Psychological Management in chronisch Pain Juliana Friederichs Psychotherapist









psychological_management_in_chronin_pain_neu.ppt
- Количество слайдов: 67
 Psychological Management in chronisch Pain Juliana Friederichs Psychotherapist Berlin
Psychological Management in chronisch Pain Juliana Friederichs Psychotherapist Berlin
 Overview 1. What is pain? 2. How to deal with pain in psychotherapy? Goal Attainment Education ACT Therapy Providing long term therapy
Overview 1. What is pain? 2. How to deal with pain in psychotherapy? Goal Attainment Education ACT Therapy Providing long term therapy
 PAIN Pain is always a subjective experience Everyone learns the meaning of “pain” through experiences in early life As an unpleasant sensation it becomes an emotional experience Pain is a significant stressor physically, emotionally
PAIN Pain is always a subjective experience Everyone learns the meaning of “pain” through experiences in early life As an unpleasant sensation it becomes an emotional experience Pain is a significant stressor physically, emotionally
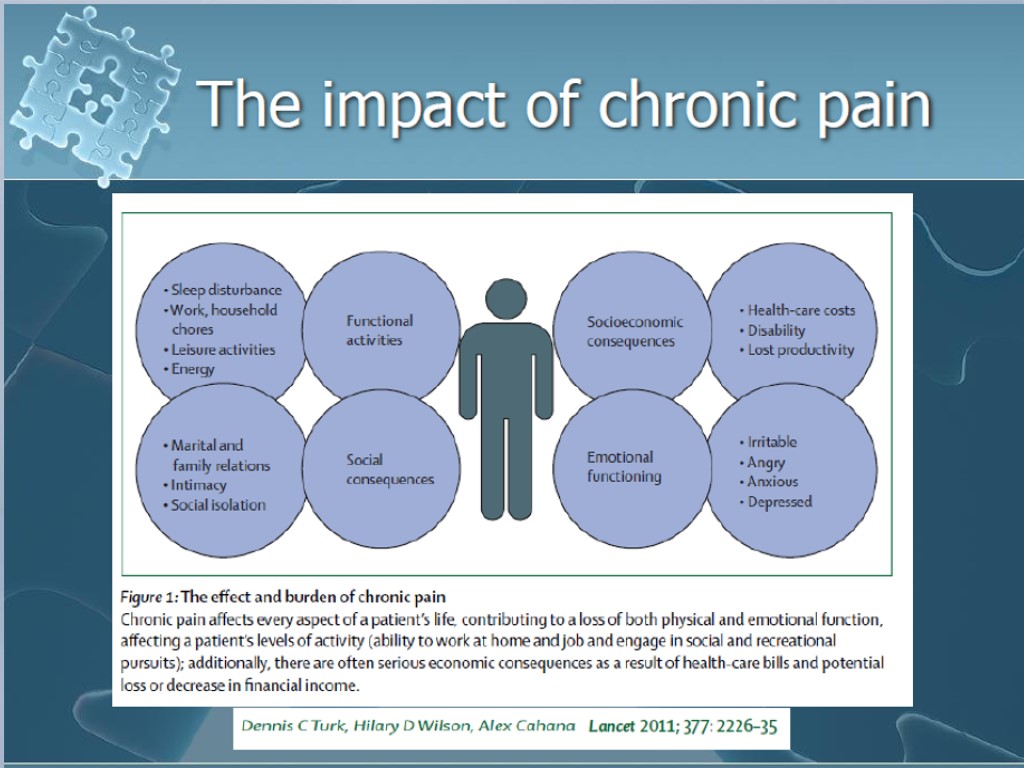
 The Problem of Pain Pain is one of the most common complaints made by patients to primary care providers Pain is typically an adaptive reaction to an injury and gradually decreases over time with conservative treatment. However, for some people pain persists past the point where it is considered adaptive and contributes to negative mood, disability, and increased use of healthcare system resources. Communication problem
The Problem of Pain Pain is one of the most common complaints made by patients to primary care providers Pain is typically an adaptive reaction to an injury and gradually decreases over time with conservative treatment. However, for some people pain persists past the point where it is considered adaptive and contributes to negative mood, disability, and increased use of healthcare system resources. Communication problem
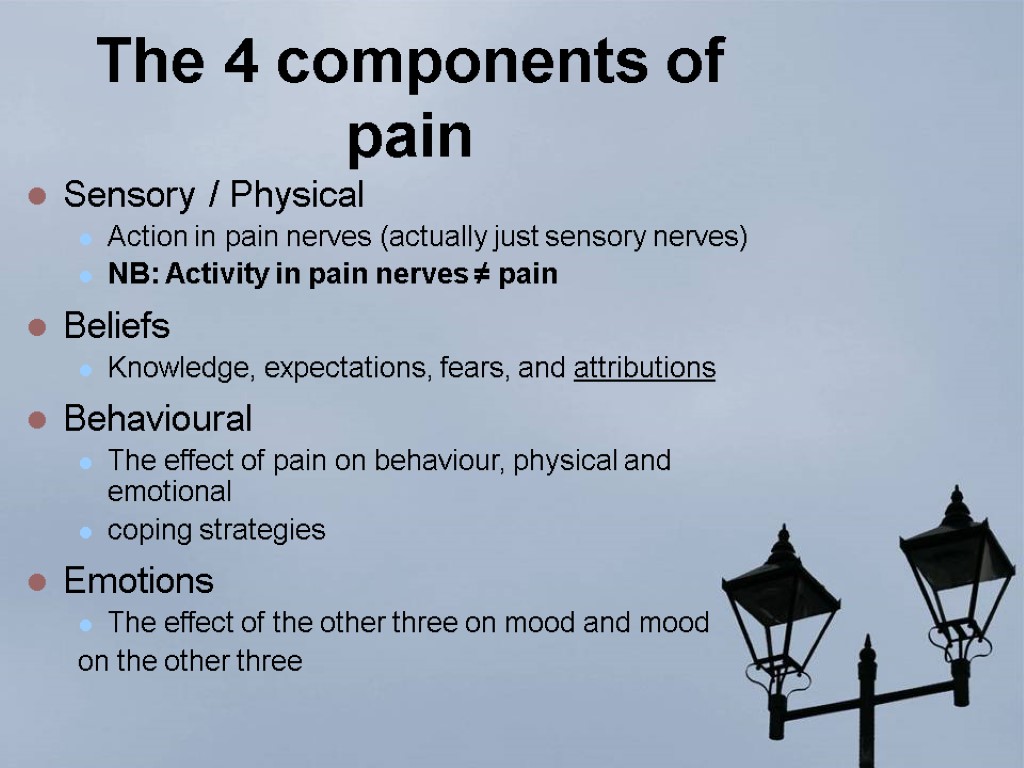
 The 4 components of pain Sensory / Physical Action in pain nerves (actually just sensory nerves) NB: Activity in pain nerves ≠ pain Beliefs Knowledge, expectations, fears, and attributions Behavioural The effect of pain on behaviour, physical and emotional coping strategies Emotions The effect of the other three on mood and mood on the other three
The 4 components of pain Sensory / Physical Action in pain nerves (actually just sensory nerves) NB: Activity in pain nerves ≠ pain Beliefs Knowledge, expectations, fears, and attributions Behavioural The effect of pain on behaviour, physical and emotional coping strategies Emotions The effect of the other three on mood and mood on the other three
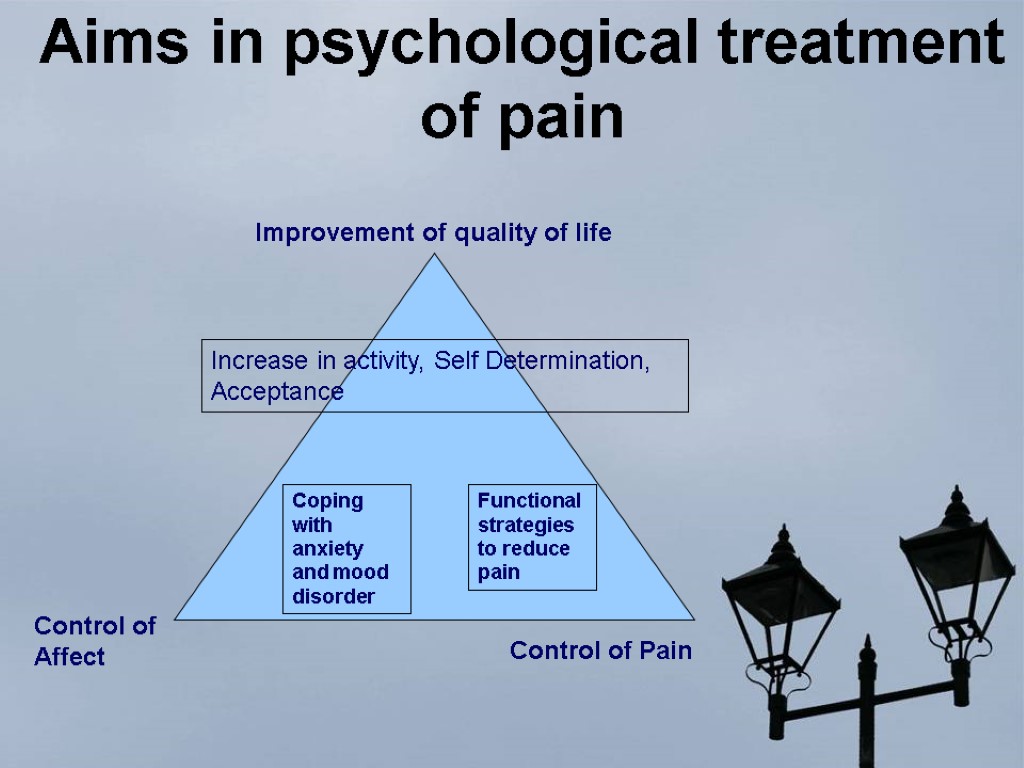
 Psychological Therapy of chronic pain Control of Affect Control of pain Improvement of quality of life Activating rescouces
Psychological Therapy of chronic pain Control of Affect Control of pain Improvement of quality of life Activating rescouces
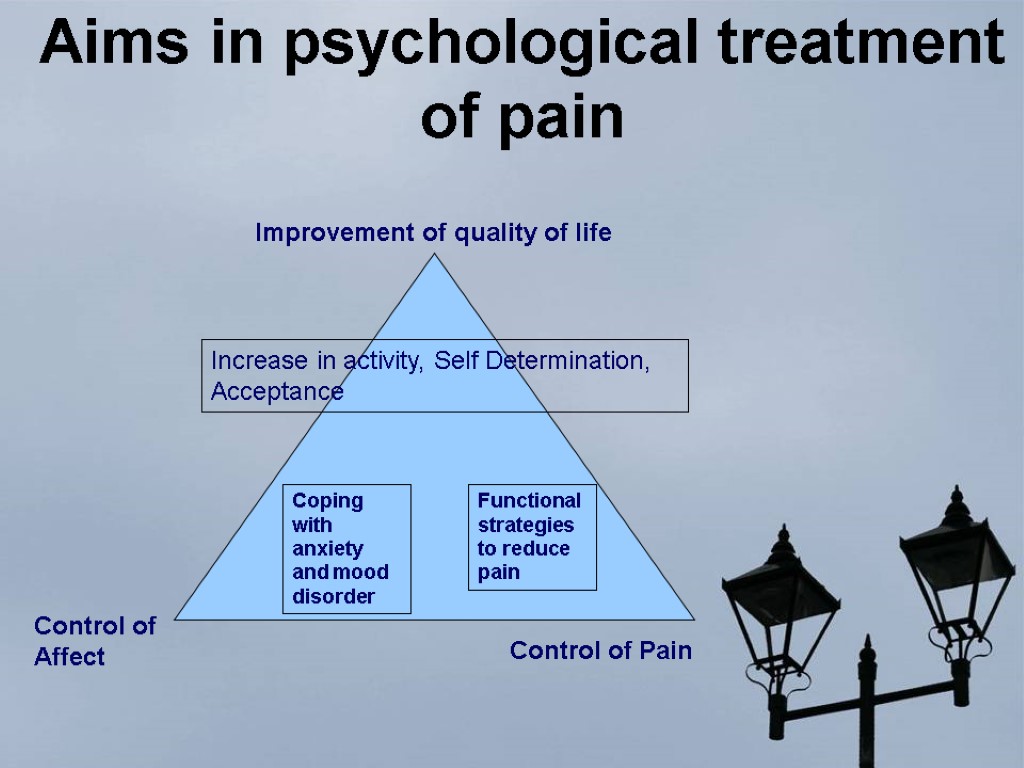 Aims in psychological treatment of pain Control of Affect Control of Pain Improvement of quality of life Increase in activity, Self Determination, Acceptance Coping with anxiety and mood disorder Functional strategies to reduce pain
Aims in psychological treatment of pain Control of Affect Control of Pain Improvement of quality of life Increase in activity, Self Determination, Acceptance Coping with anxiety and mood disorder Functional strategies to reduce pain
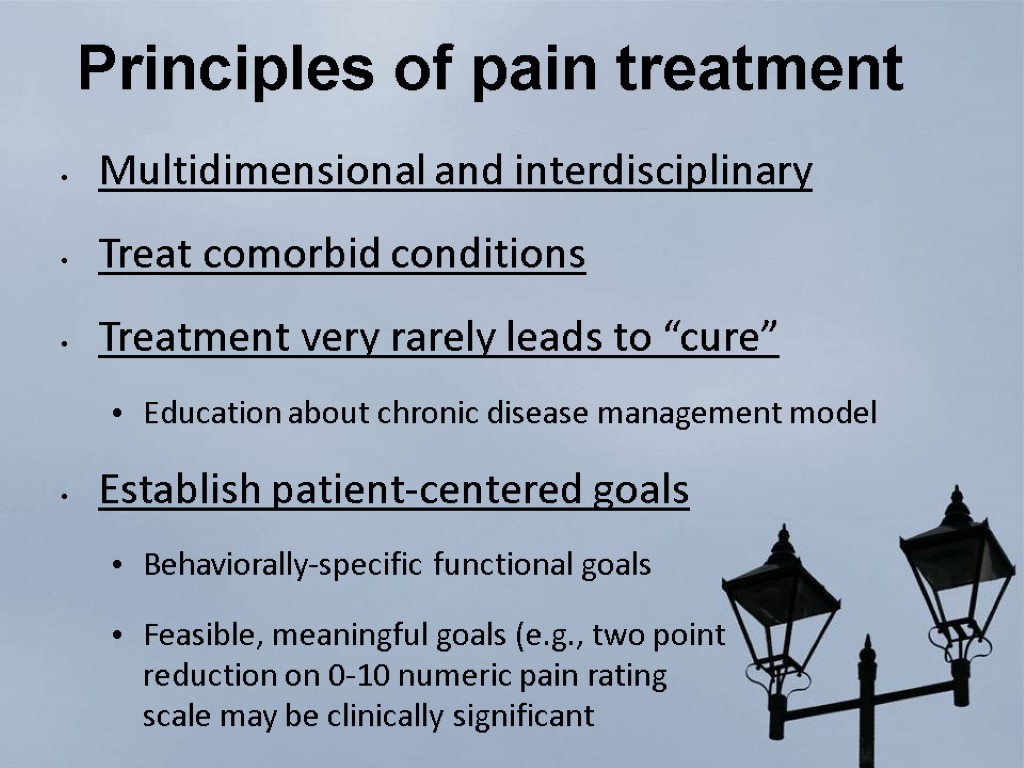 Principles of pain treatment Multidimensional and interdisciplinary Treat comorbid conditions Treatment very rarely leads to “cure” Education about chronic disease management model Establish patient-centered goals Behaviorally-specific functional goals Feasible, meaningful goals (e.g., two point reduction on 0-10 numeric pain rating scale may be clinically significant
