MMY MYOFASCIAL RELEASE, PRESENTED BY- DEBANJAN MONDAL(MPT) INTRODUCTION:


MMY MYOFASCIAL RELEASE, PRESENTED BY- DEBANJAN MONDAL(MPT)
INTRODUCTION: Myofascial release refers to the manual technique for stretching the fascia and releasing bonds between fascia and Lintegument, musles,and bones, with the goal of eliminating pain, increasing range of motion and balancing the body.
HISTORY: The first description of the myofacial pain syndrome was published in the German literature in 1843 As early as 1843,Froriep labeled the condition involving tender bands or cords within muscles as “Rheumatism” and he considered these tender palpable bands to be deposits of connective tissues.
Shortly thereafter,(1890) Grauhan histologically described these bands as fibrous tissues that surrounds muscles fibers and that is infiltrated with lymphocytes. Steindler and luck term these “Trigger Zones” and considered the sites to be within the ligaments or a muscle. Since 1942,Travell conducted many studies on trigger points.
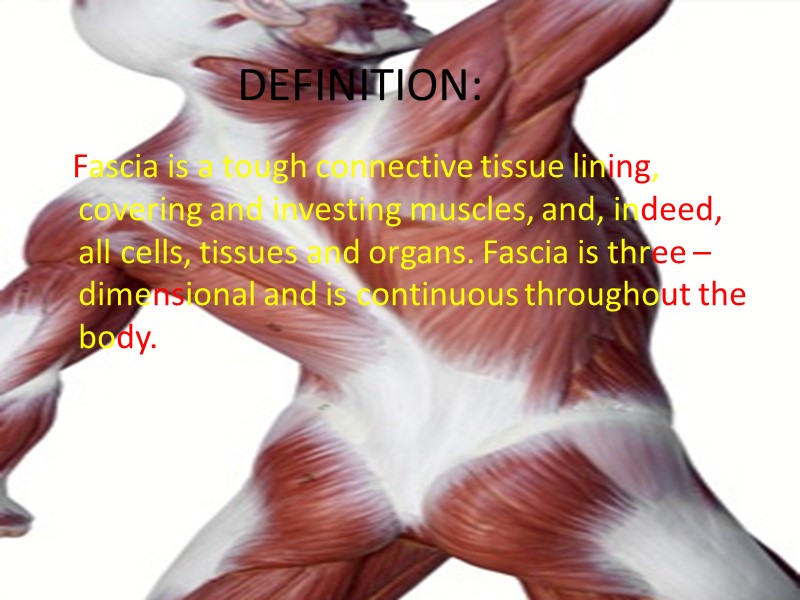
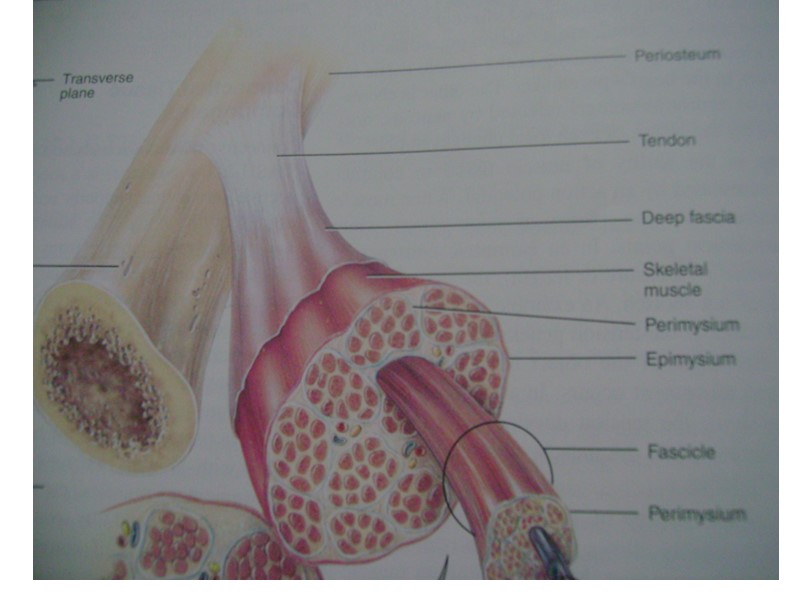
DEFINITION: Fascia is a tough connective tissue lining, covering and investing muscles, and, indeed, all cells, tissues and organs. Fascia is three – dimensional and is continuous throughout the body.

