcopy + Biopsy Treatment See staging in cervical cancer (Adapted after “ European guidelines for quality assurance in cervical cancer screening – Second edition”. Luxembourg: Office for Official Publications of the European Communities, 2008. International Agency for Research on Cancer. )
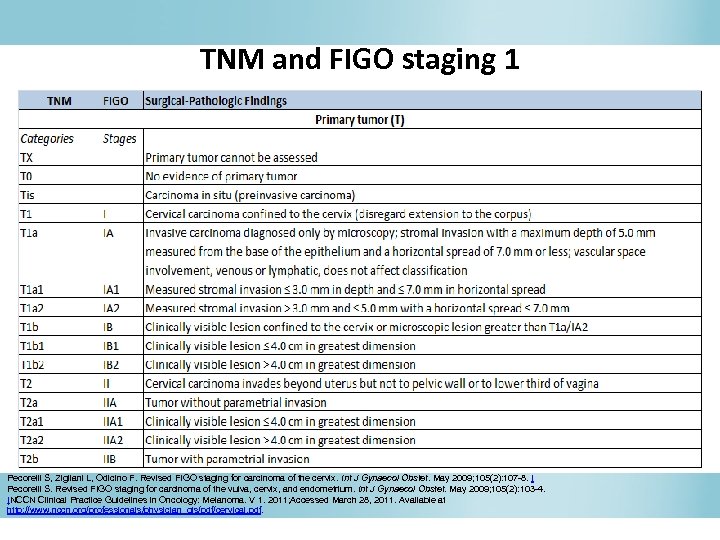 TNM and FIGO staging 1 Pecorelli S, Zigliani L, Odicino F. Revised FIGO staging for carcinoma of the cervix. Int J Gynaecol Obstet. May 2009; 105(2): 107 -8. [ Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. May 2009; 105(2): 103 -4. [NCCN Clinical Practice Guidelines in Oncology: Melanoma. V 1. 2011; Accessed March 28, 2011. Available at http: //www. nccn. org/professionals/physician_gls/pdf/cervical. pdf.
TNM and FIGO staging 1 Pecorelli S, Zigliani L, Odicino F. Revised FIGO staging for carcinoma of the cervix. Int J Gynaecol Obstet. May 2009; 105(2): 107 -8. [ Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. May 2009; 105(2): 103 -4. [NCCN Clinical Practice Guidelines in Oncology: Melanoma. V 1. 2011; Accessed March 28, 2011. Available at http: //www. nccn. org/professionals/physician_gls/pdf/cervical. pdf.
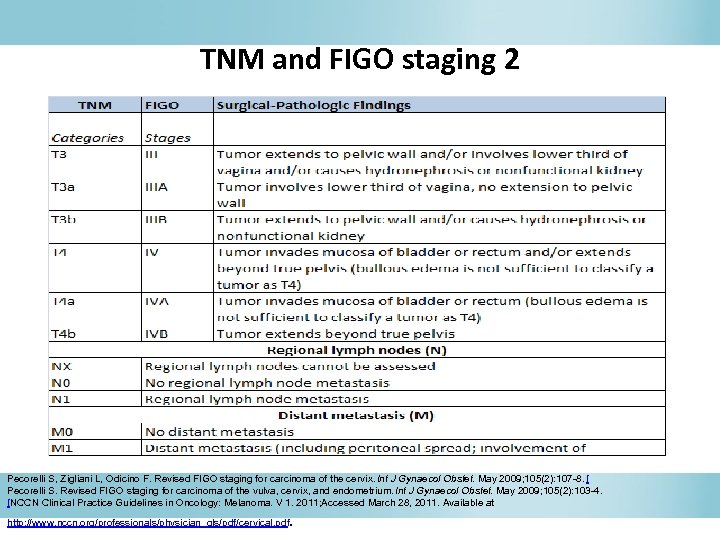 TNM and FIGO staging 2 Pecorelli S, Zigliani L, Odicino F. Revised FIGO staging for carcinoma of the cervix. Int J Gynaecol Obstet. May 2009; 105(2): 107 -8. [ Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. May 2009; 105(2): 103 -4. [NCCN Clinical Practice Guidelines in Oncology: Melanoma. V 1. 2011; Accessed March 28, 2011. Available at . http: //www. nccn. org/professionals/physician_gls/pdf/cervical. pdf
TNM and FIGO staging 2 Pecorelli S, Zigliani L, Odicino F. Revised FIGO staging for carcinoma of the cervix. Int J Gynaecol Obstet. May 2009; 105(2): 107 -8. [ Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. May 2009; 105(2): 103 -4. [NCCN Clinical Practice Guidelines in Oncology: Melanoma. V 1. 2011; Accessed March 28, 2011. Available at . http: //www. nccn. org/professionals/physician_gls/pdf/cervical. pdf
