COPD LECTURES.ppt
- Количество слайдов: 47
 COPD Dr. Yousef Noaimat MD. FCCP Consultant in pulmonary and internal medicine.
COPD Dr. Yousef Noaimat MD. FCCP Consultant in pulmonary and internal medicine.
 Definition n Syndrome of progressive airflow limitation caused by chronic inflammation of airways and lung paranchyma and is not fully reversible.
Definition n Syndrome of progressive airflow limitation caused by chronic inflammation of airways and lung paranchyma and is not fully reversible.
 Incidence In USA -13 million Americans in 1998. -4 th leading cause of death. -In 1998: caused>100000 deaths. -Second leading cause of missed work days -Only major health problem in which mortality has been increasing over the past 20 years. -Death rate 10 X greater than that of asthma
Incidence In USA -13 million Americans in 1998. -4 th leading cause of death. -In 1998: caused>100000 deaths. -Second leading cause of missed work days -Only major health problem in which mortality has been increasing over the past 20 years. -Death rate 10 X greater than that of asthma
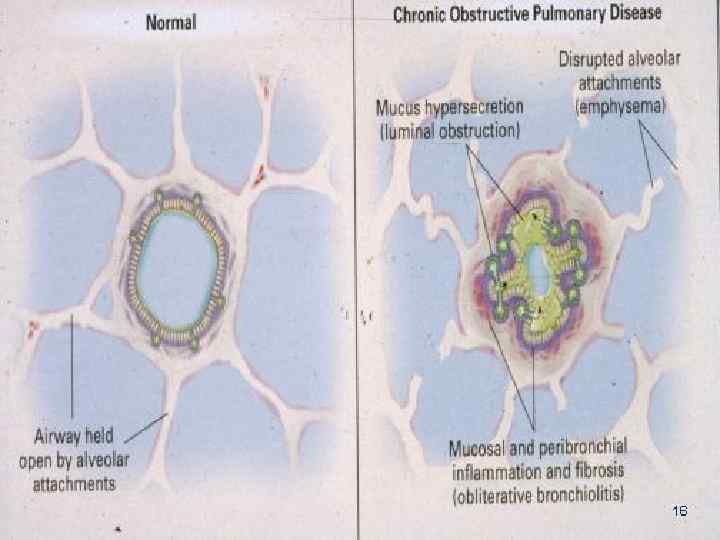
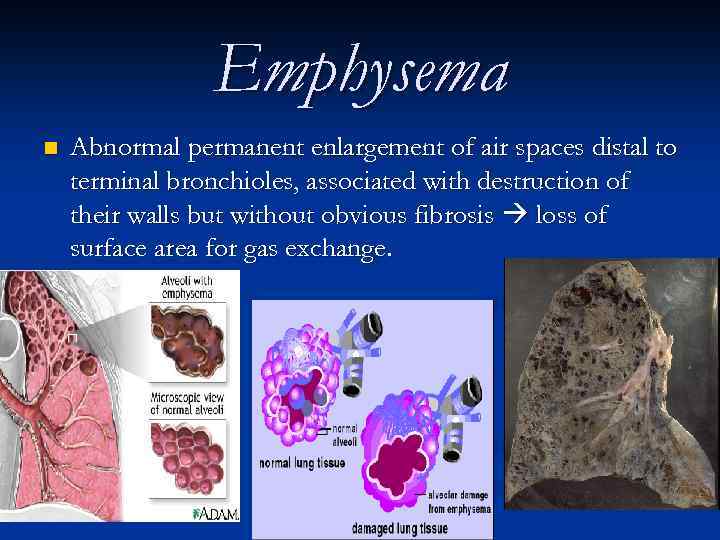 Emphysema n Abnormal permanent enlargement of air spaces distal to terminal bronchioles, associated with destruction of their walls but without obvious fibrosis loss of surface area for gas exchange.
Emphysema n Abnormal permanent enlargement of air spaces distal to terminal bronchioles, associated with destruction of their walls but without obvious fibrosis loss of surface area for gas exchange.
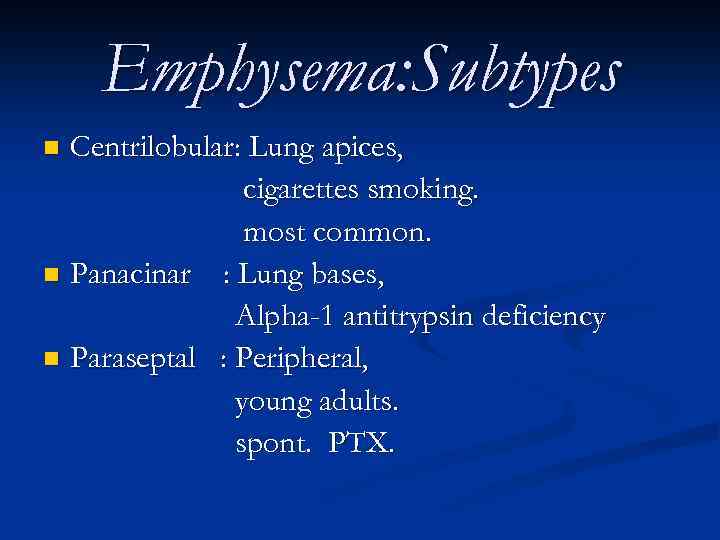 Emphysema: Subtypes Centrilobular: Lung apices, cigarettes smoking. most common. n Panacinar : Lung bases, Alpha-1 antitrypsin deficiency n Paraseptal : Peripheral, young adults. spont. PTX. n
Emphysema: Subtypes Centrilobular: Lung apices, cigarettes smoking. most common. n Panacinar : Lung bases, Alpha-1 antitrypsin deficiency n Paraseptal : Peripheral, young adults. spont. PTX. n
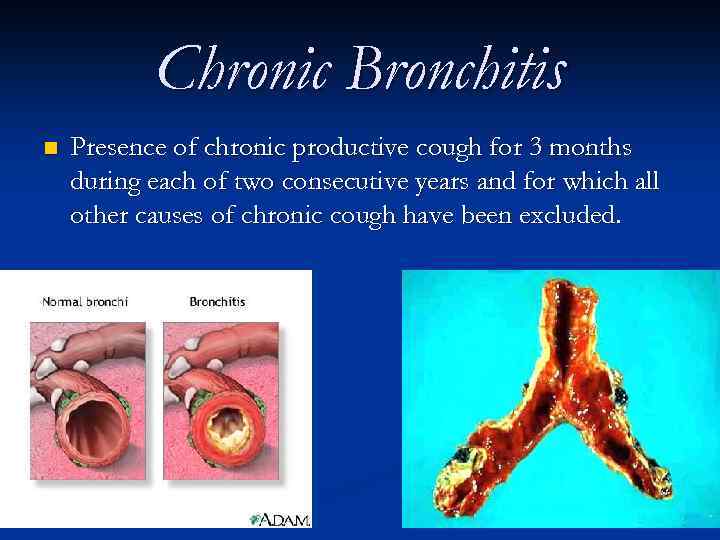 Chronic Bronchitis n Presence of chronic productive cough for 3 months during each of two consecutive years and for which all other causes of chronic cough have been excluded.
