c9f71b4dfe8c9857680f2de565710254.ppt
- Количество слайдов: 99
 1
1
 Pregnancy loss - notion, diagnostics, treatment TO BE OR NOT TO BE Petar Ivanov, MD, Ph. D, Assoc. Prof. , OB/GYNs Clinical Institute for Reproductive Medicine, IVF Unit Medical University Pleven, Biochemistry Department
Pregnancy loss - notion, diagnostics, treatment TO BE OR NOT TO BE Petar Ivanov, MD, Ph. D, Assoc. Prof. , OB/GYNs Clinical Institute for Reproductive Medicine, IVF Unit Medical University Pleven, Biochemistry Department
 What is recurrent miscarriage? • Understanding • Definition Try again Happy pregnant • Classification • Pathogenesis • Investigation and Diagnosis • Treatment Recover Few week later Pain, bleeding loss
What is recurrent miscarriage? • Understanding • Definition Try again Happy pregnant • Classification • Pathogenesis • Investigation and Diagnosis • Treatment Recover Few week later Pain, bleeding loss
 Terms. . . • Miscarriage ( = Abortion = Pregnancy loss) • Abortion (< 20 wg) • Pregnancy loss (3 -42 wg) • Stillbirth (20 -28 wg)
Terms. . . • Miscarriage ( = Abortion = Pregnancy loss) • Abortion (< 20 wg) • Pregnancy loss (3 -42 wg) • Stillbirth (20 -28 wg)
 Historical perspective • Sporadic miscarriage rate is 15% • RM rate 0. 153 = 0. 3 -0. 4%. • The actual prevalence of RM is 1 -3%
Historical perspective • Sporadic miscarriage rate is 15% • RM rate 0. 153 = 0. 3 -0. 4%. • The actual prevalence of RM is 1 -3%
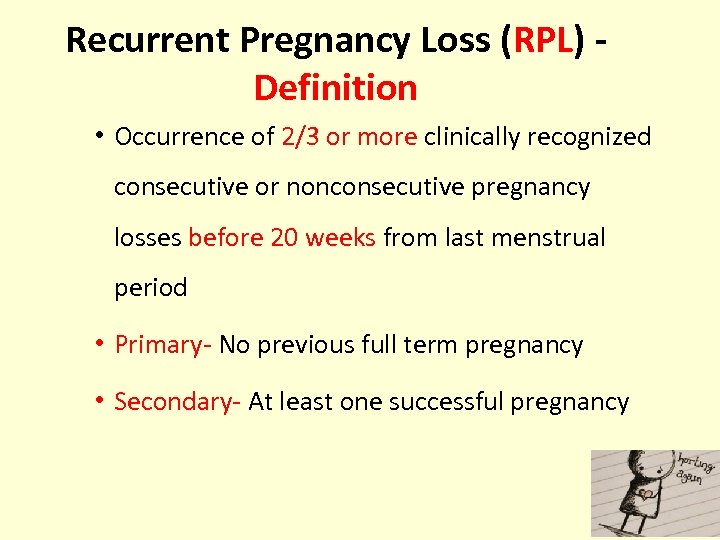 Recurrent Pregnancy Loss (RPL) Definition • Occurrence of 2/3 or more clinically recognized consecutive or nonconsecutive pregnancy losses before 20 weeks from last menstrual period • Primary- No previous full term pregnancy • Secondary- At least one successful pregnancy
Recurrent Pregnancy Loss (RPL) Definition • Occurrence of 2/3 or more clinically recognized consecutive or nonconsecutive pregnancy losses before 20 weeks from last menstrual period • Primary- No previous full term pregnancy • Secondary- At least one successful pregnancy
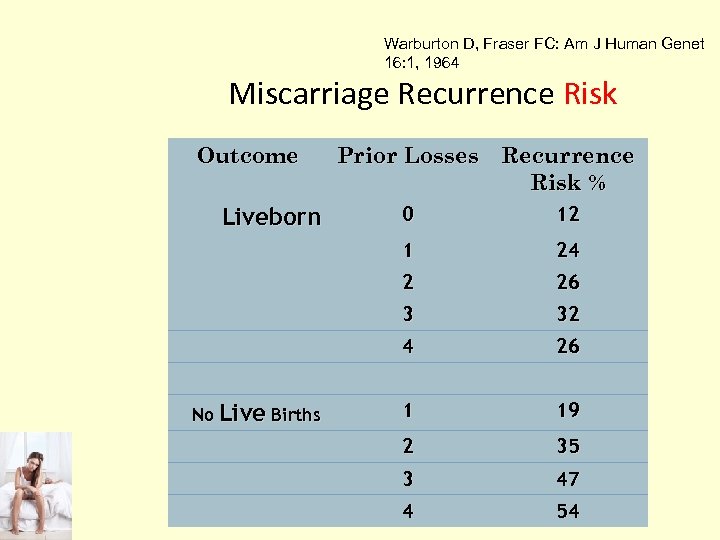 Warburton D, Fraser FC: Am J Human Genet 16: 1, 1964 Miscarriage Recurrence Risk Outcome Prior Losses Recurrence Risk % 12 24 2 26 3 32 4 No Live Births 0 1 Liveborn 26 1 19 2 35 3 47 4 54
Warburton D, Fraser FC: Am J Human Genet 16: 1, 1964 Miscarriage Recurrence Risk Outcome Prior Losses Recurrence Risk % 12 24 2 26 3 32 4 No Live Births 0 1 Liveborn 26 1 19 2 35 3 47 4 54
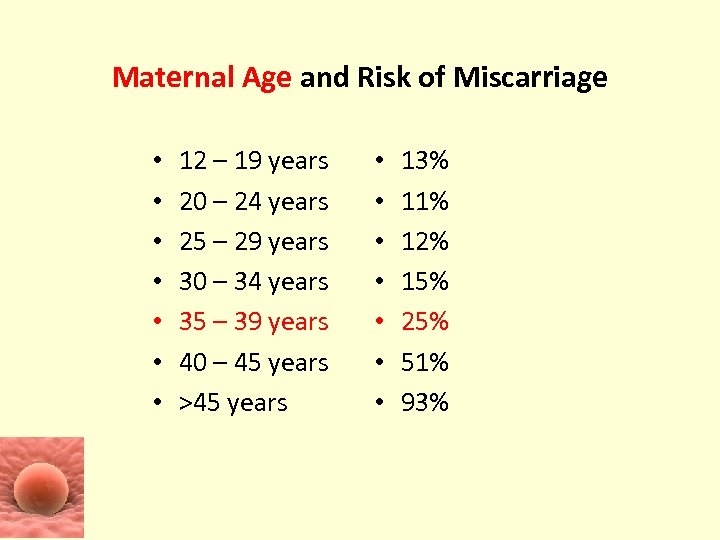 Maternal Age and Risk of Miscarriage • • 12 – 19 years 20 – 24 years 25 – 29 years 30 – 34 years 35 – 39 years 40 – 45 years >45 years • • 13% 11% 12% 15% 25% 51% 93%
Maternal Age and Risk of Miscarriage • • 12 – 19 years 20 – 24 years 25 – 29 years 30 – 34 years 35 – 39 years 40 – 45 years >45 years • • 13% 11% 12% 15% 25% 51% 93%
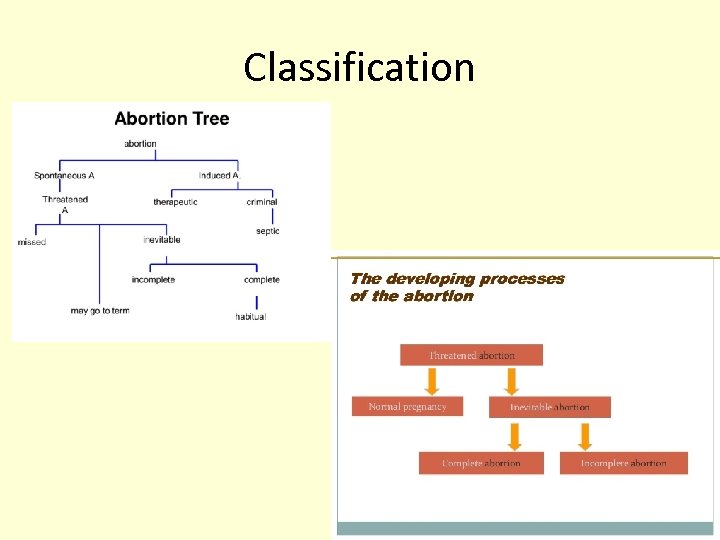 Classification
Classification
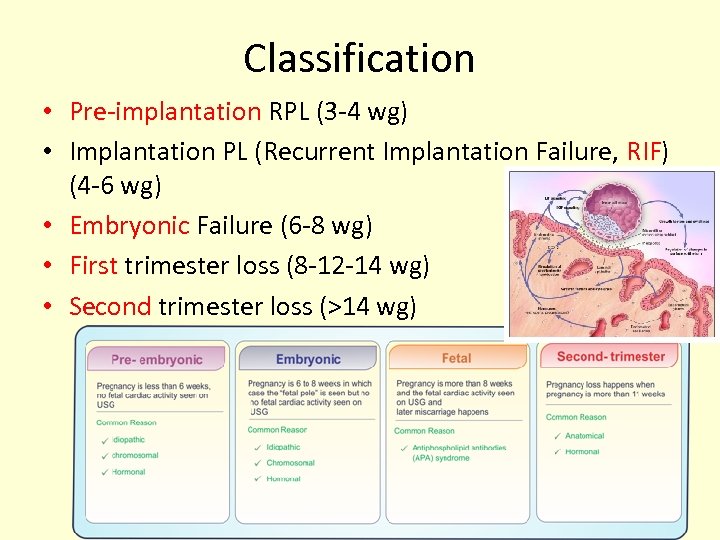 Classification • Pre-implantation RPL (3 -4 wg) • Implantation PL (Recurrent Implantation Failure, RIF) (4 -6 wg) • Embryonic Failure (6 -8 wg) • First trimester loss (8 -12 -14 wg) • Second trimester loss (>14 wg)
Classification • Pre-implantation RPL (3 -4 wg) • Implantation PL (Recurrent Implantation Failure, RIF) (4 -6 wg) • Embryonic Failure (6 -8 wg) • First trimester loss (8 -12 -14 wg) • Second trimester loss (>14 wg)
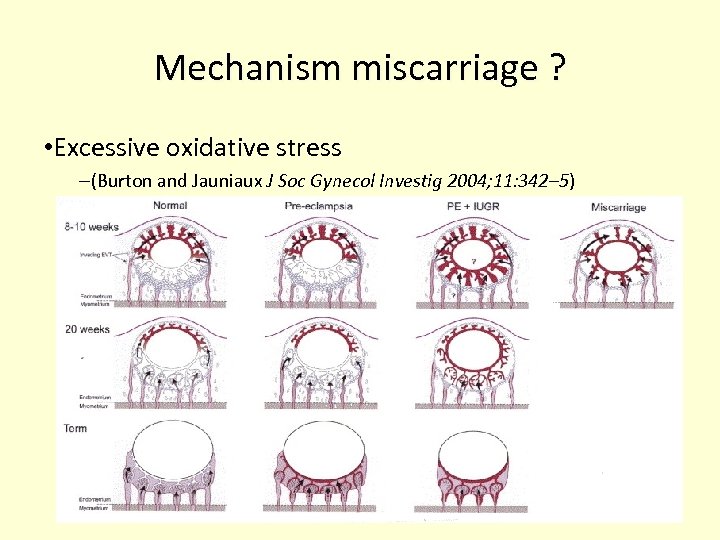 Mechanism miscarriage ? • Excessive oxidative stress –(Burton and Jauniaux J Soc Gynecol Investig 2004; 11: 342– 5)
Mechanism miscarriage ? • Excessive oxidative stress –(Burton and Jauniaux J Soc Gynecol Investig 2004; 11: 342– 5)
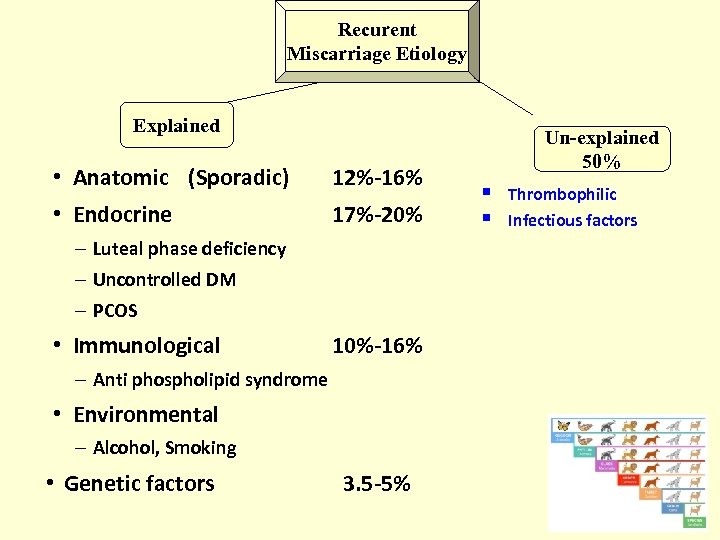 Recurent Miscarriage Etiology Explained • Anatomic (Sporadic) 12%-16% • Endocrine 17%-20% – Luteal phase deficiency – Uncontrolled DM – PCOS • Immunological 10%-16% – Anti phospholipid syndrome • Environmental – Alcohol, Smoking • Genetic factors 3. 5 -5% Un-explained 50% § § Thrombophilic Infectious factors
Recurent Miscarriage Etiology Explained • Anatomic (Sporadic) 12%-16% • Endocrine 17%-20% – Luteal phase deficiency – Uncontrolled DM – PCOS • Immunological 10%-16% – Anti phospholipid syndrome • Environmental – Alcohol, Smoking • Genetic factors 3. 5 -5% Un-explained 50% § § Thrombophilic Infectious factors
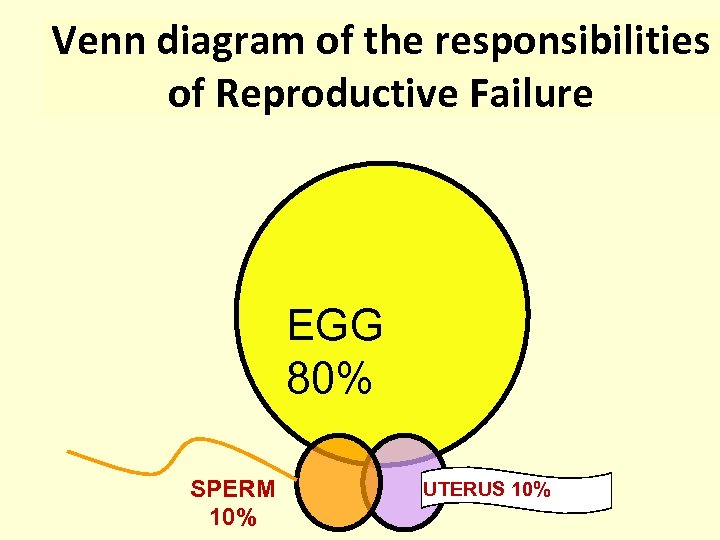 Venn diagram of the responsibilities of Reproductive Failure EGG 80% SPERM 10% UTERUS 10%
Venn diagram of the responsibilities of Reproductive Failure EGG 80% SPERM 10% UTERUS 10%
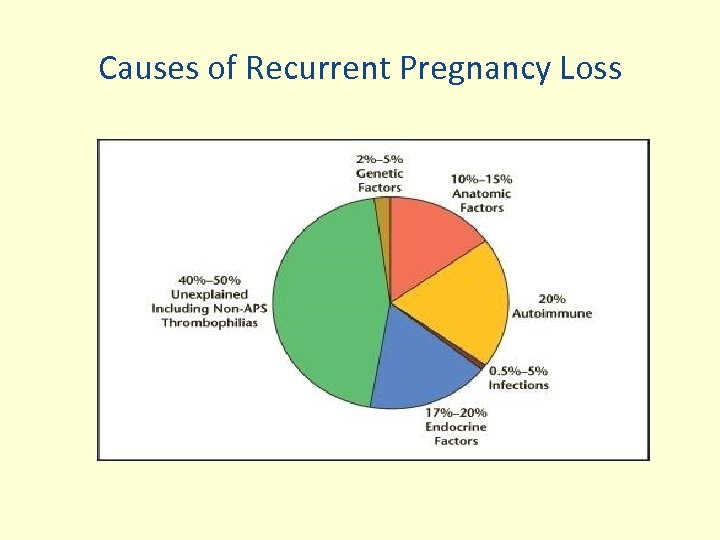 Causes of Recurrent Pregnancy Loss
Causes of Recurrent Pregnancy Loss
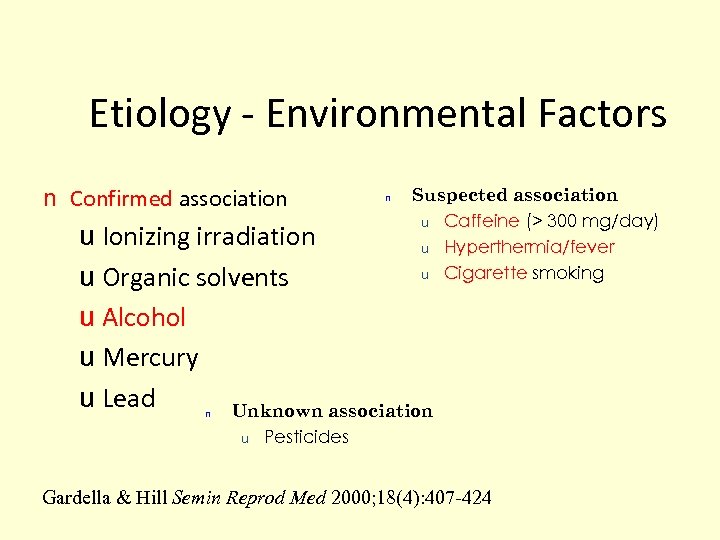 Etiology - Environmental Factors n Confirmed association n Suspected association u Caffeine (> 300 mg/day) u Hyperthermia/fever u Cigarette smoking u Ionizing irradiation u Organic solvents u Alcohol u Mercury u Lead Unknown association n u Pesticides Gardella & Hill Semin Reprod Med 2000; 18(4): 407 -424
Etiology - Environmental Factors n Confirmed association n Suspected association u Caffeine (> 300 mg/day) u Hyperthermia/fever u Cigarette smoking u Ionizing irradiation u Organic solvents u Alcohol u Mercury u Lead Unknown association n u Pesticides Gardella & Hill Semin Reprod Med 2000; 18(4): 407 -424
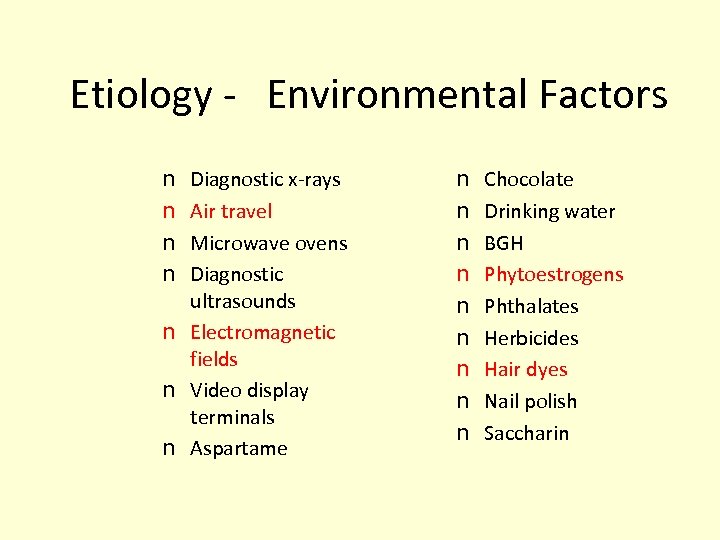 Etiology - Environmental Factors Diagnostic x-rays Air travel Microwave ovens Diagnostic ultrasounds n Electromagnetic fields n Video display terminals n Aspartame n n n n Chocolate Drinking water BGH Phytoestrogens Phthalates Herbicides Hair dyes Nail polish Saccharin
