0a7320eeb3638c558cdb8241265dd9b3.ppt
- Количество слайдов: 69
 2010 Annual Conference
2010 Annual Conference
 CDI in 2010: Spotlight on Compliance Gloryanne Bryant, RHIA, RHIT, CCS, CCDS Catherine O’Leary, RN, BSN
CDI in 2010: Spotlight on Compliance Gloryanne Bryant, RHIA, RHIT, CCS, CCDS Catherine O’Leary, RN, BSN
 AHIMA CDI Practice Brief Gloryanne Bryant, RHIA, RHIT, CCS, CCDS
AHIMA CDI Practice Brief Gloryanne Bryant, RHIA, RHIT, CCS, CCDS
 Goals/Objectives • • Background on AHIMA CDI Practice Brief High-Level Overview of CDI Practice Brief Key Takeaways from the Practice Brief Compliance and Risk in CDI
Goals/Objectives • • Background on AHIMA CDI Practice Brief High-Level Overview of CDI Practice Brief Key Takeaways from the Practice Brief Compliance and Risk in CDI
 Background—AHIMA CDI Work Group • Early 2009 AHIMA made the decision to form a CDI Work Group due to increasing requests from members and nonmembers to have more guidance regarding CDI – Kathy De. Vault, RHIA, CCS-P • Reached out to 30 individuals across the United States in a variety of roles and professions. – Physicians – Registered Nurses – HIM professionals: RHIA, RHIT, CCS
Background—AHIMA CDI Work Group • Early 2009 AHIMA made the decision to form a CDI Work Group due to increasing requests from members and nonmembers to have more guidance regarding CDI – Kathy De. Vault, RHIA, CCS-P • Reached out to 30 individuals across the United States in a variety of roles and professions. – Physicians – Registered Nurses – HIM professionals: RHIA, RHIT, CCS
 Background—AHIMA CDI Work Group (cont. ) • AHIMA asked Gail Garrett, RHIT, and Gloryanne Bryant, RHIA, RHIT, CCS, CCDS, to be the cochairs of the Work Group • The work group would function via “conference calls” and e-mail communications • A 30 -member work group determined the goals, tasks, and functions of the work group – AHIMA CDI Brochure – CDI Practice Brief – CDI Template Job Descriptions – CDI Template Physician Liaison/Champion – CDI Tool Kit • Sample Query/Clarification Forms • CDI tracking tools • P&P – CDI Ethical Standards – Need for a CDI AHIMA credential or certification
Background—AHIMA CDI Work Group (cont. ) • AHIMA asked Gail Garrett, RHIT, and Gloryanne Bryant, RHIA, RHIT, CCS, CCDS, to be the cochairs of the Work Group • The work group would function via “conference calls” and e-mail communications • A 30 -member work group determined the goals, tasks, and functions of the work group – AHIMA CDI Brochure – CDI Practice Brief – CDI Template Job Descriptions – CDI Template Physician Liaison/Champion – CDI Tool Kit • Sample Query/Clarification Forms • CDI tracking tools • P&P – CDI Ethical Standards – Need for a CDI AHIMA credential or certification
 AHIMA CDI Practice Brief Subgroup • A group of volunteers was formed: – Gloryanne Bryant, * RHIA, CCS, CCDS – Kathy De. Vault, RHIA, CCS-P – Cheryl Ericson, MS, RN – Gail Garrett, RHIT – William Haik*, MD, FCCP – Robin Holmes*, MSN, RN – Eve-Ellen Mandler, MS, RHIA, CCS * ACDIS advisory board member
AHIMA CDI Practice Brief Subgroup • A group of volunteers was formed: – Gloryanne Bryant, * RHIA, CCS, CCDS – Kathy De. Vault, RHIA, CCS-P – Cheryl Ericson, MS, RN – Gail Garrett, RHIT – William Haik*, MD, FCCP – Robin Holmes*, MSN, RN – Eve-Ellen Mandler, MS, RHIA, CCS * ACDIS advisory board member
 CDI Practice Brief Overview • Introduction and background • Policies and Procedures – Appendix B: Examples of Policies and Procedures • • • Roles, Competencies, and Staffing Models Physician Advisor Query Process CDI QA Process Query Retention Leading vs. Nonleading Queries
CDI Practice Brief Overview • Introduction and background • Policies and Procedures – Appendix B: Examples of Policies and Procedures • • • Roles, Competencies, and Staffing Models Physician Advisor Query Process CDI QA Process Query Retention Leading vs. Nonleading Queries
 CDI Practice Brief Overview • The guidance does not replace the 2008 AHIMA practice brief “Managing an Effective Query Process. ” It is, however, intended to provide greater specificity and detail related to CDI programs. • The most vital role of a CDI program is facilitating an accurate representation of healthcare services through complete and accurate reporting of diagnoses and procedures. • A successful CDI program can have an impact on CMS quality measures, present on admission, pay for performance, value-based purchasing, data used for decision-making in healthcare reform, and other national reporting initiatives that require the specificity of clinical documentation. • Improving the accuracy of clinical documentation can reduce compliance risks, minimize a healthcare facility’s vulnerability during external audits, and provide insight into legal quality of care issues.
CDI Practice Brief Overview • The guidance does not replace the 2008 AHIMA practice brief “Managing an Effective Query Process. ” It is, however, intended to provide greater specificity and detail related to CDI programs. • The most vital role of a CDI program is facilitating an accurate representation of healthcare services through complete and accurate reporting of diagnoses and procedures. • A successful CDI program can have an impact on CMS quality measures, present on admission, pay for performance, value-based purchasing, data used for decision-making in healthcare reform, and other national reporting initiatives that require the specificity of clinical documentation. • Improving the accuracy of clinical documentation can reduce compliance risks, minimize a healthcare facility’s vulnerability during external audits, and provide insight into legal quality of care issues.
 CDI Practice Brief Overview (cont. ) • CDI department must be governed by written policies and procedures. These policies and procedures should be developed with the assistance of other departments affected by clinical documentation, including compliance, case management, and HIM. • CDI policies can include (but are not limited to) education, experience, and credentials for hiring CDI professionals; initial orientation and training; ongoing education and training; compliant query practices; and a CDI quality assurance process.
