патологии пародонта.агрессивные формы.ppt
- Количество слайдов: 44
 Early Onset Periodontitis: Juvenile Periodontitis: Locally Aggressive Periodontitis Vincent Steniger
Early Onset Periodontitis: Juvenile Periodontitis: Locally Aggressive Periodontitis Vincent Steniger
 Remember l Periodontal Disease (mainly gingivitis) is the most common dental disease and is responsible for most tooth loss l 80% of American adults have some form of periodontal disease mainly gingivitis
Remember l Periodontal Disease (mainly gingivitis) is the most common dental disease and is responsible for most tooth loss l 80% of American adults have some form of periodontal disease mainly gingivitis
 The Basics l Periodontal Disease: – Gingivitis – Periodontitis Periodontal literally means “around the tooth” l What Happens? l – Chronic bacterial infection leading to an inflammatory response of the gingival tissue and eventually (but not definitely) the periodontium l Remember: – Not all cases of gingivitis will lead to Periodontitis – We were taught that Periodontitis cannot exist without Gingivitis is this correct? – Affect one tooth or many
The Basics l Periodontal Disease: – Gingivitis – Periodontitis Periodontal literally means “around the tooth” l What Happens? l – Chronic bacterial infection leading to an inflammatory response of the gingival tissue and eventually (but not definitely) the periodontium l Remember: – Not all cases of gingivitis will lead to Periodontitis – We were taught that Periodontitis cannot exist without Gingivitis is this correct? – Affect one tooth or many
 Types of Periodontal Diseases 1. 2. 3. 4. 5. 6. Gingivitis due to local factors Gingivitis due to systemic factors Gingivitis due to pharmacology Chronic Periodontitis Early Onset (Juvenile Periodontitis) Others: 1. 2. 3. ANUG ANUP …
Types of Periodontal Diseases 1. 2. 3. 4. 5. 6. Gingivitis due to local factors Gingivitis due to systemic factors Gingivitis due to pharmacology Chronic Periodontitis Early Onset (Juvenile Periodontitis) Others: 1. 2. 3. ANUG ANUP …
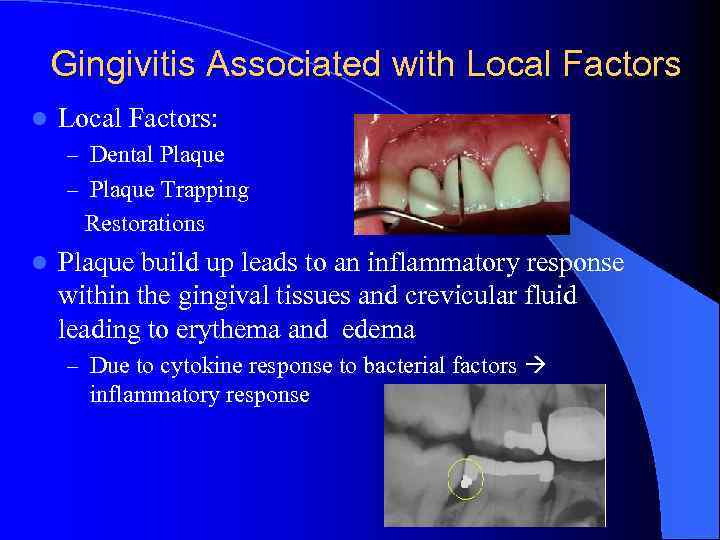 Gingivitis Associated with Local Factors l Local Factors: – Dental Plaque – Plaque Trapping Restorations l Plaque build up leads to an inflammatory response within the gingival tissues and crevicular fluid leading to erythema and edema – Due to cytokine response to bacterial factors inflammatory response
Gingivitis Associated with Local Factors l Local Factors: – Dental Plaque – Plaque Trapping Restorations l Plaque build up leads to an inflammatory response within the gingival tissues and crevicular fluid leading to erythema and edema – Due to cytokine response to bacterial factors inflammatory response
