95a6149158474fa0f5b3f9cfd5a43957.ppt
- Количество слайдов: 23
 31 st Annual Conference Indian Association of Preventive and Social Medicine Health Sector Reforms: Relevance for India 27 th February 2004 Dr. Dinesh Agarwal, M. D. , Technical advisor (Reproductive Health) UNITED NATIONS POPULATION FUND, INDIA
31 st Annual Conference Indian Association of Preventive and Social Medicine Health Sector Reforms: Relevance for India 27 th February 2004 Dr. Dinesh Agarwal, M. D. , Technical advisor (Reproductive Health) UNITED NATIONS POPULATION FUND, INDIA
 Scope of Presentation q Health Sector in India and Characteristics q Health System Outcomes: Ultimate and Intermediate q What are reforms? q Do we need reforms in Health Sector? q Building A Reforms Agenda for India q Conclusions
Scope of Presentation q Health Sector in India and Characteristics q Health System Outcomes: Ultimate and Intermediate q What are reforms? q Do we need reforms in Health Sector? q Building A Reforms Agenda for India q Conclusions
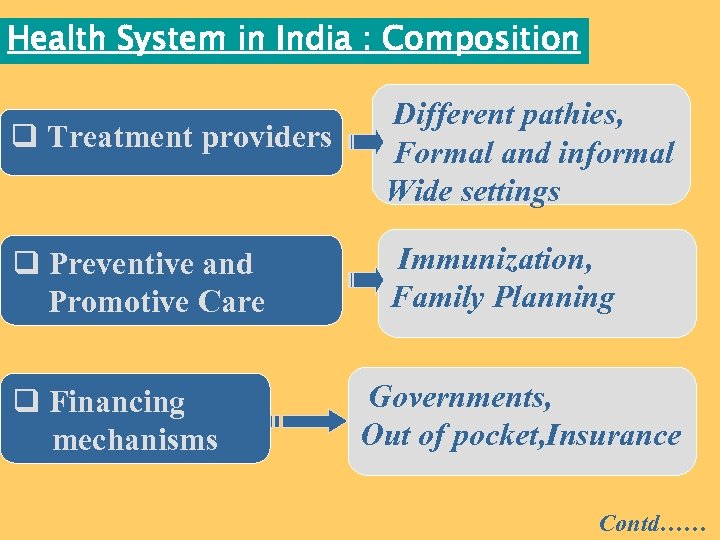 Health System in India : Composition q Treatment providers q Preventive and Promotive Care q Financing mechanisms Different pathies, Formal and informal Wide settings Immunization, Family Planning Governments, Out of pocket, Insurance Contd……
Health System in India : Composition q Treatment providers q Preventive and Promotive Care q Financing mechanisms Different pathies, Formal and informal Wide settings Immunization, Family Planning Governments, Out of pocket, Insurance Contd……
 Health System in India : Constituents q Input Producers Medical, Nurs. colleges Pharma, diagnostic Instruments q Planner and Health Managers PEOPLE , INSTITUTIONS AND ACTORS WHO WORK FOR HEALTH
Health System in India : Constituents q Input Producers Medical, Nurs. colleges Pharma, diagnostic Instruments q Planner and Health Managers PEOPLE , INSTITUTIONS AND ACTORS WHO WORK FOR HEALTH
 Health System in India : Characteristics q Vast and Complex: Multiple Planners and number of providers q 21% of Global burden of Diseases (16% population) q 25% of all Maternal Deaths Contd……
Health System in India : Characteristics q Vast and Complex: Multiple Planners and number of providers q 21% of Global burden of Diseases (16% population) q 25% of all Maternal Deaths Contd……
