5503b1a296ef0fe5c07b66c11c349f4a.ppt
- Количество слайдов: 119
 2010 Annual Fraud Awareness Training For Insurance Professionals What Every Insurance Professional Should Know About Insurance Fraud A Global Leader in Compliance and Investigation Solutions
2010 Annual Fraud Awareness Training For Insurance Professionals What Every Insurance Professional Should Know About Insurance Fraud A Global Leader in Compliance and Investigation Solutions
 2010 Annual Fraud Awareness Training For Insurance Professionals Welcome to the Matrix Absence Management, Inc. , Special Investigative Unit’s online training course. This Power. Point presentation and 10 question test is designed to meet the various state requirements for Annual Anti-Fraud Training. Matrix Absence Management, Inc. , has contracted with the national investigative firm of G 4 S Compliance & Investigations to be the company’s Special Investigations Unit. The person in charge of the outsourced SIU is Cheryl Nordheim, Compliance Manager – Matrix Absence Management, Inc. (408) 361 -7219 cheryl. nordheim@matrixcos. com Your program administrator is Valerie Beebe, FCLS SIU Compliance Manager of G 4 S Compliance & Investigations. Should you have questions, please feel free to call Valerie at (704) 560 -6203 or via. email at valerie. beebe@cni. g 4 s. com A Global Leader in Compliance and Investigation Solutions
2010 Annual Fraud Awareness Training For Insurance Professionals Welcome to the Matrix Absence Management, Inc. , Special Investigative Unit’s online training course. This Power. Point presentation and 10 question test is designed to meet the various state requirements for Annual Anti-Fraud Training. Matrix Absence Management, Inc. , has contracted with the national investigative firm of G 4 S Compliance & Investigations to be the company’s Special Investigations Unit. The person in charge of the outsourced SIU is Cheryl Nordheim, Compliance Manager – Matrix Absence Management, Inc. (408) 361 -7219 cheryl. nordheim@matrixcos. com Your program administrator is Valerie Beebe, FCLS SIU Compliance Manager of G 4 S Compliance & Investigations. Should you have questions, please feel free to call Valerie at (704) 560 -6203 or via. email at valerie. beebe@cni. g 4 s. com A Global Leader in Compliance and Investigation Solutions
 2010 Annual Fraud Awareness Training For Insurance Professionals IMPORTANT REMINDER FOR ALL MATRIX EMPLOYEES: It is critical that we maintain the confidentiality of business records, and the security of our corporate computer network. Login I. D. and password information is provided to employees so that you can access the network to perform the responsibilities of your position. Employees should never compromise the integrity of the network or the company by giving your login and/or password information to anyone else. This includes persons inside or outside of the company, including a colleague or manager. Additionally, in accordance with our Code of Conduct, if anyone asks you for password information, you should report it to your manager, any officer, Company Counsel or the Ethics Hotline immediately. A Global Leader in Compliance and Investigation Solutions
2010 Annual Fraud Awareness Training For Insurance Professionals IMPORTANT REMINDER FOR ALL MATRIX EMPLOYEES: It is critical that we maintain the confidentiality of business records, and the security of our corporate computer network. Login I. D. and password information is provided to employees so that you can access the network to perform the responsibilities of your position. Employees should never compromise the integrity of the network or the company by giving your login and/or password information to anyone else. This includes persons inside or outside of the company, including a colleague or manager. Additionally, in accordance with our Code of Conduct, if anyone asks you for password information, you should report it to your manager, any officer, Company Counsel or the Ethics Hotline immediately. A Global Leader in Compliance and Investigation Solutions
 Training Overview • Part I – General Fraud Awareness A – Fraud Facts B – 2009 NICB Statistics • Part 2 – CA SIU Compliance Regulations • Part 3 - G 4 S SIU Successful Investigations • Part 4 – Defining Insurance Fraud • Part 5 – Emerging Fraud Trends • Part 6 - Insurance Fraud & Red Flag Indicators By Line of Business A – Workers’ Compensation Fraud B – General Liability Fraud C – Auto Fraud D – Property Fraud • Part 7 – SIU Org Chart • Part 8 – SIU Contact Information A Global Leader in Compliance and Investigation Solutions
Training Overview • Part I – General Fraud Awareness A – Fraud Facts B – 2009 NICB Statistics • Part 2 – CA SIU Compliance Regulations • Part 3 - G 4 S SIU Successful Investigations • Part 4 – Defining Insurance Fraud • Part 5 – Emerging Fraud Trends • Part 6 - Insurance Fraud & Red Flag Indicators By Line of Business A – Workers’ Compensation Fraud B – General Liability Fraud C – Auto Fraud D – Property Fraud • Part 7 – SIU Org Chart • Part 8 – SIU Contact Information A Global Leader in Compliance and Investigation Solutions
 Fraud Facts • More than 220 BILLION dollars a year in fraudulent claims in the U. S. • If insurance fraud and auto theft were a business, it would rank in the Top 25 of the Fortune 500. • 13 cents of every premium dollar goes to fraudulent claims. • 15% of all claims are fraudulent or inflated. • 18% of all theft claims are fraudulent or inflated. • 33% of all bodily injury claims for auto accidents contain some fraud – but only 3% are totally fraudulent from deliberate scams such as staged accidents. • 35% of all workers’ compensation claims are fraudulent or inflated. A Global Leader in Compliance and Investigation Solutions
Fraud Facts • More than 220 BILLION dollars a year in fraudulent claims in the U. S. • If insurance fraud and auto theft were a business, it would rank in the Top 25 of the Fortune 500. • 13 cents of every premium dollar goes to fraudulent claims. • 15% of all claims are fraudulent or inflated. • 18% of all theft claims are fraudulent or inflated. • 33% of all bodily injury claims for auto accidents contain some fraud – but only 3% are totally fraudulent from deliberate scams such as staged accidents. • 35% of all workers’ compensation claims are fraudulent or inflated. A Global Leader in Compliance and Investigation Solutions
 Fraud Facts These are conservative estimates! Think about your own claims inventory? A Global Leader in Compliance and Investigation Solutions
Fraud Facts These are conservative estimates! Think about your own claims inventory? A Global Leader in Compliance and Investigation Solutions
 Acceptability of Insurance Fraud The following statistics represent the public’s view of acceptable insurance fraud: • Increase claim to make up for deductible ---------- 33% Agree • Stay out of work longer than necessary ----------- 25% Agree • Increase claim to make up for premium ----------- 22% Agree • Deliberately underestimate miles driven ----------– 18% Agree • Say vehicle is garaged in area to obtain lower rates ----- 15% Agree • Submit bills for treatment never received ---------- 13% Agree • Fail to list prior accidents, tickets, or claims --------– 8% Agree • Add old damage to new claim ------------------ 5% Agree A Global Leader in Compliance and Investigation Solutions
Acceptability of Insurance Fraud The following statistics represent the public’s view of acceptable insurance fraud: • Increase claim to make up for deductible ---------- 33% Agree • Stay out of work longer than necessary ----------- 25% Agree • Increase claim to make up for premium ----------- 22% Agree • Deliberately underestimate miles driven ----------– 18% Agree • Say vehicle is garaged in area to obtain lower rates ----- 15% Agree • Submit bills for treatment never received ---------- 13% Agree • Fail to list prior accidents, tickets, or claims --------– 8% Agree • Add old damage to new claim ------------------ 5% Agree A Global Leader in Compliance and Investigation Solutions
 Acceptability of Insurance Fraud An analysis of the National Insurance Crime Bureau (NICB) 2008 and 2009 Questionable Claims (QCs) was performed to compare Property, Casualty, Commercial, Workers’ Compensation, Vehicle, and Miscellaneous referral categories. The 2008 Questionable Claims totaled 74, 902 while 2009 Questionable Claims totaled 85, 209. All categories showed an increase in referrals in 2009, even though some individual referral reasons showed a decrease. Also, similar to previous Questionable Claims analysis reports, an increase in referrals related to natural disasters can be seen in Property, Vehicle, and Miscellaneous categories. Tables and charts are organized by greatest percent change. NICB 2009 Annual Report A Global Leader in Compliance and Investigation Solutions
Acceptability of Insurance Fraud An analysis of the National Insurance Crime Bureau (NICB) 2008 and 2009 Questionable Claims (QCs) was performed to compare Property, Casualty, Commercial, Workers’ Compensation, Vehicle, and Miscellaneous referral categories. The 2008 Questionable Claims totaled 74, 902 while 2009 Questionable Claims totaled 85, 209. All categories showed an increase in referrals in 2009, even though some individual referral reasons showed a decrease. Also, similar to previous Questionable Claims analysis reports, an increase in referrals related to natural disasters can be seen in Property, Vehicle, and Miscellaneous categories. Tables and charts are organized by greatest percent change. NICB 2009 Annual Report A Global Leader in Compliance and Investigation Solutions
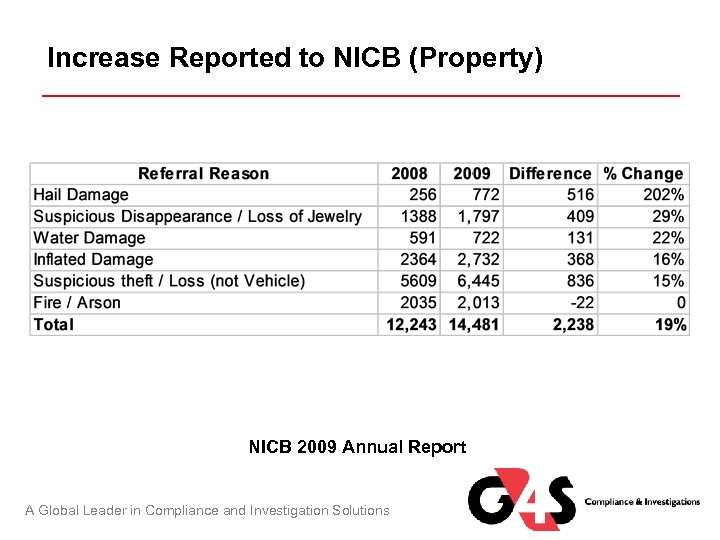 Increase Reported to NICB (Property) NICB 2009 Annual Report A Global Leader in Compliance and Investigation Solutions
Increase Reported to NICB (Property) NICB 2009 Annual Report A Global Leader in Compliance and Investigation Solutions
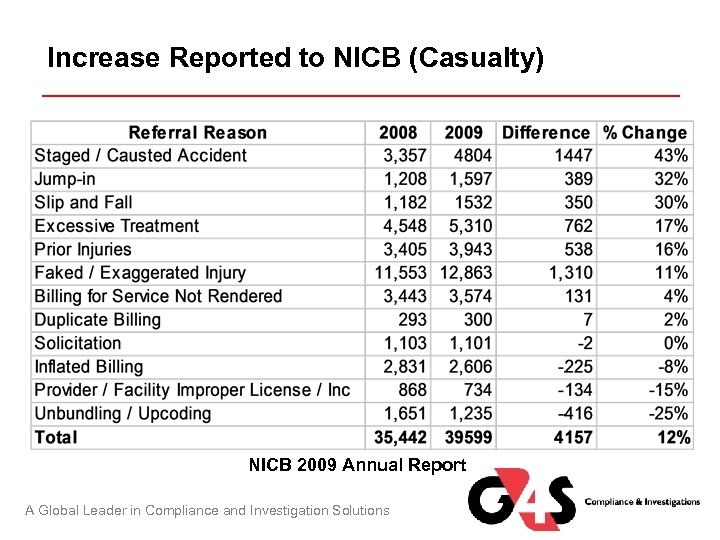 Increase Reported to NICB (Casualty) NICB 2009 Annual Report A Global Leader in Compliance and Investigation Solutions
Increase Reported to NICB (Casualty) NICB 2009 Annual Report A Global Leader in Compliance and Investigation Solutions
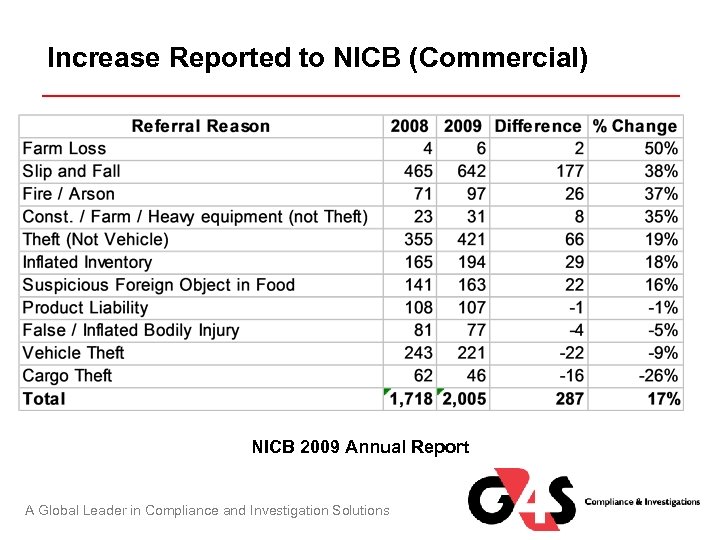 Increase Reported to NICB (Commercial) NICB 2009 Annual Report A Global Leader in Compliance and Investigation Solutions
Increase Reported to NICB (Commercial) NICB 2009 Annual Report A Global Leader in Compliance and Investigation Solutions
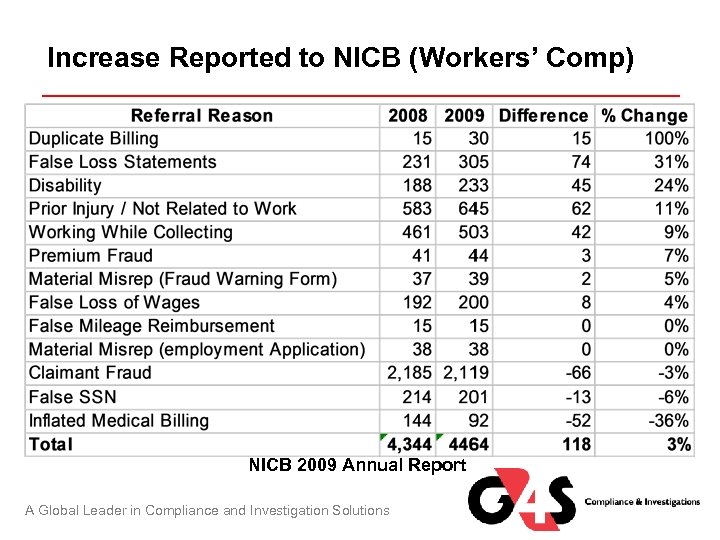 Increase Reported to NICB (Workers’ Comp) NICB 2009 Annual Report A Global Leader in Compliance and Investigation Solutions
Increase Reported to NICB (Workers’ Comp) NICB 2009 Annual Report A Global Leader in Compliance and Investigation Solutions
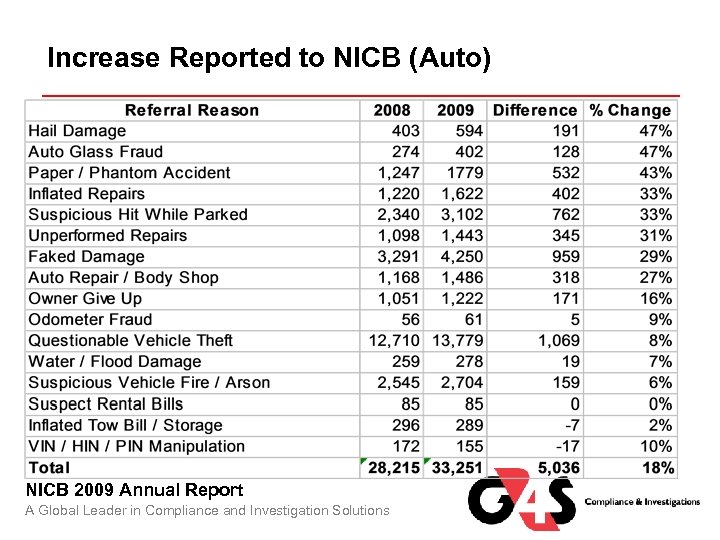 Increase Reported to NICB (Auto) NICB 2009 Annual Report A Global Leader in Compliance and Investigation Solutions
Increase Reported to NICB (Auto) NICB 2009 Annual Report A Global Leader in Compliance and Investigation Solutions
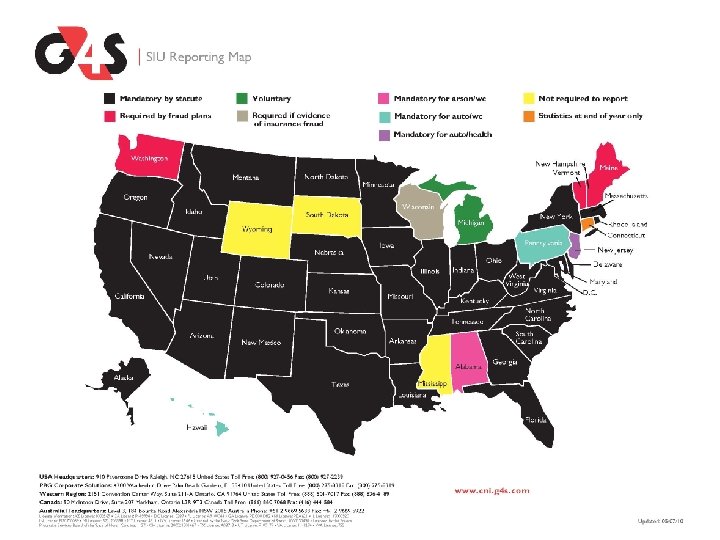
 Anti-Fraud Compliance Components of Regulatory Compliance • • • 21 states have anti-fraud plan requirements 46 states have mandatory reporting of suspicious claims 16 states require annual reports 12 states require an SIU 27 jurisdictions have a state statute or regulation concerning “Fraud Warnings” which are required on documents used with consumers (i. e. claim forms, proofs of loss, applications for insurance and in some instances - benefit checks). A Global Leader in Compliance and Investigation Solutions
Anti-Fraud Compliance Components of Regulatory Compliance • • • 21 states have anti-fraud plan requirements 46 states have mandatory reporting of suspicious claims 16 states require annual reports 12 states require an SIU 27 jurisdictions have a state statute or regulation concerning “Fraud Warnings” which are required on documents used with consumers (i. e. claim forms, proofs of loss, applications for insurance and in some instances - benefit checks). A Global Leader in Compliance and Investigation Solutions
 Function/Purpose of Your SIU Surveillance International Investigations Fraud Reviews Clinic Inspections Examinations Under Oath Scene Diagrams Alive & Wellness Checks Fraud Awareness Training Auditing & Consulting Neighborhood Canvass Hospital Searches Driver’s License Searches Criminal Records Check And many more…. A Global Leader in Compliance and Investigation Solutions Claims / Fraud Investigations State Fraud Referrals Documented Fraud Packages Statements/Recorded Interviews Video Re-enactments of the loss Scene Photographs Continuance of Disability Checks SIU Compliance & Reporting Activity Checks Nationwide Background Investigation Pharmacy Searches Skip Tracing (locates) Civil Records Searches
Function/Purpose of Your SIU Surveillance International Investigations Fraud Reviews Clinic Inspections Examinations Under Oath Scene Diagrams Alive & Wellness Checks Fraud Awareness Training Auditing & Consulting Neighborhood Canvass Hospital Searches Driver’s License Searches Criminal Records Check And many more…. A Global Leader in Compliance and Investigation Solutions Claims / Fraud Investigations State Fraud Referrals Documented Fraud Packages Statements/Recorded Interviews Video Re-enactments of the loss Scene Photographs Continuance of Disability Checks SIU Compliance & Reporting Activity Checks Nationwide Background Investigation Pharmacy Searches Skip Tracing (locates) Civil Records Searches
 Anti-Fraud Compliance CA Department of Insurance Fraud Division Regulatory Compliance A Global Leader in Compliance and Investigation Solutions
Anti-Fraud Compliance CA Department of Insurance Fraud Division Regulatory Compliance A Global Leader in Compliance and Investigation Solutions
 CA Code of Regulations: Section 2698. 35 Detecting Suspected Insurance Fraud (a) An insurer’s integral anti-fraud personnel are responsible for identifying suspected insurance fraud during the handling of insurance transactions and referring it to the SIU as part of their regular duties. A Global Leader in Compliance and Investigation Solutions
CA Code of Regulations: Section 2698. 35 Detecting Suspected Insurance Fraud (a) An insurer’s integral anti-fraud personnel are responsible for identifying suspected insurance fraud during the handling of insurance transactions and referring it to the SIU as part of their regular duties. A Global Leader in Compliance and Investigation Solutions
 Function/Purpose of Your SIU Investigating Suspected Insurance Fraud in Accordance with the California Regulations Section 2698. 36 As your SIU, we shall establish, maintain, distribute and adhere to written procedures for the investigation of possible suspected insurance fraud. An investigation of possible suspected insurance fraud shall include: (1) A thorough analysis of your claim file, application, or insurance transaction. (2) Identification and interviews of potential witnesses who may provide information on the accuracy of the claim or application. (3) Utilization of industry-recognized databases. (4) Preservation of documents and other evidence. (5) Writing a concise and complete summary of the investigation, including the investigator’s findings regarding the suspected insurance fraud and the basis for their findings. A Global Leader in Compliance and Investigation Solutions
Function/Purpose of Your SIU Investigating Suspected Insurance Fraud in Accordance with the California Regulations Section 2698. 36 As your SIU, we shall establish, maintain, distribute and adhere to written procedures for the investigation of possible suspected insurance fraud. An investigation of possible suspected insurance fraud shall include: (1) A thorough analysis of your claim file, application, or insurance transaction. (2) Identification and interviews of potential witnesses who may provide information on the accuracy of the claim or application. (3) Utilization of industry-recognized databases. (4) Preservation of documents and other evidence. (5) Writing a concise and complete summary of the investigation, including the investigator’s findings regarding the suspected insurance fraud and the basis for their findings. A Global Leader in Compliance and Investigation Solutions
 Function/Purpose of Your SIU Referral of Suspected Insurance Fraud in Accordance with California Regulations Section 2698. 37 G 4 S Compliance & Investigations shall provide for the referral of acts of suspected insurance fraud to the Fraud Division and, as required, district attorneys. Referrals shall be submitted in any insurance transaction where the facts and circumstances create a reasonable belief that a person or entity may have committed or is committing insurance fraud. All incidents of suspected insurance fraud will be submitted to the Fraud Division within 60 days of reasonable belief. A Global Leader in Compliance and Investigation Solutions
Function/Purpose of Your SIU Referral of Suspected Insurance Fraud in Accordance with California Regulations Section 2698. 37 G 4 S Compliance & Investigations shall provide for the referral of acts of suspected insurance fraud to the Fraud Division and, as required, district attorneys. Referrals shall be submitted in any insurance transaction where the facts and circumstances create a reasonable belief that a person or entity may have committed or is committing insurance fraud. All incidents of suspected insurance fraud will be submitted to the Fraud Division within 60 days of reasonable belief. A Global Leader in Compliance and Investigation Solutions
