89891a2d79cf741b99171d82041ee14a.ppt
- Количество слайдов: 142
 2006 CHAM User Orientation
2006 CHAM User Orientation
 2006 CHAM User Orientation • • Welcome and Introductions Introduce yourselves to the books Philosophy of the CHAM revision project Major changes from previous edition Introduction to the 2006 CHAM Medicine practice More scenarios
2006 CHAM User Orientation • • Welcome and Introductions Introduce yourselves to the books Philosophy of the CHAM revision project Major changes from previous edition Introduction to the 2006 CHAM Medicine practice More scenarios
 Philosophy CHAM revision project • Make a book that is user-friendly for the CHA/P • Also usable by physicians, trainers, supervisors • Compatible with Basic Training Curriculum
Philosophy CHAM revision project • Make a book that is user-friendly for the CHA/P • Also usable by physicians, trainers, supervisors • Compatible with Basic Training Curriculum
 Philosophy CHAM revision project • Additional information in CHAM, not included in the current Curriculum, such as: – End of Life Comfort Care – HIV patient care – Intraosseous infusion – Female cancer screening
Philosophy CHAM revision project • Additional information in CHAM, not included in the current Curriculum, such as: – End of Life Comfort Care – HIV patient care – Intraosseous infusion – Female cancer screening
 Philosophy CHAM revision project • Up-to-date standards of care • Looked at national, state, and Native health service guidelines • Cautious approach to practice – BP cutoff is 105 for Nitro – Orthostatic VS conservative • Extensive review by: – Rural Tribal Health Organization doctors who work with CHA/Ps – Medical specialists
Philosophy CHAM revision project • Up-to-date standards of care • Looked at national, state, and Native health service guidelines • Cautious approach to practice – BP cutoff is 105 for Nitro – Orthostatic VS conservative • Extensive review by: – Rural Tribal Health Organization doctors who work with CHA/Ps – Medical specialists
 Philosophy CHAM revision project • How to Use this Book and CHAP Overview chapters contain valuable information • Explain many of the things that are new • Helpful for all users of the book • Homework assignment handout in your folder
Philosophy CHAM revision project • How to Use this Book and CHAP Overview chapters contain valuable information • Explain many of the things that are new • Helpful for all users of the book • Homework assignment handout in your folder
 Major Changes in CHAM • Problem or chief complaint based, rather than assessment based, except chronic care. • Approach to Sick Child younger than 8 years. • Recheck section. • Emergency chapter and how it is used. • Inside Front Cover—content and clarity.
Major Changes in CHAM • Problem or chief complaint based, rather than assessment based, except chronic care. • Approach to Sick Child younger than 8 years. • Recheck section. • Emergency chapter and how it is used. • Inside Front Cover—content and clarity.
 Color for Navigation • Blue text – Assessment names – Section titles and breaks • Patient Ed boxes: Blue • Procedure boxes: Gray • Information for CHA/P boxes: White
Color for Navigation • Blue text – Assessment names – Section titles and breaks • Patient Ed boxes: Blue • Procedure boxes: Gray • Information for CHA/P boxes: White
 Telehealth • Reminder to CHA/P to use telehealth – If available – You think it will help doctor • Used in appropriate problem exam sections – – Skin Ear Musculoskeletal Etc.
Telehealth • Reminder to CHA/P to use telehealth – If available – You think it will help doctor • Used in appropriate problem exam sections – – Skin Ear Musculoskeletal Etc.
 Overview of 2006 CHAM • Emergency Field Handbook • CHAM Patient Care Visit book • CHAM Medicine Handbook – Combined VMR and 1998 CHAM Medicine Chart – No more VMR • CHAM Reference and Procedure book • Laminated sheet with exams • CD ROM
Overview of 2006 CHAM • Emergency Field Handbook • CHAM Patient Care Visit book • CHAM Medicine Handbook – Combined VMR and 1998 CHAM Medicine Chart – No more VMR • CHAM Reference and Procedure book • Laminated sheet with exams • CD ROM
 CD ROM • Contains all 4 volumes in PDF format • Can print any page • Click-on patient ed information that will print for CHA/P to give to patient. – Problem patient ed – Medicine patient ed
CD ROM • Contains all 4 volumes in PDF format • Can print any page • Click-on patient ed information that will print for CHA/P to give to patient. – Problem patient ed – Medicine patient ed
 CD ROM • Read the instructions carefully • Can navigate to anyplace in the 4 volumes by entering the desired page number • Does NOT contain any audio or video clips in this version
CD ROM • Read the instructions carefully • Can navigate to anyplace in the 4 volumes by entering the desired page number • Does NOT contain any audio or video clips in this version
 How to Use the CD • Insert the disk. • Menu will pop up. • Install Adobe Reader as needed. – Do not need internet connection to do this – Takes 5 to 10 minutes to install – Will not work for Windows ’ 98. Call your IT department.
How to Use the CD • Insert the disk. • Menu will pop up. • Install Adobe Reader as needed. – Do not need internet connection to do this – Takes 5 to 10 minutes to install – Will not work for Windows ’ 98. Call your IT department.
 How to Use the CD • Click on Instructions and read them carefully. • Click on CHAM 4 volume set. – Inside front cover comes up first. – May take a few minutes, depending on your computer. • To change pages: – – Click on page number at bottom of screen Enter a new page number, example: p. 290 Press enter P. 290 will appear
How to Use the CD • Click on Instructions and read them carefully. • Click on CHAM 4 volume set. – Inside front cover comes up first. – May take a few minutes, depending on your computer. • To change pages: – – Click on page number at bottom of screen Enter a new page number, example: p. 290 Press enter P. 290 will appear
 How to Use the CD • To go to other books: – Reference: type in R-40. Must have R and dash – Medicine handbook: type in M-114. – Emergency handbook: type in E-36 • Now install the disk and try these steps
How to Use the CD • To go to other books: – Reference: type in R-40. Must have R and dash – Medicine handbook: type in M-114. – Emergency handbook: type in E-36 • Now install the disk and try these steps
 Use the Emergency Field Handbook
Use the Emergency Field Handbook
 Scenario 1 • You are health aides in a village 250 miles from the nearest hospital. • You get a call in the middle of the night about a 4 -wheeler accident with someone hurt bad. It is summer, not raining. • You arrive at the scene with your emergency kit and Emergency Field Handbook.
Scenario 1 • You are health aides in a village 250 miles from the nearest hospital. • You get a call in the middle of the night about a 4 -wheeler accident with someone hurt bad. It is summer, not raining. • You arrive at the scene with your emergency kit and Emergency Field Handbook.
 Scenario 1 • Where do you start? • Start on p. E-1. • Scene is safe. 4 -wheeler rolled over on its side several feet away from patient. One patient wearing a helmet, moaning but not moving much. Witness says he had been drinking and the 4 -wheeler rolled over him. • What kind of problem: Trauma? Medical? Young child?
Scenario 1 • Where do you start? • Start on p. E-1. • Scene is safe. 4 -wheeler rolled over on its side several feet away from patient. One patient wearing a helmet, moaning but not moving much. Witness says he had been drinking and the 4 -wheeler rolled over him. • What kind of problem: Trauma? Medical? Young child?
 Scenario 1 • • Trauma patient. Go to p. E-5. GA: Moaning, says stomach hurts. Stabilize neck? Airway and breathing: Open, breathing a little fast. – If open chest wound, would bump out here to p. E-25. Not for this patient. – Start Oxygen. • Circulation: pulse fast, weak. • No major bleeding. • Skin: normal color, cool, dry.
Scenario 1 • • Trauma patient. Go to p. E-5. GA: Moaning, says stomach hurts. Stabilize neck? Airway and breathing: Open, breathing a little fast. – If open chest wound, would bump out here to p. E-25. Not for this patient. – Start Oxygen. • Circulation: pulse fast, weak. • No major bleeding. • Skin: normal color, cool, dry.
 Scenario 1 • Remove helmet: no • Rapid trauma exam: Abdomen, tender RUQ. • Weather: OK. • VS: P 120, R 20, BP 98/85. • SAMPLE history: Not cooperative to answer questions. • Treat for shock? – Experienced CHA/P might. – New CHA/P might or might not.
Scenario 1 • Remove helmet: no • Rapid trauma exam: Abdomen, tender RUQ. • Weather: OK. • VS: P 120, R 20, BP 98/85. • SAMPLE history: Not cooperative to answer questions. • Treat for shock? – Experienced CHA/P might. – New CHA/P might or might not.
 Scenario 1 • Serious injuries: May start at – Shock p. E-11. • E-12 sends you back to E-9, then p. E-35 Assessment chart. – Abdominal Injury p. E-35. • Assessment Chart • What is Assessment? • Other Severe Abdominal Injury. • Go to p. E-41.
Scenario 1 • Serious injuries: May start at – Shock p. E-11. • E-12 sends you back to E-9, then p. E-35 Assessment chart. – Abdominal Injury p. E-35. • Assessment Chart • What is Assessment? • Other Severe Abdominal Injury. • Go to p. E-41.
 Scenario 1 • Then go to CHAM, p. 57. • CHAM p. 66. • Back to p. E-122 for care during medevac. – The only time CHA/P is sent back to Emergency Handbook.