Etiology - Environmental Factors Diagnostic x-rays Air travel Microwave ovens Diagnostic ultrasounds n Electromagnetic fields n Video display terminals n Aspartame n n n n Chocolate Drinking water BGH Phytoestrogens Phthalates Herbicides Hair dyes Nail polish Saccharin
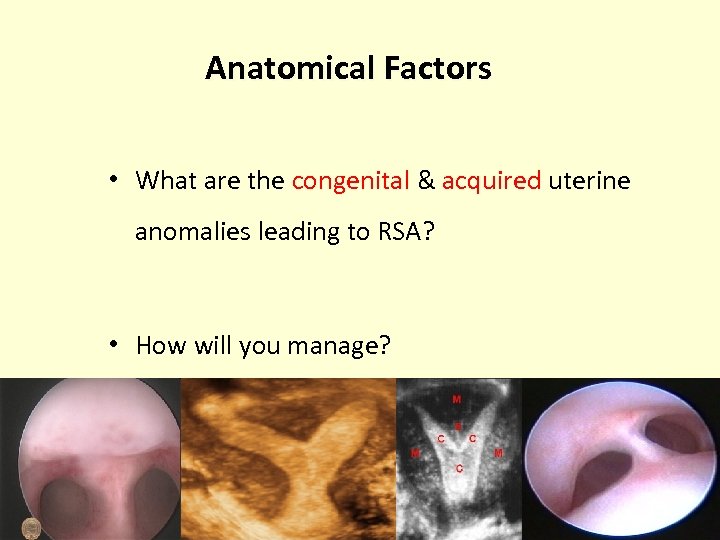 Anatomical Factors • What are the congenital & acquired uterine anomalies leading to RSA? • How will you manage?
Anatomical Factors • What are the congenital & acquired uterine anomalies leading to RSA? • How will you manage?
 Uterine Abnormalities • CONGENITAL (Mullerian Duct abnormalities) • UTERINE NEOPLASMS (Growth) • IATROGENIC (Acquired)
Uterine Abnormalities • CONGENITAL (Mullerian Duct abnormalities) • UTERINE NEOPLASMS (Growth) • IATROGENIC (Acquired)
 ANATOMICAL CAUSES • • • Septate uterus (early pregnancy loss) Bicornuate ut (unequal horns)(second trimester pregnancy loss) Unicornuate uterus T shaped uterus Submucous fibroids Large endometrial polyps . . . Adenomyosis. . Cervical insufficiency. . . Intrauterine adhesions. . .
ANATOMICAL CAUSES • • • Septate uterus (early pregnancy loss) Bicornuate ut (unequal horns)(second trimester pregnancy loss) Unicornuate uterus T shaped uterus Submucous fibroids Large endometrial polyps . . . Adenomyosis. . Cervical insufficiency. . . Intrauterine adhesions. . .
 How they affect……. Smaller Uterine Cavities Fewer suitable implantation sites Aberrations of vascularisation May be accompanied by cervical incompetence Lead to both early & later pregnancy losses • •
How they affect……. Smaller Uterine Cavities Fewer suitable implantation sites Aberrations of vascularisation May be accompanied by cervical incompetence Lead to both early & later pregnancy losses • •
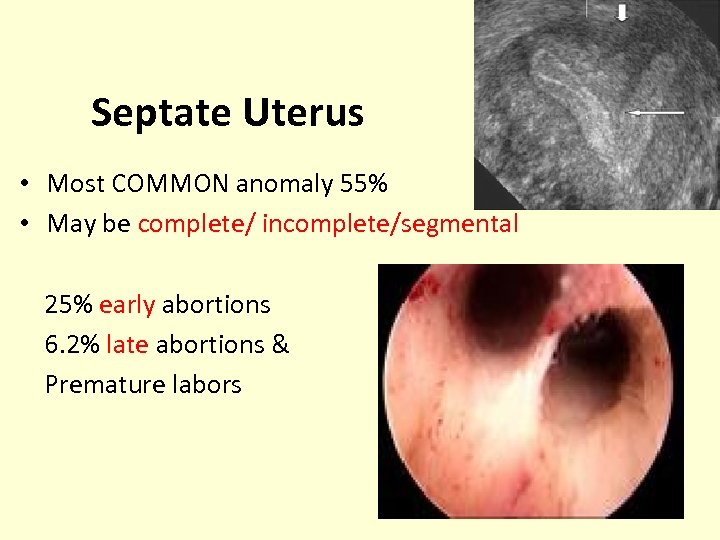 Septate Uterus • Most COMMON anomaly 55% • May be complete/ incomplete/segmental 25% early abortions 6. 2% late abortions & Premature labors
Septate Uterus • Most COMMON anomaly 55% • May be complete/ incomplete/segmental 25% early abortions 6. 2% late abortions & Premature labors
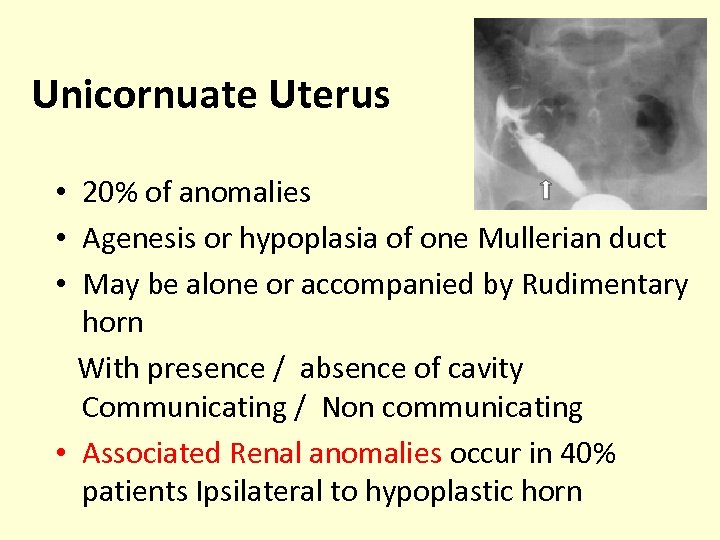 Unicornuate Uterus • 20% of anomalies • Agenesis or hypoplasia of one Mullerian duct • May be alone or accompanied by Rudimentary horn With presence / absence of cavity Communicating / Non communicating • Associated Renal anomalies occur in 40% patients Ipsilateral to hypoplastic horn
Unicornuate Uterus • 20% of anomalies • Agenesis or hypoplasia of one Mullerian duct • May be alone or accompanied by Rudimentary horn With presence / absence of cavity Communicating / Non communicating • Associated Renal anomalies occur in 40% patients Ipsilateral to hypoplastic horn
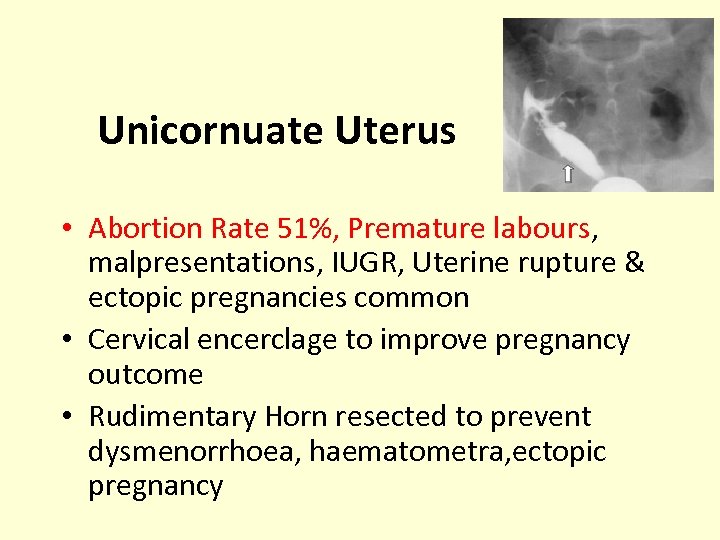 Unicornuate Uterus • Abortion Rate 51%, Premature labours, malpresentations, IUGR, Uterine rupture & ectopic pregnancies common • Cervical encerclage to improve pregnancy outcome • Rudimentary Horn resected to prevent dysmenorrhoea, haematometra, ectopic pregnancy
Unicornuate Uterus • Abortion Rate 51%, Premature labours, malpresentations, IUGR, Uterine rupture & ectopic pregnancies common • Cervical encerclage to improve pregnancy outcome • Rudimentary Horn resected to prevent dysmenorrhoea, haematometra, ectopic pregnancy
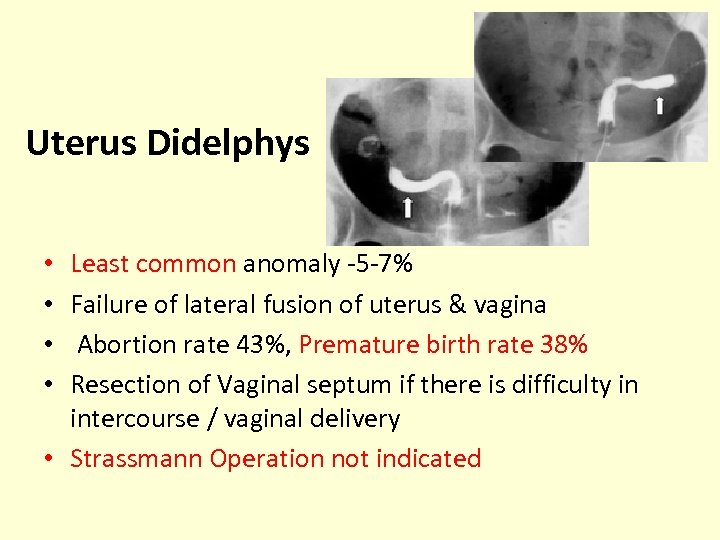 Uterus Didelphys Least common anomaly -5 -7% Failure of lateral fusion of uterus & vagina Abortion rate 43%, Premature birth rate 38% Resection of Vaginal septum if there is difficulty in intercourse / vaginal delivery • Strassmann Operation not indicated • •
Uterus Didelphys Least common anomaly -5 -7% Failure of lateral fusion of uterus & vagina Abortion rate 43%, Premature birth rate 38% Resection of Vaginal septum if there is difficulty in intercourse / vaginal delivery • Strassmann Operation not indicated • •
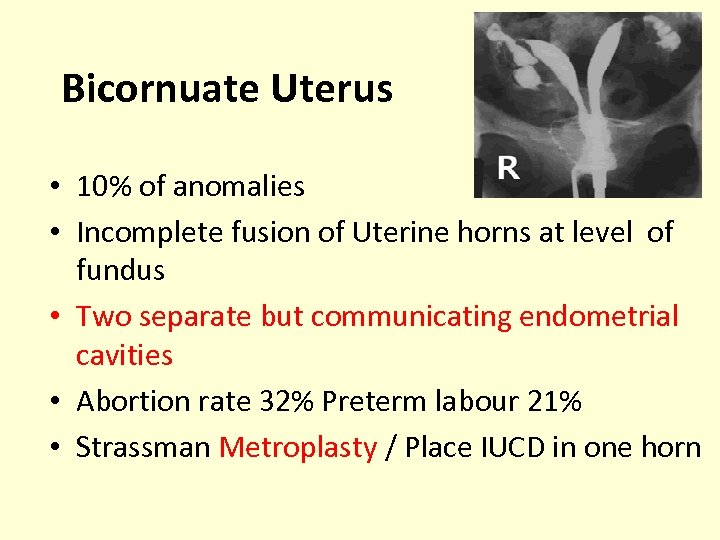 Bicornuate Uterus • 10% of anomalies • Incomplete fusion of Uterine horns at level of fundus • Two separate but communicating endometrial cavities • Abortion rate 32% Preterm labour 21% • Strassman Metroplasty / Place IUCD in one horn
Bicornuate Uterus • 10% of anomalies • Incomplete fusion of Uterine horns at level of fundus • Two separate but communicating endometrial cavities • Abortion rate 32% Preterm labour 21% • Strassman Metroplasty / Place IUCD in one horn
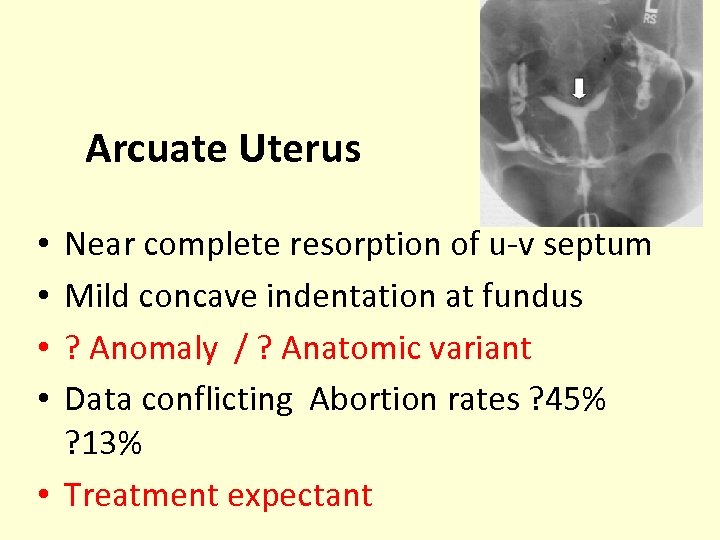 Arcuate Uterus Near complete resorption of u-v septum Mild concave indentation at fundus ? Anomaly / ? Anatomic variant Data conflicting Abortion rates ? 45% ? 13% • Treatment expectant • •
Arcuate Uterus Near complete resorption of u-v septum Mild concave indentation at fundus ? Anomaly / ? Anatomic variant Data conflicting Abortion rates ? 45% ? 13% • Treatment expectant • •
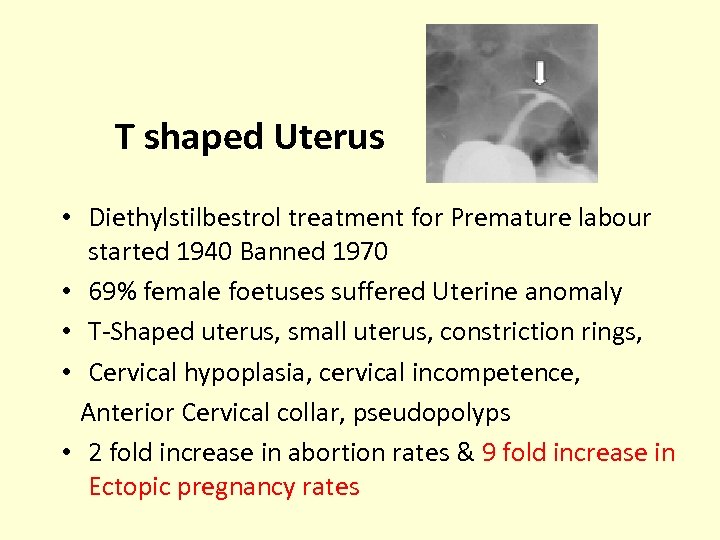 T shaped Uterus • Diethylstilbestrol treatment for Premature labour started 1940 Banned 1970 • 69% female foetuses suffered Uterine anomaly • T-Shaped uterus, small uterus, constriction rings, • Cervical hypoplasia, cervical incompetence, Anterior Cervical collar, pseudopolyps • 2 fold increase in abortion rates & 9 fold increase in Ectopic pregnancy rates
T shaped Uterus • Diethylstilbestrol treatment for Premature labour started 1940 Banned 1970 • 69% female foetuses suffered Uterine anomaly • T-Shaped uterus, small uterus, constriction rings, • Cervical hypoplasia, cervical incompetence, Anterior Cervical collar, pseudopolyps • 2 fold increase in abortion rates & 9 fold increase in Ectopic pregnancy rates
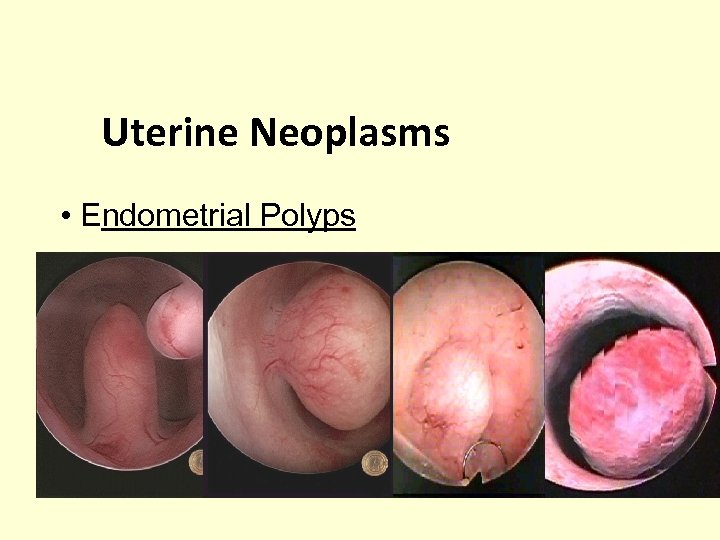 Uterine Neoplasms • Endometrial Polyps
Uterine Neoplasms • Endometrial Polyps
 Leiomyomas (Fibroids) most common…. 20 -50% of reproductive women When will you consider fibroids responsible ?
