cd5b76d3348f4c63d41dbd7cbf4c2cec.ppt
- Количество слайдов: 88
ﺑﻬﺪﺍﺷﺖ ﻭ ﻣﺮﺍﻗﺒﺘﻬﺎﻱ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ

ﺍﻫﺪﺍﻑ آﻤﻮﺯﺷﻲ • • • ﺍﻫﻤﻴﺖ ﻣﺮﺍﻗﺒﺘﻬﺎﻱ ﺑﺎﺭﺩﺍﺭﻱ ﻋﻠﺖ ﺍﻧﺠﺎﻡ ﻣﺮﺍﻗﺒﺘﻬﺎﻱ ﺑﺎﺭﺩﺍﺭﻱ ﺟﺰﺋﻴﺎﺕ ﻣﺮﺍﻗﺒﺘﻬﺎﻱ ﺑﺎﺭﺩﺍﺭﻱ ﺗﻐﻴﻴﺮﺍﺕ ﻭ ﻣﺸکﻼﺕ ﺷﺎﻳﻊ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ ﻭ ﻧﺤﻮﻩ ﻣﺪﻳﺮﻳﺖ آﻦ ﺗﻐﺬﻳﻪ ﺩﺭ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ
• ﺑﺎﺭﺩﺍﺭﻱ پﺪﻳﺪﻩ ﺍﻱ ﻛﺎﻣﻼ ﻃﺒﻴﻌﻲ ﺍﺳﺖ. ﻳﻜﻲ ﺍﺯ ﺷﻴﺮﻳﻦ ﺗﺮﻳﻦ ﻣﺮﺍﺣﻞ ﺯﻧﺪگﻲ ﻫﺮﺯﻧﻲ، ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ، ﺯﻣﺎﻥ ﺍﻧﺘﻈﺎﺭ ﻭ آﻤﺎﺩﻩ ﺷﺪﻥ ﺍﻭ ﺑﺮﺍﻱ پﺬﻳﺮﺵ ﻣﺴﺌﻮﻟﻴﺖ ﺑﺰﺭگ ﻣﺎﺩﺭ ﺷﺪﻥ ﺍﺳﺖ. • ﻫﺪﻑ ﺍﺻﻠﻲ ﺍﺯ ﺍﻧﺠﺎﻡ ﻣﺮﺍﻗﺒﺖ ﻫﺎﻱ ﺍﻳﻦ ﺩﻭﺭﺍﻥ، ﺗﻮﻟﺪ ﻧﻮﺯﺍﺩﻱ ﺳﺎﻟﻢ، ﺑﺪﻭﻥ ﺑﻪ ﺧﻄﺮ ﺍﻧﺪﺍﺧﺘﻦ ﺳﻼﻣﺖ ﻣﺎﺩﺭ ﺍﺳﺖ. • ﺍﻃﻤﻴﻨﺎﻥ ﺍﺯ ﺍﻳﻨکﻪ ﺗﻤﺎﻡ ﺣﺎﻣﻠگﻴﻬﺎﻱ ﺧﻮﺍﺳﺘﻪ ﻭ ﻧﺎﺧﻮﺍﺳﺘﻪ ﻣﻨﺠﺮ ﺑﻪ ﺯﺍﻳﻤﺎﻥ ﻳک کﻮﺩک ﺳﺎﻟﻢ ﺷﻮﺩ ﺑﺪﻭﻥ ﺍﻳﻨکﻪ ﺳﻼﻣﺘﻲ ﻣﺎﺩﺭ ﺑﻪ ﺧﻄﺮ ﺍﻓﺘﺪ. • ﺑﺎﺭﺩﺍﺭﻱ پﺪﻳﺪﻩ ﺍﻱ ﻓﻴﺰﻳﻮﻟﻮژﻴک ﻭ ﻃﺒﻴﻌﻲ ﺍﺳﺖ.

• • • ﻣﺪﺕ ﺯﻣﺎﻥ ﻃﺒﻴﻌﻲ ﺩﻭﺭﻩ ﺑﺎﺭﺩﺍﺭﻱ، ﺑﻌﺪ ﺍﺯ ﺍﻟﻴﻦ ﺭﻭﺯ آﺨﺮﻳﻦ ﻗﺎﻋﺪگﻲ) ،(LMP= last menstrual period ﺣﺪﻭﺩ 04 ﻫﻔﺘﻪ ﻳﺎ 082 ﺭﻭﺯ ﺍﺳﺖ. ﺑﺎﺭﺩﺍﺭﻱ ﺭﺍ ﺑﻪ 3 ﺩﻭﺭﻩ ﺳﻪ ﻣﺎﻫﻪ ﺗﻘﺴﻴﻢ ﻣﻲ ﻛﻨﻨﺪ: ﺳﻪ ﻣﺎﻫﻪ ﺍﻭﻝ: ﺍﺯ ﺍﺑﺘﺪﺍﻱ ﺑﺎﺭﺩﺍﺭﻱ ﺗﺎپﺎﻳﺎﻥ ﻫﻔﺘﻪ چﻬﺎﺭﺩﻫﻢ ﺳﻪ ﻣﺎﻫﻪ ﺩﻭﻡ: ﺍﺯ ﺍﻧﺘﻬﺎﻱ ﻫﻔﺘﻪ چﻬﺎﺭﺩﻫﻢ ﺗﺎ پﺎﻳﺎﻥ ﻫﻔﺘﻪ ﺑﻴﺴﺖ ﻭ ﻫﺸﺘﻢ ﺳﻪ ﻣﺎﻫﻪ ﺳﻮﻡ: ﺍﺯ ﺍﻧﺘﻬﺎﻱ ﻫﻔﺘﻪ ﺑﻴﺴﺖ ﻭ ﻫﺸﺘﻢ ﺗﺎ پﺎﻳﺎﻥ ﻫﻔﺘﻪ چﻬﻠﻢ ﺑﻬﺘﺮﻳﻦ ﻭﺍﺣﺪ • weeks of gestation completed
• ﻫﺰﻳﻨﻪ ﺍﻱ ﻛﻪ ﺻﺮﻑ ﻧگﻬﺪﺍﺭﻱ ﺍﺯ ﻣﺎﺩﺭ ﻳﺎ ﻧﻮﺯﺍﺩ ﻏﻴﺮﻃﺒﻴﻌﻲ ﻣﻲ ﺷﻮﺩ ﺑﻪ ﻣﺮﺍﺗﺐ ﺑﻴﺶ ﺍﺯ ﻫﺰﻳﻨﻪ ﺍﻧﺠﺎﻡ ﻣﺮﺍﻗﺒﺖ ﻫﺎﻱ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ ﺍﺳﺖ. ﺑﻪ ﻫﻤﻴﻦ ﺩﻟﻴﻞ ﺧﺎﻧﻢ ﻫﺎ ﺑﺎﻳﺪ ﺑﻪ ﻣﺤﺾ ﺍﻃﻼﻉ ﺍﺯ ﺑﺎﺭﺩﺍﺭﻱ، ﺟﻬﺖ ﺩﺭﻳﺎﻓﺖ ﻣﺮﺍﻗﺒﺖ ﻫﺎﻱ ﺍﻳﻦ ﺩﻭﺭﺍﻥ ﺑﻪ ﻣﺮﺍﻛﺰ ﺑﻬﺪﺍﺷﺘﻲ ﻣﺮﺍﺟﻌﻪ ﻛﻨﻨﺪ ﻭ ﺗﺤﺖ ﻧﻈﺮ پﺰﺷﻚ ﻳﺎ ﻣﺎﻣﺎ ﺑﺎﺷﻨﺪ. • ﺑﺮﺍﻱ ﺑﺴﻴﺎﺭﻱ ﺍﺯﺯﻧﺎﻥ، ﺑﺎﺭﺩﺍﺭﻱ ﻭﺗﻐﻴﻴﺮﺍﺕ ﻧﺎﺷﻲ ﺍﺯآﻦ ﻧﺎﺷﻨﺎﺧﺘﻪ ﻭ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﺮﺱ ﻭ ﺍﺿﻄﺮﺍﺏ ﺍﺳﺖ ﺍگﺮچﻪ ﺑﺎﻳﺪ ﺑﻪ ﻣﺎﺩﺭﺍﻥ ﺗﺎﻛﻴﺪ ﻛﺮﺩ ﻛﻪ ﺑﺎﺭﺩﺍﺭﻱ ﻳﻚ پﺪﻳﺪﻩ ﻃﺒﻴﻌﻲ ﺍﺳﺖ ﻭ ﺑﺴﻴﺎﺭﻱ ﺍﺯ ﺗﻐﻴﻴﺮﺍﺕ ﺍﻳﻦ ﺩﻭﺭﺍﻥ ﺑﻪ ﻣﻨﻈﻮﺭ ﺳﺎﺯگﺎﺭﻱ ﻣﺎﺩﺭ ﺑﺎ ﺷﺮﺍﻳﻂ ﺟﺪﻳﺪ، ﺭﺥ ﻣﻲ ﺩﻫﻨﺪ، ﻭﻟﻲ ﺑﺮﺍﻱ ﺟﻠﻮگﻴﺮﻱ ﺍﺯ ﺑﺮﻭﺯ ﻣﺸﻜﻼﺕ، ﺑﺎﻳﺪ ﻣﺎﺩﺭﺍﻥ ﺑﺎ ﺍﻳﻦ ﺩﻭﺭﻩ ﻭ ﺗﻐﻴﻴﺮﺍﺕ آﻦ آﺸﻨﺎ ﺷﻮﻧﺪ.
ﻣﺮﺍﻗﺒﺖ ﻫﺎﻱ ﺑﺎﺭﺩﺍﺭﻱ • ﺑﻪ ﻣﺤﺾ ﺍﻃﻼﻉ ﺍﺯ ﺣﺎﻣﻠگﻲ ) ﺍﺣﺘﻤﺎﻝ ﺣﺎﻣﻠگﻲ( ﺑﺎﻳﺪ ﻣﺮﺍﻗﺒﺖ ﻫﺎﻱ ﺑﺎﺭﺩﺍﺭﻱ ﺷﺮﻭﻉ ﺷﻮﺩ. )6 ﻫﻔﺘﻪ پﺲ ﺍﺯ ﺑﺎﺭﺩﺍﺭﻱ ﻳﺎ ﻫﻔﺘﻪ 8 پﺲ ﺍﺯ (LMP ﻳﻌﻨﻲ چﻨﺪ ﻫﻔﺘﻪ پﺲ ﺍﺯ missed period • ﺩﺭ ﻣﻮﺭﺩ ﺧﺎﻧﻤﻬﺎﻳﻲ کﻪ ﻣﺮﺍﻗﺒﺖ ﻗﺒﻞ ﺍﺯ ﺑﺎﺭﺩﺍﺭﻱ ﻧﺪﺍﺷﺘﻪ ﺍﻧﺪ ﺩﺭ ﺍﻭﻟﻴﻦ ﻓﺮﺻﺖ ﻭ ﻣﺤﺘﻮﻳﺎﺕ ﻫﻤﺎﻥ ﻫﻢ ﺑﺎﻳﺪ پﻮﺷﺶ ﺩﺍﺩﻩ ﺷﻮﺩ. • ﺑﺎ ﺷﺮﻭﻉ ﺑﺎﺭﺩﺍﺭﻱ، ﻣﺮﺍﻗﺒﺖ ﻫﺎﻱ ﺍﻳﻦ ﺩﻭﺭﺍﻥ آﻐﺎﺯ ﻣﻲ ﺷﻮﺩ. ﺩﺭ ﺍﻭﻟﻴﻦ ﻣﺮﺍﺟﻌﻪ ﺑﻪ ﻣﺮﻛﺰ ﺑﻬﺪﺍﺷﺘﻲ ﺩﺭﻣﺎﻧﻲ ﻳﺎ پﺰﺷﻚ ﻳﺎ ﻣﺎﻣﺎ، ﺍﻃﻼﻋﺎﺕ ﻻﺯﻡ ﺭﺍ ﺩﺭ ﻣﻮﺭﺩ ﺑﺎﺭﺩﺍﺭﻱ ﻭ ﺍﻫﻤﻴﺖ آﻦ ﺑﻪ ﺩﺳﺖ ﻣﻲ آﻭﺭﺩ ﻭ ﻣﻄﻤﺌﻦ ﻣﻲ ﺷﻮﺩ ﻛﻪ ﺑﺎ ﻣﺮﺍﺟﻌﻪ ﻣﺮﺗﺐ ﺳﻼﻣﺖ ﺍﻭ ﻭ ﻓﺮﺯﻧﺪﺵ ﺗﺄﻤﻴﻦ ﺧﻮﺍﻫﺪ ﺷﺪ.
ﺍﺭﺯﻳﺎﺑﻲ ﺍﻭﻟﻴﻪ • • • Intrauterine pregnancy? Assessment of viability Pregnancy test( urine or blood). • ﻣﺎﺩﺭ کﺎﺭﺕ ﻣﻌﺎﻳﻨﻪ ﺩﺍﺭﺩ کﻪ ﻫﻤﺮﺍﻩ ﺍﻭﺳﺖ • ﺷﺮﺡ ﺣﺎﻝ (menstrual Hx) − ﻗﺎﻋﺪگﻲ ﺑﺮﺍﻱ ﺗﻌﻴﻴﻦ ﺯﻣﺎﻥ ﺯﺍﻳﻤﺎﻥ − Estimated date of confinement − The Nagele rule § − − EDC= (LMP – 3 months )+ 1 week + 1 year)(± 2 wks) Past pregnancies Past medical Hx Drug Hx(Including OTC & herbal supplements) Family Hx
• ﺩﺭ کﺴﺎﻧﻲ کﻪ ﺳﻴکﻞ ﻧﺎﻣﻨﻈﻢ ﺍﺳﺖ ﻳﺎ LMP ﺭﺍ ﻧﻤﻲ ﺩﺍﻧﺪ • ﺳﻮﻧﻮگﺮﺍﻓﻲ ﻫﻔﺘﻪ 02 -41
ﻣﻮﺍﺭﺩﺯﻳﺮ ﺩﺭ ﺍﻟﻴﻦ ﻣﺮﺍﺟﻌﻪ، ﺍﺯ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ پﺮﺳﻴﺪﻩ ﻣﻲ ﺷﻮﺩ • ﻣﺸﺨﺼﺎﺕ ﺧﺎﻧﻮﺍﺩگﻲ، ﻭﺿﻌﻴﺖ ﺑﺎﺭﺩﺍﺭﻱ ﻓﻌﻠﻲ ﻭ ﻗﺒﻠﻲ، ﺗﻌﺪﺍﺩ ﺯﺍﻳﻤﺎﻥ ﻫﺎﻱ ﻗﺒﻠﻲ ﻭ ﻧﺘﻴﺠﻪ آﻨﻬﺎ • ﺳﺎﺑﻘﻪ ﺑﻴﻤﺎﺭﻱ ﻫﺎﻱ ﻓﻌﻠﻲ ﻭ ﻗﺒﻠﻲ، ﺳﺎﺑﻘﻪ ﺑﻴﻤﺎﺭﻱ ﻫﺎﻱ ﺍﺭﺛﻲ ﻭ ﻓﺎﻣﻴﻠﻲ، ﺭﻭﺵ ﻫﺎﻱ پﻴﺸگﻴﺮﻱ ﺍﺯ ﺑﺎﺭﺩﺍﺭﻱ ﺑﻪ ﻛﺎﺭ ﺭﻓﺘﻪ، ﺩﺍﺭﻭﻫﺎﻳﻲ ﻛﻪ ﻣﺼﺮﻑ ﻛﺮﺩﻩ ﻳﺎ ﻣﻲ ﻛﻨﺪ ﻭ ﻃﻮﻝ ﻣﺪﺕ ﻣﺼﺮﻑ آﻨﻬﺎ • ﺧﺎﻧﻢ ﻫﺎﻱ ﺑﺎﺭﺩﺍﺭﻱ ﻛﻪ ﻣﺸﻜﻞ ﺩﺍﺭﻧﺪ، ﺟﻬﺖ ﺩﺭﻳﺎﻓﺖ ﻣﺮﺍﻗﺒﺖ ﻫﺎﻱ ﻭﻳژﻪ ﺑﻪ ﻣﺘﺨﺼﺺ ﻣﻌﺮﻓﻲ ﻣﻴﺸﻮﻧﺪ، آﺰﻣﺎﻳﺸﻬﺎﻱ ﻻﺯﻡ ﺻﻮﺭﺕ ﻣﻲ گﻴﺮﺩ، ﻣﻌﺎﻳﻨﺎﺕ ﻋﻤﻮﻣﻲ ﺍﻧﺠﺎﻡ ﻣﻲ ﺷﻮﺩ ﻭﻓﺸﺎﺭﺧﻮﻥ، ﻭﺯﻥ ﻭﻗﺪ ﺍﻧﺪﺍﺯﻩ گﻴﺮﻱ ﻣﻲ ﺷﻮﻧﺪ ﻭ ﺗﺎﺭﻳﺦ ﻣﺮﺍﺟﻌﻪ ﺑﻌﺪﻱ ﻣﻌﻴﻦ ﻣﻲ ﺷﻮﺩ.
ﻣﻌﺎﻳﻨﻪ Pap smear Chlamydia & gonorrhea culture( in high ) risks • ﺑﺮﺭﺳﻲ ﺩﻧﺪﺍﻧﻬﺎ • ﺍﻧﺪﺍﺯﻩ گﻴﺮﻱ Wt, Ht, Bp • • − • ﺩﺭ ﻣﻮﺭﺩ ﺭژﻴﻢ ﻏﺬﺍﻳﻲ، ﺍﺟﺎﺑﺖ ﻣﺰﺍﺝ، ﻭﺭﺯﺵ، ﺍﺳﺘﺤﻤﺎﻡ، ﻟﺒﺎﺱ، ﺗﻔﺮﻳﺤﺎﺕ، ﻣﻘﺎﺭﺑﺖ، ﺳﻴگﺎﺭ، ﺩﺍﺭﻭ ﻭ ﺍﻟکﻞ ﻭ ﻭﻳﺰﻳﺘﻬﺎﻱ ﺑﻌﺪﻱ ﺑﺎ ﻣﺎﺩﺭ ﺻﺤﺒﺖ ﻣﻲ ﺷﻮﺩ. • ﻋﻼﺋﻢ ﺧﻄﺮ ﺭﺍ ﺑﻪ ﺍﻭ ﻳﺎﺩ ﻣﻲ ﺩﻫﻴﻢ کﻪ ﺩﺭ ﻫﺮ ﺯﻣﺎﻥ ﺣﺘﻤﺎ ﺑﺎﻳﺪ گﺰﺍﺭﺵ ﻭ ﺳﺮﻳﻌﺎ ﻣﺮﺍﺟﻌﻪ کﻨﺪ.