 Health System in India : Characteristics q Conflicts : Patient Care, Training and Research q Politics Influences: Goals, Priorities and Strategies: Variations in Commitment q Evolution of Health System reflect culture, history and norms
Health System in India : Characteristics q Conflicts : Patient Care, Training and Research q Politics Influences: Goals, Priorities and Strategies: Variations in Commitment q Evolution of Health System reflect culture, history and norms
 Goals of Health System 1. Health Status of Population Ø Life Expectancy ØDALYs lost ØMorbidity and Mortality rates Contd……
Goals of Health System 1. Health Status of Population Ø Life Expectancy ØDALYs lost ØMorbidity and Mortality rates Contd……
 Goal of Health Systems 2. Customer Satisfaction/Systems responsiveness Ø Client Satisfaction (NFHS) ØMay depend on non-clinical aspects of care ØDifficulty in measurement Contd……
Goal of Health Systems 2. Customer Satisfaction/Systems responsiveness Ø Client Satisfaction (NFHS) ØMay depend on non-clinical aspects of care ØDifficulty in measurement Contd……
 Goal of Health Systems 3. Financial Risk Protection Ø Are People protected against high cost of medical care? ØCatastrophic Illnesses – Poor People
Goal of Health Systems 3. Financial Risk Protection Ø Are People protected against high cost of medical care? ØCatastrophic Illnesses – Poor People
 How are we doing ? q Improved Life Expectancy: Yet averages mask equity perspectives ( Class, regional &gender) (49 years in 1970 to 63 years in 1998) q. High mortality and burden of diseases among poor: IMR, Diarrhea Diseases etc q. Client Satisfaction: ü“High” level in large scale data sets üHealth Sector most corrupt (Transparency International) Contd……
How are we doing ? q Improved Life Expectancy: Yet averages mask equity perspectives ( Class, regional &gender) (49 years in 1970 to 63 years in 1998) q. High mortality and burden of diseases among poor: IMR, Diarrhea Diseases etc q. Client Satisfaction: ü“High” level in large scale data sets üHealth Sector most corrupt (Transparency International) Contd……
 How are we doing ? q Overall Government spending 0. 9% GDP – Bottom quintile in world( WHO 2001) q. Private Expenditures: 80% of all spending on health q. Nearly 40% of hospitalized in 1995 -96 fell into debt. q. Large Scale Inter-State Variations: Risk of falling in debt after hospitalization (17% in Kerala – Double in UP/Bihar) Ref: Mehal et al 2001
