c3143b5fe861631710ec08acdc0cb068.ppt
- Количество слайдов: 98
 Main clinical symptoms in lung diseases 08. 09. 2016.
Main clinical symptoms in lung diseases 08. 09. 2016.
 Case history • • • 28 years old male Excercise induced dyspnea for 2 years No connection with daytime, season, meal Dry cough in lying position No chest pain Nonsmoker • Physical exam: Stridor
Case history • • • 28 years old male Excercise induced dyspnea for 2 years No connection with daytime, season, meal Dry cough in lying position No chest pain Nonsmoker • Physical exam: Stridor
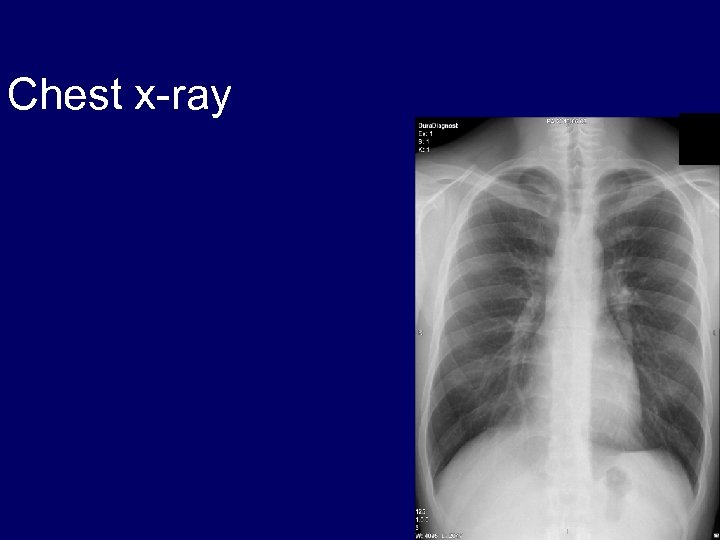 Chest x-ray
Chest x-ray
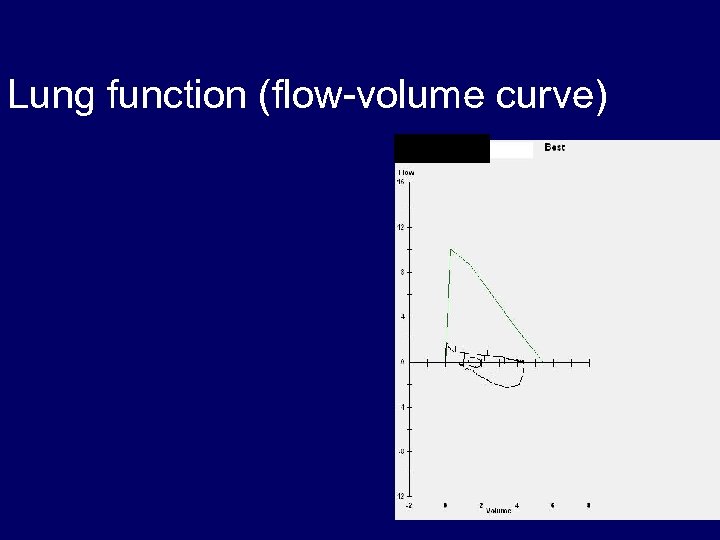 Lung function (flow-volume curve)
Lung function (flow-volume curve)
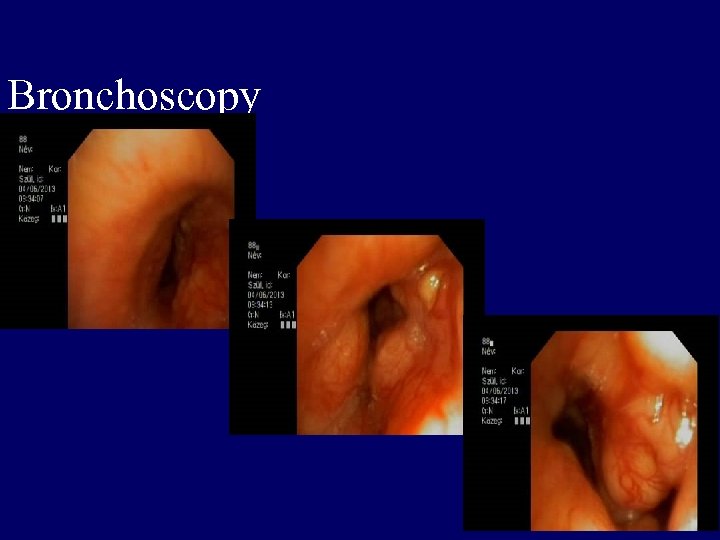 Bronchoscopy
Bronchoscopy
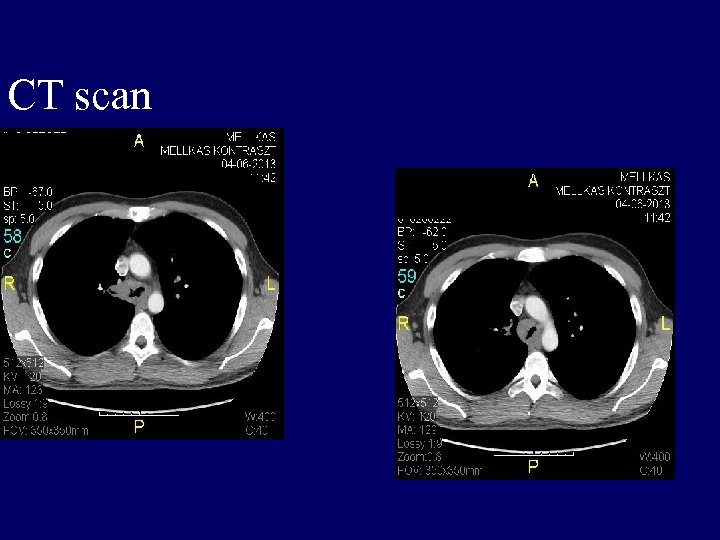 CT scan
CT scan
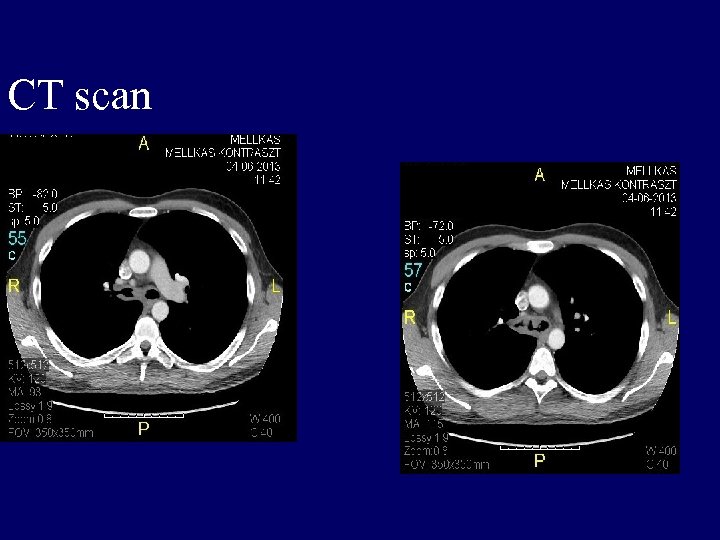 CT scan
CT scan
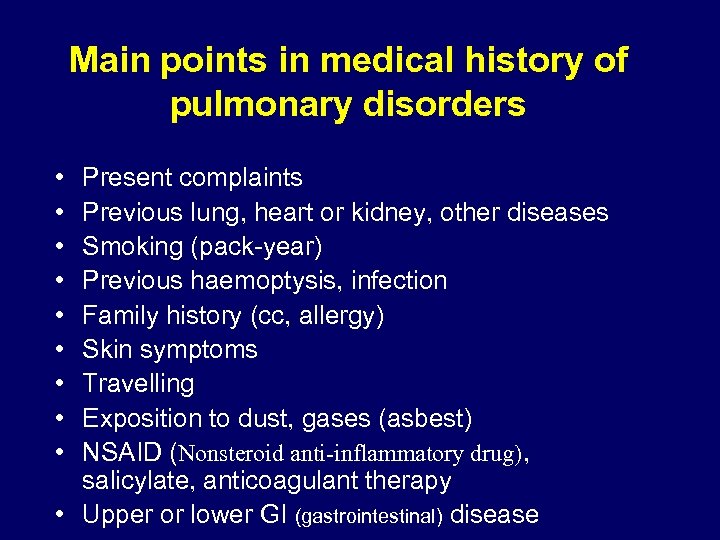 Main points in medical history of pulmonary disorders • • • Present complaints Previous lung, heart or kidney, other diseases Smoking (pack-year) Previous haemoptysis, infection Family history (cc, allergy) Skin symptoms Travelling Exposition to dust, gases (asbest) NSAID (Nonsteroid anti-inflammatory drug), salicylate, anticoagulant therapy • Upper or lower GI (gastrointestinal) disease
Main points in medical history of pulmonary disorders • • • Present complaints Previous lung, heart or kidney, other diseases Smoking (pack-year) Previous haemoptysis, infection Family history (cc, allergy) Skin symptoms Travelling Exposition to dust, gases (asbest) NSAID (Nonsteroid anti-inflammatory drug), salicylate, anticoagulant therapy • Upper or lower GI (gastrointestinal) disease
 Main clinical symptoms • • cough haemoptysis dyspnoe chest pain What to do? History Physical exam Testing -pulsoxymetry -ECG -Chest X-ray -lung function
Main clinical symptoms • • cough haemoptysis dyspnoe chest pain What to do? History Physical exam Testing -pulsoxymetry -ECG -Chest X-ray -lung function
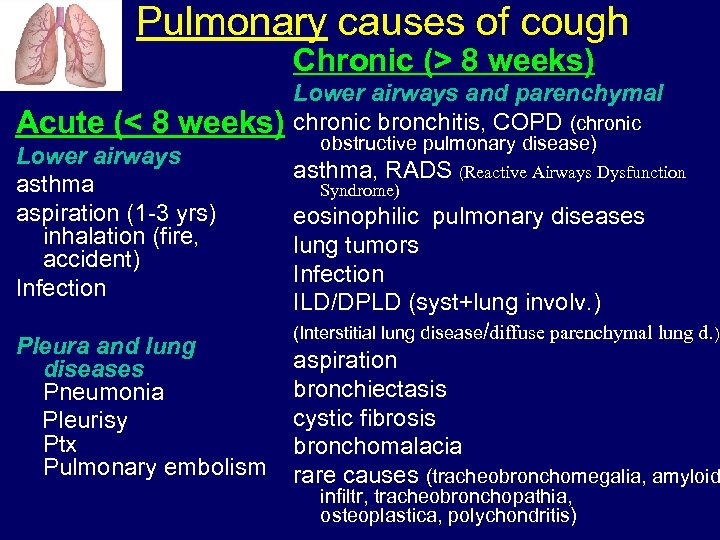 Pulmonary causes of cough Chronic (> 8 weeks) Acute (< 8 weeks) Lower airways asthma aspiration (1 -3 yrs) inhalation (fire, accident) Infection Pleura and lung diseases Pneumonia Pleurisy Ptx Pulmonary embolism Lower airways and parenchymal chronic bronchitis, COPD (chronic obstructive pulmonary disease) asthma, RADS (Reactive Airways Dysfunction Syndrome) eosinophilic pulmonary diseases lung tumors Infection ILD/DPLD (syst+lung involv. ) (Interstitial lung disease/diffuse parenchymal lung d. ) aspiration bronchiectasis cystic fibrosis bronchomalacia rare causes (tracheobronchomegalia, amyloid infiltr, tracheobronchopathia, osteoplastica, polychondritis)
Pulmonary causes of cough Chronic (> 8 weeks) Acute (< 8 weeks) Lower airways asthma aspiration (1 -3 yrs) inhalation (fire, accident) Infection Pleura and lung diseases Pneumonia Pleurisy Ptx Pulmonary embolism Lower airways and parenchymal chronic bronchitis, COPD (chronic obstructive pulmonary disease) asthma, RADS (Reactive Airways Dysfunction Syndrome) eosinophilic pulmonary diseases lung tumors Infection ILD/DPLD (syst+lung involv. ) (Interstitial lung disease/diffuse parenchymal lung d. ) aspiration bronchiectasis cystic fibrosis bronchomalacia rare causes (tracheobronchomegalia, amyloid infiltr, tracheobronchopathia, osteoplastica, polychondritis)
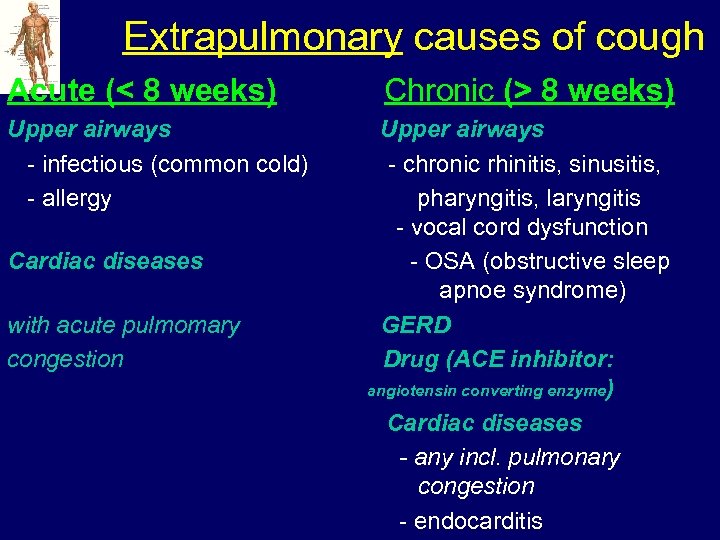 Extrapulmonary causes of cough Acute (< 8 weeks) Upper airways - infectious (common cold) - allergy Cardiac diseases with acute pulmomary congestion Chronic (> 8 weeks) Upper airways - chronic rhinitis, sinusitis, pharyngitis, laryngitis - vocal cord dysfunction - OSA (obstructive sleep apnoe syndrome) GERD Drug (ACE inhibitor: angiotensin converting enzyme) Cardiac diseases - any incl. pulmonary congestion - endocarditis
Extrapulmonary causes of cough Acute (< 8 weeks) Upper airways - infectious (common cold) - allergy Cardiac diseases with acute pulmomary congestion Chronic (> 8 weeks) Upper airways - chronic rhinitis, sinusitis, pharyngitis, laryngitis - vocal cord dysfunction - OSA (obstructive sleep apnoe syndrome) GERD Drug (ACE inhibitor: angiotensin converting enzyme) Cardiac diseases - any incl. pulmonary congestion - endocarditis
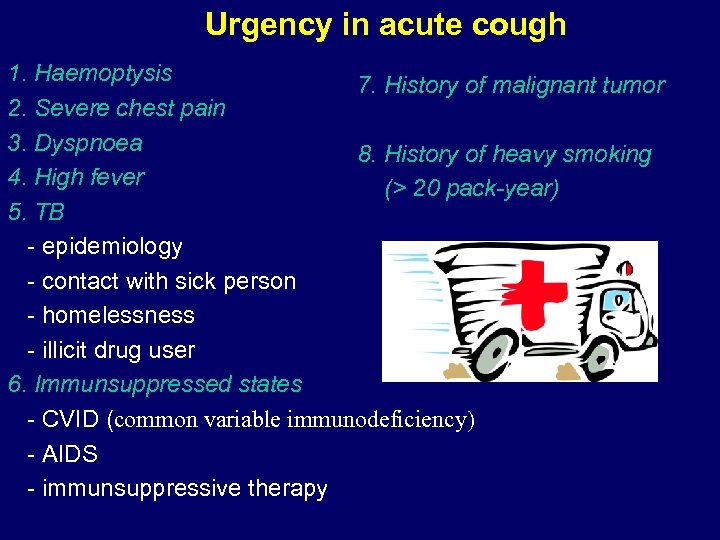 Urgency in acute cough 1. Haemoptysis 7. History of malignant tumor 2. Severe chest pain 3. Dyspnoea 8. History of heavy smoking 4. High fever (> 20 pack-year) 5. TB - epidemiology - contact with sick person - homelessness - illicit drug user 6. Immunsuppressed states - CVID (common variable immunodeficiency) - AIDS - immunsuppressive therapy
Urgency in acute cough 1. Haemoptysis 7. History of malignant tumor 2. Severe chest pain 3. Dyspnoea 8. History of heavy smoking 4. High fever (> 20 pack-year) 5. TB - epidemiology - contact with sick person - homelessness - illicit drug user 6. Immunsuppressed states - CVID (common variable immunodeficiency) - AIDS - immunsuppressive therapy
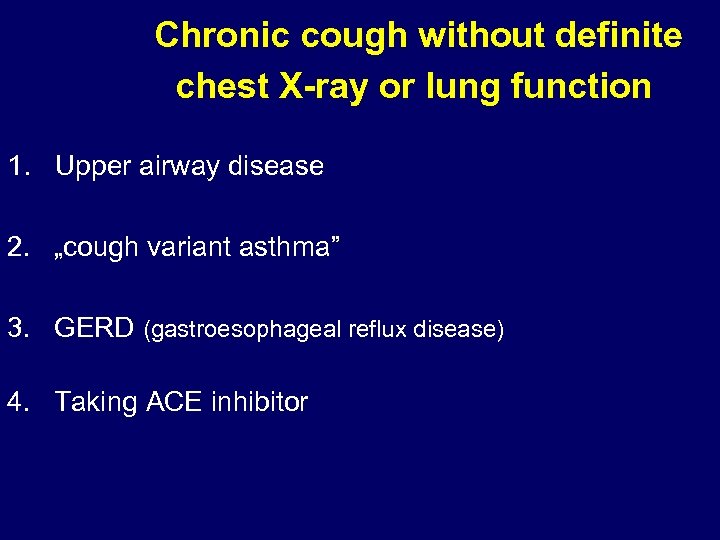 Chronic cough without definite chest X-ray or lung function 1. Upper airway disease 2. „cough variant asthma” 3. GERD (gastroesophageal reflux disease) 4. Taking ACE inhibitor
Chronic cough without definite chest X-ray or lung function 1. Upper airway disease 2. „cough variant asthma” 3. GERD (gastroesophageal reflux disease) 4. Taking ACE inhibitor
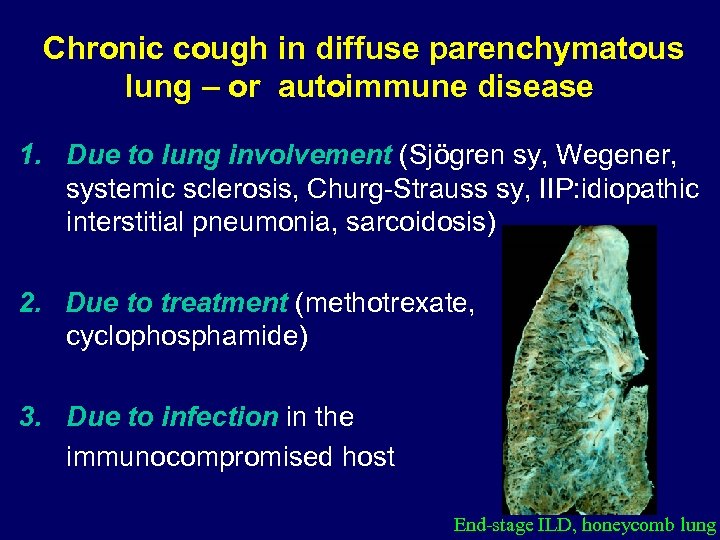 Chronic cough in diffuse parenchymatous lung – or autoimmune disease 1. Due to lung involvement (Sjögren sy, Wegener, systemic sclerosis, Churg-Strauss sy, IIP: idiopathic interstitial pneumonia, sarcoidosis) 2. Due to treatment (methotrexate, cyclophosphamide) 3. Due to infection in the immunocompromised host End-stage ILD, honeycomb lung