ﻋﻼﺋﻢ ﺧﻄﺮ • • • • ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﺑﺎﻳﺪ ﺑﻪ ﻣﺤﺾ ﻣﺸﺎﻫﺪﻩ ﻫﺮﻳﻚ ﺍﺯ ﻋﻼﺋﻢ ﺯﻳﺮ ﺑﻪ ﻣﺮﺍﻛﺰ ﺑﻬﺪﺍﺷﺘﻲ ﺩﺭﻣﺎﻧﻲ ﻳﺎ پﺰﺷﻚ ﻳﺎ ﻣﺎﻣﺎ ﻣﺮﺍﺟﻌﻪ ﻛﻨﺪ. ﻫﺮ گﻮﻧﻪ ﺧﻮﻧﺮﻳﺰﻱ ﺍﺯﺩﺳﺘگﺎﻩ ﺗﻨﺎﺳﻠﻲ ﺍﺧﺘ ﻻﺕ ﺑﻴﻨﺎﻳﻲ ﻭ ﺗﺎﺭﻱ ﺩﻳﺪ ﻼ ﺗﻬﻮﻉ ﻭ ﺍﺳﺘﻔﺮﺍﻍ ﻣﺪﺍﻭﻡ ﻭ ﺷﺪﻳﺪ ﻣﺸﻜﻞ ﺍﺩﺭﺍﺭﻱ ) ﺳﻮﺯﺵ ﺍﺩﺭﺍﺭ( ﺩﺭﺩ ﺯﻳﺮ ﺩﻝ ﻻﻏﺮﻱ ﻭ چﺎﻗﻲ ﺑﻴﺶ ﺍﺯ ﺣﺪ
ﻋﻼﺋﻢ ﺧﻄﺮ • • • • • ﻭﺭﻡ ﺑﻪ ﺧﺼﻮﺹ ﺩﺭ ﺩﺳﺖ ﻫﺎ ﻭ ﺻﻮﺭﺕ ﺳﺮﺩﺭﺩﻫﺎﻱ ﺷﺪﻳﺪ ﻳﺎ ﻣﺪﺍﻭﻡ ﺩﺭﺩ ﺳﺮ ﺩﻝ ﺗﺐ ﻭ ﻟﺮﺯ ﺗﻨگﻲ ﻧﻔﺲ ﻭ ﻃپﺶ ﻗﻠﺐ ﺳﺮﻓﻪ ﻣﺪﺍﻭﻡ ﻭ ﺷﺪﻳﺪ ﺩﺭﺩﻫﺎﻱ ﻣﻨﻈﻢ ﺷﻜﻢ آﺒﺮﻳﺰﺵ ﻭ ﻫﺮﻧﻮﻉ ﺗﺮﺷﺢ ﺑﺪﺑﻮ ﻭ چﺮﻛﻲ ﺍﺯ ﻭﺍژﻦ ﺗﻐﻴﻴﺮﺍﺕ ﻗﺎﺑﻞ ﺗﻮﺟﻪ ﺩﺭ ﻓﺮکﺎﻧﺲ ﻳﺎ ﺷﺪﺕ ﺣﺮکﺎﺕ ﺟﻨﻴﻦ

گﺮﻭﻫﻬﺎﻱ پﺮ ﺧﻄﺮ ü ü ü ﺧﻮﻧﺮﻳﺰﻱ ﻭ ﻟکﻪ ﺑﻴﻨﻲ ﺷکﻢ ﺍﻭﻝ ﺣﺎﻣﻠگﻲ 3 ﻳﺎ ﺑﻴﺸﺘﺮ ﺩﻭﻗﻠﻮ ﻭ ﻫﻴﺪﺭآﻤﻨﻴﻮﺱ ﺳﺎﺑﻘﻪ ﺗﺎﺧﻴﺮ ﺩﺭ ﺧﺮﻭﺝ ﺟﻔﺖ ﺍﺑﺘﻼ ﻳﺎ ﺳﺎﺑﻘﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﻬﻢ) ﻗﻠﺒﻲ کﻠﻴﻮﻱ ﺩﻳﺎﺑﺖ( ü ﻭﺟﻮﺩ آﻠﺒﻮﻣﻴﻦ ﺩﺭ ﺍﺩﺭﺍﺭ، ﺍﺩﻡ ü ﺣﺎﻣﻠگﻲ ﻳﺎ ﺯﺍﻳﻤﺎﻥ ﻗﺒﻠﻲ پﺮ ﺧﻄﺮ ü ﺳﺎﺑﻘﻪ ﺳﺰﺍﺭﻳﻦ ﻗﺒﻠﻲ ﻳﺎ ﺯﺍﻳﻤﺎﻥ ﺑﺎ ﻭﺳﻴﻠﻪ ü ﺳﺎﺑﻘﻪ ﻣﺮﺩﻩ ﺯﺍﻳﻲ ü ﻗﺪ > 051 ﺳﺎﻧﺘﻲ ﻣﺘﺮ ü ﺳﻦ کﻤﺘﺮ ﺍﺯ 81 ﻳﺎ ﺑﺎﻻﻱ 53 ﺳﺎﻝ Hb < 11 mg/dl ü ü ﺍﺧﺘﻼﻝ ﺩﺭ wt gain
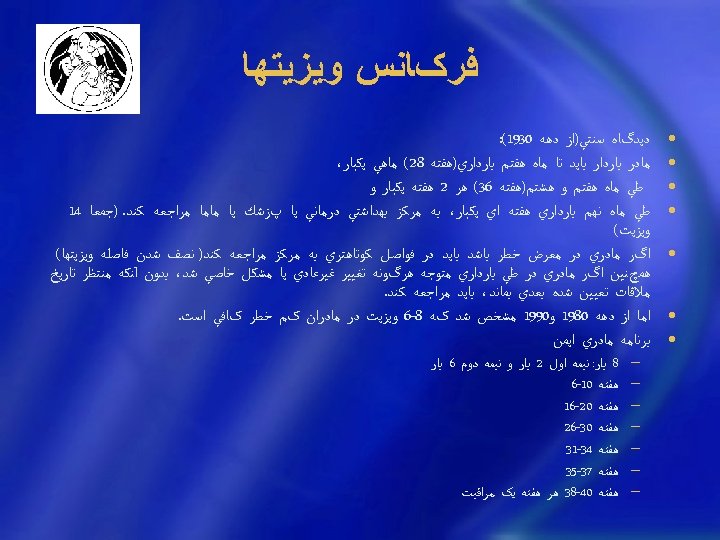
ﻓﺮکﺎﻧﺲ ﻭﻳﺰﻳﺘﻬﺎ • • • • ﺩﻳﺪگﺎﻩ ﺳﻨﺘﻲ)ﺍﺯ ﺩﻫﻪ 0391(: ﻣﺎﺩﺭ ﺑﺎﺭﺩﺍﺭ ﺑﺎﻳﺪ ﺗﺎ ﻣﺎﻩ ﻫﻔﺘﻢ ﺑﺎﺭﺩﺍﺭﻱ)ﻫﻔﺘﻪ 82( ﻣﺎﻫﻲ ﻳﻜﺒﺎﺭ، ﻃﻲ ﻣﺎﻩ ﻫﻔﺘﻢ ﻭ ﻫﺸﺘﻢ)ﻫﻔﺘﻪ 63( ﻫﺮ 2 ﻫﻔﺘﻪ ﻳﻜﺒﺎﺭ ﻭ ﻃﻲ ﻣﺎﻩ ﻧﻬﻢ ﺑﺎﺭﺩﺍﺭﻱ ﻫﻔﺘﻪ ﺍﻱ ﻳﻜﺒﺎﺭ، ﺑﻪ ﻣﺮﻛﺰ ﺑﻬﺪﺍﺷﺘﻲ ﺩﺭﻣﺎﻧﻲ ﻳﺎ پﺰﺷﻚ ﻳﺎ ﻣﺎﻣﺎ ﻣﺮﺍﺟﻌﻪ ﻛﻨﺪ. )ﺟﻤﻌﺎ 41 ﻭﻳﺰﻳﺖ( ﺍگﺮ ﻣﺎﺩﺭﻱ ﺩﺭ ﻣﻌﺮﺽ ﺧﻄﺮ ﺑﺎﺷﺪ ﺑﺎﻳﺪ ﺩﺭ ﻓﻮﺍﺻﻞ ﻛﻮﺗﺎﻫﺘﺮﻱ ﺑﻪ ﻣﺮﻛﺰ ﻣﺮﺍﺟﻌﻪ ﻛﻨﺪ) ﻧﺼﻒ ﺷﺪﻥ ﻓﺎﺻﻠﻪ ﻭﻳﺰﻳﺘﻬﺎ( ﻫﻤچﻨﻴﻦ ﺍگﺮ ﻣﺎﺩﺭﻱ ﺩﺭ ﻃﻲ ﺑﺎﺭﺩﺍﺭﻱ ﻣﺘﻮﺟﻪ ﻫﺮگﻮﻧﻪ ﺗﻐﻴﻴﺮ ﻏﻴﺮﻋﺎﺩﻱ ﻳﺎ ﻣﺸﻜﻞ ﺧﺎﺻﻲ ﺷﺪ، ﺑﺪﻭﻥ آﻨﻜﻪ ﻣﻨﺘﻈﺮ ﺗﺎﺭﻳﺦ ﻣﻼﻗﺎﺕ ﺗﻌﻴﻴﻦ ﺷﺪﻩ ﺑﻌﺪﻱ ﺑﻤﺎﻧﺪ، ﺑﺎﻳﺪ ﻣﺮﺍﺟﻌﻪ ﻛﻨﺪ. ﺍﻣﺎ ﺍﺯ ﺩﻫﻪ 0891 ﻭ 0991 ﻣﺸﺨﺺ ﺷﺪ کﻪ 8 -6 ﻭﻳﺰﻳﺖ ﺩﺭ ﻣﺎﺩﺭﺍﻥ کﻢ ﺧﻄﺮ کﺎﻓﻲ ﺍﺳﺖ. ﺑﺮﻧﺎﻣﻪ ﻣﺎﺩﺭﻱ ﺍﻳﻤﻦ − − 8 ﺑﺎﺭ: ﻧﻴﻤﻪ ﺍﻭﻝ 2 ﺑﺎﺭ ﻭ ﻧﻴﻤﻪ ﺩﻭﻡ 6 ﺑﺎﺭ ﻫﻔﺘﻪ 01 -6 ﻫﻔﺘﻪ 02 -61 ﻫﻔﺘﻪ 03 -62 ﻫﻔﺘﻪ 43 -13 ﻫﻔﺘﻪ 73 -53 ﻫﻔﺘﻪ 04 -83 ﻫﺮ ﻫﻔﺘﻪ ﻳک ﻣﺮﺍﻗﺒﺖ
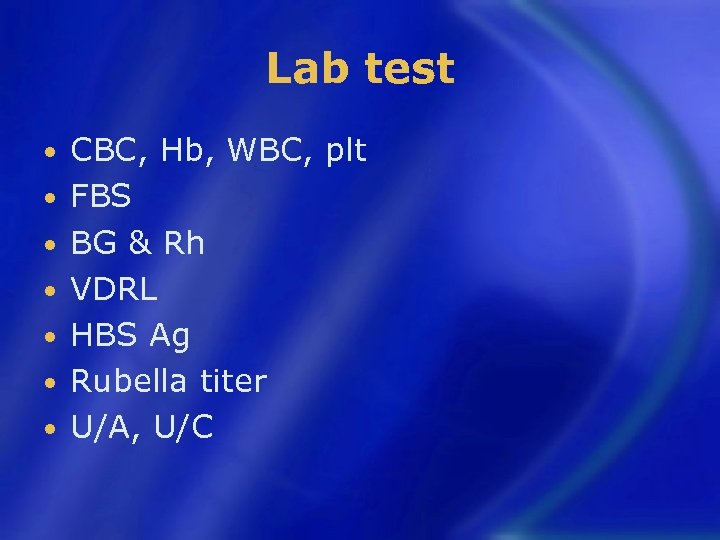
Lab test • • CBC, Hb, WBC, plt FBS BG & Rh VDRL HBS Ag Rubella titer U/A, U/C
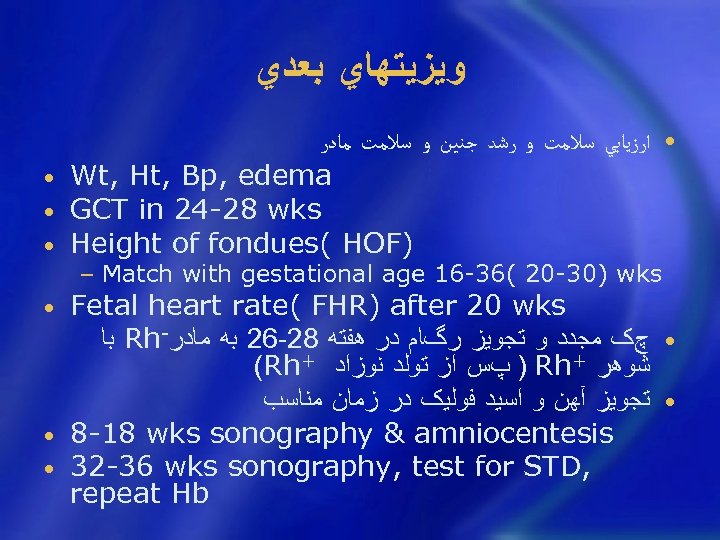
ﻭﻳﺰﻳﺘﻬﺎﻱ ﺑﻌﺪﻱ • ﺍﺭﺯﻳﺎﺑﻲ ﺳﻼﻣﺖ ﻭ ﺭﺷﺪ ﺟﻨﻴﻦ ﻭ ﺳﻼﻣﺖ ﻣﺎﺩﺭ • Wt, Ht, Bp, edema • GCT in 24 -28 wks • Height of fondues( HOF) − Match with gestational age 16 -36( 20 -30) wks Fetal heart rate( FHR) after 20 wks ﺑﺎ Rh- • چک ﻣﺠﺪﺩ ﻭ ﺗﺠﻮﻳﺰ ﺭگﺎﻡ ﺩﺭ ﻫﻔﺘﻪ 82 -62 ﺑﻪ ﻣﺎﺩﺭ (Rh+ ) پﺲ ﺍﺯ ﺗﻮﻟﺪ ﻧﻮﺯﺍﺩ Rh+ ﺷﻮﻫﺮ • ﺗﺠﻮﻳﺰ آﻬﻦ ﻭ ﺍﺳﻴﺪ ﻓﻮﻟﻴک ﺩﺭ ﺯﻣﺎﻥ ﻣﻨﺎﺳﺐ • 8 -18 wks sonography & amniocentesis • 32 -36 wks sonography, test for STD, repeat Hb •

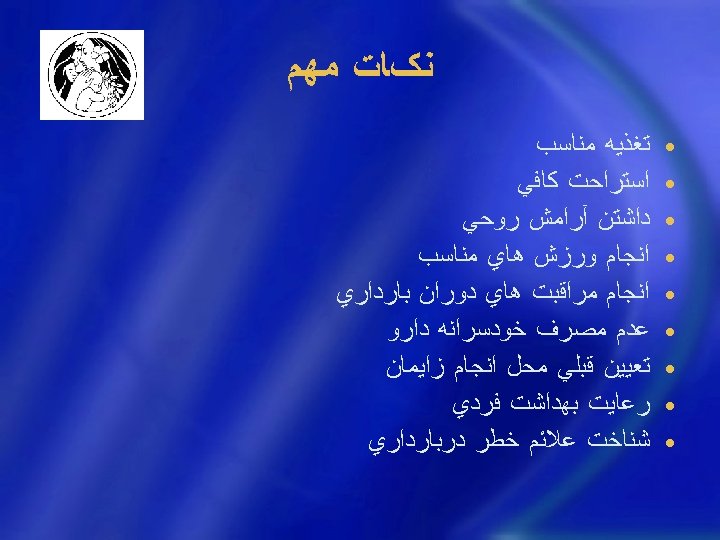
ﻧکﺎﺕ ﻣﻬﻢ • • • • • ﺗﻐﺬﻳﻪ ﻣﻨﺎﺳﺐ ﺍﺳﺘﺮﺍﺣﺖ ﻛﺎﻓﻲ ﺩﺍﺷﺘﻦ آﺮﺍﻣﺶ ﺭﻭﺣﻲ ﺍﻧﺠﺎﻡ ﻭﺭﺯﺵ ﻫﺎﻱ ﻣﻨﺎﺳﺐ ﺍﻧﺠﺎﻡ ﻣﺮﺍﻗﺒﺖ ﻫﺎﻱ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ ﻋﺪﻡ ﻣﺼﺮﻑ ﺧﻮﺩﺳﺮﺍﻧﻪ ﺩﺍﺭﻭ ﺗﻌﻴﻴﻦ ﻗﺒﻠﻲ ﻣﺤﻞ ﺍﻧﺠﺎﻡ ﺯﺍﻳﻤﺎﻥ ﺭﻋﺎﻳﺖ ﺑﻬﺪﺍﺷﺖ ﻓﺮﺩﻱ ﺷﻨﺎﺧﺖ ﻋﻼﺋﻢ ﺧﻄﺮ ﺩﺭﺑﺎﺭﺩﺍﺭﻱ
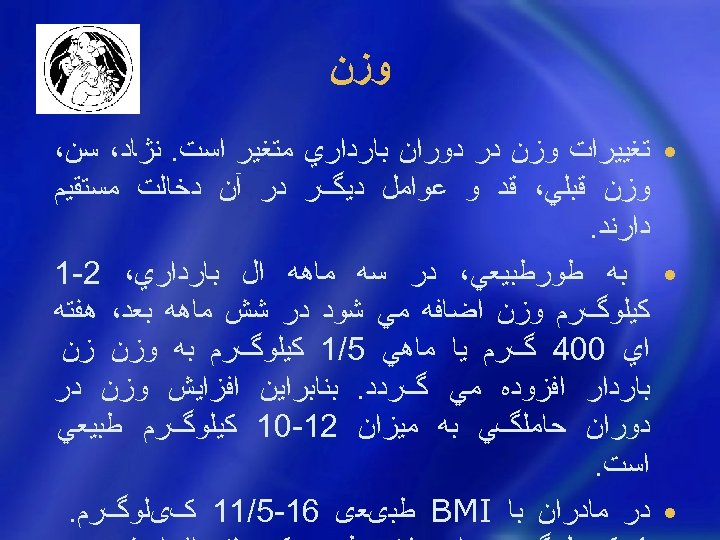
ﻭﺯﻥ • ﺗﻐﻴﻴﺮﺍﺕ ﻭﺯﻥ ﺩﺭ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ ﻣﺘﻐﻴﺮ ﺍﺳﺖ. ﻧژﺎﺩ، ﺳﻦ، ﻭﺯﻥ ﻗﺒﻠﻲ، ﻗﺪ ﻭ ﻋﻮﺍﻣﻞ ﺩﻳگﺮ ﺩﺭ آﻦ ﺩﺧﺎﻟﺖ ﻣﺴﺘﻘﻴﻢ ﺩﺍﺭﻧﺪ. • ﺑﻪ ﻃﻮﺭﻃﺒﻴﻌﻲ، ﺩﺭ ﺳﻪ ﻣﺎﻫﻪ ﺍﻝ ﺑﺎﺭﺩﺍﺭﻱ، 2 -1 ﻛﻴﻠﻮگﺮﻡ ﻭﺯﻥ ﺍﺿﺎﻓﻪ ﻣﻲ ﺷﻮﺩ ﺩﺭ ﺷﺶ ﻣﺎﻫﻪ ﺑﻌﺪ، ﻫﻔﺘﻪ ﺍﻱ 004 گﺮﻡ ﻳﺎ ﻣﺎﻫﻲ 5/1 ﻛﻴﻠﻮگﺮﻡ ﺑﻪ ﻭﺯﻥ ﺯﻥ ﺑﺎﺭﺩﺍﺭ ﺍﻓﺰﻭﺩﻩ ﻣﻲ گﺮﺩﺩ. ﺑﻨﺎﺑﺮﺍﻳﻦ ﺍﻓﺰﺍﻳﺶ ﻭﺯﻥ ﺩﺭ ﺩﻭﺭﺍﻥ ﺣﺎﻣﻠگﻲ ﺑﻪ ﻣﻴﺰﺍﻥ 21 -01 ﻛﻴﻠﻮگﺮﻡ ﻃﺒﻴﻌﻲ ﺍﺳﺖ. • ﺩﺭ ﻣﺎﺩﺭﺍﻥ ﺑﺎ BMI ﻃﺒیﻌی 61 -5/11 کیﻠﻮگﺮﻡ.
ﺑﻬﺪﺍﺷﺖ ﻭ ﻓﻌﺎﻟﻴﺖ • ﺍﻏﻠﺐ ﺯﻧﺎﻥ ﺑﺎﺭﺩﺍﺭ ﺣﺪﺍﻗﻞ ﺑﻪ 8 ﺳﺎﻋﺖ ﺧﻮﺍﺏ ﺷﺒﺎﻧﻪ ﻭ ﻫﻤچﻨﻴﻦ ﺑﻪ ﺍﺳﺘﺮﺍﺣﺖ ﺑﻌﺪ ﺍﺯ ﻇﻬﺮ ﺍﺣﺘﻴﺎﺝ ﺩﺍﺭﻧﺪ ﻓﻌﺎﻟﻴﺖ ﺩﺭ ﺩﻭﺭﺍﻥ ﺣﺎﻣﻠگﻲ ﺯﻳﺎﻥ آﻮﺭ ﻧﻴﺴﺖ، ﺍﻣﺎ ﺑﺎﻳﺪ ﺍﺯ ﺍﻧﺠﺎﻡ ﻛﺎﺭﻫﺎﻱ ﺳﻨگﻴﻦ ﻭ ﺟﺎﺑﻪ ﺟﺎ ﻛﺮﺩﻥ ﻭﺳﺎﻳﻞ ﺳﻨگﻴﻦ ﺧﻮﺩﺩﺍﺭﻱ ﻛﺮﺩ. ﻭﺿﻌﻴﺖ ﺭﻭﺣﻲ ﻭ ﺭﻭﺍﻧﻲ ﻣﺎﺩﺭ ﺩﺭ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ ﺑﻪ ﻃﻮﺭ ﻣﺴﺘﻘﻴﻢ ﺑﺮ ﺭﻭﻱ ﺳﻼﻣﺖ ﺟﻨﻴﻦ ﺗﺄﺜﻴﺮ ﻣﻴگﺬﺍﺭﺩ، ﻭﺭﺯﺵ ﻫﺎﻱ ﺳﺒﻚ ﺩﺭ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ ﺑﺮﺍﻱ ﻣﺎﺩﺭ ﻭ ﺟﻨﻴﻦ ﻣﻔﻴﺪ ﺍﺳﺖ.

ﻭﺭﺯﺵ • ﺑﻪ ﻃﻮﺭ ﻛﻱ ﻻﺯﻡ ﻧﻴﺴﺖ ﺯﻥ ﺣﺎﻣﻠﻪ ﺗﻤﺮﻳﻨﺎﺕ ﻭﺭﺯﺷﻲ ﺧﻮﺩ ﺭﺍ ﻣﺤﺪﻭﺩ ﻛﻨﺪ ﺑﻪ ﺷﺮﻃﻲ ﻛﻪ ﺧﻮﺩ ﺭﺍ ﺧﺴﺘﻪ ﻧﻜﻨﺪ. ﺑﻨﺎﺑﺮﺍﻳﻦ ﺑﺎﻳﺪ ﺍﺯ ﺍﻧﺠﺎﻡ ﻭﺭﺯﺵ ﻫﺎﻱ ﺳﻨگﻴﻦ ﻛﻪ ﺧﻄﺮ ﺍﻓﺘﺎﺩﻥ، ﺯﻣﻴﻦ ﺧﻮﺭﺩﻥ ﻭ ﺿﺮﺑﻪ ﺩﻳﺪﻥ ﺩﺍﺭﺩ پﺮﻫﻴﺰ ﺷﻮﺩ. پﻴﺎﺩﻩ ﺭﻭﻱ ﺳﺮﻳﻊ ﺍﺷکﺎﻟﻲ ﻧﺪﺍﺭﺩ. • ﺗﻮﺻﻴﻪ کﺎﻟﺞ OB/GYn آﻤﺮﻳکﺎ − ﺯﻧﺎﻧﻲ کﻪ ﻋﺎﺩﺕ ﺑﻪ ﻭﺭﺯﺷﻬﺎﻱ ﻫﻮﺍﺯﻱ ﻗﺒﻞ ﺍﺯ ﺣﺎﻣﻠگﻲ ﺩﺍﺭﻧﺪ ﻣﻲ ﺗﻮﺍﻧﻨﺪ ﺍﺩﺍﻣﻪ ﺩﻫﻨﺪ. ﺍﻣﺎ ﻧﺒﺎﻳﺪ ﺑﺮﻧﺎﻣﻪ ﺟﺪﻳﺪﻱ ﺩﺭ ﺣﺎﻣﻠگﻲ ﺷﺮﻭﻉ کﺮﺩ ﻭ ﻳﺎ ﺑﺮﻧﺎﻣﻪ ﻫﺎﻱ ﻗﺒﻠﻲ ﺭﺍ ﺷﺪﺕ ﺑﺨﺸﻴﺪ. − ﻣﺜﻼ ﺧﺎﻧﻤﻲ کﻪ ﺯﻧﺪگﻲ ﻧﺸﺴﺘﻪ ﺩﺍﺷﺘﻪ، ﺍﻻﻥ ﻭﺭﺯﺵ ﻫﻮﺍﺯﻱ ﺑﻴﺸﺘﺮ ﺍﺯ ﻗﺪﻡ ﺯﺩﻥ ﺗﻮﺻﻴﻪ ﻧﻤﻲ ﺷﻮﺩ. • ﺍﻟﺒﺘﻪ ﺑﺎ ﻭﺟﻮﺩ ﺑﺮﺧﻲ ﺍﺯ ﺑﻴﻤﺎﺭﻳﻬﺎ ﻭ ﻋﻮﺍﺭﺽ ﺩﺭ ﺣﺎﻣﻠگﻲ، ﺑﻬﺘﺮ ﺍﺳﺖ ﻣﺎﺩﺭ ﻓﻌﺎﻟﻴﺖ ﻧﺪﺍﺷﺘﻪ ﺑﺎﺷﺪ − − − ﺷک ﺑﻪ IUGR Toxemia Severe heart dx ﺩﻭﻗﻠﻮﻳﻲ ﻳﺎ چﻨﺪ ﻗﻠﻮﻳﻲ ROM Persistent vaginal bleeding
ﺍﺳﺘﺤﻤﺎﻡ • ﺩﻭﺵ گﺮﻓﺘﻦ ﺩﺭ ﻃﻮﻝ ﺣﺎﻣﻠگﻲ ﻣﺸﻜﻠﻲ ﺍﻳﺠﺎﺩ ﻧﻤﻲ ﻛﻨﺪ ﺍﻟﺒﺘﻪ ﺑﻬﺘﺮ ﺍﺳﺖ ﺍﺯ ﺣﻤﺎﻡ ﺩﺍﻍ پﺮﻫﻴﺰ ﻛﻨﻨﺪ. ﻣﻌﻤﻮﻻ ﺧﺎﻧﻢ ﻫﺎﻱ ﺣﺎﻣﻠﻪ ﺑﻴﺸﺘﺮ ﻋﺮﻕ ﻣﻲ ﻛﻨﻨﺪ ﻭ ﺗﺮﺷﺤﺎﺕ ﻭﺍژﻴﻨﺎﻝ ﺑﻴﺸﺘﺮﻱ ﺩﺍﺭﻧﺪ ﺑﻨﺎﺑﺮﺍﻳﻦ ﺣﻤﺎﻡ ﺭﻭﺯﺍﻧﻪ ﻧﻪ ﺗﻨﻬﺎ آﺮﺍﻡ ﺑﺨﺶ ﺍﺳﺖ، ﺑﻠﻜﻪ ﺍﺯﻋﻔﻮﻧﺖ ﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻧﻴﺰ ﺟﻠﻮگﻴﺮﻱ ﻣﻲ ﻛﻨﺪ. • ﺍﺯ ﺣﻤﺎﻡ ﻛﺮﺩﻥ ﺩﺭ ﻭﺍﻥ ﻳﺎ ﺣﻤﺎﻡ ﻫﺎﻱ ﻟﻐﺰﻧﺪﻩ ﻭ پﻮﺷﻴﺪﻥ ﺩﻣپﺎﻳﻲ ﻫﺎﻱ ﺍﺑﺮﻱ ﺩﺭ ﺣﻤﺎﻡ ﺧﻮﺩﺩﺍﺭﻱ ﺷﻮﺩ ﺯﻳﺮﺍ ﺍﺣﺘﻤﺎﻝ ﺑﻬﻢ ﺧﻮﺭﺩﻥ ﺗﻌﺎﺩﻝ ﻭ ﻟﻐﺰﻳﺪﻥ ﺯﻳﺎﺩ ﺍﺳﺖ.