CDI Practice Brief Overview (cont. ) • CDI department must be governed by written policies and procedures. These policies and procedures should be developed with the assistance of other departments affected by clinical documentation, including compliance, case management, and HIM. • CDI policies can include (but are not limited to) education, experience, and credentials for hiring CDI professionals; initial orientation and training; ongoing education and training; compliant query practices; and a CDI quality assurance process.
 CDI Practice Brief Overview (cont. ) • Roles, Competencies, and Staffing Models • CDI professionals can help providers achieve complete and accurate documentation by: – Facilitating and obtaining appropriate provider documentation within the health record for clinical conditions and treatment required for accurate representation of severity of illness, expected risk of mortality, and complexity of care of the patient – Exhibiting thorough knowledge of clinical documentation requirements as they relate to the classification systems, MS-DRG assignment, and clinical conditions and treatment needs of the patient population – Educating members of the patient care team and others regarding documentation guidelines
CDI Practice Brief Overview (cont. ) • Roles, Competencies, and Staffing Models • CDI professionals can help providers achieve complete and accurate documentation by: – Facilitating and obtaining appropriate provider documentation within the health record for clinical conditions and treatment required for accurate representation of severity of illness, expected risk of mortality, and complexity of care of the patient – Exhibiting thorough knowledge of clinical documentation requirements as they relate to the classification systems, MS-DRG assignment, and clinical conditions and treatment needs of the patient population – Educating members of the patient care team and others regarding documentation guidelines
 CDI Practice Brief Overview (cont. ) • Those who typically fill CDI roles include, but are not limited to, HIM professionals, nurses, physicians, and other healthcare professionals with a clinical or coding background. It is recommended that healthcare entities employ, educate, and train qualified individuals to perform the CDI role. • Key skills and competencies for those in CDI roles include: – Knowledge of coding concepts and guidelines and clinical – – terminology Ability to read analyze all information in a patient’s health record Clinical knowledge (anatomy and physiology, pathophysiology, and pharmacology) Ability to establish and maintain strong verbal and written communication with providers and other clinicians Knowledge of healthcare regulations, including reimbursement and documentation requirements
CDI Practice Brief Overview (cont. ) • Those who typically fill CDI roles include, but are not limited to, HIM professionals, nurses, physicians, and other healthcare professionals with a clinical or coding background. It is recommended that healthcare entities employ, educate, and train qualified individuals to perform the CDI role. • Key skills and competencies for those in CDI roles include: – Knowledge of coding concepts and guidelines and clinical – – terminology Ability to read analyze all information in a patient’s health record Clinical knowledge (anatomy and physiology, pathophysiology, and pharmacology) Ability to establish and maintain strong verbal and written communication with providers and other clinicians Knowledge of healthcare regulations, including reimbursement and documentation requirements
 CDI Practice Brief Overview (cont. ) • Organizations can staff their CDI programs using one of two general models: – Single Discipline Models – Hybrid Models • The program may be staffed with one or more healthcare disciplines (e. g. , HIM professionals, registered nurses, or other clinical staff). Factors that may influence an organization’s choice include patient volume, availability of qualified staff, and staff compensation. • A strong consideration for the staffing model is the inclusion of a physician advisor. – “Champion or Liaison”
CDI Practice Brief Overview (cont. ) • Organizations can staff their CDI programs using one of two general models: – Single Discipline Models – Hybrid Models • The program may be staffed with one or more healthcare disciplines (e. g. , HIM professionals, registered nurses, or other clinical staff). Factors that may influence an organization’s choice include patient volume, availability of qualified staff, and staff compensation. • A strong consideration for the staffing model is the inclusion of a physician advisor. – “Champion or Liaison”
 CDI Practice Brief Overview (cont. ) • Query Process: The CDI process is provider communication. Prior to CDI programs, the query process was the responsibility of HIM professionals; however, depending on the staffing model, the CDI professional either shares the query role with HIM professionals or assumes complete responsibility. • A query is a routine communication and education tool used to advocate complete and compliant documentation. Although AHIMA refers to this communication to providers as a “query, ” CDI programs may use different names, such as clinical clarification, documentation alerts, and documentation clarification. Regardless of what the communication is called, the query should adhere to the guidance outlined in the 2008 practice brief “Managing an Effective Query Process” and this current practice brief.
CDI Practice Brief Overview (cont. ) • Query Process: The CDI process is provider communication. Prior to CDI programs, the query process was the responsibility of HIM professionals; however, depending on the staffing model, the CDI professional either shares the query role with HIM professionals or assumes complete responsibility. • A query is a routine communication and education tool used to advocate complete and compliant documentation. Although AHIMA refers to this communication to providers as a “query, ” CDI programs may use different names, such as clinical clarification, documentation alerts, and documentation clarification. Regardless of what the communication is called, the query should adhere to the guidance outlined in the 2008 practice brief “Managing an Effective Query Process” and this current practice brief.
 CDI Practice Brief Overview (cont. ) • Written, Template, and Verbal Queries • Ensuring all queries contain consistent information (e. g. , patient name, admission date, and medical record number) is an advantage of written queries; however, using templated queries by condition could be problematic if they do not provide patient-specific clinical indicators • Organizations require a clear procedure on addressing open queries, which should include how to deal with a lack of response by the provider and how to address a response on the query form instead of the health record
CDI Practice Brief Overview (cont. ) • Written, Template, and Verbal Queries • Ensuring all queries contain consistent information (e. g. , patient name, admission date, and medical record number) is an advantage of written queries; however, using templated queries by condition could be problematic if they do not provide patient-specific clinical indicators • Organizations require a clear procedure on addressing open queries, which should include how to deal with a lack of response by the provider and how to address a response on the query form instead of the health record
 CDI Practice Brief Overview (cont. ) • Leading vs. Nonleading Queries • Nonleading applies to ALL CDI professionals and staff • Queries may take many forms, but they are never intended to lead the provider to one desired outcome. The following examples emphasize the difference between leading and nonleading queries. – Clarification for Specificity of a Diagnosis – Clarification of a Missing or Vague Diagnosis • Appendix – Checklist for Written and Verbal Queries • Query Retention – The query should be retained indefinitely if it contains information not documented in the health record. Auditors may request copies of any queries in order to validate the query wording, even if they are not considered part of the legal medical record.
