b790f7d6c531ab60dbb87b68bb072762.ppt
- Количество слайдов: 12
 1 How data can improve health care What we don’t know can hurt us Gov 2. 0 September 10, 2009 Elliott Fisher, MD, MPH Director, Population Health and Policy The Dartmouth Institute for Health Policy and Clinical Practice
1 How data can improve health care What we don’t know can hurt us Gov 2. 0 September 10, 2009 Elliott Fisher, MD, MPH Director, Population Health and Policy The Dartmouth Institute for Health Policy and Clinical Practice
 The current conundrum Rising costs a serious threat Medicare Trust Fund – runs dry 2017 Cost of family coverage projected to double ($12, 298 to $23, 842 by 2020) Two million Americans affected by medical bankruptcy each year Barriers Fear of rationing, of change, that lower cost = lower quality Ignorance of where the money’s going in health care of how to do better Data can help: four examples Regional variations in spending and quality: where’s the waste? Identifying high-performing systems -- from whom we can learn Supporting change in clinical practice Motivating change in health systems
The current conundrum Rising costs a serious threat Medicare Trust Fund – runs dry 2017 Cost of family coverage projected to double ($12, 298 to $23, 842 by 2020) Two million Americans affected by medical bankruptcy each year Barriers Fear of rationing, of change, that lower cost = lower quality Ignorance of where the money’s going in health care of how to do better Data can help: four examples Regional variations in spending and quality: where’s the waste? Identifying high-performing systems -- from whom we can learn Supporting change in clinical practice Motivating change in health systems
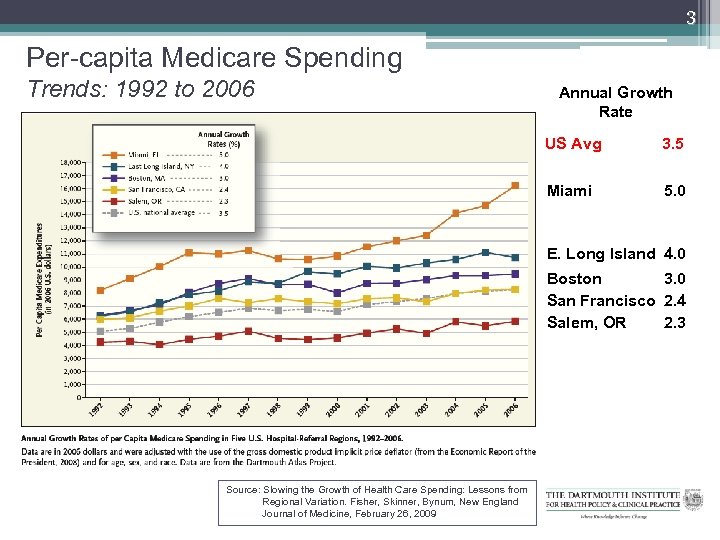 3 Per-capita Medicare Spending Trends: 1992 to 2006 Annual Growth Rate US Avg 3. 5 Miami 5. 0 E. Long Island 4. 0 Boston 3. 0 San Francisco 2. 4 Salem, OR 2. 3 Source: Slowing the Growth of Health Care Spending: Lessons from Regional Variation. Fisher, Skinner, Bynum, New England Journal of Medicine, February 26, 2009
3 Per-capita Medicare Spending Trends: 1992 to 2006 Annual Growth Rate US Avg 3. 5 Miami 5. 0 E. Long Island 4. 0 Boston 3. 0 San Francisco 2. 4 Salem, OR 2. 3 Source: Slowing the Growth of Health Care Spending: Lessons from Regional Variation. Fisher, Skinner, Bynum, New England Journal of Medicine, February 26, 2009