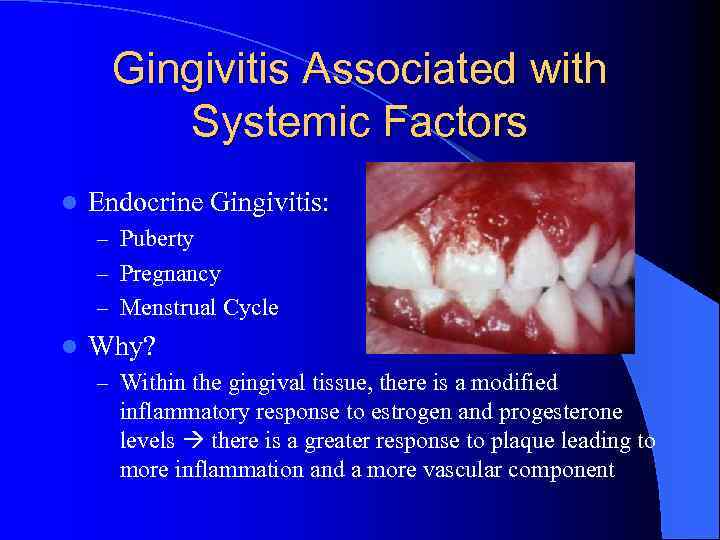 Gingivitis Associated with Systemic Factors l Endocrine Gingivitis: – Puberty – Pregnancy – Menstrual Cycle l Why? – Within the gingival tissue, there is a modified inflammatory response to estrogen and progesterone levels there is a greater response to plaque leading to more inflammation and a more vascular component
Gingivitis Associated with Systemic Factors l Endocrine Gingivitis: – Puberty – Pregnancy – Menstrual Cycle l Why? – Within the gingival tissue, there is a modified inflammatory response to estrogen and progesterone levels there is a greater response to plaque leading to more inflammation and a more vascular component
 Gingivitis Associated with Systemic Factors- Continued l Gingivitis Associated with: – Diabetes: l It is known that poor diabetic control leads to an increase in gingivitis and periodontitis as well as gingivitis and periodontitis being associated with poor diabetic control and elevated blood glucose levels – Leukemia: l l Common to see facial echymosis Common to see hypertrophic gingiva with and gingival hemorrhage
Gingivitis Associated with Systemic Factors- Continued l Gingivitis Associated with: – Diabetes: l It is known that poor diabetic control leads to an increase in gingivitis and periodontitis as well as gingivitis and periodontitis being associated with poor diabetic control and elevated blood glucose levels – Leukemia: l l Common to see facial echymosis Common to see hypertrophic gingiva with and gingival hemorrhage
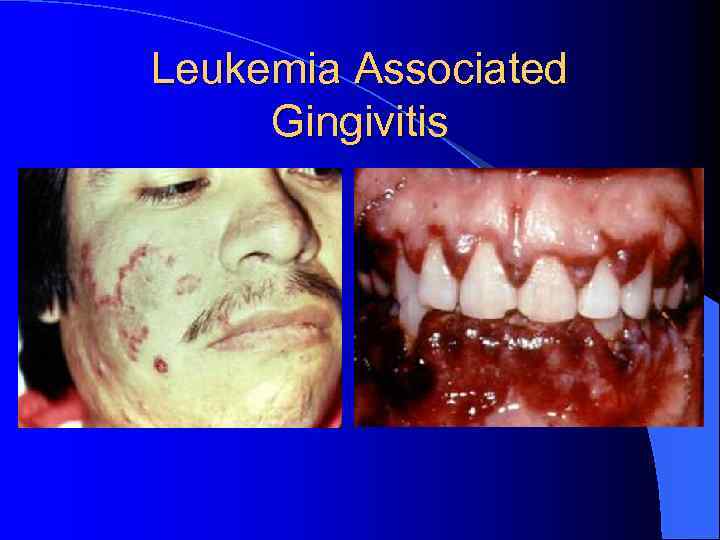 Leukemia Associated Gingivitis
Leukemia Associated Gingivitis
 Gingivitis Associated with Pharmacology l Drugs known to cause gingival inflammation: – Dilantin (Phenytoin) – Calcium Channel Blockers – Cyclosporin
Gingivitis Associated with Pharmacology l Drugs known to cause gingival inflammation: – Dilantin (Phenytoin) – Calcium Channel Blockers – Cyclosporin
 Gingivitis Associated with Pharmacology- Continued l Phenytoin induced gingival hyperplasia – Leads to pseudopocketing increased probing depth due to gingival hypertrophy, no due to bone loss – Occurs in 3 85% of those taking medication – Most likely due to increased platelet derived growth factor l Calcium Channel Blockers: – Causes gingival hypertrophy in 25 -50% of those on it l Cyclosporin: – Causes gingival hypertrophy in 30%
Gingivitis Associated with Pharmacology- Continued l Phenytoin induced gingival hyperplasia – Leads to pseudopocketing increased probing depth due to gingival hypertrophy, no due to bone loss – Occurs in 3 85% of those taking medication – Most likely due to increased platelet derived growth factor l Calcium Channel Blockers: – Causes gingival hypertrophy in 25 -50% of those on it l Cyclosporin: – Causes gingival hypertrophy in 30%