Chronic cough in diffuse parenchymatous lung – or autoimmune disease 1. Due to lung involvement (Sjögren sy, Wegener, systemic sclerosis, Churg-Strauss sy, IIP: idiopathic interstitial pneumonia, sarcoidosis) 2. Due to treatment (methotrexate, cyclophosphamide) 3. Due to infection in the immunocompromised host End-stage ILD, honeycomb lung
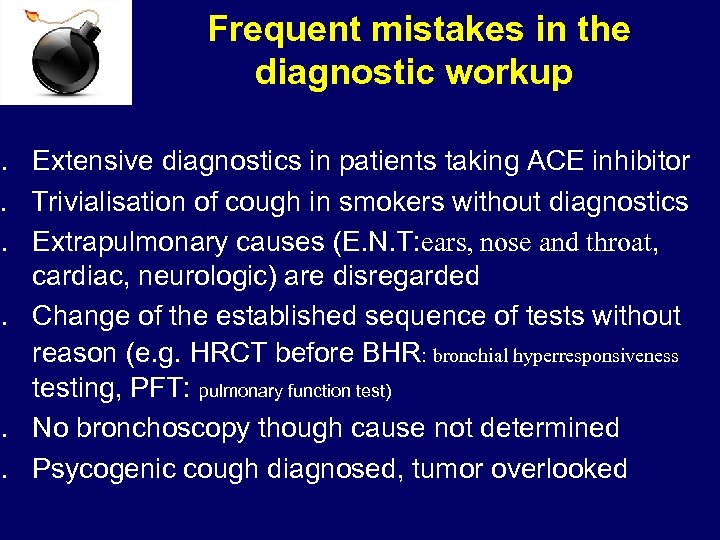 Frequent mistakes in the diagnostic workup 1. Extensive diagnostics in patients taking ACE inhibitor 2. Trivialisation of cough in smokers without diagnostics 3. Extrapulmonary causes (E. N. T: ears, nose and throat, cardiac, neurologic) are disregarded 4. Change of the established sequence of tests without reason (e. g. HRCT before BHR: bronchial hyperresponsiveness testing, PFT: pulmonary function test) 5. No bronchoscopy though cause not determined 6. Psycogenic cough diagnosed, tumor overlooked
Frequent mistakes in the diagnostic workup 1. Extensive diagnostics in patients taking ACE inhibitor 2. Trivialisation of cough in smokers without diagnostics 3. Extrapulmonary causes (E. N. T: ears, nose and throat, cardiac, neurologic) are disregarded 4. Change of the established sequence of tests without reason (e. g. HRCT before BHR: bronchial hyperresponsiveness testing, PFT: pulmonary function test) 5. No bronchoscopy though cause not determined 6. Psycogenic cough diagnosed, tumor overlooked
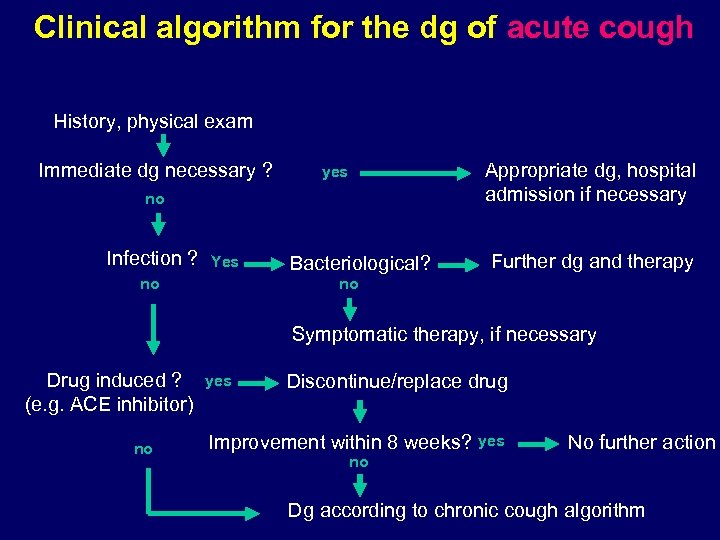 Clinical algorithm for the dg of acute cough History, physical exam Immediate dg necessary ? Appropriate dg, hospital admission if necessary yes no Infection ? Yes Bacteriological? Further dg and therapy no no Symptomatic therapy, if necessary Drug induced ? (e. g. ACE inhibitor) no yes Discontinue/replace drug Improvement within 8 weeks? no yes No further action Dg according to chronic cough algorithm
Clinical algorithm for the dg of acute cough History, physical exam Immediate dg necessary ? Appropriate dg, hospital admission if necessary yes no Infection ? Yes Bacteriological? Further dg and therapy no no Symptomatic therapy, if necessary Drug induced ? (e. g. ACE inhibitor) no yes Discontinue/replace drug Improvement within 8 weeks? no yes No further action Dg according to chronic cough algorithm
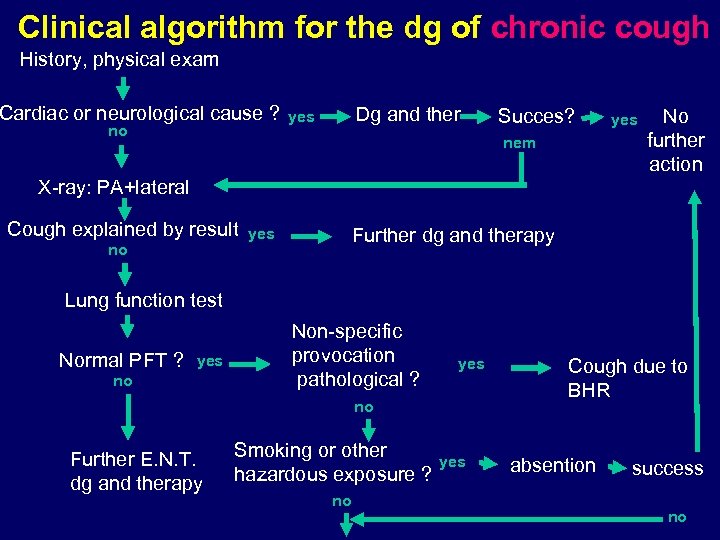 Clinical algorithm for the dg of chronic cough History, physical exam Cardiac or neurological cause ? no Dg and ther yes Succes? nem yes No further action X-ray: PA+lateral Cough explained by result no Further dg and therapy yes Lung function test Normal PFT ? yes no Non-specific provocation pathological ? yes no Further E. N. T. dg and therapy Smoking or other hazardous exposure ? no yes Cough due to BHR absention success no
Clinical algorithm for the dg of chronic cough History, physical exam Cardiac or neurological cause ? no Dg and ther yes Succes? nem yes No further action X-ray: PA+lateral Cough explained by result no Further dg and therapy yes Lung function test Normal PFT ? yes no Non-specific provocation pathological ? yes no Further E. N. T. dg and therapy Smoking or other hazardous exposure ? no yes Cough due to BHR absention success no
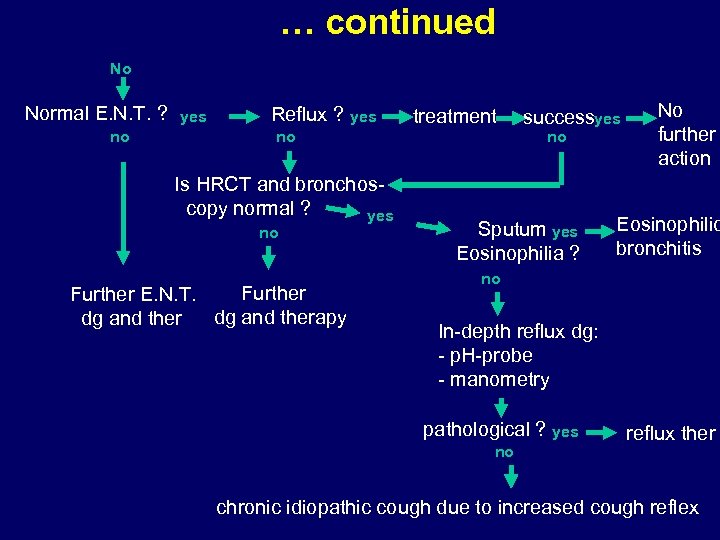 … continued No Normal E. N. T. ? no yes Reflux ? yes treatment no Is HRCT and bronchoscopy normal ? yes no Further E. N. T. dg and therapy dg and ther successyes no Sputum yes Eosinophilia ? No further action Eosinophilic bronchitis no In-depth reflux dg: - p. H-probe - manometry pathological ? yes no reflux ther chronic idiopathic cough due to increased cough reflex
… continued No Normal E. N. T. ? no yes Reflux ? yes treatment no Is HRCT and bronchoscopy normal ? yes no Further E. N. T. dg and therapy dg and ther successyes no Sputum yes Eosinophilia ? No further action Eosinophilic bronchitis no In-depth reflux dg: - p. H-probe - manometry pathological ? yes no reflux ther chronic idiopathic cough due to increased cough reflex
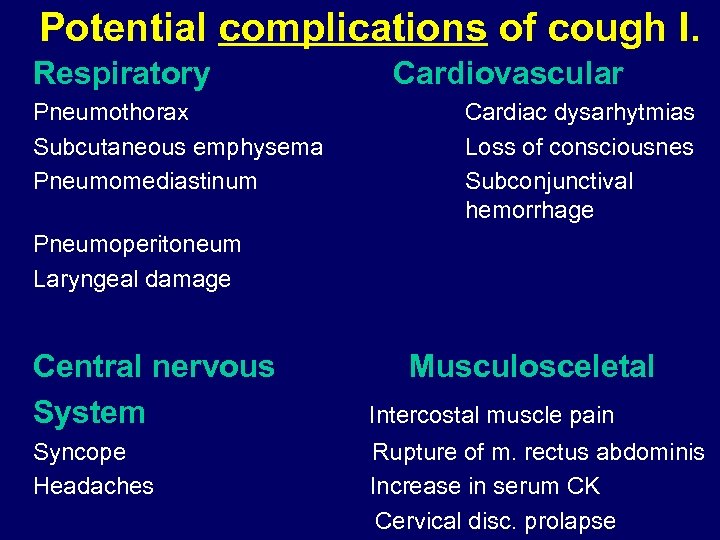 Potential complications of cough I. Respiratory Pneumothorax Subcutaneous emphysema Pneumomediastinum Cardiovascular Cardiac dysarhytmias Loss of consciousnes Subconjunctival hemorrhage Pneumoperitoneum Laryngeal damage Central nervous System Syncope Headaches Musculosceletal Intercostal muscle pain Rupture of m. rectus abdominis Increase in serum CK Cervical disc. prolapse
Potential complications of cough I. Respiratory Pneumothorax Subcutaneous emphysema Pneumomediastinum Cardiovascular Cardiac dysarhytmias Loss of consciousnes Subconjunctival hemorrhage Pneumoperitoneum Laryngeal damage Central nervous System Syncope Headaches Musculosceletal Intercostal muscle pain Rupture of m. rectus abdominis Increase in serum CK Cervical disc. prolapse
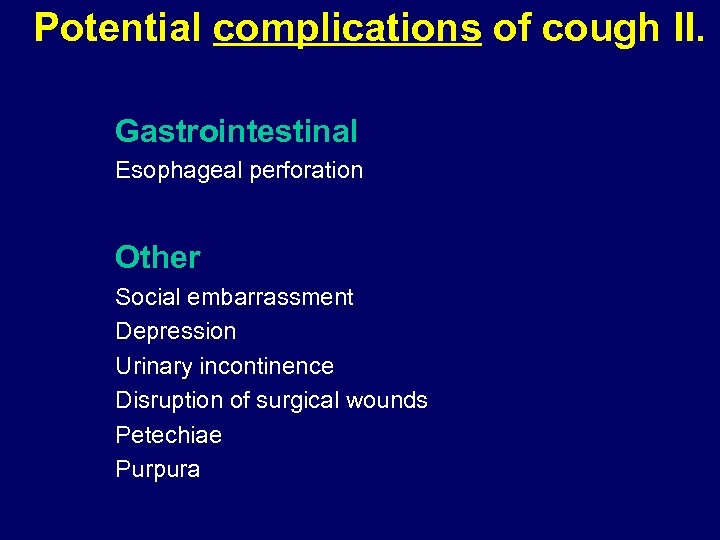 Potential complications of cough II. Gastrointestinal Esophageal perforation Other Social embarrassment Depression Urinary incontinence Disruption of surgical wounds Petechiae Purpura
Potential complications of cough II. Gastrointestinal Esophageal perforation Other Social embarrassment Depression Urinary incontinence Disruption of surgical wounds Petechiae Purpura
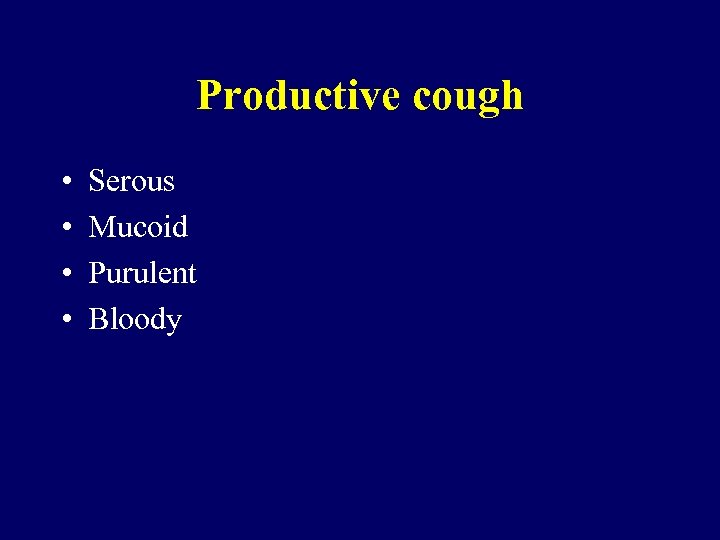 Productive cough • • Serous Mucoid Purulent Bloody
Productive cough • • Serous Mucoid Purulent Bloody
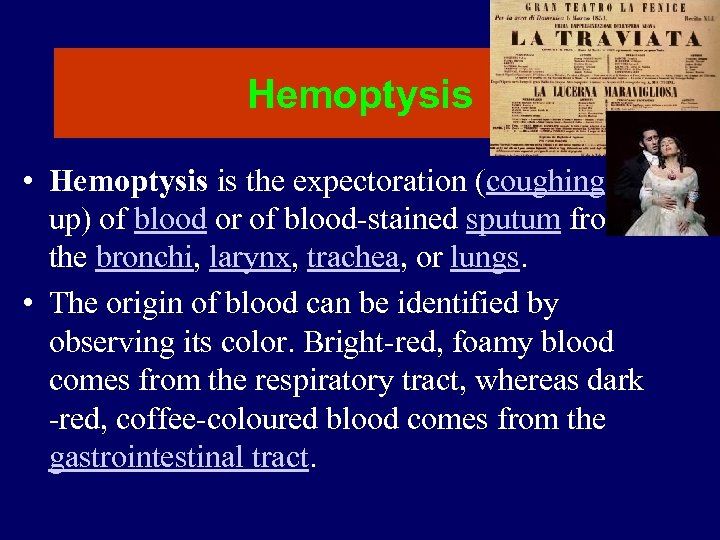 Hemoptysis • Hemoptysis is the expectoration (coughing up) of blood or of blood-stained sputum from the bronchi, larynx, trachea, or lungs. • The origin of blood can be identified by observing its color. Bright-red, foamy blood comes from the respiratory tract, whereas dark -red, coffee-coloured blood comes from the gastrointestinal tract.
Hemoptysis • Hemoptysis is the expectoration (coughing up) of blood or of blood-stained sputum from the bronchi, larynx, trachea, or lungs. • The origin of blood can be identified by observing its color. Bright-red, foamy blood comes from the respiratory tract, whereas dark -red, coffee-coloured blood comes from the gastrointestinal tract.