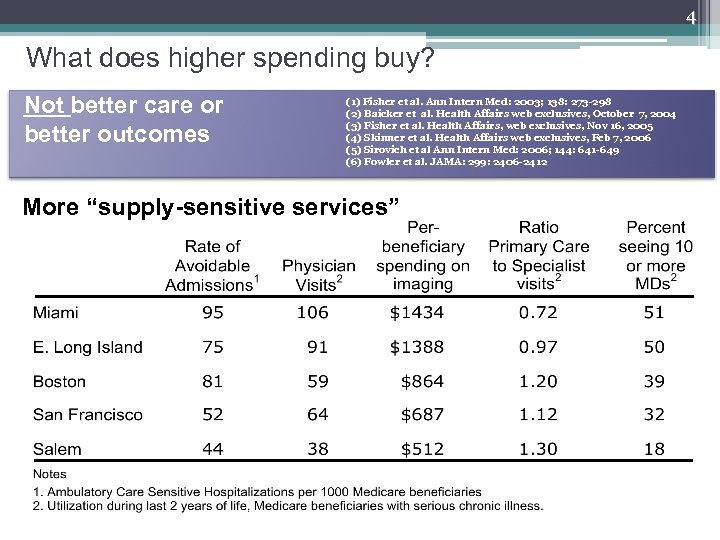 4 What does higher spending buy? Not better care or better outcomes (1) Fisher et al. Ann Intern Med: 2003; 138: 273 -298 (2) Baicker et al. Health Affairs web exclusives, October 7, 2004 (3) Fisher et al. Health Affairs, web exclusives, Nov 16, 2005 (4) Skinner et al. Health Affairs web exclusives, Feb 7, 2006 (5) Sirovich et al Ann Intern Med: 2006; 144: 641 -649 (6) Fowler et al. JAMA: 299: 2406 -2412 More “supply-sensitive services”
4 What does higher spending buy? Not better care or better outcomes (1) Fisher et al. Ann Intern Med: 2003; 138: 273 -298 (2) Baicker et al. Health Affairs web exclusives, October 7, 2004 (3) Fisher et al. Health Affairs, web exclusives, Nov 16, 2005 (4) Skinner et al. Health Affairs web exclusives, Feb 7, 2006 (5) Sirovich et al Ann Intern Med: 2006; 144: 641 -649 (6) Fowler et al. JAMA: 299: 2406 -2412 More “supply-sensitive services”
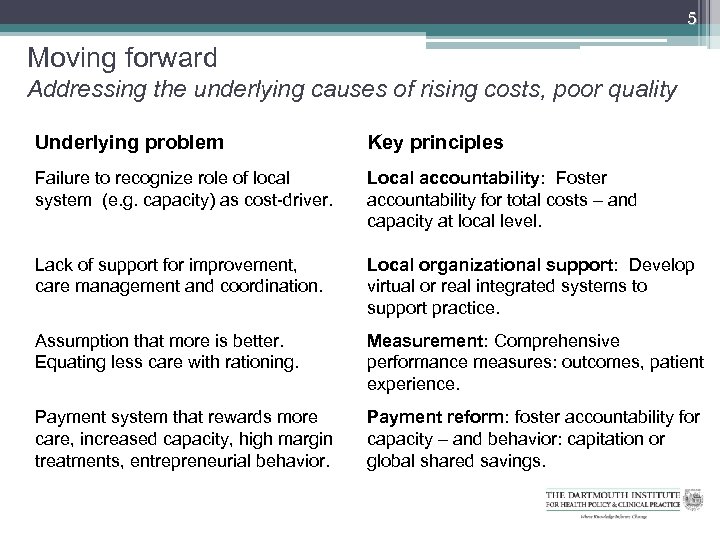 5 Moving forward Addressing the underlying causes of rising costs, poor quality Underlying problem Key principles Failure to recognize role of local system (e. g. capacity) as cost-driver. Local accountability: Foster accountability for total costs – and capacity at local level. Lack of support for improvement, care management and coordination. Local organizational support: Develop virtual or real integrated systems to support practice. Assumption that more is better. Equating less care with rationing. Measurement: Comprehensive performance measures: outcomes, patient experience. Payment system that rewards more care, increased capacity, high margin treatments, entrepreneurial behavior. Payment reform: foster accountability for capacity – and behavior: capitation or global shared savings.
5 Moving forward Addressing the underlying causes of rising costs, poor quality Underlying problem Key principles Failure to recognize role of local system (e. g. capacity) as cost-driver. Local accountability: Foster accountability for total costs – and capacity at local level. Lack of support for improvement, care management and coordination. Local organizational support: Develop virtual or real integrated systems to support practice. Assumption that more is better. Equating less care with rationing. Measurement: Comprehensive performance measures: outcomes, patient experience. Payment system that rewards more care, increased capacity, high margin treatments, entrepreneurial behavior. Payment reform: foster accountability for capacity – and behavior: capitation or global shared savings.
