Cranial and spinal trauma. Damage of the thorax:
![Crash-syndrome [compression, Bywaters‘ syndrome, traumatic rabdomyolis] Acute systemic signs of traumatic Crash-syndrome [compression, Bywaters‘ syndrome, traumatic rabdomyolis] Acute systemic signs of traumatic](https://present5.com/presentacii-2/20171208\14876-trauma.ppt\14876-trauma_30.jpg)


14876-trauma.ppt
- Количество слайдов: 83
 Cranial and spinal trauma. Damage of the thorax: pneumothorax, hemothorax, cardiac tamponade. Burns. Crash-syndrom. The management of patients with multiple trauma. Professor of the department of anesthesiology, traumatology and emergency medicine Fesenko Olga Khamitovna
Cranial and spinal trauma. Damage of the thorax: pneumothorax, hemothorax, cardiac tamponade. Burns. Crash-syndrom. The management of patients with multiple trauma. Professor of the department of anesthesiology, traumatology and emergency medicine Fesenko Olga Khamitovna
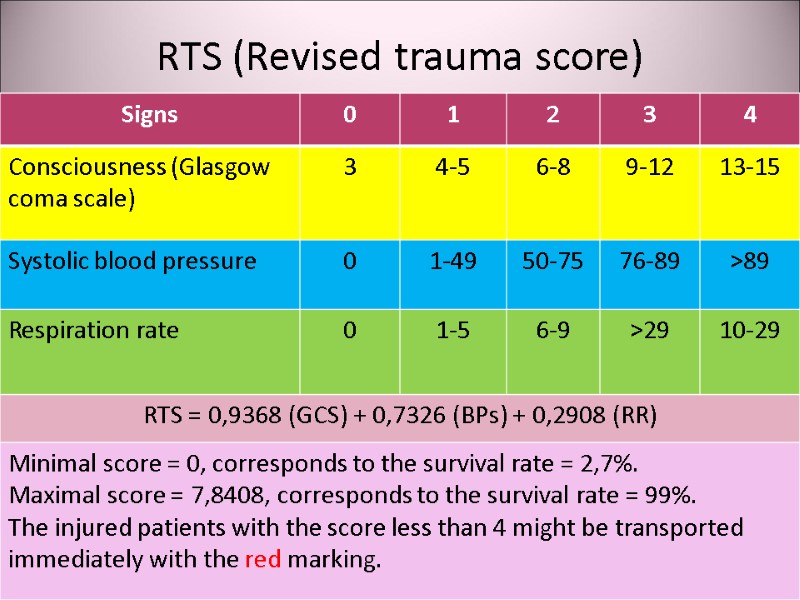
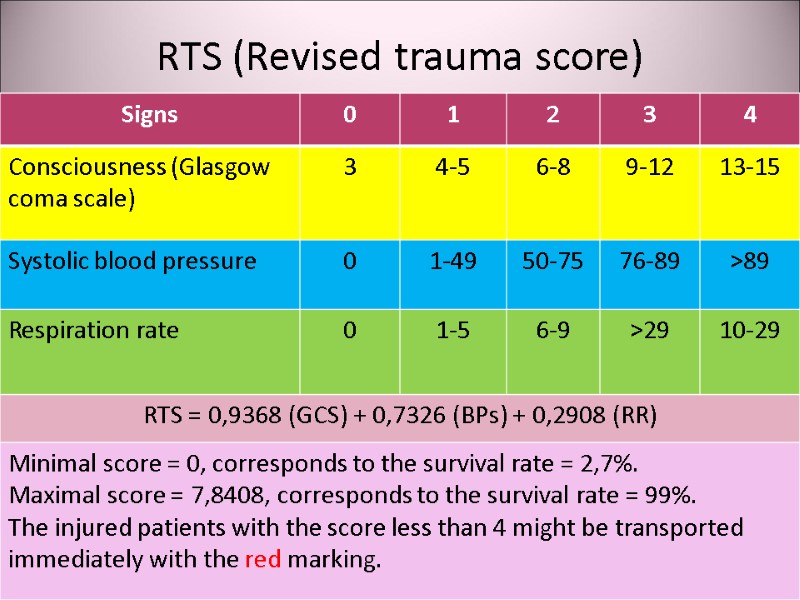 RTS (Revised trauma score)
RTS (Revised trauma score)
 Focused assessment of the unconscious patient Examination • Document the level of consciousness in objective terms, e.g. using the Glasgow Coma Scale. • Assess carefully the respiratory rate and pattern.
Focused assessment of the unconscious patient Examination • Document the level of consciousness in objective terms, e.g. using the Glasgow Coma Scale. • Assess carefully the respiratory rate and pattern.
 Focused assessment of the unconscious patient Examination • Examine for signs of head injury (e.g. scalp laceration, bruising, bleeding from an external auditory meatus or from the nose). If there are signs of head injury, assume additional cervical spine injury until proven otherwise: the neck must be immobilized in a collar and X-rayed before you check for neck stiffness and the oculocephalic response. • Check for neck stiffness.
Focused assessment of the unconscious patient Examination • Examine for signs of head injury (e.g. scalp laceration, bruising, bleeding from an external auditory meatus or from the nose). If there are signs of head injury, assume additional cervical spine injury until proven otherwise: the neck must be immobilized in a collar and X-rayed before you check for neck stiffness and the oculocephalic response. • Check for neck stiffness.
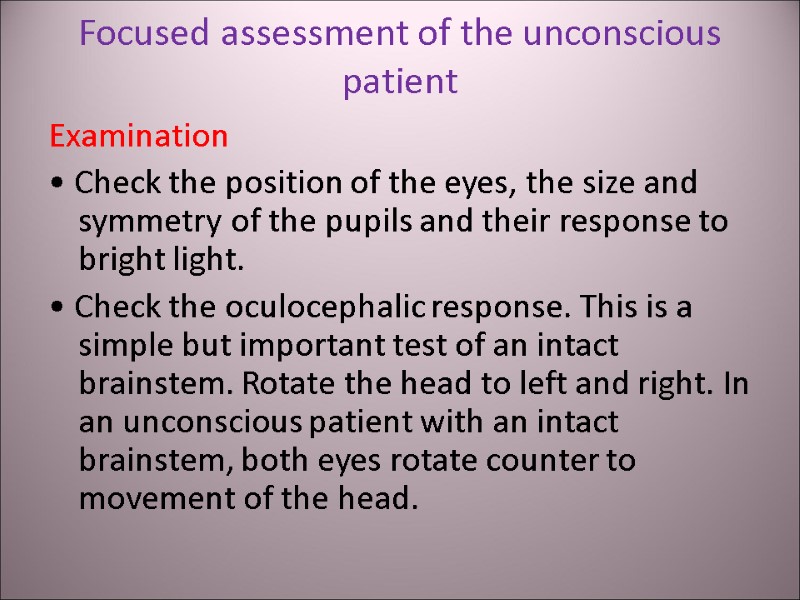
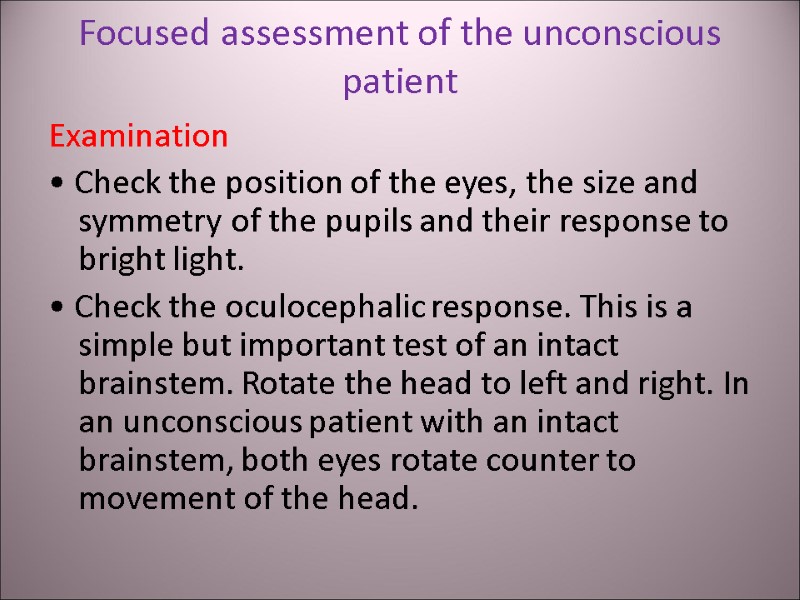 Focused assessment of the unconscious patient Examination • Check the position of the eyes, the size and symmetry of the pupils and their response to bright light. • Check the oculocephalic response. This is a simple but important test of an intact brainstem. Rotate the head to left and right. In an unconscious patient with an intact brainstem, both eyes rotate counter to movement of the head.
Focused assessment of the unconscious patient Examination • Check the position of the eyes, the size and symmetry of the pupils and their response to bright light. • Check the oculocephalic response. This is a simple but important test of an intact brainstem. Rotate the head to left and right. In an unconscious patient with an intact brainstem, both eyes rotate counter to movement of the head.
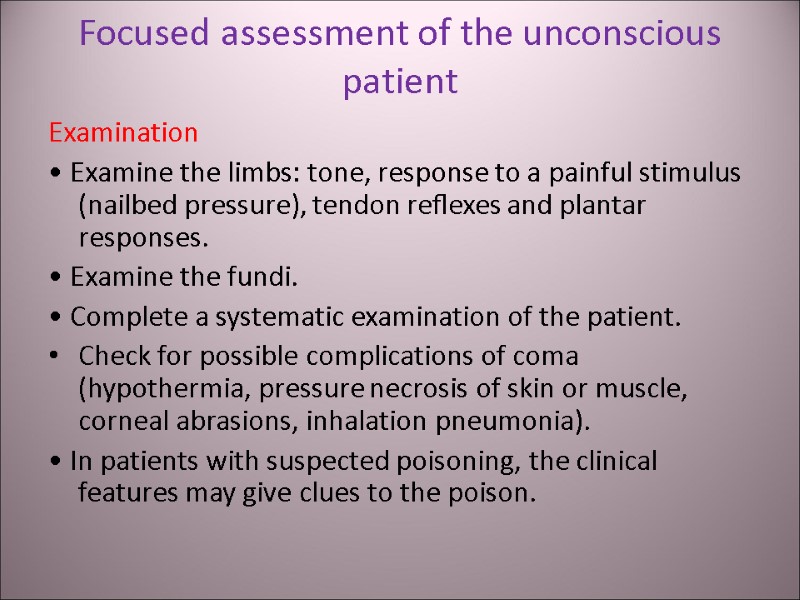