How are we doing ? q Overall Government spending 0. 9% GDP – Bottom quintile in world( WHO 2001) q. Private Expenditures: 80% of all spending on health q. Nearly 40% of hospitalized in 1995 -96 fell into debt. q. Large Scale Inter-State Variations: Risk of falling in debt after hospitalization (17% in Kerala – Double in UP/Bihar) Ref: Mehal et al 2001
 Delivery of Public Health Services: Who uses? ? 1. Richest quintile consumes 3 times more public health resources as compared to poor 2. Most States reflect “Pro-rich” distribution 3. Health needs of urban poor, marginalized and Tribal population
Delivery of Public Health Services: Who uses? ? 1. Richest quintile consumes 3 times more public health resources as compared to poor 2. Most States reflect “Pro-rich” distribution 3. Health needs of urban poor, marginalized and Tribal population
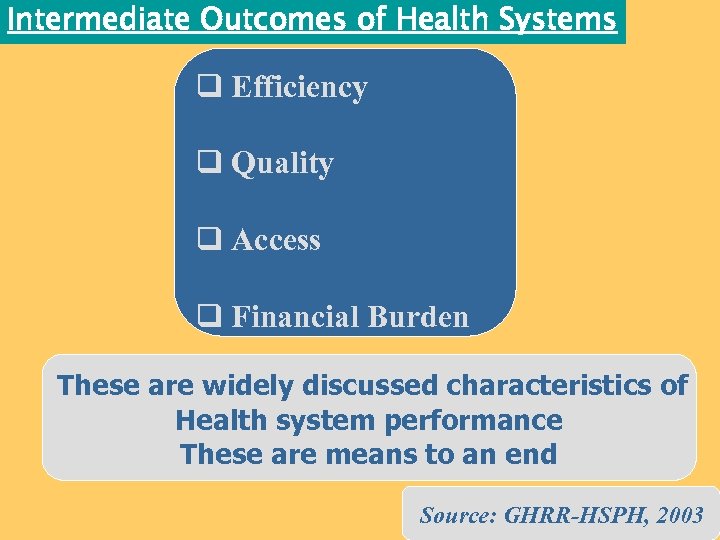 Intermediate Outcomes of Health Systems q Efficiency q Quality q Access q Financial Burden These are widely discussed characteristics of Health system performance These are means to an end Source: GHRR-HSPH, 2003
Intermediate Outcomes of Health Systems q Efficiency q Quality q Access q Financial Burden These are widely discussed characteristics of Health system performance These are means to an end Source: GHRR-HSPH, 2003
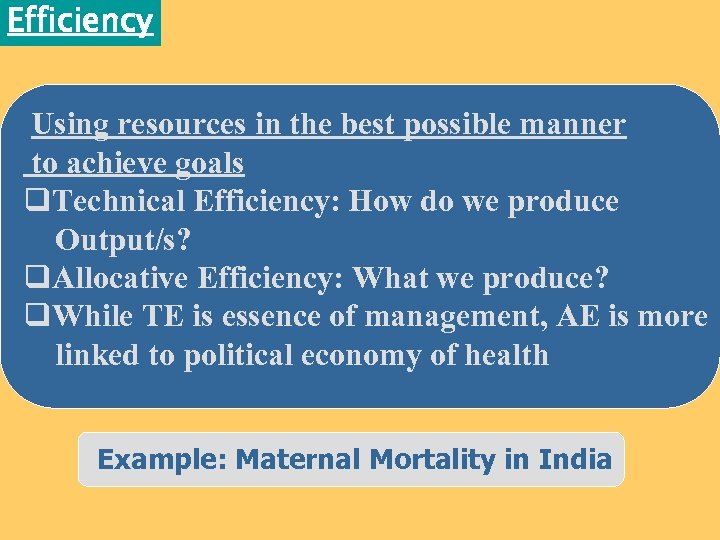 Efficiency Using resources in the best possible manner to achieve goals q. Technical Efficiency: How do we produce Output/s? q. Allocative Efficiency: What we produce? q. While TE is essence of management, AE is more linked to political economy of health Example: Maternal Mortality in India
Efficiency Using resources in the best possible manner to achieve goals q. Technical Efficiency: How do we produce Output/s? q. Allocative Efficiency: What we produce? q. While TE is essence of management, AE is more linked to political economy of health Example: Maternal Mortality in India
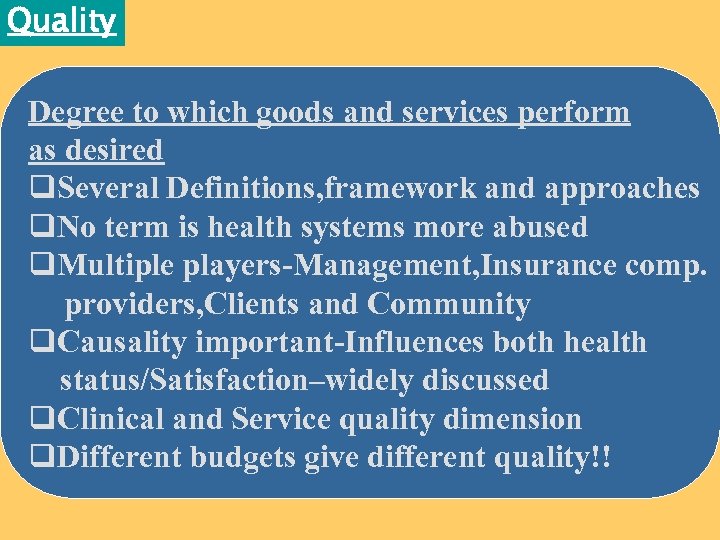 Quality Degree to which goods and services perform as desired q. Several Definitions, framework and approaches q. No term is health systems more abused q. Multiple players-Management, Insurance comp. providers, Clients and Community q. Causality important-Influences both health status/Satisfaction–widely discussed q. Clinical and Service quality dimension q. Different budgets give different quality!!