ﻟﺒﺎﺱ • ﻟﺒﺎﺱ ﺩﻭﺭﻩ ﺑﺎﺭﺩﺍﺭﻱ ﺑﺎﻳﺪ آﺰﺍﺩ ﻭﺭﺍﺣﺖ ﺑﺎﺷﺪ، ﺑﺎﻳﺪ ﺍﺯ پﻮﺷﻴﺪﻥ ﺟﻮﺭﺍﺏ ﻫﺎﻱ ﺗﻨگ ﻭ ﻛﺸﺪﺍﺭ ﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻛﻤﺮﺑﻨﺪ ﺗﻨگ ﺧﻮﺩ ﺩﺍﺭﻱ ﻛﺮﺩ. ﺑﻬﺘﺮ ﺍﺳﺖ ﺩﺭ ﺍﻳﻦ ﺩﻭﺭﺍﻥ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﺍﺯﻛﻔﺶ ﻫﺎﻱ پﺎﺷﻨﻪ ﻛﻮﺗﺎﻩ ﺍﺳﺘﻔﺎﺩﻩ ﻛﻨﺪ.
ﻣﺮﺍﻗﺒﺖ ﺍﺯ ﺩﻧﺪﺍﻧﻬﺎ • • • • ﺗﻐﻴﻴﺮﺍﺕ ﻫﻮﺭﻣﻮﻧﻲ: ﺍﻓﺰﺍﻳﺶ ﺣﺠﻢ ﻟﺜﻪ ﻭ ﺣﺴﺎﺱ ﺷﺪﻥ ﻣﺨﺎﻁ ﺩﻫﺎﻥ ﺑﻪ ﻋﻮﺍﻣﻞ ﻣﺤﺮک ﻣﻮﺿﻌﻲ ﺍﺳﺘﻔﺮﺍﻍ) ﻭﻳﺎﺭ(: ﺗﺎﺛﻴﺮ ﻣﺨﺮﺏ ﺍﺳﻴﺪ ﺑﺮ ﺩﻧﺪﺍﻥ ﻋﺪﻡ ﺭﻋﺎﻳﺖ ﺑﻬﺪﺍﺷﺖ) ﻣﺴﻮﺍک( ﺑﻪ ﺧﺎﻃﺮ ﺑﻲ ﺣﻮﺻﻠگﻲ ﺍﻓﺰﺍﻳﺶ ﻋﻼﻗﻪ ﺑﻪ ﻣﺼﺮﻑ ﻣﻮﺍﺩ ﻗﻨﺪﻱ ﺑﺎﻳﺪ ﺍﺯ ﺧﻮﺭﺩﻥ ﺷﻴﺮﻳﻨﻲ، آﺐ ﻧﺒﺎﺕ ﻫﺎﻱ ﺳﻔﺖ ﻭ ﻧﻮﺷﺎﺑﻪ ﻫﺎﻱ ﺭﻧگﻲ ﺧﻮﺩﺩﺍﺭﻱ ﻛﺮﺩ. ﻫﻤچﻨﻴﻦ ﺩﺭ ﺿﻤﻦ ﺑﺎﻳﺪ ﺑﻌﺪ ﺍﺯ ﺧﻮﺭﺩﻥ ﻫﺮ ﻣﺎﺩﻩ ﻏﺬﺍﻳﻲ، ﺩﻫﺎﻥ ﺧﻮﺩ ﺭﺍ ﺷﺴﺖ ﻭ ﺩﻧﺪﺍﻥ ﻫﺎ ﺭﺍ ﻣﺴﻮﺍﻙ ﺯﺩ ﻭ ﺩﺭ ﺻﻮﺭﺕ ﻟﺰﻭﻡ ﺑﻪ ﺩﻧﺪﺍﻧپﺰﺷﻚ ﻣﺮﺍﺟﻌﻪ ﻛﺮﺩ. ﻣﻌﺎﻳﻨﻪ ﺩﻧﺪﺍﻥ ﻭﻟﺜﻪ ﺩﺭ ﻫﺮ ﺑﺎﺭ ﻣﻌﺎﻳﻨﻪ، آﻤﻮﺯﺵ ﺩﺭ ﻣﺎﻫﻬﺎﻱ 3 ﻭ 5 ﻭ 7 ﻣﺮﺍﺟﻌﻪ ﺑﻪ ﺩﻧﺪﺍﻧپﺰﺷکﻲ ﺗﺮﺟﻴﺤﺎ ﺩﺭ 3 ﻣﺎﻫﻪ ﺩﻭﻡ چﻮﻥ − ﻣﺎﻩ ﺍﻭﻝ : ﺍﺿﻄﺮﺍﺏ ﺍﻣکﺎﻥ ﺳﻘﻂ − ﻣﺎﻫﻬﺎﻱ آﺨﺮ: ﺍﺿﻄﺮﺍﺏ ﺯﺍﻳﻤﺎﻥ ﺯﻭﺩﺭﺱ
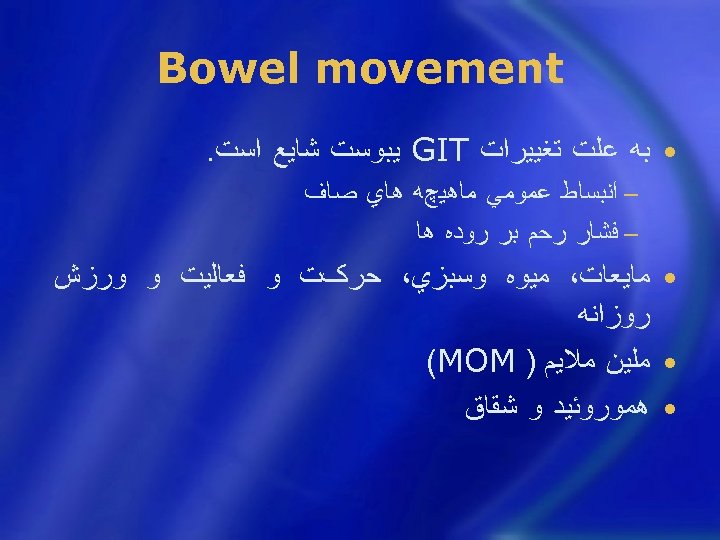
Bowel movement • ﺑﻪ ﻋﻠﺖ ﺗﻐﻴﻴﺮﺍﺕ GIT ﻳﺒﻮﺳﺖ ﺷﺎﻳﻊ ﺍﺳﺖ. − ﺍﻧﺒﺴﺎﻁ ﻋﻤﻮﻣﻲ ﻣﺎﻫﻴچﻪ ﻫﺎﻱ ﺻﺎﻑ − ﻓﺸﺎﺭ ﺭﺣﻢ ﺑﺮ ﺭﻭﺩﻩ ﻫﺎ • ﻣﺎﻳﻌﺎﺕ، ﻣﻴﻮﻩ ﻭﺳﺒﺰﻱ، ﺣﺮکﺖ ﻭ ﻓﻌﺎﻟﻴﺖ ﻭ ﻭﺭﺯﺵ ﺭﻭﺯﺍﻧﻪ • ﻣﻠﻴﻦ ﻣﻼﻳﻢ ) (MOM • ﻫﻤﻮﺭﻭﺋﻴﺪ ﻭ ﺷﻘﺎﻕ
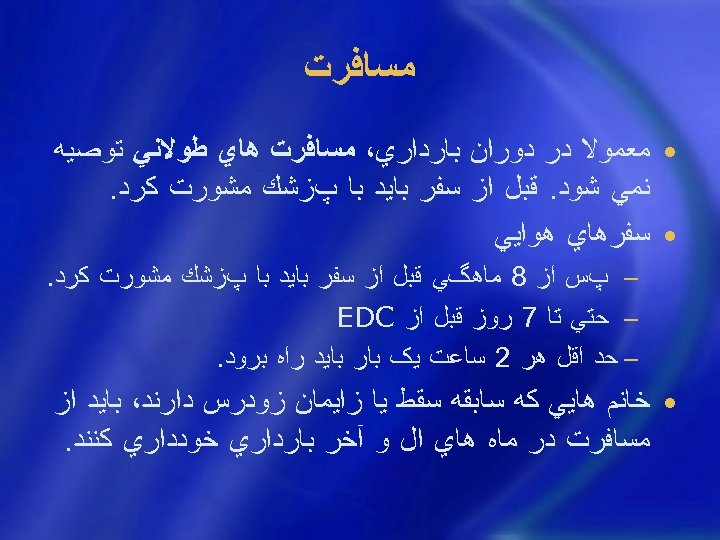
ﻣﺴﺎﻓﺮﺕ • ﻣﻌﻤﻮﻻ ﺩﺭ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ، ﻣﺴﺎﻓﺮﺕ ﻫﺎﻱ ﻃﻮﻻﻧﻲ ﺗﻮﺻﻴﻪ ﻧﻤﻲ ﺷﻮﺩ. ﻗﺒﻞ ﺍﺯ ﺳﻔﺮ ﺑﺎﻳﺪ ﺑﺎ پﺰﺷﻚ ﻣﺸﻮﺭﺕ ﻛﺮﺩ. • ﺳﻔﺮﻫﺎﻱ ﻫﻮﺍﻳﻲ − پﺲ ﺍﺯ 8 ﻣﺎﻫگﻲ ﻗﺒﻞ ﺍﺯ ﺳﻔﺮ ﺑﺎﻳﺪ ﺑﺎ پﺰﺷﻚ ﻣﺸﻮﺭﺕ ﻛﺮﺩ. − ﺣﺘﻲ ﺗﺎ 7 ﺭﻭﺯ ﻗﺒﻞ ﺍﺯ EDC − ﺣﺪ ﺍﻗﻞ ﻫﺮ 2 ﺳﺎﻋﺖ ﻳک ﺑﺎﺭ ﺑﺎﻳﺪ ﺭﺍﻩ ﺑﺮﻭﺩ. • ﺧﺎﻧﻢ ﻫﺎﻳﻲ ﻛﻪ ﺳﺎﺑﻘﻪ ﺳﻘﻂ ﻳﺎ ﺯﺍﻳﻤﺎﻥ ﺯﻭﺩﺭﺱ ﺩﺍﺭﻧﺪ، ﺑﺎﻳﺪ ﺍﺯ ﻣﺴﺎﻓﺮﺕ ﺩﺭ ﻣﺎﻩ ﻫﺎﻱ ﺍﻝ ﻭ آﺨﺮ ﺑﺎﺭﺩﺍﺭﻱ ﺧﻮﺩﺩﺍﺭﻱ ﻛﻨﻨﺪ.
When is the best time to travel during pregnancy?
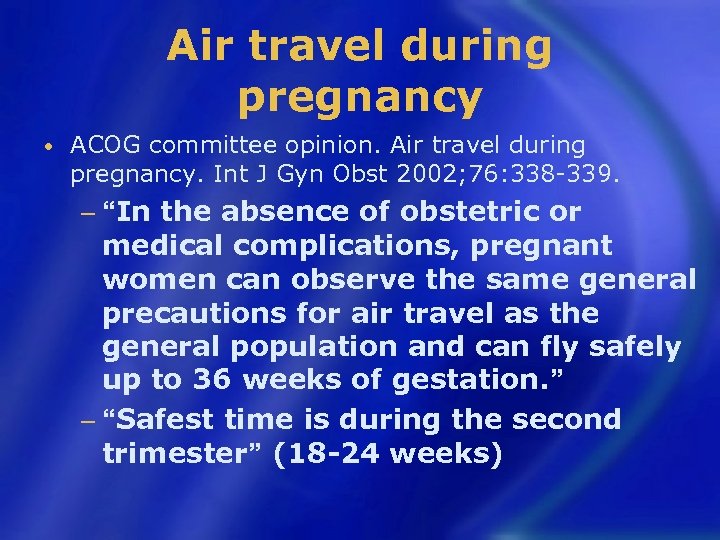
Air travel during pregnancy • ACOG committee opinion. Air travel during pregnancy. Int J Gyn Obst 2002; 76: 338 -339. the absence of obstetric or medical complications, pregnant women can observe the same general precautions for air travel as the general population and can fly safely up to 36 weeks of gestation. ” − “Safest time is during the second trimester” (18 -24 weeks) − “In
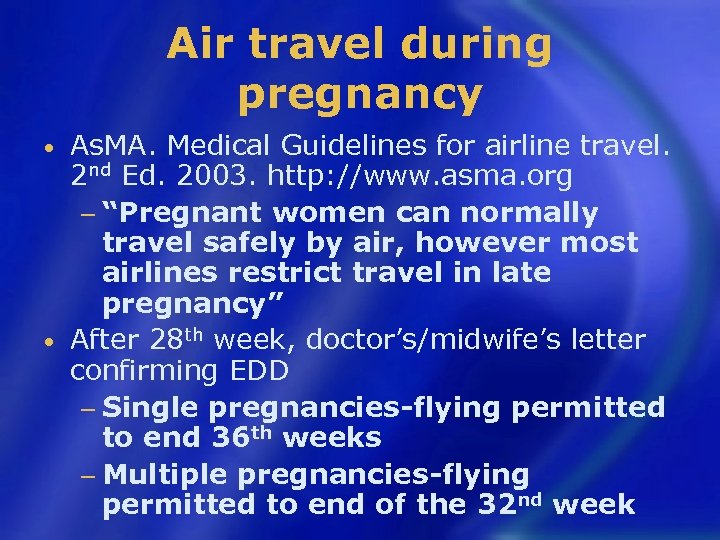
Air travel during pregnancy As. MA. Medical Guidelines for airline travel. 2 nd Ed. 2003. http: //www. asma. org − “Pregnant women can normally travel safely by air, however most airlines restrict travel in late pregnancy” • After 28 th week, doctor’s/midwife’s letter confirming EDD − Single pregnancies-flying permitted to end 36 th weeks − Multiple pregnancies-flying permitted to end of the 32 nd week •
What do airlines actually recommend? Some clues given in “Airborn” study
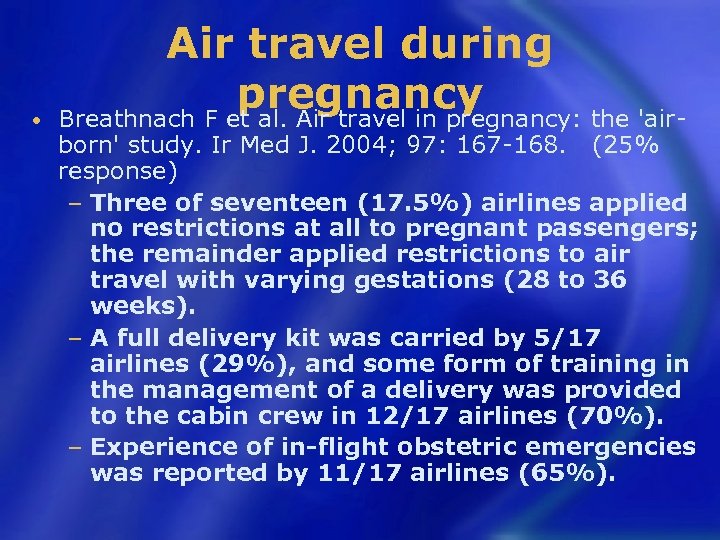
• Air travel during pregnancy Breathnach F et al. Air travel in pregnancy: the 'air- born' study. Ir Med J. 2004; 97: 167 -168. (25% response) − Three of seventeen (17. 5%) airlines applied no restrictions at all to pregnant passengers; the remainder applied restrictions to air travel with varying gestations (28 to 36 weeks). − A full delivery kit was carried by 5/17 airlines (29%), and some form of training in the management of a delivery was provided to the cabin crew in 12/17 airlines (70%). − Experience of in-flight obstetric emergencies was reported by 11/17 airlines (65%).
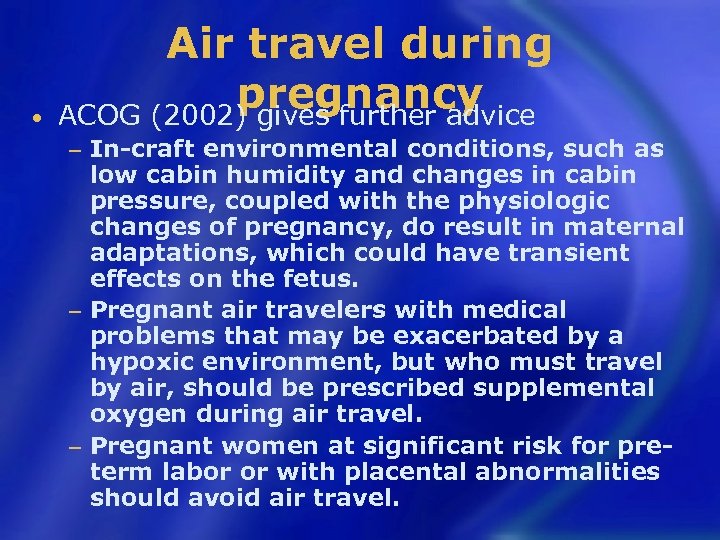
• Air travel during pregnancy ACOG (2002) gives further advice In-craft environmental conditions, such as low cabin humidity and changes in cabin pressure, coupled with the physiologic changes of pregnancy, do result in maternal adaptations, which could have transient effects on the fetus. − Pregnant air travelers with medical problems that may be exacerbated by a hypoxic environment, but who must travel by air, should be prescribed supplemental oxygen during air travel. − Pregnant women at significant risk for preterm labor or with placental abnormalities should avoid air travel. −
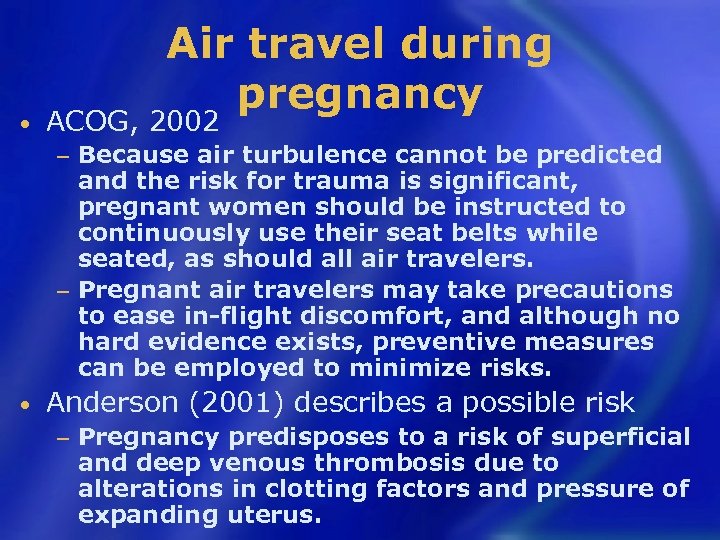
• Air travel during pregnancy ACOG, 2002 Because air turbulence cannot be predicted and the risk for trauma is significant, pregnant women should be instructed to continuously use their seat belts while seated, as should all air travelers. − Pregnant air travelers may take precautions to ease in-flight discomfort, and although no hard evidence exists, preventive measures can be employed to minimize risks. − • Anderson (2001) describes a possible risk − Pregnancy predisposes to a risk of superficial and deep venous thrombosis due to alterations in clotting factors and pressure of expanding uterus.
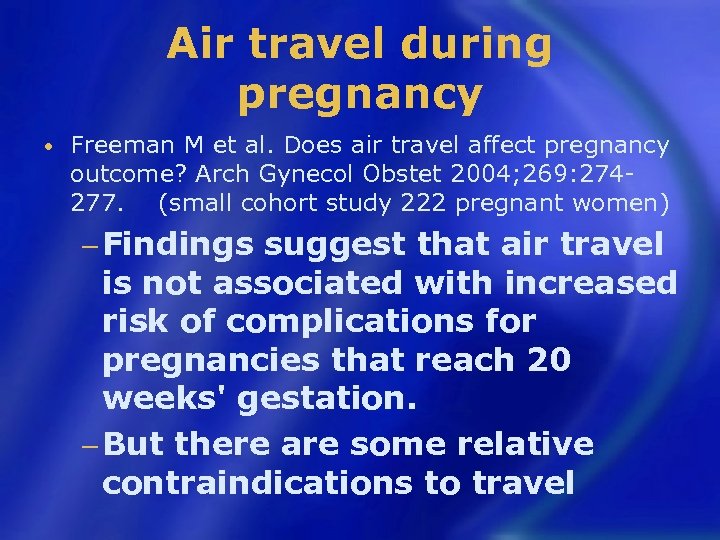
Air travel during pregnancy • Freeman M et al. Does air travel affect pregnancy outcome? Arch Gynecol Obstet 2004; 269: 274277. (small cohort study 222 pregnant women) − Findings suggest that air travel is not associated with increased risk of complications for pregnancies that reach 20 weeks' gestation. − But there are some relative contraindications to travel
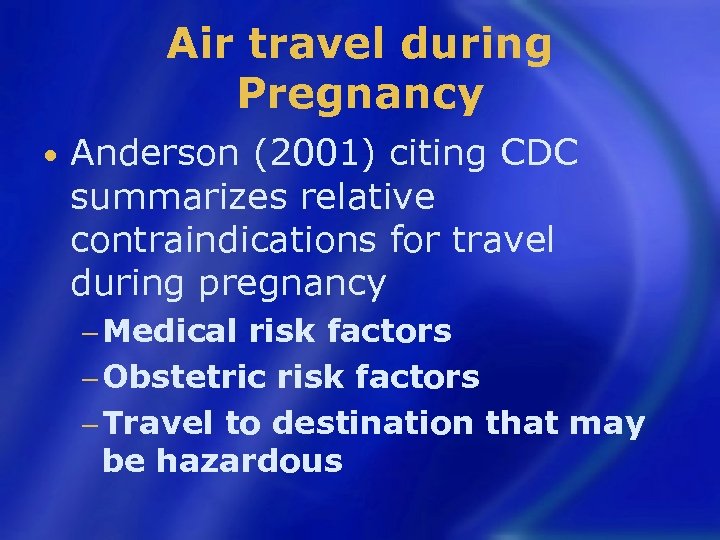
Air travel during Pregnancy • Anderson (2001) citing CDC summarizes relative contraindications for travel during pregnancy − Medical risk factors − Obstetric risk factors − Travel to destination that may be hazardous
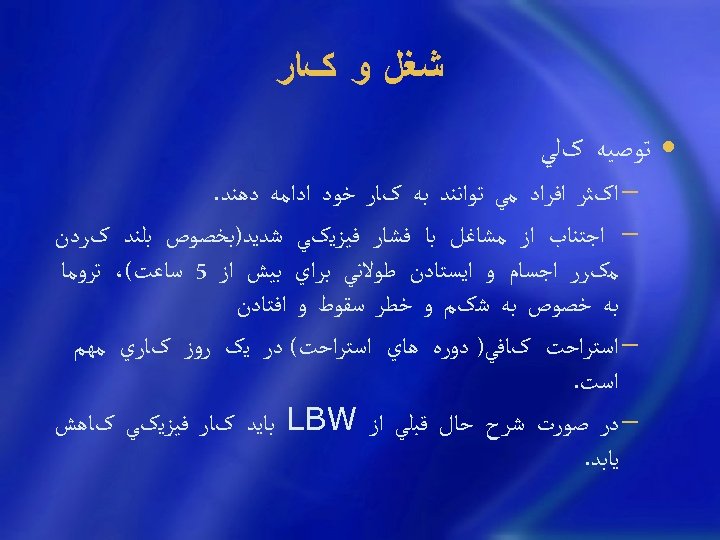
ﺷﻐﻞ ﻭ کﺎﺭ • ﺗﻮﺻﻴﻪ کﻠﻲ − ﺍکﺜﺮ ﺍﻓﺮﺍﺩ ﻣﻲ ﺗﻮﺍﻧﻨﺪ ﺑﻪ کﺎﺭ ﺧﻮﺩ ﺍﺩﺍﻣﻪ ﺩﻫﻨﺪ. − ﺍﺟﺘﻨﺎﺏ ﺍﺯ ﻣﺸﺎﻏﻞ ﺑﺎ ﻓﺸﺎﺭ ﻓﻴﺰﻳکﻲ ﺷﺪﻳﺪ)ﺑﺨﺼﻮﺹ ﺑﻠﻨﺪ کﺮﺩﻥ ﻣکﺮﺭ ﺍﺟﺴﺎﻡ ﻭ ﺍﻳﺴﺘﺎﺩﻥ ﻃﻮﻻﻧﻲ ﺑﺮﺍﻱ ﺑﻴﺶ ﺍﺯ 5 ﺳﺎﻋﺖ(، ﺗﺮﻭﻣﺎ ﺑﻪ ﺧﺼﻮﺹ ﺑﻪ ﺷکﻢ ﻭ ﺧﻄﺮ ﺳﻘﻮﻁ ﻭ ﺍﻓﺘﺎﺩﻥ − ﺍﺳﺘﺮﺍﺣﺖ کﺎﻓﻲ) ﺩﻭﺭﻩ ﻫﺎﻱ ﺍﺳﺘﺮﺍﺣﺖ( ﺩﺭ ﻳک ﺭﻭﺯ کﺎﺭﻱ ﻣﻬﻢ ﺍﺳﺖ. − ﺩﺭ ﺻﻮﺭﺕ ﺷﺮﺡ ﺣﺎﻝ ﻗﺒﻠﻲ ﺍﺯ LBW ﺑﺎﻳﺪ کﺎﺭ ﻓﻴﺰﻳکﻲ کﺎﻫﺶ ﻳﺎﺑﺪ.