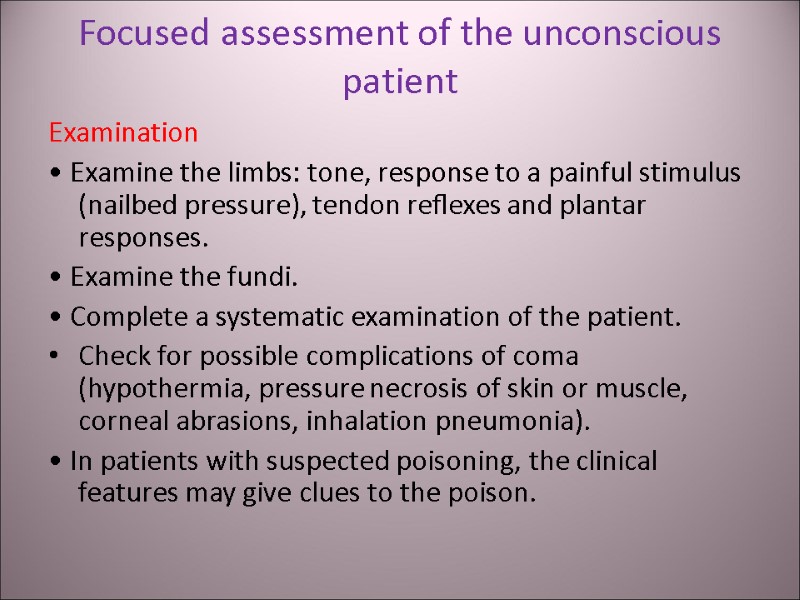 Focused assessment of the unconscious patient Examination • Examine the limbs: tone, response to a painful stimulus (nailbed pressure), tendon reflexes and plantar responses. • Examine the fundi. • Complete a systematic examination of the patient. Check for possible complications of coma (hypothermia, pressure necrosis of skin or muscle, corneal abrasions, inhalation pneumonia). • In patients with suspected poisoning, the clinical features may give clues to the poison.
Focused assessment of the unconscious patient Examination • Examine the limbs: tone, response to a painful stimulus (nailbed pressure), tendon reflexes and plantar responses. • Examine the fundi. • Complete a systematic examination of the patient. Check for possible complications of coma (hypothermia, pressure necrosis of skin or muscle, corneal abrasions, inhalation pneumonia). • In patients with suspected poisoning, the clinical features may give clues to the poison.
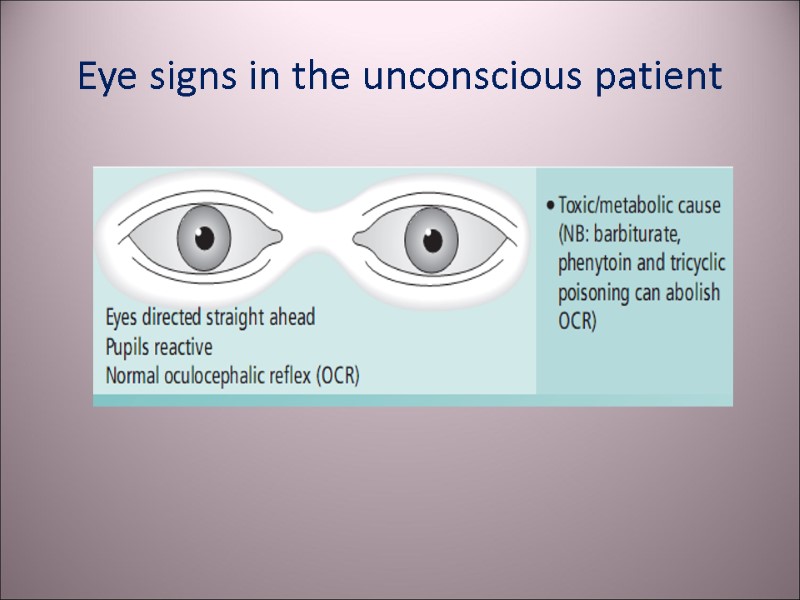
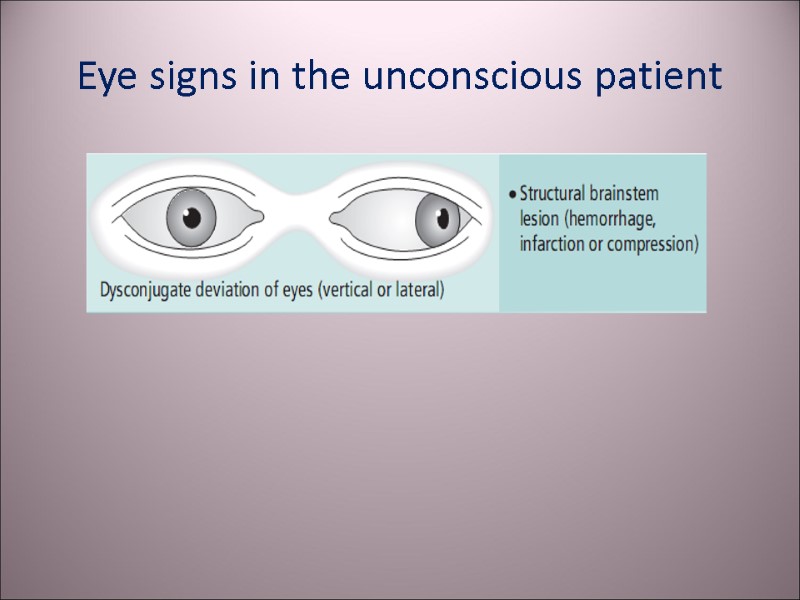
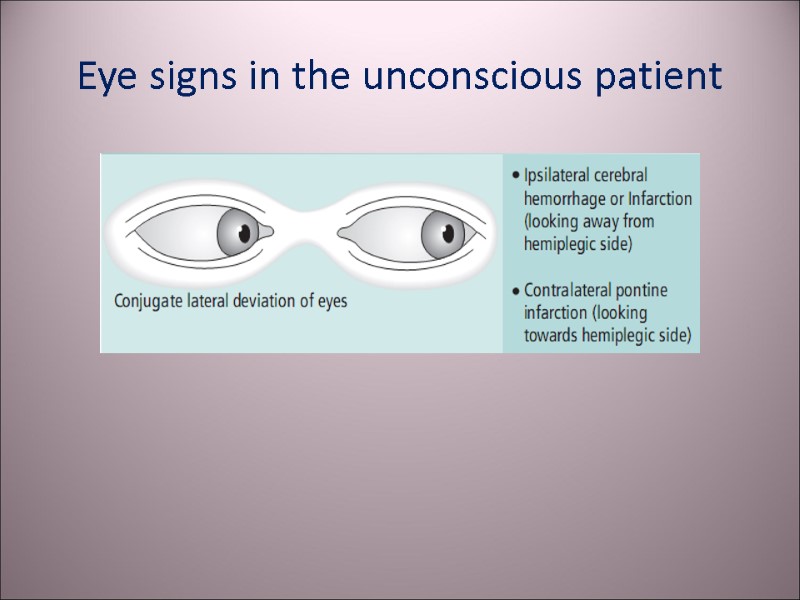
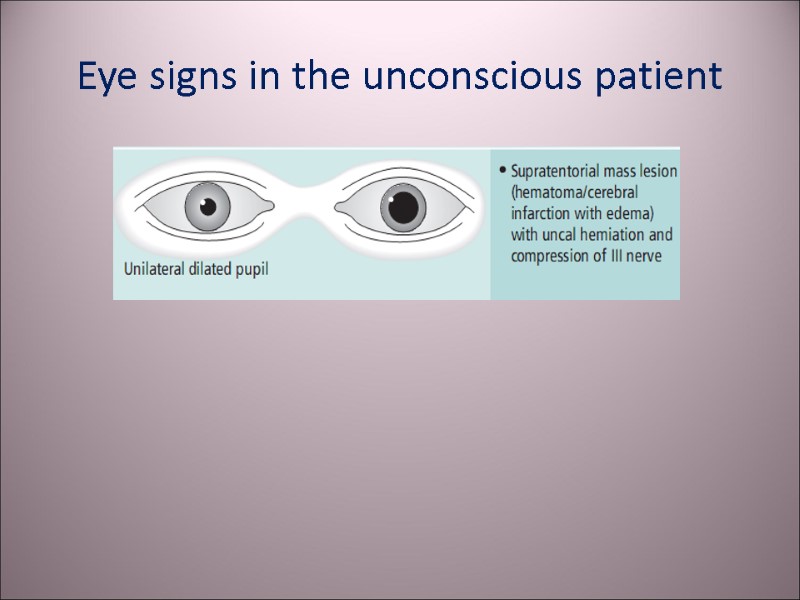
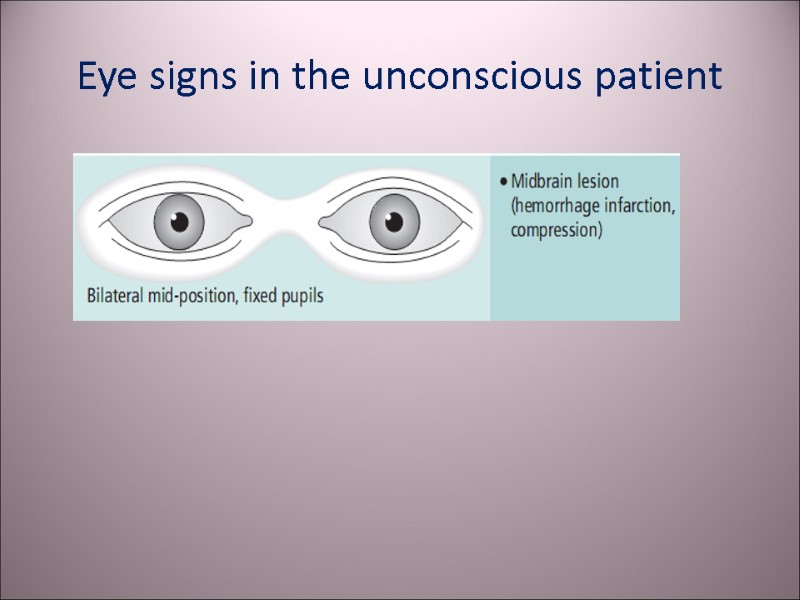
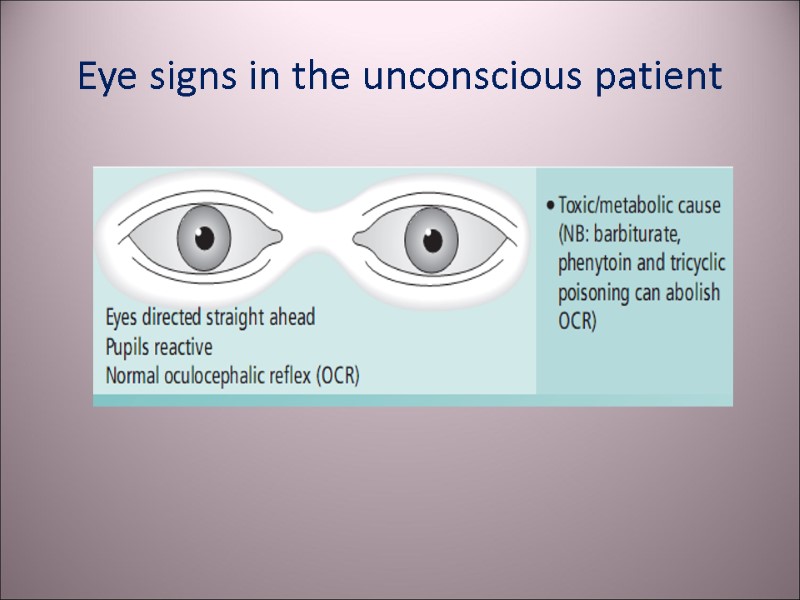 Eye signs in the unconscious patient
Eye signs in the unconscious patient
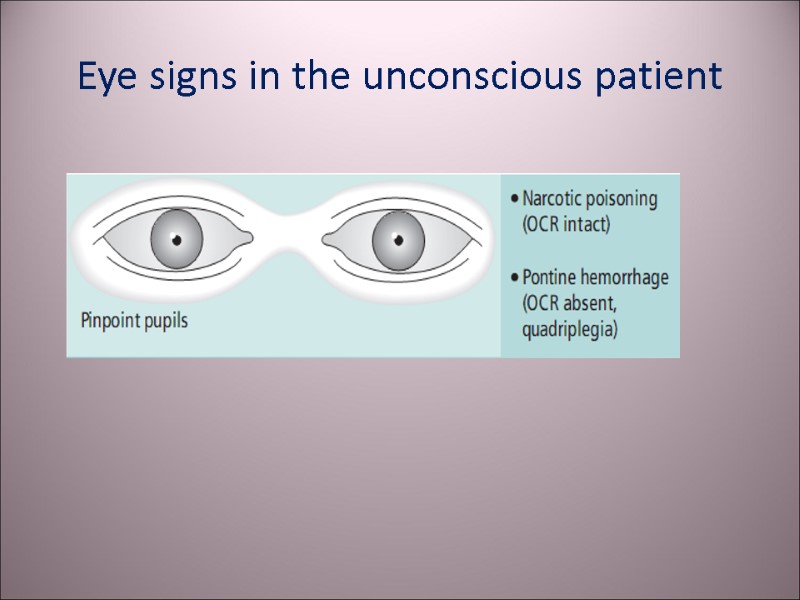 Eye signs in the unconscious patient
Eye signs in the unconscious patient
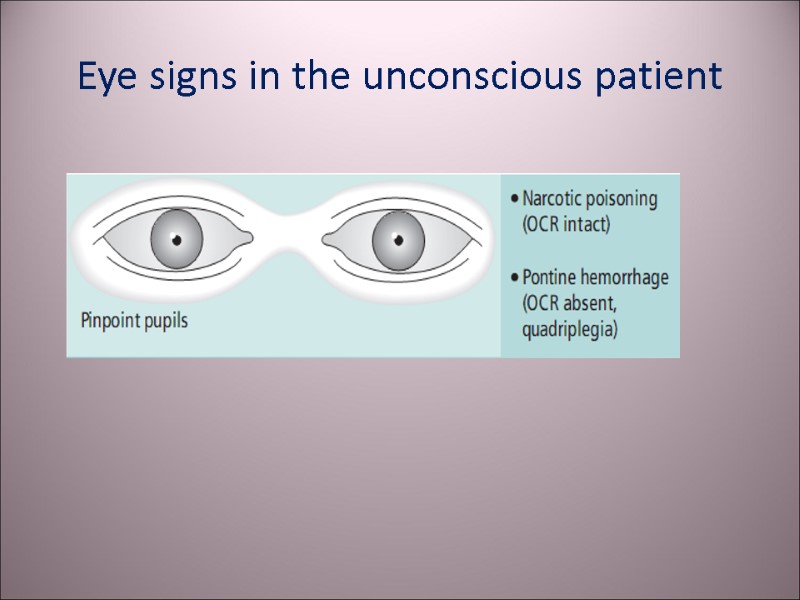
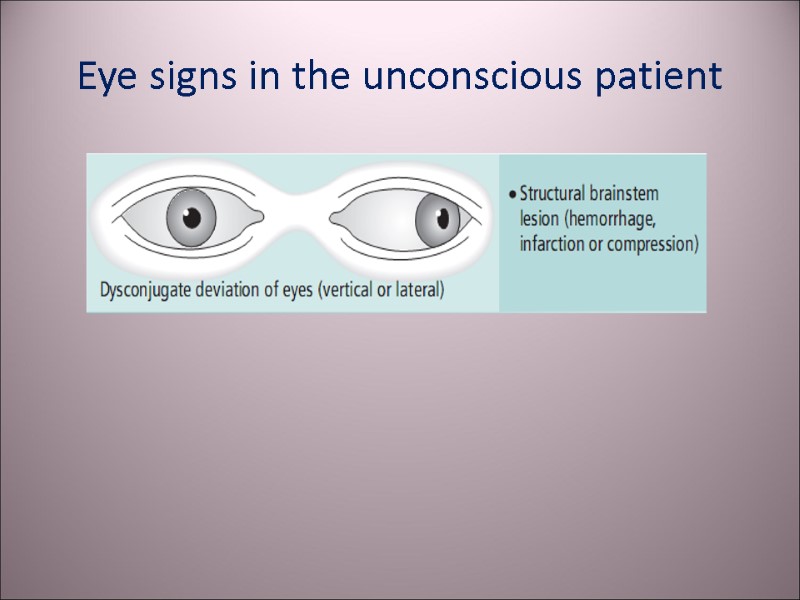 Eye signs in the unconscious patient
Eye signs in the unconscious patient
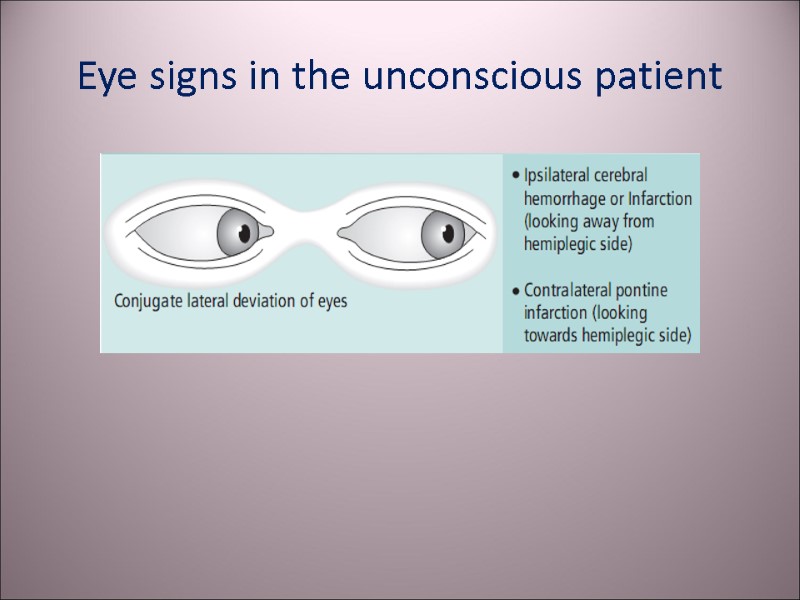 Eye signs in the unconscious patient
Eye signs in the unconscious patient
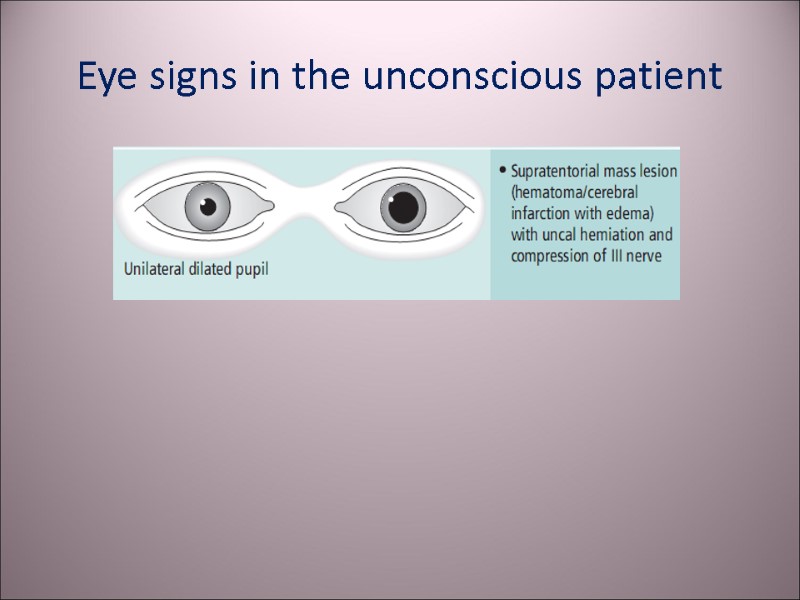 Eye signs in the unconscious patient
Eye signs in the unconscious patient
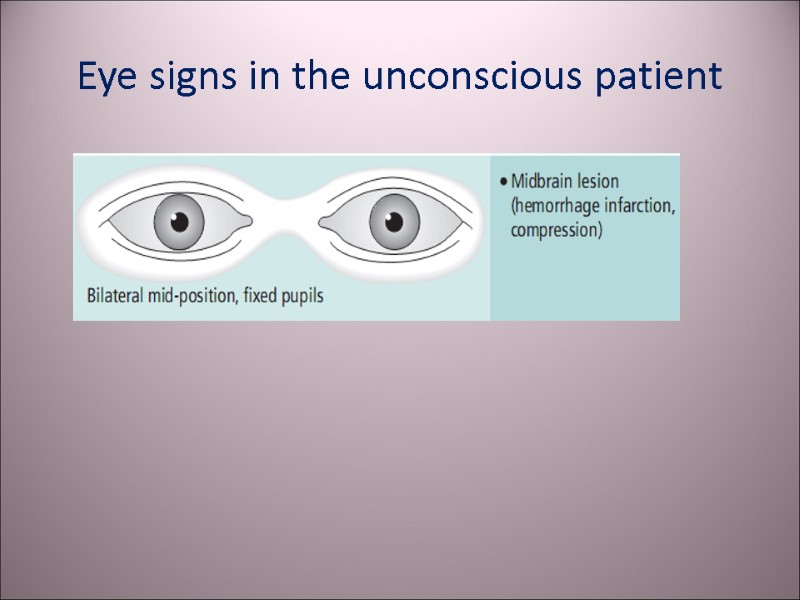 Eye signs in the unconscious patient
Eye signs in the unconscious patient
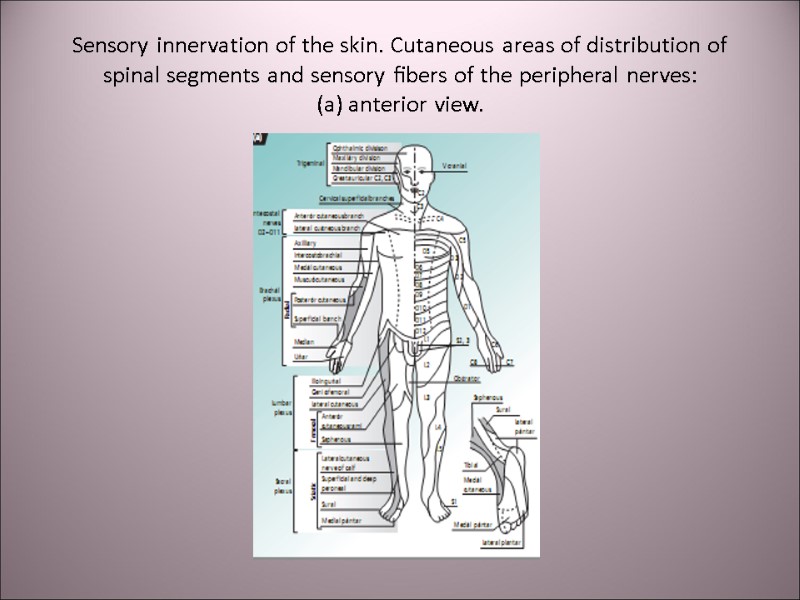
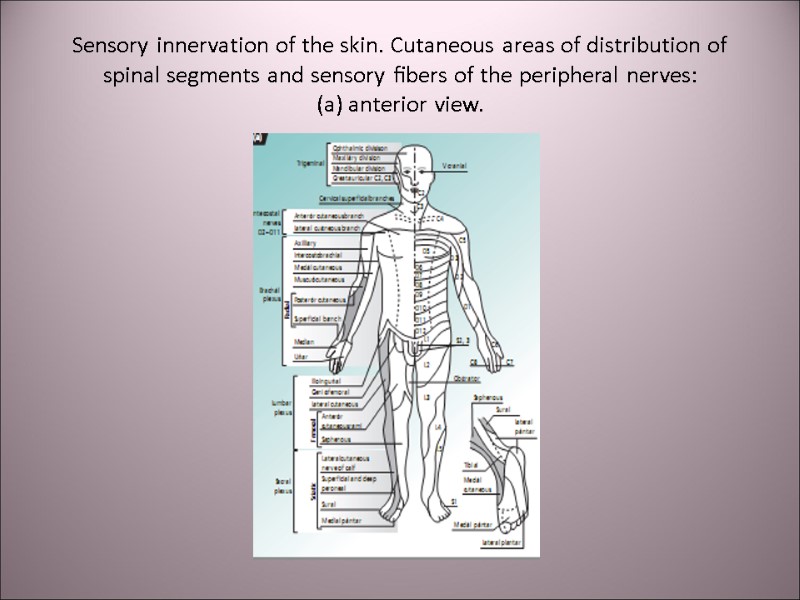 Sensory innervation of the skin. Cutaneous areas of distribution of spinal segments and sensory fibers of the peripheral nerves: (a) anterior view.
Sensory innervation of the skin. Cutaneous areas of distribution of spinal segments and sensory fibers of the peripheral nerves: (a) anterior view.
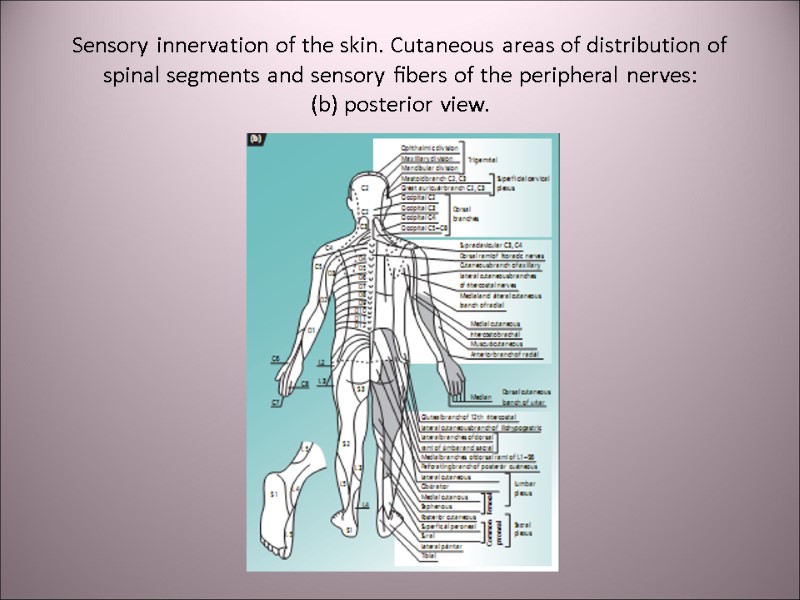
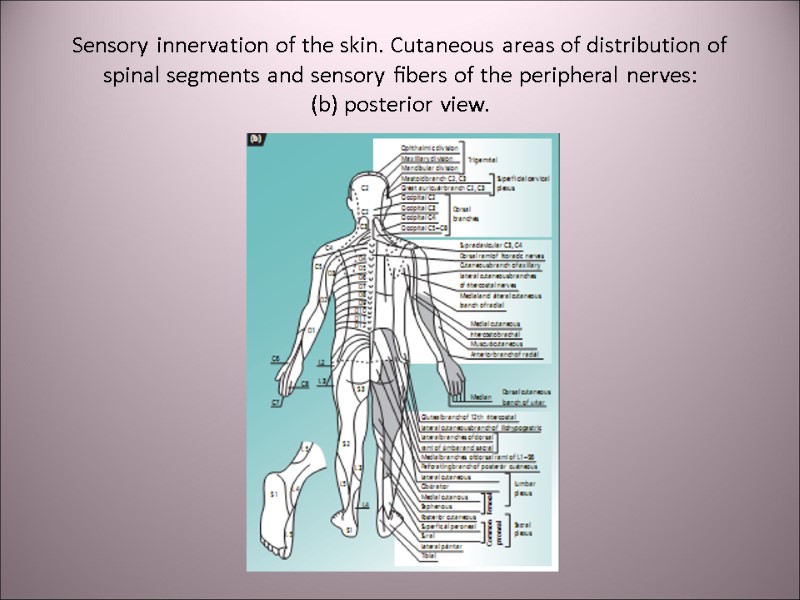 Sensory innervation of the skin. Cutaneous areas of distribution of spinal segments and sensory fibers of the peripheral nerves: (b) posterior view.
Sensory innervation of the skin. Cutaneous areas of distribution of spinal segments and sensory fibers of the peripheral nerves: (b) posterior view.
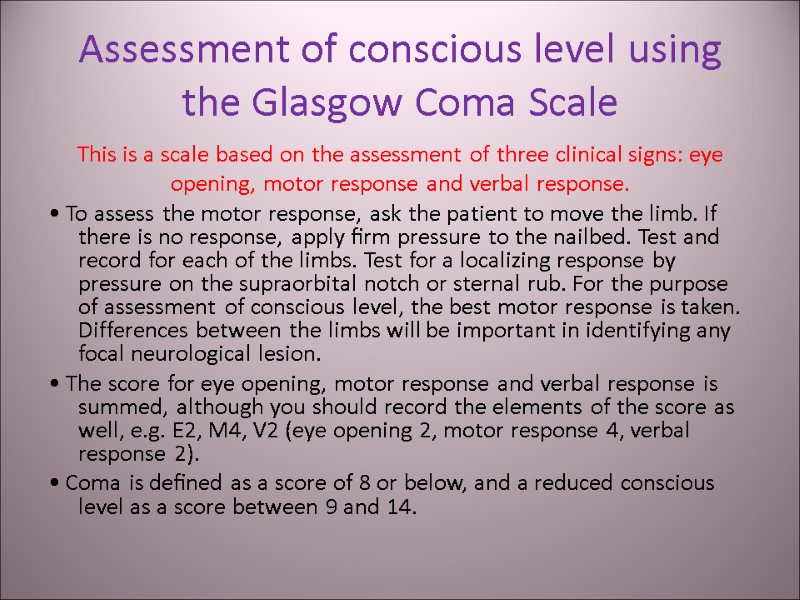
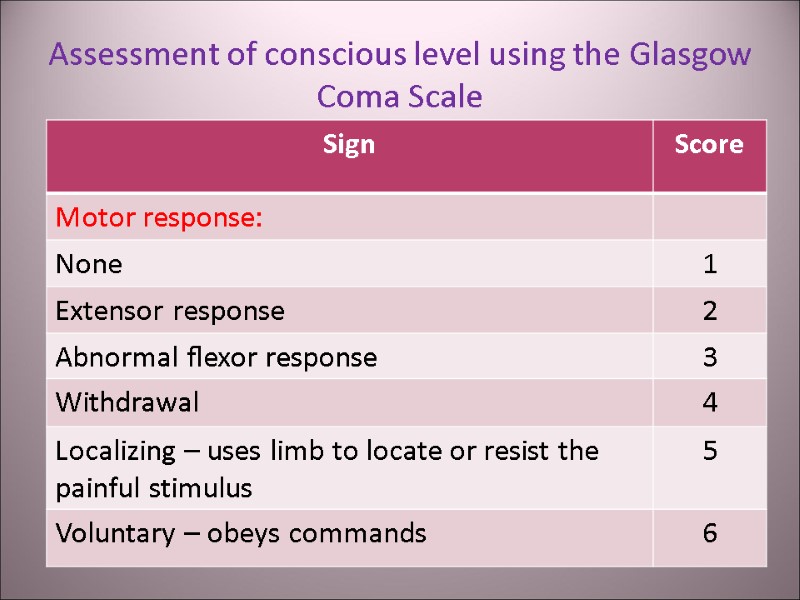
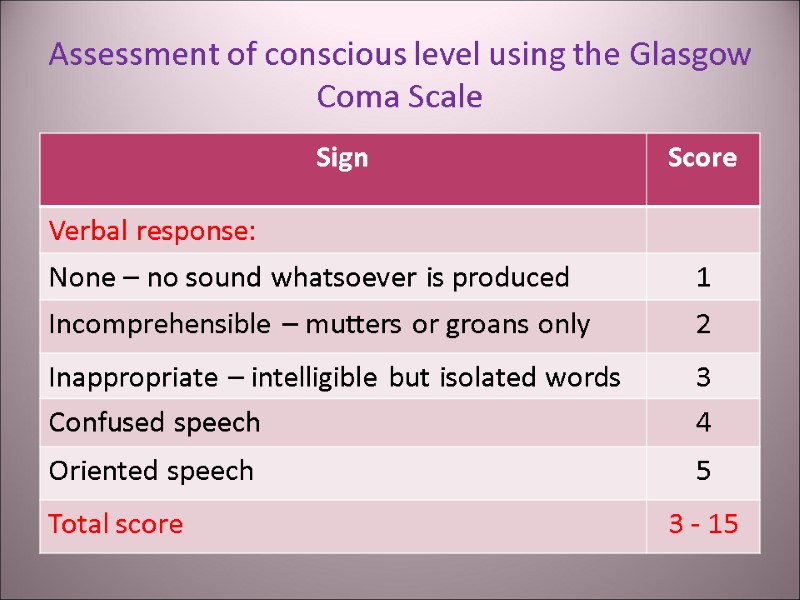
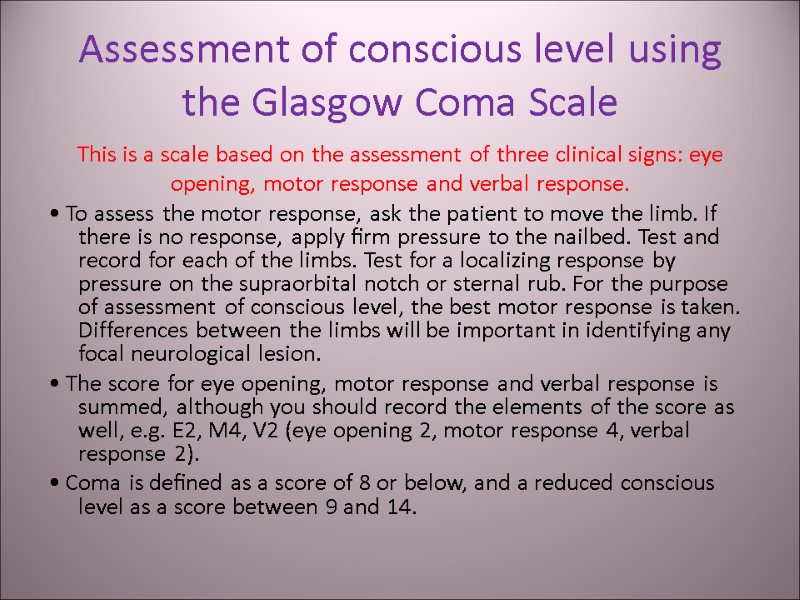 Assessment of conscious level using the Glasgow Coma Scale This is a scale based on the assessment of three clinical signs: eye opening, motor response and verbal response. • To assess the motor response, ask the patient to move the limb. If there is no response, apply firm pressure to the nailbed. Test and record for each of the limbs. Test for a localizing response by pressure on the supraorbital notch or sternal rub. For the purpose of assessment of conscious level, the best motor response is taken. Differences between the limbs will be important in identifying any focal neurological lesion. • The score for eye opening, motor response and verbal response is summed, although you should record the elements of the score as well, e.g. E2, M4, V2 (eye opening 2, motor response 4, verbal response 2). • Coma is defined as a score of 8 or below, and a reduced conscious level as a score between 9 and 14.