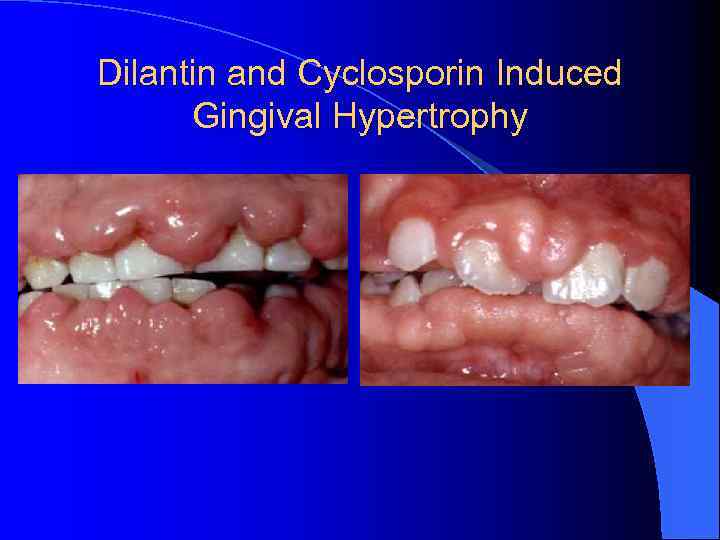 Dilantin and Cyclosporin Induced Gingival Hypertrophy
Dilantin and Cyclosporin Induced Gingival Hypertrophy
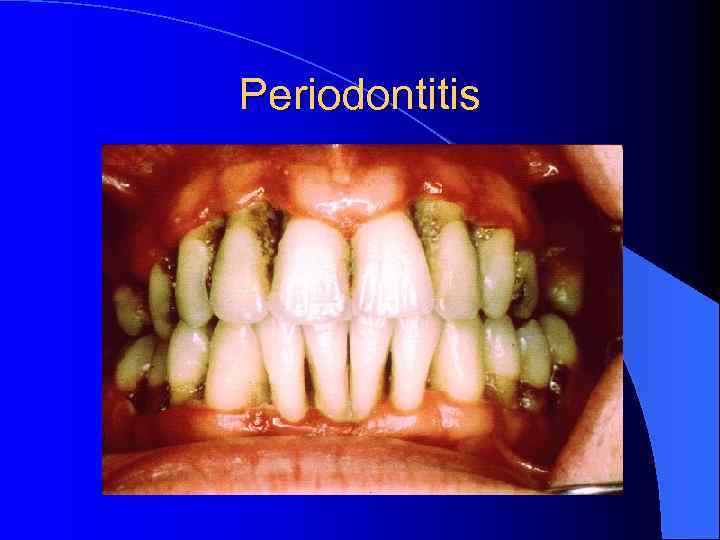 Periodontitis
Periodontitis
 Chronic Periodontitis Slowly progressive destruction of bone leading to loss of attachment l Untreated plaque leads to calcium deposition from sulcular fluid and saliva leading to: l – Supragingival Calculus: Ca from saliva – Subgingival Calculus: Ca from crevicular fluid Calculus leads to increased ability of bacteria to attach means more bacteria inflammatory response bone destruction l DEPENDANT ON LOCAL FACTORS! l
Chronic Periodontitis Slowly progressive destruction of bone leading to loss of attachment l Untreated plaque leads to calcium deposition from sulcular fluid and saliva leading to: l – Supragingival Calculus: Ca from saliva – Subgingival Calculus: Ca from crevicular fluid Calculus leads to increased ability of bacteria to attach means more bacteria inflammatory response bone destruction l DEPENDANT ON LOCAL FACTORS! l
 Chronic Periodontitis. Continued l Chronic periodontitis progresses at a rate of. 2 to. 5 mm bone loss per year l Commonly see horizontal and vertical bone loss: – Horizontal bone loss is on equally from CEJ to CEJ of adjacent teeth – Vertical crestal bone height is higher than pocket depth
Chronic Periodontitis. Continued l Chronic periodontitis progresses at a rate of. 2 to. 5 mm bone loss per year l Commonly see horizontal and vertical bone loss: – Horizontal bone loss is on equally from CEJ to CEJ of adjacent teeth – Vertical crestal bone height is higher than pocket depth
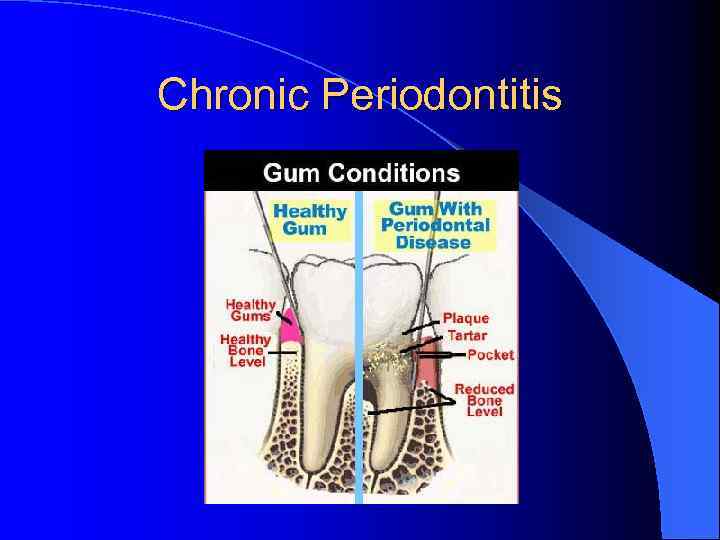 Chronic Periodontitis
Chronic Periodontitis
 Localized Aggressive Periodontitis: Formerly Juvenile Periodontitis: DEFINED… l Localized Juvenile Periodontitis LJP is defined as “severe attachment and bone loss around the first molars and incisors (but not involving more than two additional nonfirst molar/incisor teeth), which occurs between the ages of 12 to 26 years. ”
Localized Aggressive Periodontitis: Formerly Juvenile Periodontitis: DEFINED… l Localized Juvenile Periodontitis LJP is defined as “severe attachment and bone loss around the first molars and incisors (but not involving more than two additional nonfirst molar/incisor teeth), which occurs between the ages of 12 to 26 years. ”
 LAP: Epidemiology l Overall Prevalence: 0. 53% l 21 times more likely to be seen in African Americans than whites: l Prevalence in Hispanics: 1. 7%
LAP: Epidemiology l Overall Prevalence: 0. 53% l 21 times more likely to be seen in African Americans than whites: l Prevalence in Hispanics: 1. 7%
