37a9694b07d3a77a404a796977167db2.ppt
- Количество слайдов: 139
 Victor Politi, M. D. , FACP Medical Director, SVCMC Division of Allied Health, Physician Assistant Program
Victor Politi, M. D. , FACP Medical Director, SVCMC Division of Allied Health, Physician Assistant Program
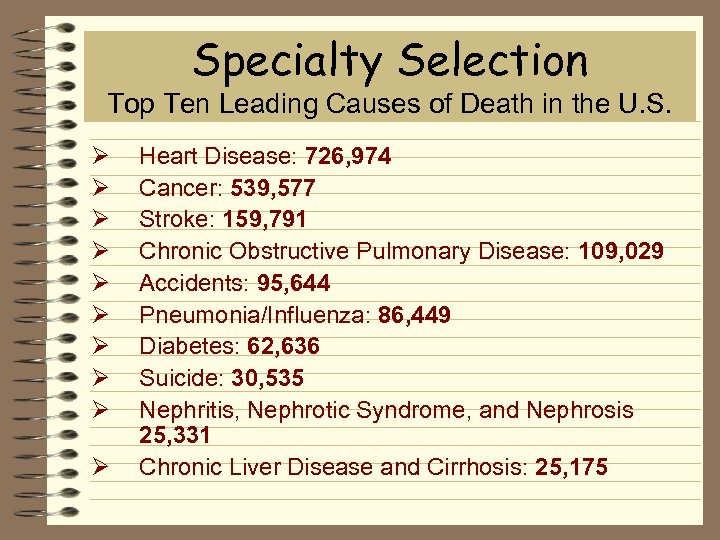 Specialty Selection Top Ten Leading Causes of Death in the U. S. Ø Ø Ø Ø Ø Heart Disease: 726, 974 Cancer: 539, 577 Stroke: 159, 791 Chronic Obstructive Pulmonary Disease: 109, 029 Accidents: 95, 644 Pneumonia/Influenza: 86, 449 Diabetes: 62, 636 Suicide: 30, 535 Nephritis, Nephrotic Syndrome, and Nephrosis 25, 331 Chronic Liver Disease and Cirrhosis: 25, 175
Specialty Selection Top Ten Leading Causes of Death in the U. S. Ø Ø Ø Ø Ø Heart Disease: 726, 974 Cancer: 539, 577 Stroke: 159, 791 Chronic Obstructive Pulmonary Disease: 109, 029 Accidents: 95, 644 Pneumonia/Influenza: 86, 449 Diabetes: 62, 636 Suicide: 30, 535 Nephritis, Nephrotic Syndrome, and Nephrosis 25, 331 Chronic Liver Disease and Cirrhosis: 25, 175
 Appeal of Emergency Medicine Ø Make an immediate difference Ø Life threatening injuries and illnesses Ø Undifferentiated patient population Ø Challenge of “anything” coming in Ø Emergency / invasive procedures Ø Safety net of healthcare
Appeal of Emergency Medicine Ø Make an immediate difference Ø Life threatening injuries and illnesses Ø Undifferentiated patient population Ø Challenge of “anything” coming in Ø Emergency / invasive procedures Ø Safety net of healthcare
 Appeal of Emergency Medicine Ø Team approach Ø Patient advocacy Ø Open job market Ø Academic opportunities Ø Shift work / set hours Ø Evolving specialty
Appeal of Emergency Medicine Ø Team approach Ø Patient advocacy Ø Open job market Ø Academic opportunities Ø Shift work / set hours Ø Evolving specialty
 Downside to Emergency Medicine Ø Interaction with difficult, intoxicated, or violent patients Ø Finding follow-up or care for uninsured Ø Work in a “fishbowl” without 20/20 hindsight Ø Working as a patient advocate
Downside to Emergency Medicine Ø Interaction with difficult, intoxicated, or violent patients Ø Finding follow-up or care for uninsured Ø Work in a “fishbowl” without 20/20 hindsight Ø Working as a patient advocate
 Subspecialties in Emergency Medicine Ø Pediatric Emergency Medicine Ø Toxicology Ø Emergency Medical Services Ø Sports Medicine
Subspecialties in Emergency Medicine Ø Pediatric Emergency Medicine Ø Toxicology Ø Emergency Medical Services Ø Sports Medicine
 Areas of Expertise Ø Toxicology Ø Emergency medical services Ø Mass gatherings Ø Disaster management Ø Wilderness medicine
Areas of Expertise Ø Toxicology Ø Emergency medical services Ø Mass gatherings Ø Disaster management Ø Wilderness medicine
 Upcoming Areas of Emergency Medicine Ø Hyperbaric medicine Ø Observation units Ø ED ultrasound Ø International emergency medicine
Upcoming Areas of Emergency Medicine Ø Hyperbaric medicine Ø Observation units Ø ED ultrasound Ø International emergency medicine
 Introduction to Trauma
Introduction to Trauma
 Trauma is a major cause of death in young people. The cost in human lives and economic terms is tremendous
Trauma is a major cause of death in young people. The cost in human lives and economic terms is tremendous
 Ø Trauma is the leading cause of death for all age groups under the age of 44 Ø In the US - it is the leading cause of death in children
Ø Trauma is the leading cause of death for all age groups under the age of 44 Ø In the US - it is the leading cause of death in children
 Trauma Statistics ð 4 th leading cause of death of Americans of all ages ð Nearly 150, 000 people of all ages in the US die from trauma each year • 60 million injuries annually • 30 million need medical treatment • 3. 6 million need hospitalization
Trauma Statistics ð 4 th leading cause of death of Americans of all ages ð Nearly 150, 000 people of all ages in the US die from trauma each year • 60 million injuries annually • 30 million need medical treatment • 3. 6 million need hospitalization
 Trauma Statistics Ø Impact of trauma is greatest in children and young adults Ø Trauma cost the American public over $300 billion annually including lost wages, medical expenses, administrative costs, employer expense Ø Approximately 40% of health care monies are spent on trauma
Trauma Statistics Ø Impact of trauma is greatest in children and young adults Ø Trauma cost the American public over $300 billion annually including lost wages, medical expenses, administrative costs, employer expense Ø Approximately 40% of health care monies are spent on trauma
 Trauma Statistics Ø Traumatic injuries, including unintentional injuries cause ð 43% of all deaths ages 1 to 4 ð 49% of all deaths ages 5 to 14 ð 64% of all deaths ages 15 to 24
Trauma Statistics Ø Traumatic injuries, including unintentional injuries cause ð 43% of all deaths ages 1 to 4 ð 49% of all deaths ages 5 to 14 ð 64% of all deaths ages 15 to 24