Assessment of conscious level using the Glasgow Coma Scale This is a scale based on the assessment of three clinical signs: eye opening, motor response and verbal response. • To assess the motor response, ask the patient to move the limb. If there is no response, apply firm pressure to the nailbed. Test and record for each of the limbs. Test for a localizing response by pressure on the supraorbital notch or sternal rub. For the purpose of assessment of conscious level, the best motor response is taken. Differences between the limbs will be important in identifying any focal neurological lesion. • The score for eye opening, motor response and verbal response is summed, although you should record the elements of the score as well, e.g. E2, M4, V2 (eye opening 2, motor response 4, verbal response 2). • Coma is defined as a score of 8 or below, and a reduced conscious level as a score between 9 and 14.
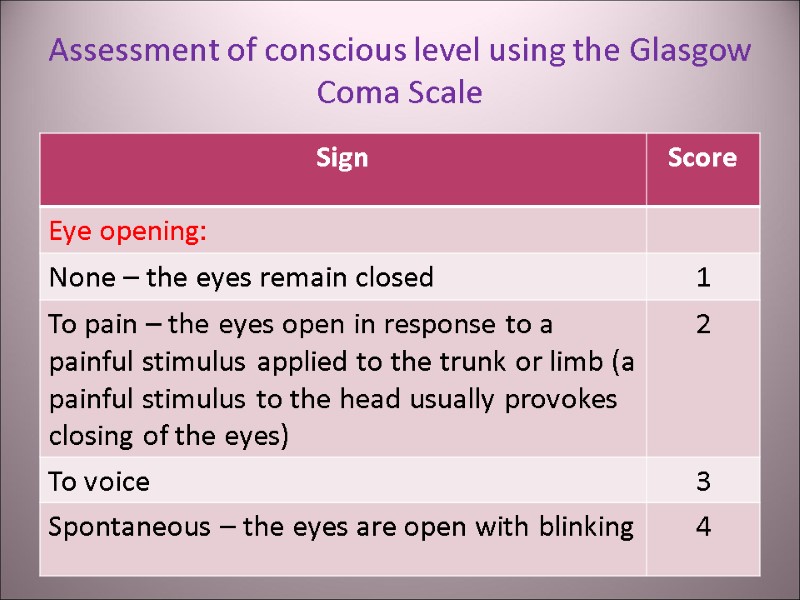
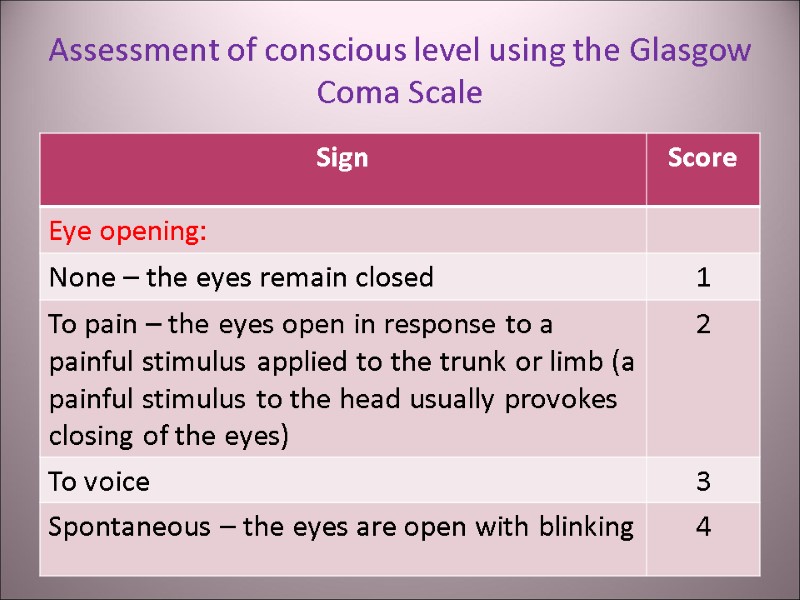 Assessment of conscious level using the Glasgow Coma Scale
Assessment of conscious level using the Glasgow Coma Scale
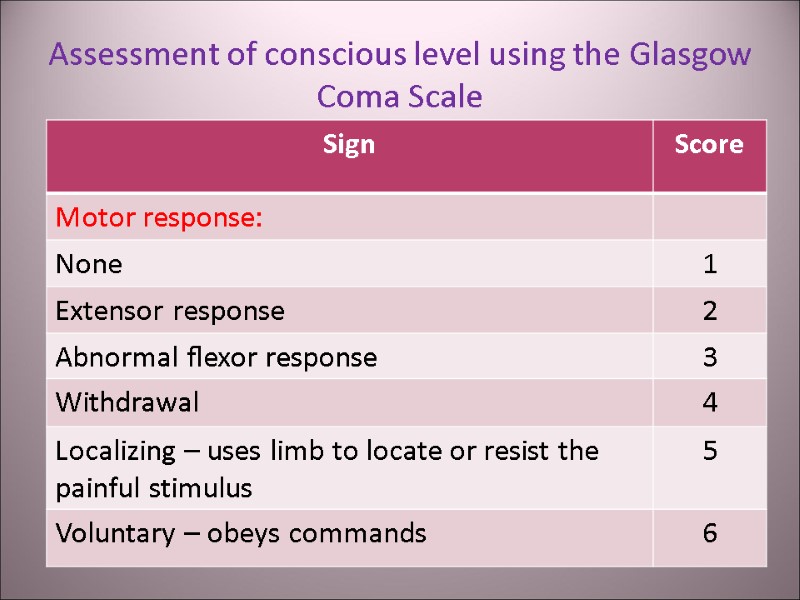 Assessment of conscious level using the Glasgow Coma Scale
Assessment of conscious level using the Glasgow Coma Scale
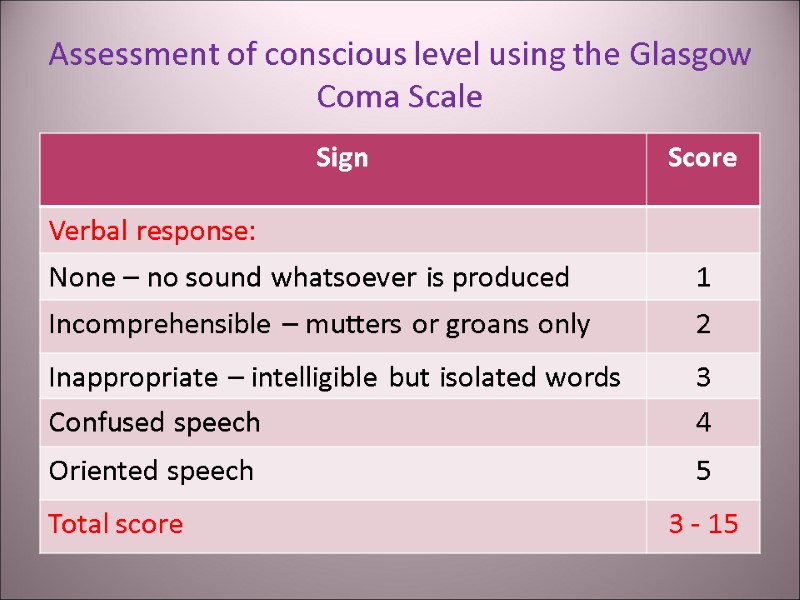 Assessment of conscious level using the Glasgow Coma Scale
Assessment of conscious level using the Glasgow Coma Scale
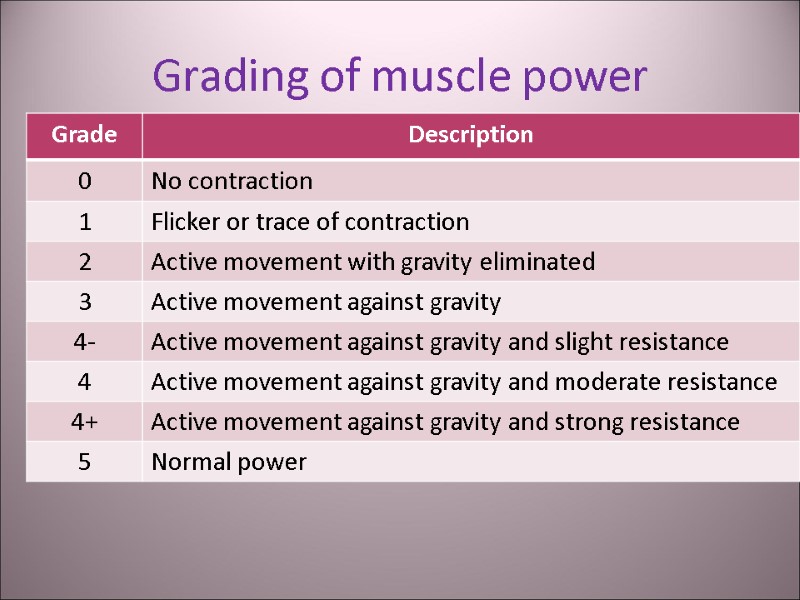
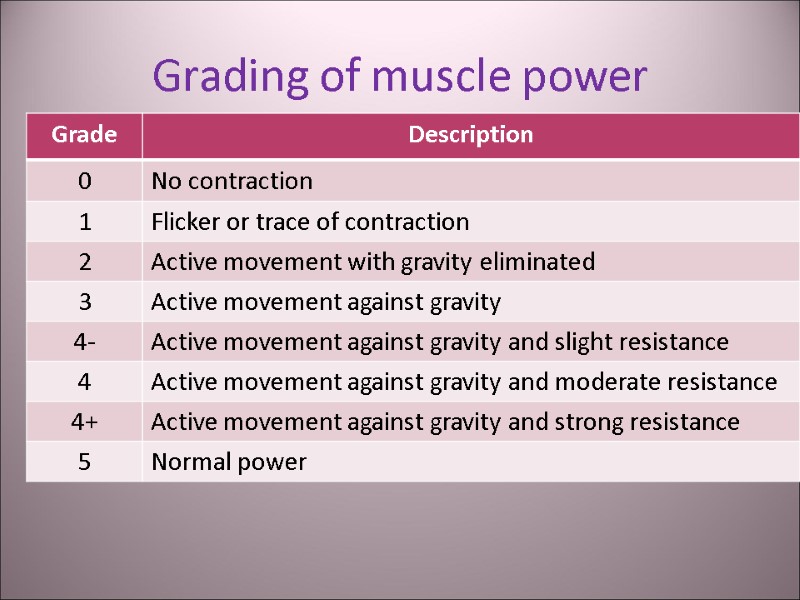 Grading of muscle power
Grading of muscle power
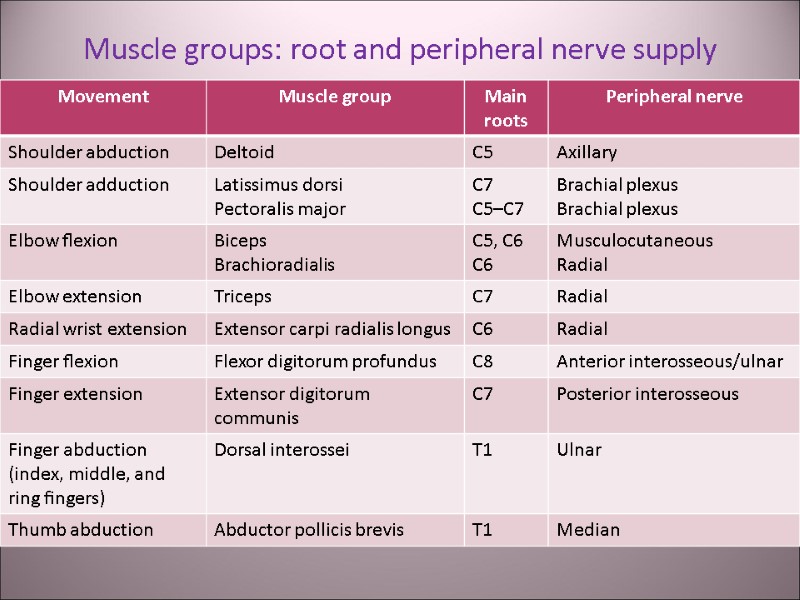
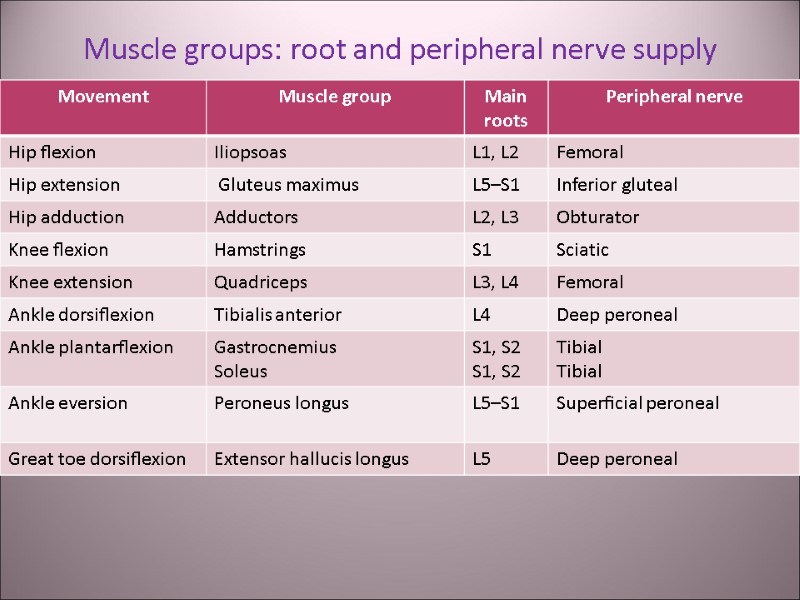
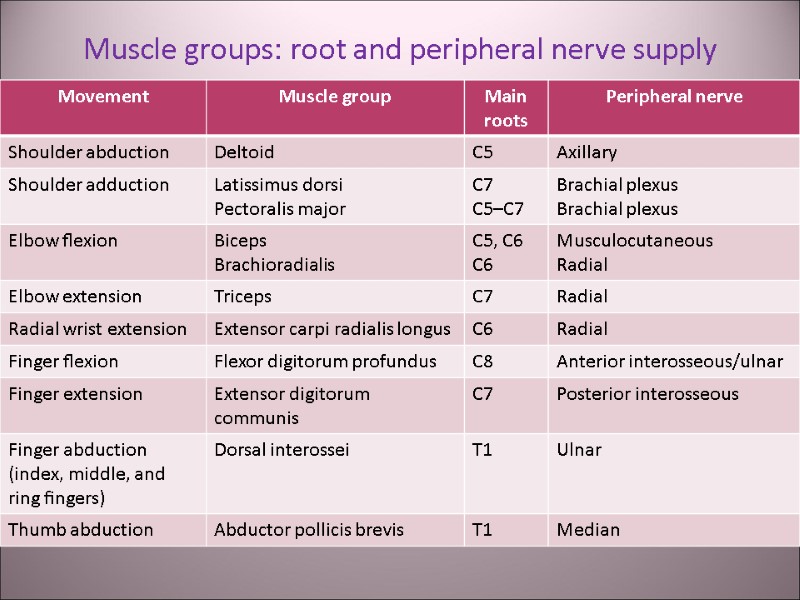 Muscle groups: root and peripheral nerve supply
Muscle groups: root and peripheral nerve supply
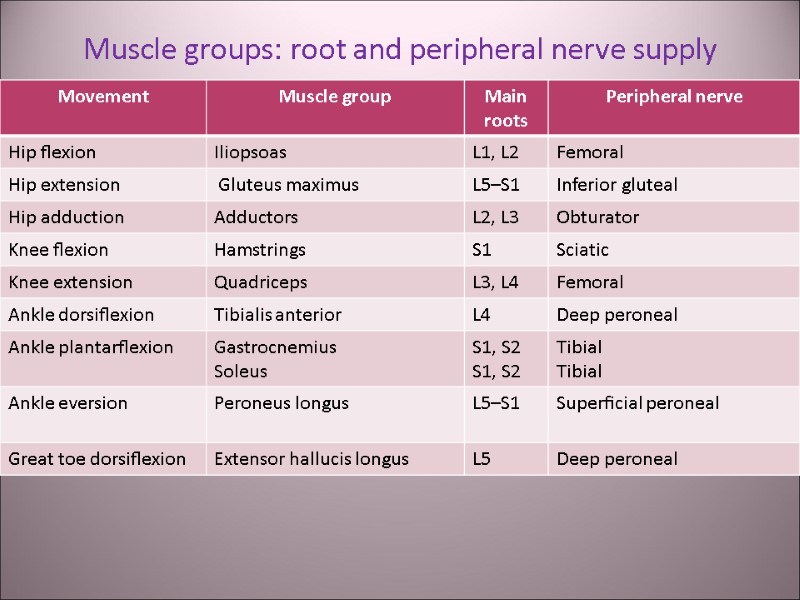 Muscle groups: root and peripheral nerve supply
Muscle groups: root and peripheral nerve supply
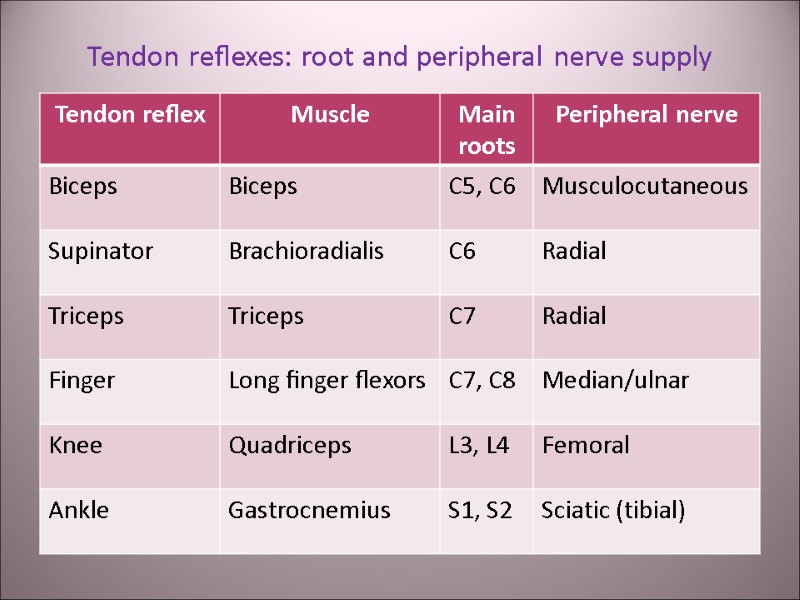
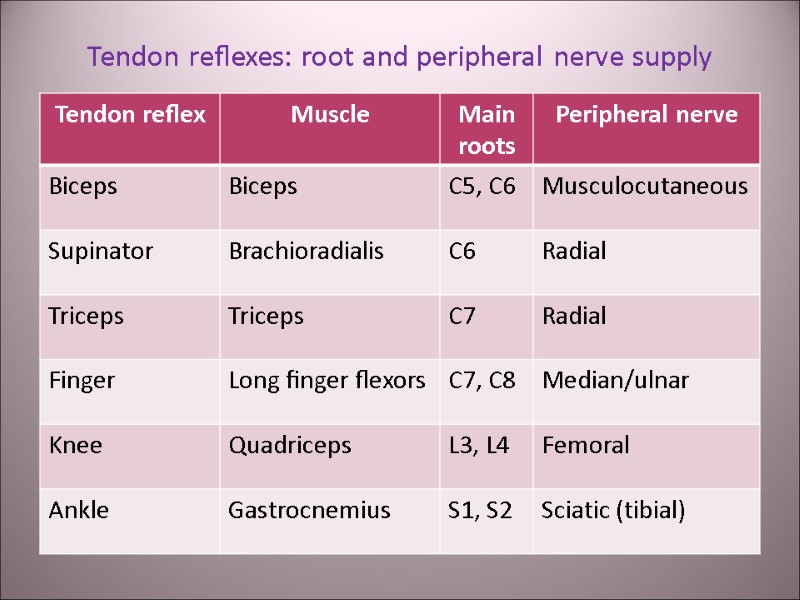 Tendon reflexes: root and peripheral nerve supply
Tendon reflexes: root and peripheral nerve supply
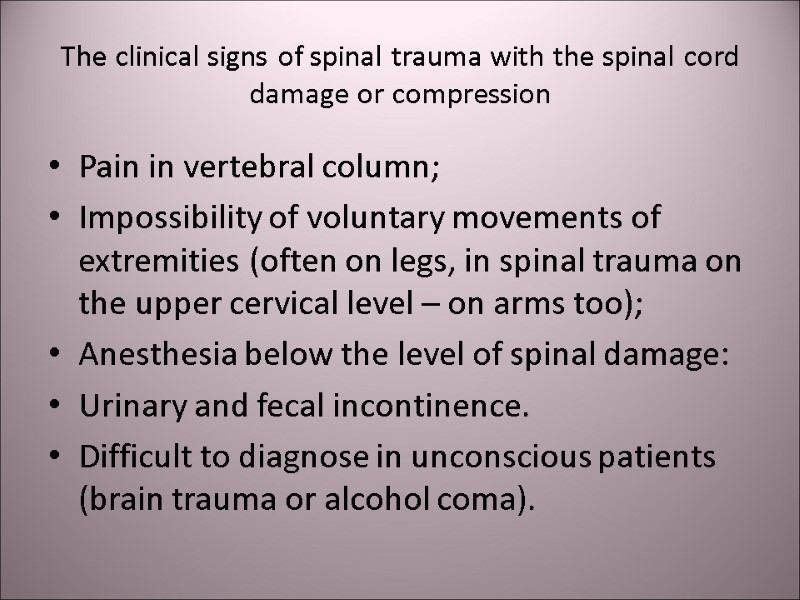 The clinical signs of spinal trauma with the spinal cord damage or compression Pain in vertebral column; Impossibility of voluntary movements of extremities (often on legs, in spinal trauma on the upper cervical level – on arms too); Anesthesia below the level of spinal damage: Urinary and fecal incontinence. Difficult to diagnose in unconscious patients (brain trauma or alcohol coma).
