3de22b94d66705ba77c73c853683c168.ppt
- Количество слайдов: 45
2008 California Guideline for Alzheimer’s Disease Management Debra Cherry, Ph. D Alzheimer’s Association, California Southland
Presenter Disclosures The following financial relationships with commercial interests relevant to this presentation existed during the past 12 months: Grants to the Alzheimer’s Association, California Southland Chapter: • Forest Laboratories • Pfizer/Eisai • Janssen Pharmaceuticals • Novartis • Elan
Objectives • Describe the process utilized to update the California Guideline for AD Management • Review the Guideline’s recommendations • Apply the recommendations to patients and caregivers • Use the Guideline to implement a quality improvement project
What is a clinical guideline? A document with the aim or guiding medical decisions and practice regarding: • Diagnosis • Management • Treatment Briefly identifies, summarized and evaluates best evidence and most current data. Includes consensus statements from experts.
History of California AD Management Guideline • • 1995: California Workgroup on Guideline for Alzheimer’s Disease Management formed 1998 Publication of the first Guideline 2002 Guideline updated & published in The American Family Physician 2008 Third update completed.
Composition of the California Workgroup Representatives from throughout the State: • Healthcare providers • Consumers • Academicians • Professional and volunteer organizations
Purpose of the Guideline Represents core care recommendations for AD management which are: • Based on scientific evidence • Supplemented by expert consensus • General guide to post-diagnostic care • Intended for Primary Care Practitioners including: – Physicians • Also defines a role for: – Nurse Practitioners/Nurses –Social Workers – Physician Assistants –Care Managers