Scenario 1 • Then go to CHAM, p. 57. • CHAM p. 66. • Back to p. E-122 for care during medevac. – The only time CHA/P is sent back to Emergency Handbook.
 Scenario 2 • Phone call: Says cannot wake up grandmother. Go to home with emergency kit and Handbook. • Where to start? • Start on p. E-1. • Scene is safe. • 60 year old woman lying in bed. • What kind of problem: Trauma? Medical? Young child?
Scenario 2 • Phone call: Says cannot wake up grandmother. Go to home with emergency kit and Handbook. • Where to start? • Start on p. E-1. • Scene is safe. • 60 year old woman lying in bed. • What kind of problem: Trauma? Medical? Young child?
 Scenario 2 • Medical. Go to p. E-60. • GA: Patient looks sick. Responds only to pain by moaning and moving a little. • Airway open, breathing slow and deep. – Start Oxygen. • Not exposed to cold. • Pulse slow, strong. • Skin: Pink, warm, dry.
Scenario 2 • Medical. Go to p. E-60. • GA: Patient looks sick. Responds only to pain by moaning and moving a little. • Airway open, breathing slow and deep. – Start Oxygen. • Not exposed to cold. • Pulse slow, strong. • Skin: Pink, warm, dry.
 Scenario 2 • SAMPLE history: woke up during the night with a headache, but went back to sleep. Unable to wake her up this morning. No allergies or meds. High blood pressure for 2 years, didn’t want to take the medicine. • Is this Severe Allergic Reaction? • Is this a Seizure? • What next?
Scenario 2 • SAMPLE history: woke up during the night with a headache, but went back to sleep. Unable to wake her up this morning. No allergies or meds. High blood pressure for 2 years, didn’t want to take the medicine. • Is this Severe Allergic Reaction? • Is this a Seizure? • What next?
 Scenario 2 • • Do blood sugar. Blood sugar is 92. Do vital signs. T: 97. 4; P 60; R 12; BP 160/90; Sp. O 2 92 • Vital signs OK • Is this Poisoning, Chest Pain, Severe Shortness of Breath, Stroke, Mental Health Emergency?
Scenario 2 • • Do blood sugar. Blood sugar is 92. Do vital signs. T: 97. 4; P 60; R 12; BP 160/90; Sp. O 2 92 • Vital signs OK • Is this Poisoning, Chest Pain, Severe Shortness of Breath, Stroke, Mental Health Emergency?
 Scenario 2 • What next? • Rapid exam: Pupils, right larger than left, slow to respond to light. • Transport to clinic. • Report. • Go to CHAM p. 74, Additional History • Negative except for headache and hypertension.
Scenario 2 • What next? • Rapid exam: Pupils, right larger than left, slow to respond to light. • Transport to clinic. • Report. • Go to CHAM p. 74, Additional History • Negative except for headache and hypertension.
 Scenario 2 • Additional Exam: neck a little stiff when flexed. Reflexes: can’t tell if they are equal. • Hgb: 12. 2; No urine • What is your Assessment? • Other Cause Decreased Level of Consciousness. • Plan p. 102, Emergency 38, Other Medical Emergency
Scenario 2 • Additional Exam: neck a little stiff when flexed. Reflexes: can’t tell if they are equal. • Hgb: 12. 2; No urine • What is your Assessment? • Other Cause Decreased Level of Consciousness. • Plan p. 102, Emergency 38, Other Medical Emergency
 • • Scenario 3 A mom calls, saying her 2 month old baby is very sick. Please come to the house. You go with emergency kit and EFH. Where do you start? Start on p. E-1. Scene is safe. Won’t eat, very sleepy. What kind of problem: Trauma? Medical? Young child?
• • Scenario 3 A mom calls, saying her 2 month old baby is very sick. Please come to the house. You go with emergency kit and EFH. Where do you start? Start on p. E-1. Scene is safe. Won’t eat, very sleepy. What kind of problem: Trauma? Medical? Young child?
 Scenario 3 • • Go to p. E-55. GA: pale, limp, sweaty, not moving. LOC: difficult to wake up. Airway open, breathing fast, shallow, grunting. – Start Oxygen. – If wheezing, could give Albuterol. • No cold exposure.
Scenario 3 • • Go to p. E-55. GA: pale, limp, sweaty, not moving. LOC: difficult to wake up. Airway open, breathing fast, shallow, grunting. – Start Oxygen. – If wheezing, could give Albuterol. • No cold exposure.
 Scenario 3 • • • Pulse 180, hard to feel. No bleeding. Skin feels cold, cap refill 4 seconds. SAMPLE History Getting sick over 2 days, won’t breastfeed or take a bottle now, was fussy and irritable, now just hard to wake up. Maybe had a fever, but now feels cold. No other symptoms.
Scenario 3 • • • Pulse 180, hard to feel. No bleeding. Skin feels cold, cap refill 4 seconds. SAMPLE History Getting sick over 2 days, won’t breastfeed or take a bottle now, was fussy and irritable, now just hard to wake up. Maybe had a fever, but now feels cold. No other symptoms.
 Scenario 3 • • • Vital signs T 96. 6; P 180; R 60, irregular; Sp. O 2 88 Is this Severe Allergic Reaction? Is this Seizure? What next? Check blood sugar Blood sugar 68 Examine quickly Eyes sunken, mouth dry Chest clear. Abdomen soft. Arms/legs: floppy, limp
Scenario 3 • • • Vital signs T 96. 6; P 180; R 60, irregular; Sp. O 2 88 Is this Severe Allergic Reaction? Is this Seizure? What next? Check blood sugar Blood sugar 68 Examine quickly Eyes sunken, mouth dry Chest clear. Abdomen soft. Arms/legs: floppy, limp
 Scenario 3 • Is this Poisoning? • Is this child very sick? • Yes – Very sleepy, will not drink – Looks very sick, pale – Vital signs: T 96. 6; P 180; Sp. O 2 88 – Eyes sunken, mouth dry – Floppy, limp – Skin cold; cap refill 4 seconds
Scenario 3 • Is this Poisoning? • Is this child very sick? • Yes – Very sleepy, will not drink – Looks very sick, pale – Vital signs: T 96. 6; P 180; Sp. O 2 88 – Eyes sunken, mouth dry – Floppy, limp – Skin cold; cap refill 4 seconds
 Scenario 3 • • Transport to clinic What next? Very sick child. Go to CHAM p. 149 Follow Plan 1 while trying to contact doctor
Scenario 3 • • Transport to clinic What next? Very sick child. Go to CHAM p. 149 Follow Plan 1 while trying to contact doctor
 Look through Emergency Handbook • New volume. For use by health aide who has completed Session I and ETT. • Designed to be used outside the village clinic. All plans send CHA/P to CHAM for continued care in clinic. • Layout and content are similar to emergency chapter in CHAM. • Tabs for major sections.
Look through Emergency Handbook • New volume. For use by health aide who has completed Session I and ETT. • Designed to be used outside the village clinic. All plans send CHA/P to CHAM for continued care in clinic. • Layout and content are similar to emergency chapter in CHAM. • Tabs for major sections.
 Emergency Handbook • Information for giving emergency medicines is in this book. – p. E-74, 75 • Section for Emergency Childbirth. • Skills summary. • Plan “Care of Patient During Medevac”, p. E-122; written plan to follow during transport.
Emergency Handbook • Information for giving emergency medicines is in this book. – p. E-74, 75 • Section for Emergency Childbirth. • Skills summary. • Plan “Care of Patient During Medevac”, p. E-122; written plan to follow during transport.
 CHAM Patient Care Book • Look at Dedication • Look at Table of Contents, p. 10 and 11 • Chapters organization – – – Emergency Childbirth Child Elders Head; Chest; Abdomen; Musculoskeletal, Skin/Soft Tissue – Urinary, Male, Female, Pregnancy – Nervous; Endocrine; Immune – Mental Health; Alcohol/Drug; Other Topics.
CHAM Patient Care Book • Look at Dedication • Look at Table of Contents, p. 10 and 11 • Chapters organization – – – Emergency Childbirth Child Elders Head; Chest; Abdomen; Musculoskeletal, Skin/Soft Tissue – Urinary, Male, Female, Pregnancy – Nervous; Endocrine; Immune – Mental Health; Alcohol/Drug; Other Topics.
 CHAM Patient Care Book • Always try to go forward in the book, not backwards. Less skipping here and there. Plans may be repetitive to avoid going to another section.
CHAM Patient Care Book • Always try to go forward in the book, not backwards. Less skipping here and there. Plans may be repetitive to avoid going to another section.
 CHAM Patient Care Book • Children: In order to identify early and as often as possible the very sick child, CHAM is designed to catch the very sick child at a number of places in the patient visit.
CHAM Patient Care Book • Children: In order to identify early and as often as possible the very sick child, CHAM is designed to catch the very sick child at a number of places in the patient visit.