Leiomyomas (Fibroids) most common…. 20 -50% of reproductive women When will you consider fibroids responsible ?
 • Preconception myomectomy to improve reproductive outcome can be considered on an individual basis • It is likely to have a place only in women who have recurrent pregnancy loss, – large submucosal fibroids, and no other identifiable cause for recurrent miscarriage Ouyang DW, Obstet Gynecol Clin North Am. 2006
• Preconception myomectomy to improve reproductive outcome can be considered on an individual basis • It is likely to have a place only in women who have recurrent pregnancy loss, – large submucosal fibroids, and no other identifiable cause for recurrent miscarriage Ouyang DW, Obstet Gynecol Clin North Am. 2006
 Iatrogenic… Intrauterine adhesions , “Asherman’s Syndrome” • Lead to Poor implantation, • Decreased blood supply , • infection Abortion rates 40% Preterm labour 23% Management : -Hysteroscopic excision of adhesions
Iatrogenic… Intrauterine adhesions , “Asherman’s Syndrome” • Lead to Poor implantation, • Decreased blood supply , • infection Abortion rates 40% Preterm labour 23% Management : -Hysteroscopic excision of adhesions
 HYSTEROSCOPIC CORRECTION • All of the above have a good pregnancy rate post hysteroscopic correction • Except ASHERMANS SYNDROME
HYSTEROSCOPIC CORRECTION • All of the above have a good pregnancy rate post hysteroscopic correction • Except ASHERMANS SYNDROME
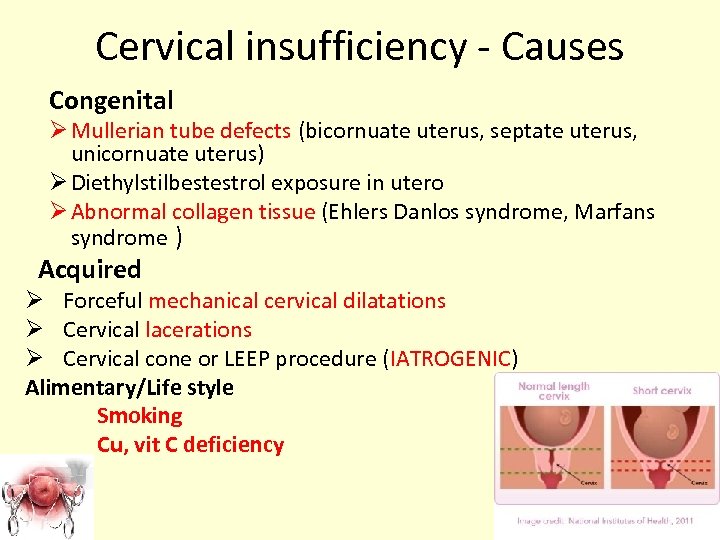 Cervical insufficiency - Causes Congenital Ø Mullerian tube defects (bicornuate uterus, septate uterus, unicornuate uterus) Ø Diethylstilbestestrol exposure in utero Ø Abnormal collagen tissue (Ehlers Danlos syndrome, Marfans syndrome ) Acquired Ø Forceful mechanical cervical dilatations Ø Cervical lacerations Ø Cervical cone or LEEP procedure (IATROGENIC) Alimentary/Life style Smoking Cu, vit C deficiency
Cervical insufficiency - Causes Congenital Ø Mullerian tube defects (bicornuate uterus, septate uterus, unicornuate uterus) Ø Diethylstilbestestrol exposure in utero Ø Abnormal collagen tissue (Ehlers Danlos syndrome, Marfans syndrome ) Acquired Ø Forceful mechanical cervical dilatations Ø Cervical lacerations Ø Cervical cone or LEEP procedure (IATROGENIC) Alimentary/Life style Smoking Cu, vit C deficiency
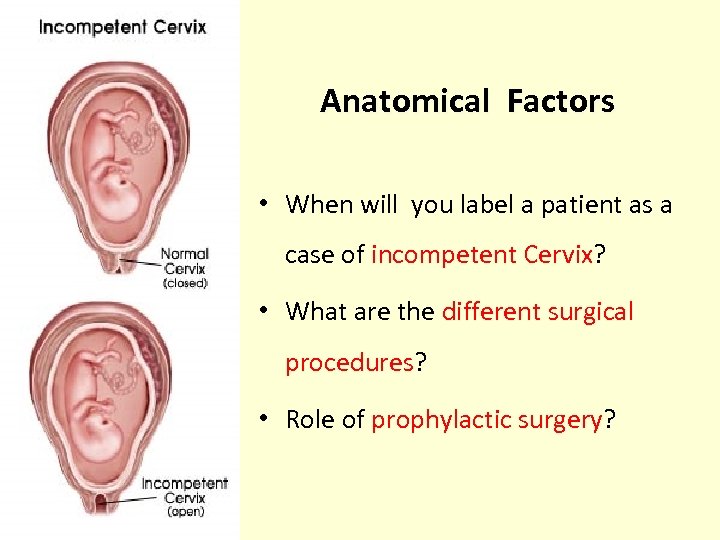 Anatomical Factors • When will you label a patient as a case of incompetent Cervix? • What are the different surgical procedures? • Role of prophylactic surgery?
Anatomical Factors • When will you label a patient as a case of incompetent Cervix? • What are the different surgical procedures? • Role of prophylactic surgery?
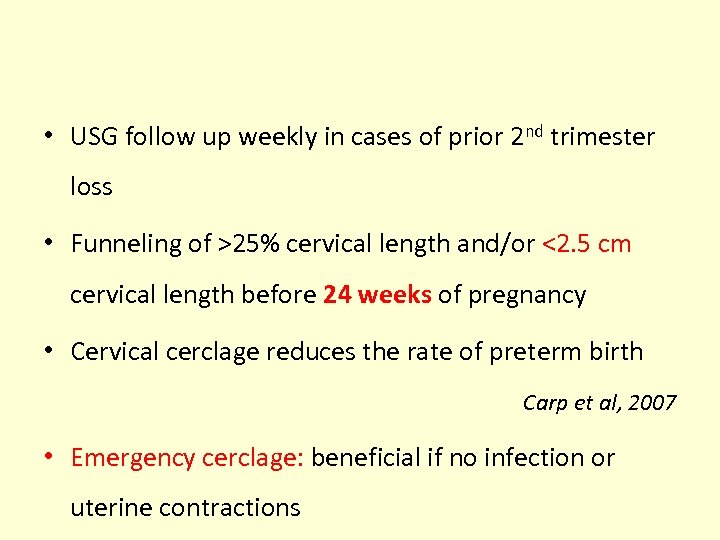 • USG follow up weekly in cases of prior 2 nd trimester loss • Funneling of >25% cervical length and/or <2. 5 cm cervical length before 24 weeks of pregnancy • Cervical cerclage reduces the rate of preterm birth Carp et al, 2007 • Emergency cerclage: beneficial if no infection or uterine contractions
• USG follow up weekly in cases of prior 2 nd trimester loss • Funneling of >25% cervical length and/or <2. 5 cm cervical length before 24 weeks of pregnancy • Cervical cerclage reduces the rate of preterm birth Carp et al, 2007 • Emergency cerclage: beneficial if no infection or uterine contractions
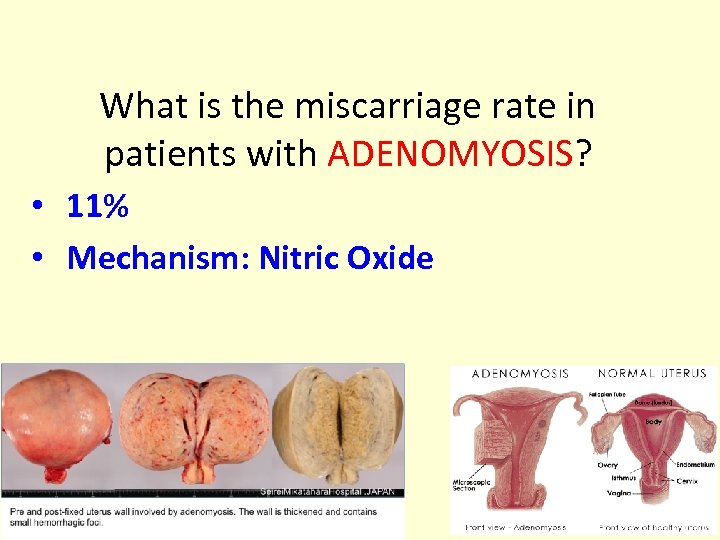 What is the miscarriage rate in patients with ADENOMYOSIS? • 11% • Mechanism: Nitric Oxide
What is the miscarriage rate in patients with ADENOMYOSIS? • 11% • Mechanism: Nitric Oxide
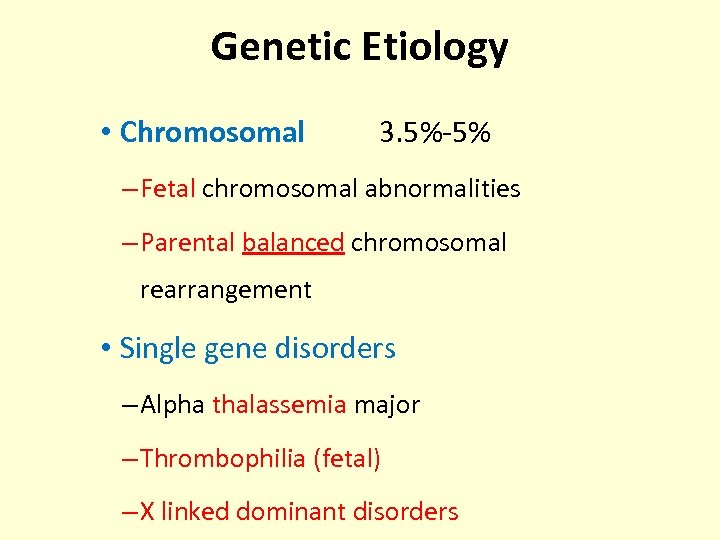 Genetic Etiology • Chromosomal 3. 5%-5% – Fetal chromosomal abnormalities – Parental balanced chromosomal rearrangement • Single gene disorders – Alpha thalassemia major – Thrombophilia (fetal) – X linked dominant disorders
Genetic Etiology • Chromosomal 3. 5%-5% – Fetal chromosomal abnormalities – Parental balanced chromosomal rearrangement • Single gene disorders – Alpha thalassemia major – Thrombophilia (fetal) – X linked dominant disorders
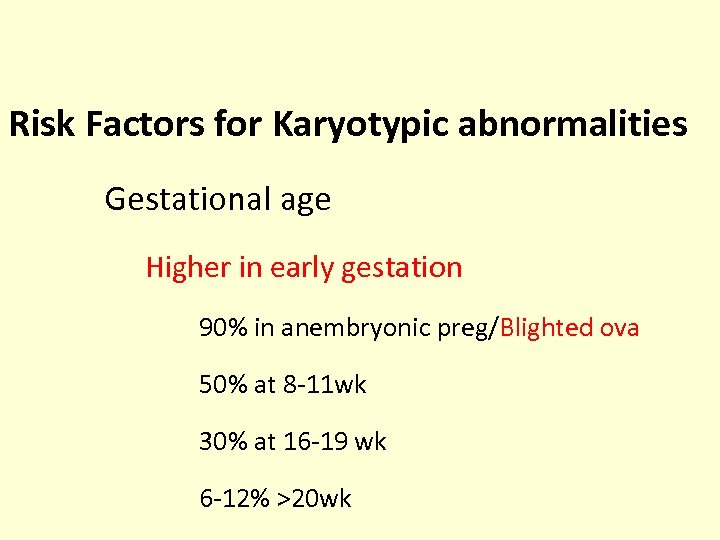 Risk Factors for Karyotypic abnormalities Gestational age Higher in early gestation 90% in anembryonic preg/Blighted ova 50% at 8 -11 wk 30% at 16 -19 wk 6 -12% >20 wk
Risk Factors for Karyotypic abnormalities Gestational age Higher in early gestation 90% in anembryonic preg/Blighted ova 50% at 8 -11 wk 30% at 16 -19 wk 6 -12% >20 wk
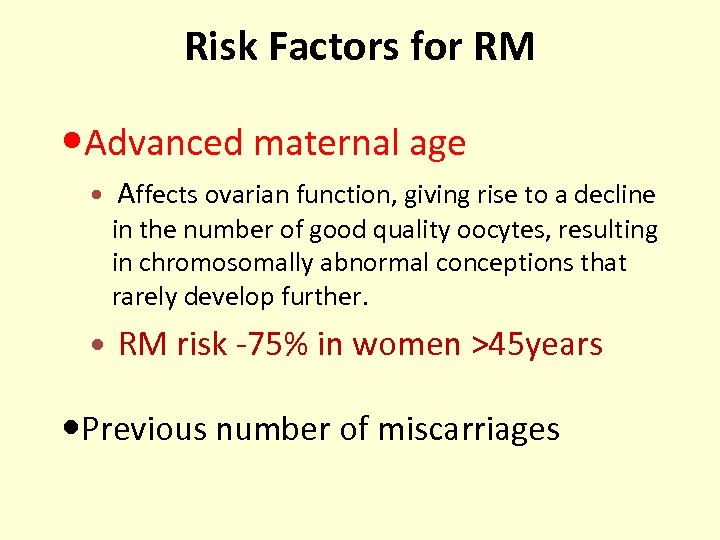 Risk Factors for RM Advanced maternal age Affects ovarian function, giving rise to a decline in the number of good quality oocytes, resulting in chromosomally abnormal conceptions that rarely develop further. RM risk -75% in women >45 years Previous number of miscarriages
Risk Factors for RM Advanced maternal age Affects ovarian function, giving rise to a decline in the number of good quality oocytes, resulting in chromosomally abnormal conceptions that rarely develop further. RM risk -75% in women >45 years Previous number of miscarriages
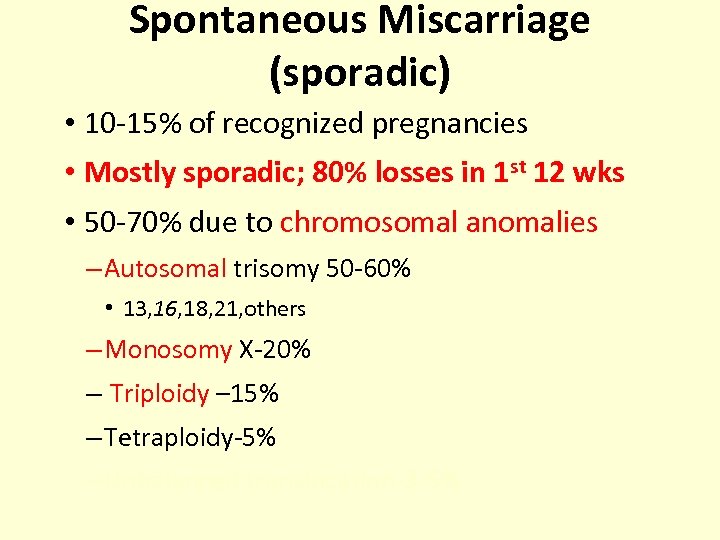 Spontaneous Miscarriage (sporadic) • 10 -15% of recognized pregnancies • Mostly sporadic; 80% losses in 1 st 12 wks • 50 -70% due to chromosomal anomalies – Autosomal trisomy 50 -60% • 13, 16, 18, 21, others – Monosomy X-20% – Triploidy – 15% – Tetraploidy-5% – Unbalanced translocation-3 -5%
Spontaneous Miscarriage (sporadic) • 10 -15% of recognized pregnancies • Mostly sporadic; 80% losses in 1 st 12 wks • 50 -70% due to chromosomal anomalies – Autosomal trisomy 50 -60% • 13, 16, 18, 21, others – Monosomy X-20% – Triploidy – 15% – Tetraploidy-5% – Unbalanced translocation-3 -5%
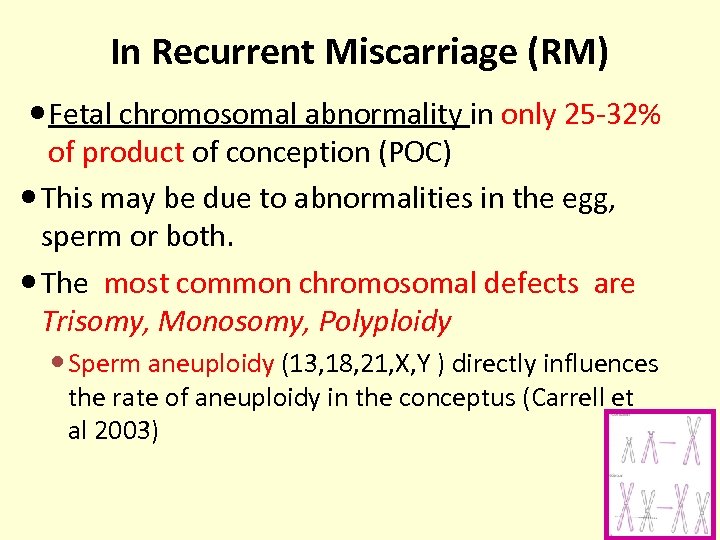 In Recurrent Miscarriage (RM) Fetal chromosomal abnormality in only 25 -32% of product of conception (POC) This may be due to abnormalities in the egg, sperm or both. The most common chromosomal defects are Trisomy, Monosomy, Polyploidy Sperm aneuploidy (13, 18, 21, X, Y ) directly influences the rate of aneuploidy in the conceptus (Carrell et al 2003)
