 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Diseases Influenza Mono Viral Hepatitis Human Immunodeficiency Virus Rabies Scrapie Creutzfeldt-Jakob (CJD) Chronic wasting disease (CWD) Bovine spongiform encephalopathy (BSE) Tuberculosis (TB) Chicken pox & Shingles Ebola
1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Diseases Influenza Mono Viral Hepatitis Human Immunodeficiency Virus Rabies Scrapie Creutzfeldt-Jakob (CJD) Chronic wasting disease (CWD) Bovine spongiform encephalopathy (BSE) Tuberculosis (TB) Chicken pox & Shingles Ebola
 Pathogens Disease causing agents that have the ability to make you sick or even cause death They are found in the air and food and on nearly every object or person who you come in contact with
Pathogens Disease causing agents that have the ability to make you sick or even cause death They are found in the air and food and on nearly every object or person who you come in contact with
 Uncontrollable Risk Factors Heredity Chromosomal traits and family history Aging Vulnerability increases with age Environmental Conditions Unsanitary conditions, drugs, chemicals, and pollutants Organism Resistance Some pathogens are resistant to our body’s defenses and/or medical treatments
Uncontrollable Risk Factors Heredity Chromosomal traits and family history Aging Vulnerability increases with age Environmental Conditions Unsanitary conditions, drugs, chemicals, and pollutants Organism Resistance Some pathogens are resistant to our body’s defenses and/or medical treatments
 Controllable Risk Factors Stress Nutrition Physical fitness level Sleep Drug use Hygiene High-risk behaviors
Controllable Risk Factors Stress Nutrition Physical fitness level Sleep Drug use Hygiene High-risk behaviors
 Routes of Pathogen Transmission Direct Contact Touching, kissing, sexual relations Indirect Contact Touching an object that an infected person has had contact with Airborne Contact Breathing in air that carries a pathogen Food-borne infection Eating something that is contaminated by microorganisms
Routes of Pathogen Transmission Direct Contact Touching, kissing, sexual relations Indirect Contact Touching an object that an infected person has had contact with Airborne Contact Breathing in air that carries a pathogen Food-borne infection Eating something that is contaminated by microorganisms
 Routes of Pathogen Transmission Animal-borne pathogens Animals can spread diseases through bites, feces, or by carrying infected insects into living areas Water-borne diseases Transmitted from drinking water, from foods washed or sprayed with contaminated water, or from wading or swimming in contaminated streams, lakes or reservoirs Perinatally Mothers can transmit diseases to an infant in the womb or as the baby passes through the vagina during birth
Routes of Pathogen Transmission Animal-borne pathogens Animals can spread diseases through bites, feces, or by carrying infected insects into living areas Water-borne diseases Transmitted from drinking water, from foods washed or sprayed with contaminated water, or from wading or swimming in contaminated streams, lakes or reservoirs Perinatally Mothers can transmit diseases to an infant in the womb or as the baby passes through the vagina during birth
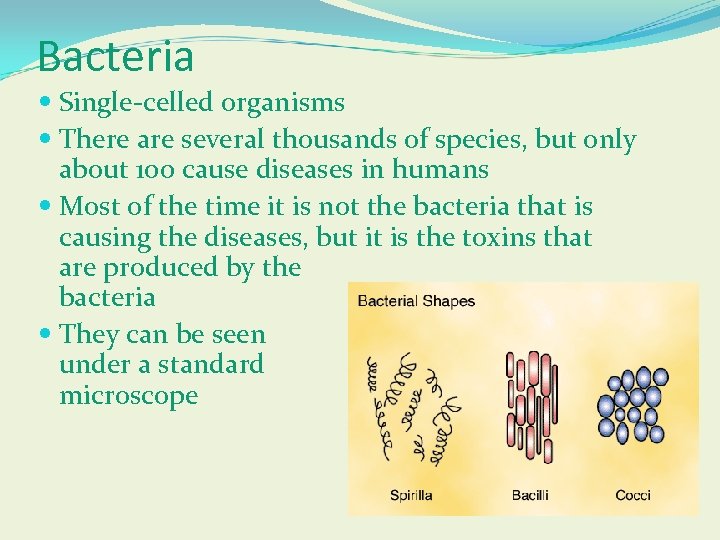 Bacteria Single-celled organisms There are several thousands of species, but only about 100 cause diseases in humans Most of the time it is not the bacteria that is causing the diseases, but it is the toxins that are produced by the bacteria They can be seen under a standard microscope
Bacteria Single-celled organisms There are several thousands of species, but only about 100 cause diseases in humans Most of the time it is not the bacteria that is causing the diseases, but it is the toxins that are produced by the bacteria They can be seen under a standard microscope
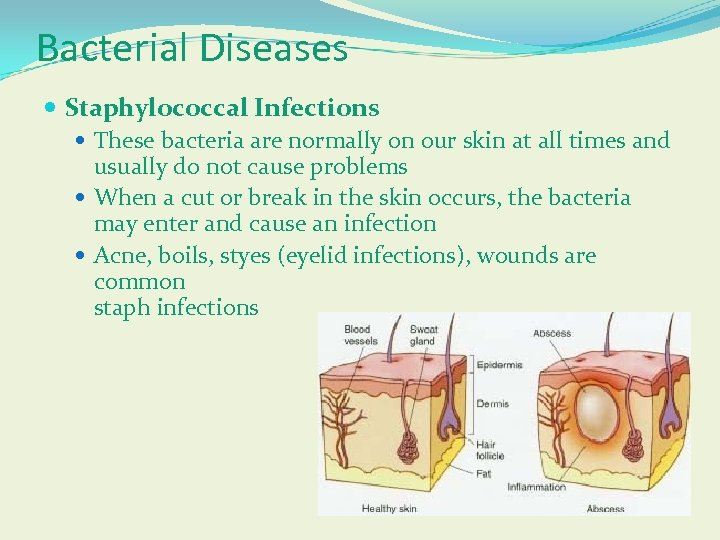 Bacterial Diseases Staphylococcal Infections These bacteria are normally on our skin at all times and usually do not cause problems When a cut or break in the skin occurs, the bacteria may enter and cause an infection Acne, boils, styes (eyelid infections), wounds are common staph infections
Bacterial Diseases Staphylococcal Infections These bacteria are normally on our skin at all times and usually do not cause problems When a cut or break in the skin occurs, the bacteria may enter and cause an infection Acne, boils, styes (eyelid infections), wounds are common staph infections
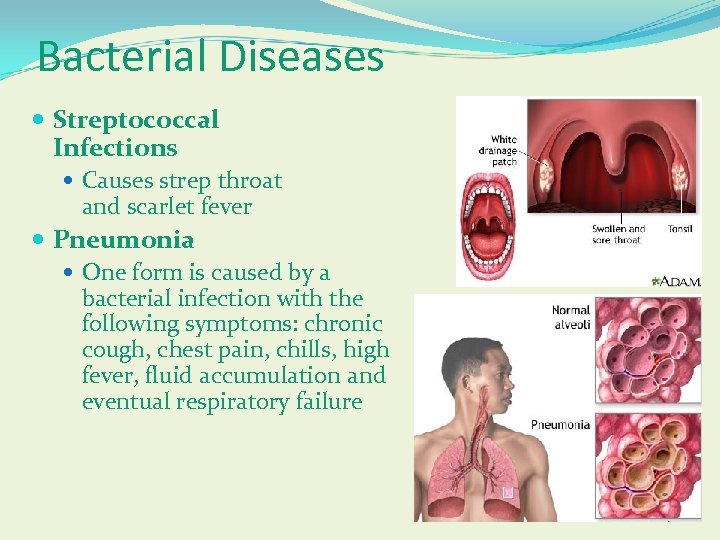 Bacterial Diseases Streptococcal Infections Causes strep throat and scarlet fever Pneumonia One form is caused by a bacterial infection with the following symptoms: chronic cough, chest pain, chills, high fever, fluid accumulation and eventual respiratory failure
Bacterial Diseases Streptococcal Infections Causes strep throat and scarlet fever Pneumonia One form is caused by a bacterial infection with the following symptoms: chronic cough, chest pain, chills, high fever, fluid accumulation and eventual respiratory failure
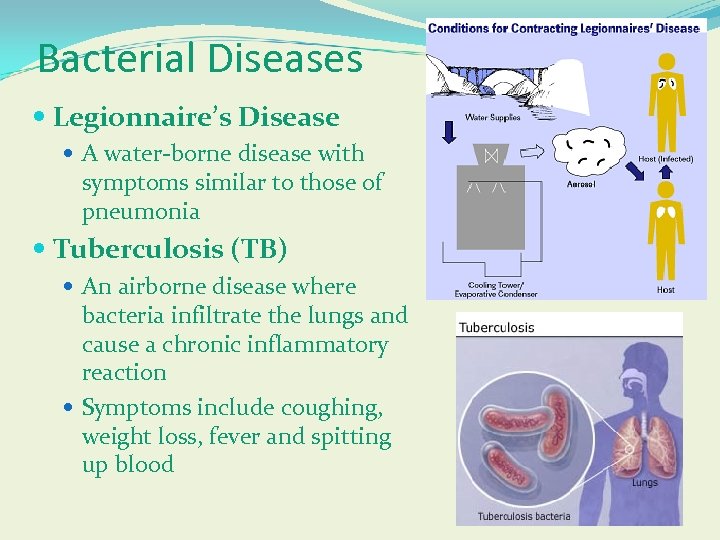 Bacterial Diseases Legionnaire’s Disease A water-borne disease with symptoms similar to those of pneumonia Tuberculosis (TB) An airborne disease where bacteria infiltrate the lungs and cause a chronic inflammatory reaction Symptoms include coughing, weight loss, fever and spitting up blood
Bacterial Diseases Legionnaire’s Disease A water-borne disease with symptoms similar to those of pneumonia Tuberculosis (TB) An airborne disease where bacteria infiltrate the lungs and cause a chronic inflammatory reaction Symptoms include coughing, weight loss, fever and spitting up blood
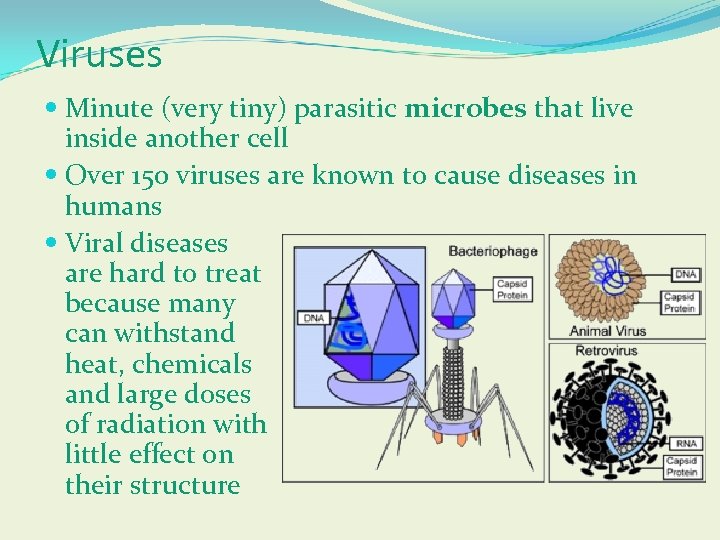 Viruses Minute (very tiny) parasitic microbes that live inside another cell Over 150 viruses are known to cause diseases in humans Viral diseases are hard to treat because many can withstand heat, chemicals and large doses of radiation with little effect on their structure
Viruses Minute (very tiny) parasitic microbes that live inside another cell Over 150 viruses are known to cause diseases in humans Viral diseases are hard to treat because many can withstand heat, chemicals and large doses of radiation with little effect on their structure
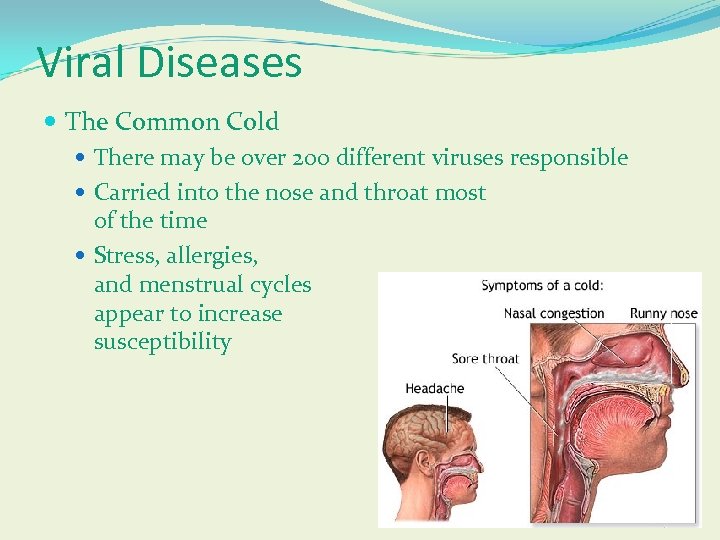 Viral Diseases The Common Cold There may be over 200 different viruses responsible Carried into the nose and throat most of the time Stress, allergies, and menstrual cycles appear to increase susceptibility
Viral Diseases The Common Cold There may be over 200 different viruses responsible Carried into the nose and throat most of the time Stress, allergies, and menstrual cycles appear to increase susceptibility
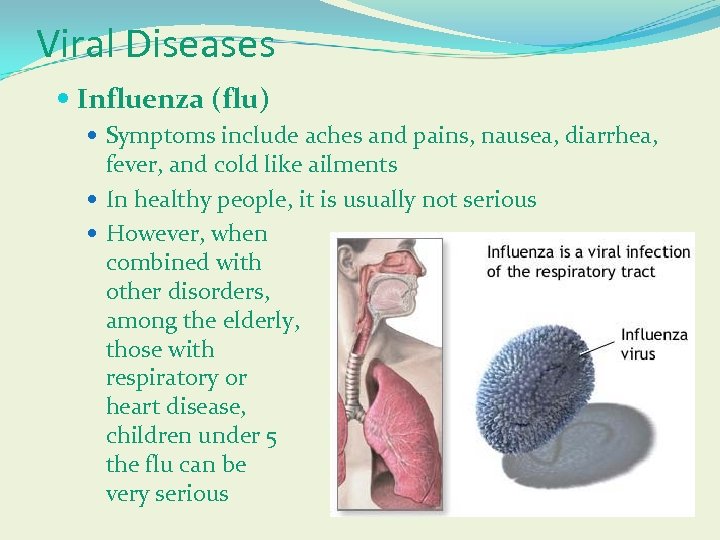 Viral Diseases Influenza (flu) Symptoms include aches and pains, nausea, diarrhea, fever, and cold like ailments In healthy people, it is usually not serious However, when combined with other disorders, among the elderly, those with respiratory or heart disease, children under 5 the flu can be very serious
Viral Diseases Influenza (flu) Symptoms include aches and pains, nausea, diarrhea, fever, and cold like ailments In healthy people, it is usually not serious However, when combined with other disorders, among the elderly, those with respiratory or heart disease, children under 5 the flu can be very serious
