1 ASEPSIS AND ANTISEPSIS History of surgery

lecture-01-asepsis-antisepsis-operation.ppt
- Размер: 18.3 Mегабайта
- Количество слайдов: 50
Описание презентации 1 ASEPSIS AND ANTISEPSIS History of surgery по слайдам
 1 ASEPSIS AND ANTISEPSIS History of surgery Department Of Surgical Diseases Professor assistant, MD Gennady N. Gerasimov
1 ASEPSIS AND ANTISEPSIS History of surgery Department Of Surgical Diseases Professor assistant, MD Gennady N. Gerasimov
 2 Surgery • Is the branch of medicine, in which various mechanical or physical therapeutic manipulations are used
2 Surgery • Is the branch of medicine, in which various mechanical or physical therapeutic manipulations are used
 3 Surgery • The art or practice of treating injures deformities and other disorders by manual operation or instrumental appliances
3 Surgery • The art or practice of treating injures deformities and other disorders by manual operation or instrumental appliances
 4 The surgeon /from Clinical Surgery. Of Michael M. Henry London/ • Is one who makes people better chiefly by the exercise of manual skills / Operate first, questions later /. Surgeons have skills in management that go beyond mere manipulative ones and look after many patients who might possibly need an operation
4 The surgeon /from Clinical Surgery. Of Michael M. Henry London/ • Is one who makes people better chiefly by the exercise of manual skills / Operate first, questions later /. Surgeons have skills in management that go beyond mere manipulative ones and look after many patients who might possibly need an operation
 5 Operation?
5 Operation?
 6 Operation • Is a specific mechanic intervention upon a part of the body for diagnosis and treatment
6 Operation • Is a specific mechanic intervention upon a part of the body for diagnosis and treatment
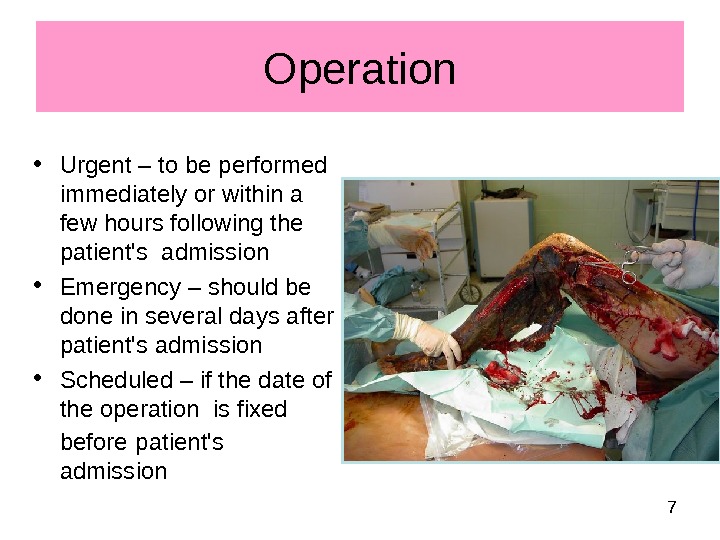
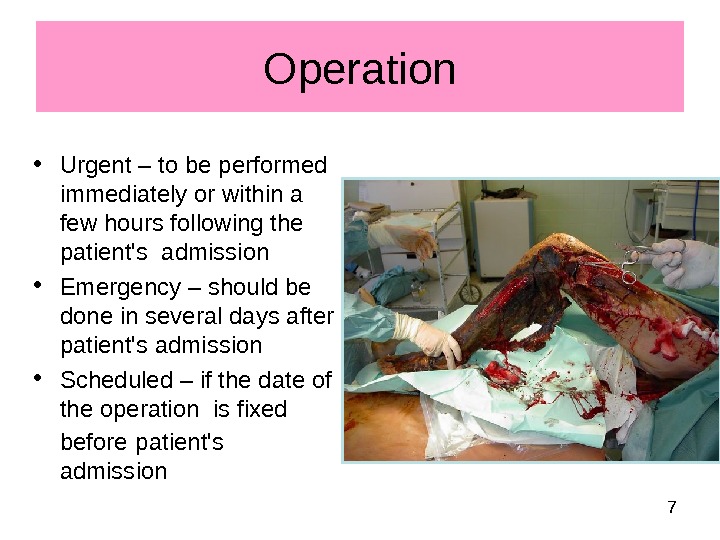 7 Operation • Urgent – to be performed immediately or within a few hours following the patient’s admission • Emergency – should be done in several days after patient’s admission • Scheduled – if the date of the operation is fixed before patient’s admission
