CHEST PAIN (Differential Diagnosis).ppt
- Количество слайдов: 47
 CHEST PAIN: Differential Diagnosis Vladimir Konstantinov MD, Professor of Cardiology St. Petersburg State Medical Academy named after I. I. Mechnikov 2007
CHEST PAIN: Differential Diagnosis Vladimir Konstantinov MD, Professor of Cardiology St. Petersburg State Medical Academy named after I. I. Mechnikov 2007
 CLINICAL CASE
CLINICAL CASE
 A 46 year-aged male patient • No complaints at the moment of examination, good physical load tolerance
A 46 year-aged male patient • No complaints at the moment of examination, good physical load tolerance
 Anamnesis morbi • • In summer, 2005 he began to feel weakness, not acute prolonged chest pain localized mainly in the back. He took aspirin and analgin several times a day without any effect. An ECG was performed only on the 3 rd day of the disease He was hospitalized, the suspected diagnosis was an acute coronary syndrome
Anamnesis morbi • • In summer, 2005 he began to feel weakness, not acute prolonged chest pain localized mainly in the back. He took aspirin and analgin several times a day without any effect. An ECG was performed only on the 3 rd day of the disease He was hospitalized, the suspected diagnosis was an acute coronary syndrome
 Anamnesis Vitae • • • His blood pressure was always normal He never smoked and his alcohol intake was very small His family history was free of cardiovascular diseases He is physically well-trained person (every day he swims about 1 km in the swimming pool) Other diseases: type 2 diabetes mellitus diagnosed 3 years ago with diet blood glucose control His profession is a medical doctor (cardiologist)
Anamnesis Vitae • • • His blood pressure was always normal He never smoked and his alcohol intake was very small His family history was free of cardiovascular diseases He is physically well-trained person (every day he swims about 1 km in the swimming pool) Other diseases: type 2 diabetes mellitus diagnosed 3 years ago with diet blood glucose control His profession is a medical doctor (cardiologist)
 Physical Examination • • Height - 176 сm, weight - 78 kg, BMI - 25 His skin was clear and had usual color
Physical Examination • • Height - 176 сm, weight - 78 kg, BMI - 25 His skin was clear and had usual color
 Cardiovascular System • • Pulse is symmetric and rhythmic, 76 bites per minute Blood pressure - 118/76 mm Hg Heart borders were normal No murmurs were heared
Cardiovascular System • • Pulse is symmetric and rhythmic, 76 bites per minute Blood pressure - 118/76 mm Hg Heart borders were normal No murmurs were heared
 Other organs • • Normal breathing sound Liver and spleen were not palpated Kidneys of normal size and no pathologic symptoms were revealed No peripheral edema
Other organs • • Normal breathing sound Liver and spleen were not palpated Kidneys of normal size and no pathologic symptoms were revealed No peripheral edema
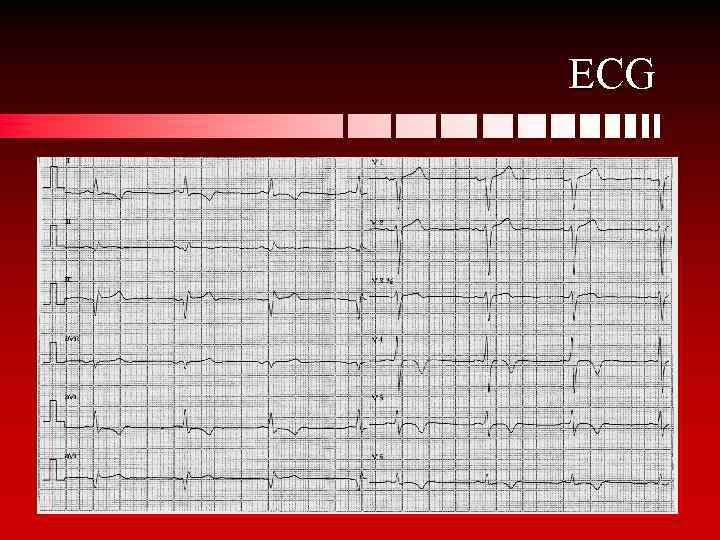 ECG
ECG
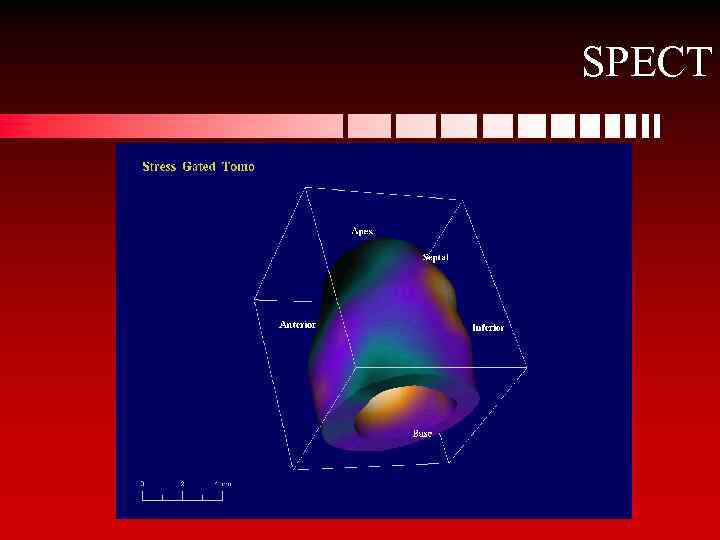 SPECT
SPECT
 PAIN: DIFFERENT POINTS OF VIEW • • • “Pain is a health guard” (Ancient Greece) “If we could know exactly what the origin of pain is there must be less mistakes in our treatment” (Leriche) “Disease – is a drama including two acts: the first one begins in tissues in the whole darkness without any pain; the second is a great fire which in some cases could hardly be stopped in others could not” (Leriche)
