10ad811ff611be6095502445d44e7dc1.ppt
- Количество слайдов: 61
 5 The Integumentary System Power. Point® Lecture Presentations prepared by Jason La. Pres Lone Star College—North Harris © 2012 Pearson Education, Inc.
5 The Integumentary System Power. Point® Lecture Presentations prepared by Jason La. Pres Lone Star College—North Harris © 2012 Pearson Education, Inc.
 An Introduction to the Integumentary System • Integument is the largest system of the body • Dermatology: study of integumentary system and associated pathologies © 2012 Pearson Education, Inc.
An Introduction to the Integumentary System • Integument is the largest system of the body • Dermatology: study of integumentary system and associated pathologies © 2012 Pearson Education, Inc.
 Integumentary System: Overall Structure 1. Cutaneous membrane or skin ØEpidermis ØDermis v. Hypodermis-not technically part of skin 2. Accessory structures ØHair ØNails ØSweat Glands (Sudoriferous glands) ØSebaceous Glands (Oil glands) © 2012 Pearson Education, Inc.
Integumentary System: Overall Structure 1. Cutaneous membrane or skin ØEpidermis ØDermis v. Hypodermis-not technically part of skin 2. Accessory structures ØHair ØNails ØSweat Glands (Sudoriferous glands) ØSebaceous Glands (Oil glands) © 2012 Pearson Education, Inc.
 Cutaneous Membrane (Skin) Epidermis − Superficial epithelium Dermis − Deeper connective tissue − Papillary Layer − Reticular layer © 2012 Pearson Education, Inc.
Cutaneous Membrane (Skin) Epidermis − Superficial epithelium Dermis − Deeper connective tissue − Papillary Layer − Reticular layer © 2012 Pearson Education, Inc.
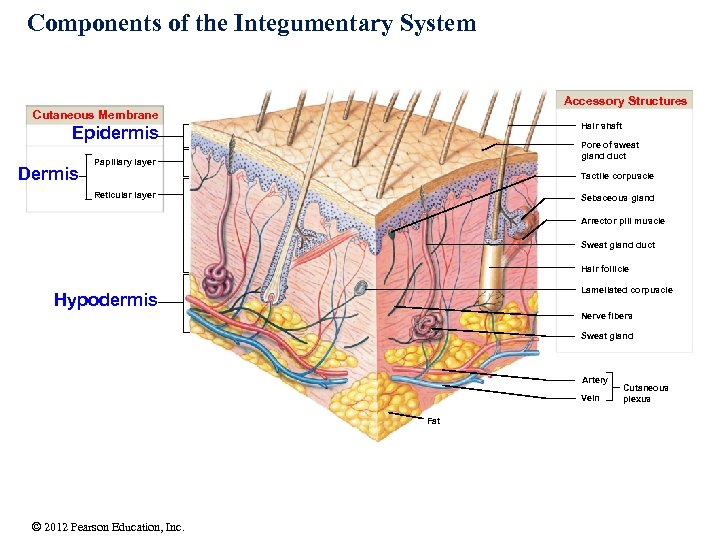 Components of the Integumentary System Accessory Structures Cutaneous Membrane Hair shaft Epidermis Dermis Pore of sweat gland duct Papillary layer Tactile corpuscle Reticular layer Sebaceous gland Arrector pili muscle Sweat gland duct Hair follicle Lamellated corpuscle Hypodermis Nerve fibers Sweat gland Artery Vein Fat © 2012 Pearson Education, Inc. Cutaneous plexus
Components of the Integumentary System Accessory Structures Cutaneous Membrane Hair shaft Epidermis Dermis Pore of sweat gland duct Papillary layer Tactile corpuscle Reticular layer Sebaceous gland Arrector pili muscle Sweat gland duct Hair follicle Lamellated corpuscle Hypodermis Nerve fibers Sweat gland Artery Vein Fat © 2012 Pearson Education, Inc. Cutaneous plexus
 Functions of the skin 1. Protection – Stratified epidermis…protects from abrasions – Keratin…water proofing – Melanin…protects from UV – WBC in dermis…immunity 2. Temperature regulation – Sweat…evaporates to cause cooling – Blood vessels…vasoconstriction/vasodilation to regulate heat loss from warm blood in the skin – Arrector pili…goose bumps © 2012 Pearson Education, Inc.
Functions of the skin 1. Protection – Stratified epidermis…protects from abrasions – Keratin…water proofing – Melanin…protects from UV – WBC in dermis…immunity 2. Temperature regulation – Sweat…evaporates to cause cooling – Blood vessels…vasoconstriction/vasodilation to regulate heat loss from warm blood in the skin – Arrector pili…goose bumps © 2012 Pearson Education, Inc.
 Functions of the skin 3. Sensation – Nerves to sense touch, temperature and injury (pain) 4. Excretion – Sweat…salts, organic substances 5. Synthesis of vitamin D – For absorption of calcium © 2012 Pearson Education, Inc.
Functions of the skin 3. Sensation – Nerves to sense touch, temperature and injury (pain) 4. Excretion – Sweat…salts, organic substances 5. Synthesis of vitamin D – For absorption of calcium © 2012 Pearson Education, Inc.
 The Epidermis • Is an avascular, keratinized stratified squamous epithelium • Nutrients and oxygen diffuse from capillaries in the dermis • Top layer of dead cells: thickness varies with body location © 2012 Pearson Education, Inc.
The Epidermis • Is an avascular, keratinized stratified squamous epithelium • Nutrients and oxygen diffuse from capillaries in the dermis • Top layer of dead cells: thickness varies with body location © 2012 Pearson Education, Inc.
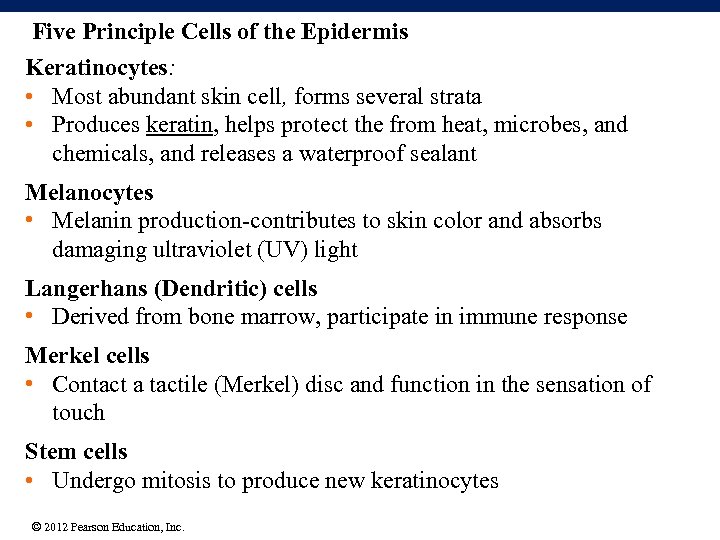 Five Principle Cells of the Epidermis Keratinocytes: • Most abundant skin cell, forms several strata • Produces keratin, helps protect the from heat, microbes, and chemicals, and releases a waterproof sealant Melanocytes • Melanin production-contributes to skin color and absorbs damaging ultraviolet (UV) light Langerhans (Dendritic) cells • Derived from bone marrow, participate in immune response Merkel cells • Contact a tactile (Merkel) disc and function in the sensation of touch Stem cells • Undergo mitosis to produce new keratinocytes © 2012 Pearson Education, Inc.
Five Principle Cells of the Epidermis Keratinocytes: • Most abundant skin cell, forms several strata • Produces keratin, helps protect the from heat, microbes, and chemicals, and releases a waterproof sealant Melanocytes • Melanin production-contributes to skin color and absorbs damaging ultraviolet (UV) light Langerhans (Dendritic) cells • Derived from bone marrow, participate in immune response Merkel cells • Contact a tactile (Merkel) disc and function in the sensation of touch Stem cells • Undergo mitosis to produce new keratinocytes © 2012 Pearson Education, Inc.
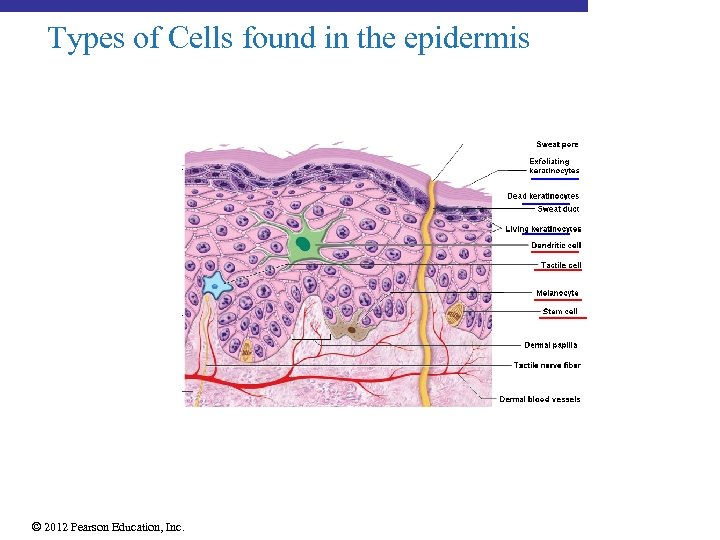 Types of Cells found in the epidermis © 2012 Pearson Education, Inc.
Types of Cells found in the epidermis © 2012 Pearson Education, Inc.
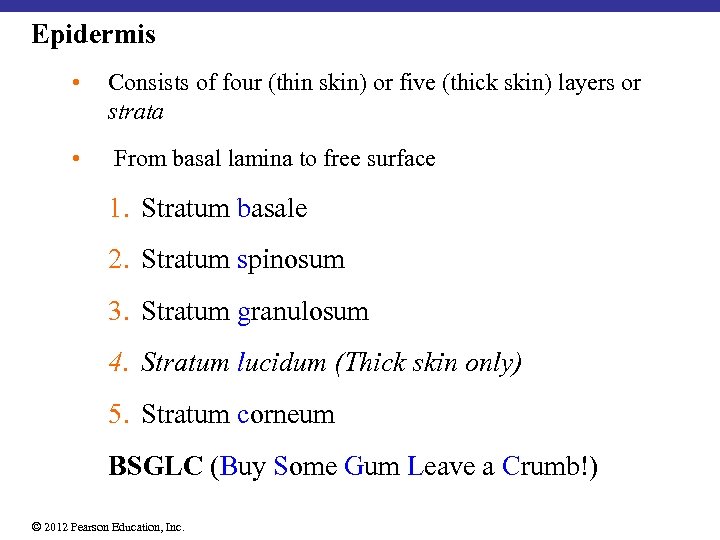 Epidermis • Consists of four (thin skin) or five (thick skin) layers or strata • From basal lamina to free surface 1. Stratum basale 2. Stratum spinosum 3. Stratum granulosum 4. Stratum lucidum (Thick skin only) 5. Stratum corneum BSGLC (Buy Some Gum Leave a Crumb!) © 2012 Pearson Education, Inc.