 Trauma Statistics Ø Leading cause of accidental death in US - motor vehicle accidents ðdrinking is a factor in 49% of these cases
Trauma Statistics Ø Leading cause of accidental death in US - motor vehicle accidents ðdrinking is a factor in 49% of these cases
 Trauma Statistics Ø Falls ð 2 nd leading cause of accidental death for ages 45 to 75 years and ð #1 cause of unintentional death for persons age 75 and older
Trauma Statistics Ø Falls ð 2 nd leading cause of accidental death for ages 45 to 75 years and ð #1 cause of unintentional death for persons age 75 and older
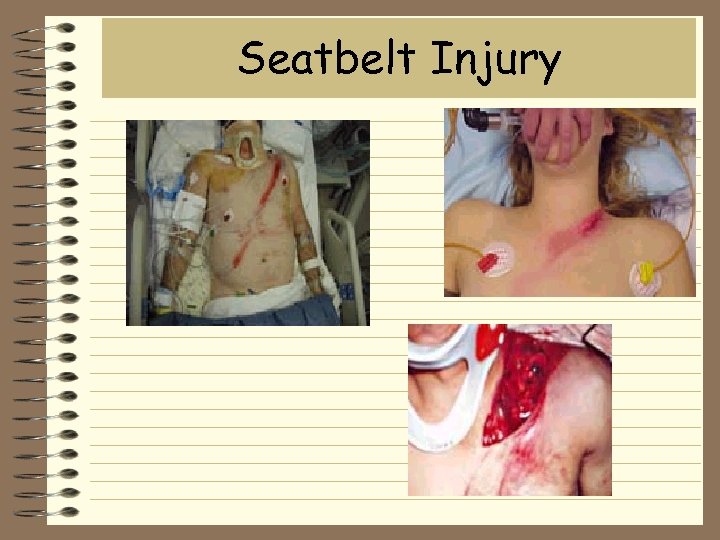 Seatbelt Injury
Seatbelt Injury
 Trauma Statistics Ø Drowning is the 4 th most common cause of unintentional injury death for all ages ð It ranks 1 st for persons age 25 to 44 ð It ranks 2 nd for ages 5 to 44
Trauma Statistics Ø Drowning is the 4 th most common cause of unintentional injury death for all ages ð It ranks 1 st for persons age 25 to 44 ð It ranks 2 nd for ages 5 to 44
 Designated Trauma Centers Ø Designated Trauma Centers ð Immediate availability of necessary resources ð Designated • • Regional Area Level II
Designated Trauma Centers Ø Designated Trauma Centers ð Immediate availability of necessary resources ð Designated • • Regional Area Level II
 Tri-modal distribution of Trauma Death Ø First peak: second - minutes ð brain injury, high spinal cord, large vessels, cardiac arrest ð best treated by prevention Ø Second peak: minutes - hours ð sub/epidurals, HTX/PTX, spleen, liver lac ð best treated by applying principles of ATLS Ø Third peak: days-weeks ð sepsis, multi-organ failure ð directly correlated to earlier Rx
Tri-modal distribution of Trauma Death Ø First peak: second - minutes ð brain injury, high spinal cord, large vessels, cardiac arrest ð best treated by prevention Ø Second peak: minutes - hours ð sub/epidurals, HTX/PTX, spleen, liver lac ð best treated by applying principles of ATLS Ø Third peak: days-weeks ð sepsis, multi-organ failure ð directly correlated to earlier Rx
 Primary Evaluation Ø Airway maintenance with c-spine control Ø Breathing and ventilation Ø Circulation with hemorrhage control Ø Disability or neurological status Ø Exposure and environmental control
Primary Evaluation Ø Airway maintenance with c-spine control Ø Breathing and ventilation Ø Circulation with hemorrhage control Ø Disability or neurological status Ø Exposure and environmental control
 Ø Control the airway with basic maneuvers ð suction ð administer 100% oxygen ð hyperventilate ð prepare to intubate ð paralyze the patient ð use appropriate Rx considering ? elevated ICP ð intubate, maintaining in-line traction
Ø Control the airway with basic maneuvers ð suction ð administer 100% oxygen ð hyperventilate ð prepare to intubate ð paralyze the patient ð use appropriate Rx considering ? elevated ICP ð intubate, maintaining in-line traction
 Circulation Ø Control exsanguinating hemorrhage Ø control external bleeding promptly Ø establish at least 2 R. L. wide-bore Ivs ð large diameter/short length Ivs ð ideally 14 ga. 1 1/4” ð add pressure bags
Circulation Ø Control exsanguinating hemorrhage Ø control external bleeding promptly Ø establish at least 2 R. L. wide-bore Ivs ð large diameter/short length Ivs ð ideally 14 ga. 1 1/4” ð add pressure bags
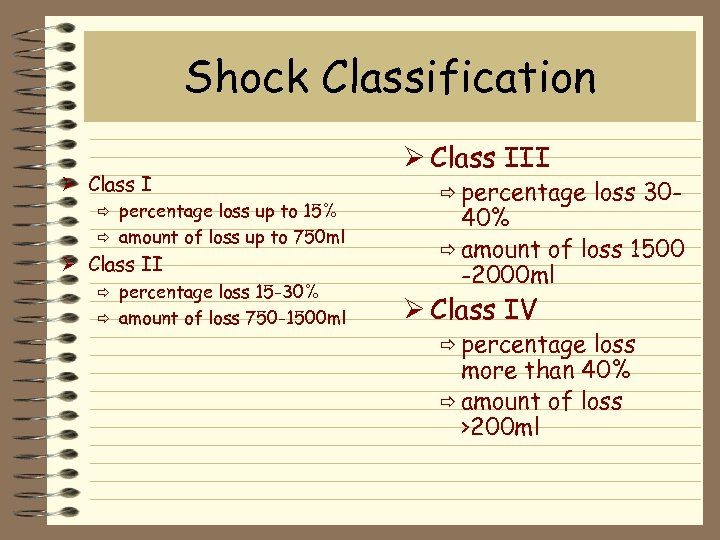 Shock Classification Ø Class I percentage loss up to 15% ð amount of loss up to 750 ml ð Ø Class II percentage loss 15 -30% ð amount of loss 750 -1500 ml ð Ø Class III ð percentage loss 30 - 40% ð amount of loss 1500 -2000 ml Ø Class IV ð percentage loss more than 40% ð amount of loss >200 ml
Shock Classification Ø Class I percentage loss up to 15% ð amount of loss up to 750 ml ð Ø Class II percentage loss 15 -30% ð amount of loss 750 -1500 ml ð Ø Class III ð percentage loss 30 - 40% ð amount of loss 1500 -2000 ml Ø Class IV ð percentage loss more than 40% ð amount of loss >200 ml
 Treatment of Hemorrhagic Shock due to trauma Ø Defined as B/P less than 90 systolic in an adult Ø The treatment of shock should be directed not toward the class of shock but to the response to initial therapy
Treatment of Hemorrhagic Shock due to trauma Ø Defined as B/P less than 90 systolic in an adult Ø The treatment of shock should be directed not toward the class of shock but to the response to initial therapy
 Class III Blood Loss Ø Respond to initial fluid bolus ð was initial bolus inadequate? ð is patient experiencing ongoing hemorrhage? Ø As fluids are slowed, patient deteriorates
Class III Blood Loss Ø Respond to initial fluid bolus ð was initial bolus inadequate? ð is patient experiencing ongoing hemorrhage? Ø As fluids are slowed, patient deteriorates
 Class III Blood Loss Ø Usually indicates 20 -40% blood loss Ø Requires continued fluids, blood products Ø The response to blood products dictates speed of surgical intervention
Class III Blood Loss Ø Usually indicates 20 -40% blood loss Ø Requires continued fluids, blood products Ø The response to blood products dictates speed of surgical intervention
 Fingertip amputation