CDI Practice Brief Overview (cont. ) • Leading vs. Nonleading Queries • Nonleading applies to ALL CDI professionals and staff • Queries may take many forms, but they are never intended to lead the provider to one desired outcome. The following examples emphasize the difference between leading and nonleading queries. – Clarification for Specificity of a Diagnosis – Clarification of a Missing or Vague Diagnosis • Appendix – Checklist for Written and Verbal Queries • Query Retention – The query should be retained indefinitely if it contains information not documented in the health record. Auditors may request copies of any queries in order to validate the query wording, even if they are not considered part of the legal medical record.
 CDI Practice Brief Overview (cont. ) • CDI QA should be included in your CDI program • A QA process of written and verbal queries, including: – Who will monitor the written queries – How many queries will be reviewed for compliance and how often – The feedback and corrective action needed, including who will take corrective action and when • Establish what your reporting documents for CDI QA processes will be
CDI Practice Brief Overview (cont. ) • CDI QA should be included in your CDI program • A QA process of written and verbal queries, including: – Who will monitor the written queries – How many queries will be reviewed for compliance and how often – The feedback and corrective action needed, including who will take corrective action and when • Establish what your reporting documents for CDI QA processes will be
 Key Takeaways • CDI Goals • Policies and Procedures • Those who typically fill CDI roles include, but are not limited to, HIM professionals, nurses, physicians, and other healthcare professionals with a clinical or coding background. • Competencies • Staffing Models—vary • CDI Physician Advisor/Liaison or Champion is needed • Query Process: Although AHIMA refers to this communication to providers as a “query, ” CDI programs may use different names, such as clinical clarification, documentation alerts, and documentation clarification. Regardless of what the communication is called, the query should adhere to the guidance outlined in the 2008 practice brief “Managing an Effective Query Process” and this current practice brief. • Leading vs. Nonleading Queries
Key Takeaways • CDI Goals • Policies and Procedures • Those who typically fill CDI roles include, but are not limited to, HIM professionals, nurses, physicians, and other healthcare professionals with a clinical or coding background. • Competencies • Staffing Models—vary • CDI Physician Advisor/Liaison or Champion is needed • Query Process: Although AHIMA refers to this communication to providers as a “query, ” CDI programs may use different names, such as clinical clarification, documentation alerts, and documentation clarification. Regardless of what the communication is called, the query should adhere to the guidance outlined in the 2008 practice brief “Managing an Effective Query Process” and this current practice brief. • Leading vs. Nonleading Queries
 Practice Brief Appendixes • Appendix A: Checklist for Written and Verbal Queries • Appendix B: Policies and Procedures • Appendix C: Examples of Leading and Nonleading Queries
Practice Brief Appendixes • Appendix A: Checklist for Written and Verbal Queries • Appendix B: Policies and Procedures • Appendix C: Examples of Leading and Nonleading Queries
 Practice Brief Appendix A • Checklist for Written and Verbal Queries • WRITTEN QUERIES SHOULD contain standard documentation with precise language and identification of clinical indicators necessary for appropriate provider response. – Organizations should outline the following processes for written and verbal queries. • Verbal Queries • Organizations should outline the following procedures for verbal queries
Practice Brief Appendix A • Checklist for Written and Verbal Queries • WRITTEN QUERIES SHOULD contain standard documentation with precise language and identification of clinical indicators necessary for appropriate provider response. – Organizations should outline the following processes for written and verbal queries. • Verbal Queries • Organizations should outline the following procedures for verbal queries
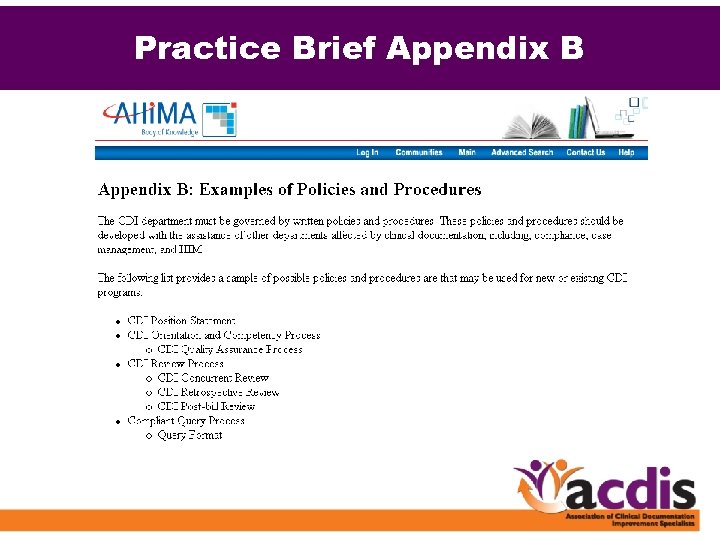 Practice Brief Appendix B
Practice Brief Appendix B
 Practice Brief Appendix C
Practice Brief Appendix C
 Practice Brief Appendix C • Four examples included: – Clarification for Specificity of a Diagnosis • Congestive Heart Failure – Clarification for Specificity of a Diagnosis • Anemia – Clarification of a Missing or Vague Diagnosis • Infectious Dx – Physician Query for Urosepsis
Practice Brief Appendix C • Four examples included: – Clarification for Specificity of a Diagnosis • Congestive Heart Failure – Clarification for Specificity of a Diagnosis • Anemia – Clarification of a Missing or Vague Diagnosis • Infectious Dx – Physician Query for Urosepsis
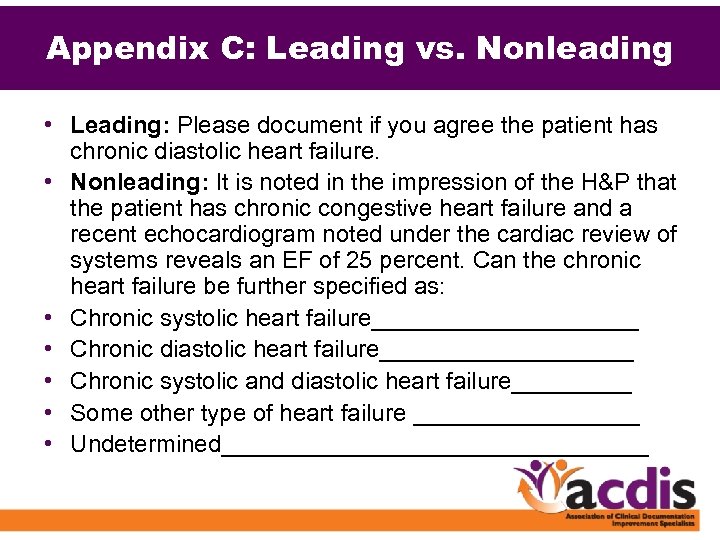 Appendix C: Leading vs. Nonleading • Leading: Please document if you agree the patient has • • • chronic diastolic heart failure. Nonleading: It is noted in the impression of the H&P that the patient has chronic congestive heart failure and a recent echocardiogram noted under the cardiac review of systems reveals an EF of 25 percent. Can the chronic heart failure be further specified as: Chronic systolic heart failure__________ Chronic diastolic heart failure__________ Chronic systolic and diastolic heart failure_____ Some other type of heart failure _________ Undetermined________________