Epidermis • Consists of four (thin skin) or five (thick skin) layers or strata • From basal lamina to free surface 1. Stratum basale 2. Stratum spinosum 3. Stratum granulosum 4. Stratum lucidum (Thick skin only) 5. Stratum corneum BSGLC (Buy Some Gum Leave a Crumb!) © 2012 Pearson Education, Inc.
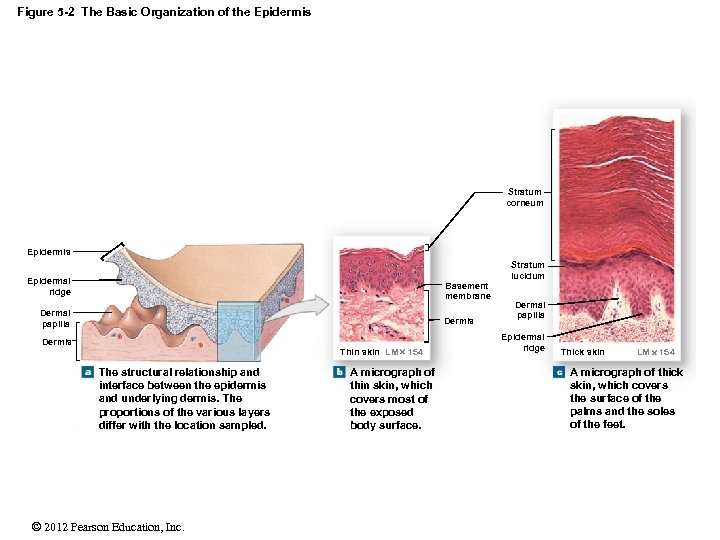 Figure 5 -2 The Basic Organization of the Epidermis Stratum corneum Epidermis Epidermal ridge Basement membrane Dermal papilla Dermis Thin skin LM 154 The structural relationship and interface between the epidermis and underlying dermis. The proportions of the various layers differ with the location sampled. © 2012 Pearson Education, Inc. A micrograph of thin skin, which covers most of the exposed body surface. Stratum lucidum Dermal papilla Epidermal ridge Thick skin LM 154 A micrograph of thick skin, which covers the surface of the palms and the soles of the feet.
Figure 5 -2 The Basic Organization of the Epidermis Stratum corneum Epidermis Epidermal ridge Basement membrane Dermal papilla Dermis Thin skin LM 154 The structural relationship and interface between the epidermis and underlying dermis. The proportions of the various layers differ with the location sampled. © 2012 Pearson Education, Inc. A micrograph of thin skin, which covers most of the exposed body surface. Stratum lucidum Dermal papilla Epidermal ridge Thick skin LM 154 A micrograph of thick skin, which covers the surface of the palms and the soles of the feet.
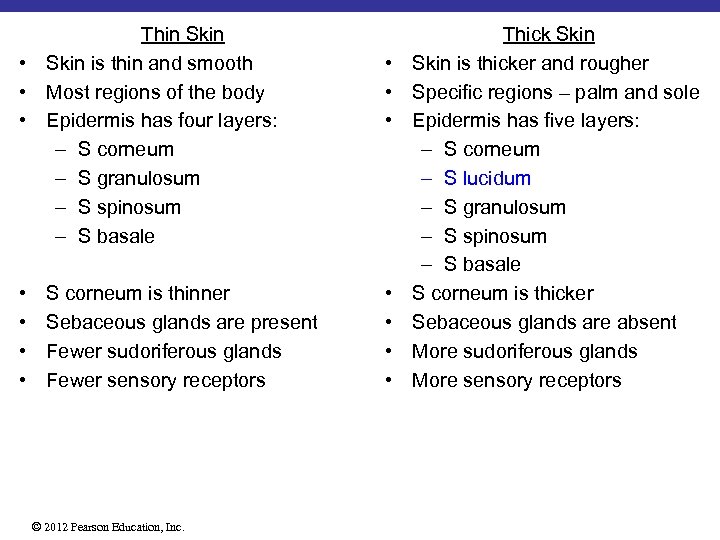 Thin Skin • Skin is thin and smooth • Most regions of the body • Epidermis has four layers: – S corneum – S granulosum – S spinosum – S basale • • S corneum is thinner Sebaceous glands are present Fewer sudoriferous glands Fewer sensory receptors © 2012 Pearson Education, Inc. • • Thick Skin is thicker and rougher Specific regions – palm and sole Epidermis has five layers: – S corneum – S lucidum – S granulosum – S spinosum – S basale S corneum is thicker Sebaceous glands are absent More sudoriferous glands More sensory receptors
Thin Skin • Skin is thin and smooth • Most regions of the body • Epidermis has four layers: – S corneum – S granulosum – S spinosum – S basale • • S corneum is thinner Sebaceous glands are present Fewer sudoriferous glands Fewer sensory receptors © 2012 Pearson Education, Inc. • • Thick Skin is thicker and rougher Specific regions – palm and sole Epidermis has five layers: – S corneum – S lucidum – S granulosum – S spinosum – S basale S corneum is thicker Sebaceous glands are absent More sudoriferous glands More sensory receptors
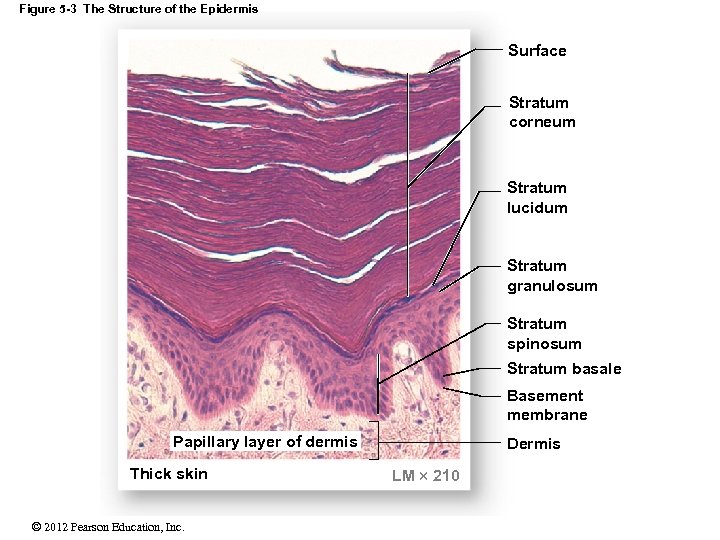 Figure 5 -3 The Structure of the Epidermis Surface Stratum corneum Stratum lucidum Stratum granulosum Stratum spinosum Stratum basale Basement membrane Papillary layer of dermis Thick skin © 2012 Pearson Education, Inc. Dermis LM 210
Figure 5 -3 The Structure of the Epidermis Surface Stratum corneum Stratum lucidum Stratum granulosum Stratum spinosum Stratum basale Basement membrane Papillary layer of dermis Thick skin © 2012 Pearson Education, Inc. Dermis LM 210
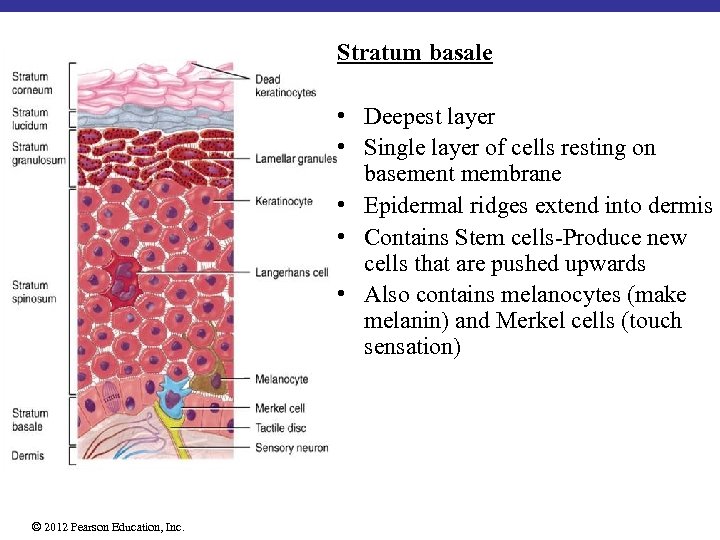 Stratum basale • Deepest layer • Single layer of cells resting on basement membrane • Epidermal ridges extend into dermis • Contains Stem cells-Produce new cells that are pushed upwards • Also contains melanocytes (make melanin) and Merkel cells (touch sensation) © 2012 Pearson Education, Inc.
Stratum basale • Deepest layer • Single layer of cells resting on basement membrane • Epidermal ridges extend into dermis • Contains Stem cells-Produce new cells that are pushed upwards • Also contains melanocytes (make melanin) and Merkel cells (touch sensation) © 2012 Pearson Education, Inc.
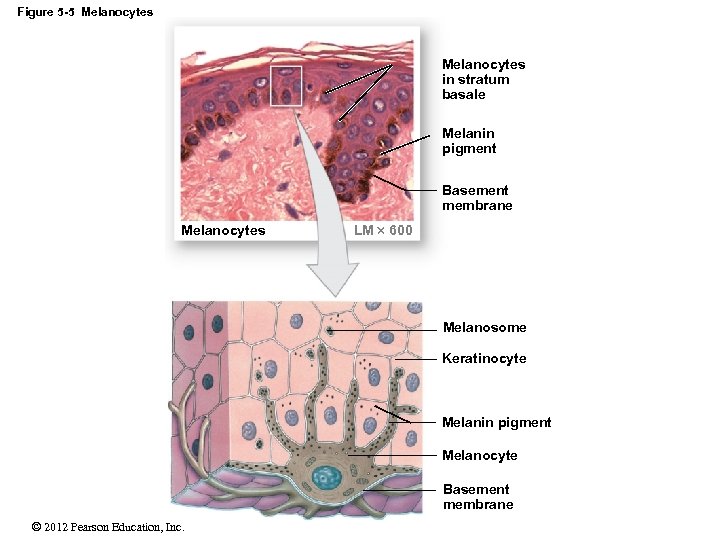 Figure 5 -5 Melanocytes in stratum basale Melanin pigment Basement membrane Melanocytes LM 600 Melanosome Keratinocyte Melanin pigment Melanocyte Basement membrane © 2012 Pearson Education, Inc.
Figure 5 -5 Melanocytes in stratum basale Melanin pigment Basement membrane Melanocytes LM 600 Melanosome Keratinocyte Melanin pigment Melanocyte Basement membrane © 2012 Pearson Education, Inc.