 CHAM Patient Care Book • Look at Digestive Chapter, p. 359 • Do Not begin here, Begin Here • Problem sections in order – Injury, Acute, Chronic • History: Most Other History is gone, was incorporated into HPI. – If not already done • Standard questions for child younger than 3 years. • Exam: Sick Child box if problem may involve a child. To eliminate the need for multiple chapter histories and exam. – If not already done
CHAM Patient Care Book • Look at Digestive Chapter, p. 359 • Do Not begin here, Begin Here • Problem sections in order – Injury, Acute, Chronic • History: Most Other History is gone, was incorporated into HPI. – If not already done • Standard questions for child younger than 3 years. • Exam: Sick Child box if problem may involve a child. To eliminate the need for multiple chapter histories and exam. – If not already done
 CHAM Patient Care Book • Assessments: – Some chapters have 2 assessment charts. Look at Assessment step for instructions. • Female, p. • Musculoskeletal, p. • Skin/Soft Tissue, p. – Possible vs definite. Medicaid issues. • Assessment charts or lists of assessments for that problem. – Example: Breast problems Assessment, p. 512. A list rather than a chart • May or may not definition
CHAM Patient Care Book • Assessments: – Some chapters have 2 assessment charts. Look at Assessment step for instructions. • Female, p. • Musculoskeletal, p. • Skin/Soft Tissue, p. – Possible vs definite. Medicaid issues. • Assessment charts or lists of assessments for that problem. – Example: Breast problems Assessment, p. 512. A list rather than a chart • May or may not definition
 CHAM Patient Care Book • Assessment charts and lists try to cover the most common findings for the problems. – Definitive assessments are those that a health aide can make using the CHAM and lab tests available in the village. – There is extensive use of the word “possible” • In order of most common or most urgent
CHAM Patient Care Book • Assessment charts and lists try to cover the most common findings for the problems. – Definitive assessments are those that a health aide can make using the CHAM and lab tests available in the village. – There is extensive use of the word “possible” • In order of most common or most urgent
 CHAM Patient Care Book • Plans – Plan names: Eye, Eyelid; Child, Teen; Mouth, Jaw, Teeth • Definitions after plan name • Generally follow a standard format. – May have immediate or emergency care. Any change in order of steps was deliberate. • New sections: While or If waiting to transport
CHAM Patient Care Book • Plans – Plan names: Eye, Eyelid; Child, Teen; Mouth, Jaw, Teeth • Definitions after plan name • Generally follow a standard format. – May have immediate or emergency care. Any change in order of steps was deliberate. • New sections: While or If waiting to transport
 CHAM Patient Care Book • Standing Orders: Many changes. Old ones gone, new ones possible. All marked; p. 624 • Employer may issue other standing orders, but are responsible for testing, etc. • Medicines NOT part of standing order: p. 304 • Special Topics and Procedure Summaries mostly gone. – Most procedures are in Reference/Procedure book.
CHAM Patient Care Book • Standing Orders: Many changes. Old ones gone, new ones possible. All marked; p. 624 • Employer may issue other standing orders, but are responsible for testing, etc. • Medicines NOT part of standing order: p. 304 • Special Topics and Procedure Summaries mostly gone. – Most procedures are in Reference/Procedure book.
 Inside Front Cover • There are 7 different places to go from Inside Front Cover.
Inside Front Cover • There are 7 different places to go from Inside Front Cover.
 Scenario 4: Emergency • Adult male walks into clinic. Looks pale, says he feels very sick and needs to lie down. • As you start to get him onto exam table, he faints. • Where to start in CHAM? • Inside Front Cover: Emergency, go to p. 40. • Scene Size-up – No apparent injury. He said he felt sick. • What kind of problem: Trauma? Medical?
Scenario 4: Emergency • Adult male walks into clinic. Looks pale, says he feels very sick and needs to lie down. • As you start to get him onto exam table, he faints. • Where to start in CHAM? • Inside Front Cover: Emergency, go to p. 40. • Scene Size-up – No apparent injury. He said he felt sick. • What kind of problem: Trauma? Medical?
 Scenario 4: Emergency • Medical Emergency Adult: go to p. 72. • Looks like emergency field handbook • Differences from handbook – References to cold weather care – Transport to clinic – Plans are expanded to include medicines and more detailed care in clinic while waiting to talk to doctor.
Scenario 4: Emergency • Medical Emergency Adult: go to p. 72. • Looks like emergency field handbook • Differences from handbook – References to cold weather care – Transport to clinic – Plans are expanded to include medicines and more detailed care in clinic while waiting to talk to doctor.
 Scenario 4: Emergency • Patient wakes up enough to tell you he has had chest pain and felt faint for about 2 hours. • Follow steps to Chest Pain listing on p. 73. • Go to p. 90. • Emergency care, if not already done. • Get history, exam. • You decide Assessment is Chest Pain, Possible Heart Attack. • Go to p. 95, Plan Emergency 33 while trying to contact doctor.
Scenario 4: Emergency • Patient wakes up enough to tell you he has had chest pain and felt faint for about 2 hours. • Follow steps to Chest Pain listing on p. 73. • Go to p. 90. • Emergency care, if not already done. • Get history, exam. • You decide Assessment is Chest Pain, Possible Heart Attack. • Go to p. 95, Plan Emergency 33 while trying to contact doctor.
 • • • Scenario 4: Emergency What medicine should you give? ASA and Nitroglycerin Morphine, ONLY after talking to doctor What additional care? Start an IV While waiting to transport – Recheck vital signs – Continue this plan – Go to p. 102, Emergency 38, Care of Patient While Waiting for Medevac
• • • Scenario 4: Emergency What medicine should you give? ASA and Nitroglycerin Morphine, ONLY after talking to doctor What additional care? Start an IV While waiting to transport – Recheck vital signs – Continue this plan – Go to p. 102, Emergency 38, Care of Patient While Waiting for Medevac
 Scenario 5: Sick Child Younger than 8 Years • 2 year old comes in fussy, fever, pulling at left ear, runny nose, cough. • Inside front cover to p. 1. – Box Young Child Who May be Very Sick • Child has none of those findings. • Back to Inside Front Cover Begin History
Scenario 5: Sick Child Younger than 8 Years • 2 year old comes in fussy, fever, pulling at left ear, runny nose, cough. • Inside front cover to p. 1. – Box Young Child Who May be Very Sick • Child has none of those findings. • Back to Inside Front Cover Begin History
 Scenario 5: Sick Child Younger than 8 Years • Mom brings 2 month old into clinic, says baby is sick • Inside front cover to p. 1, Sick Child Box • Baby looks very sick, pale, sweating, breathing very fast and grunting • Go to p. 68 • Very similar to Emergency Field Handbook
Scenario 5: Sick Child Younger than 8 Years • Mom brings 2 month old into clinic, says baby is sick • Inside front cover to p. 1, Sick Child Box • Baby looks very sick, pale, sweating, breathing very fast and grunting • Go to p. 68 • Very similar to Emergency Field Handbook
 Scenario 6: Recheck Visit • 3 1/2 year old brought to clinic by mom 3 days after being treated for Strep throat. Mom wants to be sure he is better. • Where do you start? • Recheck visit, inside back cover. • Child is better, eating some. Playing. Still taking Amoxicillin • Where do you go now? • Index: Strep throat or look at old PEF • p. 300, Strep throat Plan, recheck section.
Scenario 6: Recheck Visit • 3 1/2 year old brought to clinic by mom 3 days after being treated for Strep throat. Mom wants to be sure he is better. • Where do you start? • Recheck visit, inside back cover. • Child is better, eating some. Playing. Still taking Amoxicillin • Where do you go now? • Index: Strep throat or look at old PEF • p. 300, Strep throat Plan, recheck section.
 Scenario 6: Recheck Visit • Taking fluids well. • Exam: GA: looks well. Running around clinic room. • T 98° rectally • Throat: A little red, swollen tonsils. No white patches or bad breath. • Is patient better? • When should this patient be reported? • Only if not getting better.
Scenario 6: Recheck Visit • Taking fluids well. • Exam: GA: looks well. Running around clinic room. • T 98° rectally • Throat: A little red, swollen tonsils. No white patches or bad breath. • Is patient better? • When should this patient be reported? • Only if not getting better.
 Scenario 7: Follow-up After Hospital or Regional Clinic Visit • Patient just came home from hospital after an operation. • Where do you start? • Inside Front Cover sends you to p. 737 • Information you need for this visit: – Try to get this information before you see the patient – Otherwise do history and exam, then contact doctor to complete visit
Scenario 7: Follow-up After Hospital or Regional Clinic Visit • Patient just came home from hospital after an operation. • Where do you start? • Inside Front Cover sends you to p. 737 • Information you need for this visit: – Try to get this information before you see the patient – Otherwise do history and exam, then contact doctor to complete visit
 Scenario 7: Follow-up After Hospital or Regional Clinic Visit • Patient had gall bladder surgery one week ago • History • What do you examine? • GA, VS, Wt, Abdomen • Telehealth? • Lab?
Scenario 7: Follow-up After Hospital or Regional Clinic Visit • Patient had gall bladder surgery one week ago • History • What do you examine? • GA, VS, Wt, Abdomen • Telehealth? • Lab?