Appendix C: Leading vs. Nonleading • Leading: Please document if you agree the patient has • • • chronic diastolic heart failure. Nonleading: It is noted in the impression of the H&P that the patient has chronic congestive heart failure and a recent echocardiogram noted under the cardiac review of systems reveals an EF of 25 percent. Can the chronic heart failure be further specified as: Chronic systolic heart failure__________ Chronic diastolic heart failure__________ Chronic systolic and diastolic heart failure_____ Some other type of heart failure _________ Undetermined________________
 Compliance and Risk • Ethical standards • The issues around “leading” queries and/or clarifications increases • Bayview Hospital (Maryland) case—attend Dr. Kennedy’s session to learn more – Recognize what constitutes a “clinically appropriate query” • CDI can not … lead the physician to a diagnosis or diagnose for the physician
Compliance and Risk • Ethical standards • The issues around “leading” queries and/or clarifications increases • Bayview Hospital (Maryland) case—attend Dr. Kennedy’s session to learn more – Recognize what constitutes a “clinically appropriate query” • CDI can not … lead the physician to a diagnosis or diagnose for the physician
 Summary • Establish CDI goals – Quality, accuracy, patient safety and care – Appropriate reimbursement will follow • Determine the staffing models and competencies needed • Include a Physician Advisor in your CDI program • Develop a “Query Process” that includes follow-through • CDI QA—process and monitoring – Compliance
Summary • Establish CDI goals – Quality, accuracy, patient safety and care – Appropriate reimbursement will follow • Determine the staffing models and competencies needed • Include a Physician Advisor in your CDI program • Develop a “Query Process” that includes follow-through • CDI QA—process and monitoring – Compliance
 Summary • Two additional appendixes are included in the online version of this brief, available in the AHIMA Body of Knowledge at www. ahima. org: – Appendix B: Examples of Policies and Procedures – Appendix C: Examples of Leading and Nonleading Queries
Summary • Two additional appendixes are included in the online version of this brief, available in the AHIMA Body of Knowledge at www. ahima. org: – Appendix B: Examples of Policies and Procedures – Appendix C: Examples of Leading and Nonleading Queries
 References/Resources • AHIMA Practice Brief: “Guidance for Clinical Documentation Improvement Programs. ” Journal of AHIMA 81, no. 5 (May 2010): 45 -50.
References/Resources • AHIMA Practice Brief: “Guidance for Clinical Documentation Improvement Programs. ” Journal of AHIMA 81, no. 5 (May 2010): 45 -50.
 2010 Annual Conference
2010 Annual Conference
 Compliance and the CDI Team Making Sense of The New Integrity Auditors: RAC, MIC, and ZPIC Catherine O’Leary, RN, BSN
Compliance and the CDI Team Making Sense of The New Integrity Auditors: RAC, MIC, and ZPIC Catherine O’Leary, RN, BSN
 Objectives • Define “Integrity” • Provide Update on the Permanent RAC • Review the New Integrity Contractors: – Medicare Administrative Contractors (MAC) – Medicaid Integrity Contractors (MIC) – Zone Program Integrity Contractors (ZPIC) • Identify the role of the CDI Team
Objectives • Define “Integrity” • Provide Update on the Permanent RAC • Review the New Integrity Contractors: – Medicare Administrative Contractors (MAC) – Medicaid Integrity Contractors (MIC) – Zone Program Integrity Contractors (ZPIC) • Identify the role of the CDI Team
 “Integrity” According to Your. Dictionary. com • Integrity is defined as: – The quality or state of being complete; unbroken condition; wholeness; entirety – The quality or state of being unimpaired; perfect condition; soundness – The quality or state of being of sound moral principle; uprightness, honesty, and sincerity
“Integrity” According to Your. Dictionary. com • Integrity is defined as: – The quality or state of being complete; unbroken condition; wholeness; entirety – The quality or state of being unimpaired; perfect condition; soundness – The quality or state of being of sound moral principle; uprightness, honesty, and sincerity
 CMS Defines—“integrity” “We do not believe there is anything inappropriate, unethical or otherwise wrong with hospitals taking full advantage of coding opportunities to maximize Medicare payment that is supported by documentation in the medical record. ”… “We encourage hospitals to engage in complete and accurate coding. ” • Direct quote, CMS 2008 IPPS Final Rule, http: //www. cms. hhs. gov/Acute. Inpatient. PPS/ downloads/CMS-1533 -FC. pdf, p. 208.
CMS Defines—“integrity” “We do not believe there is anything inappropriate, unethical or otherwise wrong with hospitals taking full advantage of coding opportunities to maximize Medicare payment that is supported by documentation in the medical record. ”… “We encourage hospitals to engage in complete and accurate coding. ” • Direct quote, CMS 2008 IPPS Final Rule, http: //www. cms. hhs. gov/Acute. Inpatient. PPS/ downloads/CMS-1533 -FC. pdf, p. 208.
 Integrity vs. “Fraud and Abuse” In 1999, the Department of Health and Human Services’ (HHS) Office of Inspector General (OIG) estimated that erroneous and fraudulent claims cost Medicare $13. 5 billion (7. 97% of total Medicare fee-for -service benefit payments). Although this was significantly less than the OIG's 1996 estimate of $23. 2 billion, it showed that improper payments are still a major problem for Medicare and provided the government with ample reason to continue its wellpublicized fight against fraud. REFERENCES: Department of Health and Human Services' Office of Inspector General. Statement for the Record to the House Budget Committee Health Care Task Force: Medicare Program — Reducing Improper Payments & Fraud. Available at: www. hhs. gov/oig/testimony/00712 fin. htm.