7 Operation • Urgent – to be performed immediately or within a few hours following the patient’s admission • Emergency – should be done in several days after patient’s admission • Scheduled – if the date of the operation is fixed before patient’s admission
 8 Operation • Radical – removes the cause of diseases, or part of organ • Palliative – relieve symptoms of diseases
8 Operation • Radical – removes the cause of diseases, or part of organ • Palliative – relieve symptoms of diseases
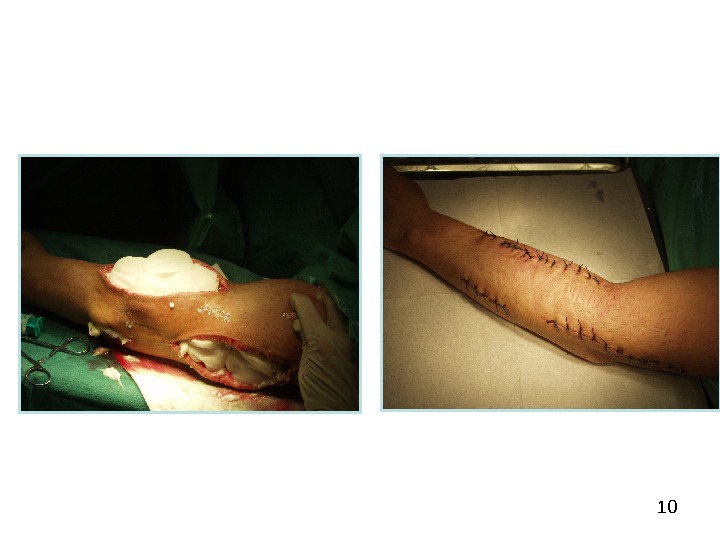
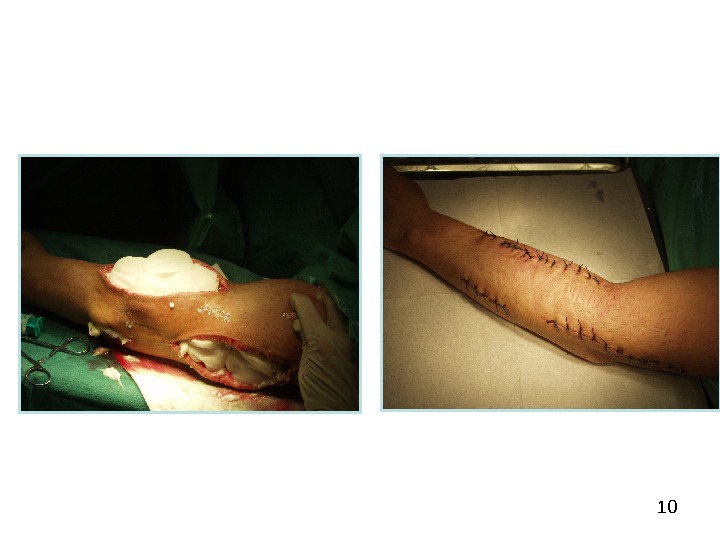
 9 • Consist of three steps : • Operative access • Primary step • Finishing the operation, suture of wound Operation
9 • Consist of three steps : • Operative access • Primary step • Finishing the operation, suture of wound Operation
 11 History of surgery asepsis
11 History of surgery asepsis
 12 Joseph Lister / 1827 – 1912 / • Made one of the great contributions to surgery by demonstrating that antisepsis could prevent infection. In march 1865 he began placing pure carbolic acid into wounds/ reduced concentration to 10, 5 and 2, 5 percent /. In 1867 he published his initial series of papers on antiepsis • In 1871 Lister began to use a carbolic acid spray to reduce contamination of the operating room atmosphere
12 Joseph Lister / 1827 – 1912 / • Made one of the great contributions to surgery by demonstrating that antisepsis could prevent infection. In march 1865 he began placing pure carbolic acid into wounds/ reduced concentration to 10, 5 and 2, 5 percent /. In 1867 he published his initial series of papers on antiepsis • In 1871 Lister began to use a carbolic acid spray to reduce contamination of the operating room atmosphere
 13 Ernst Bergman /1882/ • Aseptic sugery was not generally practiced. When asked what was new in surgery 1882, Ernst Bergman said, « Today we wash hands befor an operation»
13 Ernst Bergman /1882/ • Aseptic sugery was not generally practiced. When asked what was new in surgery 1882, Ernst Bergman said, « Today we wash hands befor an operation»