The clinical signs of spinal trauma with the spinal cord damage or compression Pain in vertebral column; Impossibility of voluntary movements of extremities (often on legs, in spinal trauma on the upper cervical level – on arms too); Anesthesia below the level of spinal damage: Urinary and fecal incontinence. Difficult to diagnose in unconscious patients (brain trauma or alcohol coma).
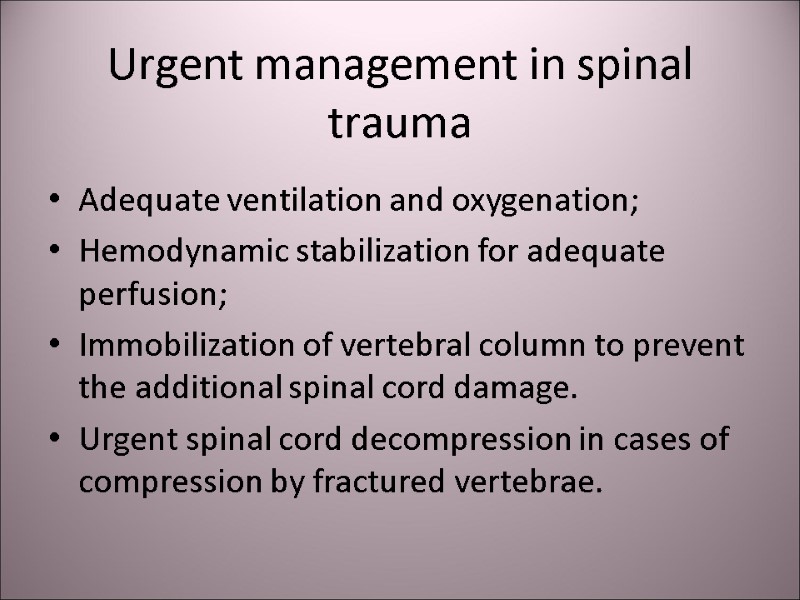 Urgent management in spinal trauma Adequate ventilation and oxygenation; Hemodynamic stabilization for adequate perfusion; Immobilization of vertebral column to prevent the additional spinal cord damage. Urgent spinal cord decompression in cases of compression by fractured vertebrae.
Urgent management in spinal trauma Adequate ventilation and oxygenation; Hemodynamic stabilization for adequate perfusion; Immobilization of vertebral column to prevent the additional spinal cord damage. Urgent spinal cord decompression in cases of compression by fractured vertebrae.
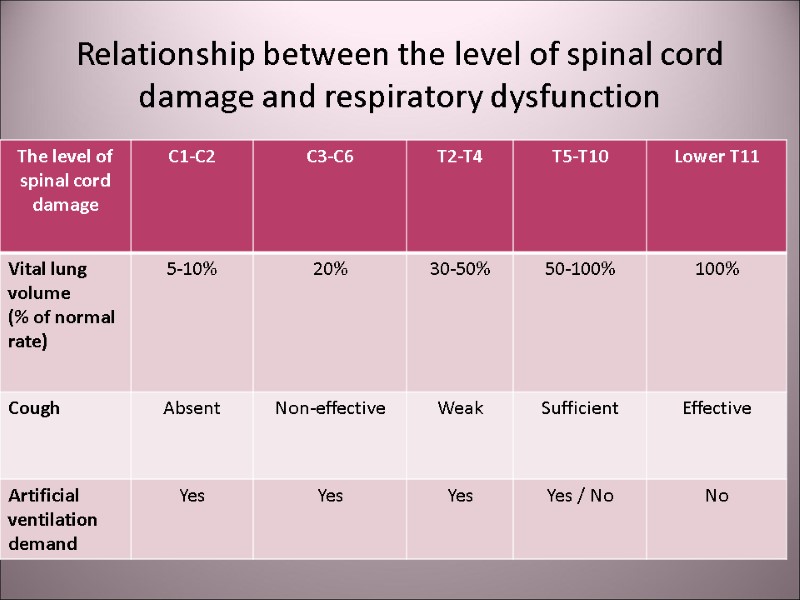
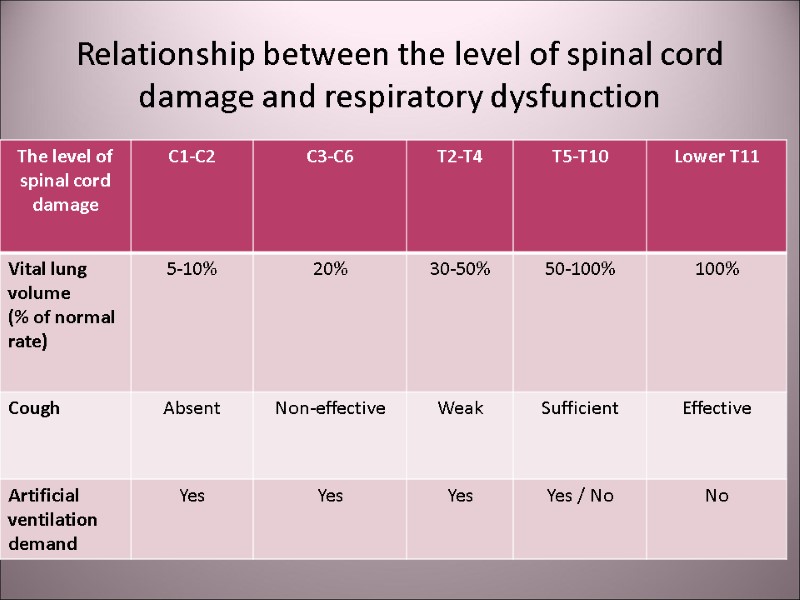 Relationship between the level of spinal cord damage and respiratory dysfunction
Relationship between the level of spinal cord damage and respiratory dysfunction
 Hemodynamic instability in spinal trauma Denervation due to spinal trauma leads to autonomic nervous system dysfunction in the affected area. This results to vasodilatation, bradychardya, hypotension and hypothermia. Hypotension is usually absent in spinal trauma below the level of T6. If it is present in such cases - suspect internal bleeding. Hb and Ht should be done 2-4 times during the 1-st day after the spinal trauma.
Hemodynamic instability in spinal trauma Denervation due to spinal trauma leads to autonomic nervous system dysfunction in the affected area. This results to vasodilatation, bradychardya, hypotension and hypothermia. Hypotension is usually absent in spinal trauma below the level of T6. If it is present in such cases - suspect internal bleeding. Hb and Ht should be done 2-4 times during the 1-st day after the spinal trauma.
 Infusion therapy in spinal trauma: solutions, volume, rate, complications In severe hypotension (systolic BP <60 – 70 mm Hg) – start with hypertonic 7,5% NaCl in rate 4 – 6 ml/kg with colloide - 5-8 ml/kg during 15-30 min. Then continue with 0,9% NaCl, up to total volume 2,5-3 liters, in rate 100-200 ml/h. This scheme is recommended for adequate perfusion in affected zone and prevention of ascending spinal cord edema. In relatively stabile hemodynamic parameters (BPs >80 mm Hg) – infuse only isotonic saline solutions. If the infusion rate can not provide the hemodynamic stabilization (BPs >100 mm Hg) – use vasopressors (norepinephrine, phenylephrine, epinephrine) for increasing BPs up to 110 - 130 mm Hg. If the bleeding is excluded, the infusion volume should not exceed 3 litres per day. In patients with spinal trauma large infusion volume can result to pulmonary edema.
Infusion therapy in spinal trauma: solutions, volume, rate, complications In severe hypotension (systolic BP <60 – 70 mm Hg) – start with hypertonic 7,5% NaCl in rate 4 – 6 ml/kg with colloide - 5-8 ml/kg during 15-30 min. Then continue with 0,9% NaCl, up to total volume 2,5-3 liters, in rate 100-200 ml/h. This scheme is recommended for adequate perfusion in affected zone and prevention of ascending spinal cord edema. In relatively stabile hemodynamic parameters (BPs >80 mm Hg) – infuse only isotonic saline solutions. If the infusion rate can not provide the hemodynamic stabilization (BPs >100 mm Hg) – use vasopressors (norepinephrine, phenylephrine, epinephrine) for increasing BPs up to 110 - 130 mm Hg. If the bleeding is excluded, the infusion volume should not exceed 3 litres per day. In patients with spinal trauma large infusion volume can result to pulmonary edema.
 The prevention of ascending spinal cord edema Methylprednyzolone 30 mg/kg bolus in 10 - 15 min. Then 5 mg/kg/h during 1-2 days. Contraindicated in patients with infection and gastric ulcers.
The prevention of ascending spinal cord edema Methylprednyzolone 30 mg/kg bolus in 10 - 15 min. Then 5 mg/kg/h during 1-2 days. Contraindicated in patients with infection and gastric ulcers.
 Nursing and nutrition in spinal trauma Prevention of bedsores: mattress for preventing pressure sores. Enteral nutrition, in unconscious patients – tube feeding after the excluding intestinal paresis. Deep vein thrombosis prophylaxis: heparin 2500-5000 units 3 times a day s/c; or fractionated small-molecular heparins. Antibiotics. Gastric stress ulcers prophylaxis: ion-pump inhibitors (omeprazole) or Н2-histamine-blokers.
Nursing and nutrition in spinal trauma Prevention of bedsores: mattress for preventing pressure sores. Enteral nutrition, in unconscious patients – tube feeding after the excluding intestinal paresis. Deep vein thrombosis prophylaxis: heparin 2500-5000 units 3 times a day s/c; or fractionated small-molecular heparins. Antibiotics. Gastric stress ulcers prophylaxis: ion-pump inhibitors (omeprazole) or Н2-histamine-blokers.
![>Crash-syndrome [compression, Bywaters‘ syndrome, traumatic rabdomyolis] Acute systemic signs of traumatic >Crash-syndrome [compression, Bywaters‘ syndrome, traumatic rabdomyolis] Acute systemic signs of traumatic](https://present5.com/presentacii-2/20171208\14876-trauma.ppt\14876-trauma_30.jpg) Crash-syndrome [compression, Bywaters‘ syndrome, traumatic rabdomyolis] Acute systemic signs of traumatic and ischemic damage of soft tissue, skeletal muscles due to prolonged compression. This lead to increased membrane permeability with K-leakage, outflow of enzymes and myoglobin from cells to plasma. Hypotension, poor renal perfusion and myoglobinemia lead to tubular necrosis and uremia.
Crash-syndrome [compression, Bywaters‘ syndrome, traumatic rabdomyolis] Acute systemic signs of traumatic and ischemic damage of soft tissue, skeletal muscles due to prolonged compression. This lead to increased membrane permeability with K-leakage, outflow of enzymes and myoglobin from cells to plasma. Hypotension, poor renal perfusion and myoglobinemia lead to tubular necrosis and uremia.
 Crash-syndrome is found in: Earthquake; Terrorism, bombing; Landfall in underground mine; Road accident.
Crash-syndrome is found in: Earthquake; Terrorism, bombing; Landfall in underground mine; Road accident.
 Clinical signs of crash-syndrome Compressing longer than 1 hour. Damage of big muscle bulk (often in leg compression). Pulse and perfusion on the damaged extremity are absent. After the pressing at the distal area capillaries are not filled. The skin on the intact area is peal, cool and wet. The pulse is rapid, weak. The pain is usually absent due to compressing of nerves. Sometimes, in spite of compressed extremity the physical state seems to be quite normal – “smiling death” syndrome.
Clinical signs of crash-syndrome Compressing longer than 1 hour. Damage of big muscle bulk (often in leg compression). Pulse and perfusion on the damaged extremity are absent. After the pressing at the distal area capillaries are not filled. The skin on the intact area is peal, cool and wet. The pulse is rapid, weak. The pain is usually absent due to compressing of nerves. Sometimes, in spite of compressed extremity the physical state seems to be quite normal – “smiling death” syndrome.
 Clinical signs of crash-syndrome Bone fractures are often take place. The affected limbs became later edematous. Haematuria. Oliguria (< 400 ml/day). ↑ serum level of creatininkinaze (>1000 unit/l), urea, creatinin, uric acid, K, phosphate.
Clinical signs of crash-syndrome Bone fractures are often take place. The affected limbs became later edematous. Haematuria. Oliguria (< 400 ml/day). ↑ serum level of creatininkinaze (>1000 unit/l), urea, creatinin, uric acid, K, phosphate.
 Before the deblocking the limb: Secure the safety of rescuers (supporting bulks, mask-respirators). Evaluation of victim before the deblocking the limb. Treatment must be started before the deblocking! The time of deblocking must be discussed with medics and survivors, rescuers! Airway protection: provide permeability and protect with mask-respirators from dust powder. Adequate oxygenation. Keep the body temperature.
Before the deblocking the limb: Secure the safety of rescuers (supporting bulks, mask-respirators). Evaluation of victim before the deblocking the limb. Treatment must be started before the deblocking! The time of deblocking must be discussed with medics and survivors, rescuers! Airway protection: provide permeability and protect with mask-respirators from dust powder. Adequate oxygenation. Keep the body temperature.
 Before the deblocking the victim: Canulate 1-2 veins. Infuse 1-2 l normal saline rapidly. If the deblocking is delayed – infusion speed must be 1,5 l/h; in children and old patient with respiratory and renal failure – only 0,5 l under the control of lung auscultation. Solutions with K are contraindicated. Dextrans also contraindicated because of renal affection. Na bicarbonate: 2 mmol/kg before the deblocking, if it is delayed – 1 mmol/kg/h. ECG monitor if available. Analgesia – on demand, fentanyl is better than morphine (the same analgesia without vasodilation). Applying the tourniquet – controversial point! After all these you can deblock the affected limb!
Before the deblocking the victim: Canulate 1-2 veins. Infuse 1-2 l normal saline rapidly. If the deblocking is delayed – infusion speed must be 1,5 l/h; in children and old patient with respiratory and renal failure – only 0,5 l under the control of lung auscultation. Solutions with K are contraindicated. Dextrans also contraindicated because of renal affection. Na bicarbonate: 2 mmol/kg before the deblocking, if it is delayed – 1 mmol/kg/h. ECG monitor if available. Analgesia – on demand, fentanyl is better than morphine (the same analgesia without vasodilation). Applying the tourniquet – controversial point! After all these you can deblock the affected limb!
 After the deblocking the limb: If the active movements are impossible, but passive movements are possible (the muscles didn’t become stiff) – tourniquet is not used, if it was applied before you must release it. If arterial bleeding – tourniquet is indicated. If the passive movements are impossible (cadaveric rigidity) – tourniquet is indicated (in the hospital the amputation will be done upper the tourniquet). Transport the victim as soon as possible to the hospital. Call the hospital for preparing the operating room. Anti-shock pants are contraindicated! Shock prevention: horizontal position, oxygen, warming. Rapid infusion of normal saline. ECG monitoring during transportation help recognize signs of hyperkalemia (peaked T wave, widened QRS > 0,12 с) – inject 10 ml 10% CaCl2.
After the deblocking the limb: If the active movements are impossible, but passive movements are possible (the muscles didn’t become stiff) – tourniquet is not used, if it was applied before you must release it. If arterial bleeding – tourniquet is indicated. If the passive movements are impossible (cadaveric rigidity) – tourniquet is indicated (in the hospital the amputation will be done upper the tourniquet). Transport the victim as soon as possible to the hospital. Call the hospital for preparing the operating room. Anti-shock pants are contraindicated! Shock prevention: horizontal position, oxygen, warming. Rapid infusion of normal saline. ECG monitoring during transportation help recognize signs of hyperkalemia (peaked T wave, widened QRS > 0,12 с) – inject 10 ml 10% CaCl2.
 Crash-syndrome Surgical treatment: The amputation is indicated if the cadaver rigidity takes place (passive movements impossible). Fasciatomy is useful in compartment syndrome. Complications: Acute renal failure – hemodialysis is needed. Infection. Prognosis: Depend on severity of compression and level of medical aid. Mortality – from 0 to 60%. High lethality in aged (>50 years), with concomitant disease and prolonged compression (after the 5 day compression usually no one survives).
Crash-syndrome Surgical treatment: The amputation is indicated if the cadaver rigidity takes place (passive movements impossible). Fasciatomy is useful in compartment syndrome. Complications: Acute renal failure – hemodialysis is needed. Infection. Prognosis: Depend on severity of compression and level of medical aid. Mortality – from 0 to 60%. High lethality in aged (>50 years), with concomitant disease and prolonged compression (after the 5 day compression usually no one survives).
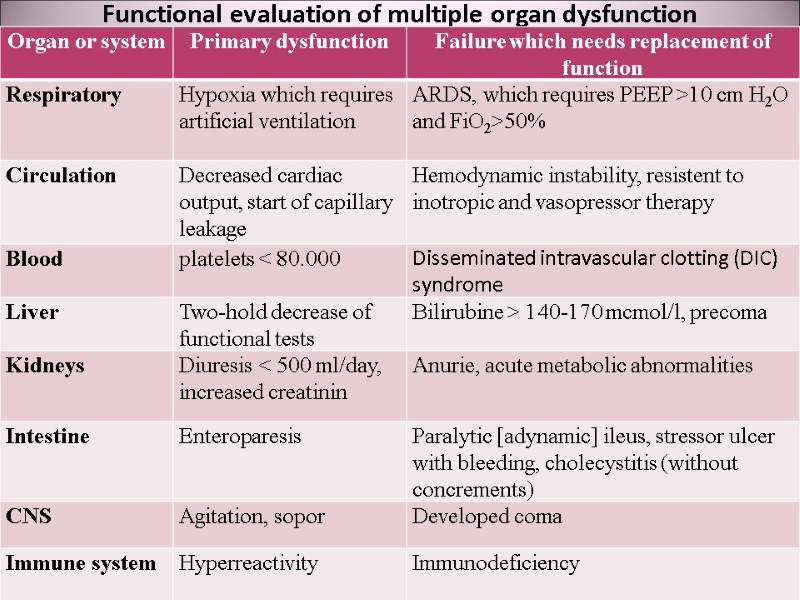
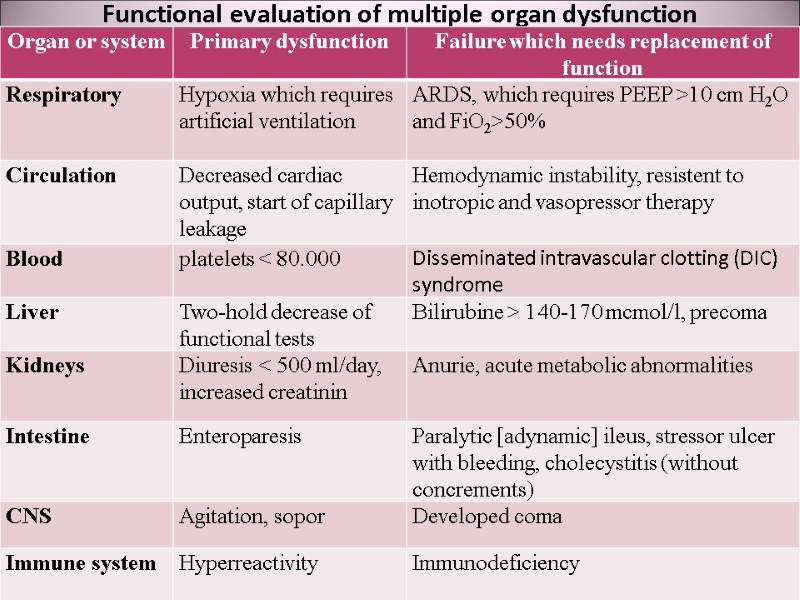 Functional evaluation of multiple organ dysfunction
Functional evaluation of multiple organ dysfunction
 Causes of cardiac and vessel obstruction in chest trauma: Cardiac tamponade Tension pneumothorax
Causes of cardiac and vessel obstruction in chest trauma: Cardiac tamponade Tension pneumothorax
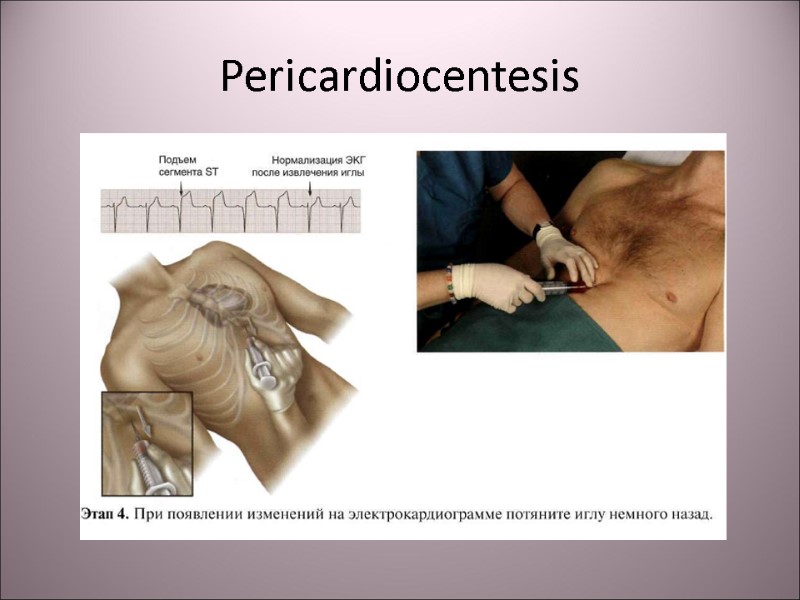
 Cardiac tamponade Accumulation of blood in pericardium can lead to acute cardiac tamponade with failure Often present in penetrating wound or aneurism rupture. Increasing pressure in pericardium decreases systolic cardiac volume and cardiac output.
Cardiac tamponade Accumulation of blood in pericardium can lead to acute cardiac tamponade with failure Often present in penetrating wound or aneurism rupture. Increasing pressure in pericardium decreases systolic cardiac volume and cardiac output.