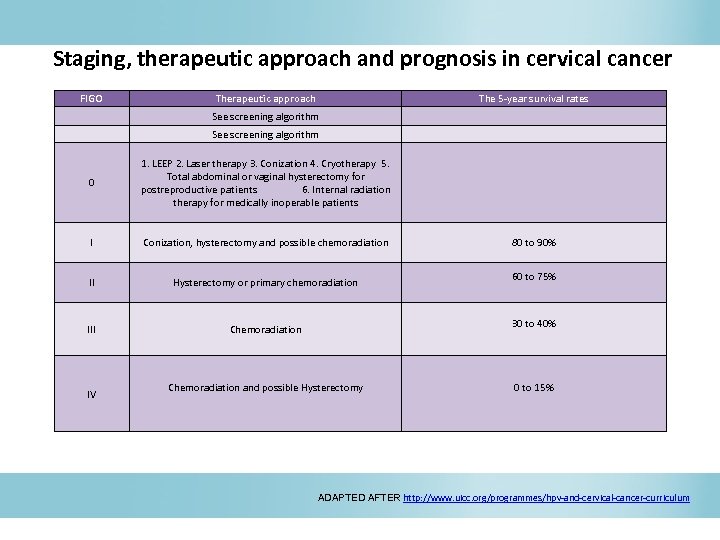 Staging, therapeutic approach and prognosis in cervical cancer FIGO Therapeutic approach See screening algorithm 0 1. LEEP 2. Laser therapy 3. Conization 4. Cryotherapy 5. Total abdominal or vaginal hysterectomy for postreproductive patients 6. Internal radiation therapy for medically inoperable patients I Conization, hysterectomy and possible chemoradiation II Hysterectomy or primary chemoradiation III Chemoradiation IV The 5 -year survival rates 80 to 90% 60 to 75% 30 to 40% Chemoradiation and possible Hysterectomy 0 to 15% ADAPTED AFTER http: //www. uicc. org/programmes/hpv-and-cervical-cancer-curriculum
Staging, therapeutic approach and prognosis in cervical cancer FIGO Therapeutic approach See screening algorithm 0 1. LEEP 2. Laser therapy 3. Conization 4. Cryotherapy 5. Total abdominal or vaginal hysterectomy for postreproductive patients 6. Internal radiation therapy for medically inoperable patients I Conization, hysterectomy and possible chemoradiation II Hysterectomy or primary chemoradiation III Chemoradiation IV The 5 -year survival rates 80 to 90% 60 to 75% 30 to 40% Chemoradiation and possible Hysterectomy 0 to 15% ADAPTED AFTER http: //www. uicc. org/programmes/hpv-and-cervical-cancer-curriculum
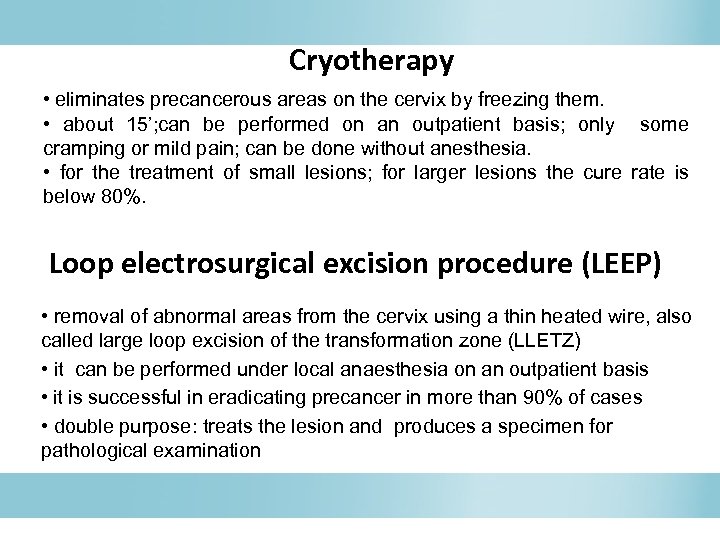 Cryotherapy • eliminates precancerous areas on the cervix by freezing them. • about 15’; can be performed on an outpatient basis; only some cramping or mild pain; can be done without anesthesia. • for the treatment of small lesions; for larger lesions the cure rate is below 80%. Loop electrosurgical excision procedure (LEEP) • removal of abnormal areas from the cervix using a thin heated wire, also called large loop excision of the transformation zone (LLETZ) • it can be performed under local anaesthesia on an outpatient basis • it is successful in eradicating precancer in more than 90% of cases • double purpose: treats the lesion and produces a specimen for pathological examination