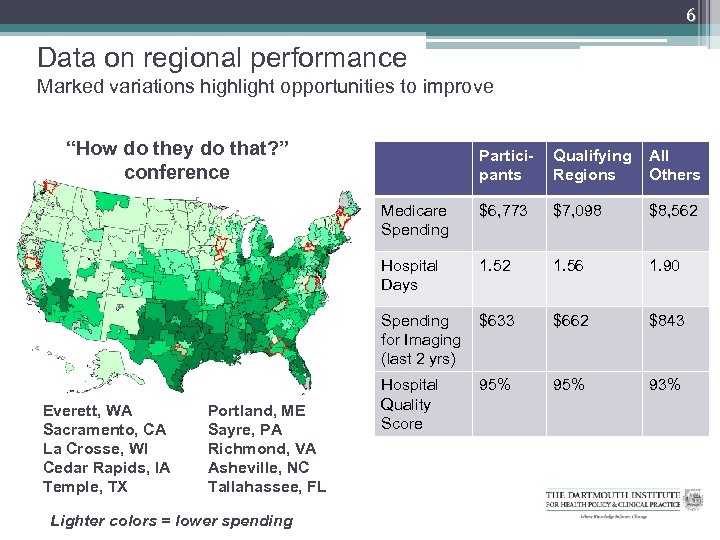 6 Data on regional performance Marked variations highlight opportunities to improve “How do they do that? ” conference $6, 773 $7, 098 $8, 562 1. 56 1. 90 Spending for Imaging (last 2 yrs) Lighter colors = lower spending All Others Hospital Days Portland, ME Sayre, PA Richmond, VA Asheville, NC Tallahassee, FL Qualifying Regions Medicare Spending Everett, WA Sacramento, CA La Crosse, WI Cedar Rapids, IA Temple, TX Participants $633 $662 $843 Hospital Quality Score 95% 93%
6 Data on regional performance Marked variations highlight opportunities to improve “How do they do that? ” conference $6, 773 $7, 098 $8, 562 1. 56 1. 90 Spending for Imaging (last 2 yrs) Lighter colors = lower spending All Others Hospital Days Portland, ME Sayre, PA Richmond, VA Asheville, NC Tallahassee, FL Qualifying Regions Medicare Spending Everett, WA Sacramento, CA La Crosse, WI Cedar Rapids, IA Temple, TX Participants $633 $662 $843 Hospital Quality Score 95% 93%
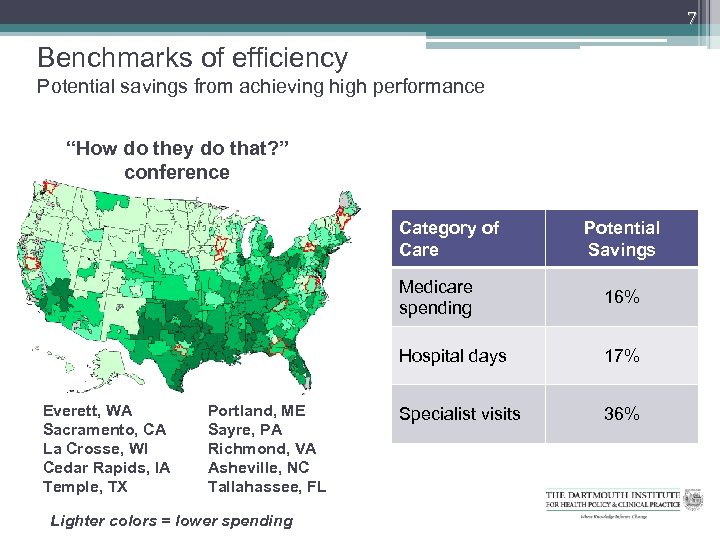 7 Benchmarks of efficiency Potential savings from achieving high performance “How do they do that? ” conference Category of Care Potential Savings Medicare spending Hospital days Everett, WA Sacramento, CA La Crosse, WI Cedar Rapids, IA Temple, TX Portland, ME Sayre, PA Richmond, VA Asheville, NC Tallahassee, FL Lighter colors = lower spending 16% 17% Specialist visits 36%
7 Benchmarks of efficiency Potential savings from achieving high performance “How do they do that? ” conference Category of Care Potential Savings Medicare spending Hospital days Everett, WA Sacramento, CA La Crosse, WI Cedar Rapids, IA Temple, TX Portland, ME Sayre, PA Richmond, VA Asheville, NC Tallahassee, FL Lighter colors = lower spending 16% 17% Specialist visits 36%
 How do they do that? Some preliminary insights Common elements across regions Shared aims; “accountable” to the community; Physician engagement as leaders; support for professional values Strong primary care foundation Use of data to support work; professional feedback; peer review Data feedback – a critical component Organizational accountability – integrated systems to support feedback Data itself – actual performance of providers