Fingertip amputation
 Identify the Site Ø Most obvious source is external hemorrhage Ø Next consider hemothorax Ø Consider abdominal source ð spleen laceration ð hemoperitoneum ð renal hematoma ð liver laceration ð injury to a great vessel
Identify the Site Ø Most obvious source is external hemorrhage Ø Next consider hemothorax Ø Consider abdominal source ð spleen laceration ð hemoperitoneum ð renal hematoma ð liver laceration ð injury to a great vessel
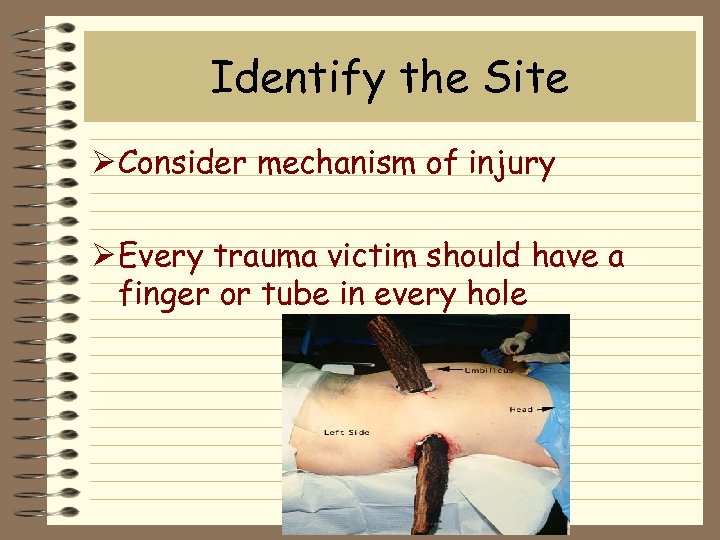 Identify the Site Ø Consider mechanism of injury Ø Every trauma victim should have a finger or tube in every hole
Identify the Site Ø Consider mechanism of injury Ø Every trauma victim should have a finger or tube in every hole
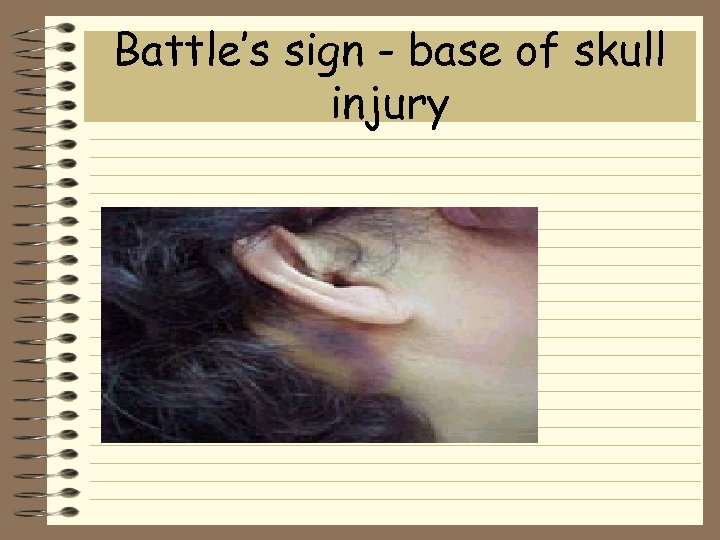 Battle’s sign - base of skull injury
Battle’s sign - base of skull injury
 'Racoon Eyes' sign of base of skull fracture
'Racoon Eyes' sign of base of skull fracture
 Minimal or No Response to Fluid Resuscitation Ø Seen in small percentage of patients Ø usually dictates need for immediate surgical intervention to control exsanguinating hemorrhage Ø Prepare the OR Ø If penetrating chest trauma consider cardiac injury
Minimal or No Response to Fluid Resuscitation Ø Seen in small percentage of patients Ø usually dictates need for immediate surgical intervention to control exsanguinating hemorrhage Ø Prepare the OR Ø If penetrating chest trauma consider cardiac injury
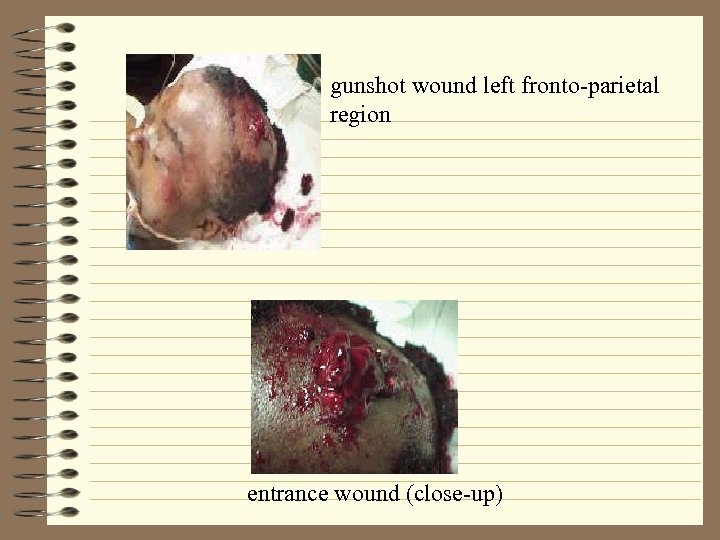 gunshot wound left fronto-parietal region entrance wound (close-up)
gunshot wound left fronto-parietal region entrance wound (close-up)
 Golden Hour Ø The hemodynamically unstable trauma patient needs only two things … ð hot lights ð cold steel
Golden Hour Ø The hemodynamically unstable trauma patient needs only two things … ð hot lights ð cold steel
 Ø Aggressive fluid resuscitation must be initiated not when blood pressure is falling/absent but as soon as the early signs/symptoms of blood loss are suspected
Ø Aggressive fluid resuscitation must be initiated not when blood pressure is falling/absent but as soon as the early signs/symptoms of blood loss are suspected
 Ø Decreasing BP increasing pulse Ø Disorientation - confusion Ø Mechanism of injury
Ø Decreasing BP increasing pulse Ø Disorientation - confusion Ø Mechanism of injury
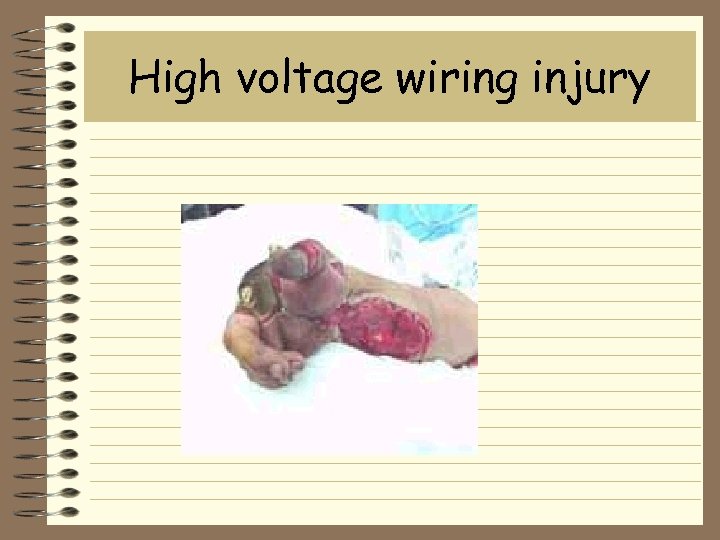 High voltage wiring injury
High voltage wiring injury
 Blood Transfusion Ø No substitute for the real thing Ø cross match if time permits Ø compatible with ABO and Rh blood types ð minor occur antibody incompatibilities may
Blood Transfusion Ø No substitute for the real thing Ø cross match if time permits Ø compatible with ABO and Rh blood types ð minor occur antibody incompatibilities may
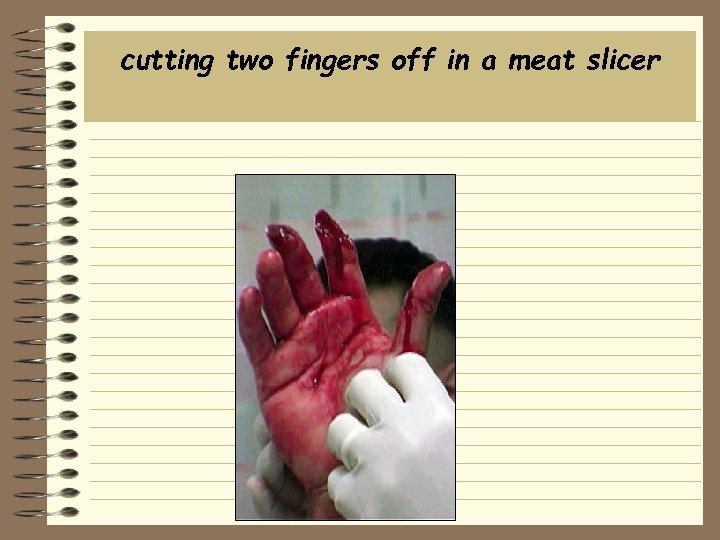 cutting two fingers off in a meat slicer
cutting two fingers off in a meat slicer
 Universal Donor Ø Type O negative is available immediately Ø used in exsanguinating hemorrhage Ø used in patient with minimal or no response to initial crystalloid fluids bolus Ø Remember ð “Give Blood Save A Life”
Universal Donor Ø Type O negative is available immediately Ø used in exsanguinating hemorrhage Ø used in patient with minimal or no response to initial crystalloid fluids bolus Ø Remember ð “Give Blood Save A Life”
 Radiologic Studies Ø C-spine, chest and pelvis x-rays Ø CAT scan or specific x-rays that are indicated based on mechanism of injury and primary exam
Radiologic Studies Ø C-spine, chest and pelvis x-rays Ø CAT scan or specific x-rays that are indicated based on mechanism of injury and primary exam
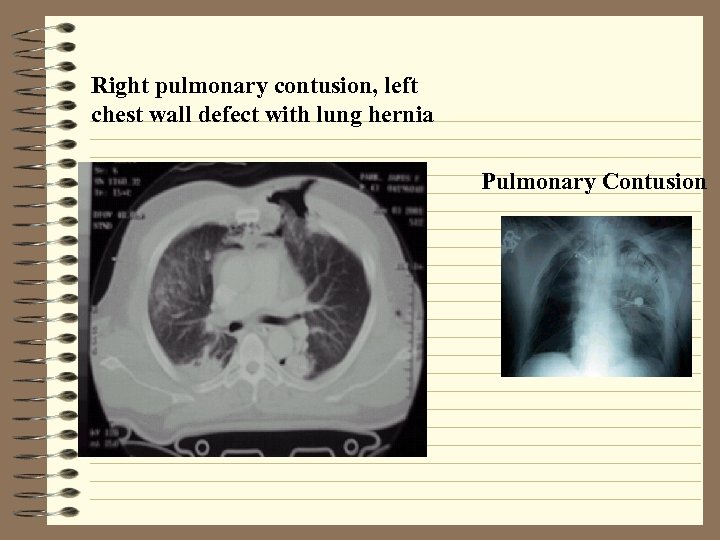 Right pulmonary contusion, left chest wall defect with lung hernia Pulmonary Contusion
Right pulmonary contusion, left chest wall defect with lung hernia Pulmonary Contusion
 C-Spine Ø Don’t become distracted by trying to clear the c-spine Ø A properly applied cervical collar never killed anyone! Ø Don’t remove cervical collar until cspine is cleared ð continue to protect c-spine during treatment
C-Spine Ø Don’t become distracted by trying to clear the c-spine Ø A properly applied cervical collar never killed anyone! Ø Don’t remove cervical collar until cspine is cleared ð continue to protect c-spine during treatment

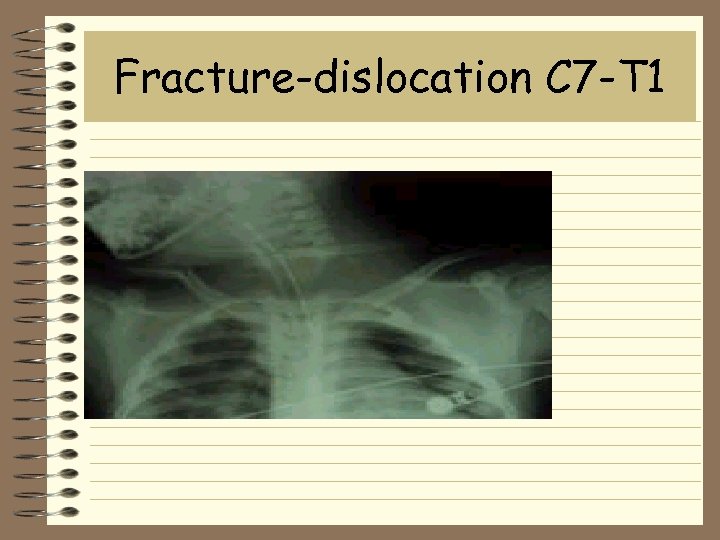 Fracture-dislocation C 7 -T 1
Fracture-dislocation C 7 -T 1
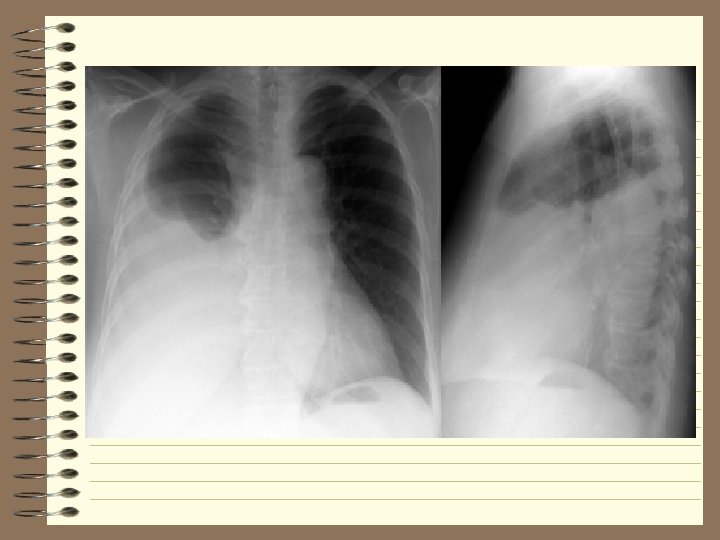
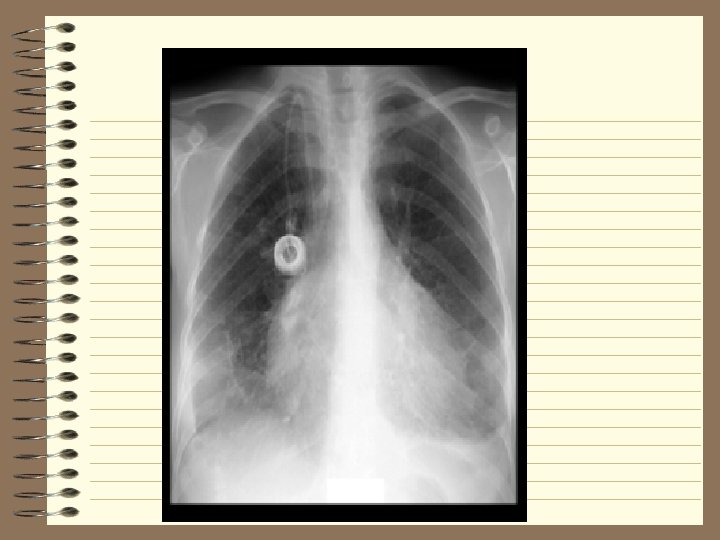
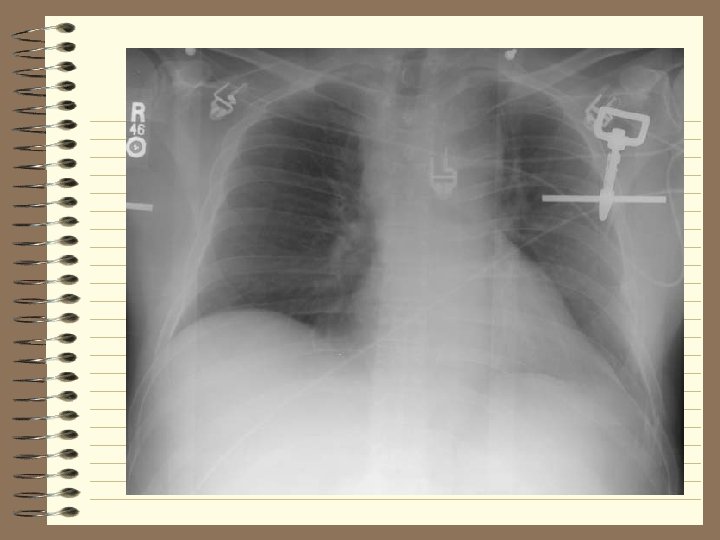
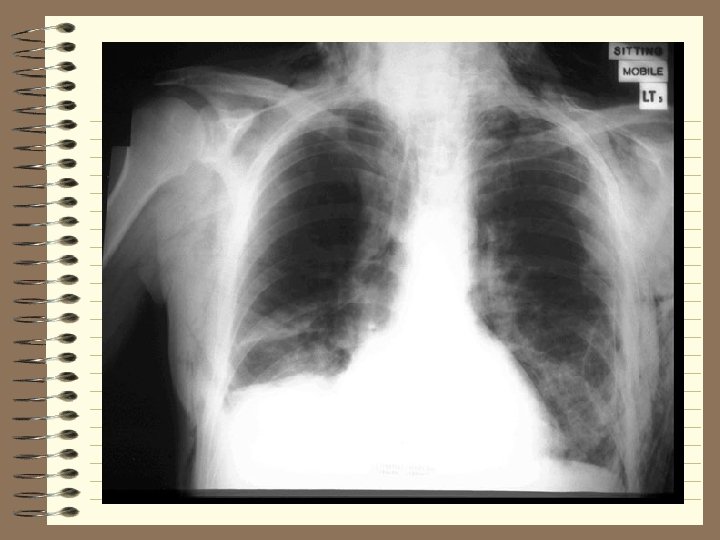
 Chest Radiograph Ø Rule-out PTX/HTX - need immediate treatment Ø Provides clues as to condition of ð heart, lung, parenchyma, mediastinum, great vessels, bronchus, diaphragm Ø Almost unheard of to have significant chest injury w/o signs of same on CXR ð CXR are frequently misinterpreted and injuries are frequently overlooked