Quality Degree to which goods and services perform as desired q. Several Definitions, framework and approaches q. No term is health systems more abused q. Multiple players-Management, Insurance comp. providers, Clients and Community q. Causality important-Influences both health status/Satisfaction–widely discussed q. Clinical and Service quality dimension q. Different budgets give different quality!!
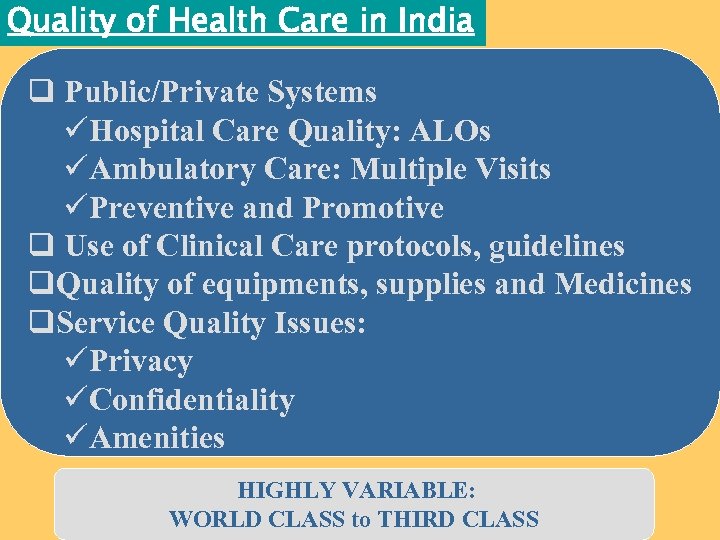 Quality of Health Care in India q Public/Private Systems üHospital Care Quality: ALOs üAmbulatory Care: Multiple Visits üPreventive and Promotive q Use of Clinical Care protocols, guidelines q. Quality of equipments, supplies and Medicines q. Service Quality Issues: üPrivacy üConfidentiality üAmenities HIGHLY VARIABLE: WORLD CLASS to THIRD CLASS
Quality of Health Care in India q Public/Private Systems üHospital Care Quality: ALOs üAmbulatory Care: Multiple Visits üPreventive and Promotive q Use of Clinical Care protocols, guidelines q. Quality of equipments, supplies and Medicines q. Service Quality Issues: üPrivacy üConfidentiality üAmenities HIGHLY VARIABLE: WORLD CLASS to THIRD CLASS
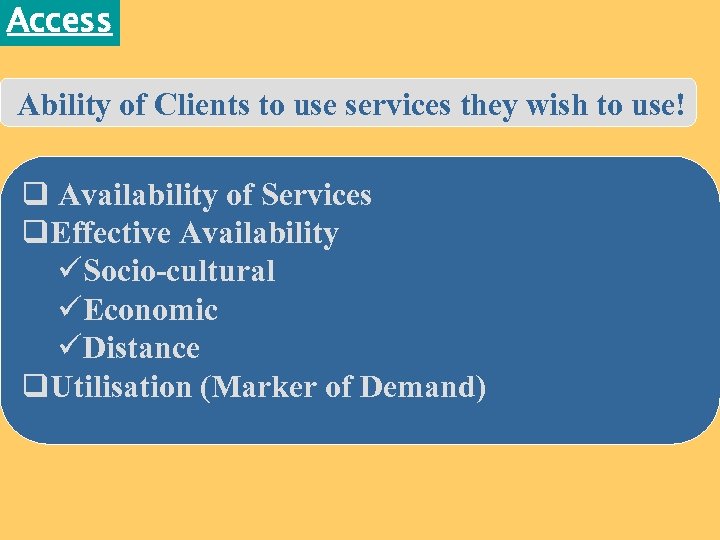 Access Ability of Clients to use services they wish to use! q Availability of Services q. Effective Availability üSocio-cultural üEconomic üDistance q. Utilisation (Marker of Demand)
Access Ability of Clients to use services they wish to use! q Availability of Services q. Effective Availability üSocio-cultural üEconomic üDistance q. Utilisation (Marker of Demand)