 What is Reasonable Suspicion? “Reasonable belief” is a level of belief that an act of insurance fraud may have or might be occurring for which there is an objective justification based on articulable fact(s) and rational inferences there from. California Statutes 2698. 30 A Global Leader in Compliance and Investigation Solutions
What is Reasonable Suspicion? “Reasonable belief” is a level of belief that an act of insurance fraud may have or might be occurring for which there is an objective justification based on articulable fact(s) and rational inferences there from. California Statutes 2698. 30 A Global Leader in Compliance and Investigation Solutions
 Reasonable Suspicion To Report Fraud • In Mandatory State Fraud reporting, the claims professional or SIU member should be able to state objective justification based on articulable fact(s) and rational inferences to justify the report to the state or appropriate agency. • A claim meets this requirement if you can answer this question; • I believe this case is fraudulent because…… • If that question can be answered, then the claim meets the mandatory state fraud referral statutes. • Keep in mind that you do not need evidence of insurance fraud to trigger these regulations except in the State of Wisconsin. A Global Leader in Compliance and Investigation Solutions
Reasonable Suspicion To Report Fraud • In Mandatory State Fraud reporting, the claims professional or SIU member should be able to state objective justification based on articulable fact(s) and rational inferences to justify the report to the state or appropriate agency. • A claim meets this requirement if you can answer this question; • I believe this case is fraudulent because…… • If that question can be answered, then the claim meets the mandatory state fraud referral statutes. • Keep in mind that you do not need evidence of insurance fraud to trigger these regulations except in the State of Wisconsin. A Global Leader in Compliance and Investigation Solutions
 What is Reasonable Suspicion? • Now that we have agreed on what % of your claims are fraudulent, and gone through what reasonable suspicion is, what % of your claims do you suspect to be fraudulent? • Obviously this number is going to be larger than the 15% we have already agreed were fraudulent or inflated. • Keep in mind the states that have Mandatory Reporting Requirements have set the threshold of “SUSPECTED TO BE FRAUDULENT”. • If you suspect a claim to be fraudulent, you must notify SIU so a State Fraud Referral can be filed and recorded on the Fraud Log. A Global Leader in Compliance and Investigation Solutions
What is Reasonable Suspicion? • Now that we have agreed on what % of your claims are fraudulent, and gone through what reasonable suspicion is, what % of your claims do you suspect to be fraudulent? • Obviously this number is going to be larger than the 15% we have already agreed were fraudulent or inflated. • Keep in mind the states that have Mandatory Reporting Requirements have set the threshold of “SUSPECTED TO BE FRAUDULENT”. • If you suspect a claim to be fraudulent, you must notify SIU so a State Fraud Referral can be filed and recorded on the Fraud Log. A Global Leader in Compliance and Investigation Solutions
 Mandatory Fraud Reporting California Insurance Code 1874 “Any company licensed to write insurance in this state that believes that a fraudulent claim is being made shall, within 60 days after determination by the insurer that the claim appears to be a fraudulent claim, send to the Bureau of Fraudulent Claims, on a form prescribed by the Department, the information requested by the form and any additional information relative to the factual circumstances of the claims and parties claiming loss or damages that the commissioner may require. ” A Global Leader in Compliance and Investigation Solutions
Mandatory Fraud Reporting California Insurance Code 1874 “Any company licensed to write insurance in this state that believes that a fraudulent claim is being made shall, within 60 days after determination by the insurer that the claim appears to be a fraudulent claim, send to the Bureau of Fraudulent Claims, on a form prescribed by the Department, the information requested by the form and any additional information relative to the factual circumstances of the claims and parties claiming loss or damages that the commissioner may require. ” A Global Leader in Compliance and Investigation Solutions
 Why Should We Comply with Mandatory Reporting? • Several States have sanctions in their statutes that can be used to compel a carrier to comply with the Mandatory Reporting Statute. • The following states can sanction a carrier for not complying with this mandatory reporting statute; – California - $5, 000 per claim. – Pennsylvania - $10, 000 for not complying with the Anti-Fraud Plan on file with the state. – Florida - $2, 000 a day back to the first date the states decides the carrier should have been complying with the fraud regulations and an additional $100, 000 at the discretion of the commissioner. – New Jersey - $12, 500 per claim. – New York - left to the discretion of the commissioner. – Other states also have sanctions in their arsenal that can be used. A Global Leader in Compliance and Investigation Solutions
Why Should We Comply with Mandatory Reporting? • Several States have sanctions in their statutes that can be used to compel a carrier to comply with the Mandatory Reporting Statute. • The following states can sanction a carrier for not complying with this mandatory reporting statute; – California - $5, 000 per claim. – Pennsylvania - $10, 000 for not complying with the Anti-Fraud Plan on file with the state. – Florida - $2, 000 a day back to the first date the states decides the carrier should have been complying with the fraud regulations and an additional $100, 000 at the discretion of the commissioner. – New Jersey - $12, 500 per claim. – New York - left to the discretion of the commissioner. – Other states also have sanctions in their arsenal that can be used. A Global Leader in Compliance and Investigation Solutions
 Example of Immunity For Reporting California Insurance Code 1872. 5 - “No insurer, or the employees or agents of any insurer, shall be subject to civil liability for libel, slander, or an other relevant tort cause of action. . . ” PROVIDED: • The investigation was conducted in good-faith • There was no malice of forethought • No willful misrepresentation was made • No intentional exclusions of relevant information • No violation of local, state or federal Privacy laws A Global Leader in Compliance and Investigation Solutions
Example of Immunity For Reporting California Insurance Code 1872. 5 - “No insurer, or the employees or agents of any insurer, shall be subject to civil liability for libel, slander, or an other relevant tort cause of action. . . ” PROVIDED: • The investigation was conducted in good-faith • There was no malice of forethought • No willful misrepresentation was made • No intentional exclusions of relevant information • No violation of local, state or federal Privacy laws A Global Leader in Compliance and Investigation Solutions
 Example of Immunity For Reporting FLORIDA Insurance Code, Title XXXVII. Insurance, Chapter 626. 989 Insurance Field Representatives (d) In addition to the immunity granted in paragraph (c), persons identified as designated employees whose responsibilities include the investigation and disposition of claims relating to suspected fraudulent insurance acts may share information relating to persons suspected of committing fraudulent insurance acts with other designated employees employed by the same or other insurers whose responsibilities include the investigation and disposition of claims relating to fraudulent insurance acts, provided the department has been given written notice of the names and job titles of such designated employees prior to such designated employees sharing information… A Global Leader in Compliance and Investigation Solutions
Example of Immunity For Reporting FLORIDA Insurance Code, Title XXXVII. Insurance, Chapter 626. 989 Insurance Field Representatives (d) In addition to the immunity granted in paragraph (c), persons identified as designated employees whose responsibilities include the investigation and disposition of claims relating to suspected fraudulent insurance acts may share information relating to persons suspected of committing fraudulent insurance acts with other designated employees employed by the same or other insurers whose responsibilities include the investigation and disposition of claims relating to fraudulent insurance acts, provided the department has been given written notice of the names and job titles of such designated employees prior to such designated employees sharing information… A Global Leader in Compliance and Investigation Solutions
 How Do I Report a Suspicious Claim? • Contact G 4 S Compliance & Investigations as your Special Investigations Unit (SIU) per your company’s written Anti-Fraud Procedures Manual. • G 4 S Case. Trak has a tab for submitting “State Fraud Referral Assignments”. • Select this tab and submit your assignment. G 4 S Compliance & Investigations will place your referral report on the proper state form and file with the appropriate State Fraud Bureau as required by regulation or statute. • Upon review, the SIU may contact you for determination of further investigation requirements. • G 4 S Compliance & Investigations SIU can also be reached at 1 -800 -927 -0456. A Global Leader in Compliance and Investigation Solutions
How Do I Report a Suspicious Claim? • Contact G 4 S Compliance & Investigations as your Special Investigations Unit (SIU) per your company’s written Anti-Fraud Procedures Manual. • G 4 S Case. Trak has a tab for submitting “State Fraud Referral Assignments”. • Select this tab and submit your assignment. G 4 S Compliance & Investigations will place your referral report on the proper state form and file with the appropriate State Fraud Bureau as required by regulation or statute. • Upon review, the SIU may contact you for determination of further investigation requirements. • G 4 S Compliance & Investigations SIU can also be reached at 1 -800 -927 -0456. A Global Leader in Compliance and Investigation Solutions
 Insurer – SIU Training Responsibilities Anti-Fraud Training in Accordance with California Regulation Section 2698. 39 Requirements for training provided by and for the SIU shall include: (a) The insurer has established and maintained an ongoing anti-fraud training program, planned and conducted to develop and improve the anti-fraud awareness skills of the integral anti-fraud personnel. (b) The insurer has designated the SIU Compliance Manager to be responsible for coordinating the ongoing anti-fraud training program. (c) The anti-fraud training program shall consist of three (3) levels: (1) All newly- hired employees shall receive an anti-fraud orientation within ninety (90) days of commencing assigned duties. (2) Integral anti-fraud personnel shall receive annual anti-fraud in-service training. (3) The SIU personnel shall receive continuing anti-fraud training. A Global Leader in Compliance and Investigation Solutions
Insurer – SIU Training Responsibilities Anti-Fraud Training in Accordance with California Regulation Section 2698. 39 Requirements for training provided by and for the SIU shall include: (a) The insurer has established and maintained an ongoing anti-fraud training program, planned and conducted to develop and improve the anti-fraud awareness skills of the integral anti-fraud personnel. (b) The insurer has designated the SIU Compliance Manager to be responsible for coordinating the ongoing anti-fraud training program. (c) The anti-fraud training program shall consist of three (3) levels: (1) All newly- hired employees shall receive an anti-fraud orientation within ninety (90) days of commencing assigned duties. (2) Integral anti-fraud personnel shall receive annual anti-fraud in-service training. (3) The SIU personnel shall receive continuing anti-fraud training. A Global Leader in Compliance and Investigation Solutions
 Fraud Warning Language Current research of the anti-fraud compliance laws of the fifty states and the District of Columbia reveals there are twentyseven [27] jurisdictions that have a state statute or regulations concerning “Fraud Warnings”. The fraud warning language in the statute MUST be used on all applicable documents in the states of Alaska, California [English & Spanish], Pennsylvania, and Rhode Island. The fraud warning language in the statute MUST be used on all applicable workers compensation documents in the states of Tennessee and Utah. A Global Leader in Compliance and Investigation Solutions
Fraud Warning Language Current research of the anti-fraud compliance laws of the fifty states and the District of Columbia reveals there are twentyseven [27] jurisdictions that have a state statute or regulations concerning “Fraud Warnings”. The fraud warning language in the statute MUST be used on all applicable documents in the states of Alaska, California [English & Spanish], Pennsylvania, and Rhode Island. The fraud warning language in the statute MUST be used on all applicable workers compensation documents in the states of Tennessee and Utah. A Global Leader in Compliance and Investigation Solutions
 Fraud Warning Language The fraud warning language to be used in applicable documents can be substantially similar to the language in the statute, and does not have to be exact in the states of Arizona, Arkansas, Colorado, District of Columbia, Florida, Hawaii, Idaho, Indiana, Kentucky, Louisiana, Maine, Minnesota, New Hampshire, New Jersey, New Mexico, Ohio, Oklahoma, Tennessee [for non-work comp claims], and Virginia. Fraud warning must appear on the back of benefit checks in the states of Delaware, New York, Rhode Island, Utah, and in CA on TTD checks in both English and Spanish [or enclosed with ck]. Please make sure that you are using the appropriate fraud warning language in each state. If you wish to receive a complete breakdown by state, please contact the SIU Compliance Manager. A Global Leader in Compliance and Investigation Solutions
Fraud Warning Language The fraud warning language to be used in applicable documents can be substantially similar to the language in the statute, and does not have to be exact in the states of Arizona, Arkansas, Colorado, District of Columbia, Florida, Hawaii, Idaho, Indiana, Kentucky, Louisiana, Maine, Minnesota, New Hampshire, New Jersey, New Mexico, Ohio, Oklahoma, Tennessee [for non-work comp claims], and Virginia. Fraud warning must appear on the back of benefit checks in the states of Delaware, New York, Rhode Island, Utah, and in CA on TTD checks in both English and Spanish [or enclosed with ck]. Please make sure that you are using the appropriate fraud warning language in each state. If you wish to receive a complete breakdown by state, please contact the SIU Compliance Manager. A Global Leader in Compliance and Investigation Solutions
 CA Code of Regulations: Section 2698. 42 - Penalties (a) If the Commissioner acts pursuant to the provisions of California Insurance Code Section 1875. 24( c) or (d) and finds that the insurer has failed to comply with the provisions of this article, the Commissioner shall impose a monetary penalty in an amount not to exceed $5, 000 for each act of non-compliance. Where the Commissioner determines that an insurer has willfully failed to comply with this article, the Commissioner may impose a monetary penalty in an amount not to exceed $ 10, 000 for each willful act of non -compliance. The Commissioner shall consider the factors enumerated at California Code of Regulations Title 10 Chapter 5, Subchapter 3, Section 2591. 3 (a)-(f) and determine if any of the enumerated factors are applicable to the insurer's conduct in the establishment and operation of its special investigative unit. If the Commissioner finds such factors are applicable to the insurer's conduct, the Commissioner may reduce the amount of the monetary penalty prescribed in subsection 2698. 42(a). A Global Leader in Compliance and Investigation Solutions
CA Code of Regulations: Section 2698. 42 - Penalties (a) If the Commissioner acts pursuant to the provisions of California Insurance Code Section 1875. 24( c) or (d) and finds that the insurer has failed to comply with the provisions of this article, the Commissioner shall impose a monetary penalty in an amount not to exceed $5, 000 for each act of non-compliance. Where the Commissioner determines that an insurer has willfully failed to comply with this article, the Commissioner may impose a monetary penalty in an amount not to exceed $ 10, 000 for each willful act of non -compliance. The Commissioner shall consider the factors enumerated at California Code of Regulations Title 10 Chapter 5, Subchapter 3, Section 2591. 3 (a)-(f) and determine if any of the enumerated factors are applicable to the insurer's conduct in the establishment and operation of its special investigative unit. If the Commissioner finds such factors are applicable to the insurer's conduct, the Commissioner may reduce the amount of the monetary penalty prescribed in subsection 2698. 42(a). A Global Leader in Compliance and Investigation Solutions