 LAP Patients will/may have bone loss, and possibly tooth loss by age 20. l Defective PMNs l LAP occurs in healthy adolescents: – Colonization of Actinobacillus actinomycetemcomitans – Minor inflammation of the gingival tissues – The disease is detected by periodontal probing or xrays, which show localized, deep (vertical) bone loss, commonly limited to the first molars and incisors. – Bone loss progresses faster than in adult periodontitis, often at a rate of 3 to 4 μm/day. l
LAP Patients will/may have bone loss, and possibly tooth loss by age 20. l Defective PMNs l LAP occurs in healthy adolescents: – Colonization of Actinobacillus actinomycetemcomitans – Minor inflammation of the gingival tissues – The disease is detected by periodontal probing or xrays, which show localized, deep (vertical) bone loss, commonly limited to the first molars and incisors. – Bone loss progresses faster than in adult periodontitis, often at a rate of 3 to 4 μm/day. l
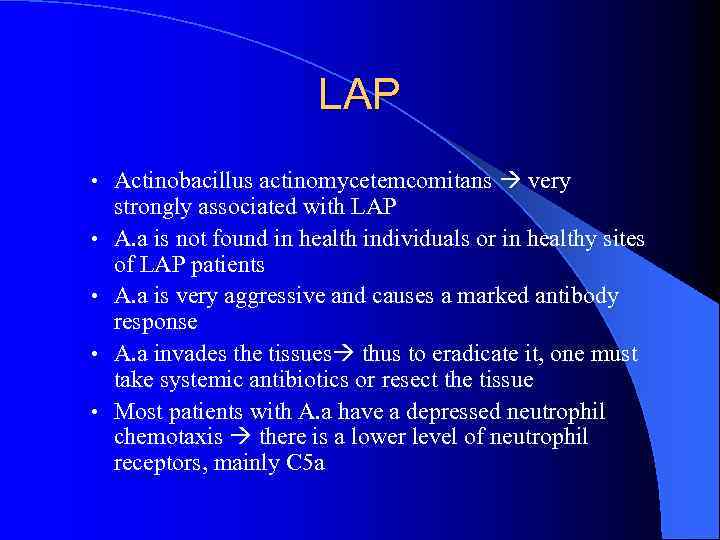 LAP • Actinobacillus actinomycetemcomitans very • • strongly associated with LAP A. a is not found in health individuals or in healthy sites of LAP patients A. a is very aggressive and causes a marked antibody response A. a invades the tissues thus to eradicate it, one must take systemic antibiotics or resect the tissue Most patients with A. a have a depressed neutrophil chemotaxis there is a lower level of neutrophil receptors, mainly C 5 a
LAP • Actinobacillus actinomycetemcomitans very • • strongly associated with LAP A. a is not found in health individuals or in healthy sites of LAP patients A. a is very aggressive and causes a marked antibody response A. a invades the tissues thus to eradicate it, one must take systemic antibiotics or resect the tissue Most patients with A. a have a depressed neutrophil chemotaxis there is a lower level of neutrophil receptors, mainly C 5 a
 LAP l Clinical Features of LAP: – Localized first molar/incisor presentation LOA on at least two permanent teeth, one of which is a first molar, and involving no more than two teeth other than first molars and incisors – Detected at ages 10 -15 – Dx made when 3 sites have CAL of 5 mm or greater – Plaque and Calculus may be absent
LAP l Clinical Features of LAP: – Localized first molar/incisor presentation LOA on at least two permanent teeth, one of which is a first molar, and involving no more than two teeth other than first molars and incisors – Detected at ages 10 -15 – Dx made when 3 sites have CAL of 5 mm or greater – Plaque and Calculus may be absent
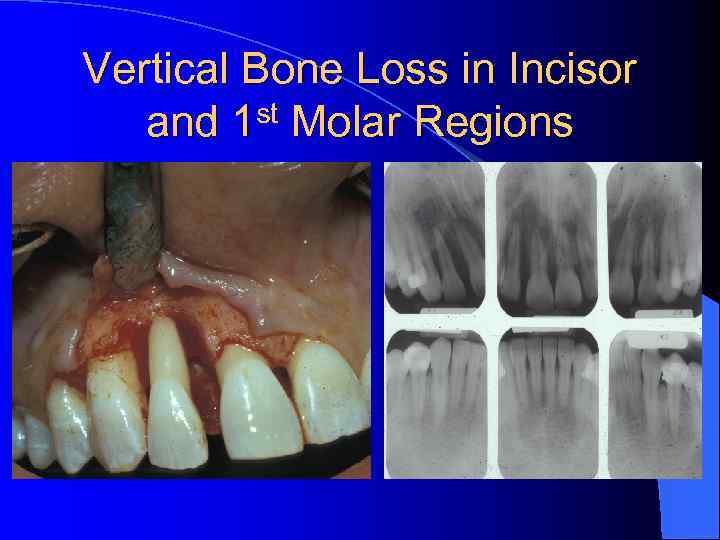 Vertical Bone Loss in Incisor and 1 st Molar Regions
Vertical Bone Loss in Incisor and 1 st Molar Regions