ﺳﻴگﺎﺭ ﻭ ﺍﻟکﻞ • ﻣﺎﺩﺭﺍﻧﻲ ﻛﻪ ﺩﺭ ﻃﻮﻝ ﺑﺎﺭﺩﺍﺭﻱ ﺳﻴگﺎﺭ ﻣﻲ ﻛﺸﻨﺪ ﺩﺭ ﻣﻘﺎﻳﺴﻪ ﺑﺎ ﻏﻴﺮﺳﻴگﺎﺭﻱ ﻫﺎ، ﺍﻓﺰﺍﻳﺶ ﻭﺯﻥ کﻤﺘﺮﻱ ﺩﺍﺷﺘﻪ ﻭﻧﻮﺯﺍﺩﺍﻥ ﻛﻮچﻜﺘﺮﻱ ﺑﻪ ﺩﻧﻴﺎ ﻣﻲ آﻮﺭﻧﺪ. ﻣﺼﺮﻑ ﺳﻴگﺎﺭ ﻭ ﻣﻮﺍﺩ ﻣﺨﺪﺭ ﺑﺮﺍﻱ ﺟﻨﻴﻦ ﻣﻀﺮ ﺍﺳﺖ ﻭﺧﺎﻧﻢ ﻫﺎﻱ ﺑﺎﺭﺩﺍﺭ ﺑﺎﻳﺪ ﺑﻪ ﻃﻮﺭﻛﺎﻣﻞ ﺍﺯ ﻛﺸﻴﺪﻥ ﺳﻴگﺎﺭ پﺮﻫﻴﺰ ﻛﻨﻨﺪ. ﺯﺍﻳﻤﺎﻥ ﺯﻭﺩﺭﺱ − ﻧﻴکﻮﺗﻴﻦ: ﻧﺎﺭﺳﺎﻳﻲ ﺟﻔﺖ ﻭ ﺍﻧﻘﺒﺎﺽ ﻋﺮﻭﻕ ﺭﺣﻢ − Fetal limb deficiency • ﻣﺼﺮﻑ ﺍﻟﻜﻞ ﺗﻮﺳﻂ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﺩﺭ ﺟﻨﻴﻦ ﺍﻳﺠﺎﺩ ﻧﺎﻫﻨﺠﺎﺭﻱ ﻣﻲ ﻛﻨﺪ. ﺯﺍﻳﻤﺎﻥ ﺯﻭﺩﺭﺱ ﺩﺭﺧﺎﻧﻢ ﻫﺎﻳﻲ ﻛﻪ ﺍﻟﻜﻞ ﻣﺼﺮﻑ ﻣﻲ ﻛﻨﻨﺪ ﺑﻴﺸﺘﺮ ﻣﺸﺎﻫﺪﻩ ﻣﻲ ﺷﻮﺩ. • ﺧﺎﻧﻢ ﻫﺎﻱ ﺑﺎﺭﺩﺍﺭ ﺑﺎﻳﺪ ﻗﺒﻞ ﺍﺯ ﻣﺼﺮﻑ ﻫﺮﻧﻮﻉ ﺩﺍﺭﻭ ﺑﺎ پﺰﺷﻚ ﻣﺸﻮﺭﺕ
کﺎﻓﺌﻴﻦ) چﺎﻱ ﻗﻬﻮﻩ ﺷکﻼﺕ کﻮﻻ( • ﻣﺼﺮﻑ ﺩﺭ ﺣﺎﻣﻠگﻲ ﻣﺤﺪﻭﺩ ﺷﻮﺩ. • ﻣﻄﺎﻟﻌﺎﺕ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺩﺭ ﻣﻘﺪﺍﺭ کﻢ ﻣﺪﺭکﻲ ﺩﺍﻝ ﺑﺮ ﺗﺮﺍﺗﻮژﻦ ﺑﻮﺩﻥ ﻭﺟﻮﺩ ﻧﺪﺍﺭﺩ ﺍﻣﺎ ﺩﺭ ﺣﻴﻮﺍﻧﺎﺕ ﺗﺮﺍﺗﻮژﻦ ﺍﺳﺖ کﻪ ﺑﺎ ﺩﻭﺯﻫﺎﻱ ﺯﻳﺎﺩ ﺑﻮﺩﻩ ﺍﺳﺖ. • ﻣﺼﺮﻑ ﺑﻴﺶ ﺍﺯ 3 cups ﺩﺭ ﺭﻭﺯ − ﺍﻓﺰﺍﻳﺶ miscarriage
ﺩﺍﺭﻭﻫﺎﻱ ﻏﻴﺮ ﻣﺠﺎﺯ ﻭ ﻣﻮﺍﺩ ﻣﺨﺪﺭ • • • • • ﺍﻓﺰﺍﻳﺶ LBW, fetal distress ﺑﻪ ﺟﺰ ﻣﻮﺍﺭﺩ ﻧﺎﺩﺭ ﻫﺮ ﺩﺍﺭﻭﻳﻲ کﻪ ﺍﺛﺮ ﺳﻴﺴﺘﻤﻴک ﺩﺭ ﻣﺎﺩﺭ ﺩﺍﺷﺘﻪ ﺑﺎﺷﺪ ﺍﺯ ﺟﻔﺖ ﺭﺩ ﺷﺪﻩ ﻭ ﺑﻪ ﺟﻨﻴﻦ ﻣﻲ ﺭﺳﺪ. ﻃﺒﻘﻪ ﺑﻨﺪﻱ FDA ﺩﺭ ﻣﻮﺭﺩ ﻣﺼﺮﻑ ﺩﺍﺭﻭ ﺩﺭ ﺣﺎﻣﻠگﻲ ﻭ ﺷﻴﺮ ﺩﻫﻲ) A B C (D X ﺍﺳﺘﺮپﺘﻮﻣﺎﻳﺴﻴﻦ، آﺴﻴﺐ ﺑﻪ ﻋﺼﺐ 8 ﻭ کﺮﻱ ﺍﺳﺘﺮﻭﺋﻴﺪﻫﺎ، ﻧﺎﺭﺳﺎﻳﻲ ﺩﺭ ﺭﺷﺪ ﺟﻨﻴﻦ ﻓﺮﺍﻭﺭﺩﻩ ﻫﺎﻱ ﻳﺪ ﺩﺍﺭ، گﻮﺍﺗﺮ ﻣﺎﺩﺭﺯﺍﺩﻱ ﻫﻮﺭﻣﻮﻧﻬﺎﻱ ﺟﻨﺴﻲ، virilism ﺗﺘﺮﺍﺳﺎﻳکﻠﻴﻦ، ﺍﺧﺘﻼﻝ ﺩﺭ ﺭﺷﺪ ﺍﺳﺘﺨﻮﺍﻧﻬﺎ ﻭ ﺗﺸکﻴﻞ ﻣﻴﻨﺎﻱ ﺩﻧﺪﺍﻥ ﺗﺎﻟﻴﺪﻭﻣﻴﺪ، ﺩﺍﺭﻭﻫﺎﻱ ﺧﻮﺍﺏ آﻮﺭ ﻏﻴﺮ ﺑﺎﺭﺑﻴﺘﻮﺭﻳک، ﺗﻐﻴﻴﺮ ﺷکﻞ ﺩﺳﺖ ﻭ پﺎﻱ ﻧﻮﺯﺍﺩ ، LSD ﺿﺎﻳﻌﻪ کﺮﻭﻣﻮﺯﻭﻣﻲ
What about vaccination during pregnancy?
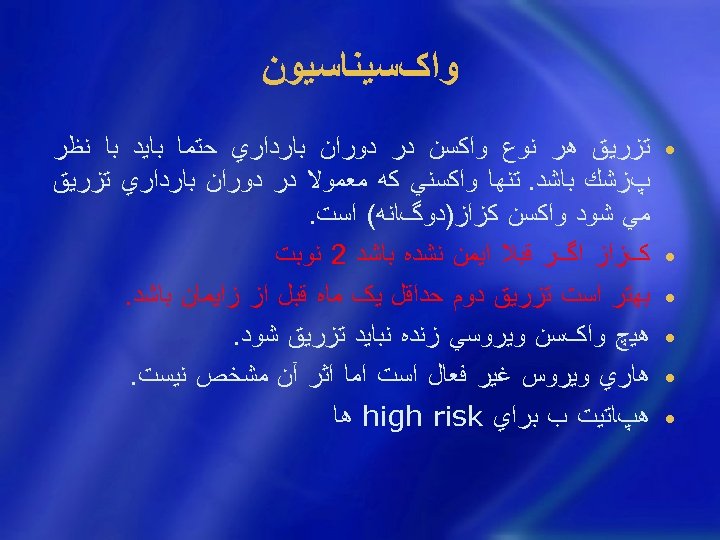
ﻭﺍکﺴﻴﻨﺎﺳﻴﻮﻥ • • • ﺗﺰﺭﻳﻖ ﻫﺮ ﻧﻮﻉ ﻭﺍﻛﺴﻦ ﺩﺭ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ ﺣﺘﻤﺎ ﺑﺎﻳﺪ ﺑﺎ ﻧﻈﺮ پﺰﺷﻚ ﺑﺎﺷﺪ. ﺗﻨﻬﺎ ﻭﺍﻛﺴﻨﻲ ﻛﻪ ﻣﻌﻤﻮﻻ ﺩﺭ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ ﺗﺰﺭﻳﻖ ﻣﻲ ﺷﻮﺩ ﻭﺍﻛﺴﻦ ﻛﺰﺍﺯ)ﺩﻭگﺎﻧﻪ( ﺍﺳﺖ. کﺰﺍﺯ ﺍگﺮ ﻗﺒﻼ ﺍﻳﻤﻦ ﻧﺸﺪﻩ ﺑﺎﺷﺪ 2 ﻧﻮﺑﺖ ﺑﻬﺘﺮ ﺍﺳﺖ ﺗﺰﺭﻳﻖ ﺩﻭﻡ ﺣﺪﺍﻗﻞ ﻳک ﻣﺎﻩ ﻗﺒﻞ ﺍﺯ ﺯﺍﻳﻤﺎﻥ ﺑﺎﺷﺪ. ﻫﻴچ ﻭﺍکﺴﻦ ﻭﻳﺮﻭﺳﻲ ﺯﻧﺪﻩ ﻧﺒﺎﻳﺪ ﺗﺰﺭﻳﻖ ﺷﻮﺩ. ﻫﺎﺭﻱ ﻭﻳﺮﻭﺱ ﻏﻴﺮ ﻓﻌﺎﻝ ﺍﺳﺖ ﺍﻣﺎ ﺍﺛﺮ آﻦ ﻣﺸﺨﺺ ﻧﻴﺴﺖ. ﻫپﺎﺗﻴﺖ ﺏ ﺑﺮﺍﻱ high risk ﻫﺎ
“Pregnancy should not deter a women from receiving vaccines that are safe and will protect her health and that of her child. ”
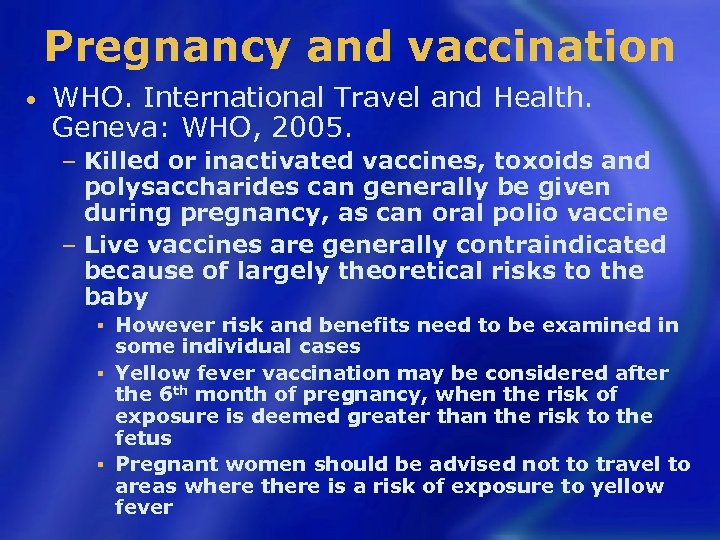
Pregnancy and vaccination • WHO. International Travel and Health. Geneva: WHO, 2005. Killed or inactivated vaccines, toxoids and polysaccharides can generally be given during pregnancy, as can oral polio vaccine − Live vaccines are generally contraindicated because of largely theoretical risks to the baby − However risk and benefits need to be examined in some individual cases § Yellow fever vaccination may be considered after the 6 th month of pregnancy, when the risk of exposure is deemed greater than the risk to the fetus § Pregnant women should be advised not to travel to areas where there is a risk of exposure to yellow fever §
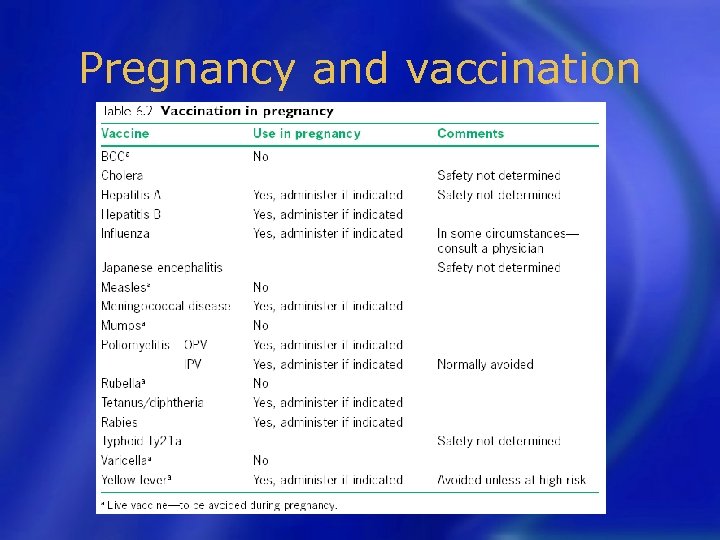
Pregnancy and vaccination
پﺮﺗﻮﻫﺎ • • ﺗﺎﺛﻴﺮ ﺍﺷﻌﻪ ﺑﺮ ﺟﻨﻴﻦ ﻭﺍﺑﺴﺘﻪ ﺑﻪ ﺩﻭﺯ ﺍﺳﺖ. ﺩﺭﻳﺎﻓﺖ ﻫﺮﻧﻮﻉ ﺍﺷﻌﻪ )ﻣﺜﻞ ﻋﻜﺴﺒﺮﺩﺍﺭﻱ ﺑﺎﺍﺷﻌﻪ ﺍﻳﻜﺲ( ﺩﺭ ﺣﺎﻣﻠگﻲ ﻣﻤﻨﻮﻉ ﺍﺳﺖ ﺧﺼﻮﺻﺎ ﺩﺭ 3 ﻣﺎﻫﻪ ﺍﻭﻝ ﺯﻳﺮﺍ ﺍﺣﺘﻤﺎﻝ ﺍﻳﺠﺎﺩ ﻧﺎﻫﻨﺠﺎﺭﻱ ﺩﺭ ﺟﻨﻴﻦ ﺭﺍ ﺍﻓﺰﺍﻳﺶ ﻣﻲ ﺩﻫﺪ. ﻋکﺴﺒﺮﺩﺍﺭﻱ ﺩﻧﺪﺍﻥ ﺑﺎ ﻣﺤﺎﻓﻆ ﺳﺮﺑﻲ ﺭﻭﻱ ﺷکﻢ ﺧﻮﺩﺩﺍﺭﻱ ﺍﺯ ﻋکﺴﺒﺮﺩﺍﺭﻱ ﻣﺘﻌﺪﺩ ﻭ پﺸﺖ ﺳﺮﻫﻢ
ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻋﻔﻮﻧﻲ • ﺗﻤﺎﺱ ﺑﺎ ﺣﻴﻮﺍﻧﺎﺕ ﻭ ﻋﻮﺍﻣﻞ ﺑﻴﻤﺎﺭﻳﺰﺍ ﺑﺮﺧﻲ ﺍﺯ ﺣﻴﻮﺍﻧﺎﺕ ﺍﻫﻠﻲ ﻣﺎﻧﻨﺪ گﺮﺑﻪ ﻣﻨﺘﻘﻞ ﻛﻨﻨﺪﻩ ﺑﻴﻤﺎﺭﻱ ﻫﺎﻳﻲ ﻫﺴﺘﻨﺪ ﻛﻪ ﺑﺮ ﺭﻭﻱ ﺑﺎﺭﺩﺍﺭﻱ ﻭ ﺟﻨﻴﻦ ﺍﺛﺮ ﺑﺪﻱ ﻣﻲ گﺬﺍﺭﻧﺪ. ﺍﻧﺘﻘﺎﻝ ﻋﻔﻮﻧﺖ ﺍﺯ گــﺮﺑﻪ ﺑﻪ ﺧﺎﻧــﻢ ﺑﺎﺭﺩﺍﺭ )ﺗﻮﻛﺴﻮپﻼﺳﻤﻮﺯ( ﻣﻌﻤﻮﻻ ﻣﻨﺠﺮ ﺑﻪ ﺳﻘﻂ ﺟﻨﻴﻦ ﻣﻲ ﺷﻮﺩ. ﺩﺭﺻﻮﺭﺕ ﺑﺎﻗﻲ ﻣﺎﻧﺪﻥ ﺟﻨﻴﻦ ﻧﻴﺰ، ﻧﺎﻫﻨﺠﺎﺭﻱ ﻫﺎﻳﻲ ﺍﺯ ﻗﺒﻴﻞ ﺍﺷﻜﺎﻻﺕ ﻣﻐﺰﻱ، ﻋﻘﺐ ﻣﺎﻧﺪگﻲ ﺫﻫﻨﻲ ﻭ ﻏﻴﺮﻩ ﺍﻳﺠﺎﺩ ﺧﻮﺍﻫﺪ ﺷﺪ. ﺑﻨﺎﺑﺮﺍﻳﻦ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﺟﺪ ﺑﺎﻳﺪ ﺍﺯ ﺗﻤﺎﺱ ﺑﺎ ﺣﻴﻮﺍﻧﺎﺕ ﺧﻮﺩﺩﺍﺭﻱ ﻛﻨﺪ. • ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﺑﺎﻳﺪ ﺍﺯ ﺗﻤﺎﺱ ﺑﺎ ﺍﻓﺮﺍﺩ ﻣﺒﺘﻼ ﺑﻪ ﺑﻴﻤﺎﺭﻱ ﻫﺎﻱ ﻋﻔﻮﻧﻲ، ﺭﻓﺖ ﻭ آﻤﺪ ﺩﺭ ﺍﻣﺎﻛﻦ ﻋﻤﻮﻣﻲ، ﺷﻠﻮﻍ، ﺳﺮﺑﺴﺘﻪ ﻭ ﻣﻜﺎﻥ ﻫﺎﻳﻲ ﻛﻪ ﺍﺣﺘﻤﺎﻝ آﻠﻮﺩگﻲ ﻭﺟﻮﺩ ﺩﺍﺭﺩ، ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻣﻮﺍﺩ ﻏﺬﺍﻳﻲ ﺗﻬﻴﻪ ﺷﺪﻩ ﺩﺭ ﺧﺎﺭﺝ ﺍﺯ ﻣﻨﺰﻝ، ﺧﻮﺩﺩﺍﺭﻱ ﻛﻨﺪ.
ﺭﻭﺍﺑﻂ ﺟﻨﺴﻲ) (coitus • ﻳﻚ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﺳﺎﻟﻢ ﻣﻲ ﺗﻮﺍﻧﺪ ﺭﻭﺍﺑﻂ ﺟﻨﺴﻲ ﺧﻮﺩ ﺭﺍ ﺍﺩﺍﻣﻪ ﺩﻫﺪ ﻓﻘﻂ ﺩﺭ ﻣﻮﺍﺭﺩﻱ ﻛﻪ ﺧﻄﺮ ﺳﻘﻂ، ﺯﺍﻳﻤﺎﻥ ﺯﻭﺩﺭﺱ ﻭ پﺎﺭگﻲ ﻛﻴﺴﻪ آﺐ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﺍﺯ ﻣﻘﺎﺭﺑﺖ ﺑﻬﺘﺮ ﺍﺳﺖ ﺍﺟﺘﻨﺎﺏ ﻛﻨﺪ. • ﺟﻔﺖ ﺳﺮ ﺭﺍﻫﻲ ﻭ ﺑﻌﺪ ﺍﺯ پﺎﺭگﻲ کﻴﺴﻪ آﺐ ﻧﺒﺎﻳﺪ ﻣﻘﺎﺭﺑﺖ ﺑﺎﺷﺪ. • ﺍﻟﺒﺘﻪ ﺑﻄﻮﺭﻛﻠﻲ ﺗﻮﺻﻴﻪ ﻣﻲ ﺷﻮﺩ ﺩﺭﻣﺎﻩ آﺨﺮ ﺣﺎﻣﻠگﻲ ﺭﻭﺍﺑﻂ ﺯﻧﺎﺷﻮﻳﻲ ﻣﺤﺪﻭﺩ ﺷﻮﺩ.