Mrs. R. L. is a retired librarian who visits her physician for a routine follow-up for her osteoarthritis, GERD, and glaucoma. She has enjoyed her 3 years of retirement, but reports that recently her husband has been worried about her memory. Mrs. L. states that she had started writing reminder notes, “which don’t always help. ” She admits to reading less than she used to; she also drives less because “traffic is such a problem. ”
Mrs. R. L. Mr. L. reports that his wife often returns from grocery shopping having forgotten to pick up several things that she intended to buy. At other times she will wander through the house, looking in drawers or closets for items that she had put away for safe-keeping. Although they used to go out to dinner at least once a week, they now go much less frequently because Mrs. L. states that “I just never know what to order, and it’s not as much fun as it used to be. ”
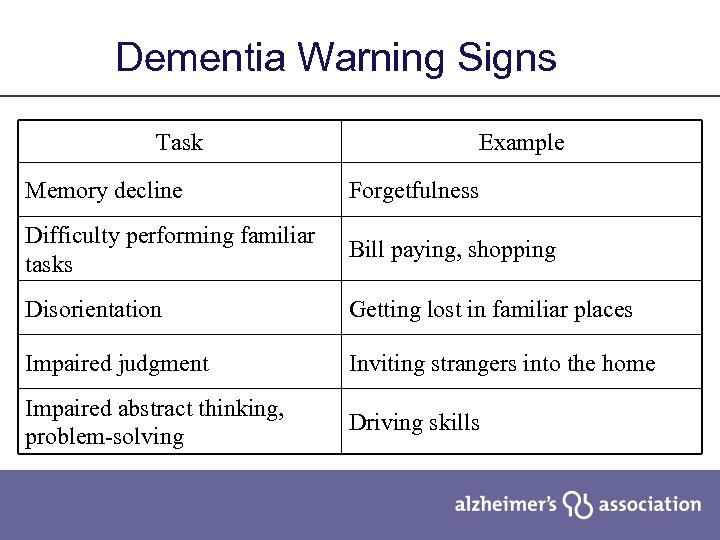
Dementia Warning Signs Task Example Memory decline Forgetfulness Difficulty performing familiar tasks Bill paying, shopping Disorientation Getting lost in familiar places Impaired judgment Inviting strangers into the home Impaired abstract thinking, problem-solving Driving skills
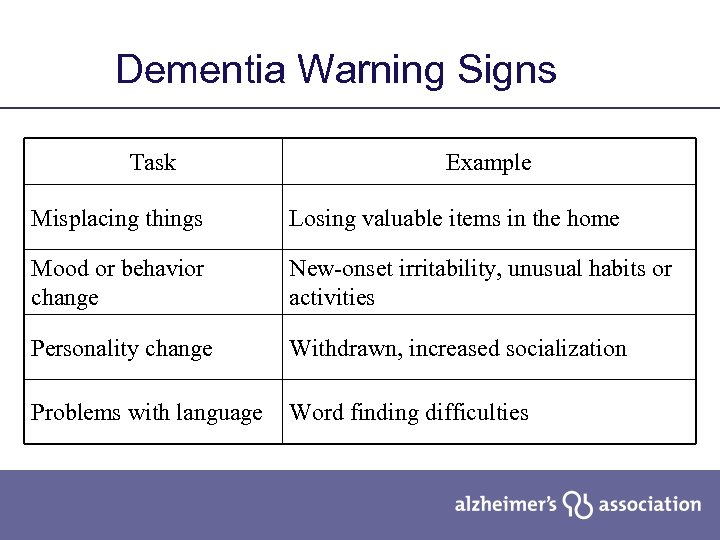
Dementia Warning Signs Task Example Misplacing things Losing valuable items in the home Mood or behavior change New-onset irritability, unusual habits or activities Personality change Withdrawn, increased socialization Problems with language Word finding difficulties
What signs and symptoms are present in Mrs. R. L. that suggest that she may have a dementia?
Guideline for AD Management • • Assessment Treatment Patient & Family Education & Support Legal Considerations
Assessment • • Cognitive status Daily function Concurrent medical conditions Medications Behavior symptoms and mood Living arrangements Support system
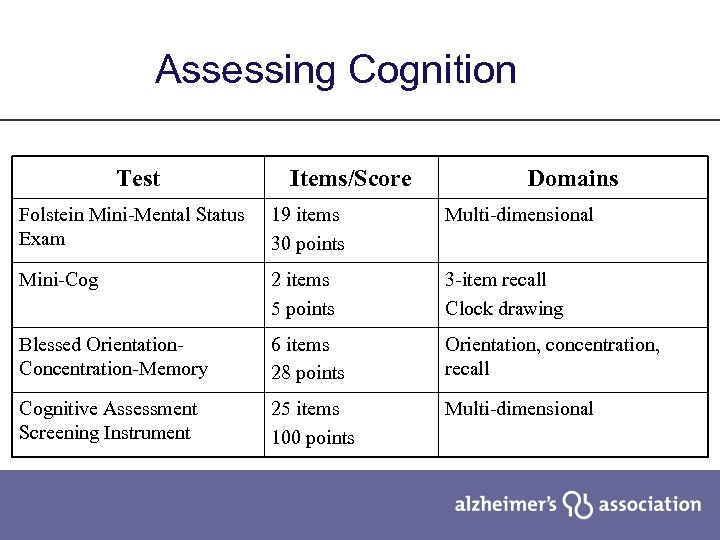
Assessing Cognition Test Items/Score Domains Folstein Mini-Mental Status Exam 19 items 30 points Multi-dimensional Mini-Cog 2 items 5 points 3 -item recall Clock drawing Blessed Orientation. Concentration-Memory 6 items 28 points Orientation, concentration, recall Cognitive Assessment Screening Instrument 25 items 100 points Multi-dimensional