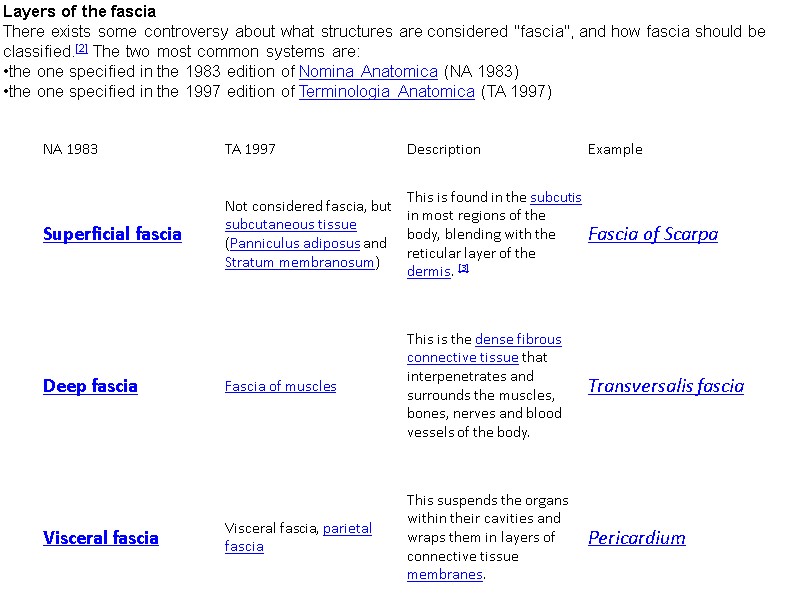
Layers of the fascia There exists some controversy about what structures are considered "fascia", and how fascia should be classified.[2] The two most common systems are: the one specified in the 1983 edition of Nomina Anatomica (NA 1983) the one specified in the 1997 edition of Terminologia Anatomica (TA 1997)
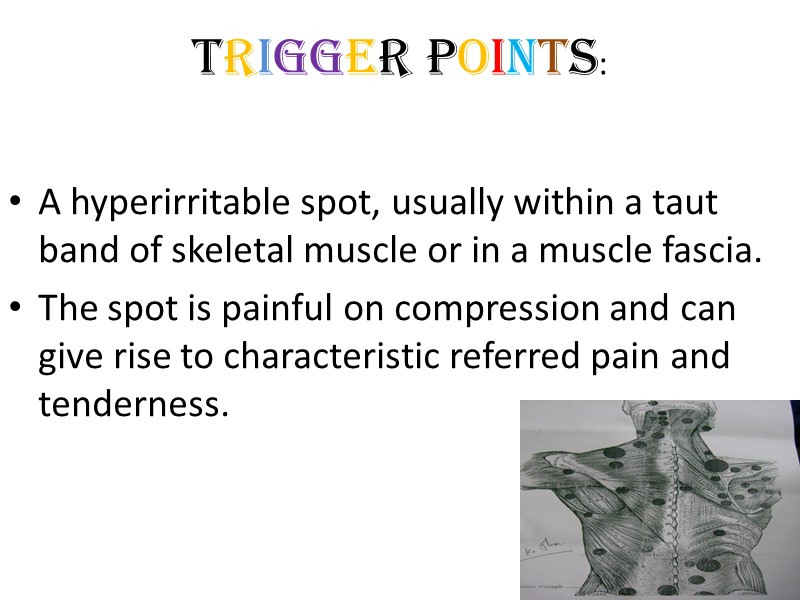
TRIGGER POINTS: A hyperirritable spot, usually within a taut band of skeletal muscle or in a muscle fascia. The spot is painful on compression and can give rise to characteristic referred pain and tenderness.
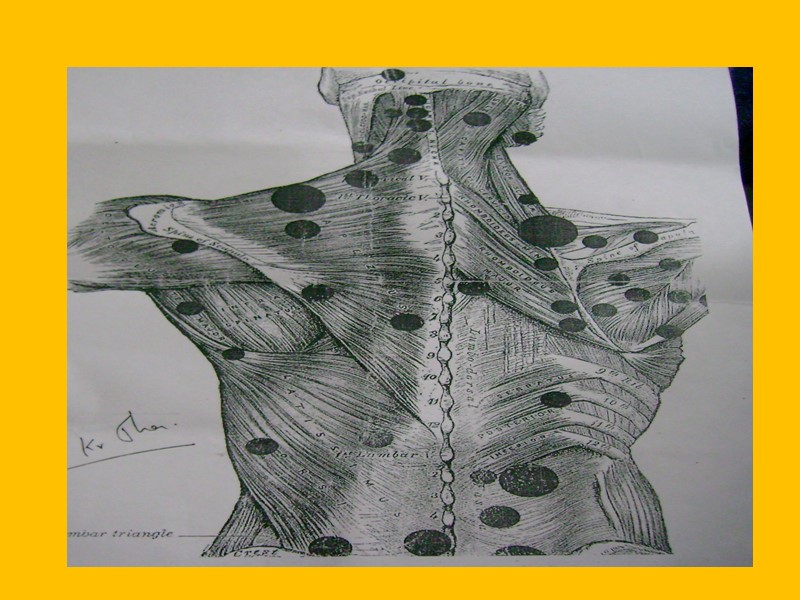
Note: Each muscle has its own characteristic pattern of referral. Often this can produce another trigger point to become active in another muscle within the zone of radiation of the original trigger. These are called “SATELLITE” trigger points.
PERPATUATING FACTORS: Mechanical: Structural inadequacies e.g The short leg syndrome, the long second metatarsal, short upper arms. Clothes: The constrictive clothing can produce myofacial trigger points due to sustained muscle compression (jeans related buttock pain, wallet sciatica)
Systemic: Metabolic endocrine, toxic, inflammatory etc. commonly found systemic factors include hypothyroidism, folic acid and iron deficiency. Metabolic inflammatory: gout Relative Growth Hormone deficiency-As growth hormone is necessary for muscle repair and its secretion is related to deep sleep which is frequently disturbed in patient with pain.
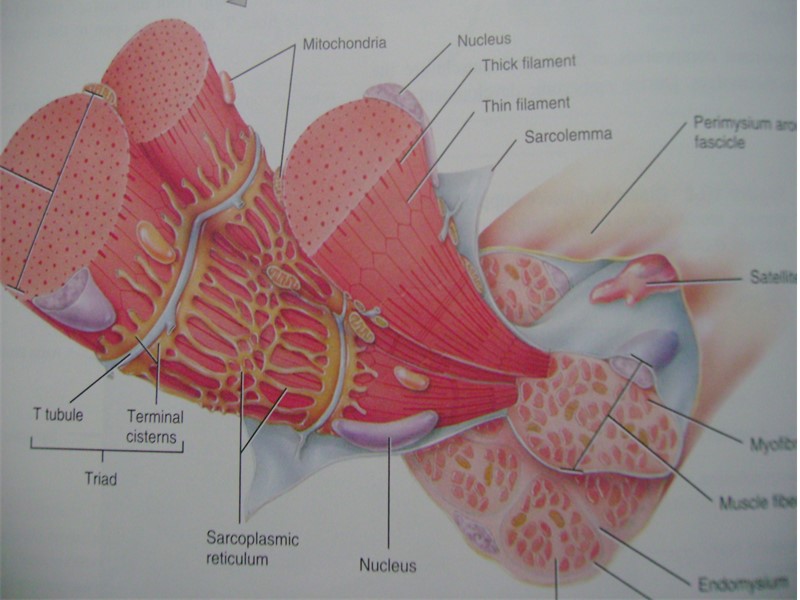
Simons,Travell and Simon’s(1999)model of central trigger points PATHOLOGY: Central trigger points forms almost directly in the centre of the muscle’s fibers, close to the motor endplate (neuromuscular junction) This formation is probably due to dysfunction endplate activity.
A metabolic crises occurs and acetylcholine (Ach )is released at synapse, usually associated with overuse or strain, leading to release of calcium. The resulting ischemia in the area creates an oxygen/nutrient deficit and a local energy crisis. Without available adenosine triphosphate (ATP), the calcium ions, which are keeping the gates open for Ach to keep flowing, cannot be removed.
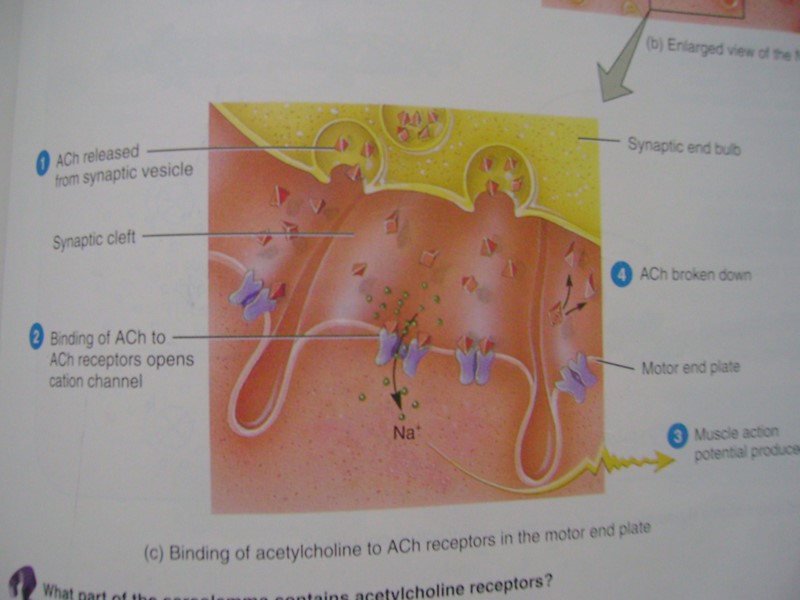
A chemically sustained contracture occurs. This is involuntary without motor potentials, and should be distinguished from a contraction, which is voluntary and involves motor potentials, and spasm, which is involuntary with motor potentials. As the endplate keeps producing this Ach flow, the Actin/myosin filaments shorten and bunch in the immediate area of the motor end plate (centre of fiber)
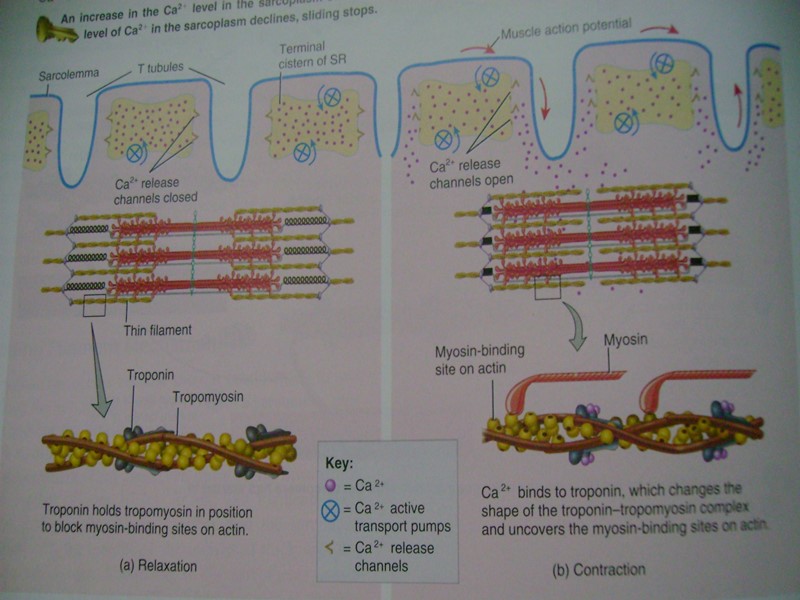
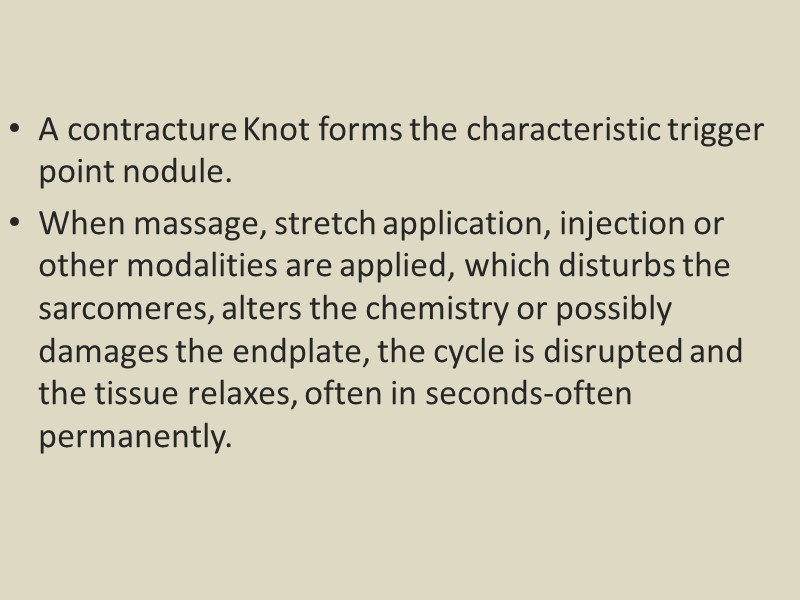
A contracture Knot forms the characteristic trigger point nodule. When massage, stretch application, injection or other modalities are applied, which disturbs the sarcomeres, alters the chemistry or possibly damages the endplate, the cycle is disrupted and the tissue relaxes, often in seconds-often permanently.
CLINICAL FEATURES: Spot Tenderness: A very tender small spot, which is found in a taut band. A taut band: A ropelike swelling found within the muscle probably due to sustained shortening of muscle fibers. Jump sign: Pressure on the tender spot causes the patient to physically react to the precipitated pain by exclaiming or moving.
Pain recognition: Digital pressure on the tender spot induces/reproduces some of the patient’s pain complaint and is recognized by the patient as being some or all of his or her pain. Twitch Response: A transient contraction of the muscle fibers of the taut band containing the trigger point. The twitch response can be elicited by “snapping” palpation of the trigger points.
Elicited referred pain: An active MTrP refers pain in a pattern characteristic of that muscle. Usually to a site distant to the MTrp. Restricted Range of Movement: Full stretching of the affected muscle is often involuntarily restricted by pain. Muscle Weakness: The patient is unable to demonstrate normal muscle strength on static testing of the affected side as compared to the contra-lateral non affected side.
ASSESSMENT & MEASUREMENT: The effective treatment of Myfacial Pain begins with defining the Tissues and or Reflex that is maintaining the pain state. 1.Find the ‘Active Trigger Point’ 2.Assess sympathetic involvement
Trigger points Before being able to effectively treat (and evaluate that treatment’s efficacy) Trigger point must be first- 1.Identified 2.quantified
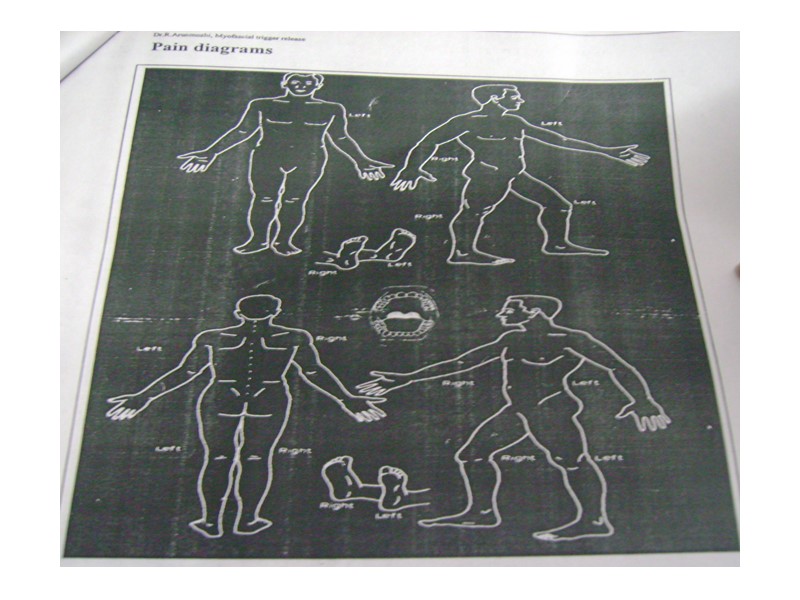
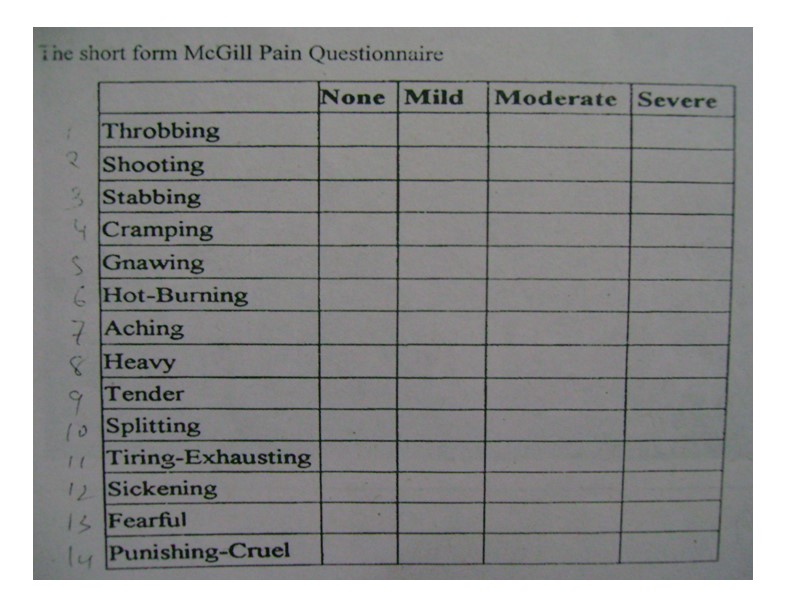
Pain assessment: Patient complaining of chronic pain deserves to be examined. Palpation and the utilization of pain assessment tools including: Pain diagram The McGill Pain Questionnaire, Visual Analogue Pain Scale.
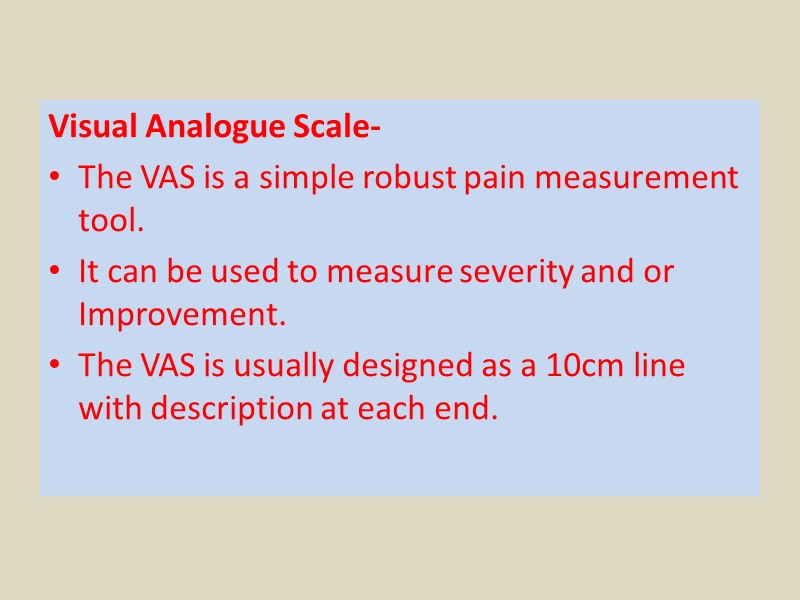
Visual Analogue Scale- The VAS is a simple robust pain measurement tool. It can be used to measure severity and or Improvement. The VAS is usually designed as a 10cm line with description at each end.
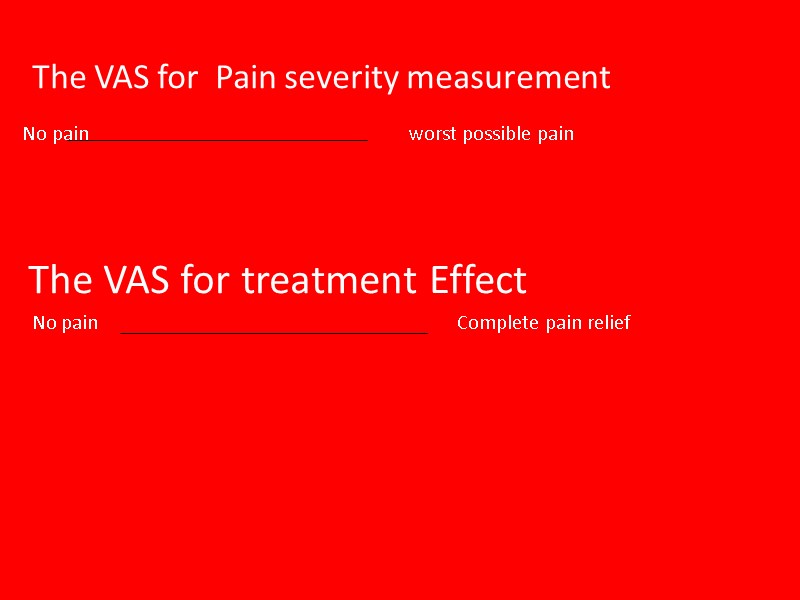
The VAS for Pain severity measurement No pain worst possible pain The VAS for treatment Effect No pain Complete pain relief
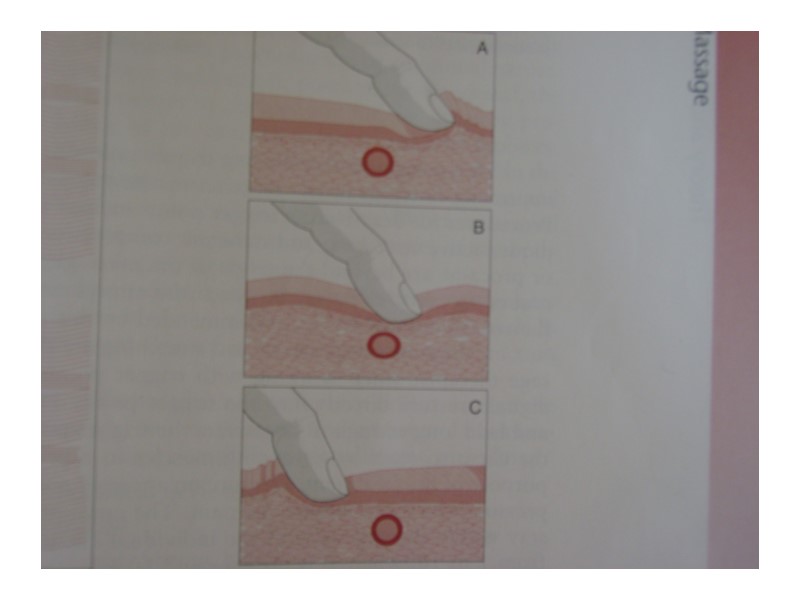
FINDING TRIGGER POINTS: Pincer palpation-Only some muscles can be lifted from surrounding tissue between the thumb and forefinger and in this manner the trigger point can be located, e.g, the upper trapezius (neck) or gastrocnemius muscle (calf).