Chronic Bronchitis n Presence of chronic productive cough for 3 months during each of two consecutive years and for which all other causes of chronic cough have been excluded.
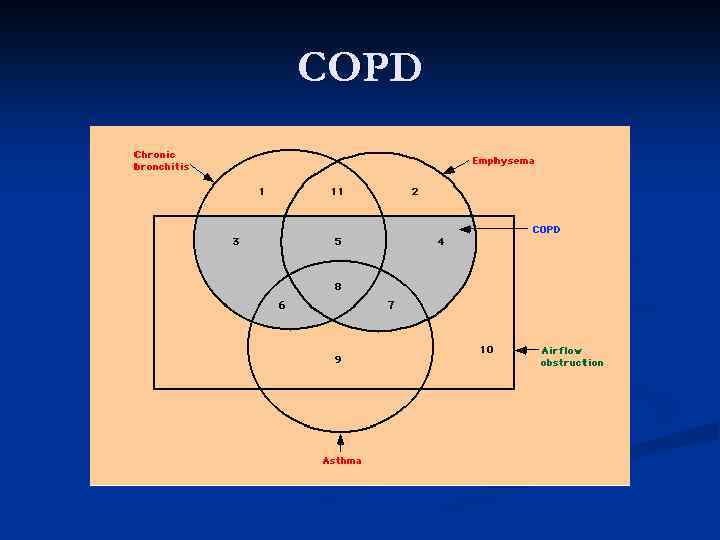 COPD
COPD
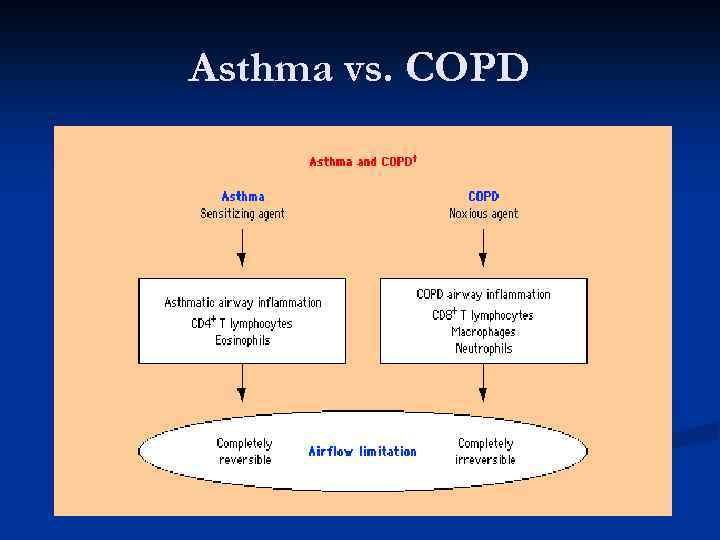 Asthma vs. COPD
Asthma vs. COPD
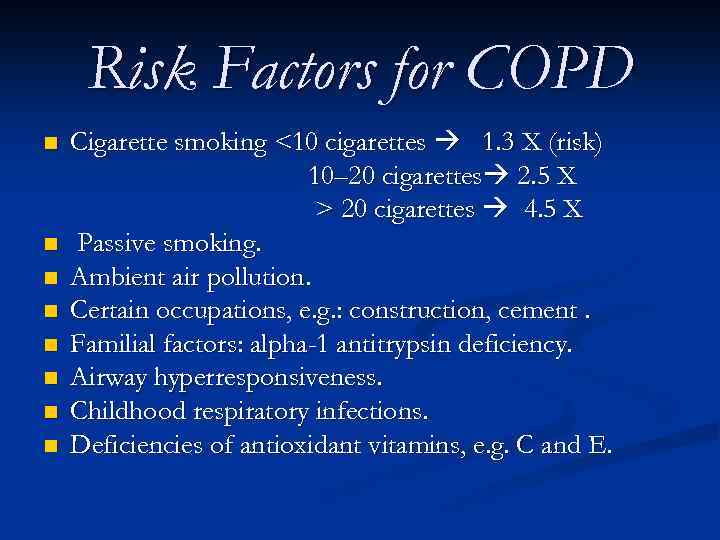 Risk Factors for COPD n n n n Cigarette smoking <10 cigarettes 1. 3 X (risk) 10– 20 cigarettes 2. 5 X > 20 cigarettes 4. 5 X Passive smoking. Ambient air pollution. Certain occupations, e. g. : construction, cement. Familial factors: alpha-1 antitrypsin deficiency. Airway hyperresponsiveness. Childhood respiratory infections. Deficiencies of antioxidant vitamins, e. g. C and E.
Risk Factors for COPD n n n n Cigarette smoking <10 cigarettes 1. 3 X (risk) 10– 20 cigarettes 2. 5 X > 20 cigarettes 4. 5 X Passive smoking. Ambient air pollution. Certain occupations, e. g. : construction, cement. Familial factors: alpha-1 antitrypsin deficiency. Airway hyperresponsiveness. Childhood respiratory infections. Deficiencies of antioxidant vitamins, e. g. C and E.
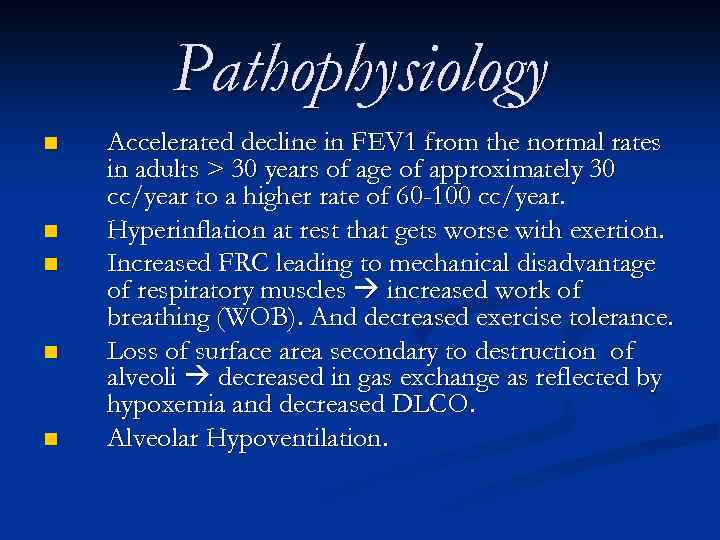 Pathophysiology n n n Accelerated decline in FEV 1 from the normal rates in adults > 30 years of age of approximately 30 cc/year to a higher rate of 60 -100 cc/year. Hyperinflation at rest that gets worse with exertion. Increased FRC leading to mechanical disadvantage of respiratory muscles increased work of breathing (WOB). And decreased exercise tolerance. Loss of surface area secondary to destruction of alveoli decreased in gas exchange as reflected by hypoxemia and decreased DLCO. Alveolar Hypoventilation.