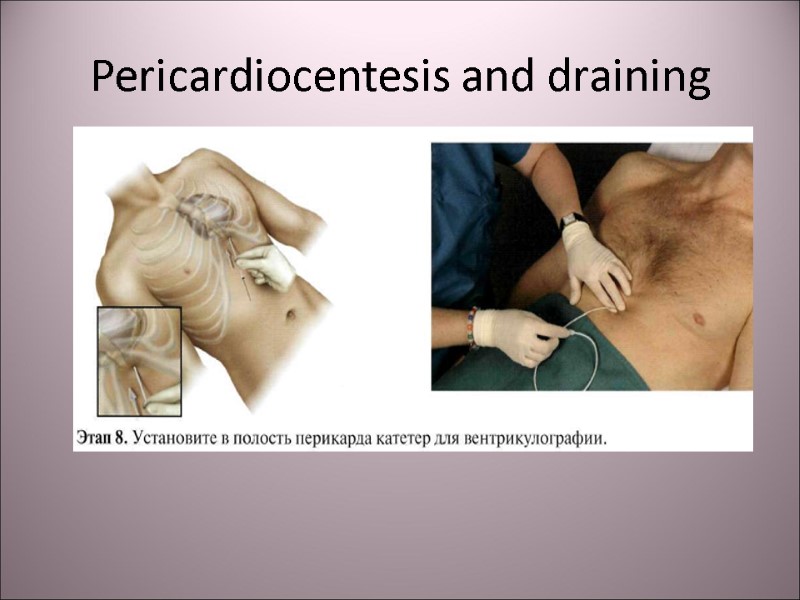
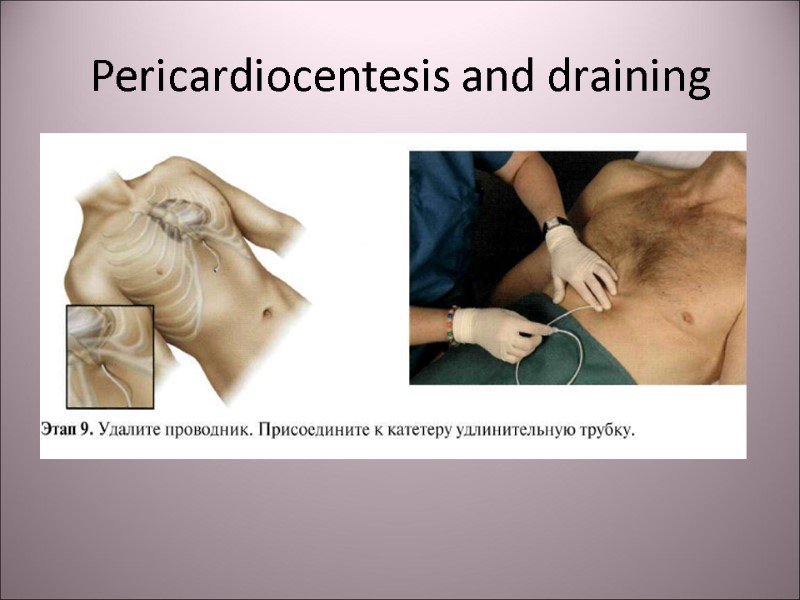
 Cardiac tamponade Clinical signs: weakness, cyanosis, decreased BP, tachycardia, increased CVP (inflated neck veins) and widened heart shadow on XR or on percussion. Emergency: pericardiocentesis and draining, treatment of shock.
Cardiac tamponade Clinical signs: weakness, cyanosis, decreased BP, tachycardia, increased CVP (inflated neck veins) and widened heart shadow on XR or on percussion. Emergency: pericardiocentesis and draining, treatment of shock.
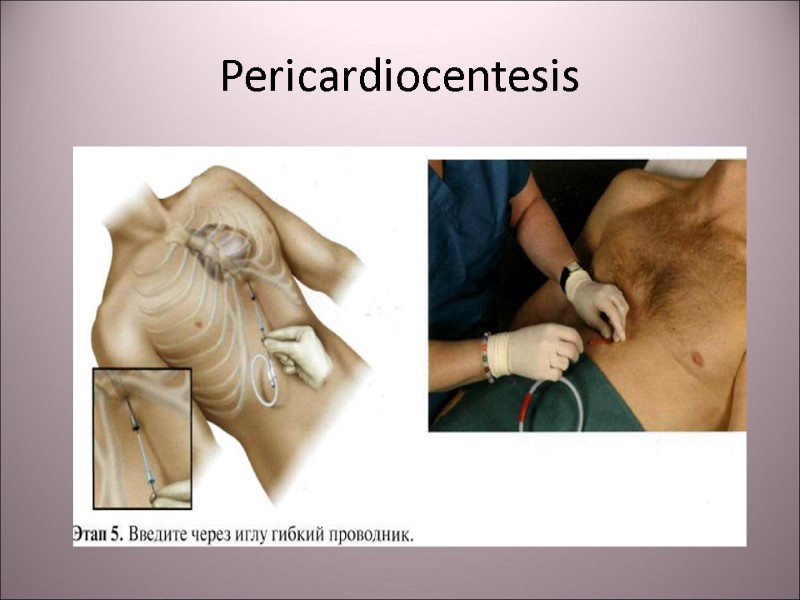
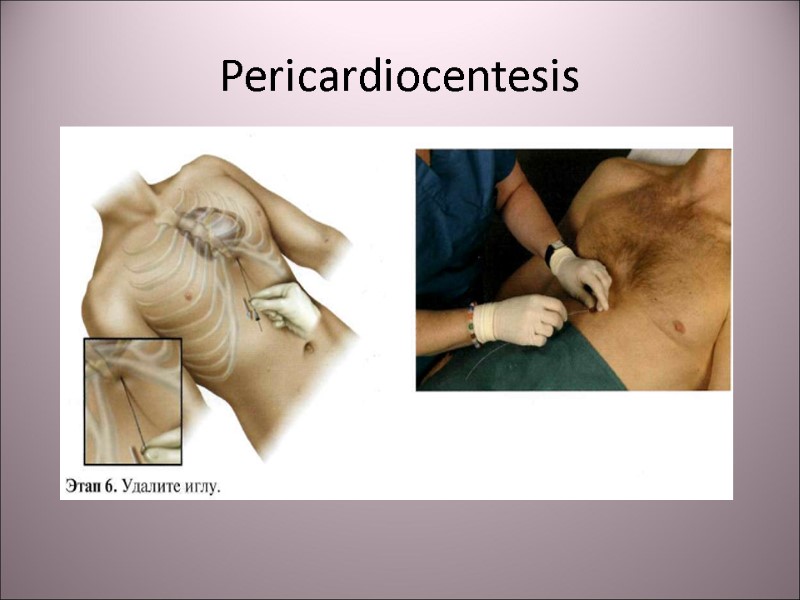
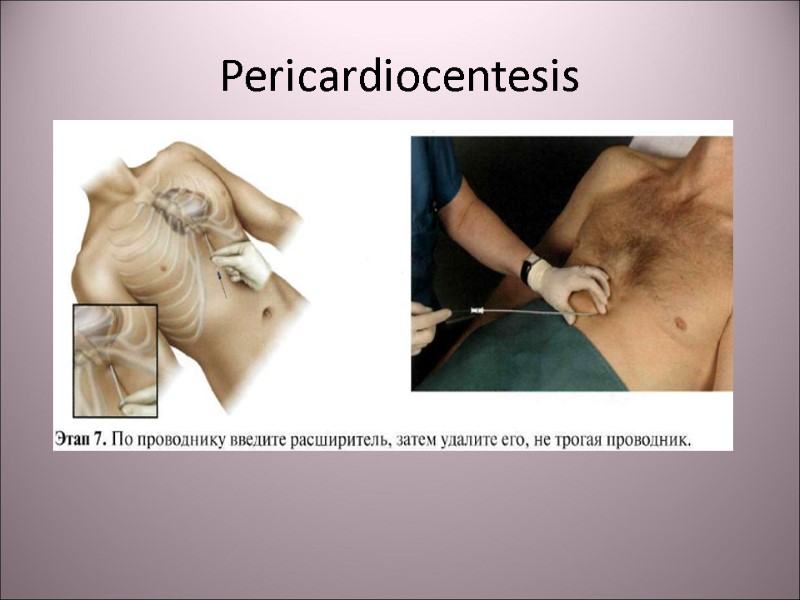
 Pericardiocentesis
Pericardiocentesis
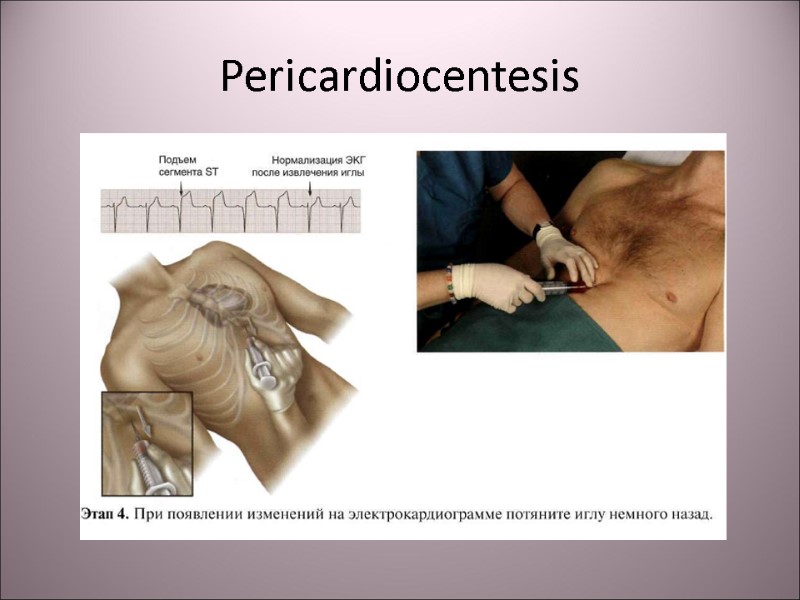 Pericardiocentesis
Pericardiocentesis
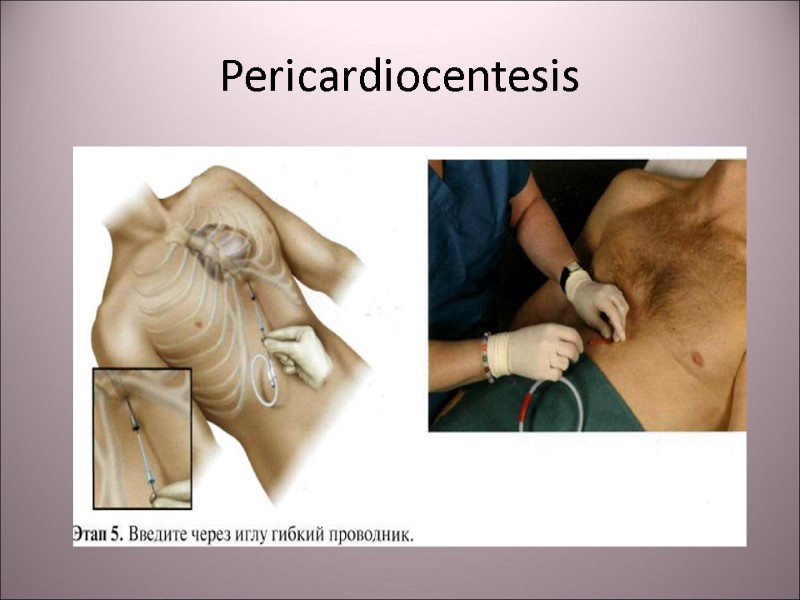 Pericardiocentesis
Pericardiocentesis
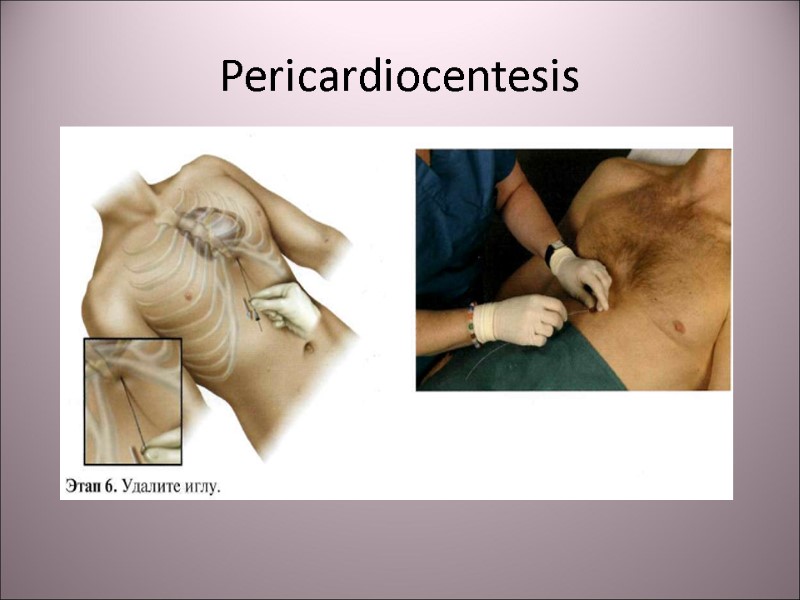 Pericardiocentesis
Pericardiocentesis
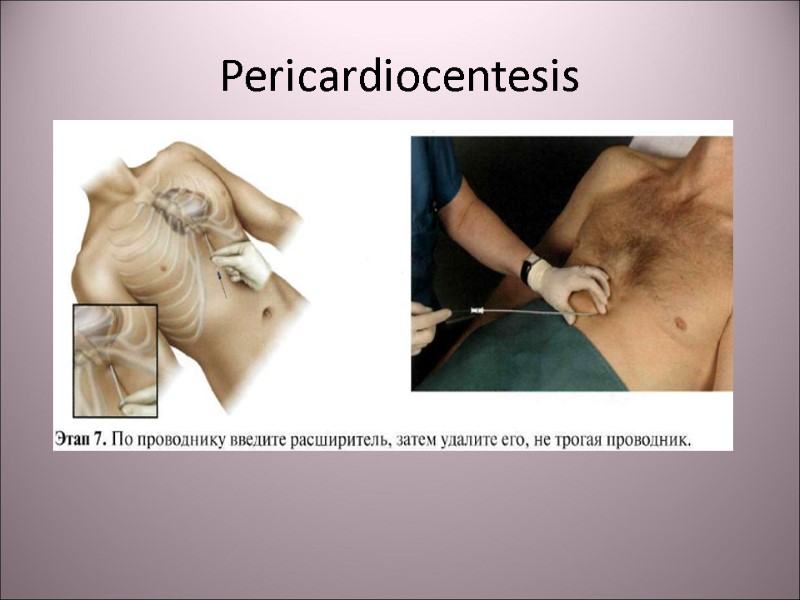 Pericardiocentesis
Pericardiocentesis
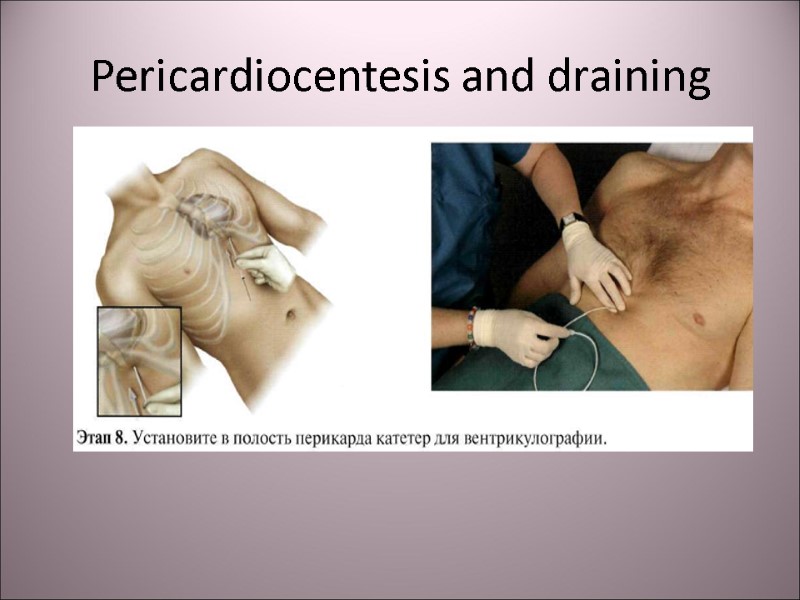 Pericardiocentesis and draining
Pericardiocentesis and draining
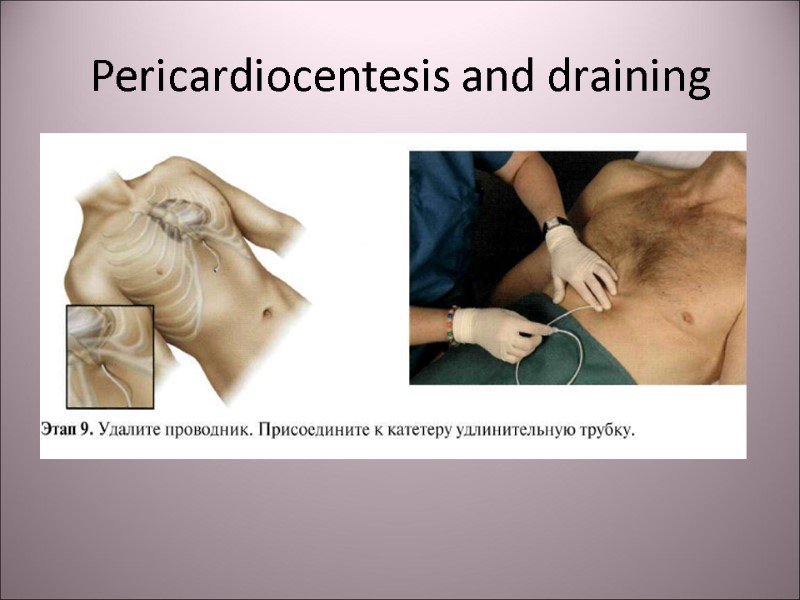 Pericardiocentesis and draining
Pericardiocentesis and draining
 Pneumothorax Pneumothorax – air accumulation in pleural cavity due to defect of lung parenchyma or thoracic wall. Clinically apparent pneumathorax can lead to pulmonary collapse (atelectasis) and deviation of mediastinum to the intact side.
Pneumothorax Pneumothorax – air accumulation in pleural cavity due to defect of lung parenchyma or thoracic wall. Clinically apparent pneumathorax can lead to pulmonary collapse (atelectasis) and deviation of mediastinum to the intact side.
 Traumatic pneumothorax The frequent complication of chest trauma with the fracture of ribs.
Traumatic pneumothorax The frequent complication of chest trauma with the fracture of ribs.
 Open and closed pneumothorax The result of penetrating chest trauma with the connection between the atmospheric air and pleural cavity. Valvular pneumothorax is the variety of open pneumothorax: soft tissues form the valve, lacing the air during inspiration into the pleural cavity and closing the connection during expiration.
Open and closed pneumothorax The result of penetrating chest trauma with the connection between the atmospheric air and pleural cavity. Valvular pneumothorax is the variety of open pneumothorax: soft tissues form the valve, lacing the air during inspiration into the pleural cavity and closing the connection during expiration.
 Clinical signs of pneumothorax Dyspnea, cyanosis, rapid respirations. On auscultation: respiration sounds are absent on the affected side of thorax. On percussion: tympanitis on the affected side, deviation of mediastinum to the intact side. Tension pneumothorax leads to arterial hypotension due to decreasing in cardiac input.
Clinical signs of pneumothorax Dyspnea, cyanosis, rapid respirations. On auscultation: respiration sounds are absent on the affected side of thorax. On percussion: tympanitis on the affected side, deviation of mediastinum to the intact side. Tension pneumothorax leads to arterial hypotension due to decreasing in cardiac input.
 Urgent management in pneumothorax Wound washing and apply occlusive aseptic bulky dressing on the wound. The adhesive plaster is used for hermetically closing the penetrating wound. Transportation in sitting position with the oxygen inhalation. Non-narcotic analgesics.
Urgent management in pneumothorax Wound washing and apply occlusive aseptic bulky dressing on the wound. The adhesive plaster is used for hermetically closing the penetrating wound. Transportation in sitting position with the oxygen inhalation. Non-narcotic analgesics.
 Urgent thoracocentesis The urgent pleural puncture is provided in the 2-nd or 3-id intercostal space on the mediaclavicular line in sitting position. After the antiseptic washing under the local anesthesia the needle must penetrate the thoracic wall close to the upper border of rib.
Urgent thoracocentesis The urgent pleural puncture is provided in the 2-nd or 3-id intercostal space on the mediaclavicular line in sitting position. After the antiseptic washing under the local anesthesia the needle must penetrate the thoracic wall close to the upper border of rib.