 Scenario 7: Follow-up After Hospital or Regional Clinic Visit • Assessment • Follow-up after Gall Bladder Surgery (date) • Plan: how much can you do? • Report • Tell patient to come back to clinic after you talk to doctor
Scenario 7: Follow-up After Hospital or Regional Clinic Visit • Assessment • Follow-up after Gall Bladder Surgery (date) • Plan: how much can you do? • Report • Tell patient to come back to clinic after you talk to doctor
 Scenario 8: Chronic Care Visit • Patient needs refill of blood pressure medicine. • Where do you start? • Inside Front Cover sends you to Inside back cover • Find High Blood Pressure • p. 348
Scenario 8: Chronic Care Visit • Patient needs refill of blood pressure medicine. • Where do you start? • Inside Front Cover sends you to Inside back cover • Find High Blood Pressure • p. 348
 Scenario 8: Chronic Care Visit • • Do not begin here, Begin here Information you need for this visit Things to remember History Exam Assessment Plan – Look at each patient ed info • Next visit: depends on regional pharmacy guidelines
Scenario 8: Chronic Care Visit • • Do not begin here, Begin here Information you need for this visit Things to remember History Exam Assessment Plan – Look at each patient ed info • Next visit: depends on regional pharmacy guidelines
 • • • Scenario 8: Chronic Care Visit Patient has chronic toe fungus and needs med refill Where to start? Inside front cover to Inside back cover Problem not listed, so use General Chronic Care, p. 734 For use with chronic problems not in the CHAM – Colostomy, boils, amputee stump check, etc
• • • Scenario 8: Chronic Care Visit Patient has chronic toe fungus and needs med refill Where to start? Inside front cover to Inside back cover Problem not listed, so use General Chronic Care, p. 734 For use with chronic problems not in the CHAM – Colostomy, boils, amputee stump check, etc
 Scenario 9: Preventive Care Visit • • • 2 year old needs a well child check-up Where to start? Inside front cover to Inside back cover Find Well Child Care in the list Go to p. 156
Scenario 9: Preventive Care Visit • • • 2 year old needs a well child check-up Where to start? Inside front cover to Inside back cover Find Well Child Care in the list Go to p. 156
 Scenario 9: Preventive Care Visit • • • Patient wants to lose weight Where to start? This is preventive care Inside front cover to Inside back cover Go to p. R-29
Scenario 9: Preventive Care Visit • • • Patient wants to lose weight Where to start? This is preventive care Inside front cover to Inside back cover Go to p. R-29
 Scenario 9: Preventive Care Visit • Define Preventive Care • Some of these things may seems like acute care visit – Wanting to get pregnant – Prenatal care • Review the list on inside back cover
Scenario 9: Preventive Care Visit • Define Preventive Care • Some of these things may seems like acute care visit – Wanting to get pregnant – Prenatal care • Review the list on inside back cover
 Scenario 10: New Problem • 2 year old comes in fussy, fever, pulling at left ear, runny nose, cough. • Inside front cover to p. 1. – Box Young Child Who May be Very Sick • Child has none of those findings. • Back to Inside Front Cover Begin History • Problem started 2 days ago, seems to be getting worse • Mom gave him Tylenol last night
Scenario 10: New Problem • 2 year old comes in fussy, fever, pulling at left ear, runny nose, cough. • Inside front cover to p. 1. – Box Young Child Who May be Very Sick • Child has none of those findings. • Back to Inside Front Cover Begin History • Problem started 2 days ago, seems to be getting worse • Mom gave him Tylenol last night
 Scenario 10: New Problem • Had an ear infection 6 months ago, treated with antibiotics • Past health history/Other history • No chronic illness • No meds/No allergies • Dad smokes at home • Alcohol/Drugs N/A • Never had a TB test
Scenario 10: New Problem • Had an ear infection 6 months ago, treated with antibiotics • Past health history/Other history • No chronic illness • No meds/No allergies • Dad smokes at home • Alcohol/Drugs N/A • Never had a TB test
 Scenario 10: New Problem • Female questions: N/A • High Risk? • Look at p. 1, High Risk Health Conditions box • Patient with any of these problems MUST always be reported, even if CHA/P has a current standing order for an assessment
Scenario 10: New Problem • Female questions: N/A • High Risk? • Look at p. 1, High Risk Health Conditions box • Patient with any of these problems MUST always be reported, even if CHA/P has a current standing order for an assessment
 Scenario 10: New Problem High Risk Health Conditions • These conditions may be affected by something the CHA/P does to patient or fetus – Medicines not used correctly by a sick liver – Medicines not eliminated properly by sick kidney – Medicine may affect the fetus • Immune system does not work well in many of these conditions
Scenario 10: New Problem High Risk Health Conditions • These conditions may be affected by something the CHA/P does to patient or fetus – Medicines not used correctly by a sick liver – Medicines not eliminated properly by sick kidney – Medicine may affect the fetus • Immune system does not work well in many of these conditions
 Scenario 10: New Problem • Child does not have any high risk health condition • Go to Index • Ear – problems, 235 – Plan for ……. . Only to be used for Recheck Visit • Go to p. 235 Ear Problem • Do history: Look at #5, child questions. – These questions are in every problem section that applies to a young child.
Scenario 10: New Problem • Child does not have any high risk health condition • Go to Index • Ear – problems, 235 – Plan for ……. . Only to be used for Recheck Visit • Go to p. 235 Ear Problem • Do history: Look at #5, child questions. – These questions are in every problem section that applies to a young child.
 Scenario 10: New Problem • Notice that respiratory questions are included so CHA/P does not have to also use Respiratory Illness section for mixed problems • If you decided he had a respiratory problem, there are ear questions in that section
Scenario 10: New Problem • Notice that respiratory questions are included so CHA/P does not have to also use Respiratory Illness section for mixed problems • If you decided he had a respiratory problem, there are ear questions in that section
 Scenario 10: New Problem • Exam: Child does not look sick, temp is 102. • What exam should you do? • Continue with exam on p. 236 – Weight is 30 pounds • Assessment chart: assessment is Acute Otitis Media • Plan: p. 240, Ear 3 • You have a current standing order for this assessment
Scenario 10: New Problem • Exam: Child does not look sick, temp is 102. • What exam should you do? • Continue with exam on p. 236 – Weight is 30 pounds • Assessment chart: assessment is Acute Otitis Media • Plan: p. 240, Ear 3 • You have a current standing order for this assessment
 Scenario 10: New Problem • • • Review Report statements Child has none of these problems What medicine do you give? Amoxicillin p. M-90. Turn to this page
Scenario 10: New Problem • • • Review Report statements Child has none of these problems What medicine do you give? Amoxicillin p. M-90. Turn to this page
 Scenario 10: New Problem • • All medicines have this information Name, strength, common brand names Brief description and uses Warnings: – Always read box carefully before you give the medicine • Dosing for CHAM plans: Find your patient’s assessment
Scenario 10: New Problem • • All medicines have this information Name, strength, common brand names Brief description and uses Warnings: – Always read box carefully before you give the medicine • Dosing for CHAM plans: Find your patient’s assessment
 Scenario 10: New Problem • • • What dose of Amoxicillin do you give? 12 ml (600 mg) by mouth How often? 2 times a day For how long? 10 days
Scenario 10: New Problem • • • What dose of Amoxicillin do you give? 12 ml (600 mg) by mouth How often? 2 times a day For how long? 10 days
 Scenario 10: New Problem • Information on p. M-91 is for the CHA/P – Serious side effects – Minor side effects – Storage and Preparation • Patient education is found on the next page • Xerox or print this page for patient. • Explain pertinent information to patient. – Child has an infection now. Do not explain “to prevent an infection” or “if a woman” info to parent. • Fill in any blanks
Scenario 10: New Problem • Information on p. M-91 is for the CHA/P – Serious side effects – Minor side effects – Storage and Preparation • Patient education is found on the next page • Xerox or print this page for patient. • Explain pertinent information to patient. – Child has an infection now. Do not explain “to prevent an infection” or “if a woman” info to parent. • Fill in any blanks
 Scenario 10: New Problem • • Medicine for pain/fever? Acetaminophen p. M-243 Find plan name and number Dose How often How much in one day
Scenario 10: New Problem • • Medicine for pain/fever? Acetaminophen p. M-243 Find plan name and number Dose How often How much in one day
 Scenario 10: New Problem • Go back to CHAM p. 240, Recheck • When does this patient need a Recheck? • In 3 days if fever over 101° • One month after finishing antibiotic • Where would you start Recheck Visit? • Inside front cover to Inside back cover
Scenario 10: New Problem • Go back to CHAM p. 240, Recheck • When does this patient need a Recheck? • In 3 days if fever over 101° • One month after finishing antibiotic • Where would you start Recheck Visit? • Inside front cover to Inside back cover
 Scenario 11: New Problem • 9 month old with vomiting and diarrhea for 12 hours • Where to start? • Inside front cover • Child younger than 8 years, p. 1 • Does not have any of these things • Back to Inside front cover questions • Index • Vomiting, p. 369 or Diarrhea, p. 369
Scenario 11: New Problem • 9 month old with vomiting and diarrhea for 12 hours • Where to start? • Inside front cover • Child younger than 8 years, p. 1 • Does not have any of these things • Back to Inside front cover questions • Index • Vomiting, p. 369 or Diarrhea, p. 369
 • • Scenario 11: New Problem Do not begin here, Begin here History, is you do not already know Child younger than 3 questions Exam Child looks sick, T 101. 6° rectal What exam should you do? Sick Child Screening Exam – Laminated sheet – p. 147
• • Scenario 11: New Problem Do not begin here, Begin here History, is you do not already know Child younger than 3 questions Exam Child looks sick, T 101. 6° rectal What exam should you do? Sick Child Screening Exam – Laminated sheet – p. 147
 Scenario 11: New Problem • Where to next? • p. 371, Lab tests – From instructions in child box • Assessment • Amount of Dehydration – Chart p. 372 • Assessment for Vomiting/Diarrhea – Chart p. 373
Scenario 11: New Problem • Where to next? • p. 371, Lab tests – From instructions in child box • Assessment • Amount of Dehydration – Chart p. 372 • Assessment for Vomiting/Diarrhea – Chart p. 373
 Scenario 11: New Problem • Assessment is Gastroenteritis with mild dehydration • Plan Digestive 6, p. 375 • You have a current standing order for this problem • Do you need to report? • Yes • When?