Pathophysiology n n n Accelerated decline in FEV 1 from the normal rates in adults > 30 years of age of approximately 30 cc/year to a higher rate of 60 -100 cc/year. Hyperinflation at rest that gets worse with exertion. Increased FRC leading to mechanical disadvantage of respiratory muscles increased work of breathing (WOB). And decreased exercise tolerance. Loss of surface area secondary to destruction of alveoli decreased in gas exchange as reflected by hypoxemia and decreased DLCO. Alveolar Hypoventilation.
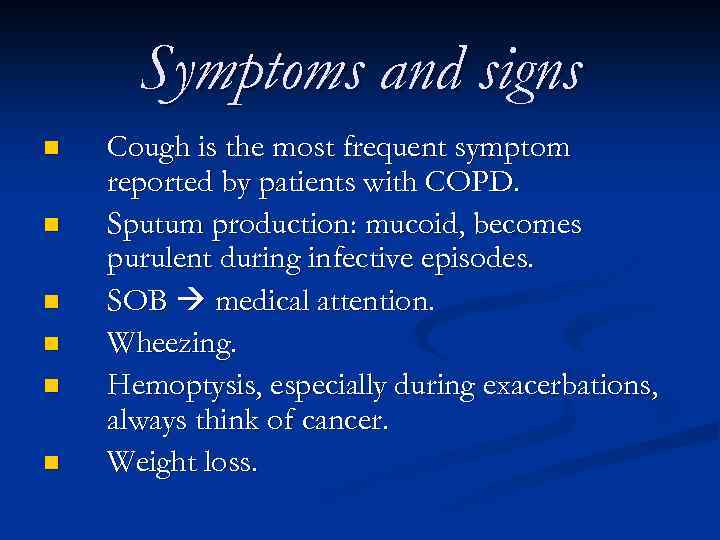 Symptoms and signs n n n Cough is the most frequent symptom reported by patients with COPD. Sputum production: mucoid, becomes purulent during infective episodes. SOB medical attention. Wheezing. Hemoptysis, especially during exacerbations, always think of cancer. Weight loss.
Symptoms and signs n n n Cough is the most frequent symptom reported by patients with COPD. Sputum production: mucoid, becomes purulent during infective episodes. SOB medical attention. Wheezing. Hemoptysis, especially during exacerbations, always think of cancer. Weight loss.
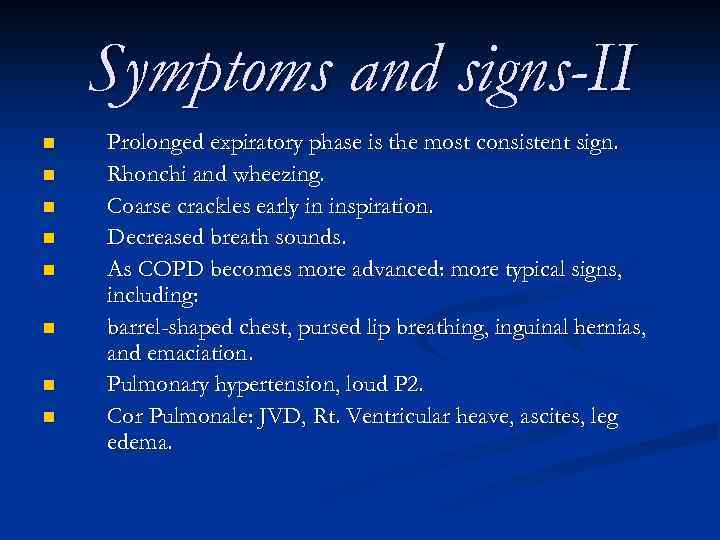 Symptoms and signs-II n n n n Prolonged expiratory phase is the most consistent sign. Rhonchi and wheezing. Coarse crackles early in inspiration. Decreased breath sounds. As COPD becomes more advanced: more typical signs, including: barrel-shaped chest, pursed lip breathing, inguinal hernias, and emaciation. Pulmonary hypertension, loud P 2. Cor Pulmonale: JVD, Rt. Ventricular heave, ascites, leg edema.
Symptoms and signs-II n n n n Prolonged expiratory phase is the most consistent sign. Rhonchi and wheezing. Coarse crackles early in inspiration. Decreased breath sounds. As COPD becomes more advanced: more typical signs, including: barrel-shaped chest, pursed lip breathing, inguinal hernias, and emaciation. Pulmonary hypertension, loud P 2. Cor Pulmonale: JVD, Rt. Ventricular heave, ascites, leg edema.