Chest Radiograph Ø Rule-out PTX/HTX - need immediate treatment Ø Provides clues as to condition of ð heart, lung, parenchyma, mediastinum, great vessels, bronchus, diaphragm Ø Almost unheard of to have significant chest injury w/o signs of same on CXR ð CXR are frequently misinterpreted and injuries are frequently overlooked
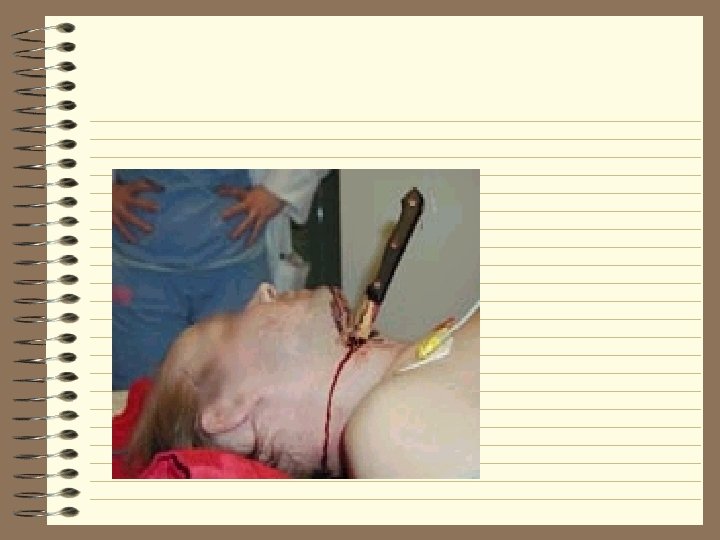
 Chest Radiograph Ø Check position of tubes Ø Locate foreign bodies (i. e. bullets) Ø Free air under diaphragm or on lateral means perforated viscus Ø Cardiac tamponade
Chest Radiograph Ø Check position of tubes Ø Locate foreign bodies (i. e. bullets) Ø Free air under diaphragm or on lateral means perforated viscus Ø Cardiac tamponade
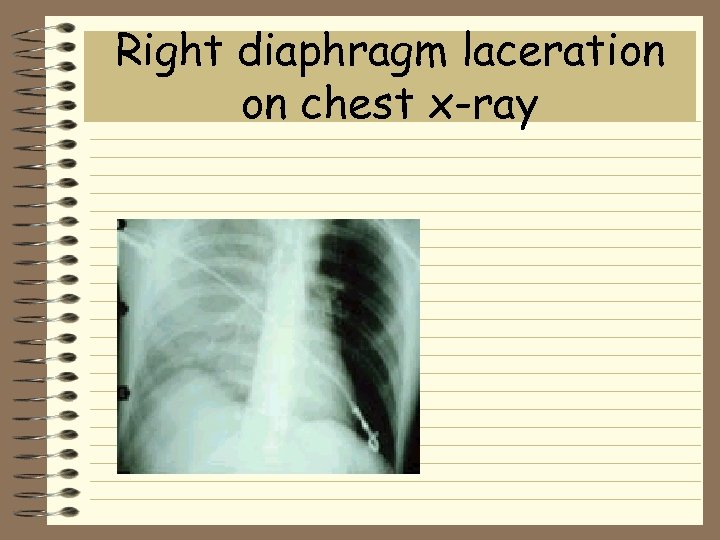 Right diaphragm laceration on chest x-ray
Right diaphragm laceration on chest x-ray
 Abdominal Trauma Ø Remove all clothing including undergarments Ø Perform adequate visual exam for injuries Ø Don’t forget the rectal exam
Abdominal Trauma Ø Remove all clothing including undergarments Ø Perform adequate visual exam for injuries Ø Don’t forget the rectal exam
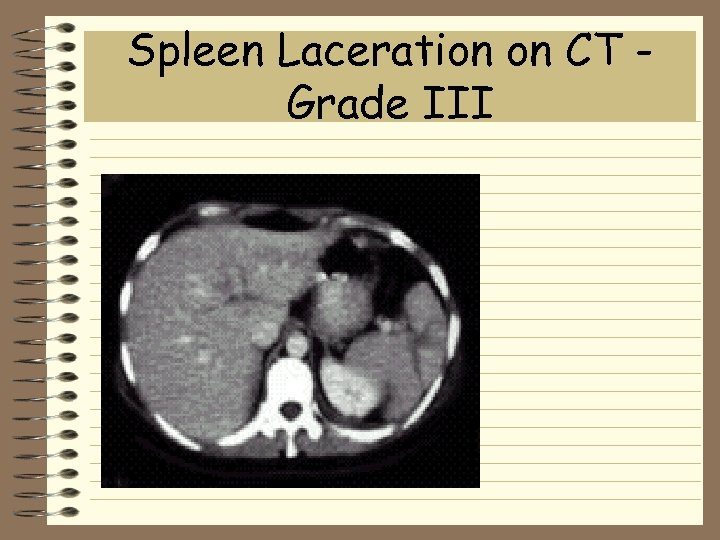 Spleen Laceration on CT Grade III
Spleen Laceration on CT Grade III
 Abdominal Trauma Ø CAT scan with contrast ð Ø Ø Ø utilizes PO and IV contrast May require NGT for administration of contrast Risk of vomiting and aspiration Risk of allergic reaction to contrast Intubation to protect airway requiring sedation Difficult to obtain CT in unstable patient
Abdominal Trauma Ø CAT scan with contrast ð Ø Ø Ø utilizes PO and IV contrast May require NGT for administration of contrast Risk of vomiting and aspiration Risk of allergic reaction to contrast Intubation to protect airway requiring sedation Difficult to obtain CT in unstable patient
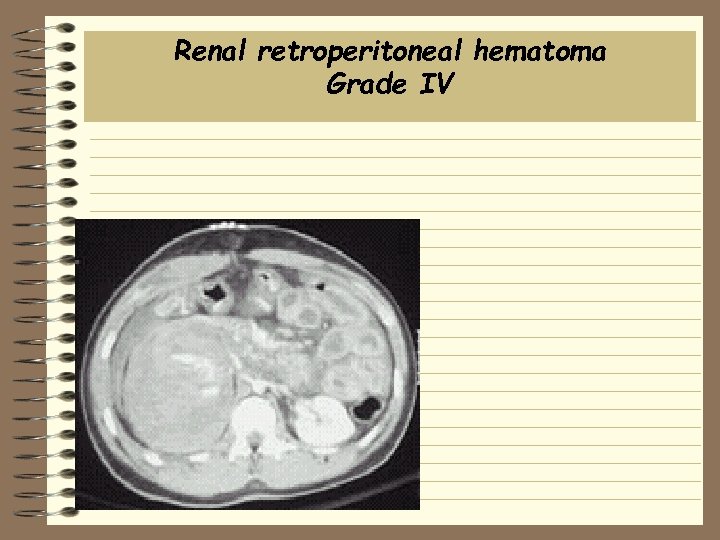 Renal retroperitoneal hematoma Grade IV
Renal retroperitoneal hematoma Grade IV
 Pelvic Trauma Ø Evaluate for pelvic, femoral neck, femur fractures Ø Provides clues as to condition of ð abdominal viscera ð bladder Ø Patients can bleed out into thigh Ø Mules and packers ð products in distal colon
Pelvic Trauma Ø Evaluate for pelvic, femoral neck, femur fractures Ø Provides clues as to condition of ð abdominal viscera ð bladder Ø Patients can bleed out into thigh Ø Mules and packers ð products in distal colon
 Ultrasound Ø Dynamic study performed in trauma room ð no need to move patient to x-ray or CT ð can immediately visualize heart, pericardium ð can visualize liver, spleen, kidney lacs ð can visualize ~ 50 cc blood, fluid in abdomen ð takes approximately 5 minutes ð highly operator dependent
Ultrasound Ø Dynamic study performed in trauma room ð no need to move patient to x-ray or CT ð can immediately visualize heart, pericardium ð can visualize liver, spleen, kidney lacs ð can visualize ~ 50 cc blood, fluid in abdomen ð takes approximately 5 minutes ð highly operator dependent

 Trauma Code: ETA 5 minutes Stick with the basics - remember ABC’s Constantly re-evaluate patient not lab’s Don’t raise your voice - remain calm You are not alone, consult the experts ð don’t get in over your head Ø Take a step back ð What are you missing ? ð What did you overlook ? Ø Ø
Trauma Code: ETA 5 minutes Stick with the basics - remember ABC’s Constantly re-evaluate patient not lab’s Don’t raise your voice - remain calm You are not alone, consult the experts ð don’t get in over your head Ø Take a step back ð What are you missing ? ð What did you overlook ? Ø Ø
 CHEST TRAUMA
CHEST TRAUMA
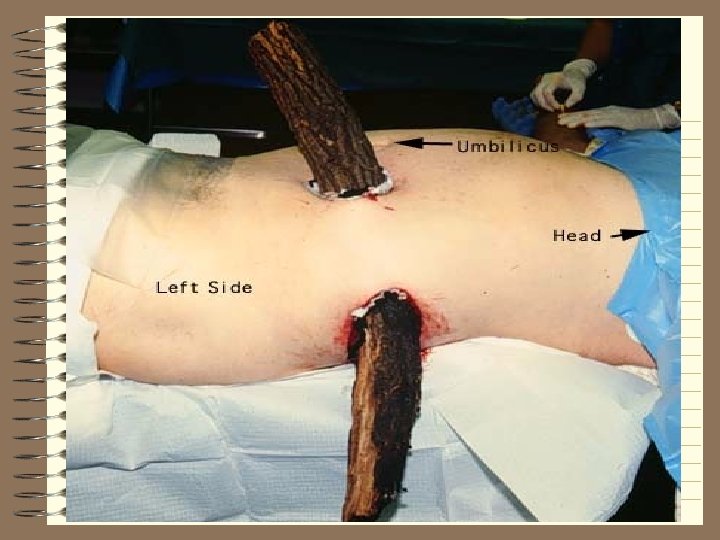
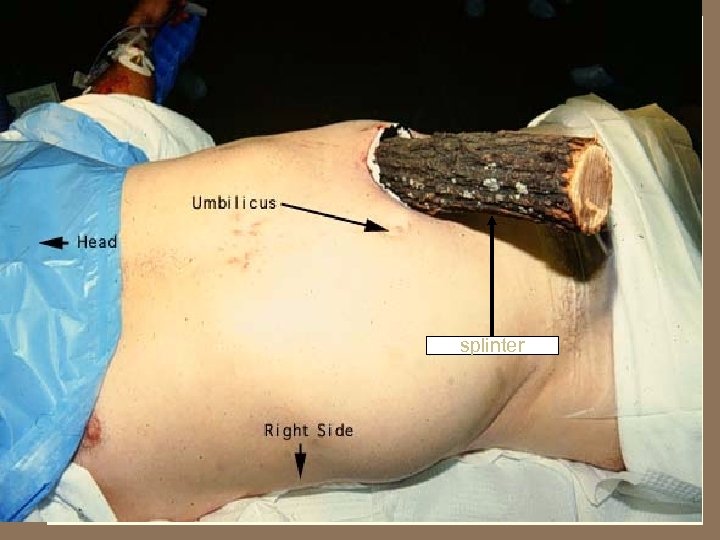 splinter
splinter
 Incidence of Chest Trauma Ø Cause 1 of 4 American trauma deaths Ø Contributes to another 1 of 4 Ø Many die after reaching hospital - could be prevented if recognized Ø <10% of blunt chest trauma needs surgery Ø 1/3 of penetrating trauma needs surgery Ø Most life-saving procedures do NOT require a thoracic surgeon
Incidence of Chest Trauma Ø Cause 1 of 4 American trauma deaths Ø Contributes to another 1 of 4 Ø Many die after reaching hospital - could be prevented if recognized Ø <10% of blunt chest trauma needs surgery Ø 1/3 of penetrating trauma needs surgery Ø Most life-saving procedures do NOT require a thoracic surgeon
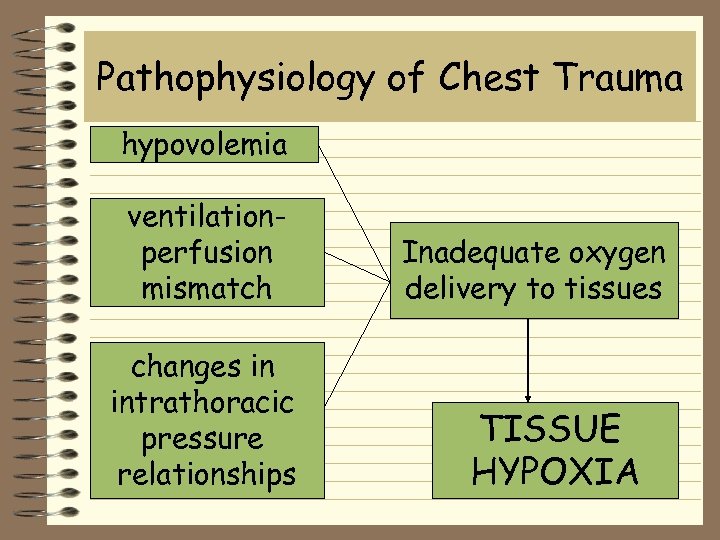 Pathophysiology of Chest Trauma hypovolemia ventilationperfusion mismatch changes in intrathoracic pressure relationships Inadequate oxygen delivery to tissues TISSUE HYPOXIA
Pathophysiology of Chest Trauma hypovolemia ventilationperfusion mismatch changes in intrathoracic pressure relationships Inadequate oxygen delivery to tissues TISSUE HYPOXIA
 Pathophysiology of Chest Trauma Ø Tissue hypoxia Ø Hypercarbia Ø Respiratory acidosis - inadequate ventilation Ø Metabolic acidosis - tissue hypoperfusion (e. g. , shock)
Pathophysiology of Chest Trauma Ø Tissue hypoxia Ø Hypercarbia Ø Respiratory acidosis - inadequate ventilation Ø Metabolic acidosis - tissue hypoperfusion (e. g. , shock)
 Initial assessment and management ØPrimary survey ØResuscitation of vital functions ØDetailed secondary survey ØDefinitive care
Initial assessment and management ØPrimary survey ØResuscitation of vital functions ØDetailed secondary survey ØDefinitive care