Scenario 11: New Problem • Assessment is Gastroenteritis with mild dehydration • Plan Digestive 6, p. 375 • You have a current standing order for this problem • Do you need to report? • Yes • When?
 Scenario 11: New Problem • Report NOW – Child looks sick • Do you need to report if child did NOT look sick? • Yes • Why? • Child is younger than 3 years • Child has mild dehydration
Scenario 11: New Problem • Report NOW – Child looks sick • Do you need to report if child did NOT look sick? • Yes • Why? • Child is younger than 3 years • Child has mild dehydration
 Scenario 11: New Problem • What should you do while waiting to report? (doctor is delivering a baby) • Patient Ed – Diet for Child Younger Than 2 – Preventing Spread of Communicable Disease, p. 379 • What meds can you give? • None: this med is NOT part of standing order
Scenario 11: New Problem • What should you do while waiting to report? (doctor is delivering a baby) • Patient Ed – Diet for Child Younger Than 2 – Preventing Spread of Communicable Disease, p. 379 • What meds can you give? • None: this med is NOT part of standing order
 Scenario 11: New Problem • Look at p. M-178, Promethazine • Would the doctor ever order this medicine for this patient? • No. – Warnings book says NOT to give to child younger than 2 years
Scenario 11: New Problem • Look at p. M-178, Promethazine • Would the doctor ever order this medicine for this patient? • No. – Warnings book says NOT to give to child younger than 2 years
 Scenario 11: New Problem • • Go back to p. 376. What next? Recheck: when? In one day, then every day until better
Scenario 11: New Problem • • Go back to p. 376. What next? Recheck: when? In one day, then every day until better
 Scenario 11: New Problem • If your assessment was Other Cause of Vomiting and Diarrhea, go to Digestive 9, p. 378 • Look at Report statement • Look at plan – Most assessment charts have an “Other Cause” assessment. – Plan for these is similar to plan on p. 378
Scenario 11: New Problem • If your assessment was Other Cause of Vomiting and Diarrhea, go to Digestive 9, p. 378 • Look at Report statement • Look at plan – Most assessment charts have an “Other Cause” assessment. – Plan for these is similar to plan on p. 378
 Summary of Changes • Look at handout, CHAM, table of contents at beginning of each chapter • Emergency Childbirth • Child/Teen
Summary of Changes • Look at handout, CHAM, table of contents at beginning of each chapter • Emergency Childbirth • Child/Teen
 Summary of Changes: Child Scenario • Mom brings in 1 year old who has fever and is fussy. • Where to start? • Inside front cover to p. 1 • Child has none of these • Back to Inside front cover • Problem is fever • Index
Summary of Changes: Child Scenario • Mom brings in 1 year old who has fever and is fussy. • Where to start? • Inside front cover to p. 1 • Child has none of these • Back to Inside front cover • Problem is fever • Index
 Summary of Changes: Child Scenario • Fever – Child younger than 8 years, p. 145 • Fussy: index, p. 145 • Just sick, no specific problem – Inside front cover right hand column, sends to p. 145 • Go to p. 145, Young child who may be sick – Review at all pages in this section
Summary of Changes: Child Scenario • Fever – Child younger than 8 years, p. 145 • Fussy: index, p. 145 • Just sick, no specific problem – Inside front cover right hand column, sends to p. 145 • Go to p. 145, Young child who may be sick – Review at all pages in this section
 Summary of Changes • Look at rest of Child/Teen chapter • Elders, p. 189 – – Look at table of contents Flip through chapter History and plan are arranged by body system All should have a screening elder exam • Eye • Ear • Mouth/Teeth
Summary of Changes • Look at rest of Child/Teen chapter • Elders, p. 189 – – Look at table of contents Flip through chapter History and plan are arranged by body system All should have a screening elder exam • Eye • Ear • Mouth/Teeth
 Summary of Changes • • Respiratory Circulatory Digestive Musculoskeletal – History, p. 397 – Exams, p. 400
Summary of Changes • • Respiratory Circulatory Digestive Musculoskeletal – History, p. 397 – Exams, p. 400
 Summary of Changes • Skin/Soft Tissue – One chapter – Wounds • Infection: Cellulitis, p. 454 • Look at medicines for type of injury and resistant bacteria (MRSA) Burns, p. 467 • Starts the same way as Emergency chapter and Emergency Field Handbook
Summary of Changes • Skin/Soft Tissue – One chapter – Wounds • Infection: Cellulitis, p. 454 • Look at medicines for type of injury and resistant bacteria (MRSA) Burns, p. 467 • Starts the same way as Emergency chapter and Emergency Field Handbook
 Summary of Changes • • Urinary Male Reproductive Female Reproductive Pregnancy – Look at table of contents, p. 563
Summary of Changes • • Urinary Male Reproductive Female Reproductive Pregnancy – Look at table of contents, p. 563
 Scenario 12: Pregnancy chapter • 30 year old pregnant woman here for 32 weeks check-up. First pregnancy. • Where to start? • Inside front cover to inside back cover, Preventive Care • Return Prenatal Visit, p. 574 • Look at Things to Remember and Information for CHA/P charts
Scenario 12: Pregnancy chapter • 30 year old pregnant woman here for 32 weeks check-up. First pregnancy. • Where to start? • Inside front cover to inside back cover, Preventive Care • Return Prenatal Visit, p. 574 • Look at Things to Remember and Information for CHA/P charts
 Scenario 12: Pregnancy chapter • What next? • Weight: 158, up 5 ½ pounds. Urine dip ok. BP 144/92. • Calculate birth/due date • History • Feels well, but a little tired. Was diagnosed with high blood sugar 4 weeks ago, seen at hospital and sent home with diet and exercise.
Scenario 12: Pregnancy chapter • What next? • Weight: 158, up 5 ½ pounds. Urine dip ok. BP 144/92. • Calculate birth/due date • History • Feels well, but a little tired. Was diagnosed with high blood sugar 4 weeks ago, seen at hospital and sent home with diet and exercise.
 Scenario 12: Pregnancy chapter • No signs of problem in pregnancy (danger signs). No contractions. Blood sugars at home 100 -200. No signs of preeclampsia. Never had high blood pressure, but problem runs in the family. • Exam • 34 cm, head down, FHTs 140. Ankles a little swollen. Hands ok. Reflexes ok.
Scenario 12: Pregnancy chapter • No signs of problem in pregnancy (danger signs). No contractions. Blood sugars at home 100 -200. No signs of preeclampsia. Never had high blood pressure, but problem runs in the family. • Exam • 34 cm, head down, FHTs 140. Ankles a little swollen. Hands ok. Reflexes ok.
 Scenario 12: Pregnancy chapter • Assessments • For BP, go to p. 592. • High Blood Pressure in Pregnancy section can be used as part of prenatal visit, or by itself for BP check-up in a pregnant woman • Skip the things you have already done • Assessment chart, p. 591 • Gestational Hypertension • Plan: Pregnancy 5, p. 580 – Return Prenatal Visit
Scenario 12: Pregnancy chapter • Assessments • For BP, go to p. 592. • High Blood Pressure in Pregnancy section can be used as part of prenatal visit, or by itself for BP check-up in a pregnant woman • Skip the things you have already done • Assessment chart, p. 591 • Gestational Hypertension • Plan: Pregnancy 5, p. 580 – Return Prenatal Visit
 Scenario 12: Pregnancy chapter • You have a current standing order • Do you need to report this patient? • Always report. – She has high blood pressure and diabetes • What should you do while waiting to report? • Special Care and Patient Ed • Look at Additional Care: does she need any of this?
Scenario 12: Pregnancy chapter • You have a current standing order • Do you need to report this patient? • Always report. – She has high blood pressure and diabetes • What should you do while waiting to report? • Special Care and Patient Ed • Look at Additional Care: does she need any of this?