 141880 s -1890 s • Sterilization of instruments came into practice, first by chemicals and then by steam • Hand washing and the wearing of masks, caps, gowns and gloves were also introduced about this time • William Stewart Halsted (1852 -1922) introduced rubber gloves for his scrub nurse, Caroline Hampton, because mercuric chloride irritated her skin • Joseph Bloodgood introduced ther routine use by the entire operating t ea m
141880 s -1890 s • Sterilization of instruments came into practice, first by chemicals and then by steam • Hand washing and the wearing of masks, caps, gowns and gloves were also introduced about this time • William Stewart Halsted (1852 -1922) introduced rubber gloves for his scrub nurse, Caroline Hampton, because mercuric chloride irritated her skin • Joseph Bloodgood introduced ther routine use by the entire operating t ea m
 15 The introductuon of antibiotics • The discovery of penicillin was first reported by Alexander Fleming \ USA\ in 1928, it was not used clinically until administered by Howard Florey in the 1948 s. • In the Soviet Union antibiotics were introduced into clinical practice in the 1940`s by Z V Ermolaeva • Antibiotic therapy was a monumental advance inthe treatment of infections
15 The introductuon of antibiotics • The discovery of penicillin was first reported by Alexander Fleming \ USA\ in 1928, it was not used clinically until administered by Howard Florey in the 1948 s. • In the Soviet Union antibiotics were introduced into clinical practice in the 1940`s by Z V Ermolaeva • Antibiotic therapy was a monumental advance inthe treatment of infections
 16 ASEPSIS AND ANTISEPSIS
16 ASEPSIS AND ANTISEPSIS
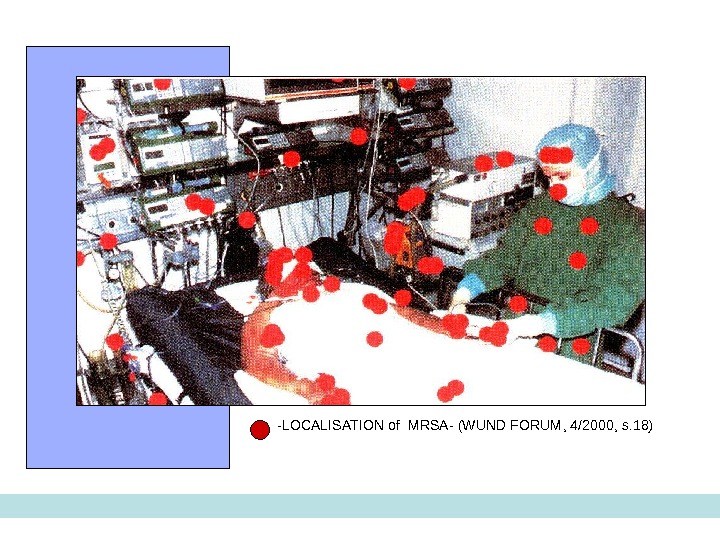
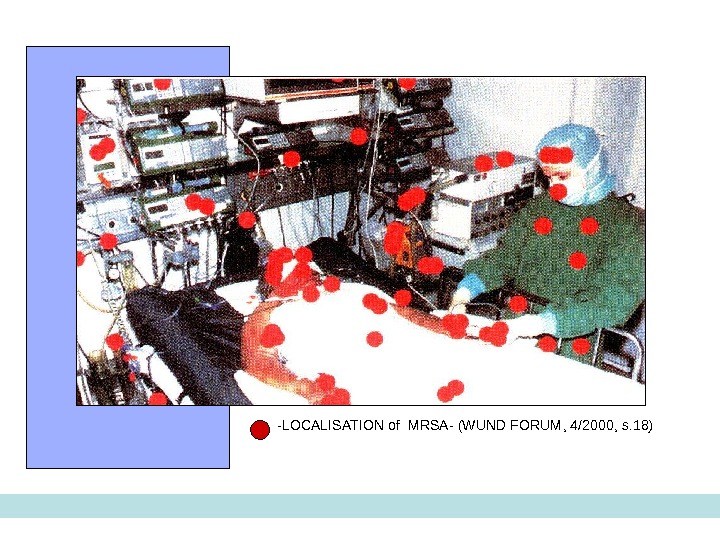 17 — LOCALISATION of MRSA — ( WUND FORUM , 4/2000, s. 18)
17 — LOCALISATION of MRSA — ( WUND FORUM , 4/2000, s. 18)
 18 Condition to make surgical operation • Asepsis — is preventing the infection of wounds and patients • Antisepsis – methods to combat bacterial infection in the wound, patient in surgical department
18 Condition to make surgical operation • Asepsis — is preventing the infection of wounds and patients • Antisepsis – methods to combat bacterial infection in the wound, patient in surgical department