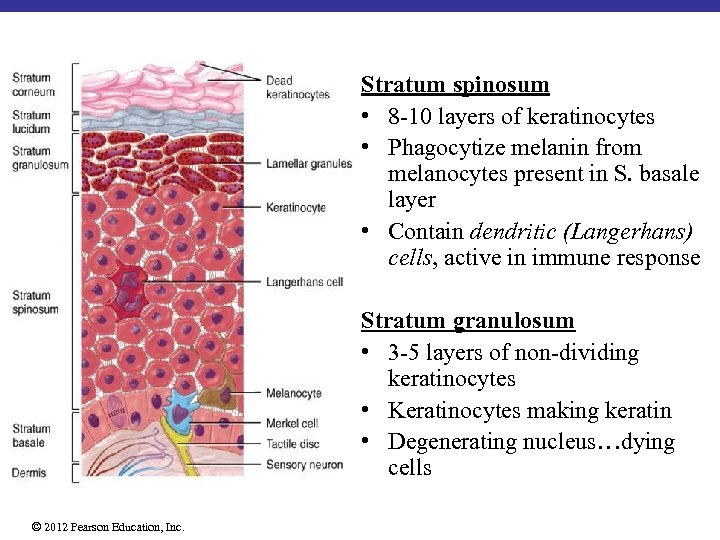 Stratum spinosum • 8 -10 layers of keratinocytes • Phagocytize melanin from melanocytes present in S. basale layer • Contain dendritic (Langerhans) cells, active in immune response Stratum granulosum • 3 -5 layers of non-dividing keratinocytes • Keratinocytes making keratin • Degenerating nucleus…dying cells © 2012 Pearson Education, Inc.
Stratum spinosum • 8 -10 layers of keratinocytes • Phagocytize melanin from melanocytes present in S. basale layer • Contain dendritic (Langerhans) cells, active in immune response Stratum granulosum • 3 -5 layers of non-dividing keratinocytes • Keratinocytes making keratin • Degenerating nucleus…dying cells © 2012 Pearson Education, Inc.
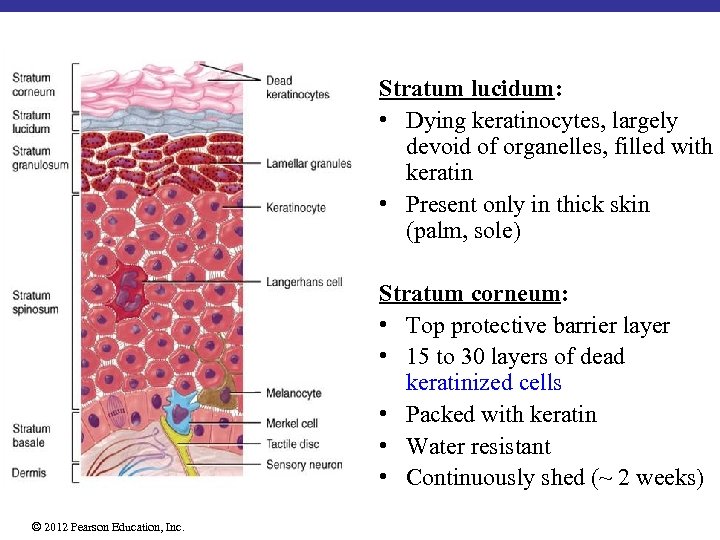 Stratum lucidum: • Dying keratinocytes, largely devoid of organelles, filled with keratin • Present only in thick skin (palm, sole) Stratum corneum: • Top protective barrier layer • 15 to 30 layers of dead keratinized cells • Packed with keratin • Water resistant • Continuously shed (~ 2 weeks) © 2012 Pearson Education, Inc.
Stratum lucidum: • Dying keratinocytes, largely devoid of organelles, filled with keratin • Present only in thick skin (palm, sole) Stratum corneum: • Top protective barrier layer • 15 to 30 layers of dead keratinized cells • Packed with keratin • Water resistant • Continuously shed (~ 2 weeks) © 2012 Pearson Education, Inc.
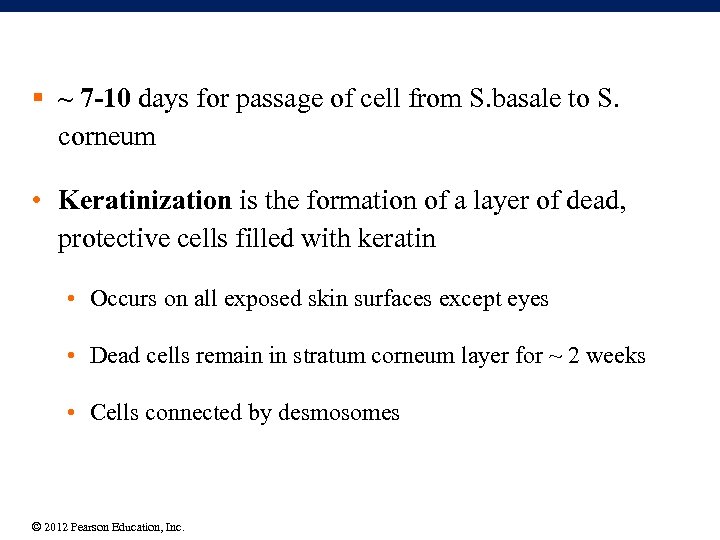 § ~ 7 -10 days for passage of cell from S. basale to S. corneum • Keratinization is the formation of a layer of dead, protective cells filled with keratin • Occurs on all exposed skin surfaces except eyes • Dead cells remain in stratum corneum layer for ~ 2 weeks • Cells connected by desmosomes © 2012 Pearson Education, Inc.
§ ~ 7 -10 days for passage of cell from S. basale to S. corneum • Keratinization is the formation of a layer of dead, protective cells filled with keratin • Occurs on all exposed skin surfaces except eyes • Dead cells remain in stratum corneum layer for ~ 2 weeks • Cells connected by desmosomes © 2012 Pearson Education, Inc.
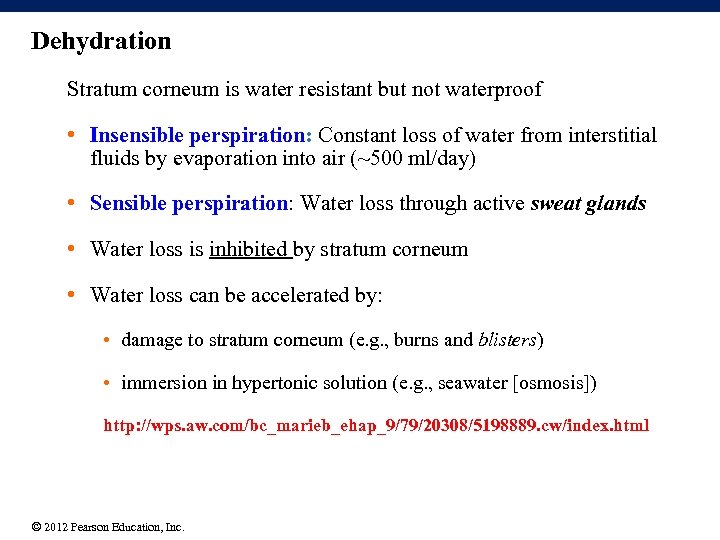 Dehydration Stratum corneum is water resistant but not waterproof • Insensible perspiration: Constant loss of water from interstitial fluids by evaporation into air (~500 ml/day) • Sensible perspiration: Water loss through active sweat glands • Water loss is inhibited by stratum corneum • Water loss can be accelerated by: • damage to stratum corneum (e. g. , burns and blisters) • immersion in hypertonic solution (e. g. , seawater [osmosis]) http: //wps. aw. com/bc_marieb_ehap_9/79/20308/5198889. cw/index. html © 2012 Pearson Education, Inc.
Dehydration Stratum corneum is water resistant but not waterproof • Insensible perspiration: Constant loss of water from interstitial fluids by evaporation into air (~500 ml/day) • Sensible perspiration: Water loss through active sweat glands • Water loss is inhibited by stratum corneum • Water loss can be accelerated by: • damage to stratum corneum (e. g. , burns and blisters) • immersion in hypertonic solution (e. g. , seawater [osmosis]) http: //wps. aw. com/bc_marieb_ehap_9/79/20308/5198889. cw/index. html © 2012 Pearson Education, Inc.
 5 -5 The Dermis § Located between epidermis and hypodermis (subcutaneous layer) § Contains Øhair follicles Øglands Ønerves Øblood vessels § Two components 1. Outer papillary layer Ø Areolar connective tissue 2. Deeper reticular layer Ø Dense irregular connective tissue © 2012 Pearson Education, Inc.
5 -5 The Dermis § Located between epidermis and hypodermis (subcutaneous layer) § Contains Øhair follicles Øglands Ønerves Øblood vessels § Two components 1. Outer papillary layer Ø Areolar connective tissue 2. Deeper reticular layer Ø Dense irregular connective tissue © 2012 Pearson Education, Inc.
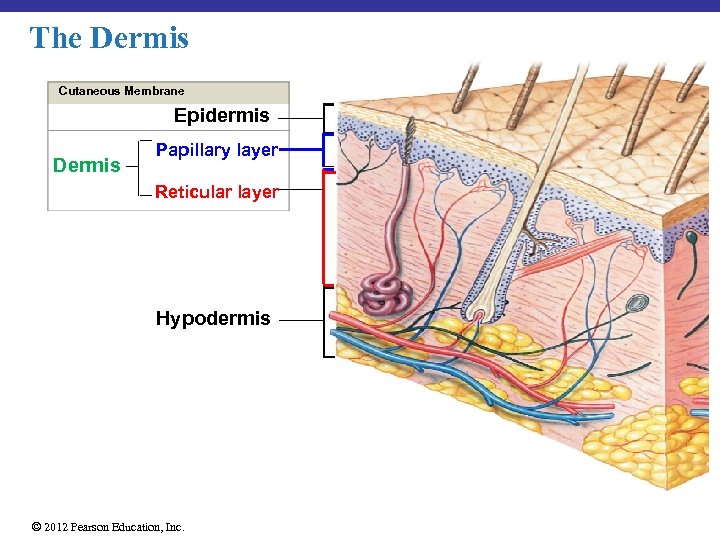 The Dermis Cutaneous Membrane Epidermis Dermis Papillary layer Reticular layer Hypodermis © 2012 Pearson Education, Inc.
The Dermis Cutaneous Membrane Epidermis Dermis Papillary layer Reticular layer Hypodermis © 2012 Pearson Education, Inc.
