TEMPORO-MANDIBULAR+JOINT+(TMJ).ppt
- Количество слайдов: 120

1 TEMPOROMANDIBULAR JOINT (TMJ)
2 INTRODUCTION • The temporomandibular joint is the synovial articulation between the mandible and the cranium (the temporal bone). • This is why, it is also sometimes called as the ‘Cranio-mandibular joint’.
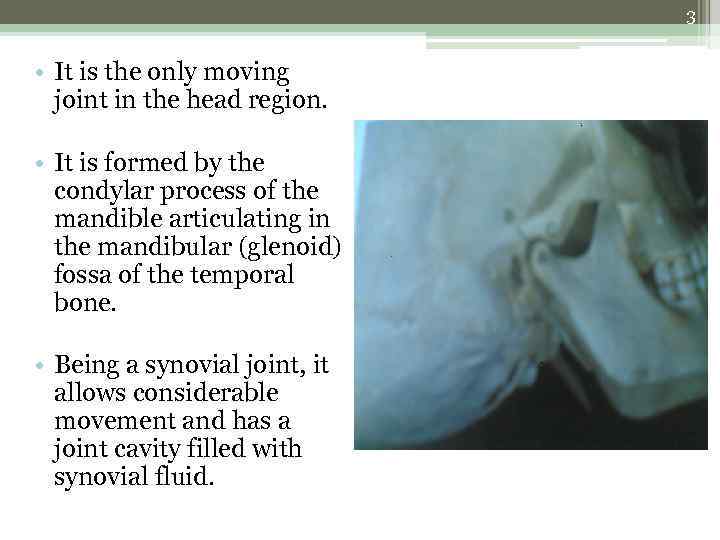
3 • It is the only moving joint in the head region. • It is formed by the condylar process of the mandible articulating in the mandibular (glenoid) fossa of the temporal bone. • Being a synovial joint, it allows considerable movement and has a joint cavity filled with synovial fluid.
4 • Being a synovial joint, TMJ has two unusual features: 1. The articular surfaces are covered with fibrous tissue (instead of usual hyaline cartilage). 2. The joint cavity is divided into two joint spaces by an intra-articular disc. The joint is unique in that the bones of its components house teeth. The shapes, alifnments and shifting occlusal engagements of these hard and unyielding units when chewing introduce an extra-ordinary influence on the positions and movements of the parts within the joint capsule.
5 STRUCTURE • The structure of TMJ is usual that of any synovial joint. • It basic structure id divided into 3 components: 1. Mandibular component. 2. Cranial component and 3. Articular component
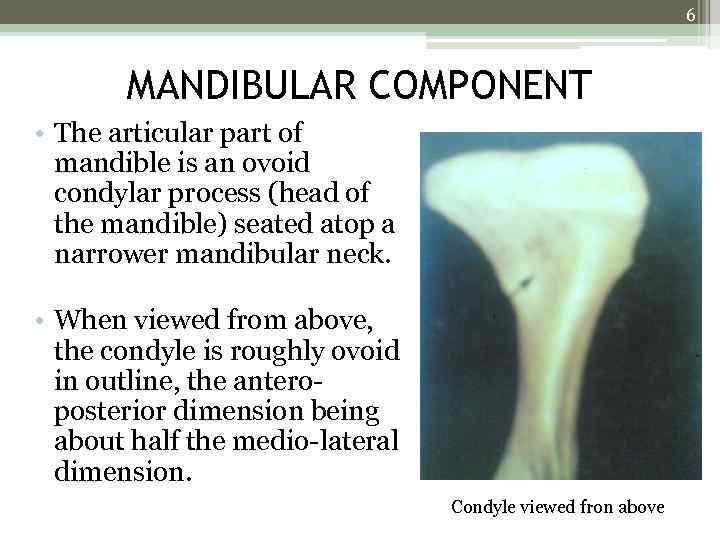
6 MANDIBULAR COMPONENT • The articular part of mandible is an ovoid condylar process (head of the mandible) seated atop a narrower mandibular neck. • When viewed from above, the condyle is roughly ovoid in outline, the anteroposterior dimension being about half the medio-lateral dimension. Condyle viewed fron above
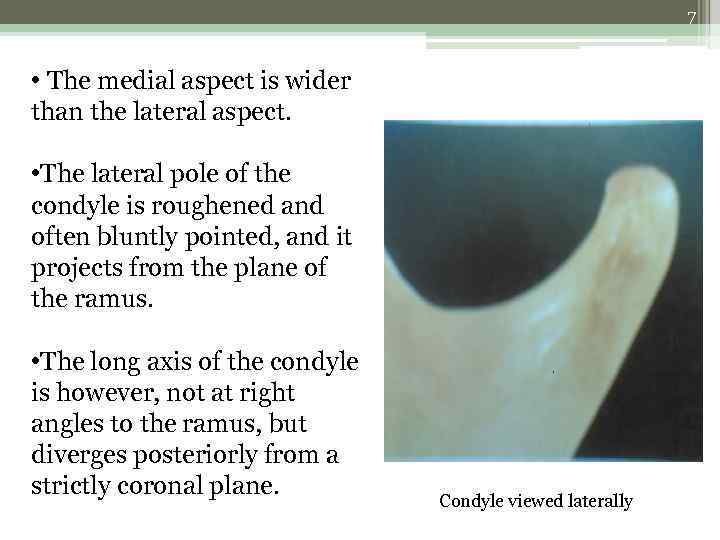
7 • The medial aspect is wider than the lateral aspect. • The lateral pole of the condyle is roughened and often bluntly pointed, and it projects from the plane of the ramus. • The long axis of the condyle is however, not at right angles to the ramus, but diverges posteriorly from a strictly coronal plane. Condyle viewed laterally
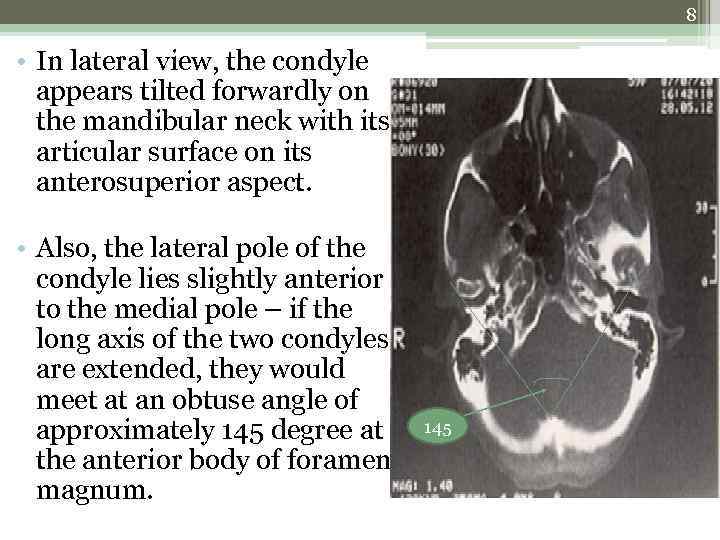
8 • In lateral view, the condyle appears tilted forwardly on the mandibular neck with its articular surface on its anterosuperior aspect. • Also, the lateral pole of the condyle lies slightly anterior to the medial pole – if the long axis of the two condyles are extended, they would meet at an obtuse angle of approximately 145 degree at the anterior body of foramen magnum. 145
9 • The articular surface continues medially downwards and around the pole of the condyle. • The condyle is around 15 -20 mm from side to side and 8 -10 mm front to back. • Also, the condyle is usually strongly convex anteroposteriorly and mildly convex mediolaterally, the convexity increasing around the medial pole.
10 • The non-articular posterior surface of the condyle is broad and flat. • The articular surface may be seperated from the non-articular surface by a slight ridge, indicating the site of attachment of the joint capsule. • The broad articular head of the condyle joins the ramus through a thin bony projection which is termed as the neck of the condyle.
11 CRANIAL COMPONENT • The articular surface of the temporal bone (facies articularis) (or the mandibular fossa) and the articular eminence constitutes the cranial component. • It is situated on the inferior aspect of the temporal squamous anterior to the tympanic element of the temporal complex.
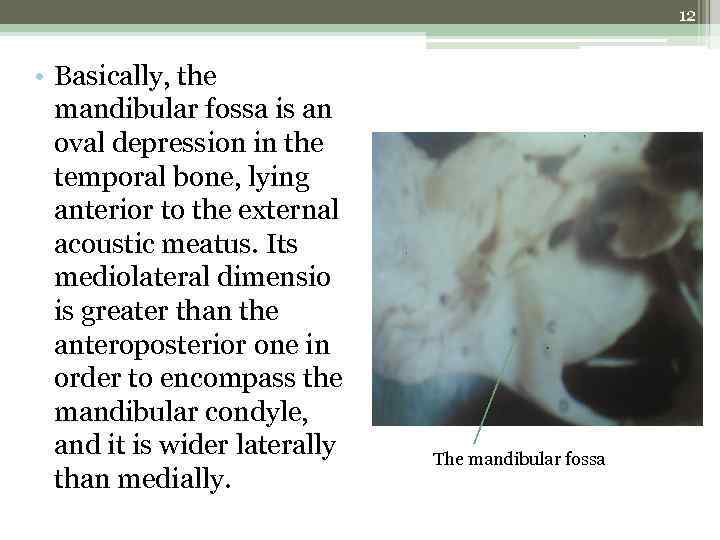
12 • Basically, the mandibular fossa is an oval depression in the temporal bone, lying anterior to the external acoustic meatus. Its mediolateral dimensio is greater than the anteroposterior one in order to encompass the mandibular condyle, and it is wider laterally than medially. The mandibular fossa
13 • The articular eminence is a small, rough, bony knob raised on the outer end of the anterior root of the zygomatic process of the temporal bone. • The pressure bearing surface here consists of 3 regions: 1. The posterior slope to the height of the convexity of the articular eminence. 2. The flattening preglenoid plane continuing anteriorly from the height of the articular eminence and; 3. The entoglenoid process continuous with the narrow medial glenoid plane on its inferior edge.