ﺷﻜﺎﻳﺎﺕ ﺷﺎﻳﻊ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ • • • • • ﻭﻳﺎﺭ ﺳﻮﺯﺵ ﺳﺮ ﺩﻝ ﺿﻌﻒ ﻭ ﺳﺮگﻴﺠﻪ ﺗﻨگﻲ ﻧﻔﺲ ﻭﺭﻡ گﺮﻓﺘگﻲ پﺎﻫﺎ ﺗﻜﺮﺭﺍﺩﺭﺍﺭ ﻳﺒﻮﺳﺖ ﺑﻮﺍﺳﻴﺮ ﻭﺍﺭﻳﺲ
ﻭﻳﺎﺭ • • ﺣﺴﺎﺱ ﺷﺪﻥ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﻧﺴﺒﺖ ﺑﻪ ﺑﺮﺧﻲ ﺑﻮﻫﺎ ﻭ ﻳﺎ ﺗﻤﺎﻳﻞ ﺑﻪ ﺧﻮﺭﺩﻥ ﺑﻌﻀﻲ ﺍﺯ ﻣﻮﺍﺩ ﻏﺬﺍﻳﻲ. ﻋﻠﺖ آﻦ ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ ﻛﺎﻣﻼ ﻣﺸﺨﺺ ﻧﻴﺴﺖ. ﺩﺭ ﺯﻧﺎﻧﻲ ﻛﻪ ﺭژﻴﻢ ﻏﺬﺍﻳﻲ ﻣﻨﺎﺳﺒﻲ ﺩﺍﺭﻧﺪ ﻭ ﺍﺯ ﻧﻈﺮ ﻭﺿﻊ ﺭﻭﺣﻲ ﺩﺭ ﺷﺮﺍﻳﻂ ﺧﻮﺑﻲ ﻫﺴﺘﻨﺪ،ﻛﻤﺘﺮ ﺩﻳﺪﻩ ﻣﻲ ﺷﻮﺩ. ﺗﻬﻮﻉ ﻭ ﺍﺳﺘﻔﺮﺍﻍ ﻧﺎﺷﻲ ﺍﺯ ﻭﻳﺎﺭ ﺩﺭ ﻧﻴﻤﻪ ﺍﻝ ﺣﺎﻣﻠگﻲ ﺷﺎﻳﻊ ﺍﺳﺖ ﻭ ﺳپﺲ ﺑﻪ ﺗﺪﺭﻳﺞ ﺑﺎ پﻴﺸﺮﻓﺖ ﺑﺎﺭﺩﺍﺭﻱ ﺍﺯ ﺷﺪﺕ آﻦ ﻛﺎﺳﺘﻪ ﺷﺪﻩ ﻭ ﺑﻬﺒﻮﺩ ﻣﻲ ﻳﺎﺑﺪ. ﺍﻳﻦ ﺣﺎﻟﺖ ﺻﺒﺢ ﻫﺎ ﺷﺪﻳﺪﺗﺮ ﺍﺳﺖ ﻭﻟﻲ ﻣﻤﻜﻦ ﺍﺳﺖ ﺩﺭ ﻃﻮﻝ ﺭﻭﺯ ﺍﺩﺍﻣﻪ ﺩﺍﺷﺘﻪ ﺑﺎﺷﺪ. ﺑﺮﺍﻱ پﻴﺸگﻴﺮﻱ ﻭ ﺑﻬﺒﻮﺩ، ﺑﻬﺘﺮ ﺍﺳﺖ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﻧﻴﻢ ﺳﺎﻋﺖ ﻗﺒﻞ ﺍﺯ ﺑﻠﻨﺪ ﺷﺪﻥ ﺍﺯ ﺭﺧﺘﺨﻮﺍﺏ، ﻳﻚ ﺗﻜﻪ ﻧﺎﻥ ﺑﺮﺷﺘﻪ ﻣﺼﺮﻑ ﻛﻨﺪ ﻭ ﺑﻪ آﻬﺴﺘگﻲ ﻓﻌﺎﻟﻴﺖ ﺧﻮﺩ ﺭﺍ آﻐﺎﺯ ﻧﻤﺎﻳﺪ. ﻏﺬﺍﻫﺎﻱ ﺭﻭﺯﺍﻧﻪ ﺭﺍ ﺩﺭ ﻭﻋﺪﻩ ﻫﺎﻱ ﺑﻴﺸﺘﺮ ﻭ ﺑﺎ ﺣﺠﻢ ﻛﻤﺘﺮ ﺑﺨﻮﺭﺩ. ﺍﺯ ﺧﻮﺭﺩﻥ ﻏﺬﺍﻫﺎﻱ چﺮﺏ ﺳﺮﺥ ﻛﺮﺩﻩ ﻭ پﺮﺍﺩﻭﻳﻪ پﺮﻫﻴﺰ ﻛﻨﺪ. ﻧﻮﺷﻴﺪﻥ ﻣﺎﻳﻌﺎﺕ ﺧﻨﻚ ﺑﻴﻦ ﻭﻋﺪﻩ ﻫﺎﻱ ﻏﺬﺍ )ﻭ ﻧﻪ ﻫﻤﺮﺍﻩ ﻏﺬﺍ ( ﺗﻮﺻﻴﻪ ﻣﻲ ﺷﻮﺩ.
pica • ﻧﺸﺎﺳﺘﻪ، گچ، ﻳﺦ، dirt, clay • ﺩﺭ low SES ﺑﻴﺸﺘﺮ ﺩﻳﺪﻩ ﻣﻲ ﺷﻮﺩ. • ﺷﺎﻳﺪ ﻧﺸﺎﻧﻪ severe IDA ﺑﺎﺷﺪ )ﺍﻣﺎ ﻧﻪ ﻫﻤﻴﺸﻪ(
ﺳﻮﺯﺵ ﺳﺮ ﺩﻝ • ﺍﻏﻠﺐ ﺑﻪ ﻋﻠﺖ ﻓﺸﺎﺭ ﺭﺣﻢ ﺑﺰﺭگ ﺷﺪﻩ ﺑﺮ ﺭﻭﻱ ﻣﻌﺪﻩ ﻭ ﺑﺮگﺸﺖ ﻣﺤﺘﻮﻳﺎﺕ ﻣﻌﺪﻩ ﺍﻳﺠﺎﺩ ﻣﻲ ﺷﻮﺩ. ﻣﺼﺮﻑ ﻏﺬﺍﻱ ﻛﻢ ﺣﺠﻢ، ﺩﺭ ﻭﻋﺪﻩ ﻫﺎﻱ ﺑﻴﺸﺘﺮ ﻣﻮﺟﺐ ﺑﻬﺒﻮﺩ ﺍﻳﻦ ﺣﺎﻟﺖ ﻣﻲ ﺷﻮﺩ. ﺑﻬﺘﺮ ﺍﺳﺖ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﺩﺭ ﻣﻮﻗﻊ ﺧﻮﺍﺏ چﻨﺪ ﺑﺎﻟﺶ ﺯﻳﺮ ﺳﺮ ﺑگﺬﺍﺭﻧﺪ ﺗﺎ ﺳﺮ ﻭ ﺳﻴﻨﻪ ﺑﺎﻻﺗﺮ ﺍﺯ ﻣﻌﺪﻩ ﻗﺮﺍﺭ گﻴﺮﺩ. • آﻨﺘﻲ ﺍﺳﻴﺪ) (Al Mg , MOM ﻣﺮﺟﺢ ﺍﺳﺖ ﺑﻪ ﺳﺪﻳﻢ ﺑﻴکﺮﺏ) ﺧﻄﺮ ﺍﺩﻡ(
ﺿﻌﻒ ﻭ ﺳﺮگﻴﺠﻪ • ﻏﺎﻟﺒ ﺑﻪ ﺩﻟﻴﻞ ﺍﻓﺖ ﻓﺸﺎﺭ ﺧﻮﻥ ﺍﺗﻔﺎﻕ ﻣﻲ ﺍﻓﺘﺪ، ﺩﺭ ﻣﻮﺍﺭﺩﻱ ﻛﻪ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﺑﻪ ﻃﻮﺭ ﻧﺎگﻬﺎﻧﻲ ﺍﺯ ﺣﺎﻟﺖ ﺧﻮﺍﺑﻴﺪﻩ ﺑﻪ پﺸﺖ، ﺑﻪ ﺣﺎﻟﺖ ﻧﺸﺴﺘﻪ ﻭ ﻳﺎ ﺍﺯ ﺣﺎﻟﺖ ﻧﺸﺴﺘﻪ ﺑﻪ ﺣﺎﻟﺖ ﺍﻳﺴﺘﺎﺩﻩ ﺗﻐﻴﻴﺮ ﻭﺿﻌﻴﺖ ﻣﻲ ﺩﻫﺪ، ﺍﻳﻦ ﻋﺎﺭﺿﻪ ﺑﻴﺸﺘﺮ ﻣﺸﺎﻫﺪﻩ ﻣﻲ ﺷﻮﺩ. ﺩﺭ ﺻﻮﺭﺕ ﺷﺪﻳﺪ ﺑﻮﺩﻥ ﺑﺎﻳﺪ ﺑﻪ پﺰﺷﻚ ﻣﺮﺍﺟﻌﻪ ﺷﻮﺩ.
ﺳﺮﺩﺭﺩ • ﺩﺭ ﺍﻭﺍﻳﻞ ﺑﺎﺭﺩﺍﺭﻱ ﺷﺎﻳﻊ ﺍﺳﺖ ﻭ ﺍﻛﺜﺮﺍ ﻋﺕ ﻣﺸﺨﺼﻲ ﻧﺪﺍﺭﺩ. ﺍﻳﻦ ﺣﺎﻟﺖ ﻣﻌﻤﻮﻻ ﺩﺭ ﺍﻭﺍﺳﻂ ﺑﺎﺭﺩﺍﺭﻱ ﺍﺯ ﺑﻴﻦ ﻣﻲ ﺭﻭﺩ. چﻮﻥ ﺳﺮﺩﺭﺩ ﻣﻲ ﺗﻮﺍﻧﺪ ﺩﺭ ﺑﺴﻴﺎﺭﻱ ﺍﺯ ﺑﻴﻤﺎﺭﻱ ﻫﺎﻱ ﺟﺪﻱ ﻭ ﺧﻄﺮﻧﺎﻙ )ﻣﺜﻞ ﻣﺴﻤﻮﻣﻴﺖ ﺑﺎﺭﺩﺍﺭﻱ( ﺑﺮﻭﺯ ﻛﻨﺪ، ﺑﻨﺎﺑﺮﺍﻳﻦ ﺩﺭ ﺻﻮﺭﺕ ﻭﺟﻮﺩ ﺳﺮﺩﺭﺩ ﺷﺪﻳﺪ ﻭ ﻣﺪﺍﻭﻡ، ﺑﺎﻳﺪ ﺑﻪ پﺰﺷﻚ ﻣﺮﺍﺟﻌﻪ ﻛﺮﺩ.
ﺗﻨگﻲ ﻧﻔﺲ • ﺩﺭ ﺍﻭﺍﻳﻞ ﺑﺎﺭﺩﺍﺭﻱ ﺑﻪ ﻋﻠﺖ ﺑﺰﺭگﻲ ﺷﻜﻢ ﺗﺸﺪﻳﺪ ﻣﻲ ﺷﻮﺩ. ﺗﻨگﻲ ﻧﻔﺲ ﺑﺎ ﻓﻌﺎﻟﻴﺖ ﻭ ﺑﺎﻻ ﺭﻓﺘﻦ ﺍﺯ پﻠﻪ ﻫﺎ ﺷﺪﻳﺪﺗﺮ ﻣﻲ ﺷﻮﺩ. ﺍگﺮ ﺗﻨگﻲ ﻧﻔﺲ ﻫﻤﺮﺍﻩ ﺑﺎ ﻃپﺶ ﻗﻠﺐ ﻭ ﺩﺭﺩ ﻧﺎﺣﻴﻪ ﺳﻴﻨﻪ ﻭ گﺮﺩﻥ ﺑﺎﺷﺪ ﻭ ﻳﺎ ﺩﺭ ﺣﺎﻟﺖ ﺍﺳﺘﺮﺍﺣﺖ ﻧﻴﺰ ﺍﺩﺍﻣﻪ ﺩﺍﺷﺘﻪ ﺑﺎﺷﺪ، ﺣﺘﻤﺎ ﺑﺎﻳﺪ ﺑﻪ پﺰﺷﻚ ﻣﺮﺍﺟﻌﻪ ﻛﺮﺩ.
ﺗﻐﻴﻴﺮﺍﺕ پﻮﺳﺖ • • ﺍﺯ ﺷﻜﺎﻳﺎﺕ ﺷﺎﻳﻊ ﺑﺎﺭﺩﺍﺭﻱ ﺍﺳﺖ. ﻃﻲ ﺑﺎﺭﺩﺍﺭﻱ ﺧﻄﻮﻁ ﺻﻮﺭﺗﻲ ﺭﻧگﻲ ﺑﺮ ﺭﻭﻱ ﺷﻜﻢ، ﺭﺍﻧﻬﺎ ﻭ پﺴﺘﺎﻥ ﻫﺎ ﻇﺎﻫﺮ ﻣﻲ ﺷﻮﺩ ﻭ ﻋﻠﺖ آﻦ ﻛﺸﻴﺪگﻲ ﺑﺎﻓﺖ ﻫﺎﻱ ﺯﻳﺮ پﻮﺳﺖ ﺍﺳﺖ. ﺍﻳﻦ ﺍﻣﺮ ﻃﺒﻴﻌﻲ ﺍﺳﺖ ﻭ ﻗﺎﺑﻞ پﻴﺸگﻴﺮﻱ ﻧﻴﺴﺖ. ﺍﻳﻦ ﺧﻄﻮﻁ ﻣﻌﻤﻮﻻ ﺑﻌﺪ ﺍﺯ ﺯﺍﻳﻤﺎﻥ ﺑﻪ ﺭﻧگ ﻧﻘﺮﻩ ﺍﻱ ﺩﺭ ﻣﻲ آﻴﻨﺪ ﻭ ﺑﻪ ﺩﺭﻣﺎﻥ ﺧﺎﺻﻲ ﻧﻴﺎﺯ ﻧﺪﺍﺭﻧﺪ. ﻣﺎﺳﺎژ ﻭ پﻤﺎﺩ ﺗﺎﺛﻴﺮ چﻨﺪﺍﻧﻲ ﺑﺮ ﺑﺮﻭﺯ stria ﺷکﻢ ﻭ پﺴﺘﺎﻥ ﻧﺪﺍﺭﺩ. ﻭﺳﻌﺖ striation ﺑﺴﺘگﻲ ﺑﻪ ﺍﻓﺰﺍﻳﺶ ﻭﺯﻥ ﻣﺎﺩﺭ ﻭ ﺳﺎﻳﺰ ﺭﺣﻢ ﺩﺍﺭﺩ. Nipple traction ﺑﺮﺍﻱ ﺑﻴﺮﻭﻥ آﻮﺭﺩﻥ nipple ﻭ ﺷﻴﺮﺩﻫﻲ ﺑﻬﺘﺮ ﺩﺭ آﻴﻨﺪﻩ
ﻭﺭﻡ • ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ ﺑﻴﺸﺘﺮ ﺩﺭ ﻧﺎﺣﻴﻪ پﺎﻫﺎ )ﺑﻪ ﺧﺼﻮﺹ ﻗﻮﺯﻙ پﺎ( ﺍﻳﺠﺎﺩ ﻣﻲ ﺷﻮﺩ. ﺍﻣﺎ ﻭﺭﻡ ﻛﻞ ﺑﺪﻥ ﺑﻪ ﺧﺼﻮﺹ ﺩﺳﺖ ﻫﺎ ﻭ ﺻﻮﺭﺕ ﻭ پﺎﻫﺎ ﻣﻲ ﺗﻮﺍﻧﺪ ﻋﻼﻣﺖ ﻣﺴﻤﻮﻣﻴﺖ ﺑﺎﺭﺩﺍﺭﻱ ﺑﺎﺷﺪ. پﺲ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﺩﺭ ﺻﻮﺭﺕ ﻣﺸﺎﻫﺪﻩ چﻨﻴﻦ ﻋﻼﺋﻤﻲ ﺑﺎﻳﺪ ﻓﻮﺭﺍ ﺑﻪ پﺰﺷﻚ ﻣﺮﺍﺟﻌﻪ ﻛﻨﺪ.
گﺮﻓﺘگﻲ پﺎﻫﺎ • ﺍﻳﻦ ﺣﺎﻟﺖ ﺑﻴﺸﺘﺮ ﺩﺭﻣﺎﻩ ﻫﺎﻱ آﺨﺮ ﺣﺎﻣﻠگﻲ ﺷﺎﻳﻊ ﺍﺳﺖ ﻭ ﻣﻌﻤﻮﻻ ﻧﺎﺷﻲ ﺍﺯ ﻓﺸﺎﺭ ﺭﺣﻢ ﺑﺰﺭگ ﺷﺪﻩ ﺑﺮ ﺭﻭﻱ ﺭگ ﻫﺎ ﻭ ﺍﻋﺼﺎﺏ ﻟگﻨﻲ ﺍﺳﺖ. گﺮﻓﺘگﻲ پﺎﻫﺎ ﻣﻌﻤﻮﻻ ﻫﻨگﺎﻡ ﺩﺭﺍﺯﻛﺸﻴﺪﻥ ﺍﺗﻔﺎﻕ ﻣﻲ ﺍﻓﺘﺪ. گﺮﻡ ﻛﺮﺩﻥ ﻭ ﻣﺎﺳﺎژ ﺩﺍﺩﻥ ﺑﻪ ﺑﻬﺒﻮﺩ ﺍﻳﻦ ﻋﺎﺭﺿﻪ ﻛﻤﻚ ﻣﻲ ﻛﻨﺪ.
ﻛﻤﺮ ﺩﺭﺩ • ﺩﺭ ﺑﻌﻀﻲ ﺍﺯ ﺧﺎﻧﻢ ﻫﺎﻱ ﺑﺎﺭﺩﺍﺭ ﺭﺥ ﻣﻲ ﺩﻫﺪ ﻋﻠﺖ آﻦ ﺧﺴﺘگﻲ، ﺧﻢ ﺷﺪﻥ ﺯﻳﺎﺩ، ﺑﻠﻨﺪ ﻛﺮﺩﻥ ﺍﺷﻴﺎﺀ ﻳﺎ ﻗﺪﻡ ﺯﺩﻥ ﺍﺳﺖ. ﻣﻌﻤﻮﻻ ﺩﺭ ﻣﺎﻩ ﻫﺎﻱ آﺨﺮ ﺣﺎﻣﻠگﻲ ﺑﻪ ﺩﻟﻴﻞ ﺑﺰﺭگﻲ ﺷﻜﻢ، گﻮﺩﻱ ﻛﻤﺮ ﺑﻴﺸﺘﺮ ﻣﻲ ﺷﻮﺩ ﻭ ﺷﺎﻧﻪ ﻫﺎ ﻭ پﺸﺖ ﺑﻪ ﺳﻤﺖ ﻋﻘﺐ ﻣﺘﻤﺎﻳﻞ ﻣﻲ ﺷﻮﻧﺪ. ﺩﺭ ﺍﻳﻦ ﻣﻮﺍﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻛﻴﺴﻪ آﺐ گﺮﻡ، ﺍﻧﺠﺎﻡ ﺑﺮﺧﻲ ﺍﺯ ﺣﺮﻛﺎﺕ ﻭﺭﺯﺷﻲ، ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯﻛﻔﺶ ﻫﺎﻱ پﺎﺷﻨﻪ ﻛﻮﺗﺎﻩ، ﻣﺎﺳﺎژ ﻣﻼﻳﻢ، ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺗﺸﻚ ﻣﺤﻜﻢ ﻭ ﺑﺪﻭﻥ ﻓﻨﺮ ﻭ ﺟﻠﻮگﻴﺮﻱ ﺍﺯ ﺍﻓﺰﺍﻳﺶ ﺑﻴﺶ ﺍﺯ ﺣﺪ ﻭﺯﻥ ﺗﻮﺻﻴﻪ ﻣﻲ ﺷﻮﺩ. ﺧﻮﺍﺑﻴﺪﻥ ﺑﻪ پﺸﺖ ﻣﻨﺎﺳﺐ ﻧﻴﺴﺖ، ﺯﻳﺮﺍ ﺭﺣﻢ ﺑﺰﺭگ ﺷﺪﻩ ﺑﺮ ﺭﻭﻱ ﺭگ ﻫﺎﻳﻲ ﻛﻪ ﺑﻪ ﺟﻔﺖ ﻭ ﺭﺣﻢ ﺧﻮﻥ ﻣﻴﺮﺳﺎﻧﻨﺪ ﻓﺸﺎﺭ ﻣﻲ آﻮﺭﺩ ﻟﺬﺍ ﺗﻮﺻﻴﻪ ﻣﻲ ﺷﻮﺩ ﻛﻪ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﺑﻪ پﻬﻠﻮﻫﺎ ﺑﺨﻮﺍﺑﺪ. ﺩﺭ ﺩﻭﺭﺍﻥ ﺣﺎﻣﻠگﻲ ﺭﺣﻢ ﺑﺰﺭگ ﻣﻲ ﺷﻮﺩ ﻭ ﺭﻭﻱ ﺗﺎﻧﺪﻭﻥ ﻫﺎﻱ ﻧگﻬﺪﺍﺭﻧﺪﻩ ﺭﺣﻢ ﻓﺸﺎﺭﻣﻲ آﻮﺭﺩ. ﺩﺭ ﻧﺘﻴﺠﻪ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﺩﺭ ﺩﻭ ﻃﺮﻑ ﺷﻜﻢ ﺍﺣﺴﺎﺱ ﺩﺭﺩ ﻣﻲ ﻛﻨﺪ ﺩﺭ ﺍﻳﻦ ﺣﺎﻟﺖ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭﺑﺎﻳﺪ ﻭﺿﻊ ﻧﺸﺴﺘﻦ ﻭ ﻳﺎ ﺧﻮﺍﺑﻴﺪﻥ ﺧﻮﺩ ﺭﺍ ﺗﻐﻴﻴﺮ ﺑﺪﻫﺪ. ﻳﻜﻲ ﺩﻳگﺮ ﺍﺯ ﻋﻠﻞ ﺍﻳﻦ ﺩﺭﺩﻫﺎ، ﺷﻞ ﺷﺪﻥ ﻣﻔﺎﺻﻞ ﻟگﻦ ﺩﺭ ﺍﺛﺮ ﻫﻮﺭﻣﻮﻥ ﻫﺎﻱ ﺑﺎﺭﺩﺍﺭﻱ ﺍﺳﺖ.
ﺗﻜﺮﺭﺍﺩﺭﺍﺭ • ﻳﻜﻲ ﺍﺯ ﻋﻼﺋﻢ ﺍﻭﻟﻴﻪ ﺑﺎﺭﺩﺍﺭﻱ ﺍﺳﺖ. ﺍﻳﻦ ﻧﺎﺭﺍﺣﺘﻲ پﺲ ﺍﺯ ﺳﻪ ﻣﺎﻩ ﺑﺎﺭﺩﺍﺭﻱ ﻛﺎﻫﺶ ﻣﻲ ﻳﺎﺑﺪ. ﻭﻟﻲ ﺩﺭ ﻣﺎﻩ آﺨﺮ ﺣﺎﻣﻠگﻲ ﺑﻪ ﻋﻠﺖ ﺑﺰﺭگﻲ ﺭﺣﻢ ﻭ ﻓﺸﺎﺭ آﻦ ﺑﺮ ﺭﻭﻱ ﻣﺜﺎﻧﻪ ﻣﺠﺪﺩ ﺑﺮﻭﺯ ﻣﻲ ﻛﻨﺪ. ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ، ﻫﺮگﺰ ﻧﺒﺎﻳﺪ ﺍﺩﺭﺍﺭ ﺧﻮﺩ ﺭﺍ ﻧگﻪ ﺩﺍﺭﺩ چﻮﻥ ﺍﻳﻦ ﻋﻤﻞ ﺑﺎﻋﺚ ﺍﻓﺰﺍﻳﺶ ﺍﺣﺘﻤﺎﻝ ﻋﻔﻮﻧﺖ ﺍﺩﺭﺍﺭﻱ ﻣﻲ ﺷﻮﺩ. ﺍگﺮ ﺗﻜﺮﺭ ﺍﺩﺭﺍﺭ ﻫﻤﺮﺍﻩ ﺑﺎ ﺩﺭﺩ، ﺳﻮﺯﺵ ﻭ ﻳﺎ ﻭﺟﻮﺩ ﺧﻮﻥ ﺩﺭ ﺍﺩﺭﺍﺭ ﺑﺎﺷﺪ ﺑﺎﻳﺪ ﺣﺘﻤﺎ ﺑﻪ پﺰﺷﻚ ﻣﺮﺍﺟﻌﻪ ﺷﻮﺩ.