PAIN: DIFFERENT POINTS OF VIEW • • • “Pain is a health guard” (Ancient Greece) “If we could know exactly what the origin of pain is there must be less mistakes in our treatment” (Leriche) “Disease – is a drama including two acts: the first one begins in tissues in the whole darkness without any pain; the second is a great fire which in some cases could hardly be stopped in others could not” (Leriche)
 EVOLUTION OF OUR KNOWLEDGE OF THE PATHOLOGY OF PAIN • • • 1920 th – histamine is the unique pain mediator 1950 th – pain could be initiated by other substances (monochloracetone, formaldehyde, KCl) Discovery of kinines – bradykinine, collydine, enterotoxin, etc. From the modern point of view pain is considered as an integrated reaction of different brain structures in order to protect the human organism
EVOLUTION OF OUR KNOWLEDGE OF THE PATHOLOGY OF PAIN • • • 1920 th – histamine is the unique pain mediator 1950 th – pain could be initiated by other substances (monochloracetone, formaldehyde, KCl) Discovery of kinines – bradykinine, collydine, enterotoxin, etc. From the modern point of view pain is considered as an integrated reaction of different brain structures in order to protect the human organism
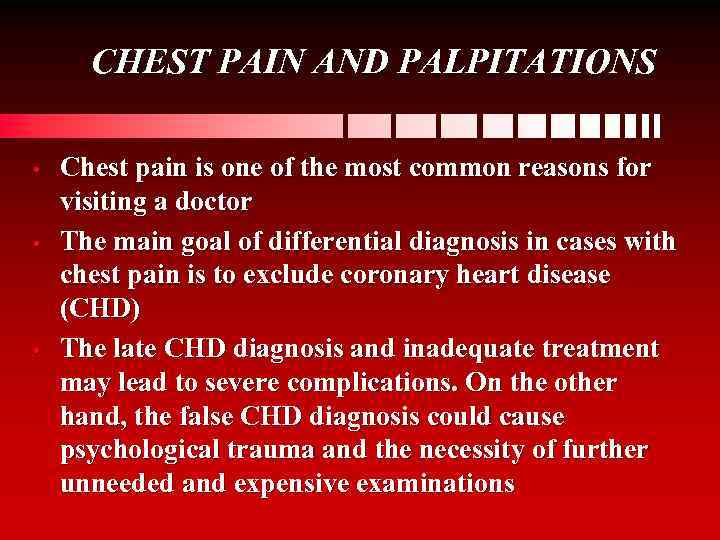 CHEST PAIN AND PALPITATIONS • • • Chest pain is one of the most common reasons for visiting a doctor The main goal of differential diagnosis in cases with chest pain is to exclude coronary heart disease (CHD) The late CHD diagnosis and inadequate treatment may lead to severe complications. On the other hand, the false CHD diagnosis could cause psychological trauma and the necessity of further unneeded and expensive examinations
CHEST PAIN AND PALPITATIONS • • • Chest pain is one of the most common reasons for visiting a doctor The main goal of differential diagnosis in cases with chest pain is to exclude coronary heart disease (CHD) The late CHD diagnosis and inadequate treatment may lead to severe complications. On the other hand, the false CHD diagnosis could cause psychological trauma and the necessity of further unneeded and expensive examinations
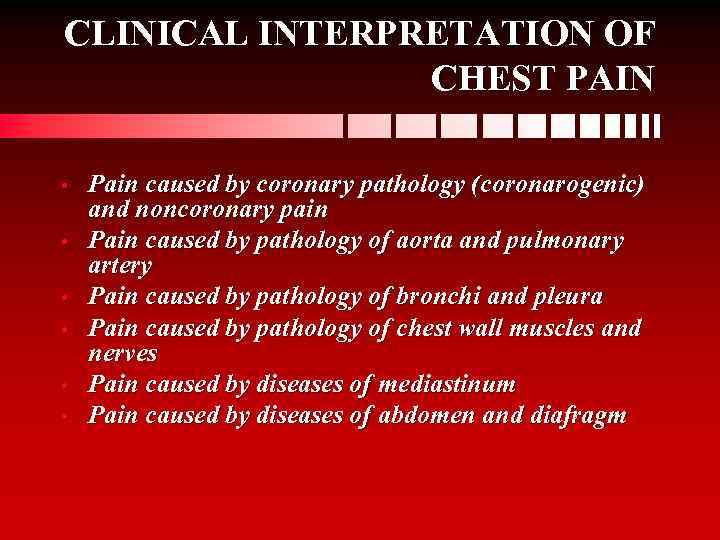 CLINICAL INTERPRETATION OF CHEST PAIN • • • Pain caused by coronary pathology (coronarogenic) and noncoronary pain Pain caused by pathology of aorta and pulmonary artery Pain caused by pathology of bronchi and pleura Pain caused by pathology of chest wall muscles and nerves Pain caused by diseases of mediastinum Pain caused by diseases of abdomen and diafragm
CLINICAL INTERPRETATION OF CHEST PAIN • • • Pain caused by coronary pathology (coronarogenic) and noncoronary pain Pain caused by pathology of aorta and pulmonary artery Pain caused by pathology of bronchi and pleura Pain caused by pathology of chest wall muscles and nerves Pain caused by diseases of mediastinum Pain caused by diseases of abdomen and diafragm
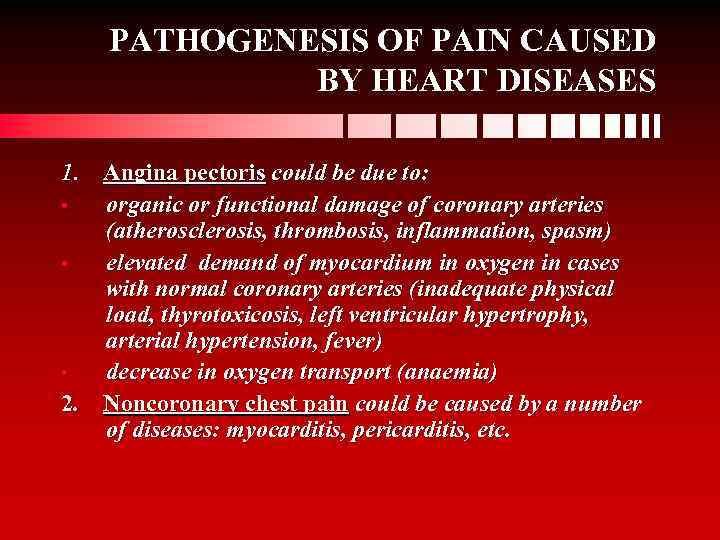 PATHOGENESIS OF PAIN CAUSED BY HEART DISEASES 1. Angina pectoris could be due to: • organic or functional damage of coronary arteries (atherosclerosis, thrombosis, inflammation, spasm) • elevated demand of myocardium in oxygen in cases with normal coronary arteries (inadequate physical load, thyrotoxicosis, left ventricular hypertrophy, arterial hypertension, fever) • decrease in oxygen transport (anaemia) 2. Noncoronary chest pain could be caused by a number of diseases: myocarditis, pericarditis, etc.