14 • The shape of the mandibular fossa do not exactly conform to the shape of the mandibular condyle. • The bones of the central part of the fossa is thin, indicating that the masticatory loads are not transferred only through the fossa, but also through the teeth and then to the facial bones and base of the cranium. The articular eminence
15 • The articular eminence is strongly convex in an anteroposterior direction and somewhat concave in a transverse direction. • The degree of its complexity is highly variable, with the radius of the curvature varying from 515 mm. • The medial and lateral borders of the articular eminence are sometimes accentuated by fine bony ridges.
16 ARTICULAR COMPONENT • The articular component is constituted by: 1. the capsule 2. the articular disc and 3. the articular ligaments. This is the main structure of the joint which contributes to the physiology of the structure.
17 CAPSULE • The capsule of the TMJ is a thin, slack cuff that limits the mandibular movements but is too weak to provide support to the joint. • Anteriorly, it is attached to the articular eminence, posteriorly to the squamo-tympanic fissure and the petro-tympanic fissures, medially to the medial glenoid plane and laterally to the lateral margin of the articular eminence.
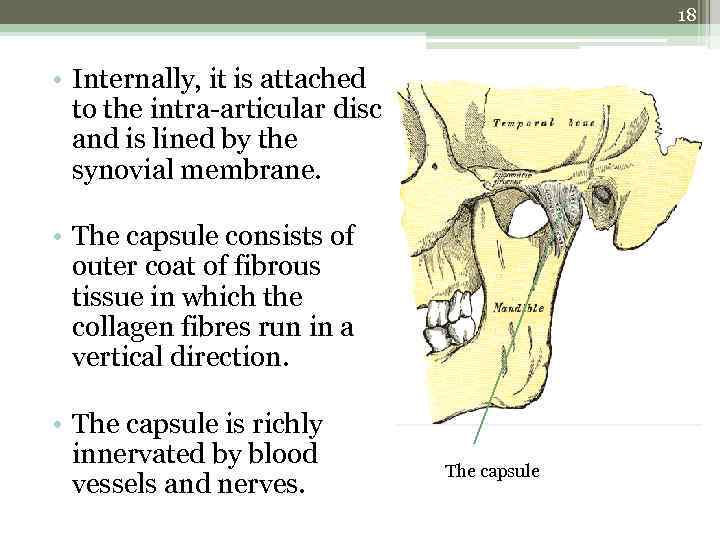
18 • Internally, it is attached to the intra-articular disc and is lined by the synovial membrane. • The capsule consists of outer coat of fibrous tissue in which the collagen fibres run in a vertical direction. • The capsule is richly innervated by blood vessels and nerves. The capsule
19 • The synovial membrane lines the capsule, but does not covers the articular surfaces. • The synovial membrane secretes the synovial fluid, which lubricates the joint (by proteoglycans), and also has nutritive function.
20 ARTICULAR LIGAMENTS • The joint capsule is strengthened by the temporo -mandibular (lateral) ligaments. This ligament cannot be separated from the capsule. • The ligament on each side is designed in two layers, a wide outer or superficial layer, and a narrow inner or deep band. • This ligament provides the main means for supportfor the joint, restricting distal and inferior movements of the mandible and resisting dislocations.
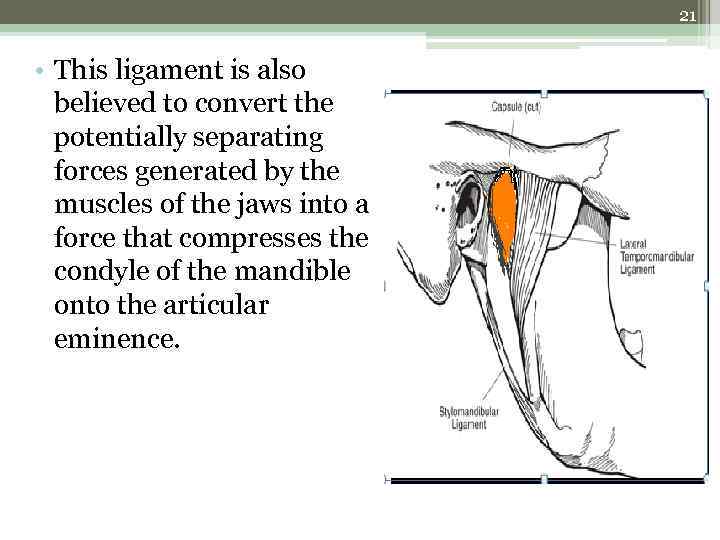
21 • This ligament is also believed to convert the potentially separating forces generated by the muscles of the jaws into a force that compresses the condyle of the mandible onto the articular eminence.
22 • The ligament has no medial attachment, it only attaches laterally to the joint, so that the right and left articulations may operate as a single joint. • Thus, when the condyles are at rest, the medial slippage of the condyles is prevented by the entoglenoid processes and the lateral slippage by the temporo-mandibular ligament. • This arrangement is remarkably similar to that of the knee joint.
23 ACCESORY LIGAMENTS • The accessory ligaments are the ‘stylomandibular ligament’ and the ‘sphenomandibular ligament’. • Only the stylomandibular ligament is believed to have significant influence on mandibular movements as the sphenomandibular ligament remains passive during jaw movements. • Both these ligaments act in conjunction with the temporomandibular ligament to support the joint. • Recently, a new ligament has been described named as the retinacular ligament. This is in association with the temporomandibular ligament.
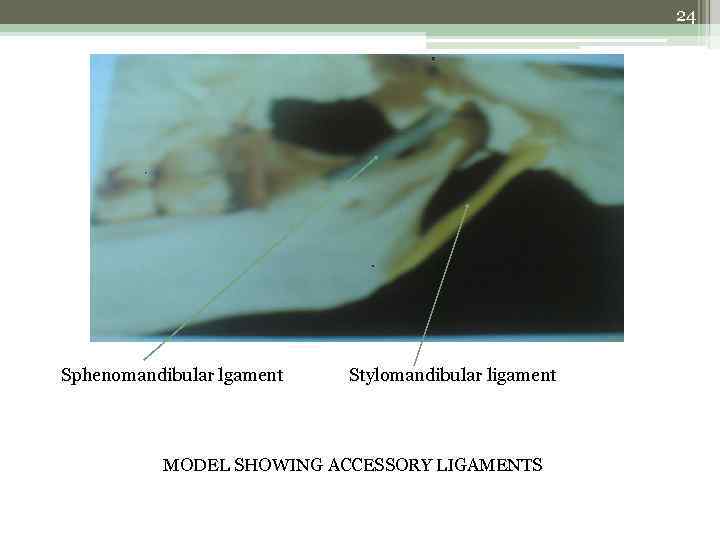
24 Sphenomandibular lgament Stylomandibular ligament MODEL SHOWING ACCESSORY LIGAMENTS
25 THE ARTICULAR COVERINGS • The smooth, slippery, pressure bearing tissue carpeting the surface of bones are the articulating surfaces. • In mandible, a bed of tough collagen fibers, bound by glycoproteins cover the condyle. It is around 0. 37 mm laterally and 0. 48 mm medially. • On the same temporal counterpart, the tissue measures 0. 49 mm and 0. 36 mm for eminence and plane, decreasing to about 0. 45 mm and 0. 34 mm medially. • The depth of the mandibular fossa is just covered by the periosteum, 0. 07 mm thick.
26 THE ARTICULAR DISC • The articular disc (meniscus), is of a dense fibrous consistency, and is moulded by the joint surfaces above and below. • Above, the disc covers the slope of the articular eminence and below it covers the condyle. In sagittal section, the upper surface of the disc appears concavo-convex from front to back and the lower surface appears concave.
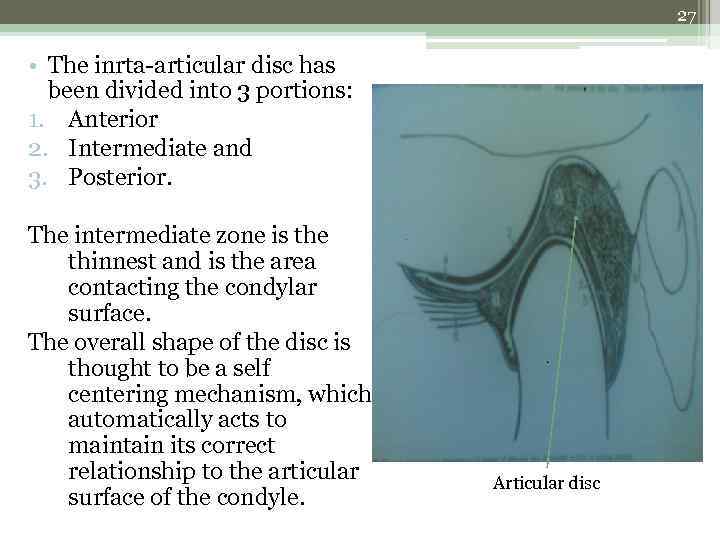
27 • The inrta-articular disc has been divided into 3 portions: 1. Anterior 2. Intermediate and 3. Posterior. The intermediate zone is the thinnest and is the area contacting the condylar surface. The overall shape of the disc is thought to be a self centering mechanism, which automatically acts to maintain its correct relationship to the articular surface of the condyle. Articular disc

28 • The margins of the intra-articular disc merges peripherally with the joint capsule. • Anteriorly, the fibrous bands connect the disc to anterior margin of the eminence. Medially and laterally, it is attached to the capsule and posteriorly it is attached to the bilaminar zone (retrodiscal tissue/pad). • The size of the spongy retrodiscal tissue here appears very large, due to engorgement of blood vessels which equilibriates the intracapsular pressure with the surroundings.