 LAP Pathogenesis l Disease is based on 3 factors: – Bacteria (certain kind) – Host response – Possibly genes Bacteria: A. a l Host Response: Impaired PMNs (phagocytosis, chemotaxis and decreased receptors) l Genes: may be AD inheritance l
LAP Pathogenesis l Disease is based on 3 factors: – Bacteria (certain kind) – Host response – Possibly genes Bacteria: A. a l Host Response: Impaired PMNs (phagocytosis, chemotaxis and decreased receptors) l Genes: may be AD inheritance l
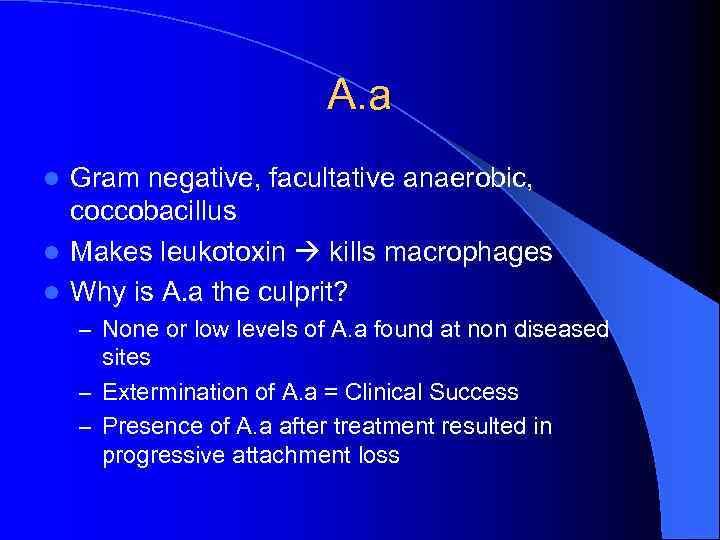 A. a Gram negative, facultative anaerobic, coccobacillus l Makes leukotoxin kills macrophages l Why is A. a the culprit? l – None or low levels of A. a found at non diseased sites – Extermination of A. a = Clinical Success – Presence of A. a after treatment resulted in progressive attachment loss
A. a Gram negative, facultative anaerobic, coccobacillus l Makes leukotoxin kills macrophages l Why is A. a the culprit? l – None or low levels of A. a found at non diseased sites – Extermination of A. a = Clinical Success – Presence of A. a after treatment resulted in progressive attachment loss
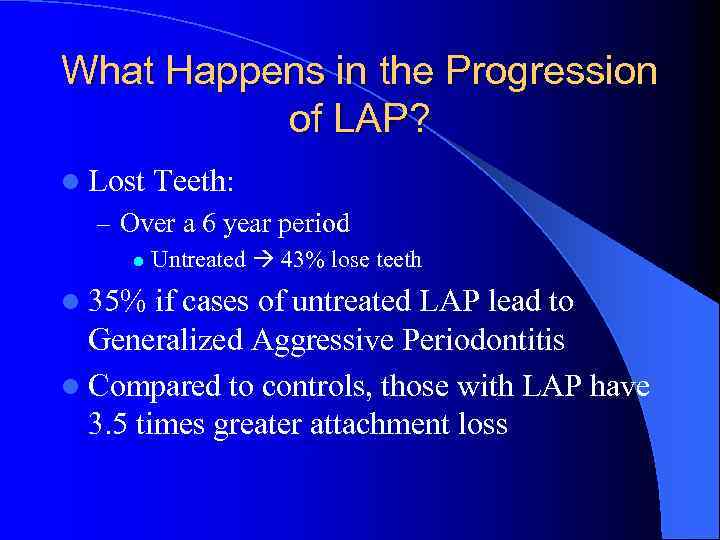 What Happens in the Progression of LAP? l Lost Teeth: – Over a 6 year period l l 35% Untreated 43% lose teeth if cases of untreated LAP lead to Generalized Aggressive Periodontitis l Compared to controls, those with LAP have 3. 5 times greater attachment loss
What Happens in the Progression of LAP? l Lost Teeth: – Over a 6 year period l l 35% Untreated 43% lose teeth if cases of untreated LAP lead to Generalized Aggressive Periodontitis l Compared to controls, those with LAP have 3. 5 times greater attachment loss
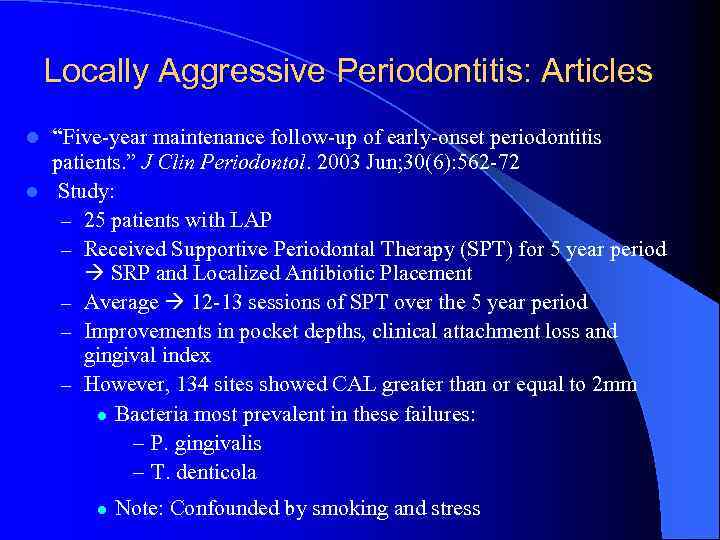 Locally Aggressive Periodontitis: Articles l “Five-year maintenance follow-up of early-onset periodontitis patients. ” J Clin Periodontol. 2003 Jun; 30(6): 562 -72 l Study: – 25 patients with LAP – Received Supportive Periodontal Therapy (SPT) for 5 year period SRP and Localized Antibiotic Placement – Average 12 -13 sessions of SPT over the 5 year period – Improvements in pocket depths, clinical attachment loss and gingival index – However, 134 sites showed CAL greater than or equal to 2 mm l Bacteria most prevalent in these failures: – P. gingivalis – T. denticola l Note: Confounded by smoking and stress
Locally Aggressive Periodontitis: Articles l “Five-year maintenance follow-up of early-onset periodontitis patients. ” J Clin Periodontol. 2003 Jun; 30(6): 562 -72 l Study: – 25 patients with LAP – Received Supportive Periodontal Therapy (SPT) for 5 year period SRP and Localized Antibiotic Placement – Average 12 -13 sessions of SPT over the 5 year period – Improvements in pocket depths, clinical attachment loss and gingival index – However, 134 sites showed CAL greater than or equal to 2 mm l Bacteria most prevalent in these failures: – P. gingivalis – T. denticola l Note: Confounded by smoking and stress