In Recurrent Miscarriage (RM) Fetal chromosomal abnormality in only 25 -32% of product of conception (POC) This may be due to abnormalities in the egg, sperm or both. The most common chromosomal defects are Trisomy, Monosomy, Polyploidy Sperm aneuploidy (13, 18, 21, X, Y ) directly influences the rate of aneuploidy in the conceptus (Carrell et al 2003)
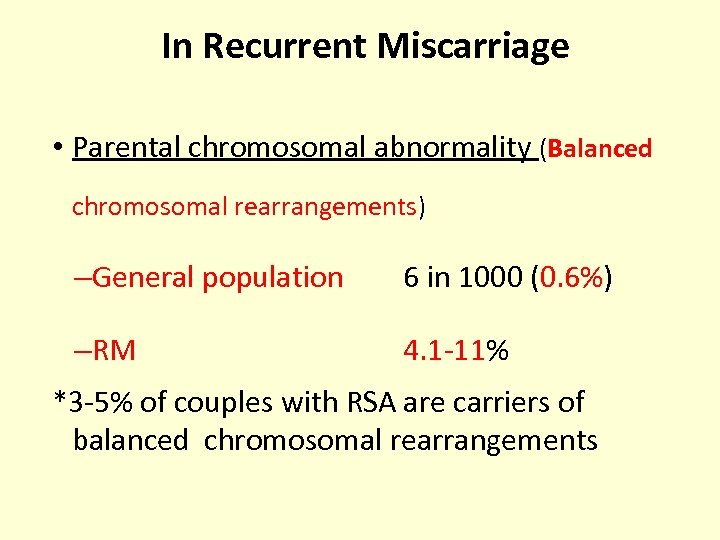 In Recurrent Miscarriage • Parental chromosomal abnormality (Balanced chromosomal rearrangements) –General population 6 in 1000 (0. 6%) –RM 4. 1 -11% *3 -5% of couples with RSA are carriers of balanced chromosomal rearrangements
In Recurrent Miscarriage • Parental chromosomal abnormality (Balanced chromosomal rearrangements) –General population 6 in 1000 (0. 6%) –RM 4. 1 -11% *3 -5% of couples with RSA are carriers of balanced chromosomal rearrangements
![Parental Chromosomal Abnormalities –Translocation (commonest) (1 in 500) • Reciprocal [50%] • Robertsonian [24%] Parental Chromosomal Abnormalities –Translocation (commonest) (1 in 500) • Reciprocal [50%] • Robertsonian [24%]](https://present5.com/presentation/c9f71b4dfe8c9857680f2de565710254/image-43.jpg) Parental Chromosomal Abnormalities –Translocation (commonest) (1 in 500) • Reciprocal [50%] • Robertsonian [24%] –Mosaicism for a numeric aberration [12%] –Inversion
Parental Chromosomal Abnormalities –Translocation (commonest) (1 in 500) • Reciprocal [50%] • Robertsonian [24%] –Mosaicism for a numeric aberration [12%] –Inversion
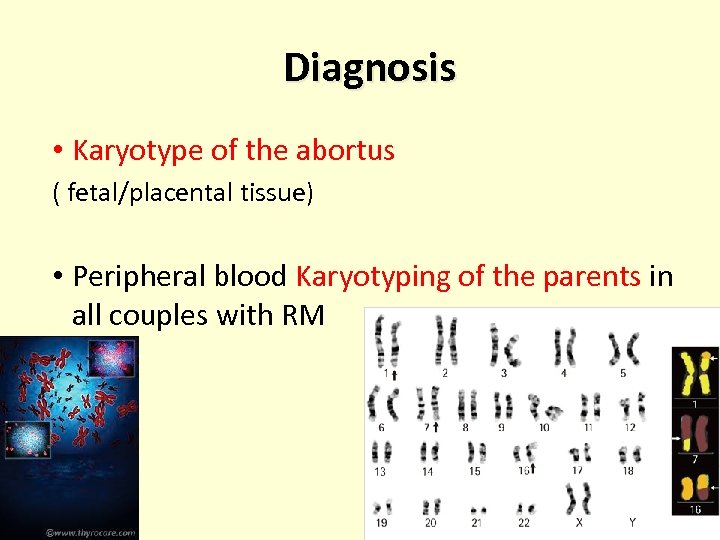 Diagnosis • Karyotype of the abortus ( fetal/placental tissue) • Peripheral blood Karyotyping of the parents in all couples with RM
Diagnosis • Karyotype of the abortus ( fetal/placental tissue) • Peripheral blood Karyotyping of the parents in all couples with RM
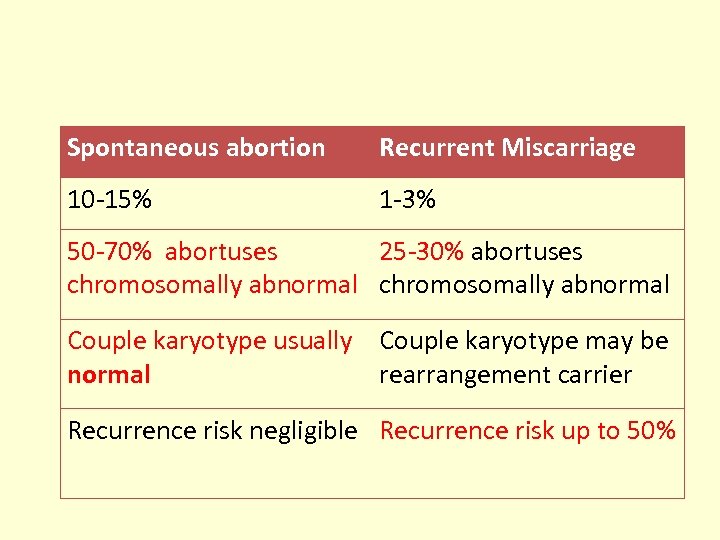 Spontaneous abortion Recurrent Miscarriage 10 -15% 1 -3% 50 -70% abortuses 25 -30% abortuses chromosomally abnormal Couple karyotype usually Couple karyotype may be normal rearrangement carrier Recurrence risk negligible Recurrence risk up to 50%
Spontaneous abortion Recurrent Miscarriage 10 -15% 1 -3% 50 -70% abortuses 25 -30% abortuses chromosomally abnormal Couple karyotype usually Couple karyotype may be normal rearrangement carrier Recurrence risk negligible Recurrence risk up to 50%
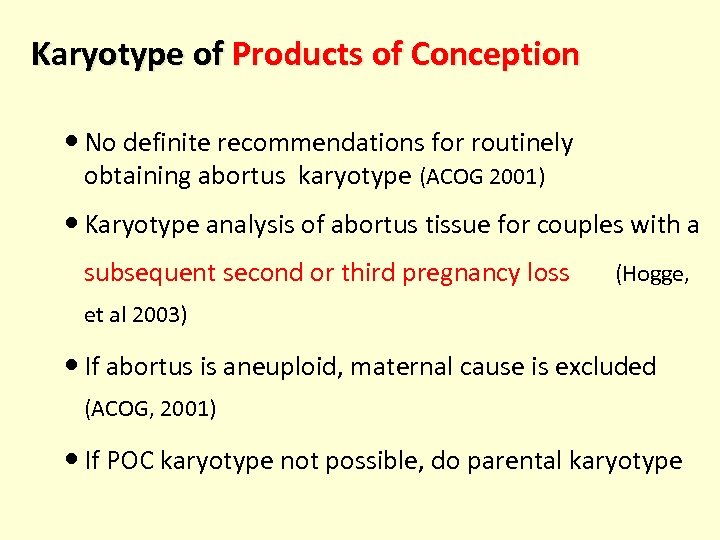 Karyotype of Products of Conception No definite recommendations for routinely obtaining abortus karyotype (ACOG 2001) Karyotype analysis of abortus tissue for couples with a subsequent second or third pregnancy loss (Hogge, et al 2003) If abortus is aneuploid, maternal cause is excluded (ACOG, 2001) If POC karyotype not possible, do parental karyotype
Karyotype of Products of Conception No definite recommendations for routinely obtaining abortus karyotype (ACOG 2001) Karyotype analysis of abortus tissue for couples with a subsequent second or third pregnancy loss (Hogge, et al 2003) If abortus is aneuploid, maternal cause is excluded (ACOG, 2001) If POC karyotype not possible, do parental karyotype
 Single Gene Disorders in RM • • Second and 3 rd trimester losses Alpha Thalassemia Myotonic dystrophy X linked Dominant disorder – – – Incontinentia Pigmenti Chondrodysplasia punctata Focal dermal hypoplasia of Goltz Rett Syndrome Aicardi Syndrome
Single Gene Disorders in RM • • Second and 3 rd trimester losses Alpha Thalassemia Myotonic dystrophy X linked Dominant disorder – – – Incontinentia Pigmenti Chondrodysplasia punctata Focal dermal hypoplasia of Goltz Rett Syndrome Aicardi Syndrome
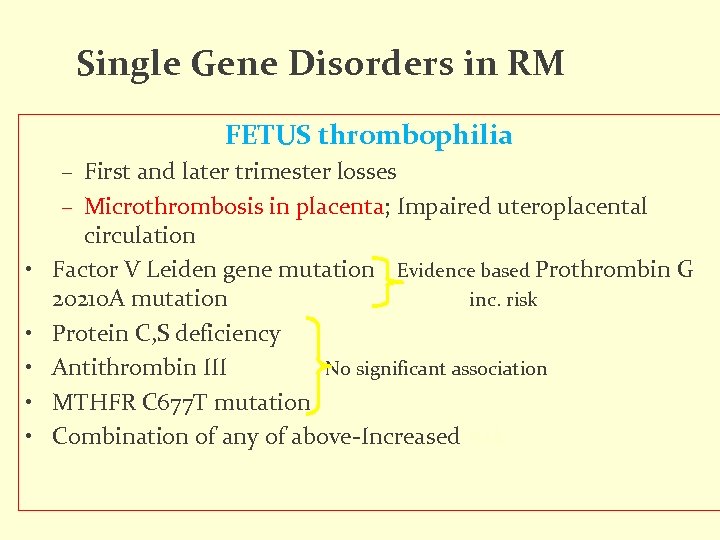 Single Gene Disorders in RM FETUS thrombophilia • • • – First and later trimester losses – Microthrombosis in placenta; Impaired uteroplacental circulation Factor V Leiden gene mutation Evidence based Prothrombin G 20210 A mutation inc. risk Protein C, S deficiency Antithrombin III No significant association MTHFR C 677 T mutation Combination of any of above-Increased risk
Single Gene Disorders in RM FETUS thrombophilia • • • – First and later trimester losses – Microthrombosis in placenta; Impaired uteroplacental circulation Factor V Leiden gene mutation Evidence based Prothrombin G 20210 A mutation inc. risk Protein C, S deficiency Antithrombin III No significant association MTHFR C 677 T mutation Combination of any of above-Increased risk
 Role of Infections
Role of Infections
 Doubtful causes of RPL • TORCH infections • Endocrine and metabolic disease – Untreated adrenal hyperplasia, hypothyroidism & diabetes mellitus. • Exogenous causes – Environmental factors, alcohol, street drugs, anesthesia gases etc
Doubtful causes of RPL • TORCH infections • Endocrine and metabolic disease – Untreated adrenal hyperplasia, hypothyroidism & diabetes mellitus. • Exogenous causes – Environmental factors, alcohol, street drugs, anesthesia gases etc
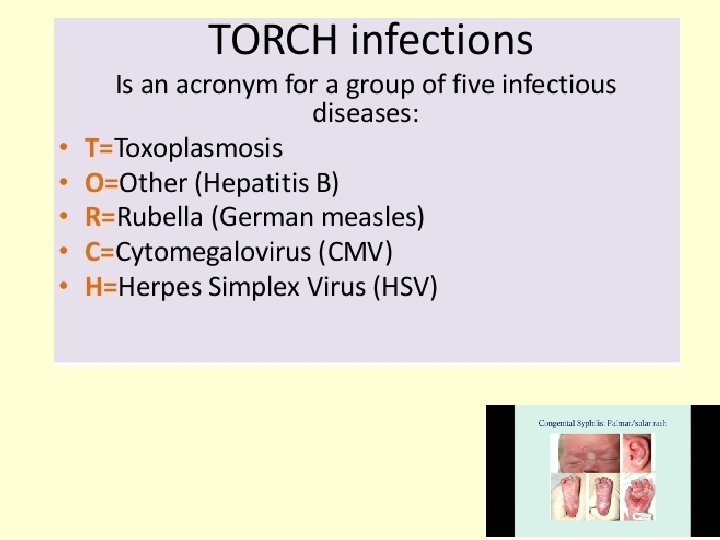 TORCH infections
TORCH infections
 Its time to say goodbye to TORCH tests……. TORCH T ESTS Cochrane Review has categorically proven in multiple meta-analysis that none of the “TORCH” group of infections are responsible for RECURRENT SPONTANEOUS ABORTIONS
Its time to say goodbye to TORCH tests……. TORCH T ESTS Cochrane Review has categorically proven in multiple meta-analysis that none of the “TORCH” group of infections are responsible for RECURRENT SPONTANEOUS ABORTIONS
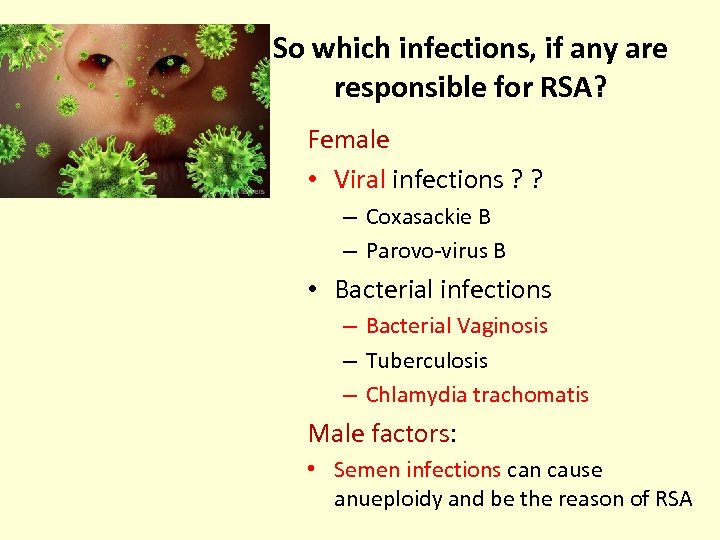 So which infections, if any are responsible for RSA? Female • Viral infections ? ? – Coxasackie B – Parovo-virus B • Bacterial infections – Bacterial Vaginosis – Tuberculosis – Chlamydia trachomatis Male factors: • Semen infections can cause anueploidy and be the reason of RSA
So which infections, if any are responsible for RSA? Female • Viral infections ? ? – Coxasackie B – Parovo-virus B • Bacterial infections – Bacterial Vaginosis – Tuberculosis – Chlamydia trachomatis Male factors: • Semen infections can cause anueploidy and be the reason of RSA
