dd486e98a806dbb1401d918aab879669.ppt
- Количество слайдов: 34
 3 rd Annual Association of Clinical Documentation Improvement Specialists Conference
3 rd Annual Association of Clinical Documentation Improvement Specialists Conference
 Strategies for achieving medical staff compliance Trey La Charité, MD CDI Program Physician Advisor, Hospitalist, Clinical Assistant Professor
Strategies for achieving medical staff compliance Trey La Charité, MD CDI Program Physician Advisor, Hospitalist, Clinical Assistant Professor
 Objectives: • Learn effective PA techniques for cultivating medical staff acceptance of and sustained participation with CDI goals – Review continuous educational efforts • “What’s wrong with the way I write in the chart? ” – Promotion of CDI program as team effort – Generation of effective CDI compliance tools
Objectives: • Learn effective PA techniques for cultivating medical staff acceptance of and sustained participation with CDI goals – Review continuous educational efforts • “What’s wrong with the way I write in the chart? ” – Promotion of CDI program as team effort – Generation of effective CDI compliance tools
 Physician CDI presentations • Make each presentation service-line specific – Orthopods don’t care about “chronic systolic CHF. ” • Make sure they understand why it is important to learn the rules of “The Game” that CMS creates: – The pressures that each treating facility faces – The pressures that each physician will face • Introduce more accurate methods and terminology to appropriately document each patient’s severity of illness in the medical record – How to effectively play CMS’ game
Physician CDI presentations • Make each presentation service-line specific – Orthopods don’t care about “chronic systolic CHF. ” • Make sure they understand why it is important to learn the rules of “The Game” that CMS creates: – The pressures that each treating facility faces – The pressures that each physician will face • Introduce more accurate methods and terminology to appropriately document each patient’s severity of illness in the medical record – How to effectively play CMS’ game
 Physician CDI presentations • Ensure that each physician understands every reason why participation in CDI efforts is so crucial for them • Ensure that each physician understands that compliance with CDI goals is strictly their responsibility – CDI is not a coding issue! • Ensure that each physician understands how to be compliant with CDI goals
Physician CDI presentations • Ensure that each physician understands every reason why participation in CDI efforts is so crucial for them • Ensure that each physician understands that compliance with CDI goals is strictly their responsibility – CDI is not a coding issue! • Ensure that each physician understands how to be compliant with CDI goals
 Why implement CDI? • To make YOU and their facility look better in the • • • public perception with quality data reporting To make YOU look better to health insurance companies & CMS for coming P 4 P initiatives To improve YOUR and their facility’s L. O. S. To appropriately categorize and justify YOUR patients’ admission status within hospital system To realize all GME educational goals To realize all appropriate reimbursements
Why implement CDI? • To make YOU and their facility look better in the • • • public perception with quality data reporting To make YOU look better to health insurance companies & CMS for coming P 4 P initiatives To improve YOUR and their facility’s L. O. S. To appropriately categorize and justify YOUR patients’ admission status within hospital system To realize all GME educational goals To realize all appropriate reimbursements
 Medical staff follow-up • Present CDI updates at quarterly medical staff meetings – Show changes in ICD-9 terminology – Give examples of cases where physicians either listened to or ignored CDI specialist queries with consequences of their actions – Give assurances that we are not asking them to lie, cheat, steal, mislead, commit fraud, etc. – Remind them why CDI is so important – Give CDI improvement tips