Integrity vs. “Fraud and Abuse” In 1999, the Department of Health and Human Services’ (HHS) Office of Inspector General (OIG) estimated that erroneous and fraudulent claims cost Medicare $13. 5 billion (7. 97% of total Medicare fee-for -service benefit payments). Although this was significantly less than the OIG's 1996 estimate of $23. 2 billion, it showed that improper payments are still a major problem for Medicare and provided the government with ample reason to continue its wellpublicized fight against fraud. REFERENCES: Department of Health and Human Services' Office of Inspector General. Statement for the Record to the House Budget Committee Health Care Task Force: Medicare Program — Reducing Improper Payments & Fraud. Available at: www. hhs. gov/oig/testimony/00712 fin. htm.
 But … Who’s Monitoring “Integrity”? • • • QIOs RACs MICs ZPICs Third-party payers State agencies OIG ? ?
But … Who’s Monitoring “Integrity”? • • • QIOs RACs MICs ZPICs Third-party payers State agencies OIG ? ?
 Recovery Audit Contractor (RAC) • RAC Pilot conducted for three (3) years in New York, Florida, and California • Tax Relief & Health Care Act of 2006, Section 302 made RAC Permanent with expansion to all 50 states by 2010 • RAC recouped > $1. 03 B in improper payments 96% overpayments + 4% underpayments to providers
Recovery Audit Contractor (RAC) • RAC Pilot conducted for three (3) years in New York, Florida, and California • Tax Relief & Health Care Act of 2006, Section 302 made RAC Permanent with expansion to all 50 states by 2010 • RAC recouped > $1. 03 B in improper payments 96% overpayments + 4% underpayments to providers
 The Purpose of RAC • To detect and “correct” past improper payments • To implement actions (such as education) to prevent future improper payments • To lower CMS “error rate” • To protect the tax payer and the future of Medicare
The Purpose of RAC • To detect and “correct” past improper payments • To implement actions (such as education) to prevent future improper payments • To lower CMS “error rate” • To protect the tax payer and the future of Medicare
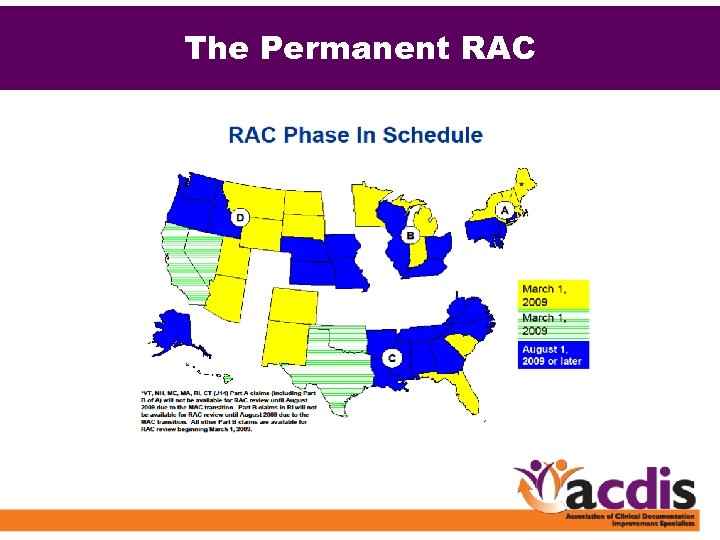 The Permanent RAC
The Permanent RAC
 The Permanent RAC: Regions • Region A: Diversified Collection Services (DCS) – www. dcsrac. com (Provider Portal/Issues Under Review) • Region B: CGI Federal – http: //racb. cgi. com (Issues) • Region C: Connolly Healthcare – www. connollyhealthcare. com/RAC (Approved Issues) • Region D: Health. Data. Insights (HDI) – https: //racinfo. healthdatainsights. com (New Issues)
The Permanent RAC: Regions • Region A: Diversified Collection Services (DCS) – www. dcsrac. com (Provider Portal/Issues Under Review) • Region B: CGI Federal – http: //racb. cgi. com (Issues) • Region C: Connolly Healthcare – www. connollyhealthcare. com/RAC (Approved Issues) • Region D: Health. Data. Insights (HDI) – https: //racinfo. healthdatainsights. com (New Issues)
 Recent Updates to the RAC—Reviews • Provider outreach has occurred in every state by • • the Regional RACs Automated Review is in progress in all 50 states DRG Validation—complex reviews are in progress—timing has varied by region DME Medical Necessity Reviews—complex review (calendar year 2010)
Recent Updates to the RAC—Reviews • Provider outreach has occurred in every state by • • the Regional RACs Automated Review is in progress in all 50 states DRG Validation—complex reviews are in progress—timing has varied by region DME Medical Necessity Reviews—complex review (calendar year 2010)
 Recent Updates to the RAC—Limits • Institutional Providers: 1% of Medicare claims submitted for the previous calendar year (2008), divided into eight periods (45 days) – Based on Tax ID Number and ZIP code • Professional services and DMEPOS suppliers limits have not yet been established • Two Caps will exist in FY 2010 through March 2010, the cap will remain at 200 ADRs per 45 days for all providers/suppliers • From April through September 2010, providers/suppliers who bill in excess of 100, 000 claims to Medicare (per TIN) will have a cap of 300 ADRs per 45 days
Recent Updates to the RAC—Limits • Institutional Providers: 1% of Medicare claims submitted for the previous calendar year (2008), divided into eight periods (45 days) – Based on Tax ID Number and ZIP code • Professional services and DMEPOS suppliers limits have not yet been established • Two Caps will exist in FY 2010 through March 2010, the cap will remain at 200 ADRs per 45 days for all providers/suppliers • From April through September 2010, providers/suppliers who bill in excess of 100, 000 claims to Medicare (per TIN) will have a cap of 300 ADRs per 45 days
 RACs vs. MACs • So … the RACs have caught our attention and we are prepared with RAC teams and RAC tracking tools and RAC appeals processes … • Why are we not more concerned or prepared with the MACs? Are they the same or significantly different from the RACs? Won’t our RAC team suffice?
RACs vs. MACs • So … the RACs have caught our attention and we are prepared with RAC teams and RAC tracking tools and RAC appeals processes … • Why are we not more concerned or prepared with the MACs? Are they the same or significantly different from the RACs? Won’t our RAC team suffice?