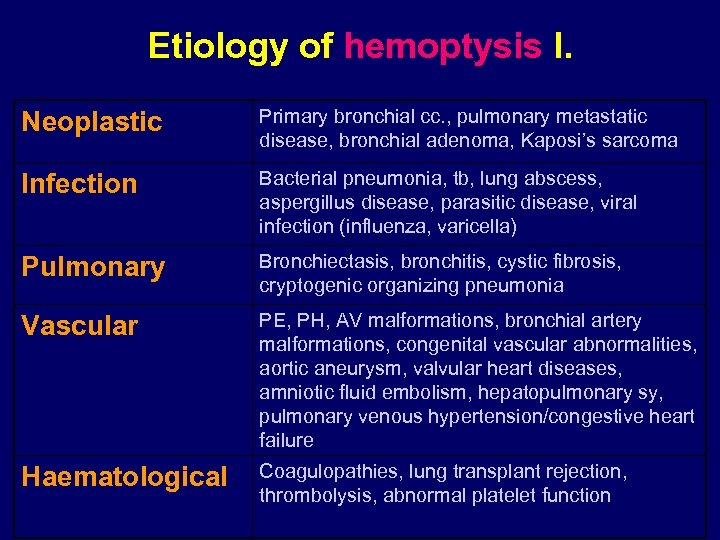 Etiology of hemoptysis I. Neoplastic Primary bronchial cc. , pulmonary metastatic disease, bronchial adenoma, Kaposi’s sarcoma Infection Bacterial pneumonia, tb, lung abscess, aspergillus disease, parasitic disease, viral infection (influenza, varicella) Pulmonary Bronchiectasis, bronchitis, cystic fibrosis, cryptogenic organizing pneumonia Vascular PE, PH, AV malformations, bronchial artery malformations, congenital vascular abnormalities, aortic aneurysm, valvular heart diseases, amniotic fluid embolism, hepatopulmonary sy, pulmonary venous hypertension/congestive heart failure Haematological Coagulopathies, lung transplant rejection, thrombolysis, abnormal platelet function
Etiology of hemoptysis I. Neoplastic Primary bronchial cc. , pulmonary metastatic disease, bronchial adenoma, Kaposi’s sarcoma Infection Bacterial pneumonia, tb, lung abscess, aspergillus disease, parasitic disease, viral infection (influenza, varicella) Pulmonary Bronchiectasis, bronchitis, cystic fibrosis, cryptogenic organizing pneumonia Vascular PE, PH, AV malformations, bronchial artery malformations, congenital vascular abnormalities, aortic aneurysm, valvular heart diseases, amniotic fluid embolism, hepatopulmonary sy, pulmonary venous hypertension/congestive heart failure Haematological Coagulopathies, lung transplant rejection, thrombolysis, abnormal platelet function
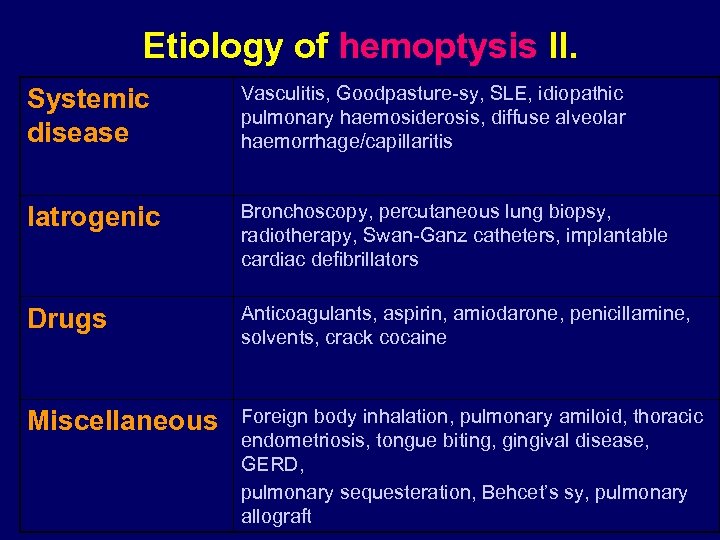 Etiology of hemoptysis II. Systemic disease Vasculitis, Goodpasture-sy, SLE, idiopathic pulmonary haemosiderosis, diffuse alveolar haemorrhage/capillaritis Iatrogenic Bronchoscopy, percutaneous lung biopsy, radiotherapy, Swan-Ganz catheters, implantable cardiac defibrillators Drugs Anticoagulants, aspirin, amiodarone, penicillamine, solvents, crack cocaine Miscellaneous Foreign body inhalation, pulmonary amiloid, thoracic endometriosis, tongue biting, gingival disease, GERD, pulmonary sequesteration, Behcet’s sy, pulmonary allograft
Etiology of hemoptysis II. Systemic disease Vasculitis, Goodpasture-sy, SLE, idiopathic pulmonary haemosiderosis, diffuse alveolar haemorrhage/capillaritis Iatrogenic Bronchoscopy, percutaneous lung biopsy, radiotherapy, Swan-Ganz catheters, implantable cardiac defibrillators Drugs Anticoagulants, aspirin, amiodarone, penicillamine, solvents, crack cocaine Miscellaneous Foreign body inhalation, pulmonary amiloid, thoracic endometriosis, tongue biting, gingival disease, GERD, pulmonary sequesteration, Behcet’s sy, pulmonary allograft
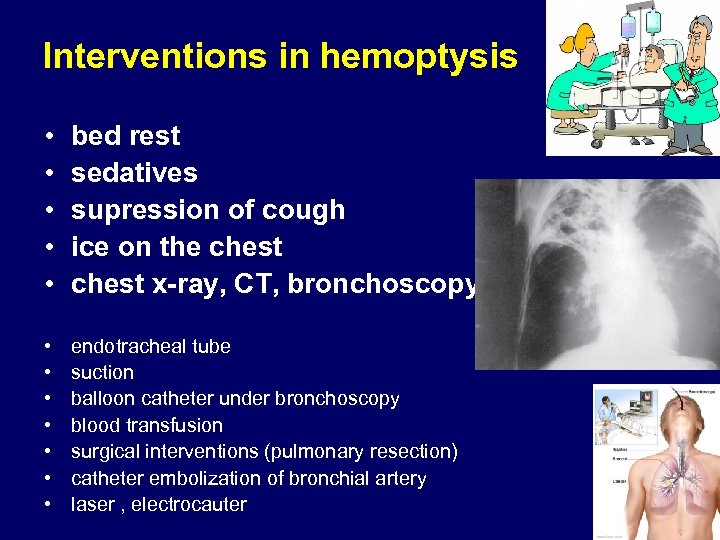 Interventions in hemoptysis • • • bed rest sedatives supression of cough ice on the chest x-ray, CT, bronchoscopy • • endotracheal tube suction balloon catheter under bronchoscopy blood transfusion surgical interventions (pulmonary resection) catheter embolization of bronchial artery laser , electrocauter
Interventions in hemoptysis • • • bed rest sedatives supression of cough ice on the chest x-ray, CT, bronchoscopy • • endotracheal tube suction balloon catheter under bronchoscopy blood transfusion surgical interventions (pulmonary resection) catheter embolization of bronchial artery laser , electrocauter
 Dyspnoe • Unpleasent or uncomfortable breathing • Difficulty in breathing, often associated with lung or heart disease and resulting in shortness of breath.
Dyspnoe • Unpleasent or uncomfortable breathing • Difficulty in breathing, often associated with lung or heart disease and resulting in shortness of breath.
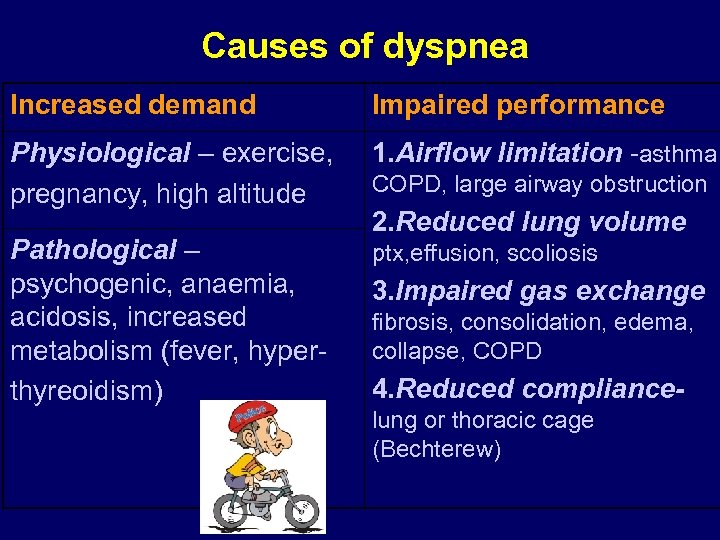 Causes of dyspnea Increased demand Impaired performance Physiological – exercise, pregnancy, high altitude 1. Airflow limitation -asthma, Pathological – psychogenic, anaemia, acidosis, increased metabolism (fever, hyperthyreoidism) ptx, effusion, scoliosis COPD, large airway obstruction 2. Reduced lung volume 3. Impaired gas exchange fibrosis, consolidation, edema, collapse, COPD 4. Reduced compliancelung or thoracic cage (Bechterew)
Causes of dyspnea Increased demand Impaired performance Physiological – exercise, pregnancy, high altitude 1. Airflow limitation -asthma, Pathological – psychogenic, anaemia, acidosis, increased metabolism (fever, hyperthyreoidism) ptx, effusion, scoliosis COPD, large airway obstruction 2. Reduced lung volume 3. Impaired gas exchange fibrosis, consolidation, edema, collapse, COPD 4. Reduced compliancelung or thoracic cage (Bechterew)
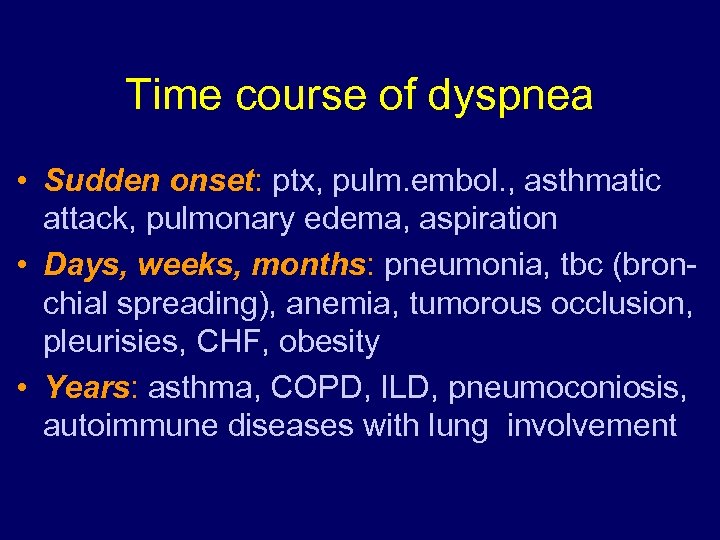 Time course of dyspnea • Sudden onset: ptx, pulm. embol. , asthmatic attack, pulmonary edema, aspiration • Days, weeks, months: pneumonia, tbc (bronchial spreading), anemia, tumorous occlusion, pleurisies, CHF, obesity • Years: asthma, COPD, ILD, pneumoconiosis, autoimmune diseases with lung involvement
Time course of dyspnea • Sudden onset: ptx, pulm. embol. , asthmatic attack, pulmonary edema, aspiration • Days, weeks, months: pneumonia, tbc (bronchial spreading), anemia, tumorous occlusion, pleurisies, CHF, obesity • Years: asthma, COPD, ILD, pneumoconiosis, autoimmune diseases with lung involvement
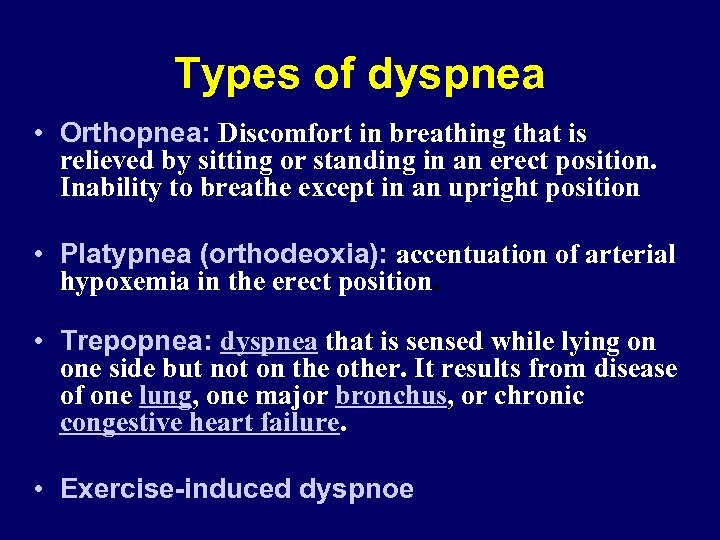 Types of dyspnea • Orthopnea: Discomfort in breathing that is relieved by sitting or standing in an erect position. Inability to breathe except in an upright position • Platypnea (orthodeoxia): accentuation of arterial hypoxemia in the erect position. • Trepopnea: dyspnea that is sensed while lying on one side but not on the other. It results from disease of one lung, one major bronchus, or chronic congestive heart failure. • Exercise-induced dyspnoe
Types of dyspnea • Orthopnea: Discomfort in breathing that is relieved by sitting or standing in an erect position. Inability to breathe except in an upright position • Platypnea (orthodeoxia): accentuation of arterial hypoxemia in the erect position. • Trepopnea: dyspnea that is sensed while lying on one side but not on the other. It results from disease of one lung, one major bronchus, or chronic congestive heart failure. • Exercise-induced dyspnoe
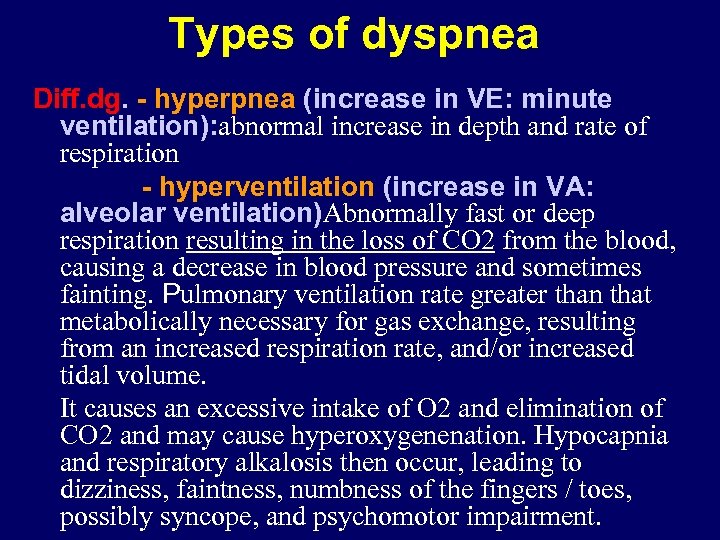 Types of dyspnea Diff. dg. - hyperpnea (increase in VE: minute ventilation): abnormal increase in depth and rate of respiration - hyperventilation (increase in VA: alveolar ventilation)Abnormally fast or deep respiration resulting in the loss of CO 2 from the blood, causing a decrease in blood pressure and sometimes fainting. Pulmonary ventilation rate greater than that metabolically necessary for gas exchange, resulting from an increased respiration rate, and/or increased tidal volume. It causes an excessive intake of O 2 and elimination of CO 2 and may cause hyperoxygenenation. Hypocapnia and respiratory alkalosis then occur, leading to dizziness, faintness, numbness of the fingers / toes, possibly syncope, and psychomotor impairment.
Types of dyspnea Diff. dg. - hyperpnea (increase in VE: minute ventilation): abnormal increase in depth and rate of respiration - hyperventilation (increase in VA: alveolar ventilation)Abnormally fast or deep respiration resulting in the loss of CO 2 from the blood, causing a decrease in blood pressure and sometimes fainting. Pulmonary ventilation rate greater than that metabolically necessary for gas exchange, resulting from an increased respiration rate, and/or increased tidal volume. It causes an excessive intake of O 2 and elimination of CO 2 and may cause hyperoxygenenation. Hypocapnia and respiratory alkalosis then occur, leading to dizziness, faintness, numbness of the fingers / toes, possibly syncope, and psychomotor impairment.