 19 ASEPSIS is preventing the infection of wounds and patients • Nosocamial infection \ all KINDS OF SURGICAL INFECTION\ : 1 Exogenous infection 2 Endogenous infection
19 ASEPSIS is preventing the infection of wounds and patients • Nosocamial infection \ all KINDS OF SURGICAL INFECTION\ : 1 Exogenous infection 2 Endogenous infection
 20 BASE PRINCIPS OF ASEPSIS • ISOLATION • STERILISATION
20 BASE PRINCIPS OF ASEPSIS • ISOLATION • STERILISATION
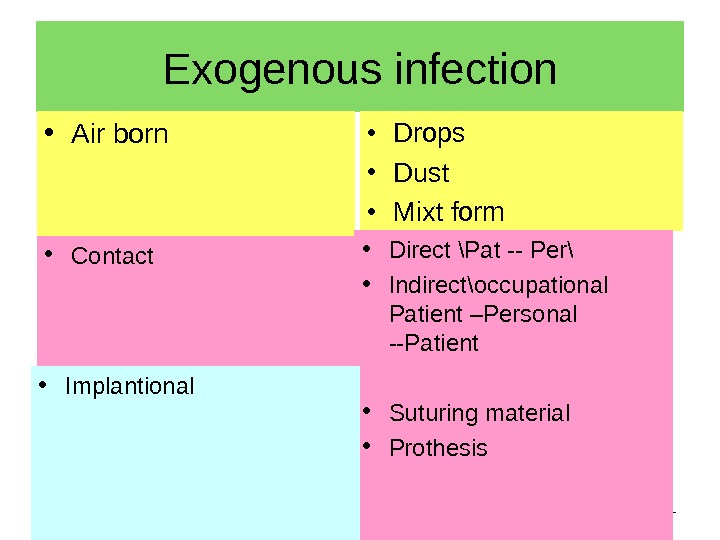
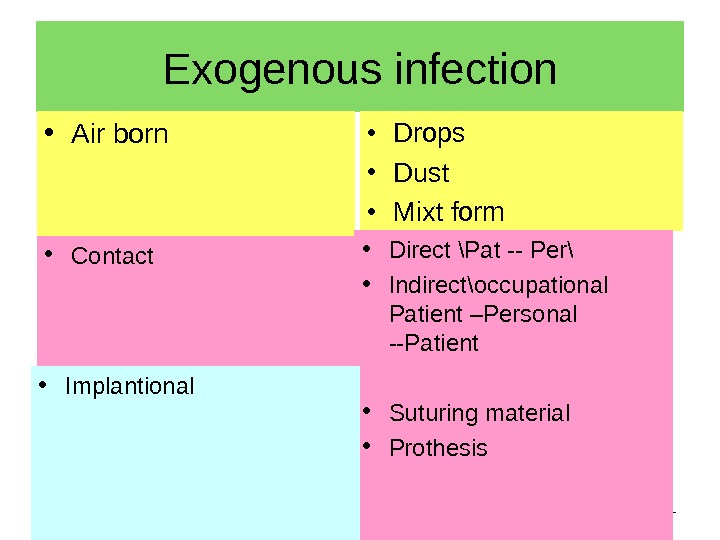 21 Exogenous infection • Air born • Drops • Dust • Mixt form • Direct \Pat — Per\ • Indirect \ occupational Patient –Personal —Patient • Suturing material • Prothesis • Contact • Implantional
21 Exogenous infection • Air born • Drops • Dust • Mixt form • Direct \Pat — Per\ • Indirect \ occupational Patient –Personal —Patient • Suturing material • Prothesis • Contact • Implantional
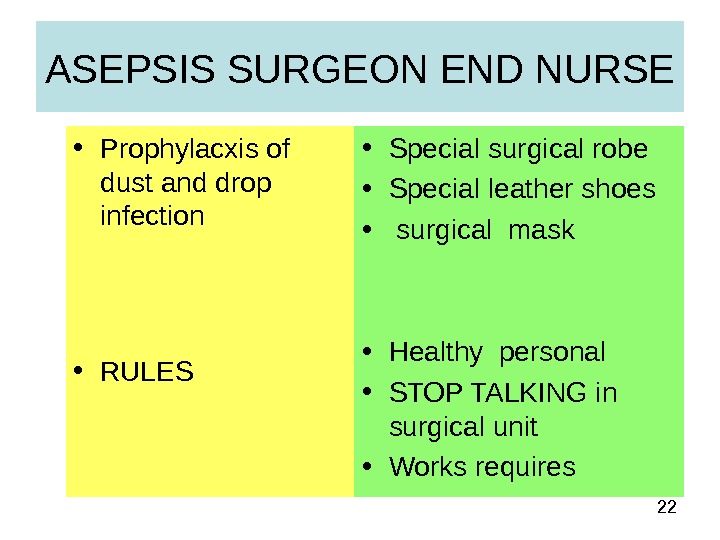
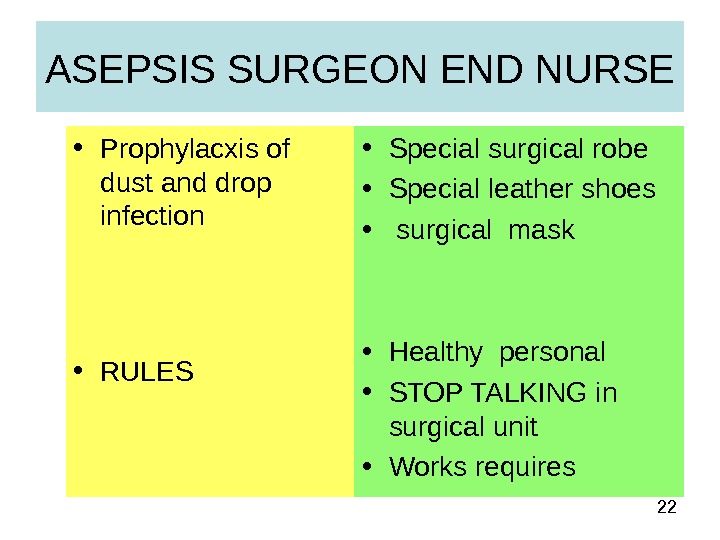 22 ASEPSIS SURGEON END NURSE • Prophylacxis of dust and drop infection • RULES • Special surgical robe • Special leather shoes • surgical mask • Healthy personal • STOP TALKING in surgical unit • Works requires
22 ASEPSIS SURGEON END NURSE • Prophylacxis of dust and drop infection • RULES • Special surgical robe • Special leather shoes • surgical mask • Healthy personal • STOP TALKING in surgical unit • Works requires
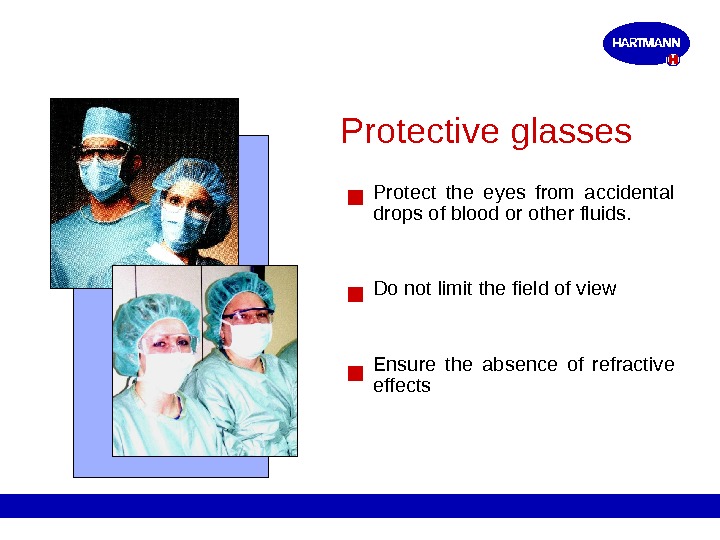
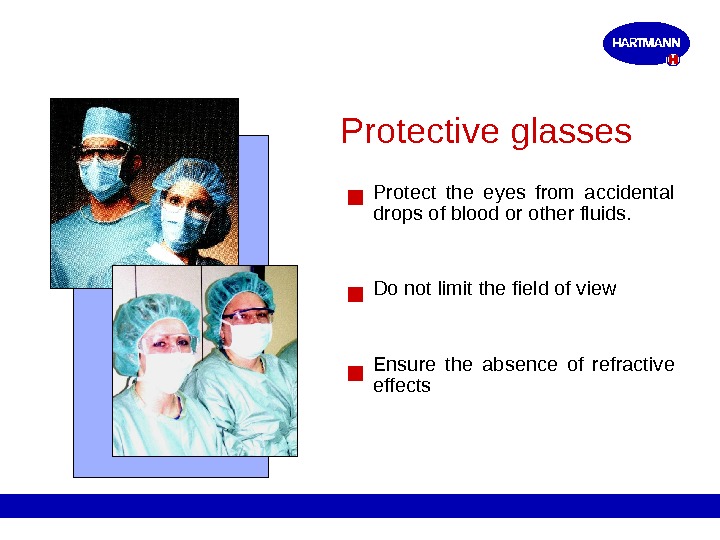 Protective glasses Protect the eyes from accidental drops of blood or other fluids. Do not limit the field of view Ensure the absence of refractive effects
Protective glasses Protect the eyes from accidental drops of blood or other fluids. Do not limit the field of view Ensure the absence of refractive effects
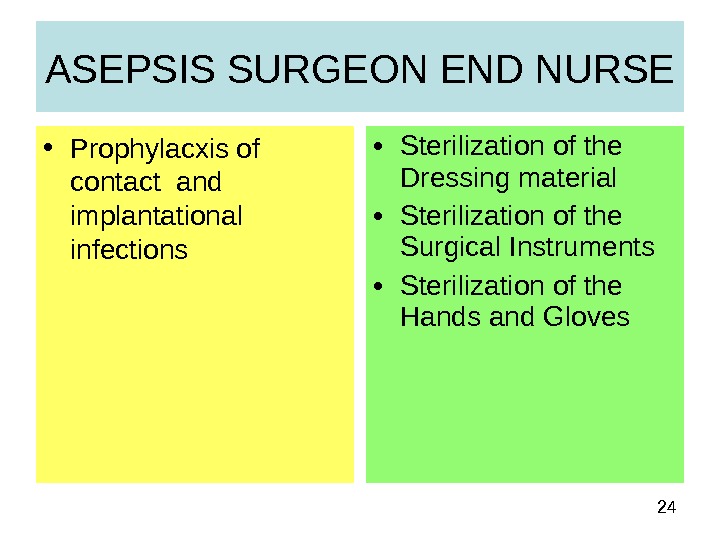
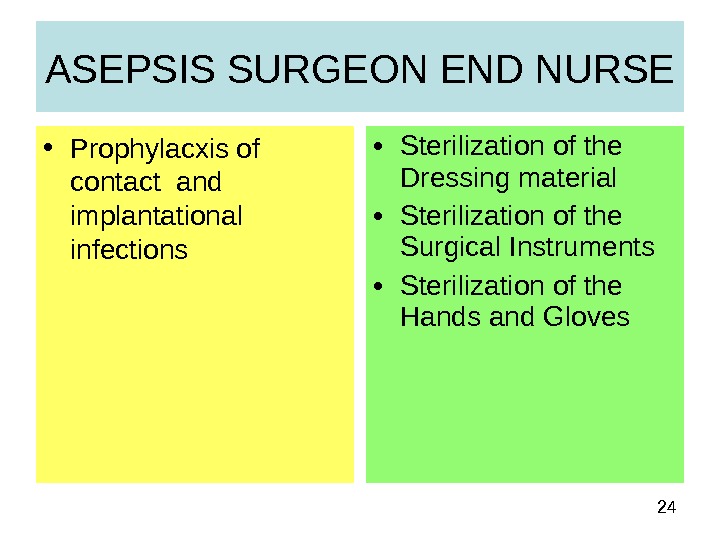 24 • Sterilization of the Dressing material • Sterilization of the Surgical Instruments • Sterilization of the Hands and Gloves. ASEPSIS SURGEON END NURSE • Prophylacxis of contact and implantational infections