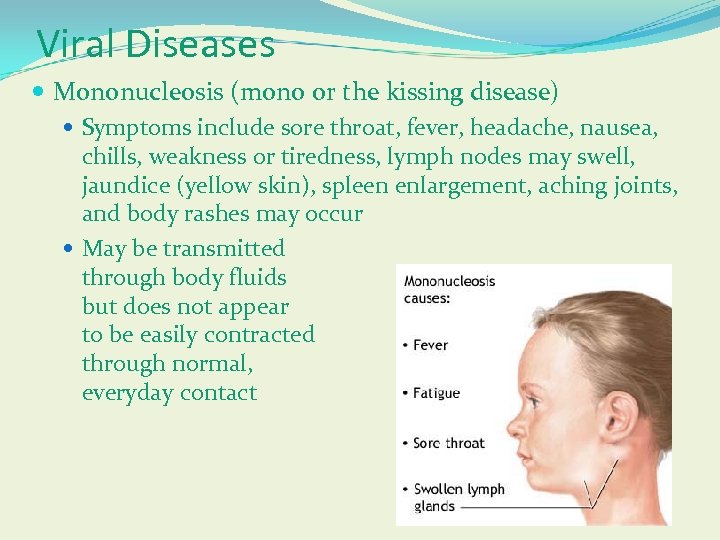 Viral Diseases Mononucleosis (mono or the kissing disease) Symptoms include sore throat, fever, headache, nausea, chills, weakness or tiredness, lymph nodes may swell, jaundice (yellow skin), spleen enlargement, aching joints, and body rashes may occur May be transmitted through body fluids but does not appear to be easily contracted through normal, everyday contact
Viral Diseases Mononucleosis (mono or the kissing disease) Symptoms include sore throat, fever, headache, nausea, chills, weakness or tiredness, lymph nodes may swell, jaundice (yellow skin), spleen enlargement, aching joints, and body rashes may occur May be transmitted through body fluids but does not appear to be easily contracted through normal, everyday contact
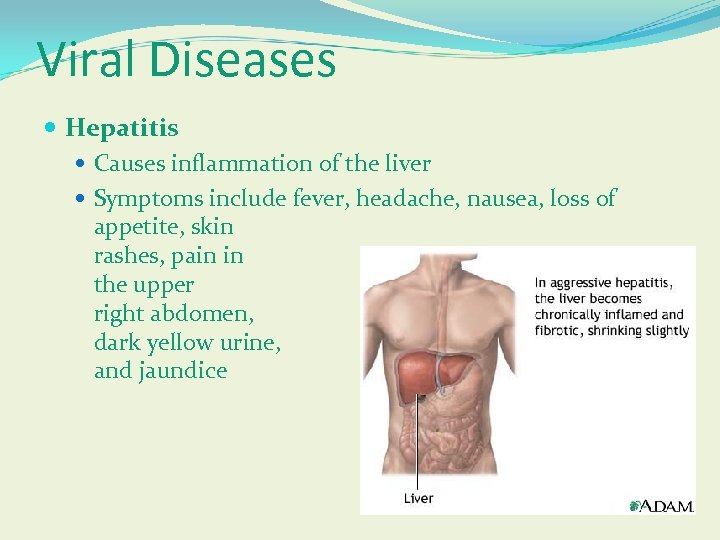 Viral Diseases Hepatitis Causes inflammation of the liver Symptoms include fever, headache, nausea, loss of appetite, skin rashes, pain in the upper right abdomen, dark yellow urine, and jaundice
Viral Diseases Hepatitis Causes inflammation of the liver Symptoms include fever, headache, nausea, loss of appetite, skin rashes, pain in the upper right abdomen, dark yellow urine, and jaundice
 Viral Diseases Hepatitis A (HAV) Contracted from eating food or drinking water contaminated with human feces Hepatitis B (HBV) Spread through body fluids, usually during unprotected sex Can lead to liver disease or liver cancer Hepatitis C (HBC) Some cases can be traced from people who share needles, blood transfusions or organ transplants Usually causes chronic infections and if not treated may cause cirrhosis of the liver, liver cancer, or liver failure
Viral Diseases Hepatitis A (HAV) Contracted from eating food or drinking water contaminated with human feces Hepatitis B (HBV) Spread through body fluids, usually during unprotected sex Can lead to liver disease or liver cancer Hepatitis C (HBC) Some cases can be traced from people who share needles, blood transfusions or organ transplants Usually causes chronic infections and if not treated may cause cirrhosis of the liver, liver cancer, or liver failure
 VI. A. Influenza Properties Member of the Orthomyxovirus family Enveloped RNA virus Two envelope proteins Hemagglutinin and Neuraminidase Segmented RNA 8 segments; packaged into helical nucleocapsids Antigenic variation & genetic exchange lead to the appearance of new strains; requires use of different vaccine combinations each year
VI. A. Influenza Properties Member of the Orthomyxovirus family Enveloped RNA virus Two envelope proteins Hemagglutinin and Neuraminidase Segmented RNA 8 segments; packaged into helical nucleocapsids Antigenic variation & genetic exchange lead to the appearance of new strains; requires use of different vaccine combinations each year
 VI. A. Influenza Symptoms & Complications of Influenza Respiratory Tract Symptoms Fever Neurological Complications: Guillain-Barré Syndrome Reye’s Syndrome
VI. A. Influenza Symptoms & Complications of Influenza Respiratory Tract Symptoms Fever Neurological Complications: Guillain-Barré Syndrome Reye’s Syndrome
 VI. B. Diseases Caused by the Herpes Family Properties of the Herpes Virus Family Large, enveloped DNA viruses Icosahedral capsids DNA replicates in the nucleus of host cells Cells may become permanently infected Host chromosomes may be altered Herpes infections associated with certain cancers
VI. B. Diseases Caused by the Herpes Family Properties of the Herpes Virus Family Large, enveloped DNA viruses Icosahedral capsids DNA replicates in the nucleus of host cells Cells may become permanently infected Host chromosomes may be altered Herpes infections associated with certain cancers
 VI. B. Diseases Caused by the Herpes Family Herpes Simplex Two major strains Type I: Oral Herpes Type II: Genital Herpes Skin lesions form at site of the infection Virus travels along sensory neurons to ganglia, where it remains During times of stress or weakened immunity, virus may travel along same neurons to re-infect the initial skin sites
VI. B. Diseases Caused by the Herpes Family Herpes Simplex Two major strains Type I: Oral Herpes Type II: Genital Herpes Skin lesions form at site of the infection Virus travels along sensory neurons to ganglia, where it remains During times of stress or weakened immunity, virus may travel along same neurons to re-infect the initial skin sites
 VI. B. Diseases Caused by the Herpes Family Chicken pox & Shingles Cause: Varicella-zoster virus Chicken pox symptoms Shingles symptoms Treatment Chicken pox vaccine Connection to Reye’s syndrome
VI. B. Diseases Caused by the Herpes Family Chicken pox & Shingles Cause: Varicella-zoster virus Chicken pox symptoms Shingles symptoms Treatment Chicken pox vaccine Connection to Reye’s syndrome
 VI. D. Human Immunodeficiency Virus Viral Properties A retrovirus An enveloped RNA virus that replicates through a DNA intermediate The DNA intermediate is synthesized by reverse transcriptase: an enzyme that makes a DNA molecule using an RNA template The DNA intermediate is spliced into host chromosomes, making the infection permanent
VI. D. Human Immunodeficiency Virus Viral Properties A retrovirus An enveloped RNA virus that replicates through a DNA intermediate The DNA intermediate is synthesized by reverse transcriptase: an enzyme that makes a DNA molecule using an RNA template The DNA intermediate is spliced into host chromosomes, making the infection permanent
 VI. D. Human Immunodeficiency Virus Viral Properties (cont. ) Host cells for HIV: CD 4+ cells Helper T (T-4) lymphocytes Macrophages Damage to the helper T cell population cripples the immune system of the host
VI. D. Human Immunodeficiency Virus Viral Properties (cont. ) Host cells for HIV: CD 4+ cells Helper T (T-4) lymphocytes Macrophages Damage to the helper T cell population cripples the immune system of the host
 VI. D. Human Immunodeficiency Virus Transmission Contact with infected body fluids Blood, blood products, semen, vaginal secretions, breast milk
VI. D. Human Immunodeficiency Virus Transmission Contact with infected body fluids Blood, blood products, semen, vaginal secretions, breast milk
 VI. D. Human Immunodeficiency Virus What is the difference between HIV & AIDS? HIV: the Human Immunodeficiency Virus The cause of AIDS Also known as: HTLV-III and LAV Two known types: HIV-1 and HIV-2 AIDS: Acquired Immune Deficiency Syndrome Catastrophic immune system failure caused by HIV infection Symptoms & cases are usually defined by the CDC case surveillance definition
VI. D. Human Immunodeficiency Virus What is the difference between HIV & AIDS? HIV: the Human Immunodeficiency Virus The cause of AIDS Also known as: HTLV-III and LAV Two known types: HIV-1 and HIV-2 AIDS: Acquired Immune Deficiency Syndrome Catastrophic immune system failure caused by HIV infection Symptoms & cases are usually defined by the CDC case surveillance definition
 VI. D. Human Immunodeficiency Virus CDC Case Surveillance Definition for AIDS Based on: Clinical Symptoms: Categories A, B, C Helper T-4 lymphocyte count: Categories 1, 2, 3 Category A Asymptomatic HIV infection Persistent Generalized L ymphadenopathy Acute HIV infection
VI. D. Human Immunodeficiency Virus CDC Case Surveillance Definition for AIDS Based on: Clinical Symptoms: Categories A, B, C Helper T-4 lymphocyte count: Categories 1, 2, 3 Category A Asymptomatic HIV infection Persistent Generalized L ymphadenopathy Acute HIV infection