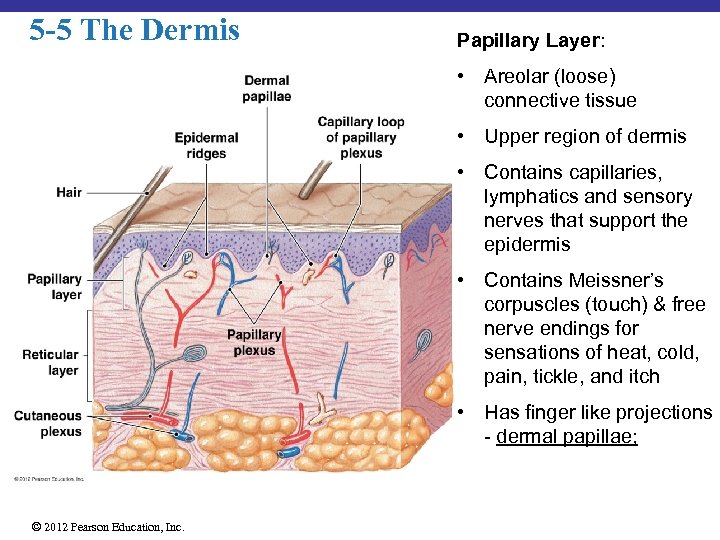 5 -5 The Dermis Papillary Layer: • Areolar (loose) connective tissue • Upper region of dermis • Contains capillaries, lymphatics and sensory nerves that support the epidermis • Contains Meissner’s corpuscles (touch) & free nerve endings for sensations of heat, cold, pain, tickle, and itch • Has finger like projections - dermal papillae; © 2012 Pearson Education, Inc.
5 -5 The Dermis Papillary Layer: • Areolar (loose) connective tissue • Upper region of dermis • Contains capillaries, lymphatics and sensory nerves that support the epidermis • Contains Meissner’s corpuscles (touch) & free nerve endings for sensations of heat, cold, pain, tickle, and itch • Has finger like projections - dermal papillae; © 2012 Pearson Education, Inc.
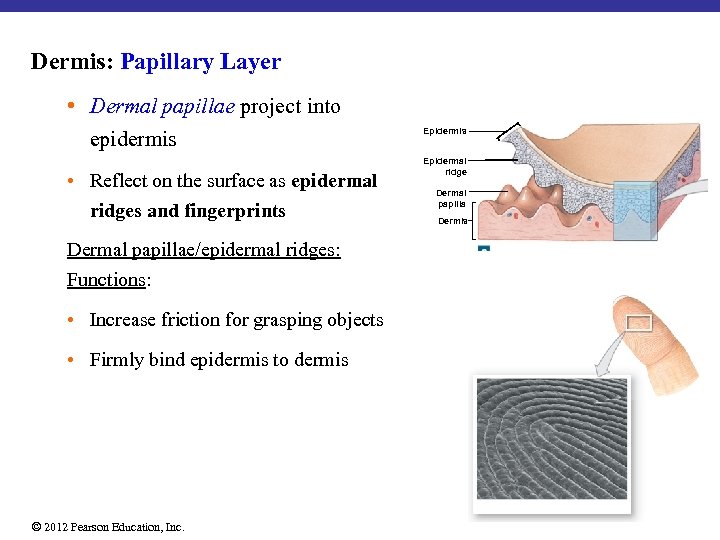 Dermis: Papillary Layer • Dermal papillae project into epidermis • Reflect on the surface as epidermal ridges and fingerprints Dermal papillae/epidermal ridges: Functions: • Increase friction for grasping objects • Firmly bind epidermis to dermis © 2012 Pearson Education, Inc. Epidermis Epidermal ridge Dermal papilla Dermis
Dermis: Papillary Layer • Dermal papillae project into epidermis • Reflect on the surface as epidermal ridges and fingerprints Dermal papillae/epidermal ridges: Functions: • Increase friction for grasping objects • Firmly bind epidermis to dermis © 2012 Pearson Education, Inc. Epidermis Epidermal ridge Dermal papilla Dermis
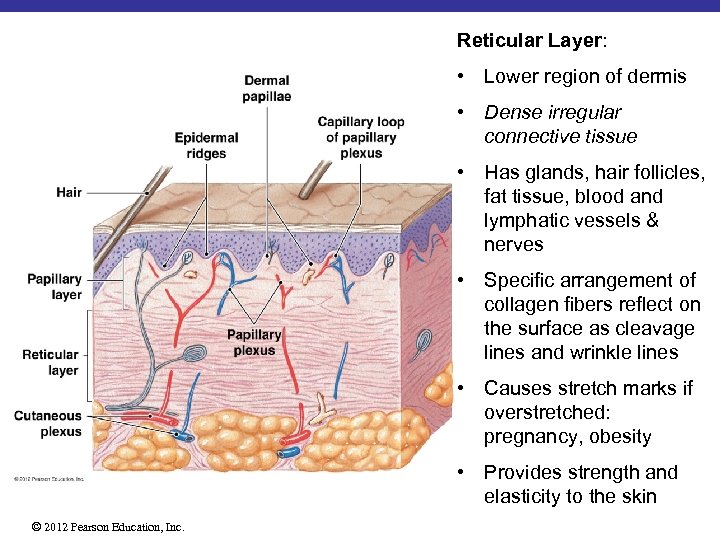 Reticular Layer: • Lower region of dermis • Dense irregular connective tissue • Has glands, hair follicles, fat tissue, blood and lymphatic vessels & nerves • Specific arrangement of collagen fibers reflect on the surface as cleavage lines and wrinkle lines • Causes stretch marks if overstretched: pregnancy, obesity • Provides strength and elasticity to the skin © 2012 Pearson Education, Inc.
Reticular Layer: • Lower region of dermis • Dense irregular connective tissue • Has glands, hair follicles, fat tissue, blood and lymphatic vessels & nerves • Specific arrangement of collagen fibers reflect on the surface as cleavage lines and wrinkle lines • Causes stretch marks if overstretched: pregnancy, obesity • Provides strength and elasticity to the skin © 2012 Pearson Education, Inc.
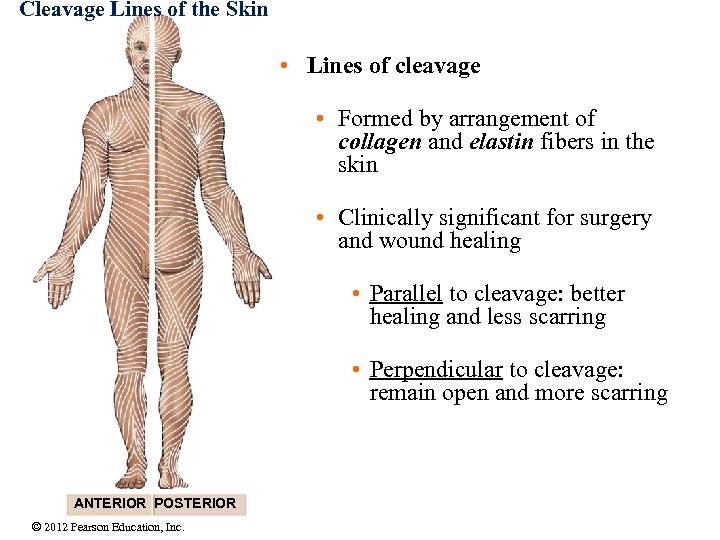 Cleavage Lines of the Skin • Lines of cleavage • Formed by arrangement of collagen and elastin fibers in the skin • Clinically significant for surgery and wound healing • Parallel to cleavage: better healing and less scarring • Perpendicular to cleavage: remain open and more scarring ANTERIOR POSTERIOR © 2012 Pearson Education, Inc.
Cleavage Lines of the Skin • Lines of cleavage • Formed by arrangement of collagen and elastin fibers in the skin • Clinically significant for surgery and wound healing • Parallel to cleavage: better healing and less scarring • Perpendicular to cleavage: remain open and more scarring ANTERIOR POSTERIOR © 2012 Pearson Education, Inc.
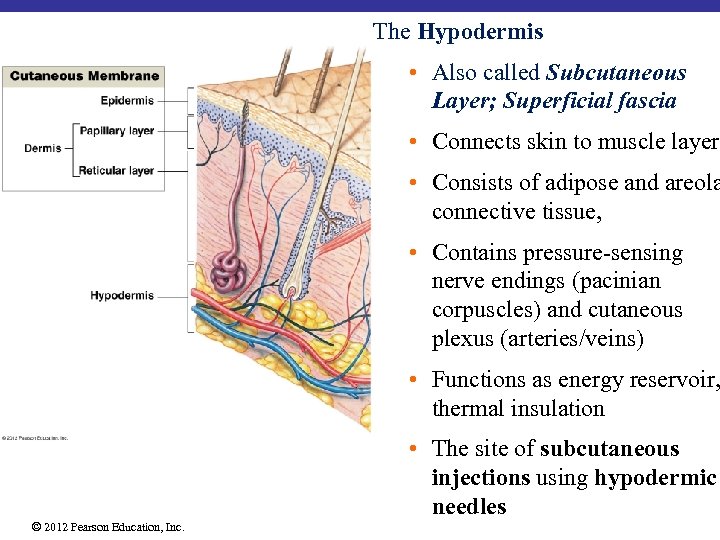 The Hypodermis • Also called Subcutaneous Layer; Superficial fascia • Connects skin to muscle layer • Consists of adipose and areola connective tissue, • Contains pressure-sensing nerve endings (pacinian corpuscles) and cutaneous plexus (arteries/veins) • Functions as energy reservoir, thermal insulation • The site of subcutaneous injections using hypodermic needles © 2012 Pearson Education, Inc.
The Hypodermis • Also called Subcutaneous Layer; Superficial fascia • Connects skin to muscle layer • Consists of adipose and areola connective tissue, • Contains pressure-sensing nerve endings (pacinian corpuscles) and cutaneous plexus (arteries/veins) • Functions as energy reservoir, thermal insulation • The site of subcutaneous injections using hypodermic needles © 2012 Pearson Education, Inc.