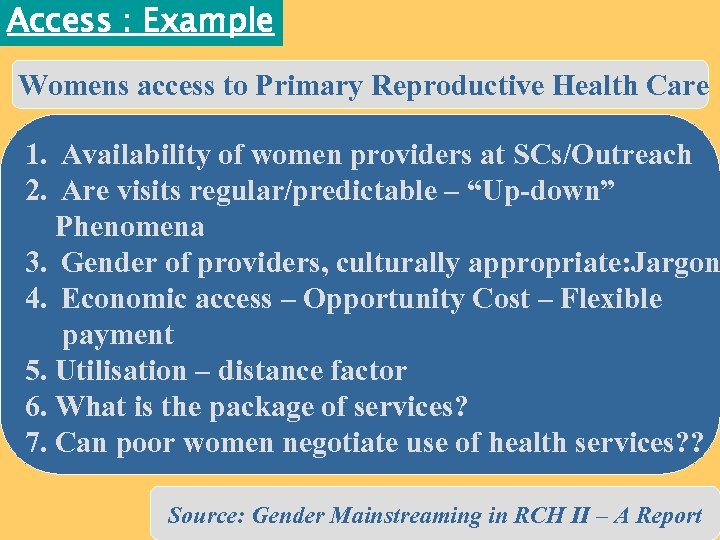 Access : Example Womens access to Primary Reproductive Health Care 1. Availability of women providers at SCs/Outreach 2. Are visits regular/predictable – “Up-down” Phenomena 3. Gender of providers, culturally appropriate: Jargon 4. Economic access – Opportunity Cost – Flexible payment 5. Utilisation – distance factor 6. What is the package of services? 7. Can poor women negotiate use of health services? ? Source: Gender Mainstreaming in RCH II – A Report
Access : Example Womens access to Primary Reproductive Health Care 1. Availability of women providers at SCs/Outreach 2. Are visits regular/predictable – “Up-down” Phenomena 3. Gender of providers, culturally appropriate: Jargon 4. Economic access – Opportunity Cost – Flexible payment 5. Utilisation – distance factor 6. What is the package of services? 7. Can poor women negotiate use of health services? ? Source: Gender Mainstreaming in RCH II – A Report
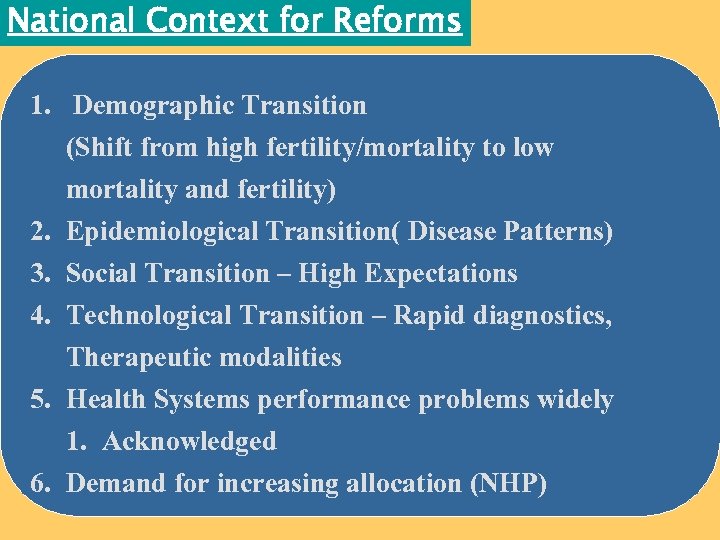 National Context for Reforms 1. Demographic Transition (Shift from high fertility/mortality to low mortality and fertility) 2. Epidemiological Transition( Disease Patterns) 3. Social Transition – High Expectations 4. Technological Transition – Rapid diagnostics, Therapeutic modalities 5. Health Systems performance problems widely 1. Acknowledged 6. Demand for increasing allocation (NHP)
National Context for Reforms 1. Demographic Transition (Shift from high fertility/mortality to low mortality and fertility) 2. Epidemiological Transition( Disease Patterns) 3. Social Transition – High Expectations 4. Technological Transition – Rapid diagnostics, Therapeutic modalities 5. Health Systems performance problems widely 1. Acknowledged 6. Demand for increasing allocation (NHP)