2.Flat palpation:Simply moving the fingertips Transversely across the muscles fibres with some pressure until a “taut band” is located.
INDICATIONS: 1.The patients has a complex, global, or specific pain complaint that does not follow dermatomes, myotomes, or visceral referral patterns. 2.The patient’s has an chronic condition that causes tightness and restriction in the soft tissue (e.g fibromyalgia and post polio syndrome).
The patient has painful complex postural asymmetry. 4. The patient has impaired respiration and an inflexible rib cage due to chronic respiratory disease,central nervous system injury,or faulty mechanical relationships of the skeletal structure and the soft tissue.
5.The patient has asymmetrical muscle weakness due to an acute or chronic peripheral or central neuropathy. 6.The patient has frequent, intense headaches that are triggered by a variety of stimuli including myofascial trigger points, tension in the posterior cervical musculature, tempomandibular joints dysfunction, and asymmetrical muscle tightness.
7.The patient has impaired mouth closure, swallowing and phonation resulting in tightness and restriction of the hyoids and muscles of the mastication. 8.The patient has dizziness secondary to active myofascial trigger points. 9.The patient is a competitive athlete or performer who needs subtle stretching to increase speed or accuracy and to prevent injury at the extreme range of motion.
CONTRAINDICATIONS: Myofascial Release should not be used in thefollowing ways- The patient does not tolerate close physical contact or touch. The patient has an unstable medical condition e.g unstable angina The patient has a dermatitis.
The patient contagious or infectious disease that is transmitted by the upper respiratory tract or by direct contact with the skin. The patient does not trust the therapist. The patient is under the influence of drugs or alcohol. The patient is unable to give informed consent to treatment due to his mental status.
PRECAUTIONS: Myofascial release consistently lowers blood pressure. All patient must rest in horizontal position for 15-20min following treatment. The patient should get up slowly and not get off the treatment table until any dizziness has resolved.
Myofascial release may lower blood sugar level, particularly when deep trigger point releases are performed. Individual who are diabetic should check their blood glucose level prior to treatment. Individual who are prone to hypoglycemia should have a snack prior to treatment. Individual with healing fractures or wounds may receive Myofascial Release to uninvolved areas.
Individuals with compromised circulation may be treated with Myofascial Release to uninvolved areas. The patient is taking medication that increases blood clotting times and causes the patient to bruise easily.