 CA Code of Regulations: Section 2698. 42 - Penalties (b) If the Commissioner acts pursuant to the provisions of California Insurance Code Section 1875. 24(c) or (d) and determines that the acts of non-compliance are inadvertent and are solely relative to the maintenance and operation of the special investigative unit of the insurer, then the Commissioner shall consider such violations to be a single act for the purposes of imposition of a monetary penalty that is no greater than $5, 000 for that single act. For all other inadvertent acts, the Commissioner shall impose a penalty in the amount of up to $5, 000 per inadvertent act that is not in compliance with this article. A Global Leader in Compliance and Investigation Solutions
CA Code of Regulations: Section 2698. 42 - Penalties (b) If the Commissioner acts pursuant to the provisions of California Insurance Code Section 1875. 24(c) or (d) and determines that the acts of non-compliance are inadvertent and are solely relative to the maintenance and operation of the special investigative unit of the insurer, then the Commissioner shall consider such violations to be a single act for the purposes of imposition of a monetary penalty that is no greater than $5, 000 for that single act. For all other inadvertent acts, the Commissioner shall impose a penalty in the amount of up to $5, 000 per inadvertent act that is not in compliance with this article. A Global Leader in Compliance and Investigation Solutions

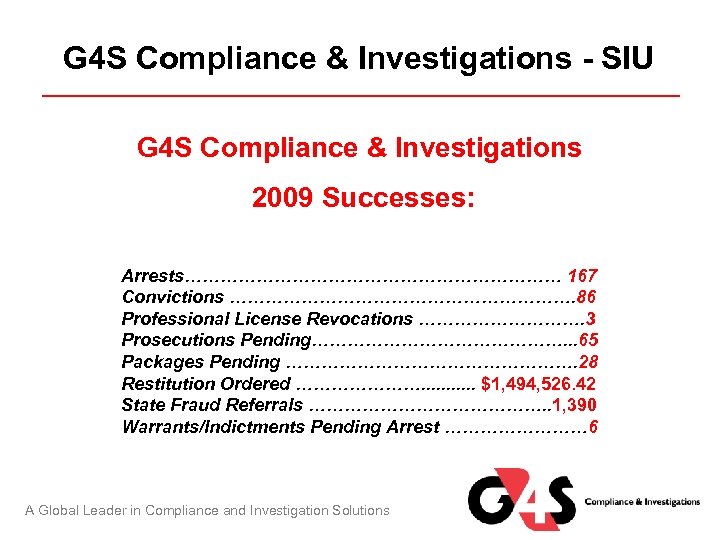 G 4 S Compliance & Investigations - SIU G 4 S Compliance & Investigations 2009 Successes: Arrests…………………………… 167 Convictions …………………………. 86 Professional License Revocations ……………. 3 Prosecutions Pending…………………. . . 65 Packages Pending ……………………. 28 Restitution Ordered …………………. . . $1, 494, 526. 42 State Fraud Referrals …………………. . 1, 390 Warrants/Indictments Pending Arrest ………… 6 A Global Leader in Compliance and Investigation Solutions
G 4 S Compliance & Investigations - SIU G 4 S Compliance & Investigations 2009 Successes: Arrests…………………………… 167 Convictions …………………………. 86 Professional License Revocations ……………. 3 Prosecutions Pending…………………. . . 65 Packages Pending ……………………. 28 Restitution Ordered …………………. . . $1, 494, 526. 42 State Fraud Referrals …………………. . 1, 390 Warrants/Indictments Pending Arrest ………… 6 A Global Leader in Compliance and Investigation Solutions
 G 4 S Compliance & Investigations - SIU G 4 S Compliance & Investigations (SIU) conducted interviews with the contractors who provided estimates for the damages to the property to Pleasure Island Shrimp House. These interviews determined that the estimates provided by the insured, Mr. Tran, were fabricated by him. Tran presented a repair estimate in the amount of $119, 900. The SIU investigation revealed that there is no such company. This estimate was fabricated by Mr. Tran also presented an estimate for the repair of refrigeration equipment in the amount of $347, 600. SIU interviewed the owner of the company that supposedly wrote the estimate and learned they have not made any repairs to Mr. Tran since 2003. In addition, they do not install any refrigeration equipment. There would never be any labor costs on any of his estimates. His highest billing ever for equipment sold to Tran was under $3000. This estimate in the amount of $347, 600 was also fabricated by Mr. Tran. Continue on next slide A Global Leader in Compliance and Investigation Solutions
G 4 S Compliance & Investigations - SIU G 4 S Compliance & Investigations (SIU) conducted interviews with the contractors who provided estimates for the damages to the property to Pleasure Island Shrimp House. These interviews determined that the estimates provided by the insured, Mr. Tran, were fabricated by him. Tran presented a repair estimate in the amount of $119, 900. The SIU investigation revealed that there is no such company. This estimate was fabricated by Mr. Tran also presented an estimate for the repair of refrigeration equipment in the amount of $347, 600. SIU interviewed the owner of the company that supposedly wrote the estimate and learned they have not made any repairs to Mr. Tran since 2003. In addition, they do not install any refrigeration equipment. There would never be any labor costs on any of his estimates. His highest billing ever for equipment sold to Tran was under $3000. This estimate in the amount of $347, 600 was also fabricated by Mr. Tran. Continue on next slide A Global Leader in Compliance and Investigation Solutions
 G 4 S Compliance & Investigations - SIU Victor Tran pled guilty to 1 count of making a false statement and was ordered to pay XL Specialty Insurance Company $500, 000. 00 in restitution. Victor Tran reimbursed XL a total of $500, 000. 00 in restitution. A Global Leader in Compliance and Investigation Solutions
G 4 S Compliance & Investigations - SIU Victor Tran pled guilty to 1 count of making a false statement and was ordered to pay XL Specialty Insurance Company $500, 000. 00 in restitution. Victor Tran reimbursed XL a total of $500, 000. 00 in restitution. A Global Leader in Compliance and Investigation Solutions
 G 4 S Compliance & Investigations - SIU Jose Diaz was hired in February 2006 as a laborer and filed a DWC-1 and an Application for Adjudication of Claim, alleging that sometime in May 2006, while working for the insured, he slipped on water and became injured when he fell landing on his left side. In addition, in June 2006, he filed a DWC-1 and an Application for Adjudication of Claim, alleging a cumulative trauma injury from February 2006 to June 2006. The Employer was not aware of any injury and the claim was delayed pending investigation. It was discovered that Jose Diaz’s attorney and physician were the same for a previous workers’ compensation claim with the State Compensation Insurance Fund. In that case this 1993 claim, Mr. Diaz reports to have been injured while lifting a 60 pound box. Jose Diaz, through his attorney, filed an Application for Adjudication of Claim in June 2003, and the claimant filed a DWC-1 in June 2003, for a cumulative trauma claim for injuries Jose Diaz and his attorney settled that claim on a Compromise and Release in September 2005. Jose Diaz was being treated for alleged injuries from a motor vehicle accident on March 26, 2006. Continue on next slide A Global Leader in Compliance and Investigation Solutions
G 4 S Compliance & Investigations - SIU Jose Diaz was hired in February 2006 as a laborer and filed a DWC-1 and an Application for Adjudication of Claim, alleging that sometime in May 2006, while working for the insured, he slipped on water and became injured when he fell landing on his left side. In addition, in June 2006, he filed a DWC-1 and an Application for Adjudication of Claim, alleging a cumulative trauma injury from February 2006 to June 2006. The Employer was not aware of any injury and the claim was delayed pending investigation. It was discovered that Jose Diaz’s attorney and physician were the same for a previous workers’ compensation claim with the State Compensation Insurance Fund. In that case this 1993 claim, Mr. Diaz reports to have been injured while lifting a 60 pound box. Jose Diaz, through his attorney, filed an Application for Adjudication of Claim in June 2003, and the claimant filed a DWC-1 in June 2003, for a cumulative trauma claim for injuries Jose Diaz and his attorney settled that claim on a Compromise and Release in September 2005. Jose Diaz was being treated for alleged injuries from a motor vehicle accident on March 26, 2006. Continue on next slide A Global Leader in Compliance and Investigation Solutions
 G 4 S Compliance & Investigations - SIU Los Angeles CA - Jose Diaz pled guilty to one count of Insurance Fraud. At sentencing, per the plea agreement, Mr. Diaz paid restitution in the amount of $5, 000. This allowed him to have no prison time, but he will have 5 years formal probation and 300 hours of Community Service. It is during this 5 year period that Mr. Diaz is ordered to make full restitution of $20, 000. Mr. Diaz also agreed to withdraw and cancel his workers' compensation claim. A Global Leader in Compliance and Investigation Solutions
G 4 S Compliance & Investigations - SIU Los Angeles CA - Jose Diaz pled guilty to one count of Insurance Fraud. At sentencing, per the plea agreement, Mr. Diaz paid restitution in the amount of $5, 000. This allowed him to have no prison time, but he will have 5 years formal probation and 300 hours of Community Service. It is during this 5 year period that Mr. Diaz is ordered to make full restitution of $20, 000. Mr. Diaz also agreed to withdraw and cancel his workers' compensation claim. A Global Leader in Compliance and Investigation Solutions
 G 4 S Compliance & Investigations - SIU Alfredo Wong Pizarro was employed by Costco Wholesale in Orlando, Florida as a seasonal temporary stocker from November 7, 2000. On December 9, 2000 at approximately 5: 00 pm, Mr. Pizarro tripped on a rope utilized to keep people out of a particular isle, and fell injuring his right foot and lower back. Mr. Pizarro received medical attention on December 9, 2000. He was released to return to work on light duty that day. Per the employer, they received first notice of injury on December 9, 2007 from Mr. Pizarro was later referred to a Wellness Center where he was treated for his right ankle, lower back and thoracic area. Over time, Mr. Pizarro’s complaints escalated to include his cervical spine, liver problems and pain in the right shoulder and lower extremities. Mr. Pizarro was placed under surveillance and was documented conducting activities he had been claiming to his physicians and in deposition that he specifically could not do. Continue on next slide A Global Leader in Compliance and Investigation Solutions
G 4 S Compliance & Investigations - SIU Alfredo Wong Pizarro was employed by Costco Wholesale in Orlando, Florida as a seasonal temporary stocker from November 7, 2000. On December 9, 2000 at approximately 5: 00 pm, Mr. Pizarro tripped on a rope utilized to keep people out of a particular isle, and fell injuring his right foot and lower back. Mr. Pizarro received medical attention on December 9, 2000. He was released to return to work on light duty that day. Per the employer, they received first notice of injury on December 9, 2007 from Mr. Pizarro was later referred to a Wellness Center where he was treated for his right ankle, lower back and thoracic area. Over time, Mr. Pizarro’s complaints escalated to include his cervical spine, liver problems and pain in the right shoulder and lower extremities. Mr. Pizarro was placed under surveillance and was documented conducting activities he had been claiming to his physicians and in deposition that he specifically could not do. Continue on next slide A Global Leader in Compliance and Investigation Solutions
 G 4 S Compliance & Investigations - SIU Alfredo Pizarro pled guilty to 1 Count of Workers' Compensation Insurance Fraud and was sentenced to a withhold of adjudication with one year of reporting probation, with the special condition of 15 days in the Dade County Jail, 50 hours of community service to be completed at a minimum of 5 hours per month, restitution in the amount of $122, 644. 88 and investigative cost to the DOIF in the amount of $1, 135. 94. A Global Leader in Compliance and Investigation Solutions
G 4 S Compliance & Investigations - SIU Alfredo Pizarro pled guilty to 1 Count of Workers' Compensation Insurance Fraud and was sentenced to a withhold of adjudication with one year of reporting probation, with the special condition of 15 days in the Dade County Jail, 50 hours of community service to be completed at a minimum of 5 hours per month, restitution in the amount of $122, 644. 88 and investigative cost to the DOIF in the amount of $1, 135. 94. A Global Leader in Compliance and Investigation Solutions
 What is Insurance Fraud? A Global Leader in Compliance and Investigation Solutions
What is Insurance Fraud? A Global Leader in Compliance and Investigation Solutions
 What is Insurance Fraud? Elements of the crime of insurance fraud are consistent: – Someone deliberately lies – (intent) – The intent of the lie is for someone else to rely on that lie, so that they may receive a benefit otherwise not entitled – The other person relies on that lie – As a result, the person who relied on that lie is harmed Each state has different thresholds an insurer must meet before the state will accept a case. – Texas requires that an insurer or self insurer pay at least $1, 500 on the claim before the DOI will accept a fraudulent claim for investigations. – Before the Federal authorities will accept a case, the loss must exceed $250, 000. A Global Leader in Compliance and Investigation Solutions
What is Insurance Fraud? Elements of the crime of insurance fraud are consistent: – Someone deliberately lies – (intent) – The intent of the lie is for someone else to rely on that lie, so that they may receive a benefit otherwise not entitled – The other person relies on that lie – As a result, the person who relied on that lie is harmed Each state has different thresholds an insurer must meet before the state will accept a case. – Texas requires that an insurer or self insurer pay at least $1, 500 on the claim before the DOI will accept a fraudulent claim for investigations. – Before the Federal authorities will accept a case, the loss must exceed $250, 000. A Global Leader in Compliance and Investigation Solutions
 What Constitutes Insurance Fraud? Looking for the Lie In order to have Insurance Fraud, you must have a Lie. The lie does not have to be something that was told to the adjustor, doctor, investigator, attorney or other. It can be something that the individual should have said. GOT M. I. L. K. ? A Global Leader in Compliance and Investigation Solutions
What Constitutes Insurance Fraud? Looking for the Lie In order to have Insurance Fraud, you must have a Lie. The lie does not have to be something that was told to the adjustor, doctor, investigator, attorney or other. It can be something that the individual should have said. GOT M. I. L. K. ? A Global Leader in Compliance and Investigation Solutions
 Fraud Defined – Got M. I. L. K. ? • Misrepresentations made must be Material to the case • The false information must have been presented Intentionally • A Lie must have been presented to prove, validate, affirm or deny a claim for injury or loss payment or to obtain insurance coverage • The information must have been presented Knowingly • The false information presented would have altered, changed or modified the manner the claim was handled, investigated, evaluated or settled A Global Leader in Compliance and Investigation Solutions
Fraud Defined – Got M. I. L. K. ? • Misrepresentations made must be Material to the case • The false information must have been presented Intentionally • A Lie must have been presented to prove, validate, affirm or deny a claim for injury or loss payment or to obtain insurance coverage • The information must have been presented Knowingly • The false information presented would have altered, changed or modified the manner the claim was handled, investigated, evaluated or settled A Global Leader in Compliance and Investigation Solutions
 Emerging Fraud Trends Key Fraud Indicators A Global Leader in Compliance and Investigation Solutions
Emerging Fraud Trends Key Fraud Indicators A Global Leader in Compliance and Investigation Solutions
 Three Main Types of External “Bad Guys” • Professional Fraud Perpetrators • Semi-Professional Fraud Perpetrators • Opportunistic Fraud Perpetrators A Global Leader in Compliance and Investigation Solutions
Three Main Types of External “Bad Guys” • Professional Fraud Perpetrators • Semi-Professional Fraud Perpetrators • Opportunistic Fraud Perpetrators A Global Leader in Compliance and Investigation Solutions
 Professional Fraud Perpetrators • These are professional criminals who have made their livelihoods from insurance fraud schemes. In some cases, they have been doctors, lawyers, business owners and other professionals. The type of fraud that professional fraud perpetrators commit is sometimes referred to as “hard-core fraud” because it has involved fake theft claims, false bodily injury claims and staged accidents that have been repeated time and again and have had the potential to cost insurance companies many thousands of dollars. • General Liability – “Slip and fall” – Product Liability • Staged Accidents • Property Losses – Homeowner and Commercial A Global Leader in Compliance and Investigation Solutions
Professional Fraud Perpetrators • These are professional criminals who have made their livelihoods from insurance fraud schemes. In some cases, they have been doctors, lawyers, business owners and other professionals. The type of fraud that professional fraud perpetrators commit is sometimes referred to as “hard-core fraud” because it has involved fake theft claims, false bodily injury claims and staged accidents that have been repeated time and again and have had the potential to cost insurance companies many thousands of dollars. • General Liability – “Slip and fall” – Product Liability • Staged Accidents • Property Losses – Homeowner and Commercial A Global Leader in Compliance and Investigation Solutions
 Professional Fraud Perpetrators • Auto Salvage Fraud – exchange VIN’s, rigged bidding, flood cars • Crime Rings – chop shops, trucking thefts, etc. • Arson-For-Profit Rings - Some rings were hired by policy owners for a fee, and some rings profited directly from the schemes • Staged Auto Accident rings A Global Leader in Compliance and Investigation Solutions
Professional Fraud Perpetrators • Auto Salvage Fraud – exchange VIN’s, rigged bidding, flood cars • Crime Rings – chop shops, trucking thefts, etc. • Arson-For-Profit Rings - Some rings were hired by policy owners for a fee, and some rings profited directly from the schemes • Staged Auto Accident rings A Global Leader in Compliance and Investigation Solutions