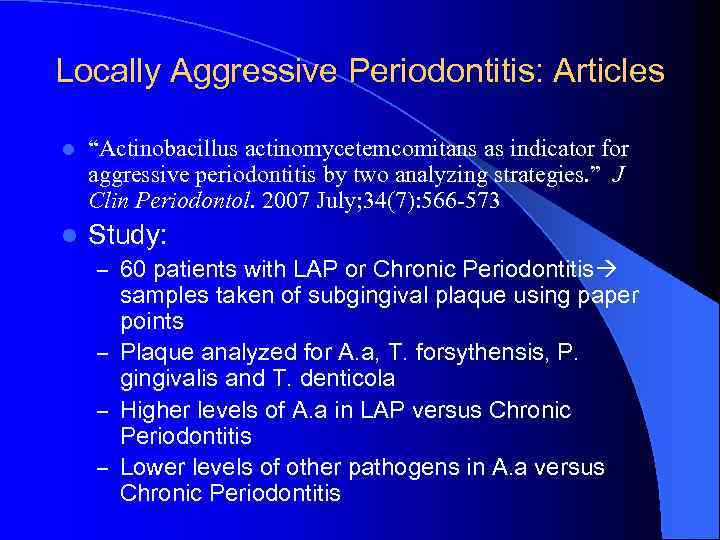 Locally Aggressive Periodontitis: Articles l “Actinobacillus actinomycetemcomitans as indicator for aggressive periodontitis by two analyzing strategies. ” J Clin Periodontol. 2007 July; 34(7): 566 -573 l Study: – 60 patients with LAP or Chronic Periodontitis samples taken of subgingival plaque using paper points – Plaque analyzed for A. a, T. forsythensis, P. gingivalis and T. denticola – Higher levels of A. a in LAP versus Chronic Periodontitis – Lower levels of other pathogens in A. a versus Chronic Periodontitis
Locally Aggressive Periodontitis: Articles l “Actinobacillus actinomycetemcomitans as indicator for aggressive periodontitis by two analyzing strategies. ” J Clin Periodontol. 2007 July; 34(7): 566 -573 l Study: – 60 patients with LAP or Chronic Periodontitis samples taken of subgingival plaque using paper points – Plaque analyzed for A. a, T. forsythensis, P. gingivalis and T. denticola – Higher levels of A. a in LAP versus Chronic Periodontitis – Lower levels of other pathogens in A. a versus Chronic Periodontitis
 Locally Aggressive Periodontitis: Articles “Comparative evaluation of surgical and conservative treatment modalities of juvenile periodontitis patients. ” Afr J Med Sci. 2001 Dec; 30(4): 313 -8. l Study: – 12 patients, 6 mon longitudinal study – Split mouth tx: l 1 side conservative l 1 side surgical and antibiotic therapy l Look at mobility and CAL l Use SRP and systemic antibiotic use – “It was therefore concluded that surgical debridement with systemic administration of tetracycline is more effective than the conservative technique in the treatment of juvenile periodontitis, although both gave improvement” l
Locally Aggressive Periodontitis: Articles “Comparative evaluation of surgical and conservative treatment modalities of juvenile periodontitis patients. ” Afr J Med Sci. 2001 Dec; 30(4): 313 -8. l Study: – 12 patients, 6 mon longitudinal study – Split mouth tx: l 1 side conservative l 1 side surgical and antibiotic therapy l Look at mobility and CAL l Use SRP and systemic antibiotic use – “It was therefore concluded that surgical debridement with systemic administration of tetracycline is more effective than the conservative technique in the treatment of juvenile periodontitis, although both gave improvement” l
 Treatment of LAP l Keep in mind: – In order to control the disease, A. a must be minimized – SRP NEVER removes 100% of bacteria – Without maintenance, disease will proceed – Disease has a high recurrence rate after first year therapy