TECHNIQUES: CONTENTS- 1.Direct myofascial release 2.Indirect myofascial release 3.Self myofascial release

Direct Myofascial Release-
Direct myofascial release- The direct myofascial release method works directly on the restricted fascia. The practitioners use Knuckles, elbows,or other tools to slowly sink into the restricted fascia applying a few kilograms-force or tens of newtons and then stretch the fascia. This is sometimes referred to as deep tissue work.
Direct Myofascial Release seeks for changes in the myofascial structures by stretching, elongation of fascia, or mobilizing adhesive tissues.
Michae!Stanborough has summarised his style of Direct Myofascial Release technique as: Land on the surface of the body with the appropriate ‘tool’(Knuckles,or forearm etc). Sink into the soft tissue. Contact the first barrier/restricted layer. Put in a ‘line of tension’. Engage the fascia by taking up the slack in the tissue. Finally,move or drag the fascia across the surface while staying in touch with the underlying layers. Exit gracefully.

Michael Stan borough applied direct myofascial release on plantar fascia-

Direct myofascial release on the thigh by Michael Stanborough-

HEAD $ FACE I NTRA -ORAL

Direct Release Myofascial Technique - The Trunk

Direct Release Myofascial Technique - The Cervical Region CERVICAL REGION

T H I G H Direct Release Myofascial Technique - Thigh

The Feet
Indirect Myofascial Release- The indirect gentle stretch, the pressure is in few grams, the hands tend to go with the restricted fascia, hold the stretch, and allow the fascia to ‘unwind’ itself. The gentle traction applied to the restricted fascia will result in heat, increase blood flow in the area. The intention is to allow the body’s inherent ability for self correction returns, thus eliminating pain and restoring the optimum performance of the body.
The indirect myofascial release,e.g. cross hand technique according to John Barnes is as follows: With relaxed hand lightly contact the fascia. Slowly stretch the fascia until reaching a barrier/restriction. Maintaining a light pressure to stretch the barrier and wait for approximately 3-5 minutes. Prior to release,the therapist will feel a therapeutic pulse(e.g. heat). As the barrier releases,the hand will feel the motion and softening of the tissue. The Key is sustained pressure over time.
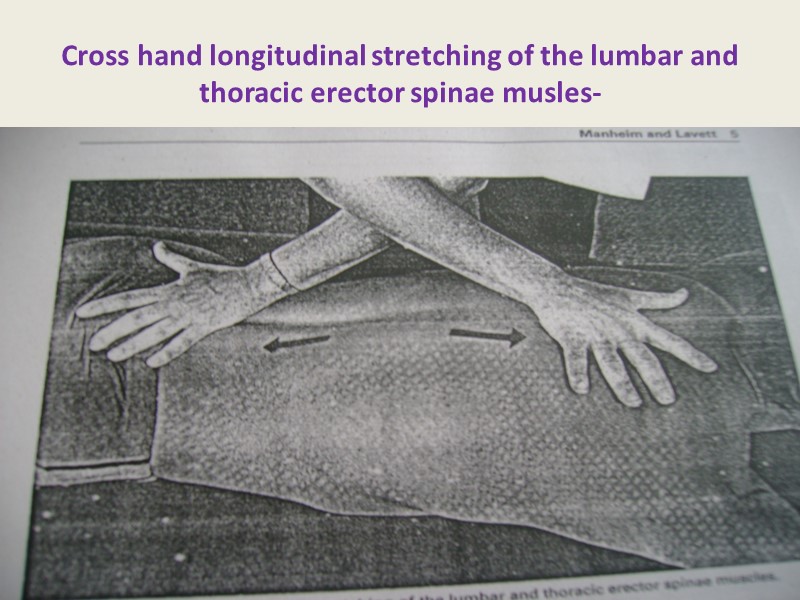
Cross hand longitudinal stretching of the lumbar and thoracic erector spinae musles-
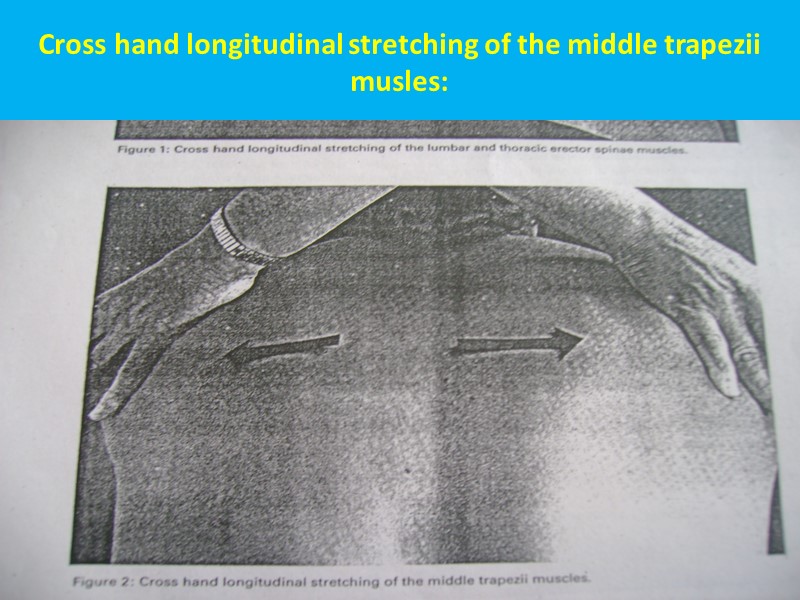
Cross hand longitudinal stretching of the middle trapezii musles:
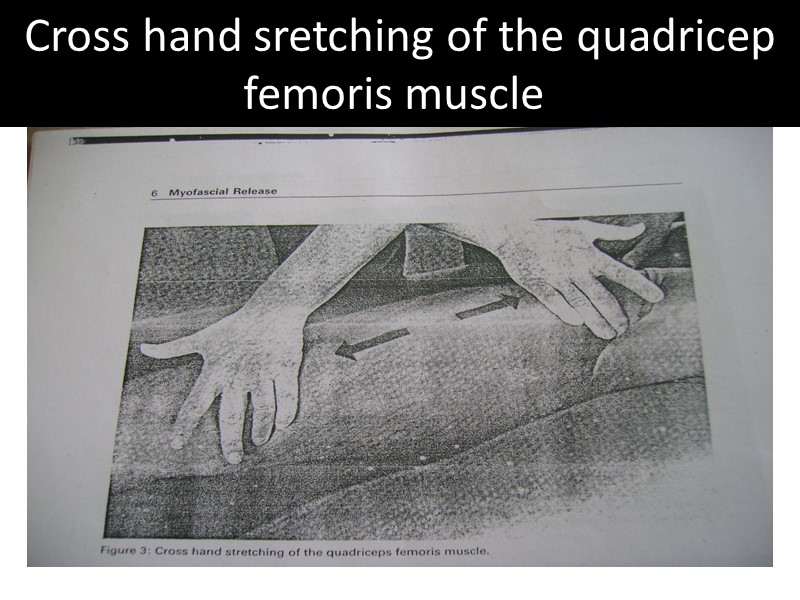
Cross hand sretching of the quadricep femoris muscle:
Self Myofascial Release- Self myofascial release(SMR) is when the individual uses a soft object to provide myofascial release under their own power. Usually an individual uses a soft roll, or ball on which to rest one’s body weight,then,by using gravity to induce pressure along the length of the specific muscle or muscle groups, rolls their body on the object, slowly allowing for the fascia to be massaged.
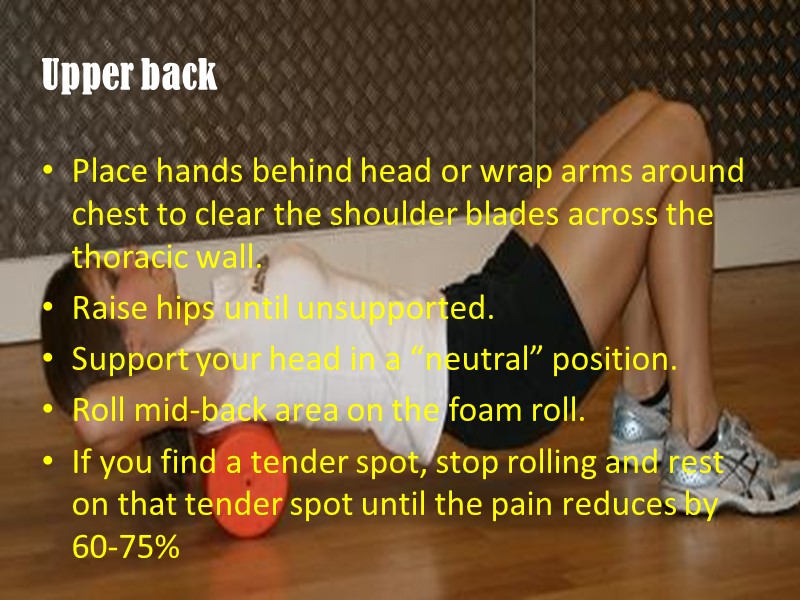
Upper back Place hands behind head or wrap arms around chest to clear the shoulder blades across the thoracic wall. Raise hips until unsupported. Support your head in a “neutral” position. Roll mid-back area on the foam roll. If you find a tender spot, stop rolling and rest on that tender spot until the pain reduces by 60-75%