 Medicare Audit Contractors (MAC) • Section 1874 A of the Social Security Act establishes the MAC authority • 23 MACs will serve as the providers' primary point of contact for the receipt, processing, and payment of claims • They will also perform all core claims processing operations for both Parts A and B
Medicare Audit Contractors (MAC) • Section 1874 A of the Social Security Act establishes the MAC authority • 23 MACs will serve as the providers' primary point of contact for the receipt, processing, and payment of claims • They will also perform all core claims processing operations for both Parts A and B
 The Purpose of the MAC • A single claims processing interface between Part A and Part B claims • A more consistent process to accurately address all Medicare claims and payment decisions • Increase the accuracy of claims payments and ensure data integrity
The Purpose of the MAC • A single claims processing interface between Part A and Part B claims • A more consistent process to accurately address all Medicare claims and payment decisions • Increase the accuracy of claims payments and ensure data integrity
 23 MACs will include • 15 to process both Part A and Part B claims (A/B MACs) • Four to process DME claims (DME MACs) • Four to process Home Health & Hospice (HH) claims (HH MACs)
23 MACs will include • 15 to process both Part A and Part B claims (A/B MACs) • Four to process DME claims (DME MACs) • Four to process Home Health & Hospice (HH) claims (HH MACs)
 A MAC Fact— Simultaneous Requests • MACs can request documentation from a third party (a physician office, for example) while simultaneously requesting information from a billing provider or supplier – If neither party responds within 45 days, the MAC may deny the claim in part or in full – Therefore, the payment of the claim is dependent on both parties responding
A MAC Fact— Simultaneous Requests • MACs can request documentation from a third party (a physician office, for example) while simultaneously requesting information from a billing provider or supplier – If neither party responds within 45 days, the MAC may deny the claim in part or in full – Therefore, the payment of the claim is dependent on both parties responding
 MACs: Part A AND Part B • The challenge for CDI teams—there has been no alignment between physicians and hospital billing, payment, etc. – The documentation is “in the chart. ” – “I don’t really care about MS-DRGs, they have nothing to do with me!” – “I get paid whether the patient is an inpatient or in an observation bed. ”
MACs: Part A AND Part B • The challenge for CDI teams—there has been no alignment between physicians and hospital billing, payment, etc. – The documentation is “in the chart. ” – “I don’t really care about MS-DRGs, they have nothing to do with me!” – “I get paid whether the patient is an inpatient or in an observation bed. ”
 MACs: Part A AND Part B • Is the ALARM going off now for all providers, including the physicians? ? ? • Do they see the “link” between their documentation and billing/coding integrity?
MACs: Part A AND Part B • Is the ALARM going off now for all providers, including the physicians? ? ? • Do they see the “link” between their documentation and billing/coding integrity?
 MACs: Part A AND Part B • Reminds us that this increased scrutiny is for any provider that bills Medicare fee- for-service such as: – Hospitals – Physicians – Durable Medical Equipment suppliers – Pharmacies – Rehab facilities, SNFs, Home Health – Outpatient, etc.
MACs: Part A AND Part B • Reminds us that this increased scrutiny is for any provider that bills Medicare fee- for-service such as: – Hospitals – Physicians – Durable Medical Equipment suppliers – Pharmacies – Rehab facilities, SNFs, Home Health – Outpatient, etc.
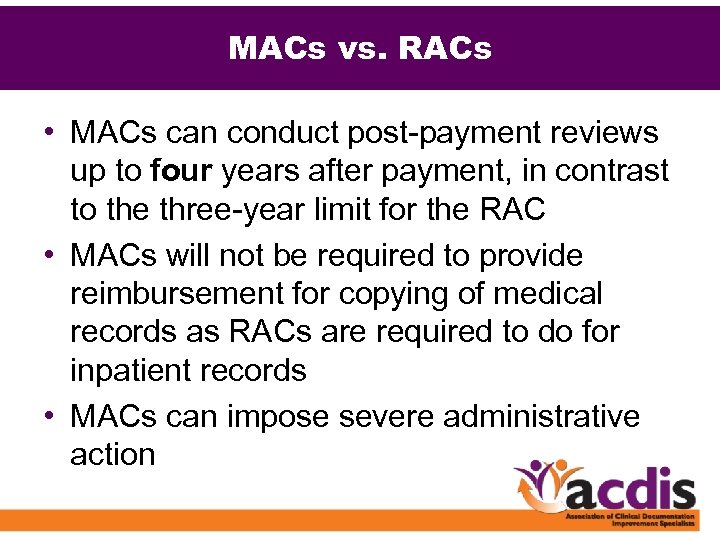 MACs vs. RACs • MACs can conduct post-payment reviews up to four years after payment, in contrast to the three-year limit for the RAC • MACs will not be required to provide reimbursement for copying of medical records as RACs are required to do for inpatient records • MACs can impose severe administrative action
MACs vs. RACs • MACs can conduct post-payment reviews up to four years after payment, in contrast to the three-year limit for the RAC • MACs will not be required to provide reimbursement for copying of medical records as RACs are required to do for inpatient records • MACs can impose severe administrative action
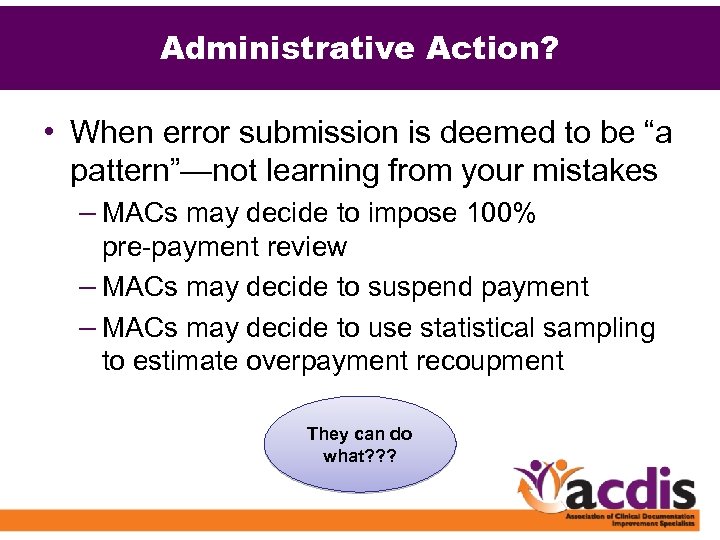 Administrative Action? • When error submission is deemed to be “a pattern”—not learning from your mistakes – MACs may decide to impose 100% pre-payment review – MACs may decide to suspend payment – MACs may decide to use statistical sampling to estimate overpayment recoupment They can do what? ? ?