24 • Sterilization of the Dressing material • Sterilization of the Surgical Instruments • Sterilization of the Hands and Gloves. ASEPSIS SURGEON END NURSE • Prophylacxis of contact and implantational infections
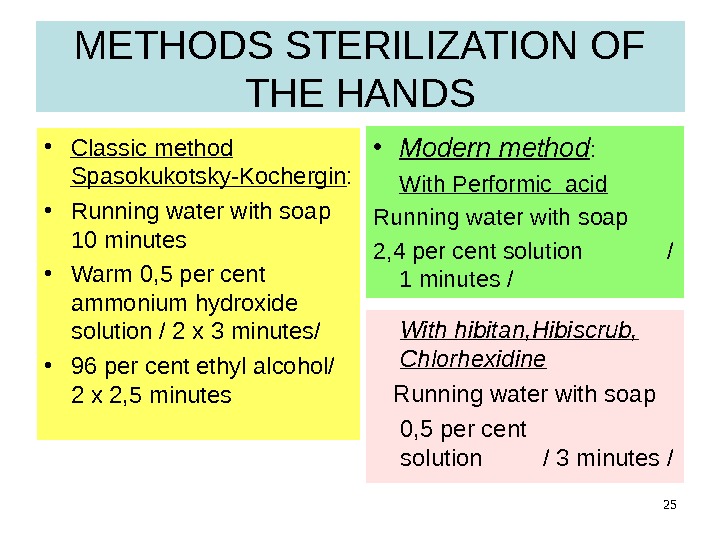
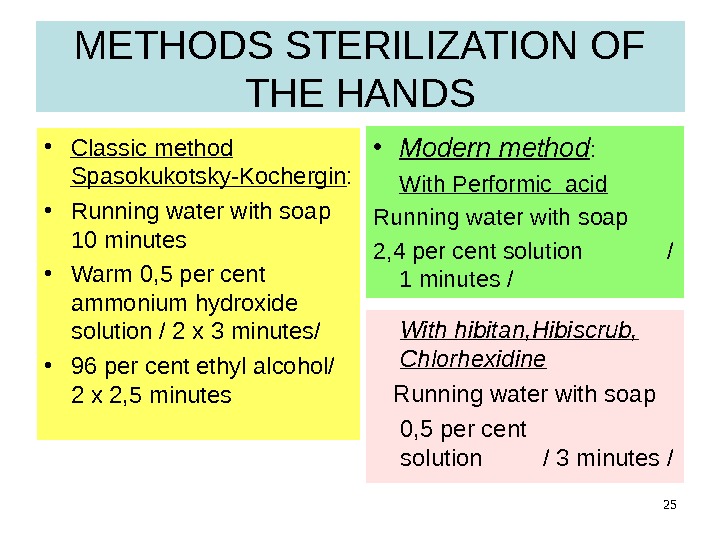 25 METHODS STERILIZATION OF THE HANDS • Classic method Spasokukotsky-Kochergin : • Running water with soap 10 minutes • Warm 0, 5 per cent ammonium hydroxide solution / 2 x 3 minutes/ • 96 per cent ethyl alcohol/ 2 x 2, 5 minutes • Modern method : With Performic acid Running water with soap 2, 4 per cent solution / 1 minutes / With hibitan, Hibiscrub, Chlorhexidine Running water with soap 0, 5 per cent solution / 3 minutes /
25 METHODS STERILIZATION OF THE HANDS • Classic method Spasokukotsky-Kochergin : • Running water with soap 10 minutes • Warm 0, 5 per cent ammonium hydroxide solution / 2 x 3 minutes/ • 96 per cent ethyl alcohol/ 2 x 2, 5 minutes • Modern method : With Performic acid Running water with soap 2, 4 per cent solution / 1 minutes / With hibitan, Hibiscrub, Chlorhexidine Running water with soap 0, 5 per cent solution / 3 minutes /
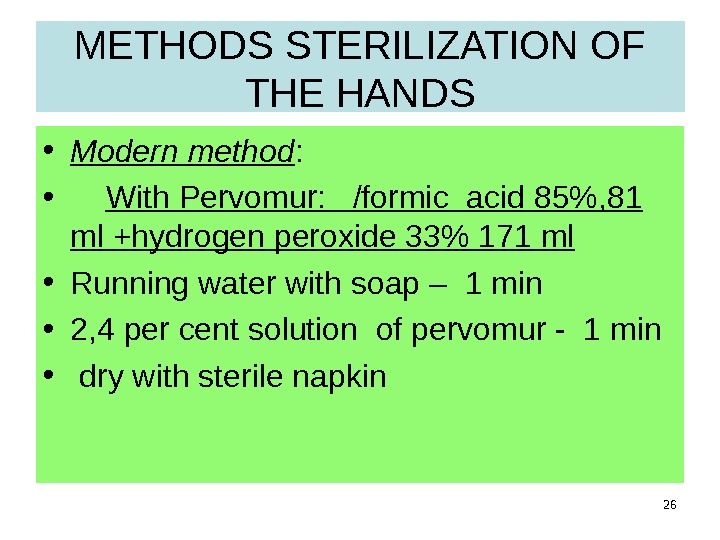 26 METHODS STERILIZATION OF THE HANDS • Modern method : • With Pervomur: /formic acid 85%, 81 ml +hydrogen peroxide 33% 171 ml • Running water with soap – 1 min • 2, 4 per cent solution of pervomur — 1 min • dry with sterile napkin
26 METHODS STERILIZATION OF THE HANDS • Modern method : • With Pervomur: /formic acid 85%, 81 ml +hydrogen peroxide 33% 171 ml • Running water with soap – 1 min • 2, 4 per cent solution of pervomur — 1 min • dry with sterile napkin
 27 METHODS STERILIZATION OF THE HANDS • With hibitan, Hibiscrub, Chlorhexidine — 0, 5% • Running water with soap- 1 min • 0, 5 per cent solution Hibiscrub, Chlorhexidine / 3 minutes /
27 METHODS STERILIZATION OF THE HANDS • With hibitan, Hibiscrub, Chlorhexidine — 0, 5% • Running water with soap- 1 min • 0, 5 per cent solution Hibiscrub, Chlorhexidine / 3 minutes /
 28 Mistakes of preparing hands
28 Mistakes of preparing hands