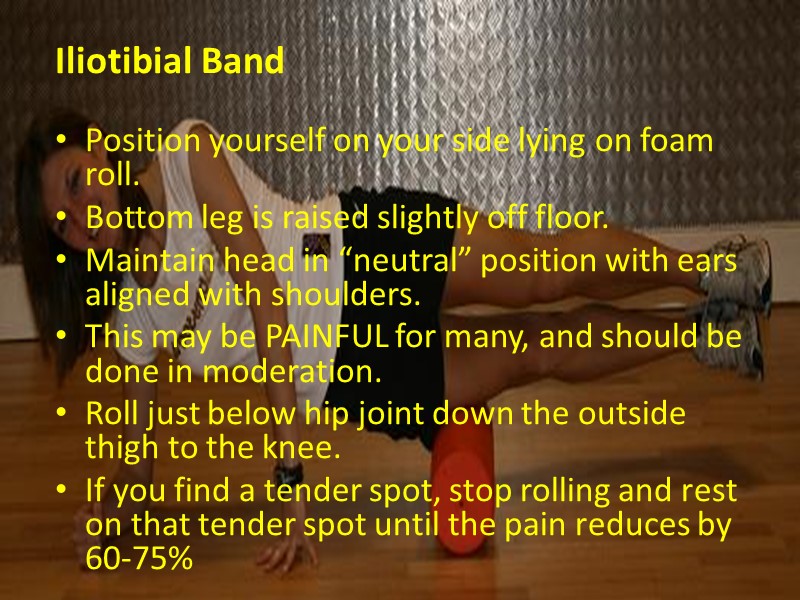
Iliotibial Band Position yourself on your side lying on foam roll. Bottom leg is raised slightly off floor. Maintain head in “neutral” position with ears aligned with shoulders. This may be PAINFUL for many, and should be done in moderation. Roll just below hip joint down the outside thigh to the knee. If you find a tender spot, stop rolling and rest on that tender spot until the pain reduces by 60-75%

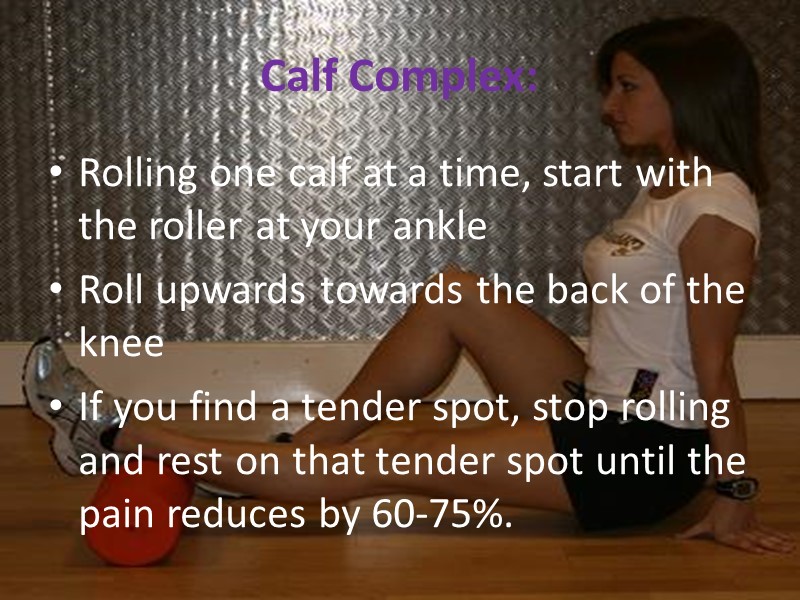
Calf Complex: Rolling one calf at a time, start with the roller at your ankle Roll upwards towards the back of the knee If you find a tender spot, stop rolling and rest on that tender spot until the pain reduces by 60-75%.

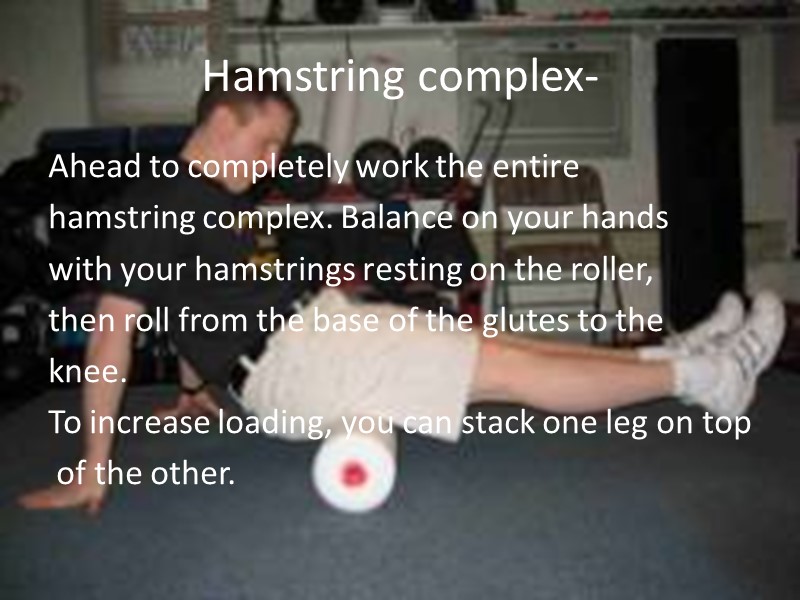
Hamstring complex- Ahead to completely work the entire hamstring complex. Balance on your hands with your hamstrings resting on the roller, then roll from the base of the glutes to the knee. To increase loading, you can stack one leg on top of the other.

HAMSTRINGS
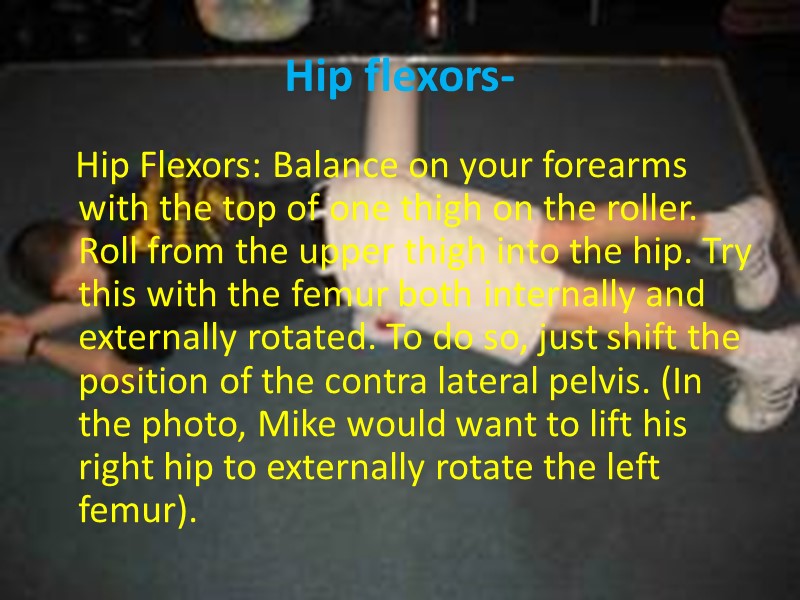
Hip flexors- Hip Flexors: Balance on your forearms with the top of one thigh on the roller. Roll from the upper thigh into the hip. Try this with the femur both internally and externally rotated. To do so, just shift the position of the contra lateral pelvis. (In the photo, Mike would want to lift his right hip to externally rotate the left femur).