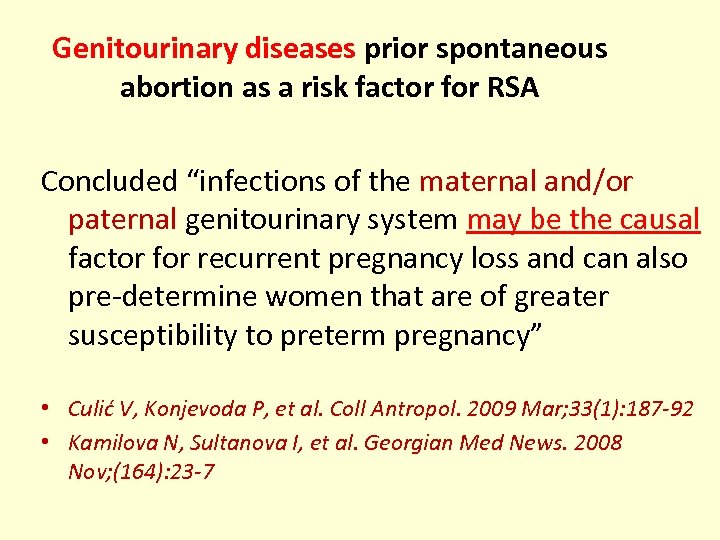 Genitourinary diseases prior spontaneous abortion as a risk factor for RSA Concluded “infections of the maternal and/or paternal genitourinary system may be the causal factor for recurrent pregnancy loss and can also pre-determine women that are of greater susceptibility to preterm pregnancy” • Culić V, Konjevoda P, et al. Coll Antropol. 2009 Mar; 33(1): 187 -92 • Kamilova N, Sultanova I, et al. Georgian Med News. 2008 Nov; (164): 23 -7
Genitourinary diseases prior spontaneous abortion as a risk factor for RSA Concluded “infections of the maternal and/or paternal genitourinary system may be the causal factor for recurrent pregnancy loss and can also pre-determine women that are of greater susceptibility to preterm pregnancy” • Culić V, Konjevoda P, et al. Coll Antropol. 2009 Mar; 33(1): 187 -92 • Kamilova N, Sultanova I, et al. Georgian Med News. 2008 Nov; (164): 23 -7
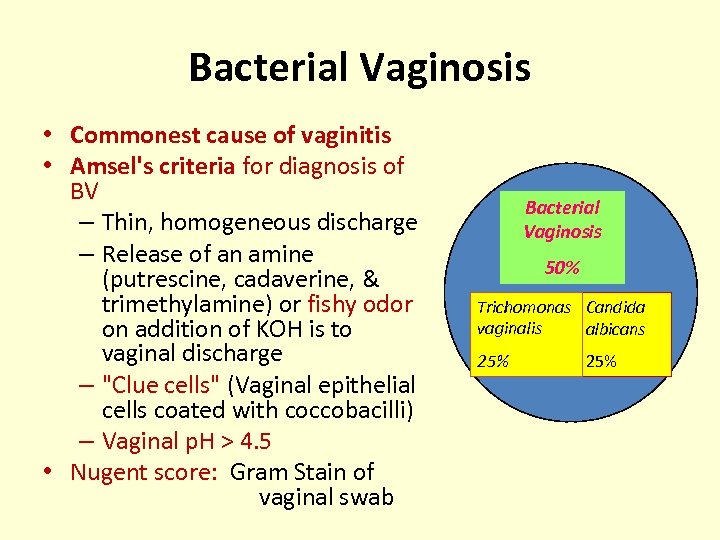 Bacterial Vaginosis • Commonest cause of vaginitis • Amsel's criteria for diagnosis of BV – Thin, homogeneous discharge – Release of an amine (putrescine, cadaverine, & trimethylamine) or fishy odor on addition of KOH is to vaginal discharge – "Clue cells" (Vaginal epithelial cells coated with coccobacilli) – Vaginal p. H > 4. 5 • Nugent score: Gram Stain of vaginal swab Bacterial Vaginosis 50% Trichomonas Candida vaginalis albicans 25%
Bacterial Vaginosis • Commonest cause of vaginitis • Amsel's criteria for diagnosis of BV – Thin, homogeneous discharge – Release of an amine (putrescine, cadaverine, & trimethylamine) or fishy odor on addition of KOH is to vaginal discharge – "Clue cells" (Vaginal epithelial cells coated with coccobacilli) – Vaginal p. H > 4. 5 • Nugent score: Gram Stain of vaginal swab Bacterial Vaginosis 50% Trichomonas Candida vaginalis albicans 25%
 BV and RSA • BV one of the most frequently founded cause of spontaneous abortions and prematurity birth • Diagnostics is easy and not expensive • High vaginal p. H is diagnostic • Treatment is simple using Metronidazole/Clindamycin 1. Damianov L, Damianova V. Akush Ginekol (Sofiia). 2004; 43 Suppl 2: 26 -7. 2. Mania-Pramanik J, Kerkar SC, et al. J Clin Lab Anal. 2008; 22(5): 375 -9. 3. Li TC, Makris M, et al. Hum Reprod Update. 2002 Sep-Oct; 8(5): 463 -81
BV and RSA • BV one of the most frequently founded cause of spontaneous abortions and prematurity birth • Diagnostics is easy and not expensive • High vaginal p. H is diagnostic • Treatment is simple using Metronidazole/Clindamycin 1. Damianov L, Damianova V. Akush Ginekol (Sofiia). 2004; 43 Suppl 2: 26 -7. 2. Mania-Pramanik J, Kerkar SC, et al. J Clin Lab Anal. 2008; 22(5): 375 -9. 3. Li TC, Makris M, et al. Hum Reprod Update. 2002 Sep-Oct; 8(5): 463 -81
 The influence of Chlamydia trachomatis infection on RSA Specific anti-chlamydial antibodies in 3 groups of women • Ig. A class – 7. 9% (p=0. 082) in group 1 (RSA group), – 4. 5% (p=0. 236) in group 2 (1 abortion) – 0% in group 3 ( no abortions) • Ig. G class in 21. 1% (p=0. 024), 36. 4% (p=0. 000) and in 4. 4%, respectively. CONCLUSIONS: • C. t. infection is an important causative agent in RSA • Anti-Chlamydial antobodies included in screening tests Wilkowska-Trojniel M. Adv Med Sci. 2009; 54(1): 86 -90 Kavalier F, BMJ. 2005 Jul 16; 331(7509): 121 -2.
The influence of Chlamydia trachomatis infection on RSA Specific anti-chlamydial antibodies in 3 groups of women • Ig. A class – 7. 9% (p=0. 082) in group 1 (RSA group), – 4. 5% (p=0. 236) in group 2 (1 abortion) – 0% in group 3 ( no abortions) • Ig. G class in 21. 1% (p=0. 024), 36. 4% (p=0. 000) and in 4. 4%, respectively. CONCLUSIONS: • C. t. infection is an important causative agent in RSA • Anti-Chlamydial antobodies included in screening tests Wilkowska-Trojniel M. Adv Med Sci. 2009; 54(1): 86 -90 Kavalier F, BMJ. 2005 Jul 16; 331(7509): 121 -2.
 Hattori Y, Nakanishi T. Am J Reprod Immunol. 2007 Oct; 58(4): 350 -7. • Uterine cervical inflammatory cytokines, interleukin 6 and - 8, as predictors of RSA • Both IL-6 and IL-8 in cervical mucus were significantly higher in patients who miscarried subsequently than in those who had a live birth.
Hattori Y, Nakanishi T. Am J Reprod Immunol. 2007 Oct; 58(4): 350 -7. • Uterine cervical inflammatory cytokines, interleukin 6 and - 8, as predictors of RSA • Both IL-6 and IL-8 in cervical mucus were significantly higher in patients who miscarried subsequently than in those who had a live birth.
 Is it time to look at the sperm?
Is it time to look at the sperm?
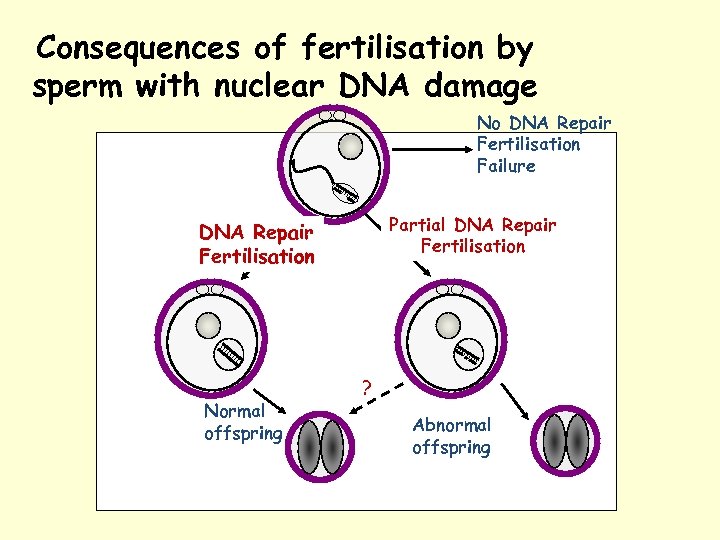 Consequences of fertilisation by sperm with nuclear DNA damage No DNA Repair Fertilisation Failure Partial DNA Repair Fertilisation Normal offspring ? Abnormal offspring
Consequences of fertilisation by sperm with nuclear DNA damage No DNA Repair Fertilisation Failure Partial DNA Repair Fertilisation Normal offspring ? Abnormal offspring
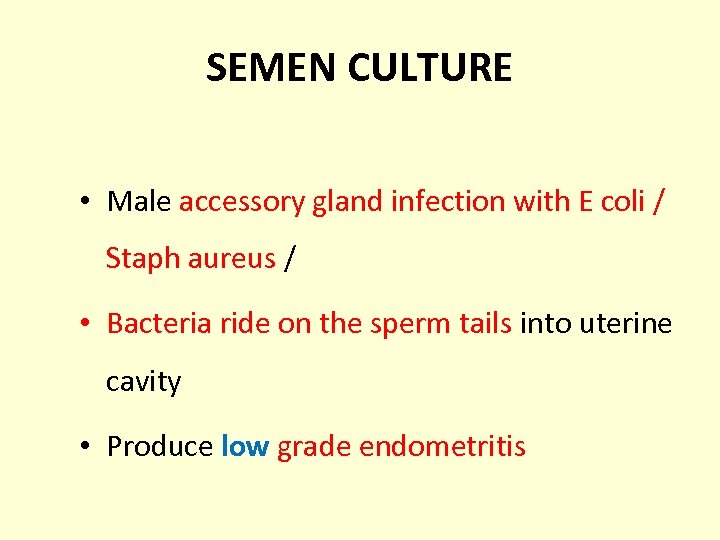 SEMEN CULTURE • Male accessory gland infection with E coli / Staph aureus / • Bacteria ride on the sperm tails into uterine cavity • Produce low grade endometritis
SEMEN CULTURE • Male accessory gland infection with E coli / Staph aureus / • Bacteria ride on the sperm tails into uterine cavity • Produce low grade endometritis
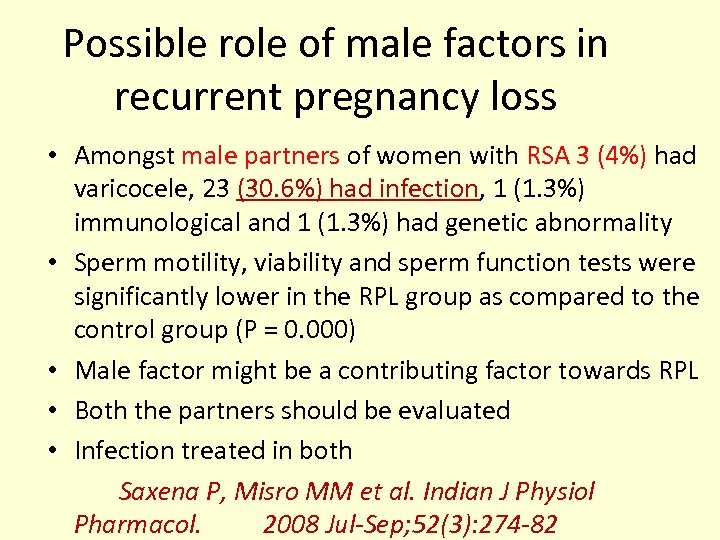 Possible role of male factors in recurrent pregnancy loss • Amongst male partners of women with RSA 3 (4%) had varicocele, 23 (30. 6%) had infection, 1 (1. 3%) immunological and 1 (1. 3%) had genetic abnormality • Sperm motility, viability and sperm function tests were significantly lower in the RPL group as compared to the control group (P = 0. 000) • Male factor might be a contributing factor towards RPL • Both the partners should be evaluated • Infection treated in both Saxena P, Misro MM et al. Indian J Physiol Pharmacol. 2008 Jul-Sep; 52(3): 274 -82
Possible role of male factors in recurrent pregnancy loss • Amongst male partners of women with RSA 3 (4%) had varicocele, 23 (30. 6%) had infection, 1 (1. 3%) immunological and 1 (1. 3%) had genetic abnormality • Sperm motility, viability and sperm function tests were significantly lower in the RPL group as compared to the control group (P = 0. 000) • Male factor might be a contributing factor towards RPL • Both the partners should be evaluated • Infection treated in both Saxena P, Misro MM et al. Indian J Physiol Pharmacol. 2008 Jul-Sep; 52(3): 274 -82