 Initial assessment and management Ø Hypoxia is most serious problem early interventions aimed at reversing Ø Immediate life-threatening injuries treated quickly and simply - usually with a tube or a needle Ø Secondary survey guided by high suspicion for specific injuries
Initial assessment and management Ø Hypoxia is most serious problem early interventions aimed at reversing Ø Immediate life-threatening injuries treated quickly and simply - usually with a tube or a needle Ø Secondary survey guided by high suspicion for specific injuries
 6 Immediate Life Threats Ø Airway obstruction Ø Tension pneumothorax Ø Open pneumothorax “sucking chest wound” Ø Massive hemothorax Ø Flail chest Ø Cardiac tamponade
6 Immediate Life Threats Ø Airway obstruction Ø Tension pneumothorax Ø Open pneumothorax “sucking chest wound” Ø Massive hemothorax Ø Flail chest Ø Cardiac tamponade
 6 Potential Life Threats Ø Pulmonary contusion Ø Myocardial contusion Ø Traumatic aortic rupture Ø Traumatic diaphragmatic rupture Ø Tracheobronchial tree injury - larynx, trachea, bronchus Ø Esophageal trauma
6 Potential Life Threats Ø Pulmonary contusion Ø Myocardial contusion Ø Traumatic aortic rupture Ø Traumatic diaphragmatic rupture Ø Tracheobronchial tree injury - larynx, trachea, bronchus Ø Esophageal trauma
 6 Other Frequent Injuries Ø Subcutaneous emphysema Ø Traumatic asphyxia Ø Simple pneumothorax Ø Hemothorax Ø Scapula fracture Ø Rib fractures
6 Other Frequent Injuries Ø Subcutaneous emphysema Ø Traumatic asphyxia Ø Simple pneumothorax Ø Hemothorax Ø Scapula fracture Ø Rib fractures
 Primary Survey ØAirway ØBreathing ØCirculation
Primary Survey ØAirway ØBreathing ØCirculation
 A = Airway Ø Assess for airway patency and air exchange - listen at nose & mouth Ø Assess for intercostal and supraclavicular muscle retractions Ø Assess oropharynx foreign body obstruction
A = Airway Ø Assess for airway patency and air exchange - listen at nose & mouth Ø Assess for intercostal and supraclavicular muscle retractions Ø Assess oropharynx foreign body obstruction
 B = Breathing Ø Assess respiratory movements and quality of respirations look, listen, feel Ø Shallow respirations are early indicator of distress cyanosis is late
B = Breathing Ø Assess respiratory movements and quality of respirations look, listen, feel Ø Shallow respirations are early indicator of distress cyanosis is late
 C = Circulation Ø Assess pulses for quality, rate, regularity Ø Assess blood pressure and pulse pressure Ø Skin - look and feel for color, temperature, capillary refill Ø Look at neck veins - flat vs. distended Ø Cardiac monitor
C = Circulation Ø Assess pulses for quality, rate, regularity Ø Assess blood pressure and pulse pressure Ø Skin - look and feel for color, temperature, capillary refill Ø Look at neck veins - flat vs. distended Ø Cardiac monitor
 Thoracotomy Ø Closed heart massage is ineffective in a hypovolemic patient Ø Left anterior thoracotomy with crossclamping of descending thoracic aorta and open-chest massage may be useful in pulseless victim of penetrating trauma
Thoracotomy Ø Closed heart massage is ineffective in a hypovolemic patient Ø Left anterior thoracotomy with crossclamping of descending thoracic aorta and open-chest massage may be useful in pulseless victim of penetrating trauma
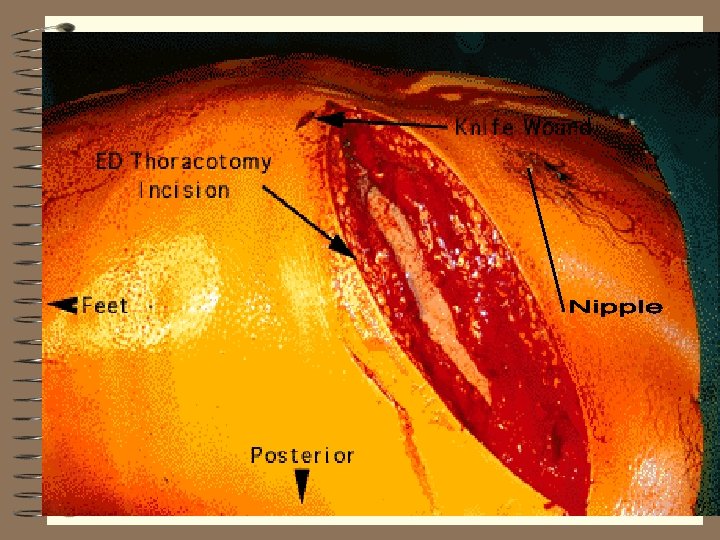 Thoracotomy
Thoracotomy
 6 Immediate Life Threats Ø Airway obstruction Ø Tension pneumothorax Ø Open pneumothorax “sucking chest wound” Ø Massive hemothorax Ø Flail chest Ø Cardiac tamponade
6 Immediate Life Threats Ø Airway obstruction Ø Tension pneumothorax Ø Open pneumothorax “sucking chest wound” Ø Massive hemothorax Ø Flail chest Ø Cardiac tamponade
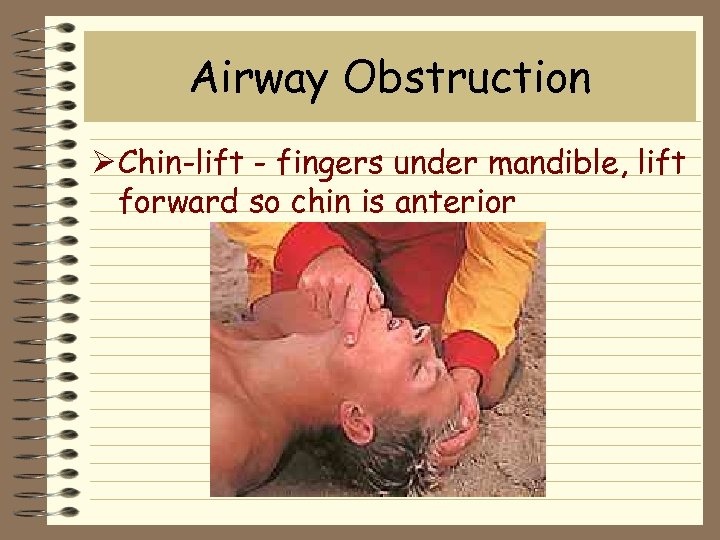 Airway Obstruction Ø Chin-lift - fingers under mandible, lift forward so chin is anterior
Airway Obstruction Ø Chin-lift - fingers under mandible, lift forward so chin is anterior
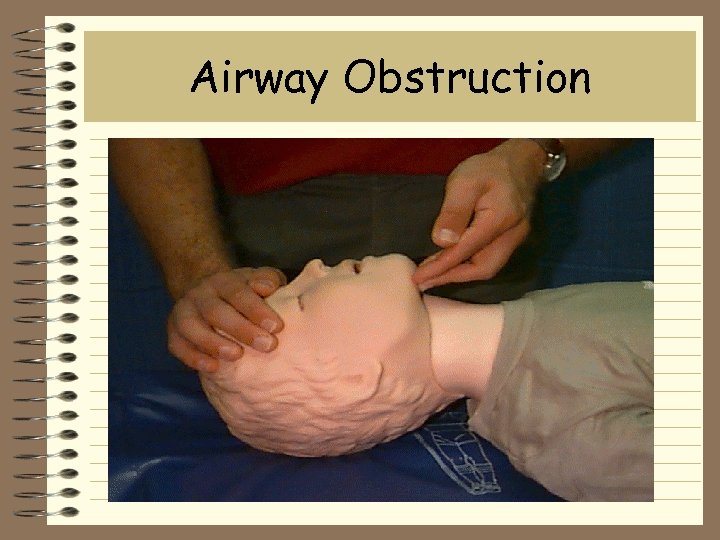 Airway Obstruction
Airway Obstruction
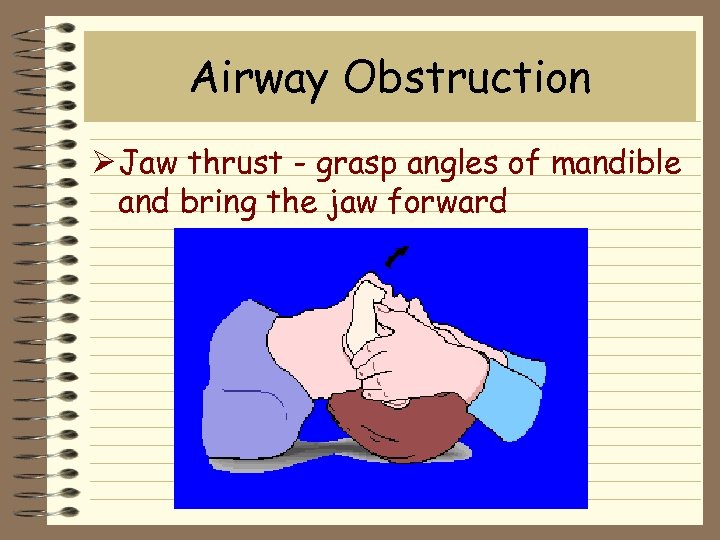 Airway Obstruction Ø Jaw thrust - grasp angles of mandible and bring the jaw forward
Airway Obstruction Ø Jaw thrust - grasp angles of mandible and bring the jaw forward
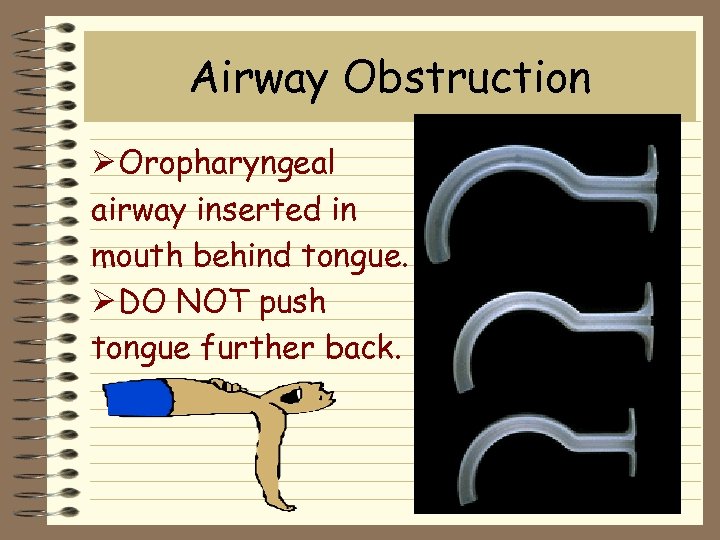 Airway Obstruction Ø Oropharyngeal airway inserted in mouth behind tongue. Ø DO NOT push tongue further back.
Airway Obstruction Ø Oropharyngeal airway inserted in mouth behind tongue. Ø DO NOT push tongue further back.
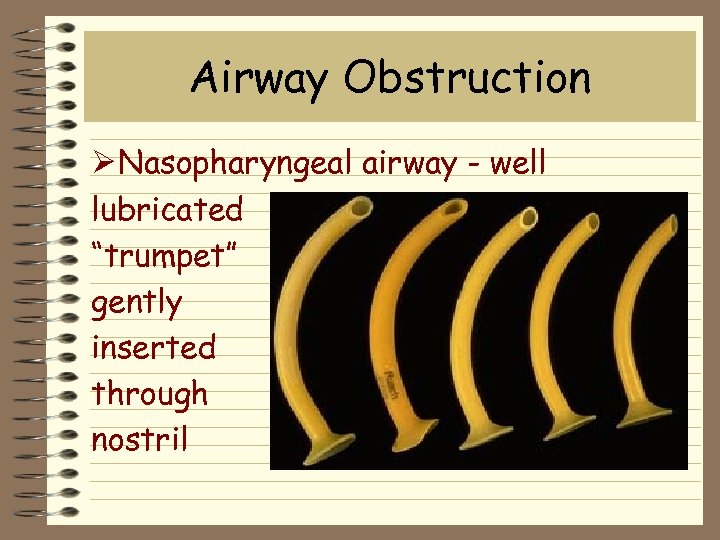 Airway Obstruction Ø Nasopharyngeal airway - well lubricated “trumpet” gently inserted through nostril
Airway Obstruction Ø Nasopharyngeal airway - well lubricated “trumpet” gently inserted through nostril
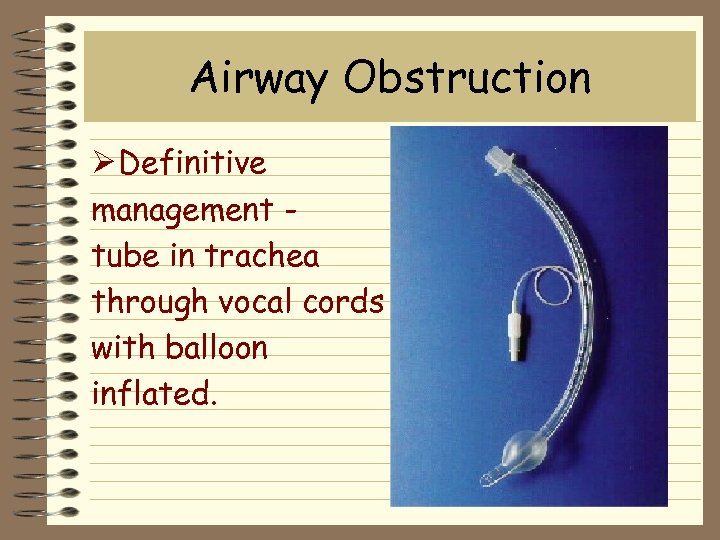 Airway Obstruction Ø Definitive management tube in trachea through vocal cords with balloon inflated.
Airway Obstruction Ø Definitive management tube in trachea through vocal cords with balloon inflated.
