27d41f56683cce9ca511395e981b0e91.ppt
- Количество слайдов: 36
A Clinical Balancing Act: Honoring the DNR Decision While Preserving the Option of Donation Brian J. Kimbrell, MD, FACS Trauma / Surgical Critical Care Director St. John’s Regional Medical Center Oxnard, CA
“How To Be” • Being in Action! • The Answers Are In the Room • “Report out” on Questions to Run-on: – Scribe – Spokesperson • All Teach / All Learn
Question to Run-On What ideas would most help you in your work with patients and families facing end-of-life decisions?
A Clinical Balancing Act: Honoring the DNR Decision While Preserving the Option of Donation Brian J. Kimbrell, MD, FACS Trauma / Surgical Critical Care Director St. John’s Regional Medical Center Oxnard, CA

DNR Decision What does the DNR decision mean to the family? • • • No Chest Compressions? No Shock? No Medications? No Labs? No Fluids? “Do not harm? ” or “Do not treat? ”
DNR Decision What does the DNR decision mean to the healthcare team? • Routine decision in the Critical Care Unit • Interpreting DNR decision varies by hospital, unit, physician, nurse
Donation Decision Understanding the donation option clinically: • Maintaining blood pressure • Normalizing electrolytes • Managing oxygenation and organ perfusion • Balancing Intake and Output • Assessing brain death accurately How can a family give the gift of life when the organs are not preserved for
Balancing DNR and Donation Devastating Traumatic Brain Injury (TBI) + Overall Clinical Deterioration + DNR Decision by Next-of-Kin + Fatal Diagnosis (Brain Death? ) “Step Down” in clinical management? - or - Maintain clinical management and
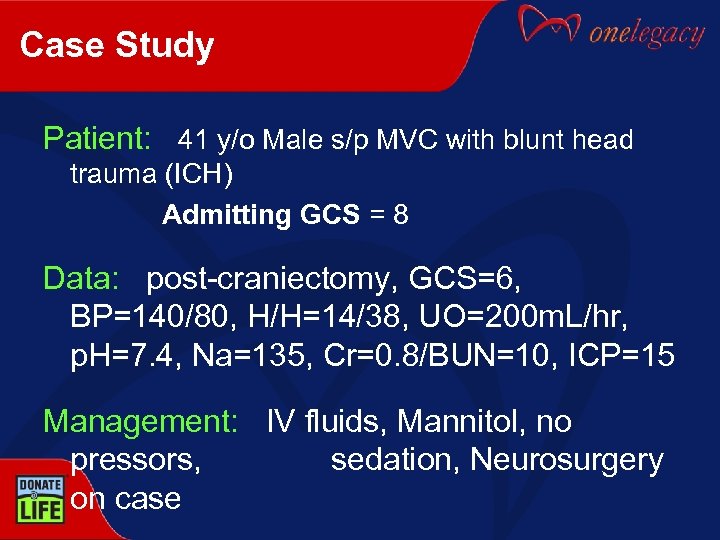