Principles of pain treatment Multidimensional and interdisciplinary Treat comorbid conditions Treatment very rarely leads to “cure” Education about chronic disease management model Establish patient-centered goals Behaviorally-specific functional goals Feasible, meaningful goals (e.g., two point reduction on 0-10 numeric pain rating scale may be clinically significant
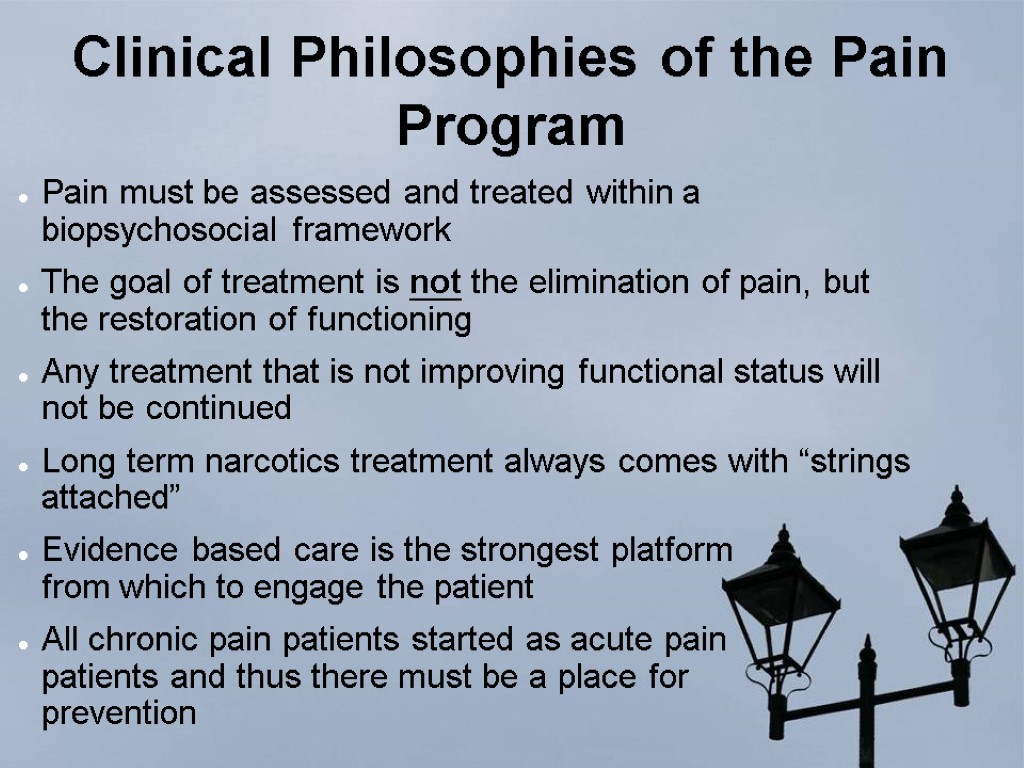
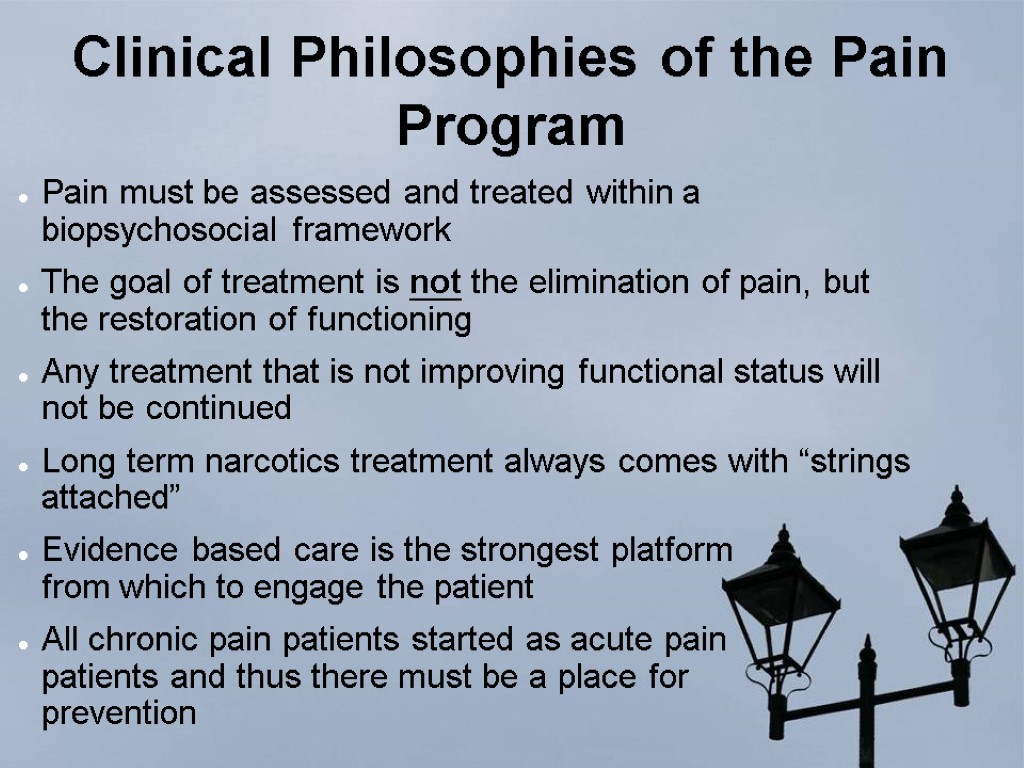 Clinical Philosophies of the Pain Program Pain must be assessed and treated within a biopsychosocial framework The goal of treatment is not the elimination of pain, but the restoration of functioning Any treatment that is not improving functional status will not be continued Long term narcotics treatment always comes with “strings attached” Evidence based care is the strongest platform from which to engage the patient All chronic pain patients started as acute pain patients and thus there must be a place for prevention
Clinical Philosophies of the Pain Program Pain must be assessed and treated within a biopsychosocial framework The goal of treatment is not the elimination of pain, but the restoration of functioning Any treatment that is not improving functional status will not be continued Long term narcotics treatment always comes with “strings attached” Evidence based care is the strongest platform from which to engage the patient All chronic pain patients started as acute pain patients and thus there must be a place for prevention
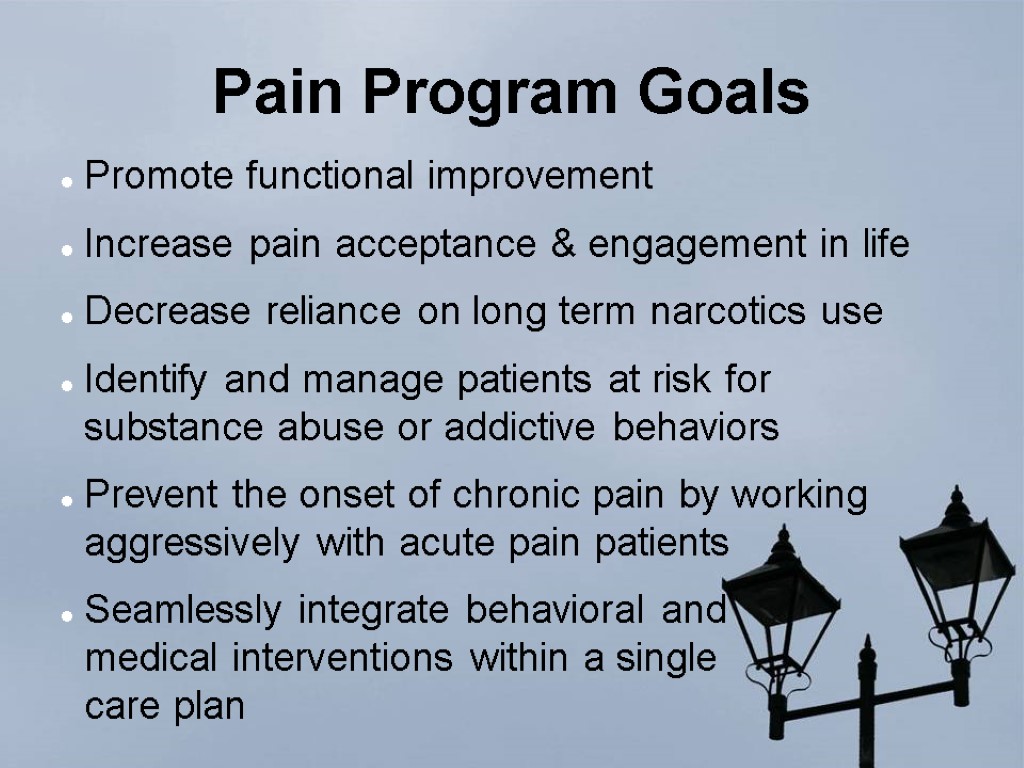
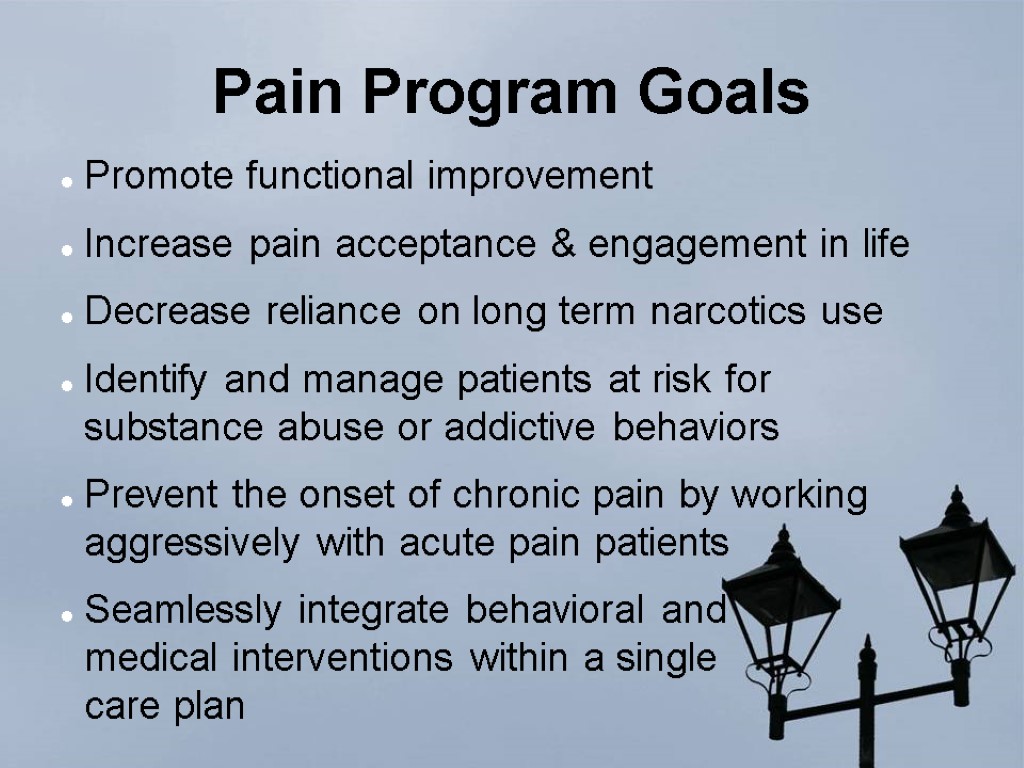 Pain Program Goals Promote functional improvement Increase pain acceptance & engagement in life Decrease reliance on long term narcotics use Identify and manage patients at risk for substance abuse or addictive behaviors Prevent the onset of chronic pain by working aggressively with acute pain patients Seamlessly integrate behavioral and medical interventions within a single care plan
Pain Program Goals Promote functional improvement Increase pain acceptance & engagement in life Decrease reliance on long term narcotics use Identify and manage patients at risk for substance abuse or addictive behaviors Prevent the onset of chronic pain by working aggressively with acute pain patients Seamlessly integrate behavioral and medical interventions within a single care plan
 Typical western treatment for pain Medication Opiods NSAIDS Muscle Relaxants Antidepressants Steroids Surgery Relaxation Techniques Psychotherapy Physiotherapy CONTROL
Typical western treatment for pain Medication Opiods NSAIDS Muscle Relaxants Antidepressants Steroids Surgery Relaxation Techniques Psychotherapy Physiotherapy CONTROL
 Patient Education
Patient Education
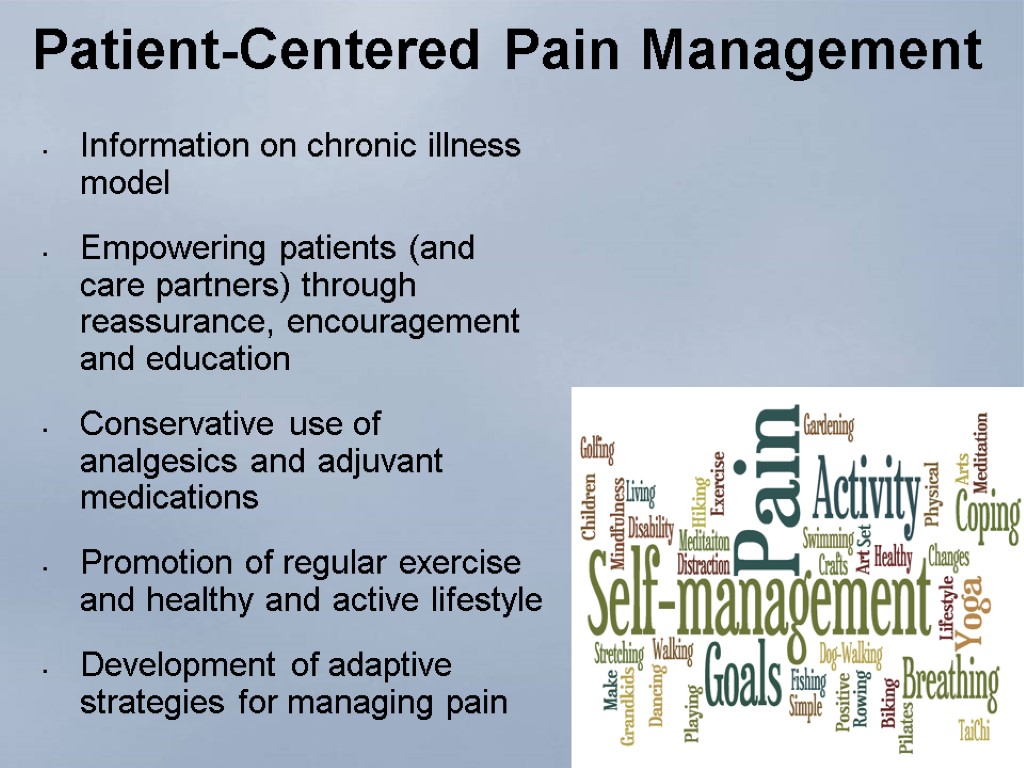
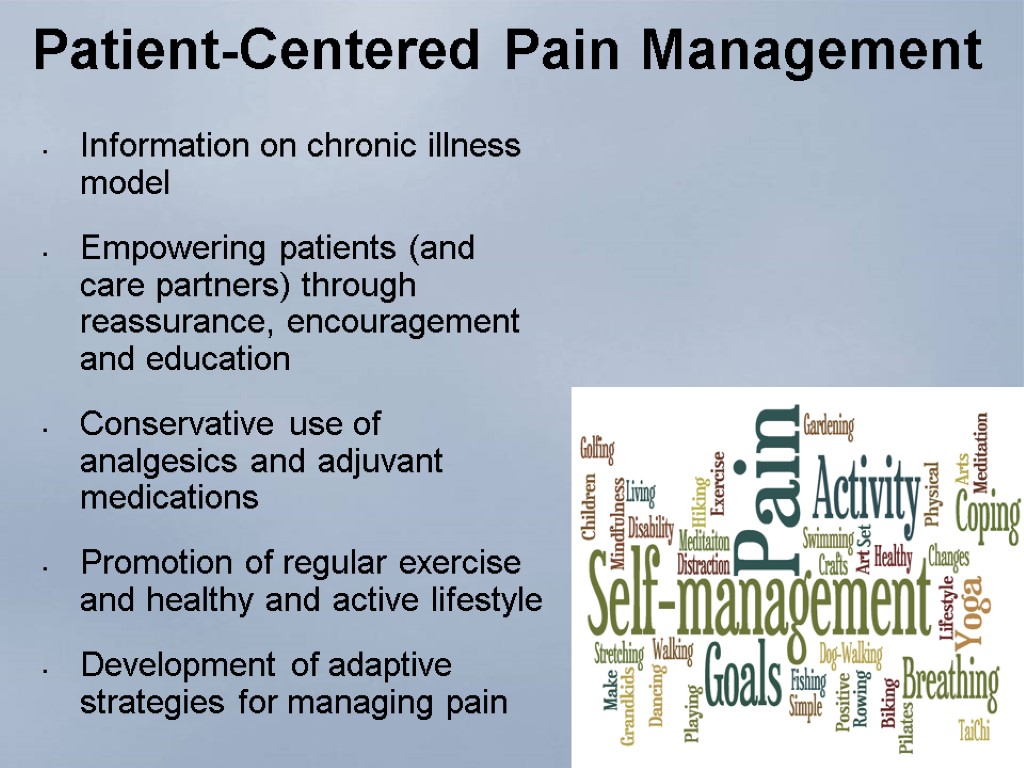 Patient-Centered Pain Management Information on chronic illness model Empowering patients (and care partners) through reassurance, encouragement and education Conservative use of analgesics and adjuvant medications Promotion of regular exercise and healthy and active lifestyle Development of adaptive strategies for managing pain 14
Patient-Centered Pain Management Information on chronic illness model Empowering patients (and care partners) through reassurance, encouragement and education Conservative use of analgesics and adjuvant medications Promotion of regular exercise and healthy and active lifestyle Development of adaptive strategies for managing pain 14
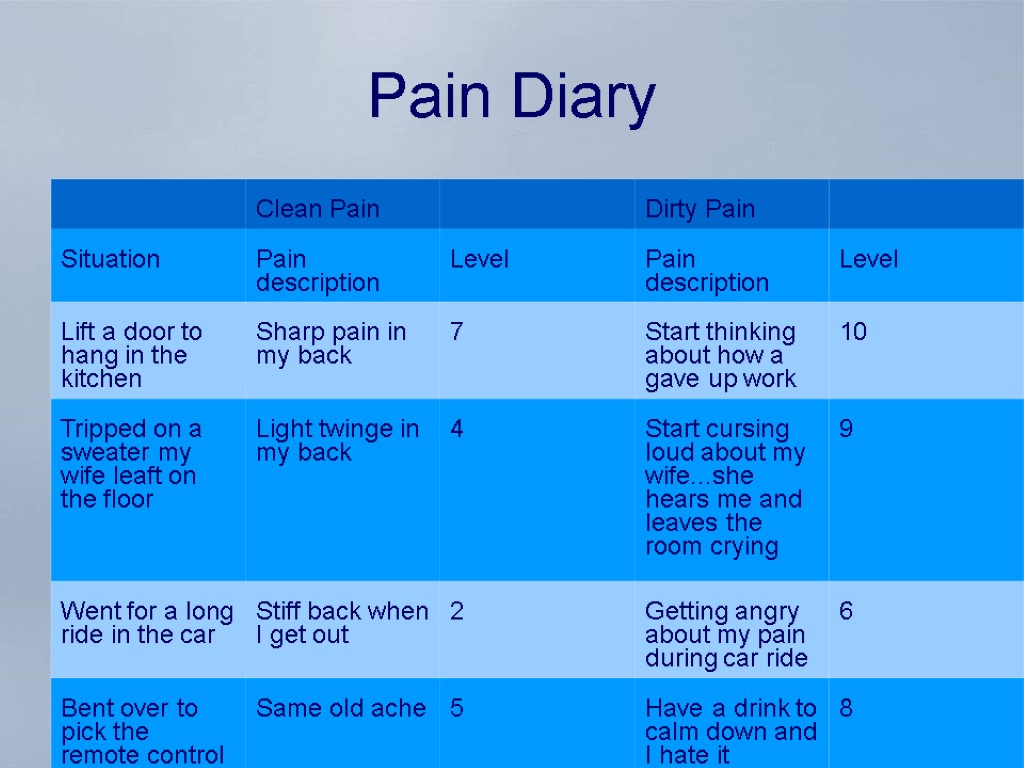
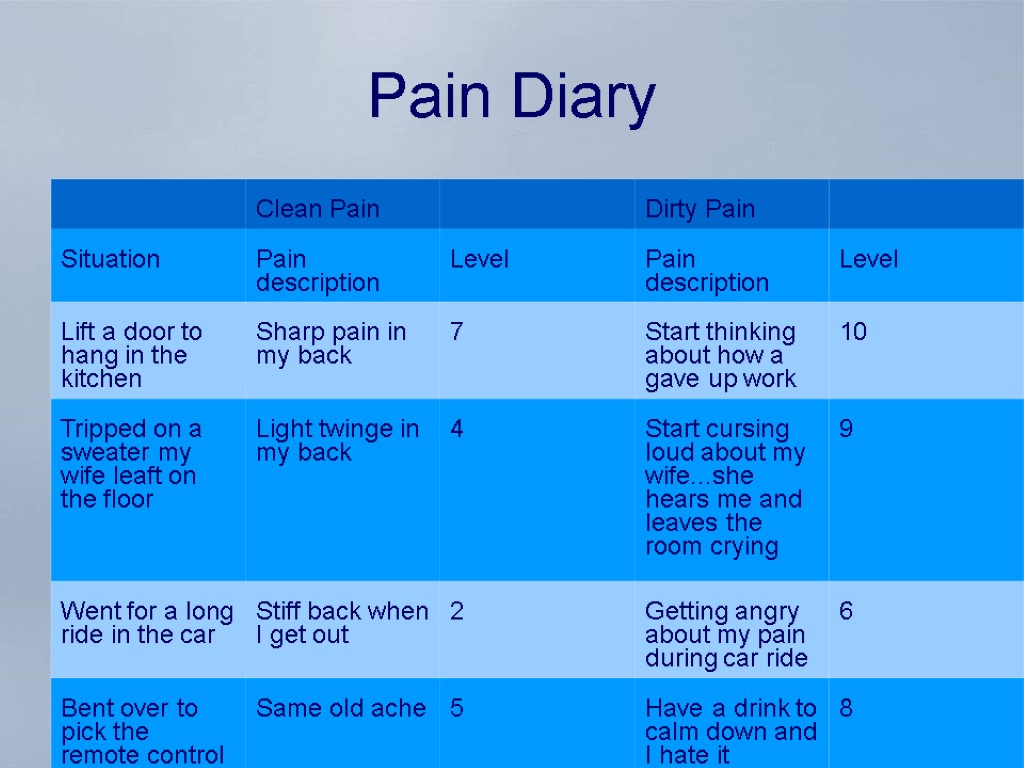 Pain Diary
Pain Diary
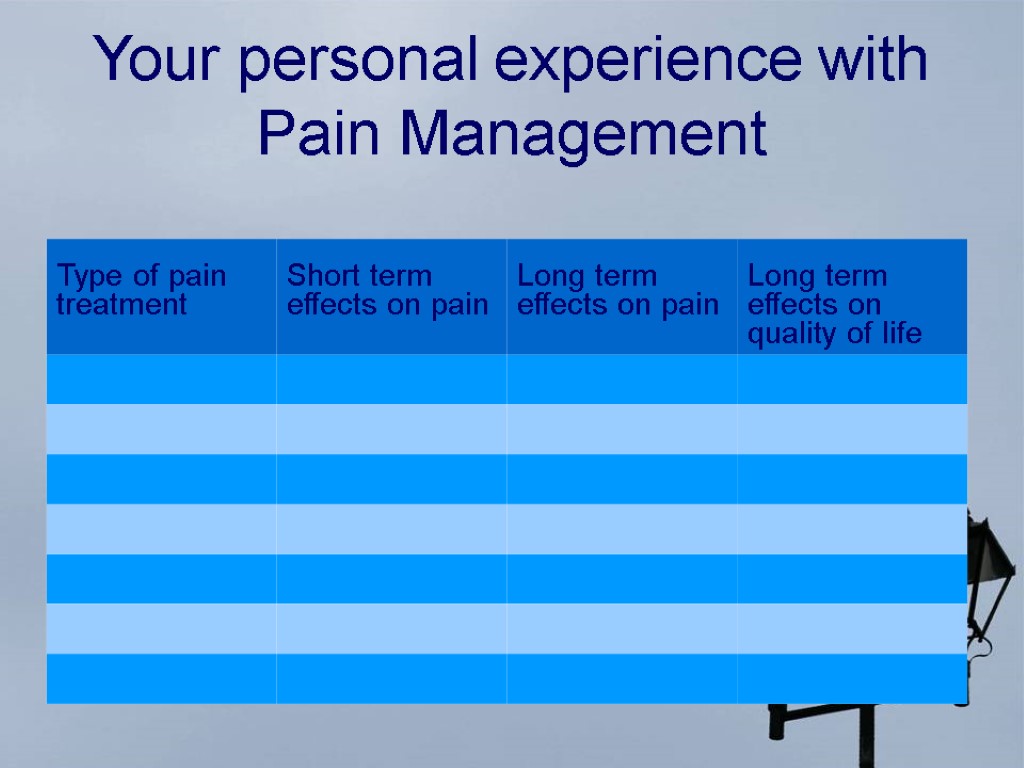