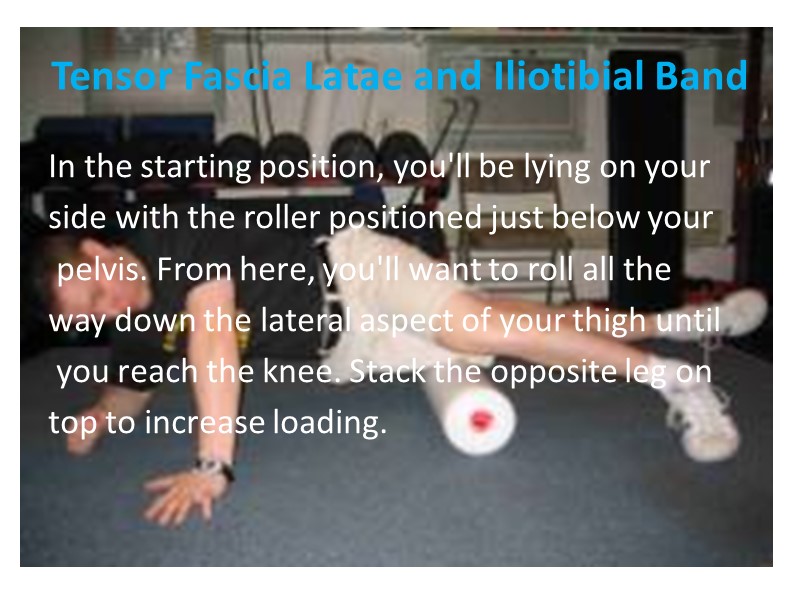
Tensor Fascia Latae and Iliotibial Band In the starting position, you'll be lying on your side with the roller positioned just below your pelvis. From here, you'll want to roll all the way down the lateral aspect of your thigh until you reach the knee. Stack the opposite leg on top to increase loading.

I.T BAND/TFL

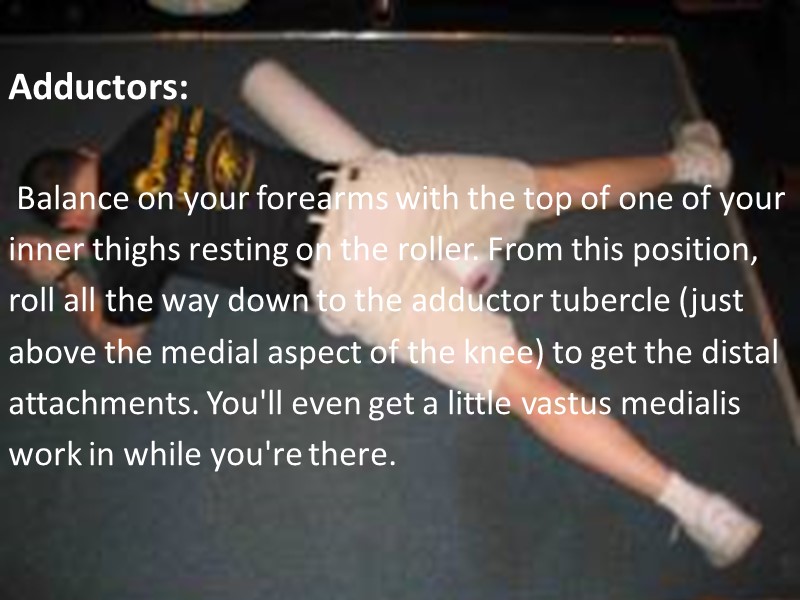
Adductors: Balance on your forearms with the top of one of your inner thighs resting on the roller. From this position, roll all the way down to the adductor tubercle (just above the medial aspect of the knee) to get the distal attachments. You'll even get a little vastus medialis work in while you're there.
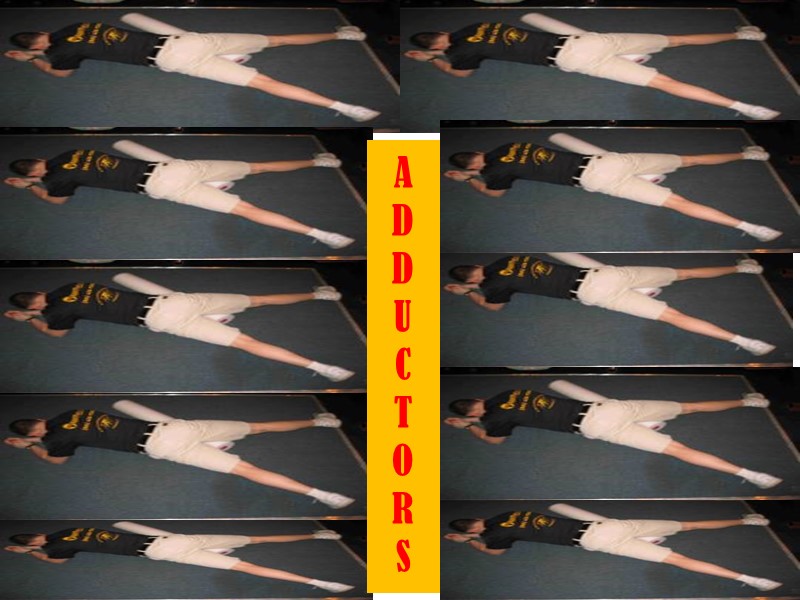
A D D U C T O R S
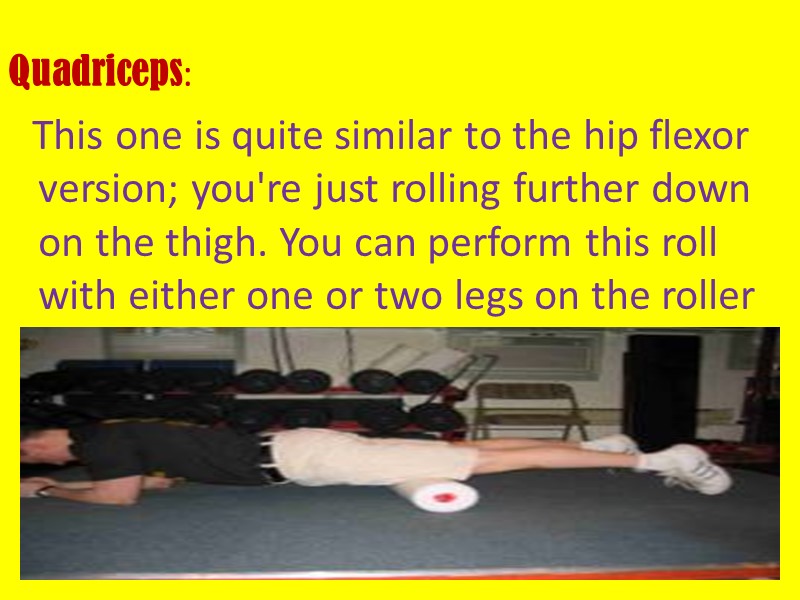
Quadriceps: This one is quite similar to the hip flexor version; you're just rolling further down on the thigh. You can perform this roll with either one or two legs on the roller

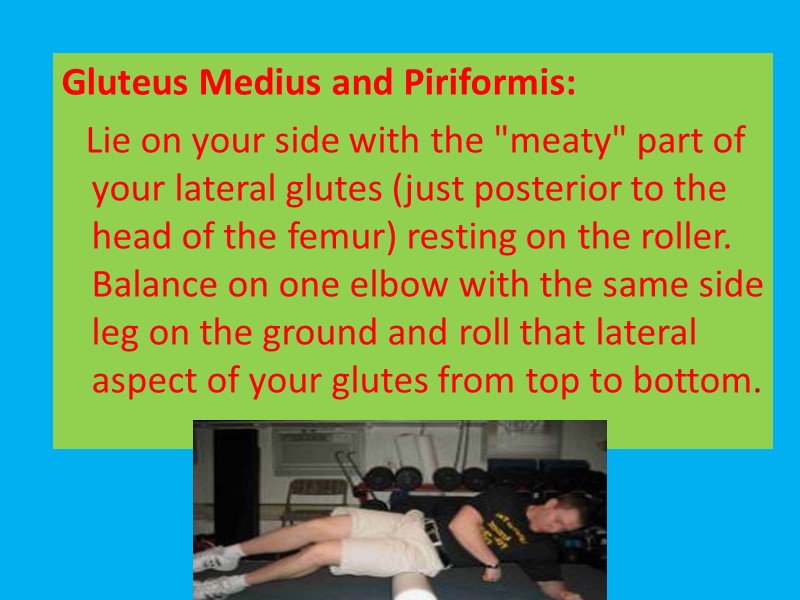
Gluteus Medius and Piriformis: Lie on your side with the "meaty" part of your lateral glutes (just posterior to the head of the femur) resting on the roller. Balance on one elbow with the same side leg on the ground and roll that lateral aspect of your glutes from top to bottom.