Case Study Patient: 41 y/o Male s/p MVC with blunt head trauma (ICH) Admitting GCS = 8 Data: post-craniectomy, GCS=6, BP=140/80, H/H=14/38, UO=200 m. L/hr, p. H=7. 4, Na=135, Cr=0. 8/BUN=10, ICP=15 Management: IV fluids, Mannitol, no pressors, sedation, Neurosurgery on case
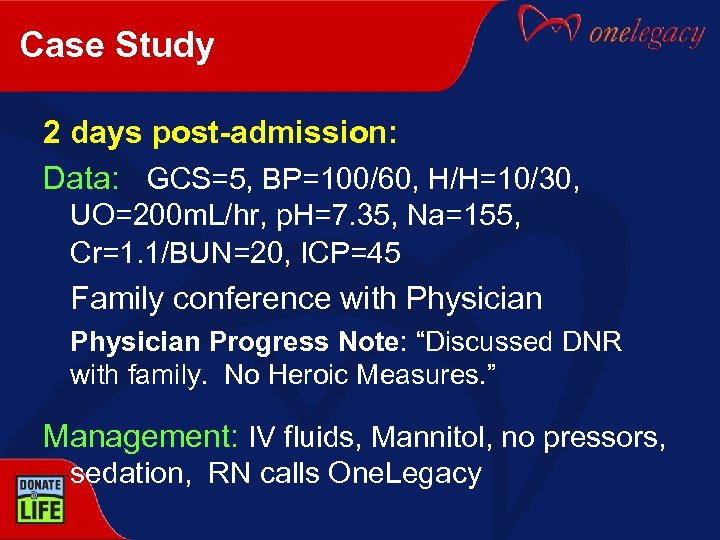
Case Study 2 days post-admission: Data: GCS=5, BP=100/60, H/H=10/30, UO=200 m. L/hr, p. H=7. 35, Na=155, Cr=1. 1/BUN=20, ICP=45 Family conference with Physician Progress Note: “Discussed DNR with family. No Heroic Measures. ” Management: IV fluids, Mannitol, no pressors, sedation, RN calls One. Legacy
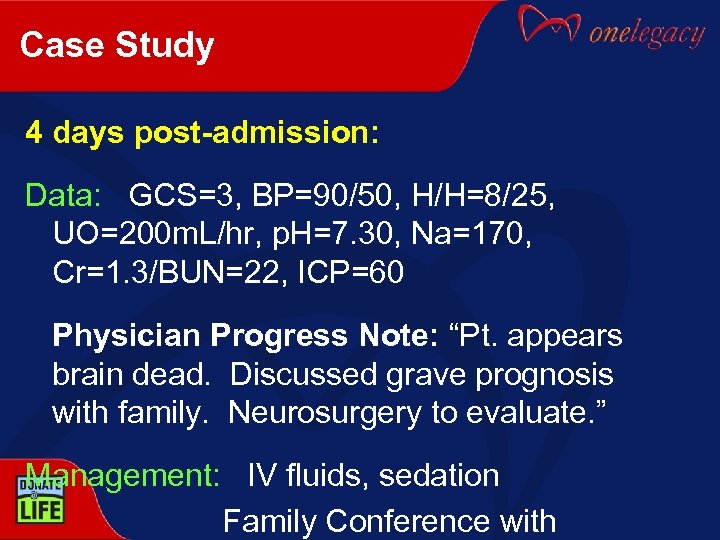
Case Study 4 days post-admission: Data: GCS=3, BP=90/50, H/H=8/25, UO=200 m. L/hr, p. H=7. 30, Na=170, Cr=1. 3/BUN=22, ICP=60 Physician Progress Note: “Pt. appears brain dead. Discussed grave prognosis with family. Neurosurgery to evaluate. ” Management: IV fluids, sedation Family Conference with
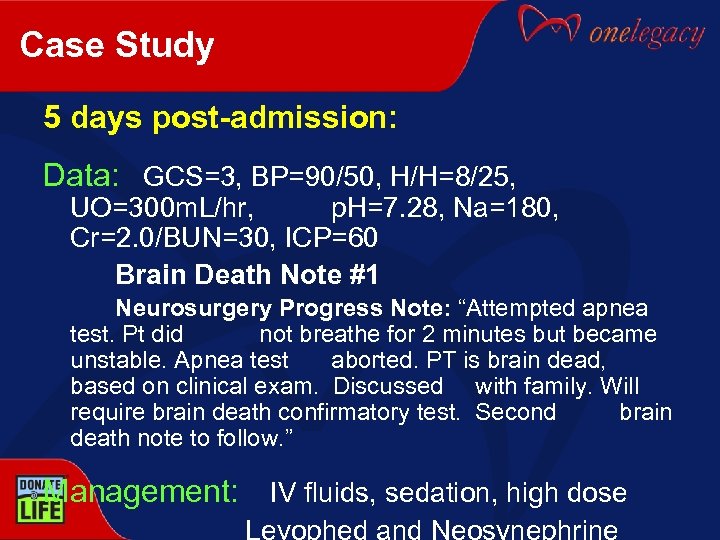
Case Study 5 days post-admission: Data: GCS=3, BP=90/50, H/H=8/25, UO=300 m. L/hr, p. H=7. 28, Na=180, Cr=2. 0/BUN=30, ICP=60 Brain Death Note #1 Neurosurgery Progress Note: “Attempted apnea test. Pt did not breathe for 2 minutes but became unstable. Apnea test aborted. PT is brain dead, based on clinical exam. Discussed with family. Will require brain death confirmatory test. Second brain death note to follow. ” Management: IV fluids, sedation, high dose
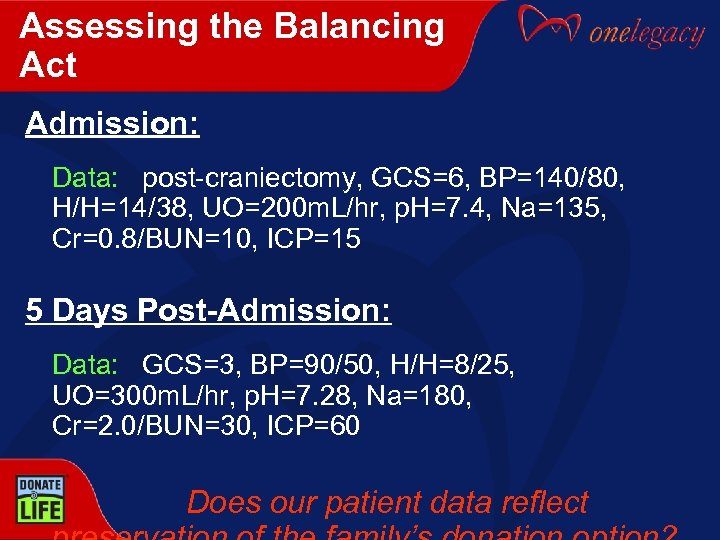
Assessing the Balancing Act Admission: Data: post-craniectomy, GCS=6, BP=140/80, H/H=14/38, UO=200 m. L/hr, p. H=7. 4, Na=135, Cr=0. 8/BUN=10, ICP=15 5 Days Post-Admission: Data: GCS=3, BP=90/50, H/H=8/25, UO=300 m. L/hr, p. H=7. 28, Na=180, Cr=2. 0/BUN=30, ICP=60 Does our patient data reflect