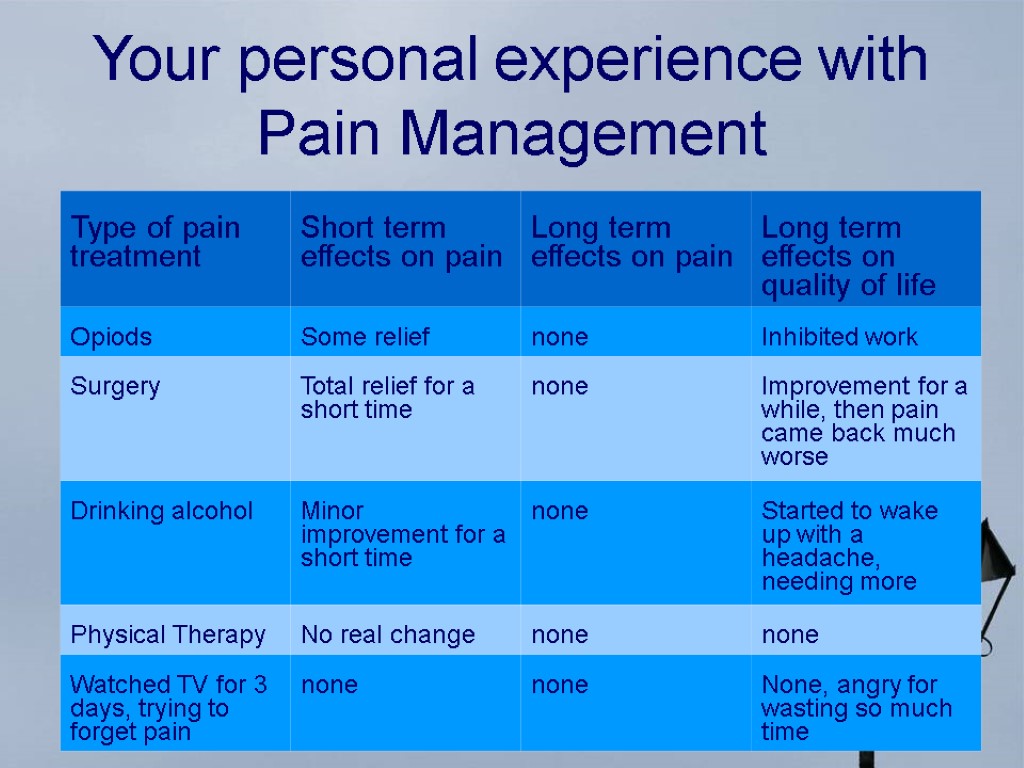
 Your personal experience with Pain Management
Your personal experience with Pain Management
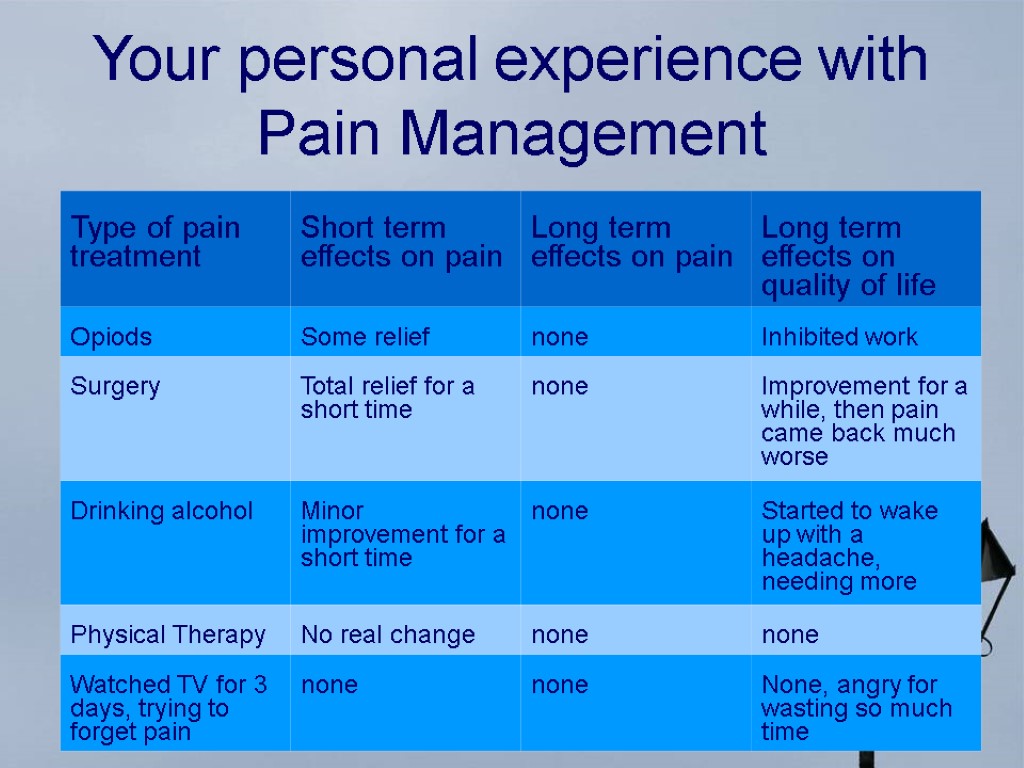 Your personal experience with Pain Management
Your personal experience with Pain Management
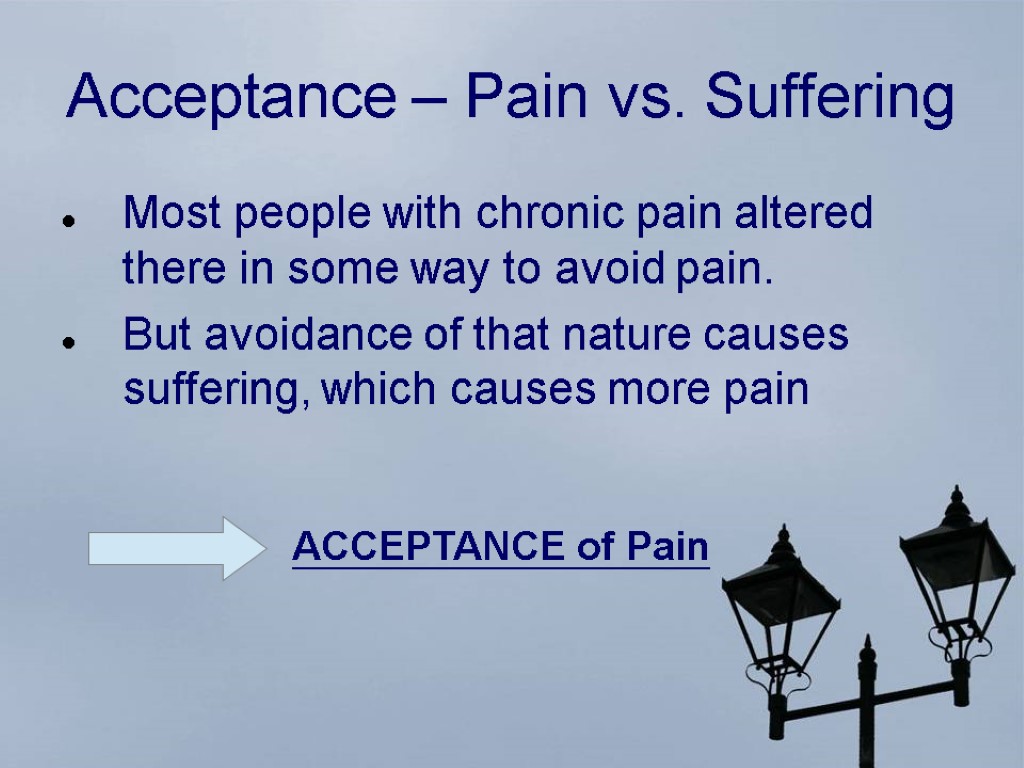
 Acceptance – Pain vs. Suffering Most people with chronic pain altered there in some way to avoid pain. But avoidance of that nature causes suffering, which causes more pain ACCEPTANCE of Pain
Acceptance – Pain vs. Suffering Most people with chronic pain altered there in some way to avoid pain. But avoidance of that nature causes suffering, which causes more pain ACCEPTANCE of Pain
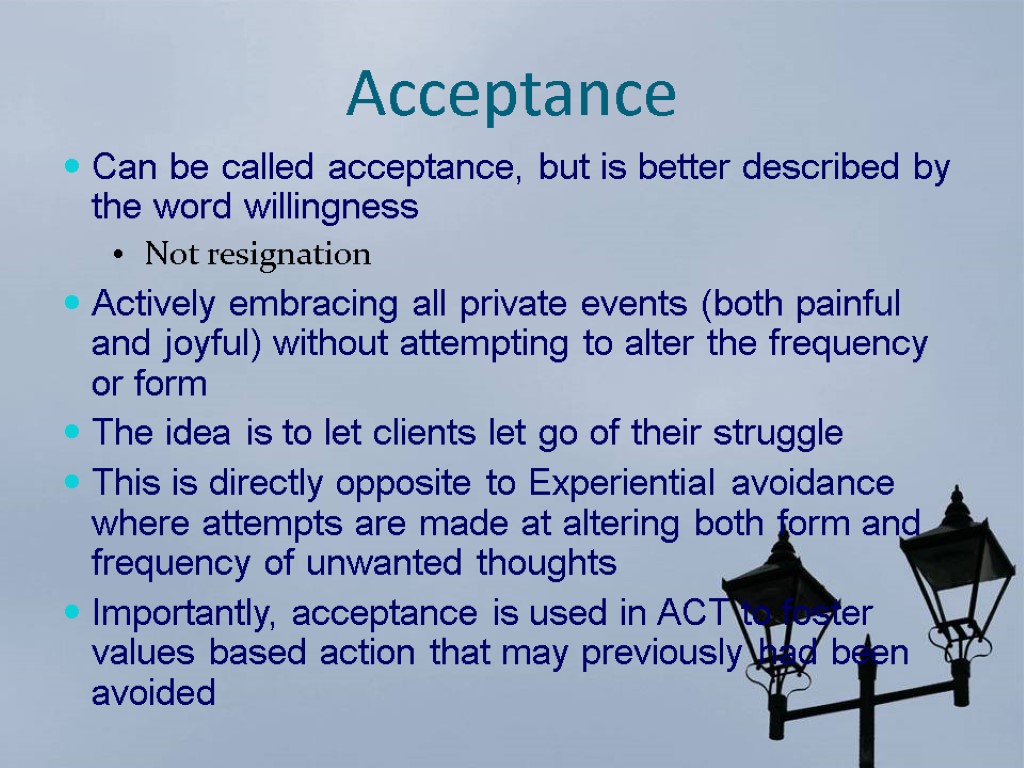
 Acceptance Can be called acceptance, but is better described by the word willingness Not resignation Actively embracing all private events (both painful and joyful) without attempting to alter the frequency or form The idea is to let clients let go of their struggle This is directly opposite to Experiential avoidance where attempts are made at altering both form and frequency of unwanted thoughts Importantly, acceptance is used in ACT to foster values based action that may previously had been avoided
Acceptance Can be called acceptance, but is better described by the word willingness Not resignation Actively embracing all private events (both painful and joyful) without attempting to alter the frequency or form The idea is to let clients let go of their struggle This is directly opposite to Experiential avoidance where attempts are made at altering both form and frequency of unwanted thoughts Importantly, acceptance is used in ACT to foster values based action that may previously had been avoided
 Acceptance Chronic pain by its definition is a pain that is not going away! If we try to get rid of it, we are fighting a losing battle! Being caugth in this struggle is the essence of chronic pain!
Acceptance Chronic pain by its definition is a pain that is not going away! If we try to get rid of it, we are fighting a losing battle! Being caugth in this struggle is the essence of chronic pain!
 Acceptance Giving Shape to your Pain If I could put my pain out of my body, what shape would it have? How big would it be? What color would it have? Would it have a voice? Can I talk to „the pain monster“?
Acceptance Giving Shape to your Pain If I could put my pain out of my body, what shape would it have? How big would it be? What color would it have? Would it have a voice? Can I talk to „the pain monster“?
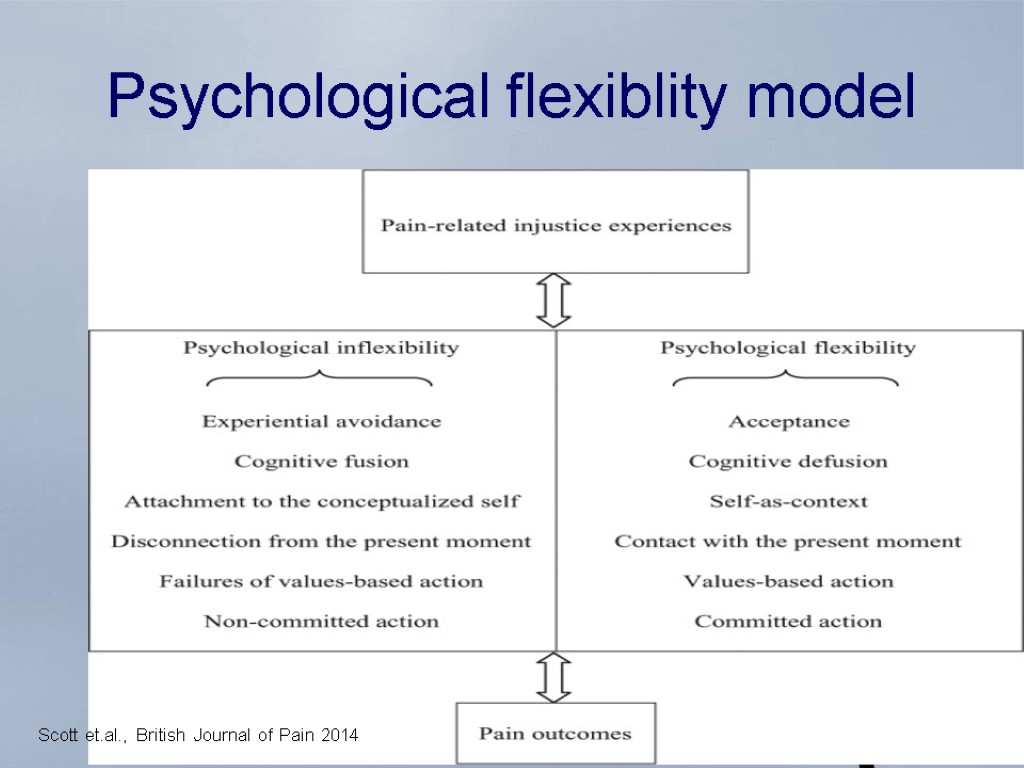
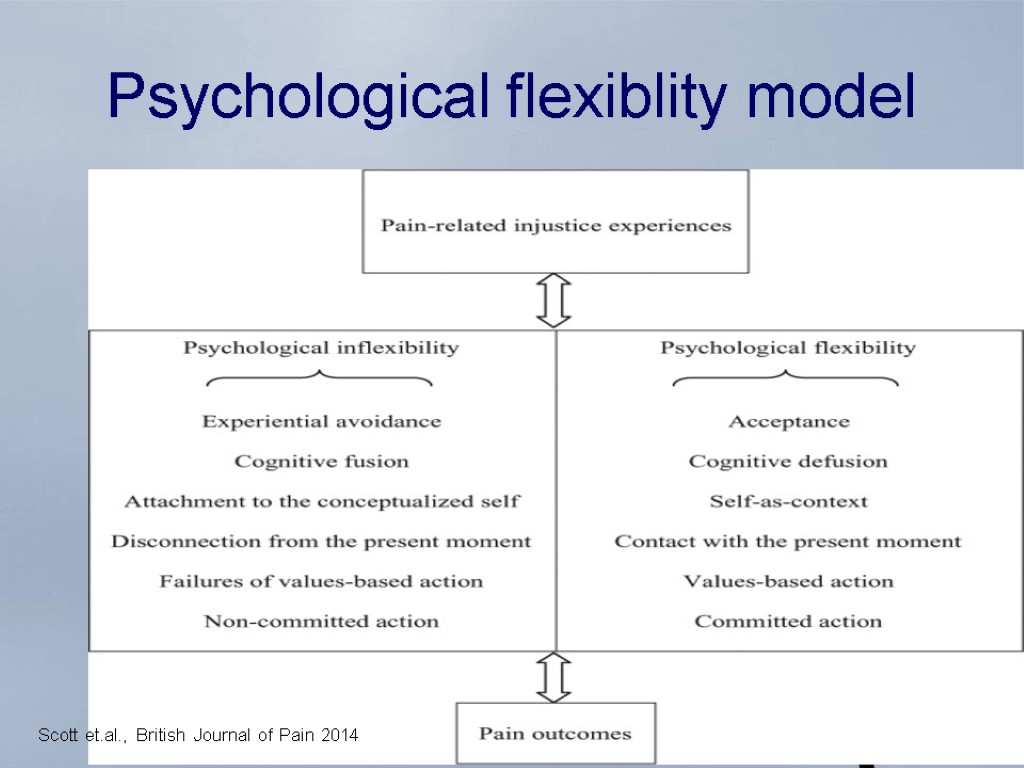 Scott et.al., British Journal of Pain 2014 Psychological flexiblity model
Scott et.al., British Journal of Pain 2014 Psychological flexiblity model
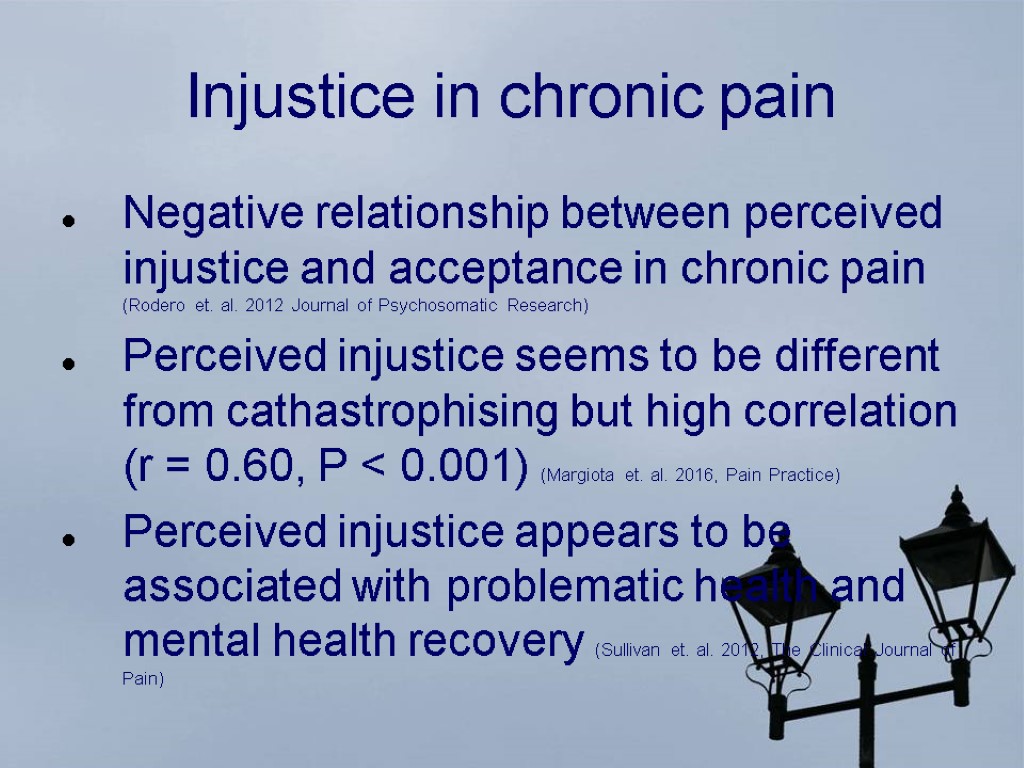 Injustice in chronic pain Negative relationship between perceived injustice and acceptance in chronic pain (Rodero et. al. 2012 Journal of Psychosomatic Research) Perceived injustice seems to be different from cathastrophising but high correlation (r = 0.60, P < 0.001) (Margiota et. al. 2016, Pain Practice) Perceived injustice appears to be associated with problematic health and mental health recovery (Sullivan et. al. 2012, The Clinical Journal of Pain)
Injustice in chronic pain Negative relationship between perceived injustice and acceptance in chronic pain (Rodero et. al. 2012 Journal of Psychosomatic Research) Perceived injustice seems to be different from cathastrophising but high correlation (r = 0.60, P < 0.001) (Margiota et. al. 2016, Pain Practice) Perceived injustice appears to be associated with problematic health and mental health recovery (Sullivan et. al. 2012, The Clinical Journal of Pain)
 What do you value?
What do you value?