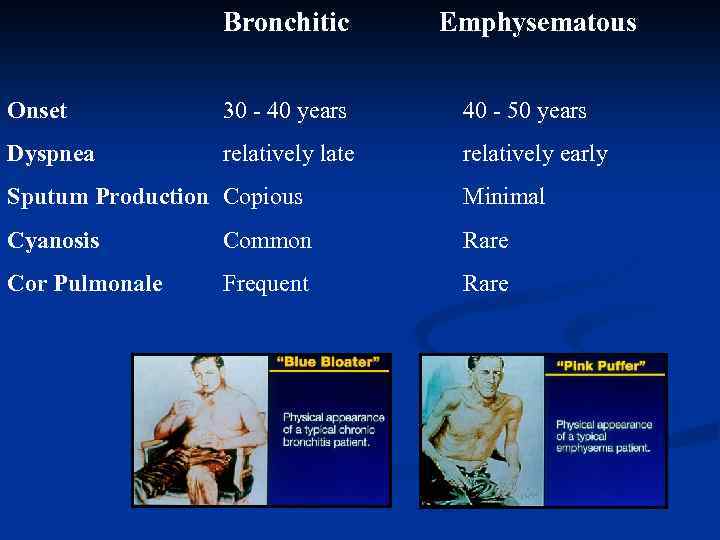 Bronchitic Emphysematous Onset 30 - 40 years 40 - 50 years Dyspnea relatively late relatively early Sputum Production Copious Minimal Cyanosis Common Rare Cor Pulmonale Frequent Rare
Bronchitic Emphysematous Onset 30 - 40 years 40 - 50 years Dyspnea relatively late relatively early Sputum Production Copious Minimal Cyanosis Common Rare Cor Pulmonale Frequent Rare
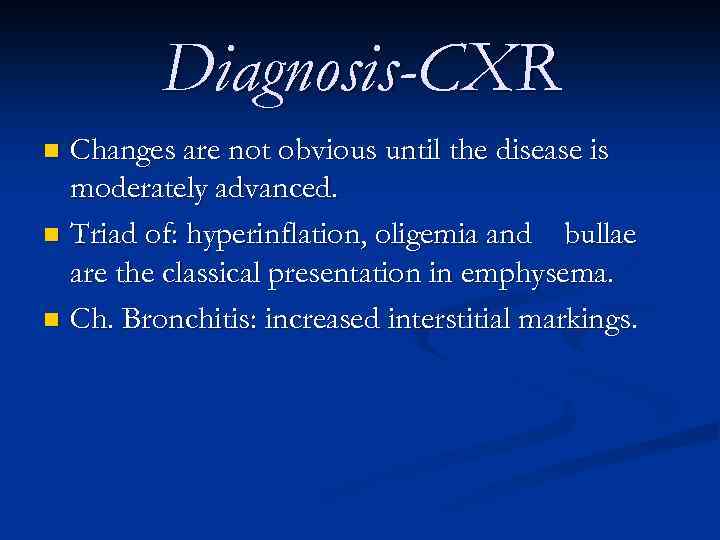 Diagnosis-CXR Changes are not obvious until the disease is moderately advanced. n Triad of: hyperinflation, oligemia and bullae are the classical presentation in emphysema. n Ch. Bronchitis: increased interstitial markings. n
Diagnosis-CXR Changes are not obvious until the disease is moderately advanced. n Triad of: hyperinflation, oligemia and bullae are the classical presentation in emphysema. n Ch. Bronchitis: increased interstitial markings. n
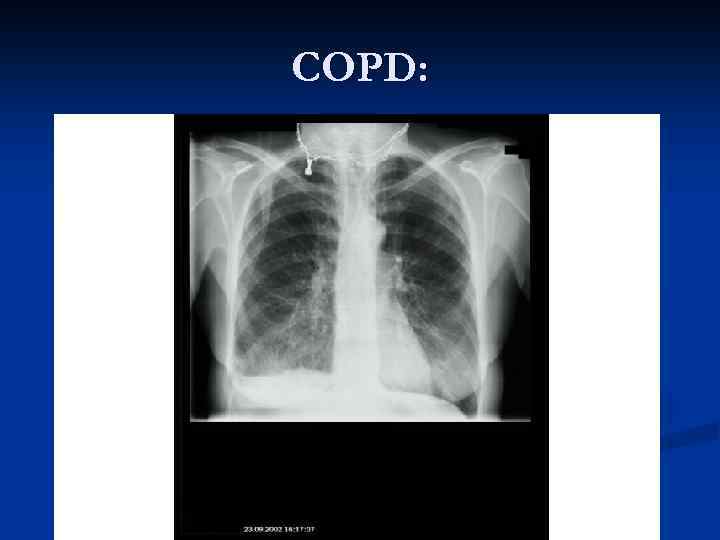 COPD:
COPD:
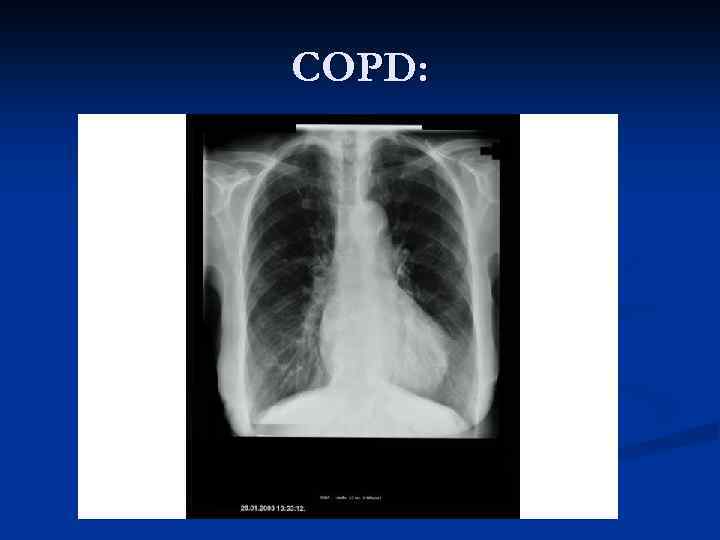 COPD:
COPD:
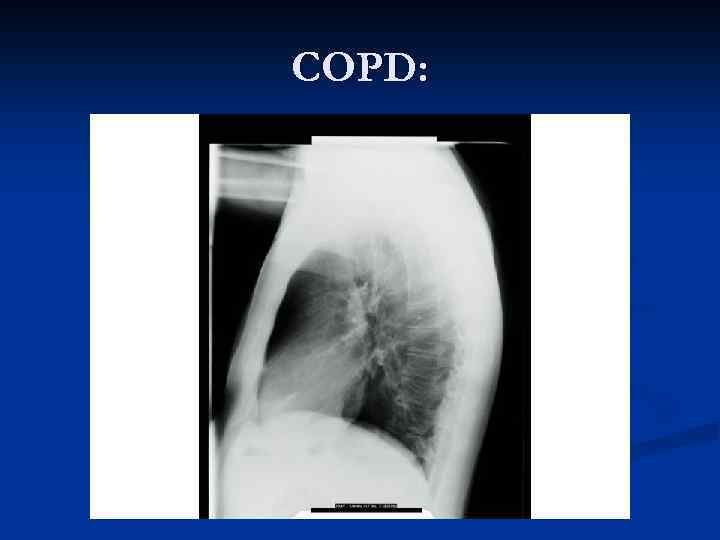 COPD:
COPD:
 Diagnosis-CT Better than CXR in delineating paranchyma and evaluate the bullae. n Can assess air trapping by comparing insp. and exp. films. n
Diagnosis-CT Better than CXR in delineating paranchyma and evaluate the bullae. n Can assess air trapping by comparing insp. and exp. films. n
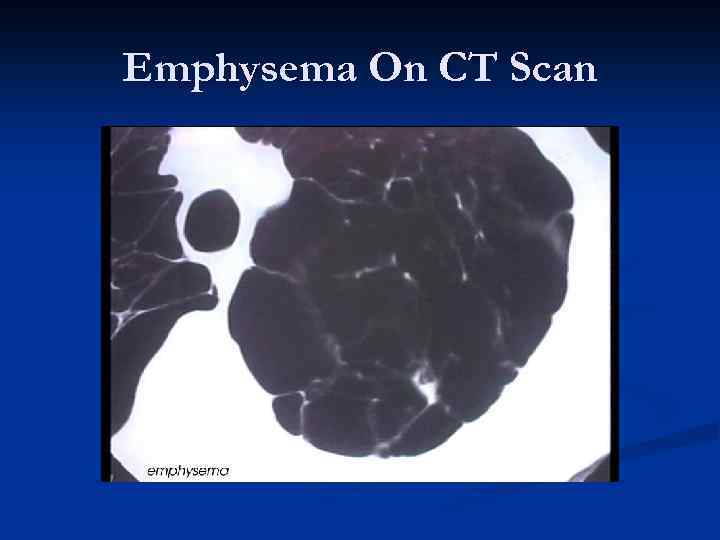 Emphysema On CT Scan
Emphysema On CT Scan
 Diagnosis-PFT FEV 1 decreased. n FVC normal to decreased. n FEV 1 / FVC decreased. n FEF 25 -75 decreased. n DLCO decreased ( in emphysema). n
Diagnosis-PFT FEV 1 decreased. n FVC normal to decreased. n FEV 1 / FVC decreased. n FEF 25 -75 decreased. n DLCO decreased ( in emphysema). n
 Diagnosis-ABG Early stages: mild to moderate hypoxemia with normal Pa. CO 2. n Advanced stages: decreased Pa. O 2, increased Pa. CO 2, increased HCO 3. n Changes get worse in acute exacerbations. n Pa. CO 2 usually starts to increase with FEV 1< 1 L. n
Diagnosis-ABG Early stages: mild to moderate hypoxemia with normal Pa. CO 2. n Advanced stages: decreased Pa. O 2, increased Pa. CO 2, increased HCO 3. n Changes get worse in acute exacerbations. n Pa. CO 2 usually starts to increase with FEV 1< 1 L. n
 Diagnosis-Lab. tests CBC: Polycythemia (chronic hypoxemia). n Increased HCO 3 (chronic resp. acidosis). n