Assessing the Balancing Act Devastating TBI + Overall Clinical Deterioration + DNR Decision + Fatal Diagnosis (Brain Death) Maintain clinical management and prevent secondary injury to organs.
Pathophysiology of Traumatic Brain Injury Physiologic collapse frequently accompanies TBI: Hypotension Endocrine Dysfunction Pulmonary Dysfunction Hematologic Dysfunction
Pathophysiology of Traumatic Brain Injury Hypotension: • “Autonomic storms” • Systemic and pulmonary vasoconstriction • Associated with herniation • Can recur unpredictably • Smooth muscle ATP depleted = vasomotor hypotension • Diuretics
Pathophysiology of Traumatic Brain Injury Hypotension: • • • Closely monitor Intake and Output – DI? Anticipate BP spike followed by BP drop Consider Fluid Resuscitation Titrate Vasopressors Consider Hormone replacement – T 4
Pathophysiology of Traumatic Brain Injury Endocrine Dysfunction: • Hypothalamic injury -> pituitary dysfunction • Thyroid dysfunction – T 4 Infusion • Glycemic control disrupted – Insulin infusion
Pathophysiology of Traumatic Brain Injury Endocrine Dysfunction: • Relative deficiency of corticosteroids – Solumedrol Infusion • Reduction of Antidiuretic Hormone / Diabetes Insipidous – ADH, Vasopressin Infusion
Pathophysiology of Traumatic Brain Injury Pulmonary Dysfunction: • Neurogenic pulmonary edema – Multifactorial – Systemic hypertension + LV dysfunction • Primary pneumatocyte dysfunction
Pathophysiology of Traumatic Brain Injury Pulmonary Dysfunction: • Iatrogenic injury due to aggressive resuscitation • Exacerbated by intubation, aspiration, atelectasis • Concurrent blunt lung injury common – Parenchymal injury problematic in immunosuppressed recipients
Pathophysiology of Traumatic Brain Injury Hematologic Dysfunction: • Thrombocytopenia – Platelets as needed • Coagulopathy/DIC – FFP / Cryo as needed • Hypothermia – Keep them warm!