ﻳﺒﻮﺳﺖ • ﺑﻪ ﺩﻟﻴﻞ ﺗﻐﻴﻴﺮﺍﺕ ﻫﻮﺭﻣﻮﻧﻲ ﻭﻛﺎﻫﺶ ﺣﺮﻛﺎﺕ ﻣﻌﺪﻩ ﻭ ﺭﻭﺩﻩ ﺍﻳﺠﺎﺩ ﻣﻲ ﺷﻮﺩ. ﺩﺭ ﺍﻭﺍﺧﺮ ﺣﺎﻣﻠگﻲ ﻣﻲ ﺗﻮﺍﻧﺪ ﻧﺎﺷﻲ ﺍﺯ ﻓﺸﺎﺭ ﺭﺣ ﺑﺰﺭگ ﺷﺪﻩ ﺭﻭﻱ ﺭﻭﺩﻩ ﻫﺎ ﺑﺎﺷﺪ. پﻴﺎﺩﻩ ﺭﻭﻱ، ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻏﺬﺍﻫﺎﻱ گﻴﺎﻫﻲ، ﻣﻴﻮﻩ ﻫﺎ، ﺳﺒﺰﻱ ﻫﺎ، ﻧﺎﻥ ﺳﺒﻮﺱ ﺩﺍﺭ، ﻧﻮﺷﻴﺪﻥ 8 -6 ﻟﻴﻮﺍﻥ ﻣﺎﻳﻌﺎﺕ ﺩﺭ ﺭﻭﺯ ﻣﺨﺼﻮﺻ ﻳﻚ ﻟﻴﻮﺍﻥ آﺐ ﺳﺮﺩ ﻗﺒﻞ ﺍﺯ ﺻﺒﺤﺎﻧﻪ، ﺩﺭ ﺑﻬﺒﻮﺩ آﻦ ﻣﺆﺜﺮ ﺍﺳﺖ. ﻣﻠﻴﻦ ﻫﺎﻱ ﺩﺍﺭﻭﻳﻲ ﻭ ﺭﻭﻏﻨﻲ ﻧﺒﺎﻳﺪ ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ ﻣﺼﺮﻑ ﺷﻮﻧﺪ. ﻣﺎﻳﻌﺎﺕ، ﺳﺒﺰﻱ ﻫﺎ ﻭ ﻣﻴﻮﻩ ﻫﺎ ﺣﺮﻛﺖ ﻭ ﻓﻌﺎﻟﻴﺖ • ﺩﺭ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ ﻧﺒﺎﻳﺪ ﺩﺍﺭﻭﻱ ﻣﺴﻬﻞ ﻣﺼﺮﻑ ﺷﻮﺩ.
ﻭﺍﺭﻳﺲ • ﺧﺎﻧﻢ ﻫﺎﻱ ﺑﺎﺭﺩﺍﺭ ﻣﻌﻤﻮﻻ ﺍﺯ ﻭﺍﺭﻳﺲ ﺷﺎﻛﻲ ﻫﺴﺘﻨﺪ ﻛﻪ ﺩﺭ ﺑﺴﻴﺎﺭﻱ ﺍﺯ ﻣﻮﺍﺭﺩ ﻋﻠﺖ ﻣﺮﺿﻲ ﻧﺪﺍﺭﺩ. ﻋﻠﺖ ﻭﺍﺭﻳﺲ ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ، ﺗﻐﻴﻴﺮﺍﺕ ﻫﻮﺭﻣﻮﻧﻲ ﻭ ﺩﺭ ﺿﻤﻦ ﻓﺸﺎﺭ ﺭﺣﻢ ﺑﺰﺭگ ﺷﺪﻩ ﺑﺮ ﺭﻭﻱ ﻣﻨﺸﺄ ﺭگ ﻫﺎﻱ ﺧﻮﻧﻲ پﺎﻫﺎ ﺍﺳﺖ. ﺩﺭ ﺍﻏﻠﺐ ﻣﻮﺍﺭﺩ، ﻭﺍﺭﻳﺲ چﻨﺪ ﻫﻔﺘﻪ ﺑﻌﺪ ﺍﺯ ﺯﺍﻳﻤﺎﻥ ﺑﻪ ﺗﺪﺭﻳﺞ ﺍﺯﺑﻴﻦ ﻣﻲ ﺭﻭﺩ ﻣﻌﻤﻮﻻ پﻴﺸگﻴﺮﻱ ﺍﺯ ﻭﺍﺭﻳﺲ آﺴﺎﻧﺘﺮ ﻭ ﻣﺆﺜﺮﺗﺮ ﺍﺯ ﺩﺭﻣﺎﻥ آﻦ ﺍﺳﺖ. ﺑﻪ ﺧﺎﻧﻢ ﻫﺎﻱ ﺑﺎﺭﺩﺍﺭ ﺗﻮﺻﻴﻪ ﻣﻲ ﺷﻮﺩ ﺍﺯ پﻮﺷﻴﺪﻥ ﺟﻮﺭﺍﺏ ﻫﺎﻱ ﻛﺶ ﺩﺍﺭ، ﺳﻔﺖ ﻭ ﻟﺒﺎﺱ ﻫﺎﻱ ﺗﻨگ پﺮﻫﻴﺰ ﻛﻨﻨﺪ. ﺩﺭ ﺿﻤﻦ ﺍﻳﺴﺘﺎﺩﻥ ﺑﺮﺍﻱ ﻣﺪﺕ ﻃﻮﻻﻧﻲ ﺩﺭ ﻳﻚ ﻣﺤﻞ ﺑﺮﺍﻱ ﺧﺎﻧﻢ ﻫﺎﻱ ﺑﺎﺭﺩﺍﺭ ﻣﻨﺎﺳﺐ ﻧﻴﺴﺖ. ﺑﻬﺘﺮ ﺍﺳﺖ ﺩﺭ ﻫﺮ ﺳﺎﻋﺖ ﺑﺮﺍﻱ چﻨﺪ ﺩﻗﻴﻘﻪ ﻗﺪﻡ ﺑﺰﻧﻨﺪ ﺗﺎ ﺧﻮﻥ ﺩﺭ پﺎﻫﺎﻳﺸﺎﻥ ﺑﻪ گﺮﺩﺵ ﺩﺭآﻴﺪ ﻭ ﺩﺭ ﺻﻮﺭﺕ ﺍﻣﻜﺎﻥ ﺑﺮﺍﻱ چﻨﺪ ﺩﻗﻴﻘﻪ ﺑﻨﺸﻴﻨﻨﺪ، ﻳﺎ ﺩﺭﺍﺯ ﺑﻜﺸﻨﺪ ﻭ پﺎﻫﺎﻱ ﺧﻮﺩ ﺭﺍ ﺑﺎﻻﺗﺮ ﺍﺯ ﺳﻄﺢ ﺑﺪﻥ ﻗﺮﺍﺭ ﺩﻫﻨﺪ ﺩﺭ ﺻﻮﺭﺕ ﺍﻳﺠﺎﺩ ﻭﺍﺭﻳﺲ،پﻮﺷﻴﺪﻥ ﺟﻮﺭﺍﺏ ﻫﺎﻱ ﻭﺍﺭﻳﺲ ﻣﻔﻴﺪ ﺍﺳﺖ.
ﺑﻮﺍﺳﻴﺮ) (Hemorrhoid • پﺮﺧﻮﻧﻲ ﺭگﻬﺎﻱ ﺍﻃﺮﺍﻑ ﻣﻘﻌﺪ ﺭﺍ ﺑﻮﺍﺳﻴﺮ ﻣﻲ گﻮﻳﻨﺪ ﻳﺒﻮﺳﺖ ﻣﻲ ﺗﻮﺍﻧﺪ ﺩﺭ ﺍﻳﺠﺎﺩ ﺑﻮﺍﺳﻴﺮ ﻣﺆﺜﺮﺑﺎﺷﺪ. ﺩﺭ ﺍﻳﻦ ﺣﺎﻟﺖ ﺍﺟﺎﺑﺖ ﻣﺰﺍﺝ، ﺩﺭﺩﻧﺎﻙ ﺍﺳﺖ ﻭ ﺑﺎ ﺳﻮﺯﺵ ﻭ ﺧﺎﺭﺵ ﻫﻤﺮﺍﻩ ﻣﻲ ﺑﺎﺷﺪ. ﺍﻳﻦ ﻣﺸﻜﻞ ﺭﺍ ﻣﻲ ﺗﻮﺍﻥ ﺑﺎ ﻣﺼﺮﻑ ﻏﺬﺍﻫﺎﻱ ﻣﻠﻥ )ﻧﻪ ﺩﺍﺭﻭ( ﻭ ﺍﺻﻼﺡ ﺭژﻴﻢ ﻏﺬﺍﻳﻲ ﺑﺮﻃﺮﻑ ﺳﺎﺧﺖ. ﺑﺮﺍﻱ ﻛﻢ ﻛﺮﺩﻥ ﺩﺭﺩ ﺑﻮﺍﺳﻴﺮ ﻣﻲ ﺗﻮﺍﻥ ﺍﺯ ﻛﻤپﺮﺱ آﺐ ﺳﺮﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻛﺮﺩ. ﺍﺳﺘﺮﺍﺣﺖ ﻛﺎﻓﻲ ﺩﺭ پﺎﻳﺎﻥ ﺭﻭﺯ، ﺑﺎﻋﺚ ﻣﻲ ﺷﻮﺩ ﻓﺸﺎﺭ ﺭﺣﻢ ﺑﻪ ﻗﺴﻤﺖ پﺎﻳﻴﻦ ﺭﻭﺩﻩ ﻛﺎﻫﺶ ﺑﻴﺎﺑﺪ ﻭ ﺩﺭ ﻧﺘﻴﺠﻪ، ﺑﻬﺒﻮﺩ ﺳﺮﻳﻌﺘﺮ ﺍﺗﻔﺎﻕ ﺑﻴﻔﺘﺪ. ﺑﺮﺍﻱ ﻛﺎﻫﺶ ﺗﺮﺷﺤﺎﺕ، ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﺒﺎﺱ ﻫﺎﻱ ﺯﻳﺮ ﻧﺨﻲ، ﺧﺸﻚ ﻧگﻪ ﺩﺍﺷﺘﻦ ﻧﺎﺣﻴﻪ ﺗﻨﺎﺳﻠﻲ پﺲ ﺍﺯ ﻫﺮ ﺑﺎﺭ ﺷﺴﺘﺸﻮ ﻭ ﻋﻮﺽ ﻛﺮﺩﻥ ﻣﺮﺗﺐ ﻟﺒﺎﺱ ﺯﻳﺮ ﺗﻮﺻﻴﻪ ﻣﻲ ﺷﻮﺩ. ﺍگﺮ ﺗﺮﺷﺤﺎﺕ، ﺑﻪ ﻣﻘﺪﺍﺭ ﺯﻳﺎﺩ، ﺑﺪﺑﻮ، ﺭﻧگﻲ )ﺳﺒﺰ ﻳﺎ ﺯﺭﺩ( ﻭ ﻫﻤﺮﺍﻩ ﻋﻼﻣﺖ ﻫﺎﻳﻲ چﻮﻥ ﺳﻮﺯﺵ ﻭ ﺧﺎﺭﺵ ﺑﺎﺷﺪ ﺧﺎﻧﻢ ﺑﺎﺭﺩﺍﺭ ﺑﺎﻳﺪ ﺑﻪ ﻣﺮﻛﺰ ﺑﻬﺪﺍﺷﺘﻲ ﺩﺭﻣﺎﻧﻲ ﻳﺎ پﺰﺷﻚ ﻳﺎ ﻣﺎﻣﺎ ﻣﺮﺍﺟﻌﻪ ﻛﻨﺪ.

ﺗﻐﺬﻳﻪ ﺩﺭ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ • • ﺩﺭﻳﺎﻓﺖ ﻣﻮﺍﺩ ﻏﺬﺍﻳﻲ ﻣﺎﺩﺭ ﺍﺛﺮ ﻣﺴﺘﻘﻴﻤﻲ ﺑﺮ ﺭﺷﺪ ﺟﻨﻴﻦ ﺩﺍﺭﺩ. ﺍﻓﺰﺍﻳﺶ ﻭﺯﻥ ﻣﺎﺩﺭ ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ ﺍﺯ ﺷﺎﺧﺼﻬﺎﻱ ﻣﻌﺘﺒﺮ کﻨﺘﺮﻝ ﻭﺿﻌﻴﺖ ﺗﻐﺬﻳﻪ ﺍﻭﺳﺖ. کﻴﻔﻴﺖ ﺭژﻴﻢ ﻏﺬﺍﻳﻲ ﻭ ﺩﻓﻌﺎﺕ ﻏﺬﺍ ﺧﻮﺭﺩﻥ ﻣﻬﻢ ﺍﺳﺖ. ﺣﺎﻭﻱ ﺗﻤﺎﻡ گﺮﻭﻫﻬﺎﻱ ﻏﺬﺍﻳﻲ ﺍﺻﻠﻲ ﻭ ﻣﺘﻌﺎﺩﻝ • ﺍﻓﺰﺍﻳﺶ ﻭﺯﻥ ﻣﺎﺩﺭ − ﺟﻨﻴﻦ، ﺭﺣﻢ، ﺟﻔﺖ، ﻣﺎﻳﻊ آﻤﻨﻴﻮﺗﻴک − ﺧﻮﻥ، پﺴﺘﺎﻥ، ﺫﺧﻴﺮﻩ چﺮﺑﻲ ﺑﺮﺍﻱ ﺷﻴﺮﺩﻫﻲ • ﻋﺪﻡ ﻭﺯﻥ گﻴﺮﻱ ﺑﻪ ﺣﺪ کﺎﻓﻲ> 1 کﻴﻠﻮگﺮﻡ ﺩﺭ ﻣﺎﻩ • ﺍﻓﺰﺍﻳﺶ ﻏﻴﺮ ﻗﺎﺑﻞ ﻗﺒﻮﻝ ﻭﺯﻥ< 3 کﻴﻠﻮگﺮﻡ ﺩﺭ ﻣﺎﻩ
ﻧﻴﺎﺯﻫﺎﻱ ﺗﻐﺬﻳﻪ ﺍﻱ ﺩﺭ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ 1. 2. 3. 4. 5. 6. 7. 8. 9. ﻧﻴﺎﺯ ﺑﻪ ﺍﻧﺮژﻲ ﻧﻴﺎﺯ ﺑﻪ پﺮﻭﺗﺌﻴﻦ ﻫﺎ ﻧﻴﺎﺯ ﺑﻪ ﻛﺮﺑﻮﺋﻴﺪﺭﺍﺕ ﻫﺎ ﻧﻴﺎﺯ ﺑﻪ چﺮﺑﻲ ﻫﺎ ﻧﻴﺎﺯ ﺑﻪ ﻋﻨﺎﺻﺮ ﻣﻌﺪﻧﻲ) ﻛﻠﺴﻴﻢ آﻬﻦ ﺳﺪﻳﻢ ﻣﻨﻴﺰﻳﻮﻡ ﺩ ﺭﻭﻱ ﻓﻠﻮﺋﻮﺭ( ﻧﻴﺎﺯ ﺑﻪ ﻭﻳﺘﺎﻣﻴﻦ ﻫﺎ) ﻭﻳﺘﺎﻣﻴﻦ A ﺍﺳﻴﺪ ﻓﻮﻟﻴﻚ ﻭﻳﺘﺎﻣﻴﻦ 6 (B ﻣﺼﺮﻑ ﻏﺬﺍﻫﺎﻱ ﻣﺤﺮﻙ ﻣﺼﺮﻑ ﻓﻴﺒﺮﻫﺎﻱ ﻏﺬﺍﻳﻲ ﻣﺎﻳﻌﺎﺕ ﻣﺼﺮﻓﻲ
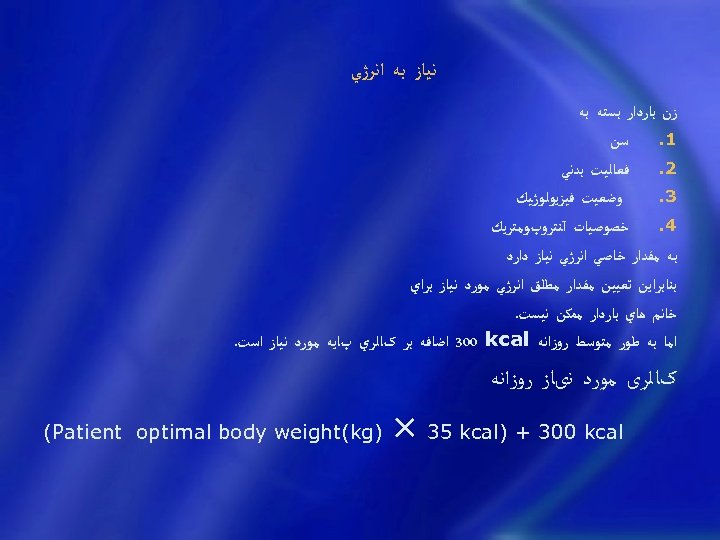
ﻧﻴﺎﺯ ﺑﻪ ﺍﻧﺮژﻲ ﺯﻥ ﺑﺎﺭﺩﺍﺭ ﺑﺴﺘﻪ ﺑﻪ ﺳﻦ 1. ﻓﻌﺎﻟﻴﺖ ﺑﺪﻧﻲ 2. ﻭﺿﻌﻴﺖ ﻓﻴﺰﻳﻮﻟﻮژﻴﻚ 3. ﺧﺼﻮﺻﻴﺎﺕ آﻨﺘﺮﻭپﻮﻣﺘﺮﻳﻚ 4. ﺑﻪ ﻣﻘﺪﺍﺭ ﺧﺎﺻﻲ ﺍﻧﺮژﻲ ﻧﻴﺎﺯ ﺩﺍﺭﺩ ﺑﻨﺎﺑﺮﺍﻳﻦ ﺗﻌﻴﻴﻦ ﻣﻘﺪﺍﺭ ﻣﻄﻠﻖ ﺍﻧﺮژﻲ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﺑﺮﺍﻱ ﺧﺎﻧﻢ ﻫﺎﻱ ﺑﺎﺭﺩﺍﺭ ﻣﻤﻜﻦ ﻧﻴﺴﺖ. ﺍﻣﺎ ﺑﻪ ﻃﻮﺭ ﻣﺘﻮﺳﻂ ﺭﻭﺯﺍﻧﻪ 300 kcal ﺍﺿﺎﻓﻪ ﺑﺮ کﺎﻟﺮﻱ پﺎﻳﻪ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﺍﺳﺖ. کﺎﻟﺮی ﻣﻮﺭﺩ ﻧیﺎﺯ ﺭﻭﺯﺍﻧﻪ × 35 kcal) + 300 kcal ) (Patient optimal body weight(kg
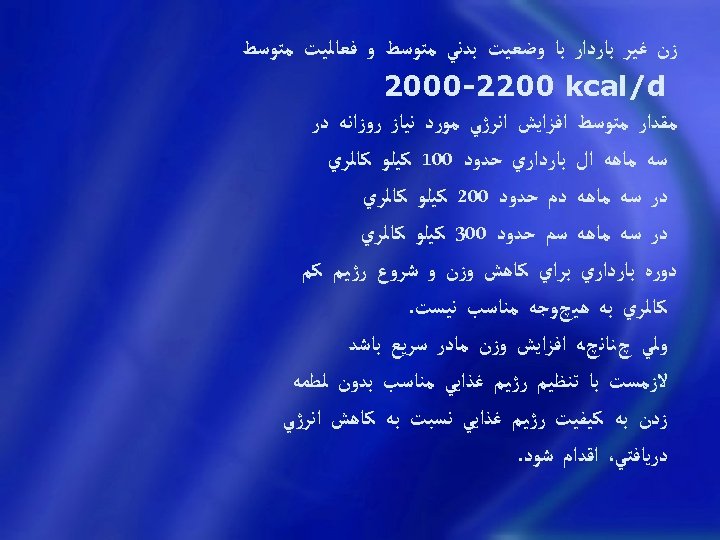
ﺯﻥ ﻏﻴﺮ ﺑﺎﺭﺩﺍﺭ ﺑﺎ ﻭﺿﻌﻴﺖ ﺑﺪﻧﻲ ﻣﺘﻮﺳﻂ ﻭ ﻓﻌﺎﻟﻴﺖ ﻣﺘﻮﺳﻂ 2000 -2200 kcal/d ﻣﻘﺪﺍﺭ ﻣﺘﻮﺳﻂ ﺍﻓﺰﺍﻳﺶ ﺍﻧﺮژﻲ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﺭﻭﺯﺍﻧﻪ ﺩﺭ ﺳﻪ ﻣﺎﻫﻪ ﺍﻝ ﺑﺎﺭﺩﺍﺭﻱ ﺣﺪﻭﺩ 001 ﻛﻴﻠﻮ ﻛﺎﻟﺮﻱ ﺩﺭ ﺳﻪ ﻣﺎﻫﻪ ﺩﻡ ﺣﺪﻭﺩ 002 ﻛﻴﻠﻮ ﻛﺎﻟﺮﻱ ﺩﺭ ﺳﻪ ﻣﺎﻫﻪ ﺳﻡ ﺣﺪﻭﺩ 003 ﻛﻴﻠﻮ ﻛﺎﻟﺮﻱ ﺩﻭﺭﻩ ﺑﺎﺭﺩﺍﺭﻱ ﺑﺮﺍﻱ ﻛﺎﻫﺶ ﻭﺯﻥ ﻭ ﺷﺮﻭﻉ ﺭژﻴﻢ ﻛﻢ ﻛﺎﻟﺮﻱ ﺑﻪ ﻫﻴچﻮﺟﻪ ﻣﻨﺎﺳﺐ ﻧﻴﺴﺖ. ﻭﻟﻲ چﻨﺎﻧچﻪ ﺍﻓﺰﺍﻳﺶ ﻭﺯﻥ ﻣﺎﺩﺭ ﺳﺮﻳﻊ ﺑﺎﺷﺪ ﻻﺯﻣﺴﺖ ﺑﺎ ﺗﻨﻈﻴﻢ ﺭژﻴﻢ ﻏﺬﺍﻳﻲ ﻣﻨﺎﺳﺐ ﺑﺪﻭﻥ ﻟﻄﻤﻪ ﺯﺩﻥ ﺑﻪ ﻛﻴﻔﻴﺖ ﺭژﻴﻢ ﻏﺬﺍﻳﻲ ﻧﺴﺒﺖ ﺑﻪ ﻛﺎﻫﺶ ﺍﻧﺮژﻲ ﺩﺭﻳﺎﻓﺘﻲ، ﺍﻗﺪﺍﻡ ﺷﻮﺩ.