 VI. D. Human Immunodeficiency Virus CDC Case Surveillance Definition for AIDS (cont. ) Category B Symptomatic HIV infection with constitutive illness & certain opportunistic infections Often an early indication that AIDS is developing *Category C Symptomatic HIV infection with opportunistic infections listed in the CDC surveillance case definition
VI. D. Human Immunodeficiency Virus CDC Case Surveillance Definition for AIDS (cont. ) Category B Symptomatic HIV infection with constitutive illness & certain opportunistic infections Often an early indication that AIDS is developing *Category C Symptomatic HIV infection with opportunistic infections listed in the CDC surveillance case definition
 VI. D. Human Immunodeficiency Virus CDC Case Surveillance Definition for AIDS (cont. ) Category 1 T-4 count greater than 400 per microliter of blood Category 2 T-4 count between 400 and 200 per microliter of blood *Category 3 T-4 count less than 200 per microliter of blood
VI. D. Human Immunodeficiency Virus CDC Case Surveillance Definition for AIDS (cont. ) Category 1 T-4 count greater than 400 per microliter of blood Category 2 T-4 count between 400 and 200 per microliter of blood *Category 3 T-4 count less than 200 per microliter of blood
 VI. D. Human Immunodeficiency Virus CDC Case Surveillance Definition for AIDS (cont. ) *These categories (C and 3) meet the CDC surveillance definition to be included among the AIDS cases Many HIV-infected individuals show no symptoms, yet are capable of transmitting the virus
VI. D. Human Immunodeficiency Virus CDC Case Surveillance Definition for AIDS (cont. ) *These categories (C and 3) meet the CDC surveillance definition to be included among the AIDS cases Many HIV-infected individuals show no symptoms, yet are capable of transmitting the virus
 VI. D. Human Immunodeficiency Virus Symptoms & Secondary Infections Associated with AIDS Acute Infection Fever, lymph node swelling, aches, fatigue, “flu-like” or “mono-like” symptoms Persistent Generalized Lymphadenopathy Lymph node swelling for greater than 6 months in two or more body areas (excluding the groin) Often an early manifestation that AIDS has developed
VI. D. Human Immunodeficiency Virus Symptoms & Secondary Infections Associated with AIDS Acute Infection Fever, lymph node swelling, aches, fatigue, “flu-like” or “mono-like” symptoms Persistent Generalized Lymphadenopathy Lymph node swelling for greater than 6 months in two or more body areas (excluding the groin) Often an early manifestation that AIDS has developed
 VI. D. Human Immunodeficiency Virus Symptoms & Secondary Infections Associated with AIDS (cont. ) Constitutive Illness Weight loss, persistent fever, diarrhea Cancers Kaposi’s sarcoma Certain lymphomas
VI. D. Human Immunodeficiency Virus Symptoms & Secondary Infections Associated with AIDS (cont. ) Constitutive Illness Weight loss, persistent fever, diarrhea Cancers Kaposi’s sarcoma Certain lymphomas
 VI. D. Human Immunodeficiency Virus Symptoms & Secondary Infections Associated with AIDS (cont. ) Bacterial Secondary Infections Mycobacterium Listeria Salmonella Mycoplasma many others
VI. D. Human Immunodeficiency Virus Symptoms & Secondary Infections Associated with AIDS (cont. ) Bacterial Secondary Infections Mycobacterium Listeria Salmonella Mycoplasma many others
 VI. D. Human Immunodeficiency Virus Symptoms & Secondary Infections Associated with AIDS (cont. ) Fungal Secondary Infections Candida and others Protozoan Secondary Infections Toxoplasma gondii Cryptosporidium Pneumocystis carinii
VI. D. Human Immunodeficiency Virus Symptoms & Secondary Infections Associated with AIDS (cont. ) Fungal Secondary Infections Candida and others Protozoan Secondary Infections Toxoplasma gondii Cryptosporidium Pneumocystis carinii
 VI. D. Human Immunodeficiency Virus Symptoms & Secondary Infections Associated with AIDS (cont. ) Viral Secondary Infections Herpes simplex Cytomegalovirus Many others Treatments Inhibitors of DNA replication Protease Inhibitors
VI. D. Human Immunodeficiency Virus Symptoms & Secondary Infections Associated with AIDS (cont. ) Viral Secondary Infections Herpes simplex Cytomegalovirus Many others Treatments Inhibitors of DNA replication Protease Inhibitors
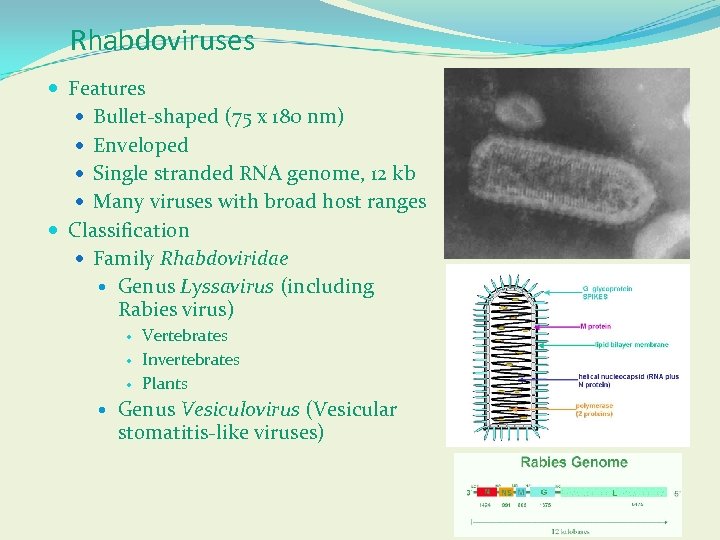 Rhabdoviruses Features Bullet-shaped (75 x 180 nm) Enveloped Single stranded RNA genome, 12 kb Many viruses with broad host ranges Classification Family Rhabdoviridae Genus Lyssavirus (including Rabies virus) Vertebrates Invertebrates Plants Genus Vesiculovirus (Vesicular stomatitis-like viruses)
Rhabdoviruses Features Bullet-shaped (75 x 180 nm) Enveloped Single stranded RNA genome, 12 kb Many viruses with broad host ranges Classification Family Rhabdoviridae Genus Lyssavirus (including Rabies virus) Vertebrates Invertebrates Plants Genus Vesiculovirus (Vesicular stomatitis-like viruses)
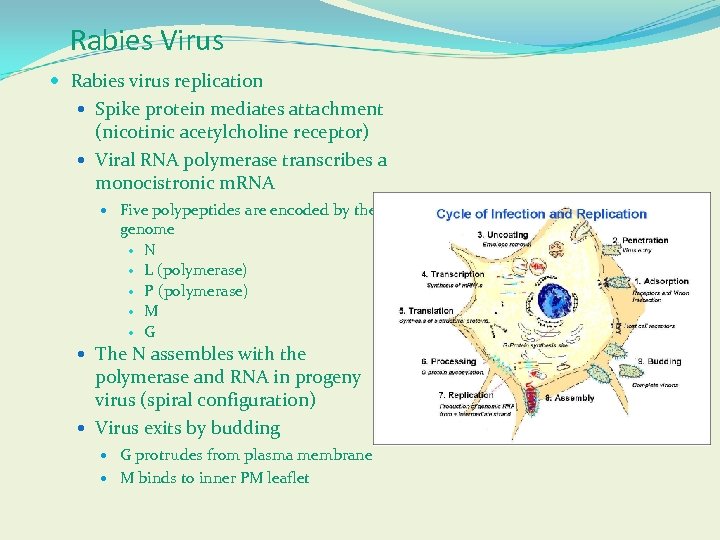 Rabies Virus Rabies virus replication Spike protein mediates attachment (nicotinic acetylcholine receptor) Viral RNA polymerase transcribes a monocistronic m. RNA Five polypeptides are encoded by the genome N L (polymerase) P (polymerase) M G The N assembles with the polymerase and RNA in progeny virus (spiral configuration) Virus exits by budding G protrudes from plasma membrane M binds to inner PM leaflet
Rabies Virus Rabies virus replication Spike protein mediates attachment (nicotinic acetylcholine receptor) Viral RNA polymerase transcribes a monocistronic m. RNA Five polypeptides are encoded by the genome N L (polymerase) P (polymerase) M G The N assembles with the polymerase and RNA in progeny virus (spiral configuration) Virus exits by budding G protrudes from plasma membrane M binds to inner PM leaflet
 Rabies Virus Animal susceptibility All warm-blooded animals can be infected with varying susceptibility High - wolves, coyotes, foxes, dogs Intermediate - skunks, raccoons, bats Low - opossums Virus occurs in saliva, nervous system, urine, lymph, milk Recovery is rare and only occurs in bats; fatal in nearly all others Vampire bats can transmit virus for months
Rabies Virus Animal susceptibility All warm-blooded animals can be infected with varying susceptibility High - wolves, coyotes, foxes, dogs Intermediate - skunks, raccoons, bats Low - opossums Virus occurs in saliva, nervous system, urine, lymph, milk Recovery is rare and only occurs in bats; fatal in nearly all others Vampire bats can transmit virus for months
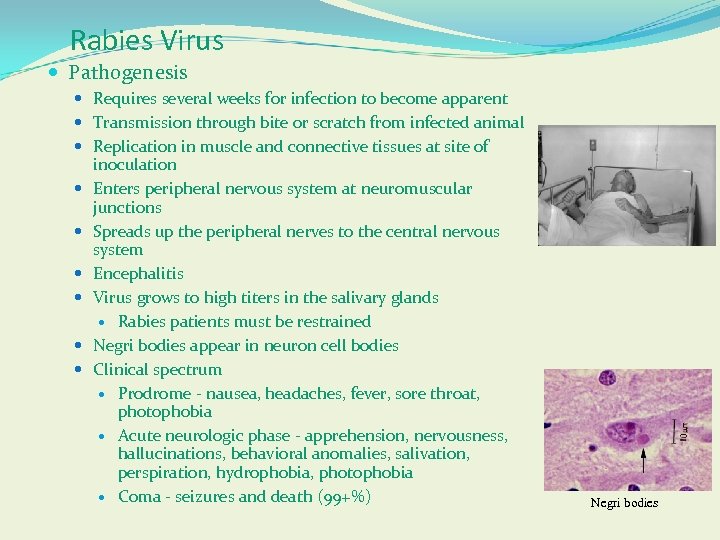 Rabies Virus Pathogenesis Requires several weeks for infection to become apparent Transmission through bite or scratch from infected animal Replication in muscle and connective tissues at site of inoculation Enters peripheral nervous system at neuromuscular junctions Spreads up the peripheral nerves to the central nervous system Encephalitis Virus grows to high titers in the salivary glands Rabies patients must be restrained Negri bodies appear in neuron cell bodies Clinical spectrum Prodrome - nausea, headaches, fever, sore throat, photophobia Acute neurologic phase - apprehension, nervousness, hallucinations, behavioral anomalies, salivation, perspiration, hydrophobia, photophobia Coma - seizures and death (99+%) Negri bodies