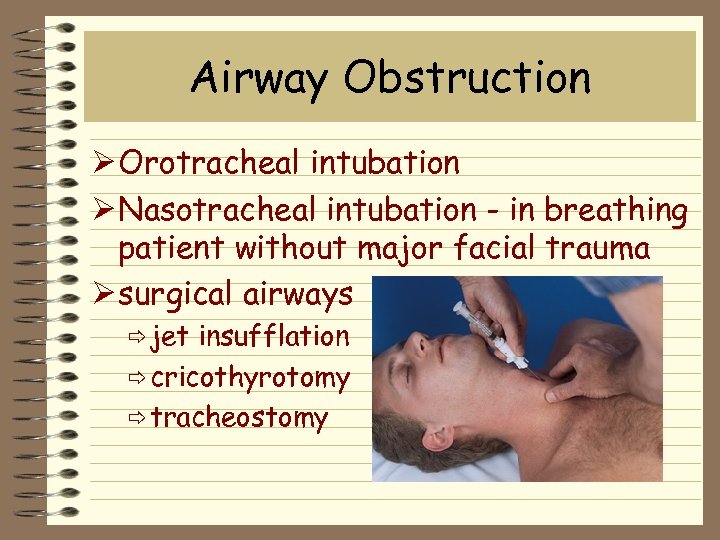 Airway Obstruction Ø Orotracheal intubation Ø Nasotracheal intubation - in breathing patient without major facial trauma Ø surgical airways ð jet insufflation ð cricothyrotomy ð tracheostomy
Airway Obstruction Ø Orotracheal intubation Ø Nasotracheal intubation - in breathing patient without major facial trauma Ø surgical airways ð jet insufflation ð cricothyrotomy ð tracheostomy
 Airway Obstruction Jet insufflation adapters
Airway Obstruction Jet insufflation adapters
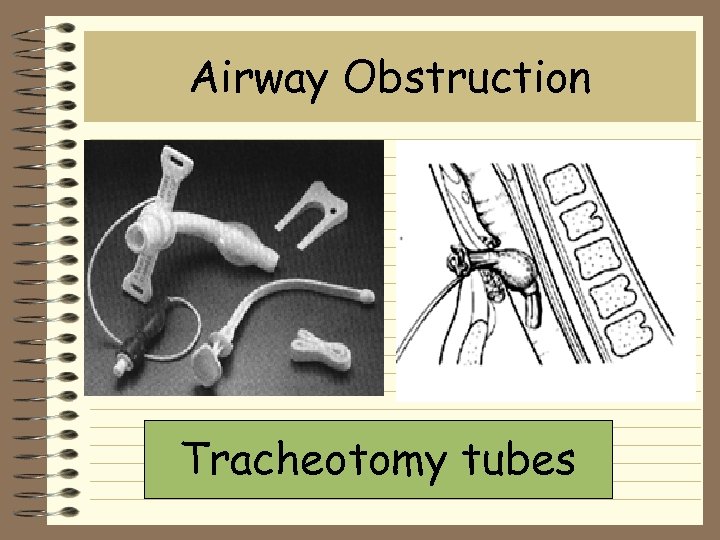 Airway Obstruction Tracheotomy tubes
Airway Obstruction Tracheotomy tubes
 Tension pneumothorax Ø Air leaks through lung or chest wall Ø “One-way” valve with lung collapse Ø Mediastinum shifts to opposite side Ø Inferior vena cava “kinks” on diaphragm, leading to decreased venous return and cardiovascular collapse
Tension pneumothorax Ø Air leaks through lung or chest wall Ø “One-way” valve with lung collapse Ø Mediastinum shifts to opposite side Ø Inferior vena cava “kinks” on diaphragm, leading to decreased venous return and cardiovascular collapse
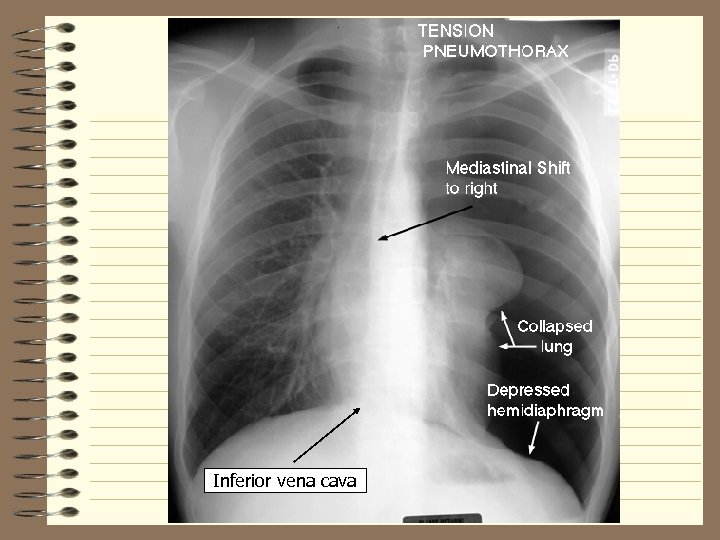 Inferior vena cava
Inferior vena cava
 Tension pneumothorax Ø Tension pneumothorax is not an xray diagnosis - it MUST be recognized clinically Ø Treatment is decompression - needle into 2 nd intercostal space of mid-clavicular line followed by thoracotomy tube
Tension pneumothorax Ø Tension pneumothorax is not an xray diagnosis - it MUST be recognized clinically Ø Treatment is decompression - needle into 2 nd intercostal space of mid-clavicular line followed by thoracotomy tube
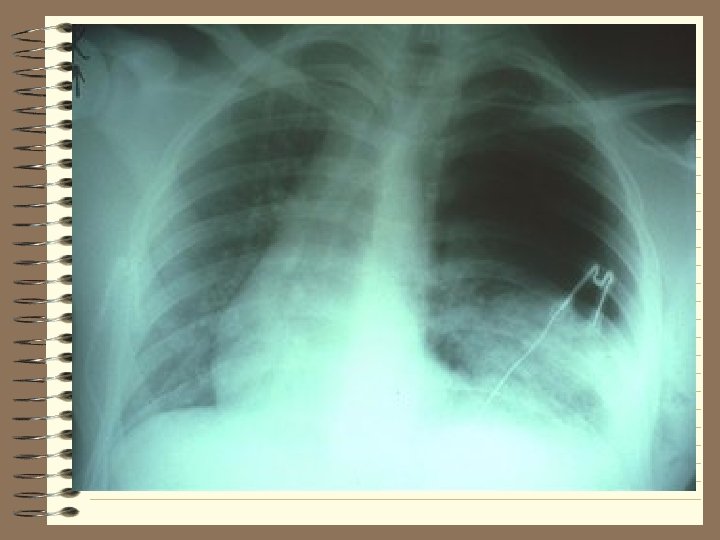
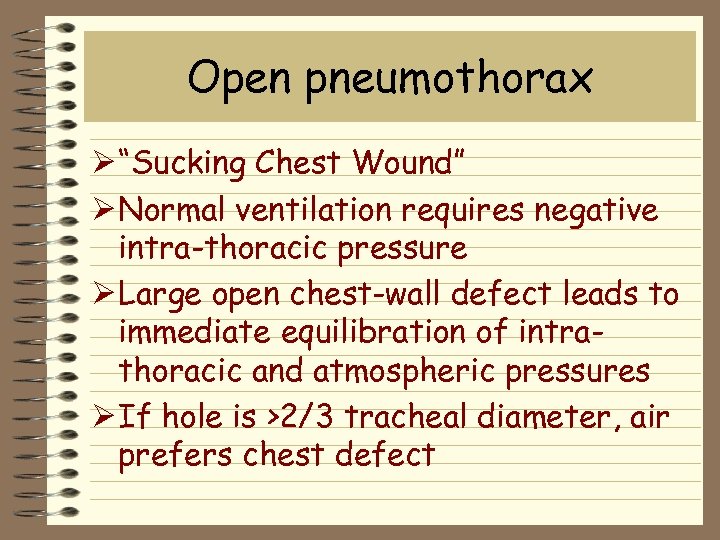 Open pneumothorax Ø “Sucking Chest Wound” Ø Normal ventilation requires negative intra-thoracic pressure Ø Large open chest-wall defect leads to immediate equilibration of intrathoracic and atmospheric pressures Ø If hole is >2/3 tracheal diameter, air prefers chest defect
Open pneumothorax Ø “Sucking Chest Wound” Ø Normal ventilation requires negative intra-thoracic pressure Ø Large open chest-wall defect leads to immediate equilibration of intrathoracic and atmospheric pressures Ø If hole is >2/3 tracheal diameter, air prefers chest defect
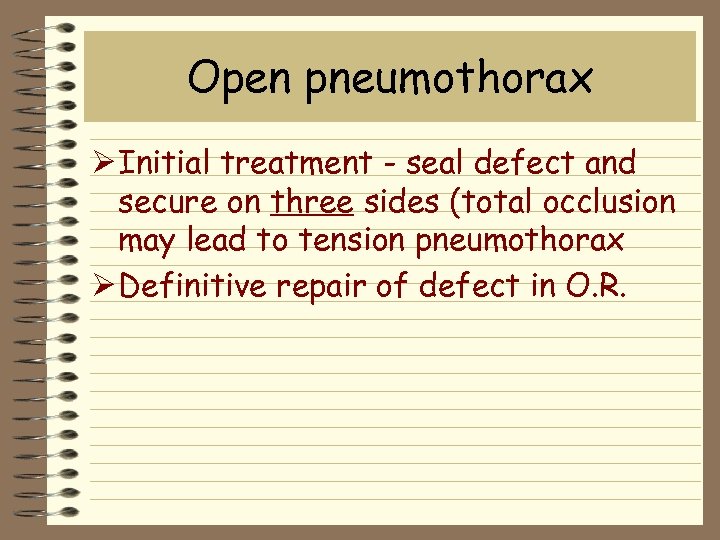 Open pneumothorax Ø Initial treatment - seal defect and secure on three sides (total occlusion may lead to tension pneumothorax Ø Definitive repair of defect in O. R.
Open pneumothorax Ø Initial treatment - seal defect and secure on three sides (total occlusion may lead to tension pneumothorax Ø Definitive repair of defect in O. R.
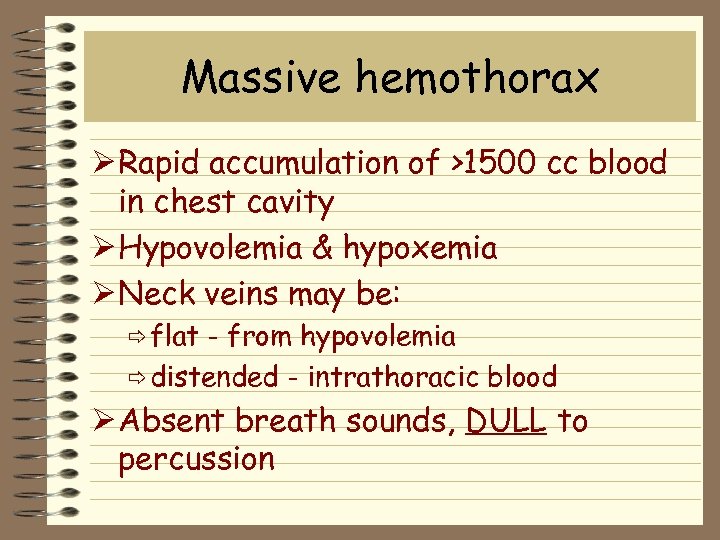 Massive hemothorax Ø Rapid accumulation of >1500 cc blood in chest cavity Ø Hypovolemia & hypoxemia Ø Neck veins may be: ð flat - from hypovolemia ð distended - intrathoracic blood Ø Absent breath sounds, DULL to percussion
Massive hemothorax Ø Rapid accumulation of >1500 cc blood in chest cavity Ø Hypovolemia & hypoxemia Ø Neck veins may be: ð flat - from hypovolemia ð distended - intrathoracic blood Ø Absent breath sounds, DULL to percussion

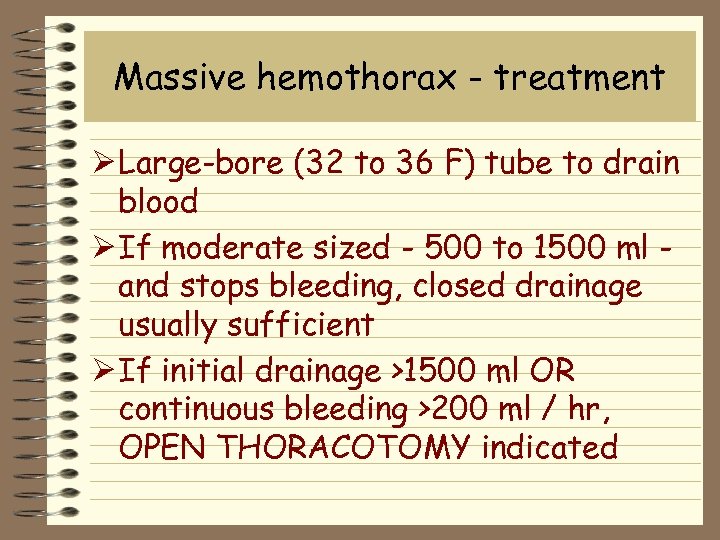 Massive hemothorax - treatment Ø Large-bore (32 to 36 F) tube to drain blood Ø If moderate sized - 500 to 1500 ml and stops bleeding, closed drainage usually sufficient Ø If initial drainage >1500 ml OR continuous bleeding >200 ml / hr, OPEN THORACOTOMY indicated
Massive hemothorax - treatment Ø Large-bore (32 to 36 F) tube to drain blood Ø If moderate sized - 500 to 1500 ml and stops bleeding, closed drainage usually sufficient Ø If initial drainage >1500 ml OR continuous bleeding >200 ml / hr, OPEN THORACOTOMY indicated

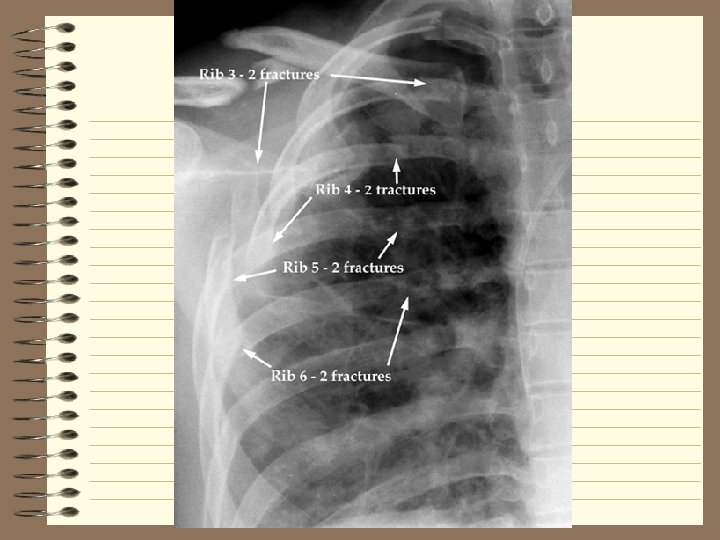
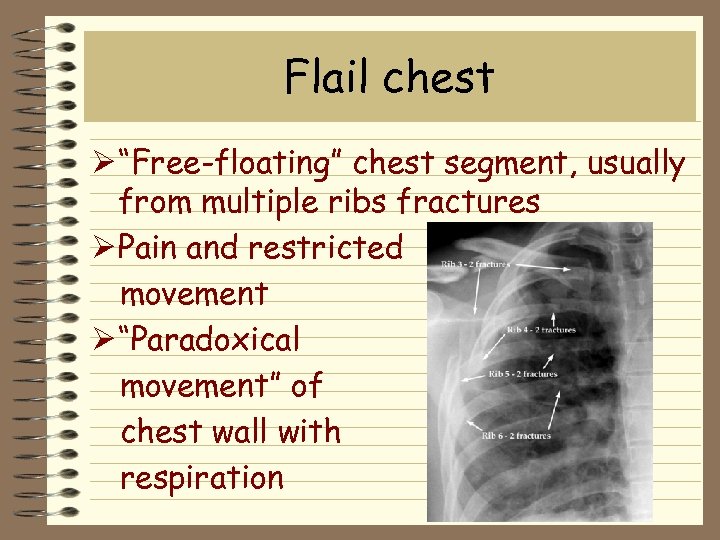 Flail chest Ø “Free-floating” chest segment, usually from multiple ribs fractures Ø Pain and restricted movement Ø “Paradoxical movement” of chest wall with respiration
Flail chest Ø “Free-floating” chest segment, usually from multiple ribs fractures Ø Pain and restricted movement Ø “Paradoxical movement” of chest wall with respiration
 Flail chest - treatment Ø Adequate ventilation Ø Humidified oxygen Ø Fluid resuscitation Ø PAIN MANAGEMENT Ø Stabilize the chest ð internal - ventilator ð external - sand bags
Flail chest - treatment Ø Adequate ventilation Ø Humidified oxygen Ø Fluid resuscitation Ø PAIN MANAGEMENT Ø Stabilize the chest ð internal - ventilator ð external - sand bags
 Cardiac tamponade Ø Usually from penetrating injuries Ø Classic “Beck’s triad” ð elevated venous pressure - neck veins ð decreased arterial pressure - BP ð muffled heart sounds Ø Blood in sac prevents cardiac activity
Cardiac tamponade Ø Usually from penetrating injuries Ø Classic “Beck’s triad” ð elevated venous pressure - neck veins ð decreased arterial pressure - BP ð muffled heart sounds Ø Blood in sac prevents cardiac activity
 Cardiac tamponade Ø May find “pulsus paradoxus” - a decrease of 10 mm Hg or greater in systolic BP during inspiration Ø Systolic to diastolic gradient of less than 30 mm Hg also suggestive