29 • The intra-articular disc divides the TMJ into superior and inferior compartments, both of which contains around 1 ml of synovial fluid. • The distinctive shape of the fibrocartilagenous disc seems to be mechanically designed to cup around the condyle in conveying it back and forth over the articular slope, eminence and the preglenoid plane. At the same time, its thinner central third is the most flexible segment which allows the disc to bend around the crest of the eminence on its way to the preglenoid plane.
30 BLOOD SUPPLY • The blood supply to the joint is profuse. • Major arterial donations come from large superficial temporal and maxillary arteries posteriorly, and the smaller posterior deep temporal, massetric and the lateral pterygoid terminals anteriorly. • The venous pattern is more diffuse and forms a plexus around the capsule.
31 NERVE SUPPLY • The mandibular nerve, the third and the major division of the trigrminal nerve, innervates the joint. • Three branches from the mandibular nerve are found sending terminals to the joint. • The largest is the auriculotemporal nerve, which supplies the posterior, medial and lateral parts of the joint. • The next 2 segments, the massetric nerve, and a branch of posterior deep temporal nerve, supplies the anterior part.
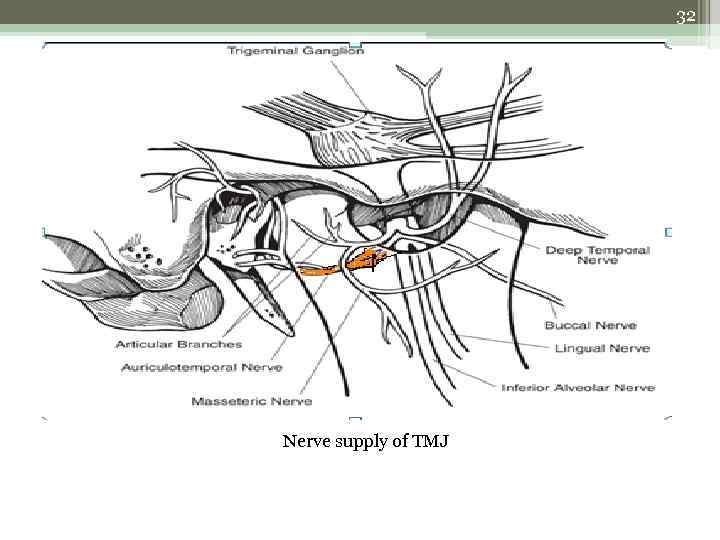
32 Nerve supply of TMJ
33 FORCES, POSTURES AND MOVEMENTS • The bone-muscle-joint-nerve complex of the apparatus acts as one integrated unit for making mouth movements. • The motion of amndible is analyzed as an interaction between two rigid constructs joined together in a special way. • The mandible is actually a class III lever (the fulcrum is placed at one end, the load at another and the effort force is in between).
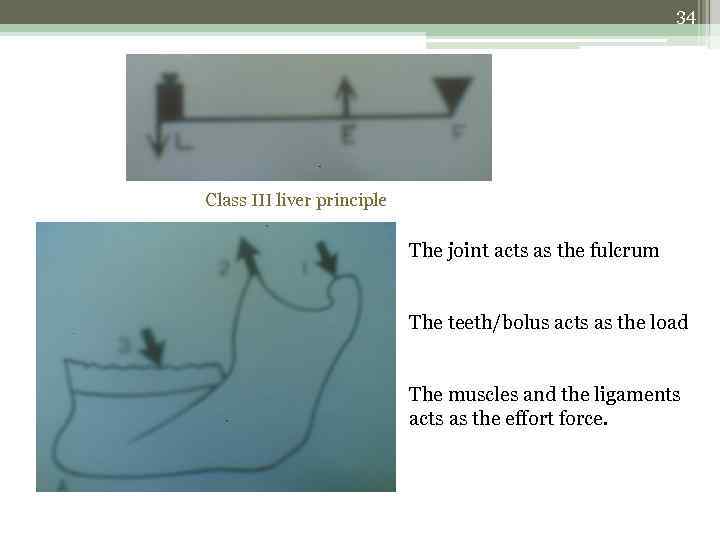
34 Class III liver principle The joint acts as the fulcrum The teeth/bolus acts as the load The muscles and the ligaments acts as the effort force.
35 FORCES • The articular surfaces of the joint are never flat and their curvatures vary from region to region. When the joint moves, limited areas of opposing pressure bearing contacts are constantly shifting. This ensures that pressure will rarely settle on a small area for long. • As the pressure increases, the contact areas spread and the load is dispersed over a broader expanse.
36 POSTURE • It is furthur divided into 5 types: 1. resting posture. 2. hinge posture. 3. centric occlusal posture. 4. protrusive occlusal posture. 5. lateral occlusive posture.
37 RESTING POSTURE • It is the position of mandible when all the musculature is ‘at rest’. • The resting posture actually varies with the person’s activity and cannot be described as a definite position (non-reproducible). • The resting tonus indicates the balance between the innate elasticity of the muscles and fibres with the gravitational pull of the mandible.
38 HINGE POSTURE • It is the posture in which condyles stop at their most retrudable limits when the teeth are barely free of occlusion. The clinical registration of this posture is repeatable. • In this posture, the condyles press against the thick rear rims of the fibrous discs and the spongy retrodiscal pads in the articular fossa. • The hinge movement rotates around a common transverse axis that runs through the approximate centres of the condyles.
39 CENTRIC OCCLUSAL POSTURE • Centric occlusion expresses a concept of normal mandibular posture in which the dentition is occluded with all teeth fully interdigitated. • The condyles in this position are rotated slightly backward from the resting posture. • In a majority of cases, the mandible in this position can still be retruded for about 0. 5 to 1 mm, indicating a normally balanced oral apparatus.
40 PROTRUSIVE OCCLUSAL POSTURE • The incisal edges of the four lower incisors are in contact with the incisal edges of upper centrals. The condyles here are slightly rotated forward from the centric position and moved downward and forward to a position on or a near the peak of the articular eminence.
41 LATERAL OCCLUSAL POSTURE • The upper and lower posterior teeth on the ipsilateral side are in contact along the line of the buccal and lingual cusps of unworn teeth in young adults. • The worn teeth in mature dentitions produce a flat continuous area as the cuspal levels are worned off.
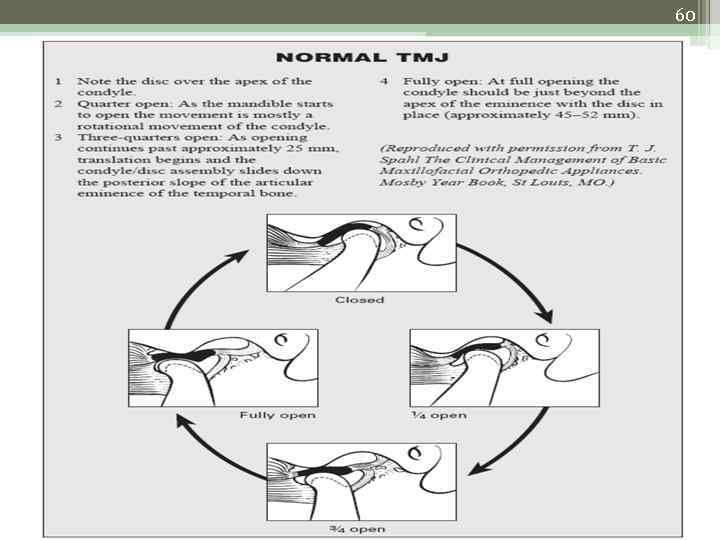
42 MOVEMENTS • Movemensof the mandible are most commonly ascribed to rotation in the lower joint compartment and rotation+translation in the upper joint compartment. • The movements of mandible are classified under: 1. Basic movements. 2. Marginal movements and 3. Functional movements.
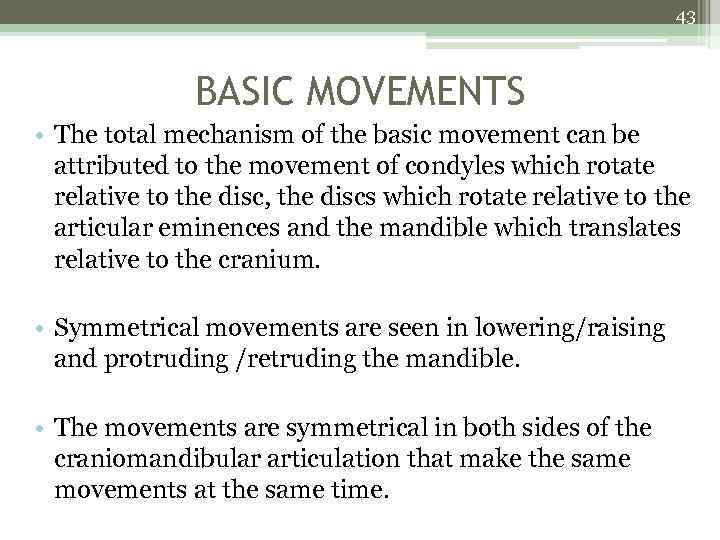
43 BASIC MOVEMENTS • The total mechanism of the basic movement can be attributed to the movement of condyles which rotate relative to the disc, the discs which rotate relative to the articular eminences and the mandible which translates relative to the cranium. • Symmetrical movements are seen in lowering/raising and protruding /retruding the mandible. • The movements are symmetrical in both sides of the craniomandibular articulation that make the same movements at the same time.