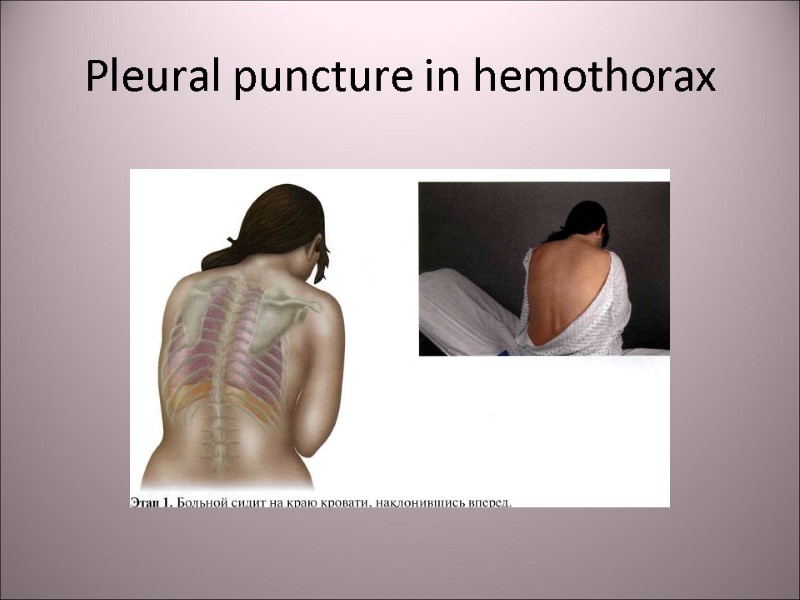
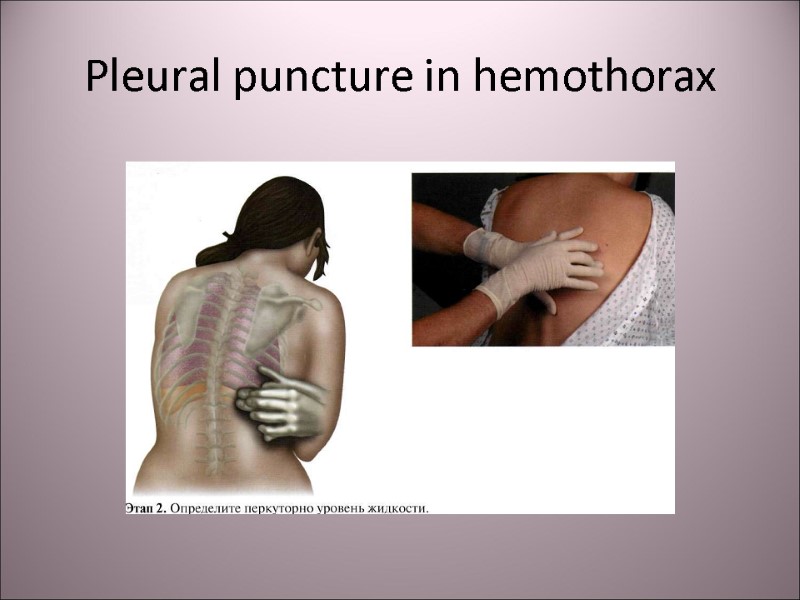
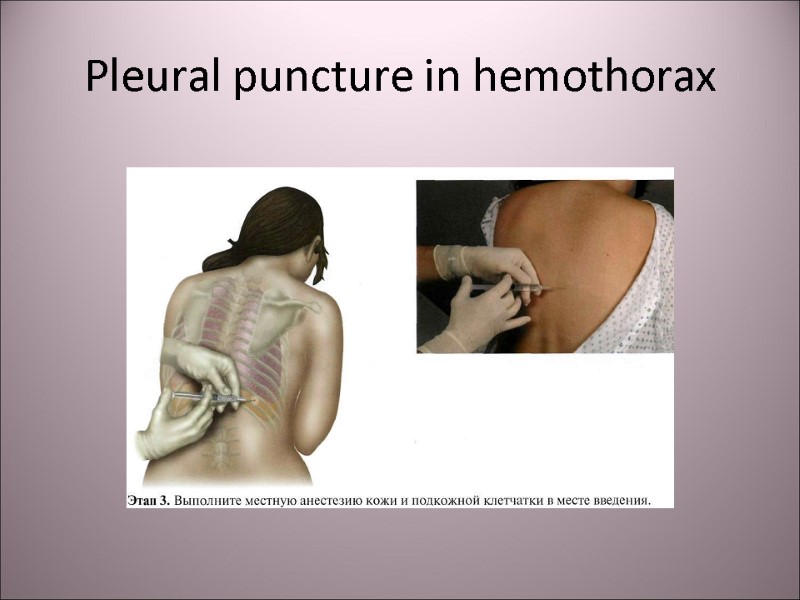
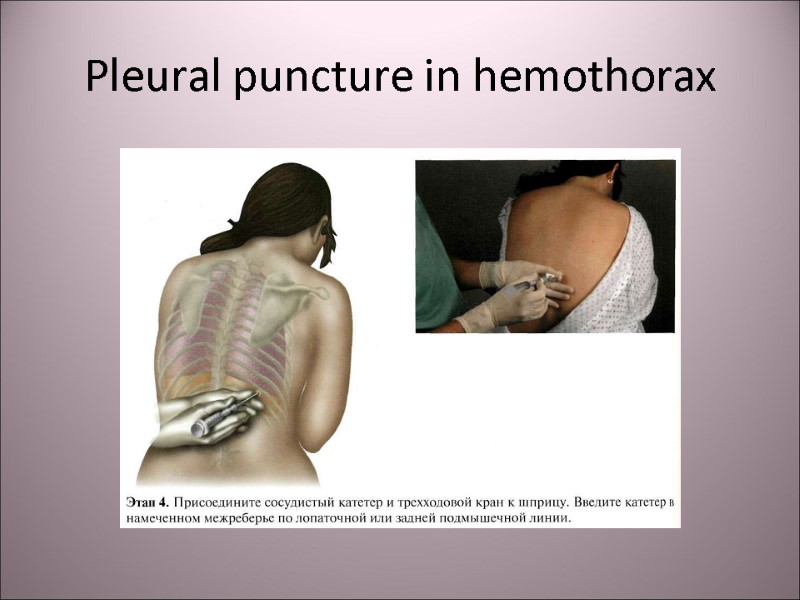
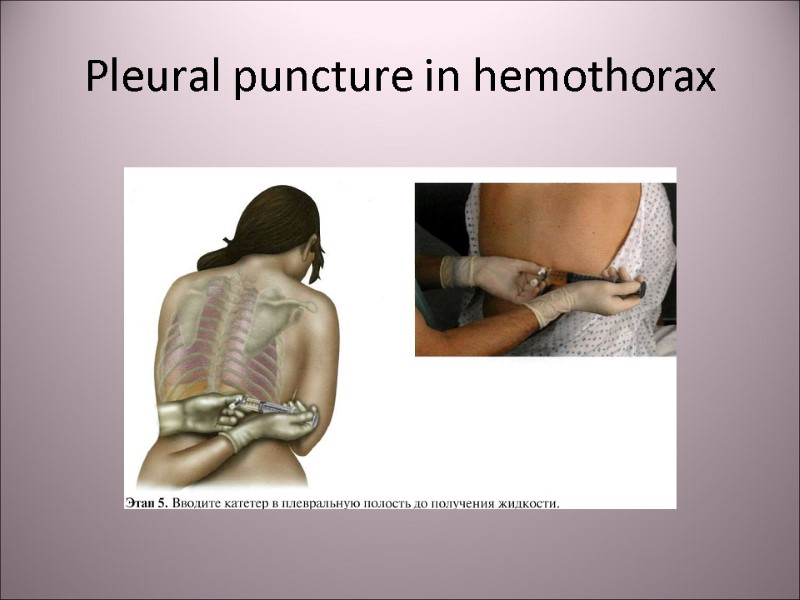
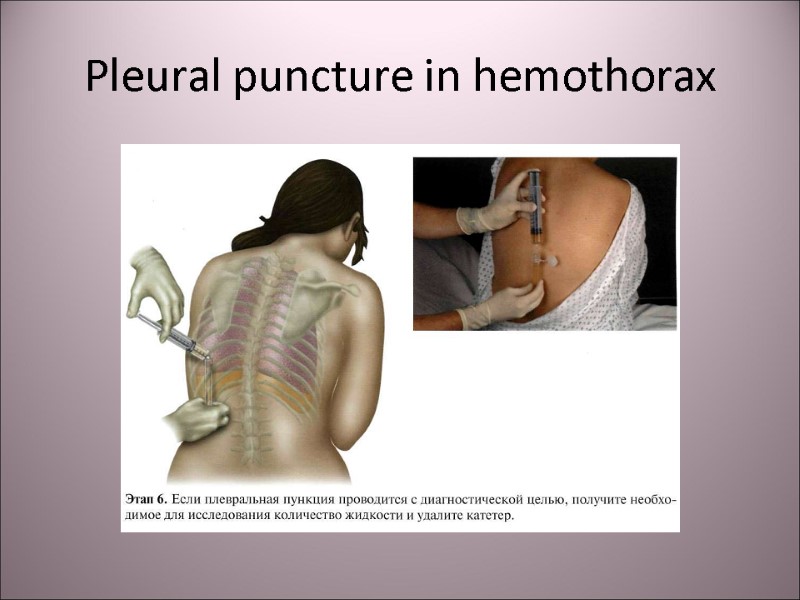
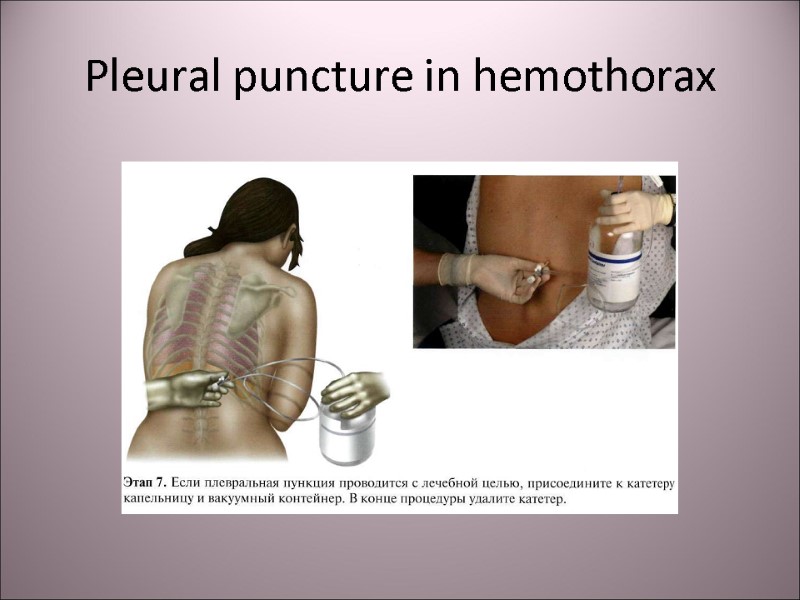
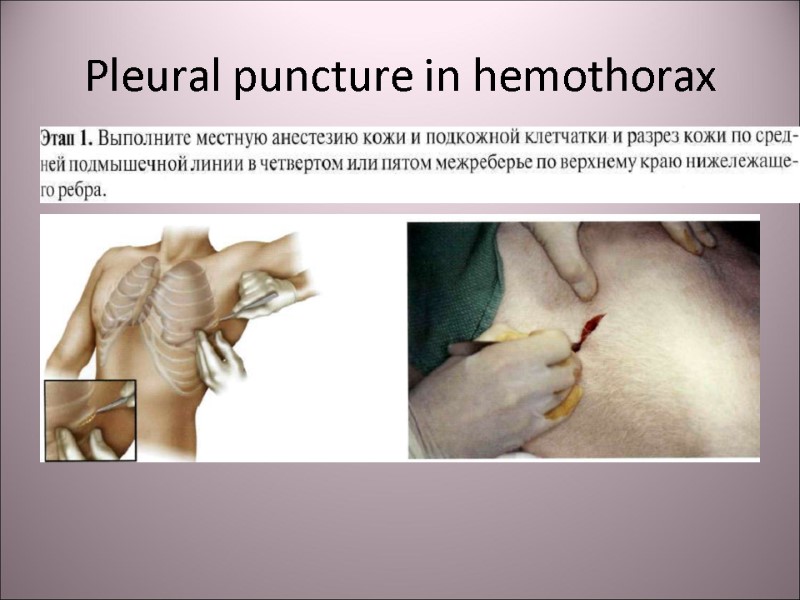
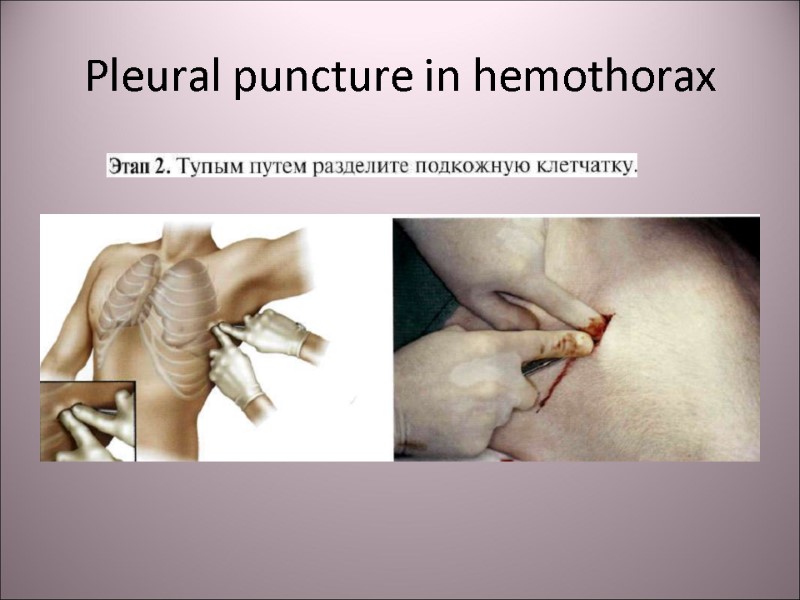
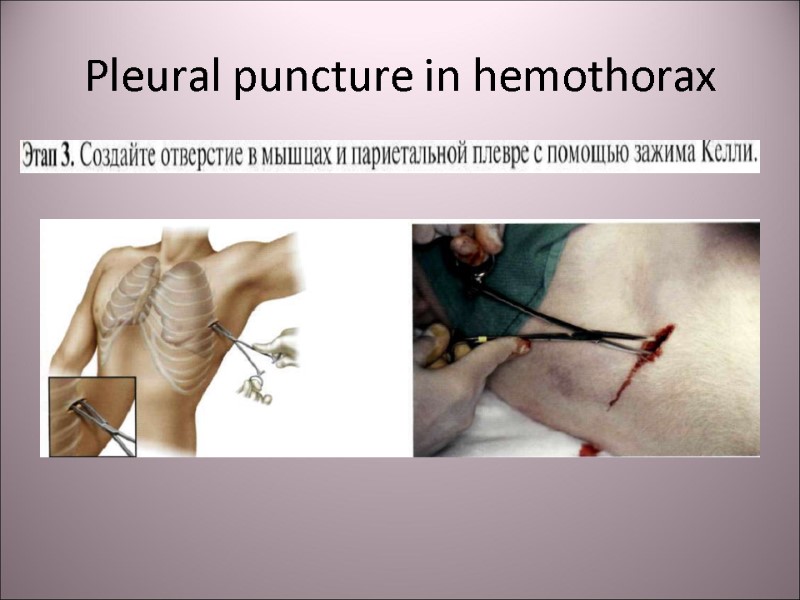
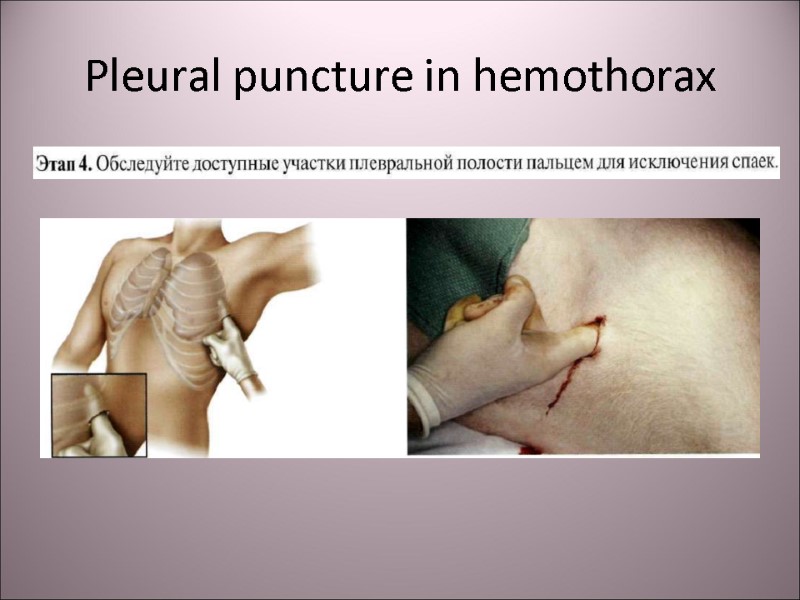
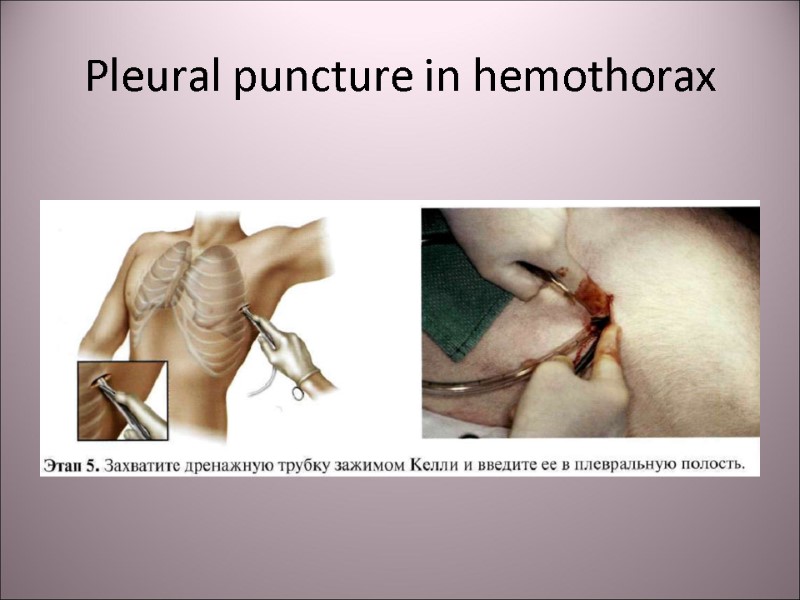
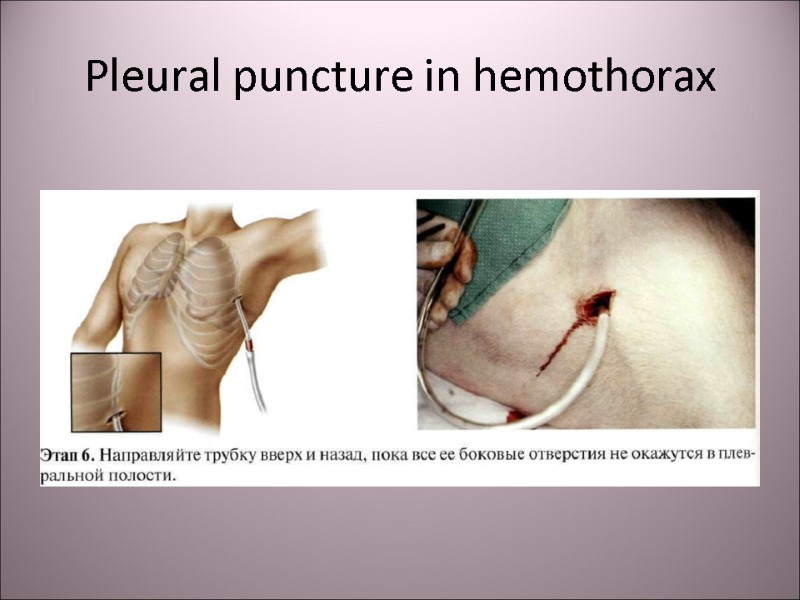
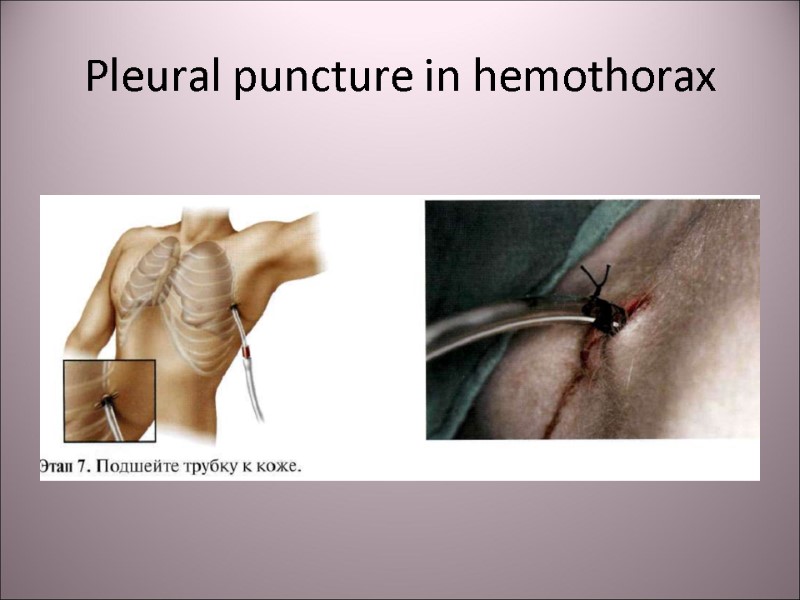
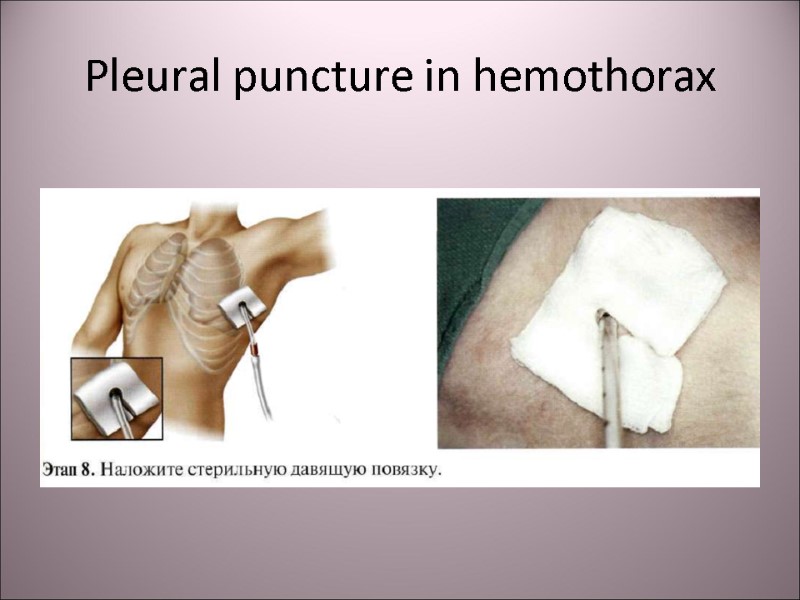
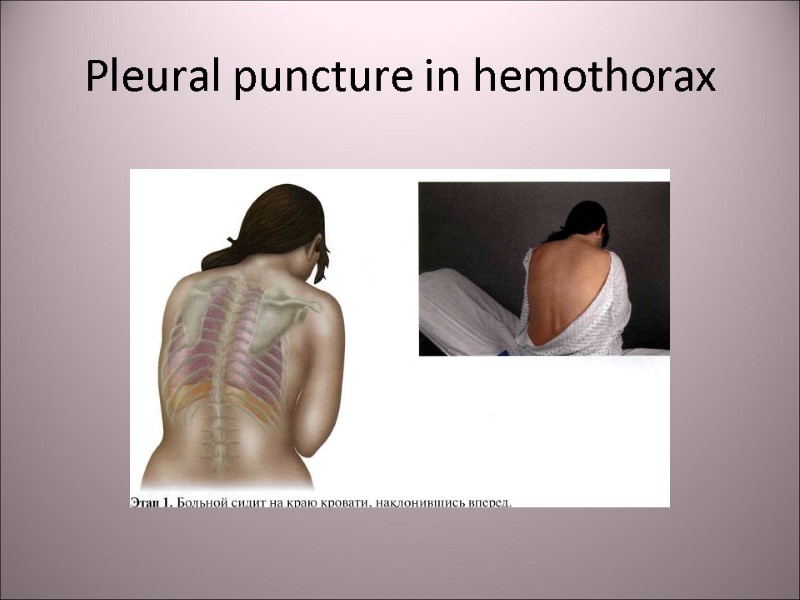 Pleural puncture in hemothorax
Pleural puncture in hemothorax
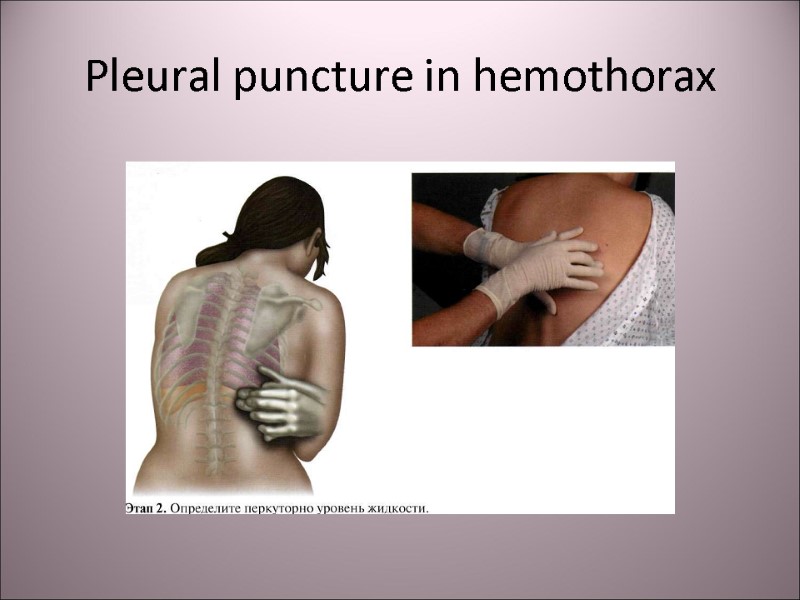 Pleural puncture in hemothorax
Pleural puncture in hemothorax
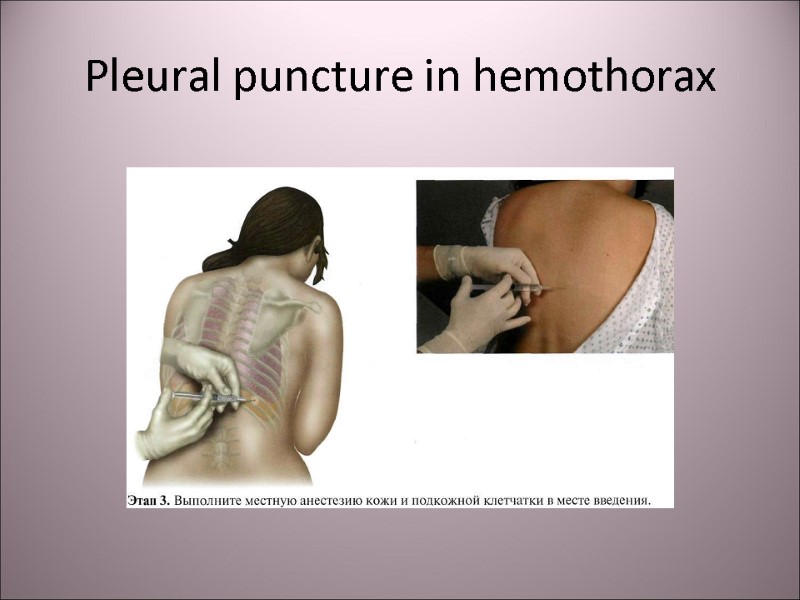 Pleural puncture in hemothorax
Pleural puncture in hemothorax
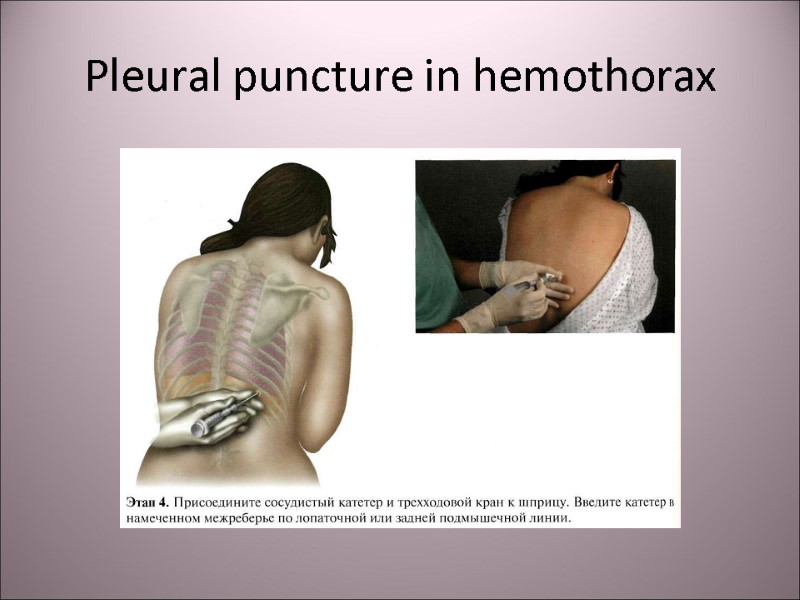 Pleural puncture in hemothorax
Pleural puncture in hemothorax
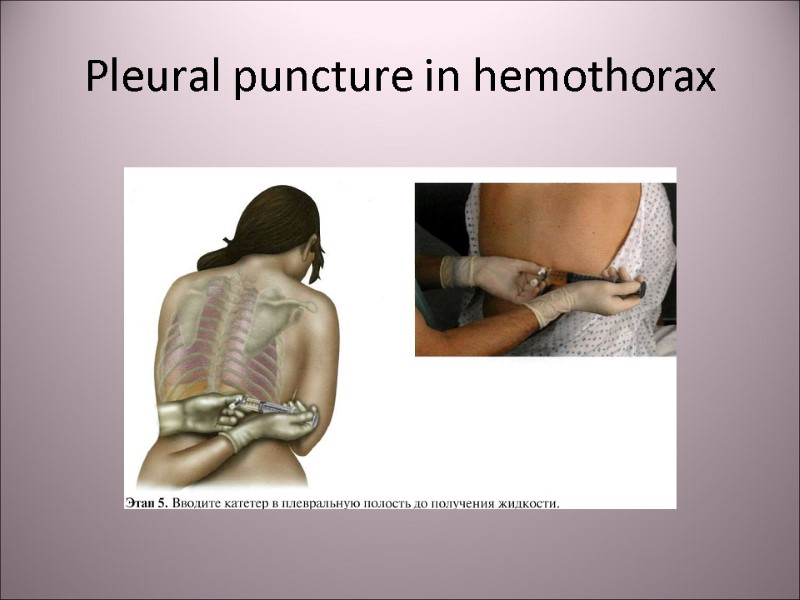 Pleural puncture in hemothorax
Pleural puncture in hemothorax
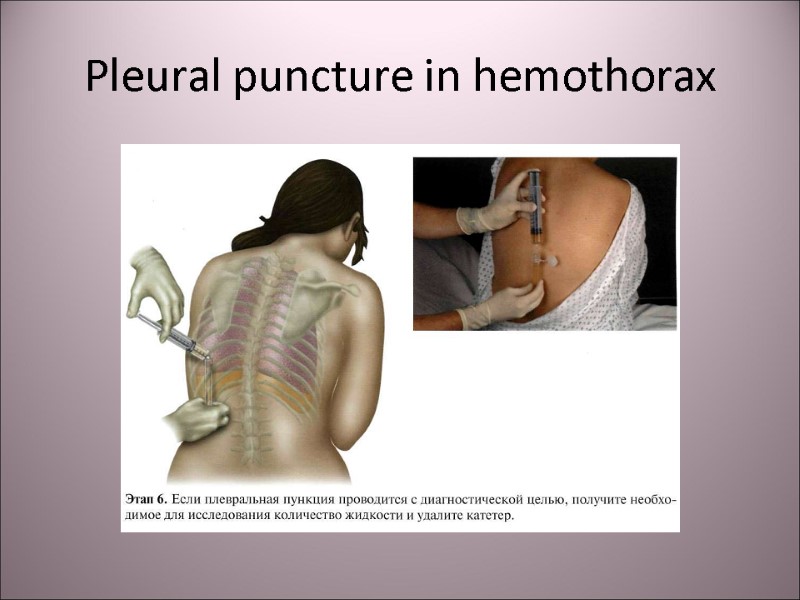 Pleural puncture in hemothorax
Pleural puncture in hemothorax