PATHOGENESIS OF PAIN CAUSED BY HEART DISEASES 1. Angina pectoris could be due to: • organic or functional damage of coronary arteries (atherosclerosis, thrombosis, inflammation, spasm) • elevated demand of myocardium in oxygen in cases with normal coronary arteries (inadequate physical load, thyrotoxicosis, left ventricular hypertrophy, arterial hypertension, fever) • decrease in oxygen transport (anaemia) 2. Noncoronary chest pain could be caused by a number of diseases: myocarditis, pericarditis, etc.
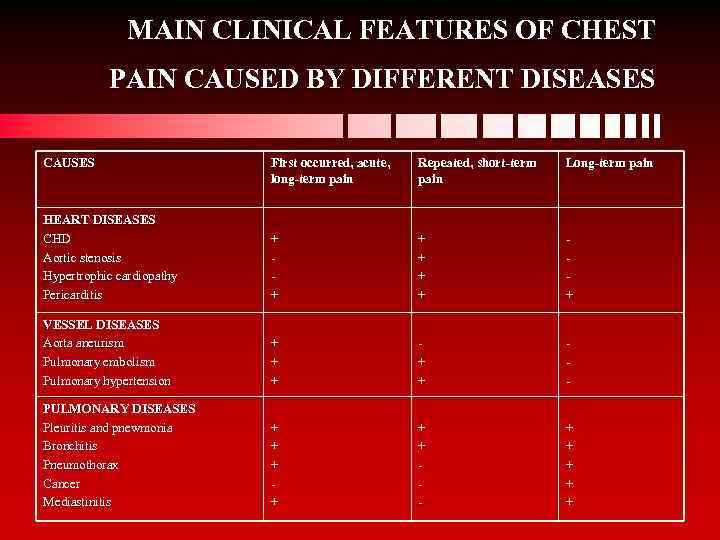 MAIN CLINICAL FEATURES OF CHEST PAIN CAUSED BY DIFFERENT DISEASES CAUSES First occurred, acute, long-term pain Repeated, short-term pain Long-term pain HEART DISEASES CHD Aortic stenosis Hypertrophic cardiopathy Pericarditis + + + + VESSEL DISEASES Aorta aneurism Pulmonary embolism Pulmonary hypertension + + + - PULMONARY DISEASES Pleuritis and pnewmonia Bronchitis Pneumothorax Cancer Mediastinitis + + + - + + +
MAIN CLINICAL FEATURES OF CHEST PAIN CAUSED BY DIFFERENT DISEASES CAUSES First occurred, acute, long-term pain Repeated, short-term pain Long-term pain HEART DISEASES CHD Aortic stenosis Hypertrophic cardiopathy Pericarditis + + + + VESSEL DISEASES Aorta aneurism Pulmonary embolism Pulmonary hypertension + + + - PULMONARY DISEASES Pleuritis and pnewmonia Bronchitis Pneumothorax Cancer Mediastinitis + + + - + + +
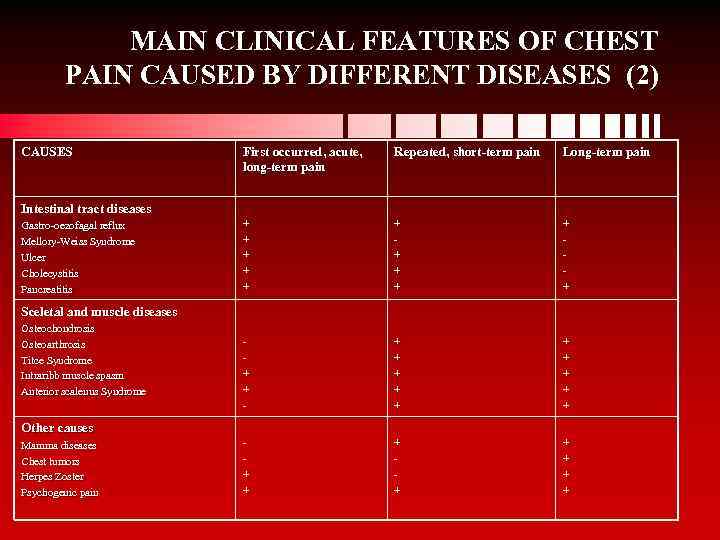 MAIN CLINICAL FEATURES OF CHEST PAIN CAUSED BY DIFFERENT DISEASES (2) CAUSES First occurred, acute, long-term pain Repeated, short-term pain Long-term pain + + + + - + + + + + Intestinal tract diseases Gastro-oezofagal reflux Gastro-oezofagal Mellory-Weiss Syndrome Mellory-Weiss Ulcer Cholecystitis Pancreatitis Sceletal and muscle diseases Osteochondrosis Osteoarthrosis Titce Syndrome Intraribb muscle spasm Anterior scalenus Syndrome Other causes Mamma diseases Chest tumors Herpes Zoster Psychogenic pain
MAIN CLINICAL FEATURES OF CHEST PAIN CAUSED BY DIFFERENT DISEASES (2) CAUSES First occurred, acute, long-term pain Repeated, short-term pain Long-term pain + + + + - + + + + + Intestinal tract diseases Gastro-oezofagal reflux Gastro-oezofagal Mellory-Weiss Syndrome Mellory-Weiss Ulcer Cholecystitis Pancreatitis Sceletal and muscle diseases Osteochondrosis Osteoarthrosis Titce Syndrome Intraribb muscle spasm Anterior scalenus Syndrome Other causes Mamma diseases Chest tumors Herpes Zoster Psychogenic pain
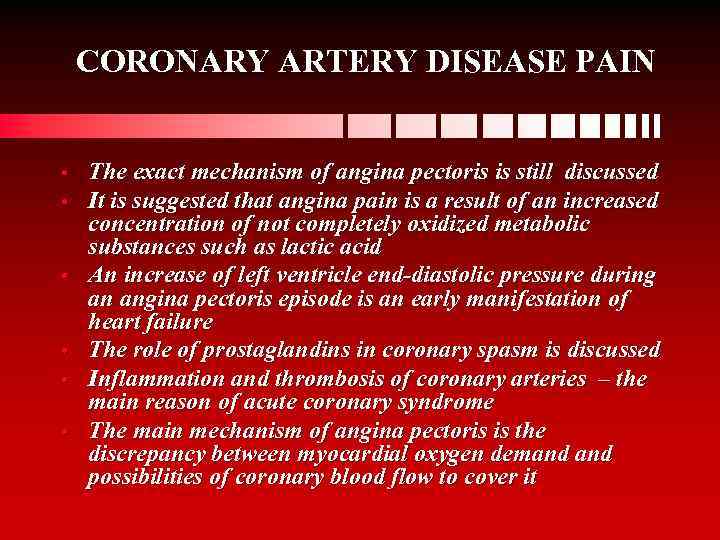 CORONARY ARTERY DISEASE PAIN • • • The exact mechanism of angina pectoris is still discussed It is suggested that angina pain is a result of an increased concentration of not completely oxidized metabolic substances such as lactic acid An increase of left ventricle end-diastolic pressure during an angina pectoris episode is an early manifestation of heart failure The role of prostaglandins in coronary spasm is discussed Inflammation and thrombosis of coronary arteries – the main reason of acute coronary syndrome The main mechanism of angina pectoris is the discrepancy between myocardial oxygen demand possibilities of coronary blood flow to cover it