 Semi-Professional Fraud Perpetrators • Medical Build up Schemes • Rolling Labs • Medical Mills • Ambulance Chasing Rings • Police and EMS selling accident lists A Global Leader in Compliance and Investigation Solutions
Semi-Professional Fraud Perpetrators • Medical Build up Schemes • Rolling Labs • Medical Mills • Ambulance Chasing Rings • Police and EMS selling accident lists A Global Leader in Compliance and Investigation Solutions
 Medical Build-up Schemes Some professionals have committed opportunistic insurance fraud. Others have gone even further and have faked medical documents and committed “medical build-up. ” Examples of medical build-up cases are doctors who have taken advantage of the system by billing other employees’ group health insurance companies and employers’ workers compensation insurers by inflating both types of bills for what were actually minor injuries. In a recent case, employees of a Miami home health care agency were charged by federal authorities with cheating Medicare out of $15 million by billing for fictitious patient visits. Sometimes, insureds have been involved in these fraud schemes. Often, however, innocent insureds were unaware insurance fraud was taking place. The bill for their treatment were sent by the medical professionals directly to the insurance companies. The insureds usually never received treatment and never knew the bills existed. A Global Leader in Compliance and Investigation Solutions
Medical Build-up Schemes Some professionals have committed opportunistic insurance fraud. Others have gone even further and have faked medical documents and committed “medical build-up. ” Examples of medical build-up cases are doctors who have taken advantage of the system by billing other employees’ group health insurance companies and employers’ workers compensation insurers by inflating both types of bills for what were actually minor injuries. In a recent case, employees of a Miami home health care agency were charged by federal authorities with cheating Medicare out of $15 million by billing for fictitious patient visits. Sometimes, insureds have been involved in these fraud schemes. Often, however, innocent insureds were unaware insurance fraud was taking place. The bill for their treatment were sent by the medical professionals directly to the insurance companies. The insureds usually never received treatment and never knew the bills existed. A Global Leader in Compliance and Investigation Solutions
 Rolling Labs Another type of scam has involved rolling labs, vans or motor homes equipped with medical laboratories where unnecessary and sometimes fake medical tests have been conducted on unsuspecting patients and paid for by their insurers. Because these labs were on wheels, they were easily moved from location to location. A Global Leader in Compliance and Investigation Solutions
Rolling Labs Another type of scam has involved rolling labs, vans or motor homes equipped with medical laboratories where unnecessary and sometimes fake medical tests have been conducted on unsuspecting patients and paid for by their insurers. Because these labs were on wheels, they were easily moved from location to location. A Global Leader in Compliance and Investigation Solutions
 Ambulance Chasing Rings Some corrupt lawyers use runners or cappers who are people hired by unscrupulous doctors or lawyers to recruit people for kickback or feesplitting schemes. The recruits have either been injured or agree to pretend to have been injured in an accident. Runners have also sometimes been hired to arrange “accidents” so they appear to be the fault of someone else. Runners often chase ambulances by using police-band radios to locate auto accidents. They would rush to the accident scenes and give one or both drivers the name of the ring’s doctor or lawyer. After the people were recruited and had contacted the ring’s doctor or lawyer, the runner received payment. The ring’s doctor performed needless medical treatments or simply billed the claimants for treatments that were never provided. The ring’s lawyer then built legal cases for the claimants in anticipation of taking those cases to court. A Global Leader in Compliance and Investigation Solutions
Ambulance Chasing Rings Some corrupt lawyers use runners or cappers who are people hired by unscrupulous doctors or lawyers to recruit people for kickback or feesplitting schemes. The recruits have either been injured or agree to pretend to have been injured in an accident. Runners have also sometimes been hired to arrange “accidents” so they appear to be the fault of someone else. Runners often chase ambulances by using police-band radios to locate auto accidents. They would rush to the accident scenes and give one or both drivers the name of the ring’s doctor or lawyer. After the people were recruited and had contacted the ring’s doctor or lawyer, the runner received payment. The ring’s doctor performed needless medical treatments or simply billed the claimants for treatments that were never provided. The ring’s lawyer then built legal cases for the claimants in anticipation of taking those cases to court. A Global Leader in Compliance and Investigation Solutions
 Semi-Professional Fraud Perpetrators • These are people who have committed insurance fraud more than once but have not relied on it as a major source of income. This category has also included certain unscrupulous doctors, lawyers and various types of business owners. • Most medical and legal professionals are honest and trustworthy. Some, however, are not. They have falsified and destroyed records and assisted others in fabricating injuries to collect large bodily injury insurance settlements or awards in lawsuits based on fraudulent claims. They have billed patients and clients excessively for medical and legal work, some of which they did not even do. • Unfortunately, the illegal activities of these relatively few corrupt medical and legal professionals can affect the reputation of integrity of the rest. A Global Leader in Compliance and Investigation Solutions
Semi-Professional Fraud Perpetrators • These are people who have committed insurance fraud more than once but have not relied on it as a major source of income. This category has also included certain unscrupulous doctors, lawyers and various types of business owners. • Most medical and legal professionals are honest and trustworthy. Some, however, are not. They have falsified and destroyed records and assisted others in fabricating injuries to collect large bodily injury insurance settlements or awards in lawsuits based on fraudulent claims. They have billed patients and clients excessively for medical and legal work, some of which they did not even do. • Unfortunately, the illegal activities of these relatively few corrupt medical and legal professionals can affect the reputation of integrity of the rest. A Global Leader in Compliance and Investigation Solutions
 Semi-Professional Fraud Perpetrators • In addition to those previously described, many others have participated in fraud schemes for money or for kickbacks. Following are some examples: – Insurance professionals who took bribes or kickbacks for filing and processing fake claims – Contractors who were hired to repair or replace damaged property, who inflated the costs for work performed or charged for work they did not perform and for materials they did not use – Dentists who wrote claimants’ dental reports so their insurance would cover the costs of non-covered treatments or false treatments – Radiologists who falsified X-rays that were then used to support fraudulent claims A Global Leader in Compliance and Investigation Solutions
Semi-Professional Fraud Perpetrators • In addition to those previously described, many others have participated in fraud schemes for money or for kickbacks. Following are some examples: – Insurance professionals who took bribes or kickbacks for filing and processing fake claims – Contractors who were hired to repair or replace damaged property, who inflated the costs for work performed or charged for work they did not perform and for materials they did not use – Dentists who wrote claimants’ dental reports so their insurance would cover the costs of non-covered treatments or false treatments – Radiologists who falsified X-rays that were then used to support fraudulent claims A Global Leader in Compliance and Investigation Solutions
 Semi-Professional Fraud Perpetrators – Employees of professionals and business owners whose employers were or were not also involved in the schemes and who falsified bills or claim forms – Real estate brokers who worked with arsonists in securing property and falsifying property values – Tow truck operators who notified corrupt professionals when accidents occurred and provided names of those who were injured A Global Leader in Compliance and Investigation Solutions
Semi-Professional Fraud Perpetrators – Employees of professionals and business owners whose employers were or were not also involved in the schemes and who falsified bills or claim forms – Real estate brokers who worked with arsonists in securing property and falsifying property values – Tow truck operators who notified corrupt professionals when accidents occurred and provided names of those who were injured A Global Leader in Compliance and Investigation Solutions
 Opportunistic Insurance Fraud Perpetrators These are people who have taken the opportunity to squeeze extra money from the insurance companies. They usually do this only one or twice which is consider so called “soft fraud”. As an example, they have padded the amounts of their otherwise legitimate claims, have contended their injuries were worse than they really were or have added previously damaged property to their claims. Such people do not view their fraudulent acts as crimes and do not consider what they are doing as wrong. – Accident – Injury Claim – Clumsy slip and fall – Liability Claim – Homeowner Loss – Pad for deductible – WC – Never injured – WC – Malingering – Kitchen fire – to remodel the home – Commercial sales are down – Cash theft A Global Leader in Compliance and Investigation Solutions
Opportunistic Insurance Fraud Perpetrators These are people who have taken the opportunity to squeeze extra money from the insurance companies. They usually do this only one or twice which is consider so called “soft fraud”. As an example, they have padded the amounts of their otherwise legitimate claims, have contended their injuries were worse than they really were or have added previously damaged property to their claims. Such people do not view their fraudulent acts as crimes and do not consider what they are doing as wrong. – Accident – Injury Claim – Clumsy slip and fall – Liability Claim – Homeowner Loss – Pad for deductible – WC – Never injured – WC – Malingering – Kitchen fire – to remodel the home – Commercial sales are down – Cash theft A Global Leader in Compliance and Investigation Solutions
 Con Artists These fraud perpetrators have frequently moved from place to place, pulling the same scams in city after city and town after town. “Slip and fall” accidents have been popular with many professional fraud perpetrators who have worked variations of this scheme in many different places. In some cases, they did not bother to stage actual falls rather they went directly to the storeowners and complained that falls have occurred on the premises. In both situations, other con artists acted as corroborative “witnesses”. The “injured” con artists usually insisted the stores were liable for the damages because of allegedly hazardous conditions, such as puddles or objects on the floor. The “injured” parties often complain of various other soft tissue or subjective injuries which rarely show up on x-rays and are therefore difficult to disprove. These people also often claim that they broke such items as eyeglasses, dentures and cameras. A Global Leader in Compliance and Investigation Solutions
Con Artists These fraud perpetrators have frequently moved from place to place, pulling the same scams in city after city and town after town. “Slip and fall” accidents have been popular with many professional fraud perpetrators who have worked variations of this scheme in many different places. In some cases, they did not bother to stage actual falls rather they went directly to the storeowners and complained that falls have occurred on the premises. In both situations, other con artists acted as corroborative “witnesses”. The “injured” con artists usually insisted the stores were liable for the damages because of allegedly hazardous conditions, such as puddles or objects on the floor. The “injured” parties often complain of various other soft tissue or subjective injuries which rarely show up on x-rays and are therefore difficult to disprove. These people also often claim that they broke such items as eyeglasses, dentures and cameras. A Global Leader in Compliance and Investigation Solutions
 Auto Salvage Fraud The insurer becomes the vehicle owner after paying for a claim on a total loss of that vehicle. In most states, the insurer obtains a salvage title from the Department of Motor Vehicles. The vehicle’s title is stamped with the words, “salvage vehicle” or “junk” to show the vehicle was previously declared a total loss. The insurer puts the salvaged vehicle up for sale, usually either through auction or sealed bid. Legitimate salvage yards often purchase such vehicles, dismantle them and resell the usable parts. The buyer of the salvaged vehicle receives the salvage title and the plate from the vehicle that shows the manufacturer’s vehicle identification number (VIN), which is a combination of letters and numbers that were originally used for the manufacturer’s inventory purposes. One type of fraud scheme is called “body swing” where fraud perpetrators purchased a salvaged vehicle with extensive body damage but with other major parts in fairly good condition. Then, they stole a matching, undamaged vehicle. Instead of grinding the VIN off the vehicle and re-stamping it, they removed the entire undamaged body from its chassis and put it on the salvaged vehicle. Then, they transferred the VIN plate from the salvaged vehicle to the stolen vehicle. A Global Leader in Compliance and Investigation Solutions
Auto Salvage Fraud The insurer becomes the vehicle owner after paying for a claim on a total loss of that vehicle. In most states, the insurer obtains a salvage title from the Department of Motor Vehicles. The vehicle’s title is stamped with the words, “salvage vehicle” or “junk” to show the vehicle was previously declared a total loss. The insurer puts the salvaged vehicle up for sale, usually either through auction or sealed bid. Legitimate salvage yards often purchase such vehicles, dismantle them and resell the usable parts. The buyer of the salvaged vehicle receives the salvage title and the plate from the vehicle that shows the manufacturer’s vehicle identification number (VIN), which is a combination of letters and numbers that were originally used for the manufacturer’s inventory purposes. One type of fraud scheme is called “body swing” where fraud perpetrators purchased a salvaged vehicle with extensive body damage but with other major parts in fairly good condition. Then, they stole a matching, undamaged vehicle. Instead of grinding the VIN off the vehicle and re-stamping it, they removed the entire undamaged body from its chassis and put it on the salvaged vehicle. Then, they transferred the VIN plate from the salvaged vehicle to the stolen vehicle. A Global Leader in Compliance and Investigation Solutions
 Title Washing The objective of still another scheme, known as “title washing” or “title laundering, ” is to eliminate the designation “salvage vehicle” or “junk” from a legitimate salvage title. Fraud perpetrators have worked this scheme by purchasing expensive, late-model, salvaged vehicles and rebuilt and disguised them. Then, they register and re-title them in states where salvage brands on titles are not required. That way, there was no indication the vehicles were ever damaged, and the insurer’s names as owners were effectively removed from the titles. Many times, these previously damaged vehicles were sold to unsuspecting buyers for much more than the vehicles were worth, and the new owners usually obtained insurance on them. The result was the buyers purchased and the insurers insured previously salvaged vehicle that likely had some very serious defects. A Global Leader in Compliance and Investigation Solutions
Title Washing The objective of still another scheme, known as “title washing” or “title laundering, ” is to eliminate the designation “salvage vehicle” or “junk” from a legitimate salvage title. Fraud perpetrators have worked this scheme by purchasing expensive, late-model, salvaged vehicles and rebuilt and disguised them. Then, they register and re-title them in states where salvage brands on titles are not required. That way, there was no indication the vehicles were ever damaged, and the insurer’s names as owners were effectively removed from the titles. Many times, these previously damaged vehicles were sold to unsuspecting buyers for much more than the vehicles were worth, and the new owners usually obtained insurance on them. The result was the buyers purchased and the insurers insured previously salvaged vehicle that likely had some very serious defects. A Global Leader in Compliance and Investigation Solutions
 TYPES OF INSURANCE FRAUD BEWARE!!!!
TYPES OF INSURANCE FRAUD BEWARE!!!!