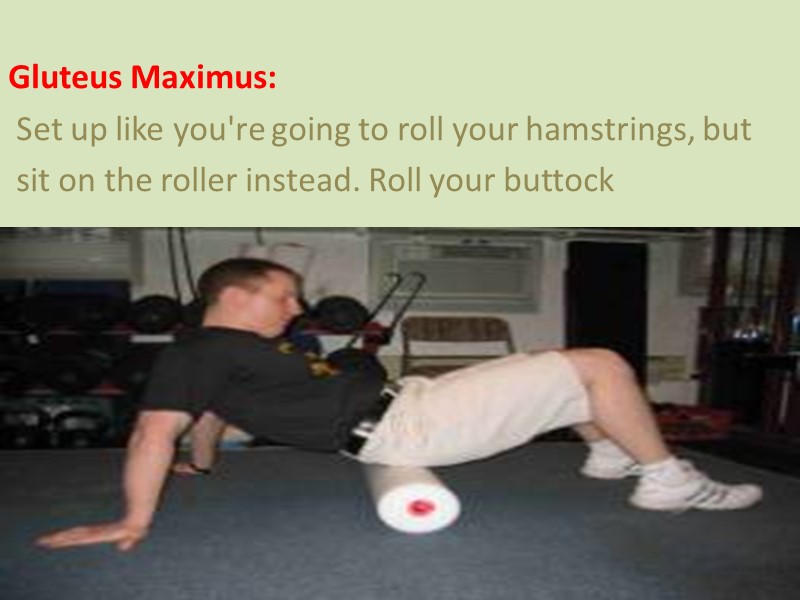
Gluteus Maximus: Set up like you're going to roll your hamstrings, but sit on the roller instead. Roll your buttock
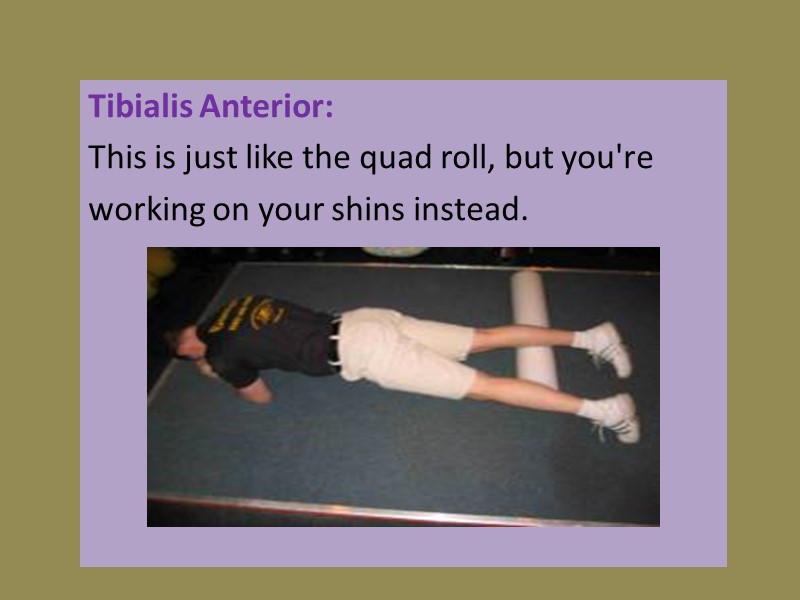
Tibialis Anterior: This is just like the quad roll, but you're working on your shins instead.
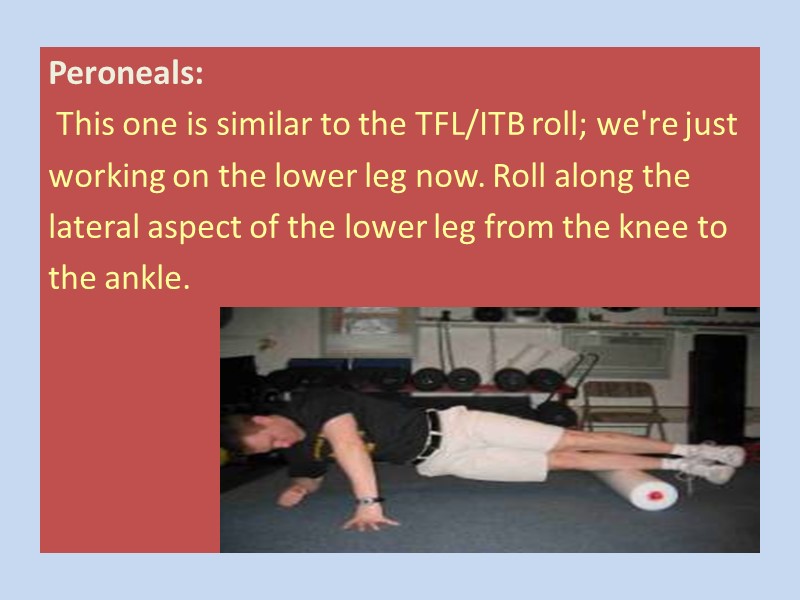
Peroneals: This one is similar to the TFL/ITB roll; we're just working on the lower leg now. Roll along the lateral aspect of the lower leg from the knee to the ankle.
Triceps: Start with your body in the same position as you would for the latissimus dorsi. Now, however, you'll want to place the roller at the top of your triceps (near your armpit) and your noggin on top of your arm to increase the tension ..

Pectoralis Major and Anterior Deltoid: Lie prone with the roller positioned at an angle slightly to one side of the sternum; the arm on this side should be abducted to about 135° (halfway between completely overhead and where it would be at the completion of a lateral raise). Roll toward the humeral head (toward the armpit).