 Goal attainment Key component in all kinds of long termn treatment (e.g. rehabilitation, mulitdisciplinary pain treatment) ( Levack 2015, Cochrane review) Best effects for psychological outcomes like quality of live, self efficacy, emotional status but also physical exercises (MOVO LISA Program) (Fuchs et.al. 2011, Journal of Physical activity & health
Goal attainment Key component in all kinds of long termn treatment (e.g. rehabilitation, mulitdisciplinary pain treatment) ( Levack 2015, Cochrane review) Best effects for psychological outcomes like quality of live, self efficacy, emotional status but also physical exercises (MOVO LISA Program) (Fuchs et.al. 2011, Journal of Physical activity & health
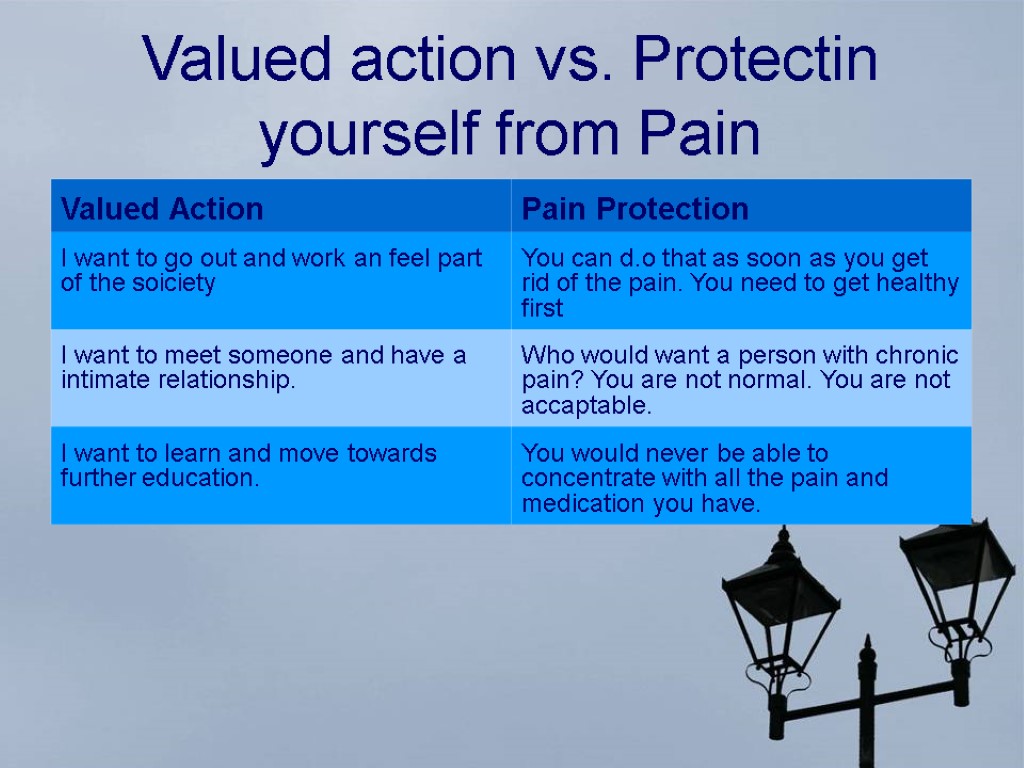
 Values Illness Giving up on a higher education because your are afraid the pain will keep you from being able to concentrate Quitting a job you`d always dreamed of due to the pain it caused you Deciding against having a family because parenting could be difficult if you are in pain
Values Illness Giving up on a higher education because your are afraid the pain will keep you from being able to concentrate Quitting a job you`d always dreamed of due to the pain it caused you Deciding against having a family because parenting could be difficult if you are in pain
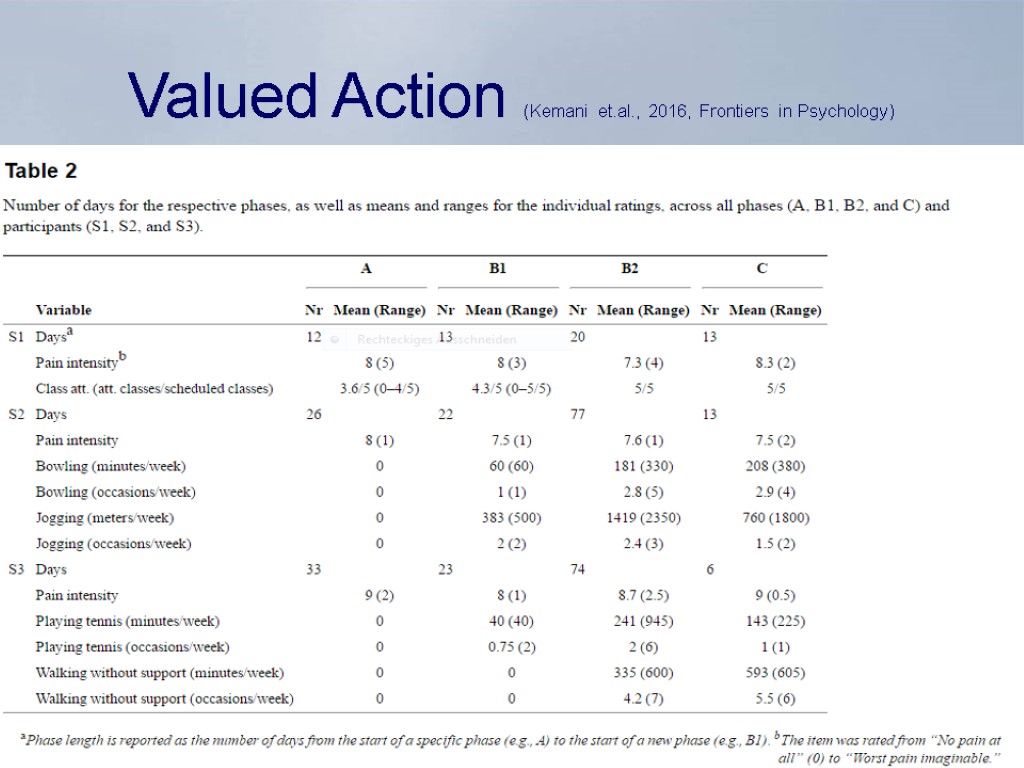
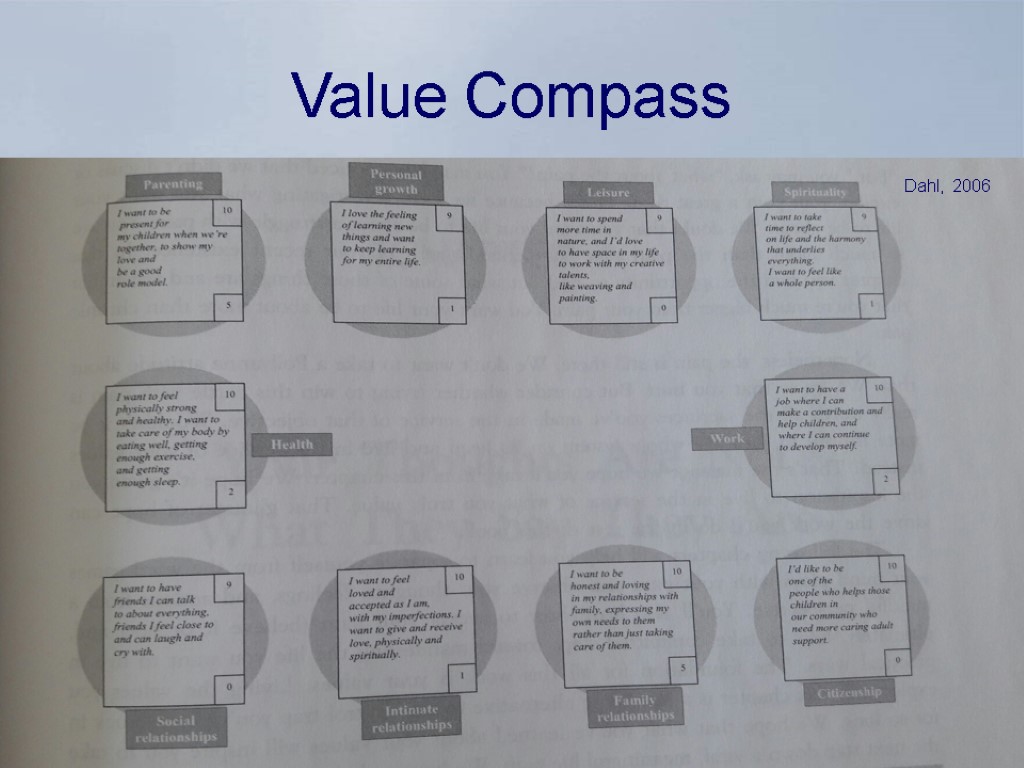
 Goals and Values Key compontent of ACT Therapy (Dahl, 2006) and predictor for individual change patterns (Kemani et. al. 2016, Frontiers in Psychology) Valued Action Study (Kemani et. al. 2016, Frontiers in Psychology) Singe Subject Design study to improve understanding of the process of change in Acceptance and Commitment Therapy for young adults with debilitation pain
Goals and Values Key compontent of ACT Therapy (Dahl, 2006) and predictor for individual change patterns (Kemani et. al. 2016, Frontiers in Psychology) Valued Action Study (Kemani et. al. 2016, Frontiers in Psychology) Singe Subject Design study to improve understanding of the process of change in Acceptance and Commitment Therapy for young adults with debilitation pain
 In summary, the ACT processes of psychopathology all add up to efforts to avoid private experiences such as thoughts, images, emotions and physical sensations. There is a mounting body of empirical evidence that suggests that experiential avoidance is at the root of many, if not most, psychological disorders. Experiential Avoidance
In summary, the ACT processes of psychopathology all add up to efforts to avoid private experiences such as thoughts, images, emotions and physical sensations. There is a mounting body of empirical evidence that suggests that experiential avoidance is at the root of many, if not most, psychological disorders. Experiential Avoidance
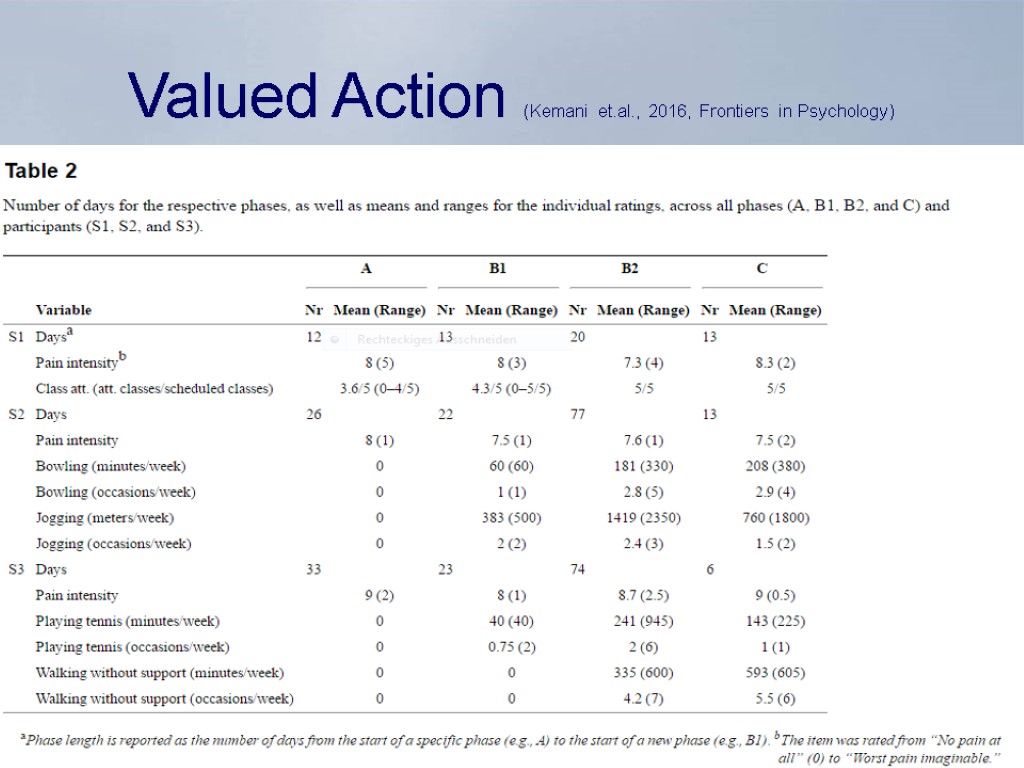 Valued Action (Kemani et.al., 2016, Frontiers in Psychology)
Valued Action (Kemani et.al., 2016, Frontiers in Psychology)
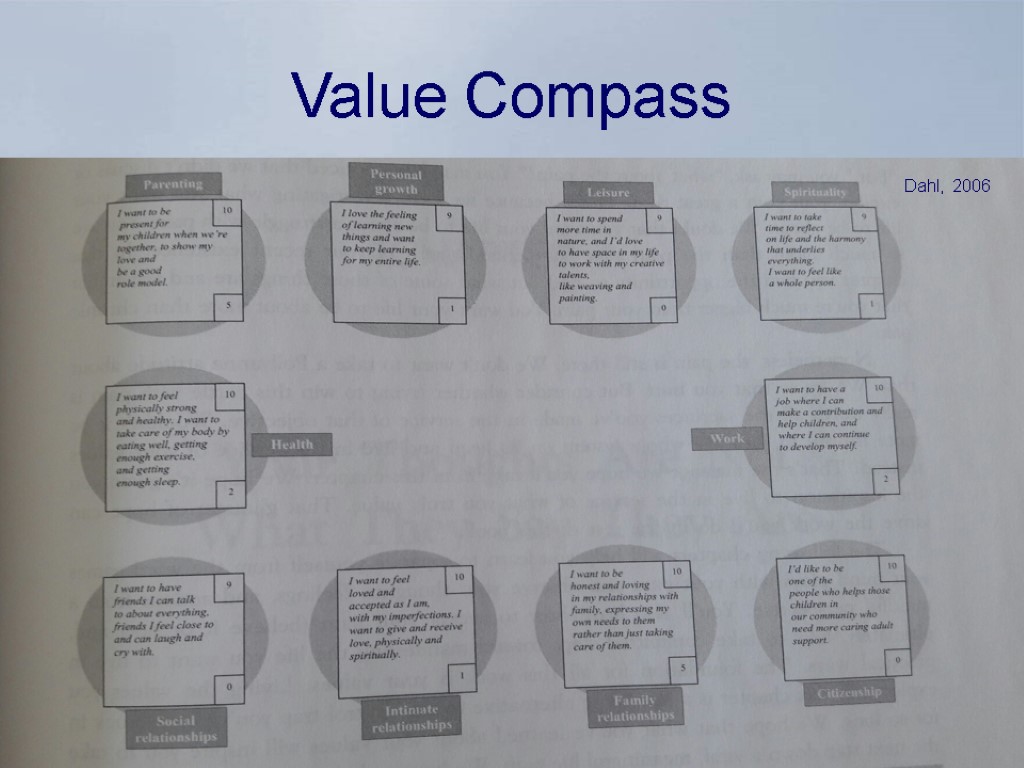 Value Compass Dahl, 2006
Value Compass Dahl, 2006
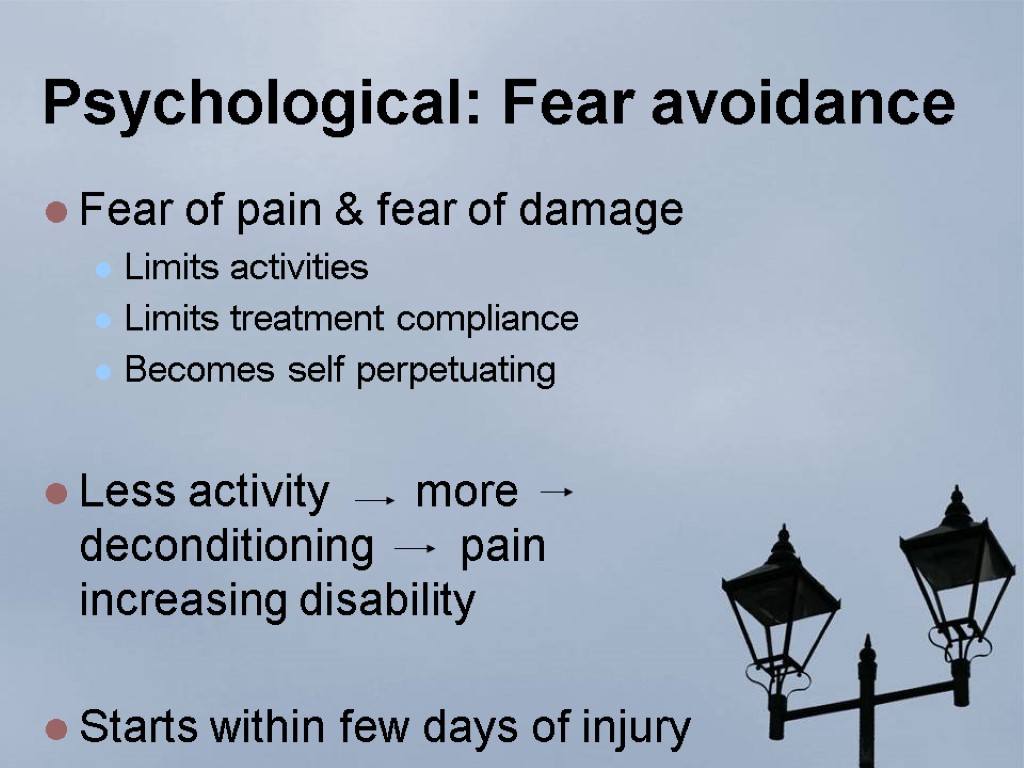
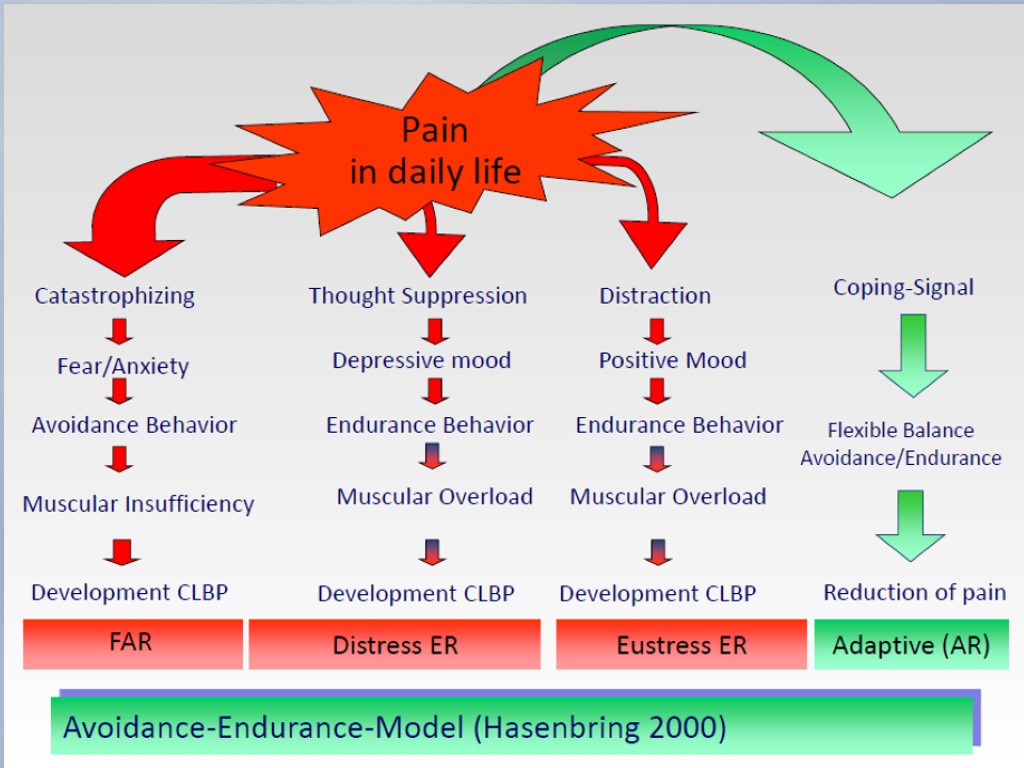
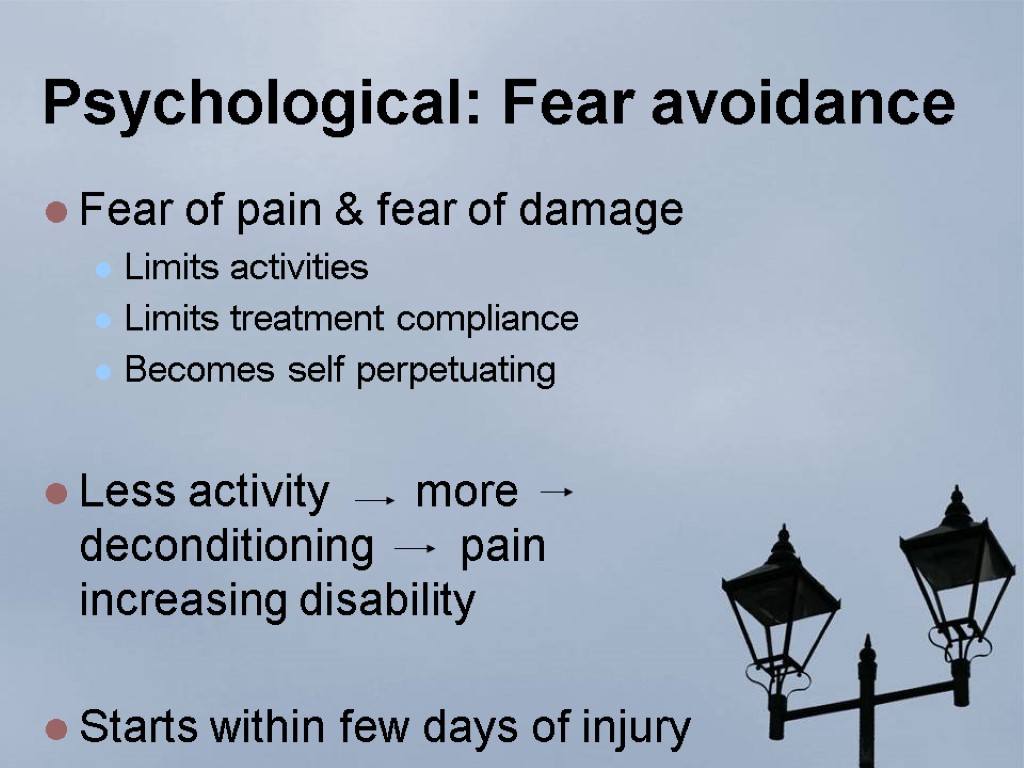 Psychological: Fear avoidance Fear of pain & fear of damage Limits activities Limits treatment compliance Becomes self perpetuating Less activity more deconditioning pain increasing disability Starts within few days of injury
Psychological: Fear avoidance Fear of pain & fear of damage Limits activities Limits treatment compliance Becomes self perpetuating Less activity more deconditioning pain increasing disability Starts within few days of injury
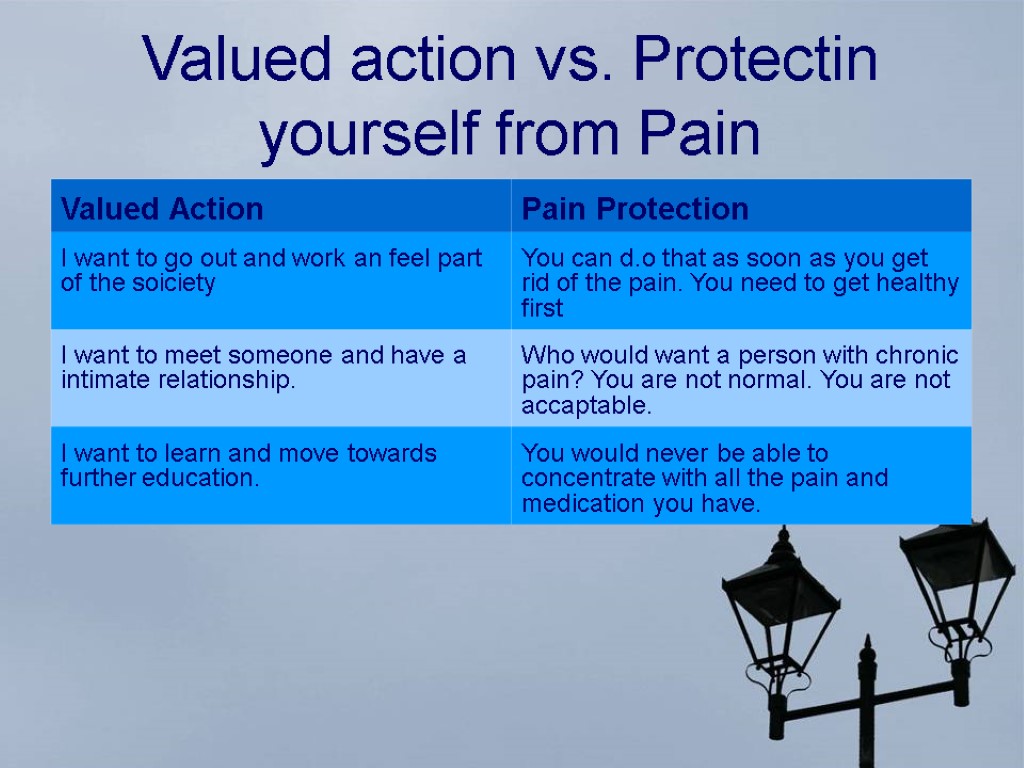 Valued action vs. Protectin yourself from Pain
Valued action vs. Protectin yourself from Pain
 Committed Action Integrated and lasting engagement with valued activities Research shows positive effects for greater life satisfaction, quality of life of patients with chronic pain (McCracken et. al. 2013 The Jounal of Pain) Changes in valued behaviors are independent of changes in pain intensity (Kemani et.al. 2016)
Committed Action Integrated and lasting engagement with valued activities Research shows positive effects for greater life satisfaction, quality of life of patients with chronic pain (McCracken et. al. 2013 The Jounal of Pain) Changes in valued behaviors are independent of changes in pain intensity (Kemani et.al. 2016)
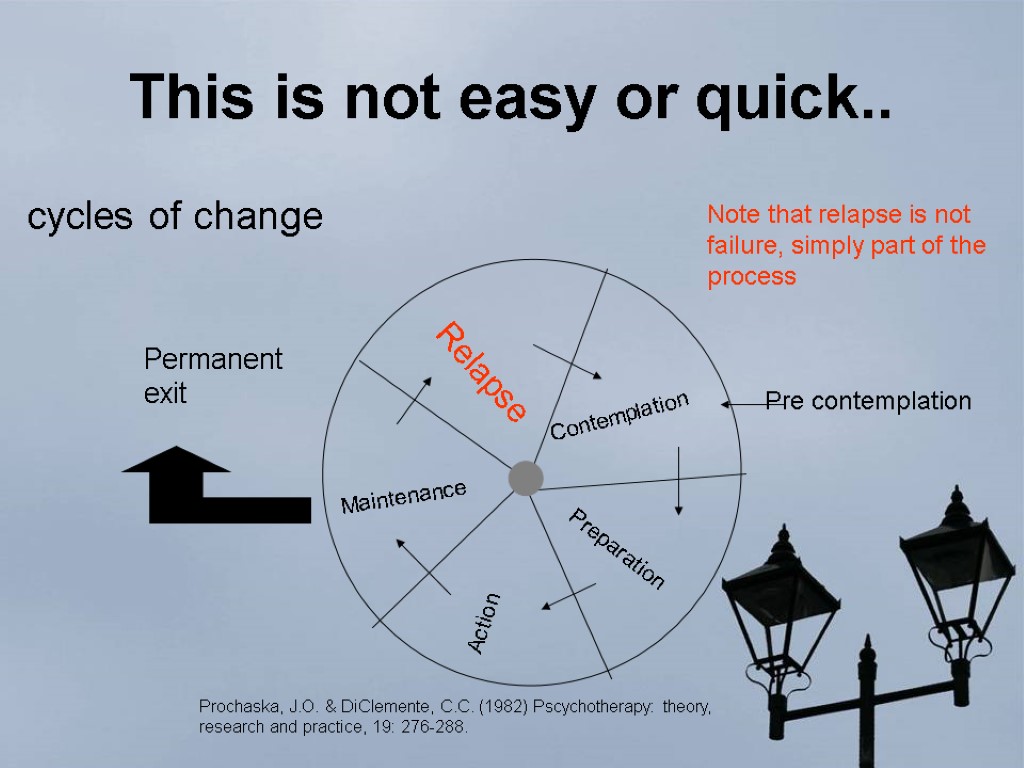