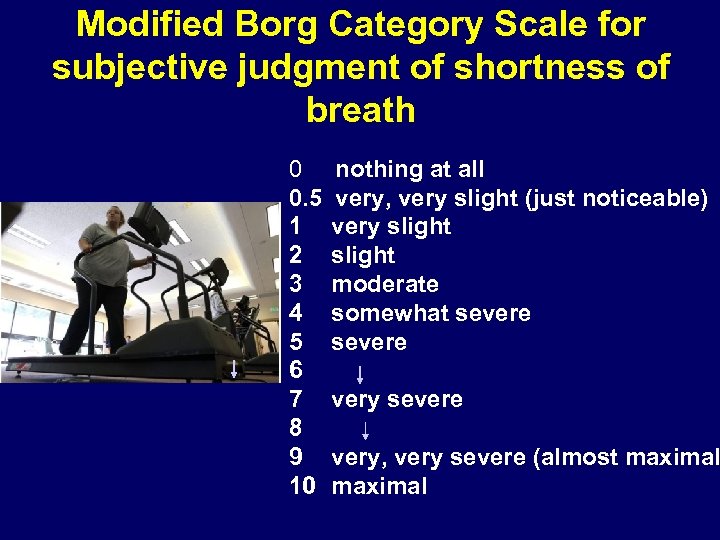 Modified Borg Category Scale for subjective judgment of shortness of breath 0 0. 5 1 2 3 4 5 6 7 8 9 10 nothing at all very, very slight (just noticeable) very slight moderate somewhat severe very, very severe (almost maximal
Modified Borg Category Scale for subjective judgment of shortness of breath 0 0. 5 1 2 3 4 5 6 7 8 9 10 nothing at all very, very slight (just noticeable) very slight moderate somewhat severe very, very severe (almost maximal
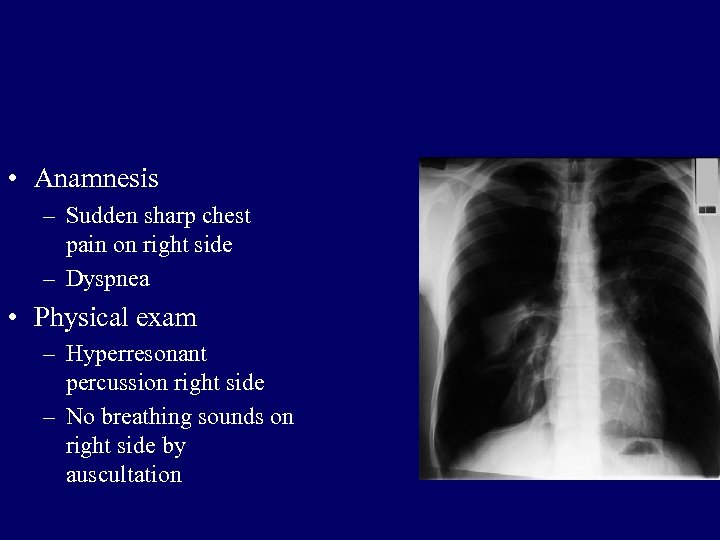 • Anamnesis – Sudden sharp chest pain on right side – Dyspnea • Physical exam – Hyperresonant percussion right side – No breathing sounds on right side by auscultation
• Anamnesis – Sudden sharp chest pain on right side – Dyspnea • Physical exam – Hyperresonant percussion right side – No breathing sounds on right side by auscultation
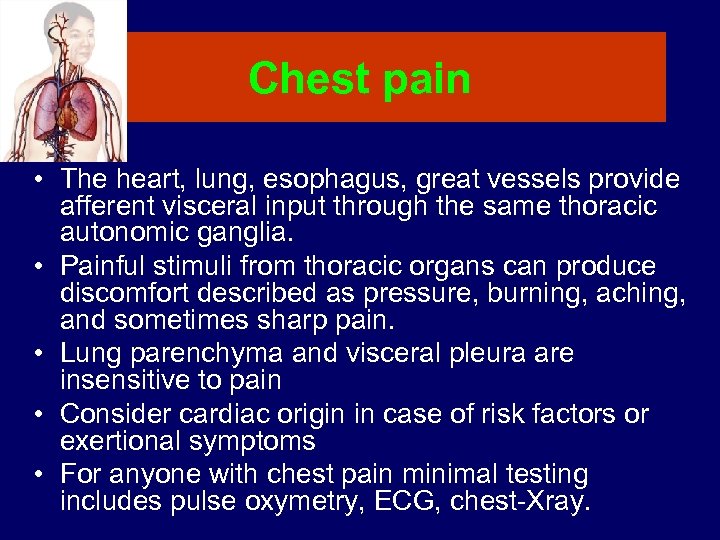 Chest pain • The heart, lung, esophagus, great vessels provide afferent visceral input through the same thoracic autonomic ganglia. • Painful stimuli from thoracic organs can produce discomfort described as pressure, burning, aching, and sometimes sharp pain. • Lung parenchyma and visceral pleura are insensitive to pain • Consider cardiac origin in case of risk factors or exertional symptoms • For anyone with chest pain minimal testing includes pulse oxymetry, ECG, chest-Xray.
Chest pain • The heart, lung, esophagus, great vessels provide afferent visceral input through the same thoracic autonomic ganglia. • Painful stimuli from thoracic organs can produce discomfort described as pressure, burning, aching, and sometimes sharp pain. • Lung parenchyma and visceral pleura are insensitive to pain • Consider cardiac origin in case of risk factors or exertional symptoms • For anyone with chest pain minimal testing includes pulse oxymetry, ECG, chest-Xray.
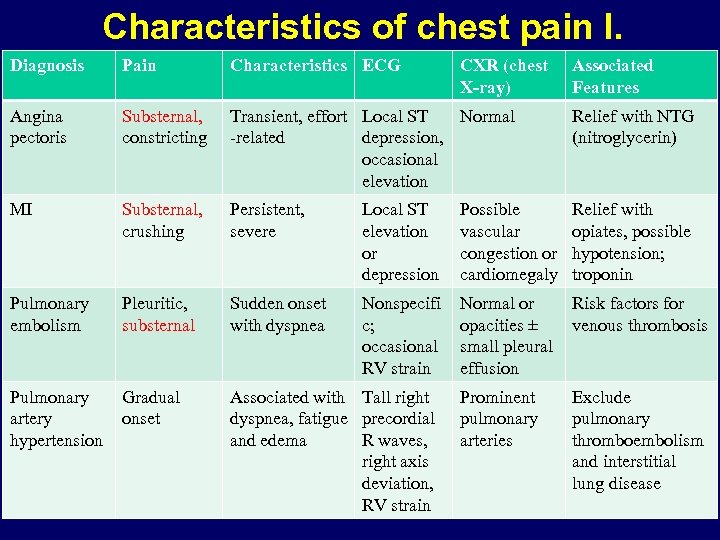 Characteristics of chest pain I. Diagnosis Pain Characteristics ECG CXR (chest X-ray) Associated Features Angina pectoris Substernal, constricting Transient, effort Local ST Normal -related depression, occasional elevation Relief with NTG (nitroglycerin) MI Substernal, crushing Persistent, severe Local ST elevation or depression Possible vascular congestion or cardiomegaly Relief with opiates, possible hypotension; troponin Pulmonary embolism Pleuritic, substernal Sudden onset with dyspnea Nonspecifi c; occasional RV strain Normal or opacities ± small pleural effusion Risk factors for venous thrombosis Pulmonary artery hypertension Gradual onset Associated with Tall right dyspnea, fatigue precordial and edema R waves, right axis deviation, RV strain Prominent pulmonary arteries Exclude pulmonary thromboembolism and interstitial lung disease
Characteristics of chest pain I. Diagnosis Pain Characteristics ECG CXR (chest X-ray) Associated Features Angina pectoris Substernal, constricting Transient, effort Local ST Normal -related depression, occasional elevation Relief with NTG (nitroglycerin) MI Substernal, crushing Persistent, severe Local ST elevation or depression Possible vascular congestion or cardiomegaly Relief with opiates, possible hypotension; troponin Pulmonary embolism Pleuritic, substernal Sudden onset with dyspnea Nonspecifi c; occasional RV strain Normal or opacities ± small pleural effusion Risk factors for venous thrombosis Pulmonary artery hypertension Gradual onset Associated with Tall right dyspnea, fatigue precordial and edema R waves, right axis deviation, RV strain Prominent pulmonary arteries Exclude pulmonary thromboembolism and interstitial lung disease
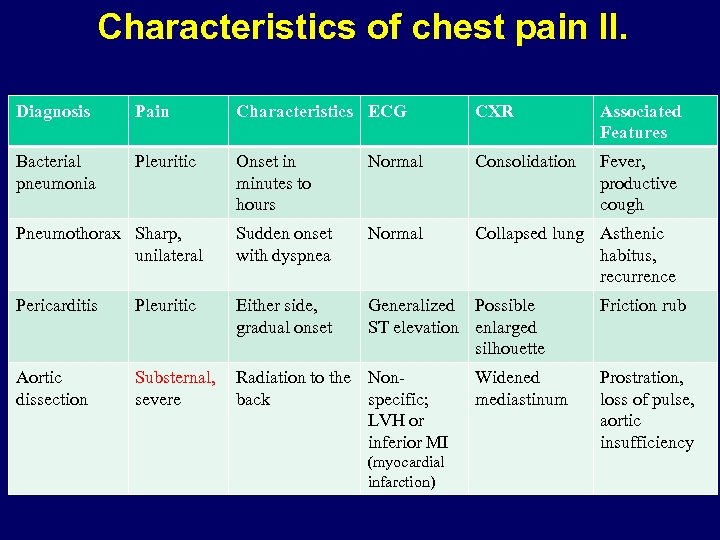 Characteristics of chest pain II. Diagnosis Pain Characteristics ECG CXR Associated Features Bacterial pneumonia Pleuritic Onset in minutes to hours Normal Consolidation Fever, productive cough Pneumothorax Sharp, unilateral Sudden onset with dyspnea Normal Collapsed lung Asthenic habitus, recurrence Pericarditis Pleuritic Either side, gradual onset Generalized Possible ST elevation enlarged silhouette Aortic dissection Substernal, severe Radiation to the Nonback specific; LVH or inferior MI (myocardial infarction) Widened mediastinum Friction rub Prostration, loss of pulse, aortic insufficiency
Characteristics of chest pain II. Diagnosis Pain Characteristics ECG CXR Associated Features Bacterial pneumonia Pleuritic Onset in minutes to hours Normal Consolidation Fever, productive cough Pneumothorax Sharp, unilateral Sudden onset with dyspnea Normal Collapsed lung Asthenic habitus, recurrence Pericarditis Pleuritic Either side, gradual onset Generalized Possible ST elevation enlarged silhouette Aortic dissection Substernal, severe Radiation to the Nonback specific; LVH or inferior MI (myocardial infarction) Widened mediastinum Friction rub Prostration, loss of pulse, aortic insufficiency
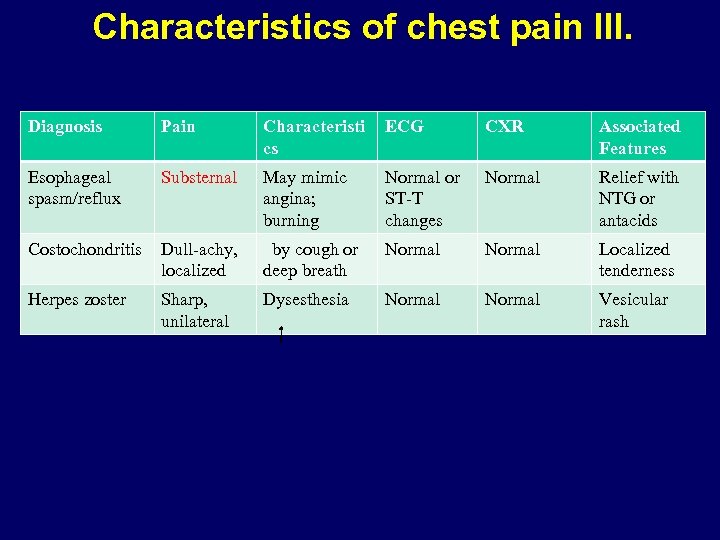 Characteristics of chest pain III. Diagnosis Pain Characteristi cs ECG CXR Associated Features Esophageal spasm/reflux Substernal May mimic angina; burning Normal or ST-T changes Normal Relief with NTG or antacids Costochondritis Dull-achy, localized by cough or deep breath Normal Localized tenderness Herpes zoster Sharp, unilateral Dysesthesia Normal Vesicular rash
Characteristics of chest pain III. Diagnosis Pain Characteristi cs ECG CXR Associated Features Esophageal spasm/reflux Substernal May mimic angina; burning Normal or ST-T changes Normal Relief with NTG or antacids Costochondritis Dull-achy, localized by cough or deep breath Normal Localized tenderness Herpes zoster Sharp, unilateral Dysesthesia Normal Vesicular rash
 Lung cancer 08. 09. 2016. 40
Lung cancer 08. 09. 2016. 40
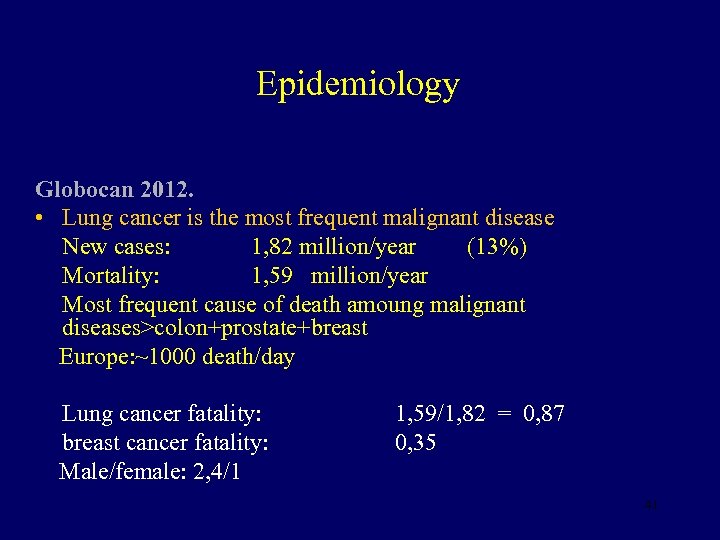 Epidemiology Globocan 2012. • Lung cancer is the most frequent malignant disease New cases: 1, 82 million/year (13%) Mortality: 1, 59 million/year Most frequent cause of death amoung malignant diseases>colon+prostate+breast Europe: ~1000 death/day Lung cancer fatality: breast cancer fatality: Male/female: 2, 4/1 1, 59/1, 82 = 0, 87 0, 35 41
Epidemiology Globocan 2012. • Lung cancer is the most frequent malignant disease New cases: 1, 82 million/year (13%) Mortality: 1, 59 million/year Most frequent cause of death amoung malignant diseases>colon+prostate+breast Europe: ~1000 death/day Lung cancer fatality: breast cancer fatality: Male/female: 2, 4/1 1, 59/1, 82 = 0, 87 0, 35 41