Diagnosis-Lab. tests CBC: Polycythemia (chronic hypoxemia). n Increased HCO 3 (chronic resp. acidosis). n
 Complications of COPD Pneumothorax : Sudden worsening of dyspnea. n Can be life threatening. n Decreased / absent B. S. n CXR is diagnostic. n Chest tube is usually necessary. n Pleurodesis. n
Complications of COPD Pneumothorax : Sudden worsening of dyspnea. n Can be life threatening. n Decreased / absent B. S. n CXR is diagnostic. n Chest tube is usually necessary. n Pleurodesis. n
 Complications of COPD - cont. Pulmonary HTN : Secondary to : n Hypoxemia. n Acidosis. n Increased intrathoracic pressure. n LV dysfunction. n Chronic PE.
Complications of COPD - cont. Pulmonary HTN : Secondary to : n Hypoxemia. n Acidosis. n Increased intrathoracic pressure. n LV dysfunction. n Chronic PE.
 Complications of COPD – cont. Cor Pulmonale : n RV enlargement secondary to P. HTN. Pneumonia : n H. influenzae, Pneumococci, M. catarrhalis, Legionella.
Complications of COPD – cont. Cor Pulmonale : n RV enlargement secondary to P. HTN. Pneumonia : n H. influenzae, Pneumococci, M. catarrhalis, Legionella.
 Complications of COPD – cont. Sleep Abnormalities : Nocturnal desaturation, esp. during REM. n Impaired sleep quality. n Less REM sleep. n PVC. n
Complications of COPD – cont. Sleep Abnormalities : Nocturnal desaturation, esp. during REM. n Impaired sleep quality. n Less REM sleep. n PVC. n
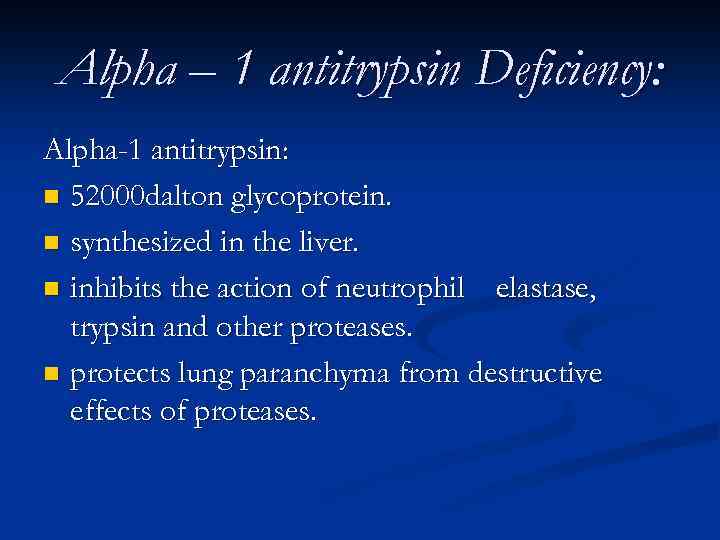 Alpha – 1 antitrypsin Deficiency: Alpha-1 antitrypsin: n 52000 dalton glycoprotein. n synthesized in the liver. n inhibits the action of neutrophil elastase, trypsin and other proteases. n protects lung paranchyma from destructive effects of proteases.
Alpha – 1 antitrypsin Deficiency: Alpha-1 antitrypsin: n 52000 dalton glycoprotein. n synthesized in the liver. n inhibits the action of neutrophil elastase, trypsin and other proteases. n protects lung paranchyma from destructive effects of proteases.
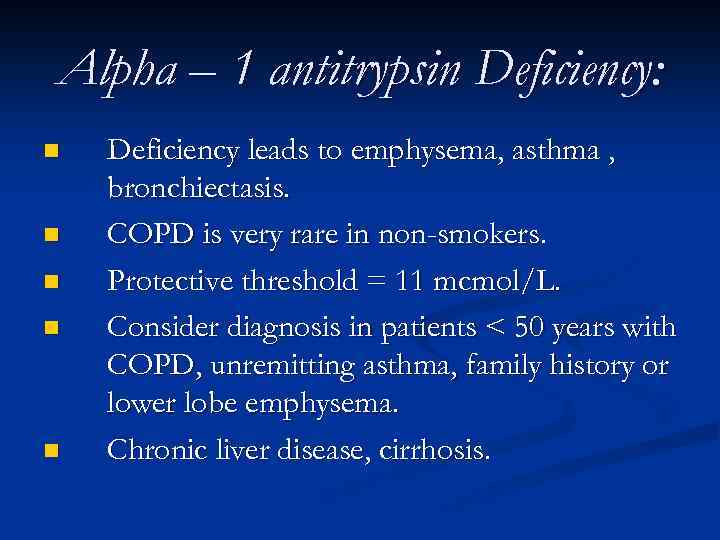 Alpha – 1 antitrypsin Deficiency: n n n Deficiency leads to emphysema, asthma , bronchiectasis. COPD is very rare in non-smokers. Protective threshold = 11 mcmol/L. Consider diagnosis in patients < 50 years with COPD, unremitting asthma, family history or lower lobe emphysema. Chronic liver disease, cirrhosis.