 When Fraud Has Been Committed • While many of the examples we’ve shared so far are of fraud that occurs when a claim is made, you should be aware that fraud can occur at any point in the insurance process. Fraud may also occur during the application process, be introduced by an agent or broker, be introduced by a third party administrator, or occur internally at the insurance company. • Generally, insurance fraud is categorized into three areas: – Application Fraud; – Claim Fraud; and – Internal Fraud A Global Leader in Compliance and Investigation Solutions
When Fraud Has Been Committed • While many of the examples we’ve shared so far are of fraud that occurs when a claim is made, you should be aware that fraud can occur at any point in the insurance process. Fraud may also occur during the application process, be introduced by an agent or broker, be introduced by a third party administrator, or occur internally at the insurance company. • Generally, insurance fraud is categorized into three areas: – Application Fraud; – Claim Fraud; and – Internal Fraud A Global Leader in Compliance and Investigation Solutions
 At The Time Of Application fraud is fraud that occurs when the policy is purchased. Application fraud is generally categorized as either contract fraud or premium fraud. An application that is denied because of a material misrepresentation is attempted insurance fraud and requires reporting to the state. A Global Leader in Compliance and Investigation Solutions
At The Time Of Application fraud is fraud that occurs when the policy is purchased. Application fraud is generally categorized as either contract fraud or premium fraud. An application that is denied because of a material misrepresentation is attempted insurance fraud and requires reporting to the state. A Global Leader in Compliance and Investigation Solutions
 Contract Fraud vs. Premium Fraud • Misstatements in a policy application that are made to convince an insurance company to enter into a contract are referred to as “contract fraud” • Misrepresentations that induce an insurance company to charge a lower premium are “premium fraud” or “rate evasion” A Global Leader in Compliance and Investigation Solutions
Contract Fraud vs. Premium Fraud • Misstatements in a policy application that are made to convince an insurance company to enter into a contract are referred to as “contract fraud” • Misrepresentations that induce an insurance company to charge a lower premium are “premium fraud” or “rate evasion” A Global Leader in Compliance and Investigation Solutions
 Contract Fraud For example, answering no to questions about: – prior at fault accidents – issues of policy cancellation or non-renewals – issues of storage of explosives – issues about sky diving or pilot license – past company name to avoid WC modifier – ownership of pets on premises A Global Leader in Compliance and Investigation Solutions
Contract Fraud For example, answering no to questions about: – prior at fault accidents – issues of policy cancellation or non-renewals – issues of storage of explosives – issues about sky diving or pilot license – past company name to avoid WC modifier – ownership of pets on premises A Global Leader in Compliance and Investigation Solutions
 Premium Fraud • An insured omits the fact he has teenager who drive his cars. • An insured lives in a city but uses someone else’s address in a suburb to reduce his auto premium. • An applicant requests non tobacco premium rates and denies tobacco use, even though he smokes. A Global Leader in Compliance and Investigation Solutions
Premium Fraud • An insured omits the fact he has teenager who drive his cars. • An insured lives in a city but uses someone else’s address in a suburb to reduce his auto premium. • An applicant requests non tobacco premium rates and denies tobacco use, even though he smokes. A Global Leader in Compliance and Investigation Solutions
 WC Premium Fraud • Not reporting all employees. • Misclassification of employees; such as classifying roofers or tree trimmers as office workers. • Misidentifying your principal place of operation in a state that provides better rates. • Misreporting the number of job sites or workers. A Global Leader in Compliance and Investigation Solutions
WC Premium Fraud • Not reporting all employees. • Misclassification of employees; such as classifying roofers or tree trimmers as office workers. • Misidentifying your principal place of operation in a state that provides better rates. • Misreporting the number of job sites or workers. A Global Leader in Compliance and Investigation Solutions
 Claim Fraud Creating a fraudulent claim may include: • • • Staged or caused auto accidents; Staged slip and fall accidents; False claim of foreign object in food or drink; Faking a death to collect benefits, or filing a phony death claim; Murder-for-profit; Phony burglary theft or vandalism; Arson; Staged auto thefts; Staged homeowner accident or burglary; “Fibbers" or “Padders" who overstate their insurance claims to make up for the deductible; • Claiming prior damage occurred in the current accident; A Global Leader in Compliance and Investigation Solutions
Claim Fraud Creating a fraudulent claim may include: • • • Staged or caused auto accidents; Staged slip and fall accidents; False claim of foreign object in food or drink; Faking a death to collect benefits, or filing a phony death claim; Murder-for-profit; Phony burglary theft or vandalism; Arson; Staged auto thefts; Staged homeowner accident or burglary; “Fibbers" or “Padders" who overstate their insurance claims to make up for the deductible; • Claiming prior damage occurred in the current accident; A Global Leader in Compliance and Investigation Solutions
 Claim Fraud…Continued Creating a fraudulent claim may include: • Claiming a minor injury created a partial or total disability; • Receiving disability payments while working elsewhere conducting the same or similar work duties; • Claiming false disability; • Medical providers billing for services not rendered; • Providing unnecessary medical treatment; • Charging for non-provided medical tests; • Pharmacist "upcoding" for medicine by issuing generic pills and charging for name brand. • Multiple Policies for Profit -- A property or vehicle owner illegally buys numerous insurance policies for one property or vehicle and then damages or destroys it, collecting on all policies. A Global Leader in Compliance and Investigation Solutions
Claim Fraud…Continued Creating a fraudulent claim may include: • Claiming a minor injury created a partial or total disability; • Receiving disability payments while working elsewhere conducting the same or similar work duties; • Claiming false disability; • Medical providers billing for services not rendered; • Providing unnecessary medical treatment; • Charging for non-provided medical tests; • Pharmacist "upcoding" for medicine by issuing generic pills and charging for name brand. • Multiple Policies for Profit -- A property or vehicle owner illegally buys numerous insurance policies for one property or vehicle and then damages or destroys it, collecting on all policies. A Global Leader in Compliance and Investigation Solutions
 Internal Fraud Internal fraud are those perpetrated against an insurance company or its policyholders by insurance agents, managers, executives, or other insurance employees. Examples include: Embezzlement – Employee stealing money from their employer. Agent, Adjuster or Personnel Claim Rings Fake/False/Forged Documents -- Agent or insurer issuing fake policies, certificates, insurance identification cards or binders. False Statements -- Agent or insurer making a false statement on a filing. Pocketing Premiums -- Agent or insurer pocketing premiums, then issuing a phony policy or none at all. A Global Leader in Compliance and Investigation Solutions
Internal Fraud Internal fraud are those perpetrated against an insurance company or its policyholders by insurance agents, managers, executives, or other insurance employees. Examples include: Embezzlement – Employee stealing money from their employer. Agent, Adjuster or Personnel Claim Rings Fake/False/Forged Documents -- Agent or insurer issuing fake policies, certificates, insurance identification cards or binders. False Statements -- Agent or insurer making a false statement on a filing. Pocketing Premiums -- Agent or insurer pocketing premiums, then issuing a phony policy or none at all. A Global Leader in Compliance and Investigation Solutions
 Effective Utilization of Investigative Results What Does a Win Look Like? A Global Leader in Compliance and Investigation Solutions
Effective Utilization of Investigative Results What Does a Win Look Like? A Global Leader in Compliance and Investigation Solutions
 Paying & Settling the Claim • Many times the initial red flags identified by the claim examiner are determined to be unfounded after an investigation. • Or, the investigation results are “undetermined” and standard claim handling continues, although consideration should be given to additional investigation. • The claimant was and is really injured and/or disabled, and unable to work. Therefore, payments to them are the appropriate course of action. A Global Leader in Compliance and Investigation Solutions
Paying & Settling the Claim • Many times the initial red flags identified by the claim examiner are determined to be unfounded after an investigation. • Or, the investigation results are “undetermined” and standard claim handling continues, although consideration should be given to additional investigation. • The claimant was and is really injured and/or disabled, and unable to work. Therefore, payments to them are the appropriate course of action. A Global Leader in Compliance and Investigation Solutions
 Mitigating Claims • Many times the information obtained during investigative activities may lead to an opportunity to use the results to mitigate the loss. • The information gained thru surveillance, field investigation (AOE/COE), background investigation, activity checks, etc. may provide the claim examiner with positive information to negotiate a reasonable settlement of the loss, or move a claimant and/or their attorney to a more favorable settlement posture. A Global Leader in Compliance and Investigation Solutions
Mitigating Claims • Many times the information obtained during investigative activities may lead to an opportunity to use the results to mitigate the loss. • The information gained thru surveillance, field investigation (AOE/COE), background investigation, activity checks, etc. may provide the claim examiner with positive information to negotiate a reasonable settlement of the loss, or move a claimant and/or their attorney to a more favorable settlement posture. A Global Leader in Compliance and Investigation Solutions
 Denying the Claim • Obviously, the denial of a reported claim is a serious issue and not to be taken lightly, or without considerable information, evaluation, and consultation with your claims management and/or claims counsel. • There must be clear and documented evidence for the reason for the denial, whether for reasons of compensability, coverage, fraud, or other specific reason where denial may be permissible. • All denials should be in writing, and specifically addressing the reasons for the denial, and reserving any other reasons that may exist. • Denial letters should NOT be form letters, but should be written specifically for the claim being denied. • Denial letters should be sent regular U. S. Mail, and also by Certified Mail return receipt. A Global Leader in Compliance and Investigation Solutions
Denying the Claim • Obviously, the denial of a reported claim is a serious issue and not to be taken lightly, or without considerable information, evaluation, and consultation with your claims management and/or claims counsel. • There must be clear and documented evidence for the reason for the denial, whether for reasons of compensability, coverage, fraud, or other specific reason where denial may be permissible. • All denials should be in writing, and specifically addressing the reasons for the denial, and reserving any other reasons that may exist. • Denial letters should NOT be form letters, but should be written specifically for the claim being denied. • Denial letters should be sent regular U. S. Mail, and also by Certified Mail return receipt. A Global Leader in Compliance and Investigation Solutions
 Additional Action • The information from the claim coupled with investigative results may lead the examiner to conclude, and form a reasonable belief that the claim (or aspects thereof) are suspicious, and thus break the threshold for mandatory reporting of a suspicious claim to the DOI, DA, or other required law enforcement authority required by statute. • If you can answer the Question… I believe this case is fraud because……. A Global Leader in Compliance and Investigation Solutions
Additional Action • The information from the claim coupled with investigative results may lead the examiner to conclude, and form a reasonable belief that the claim (or aspects thereof) are suspicious, and thus break the threshold for mandatory reporting of a suspicious claim to the DOI, DA, or other required law enforcement authority required by statute. • If you can answer the Question… I believe this case is fraud because……. A Global Leader in Compliance and Investigation Solutions
 Red Flag Indicators By Line of Business Workers’ Compensation A Global Leader in Compliance and Investigation Solutions
Red Flag Indicators By Line of Business Workers’ Compensation A Global Leader in Compliance and Investigation Solutions
 Specific Indicators of Suspicious Claims General and Line of Business Workers’ Compensation Fraud Indicators It is important to remember that indicators listed here are merely possible “red flags, ” not actual evidence of fraud. Even the presence of several indicators, while suggestive of possible fraud, does not mean that fraud has definitely been committed. When you have several of these indicators present or a pattern begins to emerge, you should consult with your SIU. A Global Leader in Compliance and Investigation Solutions
Specific Indicators of Suspicious Claims General and Line of Business Workers’ Compensation Fraud Indicators It is important to remember that indicators listed here are merely possible “red flags, ” not actual evidence of fraud. Even the presence of several indicators, while suggestive of possible fraud, does not mean that fraud has definitely been committed. When you have several of these indicators present or a pattern begins to emerge, you should consult with your SIU. A Global Leader in Compliance and Investigation Solutions
 Claimant, Prior Claims History & Current Working Status • The claimant changes physicians when a release for work has been issued • The claimant has a history of reporting subjective injuries • Review of the rehabilitation report describes the claimant as being muscular, well tanned, having callused hands and/or grease under nails • A surveillance or "tip" reveals the totally disabled worker is currently employed elsewhere • After injury, the injured worker is never home, or a spouse/relative who answers the phone says the injured worker "just stepped out" A Global Leader in Compliance and Investigation Solutions
Claimant, Prior Claims History & Current Working Status • The claimant changes physicians when a release for work has been issued • The claimant has a history of reporting subjective injuries • Review of the rehabilitation report describes the claimant as being muscular, well tanned, having callused hands and/or grease under nails • A surveillance or "tip" reveals the totally disabled worker is currently employed elsewhere • After injury, the injured worker is never home, or a spouse/relative who answers the phone says the injured worker "just stepped out" A Global Leader in Compliance and Investigation Solutions
 Claimant, Prior Claims History & Current Working Status • Return calls to the claimant's residence have strange or unexpected background noises, which indicate it may not be a residence • The claimant has several other family members also receiving workers' compensation benefits or other benefits, such as unemployment • The claimant demands quick settlement decisions of commitments or is consistently uncooperative • The claimant is unusually familiar with workers' compensation claims handling procedures and laws • Workers’ compensation claims contain whiteout or are submitted as a photocopy A Global Leader in Compliance and Investigation Solutions