Medical staff follow-up • Present CDI updates at quarterly medical staff meetings – Show changes in ICD-9 terminology – Give examples of cases where physicians either listened to or ignored CDI specialist queries with consequences of their actions – Give assurances that we are not asking them to lie, cheat, steal, mislead, commit fraud, etc. – Remind them why CDI is so important – Give CDI improvement tips
 Promote CDI as a team effort • Attend all weekly CDI core team meetings – Everyone in room has equal status • All on first name basis with no rank • All trying to reach same goal – Review problematic/denied queries with team – Provide needed clinical education to CDI team – Allows quick CDI response for acute issues – Allows for free generation of new ideas • CDI specialists much more in touch with what is happening on their floors than PA
Promote CDI as a team effort • Attend all weekly CDI core team meetings – Everyone in room has equal status • All on first name basis with no rank • All trying to reach same goal – Review problematic/denied queries with team – Provide needed clinical education to CDI team – Allows quick CDI response for acute issues – Allows for free generation of new ideas • CDI specialists much more in touch with what is happening on their floors than PA
 Promote CDI as a team effort • Give credit where and when credit is due • Search for ways to make CDS specialists’ work experience more efficient and effective – CDS specialists should be on wards, not in the office • Provide yearly membership in ACDIS • Send team members to annual ACDIS conference – All members should have opportunity to attend • Review insurance/RAC coding denials, assist in appeals, and provide medical staff education regarding changes • Participate in coder education • Keep CDI Program momentum going
Promote CDI as a team effort • Give credit where and when credit is due • Search for ways to make CDS specialists’ work experience more efficient and effective – CDS specialists should be on wards, not in the office • Provide yearly membership in ACDIS • Send team members to annual ACDIS conference – All members should have opportunity to attend • Review insurance/RAC coding denials, assist in appeals, and provide medical staff education regarding changes • Participate in coder education • Keep CDI Program momentum going
 Compliance tools • PA must be creative in order to develop physician friendly CDI compliance methods that garner consistent, sustainable results • Physicians see themselves as overworked and extremely busy – Physicians willing to comply if. . . • Request does not impact their perceived time constraints • It’s believed to be more than just an additional hassle of dubious reward
Compliance tools • PA must be creative in order to develop physician friendly CDI compliance methods that garner consistent, sustainable results • Physicians see themselves as overworked and extremely busy – Physicians willing to comply if. . . • Request does not impact their perceived time constraints • It’s believed to be more than just an additional hassle of dubious reward
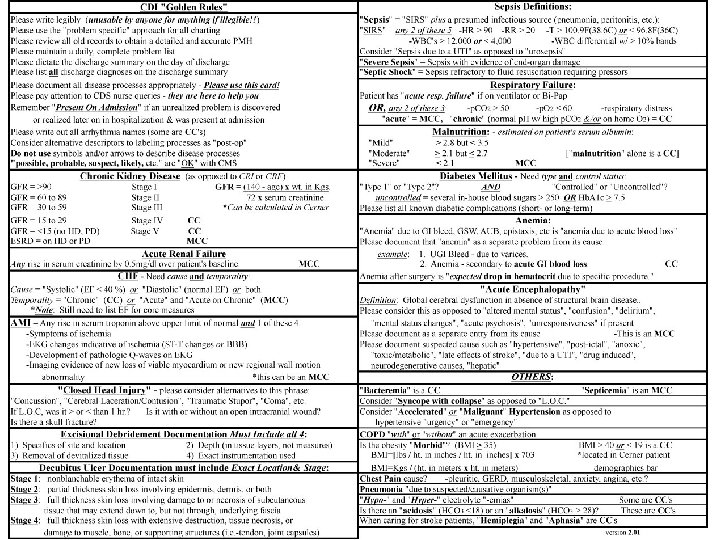
 CDI pocket cards • Everybody has one and they all work great! • “Universal” or “service-line specific”? • Advantages of universal CDI card: – Everyone speaks the same language – Promote house-wide team building vs. additional individual physician or group responsibilities – Ease of implementing CMS/RAC updates – Can be facility specific • No two hospitals alike!
CDI pocket cards • Everybody has one and they all work great! • “Universal” or “service-line specific”? • Advantages of universal CDI card: – Everyone speaks the same language – Promote house-wide team building vs. additional individual physician or group responsibilities – Ease of implementing CMS/RAC updates – Can be facility specific • No two hospitals alike!