Assessment: Function Activities of Daily Living (ADL) • • Self-feeding Dressing Ambulation Toileting • Bathing • Transfer from bed to toilet • Continence • Grooming • Communication
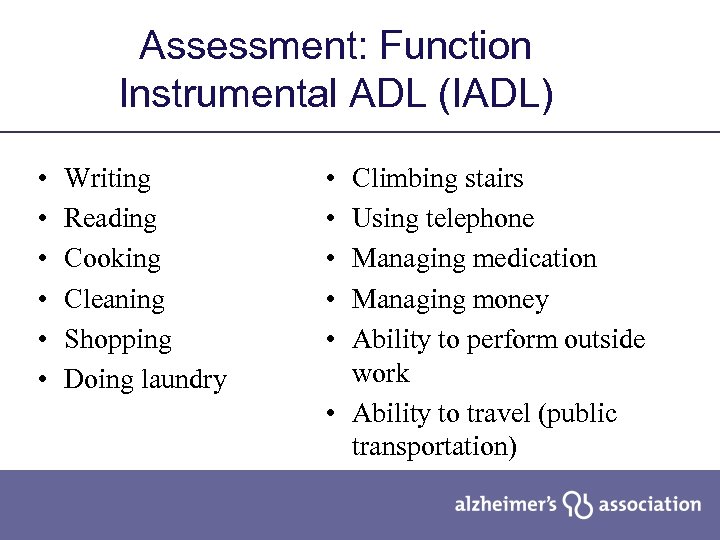
Assessment: Function Instrumental ADL (IADL) • • • Writing Reading Cooking Cleaning Shopping Doing laundry • • • Climbing stairs Using telephone Managing medication Managing money Ability to perform outside work • Ability to travel (public transportation)
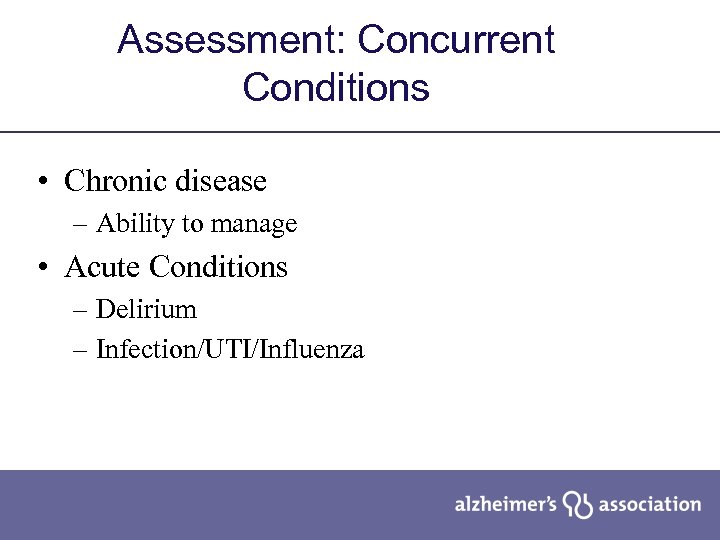
Assessment: Concurrent Conditions • Chronic disease – Ability to manage • Acute Conditions – Delirium – Infection/UTI/Influenza
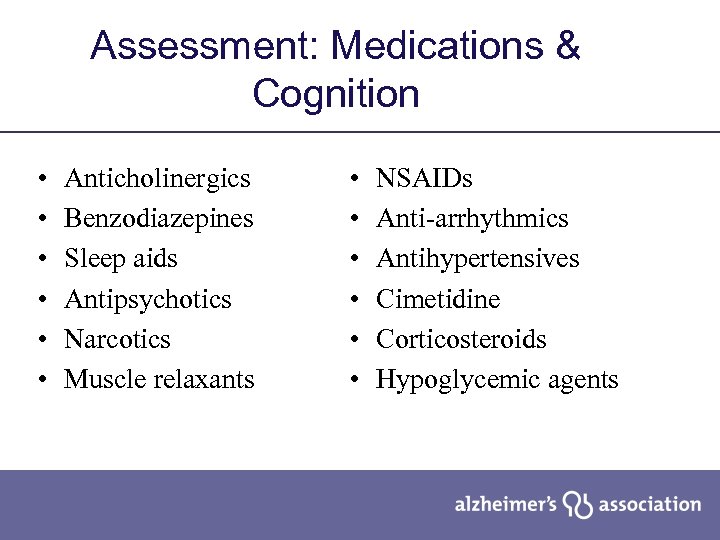
Assessment: Medications & Cognition • • • Anticholinergics Benzodiazepines Sleep aids Antipsychotics Narcotics Muscle relaxants • • • NSAIDs Anti-arrhythmics Antihypertensives Cimetidine Corticosteroids Hypoglycemic agents
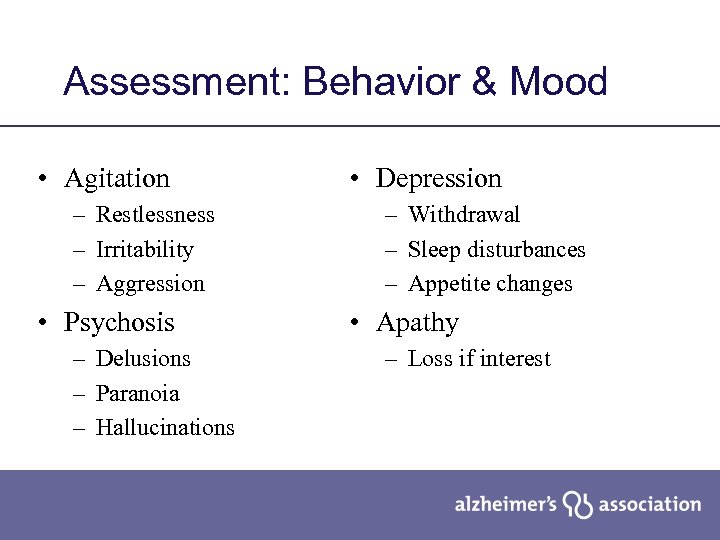
Assessment: Behavior & Mood • Agitation – Restlessness – Irritability – Aggression • Psychosis – Delusions – Paranoia – Hallucinations • Depression – Withdrawal – Sleep disturbances – Appetite changes • Apathy – Loss if interest
Assessment: Living Arrangements • Declining ability for self-care – Patient autonomy vs. need for care • Safety issues – Rugs, appliances – Driving • Abuse and neglect – Dependence – Caregiver stress
Assessment: Support System • Family’s ability to care for patient • Community supports – Alzheimer’s Association – Caregiver Resource Center – Religious or other groups • Community resources – day care, in-home care • Health care resources • Advance directives
Mrs. R has come to the Alzheimer’s Disease Center and been thoroughly assessed. She has been determined to have a diagnosis of Alzheimer’s disease. What next?