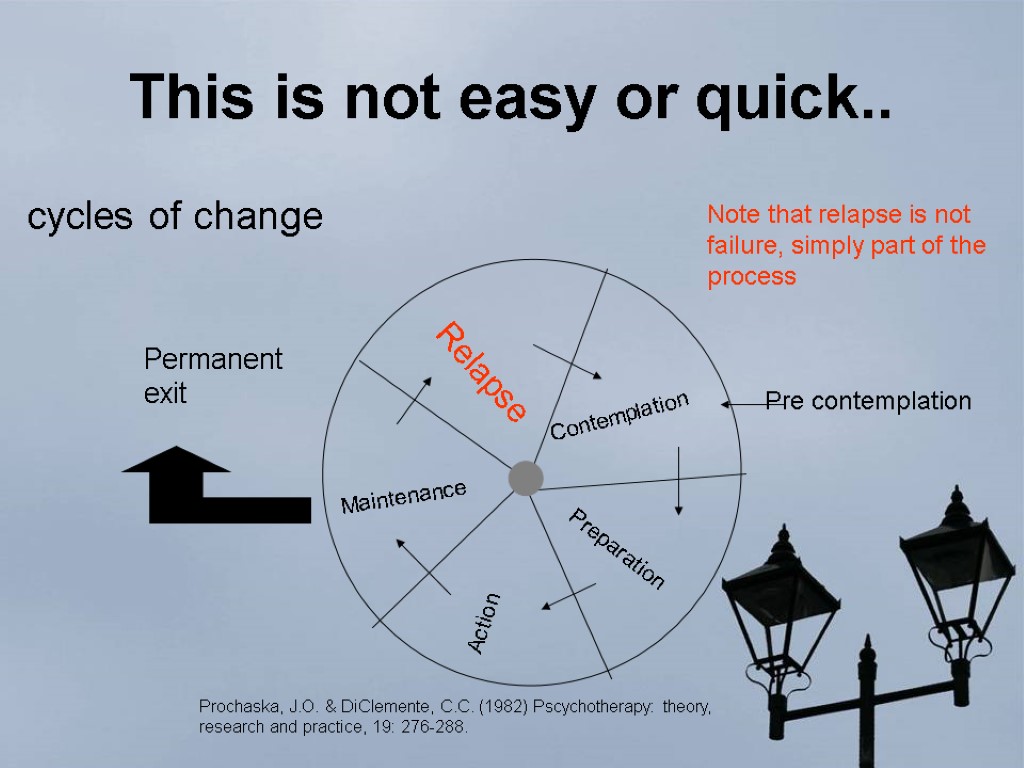 This is not easy or quick.. Contemplation Preparation Action Maintenance Relapse Permanent exit Pre contemplation cycles of change Prochaska, J.O. & DiClemente, C.C. (1982) Pscychotherapy: theory, research and practice, 19: 276-288. Note that relapse is not failure, simply part of the process
This is not easy or quick.. Contemplation Preparation Action Maintenance Relapse Permanent exit Pre contemplation cycles of change Prochaska, J.O. & DiClemente, C.C. (1982) Pscychotherapy: theory, research and practice, 19: 276-288. Note that relapse is not failure, simply part of the process
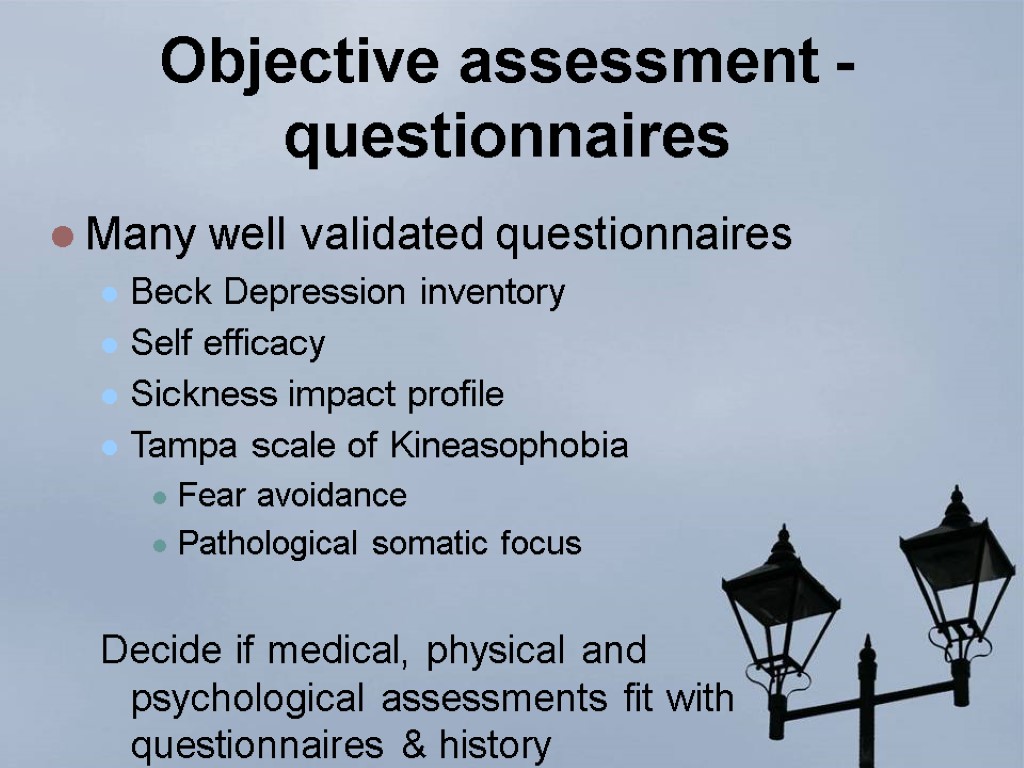
 Objective assessment - questionnaires Many well validated questionnaires Beck Depression inventory Self efficacy Sickness impact profile Tampa scale of Kineasophobia Fear avoidance Pathological somatic focus Decide if medical, physical and psychological assessments fit with questionnaires & history
Objective assessment - questionnaires Many well validated questionnaires Beck Depression inventory Self efficacy Sickness impact profile Tampa scale of Kineasophobia Fear avoidance Pathological somatic focus Decide if medical, physical and psychological assessments fit with questionnaires & history
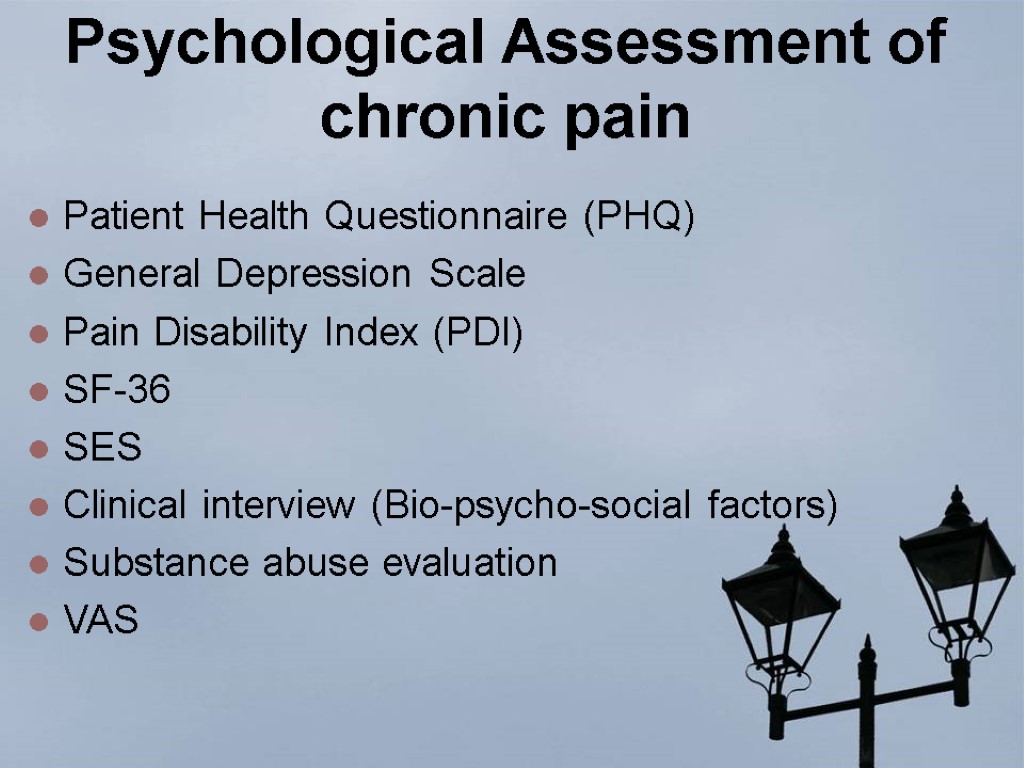
 Psychological Assessment of chronic pain Patient Health Questionnaire (PHQ) General Depression Scale Pain Disability Index (PDI) SF-36 SES Clinical interview (Bio-psycho-social factors) Substance abuse evaluation VAS
Psychological Assessment of chronic pain Patient Health Questionnaire (PHQ) General Depression Scale Pain Disability Index (PDI) SF-36 SES Clinical interview (Bio-psycho-social factors) Substance abuse evaluation VAS
 Psychotherapy
Psychotherapy
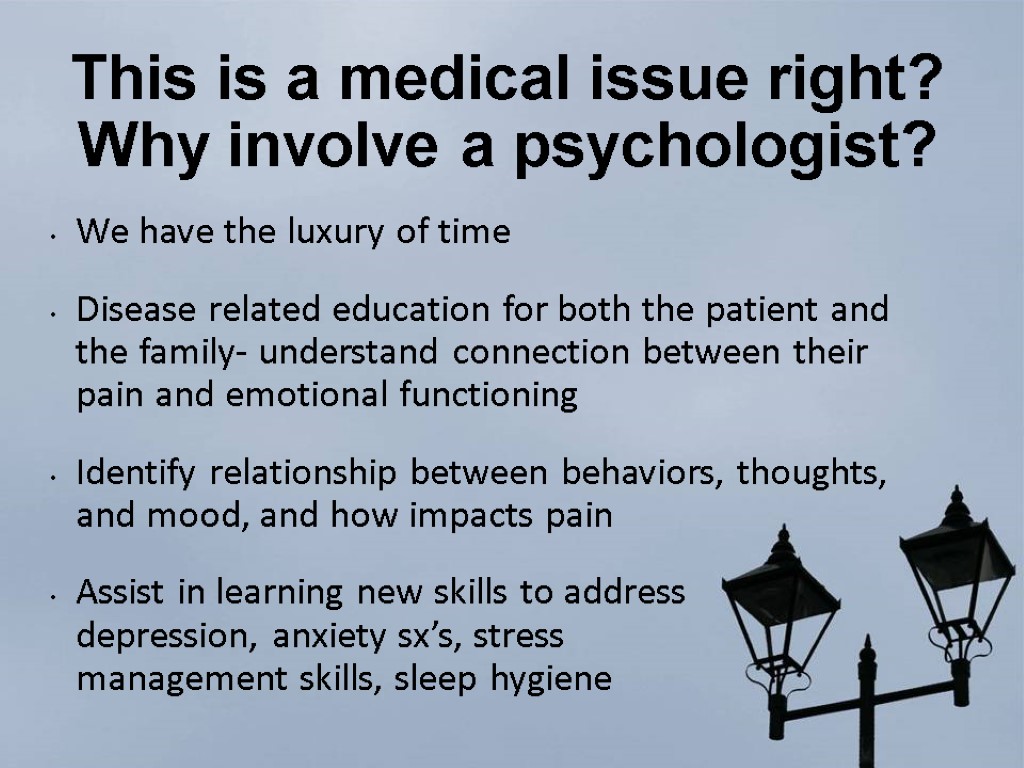
 This is a medical issue right? Why involve a psychologist? We have the luxury of time Disease related education for both the patient and the family- understand connection between their pain and emotional functioning Identify relationship between behaviors, thoughts, and mood, and how impacts pain Assist in learning new skills to address depression, anxiety sx’s, stress management skills, sleep hygiene
This is a medical issue right? Why involve a psychologist? We have the luxury of time Disease related education for both the patient and the family- understand connection between their pain and emotional functioning Identify relationship between behaviors, thoughts, and mood, and how impacts pain Assist in learning new skills to address depression, anxiety sx’s, stress management skills, sleep hygiene
 Overview on psychological treatments Supportive therapies Self-regulatory treatments (SRT) Biofeedback Relaxation training (progressive muscle relaxation; autogenic training) Hypnosis Behavioral interventions (BEH) Altering pain-relevant communication Behavioral activation via contingency management Cognitive-behavioral therapy (CBT) Reconceptualization of pain as problem to solve Coping skills training
Overview on psychological treatments Supportive therapies Self-regulatory treatments (SRT) Biofeedback Relaxation training (progressive muscle relaxation; autogenic training) Hypnosis Behavioral interventions (BEH) Altering pain-relevant communication Behavioral activation via contingency management Cognitive-behavioral therapy (CBT) Reconceptualization of pain as problem to solve Coping skills training
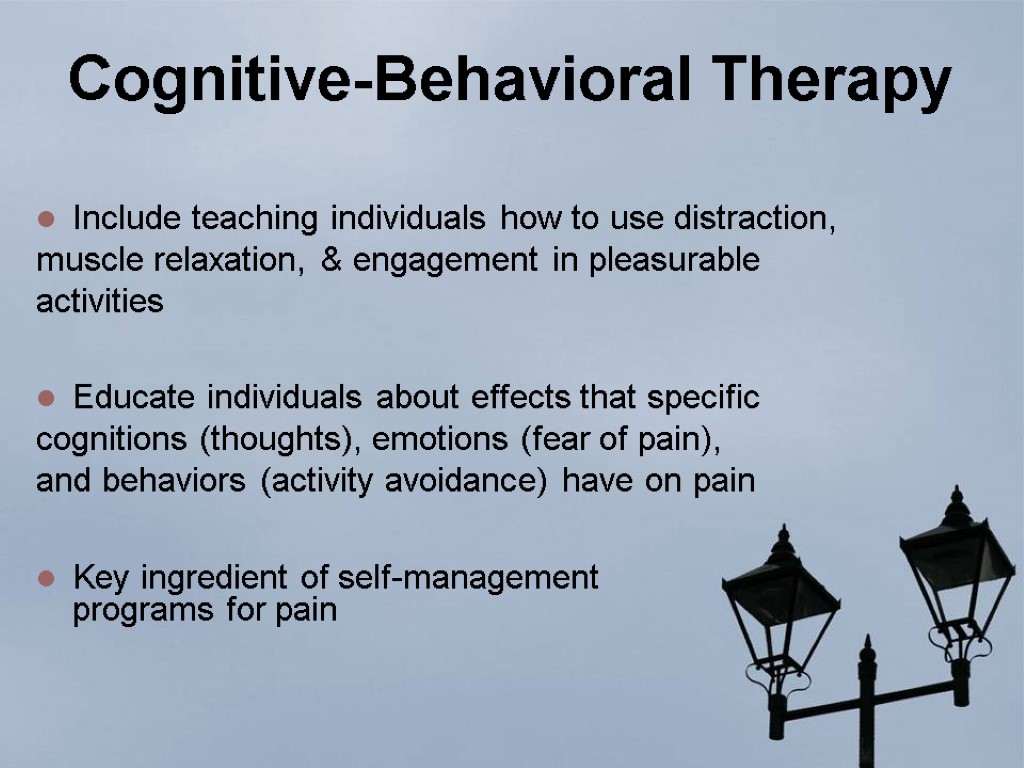
 Cognitive-Behavioral Therapy Include teaching individuals how to use distraction, muscle relaxation, & engagement in pleasurable activities Educate individuals about effects that specific cognitions (thoughts), emotions (fear of pain), and behaviors (activity avoidance) have on pain Key ingredient of self-management programs for pain
Cognitive-Behavioral Therapy Include teaching individuals how to use distraction, muscle relaxation, & engagement in pleasurable activities Educate individuals about effects that specific cognitions (thoughts), emotions (fear of pain), and behaviors (activity avoidance) have on pain Key ingredient of self-management programs for pain
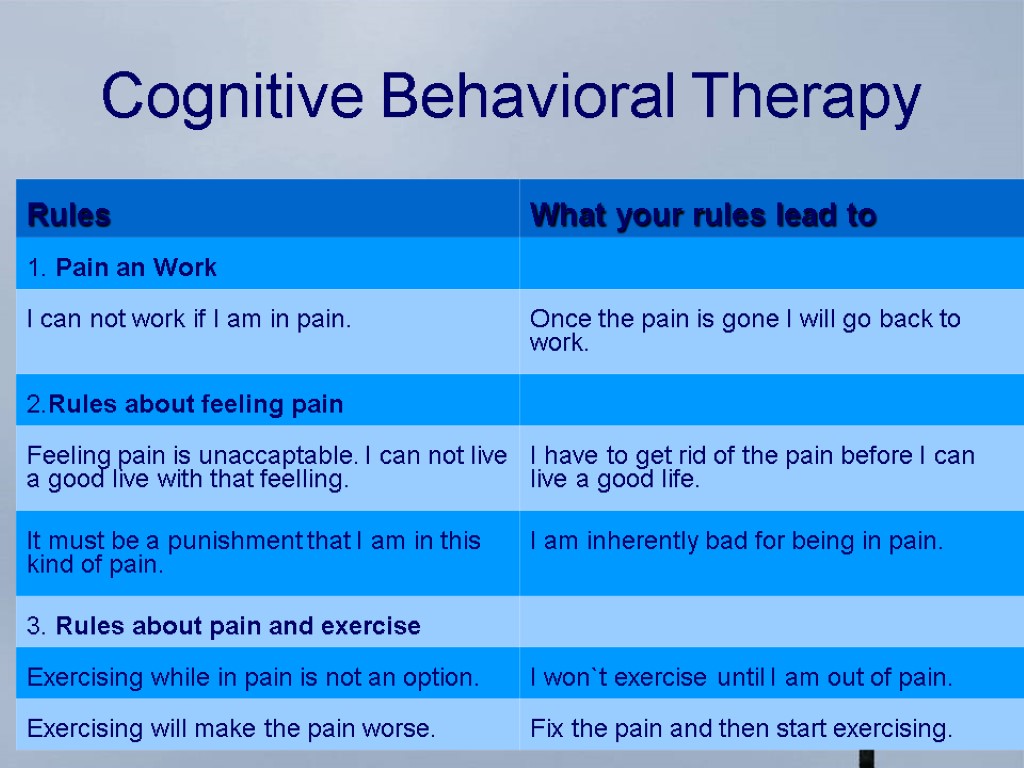
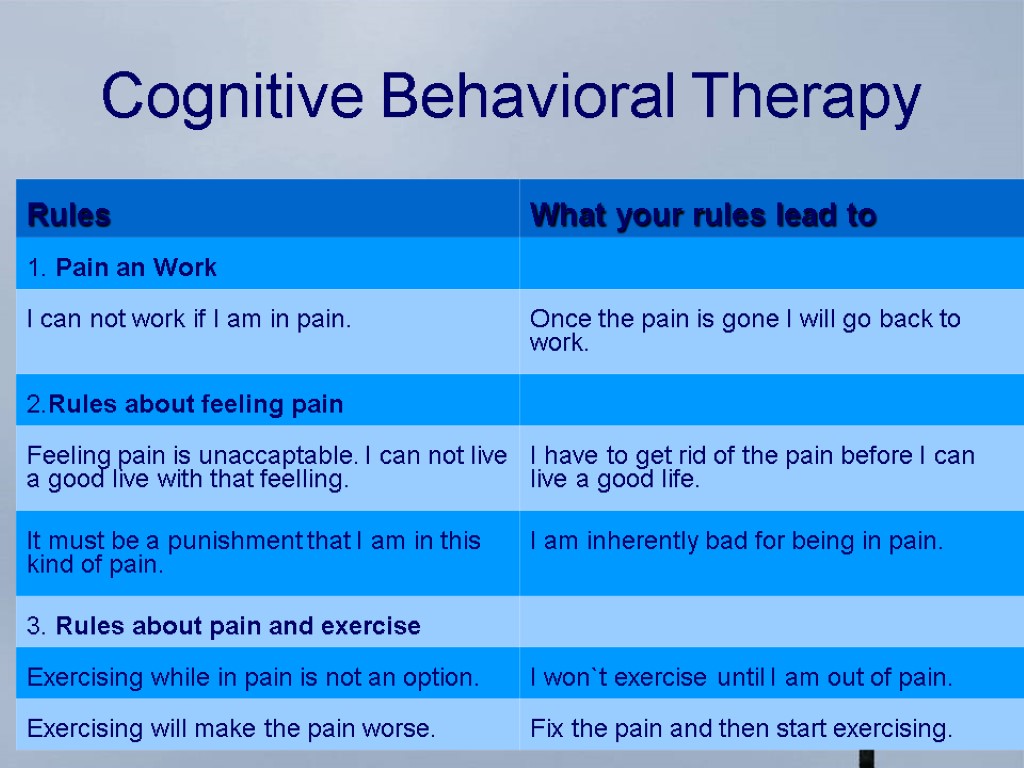 Cognitive Behavioral Therapy
Cognitive Behavioral Therapy
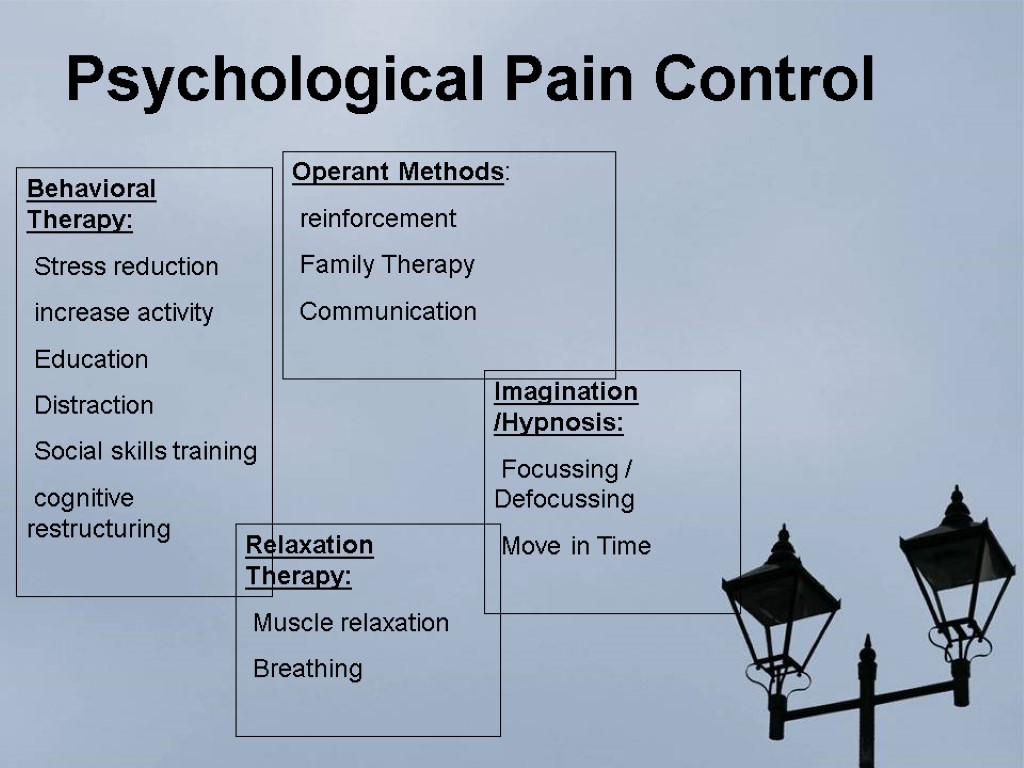
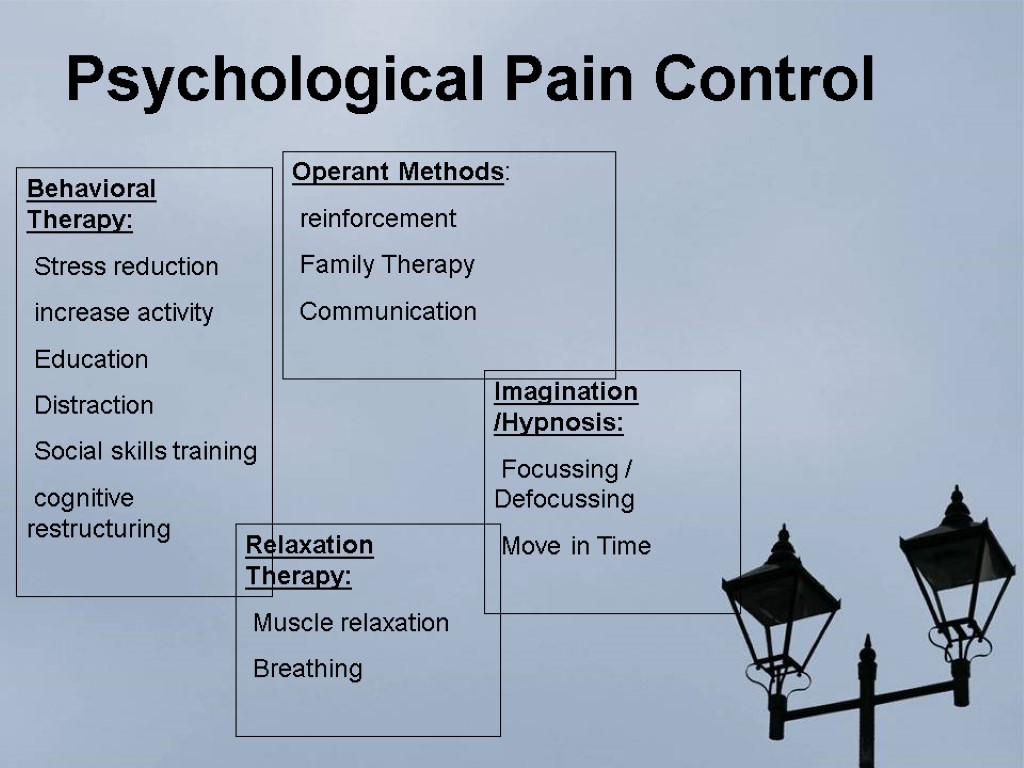 Psychological Pain Control Behavioral Therapy: Stress reduction increase activity Education Distraction Social skills training cognitive restructuring Relaxation Therapy: Muscle relaxation Breathing Imagination /Hypnosis: Focussing / Defocussing Move in Time Operant Methods: reinforcement Family Therapy Communication