Rabies Virus Pathogenesis Requires several weeks for infection to become apparent Transmission through bite or scratch from infected animal Replication in muscle and connective tissues at site of inoculation Enters peripheral nervous system at neuromuscular junctions Spreads up the peripheral nerves to the central nervous system Encephalitis Virus grows to high titers in the salivary glands Rabies patients must be restrained Negri bodies appear in neuron cell bodies Clinical spectrum Prodrome - nausea, headaches, fever, sore throat, photophobia Acute neurologic phase - apprehension, nervousness, hallucinations, behavioral anomalies, salivation, perspiration, hydrophobia, photophobia Coma - seizures and death (99+%) Negri bodies
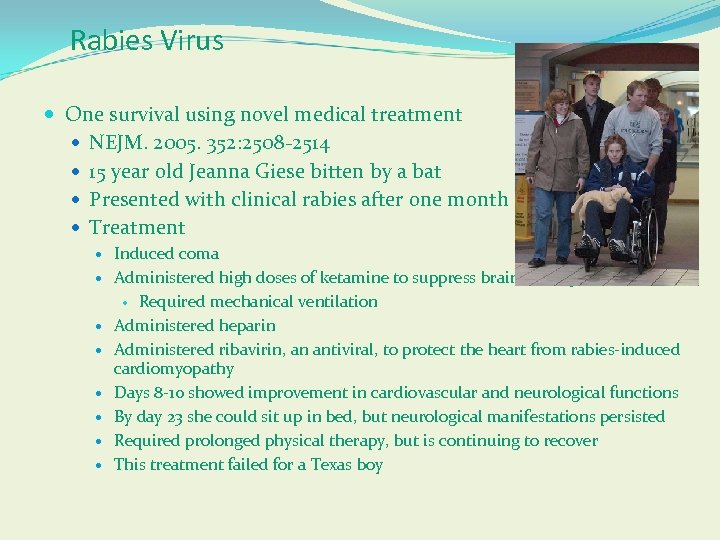 Rabies Virus One survival using novel medical treatment NEJM. 2005. 352: 2508 -2514 15 year old Jeanna Giese bitten by a bat Presented with clinical rabies after one month Treatment Induced coma Administered high doses of ketamine to suppress brain activity Required mechanical ventilation Administered heparin Administered ribavirin, an antiviral, to protect the heart from rabies-induced cardiomyopathy Days 8 -10 showed improvement in cardiovascular and neurological functions By day 23 she could sit up in bed, but neurological manifestations persisted Required prolonged physical therapy, but is continuing to recover This treatment failed for a Texas boy
Rabies Virus One survival using novel medical treatment NEJM. 2005. 352: 2508 -2514 15 year old Jeanna Giese bitten by a bat Presented with clinical rabies after one month Treatment Induced coma Administered high doses of ketamine to suppress brain activity Required mechanical ventilation Administered heparin Administered ribavirin, an antiviral, to protect the heart from rabies-induced cardiomyopathy Days 8 -10 showed improvement in cardiovascular and neurological functions By day 23 she could sit up in bed, but neurological manifestations persisted Required prolonged physical therapy, but is continuing to recover This treatment failed for a Texas boy
 Rabies Virus Laboratory diagnosis PCR Serology (IFA) Animal control Rabid or suspected rabid animals are killed and examined by histopathology for Negri bodies and viral antigen Vaccination of pets is required by law in most states Immunity and protection Vaccines First one developed by Pasteur by using spinal cords from infected dogs Today’s principal vaccine is the human diploid cell vaccine (HDCV) made in the WI-38 fibroblast cell line Virus is inactivated by βPL Post-exposure prophylaxis One dose of hyperimmune antiserum Five immunizations over 28 days
Rabies Virus Laboratory diagnosis PCR Serology (IFA) Animal control Rabid or suspected rabid animals are killed and examined by histopathology for Negri bodies and viral antigen Vaccination of pets is required by law in most states Immunity and protection Vaccines First one developed by Pasteur by using spinal cords from infected dogs Today’s principal vaccine is the human diploid cell vaccine (HDCV) made in the WI-38 fibroblast cell line Virus is inactivated by βPL Post-exposure prophylaxis One dose of hyperimmune antiserum Five immunizations over 28 days
 Rabies Virus Epidemiology Enzootic in wild and domesticated animals In the U. S. , edible vaccines are dispersed to control wild animal rabies More than 200 people die from rabies in China each month Reservoirs might be bats But the slow-growing nature of rabies virus also contributes to its persistence in nature
Rabies Virus Epidemiology Enzootic in wild and domesticated animals In the U. S. , edible vaccines are dispersed to control wild animal rabies More than 200 people die from rabies in China each month Reservoirs might be bats But the slow-growing nature of rabies virus also contributes to its persistence in nature
 Prion Diseases Proteinacious infectious agents Diseases are transmissible spongiform encephalopathies (TSEs) There also inherited spongiform encephalopathies Human Creutzfeldt-Jakob Disease - sporatic New Variant CJD - from beef (“mad cow disease”) Kuru - ritualistic cannibalism (consuming brains of infected dead) Fatal familial insomnia Animal Bovine spongiform encephalopathy (“mad cow” disease) Scrapie - sheep Chronic wasting disease - deer, elk, moose
Prion Diseases Proteinacious infectious agents Diseases are transmissible spongiform encephalopathies (TSEs) There also inherited spongiform encephalopathies Human Creutzfeldt-Jakob Disease - sporatic New Variant CJD - from beef (“mad cow disease”) Kuru - ritualistic cannibalism (consuming brains of infected dead) Fatal familial insomnia Animal Bovine spongiform encephalopathy (“mad cow” disease) Scrapie - sheep Chronic wasting disease - deer, elk, moose
 Transmissible Spongiform Encephalopathy Prion Diseases
Transmissible Spongiform Encephalopathy Prion Diseases
 TSEs Group of diseases caused by same infectious agent Causes same pathology in respective hosts Microscopic sponge like holes in brain Clinical signs are all neurological in nature Center for Food Security and Public Health Iowa State University - 2004
TSEs Group of diseases caused by same infectious agent Causes same pathology in respective hosts Microscopic sponge like holes in brain Clinical signs are all neurological in nature Center for Food Security and Public Health Iowa State University - 2004
 Human TSE’s Kuru Creutzfeldt-Jakob disease (CJD) Familial, sporadic, iatrogenic A variant of CJD (v. CJD) Gerstmann-Straussler-Scheinker syndrome (GSS) Fatal familial insomnia (FFI) Center for Food Security and Public Health Iowa State University - 2004
Human TSE’s Kuru Creutzfeldt-Jakob disease (CJD) Familial, sporadic, iatrogenic A variant of CJD (v. CJD) Gerstmann-Straussler-Scheinker syndrome (GSS) Fatal familial insomnia (FFI) Center for Food Security and Public Health Iowa State University - 2004
 Animal TSE’s Bovine Spongiform Encephalopathy (BSE, “mad cow disease”) Scrapie (sheep) Chronic wasting disease (CWD) (elk and deer) Mink Spongiform Encephalopathy (TME) Feline Spongiform Encephalopathy (FSE) Center for Food Security and Public Health Iowa State University - 2004
Animal TSE’s Bovine Spongiform Encephalopathy (BSE, “mad cow disease”) Scrapie (sheep) Chronic wasting disease (CWD) (elk and deer) Mink Spongiform Encephalopathy (TME) Feline Spongiform Encephalopathy (FSE) Center for Food Security and Public Health Iowa State University - 2004
 The Organism
The Organism
 Prion Smaller than smallest known virus Not yet completely characterized Most widely accepted theory Prion = Proteinaceous infectious particle Normal Protein Pr. PC (C for cellular) Glycoprotein normally found at cell surface inserted in plasma membrane Center for Food Security and Public Health Iowa State University - 2004
Prion Smaller than smallest known virus Not yet completely characterized Most widely accepted theory Prion = Proteinaceous infectious particle Normal Protein Pr. PC (C for cellular) Glycoprotein normally found at cell surface inserted in plasma membrane Center for Food Security and Public Health Iowa State University - 2004
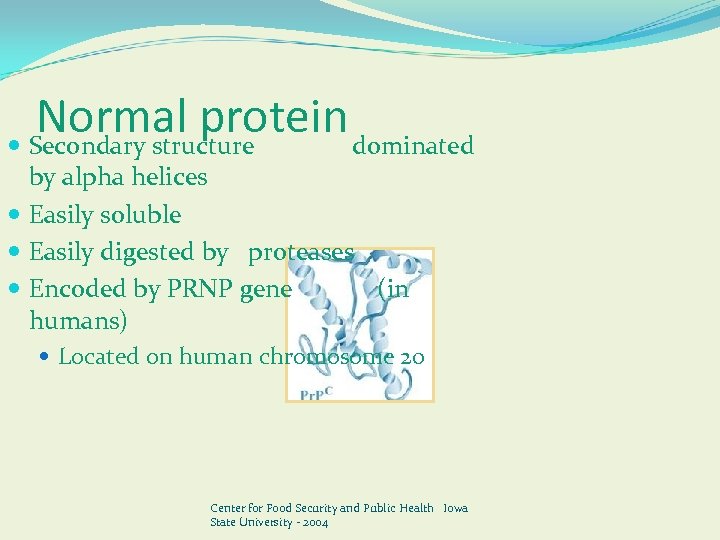 Normal protein Secondary structure dominated by alpha helices Easily soluble Easily digested by proteases Encoded by PRNP gene (in humans) Located on human chromosome 20 Center for Food Security and Public Health Iowa State University - 2004
Normal protein Secondary structure dominated by alpha helices Easily soluble Easily digested by proteases Encoded by PRNP gene (in humans) Located on human chromosome 20 Center for Food Security and Public Health Iowa State University - 2004