Treatment: Develop a Treatment Plan • • • Improve cognitive function Increase level of function Delay disease progression Manage behavior disturbances Ease caregiver burden
Treatment: Improve Cognitive Function • Cholinergic manipulation – Cholinesterase inhibitors • All agents block acetylcholinesterase activity • Rivastigmine also blocks butyrylcholinesterase • Galantamine stimulates cholinergic receptors • NMDA antagonist – Reduces glutamate activity – Regulates calcium entry into cells
Counseling Points • Effects on cognition are very mild • May stabilize or slow decline • May improve independence, self-care • Gastrointestinal effects are prominent • May slow heart rate
TREATMENT Recommendations • • Treat behavioral symptoms and mood disorders using: – Non-pharmacologic approaches, such as environmental modification, task simplification, appropriate activities, etc. IF non-pharmacological approaches prove unsuccessful, THEN use medications, targeted to specific behaviors, if clinically indicated. Note that side effects may be serious and significant.
Treatment: Behavior Symptoms • Most difficult for both patients and caregivers • Behavior symptoms contribute to: – Patient distress – Caregiver burnout – Excess disability – Institutionalization
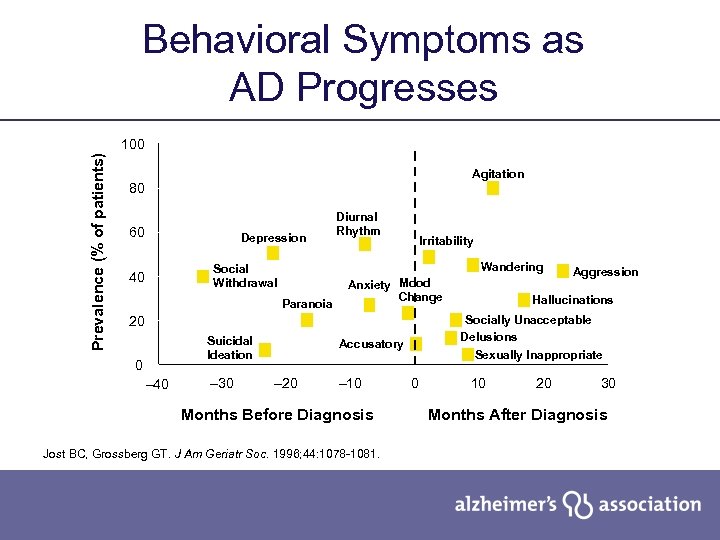
Behavioral Symptoms as AD Progresses Prevalence (% of patients) 100 Agitation 80 60 Depression Irritability Wandering Social Withdrawal 40 Diurnal Rhythm Paranoia Anxiety Mood Change 20 Suicidal Ideation 0 – 40 – 30 – 10 Months Before Diagnosis Jost BC, Grossberg GT. J Am Geriatr Soc. 1996; 44: 1078 -1081. Hallucinations Socially Unacceptable Delusions Sexually Inappropriate Accusatory – 20 Aggression 0 10 20 30 Months After Diagnosis
Mrs. R. L. Some time has passed and Mr. L. is concerned about changes in his wife’s behavior. She becomes agitated, especially in the late afternoon and leaves the house. She says she is going home and gets more agitated when he reminds her that she is in her home.