Cryotherapy • eliminates precancerous areas on the cervix by freezing them. • about 15’; can be performed on an outpatient basis; only some cramping or mild pain; can be done without anesthesia. • for the treatment of small lesions; for larger lesions the cure rate is below 80%. Loop electrosurgical excision procedure (LEEP) • removal of abnormal areas from the cervix using a thin heated wire, also called large loop excision of the transformation zone (LLETZ) • it can be performed under local anaesthesia on an outpatient basis • it is successful in eradicating precancer in more than 90% of cases • double purpose: treats the lesion and produces a specimen for pathological examination
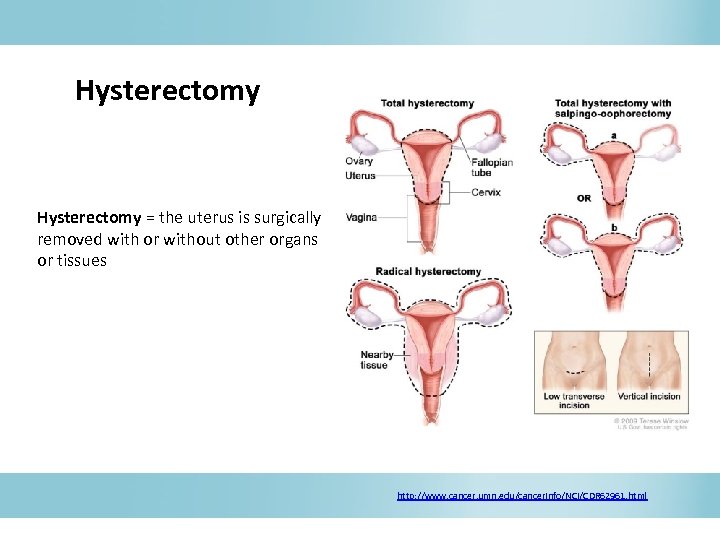 Hysterectomy = the uterus is surgically removed with or without other organs or tissues http: //www. cancer. umn. edu/cancerinfo/NCI/CDR 62961. html
Hysterectomy = the uterus is surgically removed with or without other organs or tissues http: //www. cancer. umn. edu/cancerinfo/NCI/CDR 62961. html
 Radiation therapy • Uses high-energy x-rays – kills cancer cells or keeps them from growing • Two types of radiation therapy: o External radiation therapy - a machine outside the body sends radiation toward the cancer. o Internal radiation therapy - a radioactive substance in needles, seeds, wires, or catheters that are placed directly into or near the cancer. Chemotherapy • Uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. • Taken by mouth or injected into a vein or muscle - enters the bloodstream, reaches cancer cells throughout the body (systemic chemotherapy). • Placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, mainly affects cancer cells in those areas (regional chemotherapy).
Radiation therapy • Uses high-energy x-rays – kills cancer cells or keeps them from growing • Two types of radiation therapy: o External radiation therapy - a machine outside the body sends radiation toward the cancer. o Internal radiation therapy - a radioactive substance in needles, seeds, wires, or catheters that are placed directly into or near the cancer. Chemotherapy • Uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. • Taken by mouth or injected into a vein or muscle - enters the bloodstream, reaches cancer cells throughout the body (systemic chemotherapy). • Placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, mainly affects cancer cells in those areas (regional chemotherapy).