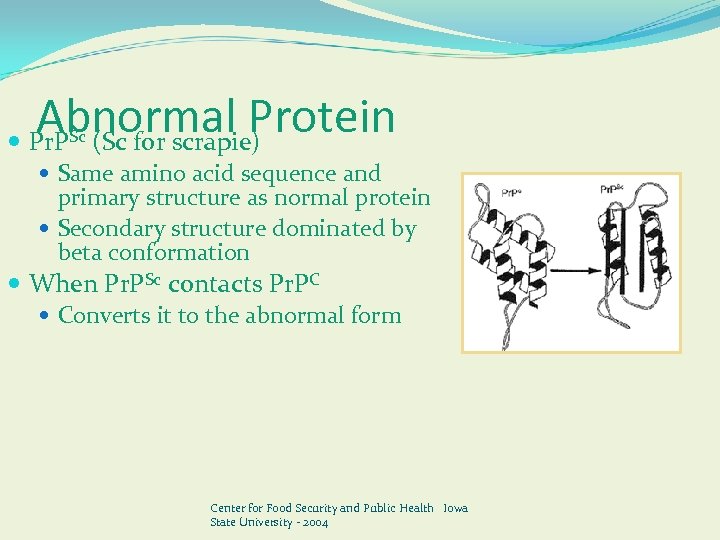 Abnormal Protein Pr. P (Sc for scrapie) Sc Same amino acid sequence and primary structure as normal protein Secondary structure dominated by beta conformation When Pr. PSc contacts Pr. PC Converts it to the abnormal form Center for Food Security and Public Health Iowa State University - 2004
Abnormal Protein Pr. P (Sc for scrapie) Sc Same amino acid sequence and primary structure as normal protein Secondary structure dominated by beta conformation When Pr. PSc contacts Pr. PC Converts it to the abnormal form Center for Food Security and Public Health Iowa State University - 2004
 Abnormal Protein Insoluble in all but strongest solvents Highly resistant to digestion by proteases Survives in tissues post-mortem Extremely resistant Heat, normal sterilization processes, sunlight No detectable immune response Center for Food Security and Public Health Iowa State University - 2004
Abnormal Protein Insoluble in all but strongest solvents Highly resistant to digestion by proteases Survives in tissues post-mortem Extremely resistant Heat, normal sterilization processes, sunlight No detectable immune response Center for Food Security and Public Health Iowa State University - 2004
 History
History
 History: Kuru New Guinea in early 1900’s People practicing cannibalism 1957 -1968 Over 1, 100 people died Majority of deaths Women, children and elderly Incubation period >30 days Center for Food Security and Public Health Iowa State University - 2004
History: Kuru New Guinea in early 1900’s People practicing cannibalism 1957 -1968 Over 1, 100 people died Majority of deaths Women, children and elderly Incubation period >30 days Center for Food Security and Public Health Iowa State University - 2004
 History: CJD Sporadic human encephalopathy Worldwide 1 -2 cases/million people Different forms Spontaneous (85%) Genetic (10 -15%) Iatrogenic (<1%) Average of onset 65 years Duration of illness, 4. 5 months Center for Food Security and Public Health Iowa State University - 2004
History: CJD Sporadic human encephalopathy Worldwide 1 -2 cases/million people Different forms Spontaneous (85%) Genetic (10 -15%) Iatrogenic (<1%) Average of onset 65 years Duration of illness, 4. 5 months Center for Food Security and Public Health Iowa State University - 2004
 History: BSE 1986, First confirmed case in United Kingdom (UK) 1988, UK bans meat and bone meal from ruminants in cattle feed 1989, USDA bans importation of ruminants from countries with BSE 1993, Peak of BSE in UK 1, 000 new cases reported weekly Center for Food Security and Public Health Iowa State University - 2004
History: BSE 1986, First confirmed case in United Kingdom (UK) 1988, UK bans meat and bone meal from ruminants in cattle feed 1989, USDA bans importation of ruminants from countries with BSE 1993, Peak of BSE in UK 1, 000 new cases reported weekly Center for Food Security and Public Health Iowa State University - 2004
 History: BSE 1997, US & Canada ban ruminant products fed back to ruminants US importation ban extended to all of Europe 2001, European Union ordered mandatory tests on cattle Older than 30 months destined for slaughter May 2003, BSE diagnosed in 6 yr. old Angus beef cow in Alberta, Canada Herd mates all tested negative Single case in 1993 was cow imported from UK Center for Food Security and Public Health Iowa State University - 2004
History: BSE 1997, US & Canada ban ruminant products fed back to ruminants US importation ban extended to all of Europe 2001, European Union ordered mandatory tests on cattle Older than 30 months destined for slaughter May 2003, BSE diagnosed in 6 yr. old Angus beef cow in Alberta, Canada Herd mates all tested negative Single case in 1993 was cow imported from UK Center for Food Security and Public Health Iowa State University - 2004
 History: BSE December 2003, BSE diagnosed in 6½ yr old Holstein cow in Washington State Possibly imported from Canada DNA testing being conducted Complications following calving Sent to slaughter Brain tissue sent to NVSL–per FSIS protocol Presumptive positive by NVSL Definitively positive by UK lab Center for Food Security and Public Health Iowa State University - 2004
History: BSE December 2003, BSE diagnosed in 6½ yr old Holstein cow in Washington State Possibly imported from Canada DNA testing being conducted Complications following calving Sent to slaughter Brain tissue sent to NVSL–per FSIS protocol Presumptive positive by NVSL Definitively positive by UK lab Center for Food Security and Public Health Iowa State University - 2004
 History: v. CJD Human encephalopathy due to consuming BSE contaminated foods 1995, UK: First confirmed case Incubation period not known Mean age at death 28 years old Mean duration of infection 14 months Center for Food Security and Public Health Iowa State University - 2004
History: v. CJD Human encephalopathy due to consuming BSE contaminated foods 1995, UK: First confirmed case Incubation period not known Mean age at death 28 years old Mean duration of infection 14 months Center for Food Security and Public Health Iowa State University - 2004
 History: Scrapie Sheep and goat disease Recognized 250 years ago Great Britain and W. Europe 1947 diagnosed in the U. S. More than 1, 000 flocks; mostly Suffolk Scrapie: Ovine Slaughter Surveillance Study (SOSS) Overall national prevalence 0. 2% Higher in black-faced sheep Center for Food Security and Public Health Iowa State University - 2004
History: Scrapie Sheep and goat disease Recognized 250 years ago Great Britain and W. Europe 1947 diagnosed in the U. S. More than 1, 000 flocks; mostly Suffolk Scrapie: Ovine Slaughter Surveillance Study (SOSS) Overall national prevalence 0. 2% Higher in black-faced sheep Center for Food Security and Public Health Iowa State University - 2004
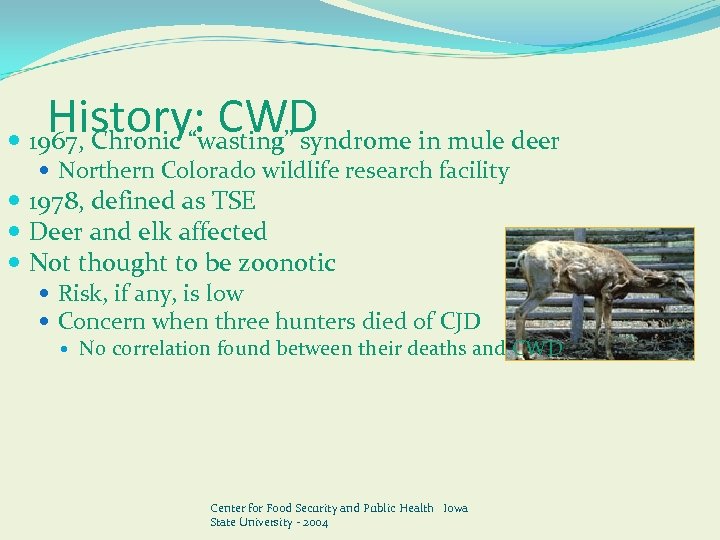 History: CWD 1967, Chronic “wasting” syndrome in mule deer Northern Colorado wildlife research facility 1978, defined as TSE Deer and elk affected Not thought to be zoonotic Risk, if any, is low Concern when three hunters died of CJD No correlation found between their deaths and CWD Center for Food Security and Public Health Iowa State University - 2004
History: CWD 1967, Chronic “wasting” syndrome in mule deer Northern Colorado wildlife research facility 1978, defined as TSE Deer and elk affected Not thought to be zoonotic Risk, if any, is low Concern when three hunters died of CJD No correlation found between their deaths and CWD Center for Food Security and Public Health Iowa State University - 2004
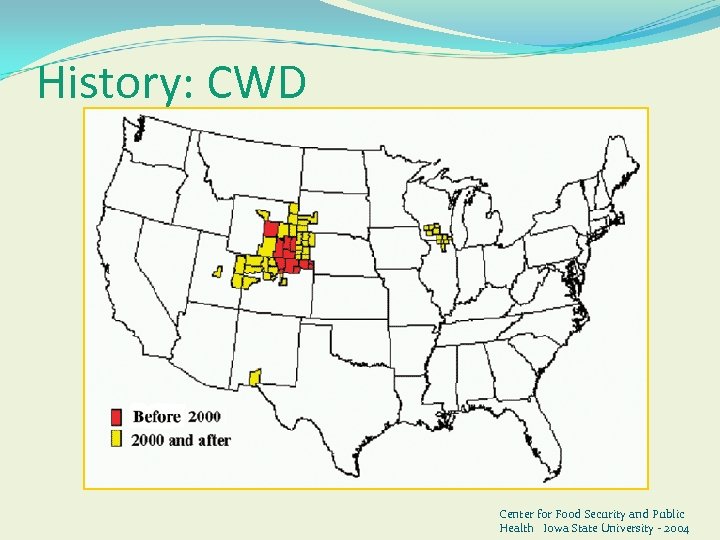 History: CWD Center for Food Security and Public Health Iowa State University - 2004
History: CWD Center for Food Security and Public Health Iowa State University - 2004
 Transmission
Transmission
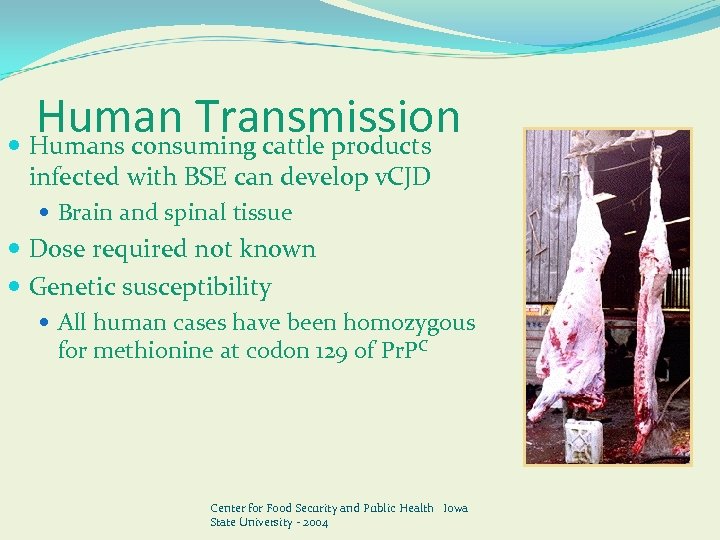 Human Transmission Humans consuming cattle products infected with BSE can develop v. CJD Brain and spinal tissue Dose required not known Genetic susceptibility All human cases have been homozygous for methionine at codon 129 of Pr. PC Center for Food Security and Public Health Iowa State University - 2004
Human Transmission Humans consuming cattle products infected with BSE can develop v. CJD Brain and spinal tissue Dose required not known Genetic susceptibility All human cases have been homozygous for methionine at codon 129 of Pr. PC Center for Food Security and Public Health Iowa State University - 2004