Psychological Pain Control Behavioral Therapy: Stress reduction increase activity Education Distraction Social skills training cognitive restructuring Relaxation Therapy: Muscle relaxation Breathing Imagination /Hypnosis: Focussing / Defocussing Move in Time Operant Methods: reinforcement Family Therapy Communication
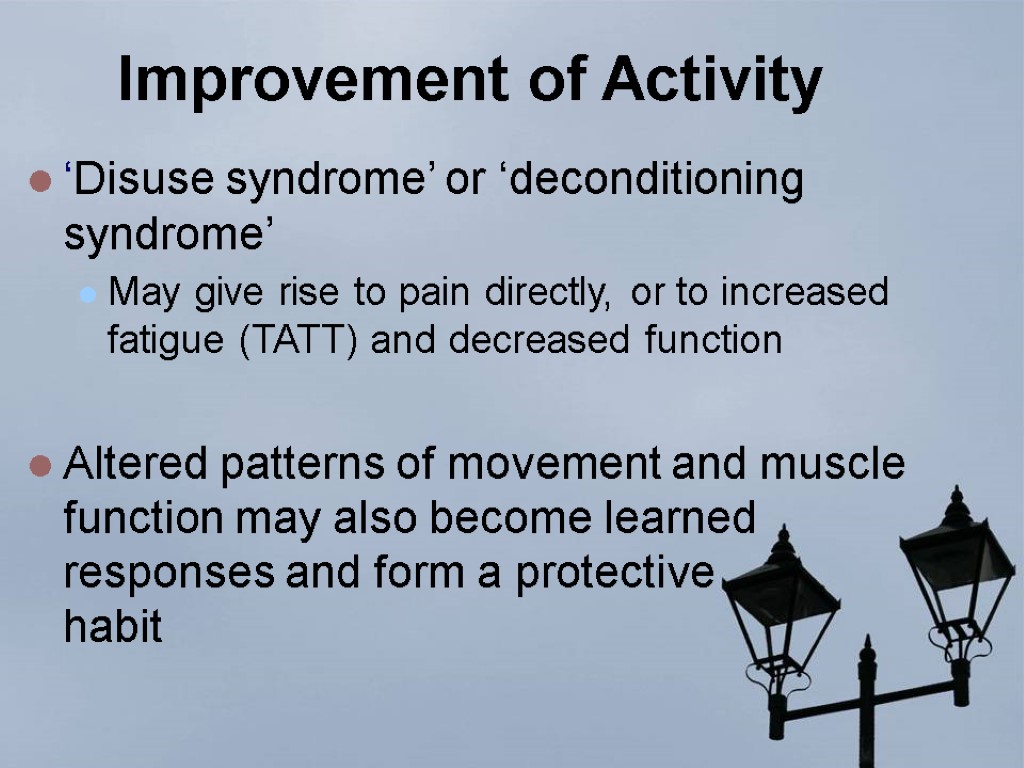 Improvement of Activity ‘Disuse syndrome’ or ‘deconditioning syndrome’ May give rise to pain directly, or to increased fatigue (TATT) and decreased function Altered patterns of movement and muscle function may also become learned responses and form a protective habit
Improvement of Activity ‘Disuse syndrome’ or ‘deconditioning syndrome’ May give rise to pain directly, or to increased fatigue (TATT) and decreased function Altered patterns of movement and muscle function may also become learned responses and form a protective habit
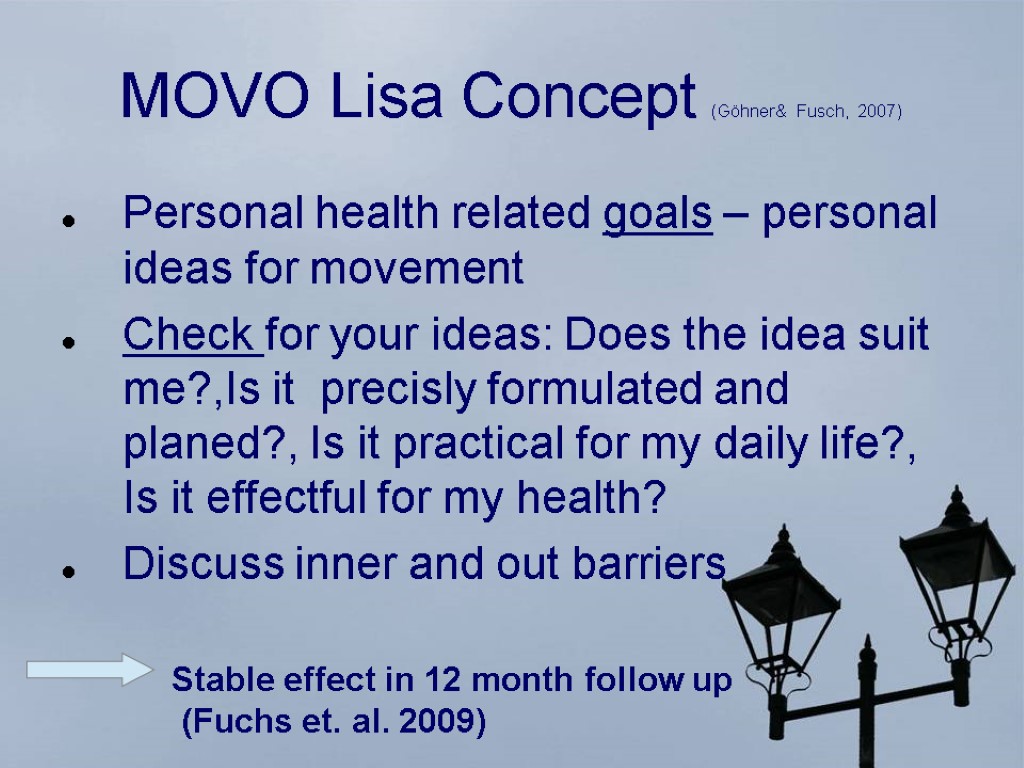 MOVO Lisa Concept (Göhner& Fusch, 2007) Personal health related goals – personal ideas for movement Check for your ideas: Does the idea suit me?,Is it precisly formulated and planed?, Is it practical for my daily life?, Is it effectful for my health? Discuss inner and out barriers Stable effect in 12 month follow up (Fuchs et. al. 2009)
MOVO Lisa Concept (Göhner& Fusch, 2007) Personal health related goals – personal ideas for movement Check for your ideas: Does the idea suit me?,Is it precisly formulated and planed?, Is it practical for my daily life?, Is it effectful for my health? Discuss inner and out barriers Stable effect in 12 month follow up (Fuchs et. al. 2009)
 Relaxation Techniques Body Scan Imagination Walking meditation Mindfulness (e.g. mindful reading, breathing) Distraction Biofeedback Hypnosis
Relaxation Techniques Body Scan Imagination Walking meditation Mindfulness (e.g. mindful reading, breathing) Distraction Biofeedback Hypnosis
 Definition ‘ACT is a psychological intervention based on modern behavioural psychology, that applies mindfulness and acceptance processes, and commitment and behavior change processes, to the creation of psychological flexibility’
Definition ‘ACT is a psychological intervention based on modern behavioural psychology, that applies mindfulness and acceptance processes, and commitment and behavior change processes, to the creation of psychological flexibility’
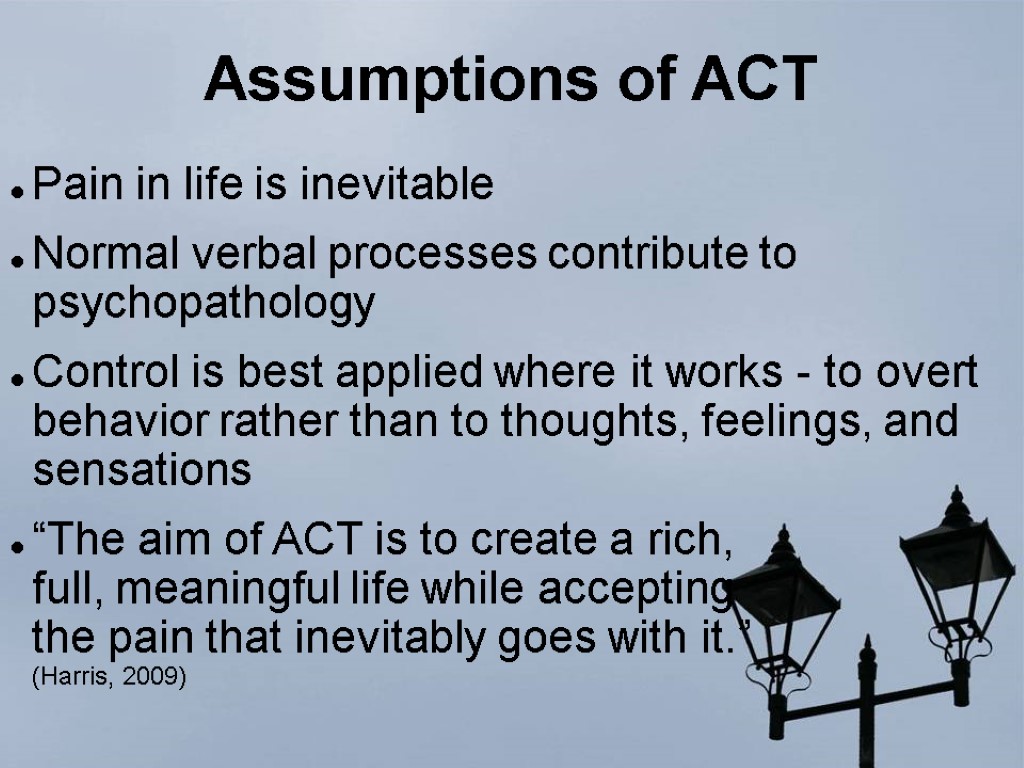
 Assumptions of ACT Pain in life is inevitable Normal verbal processes contribute to psychopathology Control is best applied where it works - to overt behavior rather than to thoughts, feelings, and sensations “The aim of ACT is to create a rich, full, meaningful life while accepting the pain that inevitably goes with it.” (Harris, 2009)
Assumptions of ACT Pain in life is inevitable Normal verbal processes contribute to psychopathology Control is best applied where it works - to overt behavior rather than to thoughts, feelings, and sensations “The aim of ACT is to create a rich, full, meaningful life while accepting the pain that inevitably goes with it.” (Harris, 2009)
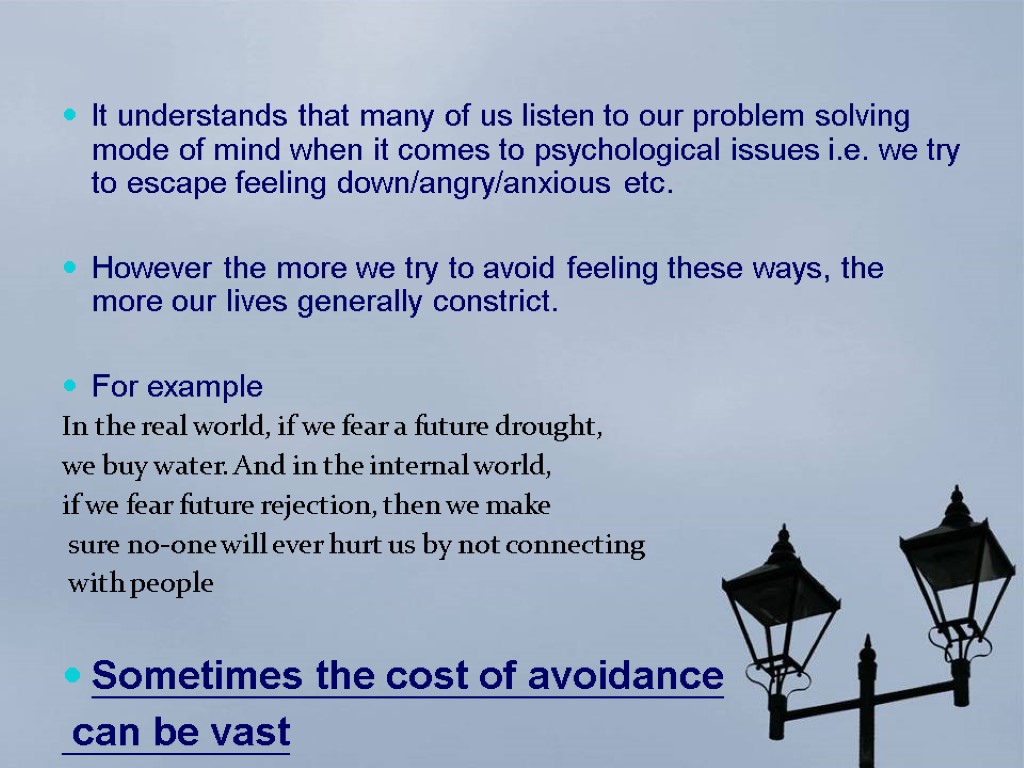
 It understands that many of us listen to our problem solving mode of mind when it comes to psychological issues i.e. we try to escape feeling down/angry/anxious etc. However the more we try to avoid feeling these ways, the more our lives generally constrict. For example In the real world, if we fear a future drought, we buy water. And in the internal world, if we fear future rejection, then we make sure no-one will ever hurt us by not connecting with people Sometimes the cost of avoidance can be vast
It understands that many of us listen to our problem solving mode of mind when it comes to psychological issues i.e. we try to escape feeling down/angry/anxious etc. However the more we try to avoid feeling these ways, the more our lives generally constrict. For example In the real world, if we fear a future drought, we buy water. And in the internal world, if we fear future rejection, then we make sure no-one will ever hurt us by not connecting with people Sometimes the cost of avoidance can be vast
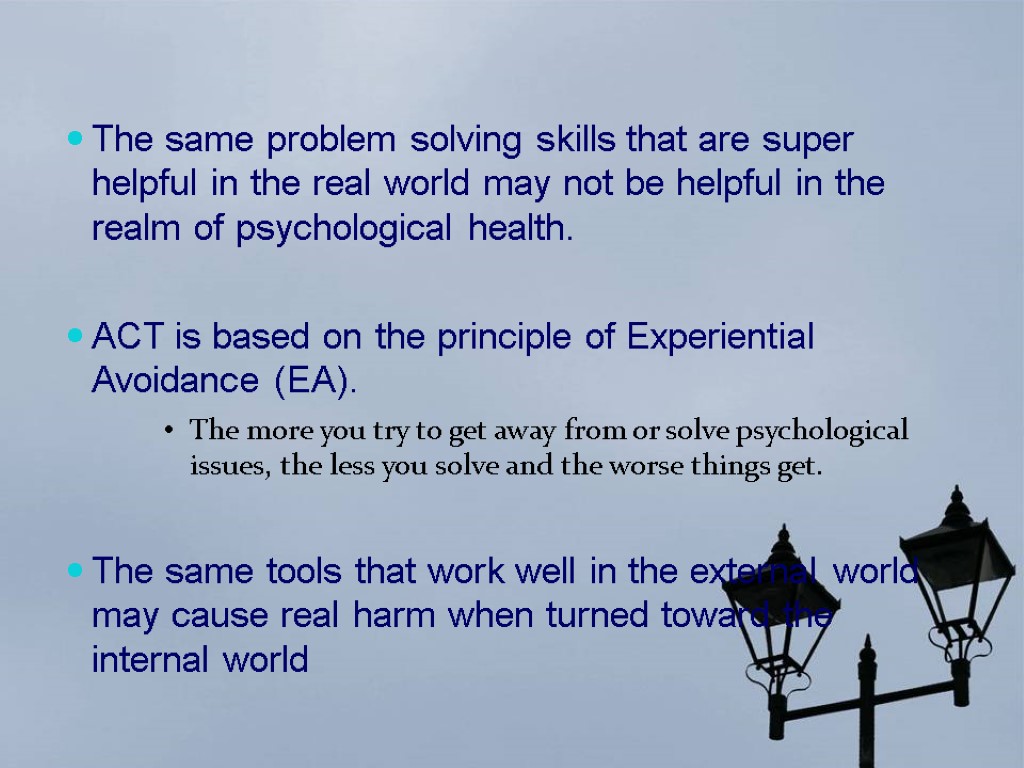
 The same problem solving skills that are super helpful in the real world may not be helpful in the realm of psychological health. ACT is based on the principle of Experiential Avoidance (EA). The more you try to get away from or solve psychological issues, the less you solve and the worse things get. The same tools that work well in the external world may cause real harm when turned toward the internal world