CORONARY ARTERY DISEASE PAIN • • • The exact mechanism of angina pectoris is still discussed It is suggested that angina pain is a result of an increased concentration of not completely oxidized metabolic substances such as lactic acid An increase of left ventricle end-diastolic pressure during an angina pectoris episode is an early manifestation of heart failure The role of prostaglandins in coronary spasm is discussed Inflammation and thrombosis of coronary arteries – the main reason of acute coronary syndrome The main mechanism of angina pectoris is the discrepancy between myocardial oxygen demand possibilities of coronary blood flow to cover it
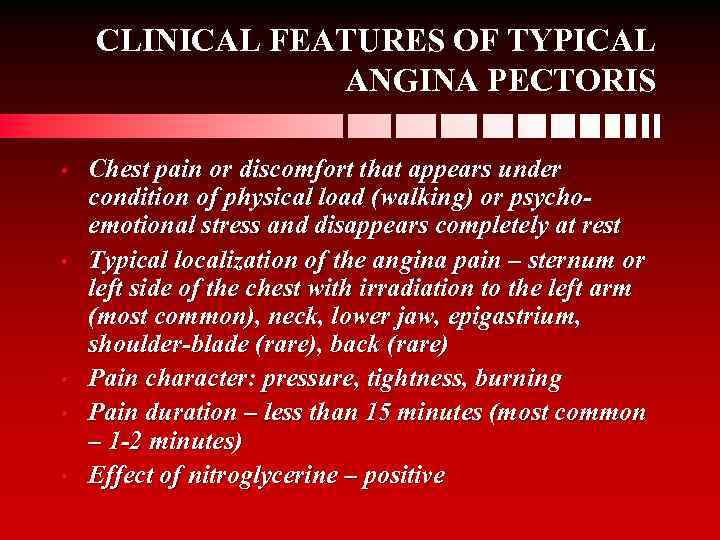 CLINICAL FEATURES OF TYPICAL ANGINA PECTORIS • • • Chest pain or discomfort that appears under condition of physical load (walking) or psychoemotional stress and disappears completely at rest Typical localization of the angina pain – sternum or left side of the chest with irradiation to the left arm (most common), neck, lower jaw, epigastrium, shoulder-blade (rare), back (rare) Pain character: pressure, tightness, burning Pain duration – less than 15 minutes (most common – 1 -2 minutes) Effect of nitroglycerine – positive
CLINICAL FEATURES OF TYPICAL ANGINA PECTORIS • • • Chest pain or discomfort that appears under condition of physical load (walking) or psychoemotional stress and disappears completely at rest Typical localization of the angina pain – sternum or left side of the chest with irradiation to the left arm (most common), neck, lower jaw, epigastrium, shoulder-blade (rare), back (rare) Pain character: pressure, tightness, burning Pain duration – less than 15 minutes (most common – 1 -2 minutes) Effect of nitroglycerine – positive
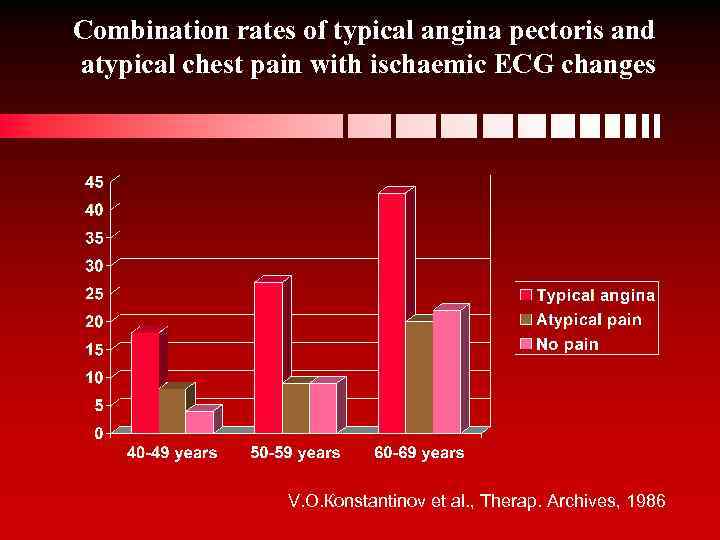 Combination rates of typical angina pectoris and atypical chest pain with ischaemic ECG changes V. О. Коnstantinov et al. , Therap. Archives, 1986
Combination rates of typical angina pectoris and atypical chest pain with ischaemic ECG changes V. О. Коnstantinov et al. , Therap. Archives, 1986
 CHD RISK FACTORS • • Age and gender Family history of premature CHD Dyslipidemia Arterial hypertension Smoking Overweight Diabetes
CHD RISK FACTORS • • Age and gender Family history of premature CHD Dyslipidemia Arterial hypertension Smoking Overweight Diabetes
 Physical Examination • • • Very often no clinical signs could be revealed The 4 th heart sound could be heard (which is due to an increased left ventricle end-diastolic pressure and pronounced systole of left atrium) Transient mitral insufficiency – systolic murmur (as a result of ischaemia of papillary muscles) Myocardial infarction or prolonged severe myocardial ischaemia could cause heart failure Aorta stenosis, hypertrophic cardiopathy, nonatherosclerotic damage of coronary arteries could be accompanied by typical angina symptoms, moreover, there would be symptoms of the main disease (systolic murmur, etc. ).
Physical Examination • • • Very often no clinical signs could be revealed The 4 th heart sound could be heard (which is due to an increased left ventricle end-diastolic pressure and pronounced systole of left atrium) Transient mitral insufficiency – systolic murmur (as a result of ischaemia of papillary muscles) Myocardial infarction or prolonged severe myocardial ischaemia could cause heart failure Aorta stenosis, hypertrophic cardiopathy, nonatherosclerotic damage of coronary arteries could be accompanied by typical angina symptoms, moreover, there would be symptoms of the main disease (systolic murmur, etc. ).