 Scenario 12: Pregnancy chapter • Also do #6 on p. 581 • When to recheck? • Every 2 weeks, plus any extra visits for high blood pressure or diabetes
Scenario 12: Pregnancy chapter • Also do #6 on p. 581 • When to recheck? • Every 2 weeks, plus any extra visits for high blood pressure or diabetes
 Scenario 13: Pregnancy chapter • 14 weeks pregnant, had normal prenatal check-up 2 weeks ago • Today comes to clinic with spotting bright red blood from vagina. No cramping • Is this a preventive care visit? • No • Where to begin?
Scenario 13: Pregnancy chapter • 14 weeks pregnant, had normal prenatal check-up 2 weeks ago • Today comes to clinic with spotting bright red blood from vagina. No cramping • Is this a preventive care visit? • No • Where to begin?
 Scenario 13: Pregnancy chapter • • • Inside front cover Vaginal bleeding in pregnancy Index Vaginal bleeding p. 600 – Notice plans listed in index: for recheck only • If CHA/P comes here directly, only questions missed will be Past Health Hx, which she/he should already have. • Briefly look through this section
Scenario 13: Pregnancy chapter • • • Inside front cover Vaginal bleeding in pregnancy Index Vaginal bleeding p. 600 – Notice plans listed in index: for recheck only • If CHA/P comes here directly, only questions missed will be Past Health Hx, which she/he should already have. • Briefly look through this section
 Scenario 13: Pregnancy chapter • Same patient came to clinic for routine prenatal check-up, and had started spotting that morning • p. 577 would bump her out to p. 600 • Plan Pregnancy 12, p. 601
Scenario 13: Pregnancy chapter • Same patient came to clinic for routine prenatal check-up, and had started spotting that morning • p. 577 would bump her out to p. 600 • Plan Pregnancy 12, p. 601
 Pregnancy chapter • All of the Prenatal Problems sections are designed to be stand-alone, or used with the Return Prenatal Visit – CHA/P would look for “if not already done” statement in history and exam • Major change in Preeclampsia assessment – High BP is defined as 140/90 or higher • Prenatal Glucose Tolerance Test patient visit
Pregnancy chapter • All of the Prenatal Problems sections are designed to be stand-alone, or used with the Return Prenatal Visit – CHA/P would look for “if not already done” statement in history and exam • Major change in Preeclampsia assessment – High BP is defined as 140/90 or higher • Prenatal Glucose Tolerance Test patient visit
 Summary of Changes • Nervous – 4 seizure sections – Emergency: Having a Seizure Now – Seizure: nervous system problem section – Seizure Disorder, Chronic Care – Pregnancy: Seizure in a Pregnant Woman • Endocrine – Look at table of contents, p. 653 – Steroid-dependent patient: Includes adrenogenital syndrome
Summary of Changes • Nervous – 4 seizure sections – Emergency: Having a Seizure Now – Seizure: nervous system problem section – Seizure Disorder, Chronic Care – Pregnancy: Seizure in a Pregnant Woman • Endocrine – Look at table of contents, p. 653 – Steroid-dependent patient: Includes adrenogenital syndrome
 Summary of Changes • Immune System: new chapter • 30 year old man comes to clinic feeling “bum. ” • Where do you start? • Inside Front Cover • Started a few days ago feeling sick, tired, weak, hot and cold. Getting worse. • No allergies, no meds, smokes 5 sticks a day, no alcohol.
Summary of Changes • Immune System: new chapter • 30 year old man comes to clinic feeling “bum. ” • Where do you start? • Inside Front Cover • Started a few days ago feeling sick, tired, weak, hot and cold. Getting worse. • No allergies, no meds, smokes 5 sticks a day, no alcohol.
 Scenario: Immune System • • What next? Index Look up fever Look up feeling Look up tired Look up fatigue All take you to p. 673 Do not begin here, begin here
Scenario: Immune System • • What next? Index Look up fever Look up feeling Look up tired Look up fatigue All take you to p. 673 Do not begin here, begin here
 Scenario: Immune System • This history and exam may help you find a specific problem • You know him pretty well, and he finally tells you he used IV drugs the last 2 trips he made to town • His temp is 103. 8° and he has swollen lymph nodes everywhere • Assessment? • Fever and swollen lymph nodes
Scenario: Immune System • This history and exam may help you find a specific problem • You know him pretty well, and he finally tells you he used IV drugs the last 2 trips he made to town • His temp is 103. 8° and he has swollen lymph nodes everywhere • Assessment? • Fever and swollen lymph nodes
 Scenario: Immune System • When to report? • Could report now if you think patient looks sick • Does he have high risk behavior for HIV? – p. 682 • Notice there is patient ed box for fever
Scenario: Immune System • When to report? • Could report now if you think patient looks sick • Does he have high risk behavior for HIV? – p. 682 • Notice there is patient ed box for fever
 Immune System • Look at table of contents, p. 673 • Patient getting cancer treatment – Section for any patient who has had treatment for cancer in the last 3 month – Look at High Risk Health Conditions, p. l, Cancer
Immune System • Look at table of contents, p. 673 • Patient getting cancer treatment – Section for any patient who has had treatment for cancer in the last 3 month – Look at High Risk Health Conditions, p. l, Cancer
 Summary of Changes: Immune Chapter • HIV or AIDS – General Information – Testing • Advanced HIV or AIDS patient visit
Summary of Changes: Immune Chapter • HIV or AIDS – General Information – Testing • Advanced HIV or AIDS patient visit
 Summary of Changes • Mental Health table of contents, p. 693 • Alcohol/Drug table of contents, p. 717 – Look at Assessment chart, p. 720 to 723 – Inhalant abuse assessment and plan – Chronic Alcohol/Drug Abuse section is primarily used when patient wants to get treatment for addiction • Designed to provide information for detox center to determine admission
Summary of Changes • Mental Health table of contents, p. 693 • Alcohol/Drug table of contents, p. 717 – Look at Assessment chart, p. 720 to 723 – Inhalant abuse assessment and plan – Chronic Alcohol/Drug Abuse section is primarily used when patient wants to get treatment for addiction • Designed to provide information for detox center to determine admission
 Summary of Changes • Other Topics – Table of contents, p. 733 – Summaries • Alcohol and Drug Use and Injury Prevention • Referred to frequently from problem-specific sections • More detailed information can be found in Alcohol chapter and Wellness – Recognizing and Reporting Abuse and Neglect • Summary: more detail found in age-specific or problemspecific chapters • Internet Resources – Here and at the end of many chapters
Summary of Changes • Other Topics – Table of contents, p. 733 – Summaries • Alcohol and Drug Use and Injury Prevention • Referred to frequently from problem-specific sections • More detailed information can be found in Alcohol chapter and Wellness – Recognizing and Reporting Abuse and Neglect • Summary: more detail found in age-specific or problemspecific chapters • Internet Resources – Here and at the end of many chapters
 CHAM Medicine Handbook • Inside front cover • Look at Table of Contents, p. M-3 • Contains only meds listed in CHAM and stocked in village clinics • How to use chapter • Medicine skills – Injections chart, p. M-24 – Controlled medicines, p. M-14 – Medicine errors, p. M-16