Alpha – 1 antitrypsin Deficiency: n n n Deficiency leads to emphysema, asthma , bronchiectasis. COPD is very rare in non-smokers. Protective threshold = 11 mcmol/L. Consider diagnosis in patients < 50 years with COPD, unremitting asthma, family history or lower lobe emphysema. Chronic liver disease, cirrhosis.
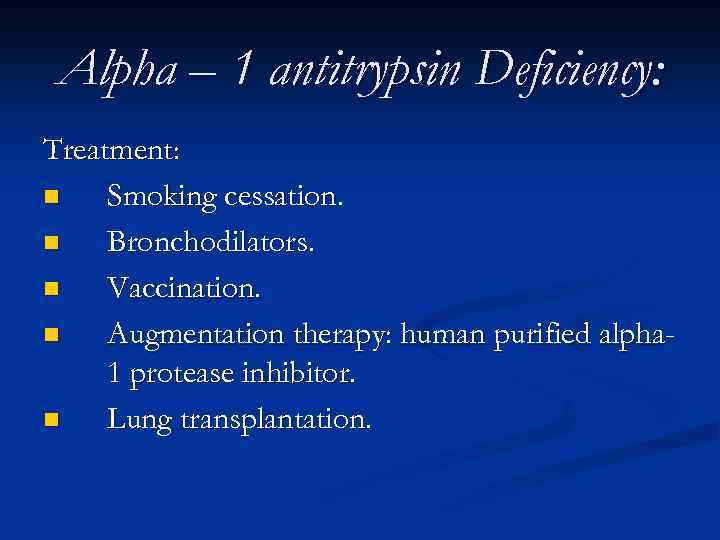 Alpha – 1 antitrypsin Deficiency: Treatment: n Smoking cessation. n Bronchodilators. n Vaccination. n Augmentation therapy: human purified alpha 1 protease inhibitor. n Lung transplantation.
Alpha – 1 antitrypsin Deficiency: Treatment: n Smoking cessation. n Bronchodilators. n Vaccination. n Augmentation therapy: human purified alpha 1 protease inhibitor. n Lung transplantation.
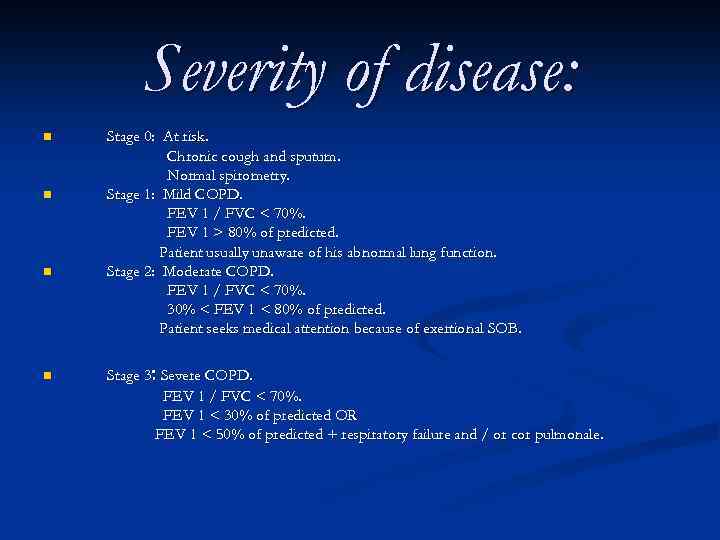 Severity of disease: n n Stage 0: At risk. Chronic cough and sputum. Normal spirometry. Stage 1: Mild COPD. FEV 1 / FVC < 70%. FEV 1 > 80% of predicted. Patient usually unaware of his abnormal lung function. Stage 2: Moderate COPD. FEV 1 / FVC < 70%. 30% < FEV 1 < 80% of predicted. Patient seeks medical attention because of exertional SOB. Stage 3: Severe COPD. FEV 1 / FVC < 70%. FEV 1 < 30% of predicted OR FEV 1 < 50% of predicted + respiratory failure and / or cor pulmonale.
Severity of disease: n n Stage 0: At risk. Chronic cough and sputum. Normal spirometry. Stage 1: Mild COPD. FEV 1 / FVC < 70%. FEV 1 > 80% of predicted. Patient usually unaware of his abnormal lung function. Stage 2: Moderate COPD. FEV 1 / FVC < 70%. 30% < FEV 1 < 80% of predicted. Patient seeks medical attention because of exertional SOB. Stage 3: Severe COPD. FEV 1 / FVC < 70%. FEV 1 < 30% of predicted OR FEV 1 < 50% of predicted + respiratory failure and / or cor pulmonale.
 Management: n n Assess and monitor the disease. Reduce the risk factors. Manage the stable patient. Manage the acute exacerbations.
Management: n n Assess and monitor the disease. Reduce the risk factors. Manage the stable patient. Manage the acute exacerbations.
 Goals of management: n n n Prevent progression. Relieve symptoms. Improve exercise tolerance. Improve overall health status. Reduce mortality. Prevent and treat complications.
Goals of management: n n n Prevent progression. Relieve symptoms. Improve exercise tolerance. Improve overall health status. Reduce mortality. Prevent and treat complications.
 Smoking cessation: The single most effective intervention to reduce risk of COPD and decrease the progression. The “ 4 As “ approach to smoking cessation: n A sk patients about their smoking habits. n A dvise patients to quit, 5 -10% quit rate at first year. n A ssess in setting a quit date. n A rrange follow-up visits.
Smoking cessation: The single most effective intervention to reduce risk of COPD and decrease the progression. The “ 4 As “ approach to smoking cessation: n A sk patients about their smoking habits. n A dvise patients to quit, 5 -10% quit rate at first year. n A ssess in setting a quit date. n A rrange follow-up visits.
 Smoking Cessation. Nicotine replacement therapy n n n Reduce withdrawal symptoms: anxiety, irritability, anger. Improve cessation rate to 25% at 6 months. Forms: gums, patches, and spray.
Smoking Cessation. Nicotine replacement therapy n n n Reduce withdrawal symptoms: anxiety, irritability, anger. Improve cessation rate to 25% at 6 months. Forms: gums, patches, and spray.