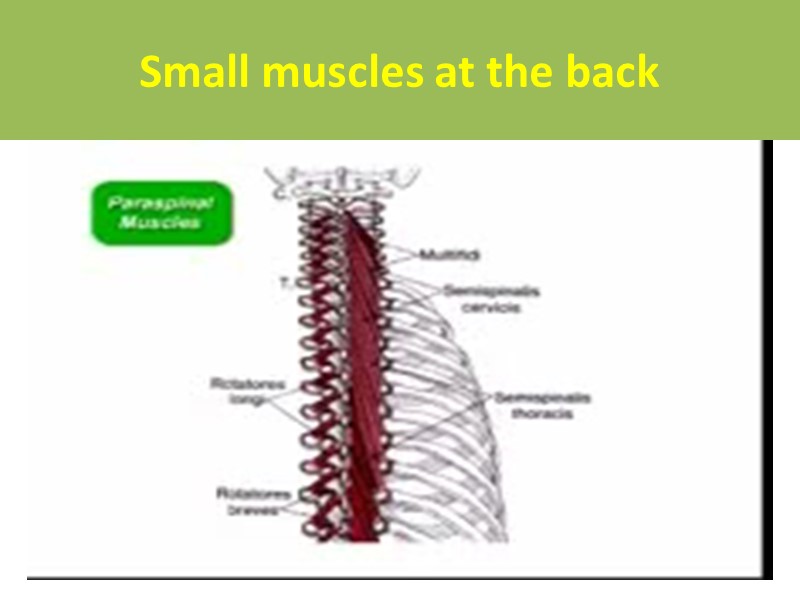
Small muscles at the back
Skin rolling /cross hand/limb pull
Myofascial release of carpal tunnel syndromme. Sucher BM. Current treatment for carpal tunnel syndrome may be ineffective or associated with complications or recurrence. In the case reported here, a myofascial release by the physician combined with the patient's self-stretch reduced pain and numbness and improved electromyographic results. The manipulative approach releases the transverse carpal ligament,-and "opens" or dilates the canal. The patient stretches the wrist, digits, and thumb, including myofascial components. An aggressive, conservative approach lessens the need for surgery in mild to moderate cases. Studies with magnetic resonance imaging may be helpful to document canal size before and after treatment. PMID: 8423131 [PubMed - indexed for MEDLINE]
Estimation of influence of myofascial release techniques on esophageal pressure in patients after total laryngectomy. Marszałek S, Zebryk-Stopa A, Kraśny J, Obrębowski A, Golusiński W. Department of Athletics, University School of Physical Education, Poznan, Poland, [email protected]. In patients after total laryngectomy, increased tension in myofascial neck and arm areas might be observed. Via fascial continuity it has an adverse impact on the superior esophageal constrictor forming the "mouth of the oesophagus", which hinders learning of esophageal speech. The aim is to assess the effect of manual myofascial release techniques on esophageal pressure in patients after total laryngectomy. Forty patients (12 F, 28 M), aged 43-75 (mean 56.8 years), 9 months to 13 years (average 3 years) after total laryngectomy, 35 patients (87.5%) after neck lymph node resection, 38 patients (95%) after radiotherapy. Esophageal pressure was assessed using modified Seeman's method. Manual myofascial release techniques were applied within head, neck, arms, upper trunk and upper limb areas. Wilcoxon and Shapiro-Wilk's test was used for the purpose of statistical analysis. Statistically significant decrease of the mean esophageal pressure was observed after the physiotherapy treatment. The average pressure among the examined patients decreased from 37.9 to 26.6 mmHg. The application of myofascial manual techniques decreases esophageal pressure, thus allowing patients to learn esophagus speech at a faster pace.
RECENT ADVANCES: Effectiveness of osteopathy in the cranial field and myofascial release versus acupuncture as complementary treatment for children with spastic cerebral palsy: a pilot study. Duncan B, McDonough-Means S, Worden K, Schnyer R, Andrews J, Meaney FJ. Department of Pediatrics at University of Arizona Health Sciences Center in Tucson, AZ, USA. [email protected]
OBJECTIVE: To assess the effectiveness of osteopathy in the cranial field, myofascial release, or both versus acupuncture in children with moderate to severe spastic cerebral palsy, as measured by several outcomes instruments in a randomized controlled trial. Children between the ages of 20 months and 12 years with moderate to severe spastic cerebral palsy were enrolled.. CONCLUSIONS: A series of treatments using osteopathy in the cranial field, myofascial release, or both improved motor function in children with moderate to severe spastic cerebral palsy. These results can be used to guide future research into the effectiveness of OMT or acupuncture in treating children with spastic cerebral palsy.
The Complementary Journal Alternative and Medicine The Effect of Deep-Tissue Massage Therapy on Blood Pressure and Heart Rate To cite this paper: Alan David Kaye, Aaron J. Kaye, Jan Swinford, Amir Baluch, Brad A. Bawcom, Thomas J. Lambert, Jason M. Hoover. The Journal of Alternative and Complementary Medicine. March 1, 2008, 14(2): 125-128. doi:10.1089/acm.2007.0665. of
ABSTRACT Aim: In the present study, we describe the effects of deep tissue massage on systolic, diastolic, and mean arterial blood pressure. Materials and methods: The study involved 263 volunteers (12% males and 88% females), with an average age of 48.5. Overall muscle spasm/muscle strain was described as either moderate or severe for each patient. Baseline blood pressure and heart rate were measured via an automatic blood pressure cuff. Twenty-one (21) different soothing CDs played in the background as the deep tissue massage was performed over the course of the study. The massages were between 45 and 60 minutes in duration. The data were analyzed using analysis of variance with post-hoc Scheffe's F-test. Results: Results of the present study demonstrated an average systolic pressure reduction of 10.4 mm Hg (p < 0.06), a diastolic pressure reduction of 5.3 mm Hg (p < 0.04), a mean arterial pressure reduction of 7.0 mm Hg (p < 0.47), and an average heart rate reduction of 10.8 beats per minute (p < 0.0003), respectively.
The effects of back massage before diagnostic cardiac catheterization. McNamara ME, Burnham DC, Smith C, Carroll DL. Massachusetts General Hospital, Boston, USA. OBJECTIVE: The purpose of this study was to measure the effects of a 20-minute back massage on the physiological and psychological human responses of patients admitted for a diagnostic cardiac catheterization. PARTICIPANTS: Forty-six subjects admitted from home for a diagnostic cardiac catheterization. MAIN OUTCOME MEASURES: Heart rate, heart rate variability, blood pressure, respiration, peripheral skin temperature, pain perception, and psychological state. INTERVENTION: A 20-minute back massage. CONCLUSIONS: A 20-minute back massage appeared to reduce systolic blood pressure in patients awaiting a diagnostic cardiac catheterization, while preparatory time in the cardiac catheterization laboratory appeared to reduce diastolic blood pressure, respiration, perceived psychological distress, and pain.
Sexual dysfunction in men with chronic prostatitis/chronic pelvic pain syndrome: improvement after trigger point release and paradoxical relaxation training. Anderson RU, Wise D, Sawyer T, Chan CA. Department of Urology, Stanford University School of Medicine, Stanford, California, USA. PURPOSE: The impact of chronic pelvic pain syndrome on sexual function in men is underestimated. We quantified sexual dysfunction (ejaculatory pain, decreased libido, erectile dysfunction and ejaculatory difficulties) in men with chronic pelvic pain syndrome and assessed the effects of pelvic muscle trigger point release concomitant with paradoxical relaxation training. CONCLUSIONS: Sexual dysfunction is common in men with refractory chronic pelvic pain syndrome but it is unexpected in the mid fifth decade of life. Application of the trigger point release/paradoxical relaxation training protocol was associated with significant improvement in pelvic pain, urinary symptoms, libido, ejaculatory pain, and erectile and ejaculatory dysfunction.
Effects of myofascial release after high-intensity exercise: a randomized clinical trial. Arroyo-Morales M, Olea N, Martinez M, Moreno-Lorenzo C, Díaz-Rodríguez L, Hidalgo-Lozano A. Physiotherapy Department, High Altitude Training Centre of Sierra Nevada, Higher Sports Council, Health Sciences School, University of Granada, Granada, Spain. [email protected] OBJECTIVE: The usefulness of massage as a recovery method after high-intensity exercise has yet to be established. We aimed to investigate the effects of whole-body massage on heart rate variability (HRV) and blood pressure (BP) after repeated high-intensity cycling exercise under controlled and standardized pretest conditions. METHODS: The study included 62 healthy active individuals. After baseline measurements, the subjects performed standardized warm-up exercises followed by three 30-second Wingate tests. After completing the exercise protocol, the subjects were randomly assigned to a massage (myofascial release) or placebo (sham treatment with disconnected ultrasound and magnetotherapy equipment) group for a 40-minute recovery period. Holter recording and BP measurements were taken after exercise protocol and after the intervention.
RESULTS: After the exercise protocol, both groups showed a significant decrease in normal-to-normal interval, HRV index, diastolic BP (P > .001), and low-frequency domain values (P = .006). After the recovery period, HRV index (P = .42) and high-frequency (HF) (P = .94) values were similar to baseline levels in the massage group, whereas the HRV index tended (P = .05) to be lower and the HF was significantly (P < .01) lower vs baseline values in the placebo group, which also showed a tendency (P = .06) for HF to be lower than after the exercise. Likewise, diastolic BP returned to baseline levels in the massage group (P = .45) but remained lower in the placebo group (P = .02). CONCLUSION: Myofascial release massage favors the recovery of HRV and diastolic BP after high-intensity exercise (3 Winga Effectiveness of a home of ischemic pressure followed by sustained stretch for treatment of myofascial trigger points.
Myofascial Effects: Massage works directly with the muscles (myo) and connective tissues (fascia), helping to facilitate greater mobility in the body. This is especially important for the diabetic because elevated blood sugars cause a thickening of connective tissue, which in turn affects mobility and elasticity of the myofascial system. This can be noted in general levels of stiffness in muscles, tendons and ligaments, as well as decreased range of motion in the joints. Stress hormones also contribute to chemical changes in the connective tissue, causing a stickiness between the layers of fascia. Massage therapy can significantly counter this effect. Range of motion, stretching and regular exercise are also important to help encourage flexibility and health of the myofascial system. Author Mary Kathleen Rose massages one of her many diabetic clients.

Myofascial Effects -- For the client with diabetes, you may likely find a thickening of their connective tissue caused by increased blood sugars. Massage will help to increase mobility and tissue elasticity that has been hindered by that thickening effect. Of course, a good exercise program -- with an efficient stretching regimen -- will also benefit your client.
Integration of myofascial trigger point release and paradoxical relaxation training treatment of chronic pelvic pain in men. Anderson RU, Wise D, Sawyer T, Chan C. Department of Urology, Stanford University School of Medicine, Stanford, California, USA. [email protected] PURPOSE: A perspective on the neurobehavioral component of the etiology of chronic prostatitis (CP) and chronic pelvic pain syndrome (CPPS) is emerging. We evaluated a new approach to the treatment of CP/CPPS with the Stanford developed protocol using myofascial trigger point assessment and release therapy (MFRT) in conjunction with paradoxical relaxation therapy (PRT). MATERIALS AND METHODS: A total of 138 men with CP/CPPS refractory to traditional therapy were treated for at least 1 month with the MFRT/PRT protocol by a team comprising a urologist, physiotherapist and psychologist. Symptoms were assessed with a pelvic pain symptom survey (PPSS) and National Institutes of Health-CP Symptom Index. Patient reported perceptions of overall effects of therapy were documented on a global response assessment questionnaire. RESULTS: Global response assessments of moderately improved or markedly improved, considered clinical successes, were reported by 72% of patients. More than half of patients treated with the MFRT/PRT protocol had a 25% or greater decrease in pain and urinary symptom scores, as assessed by the PPSS. In those at the 50% or greater improvement level median scores decreased 69% and 80% for pain and urinary symptoms, respectively. The 2 scores decreased significantly by a median of 8 points when the 25% or greater improvement was first observed, that is after a median of 5 therapy sessions. PPSS and National Institutes of Health-CP Symptom Index showed similar levels of improvement after MFRT/PRT protocol therapy. CONCLUSIONS: This case study analysis indicates that MFRT combined with PRT represents an effective therapeutic approach for the management of CP/CPPS, providing pain and urinary symptom relief superior to that of traditional therapy.
39376-myofacialrelease-150118075044-conversion-gate02.ppt
- Количество слайдов: 105