Treatment of LAP l Keep in mind: – In order to control the disease, A. a must be minimized – SRP NEVER removes 100% of bacteria – Without maintenance, disease will proceed – Disease has a high recurrence rate after first year therapy
 Treatment of LAP: continued SRP and Good OH will not eliminate A. a l Subgingival gels, irrigation and antibiotics will not eliminate A. a l Best Bet: l – Systemic Antibiotics – Surgery to remove granulation tissue in which A. a fester l Antibiotics: – Flagyl/Metronidazole and Amoxicillin
Treatment of LAP: continued SRP and Good OH will not eliminate A. a l Subgingival gels, irrigation and antibiotics will not eliminate A. a l Best Bet: l – Systemic Antibiotics – Surgery to remove granulation tissue in which A. a fester l Antibiotics: – Flagyl/Metronidazole and Amoxicillin
 Treatment of LAP: Sequencing 1 l l l OHI, patient education Gross calculus debridement if indicated Surgical treatment of pockets > 5 mm, root planing and curettage of pockets < 5 mm. Chlorhexidine 1 -2 weeks post Surgery and interproximal brushing Antibiotic therapy concurrent with surgery and/or root planning Post surgery evaluation 4 -6 weeks: success measured by good OH, decreased pockets, no BOP, gain in attachment
Treatment of LAP: Sequencing 1 l l l OHI, patient education Gross calculus debridement if indicated Surgical treatment of pockets > 5 mm, root planing and curettage of pockets < 5 mm. Chlorhexidine 1 -2 weeks post Surgery and interproximal brushing Antibiotic therapy concurrent with surgery and/or root planning Post surgery evaluation 4 -6 weeks: success measured by good OH, decreased pockets, no BOP, gain in attachment
 Treatment of LAP: Sequencing 2 l Retreatment of deep, bleeding pockets l Maintenance every 3 months l Radiographs as needed l Reinforce OH l Prophylaxis/RP
Treatment of LAP: Sequencing 2 l Retreatment of deep, bleeding pockets l Maintenance every 3 months l Radiographs as needed l Reinforce OH l Prophylaxis/RP
 LAP: Differential Diagnosis l LAP l Leukemia l Neutropenia l Langerhan’s Cell Disease
LAP: Differential Diagnosis l LAP l Leukemia l Neutropenia l Langerhan’s Cell Disease
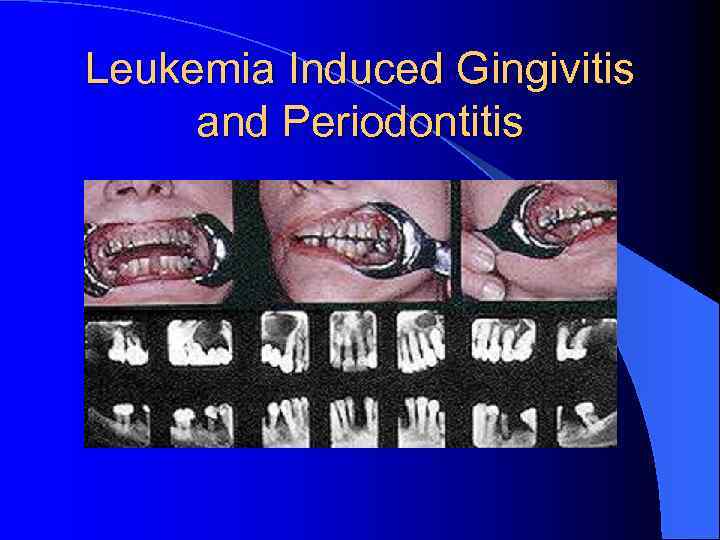 Leukemia Induced Gingivitis and Periodontitis
Leukemia Induced Gingivitis and Periodontitis
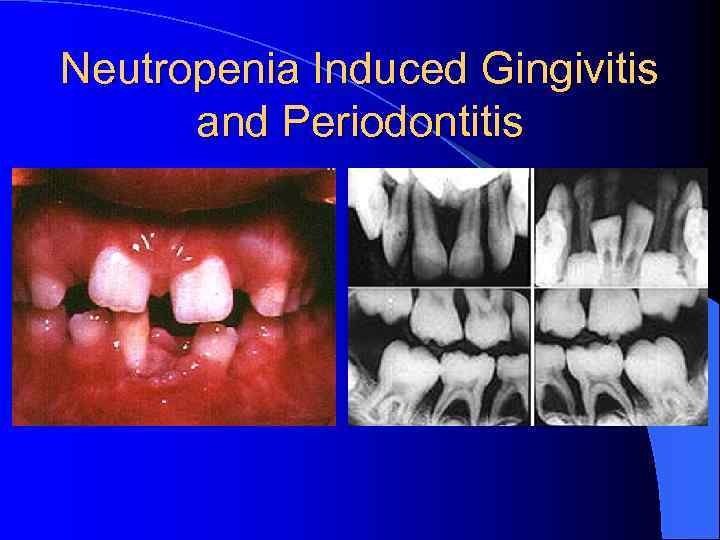 Neutropenia Induced Gingivitis and Periodontitis
Neutropenia Induced Gingivitis and Periodontitis
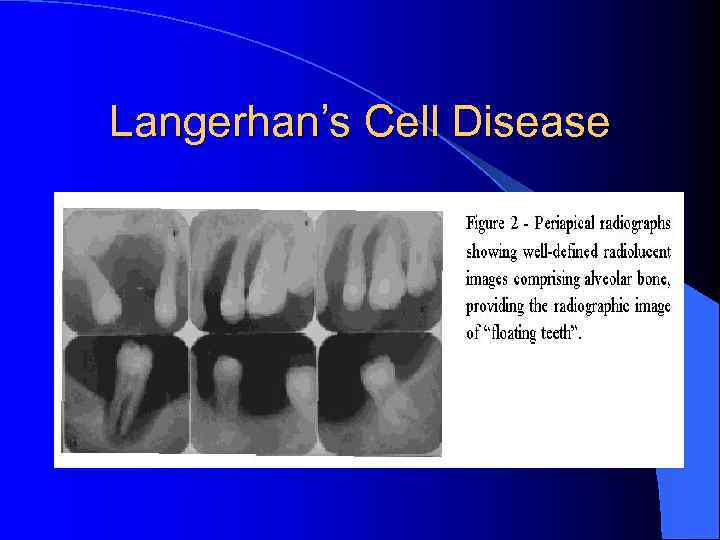 Langerhan’s Cell Disease
Langerhan’s Cell Disease
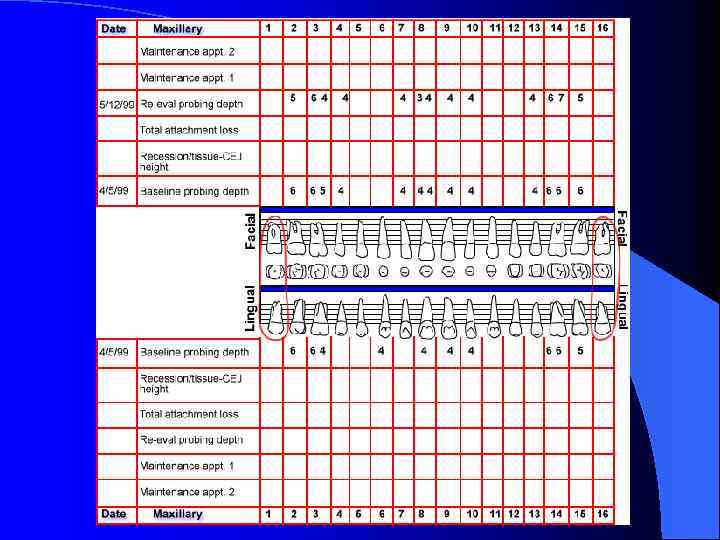
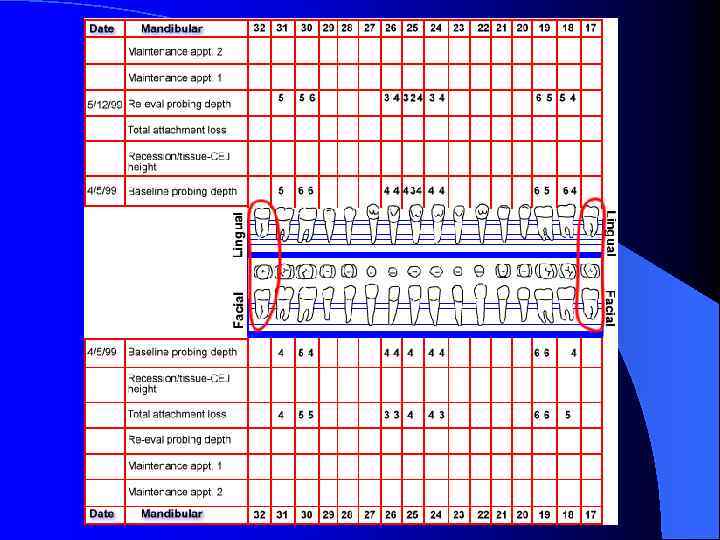
 Case Presentation 1 l Andy is a 13 year old junior high school student who likes to play sports. He is a regular recall patient but he missed his last six month visit. His health history has very few positive responses and he says he is currently in "good health".