Cardiac tamponade Ø May find “pulsus paradoxus” - a decrease of 10 mm Hg or greater in systolic BP during inspiration Ø Systolic to diastolic gradient of less than 30 mm Hg also suggestive
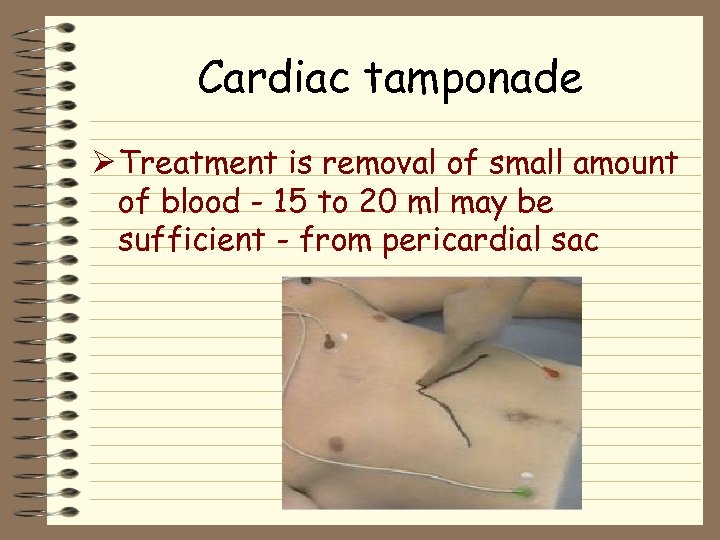 Cardiac tamponade Ø Treatment is removal of small amount of blood - 15 to 20 ml may be sufficient - from pericardial sac
Cardiac tamponade Ø Treatment is removal of small amount of blood - 15 to 20 ml may be sufficient - from pericardial sac
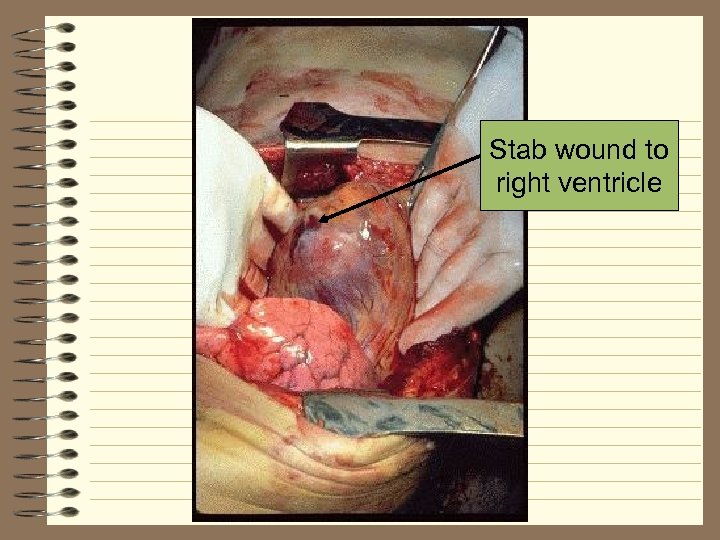 Stab wound to right ventricle
Stab wound to right ventricle
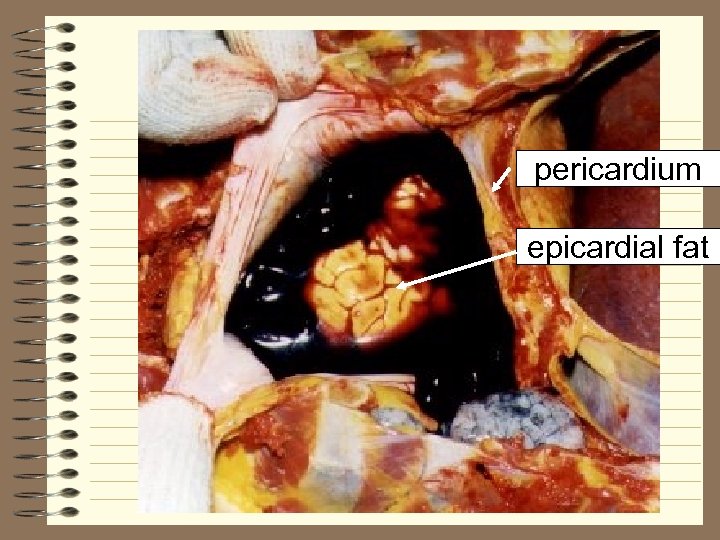 pericardium epicardial fat
pericardium epicardial fat
 6 Potential Life Threats Ø Pulmonary contusion Ø Myocardial contusion Ø Traumatic aortic rupture Ø Traumatic diaphragmatic rupture Ø Tracheobronchial tree injury larynx, trachea, bronchus Ø Esophageal trauma
6 Potential Life Threats Ø Pulmonary contusion Ø Myocardial contusion Ø Traumatic aortic rupture Ø Traumatic diaphragmatic rupture Ø Tracheobronchial tree injury larynx, trachea, bronchus Ø Esophageal trauma
 Pulmonary contusion Ø Potentially life-threatening condition with insidious onset Ø Parenchymal injury without laceration Ø More than 50% will develop pneumonia, even with treatment Ø Up to 50% have only hemoptysis as presenting symptom
Pulmonary contusion Ø Potentially life-threatening condition with insidious onset Ø Parenchymal injury without laceration Ø More than 50% will develop pneumonia, even with treatment Ø Up to 50% have only hemoptysis as presenting symptom
 Pulmonary contusion Ø Patients with pre-existing conditions emphysema, renal failure - need early intubation Ø Treatment needs to occur over time as symptoms develop
Pulmonary contusion Ø Patients with pre-existing conditions emphysema, renal failure - need early intubation Ø Treatment needs to occur over time as symptoms develop
 Myocardial contusion Ø Blunt precordial chest trauma Ø Difficult to diagnose Ø Risk for dysrhythmias, sudden death, tamponade, pericarditis, ventricular aneurysm
Myocardial contusion Ø Blunt precordial chest trauma Ø Difficult to diagnose Ø Risk for dysrhythmias, sudden death, tamponade, pericarditis, ventricular aneurysm
 Myocardial contusion Also may see: Ø myocardial concussion - “stunned” myocardium with no cell death Ø coronary artery laceration Diagnosis by: Ø trans-esophageal echocardiogram Ø serial cardiac enzymes
Myocardial contusion Also may see: Ø myocardial concussion - “stunned” myocardium with no cell death Ø coronary artery laceration Diagnosis by: Ø trans-esophageal echocardiogram Ø serial cardiac enzymes
 Traumatic aortic rupture Ø 90% or more dead at scene Ø 90% mortality each undiagnosed day Ø Must have high index of suspicion Ø Disruption occurs at ligamentum arteriosum (ductus arteriosus) Ø Contained hematoma of 500 to 1000 ml of blood
Traumatic aortic rupture Ø 90% or more dead at scene Ø 90% mortality each undiagnosed day Ø Must have high index of suspicion Ø Disruption occurs at ligamentum arteriosum (ductus arteriosus) Ø Contained hematoma of 500 to 1000 ml of blood
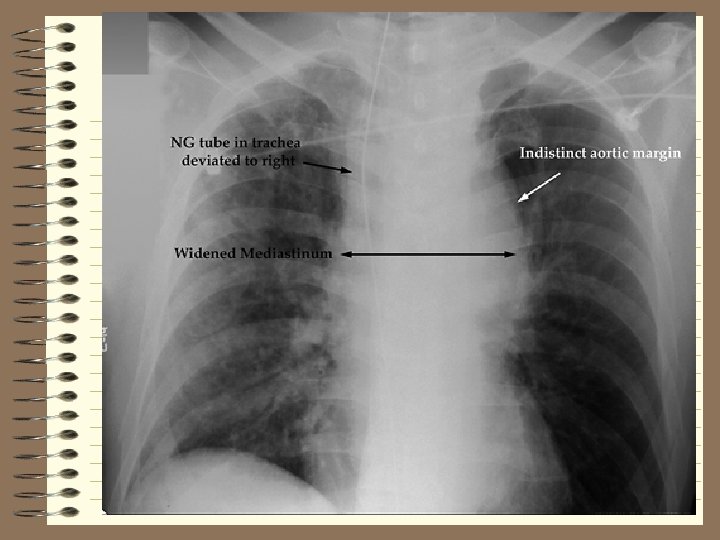
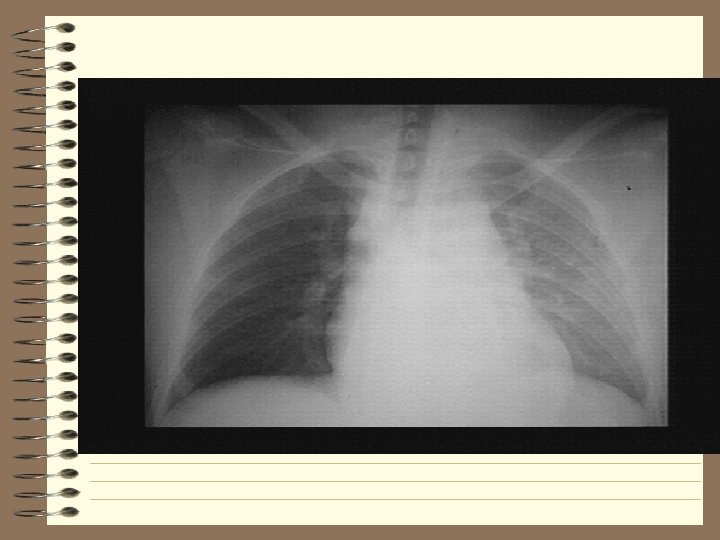
 Traumatic aortic rupture Ø Radiographic signs ð wide mediastinum ð 1 st & 2 nd rib fx ð obliteration of aortic knob ð tracheal deviation to right ð pleural cap ð depression left mainstem bronchus ð elevation and right shift mainstem bronchus ð obliteration “aortic window” ð deviation of esophagus to right
Traumatic aortic rupture Ø Radiographic signs ð wide mediastinum ð 1 st & 2 nd rib fx ð obliteration of aortic knob ð tracheal deviation to right ð pleural cap ð depression left mainstem bronchus ð elevation and right shift mainstem bronchus ð obliteration “aortic window” ð deviation of esophagus to right
 Traumatic aortic rupture Ø Treatment SURGICAL REPAIR
Traumatic aortic rupture Ø Treatment SURGICAL REPAIR
 Traumatic diaphragmatic rupture Ø Blunt trauma - tears leading to immediate herniation Ø Penetrating trauma - small tears which may take years to develop herniation Ø Usually on left side
Traumatic diaphragmatic rupture Ø Blunt trauma - tears leading to immediate herniation Ø Penetrating trauma - small tears which may take years to develop herniation Ø Usually on left side
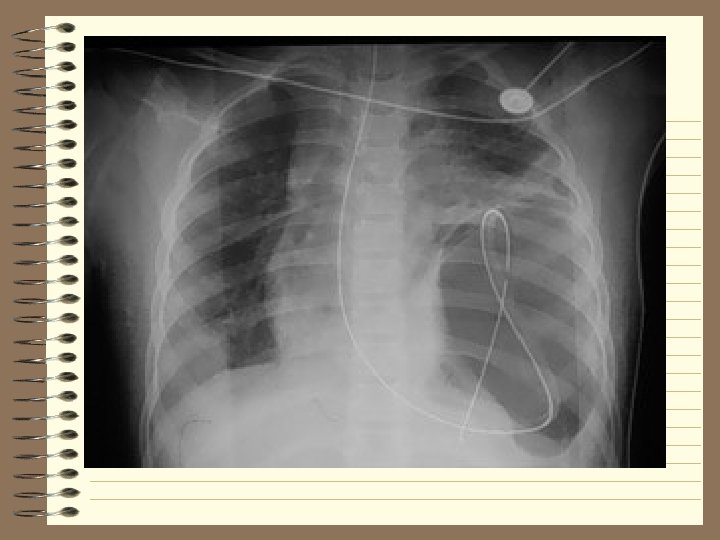
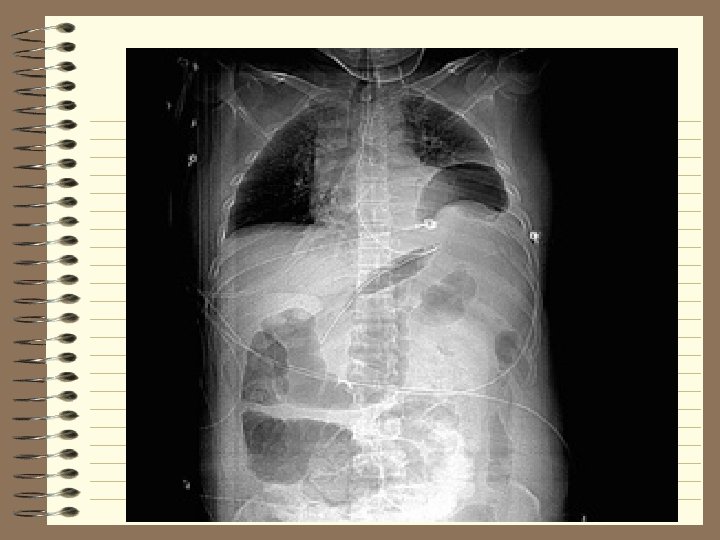
 Traumatic diaphragmatic rupture Ø Treatment - surgical repair
Traumatic diaphragmatic rupture Ø Treatment - surgical repair
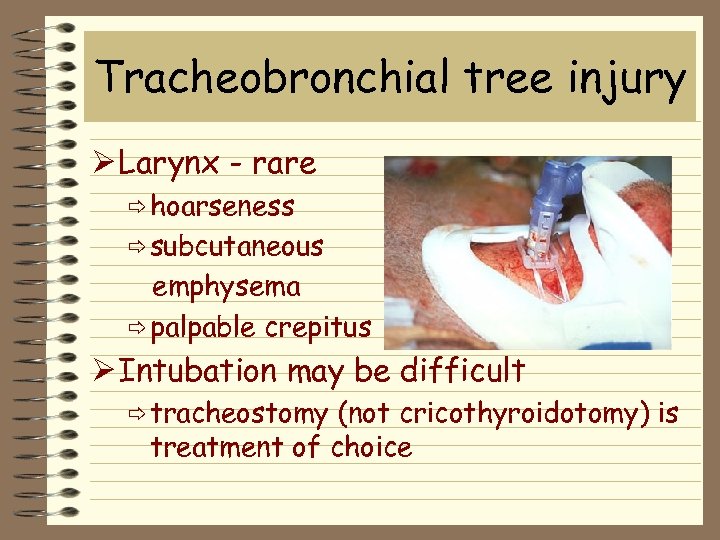 Tracheobronchial tree injury Ø Larynx - rare ð hoarseness ð subcutaneous emphysema ð palpable crepitus Ø Intubation may be difficult ð tracheostomy (not cricothyroidotomy) is treatment of choice
Tracheobronchial tree injury Ø Larynx - rare ð hoarseness ð subcutaneous emphysema ð palpable crepitus Ø Intubation may be difficult ð tracheostomy (not cricothyroidotomy) is treatment of choice
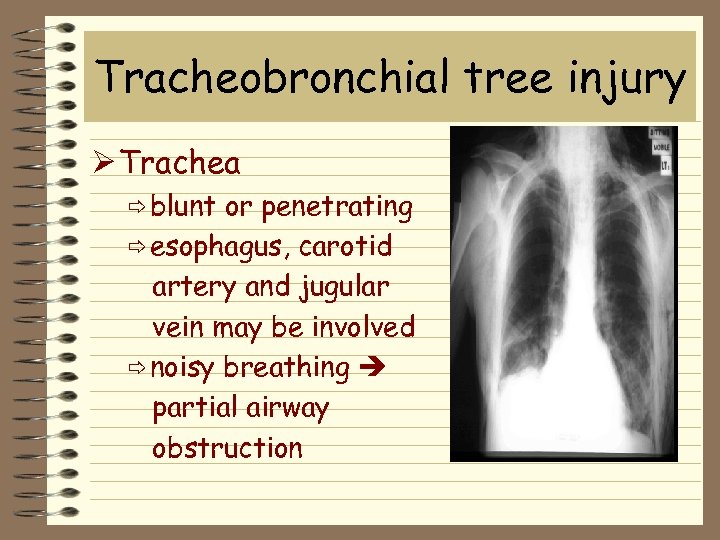 Tracheobronchial tree injury Ø Trachea ð blunt or penetrating ð esophagus, carotid artery and jugular vein may be involved ð noisy breathing partial airway obstruction