CHAM Medicine Handbook • Inside front cover • Look at Table of Contents, p. M-3 • Contains only meds listed in CHAM and stocked in village clinics • How to use chapter • Medicine skills – Injections chart, p. M-24 – Controlled medicines, p. M-14 – Medicine errors, p. M-16
 CHAM Medicine Handbook • • • Immunizations Look at charts What are side effects of DTa. P? p. M-50 What is the minimum age you can give IPV? p. M-54 What vaccines should a 6 month old get? p. M-55 What is the dose of Hepatitis B vaccine for an adult? • p. M-57
CHAM Medicine Handbook • • • Immunizations Look at charts What are side effects of DTa. P? p. M-50 What is the minimum age you can give IPV? p. M-54 What vaccines should a 6 month old get? p. M-55 What is the dose of Hepatitis B vaccine for an adult? • p. M-57
 CHAM Medicine Handbook • Where can you find information about vaccination catch-up? • p. M-58, 59 • What is the dose of flu vaccine for a 12 month old? • p. M-59 • What vaccines are required for a child entering school in Alaska? • p. M-60 • Refrigerator logs
CHAM Medicine Handbook • Where can you find information about vaccination catch-up? • p. M-58, 59 • What is the dose of flu vaccine for a 12 month old? • p. M-59 • What vaccines are required for a child entering school in Alaska? • p. M-60 • Refrigerator logs
 CHAM Medicine Handbook • • Medicines in CHAM, p. M-65 P. M-67, table of contents for chapter P. M-153, table of contents for chapter P. M-431, Index – Contains only contents of Medicine Handbook
CHAM Medicine Handbook • • Medicines in CHAM, p. M-65 P. M-67, table of contents for chapter P. M-153, table of contents for chapter P. M-431, Index – Contains only contents of Medicine Handbook
 CHAM Medicine Changes • • Dextrose 50% M-71 Epinephrine M-73 IM vs SQ Naloxone M-82— 2 strengths Cefpodoxime M-103 – Notice differences in plans • Ceftriaxone M-106— 3 dose schedules • Meds for status seizures: M-225 -232 • Ibuprofen M-259
CHAM Medicine Changes • • Dextrose 50% M-71 Epinephrine M-73 IM vs SQ Naloxone M-82— 2 strengths Cefpodoxime M-103 – Notice differences in plans • Ceftriaxone M-106— 3 dose schedules • Meds for status seizures: M-225 -232 • Ibuprofen M-259
 CHAM Reference and Procedures Book • Table of Contents • Wellness • Find information about stress management • P. R-55 • Find information about Stopping Tobacco • P. R-50
CHAM Reference and Procedures Book • Table of Contents • Wellness • Find information about stress management • P. R-55 • Find information about Stopping Tobacco • P. R-50
 CHAM Reference and Procedures Book • Lab Tests • Table of contents, p. R-59 • Some are not in basic training – Included because some corporations what their CHA/Ps to do them • PAP smear • Find information about doing a urine dipstick • P. R-81. Review these pages • All tests are explained the same way
CHAM Reference and Procedures Book • Lab Tests • Table of contents, p. R-59 • Some are not in basic training – Included because some corporations what their CHA/Ps to do them • PAP smear • Find information about doing a urine dipstick • P. R-81. Review these pages • All tests are explained the same way
 CHAM Reference and Procedures Book • Procedures and Equipment – Table of contents, p. R-97 – Moved most of procedures out of main CHAM – Only ones left in main CHAM are procedures CHA/P may need to review with doctor before doing • Opening an abscess • Packing a dry socket
CHAM Reference and Procedures Book • Procedures and Equipment – Table of contents, p. R-97 – Moved most of procedures out of main CHAM – Only ones left in main CHAM are procedures CHA/P may need to review with doctor before doing • Opening an abscess • Packing a dry socket
 CHAM Reference and Procedures Book • Anatomy and Function – Use these simple drawing for patient ed • History and Exam – Very complete history – Info about recording and reporting – Screening exams for adult, child age 6 -11 – Complete exam for each body system • Medical Words and Abbreviations – Good reference section
CHAM Reference and Procedures Book • Anatomy and Function – Use these simple drawing for patient ed • History and Exam – Very complete history – Info about recording and reporting – Screening exams for adult, child age 6 -11 – Complete exam for each body system • Medical Words and Abbreviations – Good reference section
 CHAM Reference and Procedures Book • Clinic Management, p. R-273 – General information – Your region may have more specific guidelines – Needle-stick procedure • Forms, p. R-291 • End of Life Comfort Care – For patient who comes home to die – Not usually scope of practice for CHA/P
CHAM Reference and Procedures Book • Clinic Management, p. R-273 – General information – Your region may have more specific guidelines – Needle-stick procedure • Forms, p. R-291 • End of Life Comfort Care – For patient who comes home to die – Not usually scope of practice for CHA/P
 Scenario 14: End of Life Comfort Care • 70 year old woman has terminal lung cancer. Has come home to die. • Death expected within 2 months. • Family asks for a home visit to help make patient comfortable, as she is too ill to get to clinic easily. • Where do you start?
Scenario 14: End of Life Comfort Care • 70 year old woman has terminal lung cancer. Has come home to die. • Death expected within 2 months. • Family asks for a home visit to help make patient comfortable, as she is too ill to get to clinic easily. • Where do you start?
 Scenario 14: Comfort Care • • Inside front cover P. R-307, Comfort care chapter Introduction and information for this visit History – Do not need to ask all questions • Exam – Only do starred items if death is near • Assessment chart with various problems for terminally ill patients
Scenario 14: Comfort Care • • Inside front cover P. R-307, Comfort care chapter Introduction and information for this visit History – Do not need to ask all questions • Exam – Only do starred items if death is near • Assessment chart with various problems for terminally ill patients
 Scenario 14: Comfort Care • Plans – Everyone gets Comfort Care 1, p. R-311 – Use other plans as needed – Plan Comfort Care 11, p. R-318 is for the family or other caregiver • Their health is very important to maintain
Scenario 14: Comfort Care • Plans – Everyone gets Comfort Care 1, p. R-311 – Use other plans as needed – Plan Comfort Care 11, p. R-318 is for the family or other caregiver • Their health is very important to maintain
 CHAM Reference and Procedures Book • Death and Grief – Table of contents, p. R-319 • Index – Same as CHAM patient care visit book
CHAM Reference and Procedures Book • Death and Grief – Table of contents, p. R-319 • Index – Same as CHAM patient care visit book
 Medicine Practice • Fix problem on p. M-330 – Under If for Scabies, should say Do NOT take a shower before using this medicine. • Fix problem on p. 96 in CHAM – Morphine: 0. 8 mg should be 8 mg • Give 8 mg (0. 8 ml) • Doses in charts were calculated and rounded off to make measuring easier
Medicine Practice • Fix problem on p. M-330 – Under If for Scabies, should say Do NOT take a shower before using this medicine. • Fix problem on p. 96 in CHAM – Morphine: 0. 8 mg should be 8 mg • Give 8 mg (0. 8 ml) • Doses in charts were calculated and rounded off to make measuring easier
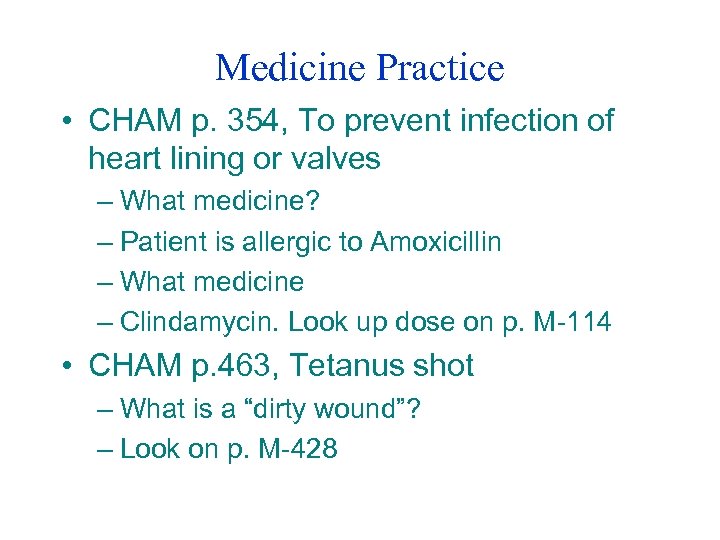 Medicine Practice • CHAM p. 354, To prevent infection of heart lining or valves – What medicine? – Patient is allergic to Amoxicillin – What medicine – Clindamycin. Look up dose on p. M-114 • CHAM p. 463, Tetanus shot – What is a “dirty wound”? – Look on p. M-428