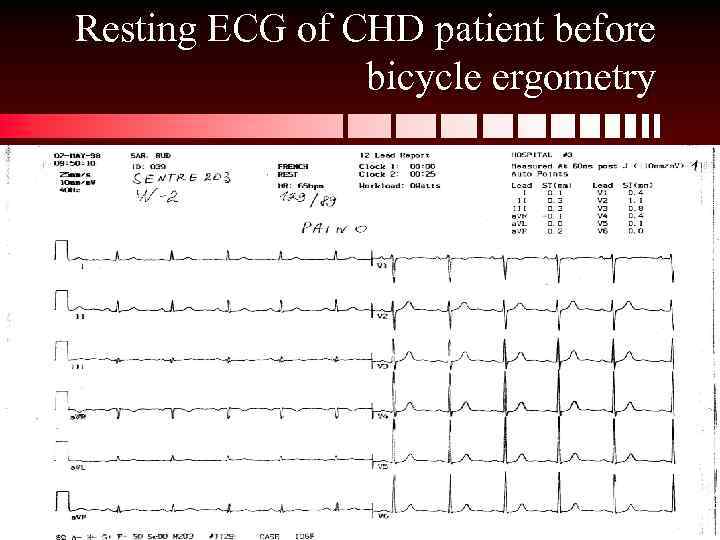 Resting ECG of CHD patient before bicycle ergometry
Resting ECG of CHD patient before bicycle ergometry
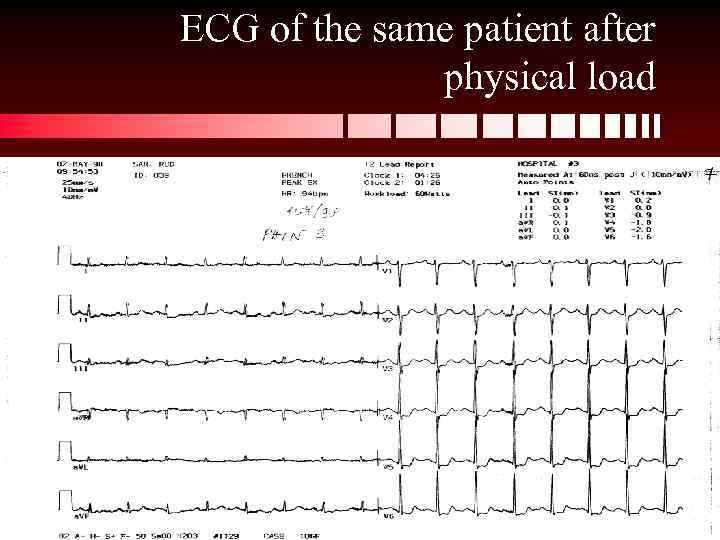 ECG of the same patient after physical load
ECG of the same patient after physical load
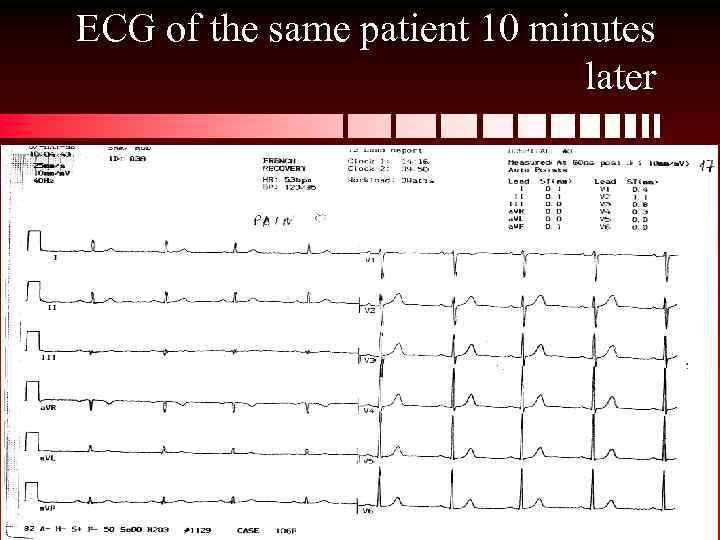 ECG of the same patient 10 minutes later
ECG of the same patient 10 minutes later
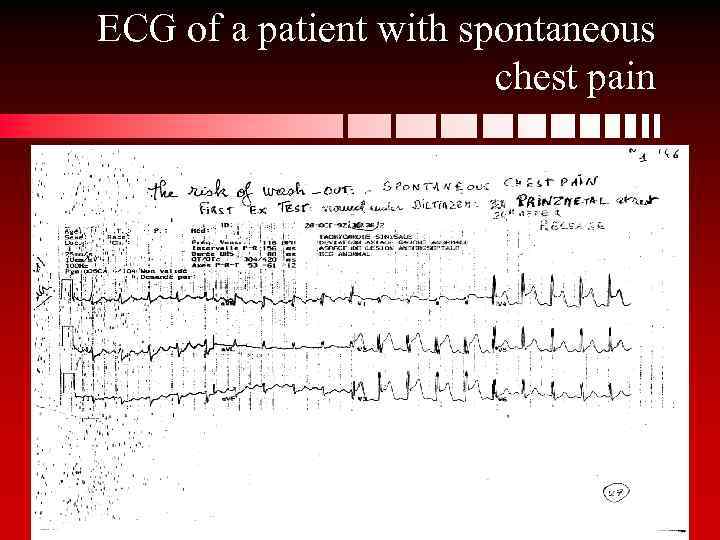 ECG of a patient with spontaneous chest pain
ECG of a patient with spontaneous chest pain
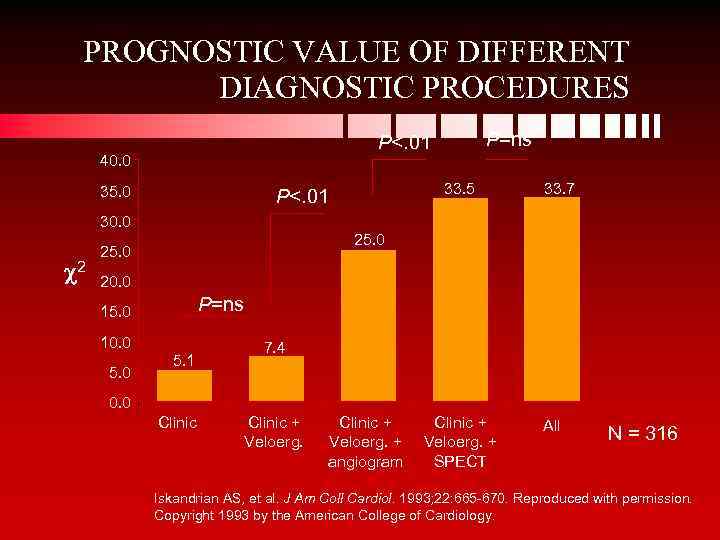 PROGNOSTIC VALUE OF DIFFERENT DIAGNOSTIC PROCEDURES P=ns P<. 01 40. 0 35. 0 33. 5 P<. 01 33. 7 30. 0 2 25. 0 20. 0 P=ns 15. 0 10. 0 5. 1 5. 0 7. 4 0. 0 Clinic NS=not significant Clinic + Veloerg. + angiogram Clinic + Veloerg. + SPECT All N = 316 Iskandrian AS, et al. J Am Coll Cardiol. 1993; 22: 665 -670. Reproduced with permission. Copyright 1993 by the American College of Cardiology.