Tracheobronchial tree injury Ø Trachea ð blunt or penetrating ð esophagus, carotid artery and jugular vein may be involved ð noisy breathing partial airway obstruction

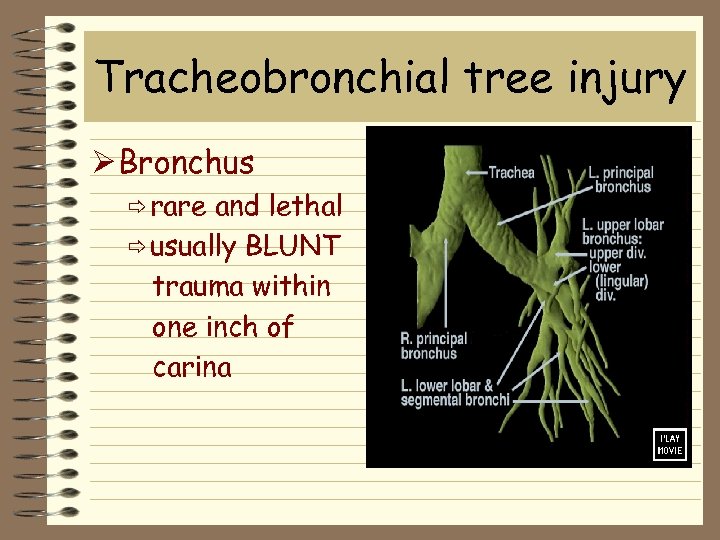 Tracheobronchial tree injury Ø Bronchus ð rare and lethal ð usually BLUNT trauma within one inch of carina
Tracheobronchial tree injury Ø Bronchus ð rare and lethal ð usually BLUNT trauma within one inch of carina
 Esophageal trauma Ø Most commonly penetrating Ø May be lethal if not recognized Ø High suspicion if ð left pneumothorax and hemothorax without rib fracture ð shock out of proportion to apparent blunt chest trauma ð particulate matter in chest tube
Esophageal trauma Ø Most commonly penetrating Ø May be lethal if not recognized Ø High suspicion if ð left pneumothorax and hemothorax without rib fracture ð shock out of proportion to apparent blunt chest trauma ð particulate matter in chest tube
 Esophageal trauma Ø If blunt trauma, linear tear in lower esophagus with leakage of stomach contents into mediastinum
Esophageal trauma Ø If blunt trauma, linear tear in lower esophagus with leakage of stomach contents into mediastinum
 6 Other Frequent Injuries Ø Subcutaneous emphysema Ø Traumatic asphyxia Ø Simple pneumothorax Ø Hemothorax Ø Scapula fracture Ø Rib fractures
6 Other Frequent Injuries Ø Subcutaneous emphysema Ø Traumatic asphyxia Ø Simple pneumothorax Ø Hemothorax Ø Scapula fracture Ø Rib fractures
 Subcutaneous emphysema Ø “Rice Krispies” Ø May result from ð airway injury ð lung injury ð blast injury Ø No treatment required - address underlying problem
Subcutaneous emphysema Ø “Rice Krispies” Ø May result from ð airway injury ð lung injury ð blast injury Ø No treatment required - address underlying problem
 Traumatic asphyxia Ø “Masque ecchymotique” - purple face from extravasation of blood Ø Major damage is to underlying structures Ø Purple face fades over time in survivors
Traumatic asphyxia Ø “Masque ecchymotique” - purple face from extravasation of blood Ø Major damage is to underlying structures Ø Purple face fades over time in survivors
 Simple pneumothorax Ø Air enters potential space between visceral and parietal pleura Ø Breath sounds down on affected side Ø Percussion shows hyper-resonance Ø Treatment: chest tube in 4 th or 5 th intercostal space anterior to midaxillary line
Simple pneumothorax Ø Air enters potential space between visceral and parietal pleura Ø Breath sounds down on affected side Ø Percussion shows hyper-resonance Ø Treatment: chest tube in 4 th or 5 th intercostal space anterior to midaxillary line
 Hemothorax Ø Lung laceration OR disruption of intercostal artery or internal mammary artery Ø Most are self-limiting Ø Surgical consultation for ð initial flow of >20 cc/kg (~1500 cc) ð continued flow of >200 cc/hr
Hemothorax Ø Lung laceration OR disruption of intercostal artery or internal mammary artery Ø Most are self-limiting Ø Surgical consultation for ð initial flow of >20 cc/kg (~1500 cc) ð continued flow of >200 cc/hr
 Scapula fractures Ø Fractures of scapula or 1 st & 2 nd ribs may indicate major mechanism of injury
Scapula fractures Ø Fractures of scapula or 1 st & 2 nd ribs may indicate major mechanism of injury
 Rib fractures Ø Ribs - most frequently injured part of thoracic cage Ø Most commonly injured - 4 th 9 th Ø If 10 th/11 th/12 th, be suspicious for liver or spleen injuries Ø If 1 st/2 nd/3 rd, worry about injury to head, neck, spinal cords, lungs, and great vessels
Rib fractures Ø Ribs - most frequently injured part of thoracic cage Ø Most commonly injured - 4 th 9 th Ø If 10 th/11 th/12 th, be suspicious for liver or spleen injuries Ø If 1 st/2 nd/3 rd, worry about injury to head, neck, spinal cords, lungs, and great vessels
 Rib frac tures Ø Treatment consists of… ð intercostal blocks ð epidural anesthesia ð systemic analgesics Ø Contraindications include… ð taping ð rib belts ð external splints
Rib frac tures Ø Treatment consists of… ð intercostal blocks ð epidural anesthesia ð systemic analgesics Ø Contraindications include… ð taping ð rib belts ð external splints
 In conclusion. . . Ø Chest trauma is very common in the multi-injured patient Ø Airway management and a judiciously placed needle can save many lives
In conclusion. . . Ø Chest trauma is very common in the multi-injured patient Ø Airway management and a judiciously placed needle can save many lives
 Trauma Code: ETA 5 minutes Stick with the basics - remember ABC’s Constantly re-evaluate patient not lab’s Don’t raise your voice - remain calm You are not alone, consult the experts ð don’t get in over your head Ø Take a step back ð What are you missing ? ð What did you overlook ? Ø Ø
Trauma Code: ETA 5 minutes Stick with the basics - remember ABC’s Constantly re-evaluate patient not lab’s Don’t raise your voice - remain calm You are not alone, consult the experts ð don’t get in over your head Ø Take a step back ð What are you missing ? ð What did you overlook ? Ø Ø
 Questions
Questions