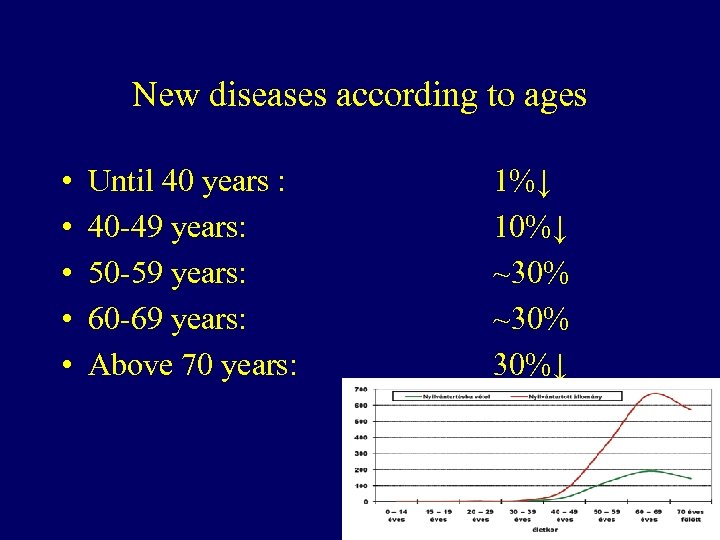 New diseases according to ages • • • Until 40 years : 40 -49 years: 50 -59 years: 60 -69 years: Above 70 years: 1%↓ 10%↓ ~30% 30%↓ 42
New diseases according to ages • • • Until 40 years : 40 -49 years: 50 -59 years: 60 -69 years: Above 70 years: 1%↓ 10%↓ ~30% 30%↓ 42
 Etiologic factors Smoking Athmospheric pollution Ionisation Occupational factors asbestos, radon, etc Other lung diseases tb, COPD, ILD Genetic events 43
Etiologic factors Smoking Athmospheric pollution Ionisation Occupational factors asbestos, radon, etc Other lung diseases tb, COPD, ILD Genetic events 43
 Smoking • 400 chemical materials • 60 carcinogens • Gas and particulate phase – Nitrosamines, aromatic amines, benzopyrene, CO 2, aldehids, nicotin, free radicals • Pack-year 44
Smoking • 400 chemical materials • 60 carcinogens • Gas and particulate phase – Nitrosamines, aromatic amines, benzopyrene, CO 2, aldehids, nicotin, free radicals • Pack-year 44
 Smoking and Lung Cancer • 85 -90% of lung cancer patients are smokers • Damages of 10 -15 gens have role in the development of lung cancer • 86% of smokers have damages of these gens 45
Smoking and Lung Cancer • 85 -90% of lung cancer patients are smokers • Damages of 10 -15 gens have role in the development of lung cancer • 86% of smokers have damages of these gens 45
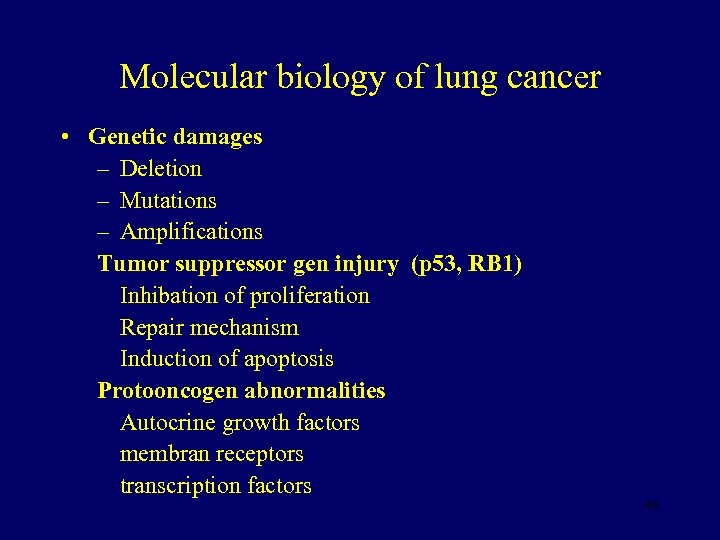 Molecular biology of lung cancer • Genetic damages – Deletion – Mutations – Amplifications Tumor suppressor gen injury (p 53, RB 1) Inhibation of proliferation Repair mechanism Induction of apoptosis Protooncogen abnormalities Autocrine growth factors membran receptors transcription factors 46
Molecular biology of lung cancer • Genetic damages – Deletion – Mutations – Amplifications Tumor suppressor gen injury (p 53, RB 1) Inhibation of proliferation Repair mechanism Induction of apoptosis Protooncogen abnormalities Autocrine growth factors membran receptors transcription factors 46
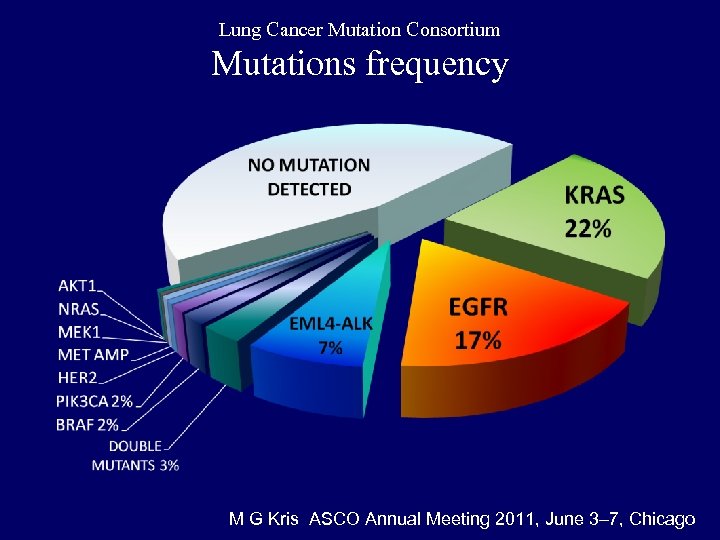 Lung Cancer Mutation Consortium Mutations frequency M G Kris ASCO Annual Meeting 2011, June 3– 7, Chicago
Lung Cancer Mutation Consortium Mutations frequency M G Kris ASCO Annual Meeting 2011, June 3– 7, Chicago
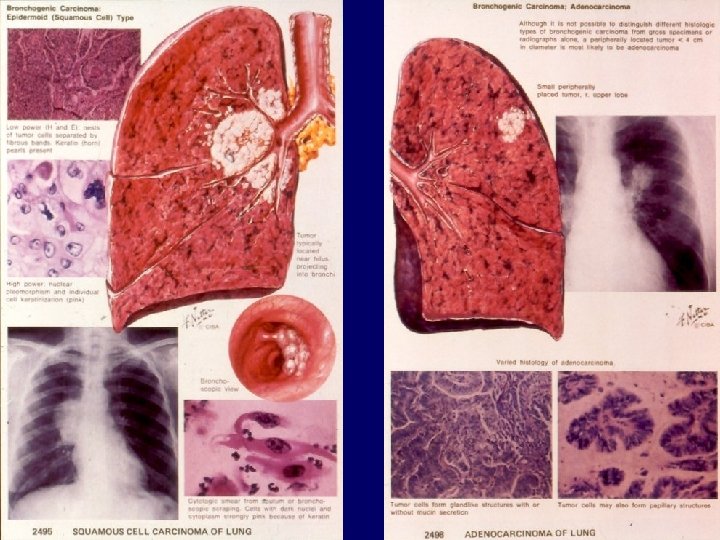
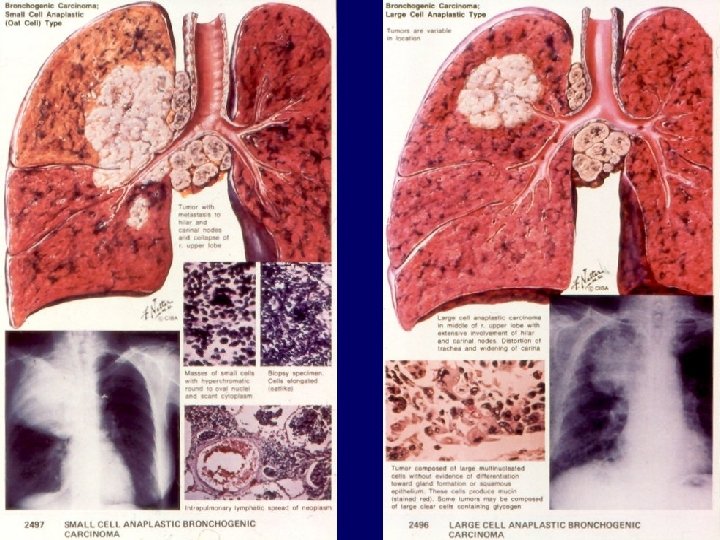
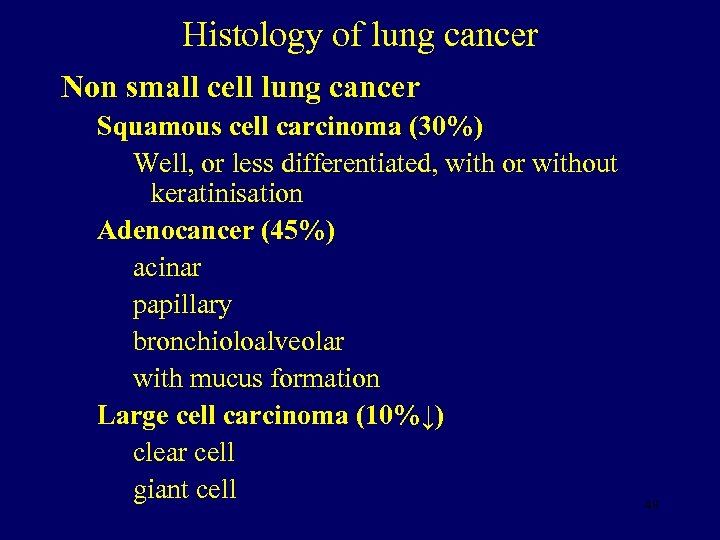 Histology of lung cancer Non small cell lung cancer Squamous cell carcinoma (30%) Well, or less differentiated, with or without keratinisation Adenocancer (45%) acinar papillary bronchioloalveolar with mucus formation Large cell carcinoma (10%↓) clear cell giant cell 49
Histology of lung cancer Non small cell lung cancer Squamous cell carcinoma (30%) Well, or less differentiated, with or without keratinisation Adenocancer (45%) acinar papillary bronchioloalveolar with mucus formation Large cell carcinoma (10%↓) clear cell giant cell 49
 50
50
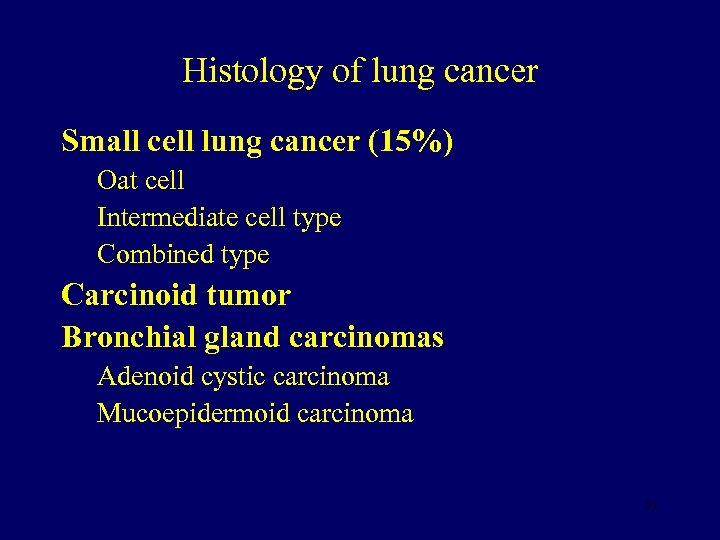 Histology of lung cancer Small cell lung cancer (15%) Oat cell Intermediate cell type Combined type Carcinoid tumor Bronchial gland carcinomas Adenoid cystic carcinoma Mucoepidermoid carcinoma 51
Histology of lung cancer Small cell lung cancer (15%) Oat cell Intermediate cell type Combined type Carcinoid tumor Bronchial gland carcinomas Adenoid cystic carcinoma Mucoepidermoid carcinoma 51
 52
52
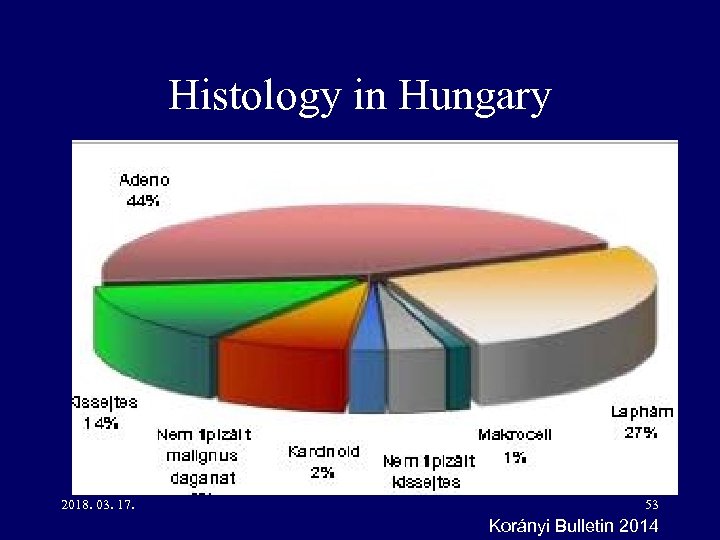 Histology in Hungary 2018. 03. 17. 53 Korányi Bulletin 2014
Histology in Hungary 2018. 03. 17. 53 Korányi Bulletin 2014
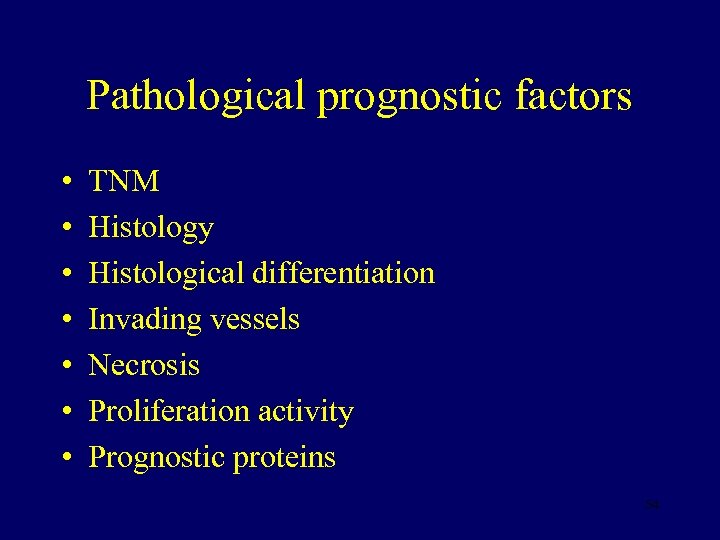 Pathological prognostic factors • • TNM Histology Histological differentiation Invading vessels Necrosis Proliferation activity Prognostic proteins 54
Pathological prognostic factors • • TNM Histology Histological differentiation Invading vessels Necrosis Proliferation activity Prognostic proteins 54
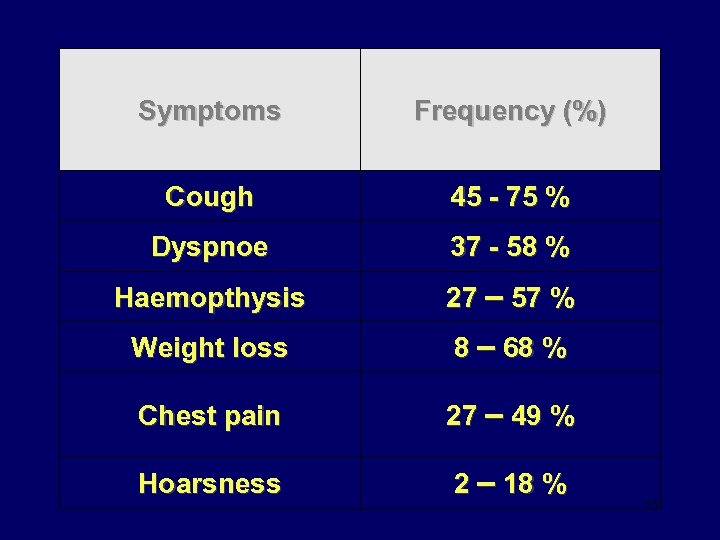 Symptoms Frequency (%) Cough 45 - 75 % Dyspnoe 37 - 58 % Haemopthysis 27 – 57 % Weight loss 8 – 68 % Chest pain 27 – 49 % Hoarsness 2 – 18 % 55
Symptoms Frequency (%) Cough 45 - 75 % Dyspnoe 37 - 58 % Haemopthysis 27 – 57 % Weight loss 8 – 68 % Chest pain 27 – 49 % Hoarsness 2 – 18 % 55
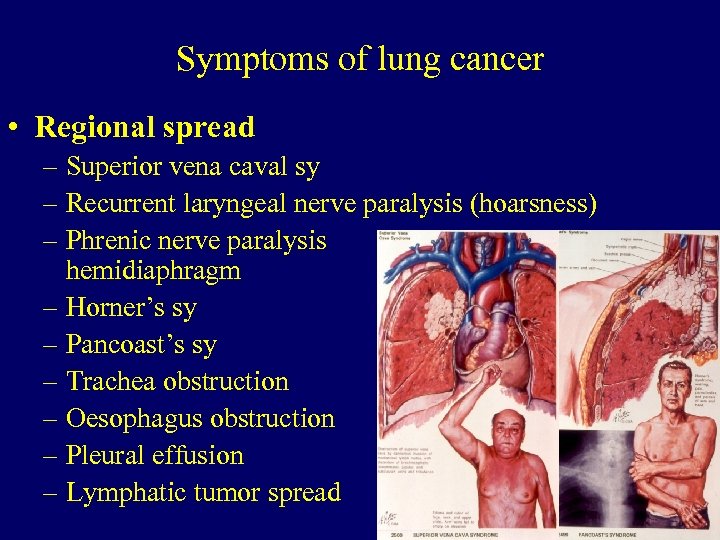 Symptoms of lung cancer • Regional spread – Superior vena caval sy – Recurrent laryngeal nerve paralysis (hoarsness) – Phrenic nerve paralysis elevated hemidiaphragm – Horner’s sy – Pancoast’s sy – Trachea obstruction – Oesophagus obstruction – Pleural effusion – Lymphatic tumor spread 56
Symptoms of lung cancer • Regional spread – Superior vena caval sy – Recurrent laryngeal nerve paralysis (hoarsness) – Phrenic nerve paralysis elevated hemidiaphragm – Horner’s sy – Pancoast’s sy – Trachea obstruction – Oesophagus obstruction – Pleural effusion – Lymphatic tumor spread 56
 57
57
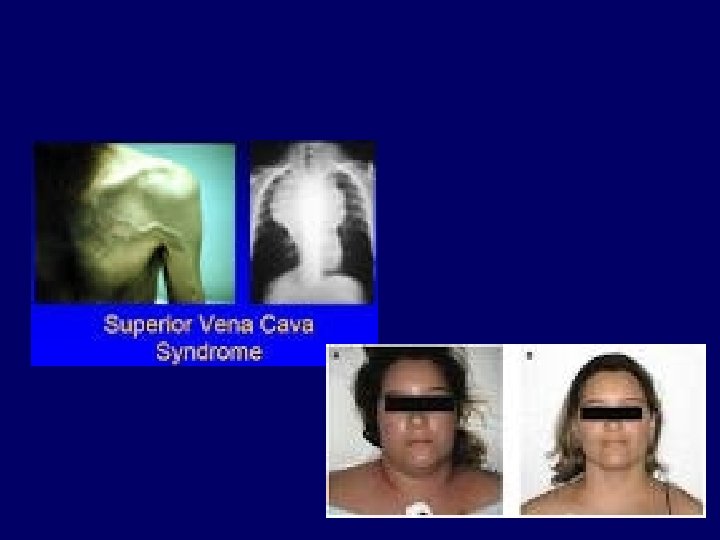
 Vena cava superior sy 2018. 03. 17. 58 Sárosi Veronika anyaga
Vena cava superior sy 2018. 03. 17. 58 Sárosi Veronika anyaga
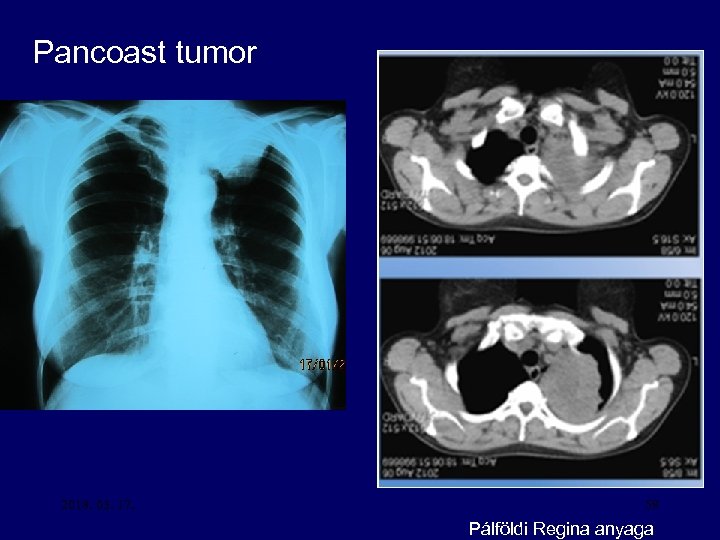 Pancoast tumor 2018. 03. 17. 59 Pálföldi Regina anyaga
Pancoast tumor 2018. 03. 17. 59 Pálföldi Regina anyaga
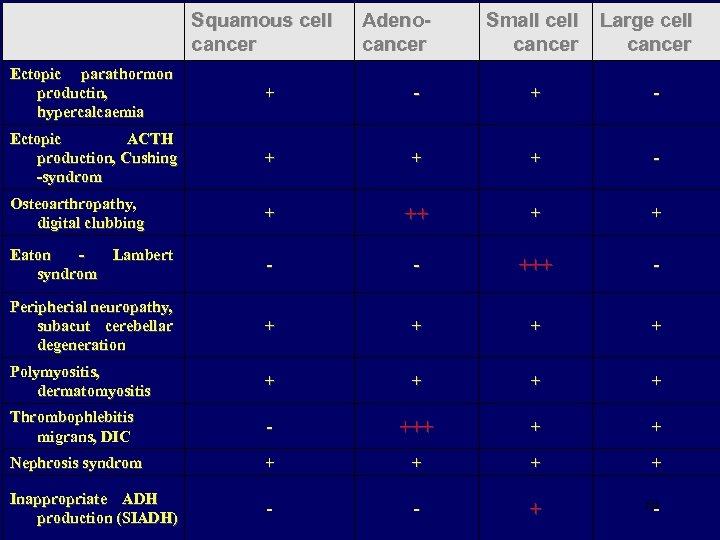 Squamous cell cancer Adenocancer Small cell cancer Large cell cancer Ectopic parathormon productin, hypercalcaemia + - Ectopic ACTH production, Cushing -syndrom + + + - Osteoarthropathy, digital clubbing + ++ + + Eaton Lambert syndrom - - +++ - Peripherial neuropathy, subacut cerebellar degeneration + + Polymyositis, dermatomyositis + + Thrombophlebitis migrans, DIC - +++ + + Nephrosis syndrom + + Inappropriate ADH production (SIADH) - - + 60 -
Squamous cell cancer Adenocancer Small cell cancer Large cell cancer Ectopic parathormon productin, hypercalcaemia + - Ectopic ACTH production, Cushing -syndrom + + + - Osteoarthropathy, digital clubbing + ++ + + Eaton Lambert syndrom - - +++ - Peripherial neuropathy, subacut cerebellar degeneration + + Polymyositis, dermatomyositis + + Thrombophlebitis migrans, DIC - +++ + + Nephrosis syndrom + + Inappropriate ADH production (SIADH) - - + 60 -
 Digital clubbing 2018. 03. 17. 61 Sárosi Veronika anyaga
Digital clubbing 2018. 03. 17. 61 Sárosi Veronika anyaga
 Diagnostic procedures • • Imaging technics Endoscopy Pathology Laboratory tests 62