 Resources • • • • • World Health Organization (http: //www. who. int/reproductivehealth/topics/cancers/en/index. html) Union for International Cancer Control (http: //www. uicc. org/programmes/hpv-and-cervical-cancer-curriculum) Merck manual (http: //www. merckmanuals. com/professional/gynecology_and_obstetrics/gynecologic_tumors/cervical_cancer. html) Center for Disease Control and Prevention (http: //www. cdc. gov/cancer/cervical/) National Cancer Institute (http: //cancer. gov/cancertopics/types/cervical) European guidelines for quality assurance in cervical cancer screening; Second Edition; International Agency for Research on Cancer Research UK (http: //cancerhelp. cancerresearchuk. org/type/cervical-cancer/) RHO/PATH (http: //www. rho. org/) American Cancer Society (http: //www. cancer. org/cancer/cervicalcancer/index) Alliance for Cervical Cancer Prevention (http: //www. alliance-cxca. org/ ) Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2009. Atlanta: U. S. Department of Health and Human Services; 2010. Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2010. MMWR 2010; 59; 69 WHO/ICO Information Centre on HPV and Cervical Cancer (HPV Information Centre). Human Papillomavirus and Related Cancers in Europe. Summary Report 2010. Available at www. who. int/ hpvcentre Human papillomavirus vaccines - WHO position paper , Weekly epidemiological record, WHO, 10 APRIL 2009, No. 15, 2009, 84, 118– 131, (http: //www. who. int/wer) WHO HPV Lab. Net Newsletter No. 8, 18 July 2011 Shepherd JP, Frampton GK, Harris P, Interventions for encouraging sexual behaviours intended to prevent cervical cancer, Cochrane Database Syst Rev. 2011 Apr 13; (4): CD 001035. Weinstein LC, Buchanan EM, Hillson C, Chambers CV, Screening and prevention: cervical cancer, Prim Care. 2009 Sep; 36(3): 559 -74. Kasap B, Yetimalar H, Keklik A, Yildiz A, Cukurova K, Soylu F. , Prevalence and risk factors for human papillomavirus DNA in cervical cytology, Eur J Obstet Gynecol Reprod Biol. 2011 Nov; 159(1): 168 -71. Gonzalez-Bosquet E, Selva L, Sabria J, Pallares L, Almeida L, Muñoz-Almagro C, Lailla JM, Predictive factors for the detection of CIN II-III in the follow-up of women with CIN I, Eur J Gynaecol Oncol. 2010; 31(4): 369 -71.
Resources • • • • • World Health Organization (http: //www. who. int/reproductivehealth/topics/cancers/en/index. html) Union for International Cancer Control (http: //www. uicc. org/programmes/hpv-and-cervical-cancer-curriculum) Merck manual (http: //www. merckmanuals. com/professional/gynecology_and_obstetrics/gynecologic_tumors/cervical_cancer. html) Center for Disease Control and Prevention (http: //www. cdc. gov/cancer/cervical/) National Cancer Institute (http: //cancer. gov/cancertopics/types/cervical) European guidelines for quality assurance in cervical cancer screening; Second Edition; International Agency for Research on Cancer Research UK (http: //cancerhelp. cancerresearchuk. org/type/cervical-cancer/) RHO/PATH (http: //www. rho. org/) American Cancer Society (http: //www. cancer. org/cancer/cervicalcancer/index) Alliance for Cervical Cancer Prevention (http: //www. alliance-cxca. org/ ) Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2009. Atlanta: U. S. Department of Health and Human Services; 2010. Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2010. MMWR 2010; 59; 69 WHO/ICO Information Centre on HPV and Cervical Cancer (HPV Information Centre). Human Papillomavirus and Related Cancers in Europe. Summary Report 2010. Available at www. who. int/ hpvcentre Human papillomavirus vaccines - WHO position paper , Weekly epidemiological record, WHO, 10 APRIL 2009, No. 15, 2009, 84, 118– 131, (http: //www. who. int/wer) WHO HPV Lab. Net Newsletter No. 8, 18 July 2011 Shepherd JP, Frampton GK, Harris P, Interventions for encouraging sexual behaviours intended to prevent cervical cancer, Cochrane Database Syst Rev. 2011 Apr 13; (4): CD 001035. Weinstein LC, Buchanan EM, Hillson C, Chambers CV, Screening and prevention: cervical cancer, Prim Care. 2009 Sep; 36(3): 559 -74. Kasap B, Yetimalar H, Keklik A, Yildiz A, Cukurova K, Soylu F. , Prevalence and risk factors for human papillomavirus DNA in cervical cytology, Eur J Obstet Gynecol Reprod Biol. 2011 Nov; 159(1): 168 -71. Gonzalez-Bosquet E, Selva L, Sabria J, Pallares L, Almeida L, Muñoz-Almagro C, Lailla JM, Predictive factors for the detection of CIN II-III in the follow-up of women with CIN I, Eur J Gynaecol Oncol. 2010; 31(4): 369 -71.