Medicine Practice • CHAM p. 354, To prevent infection of heart lining or valves – What medicine? – Patient is allergic to Amoxicillin – What medicine – Clindamycin. Look up dose on p. M-114 • CHAM p. 463, Tetanus shot – What is a “dirty wound”? – Look on p. M-428
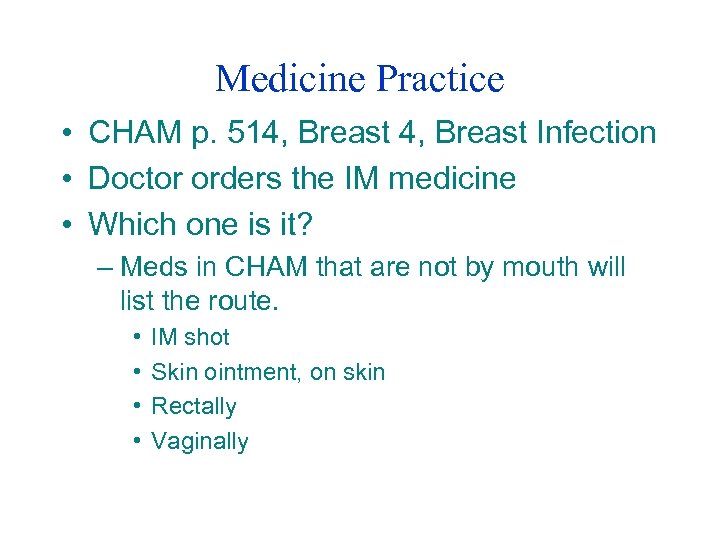 Medicine Practice • CHAM p. 514, Breast Infection • Doctor orders the IM medicine • Which one is it? – Meds in CHAM that are not by mouth will list the route. • • IM shot Skin ointment, on skin Rectally Vaginally
Medicine Practice • CHAM p. 514, Breast Infection • Doctor orders the IM medicine • Which one is it? – Meds in CHAM that are not by mouth will list the route. • • IM shot Skin ointment, on skin Rectally Vaginally
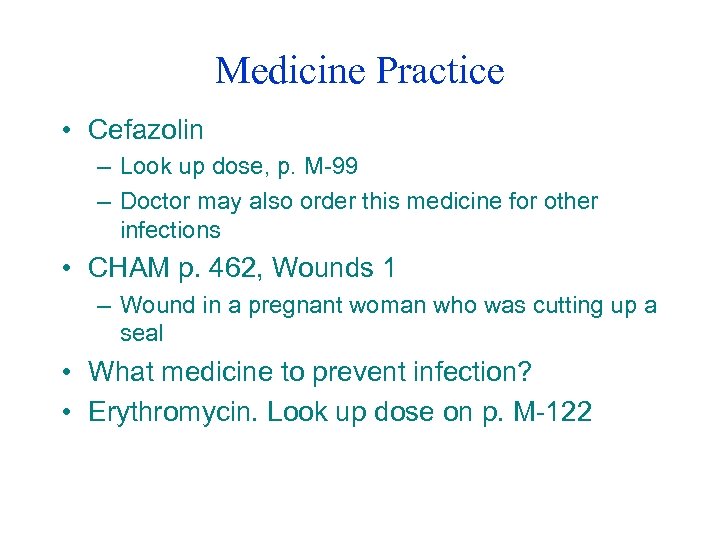 Medicine Practice • Cefazolin – Look up dose, p. M-99 – Doctor may also order this medicine for other infections • CHAM p. 462, Wounds 1 – Wound in a pregnant woman who was cutting up a seal • What medicine to prevent infection? • Erythromycin. Look up dose on p. M-122
Medicine Practice • Cefazolin – Look up dose, p. M-99 – Doctor may also order this medicine for other infections • CHAM p. 462, Wounds 1 – Wound in a pregnant woman who was cutting up a seal • What medicine to prevent infection? • Erythromycin. Look up dose on p. M-122
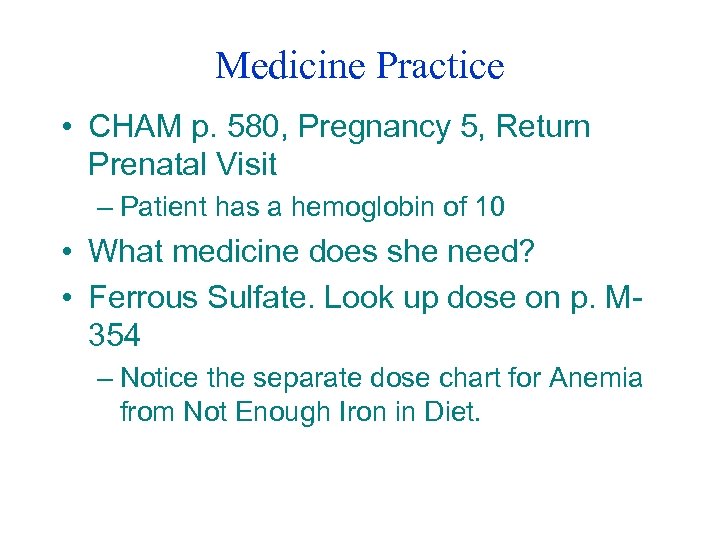 Medicine Practice • CHAM p. 580, Pregnancy 5, Return Prenatal Visit – Patient has a hemoglobin of 10 • What medicine does she need? • Ferrous Sulfate. Look up dose on p. M 354 – Notice the separate dose chart for Anemia from Not Enough Iron in Diet.
Medicine Practice • CHAM p. 580, Pregnancy 5, Return Prenatal Visit – Patient has a hemoglobin of 10 • What medicine does she need? • Ferrous Sulfate. Look up dose on p. M 354 – Notice the separate dose chart for Anemia from Not Enough Iron in Diet.
 Scenario 15 • 2 year old brought to clinic by mom with a bad cough • Inside front cover • Sick for 2 days, got worse last night. Felt a little hot. Never had before. • No allergies, no meds, no smokers in house. • No high risk health condition. • Index: cough
Scenario 15 • 2 year old brought to clinic by mom with a bad cough • Inside front cover • Sick for 2 days, got worse last night. Felt a little hot. Never had before. • No allergies, no meds, no smokers in house. • No high risk health condition. • Index: cough
 Scenario 15 • p. 290, Respiratory Illness • History • Cough worse during night and naps. Sounds like a seal. • No appetite but takes fluids well. Normal wet diapers. Normal BM. Tired, cranky.
Scenario 15 • p. 290, Respiratory Illness • History • Cough worse during night and naps. Sounds like a seal. • No appetite but takes fluids well. Normal wet diapers. Normal BM. Tired, cranky.
 Scenario 15 • Exam – GA: does not look very sick. – T 100. 8° rectally; P 130; R 32; Sp. O 2 95% – Has barky cough, sounds a little wet. Sounds hoarse and has high-pitched sound (stridor) when crying. – Chest clear, some retractions. • Assessment?
Scenario 15 • Exam – GA: does not look very sick. – T 100. 8° rectally; P 130; R 32; Sp. O 2 95% – Has barky cough, sounds a little wet. Sounds hoarse and has high-pitched sound (stridor) when crying. – Chest clear, some retractions. • Assessment?
 Scenario 15 • • • Chart p. 292 Croup Plan Respiratory 10, p. 302 When should this patient be reported? Special Care Medicines Patient Education • Recheck: When?
Scenario 15 • • • Chart p. 292 Croup Plan Respiratory 10, p. 302 When should this patient be reported? Special Care Medicines Patient Education • Recheck: When?
 Scenario 16 • 60 year old complaining of “chest cold” and cough. • Sick for 10 days, getting worse. Cough worse in the morning. Had bronchitis 2 times before in the last year. • No allergies, no meds. Smokes 2 packs/day. No interested in stopping. • No high risk health condition. • Where to now?
Scenario 16 • 60 year old complaining of “chest cold” and cough. • Sick for 10 days, getting worse. Cough worse in the morning. Had bronchitis 2 times before in the last year. • No allergies, no meds. Smokes 2 packs/day. No interested in stopping. • No high risk health condition. • Where to now?
 Scenario 16 • p. 290, Respiratory Illness • Coughing up a lot of yellow sputum. Worse in morning, and when he goes out into cold air. Feels a little more tired. Sweating some. • Has not had a flu shot this year. Never had a pneumonia shot
Scenario 16 • p. 290, Respiratory Illness • Coughing up a lot of yellow sputum. Worse in morning, and when he goes out into cold air. Feels a little more tired. Sweating some. • Has not had a flu shot this year. Never had a pneumonia shot
 Scenario 16 • Exam: GA: looks a little tired. • T 99. 8°; P 88; R 20; Sp. O 2 97% • Chest: Rhonchi all over, get better after coughing. Percussion sounds the same everywhere. • Assessment? • Bronchitis • Plan: p. 304, Respiratory 11.
Scenario 16 • Exam: GA: looks a little tired. • T 99. 8°; P 88; R 20; Sp. O 2 97% • Chest: Rhonchi all over, get better after coughing. Percussion sounds the same everywhere. • Assessment? • Bronchitis • Plan: p. 304, Respiratory 11.
 Scenario 16 • You have a current standing order for this problem • Does this patient need to be reported? • Yes, if you think patient has an infection – Coughing for 10 days, getting worse – Frequent episodes of bronchitis, he may have chronic lung disease • Patient Education Medicines: What Meds? • Recheck: When?
Scenario 16 • You have a current standing order for this problem • Does this patient need to be reported? • Yes, if you think patient has an infection – Coughing for 10 days, getting worse – Frequent episodes of bronchitis, he may have chronic lung disease • Patient Education Medicines: What Meds? • Recheck: When?
 Scenario 17 • 50 year old complaining of bad stomach pain. • Pain started 8 hours ago, getting worse. 7 on scale of 10. Started in upper left, moved to middle, now hurts everywhere. • No allergies, no meds. No tobacco or alcohol. • No high risk health condition.
Scenario 17 • 50 year old complaining of bad stomach pain. • Pain started 8 hours ago, getting worse. 7 on scale of 10. Started in upper left, moved to middle, now hurts everywhere. • No allergies, no meds. No tobacco or alcohol. • No high risk health condition.
 • • Scenario 17 Index: Abdominal Pain stomach pain p. 362, Abdominal Pain Watching TV when pain started. Started as cramping, but getting worse and worse. Hasn’t eaten, feels nauseated. Hasn’t passed any gas, would feel better if she could. Last BM yesterday morning. Had hysterectomy 10 years ago.
• • Scenario 17 Index: Abdominal Pain stomach pain p. 362, Abdominal Pain Watching TV when pain started. Started as cramping, but getting worse and worse. Hasn’t eaten, feels nauseated. Hasn’t passed any gas, would feel better if she could. Last BM yesterday morning. Had hysterectomy 10 years ago.
 Scenario 17 • Exam: GA: Looks sick, pale. • T 98. 8°; P 92; R 20 • Abdomen: no bowel sounds heard after 2 minutes. Tender everywhere, muscles feel tight. No rebound tenderness. • Assessment? • Acute Abdomen • Plan: p. 366, Digestive 2
Scenario 17 • Exam: GA: Looks sick, pale. • T 98. 8°; P 92; R 20 • Abdomen: no bowel sounds heard after 2 minutes. Tender everywhere, muscles feel tight. No rebound tenderness. • Assessment? • Acute Abdomen • Plan: p. 366, Digestive 2
 Scenario 17 • • • When should this patient be reported? Special Care Medicine: What Meds? Additional Care Recheck: When?
Scenario 17 • • • When should this patient be reported? Special Care Medicine: What Meds? Additional Care Recheck: When?
 Any Questions
Any Questions