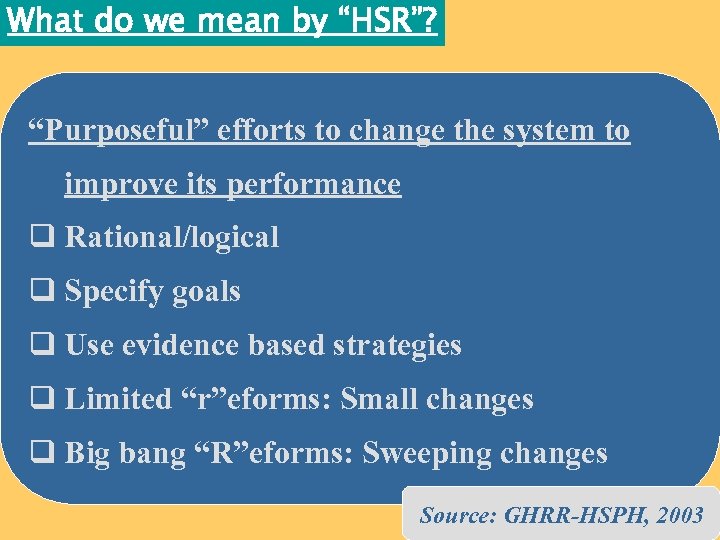 What do we mean by “HSR”? “Purposeful” efforts to change the system to improve its performance q Rational/logical q Specify goals q Use evidence based strategies q Limited “r”eforms: Small changes q Big bang “R”eforms: Sweeping changes Source: GHRR-HSPH, 2003
What do we mean by “HSR”? “Purposeful” efforts to change the system to improve its performance q Rational/logical q Specify goals q Use evidence based strategies q Limited “r”eforms: Small changes q Big bang “R”eforms: Sweeping changes Source: GHRR-HSPH, 2003
 Reforms Agenda for India 1. Health Policy Process – Decentralization, devolution, delegation: “ONE SIZE DOES NOT FIT ALL” 2. Content: Comprehensive, Epidemiological 1. Transition, Standards, private sector 3. Oversight function – Regulation (Clinical establishment, PNDT, HOT Acts) 4. Health Financing Options
Reforms Agenda for India 1. Health Policy Process – Decentralization, devolution, delegation: “ONE SIZE DOES NOT FIT ALL” 2. Content: Comprehensive, Epidemiological 1. Transition, Standards, private sector 3. Oversight function – Regulation (Clinical establishment, PNDT, HOT Acts) 4. Health Financing Options
 Barriers to “Reforms” 1. Reforms are “Hard” Choices: Truly Difficult 2. Often consequences of actions are difficult to predict 3. Doing better for one goal may not necessarily lead to improvement in other goals 4. Resistance to “Change” “Status quoists” 5. Those who can benefit from reforms are not powerfully/less organised
Barriers to “Reforms” 1. Reforms are “Hard” Choices: Truly Difficult 2. Often consequences of actions are difficult to predict 3. Doing better for one goal may not necessarily lead to improvement in other goals 4. Resistance to “Change” “Status quoists” 5. Those who can benefit from reforms are not powerfully/less organised
 THANKS
THANKS