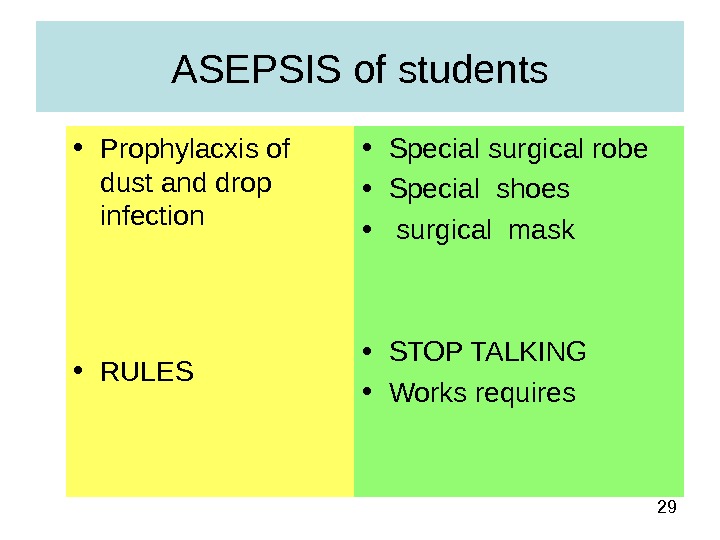 29 ASEPSIS of students • Prophylacxis of dust and drop infection • RULES • Special surgical robe • Special shoes • surgical mask • STOP TALKING • Works requires
29 ASEPSIS of students • Prophylacxis of dust and drop infection • RULES • Special surgical robe • Special shoes • surgical mask • STOP TALKING • Works requires
 30 Special requirements for students • Students can’t disturb medical personal and patient’s in surgical department • Students can’t speak loudly • Students can’t visit operation room and ward’s without teacher • All information about patient or operation is confidential
30 Special requirements for students • Students can’t disturb medical personal and patient’s in surgical department • Students can’t speak loudly • Students can’t visit operation room and ward’s without teacher • All information about patient or operation is confidential
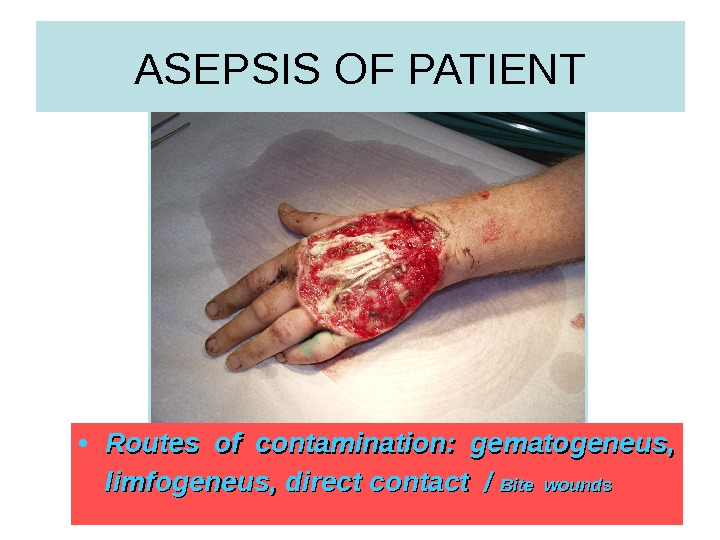
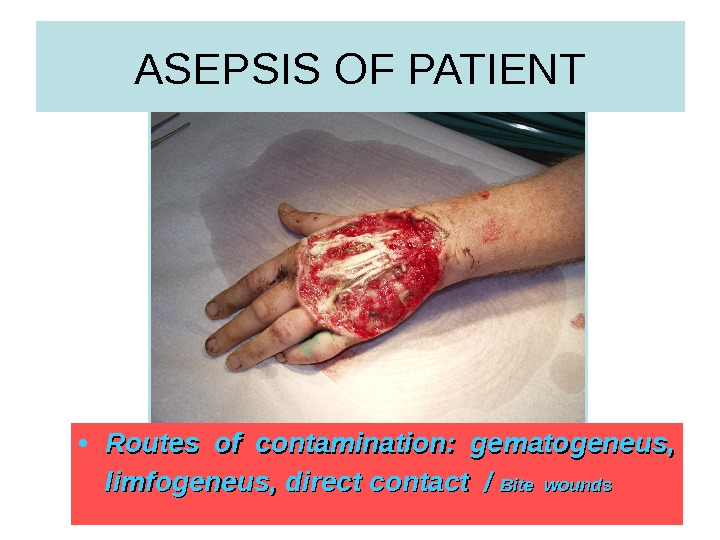 31 ASEPSIS OF PATIENT • Routes of contamination: gematogeneus, limfogeneus, direct contact / Bite wounds
31 ASEPSIS OF PATIENT • Routes of contamination: gematogeneus, limfogeneus, direct contact / Bite wounds
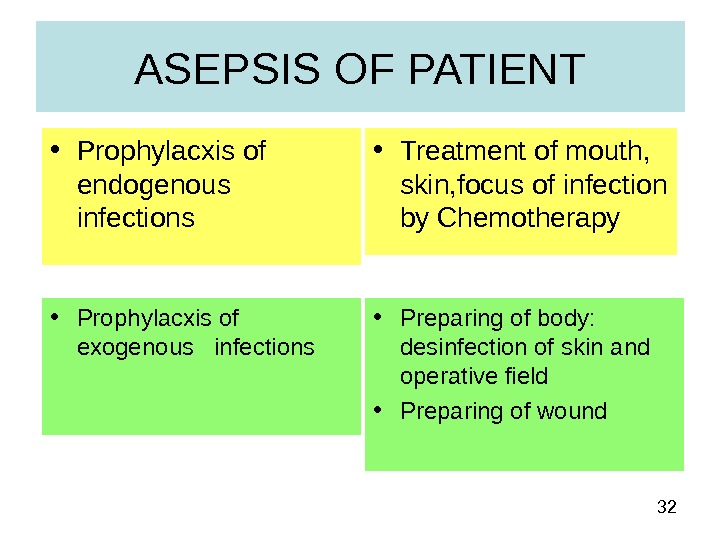 32 ASEPSIS OF PATIENT • Prophylacxis of endogenous infections • Treatment of mouth, skin, focus of infection by Chemotherapy • Prophylacxis of exogenous infections • Preparing of body: desinfection of skin and operative field • Preparing of wound
32 ASEPSIS OF PATIENT • Prophylacxis of endogenous infections • Treatment of mouth, skin, focus of infection by Chemotherapy • Prophylacxis of exogenous infections • Preparing of body: desinfection of skin and operative field • Preparing of wound
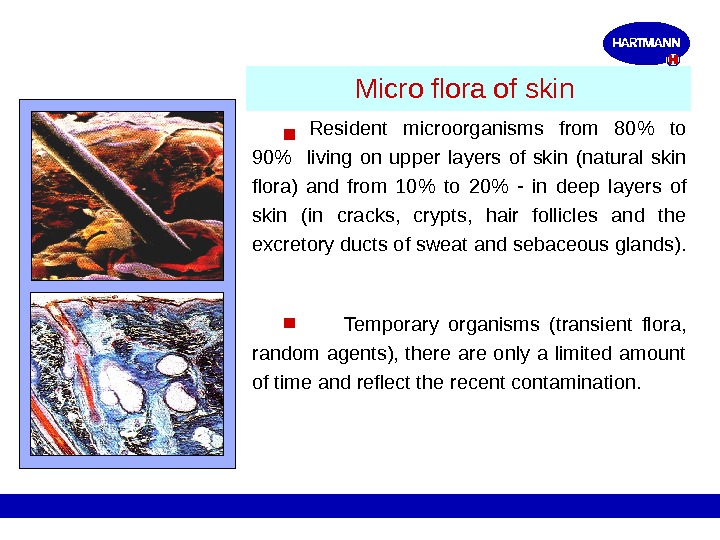
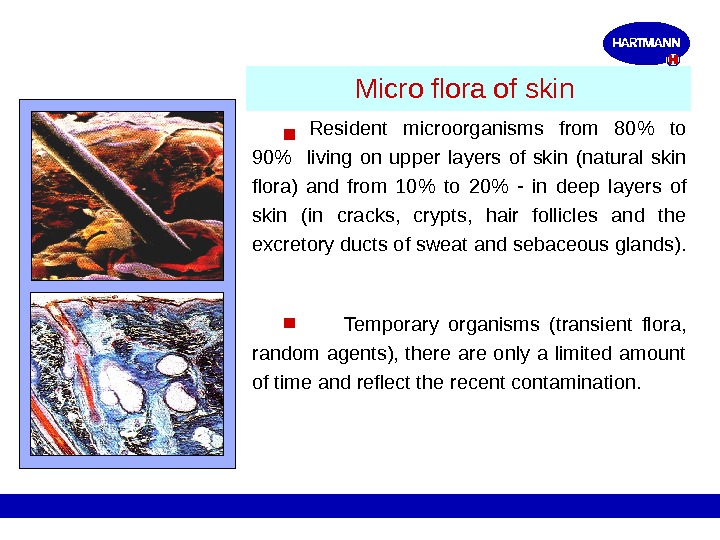 Micro flora of skin Resident microorganisms from 80% to 90% living on upper layers of skin (natural skin flora) and from 10% to 20% — in deep layers of skin ( in cracks, crypts, hair follicles and the excretory ducts of sweat and sebaceous glands ). Temporary organisms (transient flora, random agents), there are only a limited amount of time and reflect the recent contamination.