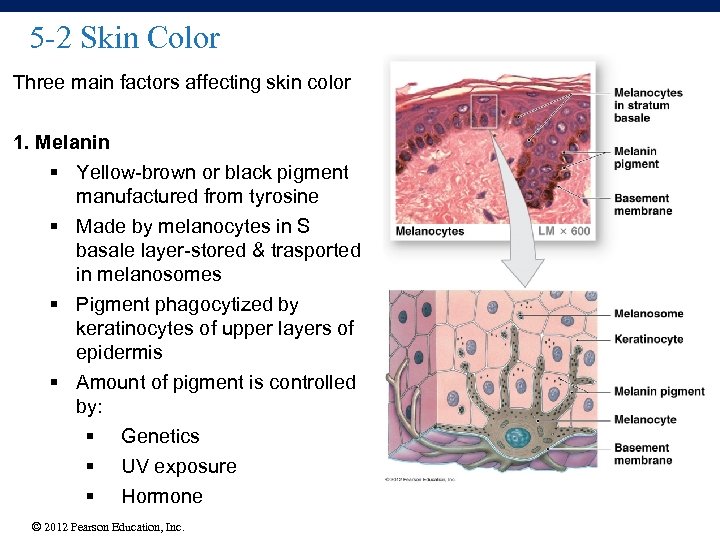 5 -2 Skin Color Three main factors affecting skin color 1. Melanin § Yellow-brown or black pigment manufactured from tyrosine § Made by melanocytes in S basale layer-stored & trasported in melanosomes § Pigment phagocytized by keratinocytes of upper layers of epidermis § Amount of pigment is controlled by: § Genetics § UV exposure § Hormone © 2012 Pearson Education, Inc.
5 -2 Skin Color Three main factors affecting skin color 1. Melanin § Yellow-brown or black pigment manufactured from tyrosine § Made by melanocytes in S basale layer-stored & trasported in melanosomes § Pigment phagocytized by keratinocytes of upper layers of epidermis § Amount of pigment is controlled by: § Genetics § UV exposure § Hormone © 2012 Pearson Education, Inc.
 5 -2 Skin Color 2. Carotene – Orange/Yellow pigment (found in yellow fruits and vegetables) – Accumulates in epidermal cells and fatty tissues of the dermis – Gives yellow hue to the skin – Used to make vitamin A: required for maintenance of epithelia and for the synthesis of photoreceptors of the eye 3. Hemoglobin-Blood vessels – Network of capillaries varies in dermis – Gives reddish color to the skin © 2012 Pearson Education, Inc.
5 -2 Skin Color 2. Carotene – Orange/Yellow pigment (found in yellow fruits and vegetables) – Accumulates in epidermal cells and fatty tissues of the dermis – Gives yellow hue to the skin – Used to make vitamin A: required for maintenance of epithelia and for the synthesis of photoreceptors of the eye 3. Hemoglobin-Blood vessels – Network of capillaries varies in dermis – Gives reddish color to the skin © 2012 Pearson Education, Inc.
 Skin Color-Diagnostics • Jaundice - yellowish color to skin and whites of eyes. Liver unable to excrete bile, buildup of yellow bilirubin in blood from liver/blood disease • Cyanosis - bluish color in the nails and skin due to severe reduction in blood flow or oxygenation-for e. g severe cold, heart failure • Erythema: redness of skin due to dilation of blood capillaries in the dermis, caused by inflammation, infection, allergy, burns, anger, embarrasment • Pallor (blanching): due to emotional stress such as fear, anemia, low blood pressure, impaired blood flow to an area © 2012 Pearson Education, Inc.
Skin Color-Diagnostics • Jaundice - yellowish color to skin and whites of eyes. Liver unable to excrete bile, buildup of yellow bilirubin in blood from liver/blood disease • Cyanosis - bluish color in the nails and skin due to severe reduction in blood flow or oxygenation-for e. g severe cold, heart failure • Erythema: redness of skin due to dilation of blood capillaries in the dermis, caused by inflammation, infection, allergy, burns, anger, embarrasment • Pallor (blanching): due to emotional stress such as fear, anemia, low blood pressure, impaired blood flow to an area © 2012 Pearson Education, Inc.
 Skin Color-Diagnostics Albinism: melanocytes are present but melanin gene is mutated little or no melanin made no color in the skin, hair and eyes Vitiligo: partial or complete loss of melanocytes patchy skin, thought to be autoimmune disorder Pituitary tumor: Produce excess Melanocyte Stimulating Hormone (MSH)-Skin darkening Addison’s disease: A disease of the pituitary gland resulting in increased secretion of adrenocorticotropic hormone (ACTH) which is structurally similar to MSH-skin darkening © 2012 Pearson Education, Inc.
Skin Color-Diagnostics Albinism: melanocytes are present but melanin gene is mutated little or no melanin made no color in the skin, hair and eyes Vitiligo: partial or complete loss of melanocytes patchy skin, thought to be autoimmune disorder Pituitary tumor: Produce excess Melanocyte Stimulating Hormone (MSH)-Skin darkening Addison’s disease: A disease of the pituitary gland resulting in increased secretion of adrenocorticotropic hormone (ACTH) which is structurally similar to MSH-skin darkening © 2012 Pearson Education, Inc.
 https: //www. polleverywhere. com/my/polls#!/my/polls 5 -7 Hair and other accessory structures Located primarily in dermis but of epidermal origin • Hair & Hair Follicles • Nails • Sebaceous Glands • Sweat Glands © 2012 Pearson Education, Inc.
https: //www. polleverywhere. com/my/polls#!/my/polls 5 -7 Hair and other accessory structures Located primarily in dermis but of epidermal origin • Hair & Hair Follicles • Nails • Sebaceous Glands • Sweat Glands © 2012 Pearson Education, Inc.
 5 -7 Hair § Hairs are mostly non-living structures produced in organs called hair follicles § strands of dead cells filled with keratin Terminal hair-large, coarse, more darkly pigmentted-eg scalp hair Vellus hair-finer, shorter-most of body surface § Hair functions Ø Protects against UV Ø Insulation Ø Guards openings (eye, ear, nostrils) against particles and insects Ø Sensory receptors-sensitive to very light touch © 2012 Pearson Education, Inc.
5 -7 Hair § Hairs are mostly non-living structures produced in organs called hair follicles § strands of dead cells filled with keratin Terminal hair-large, coarse, more darkly pigmentted-eg scalp hair Vellus hair-finer, shorter-most of body surface § Hair functions Ø Protects against UV Ø Insulation Ø Guards openings (eye, ear, nostrils) against particles and insects Ø Sensory receptors-sensitive to very light touch © 2012 Pearson Education, Inc.
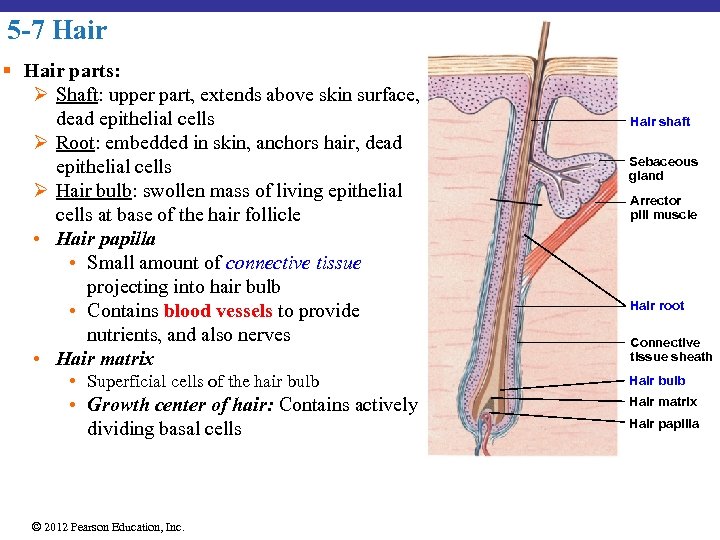 5 -7 Hair § Hair parts: Ø Shaft: upper part, extends above skin surface, dead epithelial cells Ø Root: embedded in skin, anchors hair, dead epithelial cells Ø Hair bulb: swollen mass of living epithelial cells at base of the hair follicle • Hair papilla • Small amount of connective tissue projecting into hair bulb • Contains blood vessels to provide nutrients, and also nerves • Hair matrix Hair shaft Sebaceous gland Arrector pili muscle Hair root Connective tissue sheath • Superficial cells of the hair bulb Hair bulb • Growth center of hair: Contains actively dividing basal cells Hair matrix © 2012 Pearson Education, Inc. Hair papilla
5 -7 Hair § Hair parts: Ø Shaft: upper part, extends above skin surface, dead epithelial cells Ø Root: embedded in skin, anchors hair, dead epithelial cells Ø Hair bulb: swollen mass of living epithelial cells at base of the hair follicle • Hair papilla • Small amount of connective tissue projecting into hair bulb • Contains blood vessels to provide nutrients, and also nerves • Hair matrix Hair shaft Sebaceous gland Arrector pili muscle Hair root Connective tissue sheath • Superficial cells of the hair bulb Hair bulb • Growth center of hair: Contains actively dividing basal cells Hair matrix © 2012 Pearson Education, Inc. Hair papilla
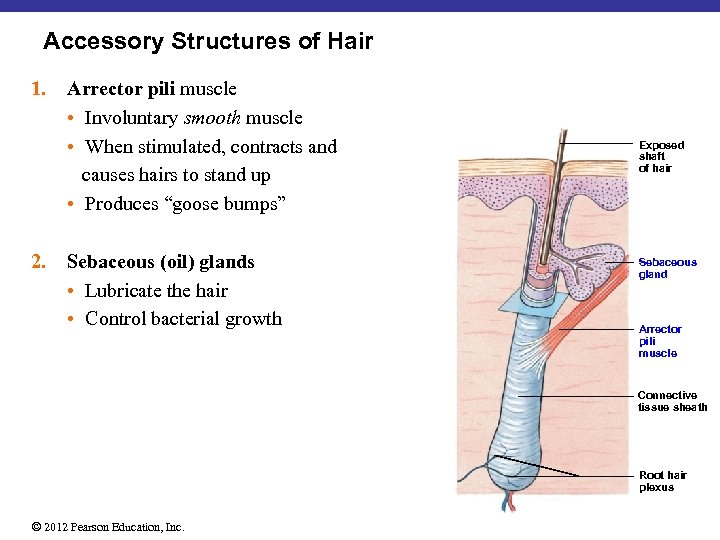 Accessory Structures of Hair 1. 2. Arrector pili muscle • Involuntary smooth muscle • When stimulated, contracts and causes hairs to stand up • Produces “goose bumps” Sebaceous (oil) glands • Lubricate the hair • Control bacterial growth Exposed shaft of hair Sebaceous gland Arrector pili muscle Connective tissue sheath Root hair plexus © 2012 Pearson Education, Inc.
Accessory Structures of Hair 1. 2. Arrector pili muscle • Involuntary smooth muscle • When stimulated, contracts and causes hairs to stand up • Produces “goose bumps” Sebaceous (oil) glands • Lubricate the hair • Control bacterial growth Exposed shaft of hair Sebaceous gland Arrector pili muscle Connective tissue sheath Root hair plexus © 2012 Pearson Education, Inc.
 Hair Color • Depends upon amount and type of melanin: • Dark hair – a lot of melanin • Gray hair – decrease in melanin production • White hair – absence of melanin and presence of air bubbles in hair medulla © 2012 Pearson Education, Inc.