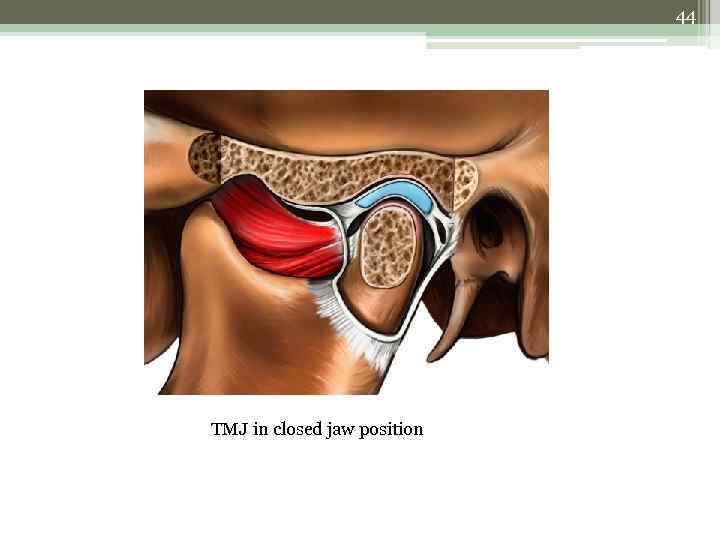
44 TMJ in closed jaw position
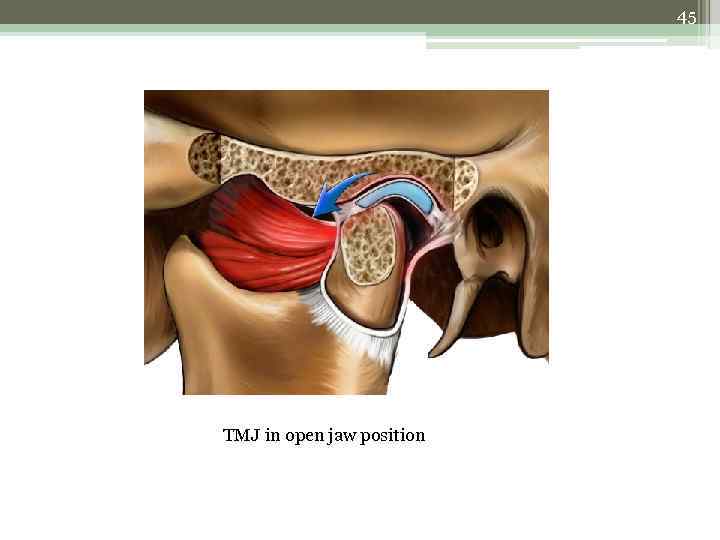
45 TMJ in open jaw position
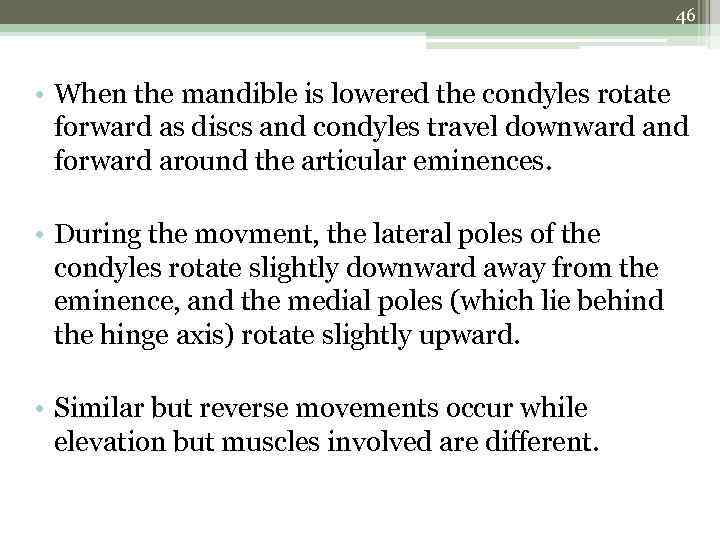
46 • When the mandible is lowered the condyles rotate forward as discs and condyles travel downward and forward around the articular eminences. • During the movment, the lateral poles of the condyles rotate slightly downward away from the eminence, and the medial poles (which lie behind the hinge axis) rotate slightly upward. • Similar but reverse movements occur while elevation but muscles involved are different.
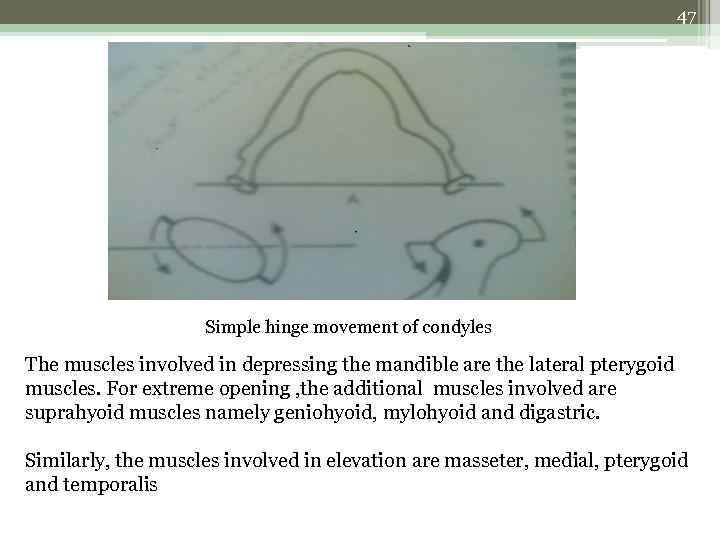
47 Simple hinge movement of condyles The muscles involved in depressing the mandible are the lateral pterygoid muscles. For extreme opening , the additional muscles involved are suprahyoid muscles namely geniohyoid, mylohyoid and digastric. Similarly, the muscles involved in elevation are masseter, medial, pterygoid and temporalis
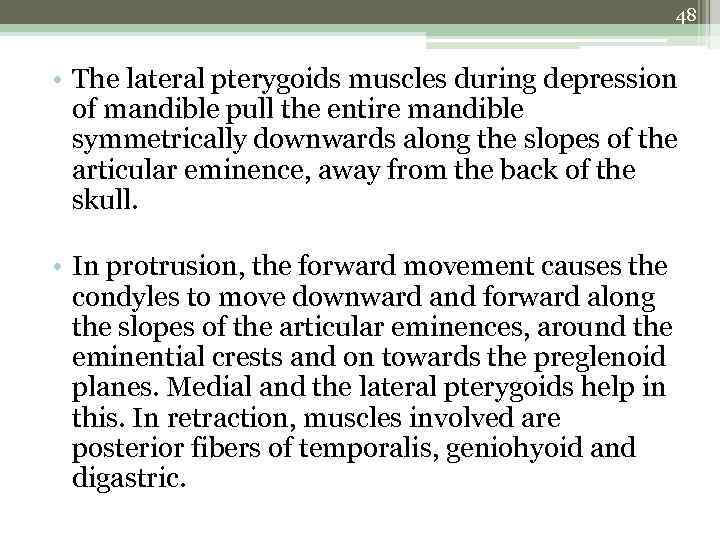
48 • The lateral pterygoids muscles during depression of mandible pull the entire mandible symmetrically downwards along the slopes of the articular eminence, away from the back of the skull. • In protrusion, the forward movement causes the condyles to move downward and forward along the slopes of the articular eminences, around the eminential crests and on towards the preglenoid planes. Medial and the lateral pterygoids help in this. In retraction, muscles involved are posterior fibers of temporalis, geniohyoid and digastric.
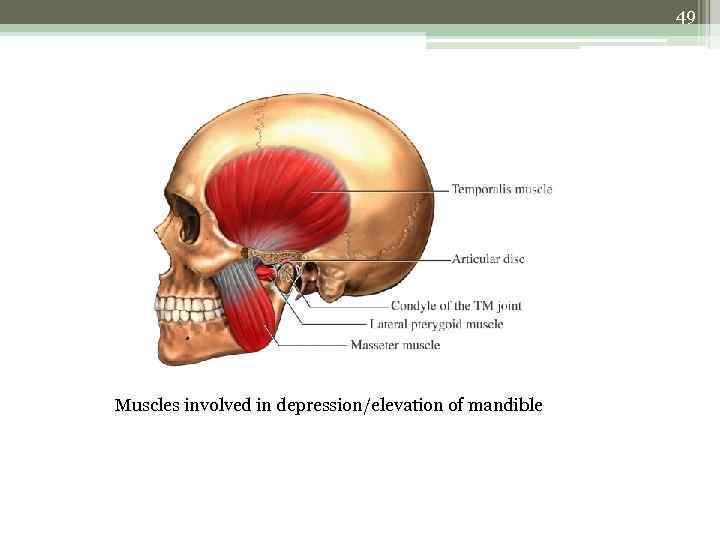
49 Muscles involved in depression/elevation of mandible
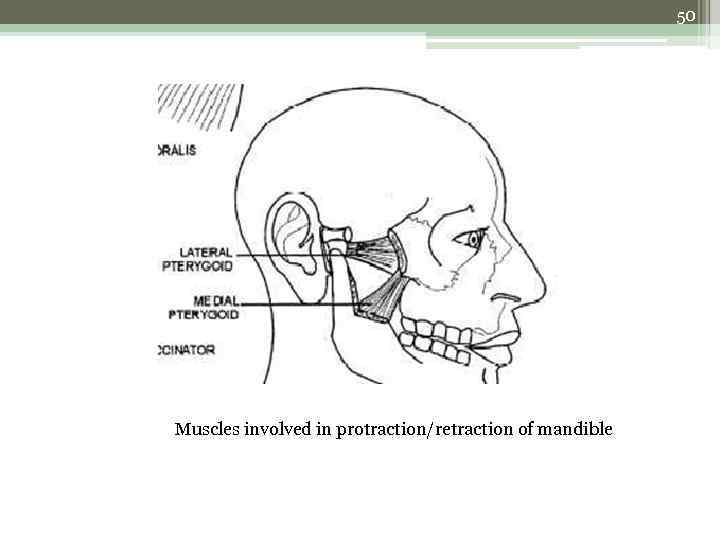
50 Muscles involved in protraction/retraction of mandible
51 BENNET MOVEMENT • A combination of tensed ligament and shifting vertical axis on one side, and the medially directed muscle vector on the opposite side , causes a short bodily movement involving the whole shift of the mandible to the deviating side. • On the return movement of the mandible towards the midline, a reverse movement is recorded. This shifting action is called “bennet movement or bennet shift”.