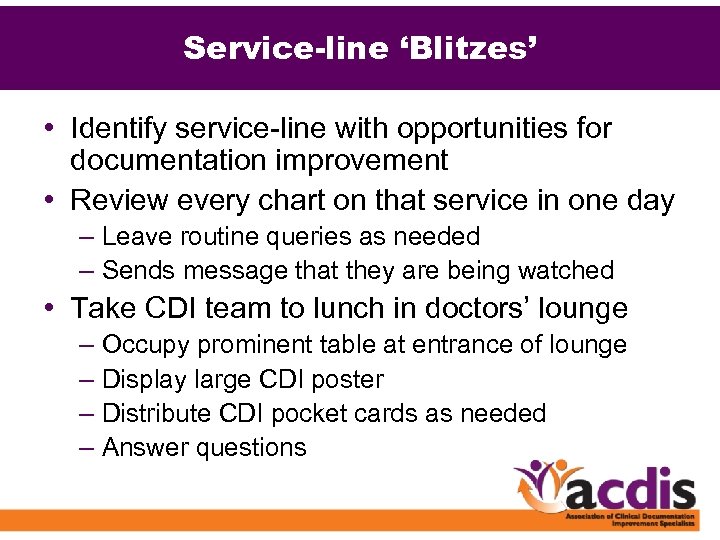 Service-line ‘Blitzes’ • Identify service-line with opportunities for documentation improvement • Review every chart on that service in one day – Leave routine queries as needed – Sends message that they are being watched • Take CDI team to lunch in doctors’ lounge – Occupy prominent table at entrance of lounge – Display large CDI poster – Distribute CDI pocket cards as needed – Answer questions
Service-line ‘Blitzes’ • Identify service-line with opportunities for documentation improvement • Review every chart on that service in one day – Leave routine queries as needed – Sends message that they are being watched • Take CDI team to lunch in doctors’ lounge – Occupy prominent table at entrance of lounge – Display large CDI poster – Distribute CDI pocket cards as needed – Answer questions
 Inciting ‘SHAME!’ • Show data to medical staff that suggests to the public they are not good doctors • Show data to the medical staff that suggests their local competition is doing a better job of taking care of patients than they do – Physicians are competitive and defensive about their abilities and skills – Use physician egos to your advantage!
Inciting ‘SHAME!’ • Show data to medical staff that suggests to the public they are not good doctors • Show data to the medical staff that suggests their local competition is doing a better job of taking care of patients than they do – Physicians are competitive and defensive about their abilities and skills – Use physician egos to your advantage!

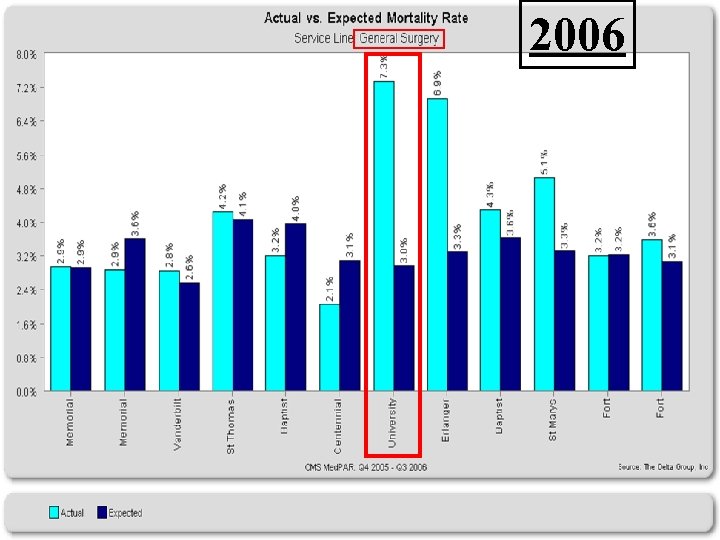 2006
2006
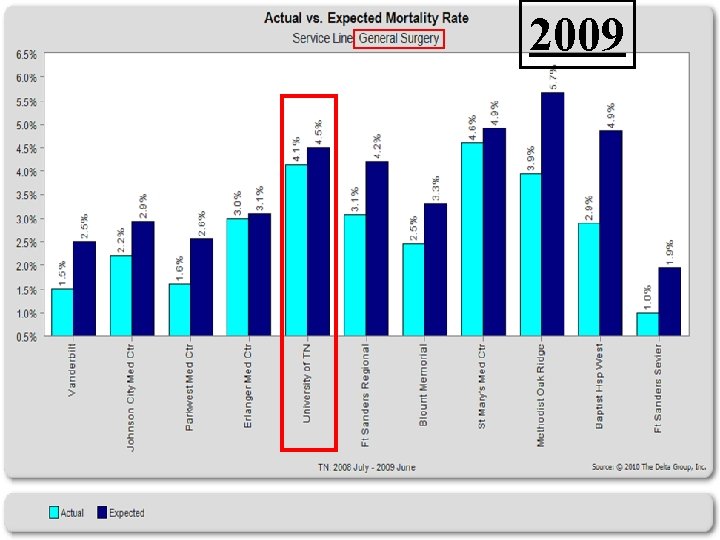 2009
2009
 Inciting ‘SHAME!’ • Save examples where physician(s) ignored or disagreed with query that would have resulted in substantial MS-DRG impact • Present those cases at general medical staff meeting with all pertinent ramifications. . . • • What diagnoses they missed Lack of meeting GM-LOS goal Loss of reimbursement to hospital Physician report card impact • Show them the error of their ways!