Hair Color • Depends upon amount and type of melanin: • Dark hair – a lot of melanin • Gray hair – decrease in melanin production • White hair – absence of melanin and presence of air bubbles in hair medulla © 2012 Pearson Education, Inc.
 5 -9 Nails • Protect fingers and toes • Made of dead cells packed with keratin • Metabolic disorders can change nail structure © 2012 Pearson Education, Inc.
5 -9 Nails • Protect fingers and toes • Made of dead cells packed with keratin • Metabolic disorders can change nail structure © 2012 Pearson Education, Inc.
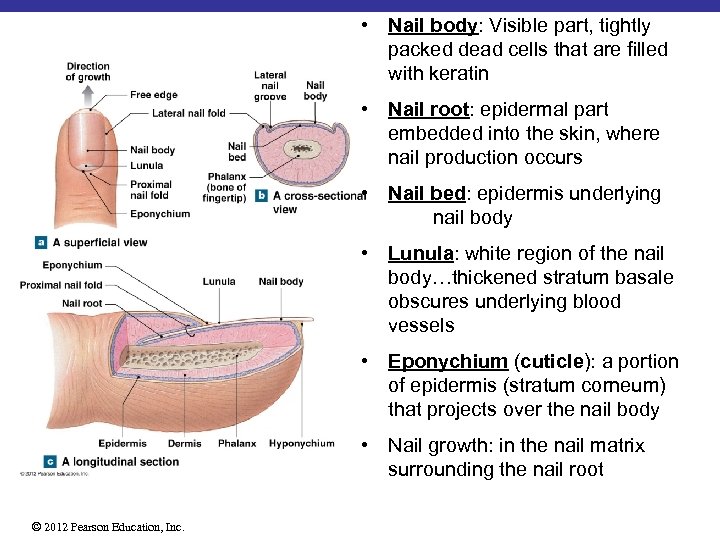 • Nail body: Visible part, tightly packed dead cells that are filled with keratin • Nail root: epidermal part embedded into the skin, where nail production occurs • Nail bed: epidermis underlying nail body • Lunula: white region of the nail body…thickened stratum basale obscures underlying blood vessels • Eponychium (cuticle): a portion of epidermis (stratum corneum) that projects over the nail body • Nail growth: in the nail matrix surrounding the nail root © 2012 Pearson Education, Inc.
• Nail body: Visible part, tightly packed dead cells that are filled with keratin • Nail root: epidermal part embedded into the skin, where nail production occurs • Nail bed: epidermis underlying nail body • Lunula: white region of the nail body…thickened stratum basale obscures underlying blood vessels • Eponychium (cuticle): a portion of epidermis (stratum corneum) that projects over the nail body • Nail growth: in the nail matrix surrounding the nail root © 2012 Pearson Education, Inc.
 5 -8 Sebaceous Glands and Sweat Glands Exocrine Glands in Skin • Sebaceous Glands (oil glands) • Secrete sebum • Sweat Glands(sudoriferous glands) • Watery secretions © 2012 Pearson Education, Inc.
5 -8 Sebaceous Glands and Sweat Glands Exocrine Glands in Skin • Sebaceous Glands (oil glands) • Secrete sebum • Sweat Glands(sudoriferous glands) • Watery secretions © 2012 Pearson Education, Inc.
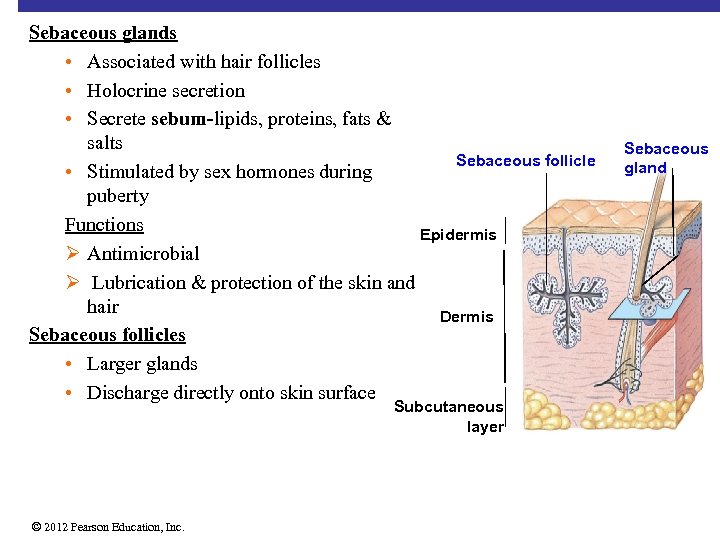 Sebaceous glands • Associated with hair follicles • Holocrine secretion • Secrete sebum-lipids, proteins, fats & salts Sebaceous follicle • Stimulated by sex hormones during puberty Functions Epidermis Ø Antimicrobial Ø Lubrication & protection of the skin and hair Dermis Sebaceous follicles • Larger glands • Discharge directly onto skin surface Subcutaneous layer © 2012 Pearson Education, Inc. Sebaceous gland
Sebaceous glands • Associated with hair follicles • Holocrine secretion • Secrete sebum-lipids, proteins, fats & salts Sebaceous follicle • Stimulated by sex hormones during puberty Functions Epidermis Ø Antimicrobial Ø Lubrication & protection of the skin and hair Dermis Sebaceous follicles • Larger glands • Discharge directly onto skin surface Subcutaneous layer © 2012 Pearson Education, Inc. Sebaceous gland
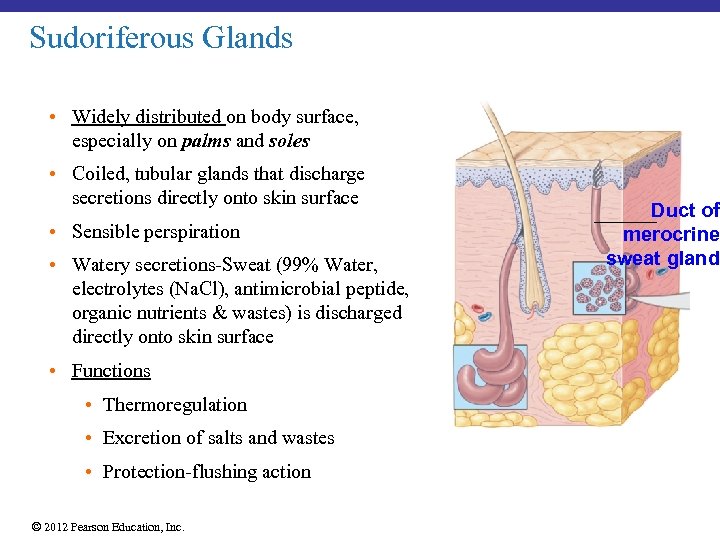 Sudoriferous Glands • Widely distributed on body surface, especially on palms and soles • Coiled, tubular glands that discharge secretions directly onto skin surface • Sensible perspiration • Watery secretions-Sweat (99% Water, electrolytes (Na. Cl), antimicrobial peptide, organic nutrients & wastes) is discharged directly onto skin surface • Functions • Thermoregulation • Excretion of salts and wastes • Protection-flushing action © 2012 Pearson Education, Inc. Duct of merocrine sweat gland
Sudoriferous Glands • Widely distributed on body surface, especially on palms and soles • Coiled, tubular glands that discharge secretions directly onto skin surface • Sensible perspiration • Watery secretions-Sweat (99% Water, electrolytes (Na. Cl), antimicrobial peptide, organic nutrients & wastes) is discharged directly onto skin surface • Functions • Thermoregulation • Excretion of salts and wastes • Protection-flushing action © 2012 Pearson Education, Inc. Duct of merocrine sweat gland
 Other Integumentary Glands 1. Mammary glands • Produce milk 2. Ceruminous glands • Found in ear canal • Produce cerumen (earwax) • Protect the eardrum © 2012 Pearson Education, Inc.
Other Integumentary Glands 1. Mammary glands • Produce milk 2. Ceruminous glands • Found in ear canal • Produce cerumen (earwax) • Protect the eardrum © 2012 Pearson Education, Inc.
 5 -10 Repair of the Integument Superficial Wound Epidermis is damaged. Stratum basale cells from the periphery of the wound --> migrate towards the center --> cells divide to form new epithelial cells to replace the loss tissue --> skin epidermis becomes normal © 2012 Pearson Education, Inc.
5 -10 Repair of the Integument Superficial Wound Epidermis is damaged. Stratum basale cells from the periphery of the wound --> migrate towards the center --> cells divide to form new epithelial cells to replace the loss tissue --> skin epidermis becomes normal © 2012 Pearson Education, Inc.
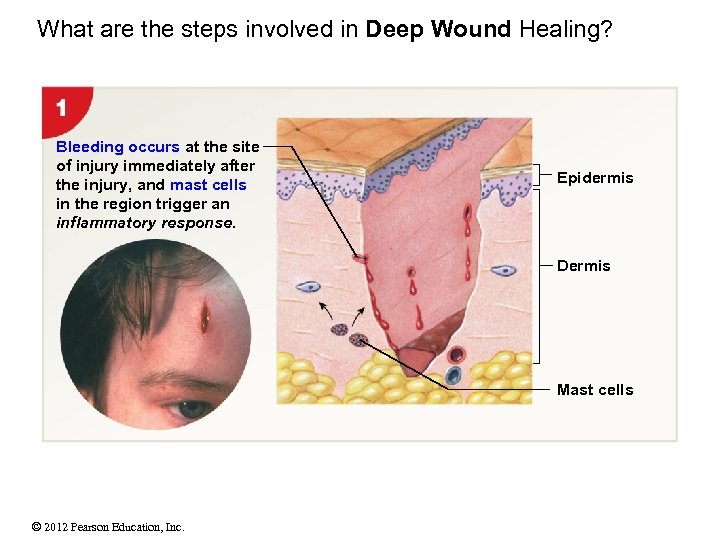 What are the steps involved in Deep Wound Healing? Bleeding occurs at the site of injury immediately after the injury, and mast cells in the region trigger an inflammatory response. Epidermis Dermis Mast cells © 2012 Pearson Education, Inc.
What are the steps involved in Deep Wound Healing? Bleeding occurs at the site of injury immediately after the injury, and mast cells in the region trigger an inflammatory response. Epidermis Dermis Mast cells © 2012 Pearson Education, Inc.