Micro flora of skin Resident microorganisms from 80% to 90% living on upper layers of skin (natural skin flora) and from 10% to 20% — in deep layers of skin ( in cracks, crypts, hair follicles and the excretory ducts of sweat and sebaceous glands ). Temporary organisms (transient flora, random agents), there are only a limited amount of time and reflect the recent contamination.
 IODONATE, povidon-iod • 1 per cent solution for desinfection the OPERATIVE FIELD, DRESSINGS
IODONATE, povidon-iod • 1 per cent solution for desinfection the OPERATIVE FIELD, DRESSINGS
 HYDROGEN PEROXID SOLUTION • 3 PER CENT SOLUTION FOR SKIN, WOUNDS , MUCOUS MEMBRANES
HYDROGEN PEROXID SOLUTION • 3 PER CENT SOLUTION FOR SKIN, WOUNDS , MUCOUS MEMBRANES
 ANTISEPSIS KINDS OF ANTISEPSIS
ANTISEPSIS KINDS OF ANTISEPSIS
 BIOLOGICAL ANTISEPSIS • ANTIBIOTICS • PROTEOLYTIC ENZYMES • VACCINE • HYPERIMMUNE SERUM • IMMUNOGLOBULINS • IMMUNOSTIMULATORS
BIOLOGICAL ANTISEPSIS • ANTIBIOTICS • PROTEOLYTIC ENZYMES • VACCINE • HYPERIMMUNE SERUM • IMMUNOGLOBULINS • IMMUNOSTIMULATORS
 Pathogenic microorganisms of surgical infections • gram positive and gram negative • Aerobic and anaerobic
Pathogenic microorganisms of surgical infections • gram positive and gram negative • Aerobic and anaerobic
 Pathogenic microorganisms • Gram-positive cocci / one of major causative organisms of surgical infections/: staphylococci, streptococci, enterococci, pnrumococci • Gram-positive class / are less important in surgery /: mycobacteria, spirochete, leptospira • Gram-positive anaerobic cocci – peptostreptococci • Gram-positive anaerobic class – clostridium, bifidobacteri
Pathogenic microorganisms • Gram-positive cocci / one of major causative organisms of surgical infections/: staphylococci, streptococci, enterococci, pnrumococci • Gram-positive class / are less important in surgery /: mycobacteria, spirochete, leptospira • Gram-positive anaerobic cocci – peptostreptococci • Gram-positive anaerobic class – clostridium, bifidobacteri
 Pathogenic microorganisms • Gram-negative cocci: actinobacter, neisseria • Gram- negative class / often causative organisms of a surgical infections/: E. coli and pseudomonas, klebsiella, enterobacter, salmonella, Helicobacter pylory • Gram-negative anaerobic coccuses — beilonella • Gram-negative anaerobic class – bacteroids, fusobactery
Pathogenic microorganisms • Gram-negative cocci: actinobacter, neisseria • Gram- negative class / often causative organisms of a surgical infections/: E. coli and pseudomonas, klebsiella, enterobacter, salmonella, Helicobacter pylory • Gram-negative anaerobic coccuses — beilonella • Gram-negative anaerobic class – bacteroids, fusobactery
 Pathogenic microorganisms • Sensitivity to a drug – is the inhibition growth of microorganism in therapeutic concentrations of antibiotics • Resistance – is the preservation of growth’s ability microorganism in therapeutic concentrations of antibiotics: primary/ before treatment with drug/ or secondary/after treatment with drug/
Pathogenic microorganisms • Sensitivity to a drug – is the inhibition growth of microorganism in therapeutic concentrations of antibiotics • Resistance – is the preservation of growth’s ability microorganism in therapeutic concentrations of antibiotics: primary/ before treatment with drug/ or secondary/after treatment with drug/
 ANTIBIOTICS • Penicillins: Natural penicillines / benzylpenicilline, bicilline, phenoxymethylpenicilline Antistaphyloccoal – oxacilline, dicloxacine / are active against G+: staphyloccocal infections – pneumonia, lung abscess, osteomyelitis, abscess and phlegmon of soft tissues • Aminopenicillines – ampicilline, amoxycilline combined – ampiox / ampicilline + oxacilline antipseudomonas – carboxypenicilines, aslocilline protected from lactamase – amoxyclav, tasocine / are effective against G-: pseudomonas, proteus – burns, peritonitis
ANTIBIOTICS • Penicillins: Natural penicillines / benzylpenicilline, bicilline, phenoxymethylpenicilline Antistaphyloccoal – oxacilline, dicloxacine / are active against G+: staphyloccocal infections – pneumonia, lung abscess, osteomyelitis, abscess and phlegmon of soft tissues • Aminopenicillines – ampicilline, amoxycilline combined – ampiox / ampicilline + oxacilline antipseudomonas – carboxypenicilines, aslocilline protected from lactamase – amoxyclav, tasocine / are effective against G-: pseudomonas, proteus – burns, peritonitis
 • Cephalosporins • 1 generation/ cefalexinum/ G-, not lactomase activity • 2 generation – cephaloridin, kefsol/ are stable to lactomase, spectrum – G+ and G- microorganisms • 3 generation – cefotaxim, cefaperazon are stable to lactomase, spectrum – G- microorganisms, anaerobic microorganism • 4 generation – cefepin, cefperoson are stable to lactomase, spectrum – G+ and G- microorganisms, anaerobic microorganisms ANTIBIOTICS
• Cephalosporins • 1 generation/ cefalexinum/ G-, not lactomase activity • 2 generation – cephaloridin, kefsol/ are stable to lactomase, spectrum – G+ and G- microorganisms • 3 generation – cefotaxim, cefaperazon are stable to lactomase, spectrum – G- microorganisms, anaerobic microorganism • 4 generation – cefepin, cefperoson are stable to lactomase, spectrum – G+ and G- microorganisms, anaerobic microorganisms ANTIBIOTICS
 • Aminoglycosides –gentamicin, kanamycin, amikacin/ have broad spectrum against G+, G- and anaerobic microorganism • Tetracyclines – tetracycline, rondomicin, vibramicin have broad spectrum against G+, G- and anaerobic microorganism • Macrolides – erytromycin, oleandomycin, azitromycin/ G+, helicobacter • Fluorquinolones – ofloxacin, pefloxacin have broad spectrum against G+, G- and anaerobic microorganism/ E. coli, enterobacteriaceae, klebsiella ANTIBIOTICS
• Aminoglycosides –gentamicin, kanamycin, amikacin/ have broad spectrum against G+, G- and anaerobic microorganism • Tetracyclines – tetracycline, rondomicin, vibramicin have broad spectrum against G+, G- and anaerobic microorganism • Macrolides – erytromycin, oleandomycin, azitromycin/ G+, helicobacter • Fluorquinolones – ofloxacin, pefloxacin have broad spectrum against G+, G- and anaerobic microorganism/ E. coli, enterobacteriaceae, klebsiella ANTIBIOTICS
 Routes of contamination • Peroral \only in mild infection • Intramuscular \ in most surgical infections • Itravenous \ to achieve high concentration in the blood • Intraarterial \ to achieve high concentration in the blood + short time • Local application
Routes of contamination • Peroral \only in mild infection • Intramuscular \ in most surgical infections • Itravenous \ to achieve high concentration in the blood • Intraarterial \ to achieve high concentration in the blood + short time • Local application
 Biologic antiseptic compounds • Proteolytic enzymes can lyse necrotic tissues. Usually used proteolytic enzymes of animal origin are trypsin, chymotypsin, ribonuclease; • those of bacterial origin – terrilitin, streptokinase, collagenase, asperase, ribonuclease, iruxol; • plant origin- papain and bromelain.