52 • Although the movement may be slight (not more than 1. 5 mm), this movement is clinically important in prosthetic reconstructions when dentures are coming into occlusion.
53 MARGINAL MOVEMENTS • Marginal movemnets are also referred to as ‘border movements’ or ‘envelope of movements’. • The marginal limits of mandibular mobility are outlined by a point on the most distal end of the moving bone, in all directions, thus giving a view of the extreme movements.
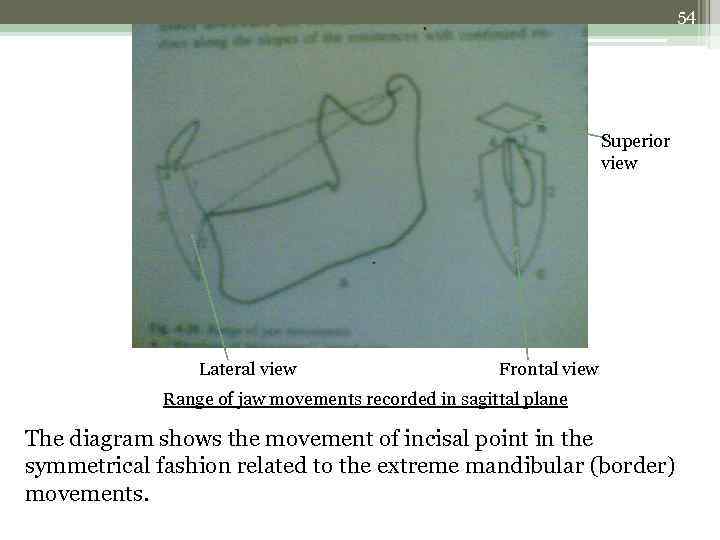
54 Superior view Lateral view Frontal view Range of jaw movements recorded in sagittal plane The diagram shows the movement of incisal point in the symmetrical fashion related to the extreme mandibular (border) movements.
55 FUNCTIONAL MOVEMENTS • This constitutes the chewing process and the movements are termed as the ‘chewing cycle’. • Two separate acts are recognized in the chewing cycle. • First is a combination of prehension and incision in which the food is secured by the lips and bitten by the front teeth. • The second is mastication, the major activity during which the food is mashed between the back teeth.
56 • The total chewing cycle occurs through three phases: 1. The opening stroke during which the mandible is lowered. 2. The beginning closing stroke during which the mandible is rapidly raised until the entrapped food is felt and 3. The power stroke in which the food is compressed, punctured, crushed and sheared.
57 • The mechanism of movement involves gliding movement in menisco-temporal compartment of one joint and rotatory movement in meniscomandibular compartment of other joint simultaneously. • The muscles involved in the action are the medial and lateral pterygoids whose alternate action produce the chewing cycle.
58 NEURAL CONTROL COMPLEX • Three major nerves are mostly responsible for all of the masticatory activity. 1. The trigeminal nerve 2. The facial nerve (as it is the motor nerve for all facial muscles)and 3. The hypoglossal nerve (innervates the muscles of tongue)
59 • The total masticatory activity or the chewing process takes place under reflexes guarded by these nerves. • These reflexes are summarized as: the mouth opening reflex and the mouth closing reflex. • Mouth opening reflex is the earliest oral reflex that appears in man, and is activated by stimulation of mechanoreceptors. • The mouth closing reflex is activated by neuromuscular spindles in the muscles and by golgi tendon organs.
60
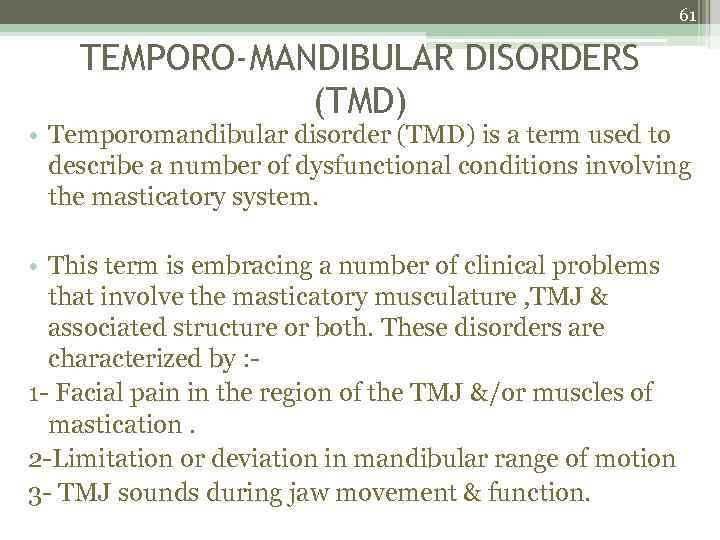
61 TEMPORO-MANDIBULAR DISORDERS (TMD) • Temporomandibular disorder (TMD) is a term used to describe a number of dysfunctional conditions involving the masticatory system. • This term is embracing a number of clinical problems that involve the masticatory musculature , TMJ & associated structure or both. These disorders are characterized by : 1 - Facial pain in the region of the TMJ &/or muscles of mastication. 2 -Limitation or deviation in mandibular range of motion 3 - TMJ sounds during jaw movement & function.
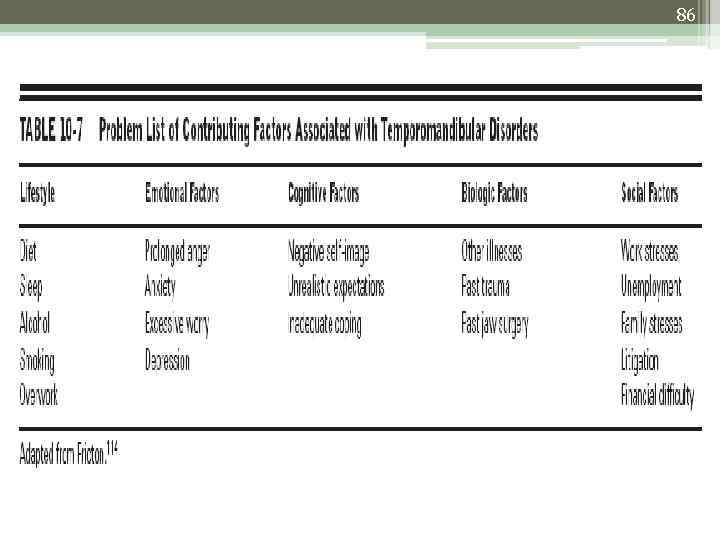
62 • TMD reflects possibilities of involvement of other factors, not just the joint capsule. • • • It may include: Occlusal factors Intra-joint dysfunction Psychological factors Skeletal misalignments
63 • There are many other suspected contributing factors, such as emotional well-being, mineral and hormonal imbalances, nutritional factors, allergies and chemical exposures. • The previously used term ‘TMJ syndrome’ is reflective of dysfunctions within the joint capsule, whereas TMD reflects possibilities of involvement of other factors, such as occlusal interferences, muscular disorders and neurological disorders.
64 COMMON SYMPTOMS • • • History of trauma, blow to jaw, dental malocclusions Pain and tenderness of the TMJ Head and/or ear pain Sore and stiff jaw muscles Locking of the jaw in a shut or open position Frequent headaches and/or neck aches Pain that worsens when teeth are clenched Grinding teeth at night Pain that worsens with stress Pain with opening of your mouth Teeth that meet differently from time to time Pain while chewing
65
66 ASSESSMENT OF TMJ • The examination methods have not yet demonstrated the ability to differentiate accurately persons with TMD from those without TMD • Most of the tests used to assess TMD patients have not been validated & are not standardized, and an ideal method for classification has not been established. • Some of the procedures usually involved to assess the TMJ function and physiology are: 1. Intercuspid alignment- check for the alignment of the canines bilaterally.
67 2. Mandibular gait pattern- the operator stands at the back of the patient and observes the movement of TMJ by asking the patient to open and close his mouth slowly. Any deviation in the path of this function may indicate abnormality. 3. Palpate joint and soft tissues- palpation of the joint is necessary to rule out any obvious findings such as scars, deformities etc. 4. Radiographic interpretation
68 5. Screening (3 finger test)- this assessment is done to check the mouth opening and to check any presence of pain or its trigger factors during mouth opening. Patient is asked to open his mouth wide and insert 3 fingers in a vertical fashion. The abnormal TMJ may present an inability to insert 3 fingers inside or patient may complain of pain during the process.