Inciting ‘SHAME!’ • Save examples where physician(s) ignored or disagreed with query that would have resulted in substantial MS-DRG impact • Present those cases at general medical staff meeting with all pertinent ramifications. . . • • What diagnoses they missed Lack of meeting GM-LOS goal Loss of reimbursement to hospital Physician report card impact • Show them the error of their ways!

 Example #1 • 67 yo WM w/ HTN & hyperlipidemia goes to OSH w/ chest pain & diaphoresis. EKG shows ST-segment elevations in anterior leads. Patient transferred to UTMCK & immediately taken to cath lab. Patient arrests @ end of procedure and is intubated and revived during Code 99. IABP is placed & patient taken to ICU.
Example #1 • 67 yo WM w/ HTN & hyperlipidemia goes to OSH w/ chest pain & diaphoresis. EKG shows ST-segment elevations in anterior leads. Patient transferred to UTMCK & immediately taken to cath lab. Patient arrests @ end of procedure and is intubated and revived during Code 99. IABP is placed & patient taken to ICU.
 Example #1 • What are the diagnoses in example #1? – HTN – Hyperlipidemia – Acute Myocardial Infarction – Cardiogenic Shock – (MCC) • IABP was placed – Acute Respiratory Failure – (MCC) • This patient was intubated when he arrested.
Example #1 • What are the diagnoses in example #1? – HTN – Hyperlipidemia – Acute Myocardial Infarction – Cardiogenic Shock – (MCC) • IABP was placed – Acute Respiratory Failure – (MCC) • This patient was intubated when he arrested.
 Example #1 • Despite repeated queries and phone calls by CDS specialists, no documentation was ever made in the medical record that this patient had “cardiogenic shock” or “acute respiratory failure. ”
Example #1 • Despite repeated queries and phone calls by CDS specialists, no documentation was ever made in the medical record that this patient had “cardiogenic shock” or “acute respiratory failure. ”
 Example #1: $31, 436. 00 4. 5950 15. 6 If “Acute Respiratory Failure” or “Cardiogenic Shock” had been documented. . . (MCCs).
Example #1: $31, 436. 00 4. 5950 15. 6 If “Acute Respiratory Failure” or “Cardiogenic Shock” had been documented. . . (MCCs).
 Example #2 • 66 yo WM w/ HTN, DM, & PVD goes to ER w/ 3 days of LLE pain, erythema, fever, & chills. T=101. 9 F, HR=113, WBCs=17 K, albumin=1. 9, & Hb. A 1 c=8. 3. BMI=18. 6. A foul smell is noted from LLE. Patient diagnosed w/ cellulitis & gangrene and undergoes BKA. Four days later, the patient unexpectedly arrests and cannot be revived.
Example #2 • 66 yo WM w/ HTN, DM, & PVD goes to ER w/ 3 days of LLE pain, erythema, fever, & chills. T=101. 9 F, HR=113, WBCs=17 K, albumin=1. 9, & Hb. A 1 c=8. 3. BMI=18. 6. A foul smell is noted from LLE. Patient diagnosed w/ cellulitis & gangrene and undergoes BKA. Four days later, the patient unexpectedly arrests and cannot be revived.