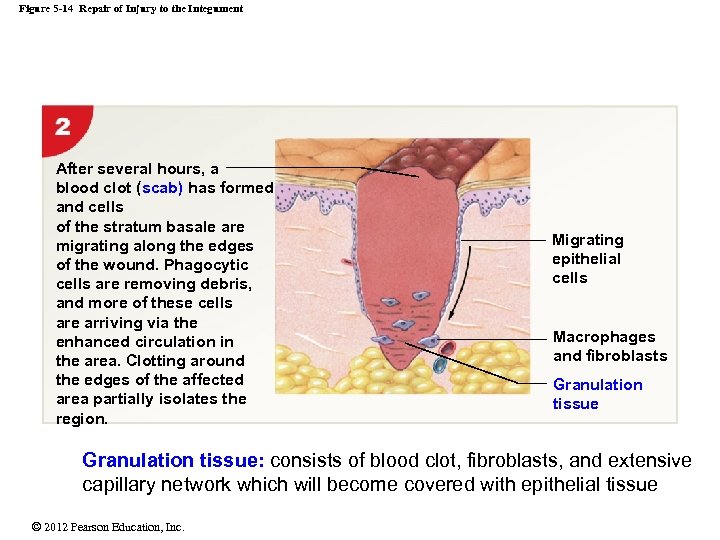 Figure 5 -14 Repair of Injury to the Integument After several hours, a blood clot (scab) has formed and cells of the stratum basale are migrating along the edges of the wound. Phagocytic cells are removing debris, and more of these cells are arriving via the enhanced circulation in the area. Clotting around the edges of the affected area partially isolates the region. Migrating epithelial cells Macrophages and fibroblasts Granulation tissue: consists of blood clot, fibroblasts, and extensive capillary network which will become covered with epithelial tissue © 2012 Pearson Education, Inc.
Figure 5 -14 Repair of Injury to the Integument After several hours, a blood clot (scab) has formed and cells of the stratum basale are migrating along the edges of the wound. Phagocytic cells are removing debris, and more of these cells are arriving via the enhanced circulation in the area. Clotting around the edges of the affected area partially isolates the region. Migrating epithelial cells Macrophages and fibroblasts Granulation tissue: consists of blood clot, fibroblasts, and extensive capillary network which will become covered with epithelial tissue © 2012 Pearson Education, Inc.
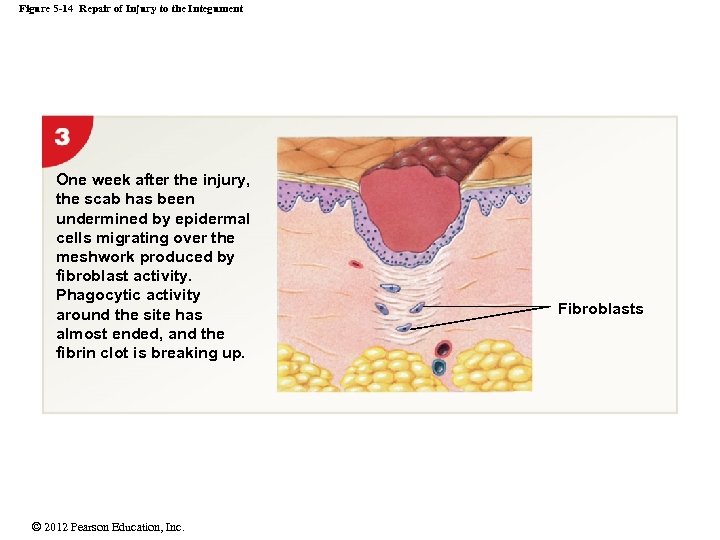 Figure 5 -14 Repair of Injury to the Integument One week after the injury, the scab has been undermined by epidermal cells migrating over the meshwork produced by fibroblast activity. Phagocytic activity around the site has almost ended, and the fibrin clot is breaking up. © 2012 Pearson Education, Inc. Fibroblasts
Figure 5 -14 Repair of Injury to the Integument One week after the injury, the scab has been undermined by epidermal cells migrating over the meshwork produced by fibroblast activity. Phagocytic activity around the site has almost ended, and the fibrin clot is breaking up. © 2012 Pearson Education, Inc. Fibroblasts
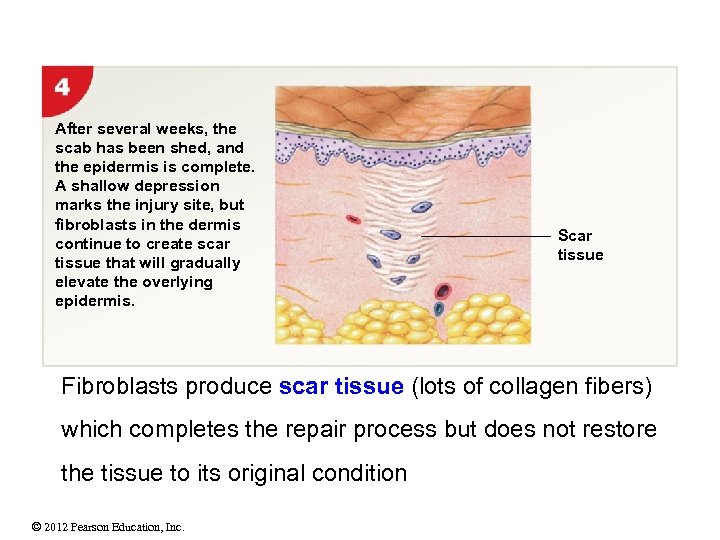 After several weeks, the scab has been shed, and the epidermis is complete. A shallow depression marks the injury site, but fibroblasts in the dermis continue to create scar tissue that will gradually elevate the overlying epidermis. Scar tissue Fibroblasts produce scar tissue (lots of collagen fibers) which completes the repair process but does not restore the tissue to its original condition © 2012 Pearson Education, Inc.
After several weeks, the scab has been shed, and the epidermis is complete. A shallow depression marks the injury site, but fibroblasts in the dermis continue to create scar tissue that will gradually elevate the overlying epidermis. Scar tissue Fibroblasts produce scar tissue (lots of collagen fibers) which completes the repair process but does not restore the tissue to its original condition © 2012 Pearson Education, Inc.
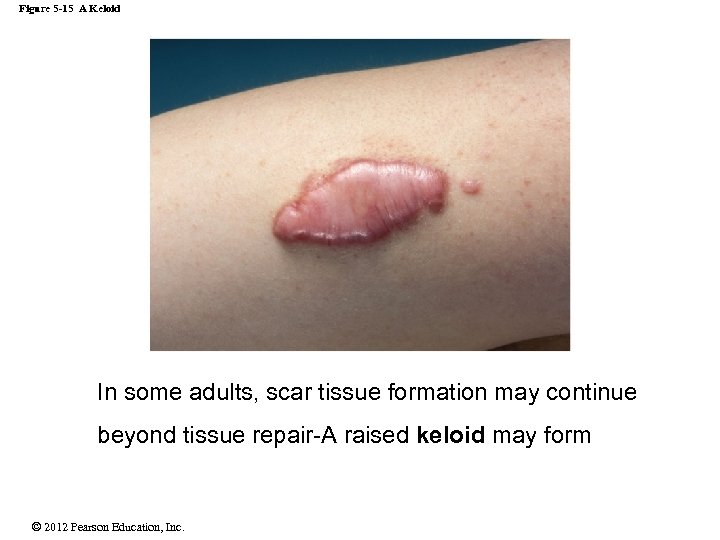 Figure 5 -15 A Keloid In some adults, scar tissue formation may continue beyond tissue repair-A raised keloid may form © 2012 Pearson Education, Inc.
Figure 5 -15 A Keloid In some adults, scar tissue formation may continue beyond tissue repair-A raised keloid may form © 2012 Pearson Education, Inc.
 5 -3 Vitamin D 3: Sources 1. Sunlight. Limited exposure to UV is beneficial Ø Epidermal cells produce vitamin D 3 (Cholecalciferol) in the presence of UV radiation Ø Liver creates intermediate product then converted to calcitriol by kidneys Ø Calcitriol aids absorption of calcium and phosphorus needed for bone maintenance and growth 2. Diet. Ø Naturally from fish, fish oils, and shellfish Ø From fortified food products © 2012 Pearson Education, Inc.
5 -3 Vitamin D 3: Sources 1. Sunlight. Limited exposure to UV is beneficial Ø Epidermal cells produce vitamin D 3 (Cholecalciferol) in the presence of UV radiation Ø Liver creates intermediate product then converted to calcitriol by kidneys Ø Calcitriol aids absorption of calcium and phosphorus needed for bone maintenance and growth 2. Diet. Ø Naturally from fish, fish oils, and shellfish Ø From fortified food products © 2012 Pearson Education, Inc.
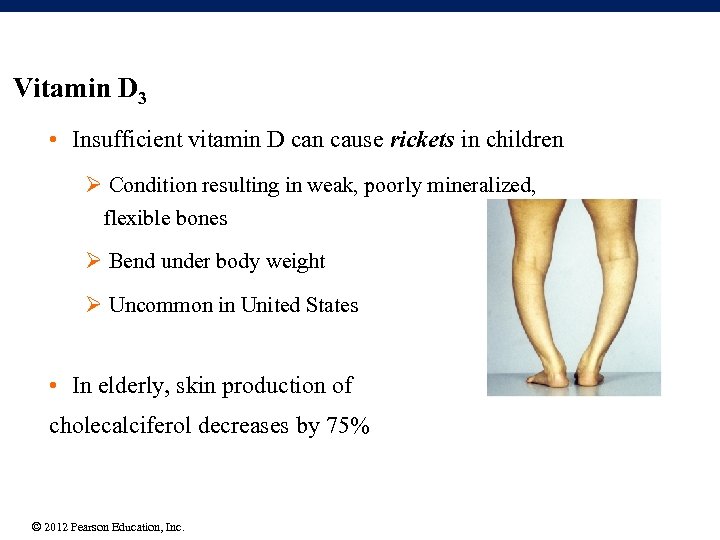 Vitamin D 3 • Insufficient vitamin D can cause rickets in children Ø Condition resulting in weak, poorly mineralized, flexible bones Ø Bend under body weight Ø Uncommon in United States • In elderly, skin production of cholecalciferol decreases by 75% © 2012 Pearson Education, Inc.
Vitamin D 3 • Insufficient vitamin D can cause rickets in children Ø Condition resulting in weak, poorly mineralized, flexible bones Ø Bend under body weight Ø Uncommon in United States • In elderly, skin production of cholecalciferol decreases by 75% © 2012 Pearson Education, Inc.
 Skin Cancer 3 common forms of skin cancer 1. Basal cell carcinoma: rarely metastasizes, most common, originates in stratum basale. 2. Squamous cell carcinoma: may metastasize, originate in stratum spinosum 3. Malignant melanomas: metastasizes rapidly • most common cancer in young women, life threatening • arise from melanocytes • key to treatment is early detection • risks factors include-- skin color, sun exposure, family history, age and immunological status © 2012 Pearson Education, Inc.