Administrative Action? • When error submission is deemed to be “a pattern”—not learning from your mistakes – MACs may decide to impose 100% pre-payment review – MACs may decide to suspend payment – MACs may decide to use statistical sampling to estimate overpayment recoupment They can do what? ? ?
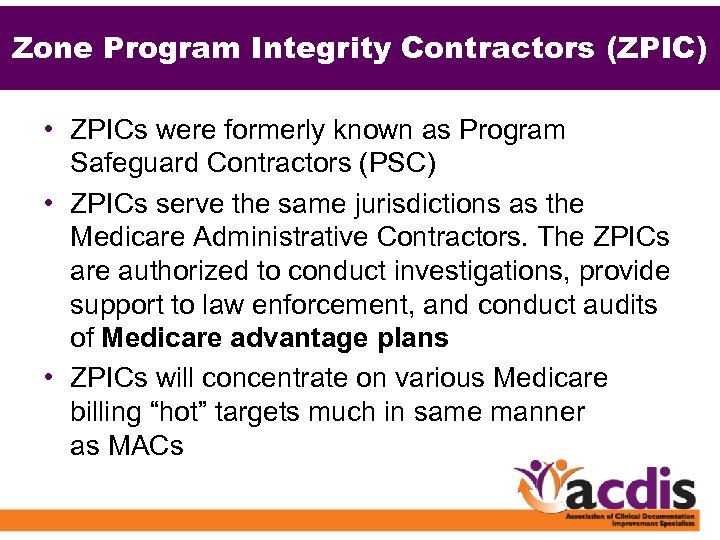 Zone Program Integrity Contractors (ZPIC) • ZPICs were formerly known as Program Safeguard Contractors (PSC) • ZPICs serve the same jurisdictions as the Medicare Administrative Contractors. The ZPICs are authorized to conduct investigations, provide support to law enforcement, and conduct audits of Medicare advantage plans • ZPICs will concentrate on various Medicare billing “hot” targets much in same manner as MACs
Zone Program Integrity Contractors (ZPIC) • ZPICs were formerly known as Program Safeguard Contractors (PSC) • ZPICs serve the same jurisdictions as the Medicare Administrative Contractors. The ZPICs are authorized to conduct investigations, provide support to law enforcement, and conduct audits of Medicare advantage plans • ZPICs will concentrate on various Medicare billing “hot” targets much in same manner as MACs
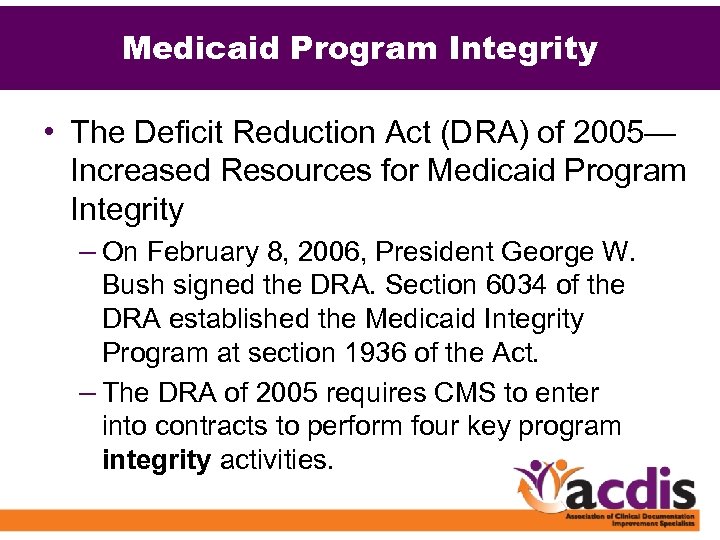 Medicaid Program Integrity • The Deficit Reduction Act (DRA) of 2005— Increased Resources for Medicaid Program Integrity – On February 8, 2006, President George W. Bush signed the DRA. Section 6034 of the DRA established the Medicaid Integrity Program at section 1936 of the Act. – The DRA of 2005 requires CMS to enter into contracts to perform four key program integrity activities.
Medicaid Program Integrity • The Deficit Reduction Act (DRA) of 2005— Increased Resources for Medicaid Program Integrity – On February 8, 2006, President George W. Bush signed the DRA. Section 6034 of the DRA established the Medicaid Integrity Program at section 1936 of the Act. – The DRA of 2005 requires CMS to enter into contracts to perform four key program integrity activities.
 The Purpose of the MIC • • Review provider actions; Audit claims; Identify overpayments; and Provide education to providers, beneficiaries, and “others” with respect to payment integrity and quality of care
The Purpose of the MIC • • Review provider actions; Audit claims; Identify overpayments; and Provide education to providers, beneficiaries, and “others” with respect to payment integrity and quality of care
 Medicaid Integrity Contractors (MIC) • MICs use a data-driven approach to focus efforts on coding and billing errors and erroneous claims overpayment, including fraud. • Examples of errors or overpayment include: – – Services provided after the death of a beneficiary Duplicate claims Unbundling of services Services billed improperly using incorrect diagnosis and/or procedure codes – Services paid that were not in accordance with covered services. – Payment for services not deemed medically necessary
Medicaid Integrity Contractors (MIC) • MICs use a data-driven approach to focus efforts on coding and billing errors and erroneous claims overpayment, including fraud. • Examples of errors or overpayment include: – – Services provided after the death of a beneficiary Duplicate claims Unbundling of services Services billed improperly using incorrect diagnosis and/or procedure codes – Services paid that were not in accordance with covered services. – Payment for services not deemed medically necessary
 Medicaid Integrity Contractors • No limit review requests • Regulations vary from state to state— challenge for healthcare systems with providers in more than one state
Medicaid Integrity Contractors • No limit review requests • Regulations vary from state to state— challenge for healthcare systems with providers in more than one state
 Compliance and the CDI Team • It is not unusual for the CDI team of specialists and coders to feel pressure to get the bills dropped and keep the case mix up • Remember: Do the right thing and keep the clinical documentation accurate and appropriate—nothing more, nothing less • CDI team may need to remind the CXOs that there are many goals of the CDI program such as ensuring “integrity of the record, ” including quality and accuracy
Compliance and the CDI Team • It is not unusual for the CDI team of specialists and coders to feel pressure to get the bills dropped and keep the case mix up • Remember: Do the right thing and keep the clinical documentation accurate and appropriate—nothing more, nothing less • CDI team may need to remind the CXOs that there are many goals of the CDI program such as ensuring “integrity of the record, ” including quality and accuracy
 How Can the CDI Team Help? • Prepare to respond to RAC additional documentation requests—including query forms when applicable. • Review processes for obtaining physician documentation. Is there a standard physician query process? • Update your CDI policies and procedures, including “Managing a Compliant Query Process”.