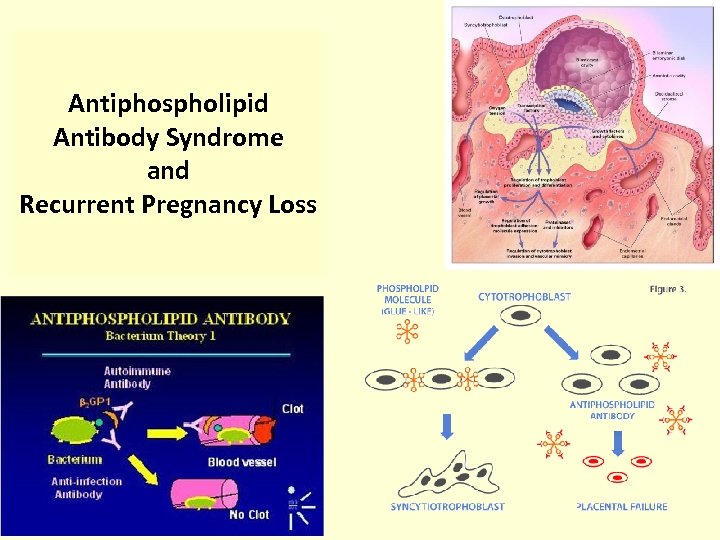 Antiphospholipid Antibody Syndrome and Recurrent Pregnancy Loss
Antiphospholipid Antibody Syndrome and Recurrent Pregnancy Loss
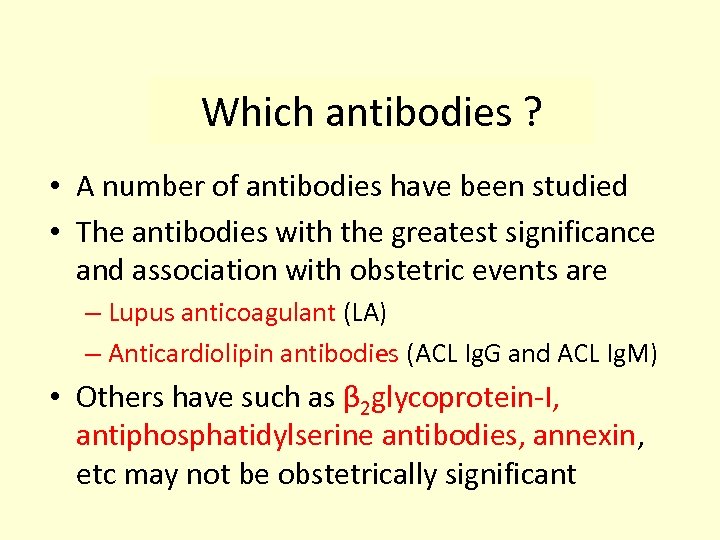 Which antibodies ? • A number of antibodies have been studied • The antibodies with the greatest significance and association with obstetric events are – Lupus anticoagulant (LA) – Anticardiolipin antibodies (ACL Ig. G and ACL Ig. M) • Others have such as β 2 glycoprotein-I, antiphosphatidylserine antibodies, annexin, etc may not be obstetrically significant
Which antibodies ? • A number of antibodies have been studied • The antibodies with the greatest significance and association with obstetric events are – Lupus anticoagulant (LA) – Anticardiolipin antibodies (ACL Ig. G and ACL Ig. M) • Others have such as β 2 glycoprotein-I, antiphosphatidylserine antibodies, annexin, etc may not be obstetrically significant
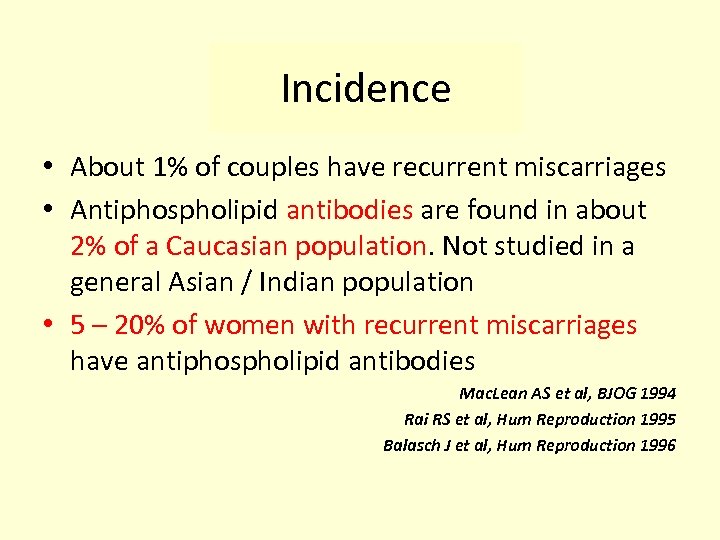 Incidence • About 1% of couples have recurrent miscarriages • Antiphospholipid antibodies are found in about 2% of a Caucasian population. Not studied in a general Asian / Indian population • 5 – 20% of women with recurrent miscarriages have antiphospholipid antibodies Mac. Lean AS et al, BJOG 1994 Rai RS et al, Hum Reproduction 1995 Balasch J et al, Hum Reproduction 1996
Incidence • About 1% of couples have recurrent miscarriages • Antiphospholipid antibodies are found in about 2% of a Caucasian population. Not studied in a general Asian / Indian population • 5 – 20% of women with recurrent miscarriages have antiphospholipid antibodies Mac. Lean AS et al, BJOG 1994 Rai RS et al, Hum Reproduction 1995 Balasch J et al, Hum Reproduction 1996
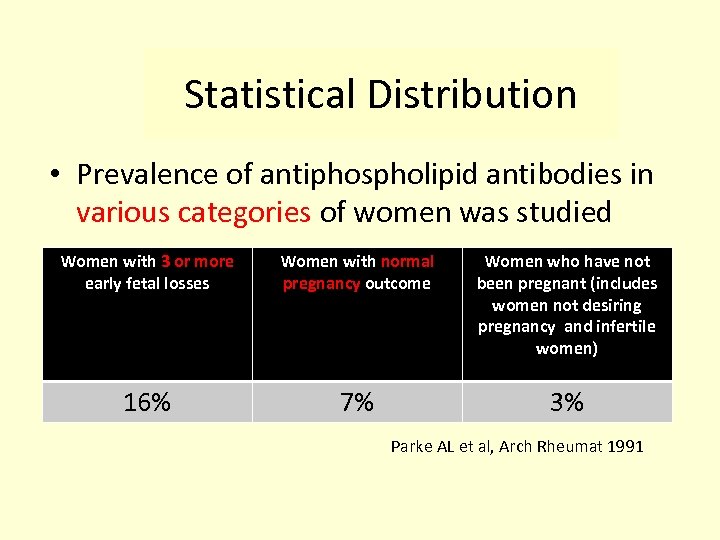 Statistical Distribution • Prevalence of antiphospholipid antibodies in various categories of women was studied Women with 3 or more early fetal losses Women with normal pregnancy outcome Women who have not been pregnant (includes women not desiring pregnancy and infertile women) 16% 7% 3% Parke AL et al, Arch Rheumat 1991
Statistical Distribution • Prevalence of antiphospholipid antibodies in various categories of women was studied Women with 3 or more early fetal losses Women with normal pregnancy outcome Women who have not been pregnant (includes women not desiring pregnancy and infertile women) 16% 7% 3% Parke AL et al, Arch Rheumat 1991
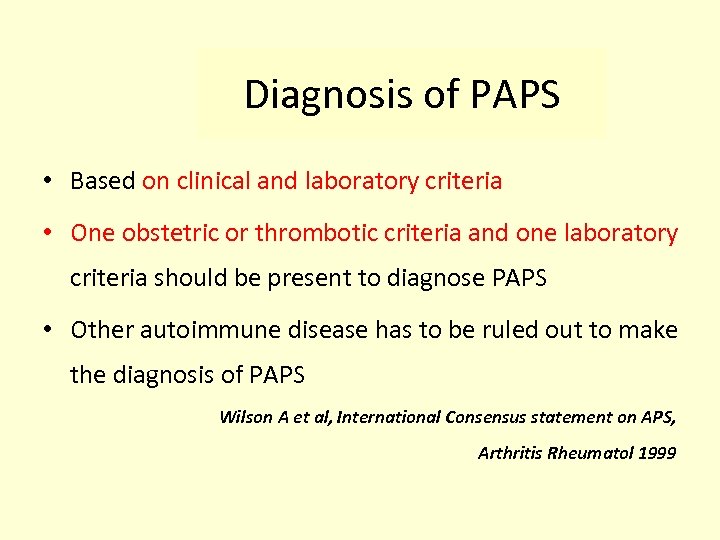 Diagnosis of PAPS • Based on clinical and laboratory criteria • One obstetric or thrombotic criteria and one laboratory criteria should be present to diagnose PAPS • Other autoimmune disease has to be ruled out to make the diagnosis of PAPS Wilson A et al, International Consensus statement on APS, Arthritis Rheumatol 1999
Diagnosis of PAPS • Based on clinical and laboratory criteria • One obstetric or thrombotic criteria and one laboratory criteria should be present to diagnose PAPS • Other autoimmune disease has to be ruled out to make the diagnosis of PAPS Wilson A et al, International Consensus statement on APS, Arthritis Rheumatol 1999
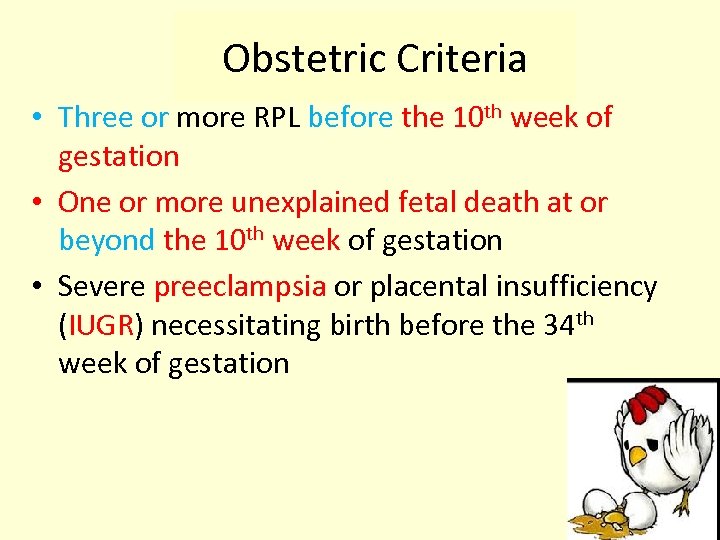 Obstetric Criteria • Three or more RPL before the 10 th week of gestation • One or more unexplained fetal death at or beyond the 10 th week of gestation • Severe preeclampsia or placental insufficiency (IUGR) necessitating birth before the 34 th week of gestation
Obstetric Criteria • Three or more RPL before the 10 th week of gestation • One or more unexplained fetal death at or beyond the 10 th week of gestation • Severe preeclampsia or placental insufficiency (IUGR) necessitating birth before the 34 th week of gestation
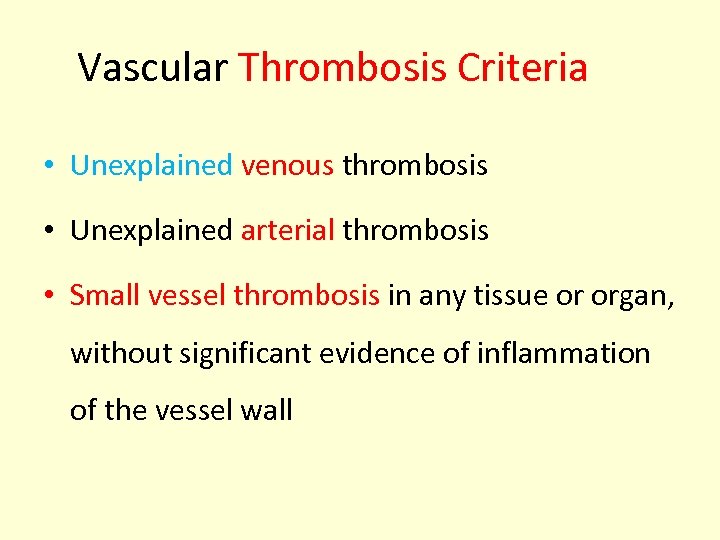 Vascular Thrombosis Criteria • Unexplained venous thrombosis • Unexplained arterial thrombosis • Small vessel thrombosis in any tissue or organ, without significant evidence of inflammation of the vessel wall
Vascular Thrombosis Criteria • Unexplained venous thrombosis • Unexplained arterial thrombosis • Small vessel thrombosis in any tissue or organ, without significant evidence of inflammation of the vessel wall
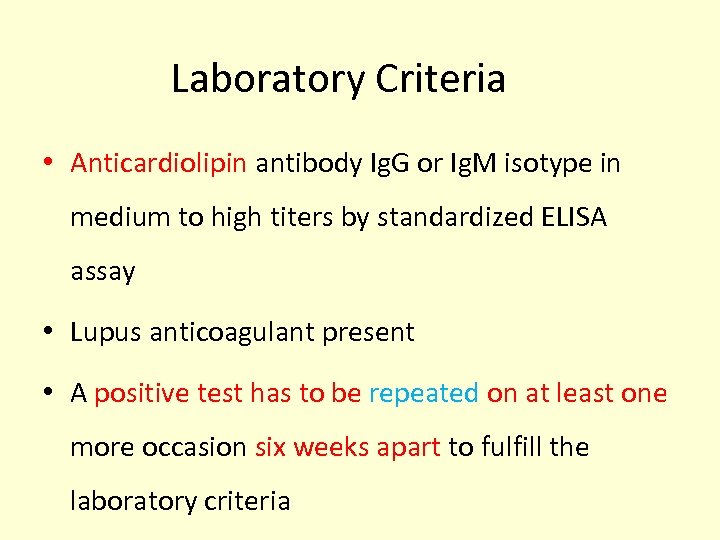 Laboratory Criteria • Anticardiolipin antibody Ig. G or Ig. M isotype in medium to high titers by standardized ELISA assay • Lupus anticoagulant present • A positive test has to be repeated on at least one more occasion six weeks apart to fulfill the laboratory criteria
Laboratory Criteria • Anticardiolipin antibody Ig. G or Ig. M isotype in medium to high titers by standardized ELISA assay • Lupus anticoagulant present • A positive test has to be repeated on at least one more occasion six weeks apart to fulfill the laboratory criteria
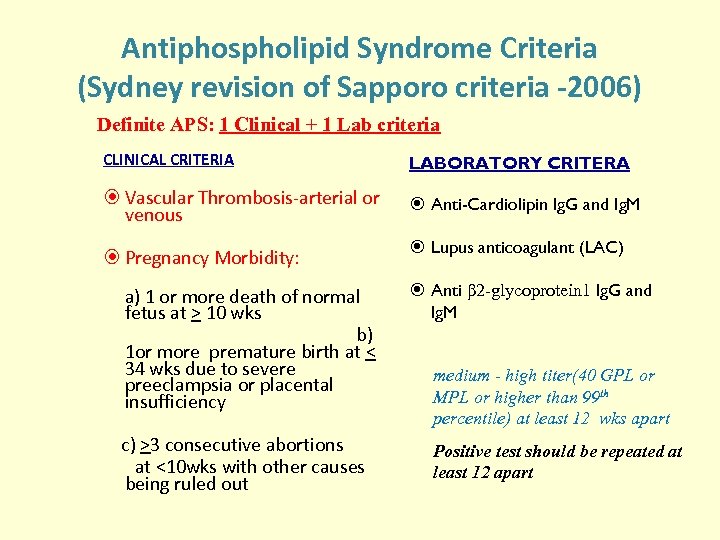 Antiphospholipid Syndrome Criteria (Sydney revision of Sapporo criteria -2006) Definite APS: 1 Clinical + 1 Lab criteria CLINICAL CRITERIA LABORATORY CRITERA Vascular Thrombosis-arterial or venous Anti-Cardiolipin Ig. G and Ig. M Lupus anticoagulant (LAC) Pregnancy Morbidity: Anti β 2 -glycoprotein 1 Ig. G and a) 1 or more death of normal Ig. M fetus at > 10 wks b) 1 or more premature birth at < 34 wks due to severe medium - high titer(40 GPL or preeclampsia or placental MPL or higher than 99 th insufficiency percentile) at least 12 wks apart c) >3 consecutive abortions at <10 wks with other causes being ruled out Positive test should be repeated at least 12 apart
Antiphospholipid Syndrome Criteria (Sydney revision of Sapporo criteria -2006) Definite APS: 1 Clinical + 1 Lab criteria CLINICAL CRITERIA LABORATORY CRITERA Vascular Thrombosis-arterial or venous Anti-Cardiolipin Ig. G and Ig. M Lupus anticoagulant (LAC) Pregnancy Morbidity: Anti β 2 -glycoprotein 1 Ig. G and a) 1 or more death of normal Ig. M fetus at > 10 wks b) 1 or more premature birth at < 34 wks due to severe medium - high titer(40 GPL or preeclampsia or placental MPL or higher than 99 th insufficiency percentile) at least 12 wks apart c) >3 consecutive abortions at <10 wks with other causes being ruled out Positive test should be repeated at least 12 apart