 Human Transmission Possible modes Transmission from surgical instruments used on tonsils, appendix, or brain tissue Growth hormone injections Vaccines Center for Food Security and Public Health Iowa State University - 2004
Human Transmission Possible modes Transmission from surgical instruments used on tonsils, appendix, or brain tissue Growth hormone injections Vaccines Center for Food Security and Public Health Iowa State University - 2004
 Human Transmission Unlikely modes Blood transmission Consumption of milk and milk products Gelatin products (when manufacturing process is done correctly) Center for Food Security and Public Health Iowa State University - 2004
Human Transmission Unlikely modes Blood transmission Consumption of milk and milk products Gelatin products (when manufacturing process is done correctly) Center for Food Security and Public Health Iowa State University - 2004
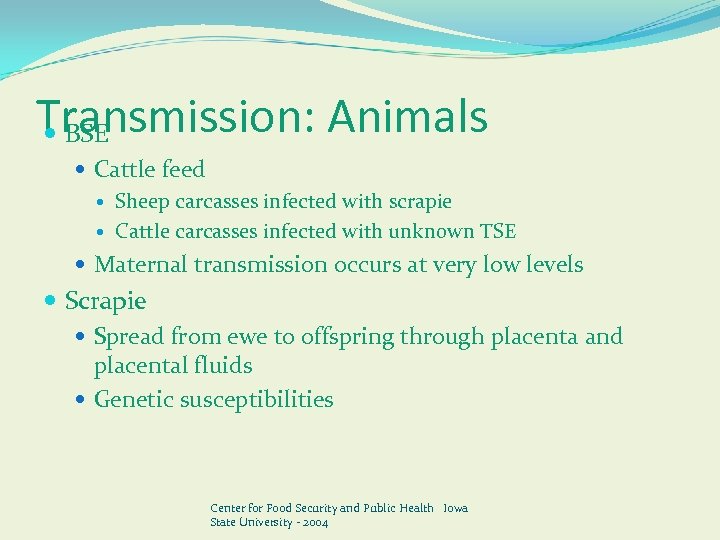 Transmission: Animals BSE Cattle feed Sheep carcasses infected with scrapie Cattle carcasses infected with unknown TSE Maternal transmission occurs at very low levels Scrapie Spread from ewe to offspring through placenta and placental fluids Genetic susceptibilities Center for Food Security and Public Health Iowa State University - 2004
Transmission: Animals BSE Cattle feed Sheep carcasses infected with scrapie Cattle carcasses infected with unknown TSE Maternal transmission occurs at very low levels Scrapie Spread from ewe to offspring through placenta and placental fluids Genetic susceptibilities Center for Food Security and Public Health Iowa State University - 2004
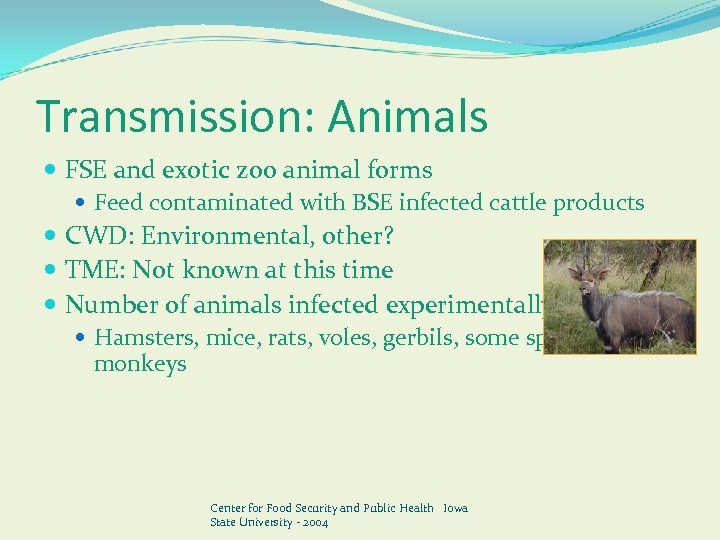 Transmission: Animals FSE and exotic zoo animal forms Feed contaminated with BSE infected cattle products CWD: Environmental, other? TME: Not known at this time Number of animals infected experimentally Hamsters, mice, rats, voles, gerbils, some species of monkeys Center for Food Security and Public Health Iowa State University - 2004
Transmission: Animals FSE and exotic zoo animal forms Feed contaminated with BSE infected cattle products CWD: Environmental, other? TME: Not known at this time Number of animals infected experimentally Hamsters, mice, rats, voles, gerbils, some species of monkeys Center for Food Security and Public Health Iowa State University - 2004
 Disease in Humans
Disease in Humans
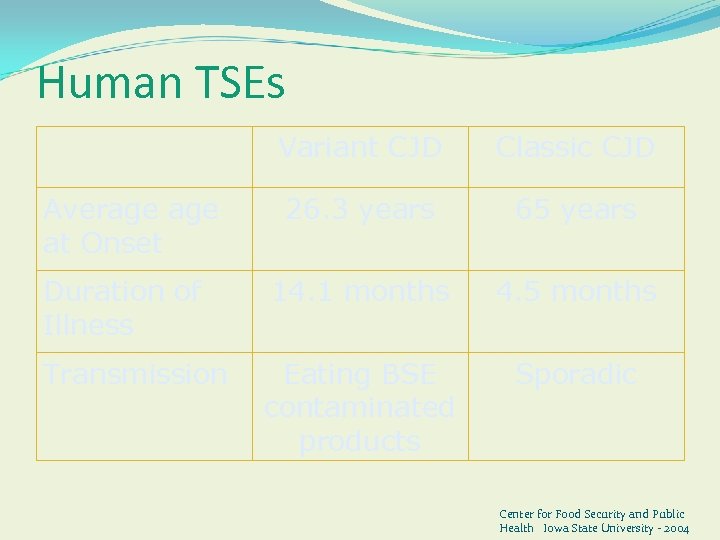 Human TSEs Variant CJD Classic CJD 26. 3 years 65 years Duration of Illness 14. 1 months 4. 5 months Transmission Eating BSE contaminated products Sporadic Average at Onset Center for Food Security and Public Health Iowa State University - 2004
Human TSEs Variant CJD Classic CJD 26. 3 years 65 years Duration of Illness 14. 1 months 4. 5 months Transmission Eating BSE contaminated products Sporadic Average at Onset Center for Food Security and Public Health Iowa State University - 2004
 Clinical Symptoms: v. CJD Initial symptoms Depression and schizophrenia like psychosis Neurological signs Unsteadiness, difficulty walking, and involuntary muscle movements Progression Become completely immobile and mute Center for Food Security and Public Health Iowa State University - 2004
Clinical Symptoms: v. CJD Initial symptoms Depression and schizophrenia like psychosis Neurological signs Unsteadiness, difficulty walking, and involuntary muscle movements Progression Become completely immobile and mute Center for Food Security and Public Health Iowa State University - 2004
 Diagnosis: v. CJD U. K. criteria for antemortem diagnosis Neuropsychiatric disorder with duration longer than 6 months Specific clinical signs Abnormal EEG Tonsilar biopsy with detection of prion protein Center for Food Security and Public Health Iowa State University - 2004
Diagnosis: v. CJD U. K. criteria for antemortem diagnosis Neuropsychiatric disorder with duration longer than 6 months Specific clinical signs Abnormal EEG Tonsilar biopsy with detection of prion protein Center for Food Security and Public Health Iowa State University - 2004
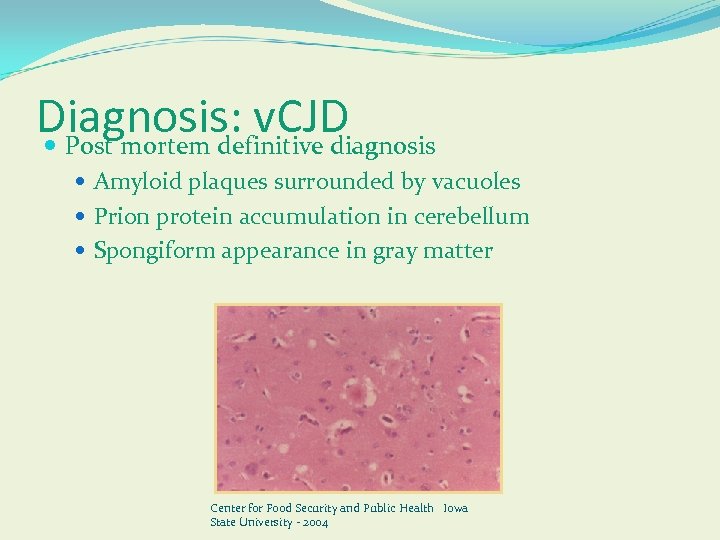 Diagnosis: v. CJD Post mortem definitive diagnosis Amyloid plaques surrounded by vacuoles Prion protein accumulation in cerebellum Spongiform appearance in gray matter Center for Food Security and Public Health Iowa State University - 2004
Diagnosis: v. CJD Post mortem definitive diagnosis Amyloid plaques surrounded by vacuoles Prion protein accumulation in cerebellum Spongiform appearance in gray matter Center for Food Security and Public Health Iowa State University - 2004
 Treatment: v. CJD No effective treatment available Experimental drugs under investigation Quinicrine Symptomatic treatment Supportive care Center for Food Security and Public Health Iowa State University - 2004
Treatment: v. CJD No effective treatment available Experimental drugs under investigation Quinicrine Symptomatic treatment Supportive care Center for Food Security and Public Health Iowa State University - 2004
 TSE’s and Animals
TSE’s and Animals
 Incubation Period Scrapie: Sheep 2 -5 years BSE: Cattle 2 -8 years CWD: Deer and elk 18 months TME: Mink 7+ months FSE: Feline unknown, most 4 -9 years of age Center for Food Security and Public Health Iowa State University - 2004
Incubation Period Scrapie: Sheep 2 -5 years BSE: Cattle 2 -8 years CWD: Deer and elk 18 months TME: Mink 7+ months FSE: Feline unknown, most 4 -9 years of age Center for Food Security and Public Health Iowa State University - 2004
 Clinical Signs: BSE, Scrapie, CWD Initial clinical signs subtle, mainly behavioral Increased excitability, nervousness, aggressiveness, and increased sensitivity to noise Pruritus and rubbing Sheep Center for Food Security and Public Health Iowa State University - 2004
Clinical Signs: BSE, Scrapie, CWD Initial clinical signs subtle, mainly behavioral Increased excitability, nervousness, aggressiveness, and increased sensitivity to noise Pruritus and rubbing Sheep Center for Food Security and Public Health Iowa State University - 2004
 Clinical Signs: BSE, Scrapie, CWD Terminal state Hypokinesis, hypermetria, falling and general paresis Tremors and muscle fasciculations Neck and face Wasting despite good appetite PU/PD in deer and elk Center for Food Security and Public Health Iowa State University - 2004
Clinical Signs: BSE, Scrapie, CWD Terminal state Hypokinesis, hypermetria, falling and general paresis Tremors and muscle fasciculations Neck and face Wasting despite good appetite PU/PD in deer and elk Center for Food Security and Public Health Iowa State University - 2004
 Diagnosis Post mortem: detection of prion Microscopic examination of brain tissue at necropsy Live animal tests: USDA/APHIS Tonsillar biopsy in deer Time consuming and expensive 3 rd eyelid test in sheep Blood tests Center for Food Security and Public Health Iowa State University - 2004
Diagnosis Post mortem: detection of prion Microscopic examination of brain tissue at necropsy Live animal tests: USDA/APHIS Tonsillar biopsy in deer Time consuming and expensive 3 rd eyelid test in sheep Blood tests Center for Food Security and Public Health Iowa State University - 2004
 Prevention and Control
Prevention and Control