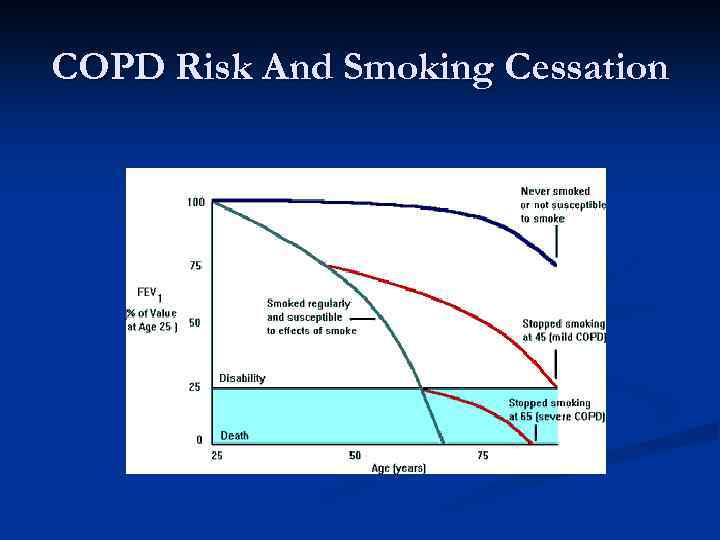 COPD Risk And Smoking Cessation
COPD Risk And Smoking Cessation
 Management of stable COPD: n n n Anticholinergics. B 2 -adrenergic agonists. Methylxanthines. Inhaled steroids. Systemic steroids. n n Long-term O 2 therapy. Pulmonary rehabilitation. Lung Volume Reduction Surgery. Lung Transplantation.
Management of stable COPD: n n n Anticholinergics. B 2 -adrenergic agonists. Methylxanthines. Inhaled steroids. Systemic steroids. n n Long-term O 2 therapy. Pulmonary rehabilitation. Lung Volume Reduction Surgery. Lung Transplantation.
 Anticholinergics: n n n n n Act as bronchodilators. Mechanism: compete with Ach. at receptors of parasympathetic cholinergic nerve endings decrease intracellular c. GMP smooth muscle relaxation. Improve exercise performance. Decrease dyspnea. Decrease mucus hypersecretion. Safe. No tachyphylaxis. Ipratropium: short acting inhaler and nebulizer. 2 -4 puffs QID. Tiotropium: Long-acting, used once/day.
Anticholinergics: n n n n n Act as bronchodilators. Mechanism: compete with Ach. at receptors of parasympathetic cholinergic nerve endings decrease intracellular c. GMP smooth muscle relaxation. Improve exercise performance. Decrease dyspnea. Decrease mucus hypersecretion. Safe. No tachyphylaxis. Ipratropium: short acting inhaler and nebulizer. 2 -4 puffs QID. Tiotropium: Long-acting, used once/day.
 B 2 -Adrenergic Agonists: n n n n n Act as bronchodilators. Mechanism: Increase intracellular c. AMP Change intracellular calcium concentration bronchial relaxation. Improve exercise tolerance. Decrease dyspnea. Enhance mucus clearance. S. E. : related to activation of B 1 -receptors: C. V. system: Increase H. R. , arrhythmias, ischemia, hypo or hypertension. CNS: tremor, agitation, insomnia. Hypokalemia. Can cause tachyphylaxis. Albuterol / Salmuterol: short acting Inhaler/ nebulizer 2 puffs QID ( PRN). Salmeterol / Formoterol: long acting. given BID.
B 2 -Adrenergic Agonists: n n n n n Act as bronchodilators. Mechanism: Increase intracellular c. AMP Change intracellular calcium concentration bronchial relaxation. Improve exercise tolerance. Decrease dyspnea. Enhance mucus clearance. S. E. : related to activation of B 1 -receptors: C. V. system: Increase H. R. , arrhythmias, ischemia, hypo or hypertension. CNS: tremor, agitation, insomnia. Hypokalemia. Can cause tachyphylaxis. Albuterol / Salmuterol: short acting Inhaler/ nebulizer 2 puffs QID ( PRN). Salmeterol / Formoterol: long acting. given BID.
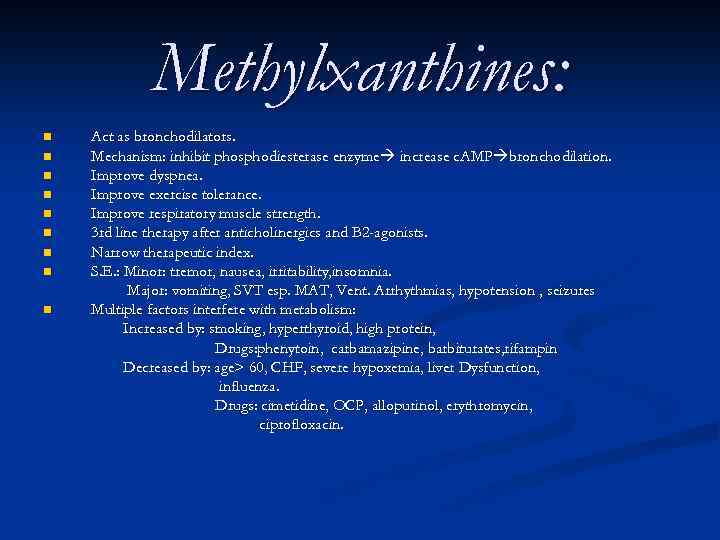 Methylxanthines: n n n n n Act as bronchodilators. Mechanism: inhibit phosphodiesterase enzyme increase c. AMP bronchodilation. Improve dyspnea. Improve exercise tolerance. Improve respiratory muscle strength. 3 rd line therapy after anticholinergics and B 2 -agonists. Narrow therapeutic index. S. E. : Minor: tremor, nausea, irritability, insomnia. Major: vomiting, SVT esp. MAT, Vent. Arrhythmias, hypotension , seizures Multiple factors interfere with metabolism: Increased by: smoking, hyperthyroid, high protein, Drugs: phenytoin, carbamazipine, barbiturates, rifampin Decreased by: age> 60, CHF, severe hypoxemia, liver Dysfunction, influenza. Drugs: cimetidine, OCP, allopurinol, erythromycin, ciprofloxacin.
Methylxanthines: n n n n n Act as bronchodilators. Mechanism: inhibit phosphodiesterase enzyme increase c. AMP bronchodilation. Improve dyspnea. Improve exercise tolerance. Improve respiratory muscle strength. 3 rd line therapy after anticholinergics and B 2 -agonists. Narrow therapeutic index. S. E. : Minor: tremor, nausea, irritability, insomnia. Major: vomiting, SVT esp. MAT, Vent. Arrhythmias, hypotension , seizures Multiple factors interfere with metabolism: Increased by: smoking, hyperthyroid, high protein, Drugs: phenytoin, carbamazipine, barbiturates, rifampin Decreased by: age> 60, CHF, severe hypoxemia, liver Dysfunction, influenza. Drugs: cimetidine, OCP, allopurinol, erythromycin, ciprofloxacin.