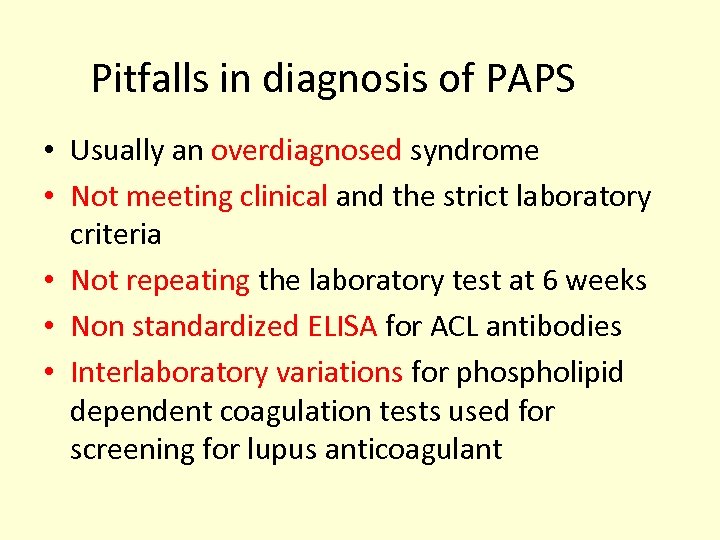 Pitfalls in diagnosis of PAPS • Usually an overdiagnosed syndrome • Not meeting clinical and the strict laboratory criteria • Not repeating the laboratory test at 6 weeks • Non standardized ELISA for ACL antibodies • Interlaboratory variations for phospholipid dependent coagulation tests used for screening for lupus anticoagulant
Pitfalls in diagnosis of PAPS • Usually an overdiagnosed syndrome • Not meeting clinical and the strict laboratory criteria • Not repeating the laboratory test at 6 weeks • Non standardized ELISA for ACL antibodies • Interlaboratory variations for phospholipid dependent coagulation tests used for screening for lupus anticoagulant
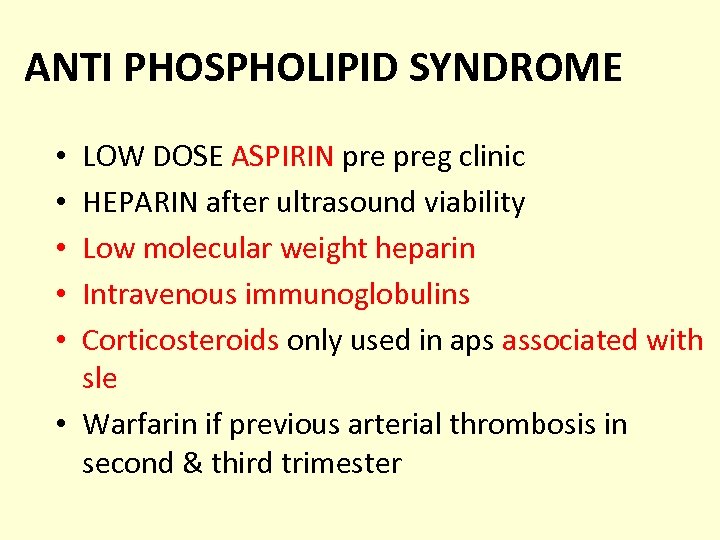 ANTI PHOSPHOLIPID SYNDROME LOW DOSE ASPIRIN preg clinic HEPARIN after ultrasound viability Low molecular weight heparin Intravenous immunoglobulins Corticosteroids only used in aps associated with sle • Warfarin if previous arterial thrombosis in second & third trimester • • •
ANTI PHOSPHOLIPID SYNDROME LOW DOSE ASPIRIN preg clinic HEPARIN after ultrasound viability Low molecular weight heparin Intravenous immunoglobulins Corticosteroids only used in aps associated with sle • Warfarin if previous arterial thrombosis in second & third trimester • • •
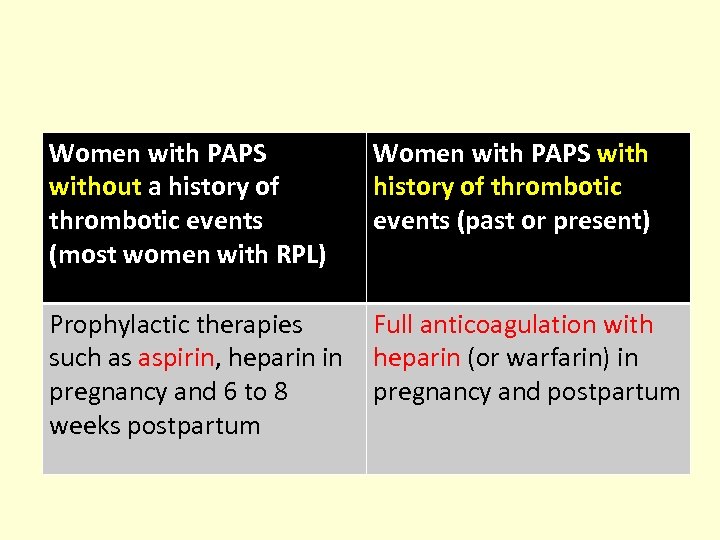 Women with PAPS without a history of thrombotic events (most women with RPL) Women with PAPS with history of thrombotic events (past or present) Prophylactic therapies Full anticoagulation with such as aspirin, heparin in heparin (or warfarin) in pregnancy and 6 to 8 pregnancy and postpartum weeks postpartum
Women with PAPS without a history of thrombotic events (most women with RPL) Women with PAPS with history of thrombotic events (past or present) Prophylactic therapies Full anticoagulation with such as aspirin, heparin in heparin (or warfarin) in pregnancy and 6 to 8 pregnancy and postpartum weeks postpartum
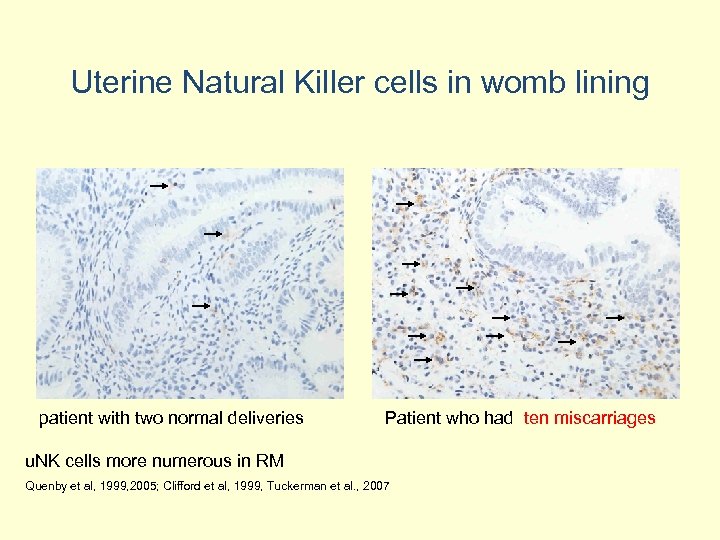 Uterine Natural Killer cells in womb lining patient with two normal deliveries Patient who had ten miscarriages u. NK cells more numerous in RM Quenby et al, 1999, 2005; Clifford et al, 1999, Tuckerman et al. , 2007
Uterine Natural Killer cells in womb lining patient with two normal deliveries Patient who had ten miscarriages u. NK cells more numerous in RM Quenby et al, 1999, 2005; Clifford et al, 1999, Tuckerman et al. , 2007
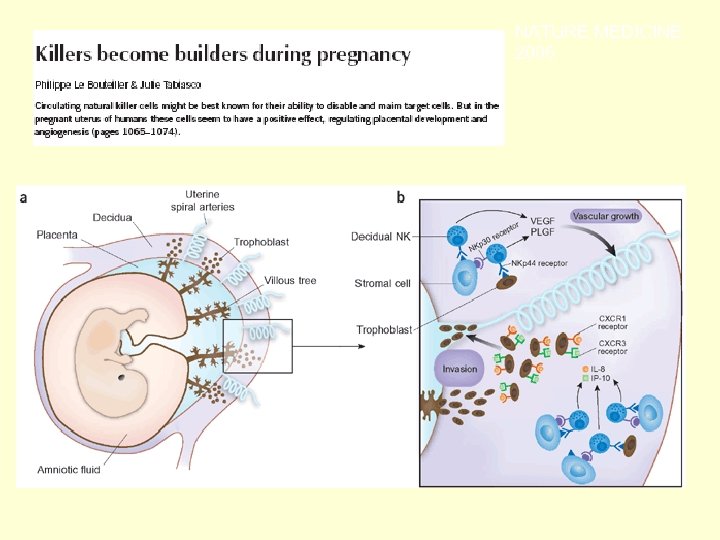 NATURE MEDICINE 2006
NATURE MEDICINE 2006
 ALLOIMMUNE CAUSES Progesterone therapy Evidence for use
ALLOIMMUNE CAUSES Progesterone therapy Evidence for use
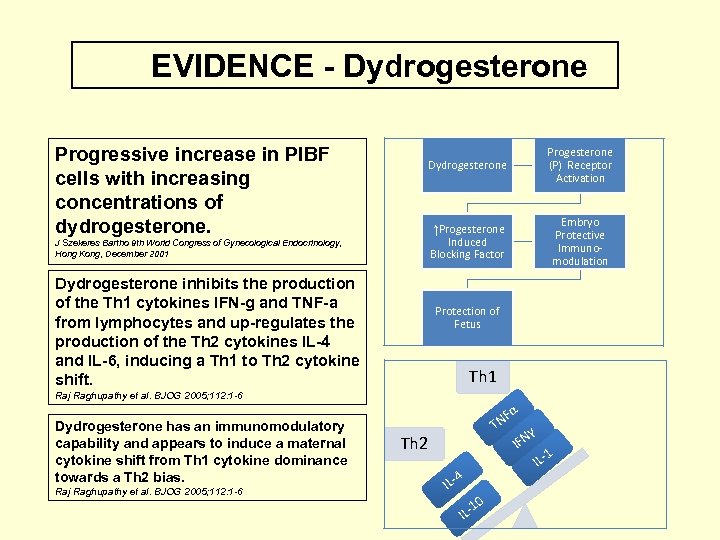 EVIDENCE - Dydrogesterone Progressive increase in PIBF cells with increasing concentrations of dydrogesterone. Dydrogesterone ↑Progesterone Induced Blocking Factor J Szekeres Bartho 9 th World Congress of Gynecological Endocrinology, Hong Kong, December 2001 Dydrogesterone inhibits the production of the Th 1 cytokines IFN-g and TNF-a from lymphocytes and up-regulates the production of the Th 2 cytokines IL-4 and IL-6, inducing a Th 1 to Th 2 cytokine shift. Progesterone (P) Receptor Activation Embryo Protective Immunomodulation Protection of Fetus Th 1 Raj Raghupathy et al. BJOG 2005; 112: 1 -6 Dydrogesterone has an immunomodulatory capability and appears to induce a maternal cytokine shift from Th 1 cytokine dominance towards a Th 2 bias. Raj Raghupathy et al. BJOG 2005; 112: 1 -6 Fα TN Th 2 4 IL- 0 1 IL- IFN γ 1 IL-
EVIDENCE - Dydrogesterone Progressive increase in PIBF cells with increasing concentrations of dydrogesterone. Dydrogesterone ↑Progesterone Induced Blocking Factor J Szekeres Bartho 9 th World Congress of Gynecological Endocrinology, Hong Kong, December 2001 Dydrogesterone inhibits the production of the Th 1 cytokines IFN-g and TNF-a from lymphocytes and up-regulates the production of the Th 2 cytokines IL-4 and IL-6, inducing a Th 1 to Th 2 cytokine shift. Progesterone (P) Receptor Activation Embryo Protective Immunomodulation Protection of Fetus Th 1 Raj Raghupathy et al. BJOG 2005; 112: 1 -6 Dydrogesterone has an immunomodulatory capability and appears to induce a maternal cytokine shift from Th 1 cytokine dominance towards a Th 2 bias. Raj Raghupathy et al. BJOG 2005; 112: 1 -6 Fα TN Th 2 4 IL- 0 1 IL- IFN γ 1 IL-
 ENDOCRINAL FACTORS • Polycystic ovaries ? metformin • Luteal phase defects progesterone / Duphaston • Thyroid replacement therapy • Optimising Hb. A 1 c levels • Correct hyperprolactinaemia
ENDOCRINAL FACTORS • Polycystic ovaries ? metformin • Luteal phase defects progesterone / Duphaston • Thyroid replacement therapy • Optimising Hb. A 1 c levels • Correct hyperprolactinaemia
 Thrombophilia Predisposition for thrombotic events Deep vein thrombosis Pulmonary embolism
Thrombophilia Predisposition for thrombotic events Deep vein thrombosis Pulmonary embolism
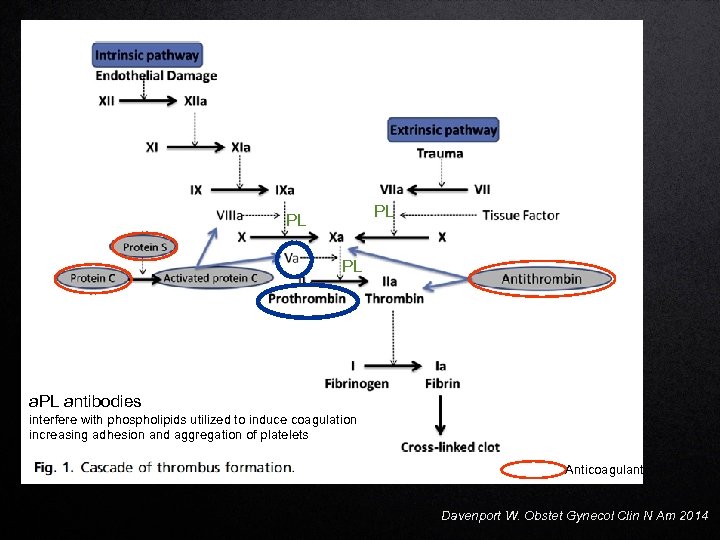 PL PL PL antibodies interfere with phospholipids utilized to induce coagulation increasing adhesion and aggregation of platelets Anticoagulant Davenport W. Obstet Gynecol Clin N Am 2014
PL PL PL antibodies interfere with phospholipids utilized to induce coagulation increasing adhesion and aggregation of platelets Anticoagulant Davenport W. Obstet Gynecol Clin N Am 2014
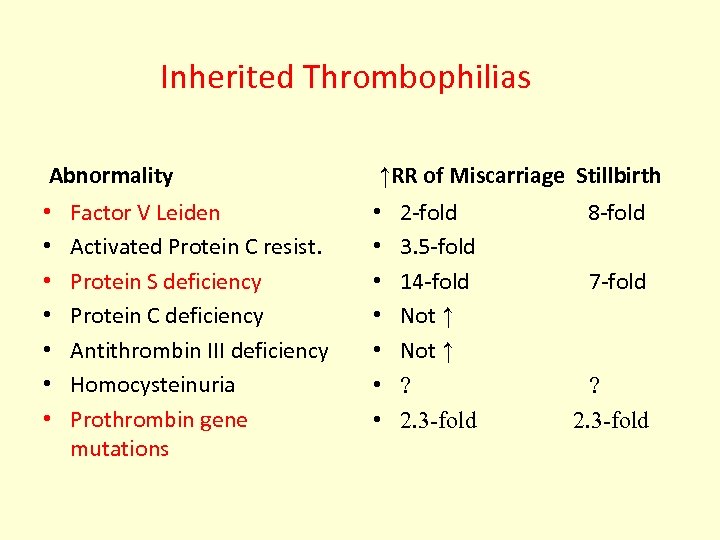 Inherited Thrombophilias Abnormality • • Factor V Leiden Activated Protein C resist. Protein S deficiency Protein C deficiency Antithrombin III deficiency Homocysteinuria Prothrombin gene mutations ↑RR of Miscarriage Stillbirth • • 2 -fold 8 -fold 3. 5 -fold 14 -fold 7 -fold Not ↑ ? ? 2. 3 -fold
Inherited Thrombophilias Abnormality • • Factor V Leiden Activated Protein C resist. Protein S deficiency Protein C deficiency Antithrombin III deficiency Homocysteinuria Prothrombin gene mutations ↑RR of Miscarriage Stillbirth • • 2 -fold 8 -fold 3. 5 -fold 14 -fold 7 -fold Not ↑ ? ? 2. 3 -fold