The same problem solving skills that are super helpful in the real world may not be helpful in the realm of psychological health. ACT is based on the principle of Experiential Avoidance (EA). The more you try to get away from or solve psychological issues, the less you solve and the worse things get. The same tools that work well in the external world may cause real harm when turned toward the internal world
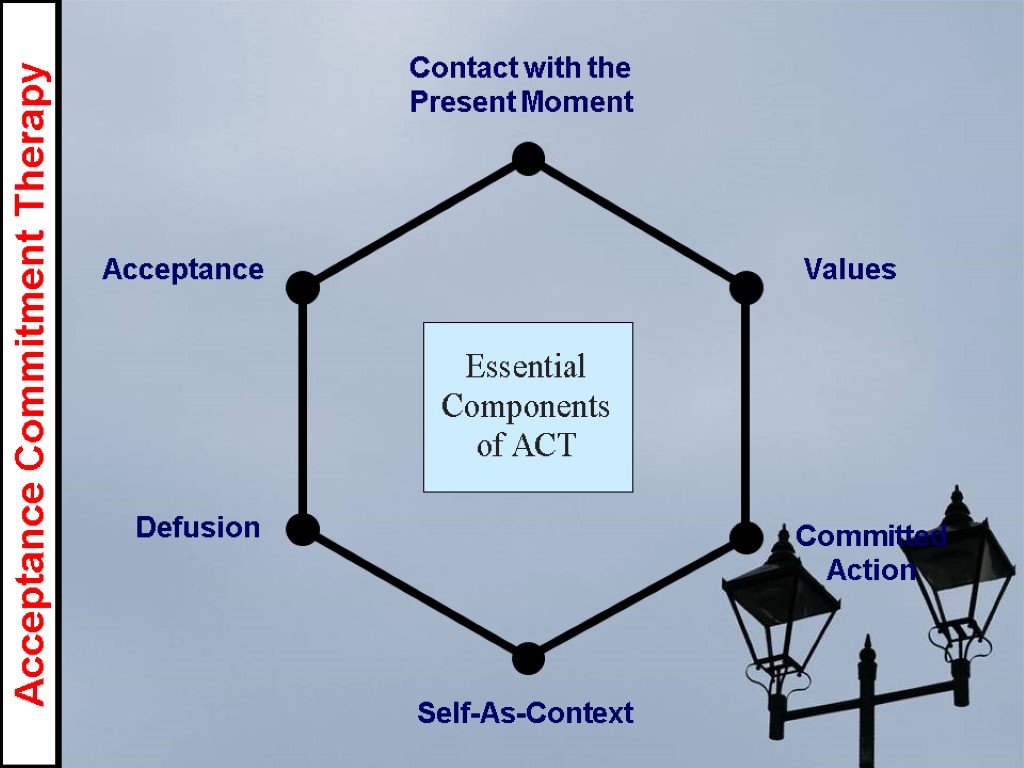
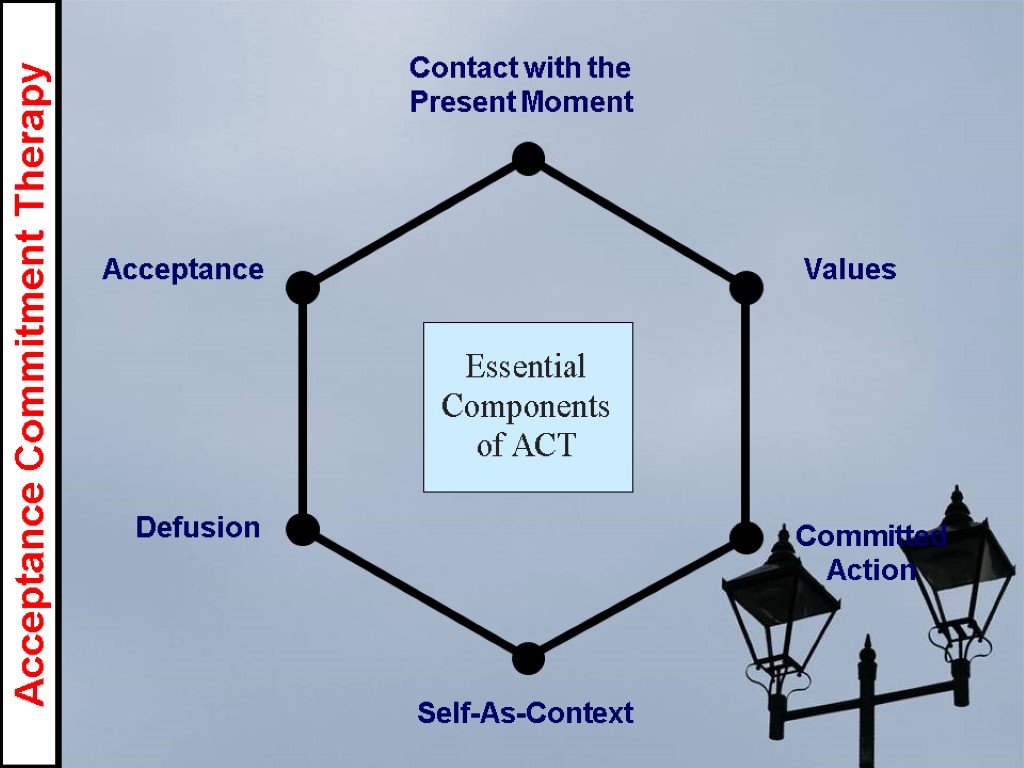 Acceptance Defusion Self-As-Context Contact with the Present Moment Values Committed Action Acceptance Commitment Therapy
Acceptance Defusion Self-As-Context Contact with the Present Moment Values Committed Action Acceptance Commitment Therapy
 Defusion The core theoretical posture behind mainstream CBT is that clients need to rid themselves of negative unwanted content to facilitate behavior change ACT and other third wave therapies are the exact opposite to this ACT suggests that people can live and behave in a value consistent manner in the face of challenging thoughts To help them do this ‘defusion’ aims to create distance between the client and their thoughts
Defusion The core theoretical posture behind mainstream CBT is that clients need to rid themselves of negative unwanted content to facilitate behavior change ACT and other third wave therapies are the exact opposite to this ACT suggests that people can live and behave in a value consistent manner in the face of challenging thoughts To help them do this ‘defusion’ aims to create distance between the client and their thoughts
 Defusion People in general tend to be fused with thoughts, and attach some literal truth and importance to them However in some context these thoughts are not helpful Defusion techniques aim to reduce the impact of thoughts by altering their believability Defusion examples include I’m having the thought Word repetition exercise Thanking your mind Silly voices
Defusion People in general tend to be fused with thoughts, and attach some literal truth and importance to them However in some context these thoughts are not helpful Defusion techniques aim to reduce the impact of thoughts by altering their believability Defusion examples include I’m having the thought Word repetition exercise Thanking your mind Silly voices
 Mindfulness Jon Kabat-Zinn has been the leading figure in bringing mindfulness to the fore in recent decades. His approach to mindfulness involves: deliberately paying attention to everything, using all the senses, to be in the present moment, and to let each experience happen moment by moment without judgement.
Mindfulness Jon Kabat-Zinn has been the leading figure in bringing mindfulness to the fore in recent decades. His approach to mindfulness involves: deliberately paying attention to everything, using all the senses, to be in the present moment, and to let each experience happen moment by moment without judgement.
 Being present Too many of us live our lives ruminating on the past or worrying about the future When we do this we lose contact with the present moment, and all that it offers to us ACT promotes on-going non judgemental contact with psychological and environmental events as they occur When in the present moment, people are flexible, responsive and aware of the possibilities afforded by the context This, in popular psychology is called mindfulness The ability to control our attention in a flexible manner
Being present Too many of us live our lives ruminating on the past or worrying about the future When we do this we lose contact with the present moment, and all that it offers to us ACT promotes on-going non judgemental contact with psychological and environmental events as they occur When in the present moment, people are flexible, responsive and aware of the possibilities afforded by the context This, in popular psychology is called mindfulness The ability to control our attention in a flexible manner
 Five Steps to Mindfulness 1) Mindful Breathing 2) Concentration 3) Awareness of Your Body 4) Releasing Tension 5) Walking Meditation
Five Steps to Mindfulness 1) Mindful Breathing 2) Concentration 3) Awareness of Your Body 4) Releasing Tension 5) Walking Meditation
 Relaxation: Deep breathing Make yourself comfortable Begin by listening to your breathing without changing its natural pattern Breathe through your nose (or mouth if your nose is blocked) Put your hands over your stomach area and feel your hands rise and fall. Imagine you are breathing into your hands. Relax your stomach muscles. Take deep, slow breaths. Remember to breathe at your own pace As you breathe out, imagine your tensions are being breathed away. Every time you breathe in, imagine you are breathing in peace