69 RADIOGRAPHIC INTERPRETATION OF TMJ • It includes: a. Plain film radiography: 1) transcranial 2) transpharyngeal 3) transorbital 4) reverse towne’s 5) cephalometric 6) water’s view 7) xeroradiography
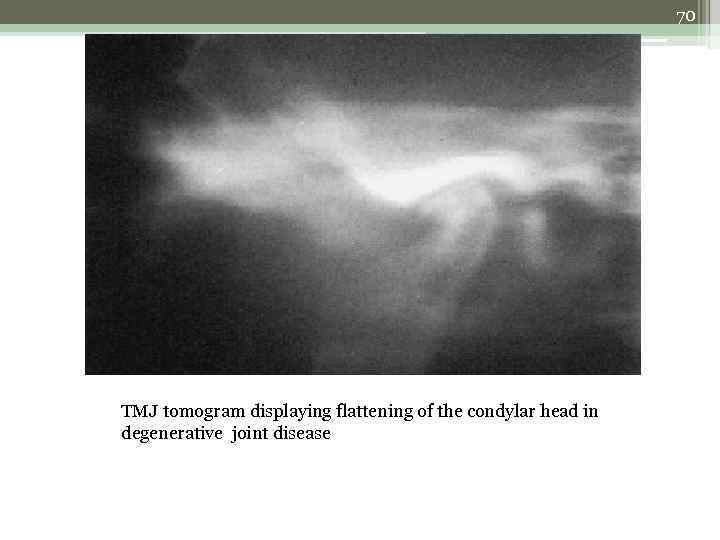
70 TMJ tomogram displaying flattening of the condylar head in degenerative joint disease
71 b. Conventional tomography 1) orthopantomography (OPG) 2) linear tomography 3) corrected tomography c. Arthrography d. Arthroscopy e. Computed tomography (CT-scan) f. Magnetic resonance imaging (MRI)
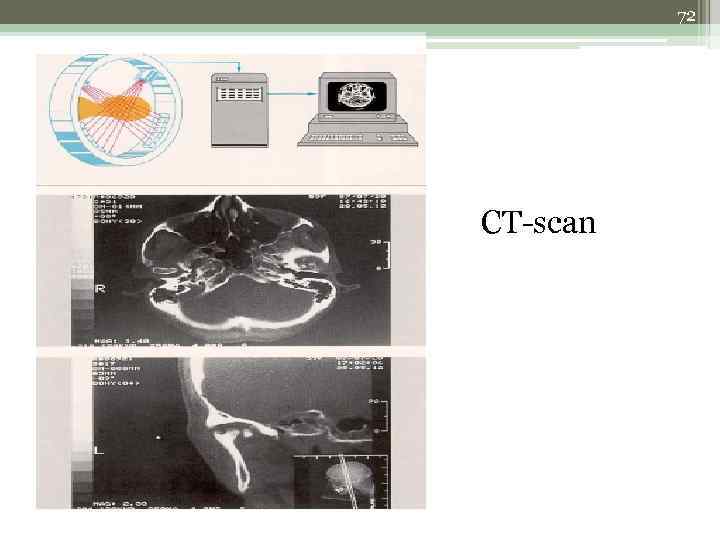
72 CT-scan
73 MRI
74 HISTORY • A thorough history and physical examination is necessary for the proper diagnosis and treatment planning. • History involves: 1. Pain diary • The most common symptoms related to TMJ disorders is pain, this pain usually shows some relation to mandibular function, or an alternative diagnosis should be suspected.
75 2. Questionnaire: • The questions that are useful as part of history to assessing mandibular function are asked such as: a. Do you have pain in the face, in front of ear and temporal areas? b. Do you have headaches, neck ache, or check pain? c. When is pain at its worst, morning (on a waking) or as day progresses (toward evening)? d. Do you have experience pain when using the jaw (during opening wide, chewing, speaking, or swallowing)? e. Do you experience pain in the teeth? f. Do you experience joint noises when moving jaw or when chewing (clicking, popping, or crepitus)? Etc.
76 CLINICAL EXAMINATION • The importance is to determine deviation of jaw from the midline during the opening and closing of the jaws. • Causes of jaw deviation. • - Traumatic injuries of the joint. • - Infection of the jaw. • - Fractures of the jaw. • - Muscles hypertrophy and hypotrophy. • The lateral mandibular range of motion or movement is assessed “normal 8 -10 mm” by having the patient to occlude the teeth and then slide the jaw in both directions. The range of movement from midline and any pain, location and severity is recorded.
77 • The maximum inter-incisal opening of mandible should be determined “normal opening in adult is usually between 35 and 50 mm. ” • The symmetry of the face is initially assessed. Although mild and moderate asymmetry is common, • A gross asymmetry may reflect a growth disturbance. This is often seen in patients who during childhood experienced trauma to the chin that resulted in TMJ ankylosis.
78 EXAMINATION OF TMJ • PALPATION: • Palpation of TMJ may be bimanual and bidigital palpation. • The palpation may reveal pain and irregularities during condylar movement, described as clicking or crepitus. • The lateral pole of condyle is most accessible for palpation during mandibular movements. • Palpation just anterior and posterior to the lateral pole detects pain associated with TMJ capsular ligament. • The comparison between both condyles must be assessed by palpation.
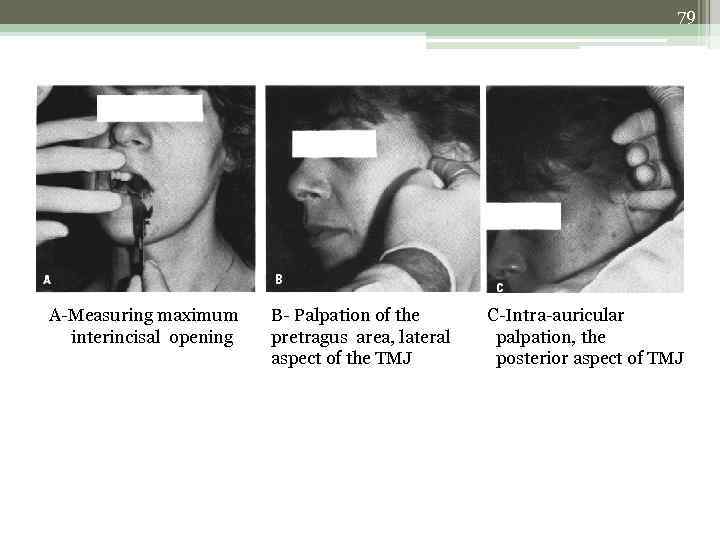
79 A-Measuring maximum interincisal opening B- Palpation of the pretragus area, lateral aspect of the TMJ C-Intra-auricular palpation, the posterior aspect of TMJ
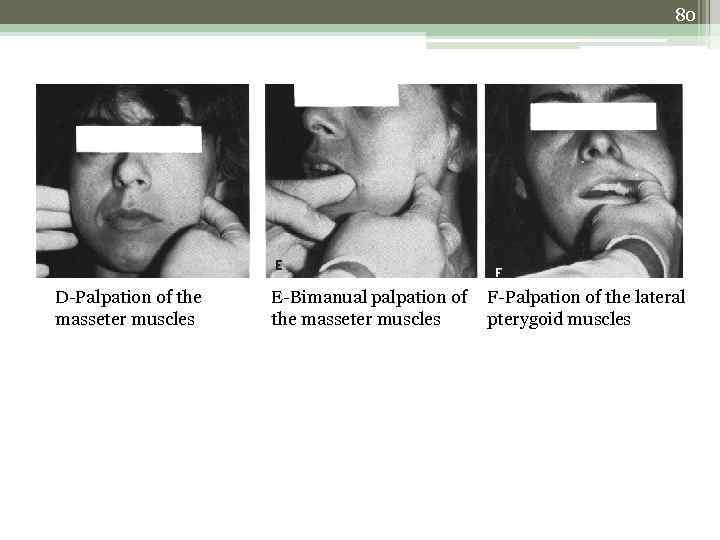
80 D-Palpation of the masseter muscles E-Bimanual palpation of the masseter muscles F-Palpation of the lateral pterygoid muscles
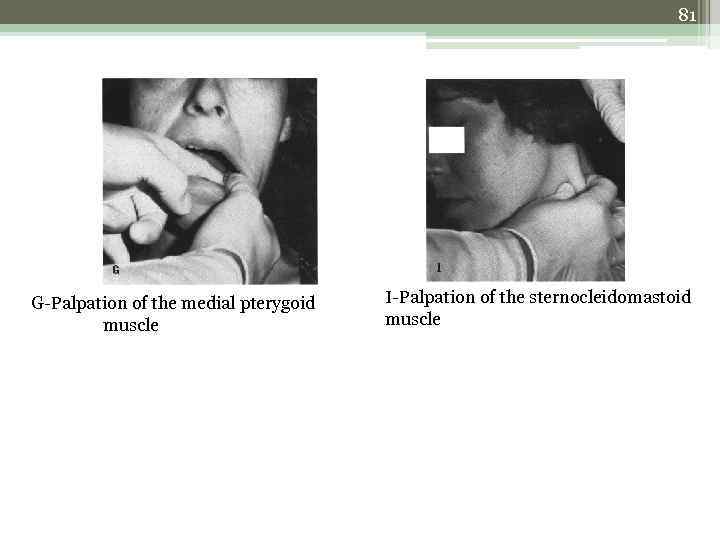
81 G-Palpation of the medial pterygoid muscle I-Palpation of the sternocleidomastoid muscle
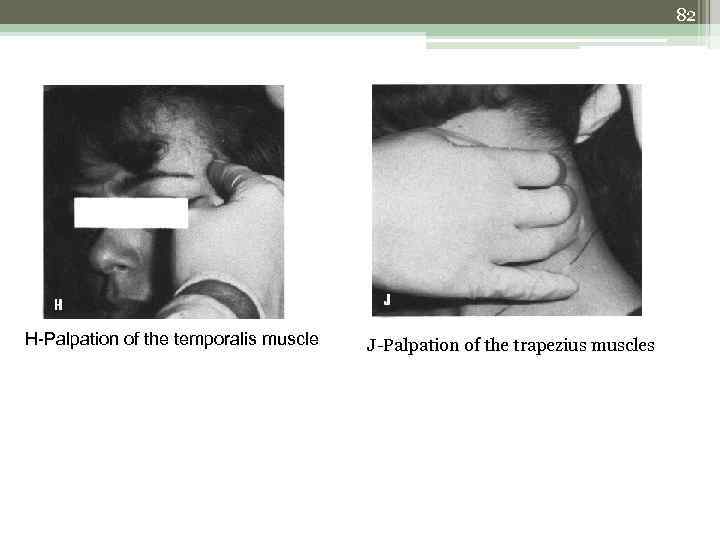
82 H-Palpation of the temporalis muscle J-Palpation of the trapezius muscles
83 EPIDEMIOLOGY OF TMD • The TMD prevalence is so wide that due to the disease there is an $30 Billion lost of productivity each year along with destruction of 550 million work days per year. • Around 10 million people are being treated for “TMJ” at any one time. • Average of onset is around 18 -26 years.