What Are Traumatic Brain Injury Guidelines? Hospital approved guidelines for treating patients with Traumatic Brain Injury 23
What Are Traumatic Brain Injury Guidelines? Prevent secondary injury, even with grave prognosis • Secondary injury includes other organs, as well as the brain Maintain Organ Perfusion • Volume Load • Monitor & Maintain adequate CVP, MAP • Oxygenation 24
What Are Traumatic Brain Injury Guidelines? Continuous fluid resuscitation • Correct electrolyte abnormalities Rule of 100’s: • SBP >100 mm Hg • U/O >100 ml/hr • Pa. O 2 >100 25
Why Implement TBI Guidelines? • Ensure consistent management of the critically ill patient • Maintain homeostasis for accurate brain death assessment • Prevent “secondary injury” to organs, even with grave prognosis • Provide a clinical bridge between determination of brain death and family’s decision on donation 26
Aggressive Organ Donor Management Significantly Increases the Number of Organs Available for Transplantation (Salim et al. J Trauma 2005; 58: 991 -994) • LAC + USC Standardized organ donor management protocol • Before-after study (January 1998) of ADM institution – January 1995 -December 2002
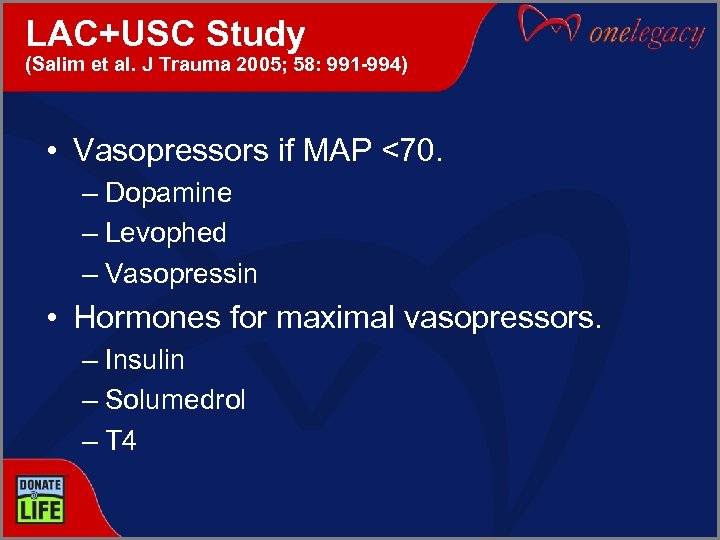
LAC+USC Study (Salim et al. J Trauma 2005; 58: 991 -994) • Vasopressors if MAP <70. – Dopamine – Levophed – Vasopressin • Hormones for maximal vasopressors. – Insulin – Solumedrol – T 4
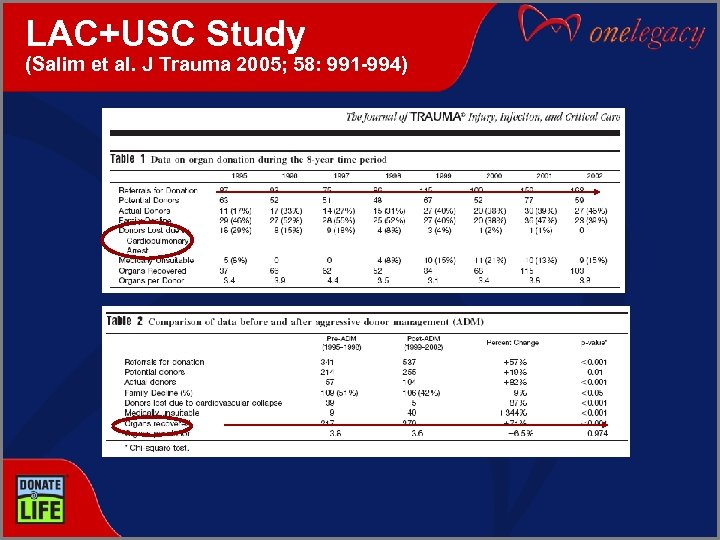
LAC+USC Study (Salim et al. J Trauma 2005; 58: 991 -994)
Results • 878 patients referred, 460 (53. 4%) patients potential organ donors and 161 (34. 3%) actual donors. • # patients referred increased 57% • # of potential donors increased 19% • # of actual donors increased 82% • # of patients lost to cardiovascular collapse decreased 87% • # of organs recovered increased 71%

How to Implement TBI Guidelines in Your Hospital? Clinical Educator Critical Practice Committee Critical Care Leadership Critical Care Physicians or Medical Director Sample Guidelines available at: www. onelegacy. org
DNR Decision What does the DNR decision mean to the family? • • • No Chest Compressions? No Shock? No Medications? No Labs? No Fluids? “Do not harm? ” or “Do not treat? ”
Summary • Critical care teams can honor the DNR decision while preserving the option of donation. • Pathophysiology of TBI can be anticipated and treated. • TBI Guidelines can be implemented to prevent “step down” in clinical management, and preserve the family’s donation option.
Question to Run On What ideas would most help you in your work with patients and families facing end-of-life decisions?

Transition to Breakout Session #2 Next Breakout Session starts at 11: 30 am Please see agenda for specific room locations Enjoy the Learning!
Transition to Lunch is from 12: 30 – 1: 30 Crystal Ballroom, main level Open seating Bon Appétit!
27d41f56683cce9ca511395e981b0e91.ppt