How do they do that? Some preliminary insights Common elements across regions Shared aims; “accountable” to the community; Physician engagement as leaders; support for professional values Strong primary care foundation Use of data to support work; professional feedback; peer review Data feedback – a critical component Organizational accountability – integrated systems to support feedback Data itself – actual performance of providers
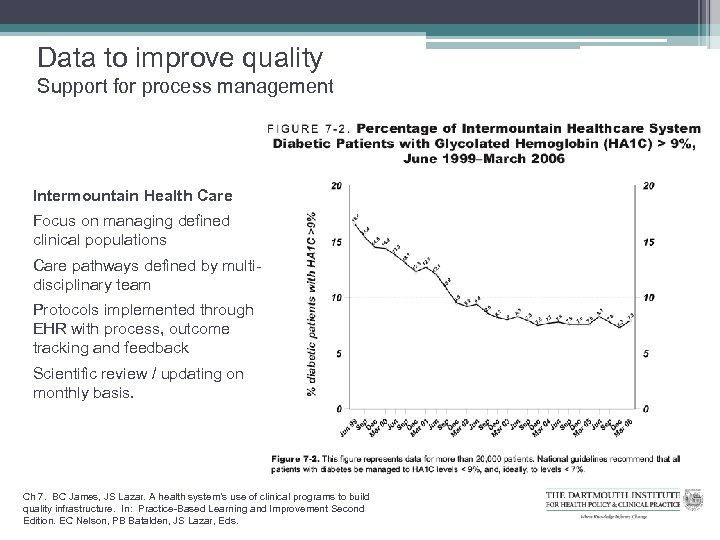 Data to improve quality Support for process management Intermountain Health Care Focus on managing defined clinical populations Care pathways defined by multidisciplinary team Protocols implemented through EHR with process, outcome tracking and feedback Scientific review / updating on monthly basis. Ch 7. BC James, JS Lazar. A health system’s use of clinical programs to build quality infrastructure. In: Practice-Based Learning and Improvement Second Edition. EC Nelson, PB Batalden, JS Lazar, Eds.
Data to improve quality Support for process management Intermountain Health Care Focus on managing defined clinical populations Care pathways defined by multidisciplinary team Protocols implemented through EHR with process, outcome tracking and feedback Scientific review / updating on monthly basis. Ch 7. BC James, JS Lazar. A health system’s use of clinical programs to build quality infrastructure. In: Practice-Based Learning and Improvement Second Edition. EC Nelson, PB Batalden, JS Lazar, Eds.
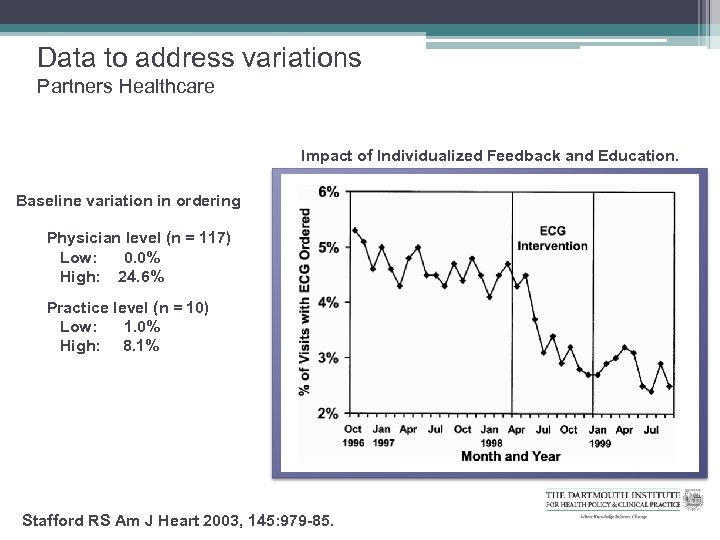 Data to address variations Partners Healthcare Impact of Individualized Feedback and Education. Baseline variation in ordering Physician level (n = 117) Low: 0. 0% High: 24. 6% Practice level (n = 10) Low: 1. 0% High: 8. 1% Stafford RS Am J Heart 2003, 145: 979 -85.