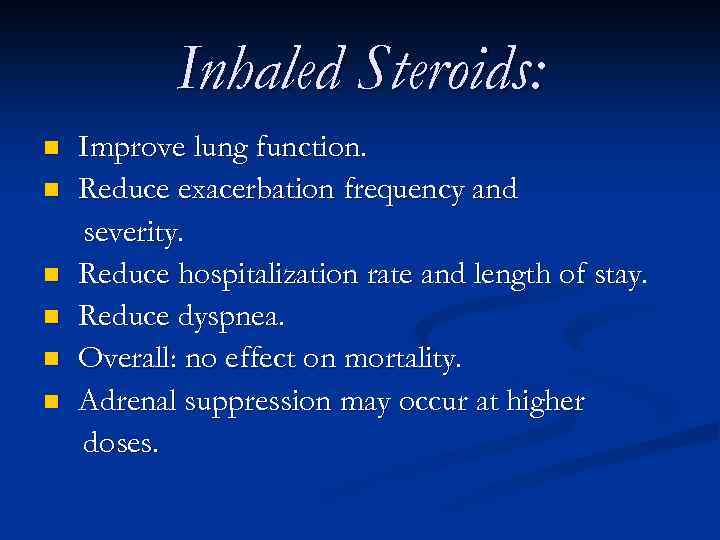 Inhaled Steroids: n n n Improve lung function. Reduce exacerbation frequency and severity. Reduce hospitalization rate and length of stay. Reduce dyspnea. Overall: no effect on mortality. Adrenal suppression may occur at higher doses.
Inhaled Steroids: n n n Improve lung function. Reduce exacerbation frequency and severity. Reduce hospitalization rate and length of stay. Reduce dyspnea. Overall: no effect on mortality. Adrenal suppression may occur at higher doses.
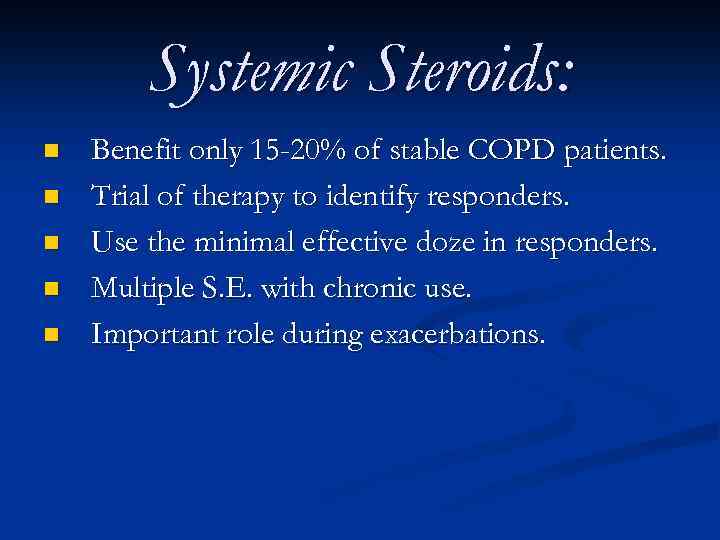 Systemic Steroids: n n n Benefit only 15 -20% of stable COPD patients. Trial of therapy to identify responders. Use the minimal effective doze in responders. Multiple S. E. with chronic use. Important role during exacerbations.
Systemic Steroids: n n n Benefit only 15 -20% of stable COPD patients. Trial of therapy to identify responders. Use the minimal effective doze in responders. Multiple S. E. with chronic use. Important role during exacerbations.
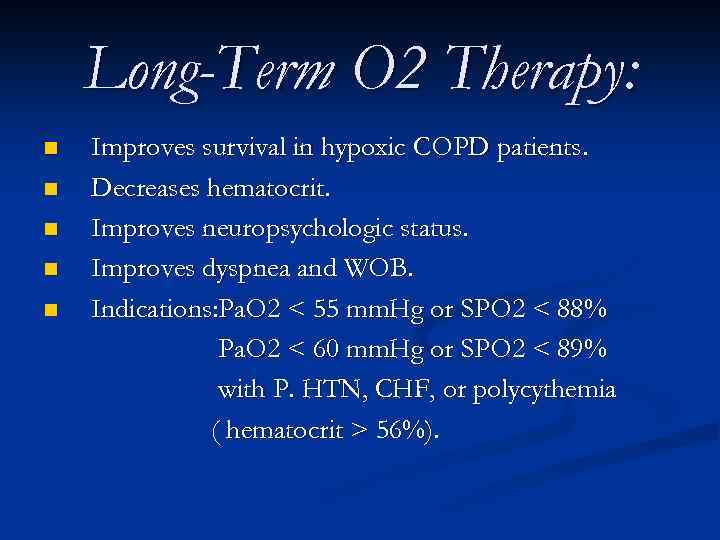 Long-Term O 2 Therapy: n n n Improves survival in hypoxic COPD patients. Decreases hematocrit. Improves neuropsychologic status. Improves dyspnea and WOB. Indications: Pa. O 2 < 55 mm. Hg or SPO 2 < 88% Pa. O 2 < 60 mm. Hg or SPO 2 < 89% with P. HTN, CHF, or polycythemia ( hematocrit > 56%).
Long-Term O 2 Therapy: n n n Improves survival in hypoxic COPD patients. Decreases hematocrit. Improves neuropsychologic status. Improves dyspnea and WOB. Indications: Pa. O 2 < 55 mm. Hg or SPO 2 < 88% Pa. O 2 < 60 mm. Hg or SPO 2 < 89% with P. HTN, CHF, or polycythemia ( hematocrit > 56%).
 Management of Acute Exacerbation: n n Usually caused by pulmonary infections or air pollution. 1/3 no identifiable cause. Others: GERD, cardiac disease, PTX. CXR is mandatory.
Management of Acute Exacerbation: n n Usually caused by pulmonary infections or air pollution. 1/3 no identifiable cause. Others: GERD, cardiac disease, PTX. CXR is mandatory.
 Management of Acute Exacerbation-II: Treatment: n n n Inhaled B 2 - agonists Aanticholinergics. Systemic steroids. Antibiotics: cover for common bacteria. O 2 for hypoxemia.
Management of Acute Exacerbation-II: Treatment: n n n Inhaled B 2 - agonists Aanticholinergics. Systemic steroids. Antibiotics: cover for common bacteria. O 2 for hypoxemia.
 Thank You
Thank You