Case Presentation 1 l Andy is a 13 year old junior high school student who likes to play sports. He is a regular recall patient but he missed his last six month visit. His health history has very few positive responses and he says he is currently in "good health".
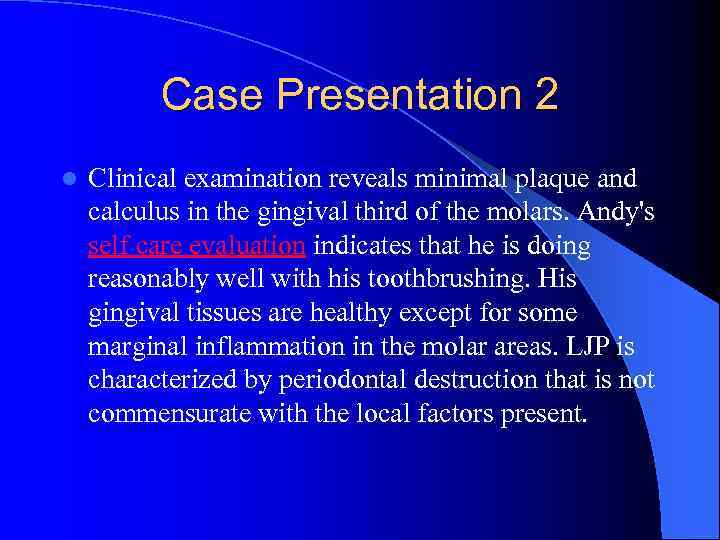 Case Presentation 2 l Clinical examination reveals minimal plaque and calculus in the gingival third of the molars. Andy's self care evaluation indicates that he is doing reasonably well with his toothbrushing. His gingival tissues are healthy except for some marginal inflammation in the molar areas. LJP is characterized by periodontal destruction that is not commensurate with the local factors present.
Case Presentation 2 l Clinical examination reveals minimal plaque and calculus in the gingival third of the molars. Andy's self care evaluation indicates that he is doing reasonably well with his toothbrushing. His gingival tissues are healthy except for some marginal inflammation in the molar areas. LJP is characterized by periodontal destruction that is not commensurate with the local factors present.
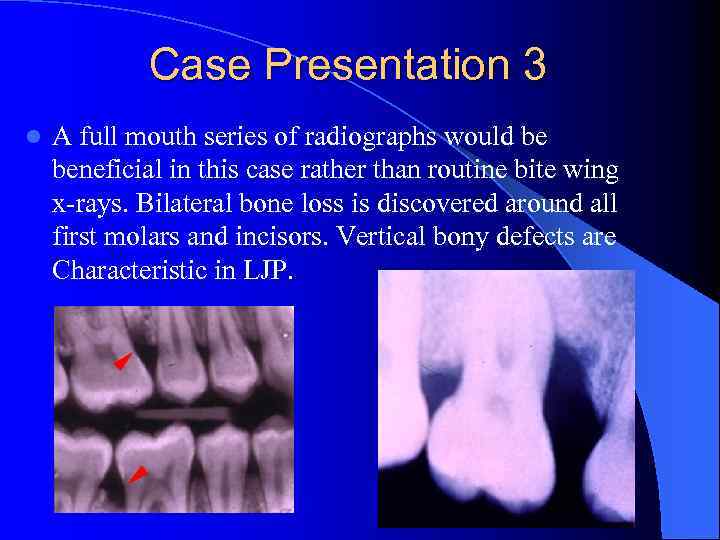 Case Presentation 3 l A full mouth series of radiographs would be beneficial in this case rather than routine bite wing x-rays. Bilateral bone loss is discovered around all first molars and incisors. Vertical bony defects are Characteristic in LJP.
Case Presentation 3 l A full mouth series of radiographs would be beneficial in this case rather than routine bite wing x-rays. Bilateral bone loss is discovered around all first molars and incisors. Vertical bony defects are Characteristic in LJP.

 Case Presentation 4 l You ask Andy if he has been having any problems in his mouth lately and he says "no". He just came to the dental office because his mom said he needed his "teeth cleaned".
Case Presentation 4 l You ask Andy if he has been having any problems in his mouth lately and he says "no". He just came to the dental office because his mom said he needed his "teeth cleaned".
 Diagnosis: Localized Aggressive Periodontitis
Diagnosis: Localized Aggressive Periodontitis