PROGNOSTIC VALUE OF DIFFERENT DIAGNOSTIC PROCEDURES P=ns P<. 01 40. 0 35. 0 33. 5 P<. 01 33. 7 30. 0 2 25. 0 20. 0 P=ns 15. 0 10. 0 5. 1 5. 0 7. 4 0. 0 Clinic NS=not significant Clinic + Veloerg. + angiogram Clinic + Veloerg. + SPECT All N = 316 Iskandrian AS, et al. J Am Coll Cardiol. 1993; 22: 665 -670. Reproduced with permission. Copyright 1993 by the American College of Cardiology.
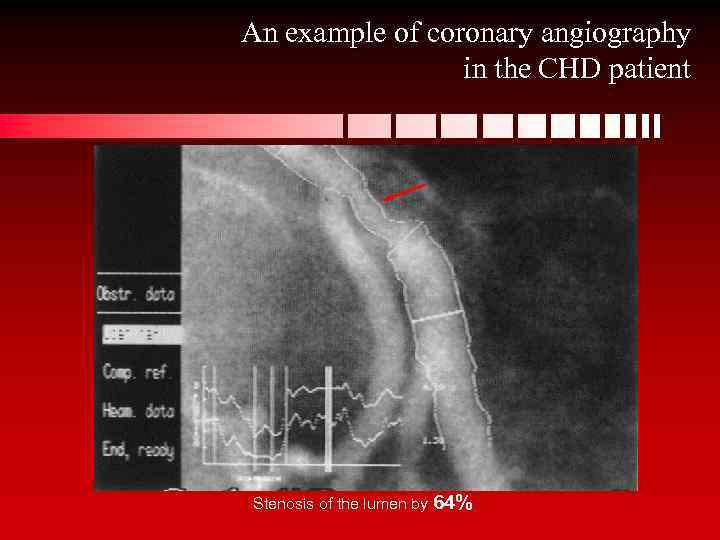 An example of coronary angiography in the CHD patient Stenosis of the lumen by 64%
An example of coronary angiography in the CHD patient Stenosis of the lumen by 64%
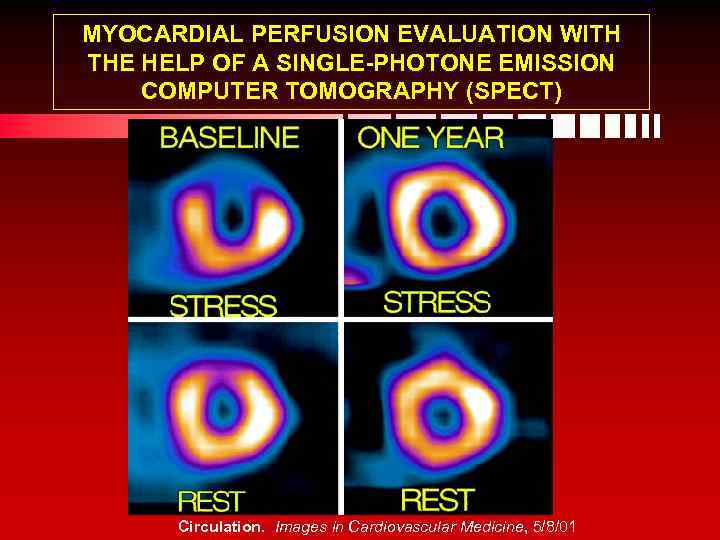 MYOCARDIAL PERFUSION EVALUATION WITH THE HELP OF A SINGLE-PHOTONE EMISSION COMPUTER TOMOGRAPHY (SPECT) Circulation. Images in Cardiovascular Medicine, 5/8/01
MYOCARDIAL PERFUSION EVALUATION WITH THE HELP OF A SINGLE-PHOTONE EMISSION COMPUTER TOMOGRAPHY (SPECT) Circulation. Images in Cardiovascular Medicine, 5/8/01
 IVUS
IVUS
 Stages of Atherosclerosis
Stages of Atherosclerosis
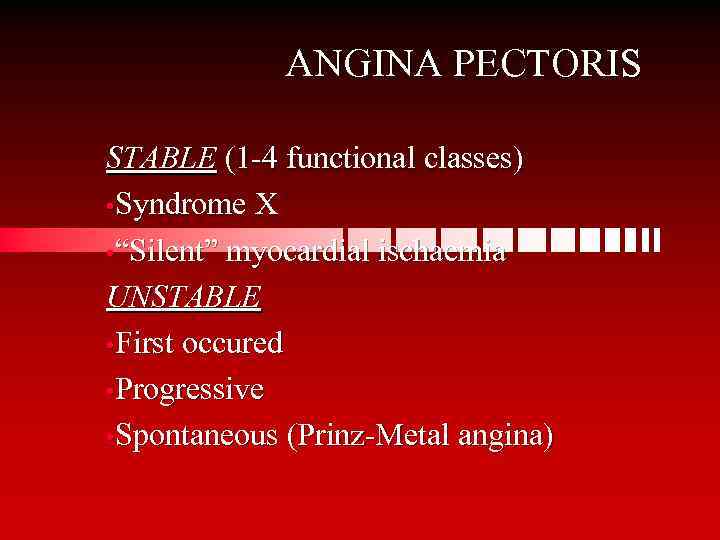 ANGINA PECTORIS STABLE (1 -4 functional classes) • Syndrome Х • “Silent” myocardial ischaemia UNSTABLE • First occured • Progressive • Spontaneous (Prinz-Metal angina)
ANGINA PECTORIS STABLE (1 -4 functional classes) • Syndrome Х • “Silent” myocardial ischaemia UNSTABLE • First occured • Progressive • Spontaneous (Prinz-Metal angina)
 Guidelines for the Identification of ACS Patients by ED Registration Clerks or Triage Nurses (ACC/AHA Practice Guidelines, 2002) Registration/Clerical Stuff Patients with the following chief complaints require immediate assessment by the triage nurse and should be referred for further evaluation Chief Complaint • Chest pain, pressure, tightness, or heaviness; pain that radiates to neck, jaw, shoulders, back, or 1 or both arms • Indigestion or “heartburn”; nausea and/or vomiting associated with chest discomfort • Persistent shortness of breath • Weakness, dizziness, lightheadedness, loss of consciousness
Guidelines for the Identification of ACS Patients by ED Registration Clerks or Triage Nurses (ACC/AHA Practice Guidelines, 2002) Registration/Clerical Stuff Patients with the following chief complaints require immediate assessment by the triage nurse and should be referred for further evaluation Chief Complaint • Chest pain, pressure, tightness, or heaviness; pain that radiates to neck, jaw, shoulders, back, or 1 or both arms • Indigestion or “heartburn”; nausea and/or vomiting associated with chest discomfort • Persistent shortness of breath • Weakness, dizziness, lightheadedness, loss of consciousness
 Guidelines for the Identification of ACS Patients by ED Registration Clerks or Triage Nurses (ACC/AHA Practice Guidelines, 2002) (2) Triage Nurse Patients with the following symptoms and signs require immediate assessement by the triage nurse for the initiation of the ACS protocol Chief Complaint Chest pain or severe epigastric pain, nontraumatic in origin, with components typical of myocardial ischemia or MI: Central/substernal compression or crushing chest pain Pressure, tightness, heaviness, cramping, burning, aching sensation Unexplained indigestion, belching, epigastric pain Radiating pain in neck, jaw, shoulders, back, or 1 or both arms • • • Associated dyspnea Associated nausea and/or vomiting Associated diaphoresis • If these symptoms are present, obtain stat ECG