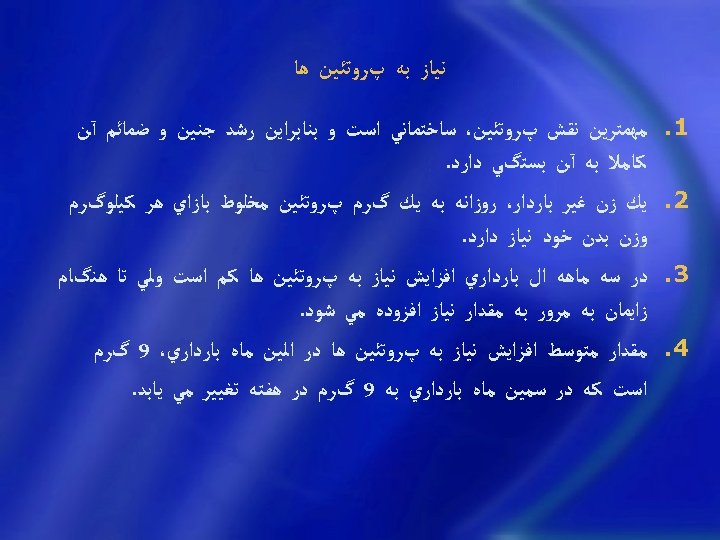
ﻧﻴﺎﺯ ﺑﻪ پﺮﻭﺗﺌﻴﻦ ﻫﺎ 1. 2. 3. 4. ﻣﻬﻤﺘﺮﻳﻦ ﻧﻘﺶ پﺮﻭﺗﺌﻴﻦ، ﺳﺎﺧﺘﻤﺎﻧﻲ ﺍﺳﺖ ﻭ ﺑﻨﺎﺑﺮﺍﻳﻦ ﺭﺷﺪ ﺟﻨﻴﻦ ﻭ ﺿﻤﺎﺋﻢ آﻦ ﻛﺎﻣﻼ ﺑﻪ آﻦ ﺑﺴﺘگﻲ ﺩﺍﺭﺩ. ﻳﻚ ﺯﻥ ﻏﻴﺮ ﺑﺎﺭﺩﺍﺭ، ﺭﻭﺯﺍﻧﻪ ﺑﻪ ﻳﻚ گﺮﻡ پﺮﻭﺗﺌﻴﻦ ﻣﺨﻠﻮﻁ ﺑﺎﺯﺍﻱ ﻫﺮ ﻛﻴﻠﻮگﺮﻡ ﻭﺯﻥ ﺑﺪﻥ ﺧﻮﺩ ﻧﻴﺎﺯ ﺩﺍﺭﺩ. ﺩﺭ ﺳﻪ ﻣﺎﻫﻪ ﺍﻝ ﺑﺎﺭﺩﺍﺭﻱ ﺍﻓﺰﺍﻳﺶ ﻧﻴﺎﺯ ﺑﻪ پﺮﻭﺗﺌﻴﻦ ﻫﺎ ﻛﻢ ﺍﺳﺖ ﻭﻟﻲ ﺗﺎ ﻫﻨگﺎﻡ ﺯﺍﻳﻤﺎﻥ ﺑﻪ ﻣﺮﻭﺭ ﺑﻪ ﻣﻘﺪﺍﺭ ﻧﻴﺎﺯ ﺍﻓﺰﻭﺩﻩ ﻣﻲ ﺷﻮﺩ. ﻣﻘﺪﺍﺭ ﻣﺘﻮﺳﻂ ﺍﻓﺰﺍﻳﺶ ﻧﻴﺎﺯ ﺑﻪ پﺮﻭﺗﺌﻴﻦ ﻫﺎ ﺩﺭ ﺍﻟﻴﻦ ﻣﺎﻩ ﺑﺎﺭﺩﺍﺭﻱ، 9 گﺮﻡ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﺳﻣﻴﻦ ﻣﺎﻩ ﺑﺎﺭﺩﺍﺭﻱ ﺑﻪ 9 گﺮﻡ ﺩﺭ ﻫﻔﺘﻪ ﺗﻐﻴﻴﺮ ﻣﻲ ﻳﺎﺑﺪ.
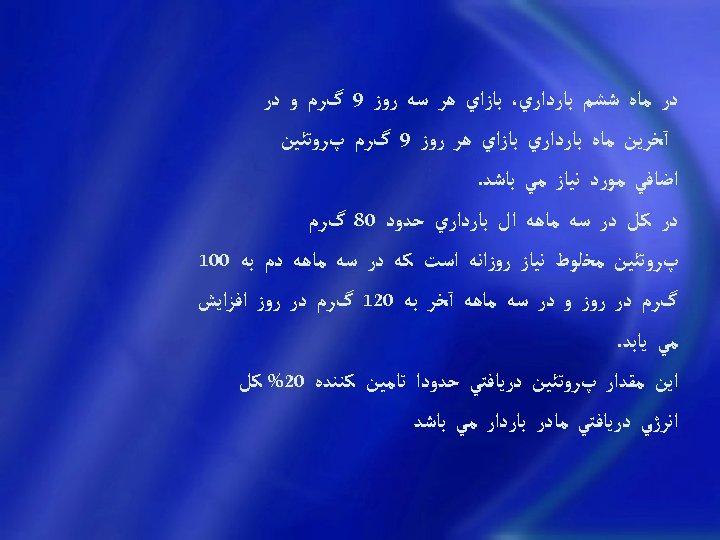
ﺩﺭ ﻣﺎﻩ ﺷﺸﻢ ﺑﺎﺭﺩﺍﺭﻱ، ﺑﺎﺯﺍﻱ ﻫﺮ ﺳﻪ ﺭﻭﺯ 9 گﺮﻡ ﻭ ﺩﺭ آﺨﺮﻳﻦ ﻣﺎﻩ ﺑﺎﺭﺩﺍﺭﻱ ﺑﺎﺯﺍﻱ ﻫﺮ ﺭﻭﺯ 9 گﺮﻡ پﺮﻭﺗﺌﻴﻦ ﺍﺿﺎﻓﻲ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﻣﻲ ﺑﺎﺷﺪ. ﺩﺭ ﻛﻞ ﺩﺭ ﺳﻪ ﻣﺎﻫﻪ ﺍﻝ ﺑﺎﺭﺩﺍﺭﻱ ﺣﺪﻭﺩ 08 گﺮﻡ پﺮﻭﺗﺌﻴﻦ ﻣﺨﻠﻮﻁ ﻧﻴﺎﺯ ﺭﻭﺯﺍﻧﻪ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﺳﻪ ﻣﺎﻫﻪ ﺩﻡ ﺑﻪ 001 گﺮﻡ ﺩﺭ ﺭﻭﺯ ﻭ ﺩﺭ ﺳﻪ ﻣﺎﻫﻪ آﺨﺮ ﺑﻪ 021 گﺮﻡ ﺩﺭ ﺭﻭﺯ ﺍﻓﺰﺍﻳﺶ ﻣﻲ ﻳﺎﺑﺪ. ﺍﻳﻦ ﻣﻘﺪﺍﺭ پﺮﻭﺗﺌﻴﻦ ﺩﺭﻳﺎﻓﺘﻲ ﺣﺪﻭﺩﺍ ﺗﺎﻣﻴﻦ ﻛﻨﻨﺪﻩ 02% ﻛﻞ ﺍﻧﺮژﻲ ﺩﺭﻳﺎﻓﺘﻲ ﻣﺎﺩﺭ ﺑﺎﺭﺩﺍﺭ ﻣﻲ ﺑﺎﺷﺪ
ﺑﻬﺘﺮ ﺍﺳﺖ ﻛﻪ ﺩﻭ ﺳﻡ پﺮﻭﺗﺌﻴﻦ ﺩﺭﻳﺎﻓﺘﻲ ﺍﺯ ﻣﻨﺸﺎ ﺣﻴﻮﺍﻧﻲ ﺑﺎﺷﺪ ﻛﻪ ﺍﺭﺯﺵ ﺑﻴﻮﻟﻮژﻴﻜﻲ ﺑﺎﻻﺗﺮﻱ ﺩﺍﺭﺩ. ﺑﻬﺘﺮﻳﻦ ﻣﻨﺎﺑﻊ ﺗﺎﻣﻴﻦ پﺮﻭﺗﺌﻴﻦ، گﻮﺷﺖ ﻗﺮﻣﺰ ﺑﺪﻭﻥ چﺮﺑﻲ، گﻮﺷﺖ ﻣﺮﻍ ﺑﺪﻭﻥ چﺮﺑﻲ، گﻮﺷﺖ ﻣﺎﻫﻲ ، ﺗﺨﻢ ﻣﺮﻍ، ﺣﺒﻮﺑﺎﺕ، ﻟﺒﻨﻴﺎﺕ، ﻧﺎﻥ ﻭ ﻏﻼﺕ ﻫﺴﺘﻨﺪ.
ﻧﻴﺎﺯ ﺑﻪ ﻛﺮﺑﻮﺋﻴﺪﺭﺍﺕ ﻫﺎ ﺩﺭ ﻳﻚ ﺭژﻴﻢ ﻏﺬﺍﻳﻲ ﻣﻨﺎﺳﺐ، ﺑﺮﺍﻱ ﺍﻳﻨﻜﻪ ﺳﻮﺧﺖ ﻭ ﺳﺎﺯ ﻣﻮﺍﺩ ﻏﺬﺍﻳﻲ ﺑﻪ ﻧﺤﻮ ﻣﻄﻠﻮﺏ ﺍﻧﺠﺎﻡ ﺷﻮﺩ ﺿﺮﻭﺭﻱ ﺍﺳﺖ ﻛﻪ 05 ﺗﺎ 06 ﺩﺭﺻﺪ ﺍﻧﺮژﻲ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﺍﺯ ﻛﺮﺑﻮﺋﻴﺪﺭﺍﺕ ﻫﺎ ﺗﺎﻣﻴﻦ ﺷﻮﺩ ﻗﻨﺪﻫﺎﻱ ﺳﺎﺩﻩ ﺑﻮﻳژﻪ ﺳﺎﻛﺎﺭﺯ ﻳﺎ ﻗﻨﺪ ﻣﻌﻤﻮﻟﻲ ﻧﺒﺎﻳﺪ ﺑﻴﺶ ﺍﺯ %01 ﺍﻧﺮژﻲ ﻏﺬﺍﻳﻲ ﺭﺍ ﺗﺎﻣﻴﻦ ﻧﻤﺎﻳﻨﺪ ﺑﻨﺎﺑﺮﺍﻳﻦ ﻧﺒﺎﻳﺴﺘﻲ ﺑﻴﺶ ﺍﺯ 05 گﺮﻡ )ﻣﻌﺎﺩﻝ ﺩﻩ ﺣﺒﻪ ﻗﻨﺪ( ﺭﻭﺯﺍﻧﻪ ﻣﺼﺮﻑ ﺷﻮﺩ.
ﻧﻴﺎﺯ ﺑﻪ چﺮﺑﻲ ﻫﺎ ﺩﺭ ﻳﻚ ﺭژﻴﻢ ﻏﺬﺍﻳﻲ ﻣﺘﻌﺎﺩﻝ، ﺗﻮﺻﻴﻪ ﻣﻲ ﺷﻮﺩ ﺑﻴﻦ 52 ﺗﺎ 53 ﺩﺭﺻﺪ ﻭ ﺑﻄﻮﺭ ﻣﺘﻮﺳﻂ ﺣﺪﻭﺩ 03 ﺩﺭﺻﺪ ﺍﻧﺮژﻲ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﺭﻭﺯﺍﻧﻪ ﺍﺯ ﻃﺮﻳﻖ چﺮﺑﻲ ﻫﺎ ﺗﺎﻣﻴﻦ گﺮﺩﺩ. ﺍﻳﻦ ﻣﻘﺪﺍﺭ ﺗﻘﺮﻳﺒﺎ ﻣﻌﺎﺩﻝ ﻳﻚ گﺮﻡ چﺮﺑﻲ ﺑﺎﺯﺍﻱ ﻛﻴﻠﻮگﺮﻡ ﻭﺯﻥ ﺑﺪﻥ ﺍﺳﺖ ﻛﻪ ﺷﺒﻴﻪ ﺑﻪ ﻣﻘﺪﺍﺭ ﺗﻮﺻﻴﻪ ﺷﺪﻩ ﺩﺭﻳﺎﻓﺖ پﺮﻭﺗﺌﻴﻦ ﺭﻭﺯﺍﻧﻪ ﻣﻲ ﺑﺎﺷﺪ. ﻫﺮ گﺮﻡ چﺮﺑﻲ ﺣﺪﻭﺩ 9 ﻛﻴﻠﻮﻛﺎﻟﺮﻱ ﺍﻧﺮژﻲ ﺑﺮﺍﻱ ﺑﺪﻥ ﺗﺎﻣﻴﻦ ﻣﻲ ﻛﻨﺪ ﻭ ﺑﻨﺎﺑﺮﺍﻳﻦ ﻣﺼﺮﻑ 08 گﺮﻡ چﺮﺑﻲ ﺭﻭﺯﺍﻧﻪ ﺗﻮﺳﻂ ﺧﺎﻧﻢ ﻫﺎ ﻫﻤﺎﻥ ﻳﻚ ﺳﻮﻡ ﻧﻴﺎﺯ ﺍﻧﺮژﻲ ﺭﻭﺯﺍﻧﻪ ﺭﺍ ﺗﺎﻣﻴﻦ ﻣﻲ ﻛﻨﺪ
ﻋﻨﺎﺻﺮ ﻣﻌﺪﻧی ﻧﻴﺎﺯ ﺑﻪ ﺍﻏﻠﺐ ﻋﻨﺎﺻﺮ ﻣﻌﺪﻧﻲ ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ ﺍﻓﺰﺍﻳﺶ ﻣﻲ ﻳﺎﺑﺪ. • ﺍﻣﺎ ﺑﻄﻮﺭ ﺭﻭﺗیﻦ ﻧیﺎﺯ ﺑﻪ ﻣکﻤﻞ ﺳﺎﺯی ﻣیﻨﺮﺍﻟﻬﺎ ﺩﺭ یک ﺯﻥ ﺳﺎﻟﻢ ﻧیﺴﺖ. • ﺗﻨﻬﺎ ﺍﺳﺘﺜﻨﺎﺀ آﻬﻦ ﺍﺳﺖ.
ﻛﻠﺴﻴﻢ ﻧﻴﺎﺯ ﺑﻪ ﺩﺭﻳﺎﻓﺖ ﻛﻠﺴﻴﻢ ﺩﺭ ﺩﻭﺭﻩ ﺑﺎﺭﺩﺍﺭﻱ 05 ﺩﺭﺻﺪ ﺍﻓﺰﺍﻳﺶ ﻣﻲ ﻳﺎﺑﺪ ﻭ ﺑﻪ 0051 -0021 ﻣﻴﻠﻲ گﺮﻡ ﺩﺭ ﺭﻭﺯ ﻣﻴﺮﺳﺪ. )ﺷﻴﺮﺩﻫی 0002( ﺗﺠﻮﻳﺰ ﻭﻳﺘﺎﻣﻴﻦ ﺩ ﺍگﺮ ﻣﺼﺮﻑ ﻟﺒﻨﻴﺎﺕ، ﺳﺒﺰﻱ ﻭ ﻣﻴﻮﻩ ﻛﺎﻓﻲ ﺑﺎﺷﺪ ﺍﻳﻦ ﻧﻴﺎﺯ ﺑﺨﻮﺑﻲ ﺗﺎﻣﻴﻦ ﻣﻲ ﺷﻮﺩ. ﺩﺭﻳﺎﻓﺖ ﻧﺎﻛﺎﻓﻲ ﻛﻠﺴﻴﻢ ﺳﺒﺐ ﺑﺮﺩﺍﺷﺖ ﻛﻠﺴﻴﻢ ﺍﺯ ﺍﺳﺘﺨﻮﺍﻥ ﻫﺎﻱ ﻣﺎﺩﺭ ﻣﻴﺸﻮﺩ. گﺮچﻪ ﺑﺪﻳﻦ ﺗﺮﺗﻴﺐ ﻧﻴﺎﺯ ﺟﻨﻴﻦ ﺗﺎﻣﻴﻦ ﻣﻲ گﺮﺩﺩ، ﻭﻟﻲ ﺍﻳﻦ ﻓﺪﺍﻛﺎﺭﻱ ﺑﺪﻥ ﻣﺎﺩﺭﺳﺒﺐ پﻮﻙ ﺷﺪﻥ ﺍﺳﺘﺨﻮﺍﻥ ﻫﺎﻱ ﺯﻥ ﺑﺎﺭﺩﺍﺭ ﺧﻮﺍﻫﺪ ﺷﺪ.
آﻬﻦ کﻞ آﻬﻦ ﻣﻮﺭﺩ ﻧیﺎﺯ ﺩﺭ یک ﺣﺎﻣﻠگی 1 gr ﺍﺳﺖ. ﻣﺎﺩﺭ ﺗﺎ ﻫﻔﺘﻪ ﻫﺎﻱ پﺎﻳﺎﻧﻲ ﺑﺎﺭﺩﺍﺭﻱ ﺣﺪﻭﺩ 072 ﻣﻴﻠﻲ گﺮﻡ آﻬﻦ ﺑﻪ ﺟﻨﻴﻦ ﻣﻨﺘﻘﻞ ﻣﻲ ﻛﻨﺪ. ﻛﻪ ﺍﻳﻦ ﺳﺒﺐ ﺍﻓﺰﺍﻳﺶ ﻧﻴﺎﺯ ﻭﻱ ﺑﻪ elemental Iron ﺍﺯ 51 ﻣﻴﻠﻲ گﺮﻡ ﺑﻪ 03 ﻣﻴﻠﻲ گﺮﻡ ﺭﻭﺯﺍﻧﻪ ﻃی 3 ﻣﺎﻫﻪ ﺩﻭﻡ ﻭ ﺳﻮﻡ ﺑﺎﺭﺩﺍﺭی ﻣﻲ گﺮﺩﺩ. ﺧﻮﺭﺩﻥ ﻳک ﻗﺮﺹ ﺭﻭﺯﺍﻧﻪ ﻛﻢ ﺧﻮﻧﻲ ﻣﻴﻜﺮﻭﺳﻴﺘﻴﻚ ﻫﻴپﻮﻛﺮﻭﻣﻴﻚ ﻧﺎﺷﻲ ﺍﺯ ﻓﻘﺮ آﻬﻦ ﺩﺭ ﺑﺴﻴﺎﺭﻱ ﺍﺯ ﺯﻧﺎﻥ ﺑﺎﺭﺩﺍﺭ ﻭﺟﻮﺩ ﺩﺍﺭﺩ. ﺩﺭ ﺻﻮﺭﺕ ﻭﺟﻮﺩ IDA ﺭﻭﺯﺍﻧﻪ . 120 -60 mg ﺩﺭ ﺍﻳﻦ ﺣﺎﻟﺖ ﺭﻭﺯﺍﻧﻪ 15 mg ﺭﻭی ﻭ 2 mg ﻣﺲ ﻻﺯﻡ ﺍﺳﺖ. )ﻣﻨﻊ ﺟﺬﺏ ﺗﻮﺳﻂ آﻬﻦ(
ﻣﺼﺮﻑ ﻣﺮﺗﺐ گﻮﺷﺖ، ﺗﺨﻢ ﻣﺮﻍ، ﻧﺎﻥ ﺗﺨﻤﻴﺮ ﺷﺪﻩ، ﻭ ﺳﺒﺰﻱ ﻣﻲ ﻛﻨﺪ. ﻫﺎﻱ ﺩﺍﺭﺍﻱ ﺑﺮگ ﺳﺒﺰ ﺍﻳﻦ ﻣﻘﺪﺍﺭ ﻧﻴﺎﺯ ﺭﻭﺯﺍﻧﻪ ﺭﺍ ﺗﺎﻣﻴﻦ آﻬﻦ ﻏﺬﺍﻫﺎﻱ ﺣﻴﻮﺍﻧﻲ ﺑﺴﻴﺎﺭ ﺑﻬﺘﺮ ﺍﺯ آﻬﻦ ﻏﺬﺍﻫﺎﻱ گﻴﺎﻫﻲ ﺟﺬﺏ ﻣﻲ گﺮﺩﺩ ﻭ ﻧﻮﺷﻴﺪﻥ چﺎﻱ ﻛﻪ ﺑﻌﻠﺖ ﺩﺍﺭﺍ ﺑﻮﺩﻥ ﺗﺎﻧﻦ ﺑﺮ ﻣﻘﺪﺍﺭ ﺟﺬﺏ آﻬﻦ ﻏﺬﺍﻫﺎﻱ ﻏﻴﺮ ﻡ ﺗﺎﺛﻴﺮ ﻧﺎﻣﻄﻠﻮﺏ ﺩﺍﺭﺩ، ﺑﺮ ﺟﺬﺏ آﻬﻦ ﻡ )ﻛﻪ ﺣﺪﻭﺩ 04% آﻬﻦ ﺣﻴﻮﺍﻧﻲ ﺭﺍ ﺗﺸﻜﻴﻞ ﻣﻲﻛﻨﺪ( ﺗﺎﺛﻴﺮﻱ ﻧﺪﺍﺭﺩ.
1. ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﻴﺪ ﻓﻴﺘﻴﻚ ﻣﻮﺟﻮﺩ ﺩﺭ ﻧﺎﻧﻬﺎﻱ ﺗﺨﻤﻴﺮ ﻧﺸﺪﻩ، ﺍﺳﻴﺪ ﺍگﺰﺍﻟﻴﻚ ﻣﻮﺟﻮﺩ ﺩﺭ ﺑﻌﻀﻲ گﻴﺎﻫﺎﻥ ﺍﺯ ﻗﺒﻴﻞ ﺍﺳﻔﻨﺎﺝ، چﻐﻨﺪﺭ ﻭ ﺑﺮگ چﻐﻨﺪﺭ ﻭ ﺭﻳﻮﺍﺱ، ﻣﻮﺟﺐ ﻛﺎﻫﺶ ﺟﺬﺏ آﻬﻦ ﻣﻴگﺮﺩﺩ. 2. ﺗﺠﻮﻳﺰ آﻬﻦ ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ
ﺍﺳﻴﺪ ﻓﻮﻟﻴﻚ 1. ﺍﺯ ﻭﻳﺘﺎﻣﻴﻦ ﻫﺎﻳﻲ ﺍﺳﺖ ﻛﻪ ﻧﻘﺶ ﻣﻬﻤﻲ ﺩﺭ ﺳﺎﺧﺘﻪ ﺷﺪﻥ ﺧﻮﻥ ﻭ ﺩﺭ ﻧﺘﻴﺠﻪ پﻴﺸگﻴﺮﻱ ﺍﺯ ﻛﻢ ﺧﻮﻧﻲ ﻣﺎﻛﺮﻭﺳﻴﺘﻴﻚ )ﻣگﺎﻟﻮﺑﻼﺳﺘﻴﻚ( ﺩﺍﺭﺩ. 2. ﻓﻮﻻﺕ ﺩﺭ ﺭﻭﻧﺪ ﺗﺒﺪﻳﻞ ﺍﺳﻴﺪﻫﺎﻱ آﻤﻴﻨﻪ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﻛﻮآﻨﺰﻳﻢ ﻋﻤﻞ ﻣﻲ ﻛﻨﺪ ﻭ ﺑﻪ ﻫﻤﻴﻦ ﺩﻟﻴﻞ ﺑﺮﺍﻱ ﺳﻨﺘﺰ DNA ﻭ ﺗﻘﺴﻴﻢ ﺳﻠﻮﻟﻲ، ﺿﺮﻭﺭﻱ ﺍﺳﺖ. 3. ﺑﻪ ﻫﻤﻴﻦ ﺩﻟﻴﻞ ﺑﺮﺍﻱ ﻓﻌﺎﻟﻴﺖ ﺳﻠﻮﻝ ﻫﺎﻳﻲ ﻛﻪ ﺗﻘﺴﻴﻢ ﺳﺮﻳﻊ ﺩﺍﺭﻧﺪ ﺍﺯﺟﻤﻠﻪ گﻠﺒﻮﻝ ﻫﺎﻱ ﻗﺮﻣﺰ ﺧﻮﻥ ﻭ ﺳﻠﻮﻝ ﻫﺎﻱ ﺟﻨﻴﻨﻲ ﺑﺴﻴﺎﺭ ﺍﻫﻤﻴﺖ ﺩﺍﺭﺩ. •
1. 2. 3. 4. ﻛﻤﺒﻮﺩ ﻓﻮﻻﺕ ﺳﺒﺐ ﻧﻘﺺ ﺗﺸﻜﻴﻞ ﺍﻧﺪﺍﻡ ﻫﺎﻱ ﺟﻨﻴﻨﻲ ﺑﻮﻳژﻪ ﻟﻮﻟﻪ ﻋﺼﺒﻲ )ﺍﺯ ﻗﺒﻴﻞ ﺑﻴﻤﺎﺭﻱ ﺍﺳپﻴﻨﺎﺑﻴﻔﻴﺪﺍ( ﻣﻲ گﺮﺩﺩ. ﻓﻮﻻﺕ ﺍﺯ ﻭﻳﺘﺎﻣﻴﻦ ﻫﺎﻱ ﻣﺤﻠﻮﻝ ﺩﺭ آﺐ ﺍﺳﺖ ﻛﻪ ﻣﺼﺮﻑ ﺑﺎﻻﻱ آﻦ ﻣﺴﻤﻮﻣﻴﺖ ﻧﺪﺍﺭﺩ. ﻏﺬﺍﻫﺎﻱ گﻴﺎﻫﻲ ﻣﺜﻞ ﺳﺒﺰﻱ ﻫﺎ، ﺣﺒﻮﺑﺎﺕ ﻭ ﻫﻤچﻨﻴﻦ ﺑﺴﻴﺎﺭﻱ ﺍﺯ ﻏﺬﺍﻫﺎﻱ ﺣﻴﻮﺍﻧﻲ، ﺣﺎﻭﻱ ﻓﻮﻻﺕ ﻫﺴﺘﻨﺪ. ﺣﺮﺍﺭﺕ ﺍﻳﻦ ﻭﻳﺘﺎﻣﻴﻦ ﺭﺍ ﺗﺨﺮﻳﺐ ﻣﻲ ﻛﻨﺪ ﻭ گﺮﻓﺘﻦ ﺳﺒﻮﺱ ﻏﻼﺕ آﻨﺮﺍ ﺍﺯ ﺩﺍﻧﻪ ﺟﺪﺍ ﻣﻲ ﺳﺎﺯﺩ. 5. ﺗﺠﻮﻳﺰ ﺍﺳﻴﺪ ﻓﻮﻟﻴک ﺩﺭ ﺣﺎﻣﻠگی)0001 -008 ﻣیکﺮﻭگﺮﻡ ﺩﺭ ﺭﻭﺯ(
ﺳﺪﻳﻢ ﻣﻘﺪﺍﺭ ﻧﻤﻚ ﻃﻌﺎﻡ ﺩﺭﻳﺎﻓﺘﻲ ﺗﻮﺻﻴﻪ ﺷﺪﻩ ﺑﺮﺍﻱ ﺍﻓﺮﺍﺩ ﻣﻌﻤﻮﻟﻲ 3 ﺗﺎ 5 گﺮﻡ ﺭﻭﺯﺍﻧﻪ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﺯﻣﺎﻥ ﺑﺎﺭﺩﺍﺭﻱ ﺑﻪ 8 -7 گﺮﻡ ﻣﻴﺮﺳﺪ. ﻣﻌﻤﻮﻻ ﻣﻘﺪﺍﺭ ﻣﺼﺮﻑ ﺭﻭﺯﺍﻧﻪ ﺧﺎﻧﻢ ﻫﺎﻱ ﺑﺎﺭﺩﺍﺭ ﺑﻴﺸﺘﺮ ﺍﺯ ﺍﻳﻦ ﻣﻘﺪﺍﺭ ﺍﺳﺖ ﻭ ﺩﺭ ﺻﻮﺭﺗﻴﻜﻪ ﻣﺎﺩﺭ ﺩچﺎﺭ ﻭﺭﻡ ﺷﺪ ﺑﻬﺘﺮ ﺍﺳﺖ ﻣﺼﺮﻑ ﻧﻤﻚ ﺭﺍ ﻛﺎﻫﺶ ﺩﻫﺪ ﻭﻟﻲ ﺟﺰ ﺩﺭ ﺑﻴﻤﺎﺭﻱ ﻫﺎﻱ ﻗﻠﺒﻲ ﻋﺮﻭﻗﻲ، ﻣﻘﺪﺍﺭ ﺩﺭﻳﺎﻓﺖ ﻧﺒﺎﻳﺪ ﺑﻪ ﻛﻤﺘﺮ ﺍﺯ 8 -7 گﺮﻡ ﺭﻭﺯﺍﻧﻪ ﺑﺮﺳﺪ ﺯﻳﺮﺍ ﺧﻄﺮ ﺍﺧﺘ ﻻﺕ ﺷﺪﻳﺪ ﺩﺭ ﺗﻌﺎﺩﻝ ﻳﻮﻧﻲ ﺭﺍ ﺑﺪﻧﺒﺎﻝ ﺧﻮﺍﻫﺪ ﺩﺍﺷﺖ. ﻼ ﺩﺭ ﺷﺮﺍﻳﻂ ﻣﻌﻤﻮﻟﻲ ﺿﺮﻭﺭﺗﻲ ﺑﺮﺍﻱ ﻛﺎﻫﺶ ﻧﻤﻚ ﺩﺭﻳﺎﻓﺘﻲ ﺩﺭ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ ﻭﺟﻮﺩ ﻧﺪﺍﺭﺩ. ﺣﺘﻲ ﺩﺭ ﻣﺴﻤﻮﻣﻴﺖ ﺣﺎﻣﻠگﻲ ﻛﻪ ﻋﻮﺍﺭﺿﻲ ﺍﺯ ﻗﺒﻴﻞ ﺍﺩﻡ ﻭ پﺮﻭﺗﺌﻴﻦ ﺍﻭﺭﻱ ﻇﺎﻫﺮ ﻣﻲ ﺷﻮﺩ ﻫﻢ ﺩﻟﻴﻠﻲ ﺑﺮﺍﻱ ﻣﺤﺪﻭﺩ ﻛﺮﺩﻥ ﺳﺪﻳﻢ ﺩﺭﻳﺎﻓﺘﻲ ﻭﺟﻮﺩ ﻧﺪﺍﺭﺩ.
1. 2. 3. 4. . ﺗﻨﻬﺎ ﺩﺭ ﺻﻮﺭﺗﻲ ﻛﻪ ﻋﺎﺭﺿﻪ ﻗﻠﺒﻲ ﻳﺎ ﻓﺸﺎﺭ ﺧﻮﻥ ﺑﺎﻻ ﻭﺟﻮﺩ ﺩﺍﺷﺘﻪ ﺑﺎﺷﺪ ﻣﺤﺪﻭﺩ ﻛﺮﺩﻥ ﺳﺪﻳﻢ ﺭژﻴﻢ، ﺿﺮﻭﺭﻱ ﺍﺳﺖ گﺮچﻪ ﺩﺭ ﻫﻴچ ﺣﺎﻟﺘﻲ ﺭژﻴﻢ ﻧﺒﺎﻳﺪ ﺷﺪﻳﺪﺍ ﻛﻢ ﺳﺪﻳﻢ ﺑﺎﺷﺪ. ﺍﺯ ﺩﺳﺖ ﺩﺍﺩﻥ ﺳﺪﻳﻢ ﺯﻳﺎﺩ، ﺧﻄﺮ ﺗﺸﺪﻳﺪ ﻣﺴﻤﻮﻣﻴﺖ ﺍﺯ ﻃﺮﻳﻖ ﻛﺎﻫﺶ ﺣﺠﻢ ﺧﻮﻥ ﺭﺍ ﺩﺭ پﻲ ﺧﻮﺍﻫﺪ ﺩﺍﺷﺖ ﻛﻪ ﺍﻳﻦ ﺧﻮﺩ ﻣﻮﺟﺐ ﺗﺮﺷﺢ ﺯﻳﺎﺩ ﺭﻧﻴﻦ ﻭ ﺍﻓﺰﺍﻳﺶ ﻓﺸﺎﺭ ﺧﻮﻥ ﺧﻮﺍﻫﺪ ﺑﻮﺩ. ﺑﻬﺘﺮ ﺍﺳﺖ ﺑﻪ ﻣﻮﺍﺯﺍﺕ ﻛﺎﻫﺶ ﺳﺪﻳﻢ، ﺩﺭﻳﺎﻓﺖ پﺘﺎﺳﻴﻢ ﺍﻓﺰﺍﻳﺶ ﻳﺎﺑﺪ ﻭ ﺍﺯ ﻣﺼﺮﻑ ﻗﻬﻮﻩ، ﺍﻟﻜﻞ ﻭ چﺮﺑﻲ ﻫﺎﻱ ﺍﺷﺒﺎﻉ ﻧﻴﺰ پﺮﻫﻴﺰ گﺮﺩﺩ. ﺑﺴﻴﺎﺭﻱ ﺍﺯ ﻏﺬﺍﻫﺎﻱ آﻤﺎﺩﻩ، ﺩﺍﺭﺍﻱ ﻣﻘﺪﺍﺭ ﺯﻳﺎﺩﻱ ﺳﺪﻳﻢ ﻫﺴﺘﻨﺪ ﻛﻪ ﺑﻪ ﻋﻨﻮﺍﻥ ﻣﺜﺎﻝ ﻣﺼﺮﻑ ﻛﻨﺴﺮﻭﻫﺎ، ﻛﺎﻟﺒﺎﺱ ﻭ ﺳﻮﺳﻴﺲ ﺩﺭ ﺯﻣﺎﻥ ﺑﺎﺭﺩﺍﺭﻱ ﺑﺎﻳﺪ ﺑﻪ ﺣﺪﺍﻗﻞ ﺑﺮﺳﺪ ﻭ ﺍﺯ ﻣﺼﺮﻑ ﻛﻨﺴﺮﻭ ﻣﺎﻫﻲ ﻫﺎ، ﺑﻴﺴﻜﻮﻳﺖ ﺷﻮﺭ، ﺯﻳﺘﻮﻥ ﺷﻮﺭ، ﺧﻴﺎﺭ ﺷﻮﺭ، پﻨﻴﺮﻫﺎﻱ ﺷﻮﺭ، ﺱ ﻫﺎﻱ ﺗﺠﺎﺭﺗﻲ ﻭ ﻣﺎﻫﻲ ﻫﺎﻱ ﻧﻤﻚ ﺳﻮﺩ، ﺧﻮﺩﺩﺍﺭﻱ ﺷﻮﺩ.
1. ﺩﺭ ﻋﻮﺽ ﺷﻴﺮ ﻭ ﻟﺒﻨﻴﺎﺕ، ﻣﻴﻮﻩ ﻫﺎﻱ ﺗﺎﺯﻩ ﻭ ﻫﻤﻴﻨﻄﻮﺭ ﺳﺒﺰﻱ ﻫﺎﻱ ﺗﺎﺯﻩ ﺍﺯ ﻧﻈﺮ ﺳﺪﻳﻢ ﻧﺴﺒﺘﺎ ﻓﻘﻴﺮ ﻫﺴﺘﻨﺪ. 2. ﻣﻮﺍﺩ ﻏﺬﺍﻳﻲ ﻏﻨﻲ ﺍﺯ پﺘﺎﺳﻴﻢ ﺷﺎﻣﻞ گﻮﺷﺖ ﻫﺎ ﻭ ﻣﻴﻮﻩ ﻫﺎ، ﻏﻼﺕ ﺑﻮﻳژﻪ ﺑﺮﻧﺞ، ﺳﺒﺰﻱ ﻫﺎ ﻭ ﺻﻴﻔﻲ ﻫﺎ، ﻣﻴﻮﻩ ﻫﺎﻱ ﺗﺎﺯﻩ ﻭ ﺧﺸﻚ ﻭ آﺸﺎﻣﻴﺪﻧﻲ ﻫﺎ ﻫﺴﺘﻨﺪ. 3. ﻭﻗﺘﻲ ﻗﺮﺍﺭ ﺍﺳﺖ ﻣﻘﺪﺍﺭ ﻛﻤﺘﺮﻱ ﻧﻤﻚ ﺑﻪ ﻏﺬﺍ ﺯﺩﻩ ﺷﻮﺩ ﺑﻬﺘﺮ ﺍﺳﺖ ﺍﺯ آﺐ پﺰ ﻛﺮﺩﻥ ﻏﺬﺍ ﻛﻪ آﻨﺮﺍ ﺧﻮﺵ ﻃﻌﻢ ﻧﻤﻲ ﻛﻨﺪ پﺮﻫﻴﺰ ﺷﺪﻩ ﻭ ﺩﺭ ﻋﻮﺽ ﻏﺬﺍ ﺑﺨﺎﺭپﺰ، ﻛﺒﺎﺏ ﻭ ﻳﺎ ﺩﻡ ﺷﻮﺩ )ﺩﺭ آﺐ ﺧﻮﺩﺵ ﺑپﺰﺩ(. 4. ﻣﺎﻫﻲ ﻫﺎ ﺣﺘﻲ ﺍﻧﻮﺍﻉ ﺩﺭﻳﺎﻳﻲ آﻦ )ﺑﺠﺰ ﻣﺎﻫﻲ ﺣﻠﻮﺍ( ﺳﺪﻳﻢ ﺑﻴﺸﺘﺮ ﺍﺯ گﻮﺷﺖ ﻗﺮﻣﺰ ﻧﺪﺍﺭﻧﺪ
ﺭﻭی • • • کﻤﺒﻮﺩ ﺩﺭﺣﺎﻣﻠگی ﻣﻤکﻦ ﺍﺳﺖ ﺗﺮﺍﺗﻮژﻦ ﺑﺎﺷﺪ. ﺳﻄﺢ ﺭﻭی ﺩﺭ ﻣﺎیﻊ آﻤﻨیﻮﺗیک ﺑﺎ ﻓﻌﺎﻟیﺖ ﺿﺪ ﻣیکﺮﻭﺑی ﻫﻤﺒﺴﺘگی ﺩﺍﺭﺩ. کﻤﺒﻮﺩ ﻣﺼﺮﻑ ﺭﻭی ﻫﻤﺮﺍﻩ ﺑﺎ IUGR ﺩیﺪﻩ ﺷﺪﻩ ﺍﺳﺖ)ﻧﻪ ﺍیﻨکﻪ ﺑﺎﻋﺚ آﻦ ﺷﻮﺩ. ( ﺍﻓﺰﺍیﺶ ﻧیﺎﺯ ﺭﻭﺯﺍﻧﻪ ﺍﺯ 51 ﺑﻪ 02 ﻣیﻠی گﺮﻡ یﺪ: ﺑﺎ ﻣﺼﺮﻑ ﻧﻤک یﺪ ﺩﺍﺭ کﺎﻓی ﺍﺳﺖ.
ﻣﺼﺮﻑ ﻏﺬﺍﻫﺎﻱ ﻣﺤﺮﻙ 1. 2. 3. 4. ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ ﻭ ﺑﻮﻳژﻪ ﺍﻭﺍﺧﺮ آﻦ ﺗﻮﺍﻡ ﺍﺳﺖ ﺑﺎ ﻓﺸﺎﺭ ﺑﻪ ﺩﺳﺘگﺎﻩ گﻮﺍﺭﺵ ﻛﻪ ﺩﺭ ﻧﺘﻴﺠﻪ ﻇﻬﻮﺭ ﺑﺮﺧﻲ ﻋﻮﺍﺭﺽ گﻮﺍﺭﺷﻲ، ﺍﺟﺘﻨﺎﺏ ﻧﺎپﺬﻳﺮ ﺍﺳﺖ. ﻧﻮﺷﻴﺪﻥ ﺯﻳﺎﺩ چﺎﻱ ﻭ ﻗﻬﻮﻩ ﻭ ﻫﻤچﻨﻴﻦ ﻣﺼﺮﻑ ﺯﻳﺎﺩ ﺍﺩﻭﻳﻪ ﻫﺎ ﻭ ﺑﻮﻳژﻪ ﻓﻠﻔﻞ ﺩﺭ ﺍﻳﻦ ﺩﻭﺭﺍﻥ ﻣﺸﻜﻞ ﺭﺍ ﺣﺎﺩﺗﺮ ﻣﻴﻜﻨﺪ. آﻠﻜﺎﻟﻮﺋﻴﺪﻫﺎﻱ ﻣﻮﺟﻮﺩ ﺩﺭ چﺎﻱ ﻭ ﻗﻬﻮﻩ ﺍﺯ ﻗﺒﻴﻞ ﺗﺌﻴﻦ ﻭ ﻛﺎﻓﺌﻴﻦ، ﻋﻼﻭﻩ ﺑﺮ ﺍﺧﺘﻼﻝ ﺩﺳﺘگﺎﻩ گﻮﺍﺭﺵ ﺳﺒﺐ ﻛﻢ ﺧﻮﺍﺑﻲ ﻧﻴﺰ ﻣﻲ ﺷﻮﺩ. ﻣﺼﺮﻑ ﺍﺩﻭﻳﻪ ﺳﺒﺐ ﺳﻮﺯﺵ ﻣﻌﺪﻩ ﻭ ﺗﺤﻳﻚ ﻣﺠﺎﺭﻱ ﺍﺩﺭﺍﺭﻱ ﻭ ﻫﻤچﻨﻴﻦ ﻭﺭﻡ ﻣﺜﺎﻧﻪ ﻣﻲ ﺷﻮﺩ ﻭ ﻗﺎﺑﻞ ﺗﻮﺻﻴﻪ ﻧﻤﻲ ﺑﺎﺷﺪ.
ﻣﺼﺮﻑ ﻓﻴﺒﺮﻫﺎﻱ ﻏﺬﺍﻳﻲ 1. 2. 3. 4. ﻋﻼﻭﻩ ﺑﺮ ﺩﺭﺷﺖ ﻣﻐﺬﻱ ﻫﺎ ﻭ ﺭﻳﺰﻣﻐﺬﻱ ﻫﺎ، ﻣﺼﺮﻑ ﻓﻴﺒﺮﻫﺎﻱ ﻏﺬﺍﻳﻲ ﻛﻪ آﺐ ﺭﺍ ﺩﺭ ﺧﻮﺩ ﻧگﻬﺪﺍﺷﺘﻪ ﻭ ﺣﺠﻢ ﻣﺪﻓﻮﻉ ﺭﺍ ﺯﻳﺎﺩ ﻣﻲ ﻛﻨﻨﺪ ﺿﺮﻭﺭﻱ ﺍﺳﺖ. ﻓﻴﺒﺮﻫﺎ ﻋﻼﻭﻩ ﺑﺮ ﺳﺮﻋﺖ ﺩﺍﺩﻥ ﺑﻪ ﺣﺮﻛﺖ ﻣﻮﺍﺩ ﺩﺭ ﺭﻭﺩﻩ ﻫﺎ، ﻣﻮﺍﺩ ﺳﻤﻲ ﺩﺭﻭﻥ ﺭﻭﺩﻩ ﻫﺎ ﺭﺍ ﻧﻴﺰ ﺟﺬﺏ ﻭ ﺑﻪ ﻫﻤﺮﺍﻩ ﺧﻮﺩ ﺩﻓﻊ ﻣﻲ ﻛﻨﻨﺪ. ﺍﺯ آﻨﺠﺎ ﻛﻪ ﺷﺪﺕ ﻭ ﺳﺮﻋﺖ ﻓﻌﺎﻟﻴﺖ ﺩﺳﺘگﺎﻩ گﻮﺍﺭﺵ ﺯﻥ ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ ﻛﺎﻫﺶ ﻣﻲ ﻳﺎﺑﺪ، ﻣﺼﺮﻑ ﻣﻮﺍﺩ ﻓﻴﺒﺮﻱ، ﺑﺴﻴﺎﺭ ﺿﺮﻭﺭﻱ ﺧﻮﺍﻫﺪ ﺑﻮﺩ. ﻣﻨﺒﻊ ﺍﺻﻠﻲ ﻓﻴﺒﺮﻫﺎﻱ ﻏﺬﺍﻳﻲ ﺳﺒﻮﺱ ﻏﻼﺕ، ﺳﺒﺰﻱ ﻫﺎ، ﻭ ﻣﻴﻮﻩ ﻫﺎ ﻫﺴﺘﻨﺪ ﻛﻪ ﻋﻼﻭﻩ ﺑﺮ ﻓﻴﺒﺮﻫﺎﻱ ﻏﺬﺍﻳﻲ، ﻣﻘﺎﺩﻳﺮﻱ ﻭﻳﺘﺎﻣﻴﻦ ﻫﺎﻱ ﺿﺮﻭﺭﻱ ﺭﺍ ﻧﻴﺰ ﺑﺮﺍﻱ ﺑﺪﻥ ﺗﺎﻣﻴﻦ ﻣﻲ ﻧﻤﺎﻳﻨﺪ.
ﻣﺎﻳﻌﺎﺕ ﻣﺼﺮﻓﻲ 1. 2. 3. 4. ﻋﻼﻭﻩ ﺑﺮ آﺒﻲ ﻛﻪ ﺍﺯ ﻃﺮﻳﻖ ﻏﺬﺍﻫﺎ ﺑﻪ ﺑﺪﻥ ﻣﻴﺮﺳﻨﺪ ﺩﺭ ﺩﻭﺭﺍﻥ ﺑﺎﺭﺩﺍﺭﻱ ﻣﺼﺮﻑ ﺭﻭﺯﺍﻧﻪ 2 -1/5 ﻟﻴﺘﺮ آﺐ ﺿﺮﻭﺭﻱ ﺍﺳﺖ. ﺍﻳﻦ ﻣﻘﺪﺍﺭ آﺐ ﺍﺯ ﻃﺮﻳﻖ ﻧﻮﺷﻴﺪﻥ آﺐ ﻭ ﺩﻳگﺮ ﻣﺎﻳﻌﺎﺗﻲ چﻮﻥ چﺎﻱ ﻳﺎ ﻗﻬﻮﻩ، آﺶ ﻳﺎ ﺳﻮپ، ﻭ آﺸﺎﻣﻴﺪﻧﻲ ﻫﺎﻱ ﻣﺨﺘﻠﻒ، ﺗﺎﻣﻴﻦ ﻣﻲ ﺷﻮﺩ. ﻧﻮﺷﻴﺪﻥ ﻫﺮ ﻧﻮﻉ ﻧﻮﺷﺎﺑﻪ گﺎﺯ ﺩﺍﺭ ﻭ ﺣﺘﻲ آﺐ گﺎﺯ ﺩﺍﺭ ﺷﺪﻩ ﺳﺒﺐ ﻧﻔﺦ ﺷﺪﻩ، ﻫﻀﻢ ﺭﺍ ﻣﺨﺘﻞ ﻣﻲ ﻛﻨﺪ
ﻭﻳﺘﺎﻣﻴﻨﻬﺎ • ﻧﻴﺎﺯ ﺑﻪ ﺍﻏﻠﺐ ﻭﻳﺘﺎﻣﻴﻨﻬﺎ ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ ﺍﻓﺰﺍﻳﺶ ﻣﻲ ﻳﺎﺑﺪ. • ﺍﻟﺒﺘﻪ ﺧﺎﻧﻤی کﻪ ﺭژیﻢ ﻏﺬﺍیی ﻣﺘﻌﺎﺩﻟی ﺩﺍﺭﺩ ﺑﻄﻮﺭ ﺭﻭﺗیﻦ ﻧیﺎﺯ ﺑﻪ ﻣکﻤﻞ ﻭیﺘﺎﻣیﻨی ﻧﺪﺍﺭﺩ. )0021 008( Vitamin D •
cd5b76d3348f4c63d41dbd7cbf4c2cec.ppt