Skin Cancer 3 common forms of skin cancer 1. Basal cell carcinoma: rarely metastasizes, most common, originates in stratum basale. 2. Squamous cell carcinoma: may metastasize, originate in stratum spinosum 3. Malignant melanomas: metastasizes rapidly • most common cancer in young women, life threatening • arise from melanocytes • key to treatment is early detection • risks factors include-- skin color, sun exposure, family history, age and immunological status © 2012 Pearson Education, Inc.
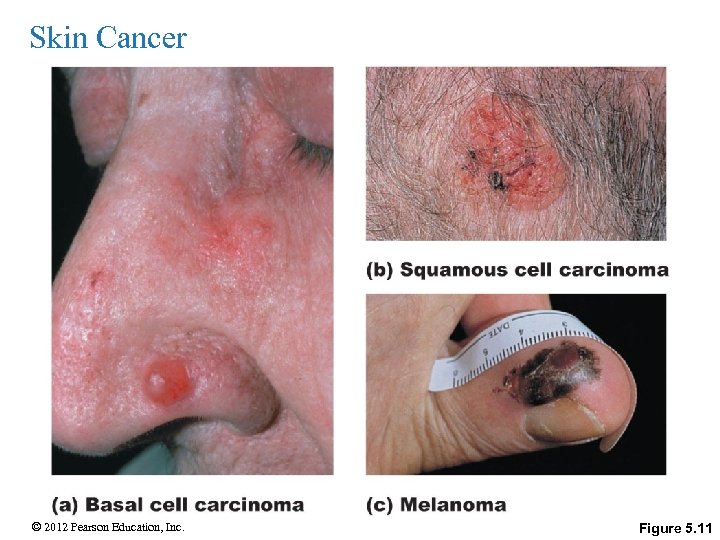 Skin Cancer © 2012 Pearson Education, Inc. Figure 5. 11
Skin Cancer © 2012 Pearson Education, Inc. Figure 5. 11
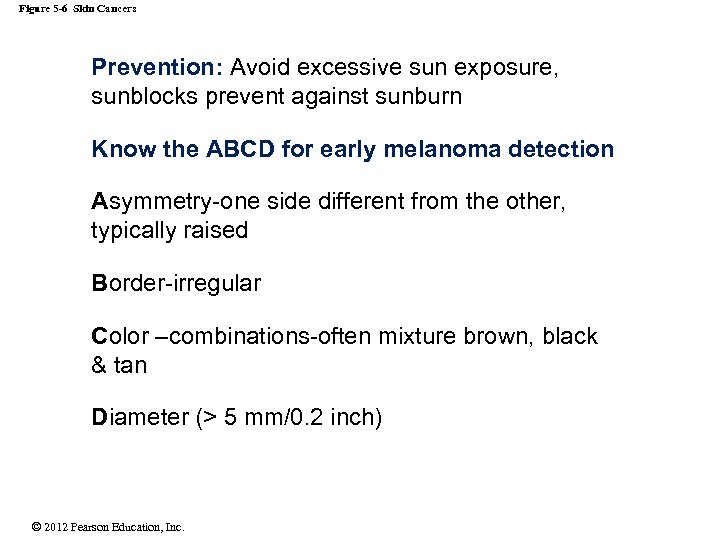 Figure 5 -6 Skin Cancers Prevention: Avoid excessive sun exposure, sunblocks prevent against sunburn Know the ABCD for early melanoma detection Asymmetry-one side different from the other, typically raised Border-irregular Color –combinations-often mixture brown, black & tan Diameter (> 5 mm/0. 2 inch) © 2012 Pearson Education, Inc.
Figure 5 -6 Skin Cancers Prevention: Avoid excessive sun exposure, sunblocks prevent against sunburn Know the ABCD for early melanoma detection Asymmetry-one side different from the other, typically raised Border-irregular Color –combinations-often mixture brown, black & tan Diameter (> 5 mm/0. 2 inch) © 2012 Pearson Education, Inc.
 Skin burns Caused by: Fire, electricity, radiations, and chemicals Effects on the body: • Dehydration • Lowered body temperature • Decreased blood pressure • Decreased or no urine production (kidneys shut down) • Infections © 2012 Pearson Education, Inc.
Skin burns Caused by: Fire, electricity, radiations, and chemicals Effects on the body: • Dehydration • Lowered body temperature • Decreased blood pressure • Decreased or no urine production (kidneys shut down) • Infections © 2012 Pearson Education, Inc.
 Severity of Burns First-degree burns • Only upper epidermis is damaged • Most sunburns • Pain, Skin is red (erythema) and swollen, flaking & peeling Second-degree burns • Epidermis and usually upper dermis are damaged • Pain, Skin is red (erythema) with blisters © 2012 Pearson Education, Inc.
Severity of Burns First-degree burns • Only upper epidermis is damaged • Most sunburns • Pain, Skin is red (erythema) and swollen, flaking & peeling Second-degree burns • Epidermis and usually upper dermis are damaged • Pain, Skin is red (erythema) with blisters © 2012 Pearson Education, Inc.
 Severity of Burns Third-degree burns (Full thickness) • Destroys the epidermis & accessory structures); may extend to hypodermis • Less painful due to destroyed sensory nerves • Extensive burns cannot repair and requires skin graft © 2012 Pearson Education, Inc.
Severity of Burns Third-degree burns (Full thickness) • Destroys the epidermis & accessory structures); may extend to hypodermis • Less painful due to destroyed sensory nerves • Extensive burns cannot repair and requires skin graft © 2012 Pearson Education, Inc.
 © 2012 Pearson Education, Inc.
© 2012 Pearson Education, Inc.
 • A third degree (full-thickness) burn injury can be life threatening if it covers >20% of body surface. • Symptoms and Treatment Ø Fluid and electrolyte loss-Ivs to replace Ø Increased evaporative cooling-High-calorie diet Ø Infection prone-Antibiotics, Aseptic environment, debridement, high calorie diet Ø Skin grafts © 2012 Pearson Education, Inc.
• A third degree (full-thickness) burn injury can be life threatening if it covers >20% of body surface. • Symptoms and Treatment Ø Fluid and electrolyte loss-Ivs to replace Ø Increased evaporative cooling-High-calorie diet Ø Infection prone-Antibiotics, Aseptic environment, debridement, high calorie diet Ø Skin grafts © 2012 Pearson Education, Inc.
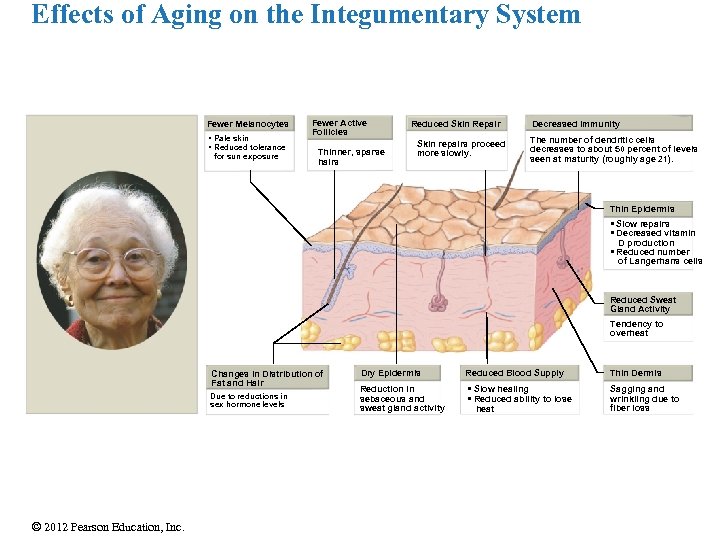 Effects of Aging on the Integumentary System Fewer Melanocytes • Pale skin • Reduced tolerance for sun exposure Fewer Active Follicles Thinner, sparse hairs Reduced Skin Repair Skin repairs proceed more slowly. Decreased Immunity The number of dendritic cells decreases to about 50 percent of levels seen at maturity (roughly age 21). Thin Epidermis • Slow repairs • Decreased vitamin D production • Reduced number of Langerhans cells Reduced Sweat Gland Activity Tendency to overheat Changes in Distribution of Fat and Hair Due to reductions in sex hormone levels © 2012 Pearson Education, Inc. Dry Epidermis Reduction in sebaceous and sweat gland activity Reduced Blood Supply • Slow healing • Reduced ability to lose heat Thin Dermis Sagging and wrinkling due to fiber loss
Effects of Aging on the Integumentary System Fewer Melanocytes • Pale skin • Reduced tolerance for sun exposure Fewer Active Follicles Thinner, sparse hairs Reduced Skin Repair Skin repairs proceed more slowly. Decreased Immunity The number of dendritic cells decreases to about 50 percent of levels seen at maturity (roughly age 21). Thin Epidermis • Slow repairs • Decreased vitamin D production • Reduced number of Langerhans cells Reduced Sweat Gland Activity Tendency to overheat Changes in Distribution of Fat and Hair Due to reductions in sex hormone levels © 2012 Pearson Education, Inc. Dry Epidermis Reduction in sebaceous and sweat gland activity Reduced Blood Supply • Slow healing • Reduced ability to lose heat Thin Dermis Sagging and wrinkling due to fiber loss
 5 -11 Importance of the Integumentary System • Protects and interacts with all organ systems For example: • Cardiovascular system: Blood vessels in the dermis • Nervous system: Sensory receptors for pain, touch, and temperature • Changes in skin appearance are used to diagnose disorders in other systems © 2012 Pearson Education, Inc.
5 -11 Importance of the Integumentary System • Protects and interacts with all organ systems For example: • Cardiovascular system: Blood vessels in the dermis • Nervous system: Sensory receptors for pain, touch, and temperature • Changes in skin appearance are used to diagnose disorders in other systems © 2012 Pearson Education, Inc.
 Integumentary System-Clinical Acne: Inflammation of the sebaceous glands, blocked follicles, onset at puberty Dermatitis: Inflammation of the papillary layer of the dermis, Caused by infection, radiation, mechanical irritation, or chemicals (e. g. , poison ivy), Characterized by itch or pain Eczema: Allergic inflammation of the skin, onset usually in early childhood Ulcer: Localized shedding of epithelium Liposuction/Lipoplasty: Surgical removal of adipose tissue from the subcutaneous layer. © 2012 Pearson Education, Inc.
Integumentary System-Clinical Acne: Inflammation of the sebaceous glands, blocked follicles, onset at puberty Dermatitis: Inflammation of the papillary layer of the dermis, Caused by infection, radiation, mechanical irritation, or chemicals (e. g. , poison ivy), Characterized by itch or pain Eczema: Allergic inflammation of the skin, onset usually in early childhood Ulcer: Localized shedding of epithelium Liposuction/Lipoplasty: Surgical removal of adipose tissue from the subcutaneous layer. © 2012 Pearson Education, Inc.