Evaluating Behaviors • Rapid onset requires search for medical cause – Pain, infection, adverse drug effect • Identify problem a. Antecedents - Behaviorial triggers b. Behaviors – Be Specific c. Consequences
Common Causes of Challenging Behaviors • • • Health problems Difficult tasks Confusing environment Communication breakdown Patient’s perceptions of the situation
What may be triggering Mrs. L. ’s behavior? What does this behavior mean to her? How should these symptoms be managed?
Mrs. R. L. has begun a daily exercise program and late afternoon agitation is now less of an issue. However, at night she awakens and becomes agitated. She believes someone is trying to break into the house. When her husband tries to reassure her, she gets angry and strikes out at him.
What may be triggering Mrs. L. ’s behavior? What does this behavior mean to her? How should these symptoms be managed?

PATIENT and FAMILY EDUCATION & SUPPORT Recommendations • Integrate medical care with education & support by connecting patient & caregiver to support organizations - Alzheimer’s Association 1 -800 -272 -3900 www. alz. org - Family Caregiver Alliance 1 -800 -445 -8106 www. caregiver. org - or your own social service department.
PATIENT and FAMILY EDUCATION & SUPPORT Early Stages Pay particular attention to the special needs of earlystage patients, involving them in care planning, heeding their opinions and wishes, and referring them to community resources, including the Alzheimer’s Association.
PATIENT and FAMILY EDUCATION & SUPPORT End of Life Decisions Discuss the intensity of care and other end-of-live care decisions with the Alzheimer’s Disease patient and involved family members while respecting their cultural preferences.
LEGAL CONSIDERATIONS Recommendations • • • Include a discussion of the importance of basic legal and financial planning as part of the treatment plan as soon as possible after the diagnosis of AD. Monitor for evidence of and report all suspicions of abuse as required by law. Report the diagnosis of AD in accordance with local laws.
Using the Guideline in a Health Care Setting Health care organizations are challenged to care for the growing number of older adults with chronic health conditions
How to use Guidelines for a QI project: • • Set quality goals derived from guideline Train practitioners Add case management Evaluate
Implementation Support Tools Provider Tool Kit • Medical Record Checklist • List of Reversible Medical Conditions • Signs/Symptoms of Elder Abuse • Mental Status Exam • Safe Return / ID Bracelet Program Application • Dementia and Driving Reporting Law • Prescription Pad
QI Projects Using Guidelines • Kaiser Permanente – Metro L. A. • ACCESS – Kaiser, Scripps & U. C. S. D. Healthcare • Health. Care Partners Medical Group • SCAN Health. Plan
Establishing Partnerships Replication Manual Based on Alzheimer’s Association – Kaiser Permanent Metropolitan Los Angeles Dementia Care Project www. alz. org/california southland Click on Professional Training then scroll down to Replication Manual
Got Guideline? 2008 California Guideline for Alzheimer’s Disease Management Available at: www. caalz. org/californiasouthland/ or contact Amy. Landers@alz. org 323 -930 -6289
3de22b94d66705ba77c73c853683c168.ppt