Diagnostic procedures • • Imaging technics Endoscopy Pathology Laboratory tests 62
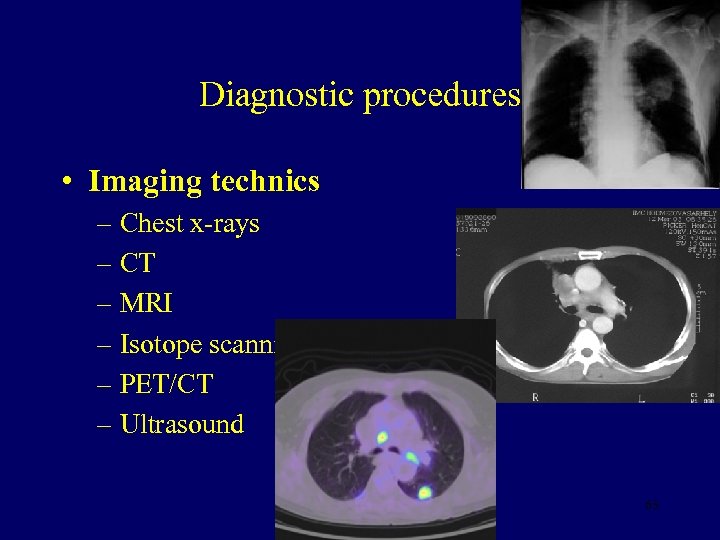 Diagnostic procedures • Imaging technics – Chest x-rays – CT – MRI – Isotope scanning – PET/CT – Ultrasound 63
Diagnostic procedures • Imaging technics – Chest x-rays – CT – MRI – Isotope scanning – PET/CT – Ultrasound 63
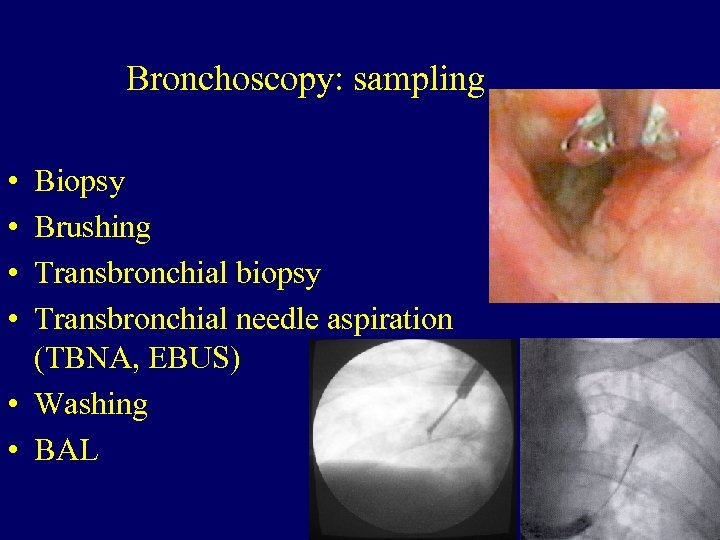 Bronchoscopy: sampling • • Biopsy Brushing Transbronchial biopsy Transbronchial needle aspiration (TBNA, EBUS) • Washing • BAL 64
Bronchoscopy: sampling • • Biopsy Brushing Transbronchial biopsy Transbronchial needle aspiration (TBNA, EBUS) • Washing • BAL 64
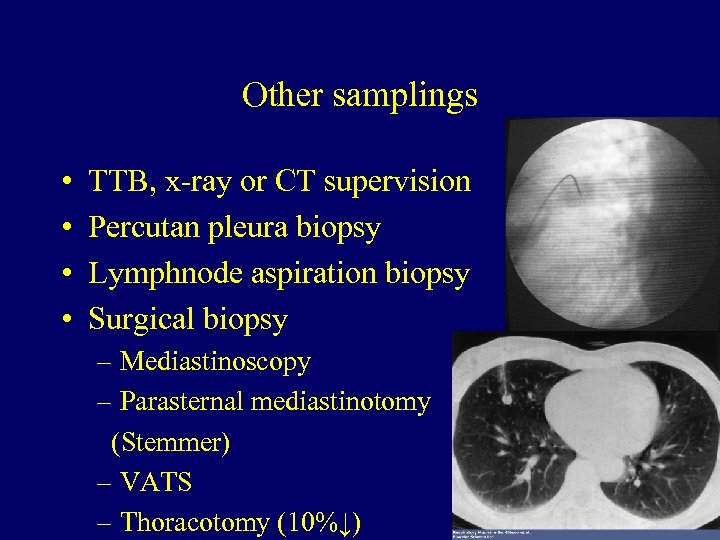 Other samplings • • TTB, x-ray or CT supervision Percutan pleura biopsy Lymphnode aspiration biopsy Surgical biopsy – Mediastinoscopy – Parasternal mediastinotomy (Stemmer) – VATS – Thoracotomy (10%↓) 65
Other samplings • • TTB, x-ray or CT supervision Percutan pleura biopsy Lymphnode aspiration biopsy Surgical biopsy – Mediastinoscopy – Parasternal mediastinotomy (Stemmer) – VATS – Thoracotomy (10%↓) 65
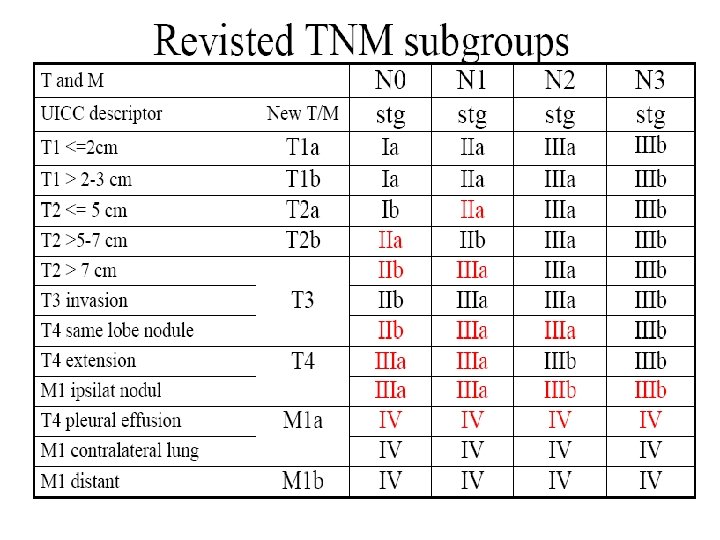
 Staging 1 • T 1 a = Tumor ≤ 2 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i. e. , not in the main bronchus). • T 1 b = Tumor >2 cm but ≤ 3 cm in greatest dimension 66
Staging 1 • T 1 a = Tumor ≤ 2 cm in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i. e. , not in the main bronchus). • T 1 b = Tumor >2 cm but ≤ 3 cm in greatest dimension 66
 Staging 2 • T 2 a = Tumor >3 cm but ≤ 5 cm in greatest dimension, or tumor with any of the following features: involves main bronchus, ≥ 2 cm distal to the carina; invades visceral pleura (PL 1 or PL 2); or is associated with atelectasis or obstructive pneumonitis that extends to the hilar region but does not involve the entire lung. • T 2 b = Tumor >5 cm but ≤ 7 cm or less in greatest dimension 67
Staging 2 • T 2 a = Tumor >3 cm but ≤ 5 cm in greatest dimension, or tumor with any of the following features: involves main bronchus, ≥ 2 cm distal to the carina; invades visceral pleura (PL 1 or PL 2); or is associated with atelectasis or obstructive pneumonitis that extends to the hilar region but does not involve the entire lung. • T 2 b = Tumor >5 cm but ≤ 7 cm or less in greatest dimension 67
 Staging 3 • T 3 = Tumor >7 cm or one that directly invades any of the following: parietal pleural (PL 3) chest wall (including superior sulcus tumors), diaphragm, phrenic nerve, mediastinal pleura, or parietal pericardium or tumor in the main bronchus (<2 cm distal to the bif. carina but without involvement of the carina) or associated atelectasis or obstructive pneumonitis of the entire lung or separate tumor nodule(s) in the same lobe 68
Staging 3 • T 3 = Tumor >7 cm or one that directly invades any of the following: parietal pleural (PL 3) chest wall (including superior sulcus tumors), diaphragm, phrenic nerve, mediastinal pleura, or parietal pericardium or tumor in the main bronchus (<2 cm distal to the bif. carina but without involvement of the carina) or associated atelectasis or obstructive pneumonitis of the entire lung or separate tumor nodule(s) in the same lobe 68
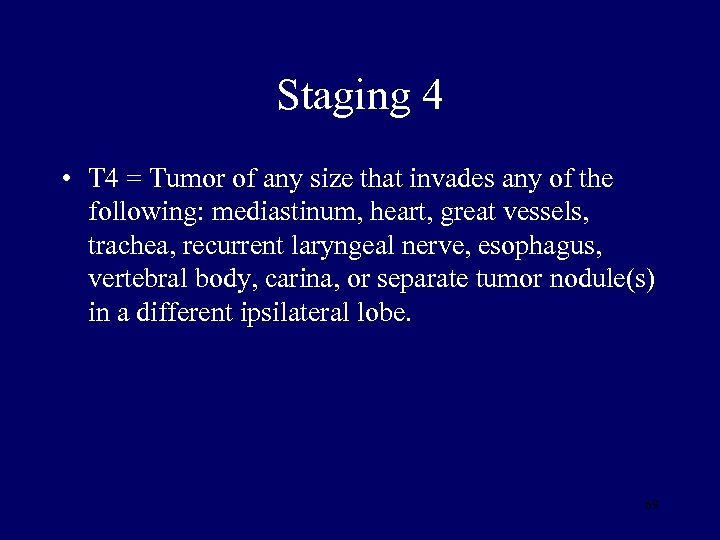 Staging 4 • T 4 = Tumor of any size that invades any of the following: mediastinum, heart, great vessels, trachea, recurrent laryngeal nerve, esophagus, vertebral body, carina, or separate tumor nodule(s) in a different ipsilateral lobe. 69
Staging 4 • T 4 = Tumor of any size that invades any of the following: mediastinum, heart, great vessels, trachea, recurrent laryngeal nerve, esophagus, vertebral body, carina, or separate tumor nodule(s) in a different ipsilateral lobe. 69
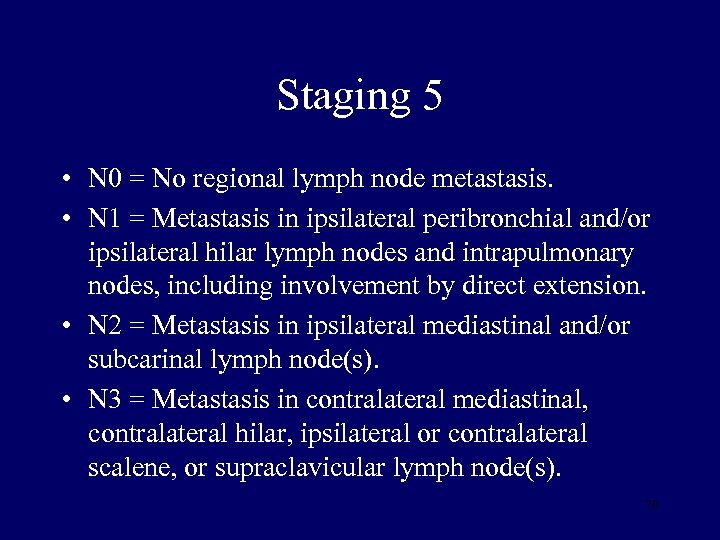 Staging 5 • N 0 = No regional lymph node metastasis. • N 1 = Metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension. • N 2 = Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s). • N 3 = Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s). 70
Staging 5 • N 0 = No regional lymph node metastasis. • N 1 = Metastasis in ipsilateral peribronchial and/or ipsilateral hilar lymph nodes and intrapulmonary nodes, including involvement by direct extension. • N 2 = Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s). • N 3 = Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s). 70
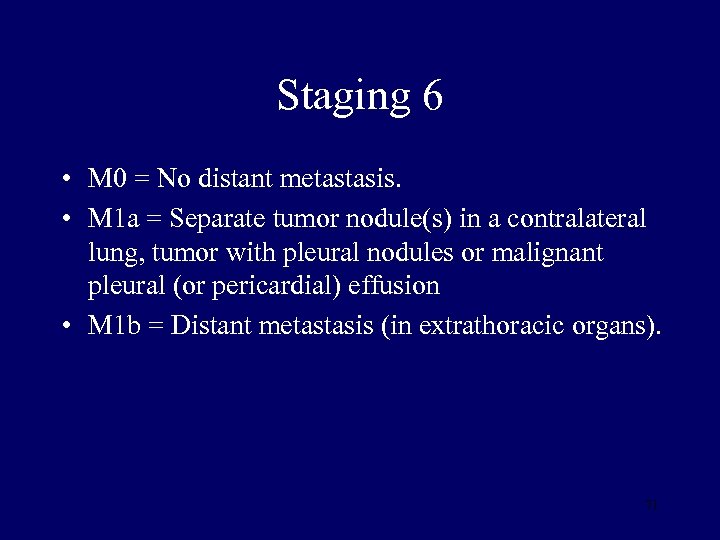 Staging 6 • M 0 = No distant metastasis. • M 1 a = Separate tumor nodule(s) in a contralateral lung, tumor with pleural nodules or malignant pleural (or pericardial) effusion • M 1 b = Distant metastasis (in extrathoracic organs). 71
Staging 6 • M 0 = No distant metastasis. • M 1 a = Separate tumor nodule(s) in a contralateral lung, tumor with pleural nodules or malignant pleural (or pericardial) effusion • M 1 b = Distant metastasis (in extrathoracic organs). 71
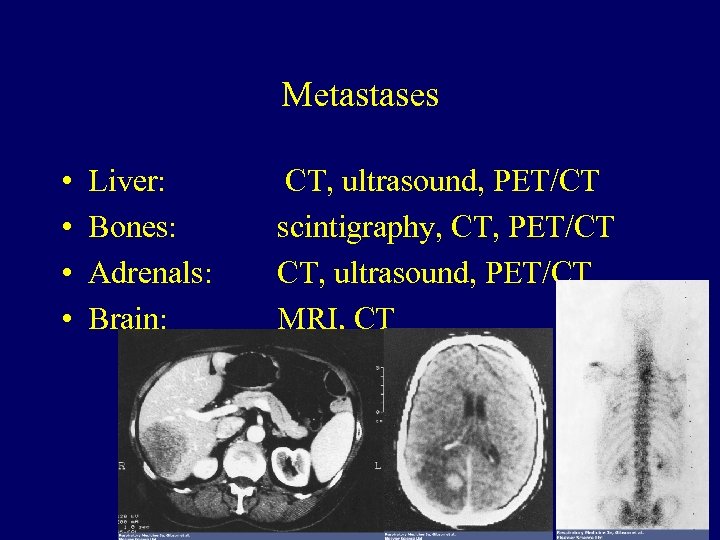 Metastases • • Liver: Bones: Adrenals: Brain: CT, ultrasound, PET/CT scintigraphy, CT, PET/CT CT, ultrasound, PET/CT MRI, CT 73
Metastases • • Liver: Bones: Adrenals: Brain: CT, ultrasound, PET/CT scintigraphy, CT, PET/CT CT, ultrasound, PET/CT MRI, CT 73
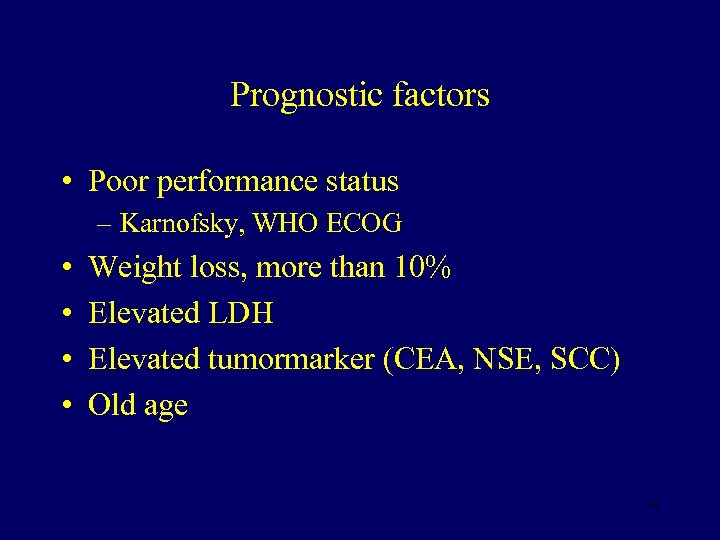 Prognostic factors • Poor performance status – Karnofsky, WHO ECOG • • Weight loss, more than 10% Elevated LDH Elevated tumormarker (CEA, NSE, SCC) Old age 74
Prognostic factors • Poor performance status – Karnofsky, WHO ECOG • • Weight loss, more than 10% Elevated LDH Elevated tumormarker (CEA, NSE, SCC) Old age 74
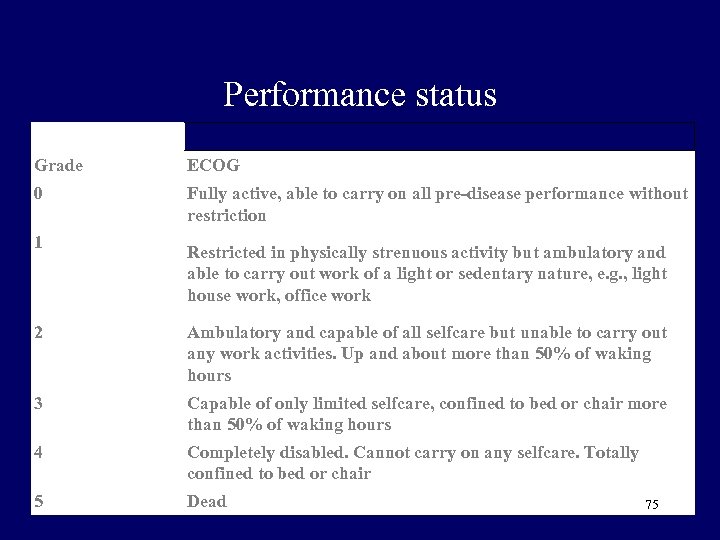 Performance status Grade ECOG 0 Fully active, able to carry on all pre-disease performance without restriction 1 Restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature, e. g. , light house work, office work 2 Ambulatory and capable of all selfcare but unable to carry out any work activities. Up and about more than 50% of waking hours 3 Capable of only limited selfcare, confined to bed or chair more than 50% of waking hours 4 Completely disabled. Cannot carry on any selfcare. Totally confined to bed or chair 5 Dead 75
Performance status Grade ECOG 0 Fully active, able to carry on all pre-disease performance without restriction 1 Restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature, e. g. , light house work, office work 2 Ambulatory and capable of all selfcare but unable to carry out any work activities. Up and about more than 50% of waking hours 3 Capable of only limited selfcare, confined to bed or chair more than 50% of waking hours 4 Completely disabled. Cannot carry on any selfcare. Totally confined to bed or chair 5 Dead 75