Data to address variations Partners Healthcare Impact of Individualized Feedback and Education. Baseline variation in ordering Physician level (n = 117) Low: 0. 0% High: 24. 6% Practice level (n = 10) Low: 1. 0% High: 8. 1% Stafford RS Am J Heart 2003, 145: 979 -85.
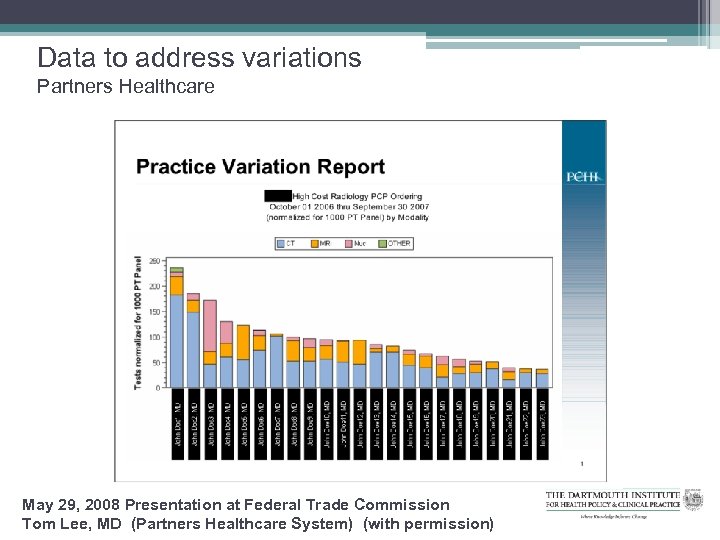 Data to address variations Partners Healthcare May 29, 2008 Presentation at Federal Trade Commission Tom Lee, MD (Partners Healthcare System) (with permission)
Data to address variations Partners Healthcare May 29, 2008 Presentation at Federal Trade Commission Tom Lee, MD (Partners Healthcare System) (with permission)
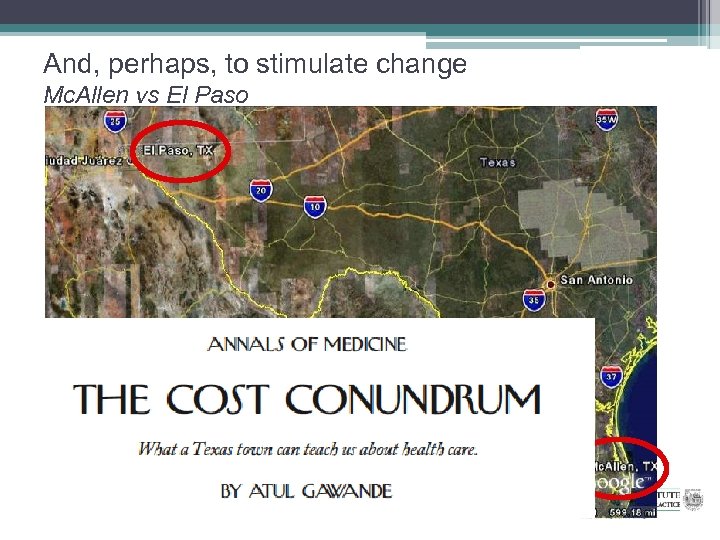 And, perhaps, to stimulate change Mc. Allen vs El Paso
And, perhaps, to stimulate change Mc. Allen vs El Paso