 Example #2 • What are the diagnoses in example #2? – HTN – PVD – Diabetes Mellitus – “Type 2” & “uncontrolled” – Cellulitis and gangrene (CC) – Sepsis – (MCC) • Elevated Temp, HR, & WBC’s @ admission met criteria for SIRS. Source was patient’s LLE cellulitis – Malnutrition – “severe” – (MCC) • Admission albumin = 1. 9 & BMI < 19
Example #2 • What are the diagnoses in example #2? – HTN – PVD – Diabetes Mellitus – “Type 2” & “uncontrolled” – Cellulitis and gangrene (CC) – Sepsis – (MCC) • Elevated Temp, HR, & WBC’s @ admission met criteria for SIRS. Source was patient’s LLE cellulitis – Malnutrition – “severe” – (MCC) • Admission albumin = 1. 9 & BMI < 19
 Example #2 • At the time of admission, the physician only documented “Cellulitis” and did not mention “Sepsis” or “Severe Malnutrition” in the medical record.
Example #2 • At the time of admission, the physician only documented “Cellulitis” and did not mention “Sepsis” or “Severe Malnutrition” in the medical record.
 Note: The physician paid attention to the query placed on the patient’s chart by CDS nurse & documented both “Sepsis” & “Severe Malnutrition. ”
Note: The physician paid attention to the query placed on the patient’s chart by CDS nurse & documented both “Sepsis” & “Severe Malnutrition. ”
 Example #2: “Sepsis” as principal diagnosis with “Severe Malnutrition” as MCC Amputation for Circulatory Disorders w/o CC or MCC with RW = 2. 99 GMLOS=7. 3 $20, 852. 56
Example #2: “Sepsis” as principal diagnosis with “Severe Malnutrition” as MCC Amputation for Circulatory Disorders w/o CC or MCC with RW = 2. 99 GMLOS=7. 3 $20, 852. 56
 What about quality ratings? • Predicted Mortality Rates for some disease processes in this case: – Cellulitis w/ gangrene = 15% – Sepsis = 30% – Septic shock = 80% • The patient expired which is never good for any physician’s report card: – However, by listening to the CDS nurse, this physician’s expected mortality bar is much higher than it would have been for “cellulitis” only.
What about quality ratings? • Predicted Mortality Rates for some disease processes in this case: – Cellulitis w/ gangrene = 15% – Sepsis = 30% – Septic shock = 80% • The patient expired which is never good for any physician’s report card: – However, by listening to the CDS nurse, this physician’s expected mortality bar is much higher than it would have been for “cellulitis” only.
 Problematic service-lines? • Concentrate CDI training efforts on consultants and residents to improve documentation – Both sources of documentation can be coded. • Treat unanswered queries as incomplete charts – May require change in medical staff by-laws • Insert CDI goals into data gathering IS tools – Do you have EHR or CPOE? • Insert CDI goals into pre-operative clinics – Pre-operative clinic H&P can be coded as long as done 30 days prior to surgery.
Problematic service-lines? • Concentrate CDI training efforts on consultants and residents to improve documentation – Both sources of documentation can be coded. • Treat unanswered queries as incomplete charts – May require change in medical staff by-laws • Insert CDI goals into data gathering IS tools – Do you have EHR or CPOE? • Insert CDI goals into pre-operative clinics – Pre-operative clinic H&P can be coded as long as done 30 days prior to surgery.

 Physician interventions? • Many programs use one-on-one PA interaction with medical staff to get needed results. – Physicians do not like “backseat drivers” – Potentially places PA in adversarial relationship with medical staff • If query is ignored while patient in hospital, convert to post-discharge query – Make medical record incomplete until answered • “Carrot Approach” as opposed to “Sticks. ”
Physician interventions? • Many programs use one-on-one PA interaction with medical staff to get needed results. – Physicians do not like “backseat drivers” – Potentially places PA in adversarial relationship with medical staff • If query is ignored while patient in hospital, convert to post-discharge query – Make medical record incomplete until answered • “Carrot Approach” as opposed to “Sticks. ”
 Physician advisor results • Physician Advisor will not be “Silver Bullet” for your CDI Program • CDI program success is team effort: – Must have CDI chart review specialists to reinforce medical staff education with good, consistent queries – Must have strong administrative support – Must have strong coding department support • Results will not happen overnight!
Physician advisor results • Physician Advisor will not be “Silver Bullet” for your CDI Program • CDI program success is team effort: – Must have CDI chart review specialists to reinforce medical staff education with good, consistent queries – Must have strong administrative support – Must have strong coding department support • Results will not happen overnight!
 Questions?
Questions?