Claimant, Prior Claims History & Current Working Status • Return calls to the claimant's residence have strange or unexpected background noises, which indicate it may not be a residence • The claimant has several other family members also receiving workers' compensation benefits or other benefits, such as unemployment • The claimant demands quick settlement decisions of commitments or is consistently uncooperative • The claimant is unusually familiar with workers' compensation claims handling procedures and laws • Workers’ compensation claims contain whiteout or are submitted as a photocopy A Global Leader in Compliance and Investigation Solutions
 Circumstances of the Accident • The accident occurs late Friday afternoon or shortly after the employee reports to work on Monday • The accident is un-witnessed or witnesses to the accident conflict with the applicant’s version or with one another • The claimant alleges an injury at an odd time, i. e. at lunch hour. • Fellow workers hear rumors circulating that the accident was not legitimate • The accident occurs in an area where the injured employee would not normally be working. A Global Leader in Compliance and Investigation Solutions
Circumstances of the Accident • The accident occurs late Friday afternoon or shortly after the employee reports to work on Monday • The accident is un-witnessed or witnesses to the accident conflict with the applicant’s version or with one another • The claimant alleges an injury at an odd time, i. e. at lunch hour. • Fellow workers hear rumors circulating that the accident was not legitimate • The accident occurs in an area where the injured employee would not normally be working. A Global Leader in Compliance and Investigation Solutions
 Circumstances of the Accident • The task that caused the accident isn’t the type the employee should be involved in such as an office worker lifting heavy objects on to a loading dock • The accident occurs just prior to a strike, job termination, layoff or near the end of the employee's probationary period • The employer's first report of injury contrasts with the description of the accident set forth in the medical history • The accident details from the claimant are vague or contradictory, have inconsistencies or are generally not credible • The accident is not promptly reported by the employee to a supervisor A Global Leader in Compliance and Investigation Solutions
Circumstances of the Accident • The task that caused the accident isn’t the type the employee should be involved in such as an office worker lifting heavy objects on to a loading dock • The accident occurs just prior to a strike, job termination, layoff or near the end of the employee's probationary period • The employer's first report of injury contrasts with the description of the accident set forth in the medical history • The accident details from the claimant are vague or contradictory, have inconsistencies or are generally not credible • The accident is not promptly reported by the employee to a supervisor A Global Leader in Compliance and Investigation Solutions
 Circumstances of the Accident • Claimant or attorney refuses to provide complete accident or injury information • Claimant alleges fall in liquid spill yet their clothes/shoes not wet from substance • Claimant alleges fall on wet/slippery area where there is no source of spill identified • Claimant states the accident was unwitnessed • Witnesses or video surveillance contradict facts presented by claimant A Global Leader in Compliance and Investigation Solutions
Circumstances of the Accident • Claimant or attorney refuses to provide complete accident or injury information • Claimant alleges fall in liquid spill yet their clothes/shoes not wet from substance • Claimant alleges fall on wet/slippery area where there is no source of spill identified • Claimant states the accident was unwitnessed • Witnesses or video surveillance contradict facts presented by claimant A Global Leader in Compliance and Investigation Solutions
 The Claimant’s Attorney • The claimant's attorney is known for handling questionable claims • The attorney lien or representation letter is dated the day of the reported accident • The same doctor/lawyer combination previously known to handle similar questionable injury claims • The claimant initially wants to settle with the insured but later retains an attorney and reports increased subjective complaints • There is wholesale claim handling by law firms and multiple class action suits • The claimant's attorney threatens legal action unless a quick settlement is made • There a high number of WC applications from a specific firm • The claimant's attorney inquires about a settlement or buyout early in the life of the claim process • There is a pattern of occupational type claims for "dying" industries, such as black lung disease or asbestosis A Global Leader in Compliance and Investigation Solutions
The Claimant’s Attorney • The claimant's attorney is known for handling questionable claims • The attorney lien or representation letter is dated the day of the reported accident • The same doctor/lawyer combination previously known to handle similar questionable injury claims • The claimant initially wants to settle with the insured but later retains an attorney and reports increased subjective complaints • There is wholesale claim handling by law firms and multiple class action suits • The claimant's attorney threatens legal action unless a quick settlement is made • There a high number of WC applications from a specific firm • The claimant's attorney inquires about a settlement or buyout early in the life of the claim process • There is a pattern of occupational type claims for "dying" industries, such as black lung disease or asbestosis A Global Leader in Compliance and Investigation Solutions
 The Medical Treatment Provider • Diagnosis inconsistent with treatment or pathology report conflicts with the diagnosis • Health care provider is known for suspicious treatment or the employer is suspicious about a particular health care provider • The medical provider repeatedly calls the patient back for treatment and keeps the "medicals" open • The claimant writes unsolicited statements about how much better they are, but treatment continues and they don't return to work • The claimant receives unauthorized treatment with a questionable emergency • The same medical provider always bills for extra time, extra body parts, and/or special considerations • Unexpected high costs (special supplies, home therapies, diagnostic testing) begin early for a minor injury, soft tissue, and subjective findings A Global Leader in Compliance and Investigation Solutions
The Medical Treatment Provider • Diagnosis inconsistent with treatment or pathology report conflicts with the diagnosis • Health care provider is known for suspicious treatment or the employer is suspicious about a particular health care provider • The medical provider repeatedly calls the patient back for treatment and keeps the "medicals" open • The claimant writes unsolicited statements about how much better they are, but treatment continues and they don't return to work • The claimant receives unauthorized treatment with a questionable emergency • The same medical provider always bills for extra time, extra body parts, and/or special considerations • Unexpected high costs (special supplies, home therapies, diagnostic testing) begin early for a minor injury, soft tissue, and subjective findings A Global Leader in Compliance and Investigation Solutions
 The Medical Treatment Provider • The claimant submits no transportation bills or is confirmed elsewhere on the same day that medical treatment is billed • Medical providers steer claimants to attorneys and/or bills through an attorney • The medical provider is reluctant to communicate with the insurer but initiates calls to a claimant attorney • The insurer receives a demand from an attorney for referral to a specific medical provider • A single medical provider with a high percentage of claimants with attorneys, especially if the same attorney • The medical provider refers claimants unnecessarily to specific medical specialists (may be kickback scheme in place) • A specific provider prescribes unnecessary Durable Medical Equipment or supplies A Global Leader in Compliance and Investigation Solutions
The Medical Treatment Provider • The claimant submits no transportation bills or is confirmed elsewhere on the same day that medical treatment is billed • Medical providers steer claimants to attorneys and/or bills through an attorney • The medical provider is reluctant to communicate with the insurer but initiates calls to a claimant attorney • The insurer receives a demand from an attorney for referral to a specific medical provider • A single medical provider with a high percentage of claimants with attorneys, especially if the same attorney • The medical provider refers claimants unnecessarily to specific medical specialists (may be kickback scheme in place) • A specific provider prescribes unnecessary Durable Medical Equipment or supplies A Global Leader in Compliance and Investigation Solutions
 The Medical Treatment Provider • Medical records consist of “template” style reports or consist of "canned" notes • There are missing dates of service or there are non-sequential notes or lot numbers on invoices • Medical records show different handwriting on same dates of service, gender is wrong or noted • Medical records show different inks on same dates of service or the same ink and handwriting covering a lengthy period of time • When medical records are requested, insurer is advised the records are lost, stolen, or burned. Records provided are photocopies of originals • Progress notes consistently reflect high degree of pain on each visit while stating "progressing as planned" or "good improvement • There are conflicting medical reports; i. e. , independent medical examinations, emergency room reports vs. subsequent office visits A Global Leader in Compliance and Investigation Solutions
The Medical Treatment Provider • Medical records consist of “template” style reports or consist of "canned" notes • There are missing dates of service or there are non-sequential notes or lot numbers on invoices • Medical records show different handwriting on same dates of service, gender is wrong or noted • Medical records show different inks on same dates of service or the same ink and handwriting covering a lengthy period of time • When medical records are requested, insurer is advised the records are lost, stolen, or burned. Records provided are photocopies of originals • Progress notes consistently reflect high degree of pain on each visit while stating "progressing as planned" or "good improvement • There are conflicting medical reports; i. e. , independent medical examinations, emergency room reports vs. subsequent office visits A Global Leader in Compliance and Investigation Solutions
 The Medical Treatment Provider • Operative reports vs. anesthesia reports, pathology reports vs. consent forms; noteworthy inconsistent findings between providers • Consistent improper billing practices, such as unbundling, up-coding, and/or double billing • Billing workers' compensation carrier and another insurer full charge for "same" services; payment is accepted from both • The medical provider holds bills and submits them all at one time, especially if submitted through an attorney, indicating possible collusion • The medical reports show excessive referrals to specific providers, yet there is no apparent serious injury • The medical bills show excessive early referrals for psychiatric testing when accident involved trauma A Global Leader in Compliance and Investigation Solutions
The Medical Treatment Provider • Operative reports vs. anesthesia reports, pathology reports vs. consent forms; noteworthy inconsistent findings between providers • Consistent improper billing practices, such as unbundling, up-coding, and/or double billing • Billing workers' compensation carrier and another insurer full charge for "same" services; payment is accepted from both • The medical provider holds bills and submits them all at one time, especially if submitted through an attorney, indicating possible collusion • The medical reports show excessive referrals to specific providers, yet there is no apparent serious injury • The medical bills show excessive early referrals for psychiatric testing when accident involved trauma A Global Leader in Compliance and Investigation Solutions
 General Liability Fraud Indicators It is important to remember that indicators listed here are merely possible “red flags, ” not actual evidence of fraud. Even the presence of several indicators, while suggestive of possible fraud, does not mean that fraud has definitely been committed. When you have several of these indicators present or a pattern begins to emerge, you should consult with your SIU. A Global Leader in Compliance and Investigation Solutions
General Liability Fraud Indicators It is important to remember that indicators listed here are merely possible “red flags, ” not actual evidence of fraud. Even the presence of several indicators, while suggestive of possible fraud, does not mean that fraud has definitely been committed. When you have several of these indicators present or a pattern begins to emerge, you should consult with your SIU. A Global Leader in Compliance and Investigation Solutions
 General Liability Fraud Indicators • Any anonymous phone call or letter alleging possible fraud • Any law enforcement inquiry regarding the validity of any part of the claim • Any false statement willfully made with the intent to deceive • The insured refuses to cooperate with our investigation • The first notice (letter or phone) from an attorney is on the day of the accident • Three or more ISO Claim Search returns in the past two years involving the claimant • The claimant’s address and/or phone number are returned as ISO Claim Search ‘hits” with names of other persons reporting the same or similar type claims and injuries (especially if within relatively short period of time) A Global Leader in Compliance and Investigation Solutions
General Liability Fraud Indicators • Any anonymous phone call or letter alleging possible fraud • Any law enforcement inquiry regarding the validity of any part of the claim • Any false statement willfully made with the intent to deceive • The insured refuses to cooperate with our investigation • The first notice (letter or phone) from an attorney is on the day of the accident • Three or more ISO Claim Search returns in the past two years involving the claimant • The claimant’s address and/or phone number are returned as ISO Claim Search ‘hits” with names of other persons reporting the same or similar type claims and injuries (especially if within relatively short period of time) A Global Leader in Compliance and Investigation Solutions
 General Liability Fraud Indicators • Claimant is having serious financial difficulties • Claimant refuses to mail information to office but insists on bringing in-person • Claimant possesses unusual knowledge of insurance terminology and procedures • Claimant lives at a PO Box or hotel and states no physical address exists • Claimant address provided as physical address actually returns to private mail box, non-existent address, or jail/prison facility • Claimant frequently changes phone number for them to be contacted • Claimant is never at home or spouse/roommate always states claimant “just stepped out. ” • Claimant obtains medical evaluation and “estimate” of charges if they have surgery but never returns to doctor or follows through with forecasted medical treatment A Global Leader in Compliance and Investigation Solutions
General Liability Fraud Indicators • Claimant is having serious financial difficulties • Claimant refuses to mail information to office but insists on bringing in-person • Claimant possesses unusual knowledge of insurance terminology and procedures • Claimant lives at a PO Box or hotel and states no physical address exists • Claimant address provided as physical address actually returns to private mail box, non-existent address, or jail/prison facility • Claimant frequently changes phone number for them to be contacted • Claimant is never at home or spouse/roommate always states claimant “just stepped out. ” • Claimant obtains medical evaluation and “estimate” of charges if they have surgery but never returns to doctor or follows through with forecasted medical treatment A Global Leader in Compliance and Investigation Solutions