Biologic antiseptic compounds • Proteolytic enzymes can lyse necrotic tissues. Usually used proteolytic enzymes of animal origin are trypsin, chymotypsin, ribonuclease; • those of bacterial origin – terrilitin, streptokinase, collagenase, asperase, ribonuclease, iruxol; • plant origin- papain and bromelain.
 IMMUNE STIMULATORS • Improve non-specific immune defence • Prodigiosan \ dificit B lymphocytes\ • Levamisol \ dificit T lymphocytes\
IMMUNE STIMULATORS • Improve non-specific immune defence • Prodigiosan \ dificit B lymphocytes\ • Levamisol \ dificit T lymphocytes\
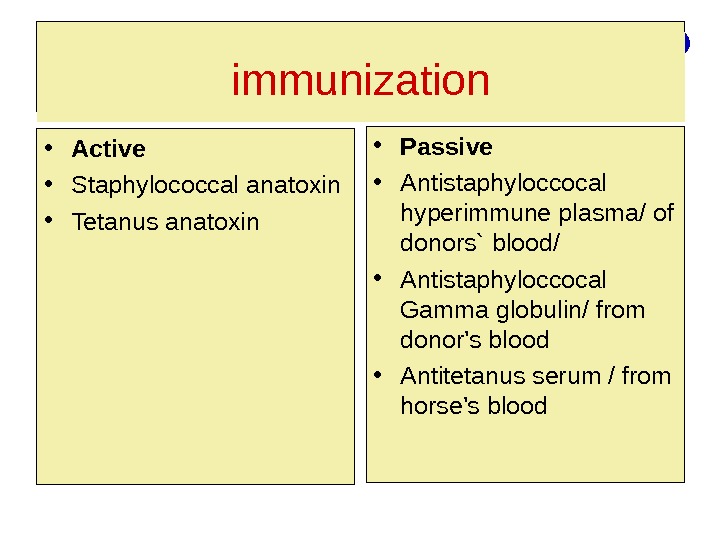 IMMUNIZATION • Active • Staphylococcal anatoxin • Tetanus anatoxin • Passive • Antistaphyloccocal hyperimmune plasma/ of donors` blood/ • Antistaphyloccocal Gamma globulin/ from donor’s blood • Antitetanus serum / from horse’s bloodimmunization
IMMUNIZATION • Active • Staphylococcal anatoxin • Tetanus anatoxin • Passive • Antistaphyloccocal hyperimmune plasma/ of donors` blood/ • Antistaphyloccocal Gamma globulin/ from donor’s blood • Antitetanus serum / from horse’s bloodimmunization
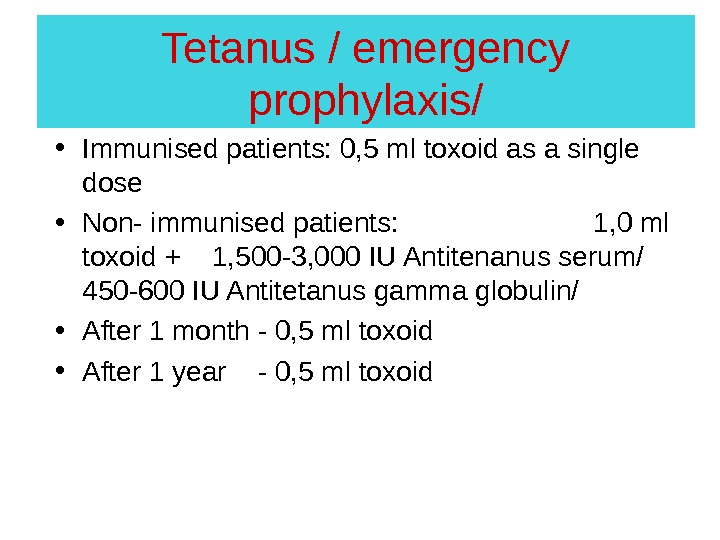
 Tetanus / emergency prophylaxis/ • Immunised patients: 0, 5 ml toxoid as a single dose • Non- immunised patients: 1, 0 ml toxoid + 1, 500 -3, 000 IU Antitenanus serum/ 450 -600 IU Antitetanus gamma globulin/ • After 1 month — 0, 5 ml toxoid • After 1 year — 0, 5 ml toxoid
Tetanus / emergency prophylaxis/ • Immunised patients: 0, 5 ml toxoid as a single dose • Non- immunised patients: 1, 0 ml toxoid + 1, 500 -3, 000 IU Antitenanus serum/ 450 -600 IU Antitetanus gamma globulin/ • After 1 month — 0, 5 ml toxoid • After 1 year — 0, 5 ml toxoid
 Tetanus • Specific tetanus prophylaxis: 0, 5 ml of toxoid are given twice a month REVACCINATION is done after 1 year — 0, 5 ml of toxoid • Repeaded REVACCINATION after 5 years — 0, 5 ml toxoid`
Tetanus • Specific tetanus prophylaxis: 0, 5 ml of toxoid are given twice a month REVACCINATION is done after 1 year — 0, 5 ml of toxoid • Repeaded REVACCINATION after 5 years — 0, 5 ml toxoid`