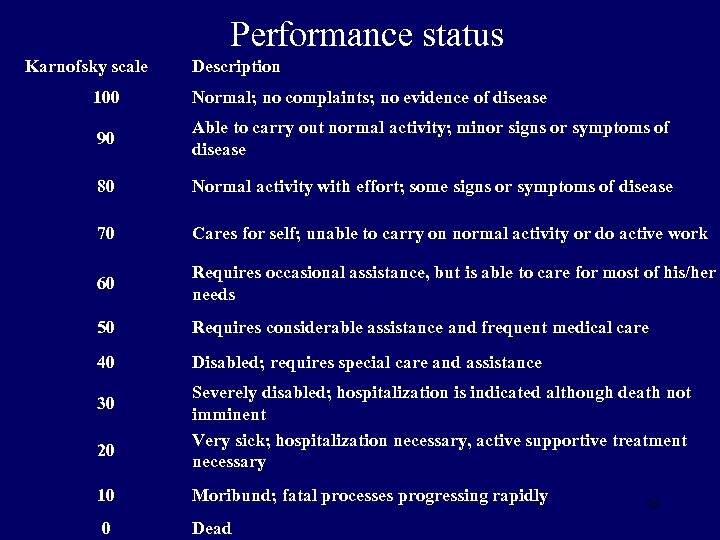 Performance status Karnofsky scale Description 100 Normal; no complaints; no evidence of disease 90 Able to carry out normal activity; minor signs or symptoms of disease 80 Normal activity with effort; some signs or symptoms of disease 70 Cares for self; unable to carry on normal activity or do active work 60 Requires occasional assistance, but is able to care for most of his/her needs 50 Requires considerable assistance and frequent medical care 40 Disabled; requires special care and assistance 30 20 Severely disabled; hospitalization is indicated although death not imminent Very sick; hospitalization necessary, active supportive treatment necessary 10 Moribund; fatal processes progressing rapidly 0 Dead 76
Performance status Karnofsky scale Description 100 Normal; no complaints; no evidence of disease 90 Able to carry out normal activity; minor signs or symptoms of disease 80 Normal activity with effort; some signs or symptoms of disease 70 Cares for self; unable to carry on normal activity or do active work 60 Requires occasional assistance, but is able to care for most of his/her needs 50 Requires considerable assistance and frequent medical care 40 Disabled; requires special care and assistance 30 20 Severely disabled; hospitalization is indicated although death not imminent Very sick; hospitalization necessary, active supportive treatment necessary 10 Moribund; fatal processes progressing rapidly 0 Dead 76
 Defining treatment • Tumor specific factors – TNM stage – Histology – Molecular features • Patient specific factors – Age – Performance status – Concomitant diseases – gender, etnicity, smoking Based on these factors multidisciplinary tumour board decides on curative-palliative therapy
Defining treatment • Tumor specific factors – TNM stage – Histology – Molecular features • Patient specific factors – Age – Performance status – Concomitant diseases – gender, etnicity, smoking Based on these factors multidisciplinary tumour board decides on curative-palliative therapy
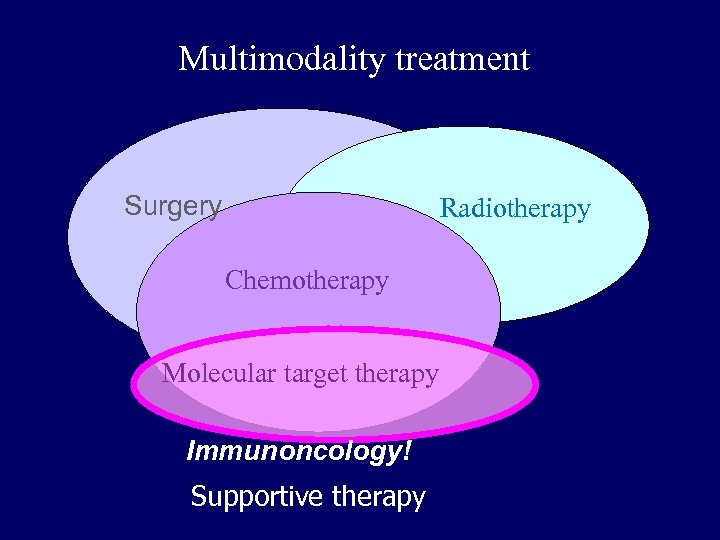 Multimodality treatment Surgery Radiotherapy Chemotherapy Molecular target therapy Immunoncology! Supportive therapy
Multimodality treatment Surgery Radiotherapy Chemotherapy Molecular target therapy Immunoncology! Supportive therapy
 Surgery • The type of surgical procedure depends on staging, the patient’s performance status, cardiopulmonal function and comorbidities. • The aim is radical resection • Sublobar resection may have a role in very early diseases. • Thoracotomy • Video assisted thoracoscopy (VATS) 79
Surgery • The type of surgical procedure depends on staging, the patient’s performance status, cardiopulmonal function and comorbidities. • The aim is radical resection • Sublobar resection may have a role in very early diseases. • Thoracotomy • Video assisted thoracoscopy (VATS) 79
 Surgery • Absolute contraindications: – haematogen metastases in the lungs – pleuritis carcinomatosa – III. b stage disease – multiplex distant metastases • Relative contraindications 80
Surgery • Absolute contraindications: – haematogen metastases in the lungs – pleuritis carcinomatosa – III. b stage disease – multiplex distant metastases • Relative contraindications 80
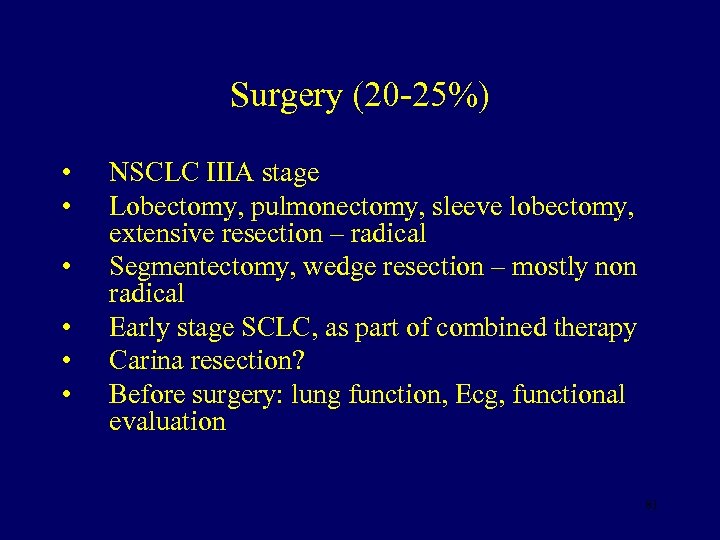 Surgery (20 -25%) • • • NSCLC IIIA stage Lobectomy, pulmonectomy, sleeve lobectomy, extensive resection – radical Segmentectomy, wedge resection – mostly non radical Early stage SCLC, as part of combined therapy Carina resection? Before surgery: lung function, Ecg, functional evaluation 81
Surgery (20 -25%) • • • NSCLC IIIA stage Lobectomy, pulmonectomy, sleeve lobectomy, extensive resection – radical Segmentectomy, wedge resection – mostly non radical Early stage SCLC, as part of combined therapy Carina resection? Before surgery: lung function, Ecg, functional evaluation 81
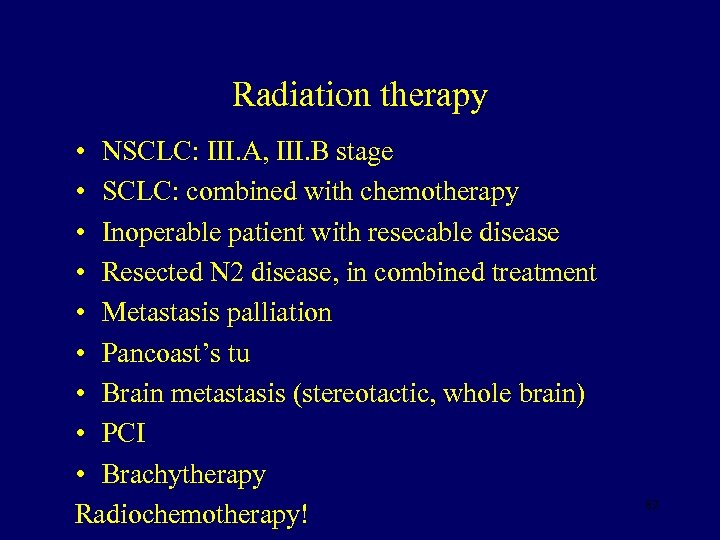 Radiation therapy • NSCLC: III. A, III. B stage • SCLC: combined with chemotherapy • Inoperable patient with resecable disease • Resected N 2 disease, in combined treatment • Metastasis palliation • Pancoast’s tu • Brain metastasis (stereotactic, whole brain) • PCI • Brachytherapy Radiochemotherapy! 82
Radiation therapy • NSCLC: III. A, III. B stage • SCLC: combined with chemotherapy • Inoperable patient with resecable disease • Resected N 2 disease, in combined treatment • Metastasis palliation • Pancoast’s tu • Brain metastasis (stereotactic, whole brain) • PCI • Brachytherapy Radiochemotherapy! 82
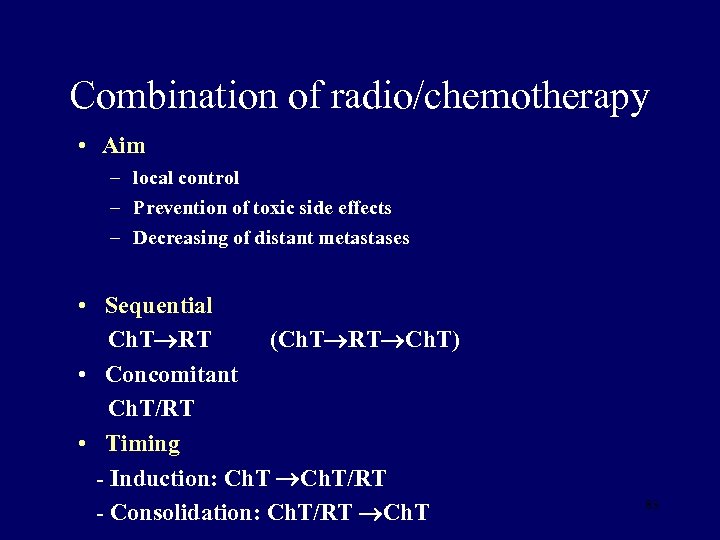 Combination of radio/chemotherapy • Aim – local control – Prevention of toxic side effects – Decreasing of distant metastases • Sequential Ch. T RT (Ch. T RT Ch. T) • Concomitant Ch. T/RT • Timing - Induction: Ch. T/RT - Consolidation: Ch. T/RT Ch. T 83
Combination of radio/chemotherapy • Aim – local control – Prevention of toxic side effects – Decreasing of distant metastases • Sequential Ch. T RT (Ch. T RT Ch. T) • Concomitant Ch. T/RT • Timing - Induction: Ch. T/RT - Consolidation: Ch. T/RT Ch. T 83
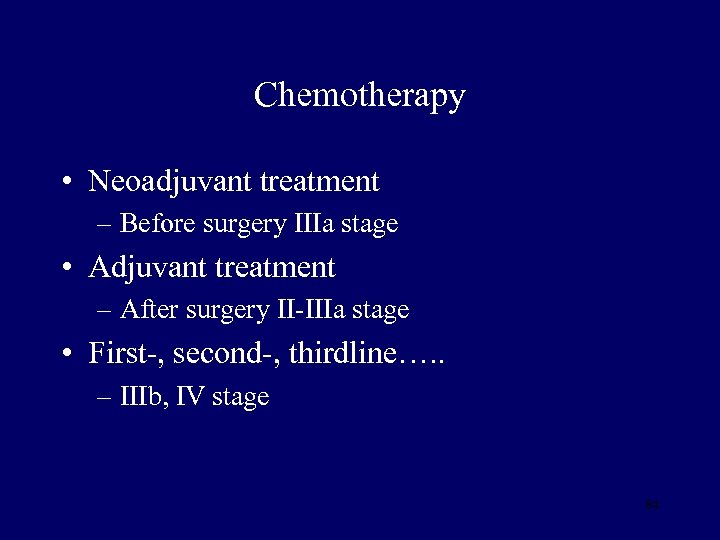 Chemotherapy • Neoadjuvant treatment – Before surgery IIIa stage • Adjuvant treatment – After surgery II-IIIa stage • First-, second-, thirdline…. . – IIIb, IV stage 84
Chemotherapy • Neoadjuvant treatment – Before surgery IIIa stage • Adjuvant treatment – After surgery II-IIIa stage • First-, second-, thirdline…. . – IIIb, IV stage 84
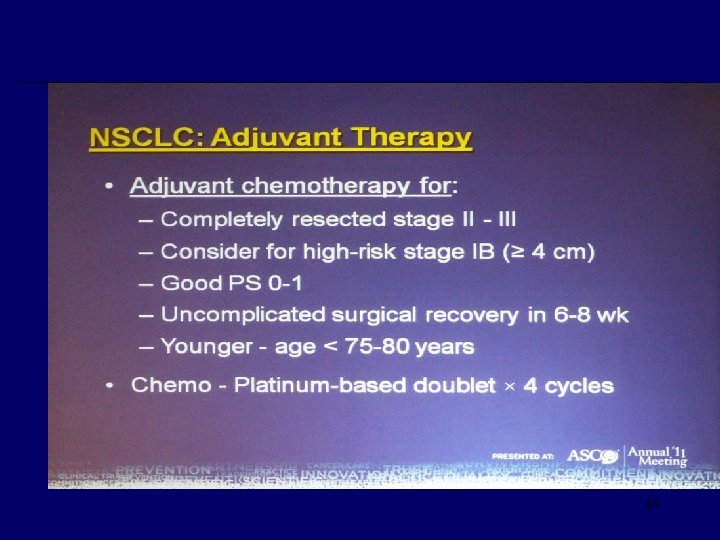 85
85
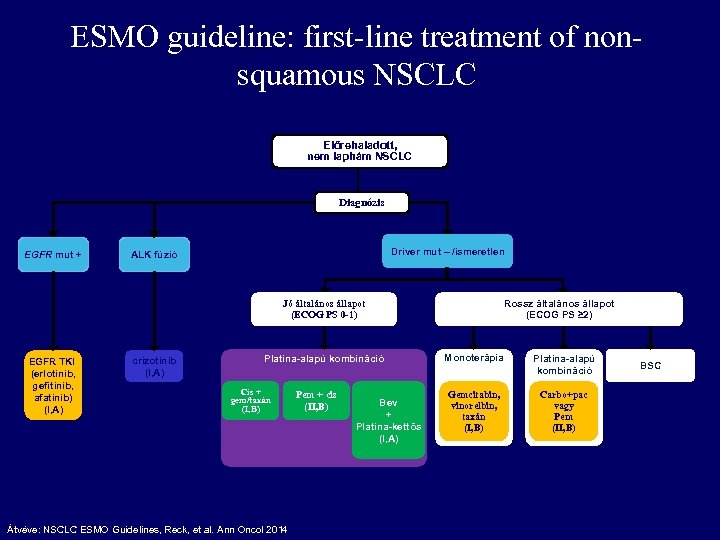 ESMO guideline: first-line treatment of nonsquamous NSCLC Előrehaladott, nem laphám NSCLC Diagnózis EGFR mut + Driver mut – /ismeretlen ALK fúzió Rossz általános állapot (ECOG PS ≥ 2) Jó általános állapot (ECOG PS 0 -1) EGFR TKI (erlotinib, gefitinib, afatinib) (I, A) crizotinib (I, A) Platina-alapú kombináció Cis + gem/taxán (I, B) Átvéve: NSCLC ESMO Guidelines, Reck, et al. Ann Oncol 2014 Pem + cis (II, B) Bev + Platina-kettős (I, A) Monoterápia Platina-alapú kombináció Gemcitabin, vinorelbin, taxán (I, B) Carbo+pac vagy Pem (II, B) BSC