 General Liability Fraud Indicators • Claimant can’t (or refuses to) produce valid government issued Identification • Claimant is accompanied by an adult (friend or relative) that can not (or refuses to) produce a government issued ID • The insured has no knowledge of accident or injury • Claimant’s accident description on day of loss differs from the account on the medical history or future interviews • Insured raises questions about the suspicious nature of the claim • Background noise on phone calls to the residence suggest it is not a “residence” phone • Claimant has disability policies which were recently obtained • No police report exists for an alleged assault with injuries reported to have occurred on insured’s property A Global Leader in Compliance and Investigation Solutions
General Liability Fraud Indicators • Claimant can’t (or refuses to) produce valid government issued Identification • Claimant is accompanied by an adult (friend or relative) that can not (or refuses to) produce a government issued ID • The insured has no knowledge of accident or injury • Claimant’s accident description on day of loss differs from the account on the medical history or future interviews • Insured raises questions about the suspicious nature of the claim • Background noise on phone calls to the residence suggest it is not a “residence” phone • Claimant has disability policies which were recently obtained • No police report exists for an alleged assault with injuries reported to have occurred on insured’s property A Global Leader in Compliance and Investigation Solutions
 Auto Insurance Fraud Indicators It is important to remember that indicators listed here are merely possible “red flags, ” not actual evidence of fraud. Even the presence of several indicators, while suggestive of possible fraud, does not mean that fraud has definitely been committed. When you have several of these indicators present or a pattern begins to emerge, you should consult with your SIU. A Global Leader in Compliance and Investigation Solutions
Auto Insurance Fraud Indicators It is important to remember that indicators listed here are merely possible “red flags, ” not actual evidence of fraud. Even the presence of several indicators, while suggestive of possible fraud, does not mean that fraud has definitely been committed. When you have several of these indicators present or a pattern begins to emerge, you should consult with your SIU. A Global Leader in Compliance and Investigation Solutions
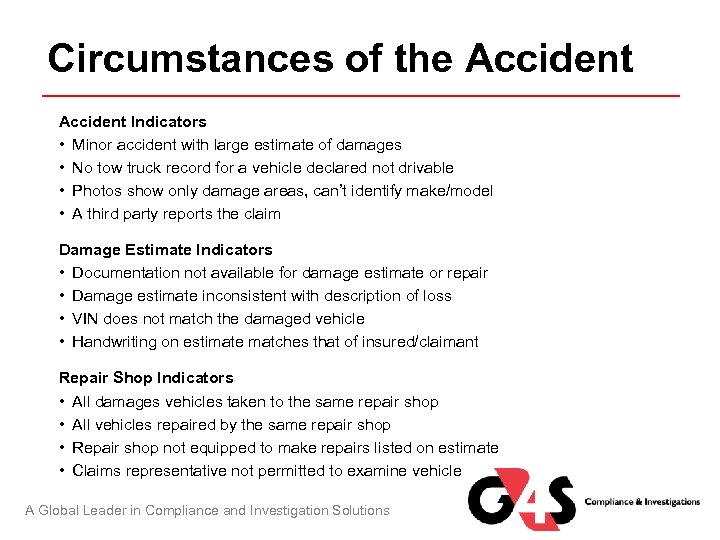 Circumstances of the Accident Indicators • Minor accident with large estimate of damages • No tow truck record for a vehicle declared not drivable • Photos show only damage areas, can’t identify make/model • A third party reports the claim Damage Estimate Indicators • Documentation not available for damage estimate or repair • Damage estimate inconsistent with description of loss • VIN does not match the damaged vehicle • Handwriting on estimate matches that of insured/claimant Repair Shop Indicators • All damages vehicles taken to the same repair shop • All vehicles repaired by the same repair shop • Repair shop not equipped to make repairs listed on estimate • Claims representative not permitted to examine vehicle A Global Leader in Compliance and Investigation Solutions
Circumstances of the Accident Indicators • Minor accident with large estimate of damages • No tow truck record for a vehicle declared not drivable • Photos show only damage areas, can’t identify make/model • A third party reports the claim Damage Estimate Indicators • Documentation not available for damage estimate or repair • Damage estimate inconsistent with description of loss • VIN does not match the damaged vehicle • Handwriting on estimate matches that of insured/claimant Repair Shop Indicators • All damages vehicles taken to the same repair shop • All vehicles repaired by the same repair shop • Repair shop not equipped to make repairs listed on estimate • Claims representative not permitted to examine vehicle A Global Leader in Compliance and Investigation Solutions
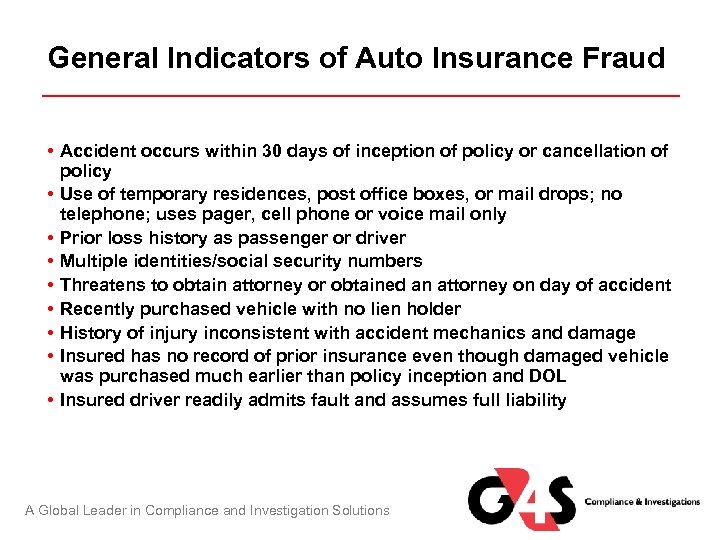 General Indicators of Auto Insurance Fraud • Accident occurs within 30 days of inception of policy or cancellation of policy • Use of temporary residences, post office boxes, or mail drops; no telephone; uses pager, cell phone or voice mail only • Prior loss history as passenger or driver • Multiple identities/social security numbers • Threatens to obtain attorney or obtained an attorney on day of accident • Recently purchased vehicle with no lien holder • History of injury inconsistent with accident mechanics and damage • Insured has no record of prior insurance even though damaged vehicle was purchased much earlier than policy inception and DOL • Insured driver readily admits fault and assumes full liability A Global Leader in Compliance and Investigation Solutions
General Indicators of Auto Insurance Fraud • Accident occurs within 30 days of inception of policy or cancellation of policy • Use of temporary residences, post office boxes, or mail drops; no telephone; uses pager, cell phone or voice mail only • Prior loss history as passenger or driver • Multiple identities/social security numbers • Threatens to obtain attorney or obtained an attorney on day of accident • Recently purchased vehicle with no lien holder • History of injury inconsistent with accident mechanics and damage • Insured has no record of prior insurance even though damaged vehicle was purchased much earlier than policy inception and DOL • Insured driver readily admits fault and assumes full liability A Global Leader in Compliance and Investigation Solutions
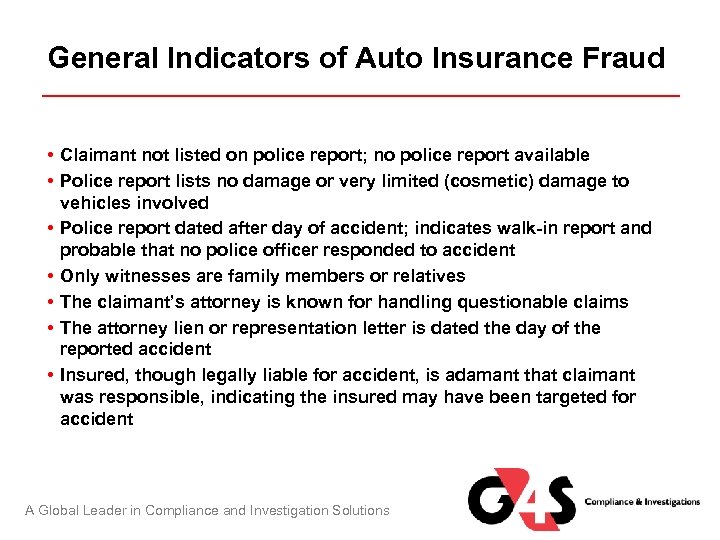 General Indicators of Auto Insurance Fraud • Claimant not listed on police report; no police report available • Police report lists no damage or very limited (cosmetic) damage to vehicles involved • Police report dated after day of accident; indicates walk-in report and probable that no police officer responded to accident • Only witnesses are family members or relatives • The claimant’s attorney is known for handling questionable claims • The attorney lien or representation letter is dated the day of the reported accident • Insured, though legally liable for accident, is adamant that claimant was responsible, indicating the insured may have been targeted for accident A Global Leader in Compliance and Investigation Solutions
General Indicators of Auto Insurance Fraud • Claimant not listed on police report; no police report available • Police report lists no damage or very limited (cosmetic) damage to vehicles involved • Police report dated after day of accident; indicates walk-in report and probable that no police officer responded to accident • Only witnesses are family members or relatives • The claimant’s attorney is known for handling questionable claims • The attorney lien or representation letter is dated the day of the reported accident • Insured, though legally liable for accident, is adamant that claimant was responsible, indicating the insured may have been targeted for accident A Global Leader in Compliance and Investigation Solutions
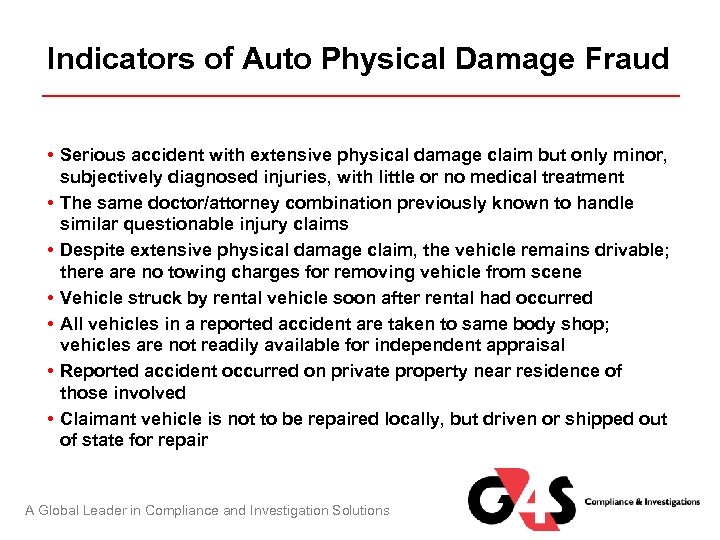 Indicators of Auto Physical Damage Fraud • Serious accident with extensive physical damage claim but only minor, subjectively diagnosed injuries, with little or no medical treatment • The same doctor/attorney combination previously known to handle similar questionable injury claims • Despite extensive physical damage claim, the vehicle remains drivable; there are no towing charges for removing vehicle from scene • Vehicle struck by rental vehicle soon after rental had occurred • All vehicles in a reported accident are taken to same body shop; vehicles are not readily available for independent appraisal • Reported accident occurred on private property near residence of those involved • Claimant vehicle is not to be repaired locally, but driven or shipped out of state for repair A Global Leader in Compliance and Investigation Solutions
Indicators of Auto Physical Damage Fraud • Serious accident with extensive physical damage claim but only minor, subjectively diagnosed injuries, with little or no medical treatment • The same doctor/attorney combination previously known to handle similar questionable injury claims • Despite extensive physical damage claim, the vehicle remains drivable; there are no towing charges for removing vehicle from scene • Vehicle struck by rental vehicle soon after rental had occurred • All vehicles in a reported accident are taken to same body shop; vehicles are not readily available for independent appraisal • Reported accident occurred on private property near residence of those involved • Claimant vehicle is not to be repaired locally, but driven or shipped out of state for repair A Global Leader in Compliance and Investigation Solutions
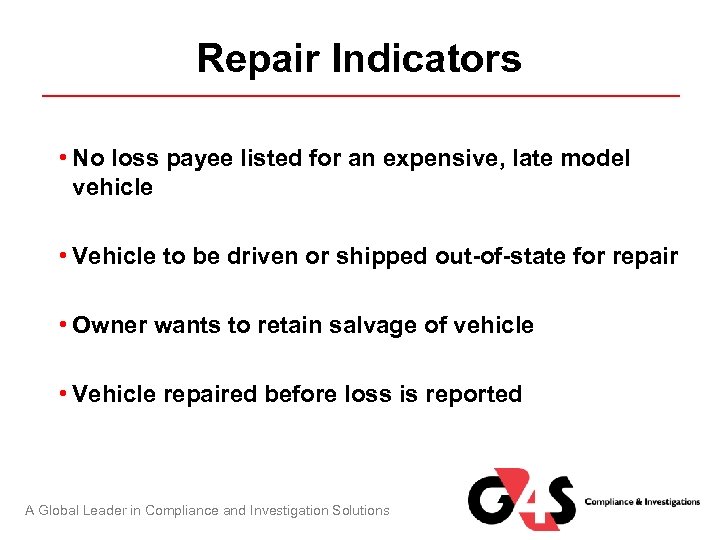 Repair Indicators • No loss payee listed for an expensive, late model vehicle • Vehicle to be driven or shipped out-of-state for repair • Owner wants to retain salvage of vehicle • Vehicle repaired before loss is reported A Global Leader in Compliance and Investigation Solutions
Repair Indicators • No loss payee listed for an expensive, late model vehicle • Vehicle to be driven or shipped out-of-state for repair • Owner wants to retain salvage of vehicle • Vehicle repaired before loss is reported A Global Leader in Compliance and Investigation Solutions
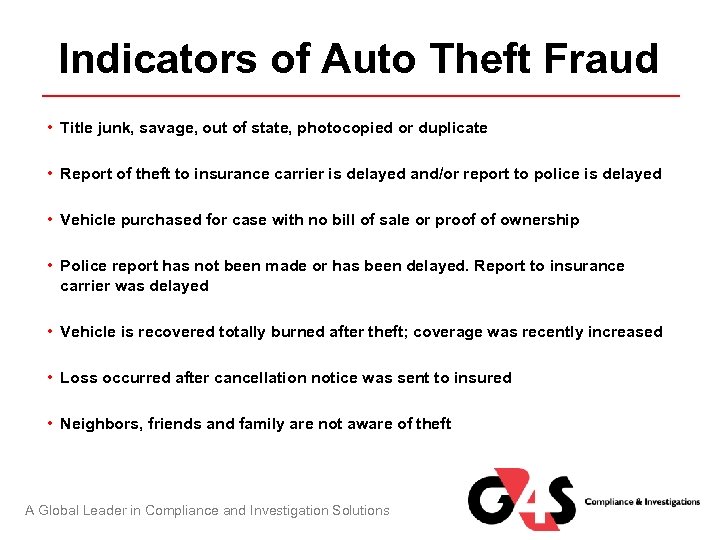 Indicators of Auto Theft Fraud • Title junk, savage, out of state, photocopied or duplicate • Report of theft to insurance carrier is delayed and/or report to police is delayed • Vehicle purchased for case with no bill of sale or proof of ownership • Police report has not been made or has been delayed. Report to insurance carrier was delayed • Vehicle is recovered totally burned after theft; coverage was recently increased • Loss occurred after cancellation notice was sent to insured • Neighbors, friends and family are not aware of theft A Global Leader in Compliance and Investigation Solutions
Indicators of Auto Theft Fraud • Title junk, savage, out of state, photocopied or duplicate • Report of theft to insurance carrier is delayed and/or report to police is delayed • Vehicle purchased for case with no bill of sale or proof of ownership • Police report has not been made or has been delayed. Report to insurance carrier was delayed • Vehicle is recovered totally burned after theft; coverage was recently increased • Loss occurred after cancellation notice was sent to insured • Neighbors, friends and family are not aware of theft A Global Leader in Compliance and Investigation Solutions
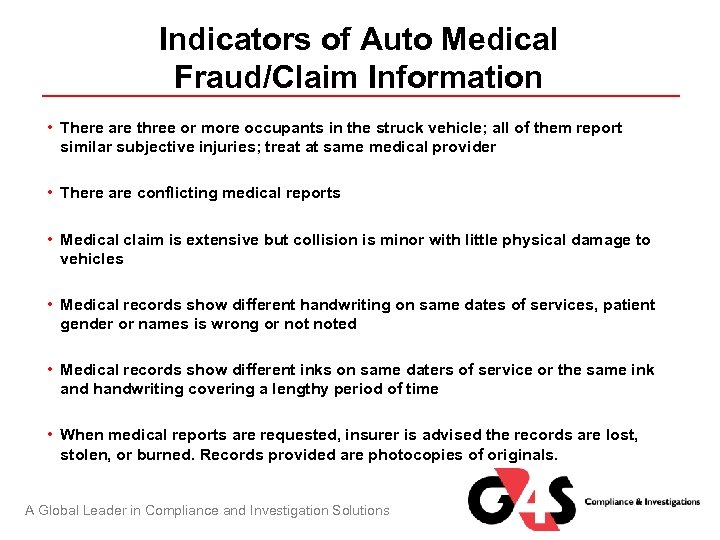 Indicators of Auto Medical Fraud/Claim Information • There are three or more occupants in the struck vehicle; all of them report similar subjective injuries; treat at same medical provider • There are conflicting medical reports • Medical claim is extensive but collision is minor with little physical damage to vehicles • Medical records show different handwriting on same dates of services, patient gender or names is wrong or noted • Medical records show different inks on same daters of service or the same ink and handwriting covering a lengthy period of time • When medical reports are requested, insurer is advised the records are lost, stolen, or burned. Records provided are photocopies of originals. A Global Leader in Compliance and Investigation Solutions
Indicators of Auto Medical Fraud/Claim Information • There are three or more occupants in the struck vehicle; all of them report similar subjective injuries; treat at same medical provider • There are conflicting medical reports • Medical claim is extensive but collision is minor with little physical damage to vehicles • Medical records show different handwriting on same dates of services, patient gender or names is wrong or noted • Medical records show different inks on same daters of service or the same ink and handwriting covering a lengthy period of time • When medical reports are requested, insurer is advised the records are lost, stolen, or burned. Records provided are photocopies of originals. A Global Leader in Compliance and Investigation Solutions
 Indicators of Auto Medical Fraud/Claim Information • Unexpected high costs (special supplies, home therapies, diagnostic testing) begin very early for a minor injury, soft tissue, and subjective findings • The claimant submits no transportation bills or is confirmed elsewhere on the same day that medical treatment is billed • The medical provider is reluctant to communicate with the insurer but initiates calls to a claimant attorney • The insurer receives a demand from an attorney for referral to a specific medical provider • A single medical provider with a high percentage of claimants with attorneys, especially if the same attorney • The medical provider refers claimants unnecessarily to specific medical specialists • Medical records consist of “template” style reports or consist of “canned” notes A Global Leader in Compliance and Investigation Solutions
Indicators of Auto Medical Fraud/Claim Information • Unexpected high costs (special supplies, home therapies, diagnostic testing) begin very early for a minor injury, soft tissue, and subjective findings • The claimant submits no transportation bills or is confirmed elsewhere on the same day that medical treatment is billed • The medical provider is reluctant to communicate with the insurer but initiates calls to a claimant attorney • The insurer receives a demand from an attorney for referral to a specific medical provider • A single medical provider with a high percentage of claimants with attorneys, especially if the same attorney • The medical provider refers claimants unnecessarily to specific medical specialists • Medical records consist of “template” style reports or consist of “canned” notes A Global Leader in Compliance and Investigation Solutions
 Indicators of Auto Medical Fraud/Claim Information • There are missing dates of service or there are non-sequential notes or lot numbers on invoices • Consistent improper billing practices, such as unbundling, up-coding, and/or double billing • The medical provider holds bills and submits them all at one time, especially if submitted through an attorney, indicating possible collusion • The medical reports show excessive referrals to specific providers, yet there is no apparent serious injury • The medical bills show excessive early referrals for psychiatric testing when accident involved trauma only • No emergency room treatment or emergency response on extensive injury claim • Medical treatment starts after attorney representation A Global Leader in Compliance and Investigation Solutions
Indicators of Auto Medical Fraud/Claim Information • There are missing dates of service or there are non-sequential notes or lot numbers on invoices • Consistent improper billing practices, such as unbundling, up-coding, and/or double billing • The medical provider holds bills and submits them all at one time, especially if submitted through an attorney, indicating possible collusion • The medical reports show excessive referrals to specific providers, yet there is no apparent serious injury • The medical bills show excessive early referrals for psychiatric testing when accident involved trauma only • No emergency room treatment or emergency response on extensive injury claim • Medical treatment starts after attorney representation A Global Leader in Compliance and Investigation Solutions
 Indicators of Automobile Accident Schemes • Either no police report or an over-the-counter report for accident resulting in multiple injuries and/or extensive physical damage • Accident occurred shortly after one or more vehicles were purchased or registered, or after the addition of comprehensive and collision coverage to the policy • Insured has history of accidents within short period of time on one policy. Index returns an active claims history • Expensive late model vehicle was recently purchased with cash (no lien holder) • Involved vehicle was expensive model less than 10 years old, purchased at auction with existing damage A Global Leader in Compliance and Investigation Solutions
Indicators of Automobile Accident Schemes • Either no police report or an over-the-counter report for accident resulting in multiple injuries and/or extensive physical damage • Accident occurred shortly after one or more vehicles were purchased or registered, or after the addition of comprehensive and collision coverage to the policy • Insured has history of accidents within short period of time on one policy. Index returns an active claims history • Expensive late model vehicle was recently purchased with cash (no lien holder) • Involved vehicle was expensive model less than 10 years old, purchased at auction with existing damage A Global Leader in Compliance and Investigation Solutions
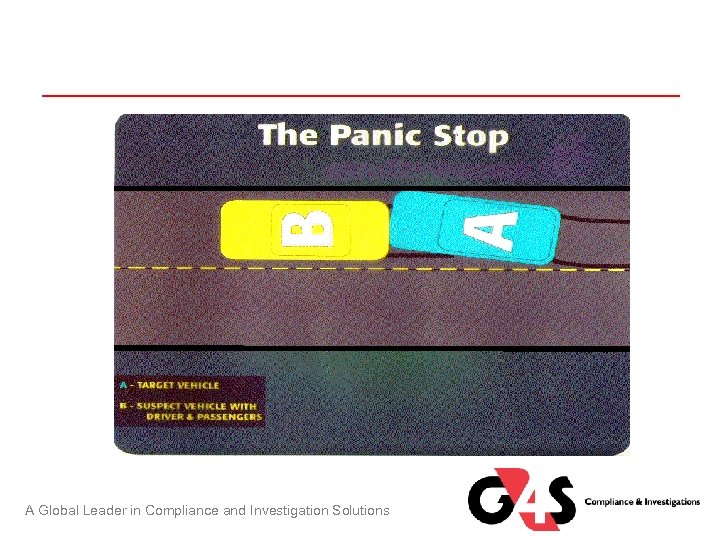 A Global Leader in Compliance and Investigation Solutions
A Global Leader in Compliance and Investigation Solutions