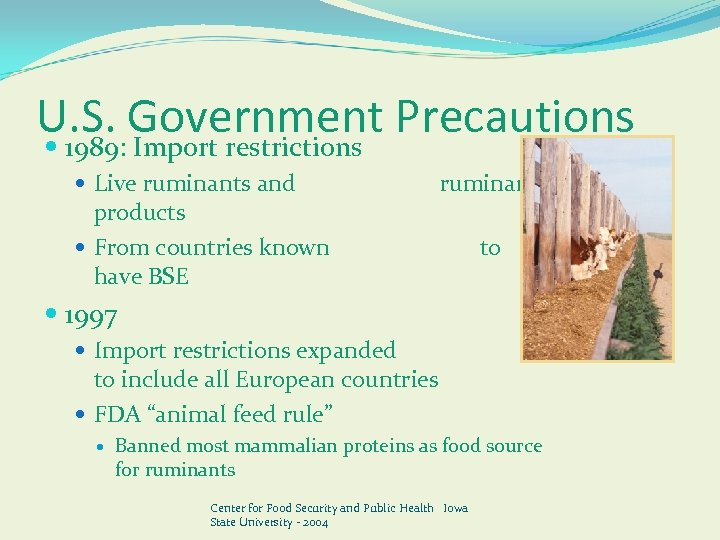 U. S. Government Precautions 1989: Import restrictions Live ruminants and ruminant products From countries known to have BSE 1997 Import restrictions expanded to include all European countries FDA “animal feed rule” Banned most mammalian proteins as food source for ruminants Center for Food Security and Public Health Iowa State University - 2004
U. S. Government Precautions 1989: Import restrictions Live ruminants and ruminant products From countries known to have BSE 1997 Import restrictions expanded to include all European countries FDA “animal feed rule” Banned most mammalian proteins as food source for ruminants Center for Food Security and Public Health Iowa State University - 2004
 U. S. Government Precautions Targeted surveillance High risk animals Adult animals with neurological signs Non-ambulatory “downer” cows Rabies- negative cattle Cattle dying on farms 2003: 20, 000 animals tested for BSE 47 times the number required by the OIE 2004: Enhanced surveillance Test maximum number of animals possible Center for Food Security and Public Health Iowa State University - 2004
U. S. Government Precautions Targeted surveillance High risk animals Adult animals with neurological signs Non-ambulatory “downer” cows Rabies- negative cattle Cattle dying on farms 2003: 20, 000 animals tested for BSE 47 times the number required by the OIE 2004: Enhanced surveillance Test maximum number of animals possible Center for Food Security and Public Health Iowa State University - 2004
 Specific Guidelines for Hunters Regarding CWD Public health officials recommend avoiding human exposure to CWD agent Harvest only animals that look and behave normally Do not eat any animal products of sick or infected elk and deer Do not eat brain, spinal cord, eyes, spleen, tonsils and lymph nodes Center for Food Security and Public Health Iowa State University - 2004
Specific Guidelines for Hunters Regarding CWD Public health officials recommend avoiding human exposure to CWD agent Harvest only animals that look and behave normally Do not eat any animal products of sick or infected elk and deer Do not eat brain, spinal cord, eyes, spleen, tonsils and lymph nodes Center for Food Security and Public Health Iowa State University - 2004
 Specific Guidelines for Hunters Regarding CWD Dress the deer/elk properly Minimize handling of brain and spinal tissues Wear rubber gloves when field dressing Use strong household bleach for cleaning knifes and saws Any suspicious elk and deer should be reported to health officials Testing of elk and deer available in many states Center for Food Security and Public Health Iowa State University - 2004
Specific Guidelines for Hunters Regarding CWD Dress the deer/elk properly Minimize handling of brain and spinal tissues Wear rubber gloves when field dressing Use strong household bleach for cleaning knifes and saws Any suspicious elk and deer should be reported to health officials Testing of elk and deer available in many states Center for Food Security and Public Health Iowa State University - 2004
 Prevention and Control Surveillance for CJD in US CDC Blood/plasma donation restrictions Persons who have traveled or resided in the U. K. for 3 or more cumulative months from 1980 to 1996 FDA Website www. fda. gov/cber/gdlns/cjdvcjd. pdf Center for Food Security and Public Health Iowa State University - 2004
Prevention and Control Surveillance for CJD in US CDC Blood/plasma donation restrictions Persons who have traveled or resided in the U. K. for 3 or more cumulative months from 1980 to 1996 FDA Website www. fda. gov/cber/gdlns/cjdvcjd. pdf Center for Food Security and Public Health Iowa State University - 2004
 Ebola Virus Hemorrhagic Fever
Ebola Virus Hemorrhagic Fever
 Outbreaks 1976 - First Major Outbreak (ZEBOV) 1976 - Sudan (SEBOV) Occur Sporadically Currently another going on right now in Africa
Outbreaks 1976 - First Major Outbreak (ZEBOV) 1976 - Sudan (SEBOV) Occur Sporadically Currently another going on right now in Africa
 Where does Ebola hide? 2002 - Fruit Bats Antibodies against Ebola Gene sequences in liver and spleen Fruit bats do not show any symptoms Best candidate to be the reservoir More research needs to be done
Where does Ebola hide? 2002 - Fruit Bats Antibodies against Ebola Gene sequences in liver and spleen Fruit bats do not show any symptoms Best candidate to be the reservoir More research needs to be done
 Geography The link between human infection by the Ebola virus and their proximity to primates is clear. -Outbreaks occurred in countries that house 80 percent of the world’s remaining wild gorilla and chimpanzee populations. - The outbreaks coincided with the outbreaks in wild animals. - The same distinct viral strains were isolated in animal carcasses and in the bodies of those who handled those carcasses. - These outbreaks were preceded by an abnormally large death in wild Gorilla populations.
Geography The link between human infection by the Ebola virus and their proximity to primates is clear. -Outbreaks occurred in countries that house 80 percent of the world’s remaining wild gorilla and chimpanzee populations. - The outbreaks coincided with the outbreaks in wild animals. - The same distinct viral strains were isolated in animal carcasses and in the bodies of those who handled those carcasses. - These outbreaks were preceded by an abnormally large death in wild Gorilla populations.
 Clinical Observations Incubation period: 2 -21 days Stage I (unspecific): -Extreme asthenia (body weakness) -diarrhea, nausea and vomiting, anorexia abdominal pain - headaches - arthralgia (neuralgic pain in joints) - myalgia (muscular pain or tenderness), back pain - mucosal redness of the oral cavity, dysphagia (difficulty in swallowing) - conjunctivitis. - rash all over body except in face
Clinical Observations Incubation period: 2 -21 days Stage I (unspecific): -Extreme asthenia (body weakness) -diarrhea, nausea and vomiting, anorexia abdominal pain - headaches - arthralgia (neuralgic pain in joints) - myalgia (muscular pain or tenderness), back pain - mucosal redness of the oral cavity, dysphagia (difficulty in swallowing) - conjunctivitis. - rash all over body except in face
 Stage II (Specific): • • Diarrhea vomiting Rash impaired kidney and liver function both internal and external bleeding (Hemorrhaging) neuropsychiatric abnormalities anuria (the absence of urine formation) tachypnea (rapid breathing) EVD outbreaks have a case fatality rate of up to 90%. Late Complications: -Arthralgia - ocular diseases (ocular pain, photophobia and hyperlacrimation) - hearing loss - unilateral orchitis( inflammation of one or both of the testes)
Stage II (Specific): • • Diarrhea vomiting Rash impaired kidney and liver function both internal and external bleeding (Hemorrhaging) neuropsychiatric abnormalities anuria (the absence of urine formation) tachypnea (rapid breathing) EVD outbreaks have a case fatality rate of up to 90%. Late Complications: -Arthralgia - ocular diseases (ocular pain, photophobia and hyperlacrimation) - hearing loss - unilateral orchitis( inflammation of one or both of the testes)
 Epidemiology Ebola Hemorrhagic Fever was first found in 1976 It struck two countries within that year a. Sudan – in a town called N’zara b. Zaire, now known as the Democratic Republic of Congo In these two instances the mortality rate was between 50 – 90% Following those epidemics, Ebola hit Africa in many other instances the worst yet being in the year 2000 when it struck Uganda infecting more than 400 people.