ESMO guideline: first-line treatment of nonsquamous NSCLC Előrehaladott, nem laphám NSCLC Diagnózis EGFR mut + Driver mut – /ismeretlen ALK fúzió Rossz általános állapot (ECOG PS ≥ 2) Jó általános állapot (ECOG PS 0 -1) EGFR TKI (erlotinib, gefitinib, afatinib) (I, A) crizotinib (I, A) Platina-alapú kombináció Cis + gem/taxán (I, B) Átvéve: NSCLC ESMO Guidelines, Reck, et al. Ann Oncol 2014 Pem + cis (II, B) Bev + Platina-kettős (I, A) Monoterápia Platina-alapú kombináció Gemcitabin, vinorelbin, taxán (I, B) Carbo+pac vagy Pem (II, B) BSC
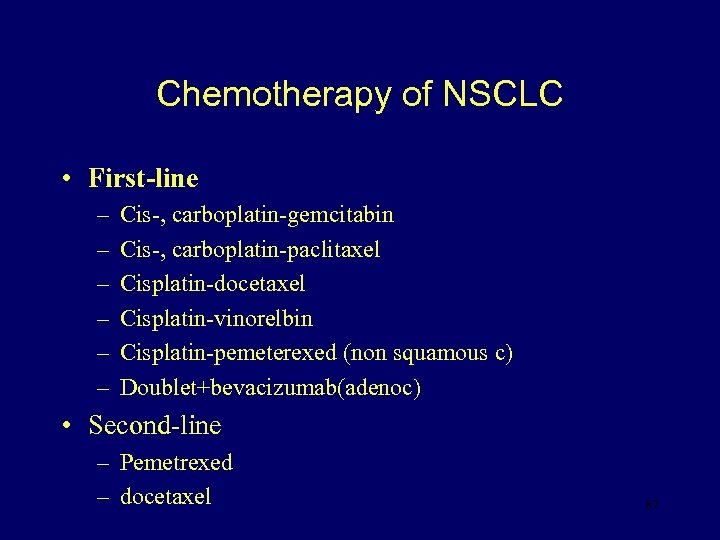 Chemotherapy of NSCLC • First-line – – – Cis-, carboplatin-gemcitabin Cis-, carboplatin-paclitaxel Cisplatin-docetaxel Cisplatin-vinorelbin Cisplatin-pemeterexed (non squamous c) Doublet+bevacizumab(adenoc) • Second-line – Pemetrexed – docetaxel 87
Chemotherapy of NSCLC • First-line – – – Cis-, carboplatin-gemcitabin Cis-, carboplatin-paclitaxel Cisplatin-docetaxel Cisplatin-vinorelbin Cisplatin-pemeterexed (non squamous c) Doublet+bevacizumab(adenoc) • Second-line – Pemetrexed – docetaxel 87
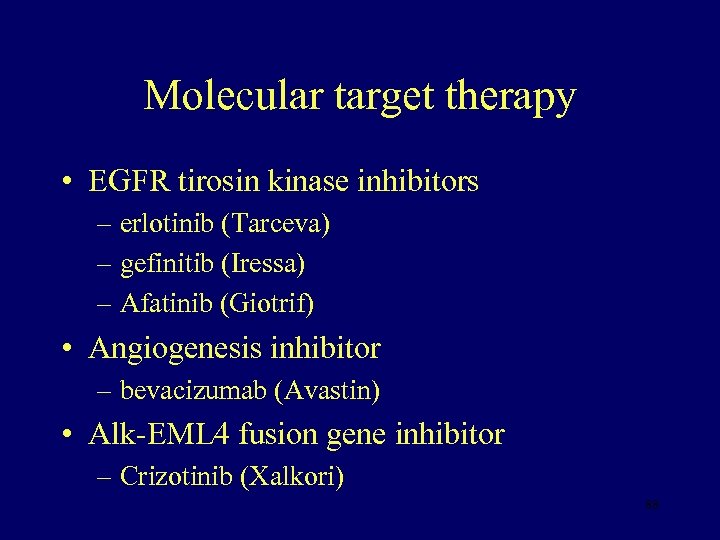 Molecular target therapy • EGFR tirosin kinase inhibitors – erlotinib (Tarceva) – gefinitib (Iressa) – Afatinib (Giotrif) • Angiogenesis inhibitor – bevacizumab (Avastin) • Alk-EML 4 fusion gene inhibitor – Crizotinib (Xalkori) 88
Molecular target therapy • EGFR tirosin kinase inhibitors – erlotinib (Tarceva) – gefinitib (Iressa) – Afatinib (Giotrif) • Angiogenesis inhibitor – bevacizumab (Avastin) • Alk-EML 4 fusion gene inhibitor – Crizotinib (Xalkori) 88
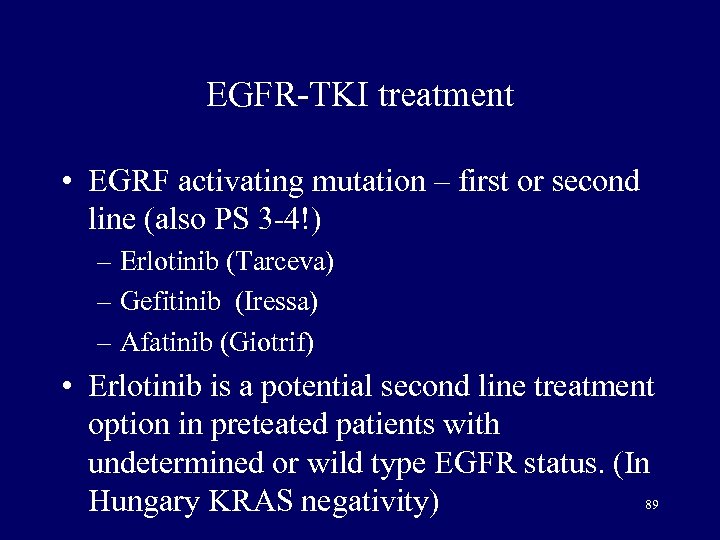 EGFR-TKI treatment • EGRF activating mutation – first or second line (also PS 3 -4!) – Erlotinib (Tarceva) – Gefitinib (Iressa) – Afatinib (Giotrif) • Erlotinib is a potential second line treatment option in preteated patients with undetermined or wild type EGFR status. (In 89 Hungary KRAS negativity)
EGFR-TKI treatment • EGRF activating mutation – first or second line (also PS 3 -4!) – Erlotinib (Tarceva) – Gefitinib (Iressa) – Afatinib (Giotrif) • Erlotinib is a potential second line treatment option in preteated patients with undetermined or wild type EGFR status. (In 89 Hungary KRAS negativity)
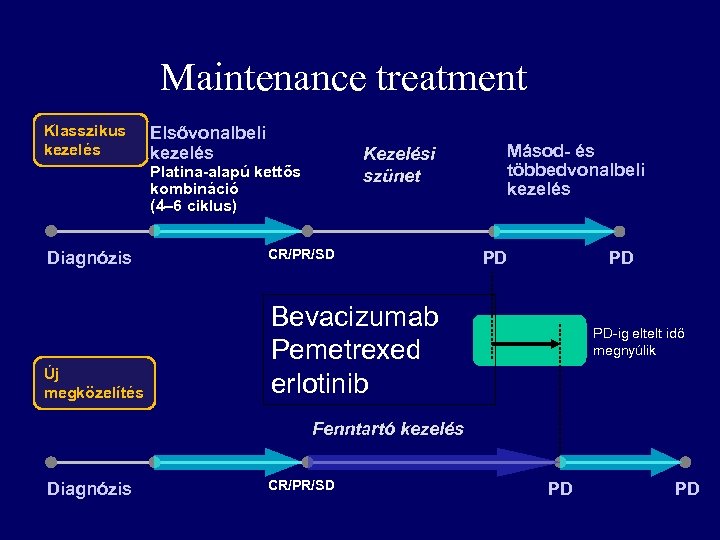 Maintenance treatment Klasszikus kezelés Elsővonalbeli kezelés Kezelési szünet Platina-alapú kettős kombináció (4– 6 ciklus) Diagnózis CR/PR/SD Új megközelítés Másod- és többedvonalbeli kezelés Bevacizumab Pemetrexed erlotinib PD PD PD-ig eltelt idő megnyúlik Fenntartó kezelés Diagnózis CR/PR/SD PD PD
Maintenance treatment Klasszikus kezelés Elsővonalbeli kezelés Kezelési szünet Platina-alapú kettős kombináció (4– 6 ciklus) Diagnózis CR/PR/SD Új megközelítés Másod- és többedvonalbeli kezelés Bevacizumab Pemetrexed erlotinib PD PD PD-ig eltelt idő megnyúlik Fenntartó kezelés Diagnózis CR/PR/SD PD PD
 Immuntherapy • Immun check point inhibitors – PD-1 and PDL-1 inhibitors • Nivolumab: Opdivo – 2. and 3. line • Pembrolizumab: Keytruda – 2. line 91
Immuntherapy • Immun check point inhibitors – PD-1 and PDL-1 inhibitors • Nivolumab: Opdivo – 2. and 3. line • Pembrolizumab: Keytruda – 2. line 91
 Surgery in SCLC • I/A-I/B: resection • Postoperative chemotherapy • Adjuvant irradiation in positive node status • Induction chemotherapy
Surgery in SCLC • I/A-I/B: resection • Postoperative chemotherapy • Adjuvant irradiation in positive node status • Induction chemotherapy
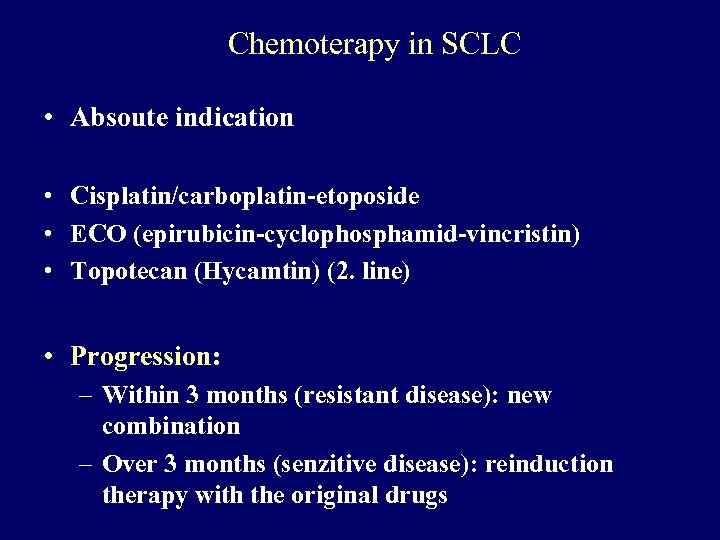 Chemoterapy in SCLC • Absoute indication • Cisplatin/carboplatin-etoposide • ECO (epirubicin-cyclophosphamid-vincristin) • Topotecan (Hycamtin) (2. line) • Progression: – Within 3 months (resistant disease): new combination – Over 3 months (senzitive disease): reinduction therapy with the original drugs
Chemoterapy in SCLC • Absoute indication • Cisplatin/carboplatin-etoposide • ECO (epirubicin-cyclophosphamid-vincristin) • Topotecan (Hycamtin) (2. line) • Progression: – Within 3 months (resistant disease): new combination – Over 3 months (senzitive disease): reinduction therapy with the original drugs
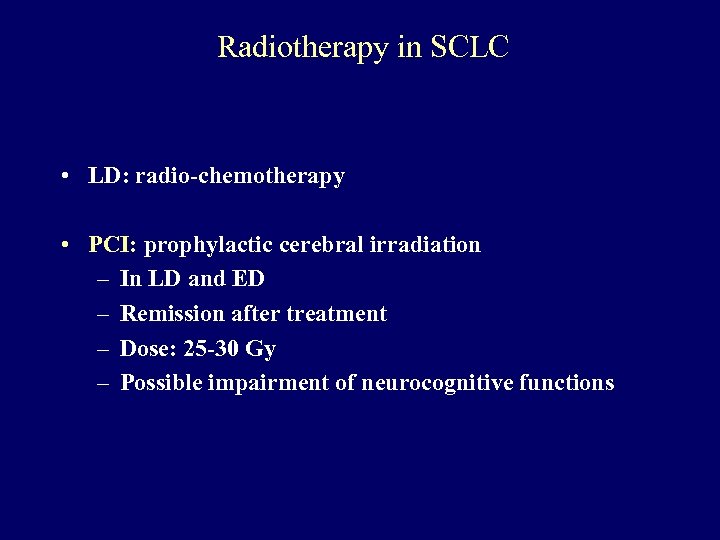 Radiotherapy in SCLC • LD: radio-chemotherapy • PCI: prophylactic cerebral irradiation – In LD and ED – Remission after treatment – Dose: 25 -30 Gy – Possible impairment of neurocognitive functions
Radiotherapy in SCLC • LD: radio-chemotherapy • PCI: prophylactic cerebral irradiation – In LD and ED – Remission after treatment – Dose: 25 -30 Gy – Possible impairment of neurocognitive functions
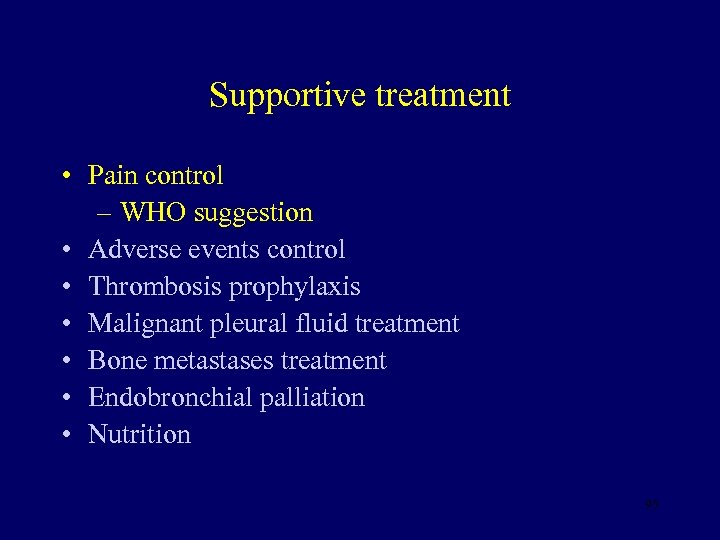 Supportive treatment • Pain control – WHO suggestion • Adverse events control • Thrombosis prophylaxis • Malignant pleural fluid treatment • Bone metastases treatment • Endobronchial palliation • Nutrition 95
Supportive treatment • Pain control – WHO suggestion • Adverse events control • Thrombosis prophylaxis • Malignant pleural fluid treatment • Bone metastases treatment • Endobronchial palliation • Nutrition 95
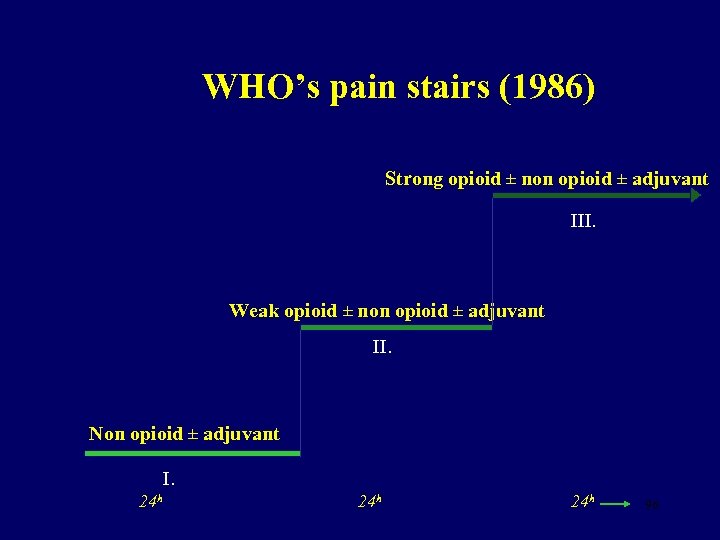 WHO’s pain stairs (1986) Strong opioid ± non opioid ± adjuvant III. Weak opioid ± non opioid ± adjuvant II. Non opioid ± adjuvant I. 24 h 24 h 96
WHO’s pain stairs (1986) Strong opioid ± non opioid ± adjuvant III. Weak opioid ± non opioid ± adjuvant II. Non opioid ± adjuvant I. 24 h 24 h 96
 Supportive treatment • Pain control • Adverse events control – febrile neutopenia – Anaemia (erythropoetin) – Nausea, vomiting • Thrombosis prophylaxis • Malignant pleural fluid treatment – pleurodesis • Bone metastases treatment – bisphonat • Endobronchial palliation 97
Supportive treatment • Pain control • Adverse events control – febrile neutopenia – Anaemia (erythropoetin) – Nausea, vomiting • Thrombosis prophylaxis • Malignant pleural fluid treatment – pleurodesis • Bone metastases treatment – bisphonat • Endobronchial palliation 97
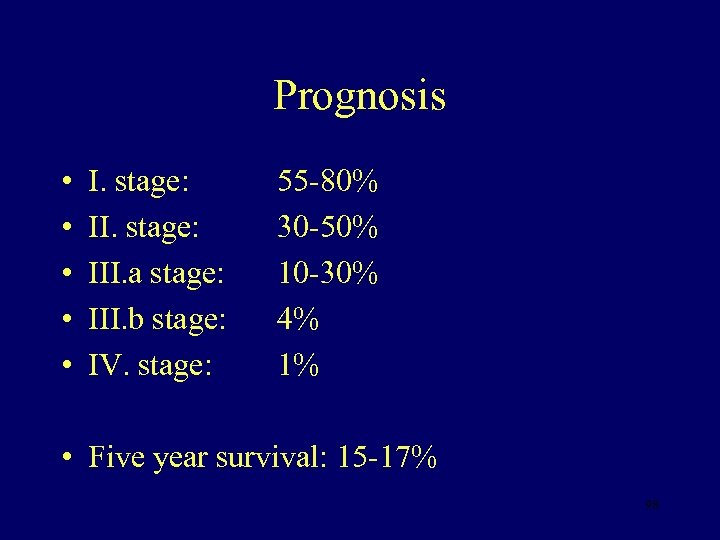 Prognosis • • • I. stage: III. a stage: III. b stage: IV. stage: 55 -80% 30 -50% 10 -30% 4% 1% • Five year survival: 15 -17% 98
Prognosis • • • I. stage: III. a stage: III. b stage: IV. stage: 55 -80% 30 -50% 10 -30% 4% 1% • Five year survival: 15 -17% 98
 Prevention • Primary – Smoking sessation • Secundary – Screening • X-ray • LDCT 99
Prevention • Primary – Smoking sessation • Secundary – Screening • X-ray • LDCT 99
 Thank you for your attention!
Thank you for your attention!