 Video Content – The Panic Stop Click Here to Launch Video A Global Leader in Compliance and Investigation Solutions
Video Content – The Panic Stop Click Here to Launch Video A Global Leader in Compliance and Investigation Solutions
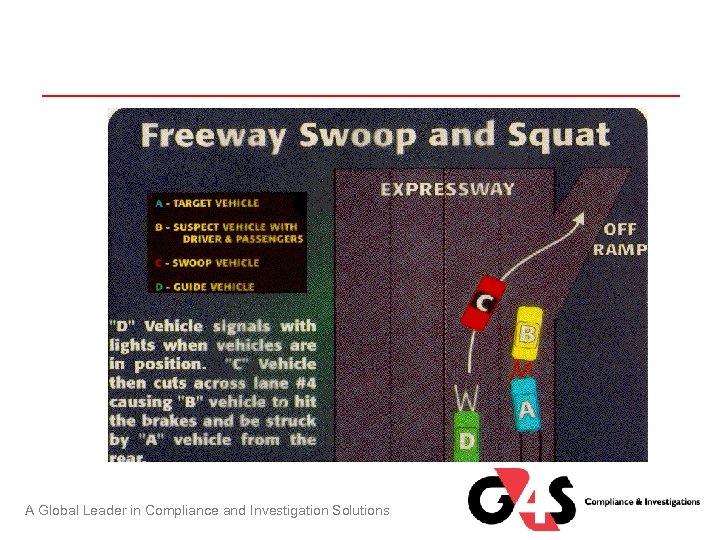 A Global Leader in Compliance and Investigation Solutions
A Global Leader in Compliance and Investigation Solutions
 Video Content – Freeway Swoop & Squat Click Here to Launch Video A Global Leader in Compliance and Investigation Solutions
Video Content – Freeway Swoop & Squat Click Here to Launch Video A Global Leader in Compliance and Investigation Solutions
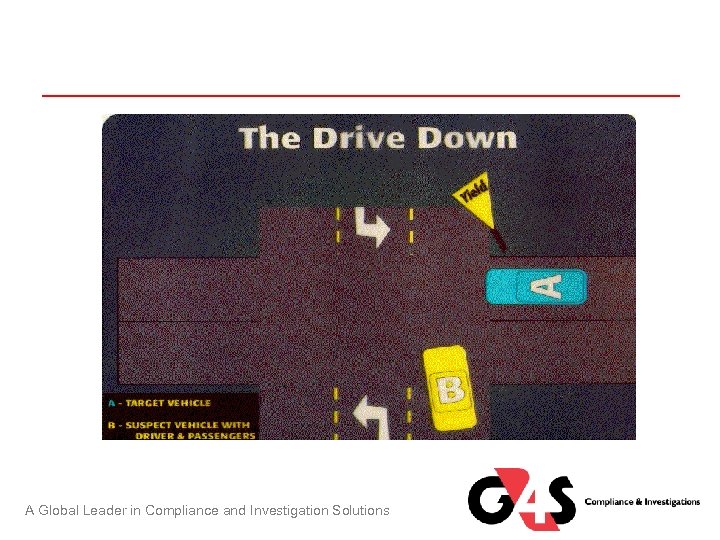 A Global Leader in Compliance and Investigation Solutions
A Global Leader in Compliance and Investigation Solutions
 Video Content – The Drive Down Click Here to Launch Video A Global Leader in Compliance and Investigation Solutions
Video Content – The Drive Down Click Here to Launch Video A Global Leader in Compliance and Investigation Solutions
 Property Fraud Indicators It is important to remember that indicators listed here are merely possible “red flags, ” not actual evidence of fraud. Even the presence of several indicators, while suggestive of possible fraud, does not mean that fraud has definitely been committed. When you have several of these indicators present or a pattern begins to emerge, you should consult with your SIU. A Global Leader in Compliance and Investigation Solutions
Property Fraud Indicators It is important to remember that indicators listed here are merely possible “red flags, ” not actual evidence of fraud. Even the presence of several indicators, while suggestive of possible fraud, does not mean that fraud has definitely been committed. When you have several of these indicators present or a pattern begins to emerge, you should consult with your SIU. A Global Leader in Compliance and Investigation Solutions
 General Indicators of Property Insurance Fraud • Insured is overly pushy for a quick settlement • Insured is unusually knowledgeable regarding insurance terminology and the claims settlement process • Insured handles all business in person, thus avoiding the use of the mail • Insured is willing to accept an inordinately small settlement rather than document all claims losses • Insured contacts agent to verify coverage or extent of coverage just prior to loss date • Insured is recently separated or divorced • Suspiciously coincidental absence of insured or family at the time of the incident A Global Leader in Compliance and Investigation Solutions
General Indicators of Property Insurance Fraud • Insured is overly pushy for a quick settlement • Insured is unusually knowledgeable regarding insurance terminology and the claims settlement process • Insured handles all business in person, thus avoiding the use of the mail • Insured is willing to accept an inordinately small settlement rather than document all claims losses • Insured contacts agent to verify coverage or extent of coverage just prior to loss date • Insured is recently separated or divorced • Suspiciously coincidental absence of insured or family at the time of the incident A Global Leader in Compliance and Investigation Solutions
 General Indicators of Property Insurance Fraud • Losses occur just after coverage takes effect, just before it ceases or just after it has been increased • Losses are incompatible with insured's residence, occupation and/or income • Losses include a large amount of cash • Commercial losses that primarily involve seasonal inventory or equipment, and that occur at the end of the selling season A Global Leader in Compliance and Investigation Solutions
General Indicators of Property Insurance Fraud • Losses occur just after coverage takes effect, just before it ceases or just after it has been increased • Losses are incompatible with insured's residence, occupation and/or income • Losses include a large amount of cash • Commercial losses that primarily involve seasonal inventory or equipment, and that occur at the end of the selling season A Global Leader in Compliance and Investigation Solutions
 Indicators Associated with the Loss Incident • Fire occurs at night, especially after 11 P. M. • Commercial fire occurs on holiday, weekend or when business is closed • Fire department reports fire cause is incendiary, suspicious, or unknown • Fire alarm and/or sprinkler system failed to work at the time of the loss A Global Leader in Compliance and Investigation Solutions
Indicators Associated with the Loss Incident • Fire occurs at night, especially after 11 P. M. • Commercial fire occurs on holiday, weekend or when business is closed • Fire department reports fire cause is incendiary, suspicious, or unknown • Fire alarm and/or sprinkler system failed to work at the time of the loss A Global Leader in Compliance and Investigation Solutions
 Indicators of Burglary/Theft Fraud • Losses include total contents of business/home including items of little or no value • Losses are questionable, e. g. home stereo stolen out of car, fur coat stolen on trip to Hawaii • Losses include numerous family heirlooms • Losses include numerous appraised items and/or items of scheduled property • Extensive commercial losses occur at site where few or no security measures are in effect • No police report or an over-the-counter report in situations where police would normally investigate A Global Leader in Compliance and Investigation Solutions
Indicators of Burglary/Theft Fraud • Losses include total contents of business/home including items of little or no value • Losses are questionable, e. g. home stereo stolen out of car, fur coat stolen on trip to Hawaii • Losses include numerous family heirlooms • Losses include numerous appraised items and/or items of scheduled property • Extensive commercial losses occur at site where few or no security measures are in effect • No police report or an over-the-counter report in situations where police would normally investigate A Global Leader in Compliance and Investigation Solutions
 Indicators of Arson-for-profit of Fire Related Fraud • Building and/or contents were up for sale at the time of the loss • Suspiciously coincidental absence of family pet at time of fire • Insured had loss at the same site within the preceding year. The initial loss, though small, may have been a failed attempt to liquidate contents • Building and/or business was recently purchased • Commercial losses include old or non-saleable inventory or illegal chemicals/materials. Insured or insured's business is experiencing financial difficulties, e. g. bankruptcy, foreclosure • Fire site is claimed by multiple mortgages or chattel mortgages A Global Leader in Compliance and Investigation Solutions
Indicators of Arson-for-profit of Fire Related Fraud • Building and/or contents were up for sale at the time of the loss • Suspiciously coincidental absence of family pet at time of fire • Insured had loss at the same site within the preceding year. The initial loss, though small, may have been a failed attempt to liquidate contents • Building and/or business was recently purchased • Commercial losses include old or non-saleable inventory or illegal chemicals/materials. Insured or insured's business is experiencing financial difficulties, e. g. bankruptcy, foreclosure • Fire site is claimed by multiple mortgages or chattel mortgages A Global Leader in Compliance and Investigation Solutions
 Indicators Associated with the Claims Process • Insured over-documents losses with a receipt for every loss and/or receipts for older items of property • Insured's loss inventory differs significantly from police department's crime report • Insured cannot provide receipts, cancelled checks or other proof of ownership for recently purchased items • Insured provides numerous receipts for inexpensive items, but no receipts for items of significant value • Insured provides receipts with incorrect or no sales tax figures • Insured provides receipts with no store logo (blank receipt) A Global Leader in Compliance and Investigation Solutions
Indicators Associated with the Claims Process • Insured over-documents losses with a receipt for every loss and/or receipts for older items of property • Insured's loss inventory differs significantly from police department's crime report • Insured cannot provide receipts, cancelled checks or other proof of ownership for recently purchased items • Insured provides numerous receipts for inexpensive items, but no receipts for items of significant value • Insured provides receipts with incorrect or no sales tax figures • Insured provides receipts with no store logo (blank receipt) A Global Leader in Compliance and Investigation Solutions
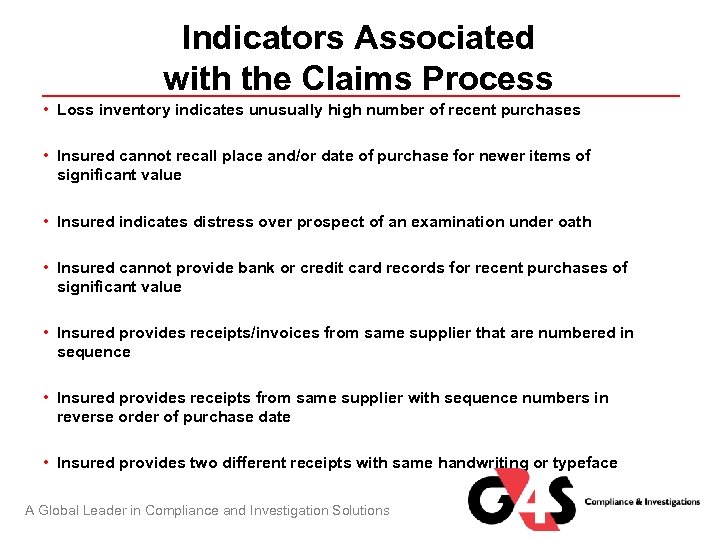 Indicators Associated with the Claims Process • Loss inventory indicates unusually high number of recent purchases • Insured cannot recall place and/or date of purchase for newer items of significant value • Insured indicates distress over prospect of an examination under oath • Insured cannot provide bank or credit card records for recent purchases of significant value • Insured provides receipts/invoices from same supplier that are numbered in sequence • Insured provides receipts from same supplier with sequence numbers in reverse order of purchase date • Insured provides two different receipts with same handwriting or typeface A Global Leader in Compliance and Investigation Solutions
Indicators Associated with the Claims Process • Loss inventory indicates unusually high number of recent purchases • Insured cannot recall place and/or date of purchase for newer items of significant value • Insured indicates distress over prospect of an examination under oath • Insured cannot provide bank or credit card records for recent purchases of significant value • Insured provides receipts/invoices from same supplier that are numbered in sequence • Insured provides receipts from same supplier with sequence numbers in reverse order of purchase date • Insured provides two different receipts with same handwriting or typeface A Global Leader in Compliance and Investigation Solutions
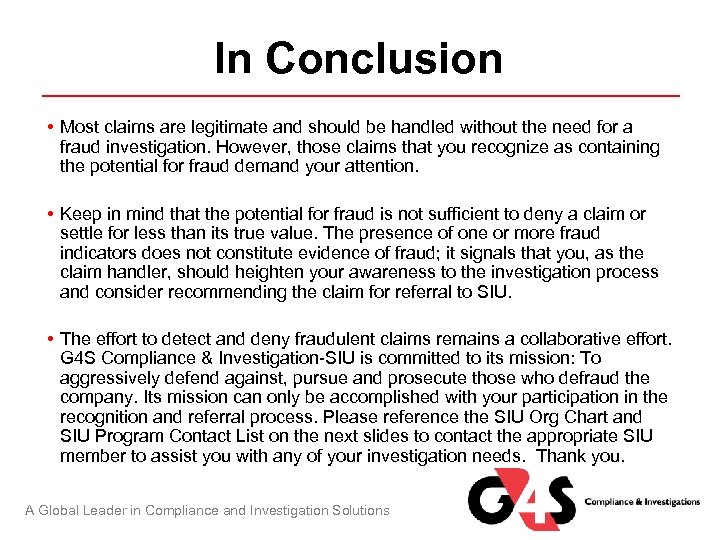 In Conclusion • Most claims are legitimate and should be handled without the need for a fraud investigation. However, those claims that you recognize as containing the potential for fraud demand your attention. • Keep in mind that the potential for fraud is not sufficient to deny a claim or settle for less than its true value. The presence of one or more fraud indicators does not constitute evidence of fraud; it signals that you, as the claim handler, should heighten your awareness to the investigation process and consider recommending the claim for referral to SIU. • The effort to detect and deny fraudulent claims remains a collaborative effort. G 4 S Compliance & Investigation-SIU is committed to its mission: To aggressively defend against, pursue and prosecute those who defraud the company. Its mission can only be accomplished with your participation in the recognition and referral process. Please reference the SIU Org Chart and SIU Program Contact List on the next slides to contact the appropriate SIU member to assist you with any of your investigation needs. Thank you. A Global Leader in Compliance and Investigation Solutions
In Conclusion • Most claims are legitimate and should be handled without the need for a fraud investigation. However, those claims that you recognize as containing the potential for fraud demand your attention. • Keep in mind that the potential for fraud is not sufficient to deny a claim or settle for less than its true value. The presence of one or more fraud indicators does not constitute evidence of fraud; it signals that you, as the claim handler, should heighten your awareness to the investigation process and consider recommending the claim for referral to SIU. • The effort to detect and deny fraudulent claims remains a collaborative effort. G 4 S Compliance & Investigation-SIU is committed to its mission: To aggressively defend against, pursue and prosecute those who defraud the company. Its mission can only be accomplished with your participation in the recognition and referral process. Please reference the SIU Org Chart and SIU Program Contact List on the next slides to contact the appropriate SIU member to assist you with any of your investigation needs. Thank you. A Global Leader in Compliance and Investigation Solutions
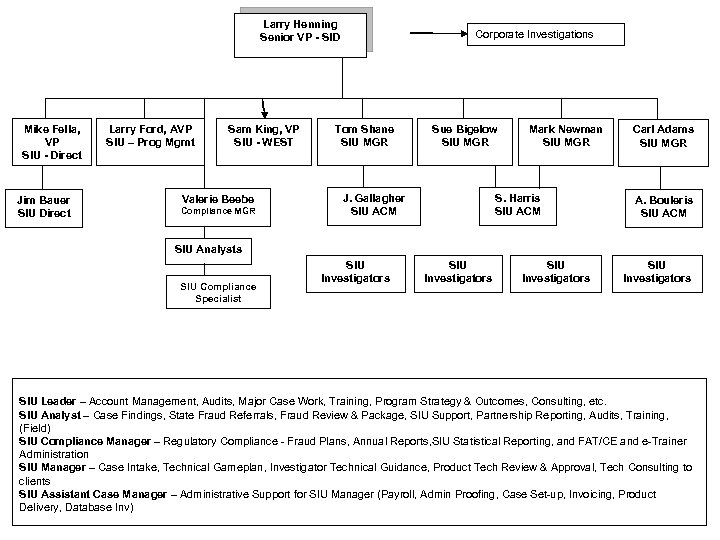 Larry Henning Senior VP - SID Mike Fella, VP SIU - Direct Larry Ford, AVP SIU – Prog Mgmt Jim Bauer SIU Direct Sam King, VP SIU - WEST Valerie Beebe Compliance MGR Corporate Investigations Tom Shane SIU MGR Sue Bigelow SIU MGR J. Gallagher SIU ACM Mark Newman SIU MGR S. Harris SIU ACM Carl Adams SIU MGR A. Bouleris SIU ACM SIU Analysts SIU Compliance Specialist SIU Investigators SIU Leader – Account Management, Audits, Major Case Work, Training, Program Strategy & Outcomes, Consulting, etc. SIU Analyst – Case Findings, State Fraud Referrals, Fraud Review & Package, SIU Support, Partnership Reporting, Audits, Training, (Field) SIU Compliance Manager – Regulatory Compliance - Fraud Plans, Annual Reports, SIU Statistical Reporting, and FAT/CE and e-Trainer Administration SIU Manager – Case Intake, Technical Gameplan, Investigator Technical Guidance, Product Tech Review & Approval, Tech Consulting to clients SIU Assistant Case Manager – Administrative Support for SIU Manager (Payroll, Admin Proofing, Case Set-up, Invoicing, Product Delivery, Database Inv)
Larry Henning Senior VP - SID Mike Fella, VP SIU - Direct Larry Ford, AVP SIU – Prog Mgmt Jim Bauer SIU Direct Sam King, VP SIU - WEST Valerie Beebe Compliance MGR Corporate Investigations Tom Shane SIU MGR Sue Bigelow SIU MGR J. Gallagher SIU ACM Mark Newman SIU MGR S. Harris SIU ACM Carl Adams SIU MGR A. Bouleris SIU ACM SIU Analysts SIU Compliance Specialist SIU Investigators SIU Leader – Account Management, Audits, Major Case Work, Training, Program Strategy & Outcomes, Consulting, etc. SIU Analyst – Case Findings, State Fraud Referrals, Fraud Review & Package, SIU Support, Partnership Reporting, Audits, Training, (Field) SIU Compliance Manager – Regulatory Compliance - Fraud Plans, Annual Reports, SIU Statistical Reporting, and FAT/CE and e-Trainer Administration SIU Manager – Case Intake, Technical Gameplan, Investigator Technical Guidance, Product Tech Review & Approval, Tech Consulting to clients SIU Assistant Case Manager – Administrative Support for SIU Manager (Payroll, Admin Proofing, Case Set-up, Invoicing, Product Delivery, Database Inv)
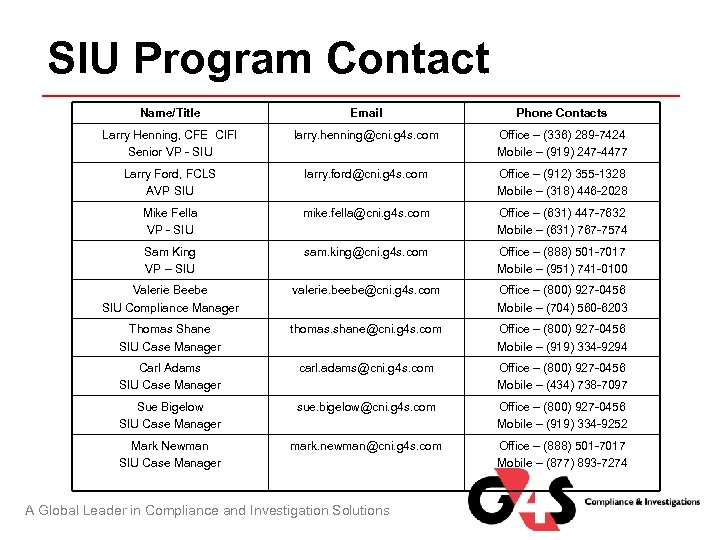 SIU Program Contact Name/Title Email Phone Contacts Larry Henning, CFE CIFI Senior VP - SIU larry. henning@cni. g 4 s. com Office – (336) 289 -7424 Mobile – (919) 247 -4477 Larry Ford, FCLS AVP SIU larry. ford@cni. g 4 s. com Office – (912) 355 -1328 Mobile – (318) 446 -2028 Mike Fella VP - SIU mike. fella@cni. g 4 s. com Office – (631) 447 -7632 Mobile – (631) 767 -7574 Sam King VP – SIU sam. king@cni. g 4 s. com Office – (888) 501 -7017 Mobile – (951) 741 -0100 Valerie Beebe SIU Compliance Manager valerie. beebe@cni. g 4 s. com Office – (800) 927 -0456 Mobile – (704) 560 -6203 Thomas Shane SIU Case Manager thomas. shane@cni. g 4 s. com Office – (800) 927 -0456 Mobile – (919) 334 -9294 Carl Adams SIU Case Manager carl. adams@cni. g 4 s. com Office – (800) 927 -0456 Mobile – (434) 738 -7097 Sue Bigelow SIU Case Manager sue. bigelow@cni. g 4 s. com Office – (800) 927 -0456 Mobile – (919) 334 -9252 Mark Newman SIU Case Manager mark. newman@cni. g 4 s. com Office – (888) 501 -7017 Mobile – (877) 893 -7274 A Global Leader in Compliance and Investigation Solutions
SIU Program Contact Name/Title Email Phone Contacts Larry Henning, CFE CIFI Senior VP - SIU larry. henning@cni. g 4 s. com Office – (336) 289 -7424 Mobile – (919) 247 -4477 Larry Ford, FCLS AVP SIU larry. ford@cni. g 4 s. com Office – (912) 355 -1328 Mobile – (318) 446 -2028 Mike Fella VP - SIU mike. fella@cni. g 4 s. com Office – (631) 447 -7632 Mobile – (631) 767 -7574 Sam King VP – SIU sam. king@cni. g 4 s. com Office – (888) 501 -7017 Mobile – (951) 741 -0100 Valerie Beebe SIU Compliance Manager valerie. beebe@cni. g 4 s. com Office – (800) 927 -0456 Mobile – (704) 560 -6203 Thomas Shane SIU Case Manager thomas. shane@cni. g 4 s. com Office – (800) 927 -0456 Mobile – (919) 334 -9294 Carl Adams SIU Case Manager carl. adams@cni. g 4 s. com Office – (800) 927 -0456 Mobile – (434) 738 -7097 Sue Bigelow SIU Case Manager sue. bigelow@cni. g 4 s. com Office – (800) 927 -0456 Mobile – (919) 334 -9252 Mark Newman SIU Case Manager mark. newman@cni. g 4 s. com Office – (888) 501 -7017 Mobile – (877) 893 -7274 A Global Leader in Compliance and Investigation Solutions