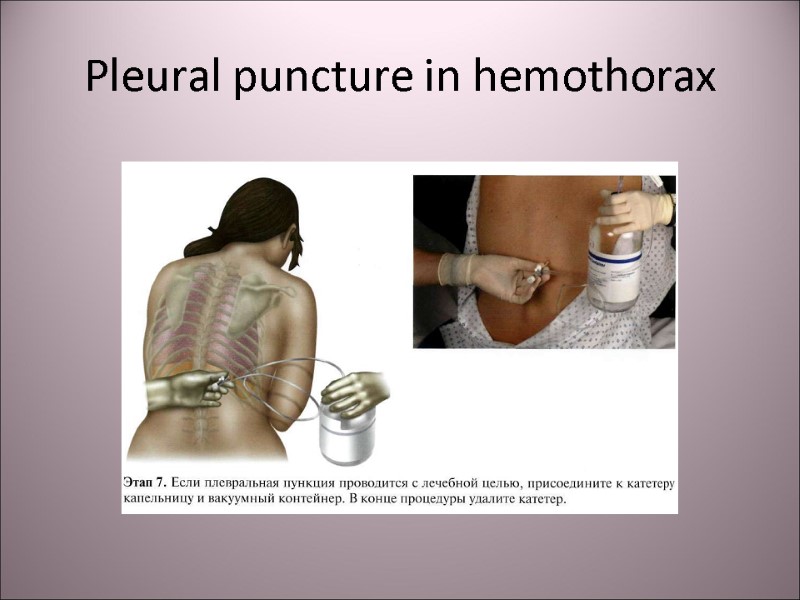 Pleural puncture in hemothorax
Pleural puncture in hemothorax
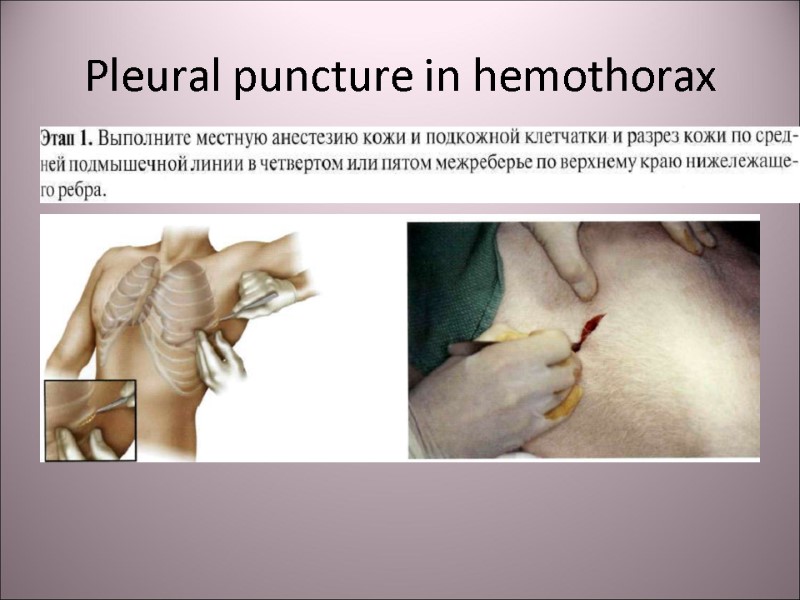 Pleural puncture in hemothorax
Pleural puncture in hemothorax
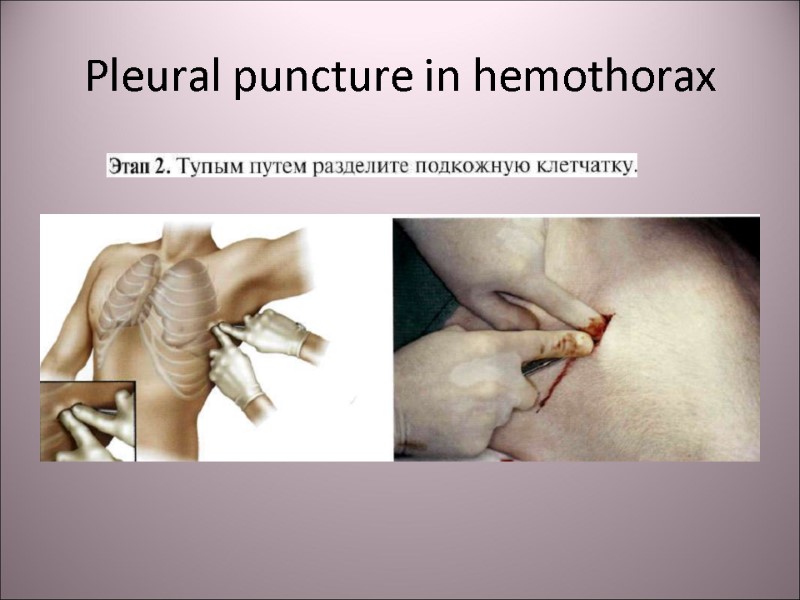 Pleural puncture in hemothorax
Pleural puncture in hemothorax
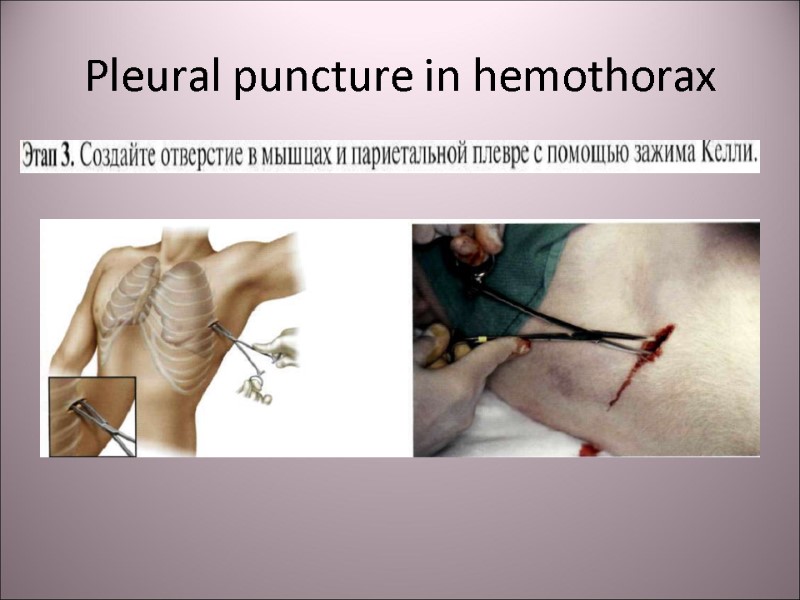 Pleural puncture in hemothorax
Pleural puncture in hemothorax
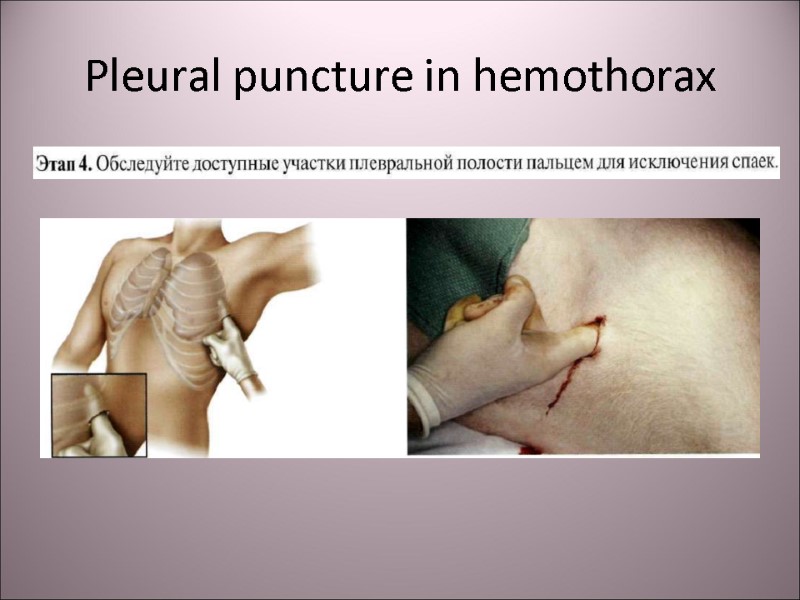 Pleural puncture in hemothorax
Pleural puncture in hemothorax
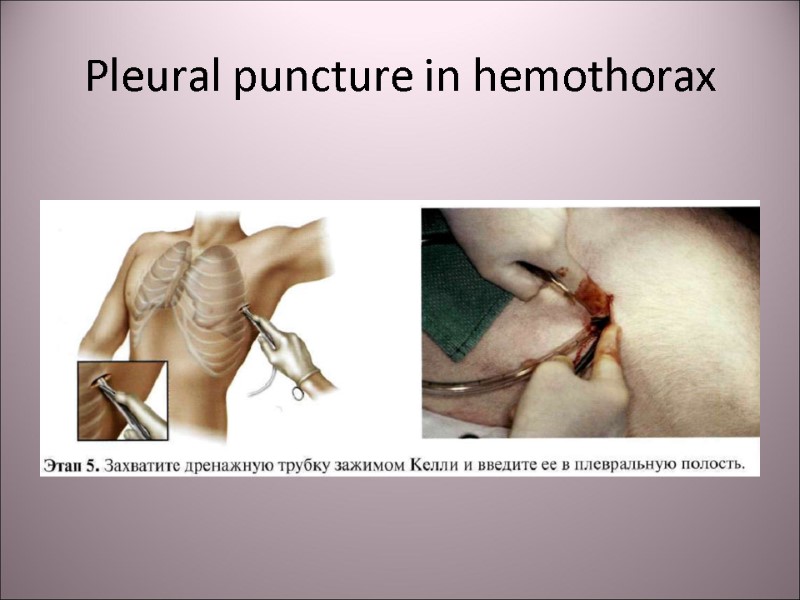 Pleural puncture in hemothorax
Pleural puncture in hemothorax
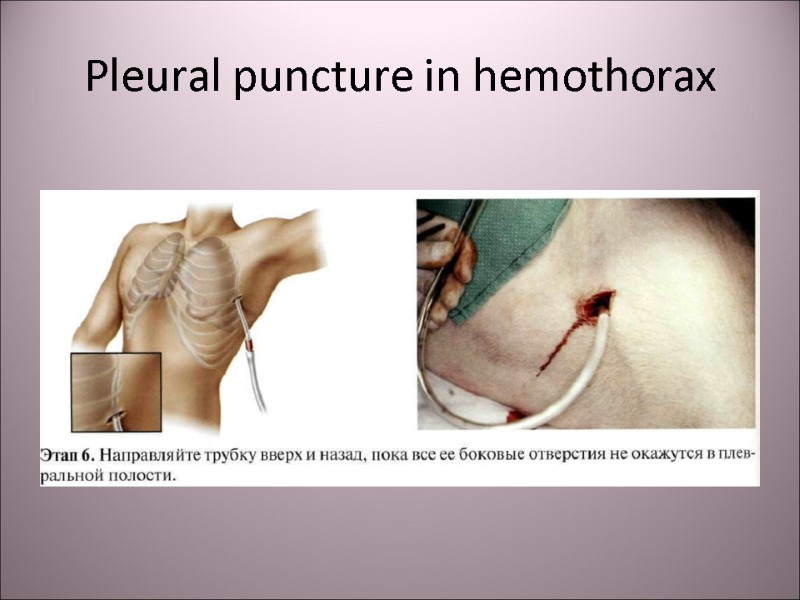 Pleural puncture in hemothorax
Pleural puncture in hemothorax
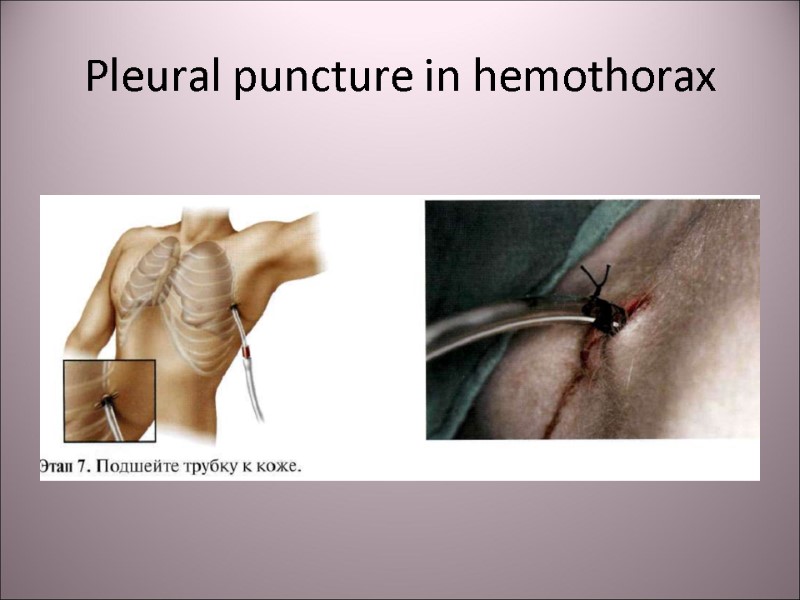 Pleural puncture in hemothorax
Pleural puncture in hemothorax
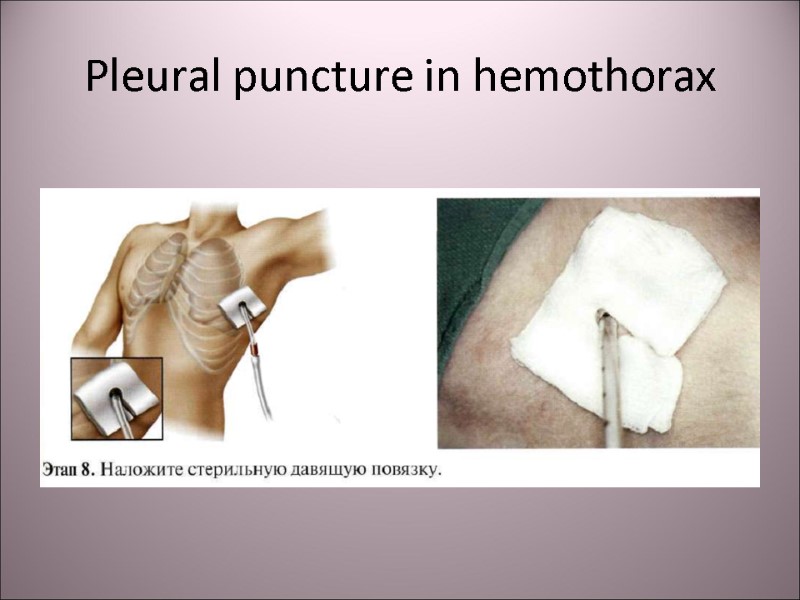 Pleural puncture in hemothorax
Pleural puncture in hemothorax
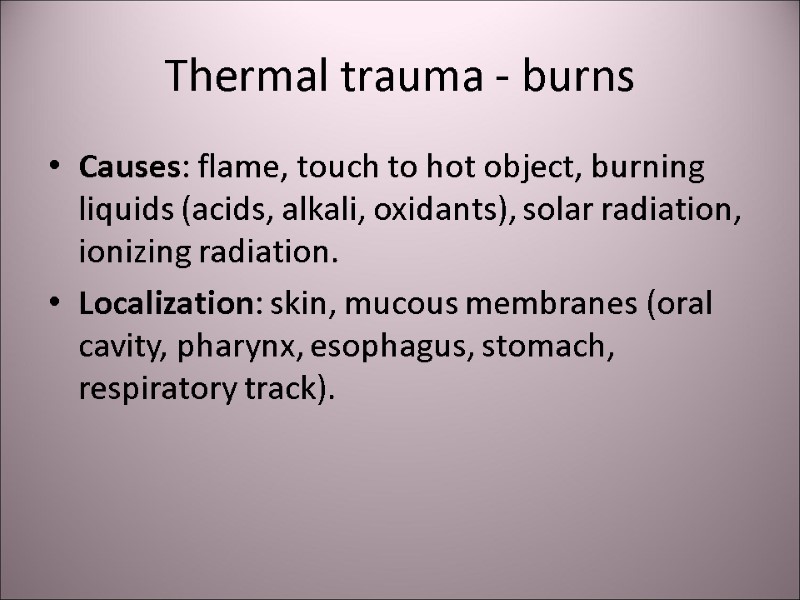
 Thermal trauma - burns Causes: flame, touch to hot object, burning liquids (acids, alkali, oxidants), solar radiation, ionizing radiation. Localization: skin, mucous membranes (oral cavity, pharynx, esophagus, stomach, respiratory track).