Guidelines for the Identification of ACS Patients by ED Registration Clerks or Triage Nurses (ACC/AHA Practice Guidelines, 2002) (2) Triage Nurse Patients with the following symptoms and signs require immediate assessement by the triage nurse for the initiation of the ACS protocol Chief Complaint Chest pain or severe epigastric pain, nontraumatic in origin, with components typical of myocardial ischemia or MI: Central/substernal compression or crushing chest pain Pressure, tightness, heaviness, cramping, burning, aching sensation Unexplained indigestion, belching, epigastric pain Radiating pain in neck, jaw, shoulders, back, or 1 or both arms • • • Associated dyspnea Associated nausea and/or vomiting Associated diaphoresis • If these symptoms are present, obtain stat ECG
 Guidelines for the Identification of ACS Patients by ED Registration Clerks or Triage Nurses (ACC/AHA Practice Guidelines, 2002) (3) Medical History The triage nurse should take a brief, targeted, initial history with an assessment of current or past history of: • CABG, angioplasty, CAD, angina on effort, or MI • NTG use to relieve chest discomfort • Risk factors, including smoking, hyperlipidemia, hypertension, diabetes mellitus, family history, and cocaine use This brief history must not delay entry into the ACS protocol Special Considerations • • • Women may present more frequently than men with atypical chest pain and symptoms Diabetic patients may have atypical presentations due to autonomic dysfunction Elderly patients may have atypical symptoms such as generalized weakness, stroke, syncope, or a change in mental status
Guidelines for the Identification of ACS Patients by ED Registration Clerks or Triage Nurses (ACC/AHA Practice Guidelines, 2002) (3) Medical History The triage nurse should take a brief, targeted, initial history with an assessment of current or past history of: • CABG, angioplasty, CAD, angina on effort, or MI • NTG use to relieve chest discomfort • Risk factors, including smoking, hyperlipidemia, hypertension, diabetes mellitus, family history, and cocaine use This brief history must not delay entry into the ACS protocol Special Considerations • • • Women may present more frequently than men with atypical chest pain and symptoms Diabetic patients may have atypical presentations due to autonomic dysfunction Elderly patients may have atypical symptoms such as generalized weakness, stroke, syncope, or a change in mental status
 Myocardial Infarction • • With pathologic Q wave (transmural) Without Q wave (subendocardial, subepicardial, intramural) The degree of myocardial damage could be evaluated by CPK (myocardial fraction) activity 99 m. Tc pyrophosphate myocardial scintigraphy – a very sensitive marker of myocardial damage
Myocardial Infarction • • With pathologic Q wave (transmural) Without Q wave (subendocardial, subepicardial, intramural) The degree of myocardial damage could be evaluated by CPK (myocardial fraction) activity 99 m. Tc pyrophosphate myocardial scintigraphy – a very sensitive marker of myocardial damage
 NONANGINAL CHEST PAIN • • Different functional disturbances – the so -called cardiovascular syndrome of neurotic origin or neuro-circulatory dystonia with panic attacks Pericardium diseases Inflammatory myocardium diseases Myocardial dystrophy caused by anaemia, alcohol excess, lack of vitamins, thyrotoxicosis, hypothyroidism, etc.
NONANGINAL CHEST PAIN • • Different functional disturbances – the so -called cardiovascular syndrome of neurotic origin or neuro-circulatory dystonia with panic attacks Pericardium diseases Inflammatory myocardium diseases Myocardial dystrophy caused by anaemia, alcohol excess, lack of vitamins, thyrotoxicosis, hypothyroidism, etc.