84 • There is a predilection of females for this disorder with a sex ratio of 5: 1. • Around 50% of the cases accommodate by functioning within physiologic limits.
85
86
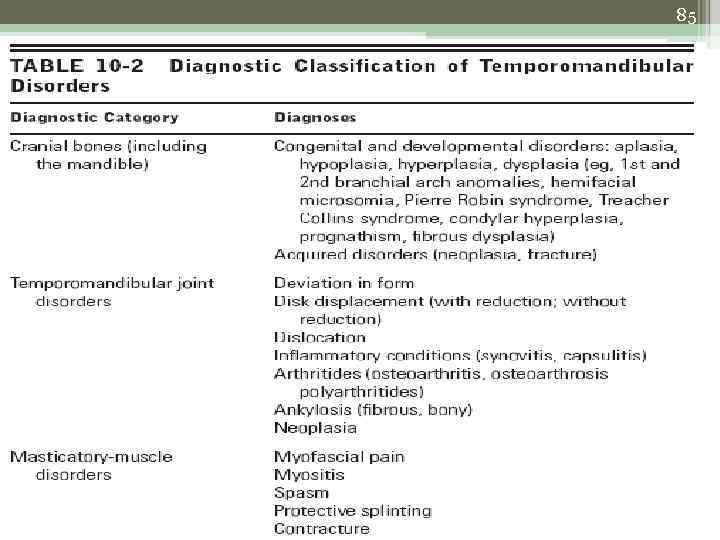
87 CLASSIFICATION OF TMJ DISORDERS • Another claasification: 1. Developmental diorders: a. hypoplasia: it includes two types- unilateral and bilateral b. agenesis c. hyperplasia: unilateral and bilateral d. double condyle
88 2. Acquired disorders: a. intracapsular: it includes sub types: 1. degenerative joint disease; eg. Osteoarthritis 2. inflammatory; eg. Rheumatoid arthritis 3. infectious diseases; eg gonorrhea, tuberculosis, syphilis 4. traumatic; eg. Condylar fracture, ankylosis, dislocation, disc displacement. 5. metabolic; eg. Gout 6. neoplasia: benign and malignant 7. drug induced such as steroids.
89 b. extracapsular: 1. psychophysiologic (MPD) 2. iatrogenic 3. traumatic 4. referred from local dental origin 5. infection 6. otologic 7. neoplastic
90 HYPOPLASIA • It is of two types: unilateral and bilateral Causes: 1. prenatal growth distubances including both hereditary distubances like mandibulofacial dysostosis and non-hereditary disturbances like pierre robin syndrome. 2. postnatal growth disturbances like endocrine dysfunction, dietary deficiency, trauma and irradiation Management: surgical, orthodontic and prosthetic correction for functional and cosmetic improvement is required.
91 AGENESIS Causes: 1. hemifacial macrostomia 2. goldenhar syndrome 3. hallermann-streiff syndrome Management: dental intervention is treated by establishment of an acceptable plane of occlusion. Osteoplasty can be done in severe derangement cases.
92 HYPERPLASIA Causes: 1. developmental- eg. Hemi-facial hypertrophy 2. neoplastic- eg. Chondroma or osteochondroma 3. bone disease- eg. Paget’s disease 4. hereditary- eg. Klinefelter’s disease 5. endocrine – eg. gigantism 6. hypertrophic arthritis. Management: orthognathic surgery to improve esthetics and function.
93 DOUBLE CONDYLE Causes: Developmental causes Management: surgical intervention
94 OSTEOARTHRITIS • Also called as degenerative arthritis. • There is destruction of soft tissue component of the joint and subsequent erosion with hypertrophic changes in bone.
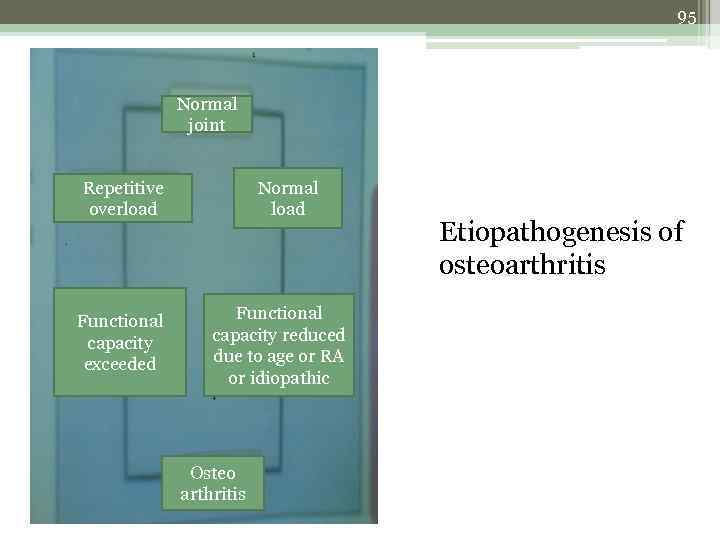
95 Normal joint Repetitive overload Functional capacity exceeded Normal load Functional capacity reduced due to age or RA or idiopathic Osteo arthritis Etiopathogenesis of osteoarthritis
96 Causes: 1. developmental- perthe’s disease, epiphysiolysis 2. metabolic- alkaptonuria, wilson’s disease 3. traumatic- hypermobility, arthropathy 4. endocrine- acromegaly, gout 5. others- haemophilia, tabes dorsalis etc. Ely’s cyst: these are minute areas of degeneration filled with fibrous tissue seen just below the bony surface of the condyle. Management: elimination of the cause, physiontherapy, muscle exercises, corticosteroids.
97 RHEUMATOID ARTHRITIS • It is a debilitating systemic disease of unknown origin, characterized by progressive involvement of the joint, particularly the large joints. • It causes bilateral stiffness, crepitus and tenderness of the joint. Severe involvement can lead to tendon rupture and joint collapse. • Anterior openbite or fibrous ankylosis may be present due to bilateral destruction of condyle.
98 • The radiographic feature typically shows the ‘sharpened pencil’ or ‘mouthpiece of flute’ appearance. • Management: adequate rest, soft diet. - intra-auricular corticosteriod injection - non steroidal anti-inflammatory drugs - slow acting anti-rheumatic drugs eg. Sulphasalazine - medical/surgical synovectomy
99 MYOFACIAL PAIN DYSFUNCTION SYNDROME (MPDS) • Muscular Disorders (Myofascial Pain Disorders) are the most common cause of TMJ pain. • Common etiologies include: 1. Many patient with “high stress level” 2. Poor habits including gum chewing, bruxism, hard candy chewing 3. Poor dentition
100 • Classified under five categories: 1. Myositis 2. Muscle spasm 3. Contracture 4. Hysterical trismus 5. Fibromyalgia Myositis: it presents with acute inflammation and pain, edema. Usually seen secondary to trauma. Management: joint rest, NSAIDs, removing the underlying etiology.
101 • Muscle spasm: it presents with acute contraction of facial and jaw muscles due to overuse and overstretching of the myofacial apparatus. Management: rest, NSAIDs, massage therapy, heat packs and muscle relaxants. Contracture: it is the end stage of untreated muscle spasm. It occurs due to fibrosis of muscle and connective tissue. Management: NSAIDs, massage, vigourous physical therapy, occasional surgical removal of granulosed tissue.
102 • Hysterical trismus: It has a psychosocial etiology, and is found more common in females. Fibromyalgia: It usually presents with firm, painful muscle bands. It is usually seen in weight bearing muscles and is often associated with sleep disturbances. More common in female patients.