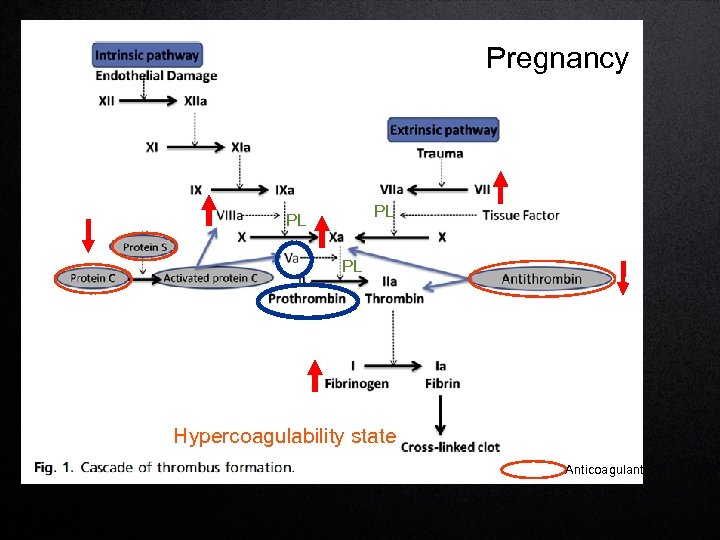 Pregnancy PL PL PL Hypercoagulability state Anticoagulant
Pregnancy PL PL PL Hypercoagulability state Anticoagulant
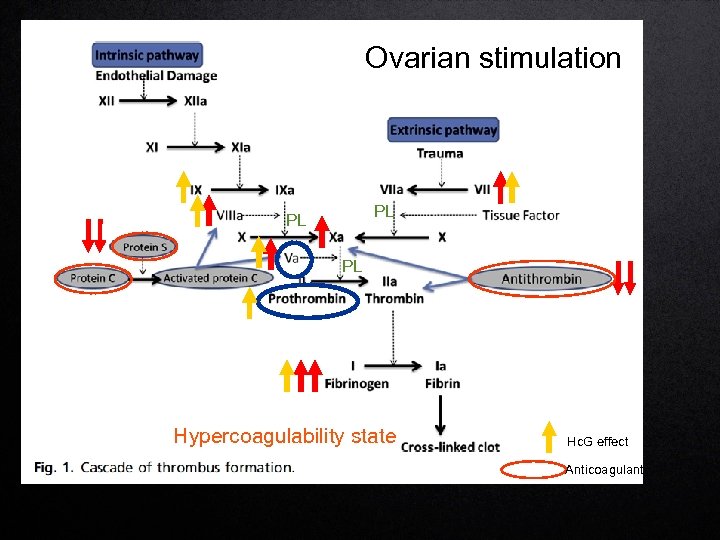 Ovarian stimulation PL PL PL Hypercoagulability state Hc. G effect Anticoagulant
Ovarian stimulation PL PL PL Hypercoagulability state Hc. G effect Anticoagulant
 Battinelli EM. Thrombosis 2013
Battinelli EM. Thrombosis 2013
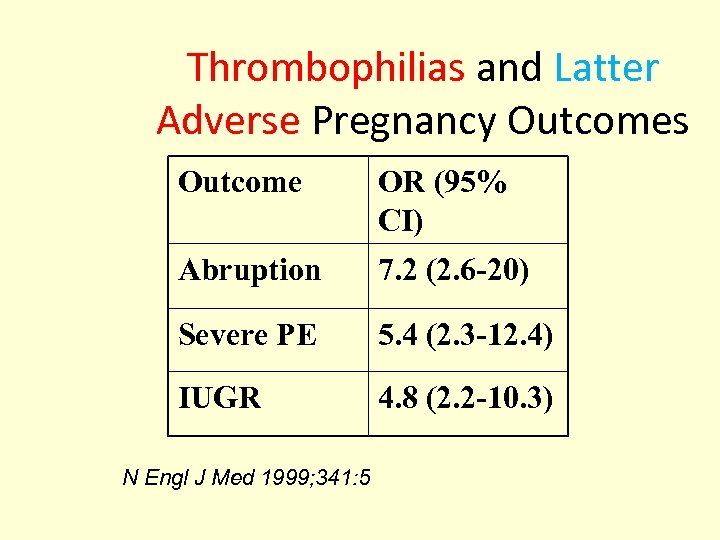 Thrombophilias and Latter Adverse Pregnancy Outcomes Outcome OR (95% CI) Abruption 7. 2 (2. 6 -20) Severe PE 5. 4 (2. 3 -12. 4) IUGR 4. 8 (2. 2 -10. 3) N Engl J Med 1999; 341: 5
Thrombophilias and Latter Adverse Pregnancy Outcomes Outcome OR (95% CI) Abruption 7. 2 (2. 6 -20) Severe PE 5. 4 (2. 3 -12. 4) IUGR 4. 8 (2. 2 -10. 3) N Engl J Med 1999; 341: 5
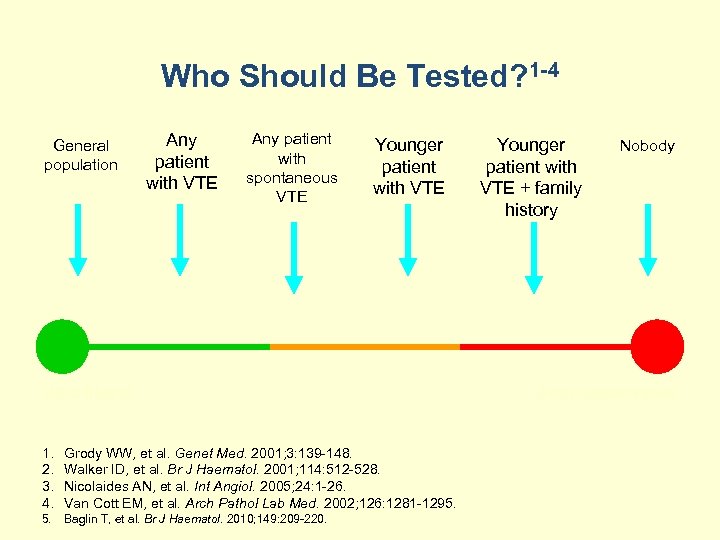 Who Should Be Tested? 1 -4 General population Any patient with VTE Any patient with spontaneous VTE Younger patient with VTE Ultra-liberal 1. 2. 3. 4. Grody WW, et al. Genet Med. 2001; 3: 139 -148. Walker ID, et al. Br J Haematol. 2001; 114: 512 -528. Nicolaides AN, et al. Int Angiol. 2005; 24: 1 -26. Van Cott EM, et al. Arch Pathol Lab Med. 2002; 126: 1281 -1295. 5. Baglin T, et al. Br J Haematol. 2010; 149: 209 -220. Younger patient with VTE + family history Nobody Arch-conservative
Who Should Be Tested? 1 -4 General population Any patient with VTE Any patient with spontaneous VTE Younger patient with VTE Ultra-liberal 1. 2. 3. 4. Grody WW, et al. Genet Med. 2001; 3: 139 -148. Walker ID, et al. Br J Haematol. 2001; 114: 512 -528. Nicolaides AN, et al. Int Angiol. 2005; 24: 1 -26. Van Cott EM, et al. Arch Pathol Lab Med. 2002; 126: 1281 -1295. 5. Baglin T, et al. Br J Haematol. 2010; 149: 209 -220. Younger patient with VTE + family history Nobody Arch-conservative
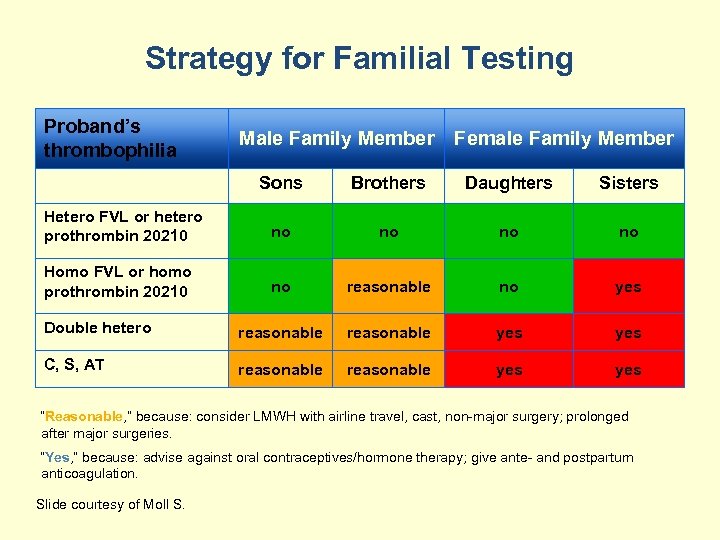 Strategy for Familial Testing Proband’s thrombophilia Male Family Member Female Family Member Sons Brothers Daughters Sisters Hetero FVL or hetero prothrombin 20210 no no Homo FVL or homo prothrombin 20210 no reasonable no yes Double hetero reasonable yes C, S, AT reasonable yes “Reasonable, ” because: consider LMWH with airline travel, cast, non-major surgery; prolonged after major surgeries. “Yes, ” because: advise against oral contraceptives/hormone therapy; give ante- and postpartum anticoagulation. Slide courtesy of Moll S.
Strategy for Familial Testing Proband’s thrombophilia Male Family Member Female Family Member Sons Brothers Daughters Sisters Hetero FVL or hetero prothrombin 20210 no no Homo FVL or homo prothrombin 20210 no reasonable no yes Double hetero reasonable yes C, S, AT reasonable yes “Reasonable, ” because: consider LMWH with airline travel, cast, non-major surgery; prolonged after major surgeries. “Yes, ” because: advise against oral contraceptives/hormone therapy; give ante- and postpartum anticoagulation. Slide courtesy of Moll S.
 THROMBOPHILIA SCREEN POSITIVE • LOW MOLECULAR WEIGHT HEPARIN • UNFRACTIONATED HEPARIN (From 6 weeks to 36 weeks of pregnancy)
THROMBOPHILIA SCREEN POSITIVE • LOW MOLECULAR WEIGHT HEPARIN • UNFRACTIONATED HEPARIN (From 6 weeks to 36 weeks of pregnancy)
 Pregnancy thrombophilia - the unsuspected risk Rijeka, Croatia: In. Tech; 2013.
Pregnancy thrombophilia - the unsuspected risk Rijeka, Croatia: In. Tech; 2013.
 ROLE OF TENDER LOVING CARE
ROLE OF TENDER LOVING CARE
 DESTRESS & REASSURE • Psycho-neuro-immunology • Stress affects immune system • Changes th 2 response in endometrium to th 1 response • Hypothalamus affects endocrine system • Adrenaline release reduces placental blood flow
DESTRESS & REASSURE • Psycho-neuro-immunology • Stress affects immune system • Changes th 2 response in endometrium to th 1 response • Hypothalamus affects endocrine system • Adrenaline release reduces placental blood flow
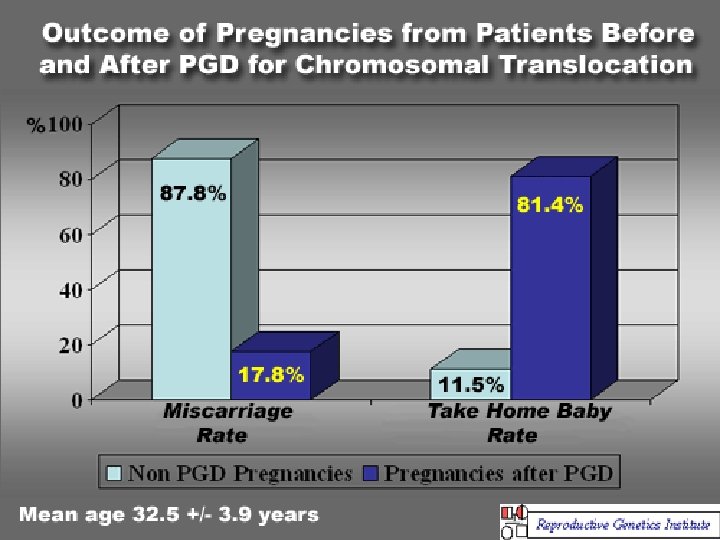
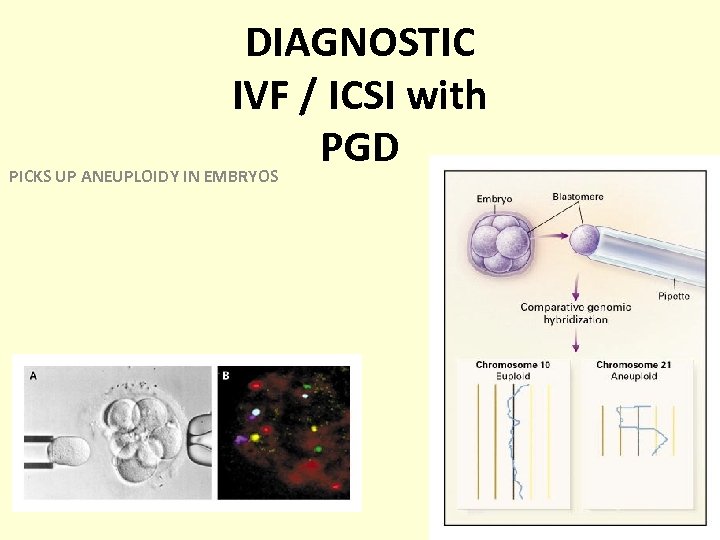 DIAGNOSTIC IVF / ICSI with PGD PICKS UP ANEUPLOIDY IN EMBRYOS
DIAGNOSTIC IVF / ICSI with PGD PICKS UP ANEUPLOIDY IN EMBRYOS
 SURROGACY n If diagnostic IVF & PGD confirm normal gametes / embryos n All treatment modalities have failed
SURROGACY n If diagnostic IVF & PGD confirm normal gametes / embryos n All treatment modalities have failed
 Conclusion / Problems of RPL • The cause of individual abortion may be different • More than one factor may exist • Thorough investigation often fails to reveal a cause Fertil Steril. 2010 Mar 1; 93(4): 1234 -43. Epub 2009 Mar 31
Conclusion / Problems of RPL • The cause of individual abortion may be different • More than one factor may exist • Thorough investigation often fails to reveal a cause Fertil Steril. 2010 Mar 1; 93(4): 1234 -43. Epub 2009 Mar 31
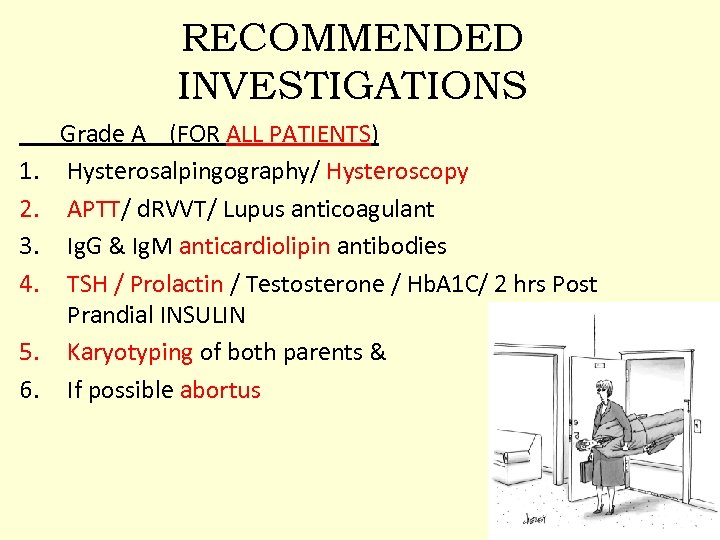 RECOMMENDED INVESTIGATIONS Grade A (FOR ALL PATIENTS) 1. Hysterosalpingography/ Hysteroscopy 2. APTT/ d. RVVT/ Lupus anticoagulant 3. Ig. G & Ig. M anticardiolipin antibodies 4. TSH / Prolactin / Testosterone / Hb. A 1 C/ 2 hrs Post Prandial INSULIN 5. Karyotyping of both parents & 6. If possible abortus
RECOMMENDED INVESTIGATIONS Grade A (FOR ALL PATIENTS) 1. Hysterosalpingography/ Hysteroscopy 2. APTT/ d. RVVT/ Lupus anticoagulant 3. Ig. G & Ig. M anticardiolipin antibodies 4. TSH / Prolactin / Testosterone / Hb. A 1 C/ 2 hrs Post Prandial INSULIN 5. Karyotyping of both parents & 6. If possible abortus
 RECOMMENDED INVESTIGATIONS Grade B (FOR SELECTED PATIENTS) 1. 2. 3. 4. 5. 6. ANDROGENS, LH, FSH IN PATIENTS WITH IRREGULAR MENSTRUATION SERUM PROGESTERONE EB FOR DATING & TB PCR, CULTURE SERUM HOMOCYSTEINE LEVELS / THROMBOPHILIA SCREEN HVS / WET PREP & p. H / KOH Whiff test SEMEN CULTURE / TB PCR
RECOMMENDED INVESTIGATIONS Grade B (FOR SELECTED PATIENTS) 1. 2. 3. 4. 5. 6. ANDROGENS, LH, FSH IN PATIENTS WITH IRREGULAR MENSTRUATION SERUM PROGESTERONE EB FOR DATING & TB PCR, CULTURE SERUM HOMOCYSTEINE LEVELS / THROMBOPHILIA SCREEN HVS / WET PREP & p. H / KOH Whiff test SEMEN CULTURE / TB PCR