Relaxation: Deep breathing Make yourself comfortable Begin by listening to your breathing without changing its natural pattern Breathe through your nose (or mouth if your nose is blocked) Put your hands over your stomach area and feel your hands rise and fall. Imagine you are breathing into your hands. Relax your stomach muscles. Take deep, slow breaths. Remember to breathe at your own pace As you breathe out, imagine your tensions are being breathed away. Every time you breathe in, imagine you are breathing in peace
 Why long- term treatment?
Why long- term treatment?
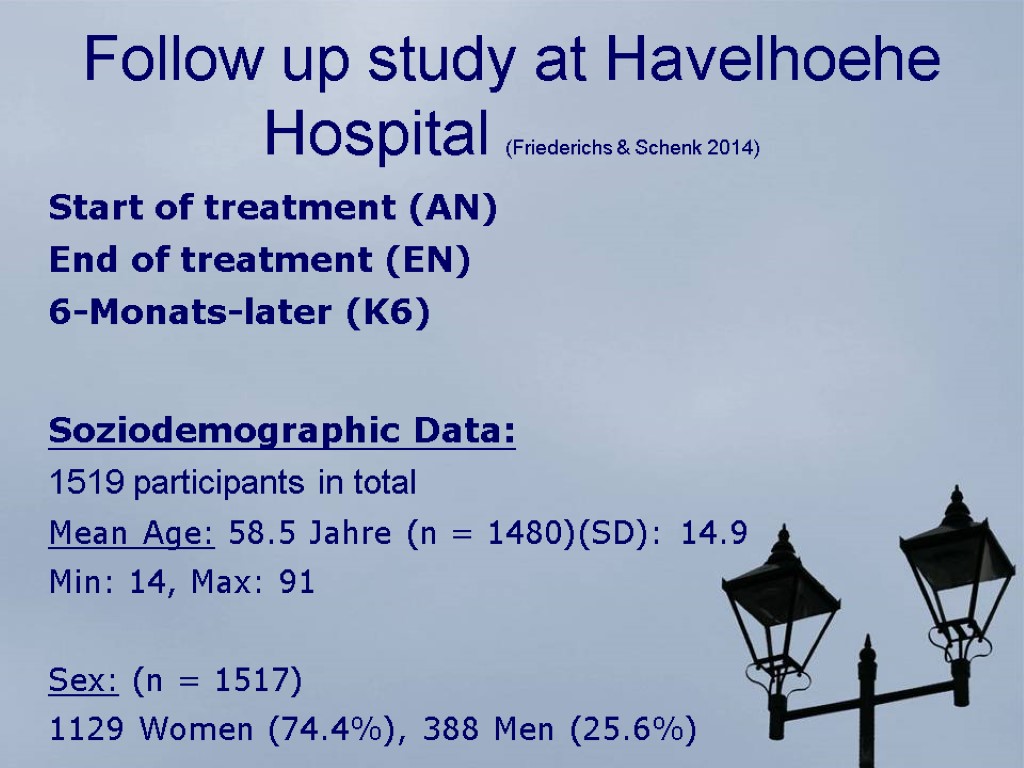
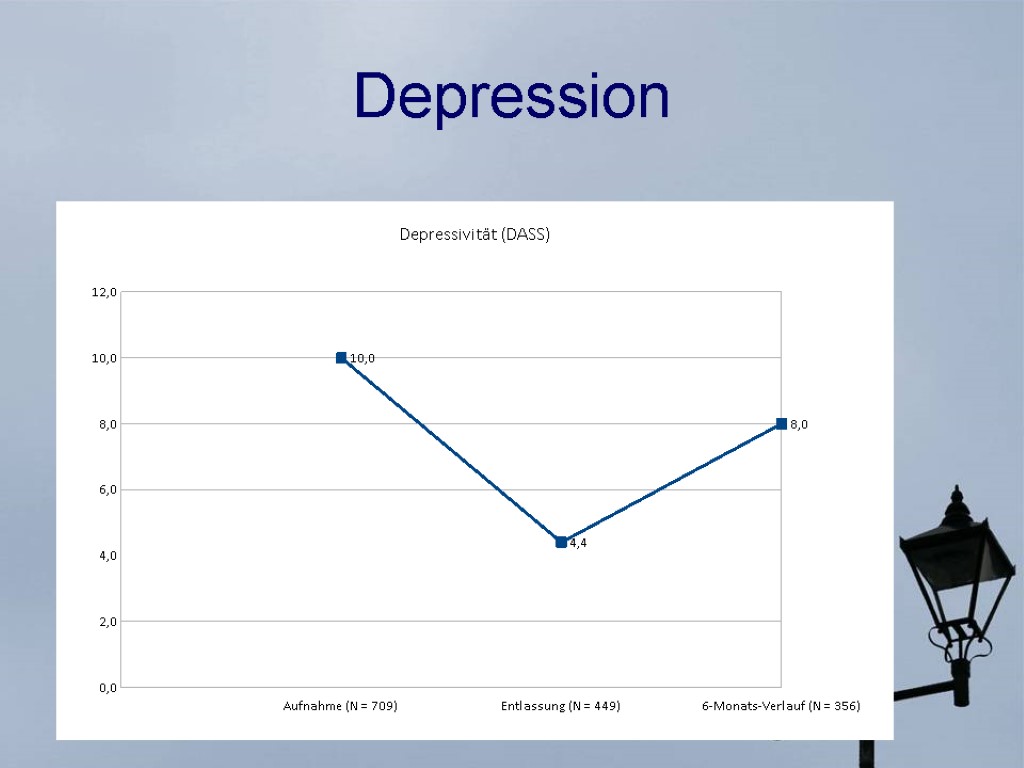
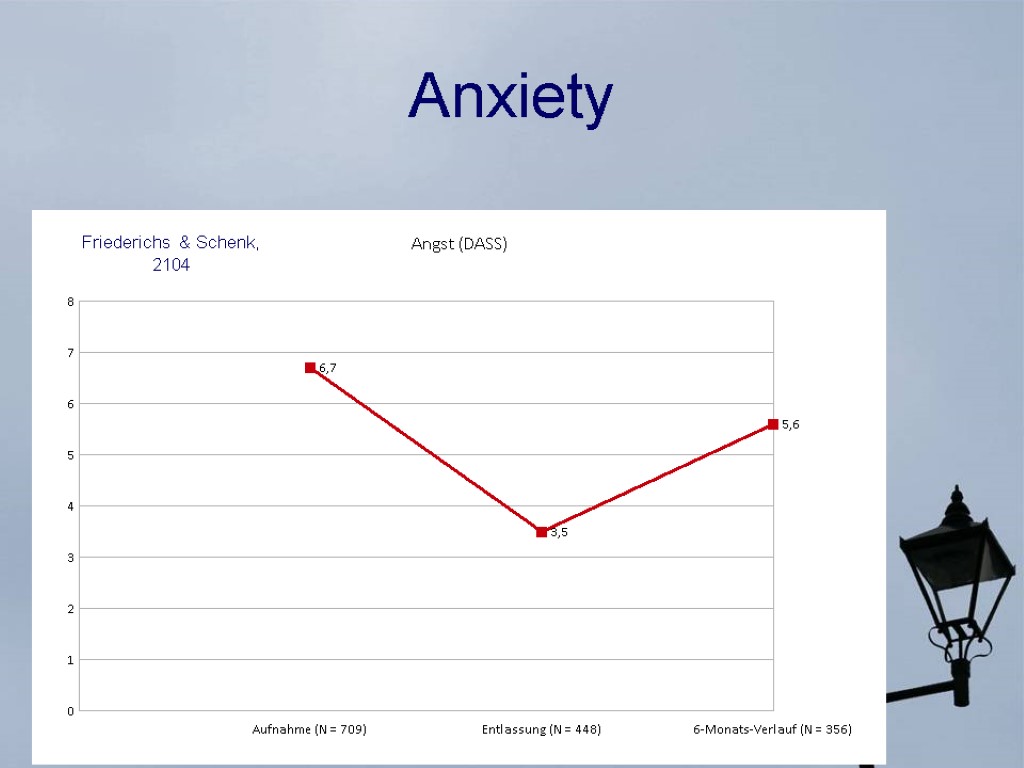
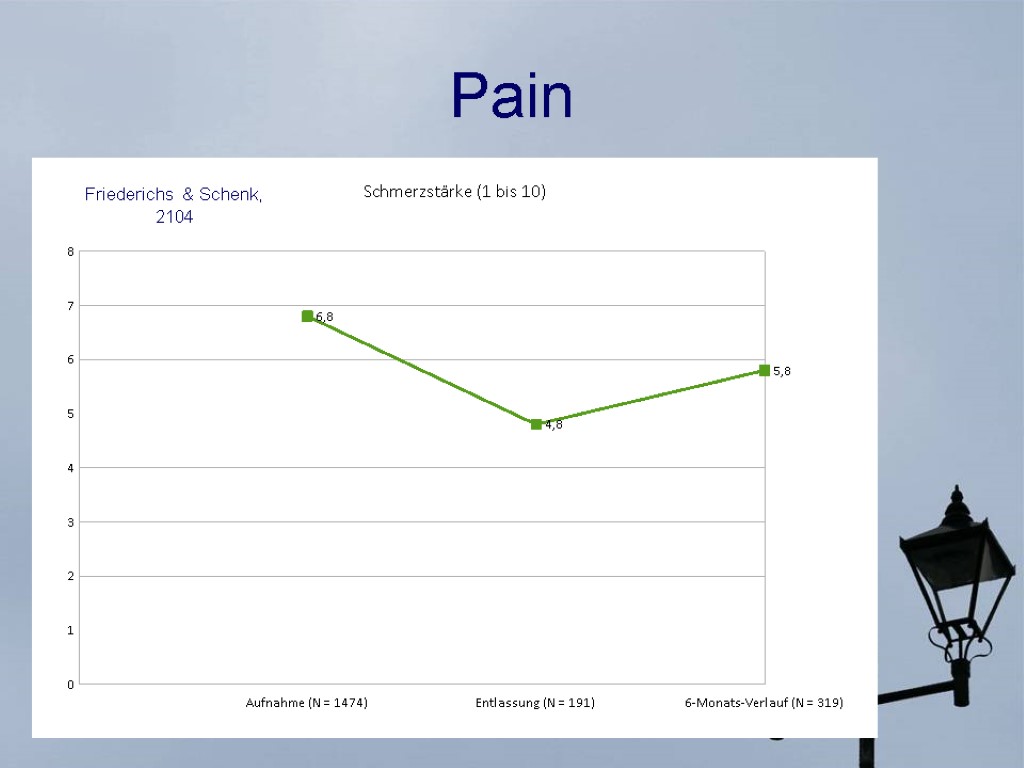
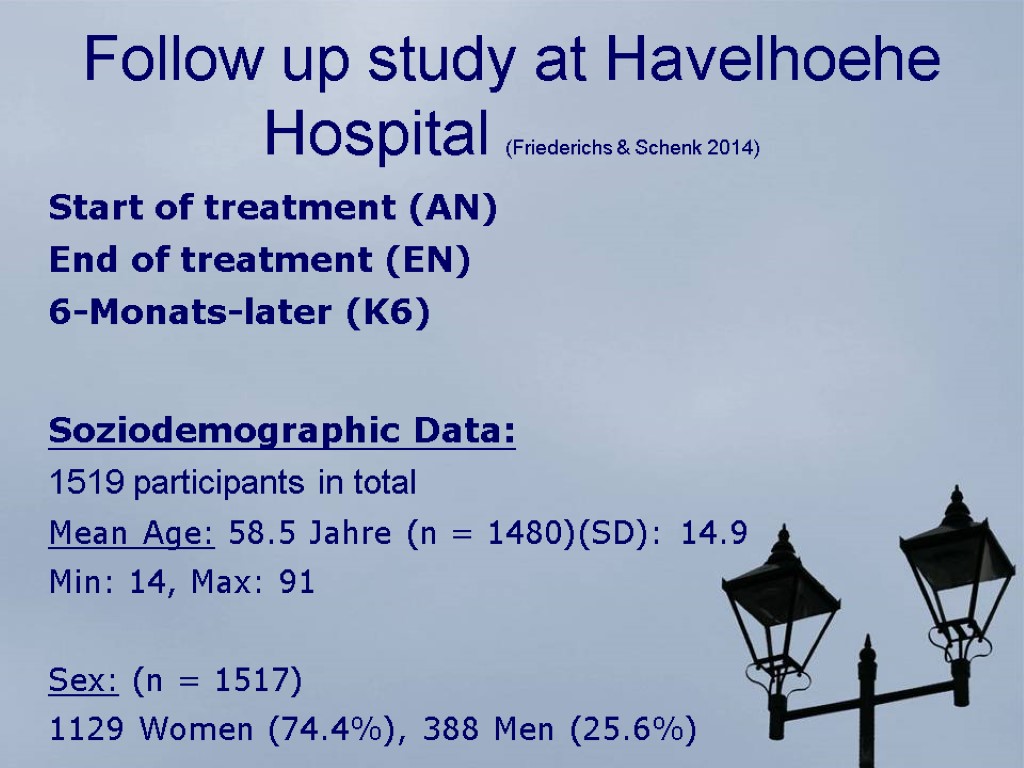 Follow up study at Havelhoehe Hospital (Friederichs & Schenk 2014) Start of treatment (AN) End of treatment (EN) 6-Monats-later (K6) Soziodemographic Data: 1519 participants in total Mean Age: 58.5 Jahre (n = 1480)(SD): 14.9 Min: 14, Max: 91 Sex: (n = 1517) 1129 Women (74.4%), 388 Men (25.6%)
Follow up study at Havelhoehe Hospital (Friederichs & Schenk 2014) Start of treatment (AN) End of treatment (EN) 6-Monats-later (K6) Soziodemographic Data: 1519 participants in total Mean Age: 58.5 Jahre (n = 1480)(SD): 14.9 Min: 14, Max: 91 Sex: (n = 1517) 1129 Women (74.4%), 388 Men (25.6%)
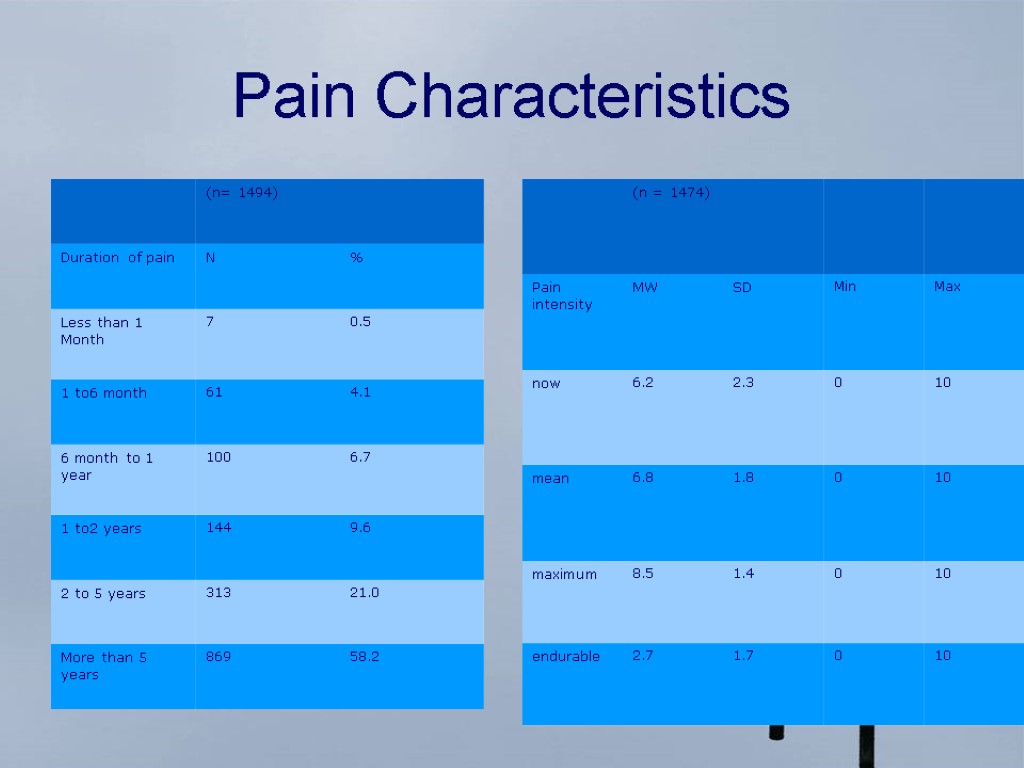
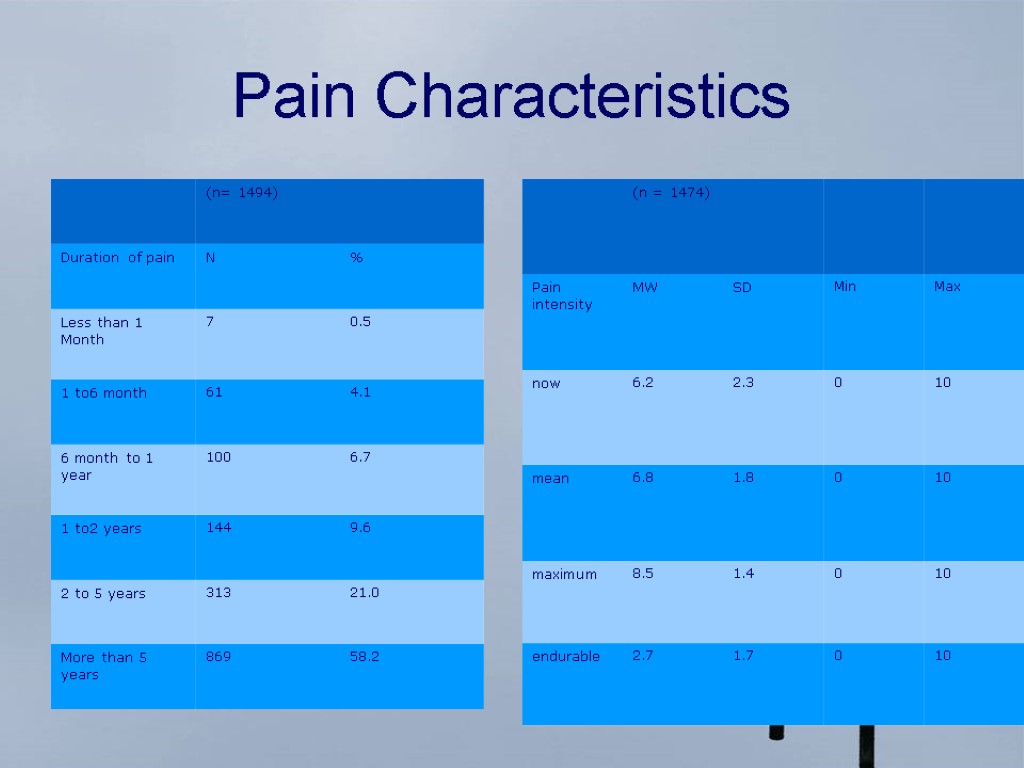 Pain Characteristics
Pain Characteristics
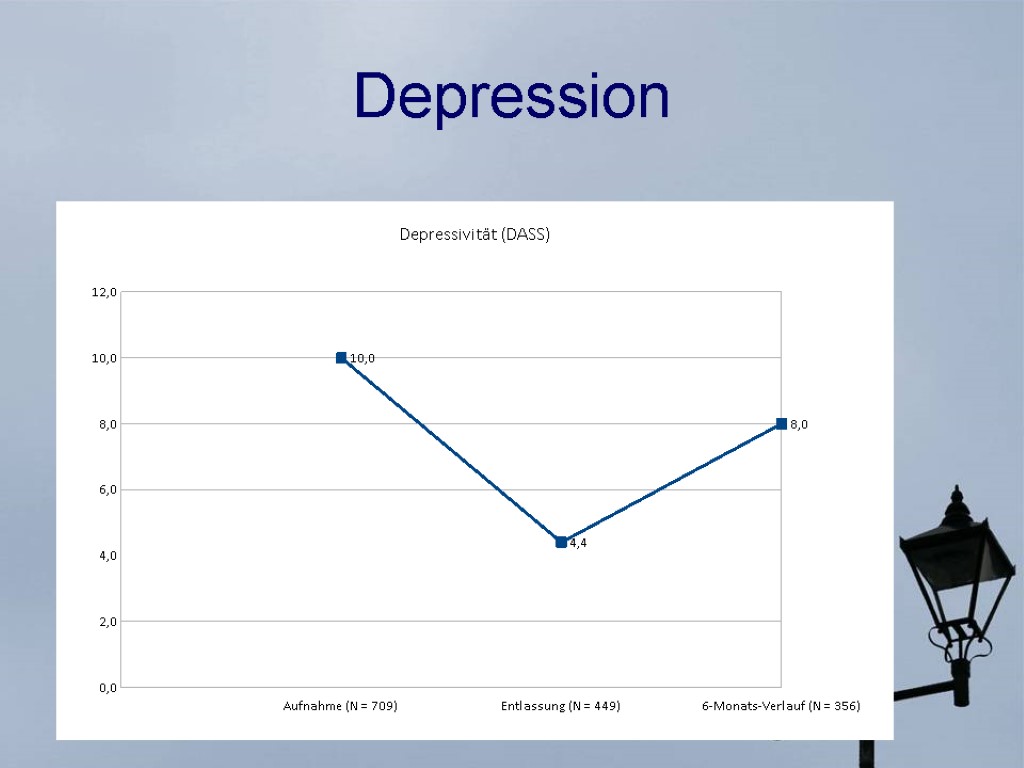 Depression
Depression
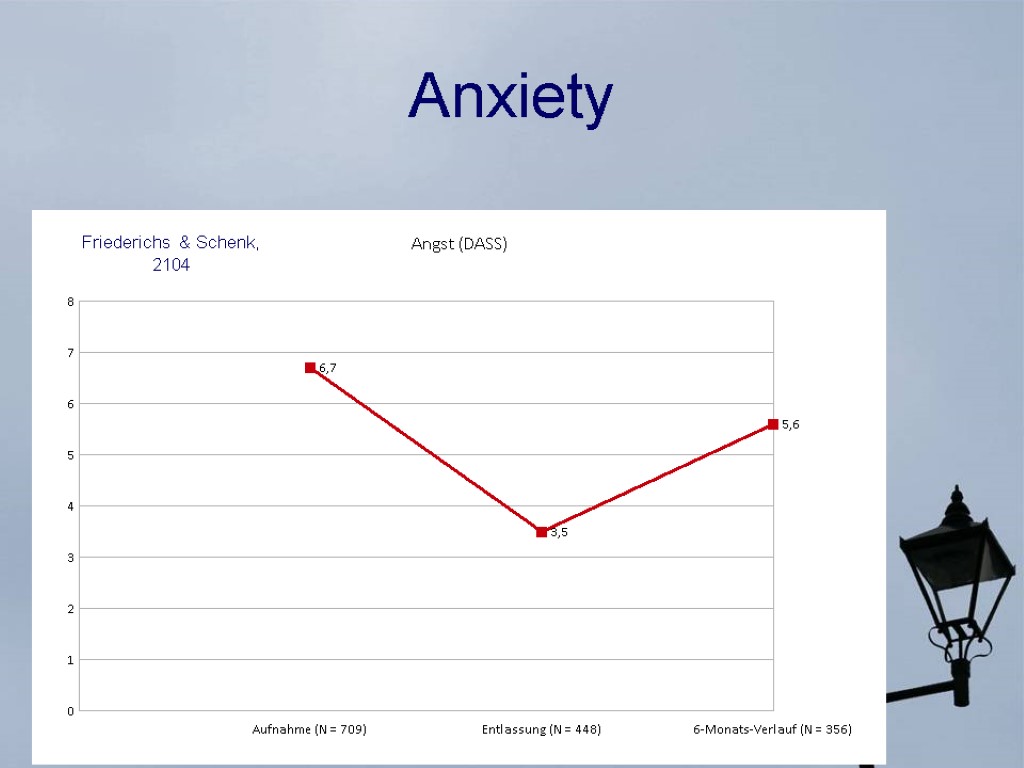 Anxiety Friederichs & Schenk, 2104
Anxiety Friederichs & Schenk, 2104
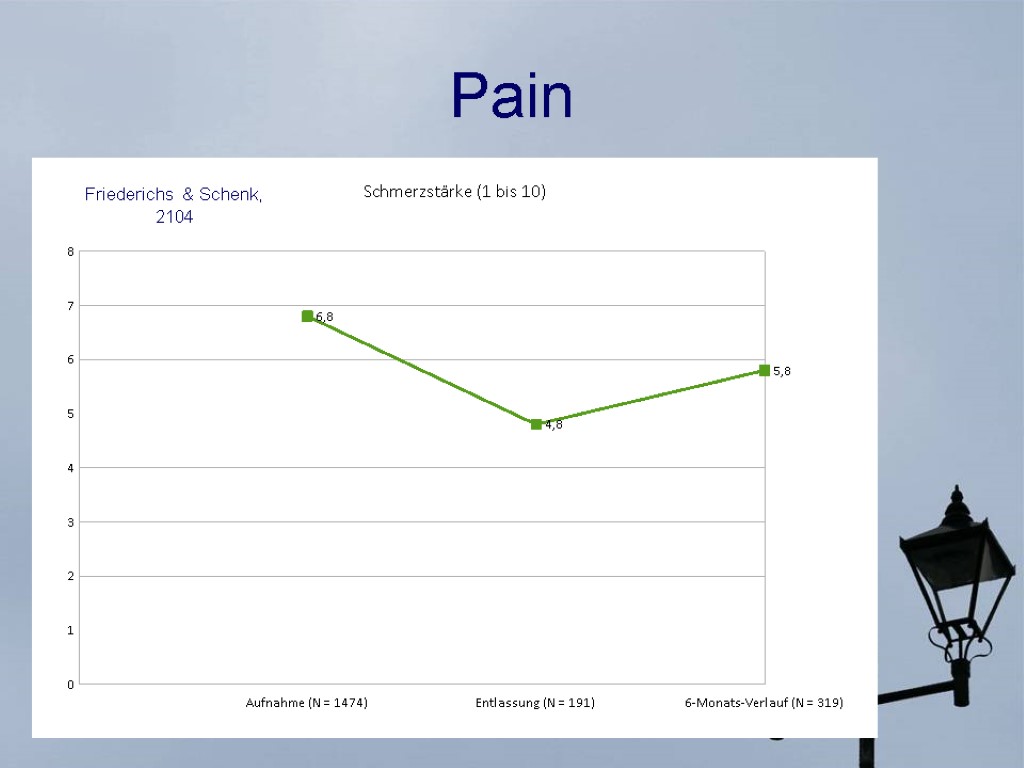 Pain Friederichs & Schenk, 2104
Pain Friederichs & Schenk, 2104
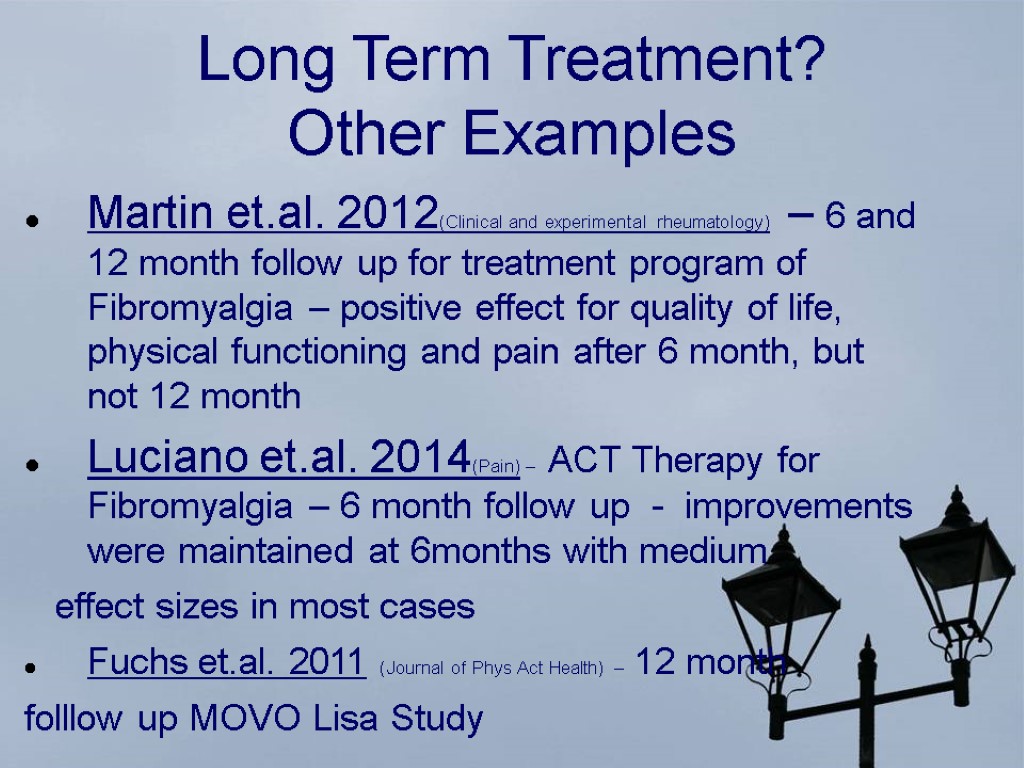
 Long Term Treatment? Other Examples Martin et.al. 2012(Clinical and experimental rheumatology) – 6 and 12 month follow up for treatment program of Fibromyalgia – positive effect for quality of life, physical functioning and pain after 6 month, but not 12 month Luciano et.al. 2014(Pain) – ACT Therapy for Fibromyalgia – 6 month follow up - improvements were maintained at 6months with medium effect sizes in most cases Fuchs et.al. 2011 (Journal of Phys Act Health) – 12 month folllow up MOVO Lisa Study
Long Term Treatment? Other Examples Martin et.al. 2012(Clinical and experimental rheumatology) – 6 and 12 month follow up for treatment program of Fibromyalgia – positive effect for quality of life, physical functioning and pain after 6 month, but not 12 month Luciano et.al. 2014(Pain) – ACT Therapy for Fibromyalgia – 6 month follow up - improvements were maintained at 6months with medium effect sizes in most cases Fuchs et.al. 2011 (Journal of Phys Act Health) – 12 month folllow up MOVO Lisa Study
 What kind of long term help? MOVO Lisa Concept (Goehner & Fuchs) – telephone based instruction Meta analysis (Cuijpers et.al. 2010) - of randomized controlled trials in which the effects of guided self-help on depression and anxiety were compared directly with face-to-face psychotherapies - guided self-help and face-to-face treatments can have comparable effects Cochrane Review 2014 - insufficient evidence to make conclusions regarding the efficacy of psychological therapies delivered via the Internet in participants with headache conditions
What kind of long term help? MOVO Lisa Concept (Goehner & Fuchs) – telephone based instruction Meta analysis (Cuijpers et.al. 2010) - of randomized controlled trials in which the effects of guided self-help on depression and anxiety were compared directly with face-to-face psychotherapies - guided self-help and face-to-face treatments can have comparable effects Cochrane Review 2014 - insufficient evidence to make conclusions regarding the efficacy of psychological therapies delivered via the Internet in participants with headache conditions
 Summary Most high-quality guidelines recommend education, staying active/exercise Psychological interventions for chronic pain and its consequences have been shown to improve mood, disability, pain, and catastrophic thinking CBT and ACT are effective in altering mood and catastrophising outcomes
Summary Most high-quality guidelines recommend education, staying active/exercise Psychological interventions for chronic pain and its consequences have been shown to improve mood, disability, pain, and catastrophic thinking CBT and ACT are effective in altering mood and catastrophising outcomes