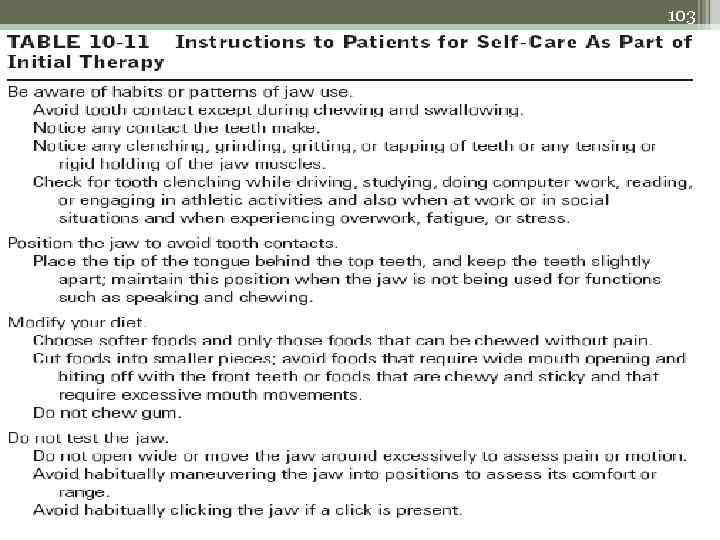
103
104 • Treatment of MPDS: • Treatment is divided into four phases: Phase I (four weeks, it is estimated to bring about 50% improvement) • firstly, educate the patient about muscle fatigue and explain referred pain • maintaining “oral” hygiene: no gum chewing, candy chewing, jaw clenching • soft diet is advised • NSAIDs (usually ibuprofen) • muscle relaxants
105 Phase II (four weeks) • Continue NSAIDs, and muscle relaxants • Add bite appliance (splint) This is done to: - decrease effects of bruxism - “splints” the muscles of mastication - it improves occlusion while wearing and allows a more natural jaw position This bite appliance is usually worn at night.
106 Phase III: (four weeks) • Patient is advised to continue NSAIDs and the bite appliance • the additional treatment procedures involve ultrasonic therapy, electrogalvanic stimulation or biofeedback Phase IV: TMJ Center • This phase includes multidisciplinary approach utilizing psychological counseling, medications, trigger point injections and physical therapy.
107 CONDYLAR FRACTURE • The condyle may be found displaced medially, inferiorly or anteriorly due to muscle pull. • • • Clinically, condylar fracture may be classified as: No displacement Deviation Comminuted fracture Greenstick fracture Dislocation
108 • Unilateral fractures show pain and tenderness on the affected side, inability to bring the jaw forward and paresthesia of lower lip. Also, bleeding from ear may occur. • Bilateral fractures show an additional sign of frequent gagging when occlusion is tried to achieve. • Mangement: • Fractures with slight displacement may be treated by immobilization for 4 weeks and IMF. • Extensive involvement includes open reduction and bone plates.
109 ANKYLOSIS • It is and abnormal immobility and consolidation of the joint. • Classified as bony/ fibrous and partial/ complete. • Etiology: 1. myogenic: most common. Occurs due to fibrosis of muscles. 2. neurogenic: due to epilepsy or paralysis. 3. psychogenic 4. bone impingement: most common is coronoid impingement. 5. neoplastic disease.
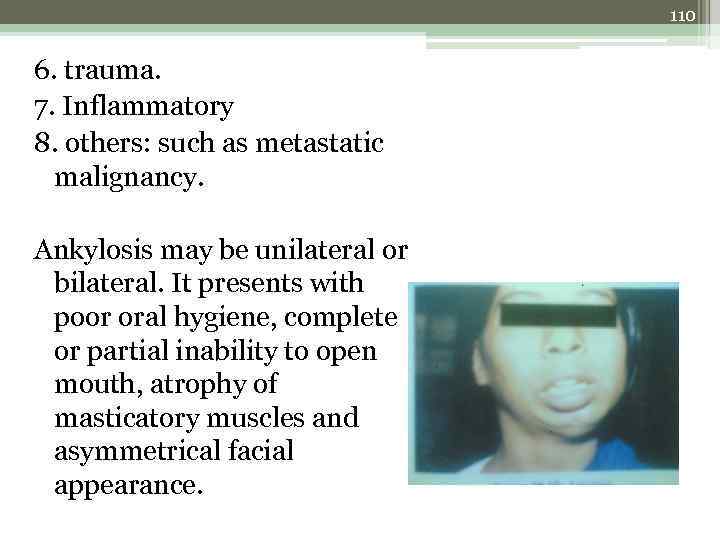
110 6. trauma. 7. Inflammatory 8. others: such as metastatic malignancy. Ankylosis may be unilateral or bilateral. It presents with poor oral hygiene, complete or partial inability to open mouth, atrophy of masticatory muscles and asymmetrical facial appearance.
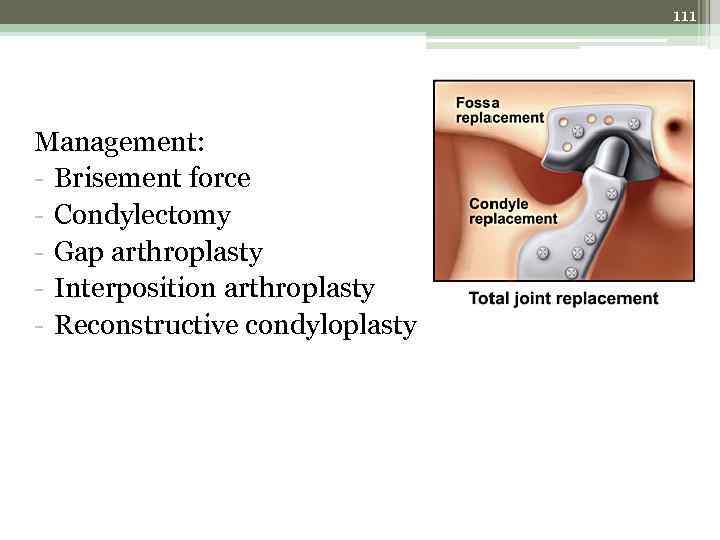
111 Management: - Brisement force - Condylectomy - Gap arthroplasty - Interposition arthroplasty - Reconstructive condyloplasty
112 DISLOCATION • It results when condyle is forcefully displaced out of the articular fossa but remains within the capsule of the joint. • Classified under acute/ chronic or anterior/ posterior/ medial/ lateral dislocation. • The usual clinical signs are difficulty in swallowing, pain in the temporal fossa, gagging, locking of condyle and drooling of saliva.
113 Management: Reduction of dislocation should be done with or without anaesthesia as required. Immobilization for 2 weeks and soft diet is advised. Sometimes, open reduction is also required.
114 SUBLUXATION (HYPERMOBILITY) • It is the frequent unilateral or bilateral positioning of the condyle anterior to the articular eminence, with repositioning to normal accomplished physiologic activity. • The patient presents with cracking noise, temporary locking of the condyle and immobilization of the jaw. The jaw comes back in a jumping motion, accompained by a sound. • Management: Conservative method: shrinkage of the capsule occurs by the injection of sclerosing agent which causes its fibrosis. Surgical intervention: insertion of bone graft.
115 GOUT • It is a chronic metabolic disorder characterized by acute exacerbations of joint pain and swelling associated with elevated blood urea levels. • Patients present with sudden, excruciating pain in the TMJ, followed by a swelling and tenderness. • Management: diet should be low in uric acid • Symptomatic relief.
116 NEOPLASTIC TUMORS • Benign tumors: produce restricted movements of TMJ and facial asymmetry. • Management is by surgical approach • Malignant tumors: produce diffuse pain in the area and diminished hearing, associated with swelling. • Management is by surgery, radiotherapy and chemotherapy.
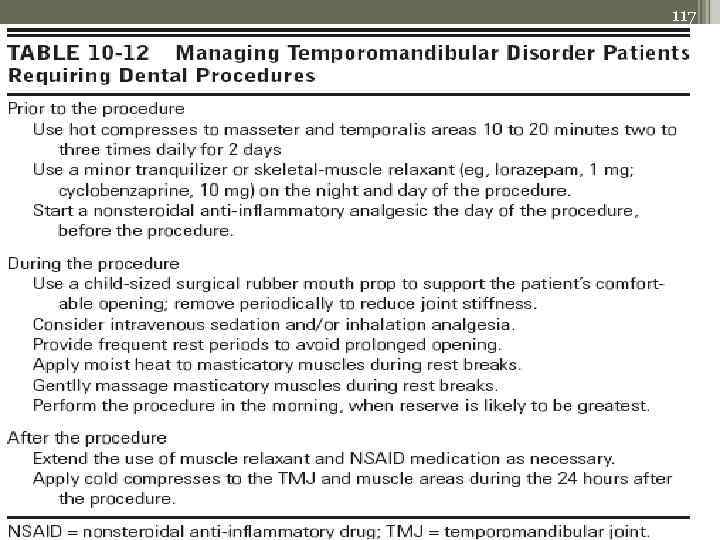
117
118 REFERENCES • Oral diagnosis: the clinician’s guide- by Birnbaum, Dunne, 2 nd ed. • Human anatomy by B. D. Chaurasia, 3 rd ed. • Human anatomy by dental students by M. K. Anand, 1 st ed. • Clinical anatomy and physiology for medical students, by Snell. • Essentials of oral anatomy, histology and embryology, by Avery and Chiego, 3 rd ed.
119 REFERENCES • Textbook of oral pathology by Shafers, 4 th ed. • Textbook of oral medicine, by Avindrao ghom, 1 st ed. • Oral anatomy and physiology, bu Du. Buller • Burket’s oral medicine: diagnosis and treatment, 10 th ed.
120 THANK YOU
TEMPORO-MANDIBULAR+JOINT+(TMJ).ppt