How Can the CDI Team Help? • Prepare to respond to RAC additional documentation requests—including query forms when applicable. • Review processes for obtaining physician documentation. Is there a standard physician query process? • Update your CDI policies and procedures, including “Managing a Compliant Query Process”.
 Query Forms and RAC • Auditors may request copies of query forms to validate “wording” even if not part of the permanent medical record
Query Forms and RAC • Auditors may request copies of query forms to validate “wording” even if not part of the permanent medical record
 Query Forms and RAC • Q: Should the Physician Query be included as a submission when RAC asks for additional documentation? There seems to be conflicting information as to whether CMS has authorized the submission of queries or whether it is up to the individual RAC. • CMS: Yes, that would be up to the RAC. They can request what they feel is necessary to conduct the review. (Seem pretty vague? ) – Reference: “Nationwide RAC 101 Calls, ” April 28, 2010.
Query Forms and RAC • Q: Should the Physician Query be included as a submission when RAC asks for additional documentation? There seems to be conflicting information as to whether CMS has authorized the submission of queries or whether it is up to the individual RAC. • CMS: Yes, that would be up to the RAC. They can request what they feel is necessary to conduct the review. (Seem pretty vague? ) – Reference: “Nationwide RAC 101 Calls, ” April 28, 2010.
 How Can the CDI Team Help? • Know where previous improper payments have been found by the RACs, OIG, and CERT – Demonstration findings: www. cms. hhs. gov/rac – OIG reports: www. oig. hhs. gov/reports. asp – CERT reports: www. cms. hhs. gov/cert • Get to know your regional RACs, MACs, and MICs
How Can the CDI Team Help? • Know where previous improper payments have been found by the RACs, OIG, and CERT – Demonstration findings: www. cms. hhs. gov/rac – OIG reports: www. oig. hhs. gov/reports. asp – CERT reports: www. cms. hhs. gov/cert • Get to know your regional RACs, MACs, and MICs
 How Can the CDI Team Help? • Distinguish which group is requesting the information—as processes may be different for the various groups • Ensure you are not “dialing for dollars” with your CDI program • Know if you are submitting claims with improper payments—get to know the PEPPER Reports
How Can the CDI Team Help? • Distinguish which group is requesting the information—as processes may be different for the various groups • Ensure you are not “dialing for dollars” with your CDI program • Know if you are submitting claims with improper payments—get to know the PEPPER Reports
 Program for Evaluating Payment Patterns Electronic Report (PEPPER) • PEPPER provides electronic hospitalspecific data statistics for Medicare severity diagnosis-related groups (MS-DRG) and discharges at high risk for payment errors • www. pepperresources. org is the official site for information, training, and support related to the Program for Evaluating Payment Patterns Electronic Report (PEPPER)
Program for Evaluating Payment Patterns Electronic Report (PEPPER) • PEPPER provides electronic hospitalspecific data statistics for Medicare severity diagnosis-related groups (MS-DRG) and discharges at high risk for payment errors • www. pepperresources. org is the official site for information, training, and support related to the Program for Evaluating Payment Patterns Electronic Report (PEPPER)
 PEPPER • PEPPER can support a hospital’s compliance efforts by identifying where the hospital is an outlier for the risk areas, such as medical necessity. • PEPPER data can assist the hospital in identifying both potential overpayments as well as potential underpayments. • Important to share information with the CDI team!
PEPPER • PEPPER can support a hospital’s compliance efforts by identifying where the hospital is an outlier for the risk areas, such as medical necessity. • PEPPER data can assist the hospital in identifying both potential overpayments as well as potential underpayments. • Important to share information with the CDI team!
 How Can the CDI Team Help? • Consider conducting routine, internal “self -audits” with the guidance of the compliance officer • Determine process for self-reporting only with guidance from legal counsel • Assist with appeals as necessary
How Can the CDI Team Help? • Consider conducting routine, internal “self -audits” with the guidance of the compliance officer • Determine process for self-reporting only with guidance from legal counsel • Assist with appeals as necessary
 How Can the CDI Team Help? • Utilize the documentation expertise of the CDI team on the RAC Committee— expanded to become a Documentation Oversight Committee • Assess the process for “integration” with case management—how do the various organizational silos communicate with one another?
How Can the CDI Team Help? • Utilize the documentation expertise of the CDI team on the RAC Committee— expanded to become a Documentation Oversight Committee • Assess the process for “integration” with case management—how do the various organizational silos communicate with one another?
 Key Considerations • Focus on quality documentation that is complete and accurate—the coding (and hence, the appropriate revenue) will “fall where it falls” • Remember third-party agencies will always come knocking • All parties—case management, HIM, CDI, physicians, compliance, billing—need communication processes
Key Considerations • Focus on quality documentation that is complete and accurate—the coding (and hence, the appropriate revenue) will “fall where it falls” • Remember third-party agencies will always come knocking • All parties—case management, HIM, CDI, physicians, compliance, billing—need communication processes
 Key Considerations • Help physicians understand how to “tell the patient’s story” • Risk vs. reward: Don’t try to “push the envelope” • Focus on doing the right thing—ask yourself, “Could I defend this case in an appeal? Does the documentation and clinical story support the codes assigned? ”
Key Considerations • Help physicians understand how to “tell the patient’s story” • Risk vs. reward: Don’t try to “push the envelope” • Focus on doing the right thing—ask yourself, “Could I defend this case in an appeal? Does the documentation and clinical story support the codes assigned? ”
 Thank You Questions?
Thank You Questions?