Thermal trauma - burns Causes: flame, touch to hot object, burning liquids (acids, alkali, oxidants), solar radiation, ionizing radiation. Localization: skin, mucous membranes (oral cavity, pharynx, esophagus, stomach, respiratory track).
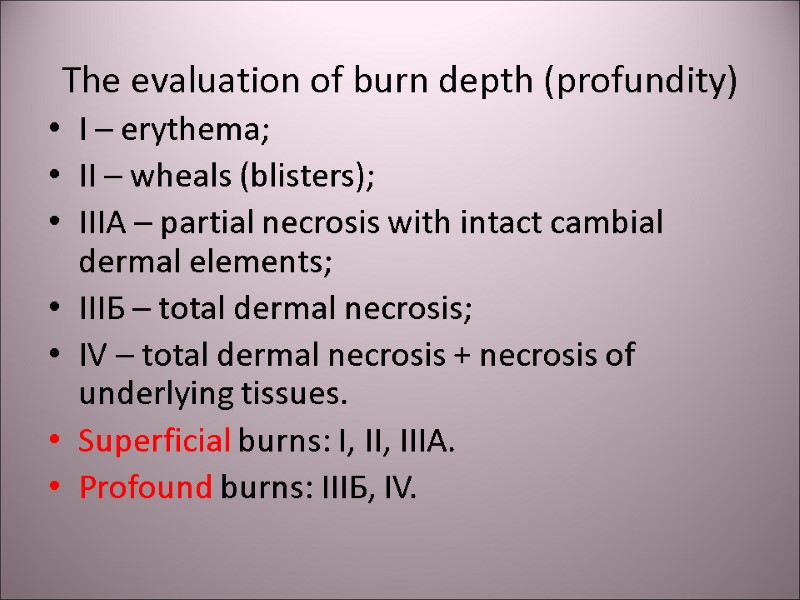
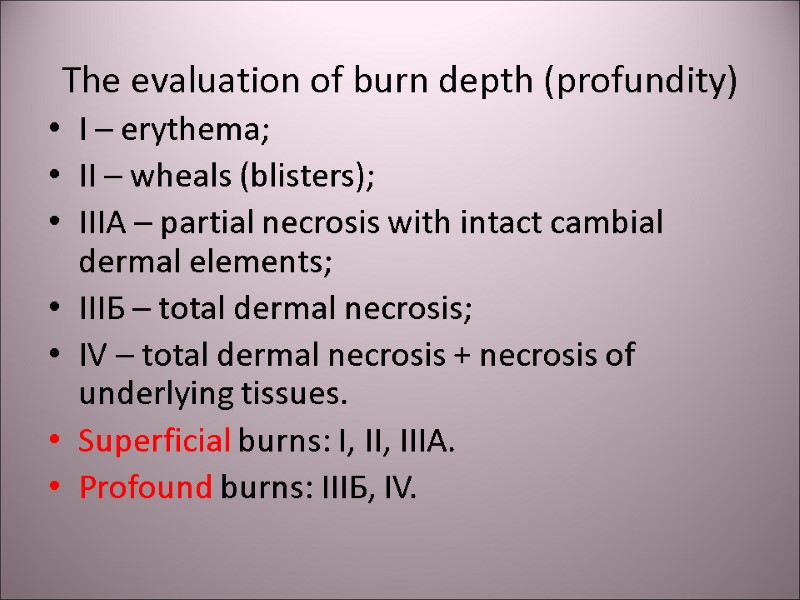 The evaluation of burn depth (profundity) I – erythema; II – wheals (blisters); IIIА – partial necrosis with intact cambial dermal elements; IIIБ – total dermal necrosis; IV – total dermal necrosis + necrosis of underlying tissues. Superficial burns: I, II, IIIА. Profound burns: IIIБ, IV.
The evaluation of burn depth (profundity) I – erythema; II – wheals (blisters); IIIА – partial necrosis with intact cambial dermal elements; IIIБ – total dermal necrosis; IV – total dermal necrosis + necrosis of underlying tissues. Superficial burns: I, II, IIIА. Profound burns: IIIБ, IV.
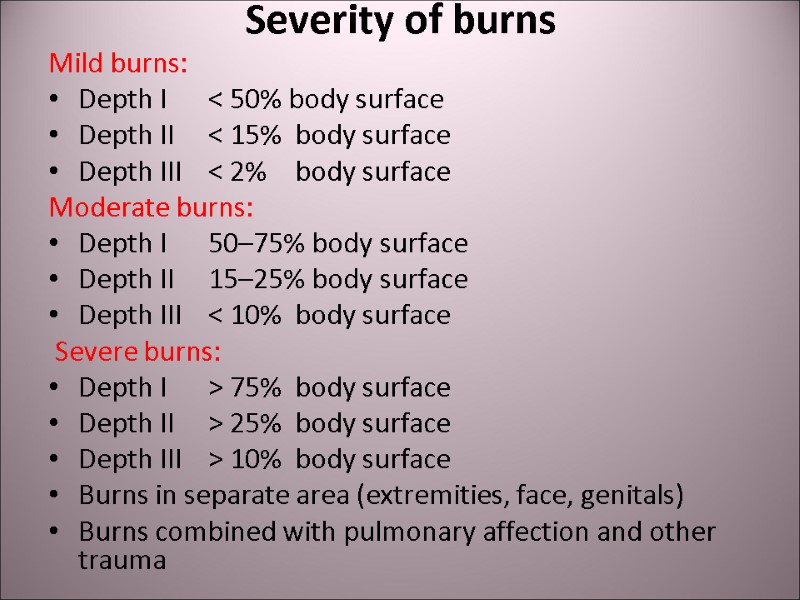
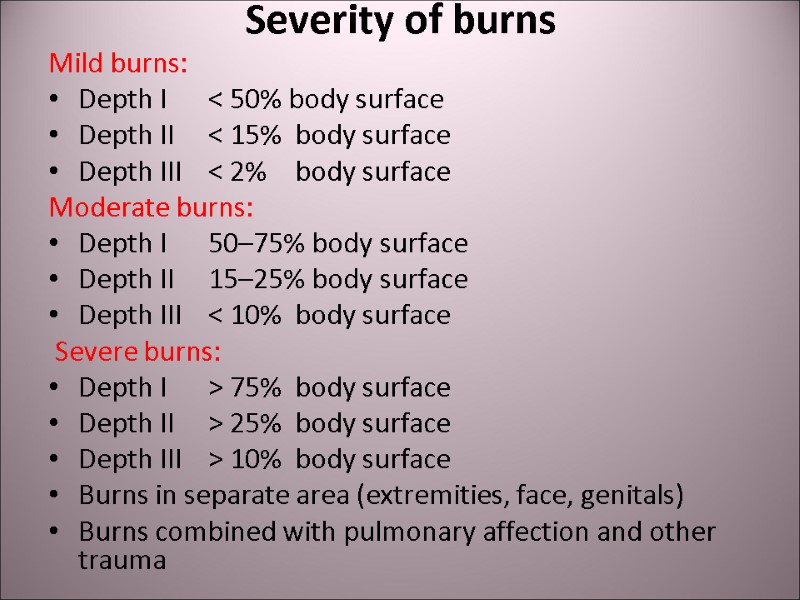 Severity of burns Mild burns: Depth I < 50% body surface Depth II < 15% body surface Depth III < 2% body surface Moderate burns: Depth I 50–75% body surface Depth II 15–25% body surface Depth III < 10% body surface Severe burns: Depth I > 75% body surface Depth II > 25% body surface Depth III > 10% body surface Burns in separate area (extremities, face, genitals) Burns combined with pulmonary affection and other trauma
Severity of burns Mild burns: Depth I < 50% body surface Depth II < 15% body surface Depth III < 2% body surface Moderate burns: Depth I 50–75% body surface Depth II 15–25% body surface Depth III < 10% body surface Severe burns: Depth I > 75% body surface Depth II > 25% body surface Depth III > 10% body surface Burns in separate area (extremities, face, genitals) Burns combined with pulmonary affection and other trauma
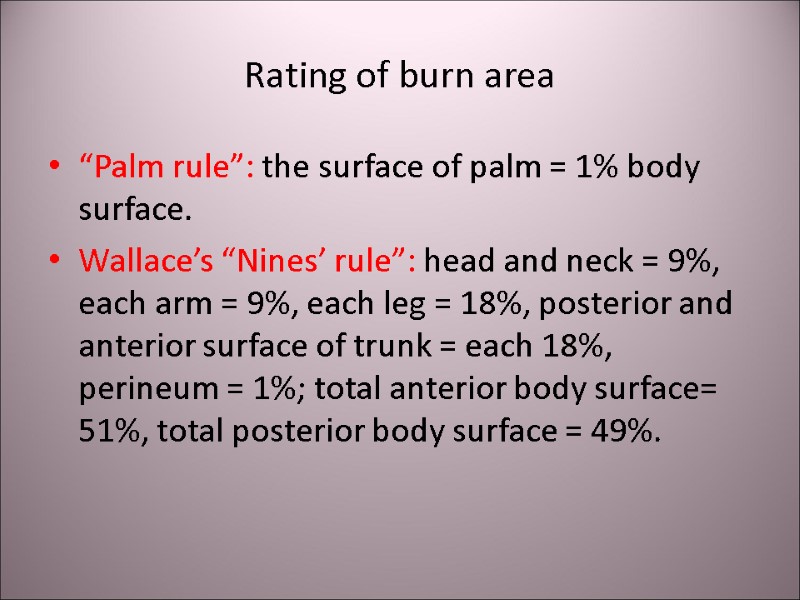
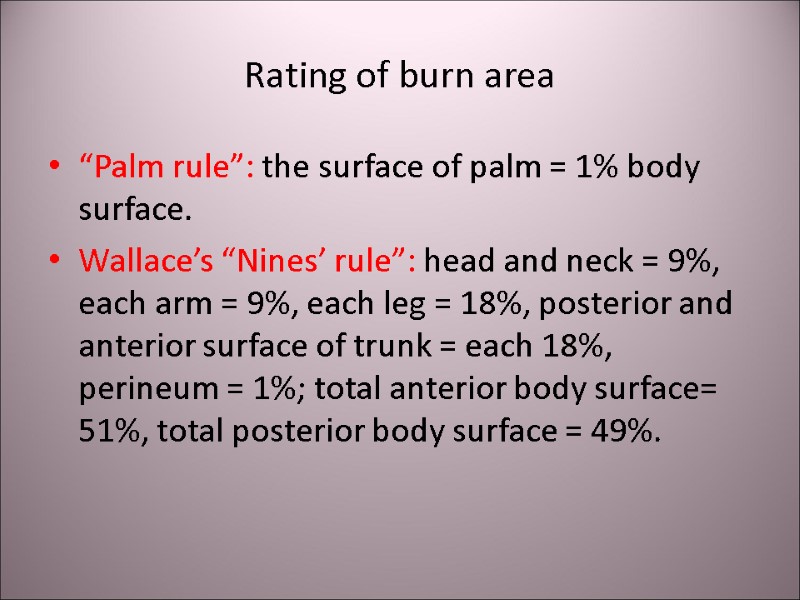 Rating of burn area “Palm rule”: the surface of palm = 1% body surface. Wallace’s “Nines’ rule”: head and neck = 9%, each arm = 9%, each leg = 18%, posterior and anterior surface of trunk = each 18%, perineum = 1%; total anterior body surface= 51%, total posterior body surface = 49%.
Rating of burn area “Palm rule”: the surface of palm = 1% body surface. Wallace’s “Nines’ rule”: head and neck = 9%, each arm = 9%, each leg = 18%, posterior and anterior surface of trunk = each 18%, perineum = 1%; total anterior body surface= 51%, total posterior body surface = 49%.
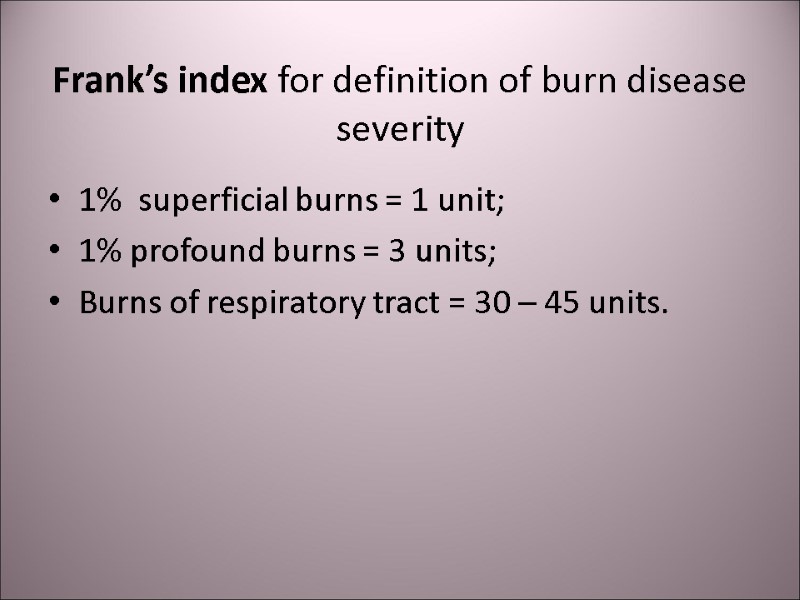
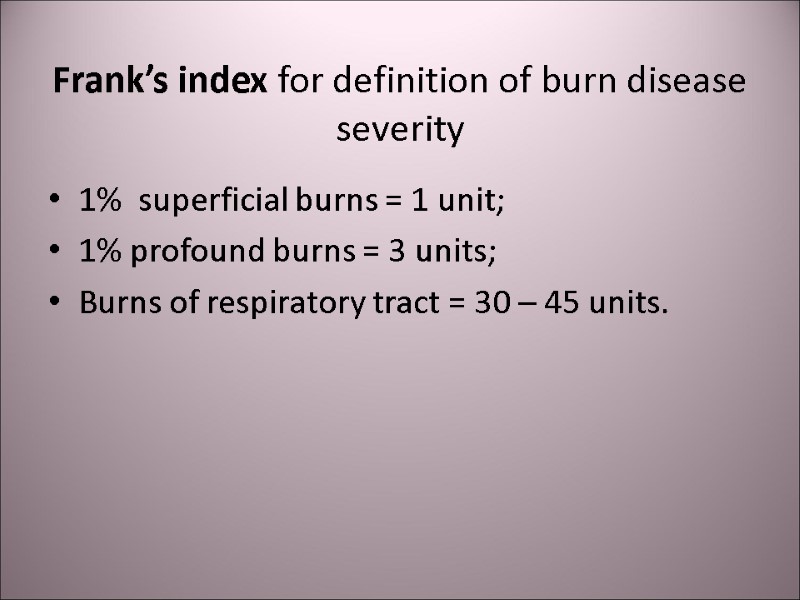 Frank’s index for definition of burn disease severity 1% superficial burns = 1 unit; 1% profound burns = 3 units; Burns of respiratory tract = 30 – 45 units.
Frank’s index for definition of burn disease severity 1% superficial burns = 1 unit; 1% profound burns = 3 units; Burns of respiratory tract = 30 – 45 units.
 Mild burn disease (Frank’s index < 30 units): Euphoria, agitation, paleness and gooseflesh (cutis anserina) in intact area, chill, short breath, tachycardia 100 – 120 per min, BP is normal or slightly increased.
Mild burn disease (Frank’s index < 30 units): Euphoria, agitation, paleness and gooseflesh (cutis anserina) in intact area, chill, short breath, tachycardia 100 – 120 per min, BP is normal or slightly increased.
 Moderate burn disease (Frank’s index = 31 – 60 units) and severe burn disease (Frank’s index = 61 – 90 units): CNS depression, pain, shivering, thirst, nausea, vomiting, hypothermia, dry skin (xeroderma) in intact area, tachypnoe, tachycardia 120 – 140 per min, moderate decrease of BP.
Moderate burn disease (Frank’s index = 31 – 60 units) and severe burn disease (Frank’s index = 61 – 90 units): CNS depression, pain, shivering, thirst, nausea, vomiting, hypothermia, dry skin (xeroderma) in intact area, tachypnoe, tachycardia 120 – 140 per min, moderate decrease of BP.
 Extreme burn shock (Frank’s index > 90 units): Unconsciousness, unquenchable thirst, uncontrollable vomiting, paleness with mottled skin (cutis marmorata) in intact area, acracyanosis, tachycardia > 140 per min, thready pulse, BPs < 100 mm Hg.
Extreme burn shock (Frank’s index > 90 units): Unconsciousness, unquenchable thirst, uncontrollable vomiting, paleness with mottled skin (cutis marmorata) in intact area, acracyanosis, tachycardia > 140 per min, thready pulse, BPs < 100 mm Hg.
 Emergency care in burns: Stop burning: cover firing surface with dense rag for stopping the access for air. Cooling the burned surface with cool water, ice, snow. Take out the victim from the zone of high temperature. Take off the firing clothes. Cover the victim with blanket to prevent undercooling. Adherent parts of clothes should be left under the aseptic wound dressing before surgical treatment. Apply the aseptic bandage wetted with anti-burn liquid on the burned surface. In acid burn – the bandage should be wetted with 3% Na hydrocarbonate, in alkali burn – 1 – 3% acetic or citric acid, in phosphoric burn – 5% copper sulfate.
Emergency care in burns: Stop burning: cover firing surface with dense rag for stopping the access for air. Cooling the burned surface with cool water, ice, snow. Take out the victim from the zone of high temperature. Take off the firing clothes. Cover the victim with blanket to prevent undercooling. Adherent parts of clothes should be left under the aseptic wound dressing before surgical treatment. Apply the aseptic bandage wetted with anti-burn liquid on the burned surface. In acid burn – the bandage should be wetted with 3% Na hydrocarbonate, in alkali burn – 1 – 3% acetic or citric acid, in phosphoric burn – 5% copper sulfate.
 Emergency care in burns: Canulate the vein, Begin crystalloid infusion, Analgesia, Oxygen inhalation, Vasopressors if indicated, Sparing transportation to the burn center.
Emergency care in burns: Canulate the vein, Begin crystalloid infusion, Analgesia, Oxygen inhalation, Vasopressors if indicated, Sparing transportation to the burn center.
 Infusion therapy in burn shock Parklend’s rule: Ringer-lactate (4 ml/kg/% burn) infusion volume for the 1-st day. 50% of this volume – during the first 8 hours, 50% - for the next 16 hours. The 2-nd day – 5% dextrose and albumine. Evans’s rule: The 1-st day – crystalloides and colloides 1 ml/kg/% burn each + 2000 ml 5% dextrose. The 2-nd day – crystalloides and colloides 0,5 ml/kg/% burn each + 2000 ml 5% dextrose.
Infusion therapy in burn shock Parklend’s rule: Ringer-lactate (4 ml/kg/% burn) infusion volume for the 1-st day. 50% of this volume – during the first 8 hours, 50% - for the next 16 hours. The 2-nd day – 5% dextrose and albumine. Evans’s rule: The 1-st day – crystalloides and colloides 1 ml/kg/% burn each + 2000 ml 5% dextrose. The 2-nd day – crystalloides and colloides 0,5 ml/kg/% burn each + 2000 ml 5% dextrose.
 The causes of death in burned patients In the first 3 days: volume deficite. In the first 2 weeks: loss of energy (catabolism, dehidration). In the further period: sepsis, hyporeactivity.
The causes of death in burned patients In the first 3 days: volume deficite. In the first 2 weeks: loss of energy (catabolism, dehidration). In the further period: sepsis, hyporeactivity.
 Thank you for your attention! Questions?
Thank you for your attention! Questions?
 Announcement! For the practical classes you must have a surgical coat, cap, mask and slippers! All these are required for visiting the operating rooms, intensive care department! Flash-cards with memory volume >1 GB for copying the information!
Announcement! For the practical classes you must have a surgical coat, cap, mask and slippers! All these are required for visiting the operating rooms, intensive care department! Flash-cards with memory volume >1 GB for copying the information!