 PERICARDITIS • • • Pericardium has no pain receptors, pain in pericarditis is usually caused by inflammatory damage of parietal pleura Localization of pain – chest, neck, abdomen Pain is similar to pleural: increases during deep inspiration, coughing, ingestion and horizontal position
PERICARDITIS • • • Pericardium has no pain receptors, pain in pericarditis is usually caused by inflammatory damage of parietal pleura Localization of pain – chest, neck, abdomen Pain is similar to pleural: increases during deep inspiration, coughing, ingestion and horizontal position
 CLINICAL FEATURES OF ACUTE PERICARDITIS • • • Chest pain differs from angina pectoris: increases during body movements, breathing, coughing Dyspnea Fever Pericardial murmur – the main symptom of acute pericarditis Symptoms of heart tamponade (X-ray, ECG, Echo)
CLINICAL FEATURES OF ACUTE PERICARDITIS • • • Chest pain differs from angina pectoris: increases during body movements, breathing, coughing Dyspnea Fever Pericardial murmur – the main symptom of acute pericarditis Symptoms of heart tamponade (X-ray, ECG, Echo)
 CLINICAL FEATURES OF ACUTE PERICARDITIS (2) • • • Increased leukocyte concentration and erythrocyte sedimentation rate ST segment elevation in leads I and II (without pathologic Q waves, QRS alternation) X-ray – does not reveal an increase of the heart size if the effusion amount is less than 250 ml
CLINICAL FEATURES OF ACUTE PERICARDITIS (2) • • • Increased leukocyte concentration and erythrocyte sedimentation rate ST segment elevation in leads I and II (without pathologic Q waves, QRS alternation) X-ray – does not reveal an increase of the heart size if the effusion amount is less than 250 ml
 DIAGNOSIS OF PERICARDITIS • • Character of pain, typical ECG changes, pericardial murmur Differential diagnosis should be made out with MI, pulmonary embolism and pain caused by pleura X-ray examination helps in diagnosis of pericarditis The best method of evaluation of pericardial effusion is Echo-cardiography
DIAGNOSIS OF PERICARDITIS • • Character of pain, typical ECG changes, pericardial murmur Differential diagnosis should be made out with MI, pulmonary embolism and pain caused by pleura X-ray examination helps in diagnosis of pericarditis The best method of evaluation of pericardial effusion is Echo-cardiography
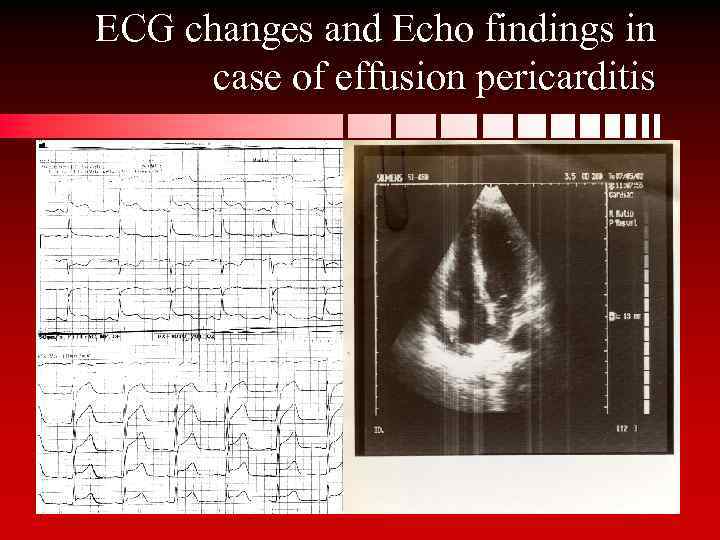 ECG changes and Echo findings in case of effusion pericarditis
ECG changes and Echo findings in case of effusion pericarditis
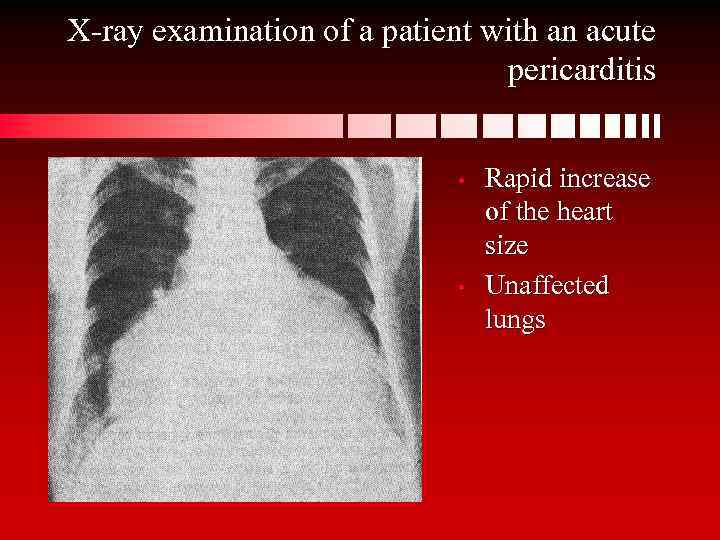 X-ray examination of a patient with an acute pericarditis • • Rapid increase of the heart size Unaffected lungs
X-ray examination of a patient with an acute pericarditis • • Rapid increase of the heart size Unaffected lungs
 DIAGNOSIS OF PERICARDITIS (2) • • • The onset of pericarditis caused by tuberculosis is often silent Immunological tests are often positive Bacteriological examination of effusion may help Positive results of specific antituberculosis therapy helps to reveal the etiology of the disease Etiology of viral, bacterial pericarditis, pericarditis caused by rheumatic fever, uremia, MI becomes clear when the main cause of the disease is revealed
DIAGNOSIS OF PERICARDITIS (2) • • • The onset of pericarditis caused by tuberculosis is often silent Immunological tests are often positive Bacteriological examination of effusion may help Positive results of specific antituberculosis therapy helps to reveal the etiology of the disease Etiology of viral, bacterial pericarditis, pericarditis caused by rheumatic fever, uremia, MI becomes clear when the main cause of the disease is revealed
 PAINS CAUSED BY PATHOLOGY OF MAGISTRAL ARTERIES • • • The of aorta aneurism dissection may cause no pain if it does not press neighboring tissues Pulmonary embolism often leads to an increase of pulmonary artery volume and as a result – to pericardial pain. Pulmonary infarction that damages pleura lead to pleural pain Primary pulmonary hypertension: pain is due to an increase of blood pressure in pulmonary artery (angina pulmonale)
PAINS CAUSED BY PATHOLOGY OF MAGISTRAL ARTERIES • • • The of aorta aneurism dissection may cause no pain if it does not press neighboring tissues Pulmonary embolism often leads to an increase of pulmonary artery volume and as a result – to pericardial pain. Pulmonary infarction that damages pleura lead to pleural pain Primary pulmonary hypertension: pain is due to an increase of blood pressure in pulmonary artery (angina pulmonale)
 CHEST PAIN CAUSED BY NONCARDIAC DISORDERS • • Pathology of bronchi, lungs or pleura (pneumonia, tumors, pleuritis) Diseases of spinal cord and chest wall muscles (osteochondrosis, Titze syndrome, scalenus syndrome, etc. Diseases of mediastinum (reflux-oesophagitis, tumors, mediastinitis) Pathology of abdomen (ulcer, cholelithiasis, oesophagal hernia, etc. )
CHEST PAIN CAUSED BY NONCARDIAC DISORDERS • • Pathology of bronchi, lungs or pleura (pneumonia, tumors, pleuritis) Diseases of spinal cord and chest wall muscles (osteochondrosis, Titze syndrome, scalenus syndrome, etc. Diseases of mediastinum (reflux-oesophagitis, tumors, mediastinitis) Pathology of abdomen (ulcer, cholelithiasis, oesophagal hernia, etc. )