Epidemiology Ebola Hemorrhagic Fever was first found in 1976 It struck two countries within that year a. Sudan – in a town called N’zara b. Zaire, now known as the Democratic Republic of Congo In these two instances the mortality rate was between 50 – 90% Following those epidemics, Ebola hit Africa in many other instances the worst yet being in the year 2000 when it struck Uganda infecting more than 400 people.
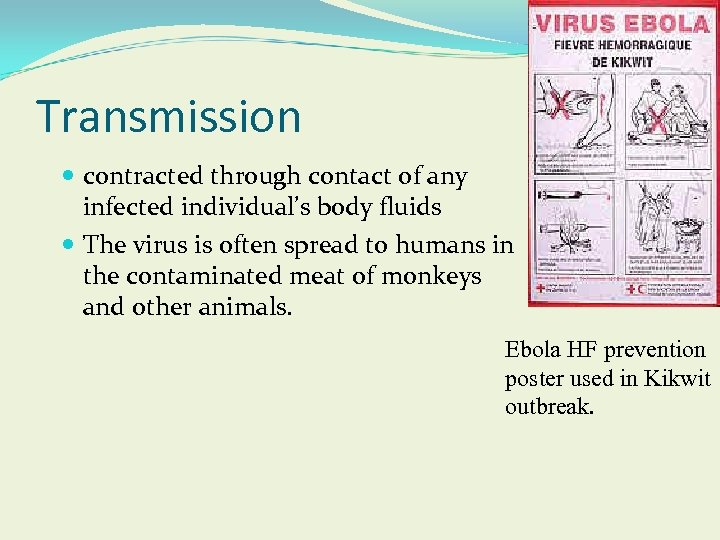 Transmission contracted through contact of any infected individual’s body fluids The virus is often spread to humans in the contaminated meat of monkeys and other animals. Ebola HF prevention poster used in Kikwit outbreak.
Transmission contracted through contact of any infected individual’s body fluids The virus is often spread to humans in the contaminated meat of monkeys and other animals. Ebola HF prevention poster used in Kikwit outbreak.
 Controlling the spread of Ebola human to human a. Hospitals must follow precautionary methods, such as: 1. wearing gloves 2. isolating infected individuals 3. practicing nurse barrier techniques 4. proper sterilization and disposal of all equipment b. Burials must be done correctly 1. no washing or touching carcass 2. put into body bags and bury outside city c. Report any questionable illness to officials
Controlling the spread of Ebola human to human a. Hospitals must follow precautionary methods, such as: 1. wearing gloves 2. isolating infected individuals 3. practicing nurse barrier techniques 4. proper sterilization and disposal of all equipment b. Burials must be done correctly 1. no washing or touching carcass 2. put into body bags and bury outside city c. Report any questionable illness to officials
 Structure of Ebola genome and proteins Transcribed into 8 sub-genomic m. RNA proteins: 7 structural and 1 nonstructural 7 structural proteins: nucleoprotein (NP) 4 viral/virion proteins (VP 35, VP 40, VP 30, VP 24) glycoprotein (GP) RNA-dependent RNA polymerase (L protein) NP, VP 35, VP 30, L protein: required for transcription & replication VP 40, GP, VP 24: associated with the membrane
Structure of Ebola genome and proteins Transcribed into 8 sub-genomic m. RNA proteins: 7 structural and 1 nonstructural 7 structural proteins: nucleoprotein (NP) 4 viral/virion proteins (VP 35, VP 40, VP 30, VP 24) glycoprotein (GP) RNA-dependent RNA polymerase (L protein) NP, VP 35, VP 30, L protein: required for transcription & replication VP 40, GP, VP 24: associated with the membrane
 Vaccine? Not yet… Why? That is a Ethics Question Biogeograophical Ethics is defined as motivation based on ideas of right and wrong when dealing with the geographical distribution of animals and plants. This concept of can be used to explain the world’s shockingly small response to the Ebola Virus. Because there was little travel to that region by people of more developed countries, there was not much economic drive for a vaccine, treatment, and aid in prevention.
Vaccine? Not yet… Why? That is a Ethics Question Biogeograophical Ethics is defined as motivation based on ideas of right and wrong when dealing with the geographical distribution of animals and plants. This concept of can be used to explain the world’s shockingly small response to the Ebola Virus. Because there was little travel to that region by people of more developed countries, there was not much economic drive for a vaccine, treatment, and aid in prevention.
 Bioterrorism Since the September 11 bombings in the United States, the locality of this virus has become less isolated as the threat of bioterrorism looms large. The Ebola virus is now on the “A” list for hopeful vaccination development.
Bioterrorism Since the September 11 bombings in the United States, the locality of this virus has become less isolated as the threat of bioterrorism looms large. The Ebola virus is now on the “A” list for hopeful vaccination development.
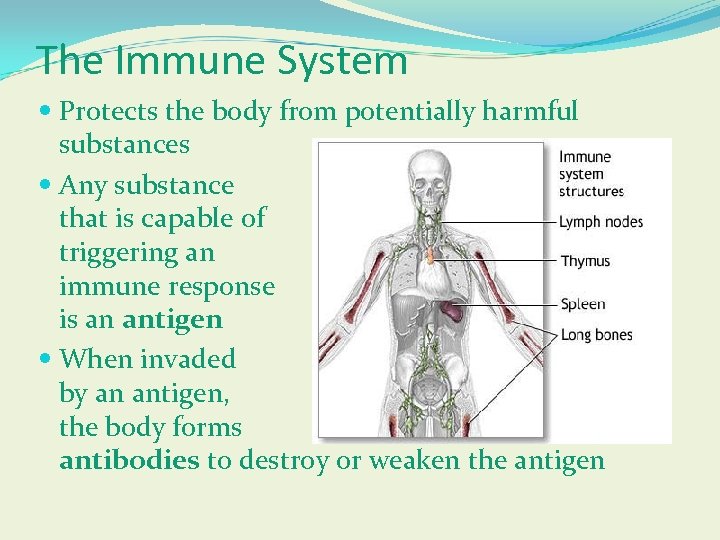 The Immune System Protects the body from potentially harmful substances Any substance that is capable of triggering an immune response is an antigen When invaded by an antigen, the body forms antibodies to destroy or weaken the antigen
The Immune System Protects the body from potentially harmful substances Any substance that is capable of triggering an immune response is an antigen When invaded by an antigen, the body forms antibodies to destroy or weaken the antigen
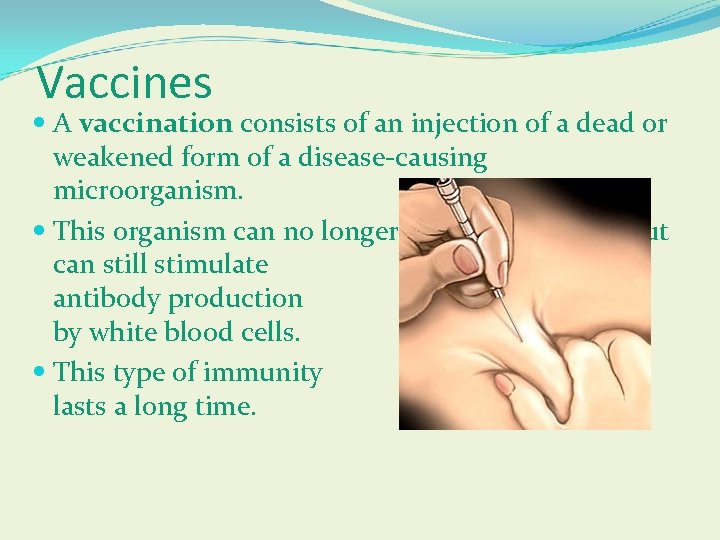 Vaccines A vaccination consists of an injection of a dead or weakened form of a disease-causing microorganism. This organism can no longer cause the disease, but can still stimulate antibody production by white blood cells. This type of immunity lasts a long time.
Vaccines A vaccination consists of an injection of a dead or weakened form of a disease-causing microorganism. This organism can no longer cause the disease, but can still stimulate antibody production by white blood cells. This type of immunity lasts a long time.
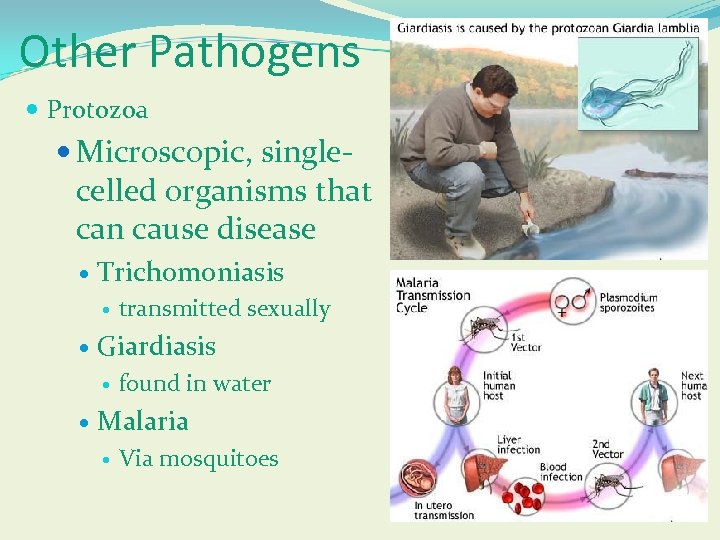 Other Pathogens Protozoa Microscopic, single- celled organisms that can cause disease Trichomoniasis Giardiasis transmitted sexually found in water Malaria Via mosquitoes
Other Pathogens Protozoa Microscopic, single- celled organisms that can cause disease Trichomoniasis Giardiasis transmitted sexually found in water Malaria Via mosquitoes
 Please note that this ppt is a compilation of work provided by the following: Dr. Durden, Emerging Diseases GSU Baldwinsville Central School District Henry County School District Kennesaw State University CDC Weekly Report - Jeanna Geise Case Report CDC reduces PEP from 5 to 4 doses vaccine Jamie Snow, DVM, MPH Danelle Bickett-Weddle, DVM, MPH Glenda Dvorak, DVM, MS, MPH Katie Steneroden, DVM, MPH Radford Davis, DVM, MPH Jean Gladon, BS WHO Conner
Please note that this ppt is a compilation of work provided by the following: Dr. Durden, Emerging Diseases GSU Baldwinsville Central School District Henry County School District Kennesaw State University CDC Weekly Report - Jeanna Geise Case Report CDC reduces PEP from 5 to 4 doses vaccine Jamie Snow, DVM, MPH Danelle Bickett-Weddle, DVM, MPH Glenda Dvorak, DVM, MS, MPH Katie Steneroden, DVM, MPH Radford Davis, DVM, MPH Jean Gladon, BS WHO Conner


